A Comprehensive Guide to In Vitro Immunogenicity Assessment for Peptide-Based Vaccines
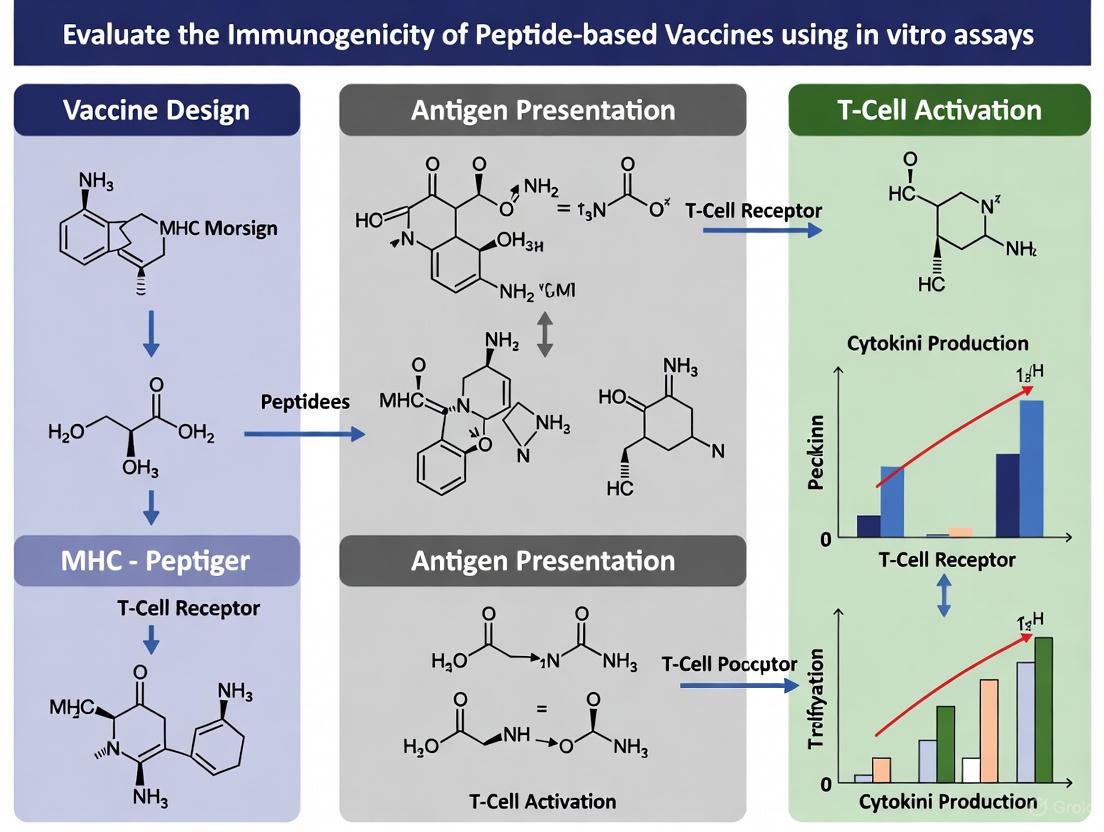
This article provides a systematic framework for researchers and drug development professionals to evaluate the immunogenicity of peptide-based vaccines using in vitro assays.
A Comprehensive Guide to In Vitro Immunogenicity Assessment for Peptide-Based Vaccines
Abstract
This article provides a systematic framework for researchers and drug development professionals to evaluate the immunogenicity of peptide-based vaccines using in vitro assays. It covers the foundational principles of immune responses to peptides, details core methodologies like ELISpot and MHC-binding assays, addresses common challenges in assay optimization and specificity, and outlines strategies for validating results and comparing vaccine candidates. By integrating current regulatory perspectives with advanced technological approaches such as high-throughput immunoarrays and nanoparticle delivery systems, this guide serves as a critical resource for de-risking vaccine development and accelerating the translation of preclinical findings to clinical applications.
Understanding Immunogenicity: Peptide Characteristics and Immune Activation Pathways
In the development of peptide-based therapeutics and vaccines, predicting and controlling immunogenicity is a paramount challenge. Unwanted immune responses can compromise drug efficacy and patient safety, as seen with the investigational drug Taspoglutide, where immunogenicity led to hypersensitivity and injection site reactions, potentially halting its development [1]. The immunogenic potential of a peptide product is not dictated by a single factor but arises from the complex interplay of three core drivers: its origin (whether self or non-self), its amino acid sequence (and resultant structure), and its aggregation potential [2] [3]. For researchers using in vitro assays to evaluate risk, a deep understanding of these drivers and their measurement is essential. This guide provides a comparative overview of these key immunogenic drivers, supported by experimental data and methodologies relevant for preclinical assessment.
Peptide Origin: Self, Non-Self, and Modified
The biological origin of a peptide antigen fundamentally shapes its immunogenic profile by determining the pre-existing state of host immune tolerance.
Comparative Immunogenicity of Antigen Types
Table 1: Comparison of Peptide Antigen Types by Origin
| Antigen Type | Origin & Description | Key Example | Immunogenic Potential | Primary Immune Response | Considerations for Vaccine Design |
|---|---|---|---|---|---|
| Tumor-Associated Antigens (TAAs) | Self-antigens overexpressed on cancer cells (e.g., tissue-specific, germline antigens) | HER2/Neu, gp100, WT1 [3] | Low to Moderate | CD8+ T cells; CD4+ T cells [3] | Limited by central T-cell tolerance; risk of autoimmunity [3] |
| Tumor-Specific Antigens (TSAs) | Non-self antigens unique to tumor cells due to somatic mutations | Neoantigens from KRAS, TP53 [3] | High | CD8+ T cells; CD4+ T cells [3] | Bypasses central tolerance; ideal for personalized vaccines [3] |
| Viral Antigens | Foreign proteins from oncogenic viruses | EBV LMP1/LMP2, HPV E6/E7 [3] | High | CD8+ T cells; CD4+ T cells [3] | Not subject to self-tolerance; strong, specific T-cell responses [3] |
| Fusion Junction Neopeptides | Novel sequences from chimeric RNAs in cancer | KIF5B-RET fusion protein [4] | High | CD8+ T cells [4] | Tumor-specific with low cross-reactivity to normal tissues [4] |
Experimental Analysis of Origin and Immunogenicity
The immunogenicity of non-self origins is clearly demonstrated in studies on fusion neopeptides. Research on the KIF5B-RET fusion junction identified specific 9-mer peptides (e.g., NNDVKEDPK) with high affinity for HLA-C*07:02. In vitro ELISpot assays using HLA-matched donor PBMCs showed that CD8+ T cells from multiple donors responded to these junction peptides, confirming their immunogenic potential. Single-cell RNA sequencing of activated T cells further identified 15 distinct TCR clonotypes, underscoring the ability of these novel sequences to drive a robust and diverse T-cell response [4].
Peptide Sequence and Structure
The amino acid sequence is a primary determinant of immunogenicity, as it dictates both the peptide's affinity for HLA molecules and its potential for chemical degradation.
Sequence-Based Immunogenicity Drivers
- T-cell Epitope Content: The presence of sequences that can bind to HLA class I or II molecules is a prerequisite for T-cell dependent immunogenicity. Impurities in generic peptide drugs that introduce novel HLA-binding sequences not found in the reference product can drive new, unwanted adaptive immune responses [1].
- Amino Acid Substitutions: Specific mutations can significantly enhance HLA-binding. Research on SARS-CoV-2 variants revealed that C>U mutations, which often result in amino acid substitutions like Threonine>Isoleucine (T>I) and Alanine>Valine (A>V), generally increase peptide binding to common HLA-I alleles. This enhanced binding is driven by an increase in peptide hydrophobicity, a property favored by many HLA molecules [5].
- Post-Translational Modifications (PTMs): Deamidation, oxidation, and racemization are common PTMs that can occur during manufacturing or storage. These modifications can alter the peptide's structure and create novel epitopes. For instance, software algorithms can sometimes misassign deamidation sites based on MS/MS data, leading to incorrect sequence confirmation and an incomplete understanding of potential immunogenic variants [6].
Experimental Protocol: In Silico Immunogenicity Risk Assessment
A critical first step in sequence analysis is computational screening.
- Objective: To computationally predict the potential of a peptide sequence (API or impurity) to contain T-cell epitopes.
- Method:
- Input: FASTA format sequences of the peptide drug and any known impurities.
- Analysis: Utilize a panel of in silico T cell epitope prediction tools (e.g., NetMHCpan-4.0) to predict binding affinity to a suite of common HLA class I and class II alleles [5] [1].
- Output: Peptides are ranked based on predicted binding affinity (e.g., IC50 values). Impurities are flagged if they contain novel, strong HLA-binding sequences not present in the API or Reference Listed Drug (RLD) [1].
- Application: This orthogonal method is recommended by FDA guidelines for ANDA submissions of generic peptides to evaluate the risk posed by impurities present at 0.1-0.5% of the API [1].
Figure 1: Workflow for In Silico Immunogenicity Risk Assessment. This diagram outlines the computational process for predicting T-cell epitopes in peptide sequences, a key step in evaluating sequence-based immunogenic risk.
Peptide Aggregation and Impurities
Product-related factors such as aggregation and impurities are critical modulators of immunogenicity, capable of converting a otherwise low-risk peptide into a highly immunogenic one.
The Role of Aggregates and Impurities
- Enhancing Innate Immune Activation: Peptide aggregates can act as danger signals, stimulating the innate immune system and creating an inflammatory environment that promotes the breaking of immune tolerance to the peptide drug itself [2] [1].
- Introducing Novel Epitopes: The process of aggregation can expose buried hydrophobic regions or promote chemical degradation (e.g., deamidation, oxidation), leading to the formation of new epitopes [2]. Furthermore, impurities arising from incomplete synthesis (e.g., deletion sequences, truncated products) or side-chain modifications can contain entirely new HLA-binding sequences [1].
Experimental Protocol: MHC-Associated Peptide Proteomics (MAPPs) Assay
To experimentally evaluate how peptide products are processed and presented by antigen-presenting cells (APCs), the MAPPs assay is employed.
- Objective: To identify peptides derived from a therapeutic protein or vaccine that are actually processed and presented on the surface of APCs by HLA-II molecules.
- Method:
- Step 1: Differentiate human monocyte-derived dendritic cells (moDCs) from naive donors.
- Step 2: Pulse the moDCs with the peptide product of interest.
- Step 3: Lyse the cells and immunoaffinity-purify HLA-II/peptide complexes.
- Step 4: Elute and analyze the bound peptides via liquid chromatography-mass spectrometry (LC-MS/MS).
- Data Analysis: The identified peptide sequences are mapped back to the drug product to reveal the exact epitopes being presented. This provides a direct, functional readout of the T-cell epitopes that could potentially drive an immune response in vivo [1].
Table 2: Key Impurity Types and Their Immunogenic Potential in Synthetic Peptides
| Impurity Type | Source | Potential Immunogenic Consequence | Control Strategy |
|---|---|---|---|
| Sequence Variants | Insertions, deletions, truncations during SPPS [1] | Introduction of novel T-cell epitopes with high HLA-binding affinity [1] | Robust analytical characterization (e.g., HRAM MS) and purification [6] |
| Post-Translational Modifications (PTMs) | Deamidation, oxidation, hydrolysis during manufacturing/storage [2] | Altered peptide structure creating or destroying epitopes; potential for neoepitopes [2] [6] | Control of manufacturing conditions (temp, pH); formulation optimization |
| Aggregates & Fibrils | Physical degradation and self-association [2] [1] | Innate immune activation; provision of T-cell help; enhanced B-cell responses [2] [1] | Monitor via SEC, DLS; optimize formulation excipients |
The Scientist's Toolkit: Essential Reagents and Assays
Table 3: Key Research Reagent Solutions for Immunogenicity Assessment
| Reagent/Assay | Function | Application Context |
|---|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Source of naive T cells and antigen-presenting cells from multiple HLA-typed donors [4] [1] | In vitro T-cell activation assays (ELISpot); dendritic cell priming assays |
| Enzyme-Linked Immunosorbent Spot (ELISpot) | Quantify antigen-specific T-cell responses (e.g., IFN-γ release) at the single-cell level [4] | Measuring T-cell activation in response to peptide antigens or impurities |
| HLA-I and HLA-II Tetramers | Directly identify and isolate T cells with specificity for a given peptide-HLA complex [3] | Tracking the frequency and phenotype of antigen-specific T cells pre- and post-vaccination |
| Toll-Like Receptor (TLR) Agonists (e.g., Poly-ICLC) | Potent adjuvants that activate dendritic cells via TLR3 and MDA5 pathways [7] | Enhancing the immunogenicity of peptide vaccines in preclinical models and clinical trials |
| High-Resolution Mass Spectrometry | Precisely characterize peptide sequence, PTMs, and impurities [6] | Peptide mapping for identity confirmation; detecting and quantifying product-related variants |
| 3,6-Dihydroxyflavone | 3,6-Dihydroxyflavone|High-Purity Research Compound | |
| 6-Methoxywogonin | 6-Methoxywogonin, CAS:3162-45-6, MF:C17H14O6, MW:314.29 g/mol | Chemical Reagent |
A systematic, multi-faceted approach is essential for accurately profiling the immunogenic risk of peptide-based products. The three drivers—origin, sequence, and aggregation—are not independent; a peptide with a low-risk self-origin can become immunogenic if its sequence is prone to aggregation or degradation into impurity forms containing novel T-cell epitopes. Therefore, a robust immunogenicity risk assessment strategy must integrate orthogonal methods: in silico tools for initial sequence screening, advanced analytical techniques (HRAM MS) for impurity and PTM detection, and functional in vitro assays (MAPPs, ELISpot) using primary human immune cells to confirm biological presentation and response. By systematically evaluating these key drivers, researchers can de-risk development pipelines and design safer, more effective peptide-based vaccines and therapeutics.
The adaptive immune system mounts a highly specific response against pathogens, primarily orchestrated by B and T lymphocytes. While both cell types are essential for immunological protection, they recognize antigens through fundamentally distinct mechanisms. B cells identify native antigens via B cell receptors (BCRs), while T cells recognize processed peptide fragments presented by Major Histocompatibility Complex (MHC) molecules on antigen-presenting cells (APCs) [8] [9]. These differences in recognition underlie specialized roles in humoral and cell-mediated immunity. Understanding the precise mechanisms of HLA presentation and antibody production is crucial for developing effective peptide-based vaccines and evaluating immunogenicity through in vitro assays [8] [10]. This guide provides a systematic comparison of T-cell and B-cell epitopes, detailing their characteristic features, experimental identification methods, and implications for vaccine design.
Core Biological Differences: A Comparative Framework
The table below summarizes the fundamental biological distinctions between T-cell and B-cell epitopes that determine their respective roles in adaptive immunity.
Table 1: Fundamental Biological Characteristics of T-cell and B-cell Epitopes
| Characteristic | T-cell Epitopes | B-cell Epitopes |
|---|---|---|
| Recognizing Lymphocyte | T lymphocytes (CD4+ helper, CD8+ cytotoxic) [11] [12] | B lymphocytes [11] |
| Native Structure Recognition | Recognizes processed linear peptides [9] | Recognizes intact, conformational, or linear epitopes on native antigens [8] |
| MHC/HLA Restriction | Strictly requires MHC presentation (Class I for CD8+, Class II for CD4+) [8] [9] | No MHC restriction for initial recognition [8] |
| Typical Epitope Size | MHC-I: 8-11 amino acids [8]MHC-II: 13-25 amino acids (core 9 aa bound) [8] [9] | 5-15 amino acids (conformational or linear) [8] |
| Chemical Nature | Primarily proteins (processed peptides) [8] | Proteins, polysaccharides, lipids, nucleic acids [8] |
| Epitope Location | Hidden, internal linear sequences [8] | Solvent-exposed regions of the antigen [8] |
Structural Basis of Epitope Presentation and Recognition
T-cell Epitopes and MHC Restriction
T-cell epitopes are short peptides derived from proteolytic processing of protein antigens, presented by MHC molecules on the surface of APCs. The MHC binding groove structure dictates key differences between Class I and Class II presentation [8].
MHC Class I Presentation: The peptide-binding cleft is closed at both ends, accommodating shorter peptides (typically 9-11 amino acids). The N- and C-terminal are anchored by conserved hydrogen bonds to the MHC molecule. Deep binding pockets with tight physicochemical preferences facilitate relatively accurate binding predictions [8].
MHC Class II Presentation: The peptide-binding groove is open, allowing bound peptides to extend beyond the groove. This accommodates longer peptides (typically 13-25 amino acids), with only a core of nine residues sitting within the binding groove. Shallower, less demanding binding pockets make peptide-MHC II binding prediction less accurate compared to MHC I [8].
B-cell Epitopes and Direct Recognition
B-cell epitopes constitute the specific region of an antigen that binds to an immunoglobulin or antibody. These epitopes are typically solvent-exposed regions and can be of diverse chemical nature, including proteins, polysaccharides, and lipids [8]. Unlike T-cells, B-cells recognize antigens in their native, three-dimensional conformation without a requirement for antigen processing or MHC presentation [8] [11]. B-cell epitopes can be conformational (dependent on the tertiary structure of the antigen) or linear (sequential amino acids) [8].
Figure 1: Divergent Antigen Recognition Pathways. T-cells require antigen processing and MHC presentation, while B-cells recognize native antigen structures directly.
Experimental Methods for Epitope Identification
Epitope mapping is crucial for understanding disease etiology, immune monitoring, and vaccine design [8]. The table below compares established experimental protocols for identifying T-cell and B-cell epitopes.
Table 2: Experimental Methods for Epitope Identification and Characterization
| Method Category | Specific Techniques | Key Readout | Utility in Vaccine Development |
|---|---|---|---|
| T-cell Epitope Mapping | ELISPOT [8], MHC Multimers [8], Intracellular Cytokine Staining, Lymphoproliferation Assays [8] | T-cell activation, cytokine secretion, proliferation | Identifies immunogenic peptides for inclusion in vaccines to stimulate cellular immunity |
| B-cell Epitope Mapping | X-ray Crystallography (Ag-Ab complexes) [8], Peptide Library Screening [8], Phage Display, Mutational Analysis [8] | Antibody binding to antigenic regions | Defines targets for neutralizing antibodies; guides reverse vaccinology |
Detailed Protocol: ELISPOT for T-cell Epitope Immunogenicity
The Enzyme-Linked Immunospot (ELISPOT) assay is a sensitive method for quantifying antigen-specific T cells based on their cytokine secretion [8].
Workflow:
- Plate Coating: A 96-well plate with a polyvinylidene difluoride (PVDF) membrane is coated with a primary capture antibody against a specific cytokine (e.g., IFN-γ for CD8+ T cells, IL-4/IL-5 for CD4+ Th2 cells).
- Cell Seeding and Stimulation: Peripheral blood mononuclear cells (PBMCs) or purified T cells are plated at varying densities alongside the test peptides (candidate epitopes). Positive control (e.g., phytohemagglutinin) and negative control (no peptide) wells are included.
- Incubation: Cells are incubated for 24-48 hours. During this time, activated T cells secrete cytokine, which is captured by the surrounding antibody.
- Detection: Cells are removed, and a biotinylated secondary detection antibody is added, followed by an enzyme-conjugated streptavidin (e.g., alkaline phosphatase or horseradish peroxidase).
- Spot Development: A precipitating substrate is added, producing colored spots at the sites of cytokine capture. Each spot represents a single reactive T cell.
- Analysis: Spots are counted using an automated ELISPOT reader. The frequency of antigen-specific T cells is calculated as spot-forming units (SFU) per million input cells. A response is typically considered positive if it significantly exceeds the negative control (e.g., 2-fold increase and >50 SFU/million).
Detailed Protocol: Peptide Library Screening for B-cell Epitopes
This method identifies linear B-cell epitopes by screening overlapping peptides derived from the antigen sequence against antisera or monoclonal antibodies.
Workflow:
- Peptide Synthesis: A library of synthetic peptides (typically 12-15 amino acids long with an overlap of 5-10 residues) spanning the entire protein sequence is synthesized on a cellulose membrane (SPOT synthesis) or in 96-well plates.
- Membrane Blocking: The membrane is incubated with a blocking buffer (e.g., 5% bovine serum albumin in TBST) to prevent non-specific antibody binding.
- Antibody Probing: The membrane is probed with the primary antibody (patient sera, monoclonal antibody) diluted in blocking buffer.
- Washing and Detection: Unbound antibody is washed away, and a labeled secondary antibody (e.g., horseradish peroxidase-conjugated anti-human IgG) is added.
- Signal Visualization: A chemiluminescent or colorimetric substrate is used to visualize the bound antibodies. Positive reactions appear as spots or colored wells corresponding to reactive peptides.
- Epitope Mapping: The amino acid sequences of the reactive peptides are aligned to define the minimal linear epitope core.
In Silico Prediction Tools and Computational Approaches
Traditional epitope identification is costly and time-consuming. In silico prediction methods dramatically reduce the experimental burden by prioritizing candidates for validation [8]. These tools are indispensable for rational vaccine design.
Table 3: Computational Tools for Epitope Prediction
| Tool Name | Prediction Target | Methodology | URL/Access |
|---|---|---|---|
| SYFPEITHI [8] | MHC-I & MHC-II binding | Motif/Matrix-based (MM) | http://www.syfpeithi.de/ |
| Rankpep [8] | MHC-I & MHC-II binding | Motif/Matrix-based (MM) | http://imed.med.ucm.es/Tools/rankpep.html |
| EpiDOCK [8] | MHC-II binding | Structure-Based (SB) | http://epidock.ddg-pharmfac.net |
| MHCPred [8] | MHC-I & MHC-II binding | Quantitative Structure-Activity Relationship (QSAR) | http://www.ddg-pharmfac.net/mhcpred/MHCPred/ |
| BIMAS [8] | MHC-I binding | Quantitative Affinity Matrix (QAM) | https://www-bimas.cit.nih.gov/molbio/hla_bind/ |
Figure 2: Computational Epitope Prediction Workflow. In silico tools use data-driven or structure-based approaches to predict T-cell and B-cell epitopes from antigen sequences, streamlining experimental validation.
This section details key reagents and tools essential for conducting epitope mapping and immunogenicity studies in vitro.
Table 4: Essential Research Reagents for Epitope and Immunogenicity Studies
| Reagent / Resource | Function/Description | Application Example |
|---|---|---|
| Synthetic Peptides | Short amino acid sequences (typically >70% purity) representing potential epitopes. | T-cell activation assays (ELISPOT), peptide library screens for B-cell epitope mapping [8]. |
| MHC Multimers (Tetramers, Dextramers) | Fluorescently labeled MHC-peptide complexes for staining antigen-specific T cells. | Flow cytometric identification, enumeration, and isolation of epitope-specific T cells [8]. |
| Recombinant Proteins | Purified, full-length or truncated antigen proteins. | B cell activation studies, antibody binding assays (ELISA), source material for antigen processing studies. |
| Cytokine-Specific Capture Antibodies | High-affinity antibodies for specific cytokines (IFN-γ, IL-4, IL-17, etc.). | ELISPOT and intracellular cytokine staining to quantify functional T-cell responses [8]. |
| Fluorochrome-conjugated Anti-Human Ig | Antibodies targeting human immunoglobulin isotypes (IgG, IgA, IgM) and subclasses (IgG1-4). | Flow cytometry for B cell phenotyping, ELISA for measuring isotype-switched antibody responses [13]. |
| TLR Agonists (e.g., MPLA) | Toll-like receptor ligands used as adjuvants. | Mimic pathogen-associated molecular patterns to provide co-stimulatory signals in in vitro B cell activation models [14]. |
| In Silico Prediction Tools | Software and web servers for computational epitope prediction. | Prioritizing candidate T-cell and B-cell epitopes for experimental validation, reducing time and cost [8] [15]. |
Implications for Peptide-Based Vaccine Design
The distinct mechanisms of epitope recognition directly inform the rational design of peptide-based vaccines. A critical consideration is the coordinated engagement of both B and T cell arms of the immune system.
Engaging T-cell Help for B Cell Responses
For most protein antigens, robust and high-affinity antibody responses require CD4+ T cell help, which is a T-cell dependent (TD) response [15]. In this pathway:
- B cells internalize the antigen bound to their BCR, process it, and present derived peptides on MHC class II molecules.
- Cognate CD4+ helper T cells recognize this peptide-MHC complex and provide co-stimulatory signals (e.g., CD40L, cytokines) to the B cell.
- This help drives B cell proliferation, immunoglobulin class switching from IgM to IgG, IgA, or IgE, and affinity maturation in germinal centers, leading to memory B cell and long-lived plasma cell formation [15].
The Challenge of Immunodominance
A significant hurdle in designing universal vaccines against viruses like HIV and influenza is immunodominance, where responses focus on a few dominant, often variable epitopes at the expense of subdominant, conserved epitopes targeted by broadly neutralizing antibodies (bnAbs) [10]. Recent theories, such as the "immunodominance relativity" theory, suggest that the physical positioning of B and T cell epitopes within the antigen matters. Antibody binding can enhance the presentation of adjacent CD4+ T cell epitopes while suppressing the presentation of overlapping ones. In several pathogens, conserved B cell epitopes targeted by bnAbs overlap with clusters of dominant CD4+ T cell epitopes, potentially putting B cells bearing bnAbs at a competitive disadvantage in germinal centers [10]. Strategic epitope engineering to disrupt these unfavorable overlaps or to create new, favorable B-T epitope partnerships could be key to guiding the immune system toward desired bnAb responses.
T-cell Independent B Cell Activation
Emerging evidence also reveals that under specific conditions, such as with highly dense, repetitive antigen arrays presented on liposomes with a TLR4 agonist like MPLA, B cells can be activated in a T-cell independent (TI) manner [14]. This pathway can induce rapid IgG class switching, germinal center formation, and long-lived memory, characteristics previously attributed solely to TD responses [14]. This knowledge opens avenues for designing vaccines that can elicit rapid and potent antibody responses even in individuals with compromised T-cell immunity.
The immunogenicity of peptide-based products—encompassing therapeutics, subunit proteins, and vaccines—is a critical determinant of their safety and efficacy. Unlike small molecule drugs, these biologics are susceptible to eliciting unwanted immune responses, which can range from reduced therapeutic effectiveness to severe adverse effects. This immunogenic potential is not solely an inherent property of the active pharmaceutical ingredient (API) but is profoundly influenced by product-related factors, including impurities, structural modifications, and the presence of adjuvants [2] [1]. For peptide-based vaccines, the careful incorporation of adjuvants is essential to enhance immunogenicity, whereas for therapeutic peptides, their presence is undesirable [16] [17]. A thorough understanding and control of these factors through advanced in vitro assays is therefore paramount for the rational design and regulatory approval of peptide-based products, ensuring they achieve their desired immunological outcome without compromising safety [18] [19].
Impact of Impurities on Immunogenicity
Peptide-related impurities are undesirable chemical components that can be introduced during synthesis, manufacturing, or storage. In Solid-Phase Peptide Synthesis (SPPS), the industry standard for peptides under 40 amino acids, impurities arise from incomplete reactions or side processes [2] [1]. For recombinant peptides, process-related impurities like host cell proteins are a greater concern [2]. The table below classifies common impurities and their immunogenicity risks.
Table 1: Types and Immunogenic Risks of Peptide Impurities
| Impurity Category | Specific Examples | Source | Potential Immunogenic Risk |
|---|---|---|---|
| Product-Related | Amino acid deletions, insertions, truncations | SPPS process | Introduction of novel T-cell epitopes [1]. |
| D-stereoisomer incorporation | SPPS process | Potential structural changes leading to new immune recognition. | |
| Post-Synthetic Modifications | Deamidation, oxidation, disulfide bond breakage | Manufacturing and storage | Altered peptide structure and potential neo-epitope formation [2]. |
| Process-Related | Host Cell Proteins (HCPs), DNA | Recombinant expression systems | Can act as adjavants, activating innate immunity [2]. |
| Aggregates & Fibrils | Oligomers, higher-order structures | Formulation and storage | Can enhance B-cell and T-cell responses by repetitive antigen display [2] [1]. |
Mechanisms of Immunogenicity
Impurities can drive immunogenicity through two primary, interconnected mechanisms: adaptive immune response and innate immune activation.
Adaptive Immune Response: Peptide impurities may contain sequences that are efficiently presented by Major Histocompatibility Complex (MHC) molecules, particularly HLA Class II, to CD4+ T-cells [1]. The activation of naive T-cells is a critical step for providing help to B-cells, leading to the production of anti-drug antibodies (ADAs) [1]. Even minor sequence variations in an impurity, such as a single amino acid substitution, can create a novel T-cell epitope that was not present in the API, breaking immune tolerance and initiating an unwanted adaptive immune response [1].
Innate Immune Activation (IIRMI): Trace impurities can function as Innate Immune Response Modulating Impurities (IIRMI). These substances act as inadvertent adjuvants by activating Pattern Recognition Receptors (PRRs), such as Toll-like Receptors (TLRs), on antigen-presenting cells (APCs) like dendritic cells and monocytes [18] [19]. This activation triggers inflammatory signaling pathways, leading to the upregulation of costimulatory molecules and the secretion of pro-inflammatory cytokines. This process creates a local immunogenic environment that promotes the activation of antigen-specific T-cells, thereby increasing the risk of an adaptive immune response against the peptide drug itself [18].
The following diagram illustrates the signaling pathways through which IIRMI trigger innate immune activation, a key mechanism in adjuvant function.
Experimental Assays for Detecting Impurity-Related Immunogenicity
Robust in vitro assays are essential for quantifying the immunogenic risk posed by impurities. Regulatory guidance for generic peptides recommends using orthogonal methods to provide independent lines of evidence [1].
Table 2: Key Assays for Immunogenicity Risk Assessment of Impurities
| Assay Type | Methodology Overview | Key Readouts | Application & Purpose |
|---|---|---|---|
| In Silico Epitope Prediction | Computational screening of peptide sequences for predicted binding affinity to a panel of common HLA-DR alleles [1]. | Binding score, % Rank. | Early risk assessment; identifies impurities with high potential to contain novel T-cell epitopes [1]. |
| In Vitro T-cell Assay | Co-culture of naive T-cells from diverse human donors with APCs pulsed with the impurity or API [1]. | T-cell proliferation (e.g., by CFSE), cytokine secretion (e.g., IFN-γ). | Functional assessment of naive T-cell activation; compares impurity to API [1]. |
| Cell-Based IIRMI Assay | Exposure of reporter cell lines (e.g., THP-1, RAW-Blue) or human PBMCs to the product [18] [19]. | NF-κB activation (SEAP), gene expression (IL-1β, IL-6, CCL3) via qPCR. | Detects innate immune activation potential of impurities; assesses overall adjuvant effect [18] [19]. |
Detailed Protocol: Cell-Based IIRMI Assay [18] [19]
- Cell Model: THP-1-Blue cells (human monocyte line with an NF-κB/AP-1-inducible SEAP reporter) or primary human PBMCs from healthy donors.
- Stimulation: Cells are plated and stimulated with the test article (API with impurities), a negative control (vehicle), and positive controls (known PRR agonists like LPS for TLR4) for 24 hours.
- Culture Conditions: Optimization is critical, as product excipients can sometimes mask immune responses [19]. A typical drug product concentration of 1-10 IU/mL can be used.
- Readout: SEAP activity in the supernatant is measured colorimetrically using Quanti-Blue detection medium. Viability is assessed in parallel using a reagent like CCK-8.
- Data Analysis: Results are compared to the reference listed drug (RLD) to determine if the test product elicits a significantly stronger innate immune response.
Impact of Structural and Chemical Modifications
Types of Modifications
Structural modifications are often deliberately introduced to improve the stability and pharmacokinetic profile of therapeutic peptides, but they can inadvertently alter immunogenicity.
Table 3: Impact of Common Peptide Modifications on Immunogenicity
| Modification Type | Purpose | Impact on Immunogenicity |
|---|---|---|
| Amino Acid Substitution (Unnatural) | Enhance metabolic stability, receptor affinity. | May create novel T-cell epitopes if the new residue improves binding to HLA [2] [1]. |
| Peptide Cyclization | Conformational restraint, protease resistance. | Can better mimic native protein epitopes, potentially enhancing desired immune responses for vaccines [17]. |
| Pegylation | Increase hydrodynamic size, reduce renal clearance. | Can shield immunogenic epitopes, but the PEG polymer itself can be immunogenic [2]. |
| Glycosylation | Improve solubility and stability. | Alters peptide structure; the glycan moiety can be recognized by immune cells [2]. |
Case Study: The Taspoglutide Incident
The development of the GLP-1 analog Taspoglutide provides a cautionary tale. During Phase 3 trials, a high incidence of systemic hypersensitivity reactions and injection-site reactions was observed [1]. Subsequent investigation linked these adverse events to the development of anti-drug antibodies. Retrospective studies suggested that sequence impurities introduced during synthesis were the likely culprit. These impurities contained sequences that were presented by specific HLA-DR alleles and activated T-cells in a subset of patients, leading to the adaptive immune response and clinical immunogenicity [1]. This case underscores the critical need for stringent impurity control and immunogenicity assessment.
Impact of Adjuvants in Peptide-Based Vaccines
The Role of Adjuvants
In contrast to therapeutic peptides where immunogenicity is undesirable, peptide-based vaccines often require adjuvants to be effective. Peptide antigens alone are typically poorly immunogenic as they lack the innate immune activation provided by whole pathogens [17] [20]. Adjuvants, which are components included in vaccine formulations, enhance the magnitude, breadth, and durability of the adaptive immune response [16] [17]. They function by activating innate immunity, mimicking the "danger signal" of an infection, which leads to enhanced antigen presentation and T-cell activation, as illustrated in the pathway diagram in Section 2.2.
Comparing Adjuvant Platforms and Formulations
Recent research focuses on novel adjuvant formulations and delivery systems to maximize immune responses against peptide antigens.
Table 4: Comparison of Adjuvant Platforms for Peptide Vaccines
| Adjuvant Platform | Composition / Key Molecule | Proposed Mechanism of Action | Reported Efficacy (Model) |
|---|---|---|---|
| TLR4 Agonist Formulations [16] | EmT4, LiT4Q (Liposomal), AlT4 (Alum-adsorbed). | Activation of TLR4 signaling pathway, leading to robust NF-κB-driven cytokine production. | Significantly boosted antibody breadth against SARS-CoV-2 variants (Omicron) when used as a protein boost after an RNA prime in mice [16]. |
| Nanotechnology-Based Systems [20] | Lipid nanoparticles (LNPs), polymer-based nanoparticles. | Protects antigen, enhances drainage to lymph nodes, promotes co-delivery of antigen and adjuvant to APCs. | Improves cross-presentation for CD8+ T-cell activation, critical for cancer vaccines; enhances stability of peptide antigens [20]. |
| Virus-Like Particles (VLPs) [21] | Self-assembling structural proteins lacking viral genome. | Presents a repetitive, high-density antigen array to B-cells; can have built-in PAMP activity. | Demonstrated higher protection (RR=1.66) in an FMDV vaccine meta-analysis compared to peptide vaccines [21]. |
Detailed Protocol: Evaluating Adjuvant Efficacy In Vivo [16]
- Vaccination Regimen: Mice are primed with an antigen (e.g., RNA vaccine or protein) and later boosted with the peptide antigen formulated with the test adjuvant. Control groups receive antigen alone or with a known adjuvant.
- Immunogenicity Assessment:
- Humoral Response: Serum is collected periodically and analyzed by ELISA to measure antigen-specific IgG titers. A pseudovirus neutralization assay can evaluate functional antibody responses.
- Cellular Response: Splenocytes are isolated and re-stimulated with the antigen to measure T-cell responses via ELISpot (for IFN-γ) or intracellular cytokine staining.
- Analysis: The strength and breadth of the immune response against the target pathogen or variants are compared between adjuvant groups.
The Scientist's Toolkit: Essential Research Reagents
This table lists key reagents and their functions for conducting immunogenicity assays as discussed in this guide.
Table 5: Key Reagents for Immunogenicity and Vaccine Research
| Research Reagent / Assay | Primary Function | Example Application |
|---|---|---|
| THP-1-Blue Cells | Reporter cell line for detecting NF-κB/AP-1 activation via SEAP. | Screening for IIRMI in drug products and impurities [18] [19]. |
| RAW-Blue Cells | Mouse macrophage reporter cell line for NF-κB/AP-1 activation. | Orthogonal model for innate immune activation studies [19]. |
| Quanti-Blue | SEAP detection substrate. Colorimetric readout for NF-κB activation in reporter assays [18]. | |
| Primary Human PBMCs | Provide a diverse, physiologically relevant immune cell population. | Comprehensive in vitro immunogenicity testing [18]. |
| TLR Agonists (e.g., LPS, FSL-1) | Positive control ligands for specific PRR pathways. | Assay validation and as model IIRMIs [18] [19]. |
| HLA Typing Kits | Determine the HLA allele composition of human donor cells. | Stratify T-cell assay results by HLA type for risk assessment [1]. |
| ELISpot Kits (e.g., IFN-γ) | Quantify antigen-specific T-cell responses at the single-cell level. | Evaluating cellular immunogenicity of vaccine formulations [16]. |
| T-1330 | T-1330, CAS:106461-41-0, MF:C22H27N5O2, MW:393.5 g/mol | Chemical Reagent |
| 2-Hydroxy Atorvastatin Lactone-d5 | 2-Hydroxy Atorvastatin Lactone-d5, CAS:265989-50-2, MF:C33H33FN2O5, MW:561.7 g/mol | Chemical Reagent |
The immunogenicity of peptide-based products is a complex trait heavily influenced by product-related factors. Impurities, even at trace levels, can introduce novel T-cell epitopes or act as adjuvants, driving unwanted adaptive immune responses. Conversely, deliberate structural modifications can either enhance or diminish immunogenicity, requiring careful evaluation. For peptide vaccines, the strategic use of adjuvants is non-negotiable for achieving protective immunity. The evolving regulatory landscape, particularly for generic and follow-on products, emphasizes the critical role of advanced in vitro models—including in silico tools, cell-based IIRMI assays, and in vitro T-cell assays—in assessing immunogenicity risk. Mastering the control and characterization of these product-related factors is essential for developing safer, more effective peptide-based therapeutics and vaccines.
Immunogenicity—the unwanted propensity of a therapeutic product to provoke an immune response—is a critical parameter in drug development, influencing both the safety and efficacy of biopharmaceuticals [22]. For peptide-based vaccines and therapeutics, assessing this risk is a multifaceted challenge that spans the entire drug development lifecycle, from candidate selection to post-marketing surveillance [2]. The global market for therapeutic peptides is projected to grow rapidly, reaching US$86.9 billion by 2032, intensifying the need for robust immunogenicity assessment frameworks [2]. This guide objectively compares the experimental approaches and regulatory considerations for immunogenicity risk assessment, providing researchers with a detailed comparison of methodologies, their applications, and supporting data.
Regulatory Framework and Lifecycle Approach
Regulatory guidance emphasizes an integrated risk assessment strategy where immunogenicity is evaluated at every stage of development [2] [22]. The United States Food and Drug Administration (FDA) and the European Medicines Agency (EMA) both require immunogenicity assessment for therapeutic proteins and peptides, with reporting under ‘adverse effects’ in drug labeling [22]. A significant regulatory gap exists for follow-on therapeutic peptide products; specifically, "broadly applicable impurity qualification thresholds are not available for peptide drug products," and controls are established on a case-by-case basis [2]. For chemical peptides, principles from ICH Q3A and Q3B may be considered, while recombinant peptides fall under ICH Q6B, though none provide specific acceptance criteria for impurities [2].
Table 1: Immunogenicity Risk Factors Throughout the Drug Lifecycle
| Development Stage | Primary Risk Factors | Key Assessment Methods | Regulatory Considerations |
|---|---|---|---|
| Candidate Selection | Sequence similarity to self-proteins, intrinsic immunogenic epitopes [2] | In silico T-cell epitope prediction, in vitro MHC binding assays [2] [22] | Justification of candidate sequence based on predicted low immunogenic potential [22] |
| Manufacturing | Process-related impurities, peptide-related impurities (e.g., deletions, substitutions), aggregates, host cell proteins [2] | Analytical characterization (SEC, MALS, DLS, MFI), accelerated stability studies [2] [22] | Control strategies for impurities and aggregates; case-by-case justification for synthetic peptide impurities [2] |
| Pre-clinical | Immunotoxicity, innate immune activation, breaking of immune tolerance [2] | GLP toxicology studies in relevant species, immune monitoring for ADA [2] [22] | Species relevance is critical; data used to flag potential clinical risks [22] |
| Clinical Stage | Patient factors (genetics, disease), treatment factors (dose, route), product quality [2] | Validated anti-drug antibody (ADA) assays, PK/PD impact assessment, safety monitoring [2] [22] | FDA & EMA require clinical immunogenicity testing and reporting of ADA incidence and impact [22] |
| Post-Marketing | Rare immune-related adverse events [2] | Phase IV studies, pharmacovigilance systems [2] | Monitoring for rare events not captured in clinical trials [2] |
The following workflow diagram illustrates the integrated immunogenicity risk assessment process across the drug development lifecycle, incorporating both forward and reverse translational approaches [22].
Diagram 1: Immunogenicity Risk Assessment Workflow
In Vitro Assays for Immunogenicity Risk Assessment
A suite of in vitro assays is employed to predict and measure immunogenic potential, especially before clinical studies. These assays evaluate the innate and adaptive immune system activation potential of peptide products and their impurities.
Key Assay Methodologies and Protocols
Dendritic Cell (DC) Activation Assay
- Objective: To assess the potential of a peptide product or impurity to activate dendritic cells, a critical step in initiating an adaptive immune response [22].
- Protocol:
- Cell Culture: Isolate human monocyte-derived dendritic cells (moDCs) from healthy donor PBMCs using CD14+ magnetic beads. Differentiate monocytes in RPMI-1640 medium supplemented with GM-CSF (50 ng/mL) and IL-4 (20 ng/mL) for 5-7 days [22].
- Stimulation: Harvest immature DCs and seed in 96-well plates. Expose cells to the peptide product, relevant impurities (e.g., aggregates, oxidized species), or controls (LPS as positive control, culture medium as negative control) for 24 hours.
- Analysis: Harvest supernatant for cytokine analysis (e.g., IL-6, TNF-α, IL-12p70) via ELISA or multiplex immunoassay. Analyze cells by flow cytometry for surface activation markers (e.g., CD80, CD83, CD86, HLA-DR) [22].
- Data Interpretation: A statistically significant increase in cytokine secretion and/or surface marker expression compared to the negative control indicates innate immune activation and higher immunogenic potential.
T-Cell Activation Assay (ELISpot/T-Cell Proliferation)
- Objective: To measure the activation and proliferation of peptide-specific T-cells, which drive adaptive cellular immunity [22].
- Protocol:
- PBMC Isolation: Isolate PBMCs from multiple healthy human donors using density gradient centrifugation (e.g., Ficoll-Paque). The use of donors with diverse HLA types is critical for a representative assessment [22].
- Culture and Stimulation: Seed PBMCs in 96-well plates. Add the peptide product, its fragments, or positive controls (e.g., PHA). For IFN-γ ELISpot, use pre-coated plates. For proliferation assays, use CFSE staining tracked by flow cytometry.
- Incubation: Culture cells for 5-7 days in a CO₂ incubator at 37°C.
- Detection (ELISpot): Develop plates according to manufacturer's instructions after adding detection antibodies. Spot-forming units (SFUs) are counted using an automated ELISpot reader [22].
- Data Interpretation: An increase in IFN-γ SFUs or CFSE-dim T-cells in test wells compared to negative control wells indicates a T-cell response.
MHC-Associated Peptide Proteomics (MAPPs) Assay
- Objective: To identify specific peptides from a biotherapeutic that are processed by DCs and presented on MHC class II molecules, directly characterizing the potential T-cell epitope repertoire [22].
- Protocol:
- Pulse DCs with Antigen: Immature human DCs are pulsed with the peptide product for 24-48 hours.
- MHC Peptide Complex Isolation: Lyse cells and immunoprecipitate HLA-DR molecules using a specific antibody.
- Peptide Elution and Analysis: Elute bound peptides from the MHC complex and identify them by liquid chromatography-mass spectrometry (LC-MS/MS) [22].
- Data Interpretation: The presence of peptide sequences derived from the drug product in the MHC-II immunoprecipitate confirms their presentation to T-cells. Sequences with high abundance or similarity to known immunogenic epitopes pose a higher risk.
Comparative Analysis of In Vitro Assays
Table 2: Comparison of Key In Vitro Immunogenicity Assays
| Assay Type | Measured Endpoint | Key Advantages | Key Limitations | Typical Readout | Predictive Value |
|---|---|---|---|---|---|
| DC Activation Assay | Innate immune activation; DC maturation markers & cytokine release [22] | Detects innate immune danger signals; high sensitivity to aggregates and impurities [22] | Does not directly measure T-cell activation; donor variability [22] | Cytokine concentration (pg/mL); % CD86+ cells | High for innate immunogenicity |
| T-Cell Assay (ELISpot) | Antigen-specific T-cell response (e.g., IFN-γ production) [22] | Directly measures adaptive T-cell response; uses human PBMCs [22] | Requires donor pools with diverse HLA; may lack sensitivity for low-frequency T-cells [22] | Spot-forming units (SFU) per million cells | Moderate to high for cellular immunogenicity |
| MAPPs Assay | Peptide sequences presented on MHC class II [22] | Directly identifies potential T-cell epitopes; highly informative for sequence optimization [22] | Technically complex and expensive; requires expertise in LC-MS/MS [22] | Peptide sequences and abundance | High for de-risking T-cell responses |
| NF-κB Reporter Assay | TLR pathway activation (e.g., TLR4) [16] | High-throughput; specific for TLR-mediated immunogenicity [16] | Limited to specific pathways; may not reflect full cellular context [16] | Luminescence or fluorescence units | Moderate for specific TLR engagement |
The relationship between these assays and the immunological pathways they probe is complex. The following diagram outlines the core immunogenicity pathway and the points where key in vitro assays provide critical data.
Diagram 2: Immunogenicity Pathways and Assay Targets
Case Study: Peptide-Based Vaccines
Peptide-based vaccines, such as those developed for Foot-and-Mouth Disease Virus (FMDV), provide compelling real-world data on immunogenicity assessment. A systematic review and meta-analysis of FMDV vaccines (2020-2025) compared the protective efficacy of different platforms [21].
Table 3: Meta-Analysis of FMDV Vaccine Efficacy (2020-2025) [21]
| Vaccine Platform | Pooled Risk Ratio (RR) | 95% Confidence Interval (CI) | Interpretation |
|---|---|---|---|
| Virus-Like Particle (VLP) | 1.66 | 0.97 – 2.86 | Higher protection, wide CI indicates variability [21] |
| Viral Vector | 1.90 | 0.08 – 46.65 | Highest point estimate, but very wide CI [21] |
| Peptide-Based | 1.09 | 0.75 – 1.57 | Moderate efficacy [21] |
| Dendritic Cell-Based | Not Significant | Not Significant | Limited demonstrable benefit [21] |
A specific FMDV peptide vaccine, the Bâ‚‚T-TBâ‚‚ dendrimer, demonstrates how rational design mitigates immunogenicity risks while ensuring efficacy. This multiepitopic platform incorporates four copies of a VP1 B-cell epitope and two copies of a 3A T-cell epitope from FMDV, assembled via chemoselective "click" chemistry (thiol-ene and CuAAC) [23].
- Experimental Protocol for Challenge Study:
- Vaccination: Domestic pigs (natural FMDV host) were immunized with a single low dose (0.5 mg) of either Bâ‚‚T-TBâ‚‚ or its predecessor B2T, formulated with adjuvant [23].
- Immune Monitoring: Serum was collected periodically to measure FMDV-neutralizing antibody titers via virus neutralization test. T-cell responses were assessed by IFN-γ ELISpot upon stimulation with the T-cell epitope [23].
- Challenge: At 25 days post-immunization (dpi), pigs were intradermally challenged with FMDV O-UK/11/2001. Animals were monitored daily for clinical signs (vesicular lesions on snout and feet) and viremia was tracked by RT-qPCR [23].
- Results: A single low dose of Bâ‚‚T-TBâ‚‚ induced a rapid and robust neutralizing antibody response and protected 100% of swine (no clinical signs post-challenge), outperforming the already effective B2T prototype and confirming that well-defined peptide vaccines can achieve high levels of protection without unwanted immunopathology [23].
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions
| Reagent / Material | Function in Immunogenicity Assessment | Specific Example / Application |
|---|---|---|
| Human PBMCs from Diverse Donors | Provides a genetically diverse human immune cell source for in vitro T-cell and DC assays [22] | Used in ELISpot and DC activation assays to account for HLA polymorphism [22] |
| Magnetic Cell Separation Kits | Isolation of specific immune cell populations (e.g., CD14+ monocytes) from PBMCs for defined assays [22] | Differentiation of CD14+ monocytes into Dendritic Cells for DC activation studies [22] |
| Recombinant Human Cytokines | Differentiation and maintenance of primary immune cells in culture [22] | GM-CSF and IL-4 for generating monocyte-derived Dendritic Cells (moDCs) [22] |
| ELISpot Kits (e.g., IFN-γ) | Detection and quantification of antigen-specific T-cell responses at the single-cell level [22] | Measuring T-cell responses to peptide antigens in PBMC cultures [23] [22] |
| TLR Agonist Adjuvants | Positive controls for innate immune activation assays; components in vaccine formulations [16] | EmT4TM, LiT4QTM (TLR4 agonists) used as adjuvants and controls [16] |
| Click Chemistry Reagents | Modular, chemoselective conjugation for constructing defined multi-epitope peptide vaccines [23] | Synthesis of Bâ‚‚T-TBâ‚‚ dendrimer vaccine via CuAAC and thiol-ene reactions [23] |
| 5-Nitrouracil | 5-Nitrouracil CAS 611-08-5|Research Chemical | |
| Rsu 1164 | Rsu 1164, CAS:105027-77-8, MF:C10H16N4O3, MW:240.26 g/mol | Chemical Reagent |
A proactive and integrated immunogenicity risk assessment strategy is paramount for developing safe and effective peptide-based drugs and vaccines. This requires leveraging complementary in vitro assays—from DC activation and MAPPs to T-cell ELISpot—to build a robust risk profile before clinical trials [22]. The regulatory landscape demands careful control of product-related factors, especially impurities and aggregates, throughout the drug lifecycle [2]. As demonstrated by advanced peptide vaccine candidates, rational molecular design and precise analytical control can successfully minimize unwanted immunogenicity while achieving desired protective immunity. This structured, data-driven approach provides a reliable framework for researchers navigating the complex intersection of immunology, product quality, and regulatory science.
Core In Vitro Assays: From Epitope Screening to Functional Immune Readouts
The evaluation of cellular immunogenicity is a critical component in the development of peptide-based vaccines. Among the various techniques available, the Interferon-gamma (IFN-γ) Enzyme-Linked Immunospot (ELISpot) assay has emerged as a cornerstone method for detecting and quantifying antigen-specific T-cell responses. This guide provides an objective comparison of the IFN-γ ELISpot assay with alternative methodologies, presenting experimental data and detailed protocols to inform assay selection in vaccine research and development. The focus is on practical implementation within the context of immunogenicity assessment for peptide-based vaccines, addressing the needs of researchers and drug development professionals seeking robust, sensitive, and reproducible immune monitoring tools.
Performance Comparison of T-Cell Activation Assays
Head-to-Head Assay Comparison
The selection of an appropriate T-cell activation assay depends on multiple factors, including the research question, sample availability, and required data granularity. The table below provides a comparative overview of three key technologies used in immunogenicity assessment.
Table 1: Technical Comparison of Key T-Cell Immunogenicity Assays
| Parameter | IFN-γ ELISpot | Intracellular Cytokine Staining (ICS) | Cytokine Production (CP) ELISA |
|---|---|---|---|
| What is Measured | Frequency of cytokine-secreting cells [24] | Intracellular cytokines with cellular phenotype [25] | Total soluble cytokine concentration in supernatant [24] |
| Sample Type | Live PBMCs [24] | Live PBMCs [25] | Serum, plasma, or cell culture supernatant [24] |
| Sensitivity | Very high; detects rare responder cells [24] | Similar to ELISpot when optimized [25] | Moderate to high [24] |
| Key Output | Spot-forming units (SFU) per million cells [24] | Percentage or count of cytokine-positive T-cell subsets [25] | Cytokine concentration (e.g., pg/mL) [24] |
| Phenotypic Data | No | Yes (e.g., CD4/CD8, memory subsets) [25] | No |
| Multiplexing Capability | Single-plex (unless using Fluorospot) [25] | High (multiple cytokines and markers) [25] | Limited |
| Throughput | Moderate (cell handling can be a bottleneck) [24] | Moderate to High | High (easily automated) [24] |
| Specialized Equipment | ELISpot plate reader [24] | Flow cytometer [25] | Standard ELISA plate reader [24] |
Comparative Clinical Performance Data
Data from clinical studies directly comparing these assays demonstrate context-dependent performance. A 2025 study on tuberculosis diagnosis in a BCG-vaccinated Pakistani population found that an ELISPOT-based IGRA (X-DOT-TB) showed significantly higher sensitivity (79.5%, 95% CI: 77.4-81.5) for detecting Mycobacterium tuberculosis infection compared to an ELISA-based IGRA (QFT-Plus) at 55.7% (95% CI: 52.9-58.5) and the tuberculin skin test (TST) at 35.8% (95% CI: 34.4-37.1) [26]. The specificities were comparable at 85.1%, 78.1%, and 82.2%, respectively [26].
Similarly, a 2022 study comparing ELISpot and ICS for detecting SARS-CoV-2 T-cells in paucisymptomatic patients found that ELISpot identified a higher proportion of responders (67%) compared to ICS (44%), suggesting superior sensitivity for detecting low-frequency responses in certain contexts [27]. The magnitude of responses was also generally low, with a median of 61 Spot-Forming Cells (SFCs) per million PBMCs with ELISpot [27].
Table 2: Summary of Comparative Clinical Performance from Recent Studies
| Study Context | Compared Assays | Key Performance Finding | Study Reference |
|---|---|---|---|
| Tuberculosis diagnosis (Pakistani population) | ELISPOT-based IGRA vs. ELISA-based IGRA vs. TST | ELISPOT sensitivity: 79.5%ELISA IGRA sensitivity: 55.7%TST sensitivity: 35.8% [26] | Sci Rep. 2025 |
| SARS-CoV-2 T-cell detection (Paucisymptomatic patients) | ELISpot vs. ICS | Proportion of responders with ELISpot: 67%Proportion of responders with ICS: 44% [27] | Immunol Infect Dis. 2022 |
| HIV-specific T-cell responses | ELISpot vs. Cytokine Production (CP) ELISA | Both ELISpot and CP ELISA distinguished between patient groups; strong correlation between these two assays [28] | Clin Vaccine Immunol. 2010 |
Detailed Experimental Protocols
Standard IFN-γ ELISpot Protocol for Peptide-Based Vaccines
The following protocol is adapted from established methodologies used in vaccine immunogenicity studies [27] [29] [30].
Day 1: Plate Coating and Cell Preparation
- Coating: Add 100 μL/well of anti-IFN-γ capture antibody (e.g., 15 μg/mL in sterile PBS) to a PVDF-backed 96-well plate. Incubate overnight at 4°C.
- PBMC Thawing: Remove a cryovial of PBMCs from liquid nitrogen storage and thaw rapidly in a 37°C water bath.
- Washing: Transfer cells to a 15 mL tube pre-filled with warm R10 culture medium (RPMI-1640 with 10% FBS, L-glutamine, and antibiotics). Centrifuge at 400 × g for 10 minutes. Aspirate supernatant.
- Cell Counting: Resuspend cell pellet in 5-10 mL of R10 medium. Perform a viable cell count using Trypan Blue exclusion.
- Resting: Adjust cell concentration to 5-10 × 10^6 cells/mL and place the tube in a 37°C, 5% CO2 incubator for at least 4 hours to allow cell recovery.
Day 2: Antigen Stimulation and Incubation
- Plate Blocking: Decant the coating antibody from the plate. Wash the plate 3 times with sterile PBS. Add 200 μL/well of R10 medium to block non-specific binding. Incurate for at least 2 hours at 37°C.
- Peptide Pools: Prepare the peptide pool(s) representing the vaccine antigens in R10 medium. Typical working concentration for individual 15-mer peptides overlapping by 11 amino acids is 1-2 μg/mL [27].
- Plate Setup:
- Test Wells: Add 100 μL of peptide solution per well in duplicate or triplicate.
- Positive Control Wells: Add 100 μL of a mitogen (e.g., PHA at 5 μg/mL).
- Negative Control Wells: Add 100 μL of R10 medium alone (with equivalent DMSO concentration if used for peptide solubilization).
- Cell Plating: Resuspend the rested PBMCs and plate at 100,000 to 250,000 cells per well in a volume of 100 μL [27] [24].
- Incubation: Incubate the plate for 16-24 hours at 37°C, 5% CO2. Do not move or disturb the plate during this time.
Day 3: Detection and Spot Development
- Cell Removal: Decant cell suspension and wash the plate 5 times with PBS containing 0.05% Tween-20 (PBST).
- Detection Antibody: Add 100 μL/well of biotinylated anti-IFN-γ detection antibody (e.g., 1 μg/mL in PBST with 1% BSA). Incubate for 2 hours at room temperature.
- Enzyme Conjugate: Wash plate 5 times with PBST. Add 100 μL/well of Streptavidin-Horseradish Peroxidase (HRP) conjugate, diluted per manufacturer's instructions. Incubate for 1 hour at room temperature.
- Spot Development: Wash plate 5 times with PBST and then 2 times with PBS alone. Add 100 μL/well of precipitating substrate (e.g., AEC or TMB). Develop for 5-30 minutes at room temperature in the dark. Monitor spot formation.
- Stop Reaction: Once spots are distinct and background is low, stop the reaction by thoroughly washing the plate with tap water. Remove the plate underdrain and allow to air dry completely in the dark.
Day 3/4: Plate Reading and Analysis
- Reading: Count spots using an automated ELISpot plate reader.
- Analysis: Calculate the antigen-specific response for each sample:
Mean SFC (test) - Mean SFC (negative control) = Net SFC per well
(Net SFC per well / Number of cells plated per well) × 10^6 = SFC per million PBMCs
- Quality Control: The assay is valid if the negative control has low background (typically <10-20 spots) and the positive control shows a strong, expected response [27]. A response is typically considered positive if it is at least 2-fold above the negative control and exceeds a pre-defined threshold (e.g., 50 SFC/million PBMCs above background).
Protocol for Intracellular Cytokine Staining (ICS)
For comparative studies, ICS can be performed in parallel. This protocol is adapted from studies comparing ICS with ELISpot [27] [28].
- Stimulation: Stimulate 0.5-1 × 10^6 PBMCs per condition with the peptide pool (1 μg/mL) in the presence of a costimulatory antibody (e.g., anti-CD28/CD49d) and a protein transport inhibitor (e.g., Brefeldin A) for 4-18 hours at 37°C [27].
- Staining:
- Surface Staining: Wash cells and stain with surface marker antibodies (e.g., anti-CD3, CD4, CD8) for 20-30 minutes at 4°C.
- Fixation/Permeabilization: Wash cells, then fix and permeabilize them using a commercial cytofix/cytoperm solution.
- Intracellular Staining: Wash with perm/wash buffer and stain with antibodies against intracellular cytokines (e.g., IFN-γ, IL-2, TNF-α) for 30 minutes at 4°C.
- Acquisition and Analysis: Wash cells and resuspend in fixation buffer. Acquire data on a flow cytometer. Analyze using flow cytometry software, gating on live, single lymphocytes, then on CD3+ T-cells, and further subdividing into CD4+ and CD8+ populations to identify the frequency of cytokine-positive cells within these subsets [27] [25].
Workflow and Decision-Making Diagrams
ELISpot Experimental Workflow
Assay Selection Decision Pathway
Essential Research Reagent Solutions
Successful implementation of the IFN-γ ELISpot assay requires high-quality, validated reagents. The following table details key materials and their functions.
Table 3: Essential Research Reagents for IFN-γ ELISpot
| Reagent / Material | Function / Role in the Assay | Examples & Notes |
|---|---|---|
| Pre-coated ELISpot Plates | Solid phase for capturing secreted cytokine; PVDF membranes are standard for high sensitivity. | Commercial kits (e.g., Mabtech, Oxford Immunotec, R&D Systems) ensure consistency and reliability [29]. |
| Peptide Pools / Antigens | Stimulate antigen-specific T-cells to secrete IFN-γ. | Overlapping peptide libraries (15-mers with 11-aa overlap) spanning vaccine antigens [27]. Use endotoxin-free peptides. |
| Cell Culture Medium | Maintain cell viability and support immune cell function during stimulation. | RPMI-1640 supplemented with fetal bovine serum (5-10%), L-glutamine, and antibiotics [27]. |
| Antibody Pairs | Capture and detect the cytokine of interest (IFN-γ). | Matched antibody pairs are critical for specificity and low background [24]. |
| Detection System | Amplify the signal for visualization of spots. | Typically involves a biotin-streptavidin-enzyme (HRP or AP) complex with a precipitating substrate [24]. |
| Positive Control Stimuli | Verify cell viability and functionality. | Mitogens like PHA or PMA/Ionomycin. Peptide pools from common pathogens (e.g., CEF pool) can also be used [27]. |
| Cryopreserved PBMCs | Starting material for the assay; allows batch testing. | High-quality PBMCs with high post-thaw viability are essential. Use controlled-rate freezing and proper cryoprotectant (e.g., DMSO/FCS) [31]. |
The IFN-γ ELISpot assay remains a powerful, highly sensitive tool for quantifying antigen-specific T-cell responses in peptide-based vaccine development. Its primary advantage lies in its exceptional sensitivity for detecting low-frequency T-cell responses, making it ideal for screening immunogenicity. However, the choice between ELISpot, ICS, and other immunoassays is not a matter of which is universally superior, but which is most appropriate for the specific research objective. ICS provides unparalleled detail on T-cell phenotype and polyfunctionality, while ELISA offers a high-throughput method for quantifying total cytokine secretion. A strategic approach often involves using ELISpot for initial screening and ICS for in-depth characterization of positive responses, thereby leveraging the strengths of both assays to build a comprehensive understanding of vaccine-induced cellular immunity.
The Enzyme-Linked Immunosorbent Assay (ELISA) stands as a cornerstone technique for assessing humoral immune responses, particularly in the development of peptide-based vaccines. This immunological biochemical assay detects antigen-antibody interactions using enzyme-labelled conjugates and substrates that generate measurable color changes, providing critical data on vaccine immunogenicity [32]. In vaccine development, ELISA enables researchers to quantify antigen-specific antibody titers, establishing correlates of protection and bridging immunological results across different vaccine platforms and clinical trials [33]. The technique's high throughput, quantitative capabilities, and specificity make it indispensable for evaluating vaccine-induced immune responses, monitoring antibody persistence, and facilitating vaccine licensure [34] [33].
For peptide-based vaccines, which often consist of synthetic immunogenic epitopes, ELISA provides a direct method to measure the magnitude and quality of the antibody response against target antigens. As demonstrated in Shigella vaccine studies, measurement of serum immunoglobulin G (IgG) to pathogen-specific antigens has been proposed as a key correlate of protection against infection [33]. Similarly, in cancer vaccine development, including multi-epitope peptide vaccines targeting triple-negative breast cancer, ELISA methodologies enable researchers to verify that designed constructs elicit robust antibody responses against selected tumor-associated antigens [35] [36]. The ability to precisely quantify these humoral responses is essential for selecting the most promising vaccine candidates for further development.
ELISA Methodologies: A Comparative Analysis
Core ELISA Formats and Applications
Different ELISA formats offer distinct advantages for specific applications in vaccine immunogenicity assessment. Understanding these methodologies is crucial for selecting the appropriate approach for evaluating antigen-specific antibody titers.
Table 1: Comparison of Major ELISA Formats for Antibody Detection
| Format | Principle | Sensitivity | Specificity | Best Applications in Vaccine Studies | Key Limitations |
|---|---|---|---|---|---|
| Direct ELISA | Antigen coated on plate; detected with enzyme-labeled primary antibody | Low | Moderate | High-throughput screening of purified antibodies; epitope mapping | Requires labeled primary antibodies for each target; lower sensitivity |
| Indirect ELISA | Antigen coated on plate; detected with unlabeled primary and enzyme-labeled secondary antibodies | High | Moderate | Measuring antibody titers in immunized sera; vaccine response monitoring | Potential cross-reactivity with secondary antibodies |
| Sandwich ELISA | Capture antibody coated on plate; antigen "sandwiched" between capture and detection antibodies | Highest | Highest | Complex samples; low abundance antigens; precise quantification of specific antibodies | Requires matched antibody pairs; more complex optimization |
| Competitive/Inhibition ELISA | Sample antibodies compete with labeled reference for antigen binding | Variable | High | Measuring antibodies against small molecules; analyzing antibody affinity | Inverse signal relationship; complex data interpretation |
The indirect ELISA format is particularly valuable in vaccine studies for measuring antibody titers in immunized subjects, as it offers high sensitivity and flexibility without requiring labeled primary antibodies [34]. The signal amplification achieved through multiple secondary antibodies binding to a single primary antibody makes this format ideal for detecting lower antibody concentrations often encountered in early vaccine development. For peptide-based vaccines, where targets are well-defined and purity is high, indirect ELISA provides reliable quantification of antigen-specific responses.
The sandwich ELISA format offers superior specificity for complex sample matrices, as two antibodies are required to recognize the target antigen simultaneously [34]. This format is especially useful when analyzing serum samples with potential cross-reactive antibodies or when measuring specific antibody isotypes in polyclonal responses. However, this approach requires carefully optimized antibody pairs that recognize non-overlapping epitopes, which can be challenging for small peptide antigens.
Competitive ELISA formats are particularly valuable for assessing antibody responses against small epitopes or when evaluating antibody affinity maturation following vaccination [34] [37]. The inverse relationship between signal and analyte concentration (higher antibody titer produces lower signal) provides a robust method for quantifying antibodies in complex biological fluids without requiring extensive sample purification.
Experimental Protocol: Indirect ELISA for Vaccine Antibody Assessment
The following detailed protocol outlines the standard procedure for quantifying antigen-specific antibody titers using indirect ELISA, adapted from established methodologies in vaccine research [34] [32]:
Plate Coating: Dilute purified antigen (e.g., vaccine peptide or target protein) in carbonate-bicarbonate buffer (pH 9.6) to a concentration of 1-10 μg/mL. Add 100 μL/well to a 96-well polystyrene microplate and incubate overnight at 4°C. The optimal coating concentration should be determined empirically for each antigen.
Washing: Discard the coating solution and wash the plate three times with PBS-Tween 20 (0.05%) using an automated plate washer or manual washing system. Each wash should consist of filling wells completely, soaking for 30-60 seconds, and thoroughly decanting the solution.
Blocking: Add 200-300 μL/well of blocking buffer (1-5% BSA or non-fat dry milk in PBS) to cover all potential binding sites. Incubate for 1-2 hours at room temperature or overnight at 4°C. Wash plate three times as before.
Primary Antibody Incubation: Prepare serial dilutions of test sera (from vaccinated subjects) and controls in sample diluent (blocking buffer with 0.05% Tween-20). Include negative control sera (pre-immune or from unvaccinated subjects) and positive control sera when available. Add 100 μL/well of each dilution in duplicate or triplicate. Incubate for 1-2 hours at room temperature or 37°C. Wash plate three times.
Secondary Antibody Incubation: Dilute enzyme-conjugated secondary antibody (e.g., HRP-anti-species IgG) in sample diluent according to manufacturer's recommendations. Add 100 μL/well and incubate for 1-2 hours at room temperature. Wash plate three times.
Signal Detection: Prepare enzyme substrate solution immediately before use (e.g., TMB for HRP). Add 100 μL/well and incubate in the dark for 15-30 minutes, monitoring color development.
Reaction Stopping: Add 50-100 μL/well of stop solution (e.g., 1M H₂SO₄ for TMB). The solution color will change from blue to yellow when using acid stop solutions with TMB.
Absorbance Measurement: Read optical density (OD) at appropriate wavelength (e.g., 450nm for TMB) using a microplate spectrophotometer within 30 minutes of stopping the reaction.
For quantitative assessment, include a standard curve with known concentrations of the target antibody whenever possible. When absolute quantification is not feasible, report results as endpoint titers, defined as the highest serum dilution that produces an OD value significantly above the negative control (typically 2-3 standard deviations above the mean negative control value) [33] [38].
Quantitative Data Analysis and Standardization
Standard Curve Generation and Data Interpretation
Accurate quantification of antibody titers relies on proper standard curve implementation and data analysis techniques. The following workflow ensures reliable results:
Standard Preparation: Prepare a series of 2-fold or 3-fold dilutions from a high-concentration standard, ensuring the range covers expected sample values. Include at least 6-8 standard points plus a zero standard (blank) [38].
Background Subtraction: Subtract the OD of the blank well (zero standard) from all other readings to eliminate background signal: Adjusted OD = Sample OD - Blank OD [38].
Curve Fitting: Use appropriate curve-fitting models for the standard curve. The 4-parameter logistic (4PL) model is recommended for most ELISA applications due to its flexibility and sigmoidal fit [38] [39]. The 4PL equation is: Y = D + (A - D) / (1 + (X / C)á´®), where A = minimum asymptote, D = maximum asymptote, C = inflection point (ECâ‚…â‚€), and B = slope factor.
Sample Concentration Interpolation: Use the fitted standard curve to interpolate concentrations of unknown samples from their adjusted OD values. Ensure sample ODs fall within the standard curve range. If not, dilute samples further and re-test [38].
Dilution Factor Correction: Multiply interpolated values by the dilution factor to obtain original concentrations: Final concentration = Interpolated value × Dilution factor [38].
For qualitative or semi-quantitative analysis, establish a cutoff value using statistical approaches: Cutoff = Mean OD of negative controls + 2 × Standard Deviation (SD). Samples with OD values above this cutoff are considered positive [38].
Inter-laboratory Standardization and Bridging Studies
Standardization of ELISA methodologies across different laboratories is essential for meaningful comparison of immunogenicity data from various vaccine trials. As highlighted in Shigella vaccine research, lack of standardization means that antibody measurements from different studies cannot be easily compared [33]. Bridging studies using shared serum panels enable conversion of results between different ELISA methods.
Table 2: Cross-Comparison of ELISA Methodologies from Shigella Vaccine Studies
| Laboratory/Method | Reported Units | Correlation with Reference Method | *Corresponding Titer to Protective Threshold | Application in Vaccine Trials |
|---|---|---|---|---|
| Tel Aviv University (TAU) ELISA | Endpoint titer | Reference method | 1,600 (established protective threshold) | Original efficacy trials |
| GVGH ELISA | ELISA Units (EU/mL) vs. internal reference | Excellent correlation | Calculated equivalent value | GMMA-based vaccine trials |
| Walter Reed Army Institute of Research (WRAIR) ELISA | Endpoint titer | Excellent correlation | Calculated equivalent value | Multiple vaccine candidates |
*Protective threshold established as ≥1,600 anti-S. sonnei LPS IgG at day 17 post-vaccination, associated with 73.6% vaccine efficacy [33].
The excellent correlation observed between different ELISA methodologies in Shigella research demonstrates that properly standardized assays can generate comparable data, facilitating vaccine development and licensure [33]. Such bridging studies are particularly valuable when international standard sera are not yet available, allowing immunological bridging to other populations, vaccine formulations, or platforms.
Essential Reagents and Research Solutions
Table 3: Research Reagent Solutions for ELISA-Based Humoral Immunity Assessment
| Reagent/Category | Function | Key Considerations |
|---|---|---|
| Solid Phase | Provides surface for antigen or antibody immobilization | 96-well polystyrene plates; high protein-binding capacity; uniform well dimensions |
| Coating Antigens | Target for antibody detection in sample | Peptide purity >90%; correct folding/conformation; lyophilized for stability |
| Detection Antibodies | Enzyme-conjugated antibodies for signal generation | Species specificity; minimal cross-reactivity; HRP or AP conjugation |
| Reference Standards | Quantitative calibration of assay | International standards if available; in-house reference sera characterized for stability |
| Enzyme Substrates | Chromogenic or chemiluminescent signal generation | TMB (colorimetric) for HRP; pNPP for AP; sensitivity and dynamic range |
| Blocking Buffers | Prevent non-specific binding | BSA, non-fat milk, or commercial protein blockers; compatibility with antigens |
| Sample Diluents | Matrix for serum/plasma samples | Maintain antibody stability; minimize background; protein-based with preservatives |
| Plate Washers | Remove unbound materials | Consistent washing pressure; complete well coverage; minimal cross-contamination |
| Microplate Readers | Absorbance measurement | Accurate wavelength selection; sensitivity across dynamic range; data export capabilities |
Visualization of ELISA Workflow and Data Analysis
ELISA Experimental Workflow
ELISA Data Analysis Process
ELISA methodologies provide robust, quantitative tools for assessing antigen-specific antibody titers in peptide-based vaccine development. The selection of appropriate formats—whether indirect, sandwich, or competitive ELISA—depends on the specific vaccine antigens, available reagents, and required sensitivity. Standardization through bridging studies and implementation of rigorous data analysis protocols, including 4-parameter logistic curve fitting, enables reliable comparison of immunogenicity data across vaccine candidates and clinical trials. As vaccine technologies evolve, particularly in the realm of synthetic peptide vaccines, ELISA remains an essential component in the immunogenicity assessment toolkit, providing critical data to establish correlates of protection and guide vaccine development decisions.
For researchers and drug development professionals, predicting and mitigating the immunogenicity of biotherapeutic proteins, such as monoclonal antibodies and protein-based vaccines, is a critical challenge. Unwanted immune responses can lead to the production of anti-drug antibodies (ADAs), which may compromise drug efficacy, alter pharmacokinetics, or cause adverse safety events [40] [41]. The process is initiated when antigen-presenting cells (APCs) internalize a therapeutic protein, process it into peptide fragments, and present these on Human Leukocyte Antigen (HLA) class II molecules for recognition by CD4+ T-cells. This presentation is a prerequisite for triggering an adaptive immune response [40] [42]. Two key in vitro assays used in preclinical immunogenicity risk assessment are MHC-Associated Peptide Proteomics (MAPPs) and HLA-binding assays. This guide provides an objective comparison of these technologies, detailing their methodologies, performance, and appropriate applications within a comprehensive immunogenicity assessment framework.
While both assays investigate peptide-HLA interactions, they operate on fundamentally different principles. MAPPs assays provide a holistic, empirical view of the entire antigen processing and presentation pathway. They identify the exact peptide sequences from a therapeutic protein that are naturally processed by dendritic cells and presented on HLA class II molecules [40] [43]. In contrast, HLA-binding assays are reductionist and mechanistic, measuring the binding affinity of synthetically derived peptides to HLA molecules, typically without the cellular context of protein processing [41] [43].
The table below summarizes the core characteristics of each assay.
Table 1: Core Characteristics of MAPPs and HLA-Binding Assays
| Feature | MAPPs Assay | HLA-Binding Assay |
|---|---|---|
| Primary Objective | Identify naturally processed and presented peptides | Measure binding affinity of predefined peptides to HLA molecules |
| Cellular Context | Uses live antigen-presenting cells (e.g., moDCs) | Typically cell-free; uses purified HLA molecules |
| Antigen Form | Full-length, native protein | Synthetic peptides (usually 15-mers or 9-mer cores) |
| Key Output | Set of presented peptide sequences & "hotspot" clusters | Binding affinity (IC50) or percentile rank |
| Throughput | Lower, resource-intensive | Higher, amenable to screening |
| Incorporates Antigen Processing | Yes | No |
Experimental Protocols and Workflows
Standardized MAPPs Assay Workflow
A robust MAPPs protocol involves multiple critical steps over several days [40] [41] [44].
- Donor Selection and APC Differentiation: Peripheral blood mononuclear cells (PBMCs) are isolated from HLA-typed healthy donors to ensure population-representative HLA coverage. CD14+ monocytes are magnetically isolated and differentiated into monocyte-derived dendritic cells (moDCs) over 5-7 days using cytokines like IL-4 and GM-CSF [40] [45].
- Therapeutic Protein Exposure: Differentiated moDCs are pulsed with the full-length therapeutic protein at a relevant concentration (e.g., 0.33 µM). The cells are simultaneously matured using an agent like lipopolysaccharide (LPS) to mimic an immunogenic environment [40] [44].
- Cell Lysis and HLA Immunoprecipitation: After ~18 hours, cells are harvested and lysed. HLA class II-peptide complexes are isolated from the lysate using immunoprecipitation with monoclonal antibodies against HLA-DR, -DP, and -DQ conjugated to magnetic beads. Bead type (e.g., streptavidin, NHS-activated) can impact peptide recovery and is an area of protocol optimization [40] [44].
- Peptide Elution and Purification: Bound peptides are dissociated from the HLA complexes under mild acidic conditions and purified via solid-phase extraction [40].
- LC-MS/MS Analysis and Identification: The eluted peptides are analyzed using high-resolution liquid chromatography-tandem mass spectrometry (LC-MS/MS). The resulting spectra are searched against a database containing the human proteome and the sequence of the therapeutic protein to identify drug-derived peptides, typically with a <1% false discovery rate (FDR) [40] [45].
The following diagram illustrates this multi-step workflow.
HLA-Binding Assay Workflow
HLA-binding assays follow a more direct path [41] [43].
- Peptide Selection: A set of overlapping peptides (e.g., 15-mers overlapping by 10-12 amino acids) spanning the entire sequence of the therapeutic protein is synthesized.
- Competitive Binding Assay: Each peptide is incubated with a purified HLA molecule and a labeled reporter peptide known to bind that allele with high affinity.
- Quantification: The displacement of the reporter peptide is measured, and the peptide's binding affinity is calculated and expressed as an IC50 value or a percentile rank compared to a set of reference peptides.
Performance and Application Data
Comparative Strengths and Limitations
The choice between MAPPs and HLA-binding assays depends on the stage of drug development and the specific question being addressed.
Table 2: Performance Comparison of Immunogenicity Assays
| Aspect | MAPPs Assay | HLA-Binding Assay | In Silico Prediction |
|---|---|---|---|
| Biological Relevance | High (includes cellular processing) | Moderate (measures binding only) | Low (algorithmic prediction) |
| Risk of Over-prediction | Low | Moderate | High [43] |
| Identification of 'Hotspots' | Directly identifies clustered regions [40] | Indirect, based on dense binding regions | Indirect, based on predicted binders |
| Correlation with T-cell Assays | Strong correlation demonstrated [41] [42] | Variable correlation | Poor to variable correlation |
| Typical Application | Candidate ranking, mechanistic root-cause analysis [40] [42] | High-throughput screening of peptide libraries | Early-stage sequence design |
| Resource Requirement | High (cost, time, expertise) [41] | Moderate | Low |
Supporting Experimental Data
Case studies and published data highlight the complementary nature of these assays.
- Clinical Correlation with MAPPs: A study analyzing six marketed mAbs (e.g., infliximab, adalimumab, nivolumab) found that the number and clustering of drug-derived peptides identified by MAPPs correlated with clinical ADA incidence. Infliximab and adalimumab, known to be highly immunogenic, yielded the most extensive peptide presentation, while nivolumab, with low clinical ADA, showed minimal peptide presentation [40].
- De-immunization of Vatreptacog Alfa: The immunogenic FVIIa variant, Vatreptacog Alfa, was re-engineered. MAPPs analysis showed that the de-immunized variants (DI-1 and DI-2) presented fewer peptides from known immunogenic clusters than the original variant, a finding consistent with their reduced T-cell responses in proliferation assays [45] [46].
- Validation of In Silico Predictions: A study on the SARS-CoV-2 spike protein found a low correlation between peptides presented by dendritic cells in a MAPPs assay and those predicted by in silico algorithms to be dominant HLA-II binders. This underscores the value of empirical MAPPs data in validating or correcting computational predictions [46].
The Scientist's Toolkit: Key Research Reagents and Materials
Successful execution of these assays relies on specific, high-quality reagents.
Table 3: Essential Research Reagents for Antigen Presentation Assays
| Reagent / Material | Function | Example Application |
|---|---|---|
| HLA-Typed PBMCs | Source of primary human antigen-presenting cells; ensures population diversity. | Differentiated into moDCs for MAPPs; used as a source of HLA for binding assays [40] [45]. |
| Cytokines (IL-4, GM-CSF) | Drives the differentiation of monocytes into immature dendritic cells. | Critical step in the 5-7 day moDC generation protocol for MAPPs [40] [44]. |
| Anti-HLA Class II Antibodies | Immunoprecipitation of HLA-peptide complexes from cell lysates. | Pan-HLA-II antibodies (e.g., against DR, DP, DQ) are conjugated to beads for complex isolation in MAPPs [40] [47]. |
| Magnetic Beads | Solid support for immunoprecipitation. | Streptavidin or NHS-activated magnetic beads are used to bind antibody-conjugated HLA complexes [44]. |
| High-Resolution Mass Spectrometer | Identifies and sequences eluted peptides. | Instruments like the TimsTOF SCP or Orbitrap series are used for LC-MS/MS analysis in MAPPs [40] [45]. |
| Purified HLA Molecules | The target for binding measurements in biochemical assays. | Used in competitive binding assays to determine peptide affinity [41]. |
| Pyrene-d10 | Pyrene-d10, CAS:1718-52-1, MF:C16H10, MW:212.31 g/mol | Chemical Reagent |
| UK-78282 hydrochloride | UK-78282 hydrochloride, CAS:136647-02-4, MF:C29H36ClNO2, MW:466.1 g/mol | Chemical Reagent |
Integrated Data Analysis and Interpretation
MAPPs Data Analysis Pipeline
The raw data from a MAPPs experiment undergoes a rigorous analytical process:
- Quality Control: Peptide length distribution (expected unimodal peak at 15-16 amino acids) and motif deconvolution are used to confirm the enrichment of bona fide HLA class II peptides [40].
- Peptide Annotation and Clustering: Identified peptides are mapped back to the therapeutic protein sequence. Peptides often accumulate in specific sequence regions known as "clusters," which are considered immunogenic "hotspots" [40] [42].
- Donor Variability and HLA Restriction: Analysis across multiple donors reveals patterns of presentation linked to specific HLA alleles, enabling HLA-aware risk stratification for different patient populations [40] [47].
Pathway to T-Cell Activation
The ultimate goal of identifying presented or binding peptides is to understand their potential to activate T-cells. The following pathway illustrates this immunological cascade, showing where MAPPs and HLA-binding assays provide critical data.
MAPPs and HLA-binding assays are not mutually exclusive but are powerful components of an orthogonal immunogenicity assessment strategy. HLA-binding assays, with their higher throughput, are ideal for the initial screening of large peptide libraries or during early protein engineering to rapidly eliminate sequences with high HLA-binding affinity. The MAPPs assay, with its higher biological fidelity, is unparalleled for ranking lead candidates, investigating the root causes of clinical immunogenicity, and validating the impact of sequence modifications or product-related factors (e.g., aggregates, glycosylation) on antigen presentation [41] [42].
The future of preclinical immunogenicity assessment lies in the intelligent integration of these methods. Using in silico tools for initial scans, followed by HLA-binding assays for targeted screening, and culminating in MAPPs analysis for critical candidates, creates a robust and efficient workflow. Emerging technologies, such as monoallelic HLA-DR cell platforms [47] and advanced deep learning models like HLAIIPred [48], promise to further refine the resolution and predictive power of these analyses, ultimately enabling the development of safer and more effective biotherapeutics and peptide-based vaccines.
Peptide immunoarrays represent a powerful high-throughput technology that has revolutionized epitope mapping—the process of identifying the precise regions on antigens that are recognized by the immune system. These arrays function by arranging thousands of unique peptide sequences on a solid surface, enabling simultaneous screening of antibody binding events across a vast potential epitope space [49] [50]. The fundamental principle resembles a traditional enzyme-linked immunosorbent assay (ELISA) but with massively parallel capacity, where peptides affixed to a solid phase are reacted with serum, plasma, or purified antibodies, and antigen-antibody complexes are detected using reporter-conjugated secondary antibodies [50]. This technology has become an indispensable tool for global characterization of antibody populations, mapping antigenic determinants of proteins, profiling antibody signatures, and discovering disease biomarkers across infectious diseases, autoimmune disorders, and cancer research [49] [50].
The significance of epitope mapping extends to multiple therapeutic areas, particularly in vaccine development, where identifying precise B-cell and T-cell epitopes enables rational vaccine design. For peptide-based vaccines, understanding which linear epitopes elicit protective immune responses allows researchers to construct multi-epitope vaccines targeting specific pathogens or cancer antigens [36]. Recent advances in array technology now permit unprecedented resolution, with ultrahigh-density peptide microarrays containing up to hundreds of thousands of different peptides per array, enabling exhaustive length and substitution analysis for detailed specificity profiling [51]. This high-throughput capacity replaces traditional resource-intensive experiments, dramatically accelerating the epitope discovery process while providing comprehensive insights into immune recognition patterns [49].
Technology Comparison: Peptide Immunoarrays Versus Alternative Methods
Comparative Analysis of Epitope Mapping Techniques
Table 1: Comparison of key epitope mapping technologies and their characteristics
| Method | Throughput | Epitope Types Detected | Sensitivity | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Peptide Immunoarrays | High (Thousands of peptides/assay) | Linear B-cell and T-cell epitopes | High with fluorescence/chemiluminescence detection | Comprehensive profiling, high reproducibility, customizable content | Limited to linear epitopes, peptide synthesis costs |
| ELISA | Low to Medium (Single to dozens of peptides/assay) | Primarily linear epitopes | Moderate (Nanogram range) | Well-established, accessible, quantitative | Low throughput, limited multiplexing capability |
| Chemiluminescent Immunoassay (CLIA) | Medium to High | Linear and conformational epitopes | High (Picogram range) | Automation-friendly, wide dynamic range | Specialized equipment required, higher cost per test |
| Radioimmunoassay (RIA) | Low | Linear epitopes | High (Picogram range) | Extreme sensitivity for low-abundance targets | Radioactive materials require special handling, safety concerns |
| Phage Display | High (Library screening) | Primarily linear epitopes | Variable | Can discover unknown epitopes, in vivo relevance | Library bias, time-consuming screening process |
| Mass Spectrometry | Medium | Linear and conformational epitopes | High with modern instruments | Can identify natural MHC-presented epitopes | Complex instrumentation, requires expertise in data analysis |
Performance Metrics and Experimental Validation
When comparing assay performance, peptide immunoarrays demonstrate distinct advantages in comprehensive epitope profiling. In SARS-CoV-2 serology studies, high-throughput automated immunoassays including CLIAs demonstrated sensitivities exceeding 97% from 14 days post-symptom onset, with excellent agreement (kappa scores >0.9) between different platforms [52] [53]. However, these commercial assays typically focus on a limited set of antigenic targets, whereas peptide immunoarrays can simultaneously evaluate the entire proteome of a pathogen. For instance, researchers have developed arrays representing the complete proteome of SARS-CoV-2 plus four other pathogenic human coronaviruses, enabling unprecedented comparison of immune responses across related pathogens [50].
The resolution capability of modern peptide immunoarrays is particularly impressive. Using ultrahigh-density platforms generating several hundred thousand different peptides per array, researchers can perform exhaustive length and substitution analysis, obtaining detailed descriptions of antibody specificities [51]. These studies have revealed that antibody epitopes typically range from 4 to 12 amino acids in size and frequently disallow even single conservative substitutions, demonstrating exquisite specificity [51]. This high-resolution mapping enables identification of multiple distinct epitopes for the same target protein, facilitating generation of paired antibodies for enhanced diagnostic or therapeutic applications [51].
For cytokine profiling—a critical component of immunogenicity assessment—technologies like Meso Scale Discovery (MSD) demonstrate superior sensitivity with low detection limits and broad dynamic ranges, while cytometric bead arrays (CBA) and Luminex platforms offer excellent performance for high-throughput screening with multiplexing capability [54]. These technologies complement peptide immunoarrays by providing functional data on immune activation following epitope recognition.
Experimental Protocols and Methodologies
Peptide Immunoarray Workflow
Table 2: Key research reagents and solutions for peptide immunoarray experiments
| Reagent Category | Specific Examples | Function in Experiment |
|---|---|---|
| Array Platforms | Ultrahigh-density peptide microarrays | Solid support presenting peptide sequences for antibody binding |
| Detection Reagents | Fluorescent-conjugated secondary antibodies | Signal generation for bound primary antibodies |
| Cell Culture Components | DC2.4 cell line (immortalized murine dendritic cells) | Antigen presentation and T-cell activation studies |
| Buffer Systems | PBS, HEPES, blocking buffers (BSA, milk) | Maintain pH, ionic strength, reduce non-specific binding |
| Analysis Software | EPIphany, GenePix Pro, FlowJo | Data extraction, normalization, visualization, and statistical analysis |
| Flow Cytometry Antibodies | Anti-CD40, MHC-II, CD80, CD86, CD11c | Dendritic cell maturation marker detection |
Detailed Protocol for Epitope Mapping Using Peptide Immunoarrays
The standard workflow for epitope mapping using peptide immunoarrays begins with array design and fabrication. Peptides are typically 14-26 amino acids in length and can represent overlapping sequences covering specific proteins of interest, random sequences for unbiased immunosignature discovery, or targeted variants for fine specificity mapping [50]. Modern arrays can contain up to 2,000,000 individual peptides, enabling proteome-wide epitope mapping [51]. The peptides are synthesized directly on the array surface or spotted onto functionalized glass slides using robotic arrayers.
For sample processing, serum, plasma, or purified antibodies are diluted in appropriate blocking buffers and incubated with the array surface. Typical incubation conditions range from 2-24 hours at temperatures between 4°C and 37°C, depending on the antibody affinity and kinetics being studied [50] [51]. Following extensive washing to remove unbound antibodies, detection is achieved using fluorophore- or enzyme-conjugated secondary antibodies specific to the antibody isotype of interest. For fluorescence detection, commonly used fluorophores include Cy3, Cy5, or Alexa Fluor dyes, while chemiluminescent detection employs horseradish peroxidase (HRP) or alkaline phosphatase (AP) systems [50].
Data acquisition utilizes microarray scanners for fluorescence-based arrays or chemiluminescence imagers for corresponding detection methods. The resulting images are processed using specialized software such as GenePix Pro to extract foreground and background intensity values for each peptide spot [50]. Data analysis involves multiple steps including background subtraction, normalization across arrays, and statistical analysis to identify significantly bound peptides. Tools like EPIphany provide user-friendly interfaces for these analyses, offering various normalization options and visualization methods to facilitate biological interpretation [50].
For in vitro validation of immunogenicity identified through peptide arrays, dendritic cell activation assays provide crucial functional data. The DC2.4 immortalized murine dendritic cell line offers a standardized model for this purpose [55]. In this protocol, DC2.4 cells are cultured in RPMI-1640 medium supplemented with 10% fetal bovine serum, HEPES buffer, L-glutamine, non-essential amino acids, penicillin-streptomycin-glutamine, and 2-mercaptoethanol [55]. Peptide antigens are added to the culture, and after incubation, cells are analyzed for surface maturation markers (CD40, MHC-II, CD80, CD86) via flow cytometry and cytokine secretion (TNF-α, IL-10) via ELISA or multiplex assays [55]. This comprehensive assessment provides a cost-effective proxy for antigen presentation efficacy before advancing to in vivo studies.
Structural Epitope Mapping and Visualization
Advanced structural analysis has become increasingly accessible through resources like the Immune Epitope Database (IEDB)-3D 2.0, which provides tools for mapping epitopes onto three-dimensional structures of their source antigens [56]. This platform integrates experimental structures from the Protein Data Bank (PDB) and predicted models from AlphaFold, enabling researchers to visualize epitopes in structural context even when experimental structures are unavailable [56]. The system employs a mapping algorithm that uses data from the Structure Integration with Function, Taxonomy, and Sequence (SIFTS) project for residue-level mapping between UniProt and PDB entries, applying a 20% identity cutoff to ensure meaningful epitope-structure alignment [56]. This structural perspective is invaluable for understanding how linear epitopes correspond to surface accessibility and for designing epitope-based vaccines that target functionally relevant sites.
Computational Integration and AI-Driven Prediction
The growing integration of artificial intelligence with experimental epitope mapping has significantly enhanced prediction accuracy and efficiency. Modern AI tools, particularly convolutional neural networks (CNNs) and graph neural networks (GNNs), have demonstrated remarkable performance in epitope prediction, with some models achieving 87.8% accuracy (AUC = 0.945) for B-cell epitope prediction—a 59% improvement in Matthews correlation coefficient over traditional methods [57]. For T-cell epitope prediction, the MUNIS framework shows 26% higher performance than previous algorithms and has successfully identified novel CD8+ T-cell epitopes that were experimentally validated through HLA binding and T-cell assays [57].
These AI approaches learn complex sequence and structural patterns from large immunological datasets, enabling them to discover nonlinear correlations between amino acid features and immunogenicity that traditional motif-based methods miss [57]. The practical impact is substantial; for example, AI-optimized spike protein antigens for SARS-CoV-2 vaccines have demonstrated up to 17-fold higher binding affinity for neutralizing antibodies while maintaining broad-spectrum neutralization against multiple viral variants [57]. This synergy between computational prediction and experimental validation creates a powerful feedback loop that accelerates epitope discovery and vaccine design.
Diagram 1: Integrated workflow for epitope discovery combining computational prediction, high-throughput screening, and experimental validation
Application in Vaccine Development: A Case Study
The practical application of peptide immunoarrays in vaccine development is exemplified by recent work on triple-negative breast cancer (TNBC). Researchers employed an immunoinformatics pipeline to identify immunodominant epitopes from TNBC-associated proteins including MZF-1, Mucin-1, SOX-9, Keratin 5, Keratin 14, Twist1, and Progranulin [36]. Using peptide array technology complemented by AI prediction tools, they identified 13 CD8+ cytotoxic T lymphocyte (CTL) epitopes, 13 CD4+ helper T lymphocyte (HTL) epitopes, and 7 B-cell epitopes based on favorable immunogenic properties and high HLA promiscuity [36].
These epitopes were incorporated into multi-epitope vaccine constructs using different adjuvants (GM-CSF, β-defensin, IL-2, cholera enterotoxin, and 50S ribosomal protein L7/L12) enhanced with PADRE and HEYGAEALERA sequences [36]. Constructs V1 (GM-CSF-linked) and V5 (β-defensin-linked) exhibited superior TLR2/4 docking affinity in computational models, while immune simulations showed that V2 and V5 induced strong cytokine release and memory cell responses [36]. Subsequent in vitro validation using MDA-MB-231 cells demonstrated enhanced expression of MZF-1, SOX-9, and Twist1, confirming epitope-driven immune activation [36]. This integrated approach demonstrates how peptide immunoarray technology fits within a comprehensive vaccine development pipeline, from initial epitope discovery to final vaccine candidate validation.
Peptide immunoarrays have established themselves as a cornerstone technology for high-throughput epitope mapping, offering unparalleled capacity for comprehensive antibody profiling. When compared to traditional methods like ELISA, RIA, and CLIA, immunoarrays provide superior throughput and mapping resolution, though they are often complemented by these other techniques for validation and functional assessment. The integration of AI-driven prediction tools with experimental array data has created a powerful synergy that accelerates epitope discovery, while standardized in vitro validation assays using dendritic cell lines provide cost-effective screening before advancing to animal studies.
As the field continues to evolve, several trends are shaping the future of peptide immunoarrays. The increasing availability of structural data through resources like IEDB-3D and AlphaFold integration enables more informed epitope selection based on structural context [56]. Meanwhile, advances in array density and detection sensitivity continue to push the boundaries of mapping resolution [51]. For researchers developing peptide-based vaccines, these technologies collectively provide an robust toolkit for identifying immunogenic epitopes, constructing multi-epitope vaccines, and evaluating immunogenicity through standardized in vitro assays—ultimately accelerating the development of novel immunotherapeutics for infectious diseases, cancer, and other challenging conditions.
Dendritic cells (DCs) are professional antigen-presenting cells that play a critical role in initiating and modulating adaptive immune responses, making their activation profile a central focus in therapeutic areas like vaccine development [58]. Upon encountering pathogens, damaged cells, or vaccine antigens, DCs undergo a complex maturation process characterized by distinct changes in surface marker expression and cytokine secretion [59]. These changes enable DCs to effectively present antigens and provide the co-stimulatory signals necessary for T-cell activation and differentiation.
The evaluation of DC activation is particularly crucial in the context of immunogenicity assessment for peptide-based vaccines. Product-related factors, including impurities and structural modifications, can significantly impact a therapeutic product's immunogenicity risk profile [2]. Therefore, robust in vitro assays that accurately characterize DC activation states are essential tools for predicting immune responses and optimizing vaccine design. This guide provides a comparative analysis of experimental approaches and readouts for monitoring DC activation, with specific application to immunogenicity testing of peptide-based therapeutics.
Surface Marker Expression During Dendritic Cell Activation
During maturation, DCs significantly upregulate surface molecules essential for their antigen-presenting and T-cell priming functions. The specific markers and their expression levels can vary depending on the DC subset and the nature of the activating stimulus.
Key Activation Markers and Their Functions
Table 1: Key Dendritic Cell Surface Markers and Their Changes Upon Activation
| Marker | Steady-State Expression | Activated-State Expression | Primary Function |
|---|---|---|---|
| MHC Class II | Moderate | Strongly Upregulated [60] | Antigen presentation to CD4+ T cells |
| CD83 | Low/Absent | Strongly Upregulated [60] | Co-stimulation; stabilizes MHC II and CD86 [60] |
| CD86 | Low | Strongly Upregulated [60] | Co-stimulation via CD28/CTLA-4 on T cells [61] |
| CCR7 | Low | Strongly Upregulated [62] | Migration to lymph nodes via CCL19/CCL21 gradients [59] |
| CD80 | Low | Upregulated | Co-stimulation via CD28/CTLA-4 on T cells |
| CD40 | Low | Upregulated | T-cell co-stimulation via CD40L binding |
| PD-L1 | Variable | Upregulated (in some contexts) [59] | Immunoregulatory function; dampens T-cell responses |
DC Subsets and Specific Markers
The DC family is heterogeneous, and different subsets can be identified by specific marker combinations. The table below outlines the classic surface markers used to identify major human DC subsets, which is critical for designing assays that target the relevant population for a given therapeutic context.
Table 2: Classic Surface Markers for Identifying Human Dendritic Cell Subsets
| Marker | cDC1 | cDC2 | pDC | Langerhans Cells | Mo-DC |
|---|---|---|---|---|---|
| CD141 (BDCA-3) | High | Low/Absent | Absent | Low/Absent | Low/Absent |
| CD1c (BDCA-1) | Absent | High | Absent | Low/Absent | Low/Absent |
| CD11c | High | High | Low/Absent | Positive | Positive |
| MHC II | High | High | Positive/High | High | High |
| CD123 | Low/Absent | Low/Absent | High | Absent | Low/Absent |
| CD303 (BDCA-2) | Absent | Absent | High | Absent | Absent |
| CD207 (Langerin) | Low/Absent | Absent | Absent | High | Absent |
| CD1a | Absent | Low/Absent | Absent | High | Low/Absent |
Note: cDC = conventional DC; pDC = plasmacytoid DC; Mo-DC = monocyte-derived DC. Adapted from [58].
A recently identified regulatory module, mature DCs enriched in immunoregulatory molecules (mregDCs), exhibits a distinct marker profile. These cells, which can arise in various contexts including tumors, consistently express LAMP3, CCR7, and often PD-L1, while lacking key lineage markers for cDC1s (XCR1, CLEC9A) and cDC2s (CD1C, FCER1A) [59]. The presence of such subsets underscores the complexity of DC activation beyond the classical maturation paradigm.
Cytokine Secretion Profiles of Activated Dendritic Cells
The cytokine milieu produced by activated DCs is a major determinant of the polarization of subsequent T-cell responses. The profile is heavily influenced by the activation stimulus.
- Inflammatory/TLR-Mediated Activation: Stimulation via Toll-like receptors (TLRs) with compounds like LPS (TLR4) or poly(I:C) (TLR3) typically triggers a pro-inflammatory cytokine signature. This includes the production of IL-12, which is critical for driving T-helper 1 (Th1) and cytotoxic T-cell responses, as well as TNF-α and IL-6 [62].
- Regulatory/Tolerogenic Profiles: In certain contexts, such as steady-state migration or exposure to immunoregulatory signals, DCs may mature without producing high levels of pro-inflammatory cytokines. These cells can secrete cytokines like IL-10, which promotes tolerogenic or regulatory T-cell responses [59].
- Impact of Physical Cues: Recent research shows that physical signals alone can reprogram DC transcription. Confinement-induced nuclear deformation can activate an ARP2/3–cPLA2–NF-κB pathway, leading to CCR7 upregulation, but this "shape-sensing" mechanism reprograms transcription differently than microbial sensing [62].
Experimental Models for Assessing DC Activation
A variety of in vitro models are available to study DC activation, ranging from simple 2D cultures to more complex 3D tissue-engineered systems.
Standard In Vitro Protocols
Protocol 1: Generating Monocyte-Derived Dendritic Cells (Mo-DCs) for Activation Assays
This is a widely used protocol to generate human immature DCs for downstream activation studies [61].
- Isolation: Isolate CD14+ monocytes from human peripheral blood mononuclear cells (PBMCs) using positive selection.
- Differentiation: Culture monocytes (e.g., 2x10^5 cells/mL) in complete RPMI medium supplemented with:
- 1000 U/mL rhGM-CSF
- 400 U/mL rhIL-4
- Incubation: Incubate cells for 5-7 days at 37°C and 5% CO2. Refresh cytokines on day 3 or 4.
- Validation: Confirm differentiation into immature DCs (iDCs) by flow cytometry. iDCs should exhibit high CD1a and MHC II expression, and low-to-absent levels of CD14 and CD83.
Protocol 2: Activating DCs with Model Stimuli
- Stimulation: Treat iDCs with a chosen stimulus.
- Positive Control (Inflammatory Maturation): 100 ng/mL LPS for 24 hours.
- Test Article: Co-culture with the peptide-based vaccine candidate or its components at relevant concentrations for 24-48 hours.
- Negative Control: Culture in medium alone.
- Analysis: Harvest cells and supernatant for analysis.
- Surface Markers: Analyze by flow cytometry for CD83, CD86, HLA-DR, and CCR7.
- Cytokines: Quantify IL-12p70, TNF-α, IL-10, IL-6 in culture supernatant via ELISA or multiplex immunoassay.
Advanced 3D Tissue-Engineered Models
For a more physiologically relevant context, full-thickness human skin tissue equivalents can be engineered. These models incorporate DC surrogates in both the epidermal and dermal compartments.
- LC Surrogates: Differentiate from the Mutz-3 cell line using cytokines (rhGM-CSF, TGF-β, TNF-α) over 9 days to generate CD1a+ CD207+ cells [61].
- DDC Surrogates: Differentiate from THP-1 cell line using rhGM-CSF and IL-4 over 5 days to generate CD11c+ immature DCs [61].
- Model Assembly: Seed primary human keratinocytes together with the DC surrogates onto a fibroblast-populated collagen matrix to form a stratified epidermis [61].
- Application: Topically apply sensitizers (e.g., NiSO4, DNCB) or test articles to the model. Analyze DC activation by monitoring migration out of the epidermis and marker upregulation (CD83, CD86, HLA-DR) via immunohistochemistry or flow cytometry after tissue dissociation [61].
Signaling Pathways in Dendritic Cell Activation
The process of DC activation is governed by intricate signaling pathways. The diagram below illustrates the key pathway identified in DC mechanosensing, which leads to specific activation features like CCR7 upregulation.
Diagram Title: DC Shape-Sensing Pathway for CCR7 Upregulation
This pathway, activated by specific nuclear deformation, operates alongside canonical activation pathways (e.g., TLR-NF-κB) but results in a distinct transcriptional program, highlighting how different stimuli can license DCs for specific functions [62].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying Dendritic Cell Activation
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Cytokines for Differentiation | rhGM-CSF, rhIL-4 [61] | Generate monocyte-derived immature DCs (mo-DCs) from primary monocytes or cell lines. |
| Activation Stimuli | LPS, poly(I:C), Resiquimod (R848) [63] | Positive controls for inducing inflammatory DC maturation via TLR pathways. |
| Flow Cytometry Antibodies | Anti-human CD83, CD86, HLA-DR, CD1c, CD141, CCR7 [58] [61] | Quantify surface marker expression and identify DC subsets. |
| Cytokine Detection Kits | ELISA/Multiplex Kits for IL-12p70, TNF-α, IL-10, IL-6 | Measure secreted cytokine profiles in cell culture supernatants. |
| Cell Culture Models | Mutz-3 cell line [61], THP-1 cell line [61], Primary CD14+ Monocytes | Sources for generating Langerhans cell and dermal DC surrogates for in vitro models. |
| Pathway Inhibitors | AACOCF3 (cPLA2 inhibitor) [62] | Tool for probing the role of specific signaling pathways in DC activation. |
| VU6007477 | VU6007477, MF:C24H26N6O2, MW:430.5 g/mol | Chemical Reagent |
| VU6012962 | VU6012962, MF:C21H19F3N4O4, MW:448.4 g/mol | Chemical Reagent |
Assay Challenges and Strategic Optimization for Reliable Immunogenicity Data
Peptide-based vaccines represent a promising frontier in immunology, offering advantages in safety and precise antigen targeting. However, a significant challenge impedes their clinical translation: low immunogenicity. Unlike whole-pathogen vaccines, short peptide sequences are often poorly immunogenic, failing to elicit robust and durable adaptive immune responses necessary for protective immunity [64]. This deficiency stems from their inability to efficiently activate antigen-presenting cells (APCs), provide adequate T-cell co-stimulation, or overcome major histocompatibility complex (MHC) restriction [65]. Consequently, overcoming this hurdle requires sophisticated adjuvant systems and delivery platforms that can enhance and direct immune responses. Among the most promising innovations are Spherical Nucleic Acids (SNAs), which represent a convergence of nanotechnology and immunology to create nanostructures capable of codelivering antigens and immunostimulatory molecules with precise architectural control [66]. This guide provides a comparative analysis of adjuvant platforms, with a focus on SNAs, to inform strategic decisions in peptide vaccine design and evaluation through in vitro assays.
Adjuvant Mechanisms and Platforms
Fundamental Mechanisms of Action
Adjuvants enhance vaccine immunogenicity through two primary, often synergistic, mechanisms: acting as delivery systems or as immunostimulants [67].
- Delivery Systems: These function primarily as carrier materials that facilitate antigen presentation. They enhance immunogenicity by prolonging antigen bioavailability, targeting antigens to lymph nodes or APCs, and protecting antigens from premature degradation. Examples include aluminum salts, liposomes, and various nanoparticles [67].
- Immunostimulants: These are typically danger signal molecules that activate innate immunity by targeting pattern recognition receptors (PRRs) on APCs. This activation leads to APC maturation, enhanced antigen presentation (Signal 1), and upregulation of co-stimulatory molecules and cytokines (Signal 2), ultimately driving potent adaptive immune responses [67]. Key PRR families include Toll-like receptors (TLRs), C-type lectin receptors (CLRs), RIG-I-like receptors (RLRs), and NOD-like receptors (NLRs) [68].
The following diagram illustrates how these components work together within a dendritic cell to generate an adaptive immune response.
Comparative Analysis of Adjuvant Platforms
The table below summarizes the key characteristics, mechanisms, and experimental evidence for several advanced adjuvant platforms, including SNAs.
Table 1: Comparison of Advanced Adjuvant Platforms for Peptide Vaccines
| Adjuvant Platform | Composition | Mechanism of Action | Key Immune Responses | Reported Experimental Efficacy (In Vivo) |
|---|---|---|---|---|
| Spherical Nucleic Acids (SNAs) | Liposome or gold nanoparticle core with dense nucleic acid shell (e.g., CpG), conjugated with peptide antigen [66] [65]. | Codelivery of antigen and adjuvant (e.g., TLR9 agonist); enhanced cellular uptake; spatial control over antigen and adjuvant presentation synchronizes APC activation and antigen presentation [66]. | Robust antigen-specific CD8+ T cell activation; high IgG antibody titers; complete tumor elimination in 30% of mice in TC-1 model; immunological memory [66] [65]. | |
| STING Nanoadjuvants (SNA-L/US) | Biodegradable polypeptide conjugated with STING agonist and photo/sonosensitizer [69]. | Spatiotemporally-controlled ROS generation via laser/ultrasound activates NF-κB and STING pathways, amplifying innate immune activation in dendritic cells [69]. | Enhanced DC maturation and antigen-specific CD8+ T cell response; potent antitumor immunity; synergy with immune checkpoint blockade [69]. | |
| TLR4-Agonist Formulations (e.g., LiT4Q, EmT4) | Novel formulations (liposomal, emulsion) containing TLR4 agonists [16]. | Activation of TLR4 signaling pathway on APCs, leading to pro-inflammatory cytokine production and enhanced co-stimulatory marker expression [67]. | Improved strength and breadth of antibody response against viral variants (e.g., SARS-CoV-2 Omicron); effective as protein-adjuvant boost after RNA prime [16]. | |
| Squalane Nano-Emulsion (SNA - Note: Homonym) | Squalane oil, surfactants (Span85, Tween60), PEG400, and CpG in aqueous solution [70]. | Oil-in-water nano-emulsion acts as a delivery system, while CpG acts as a TLR9 immunostimulant, promoting both humoral and cellular immunity [70]. | Significant increase in IgG1 and IgG2a antibodies and IFN-γ/IL-1β in mice; 83.3% protection in guinea pigs challenged with FMDV [70]. |
Spherical Nucleic Acids (SNAs): A Deep Dive
SNA Architectures and Their Impact on Immunogenicity
The structural arrangement of antigen and adjuvant within an SNA is a critical determinant of vaccine efficacy. A seminal study systematically compared three compositionally similar but structurally distinct SNA architectures, differentiated by the position and conjugation chemistry of the peptide antigen [66].
Table 2: Impact of SNA Antigen Architecture on Immune Outcomes
| SNA Architecture | Antigen Position and Conjugation | Antigen Presentation & DC Activation | CD8+ T Cell Cross-Priming | In Vivo Tumor Model Outcome |
|---|---|---|---|---|
| Encapsulated (E) | Soluble antigen encapsulated within the liposome core. | Poor synchronization of antigen presentation and costimulatory marker expression. | Low | Minimal antitumor effect. |
| Anchored (A) | Antigen chemically conjugated to 3'-cholesterol-functionalized oligonucleotides adsorbed to the liposome surface. | Intermediate performance. | Intermediate | Moderate antitumor effect. |
| Hybridized (H) | Anticonjugated to oligonucleotides hybridized to CpG oligonucleotides on the liposome surface. | Superior synchronization of maximum antigen presentation and costimulatory marker expression. | High | Complete tumor elimination in 30% of mice; extended survival; immunological memory. |
Experimental Protocol: Synthesis and In Vitro Evaluation of SNAs
For researchers aiming to develop and test SNA-based vaccines, the following protocol, synthesized from recent studies, provides a detailed methodological roadmap.
Synthesis of SNA with Hybridized (H) Architecture [66] [65]
- Core Formation: Generate unilamellar liposomes (e.g., from dioleoyl-sn-glycero-3-phosphocholine) with an average diameter of 40-45 nm via thin-film hydration and extrusion.
- Oligonucleotide Functionalization: a. For CpG Adjuvant: Use 3'-cholesterol-functionalized TLR9 agonist oligonucleotides (e.g., sequence "1826" for murine TLR9). Adsorb these onto the liposome surface via hydrophobic interactions. b. For Antigen Conjugation: i. Synthesize a peptide-oligonucleotide conjugate where the peptide antigen is linked via a biochemically labile linker (e.g., a disulfide bond) to an oligonucleotide with a sequence complementary to the CpG adjuvant. ii. Hybridize this peptide-oligonucleotide conjugate to the CpG oligonucleotides before or during adsorption to the liposome surface.
- Purification and Characterization: Purify the resulting SNA structures via size exclusion chromatography or centrifugation. Characterize using Dynamic Light Scattering (DLS) for hydrodynamic diameter and zeta potential, and Transmission Electron Microscopy (TEM) for morphology [65]. Ensure a final formulation with a consistent and known ratio of antigen and adjuvant per nanoparticle (e.g., ~75 molecules each per liposome [66]).
In Vitro Assays for Evaluating SNA Immunogenicity [65]
- Cellular Uptake:
- Method: Incubate fluorescently labelled (e.g., Cy5) SNAs with Bone Marrow-Derived Dendritic Cells (BMDCs) for 4-24 hours.
- Analysis: Analyze using flow cytometry or confocal microscopy. Compare against free antigen and adjuvant mixtures. SNAs typically show significantly enhanced and more rapid uptake.
- Dendritic Cell Maturation and Activation:
- Method: Treat BMDCs with SNAs, free component mixtures, and controls (e.g., LPS) for 18-24 hours.
- Analysis: Harvest cells and stain for surface activation markers (CD80, CD86, MHC-II) for analysis by flow cytometry. Collect culture supernatant and quantify secreted pro-inflammatory cytokines (e.g., IL-12p70, TNF-α, IL-6, IL-1β) using ELISA or multiplex bead-based assays.
- Antigen Presentation (Signal 1):
- Method: Use BMDCs that express a specific MHC-I molecule. After pulsing with SNA, incubate them with a T-cell hybridoma reporter cell line that produces a quantifiable readout (e.g., β-galactosidase) upon T-cell receptor engagement with the peptide-MHC-I complex.
- Analysis: Measure the reporter signal (e.g., luminescence for luciferase or colorimetric for β-gal) to quantify the level of antigen presentation.
The workflow for the synthesis and in vitro evaluation is summarized in the following diagram.
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and their functions for synthesizing and evaluating SNA vaccines, based on protocols from the cited research.
Table 3: Essential Reagents for SNA Vaccine Research
| Reagent / Material | Function in SNA Research | Example / Note |
|---|---|---|
| Lipid Components | Forms the nanoparticle core structure for encapsulation or surface functionalization. | Dioleoyl-sn-glycero-3-phosphocholine (DOPC) is used for liposomal SNAs [66]. |
| Cholesterol-modified Oligonucleotides | Anchors nucleic acids (e.g., CpG adjuvant) to the lipid core via hydrophobic insertion. | 3'-cholesterol-functionalized CpG [66]. |
| TLR Agonists | Acts as an immunostimulant by activating PRRs on APCs to provide Signal 2. | CpG ODN (TLR9 agonist) is most common; STING agonists are also used [66] [69] [65]. |
| Peptide Antigen with Labile Linker | The target antigen conjugated for traceless release after cellular internalization. | Contains a disulfide linker or enzymatically cleavable sequence for intracellular antigen release [66]. |
| Bone Marrow-Derived Dendritic Cells (BMDCs) | Primary in vitro model for evaluating APC uptake, maturation, and antigen presentation. | Differentiated from mouse bone marrow progenitors using GM-CSF [65]. |
| T-Cell Hybridoma Reporter Line | In vitro model for quantifying antigen-specific MHC-I presentation. | B3Z hybridoma for OVA/SIINFEKL model [66]. |
| Cytokine Detection Kits | Quantifies secreted cytokines as a measure of DC activation and immune polarization. | ELISA or Luminex kits for IL-12p70, TNF-α, IFN-β [69] [65]. |
| Flow Cytometry Antibodies | Measures surface expression of co-stimulatory molecules and MHC on activated DCs. | Antibodies against CD80, CD86, MHC-I, MHC-II [66] [65]. |
| AQ-RA 741 | AQ-RA 741, CAS:123548-16-3, MF:C27H37N5O2, MW:463.6 g/mol | Chemical Reagent |
The strategic selection of adjuvants and delivery platforms is paramount to overcoming the intrinsic low immunogenicity of peptide-based vaccines. While traditional adjuvants like alum primarily stimulate humoral immunity, next-generation platforms offer refined control over the immune response. Among these, Spherical Nucleic Acids stand out due to their unique modular architecture, which enables synchronized antigen presentation and dendritic cell activation. The structural paradigm of the "Hybridized" (H) SNA, where the antigen is conjugated to an oligonucleotide hybridized with the CpG adjuvant, has demonstrated superior efficacy in inducing cytotoxic T-cell responses and antitumor immunity in preclinical models, outperforming other architectural configurations [66]. This highlights that beyond mere composition, the spatial arrangement of vaccine components is a critical design parameter. For researchers, a systematic approach starting with in vitro assays—evaluating DC uptake, maturation, cytokine secretion, and antigen presentation—provides a critical foundation for selecting the optimal adjuvant platform before advancing to complex in vivo studies.
The evaluation of immunogenicity is a critical step in the development of peptide-based vaccines. In vitro assays provide a controlled environment for assessing the potential of vaccine candidates to elicit immune responses, but their utility depends entirely on the rigor of their design. Two pillars underpin the reliability of these assays: the careful selection of donor cells and the strategic implementation of assay controls. This guide objectively compares methodologies and provides supporting experimental data to help researchers optimize these critical components, thereby enhancing the specificity and reproducibility of immunogenicity assessments for peptide-based vaccines within the broader context of vaccine development research.
Donor Selection: Sourcing a Representative Immune System
The biological relevance of an in vitro immunogenicity assay hinges on the donor-derived cells used in the experiment. The selection criteria directly impact the predictability of the assay for real-world population responses.
Key Donor Characteristics and Their Impact on Assay Outcomes
The table below summarizes the critical donor factors that must be considered and their documented influence on experimental data.
Table 1: Impact of Donor Selection Criteria on Assay Outcomes
| Donor Characteristic | Experimental Impact | Supporting Data |
|---|---|---|
| HLA Haplotype | Determines peptide presentation and T-cell receptor recognition. | A tailored approach for a Colombian population incorporated HLA-I and II haplotypes into the prediction algorithm, enabling identification of immunogenic SARS-CoV-2 peptides [71]. |
| Health Status | Alters baseline immune reactivity and precursor T-cell frequency. | Studies noted a trend of higher Flu-specific T-cell precursors in healthy donors compared to carcinoma patients, and slightly higher CEA-specific responses in cancer patients versus healthy donors [72]. |
| Prior Antigen Exposure | Influences the frequency of memory T and B cells. | Assays on PBMCs from patients pre- and post-vaccination showed expanded memory CD8+ T lymphocytes specific to predicted immunogenic peptides [71]. |
Methodologies for Donor Cohort Assembly
- Diverse HLA Representation: For population-tailored vaccines, donor cohorts should reflect the HLA allele frequencies of the target population. Mathematical frameworks for epitope selection prioritize peptides that provide coverage across a defined set of MHC alleles [73]. In practice, this means sourcing Peripheral Blood Mononuclear Cells (PBMCs) from multiple donors to ensure a representative mix of common HLA class I and II alleles.
- Screening and Stratification: It is critical to use HLA-typed donors. Furthermore, researchers should stratify donors based on relevant clinical history (e.g., disease status, prior vaccination) during data analysis to account for inherent variability in immune repertoires [72]. For cell-based assays investigating off-target toxicity, the availability of HLA information for both PBMCs and target tissue cells is a key characteristic [74].
Assay Controls: Anchoring Data Interpretation
Robust controls are non-negotiable for distinguishing specific vaccine-induced immune responses from non-specific background noise. They validate the assay's performance in every run.
A Comparative Analysis of Essential Assay Controls
The function and implementation of critical controls are detailed in the following table.
Table 2: Types and Applications of Essential Assay Controls
| Control Type | Function | Experimental Protocol Example |
|---|---|---|
| Positive Control | Confirms assay functionality and cell viability. | Using a known immunogenic peptide, such as a Flu 9-mer peptide, to validate T-cell activation in an ELISPOT assay [72]. |
| Negative Control | Measures background noise and non-specific activation. | Using cells cultured with a non-stimulatory media or an irrelevant peptide. The use of a "no antigen" control is implicit in assays comparing pre- and post-vaccination responses [72] [75]. |
| Reference Standard | Enables inter-assay reproducibility and cross-experiment data normalization. | An internal standard was used in each ELISPOT assay to define reproducibility, with all patient samples analyzed simultaneously to minimize run-to-run variability [72]. |
Protocols for Control Implementation
- ELISPOT Assay Protocol: A standardized protocol for assessing peptide-specific T-cell responses involves isolating PBMCs from HLA-typed donors. Cells are cultured in duplicate or triplicate wells with the candidate peptide vaccine (test), a known immunogenic peptide (positive control), or media alone (negative control). After a 24-hour stimulation, the number of interferon-gamma (IFN-γ) secreting cells is quantified. The use of an internal standard and the simultaneous analysis of all samples for a given patient are critical for reproducibility [72].
- In Vitro Comparative Immunogenicity Assessment (IVCIA): This assay uses PBMCs from up to 50 healthy human donors. Over 8 days, it monitors T-cell proliferation, the number of IL-2 or IFN-γ secreting cells (e.g., via ELISPOT), and the concentration of a panel of secreted cytokines. The response to a test biotherapeutic is compared against a benchmark to assess relative immunogenicity risk [75].
Integrated Experimental Workflow
The relationship between donor selection, assay execution, and data interpretation can be visualized in the following workflow. This diagram integrates the critical components discussed to ensure specificity and reproducibility.
Diagram 1: Integrated immunogenicity assessment workflow.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues key reagents and their functions for establishing controlled and reproducible in vitro immunogenicity assays.
Table 3: Essential Reagents for In Vitro Immunogenicity Assays
| Research Reagent | Function in Assay |
|---|---|
| Cryopreserved PBMCs | Provides a standardized, readily available source of human immune cells from characterized donors. |
| HLA Typing Kits | Determines the major histocompatibility complex profile of donor cells, which is critical for epitope presentation. |
| Synthetic Peptide Antigens | Serve as the vaccine candidate test articles, positive controls (e.g., Flu peptide), and irrelevant peptide controls. |
| Recombinant Cytokines & Antibodies | Used in ELISPOT or flow cytometry to capture and detect secreted factors (e.g., IFN-γ) or cell surface markers. |
| Cell Culture Media & Supplements | Provides the necessary nutrients and environment for maintaining cell viability and function during the assay. |
| Adjuvants (e.g., MF59) | Can be incorporated in vitro to model the enhanced immunogenicity provided by adjuvants in vivo [76]. |
The path to a reliable in vitro assessment of peptide vaccine immunogenicity is built upon meticulous donor selection and a rigorous control strategy. By choosing donors whose HLA haplotypes and immune history are relevant to the research question, and by employing a comprehensive suite of controls including a reference standard, researchers can anchor their data in biological relevance and technical robustness. The experimental protocols and comparative data presented here provide a framework for achieving the high levels of specificity and reproducibility required to advance the next generation of epitope-based vaccines.
Peptide-based vaccines represent a promising frontier in immunology, offering a high degree of specificity and synthetic simplicity. However, their development and commercialization face significant challenges related to stability, solubility, and stereo-isomer purity. These physicochemical properties directly influence the safety, efficacy, and immunogenicity of the final vaccine product. For researchers and drug development professionals, navigating these challenges requires a comprehensive understanding of the underlying principles and evidence-based mitigation strategies. This guide provides a comparative analysis of current methodologies and solutions, supported by experimental data, to facilitate the development of robust peptide vaccine formulations, particularly for evaluation in in vitro immunogenicity assays.
Peptide Solubility: Mechanisms and Comparison
Solubility is a critical initial parameter that affects peptide handling, formulation, and bioavailability. It is governed by complex interactions between the peptide backbone and side-chains with the solvent environment [77].
Comparative Solubility of Pentapeptides
Research calculating the solubility limit of pentapeptides in water revealed the following order, which aligns with the solubility of individual amino acid monomers [77]:
Table 1: Solubility Limit and Aggregation Dynamics of Model Pentapeptides
| Peptide Sequence | Solubility Limit Order | Notes on Aggregation Behavior |
|---|---|---|
| GGRGG | Highest | Charged side-chain (Arg); least time spent in aggregated clusters |
| GGDGG | ↑ | Charged side-chain (Asp) |
| GGGGG | ↑ | Reference peptide; no side-chain |
| GGVGG | ↓ | Hydrophobic side-chain (Val) |
| GGQGG | ↓ | Polar side-chain (Gln) |
| GGNGG | ↓ | Polar side-chain (Asn) |
| GGFGG | Lowest | Hydrophobic side-chain (Phe); most time spent in aggregated clusters |
Key findings from this study indicate that fluctuations in conformation and hydration number in the monomeric form are correlated with solubility. Furthermore, backbone carbonyl-carbonyl (CO–CO) interactions were found to be as significant as, or even more important than, traditional interbackbone hydrogen bonds in driving peptide self-assembly and association [77].
Practical Guidelines for Enhancing Solubility
While predictive algorithms are unreliable, several practical strategies can be employed [78]:
- Sequence Analysis: Peptides with a higher number of charged residues (Arg/Lys, Asp/Glu) are more likely to dissolve in pure water.
- pH Adjustment: Solubility can often be improved by shifting the pH away from the peptide's iso-electric point using a base or acid.
- Physical Methods: Gentle heating or sonication can aid dissolution.
- Organic Solvents: For research applications not involving live cells, dissolving the peptide in a small volume of a solvent like DMSO before diluting to the working concentration is a common and effective strategy [78].
Peptide Stability: Thermal and Long-Term Storage
Stability is paramount for vaccine shelf-life, distribution, and accessibility, especially in resource-limited settings that cannot maintain a continuous "cold chain" [79].
Experimental Stability Data for Vaccine Peptides
Significant advances have been made in developing thermally stable peptide vaccines. The following table summarizes experimental findings from stability studies on various peptide vaccine platforms.
Table 2: Experimental Stability of Peptide Vaccine Formulations
| Peptide / Vaccine Platform | Storage Conditions | Key Stability Findings | Analytical Methods | Reference |
|---|---|---|---|---|
| ESAT6â‚–₇₀-Q11 (Self-assembled) | 45°C for 6 months (dry powder & aqueous) | Undiminished immunogenicity; no chemical/conformational changes after 7 days at 45°C | HPLC, Mass Spectrometry | [79] |
| OVA₃₂₃–₃₃₉-Q11 (Self-assembled nanofibers) | 45°C for 6 months (aqueous suspension) | Antibody titers and affinities undiminished in mice | HPLC, Mass Spectrometry, Immunogenicity Assays | [79] |
| Multi-Peptide Melanoma Vaccines (6MHP & 12MP) | +4°C & room temp (~20-22°C) for 3 months (lyophilized) | 17 of 18 peptides stable; 1 peptide showed increased oxidized methionine | HPLC, Mass Spectrometry | [80] |
| Alum-adjuvanted protein carrier | 45°C | Marked thermal sensitivity; lost potency over days/weeks | Immunogenicity Assays | [79] |
These studies highlight the exceptional stability of certain peptide vaccine platforms, particularly self-assembled peptides and lyophilized multi-peptide mixtures, which can retain their integrity and immunogenicity even under stressful thermal conditions [79] [80].
General Storage Guidelines
For long-term storage of research peptides, the recommended best practice is to store them lyophilised, airtight, desiccated, and at -20°C or colder. Under these conditions, peptides are generally stable for several years. Aliquoting is advised to avoid repeated freeze-thaw cycles [78].
Stereo-isomer Purity: Analysis and Control
The enantiomeric purity of synthetic therapeutic peptides is critical for their safety and efficacy. Racemization, the unintended formation of D-isomers, is a common side reaction during solid-phase peptide synthesis (SPPS) or can be introduced via the starting amino acids [81] [82].
Implications of Stereochemical Impurities
The therapeutic effect of a bioactive peptide depends on its amino acid enantiomeric purity and higher-order structure. D-isomeric impurities can be introduced from impure starting materials, during amino acid activation prior to coupling, or in subsequent processing steps [81] [82]. These impurities can potentially alter the biological activity and modulate the immunogenicity of the drug product, making their control essential [83].
Comparison of Analytical Methods for Enantiomeric Purity
Accurate determination of chiral purity faces analytical challenges because D/L isomers have identical physicochemical properties aside from their stereochemical configuration [81]. The table below compares key analytical techniques.
Table 3: Comparison of Analytical Methods for Peptide Enantiomeric Purity
| Method | Principle | Key Steps | Advantages / Applications |
|---|---|---|---|
| Traditional GC-MS or HPLC-MS | Hydrolysis + Derivatization + Separation | 1. Acid hydrolysis2. Chiral derivatization (e.g., Marfey's reagent)3. GC-MS or HPLC-MS analysis | Established methodology; uses commonly available equipment [82] |
| Chiral HPLC-ESI-MS/MS (Advanced method) | Hydrolysis + Direct Chiral Separation | 1. Acid hydrolysis in DCl2. Direct chiral HPLC separation3. ESI-MS/MS detection | Simpler & more robust: No derivatization needed; higher throughput; accurate quantitation down to 0.1% for each D-isomer [82] |
A critical technical aspect of these methods is the use of deuterated solvents (DCl) during hydrolysis. This ensures that any racemization occurring during the hydrolysis step itself results in a +1 mass difference, allowing the mass spectrometer to exclude these artificially generated D-isomers and report only the inherent impurities present in the original sample [82].
The Scientist's Toolkit: Research Reagent Solutions
This table details key reagents and materials essential for experiments focused on peptide stability, solubility, and purity analysis.
Table 4: Essential Research Reagents and Materials
| Item | Function / Application | Example / Note |
|---|---|---|
| Chiral Stationary Phases | Direct enantiomeric separation of underivatized amino acids. | Crownpak, Chiralpak ZWIX [82] |
| Deuterated Solvents (DCl) | Hydrolysis for enantiomeric purity analysis; prevents artifactual racemization. | Enables differentiation of inherent vs. process-generated D-isomers [82] |
| Liposome Formulations | Serve as both adjuvant and delivery system for peptide vaccines; enhance immunogenicity. | Compositions can include POPG, POPC, Cholesterol, Lipid A [84] |
| Lyophilization Excipients | Stabilize peptides during freeze-drying for long-term storage. | Lactated Ringer's solution, salts for osmolarity [80] |
| Fmoc-Protected Amino Acids | Building blocks for standard solid-phase peptide synthesis (SPPS). | Quality is critical to minimize D-isomer impurities [82] |
Experimental Protocols for Key Assays
Protocol 1: Assessing Thermal Stability of Lyophilized Peptide Vaccines
This protocol is adapted from studies demonstrating the stability of multi-peptide vaccines at elevated temperatures [80].
- Preparation: Obtain clinical-grade, lyophilized peptide mixtures (e.g., 6MHP, 12MP) vialed under GMP conditions.
- Storage Conditions: Store lyophilized samples in a light-protected environment at various temperatures (e.g., -80°C, +4°C, room temperature [20-22°C]) for defined durations (e.g., 1 day, 1 week, 1 month, 3 months).
- Reconstitution: After storage, reconstitute each vial with sterile water.
- Analysis by HPLC:
- Inject a 3-μg sample onto a reverse-phase C18 column.
- Use a gradient elution with Solvent A (0.1% Trifluoroacetic Acid) and Solvent B (0.09% TFA in acetonitrile).
- Monitor the effluent by absorbance at 215 nm.
- Assessment: Compare the chromatograms (number of peaks, retention times) to those of a reference standard stored at -80°C.
- Analysis by Mass Spectrometry:
- Collect HPLC fractions and analyze via LC-MS (e.g., Orbitrap system).
- Operate in positive, data-dependent mode for MS and MS/MS acquisition.
- Assessment: Manually examine MS scans for non-background ions. Determine the (M+H)+ mass and confirm the amino acid sequence via MS/MS fragmentation. Check for common modifications like methionine oxidation.
Protocol 2: Direct Chiral HPLC-ESI-MS/MS for Enantiomeric Purity
This protocol outlines the modern, derivatization-free method for quantifying D-isomer impurities [82].
- Hydrolysis:
- Hydrolyze the synthetic peptide sample in Deuterated Chloride (DCl). This step breaks peptide bonds and converts Asn to Asp and Gln to Glu.
- Chiral HPLC Separation:
- Inject the hydrolysate onto a chiral stationary phase (e.g., Crownpak CR-I(+) column).
- Use an isocratic mobile phase of 20 mM Formic Acid in 80:20 Methanol:Water.
- Maintain the column at 25°C.
- ESI-MS/MS Detection:
- Interface the HPLC system with an ESI-MS/MS detector.
- Use Selected Ion Monitoring (SIM) to monitor the protonated molecular ions specific to each D- and L-amino acid.
- Quantitation:
- Use a high-low chromatography strategy. Calculate the percentage of each D-isomer using the formula:
%D = [Area<sub>D</sub> / (Area<sub>D</sub> + Area<sub>L</sub>)] × 100 - The method reporting limit can be validated down to 0.1% for each D-isomer.
- Use a high-low chromatography strategy. Calculate the percentage of each D-isomer using the formula:
Pathways and Workflows
Diagram 1: An integrated workflow diagram illustrating the logical relationships between fundamental peptide properties, the analytical methods used to assess them, the resulting mitigation strategies, and the ultimate outcomes for vaccine development. This framework guides researchers in systematically addressing key challenges.
The successful development of peptide-based vaccines hinges on a rigorous and holistic approach to managing solubility, stability, and stereo-isomer purity. Evidence demonstrates that self-assembling peptides and lyophilized formulations offer superior thermal stability, potentially reducing reliance on the cold chain. Furthermore, modern analytical techniques like chiral HPLC-ESI-MS/MS provide robust and efficient means to control critical quality attributes such as enantiomeric purity. By integrating the comparative data, experimental protocols, and mitigation strategies outlined in this guide, researchers can make informed decisions to advance stable, efficacious, and safe peptide-based vaccines through development and into clinical evaluation.
In the development of peptide-based vaccines and therapeutics, immunogenicity risk assessment is a critical safety requirement. Immunogenicity, defined as the ability of a substance to induce immune responses, presents a significant challenge for peptide drugs and vaccines, potentially impairing their efficacy and safety through undesirable side effects such as systemic allergic or anaphylactic responses [1]. The orthogonal methodology approach employs multiple independent assays to provide a comprehensive risk assessment by cross-validating results through different biological or technical principles, thereby reducing the likelihood of false conclusions from any single method [85].
Regulatory agencies have formally recognized the necessity of orthogonal assessment. The U.S. Food and Drug Administration's (FDA) Abbreviated New Drug Application (ANDA) pathway specifically requires sponsors to use orthogonal methods to demonstrate that proposed generic peptide drugs are immunologically equivalent to their reference listed drugs [1]. This requirement is particularly crucial for assessing peptide impurities, which may introduce novel Human Leukocyte Antigen (HLA)-binding sequences not present in the original drug, potentially driving new immune responses that could compromise product safety [1]. The fundamental principle underlying orthogonal assessment is that combining results from multiple, independent experimental techniques provides verification that strengthens confidence in findings, as corroborating data from unrelated methods helps control bias and delivers more conclusive evidence of specificity and risk [85].
Key Orthogonal Assay Platforms and Methodologies
In Silico and In Vitro T-cell Epitope Screening
A primary orthogonal approach for immunogenicity risk assessment combines in silico screening with in vitro T-cell assays.
- In silico methods utilize computational tools to screen peptide sequences for potential T-cell epitopes by predicting their binding affinity to HLA molecules, a critical step in T-cell activation [1]. These bioinformatic approaches allow for high-throughput screening of peptide sequences and impurities before synthetic production.
- In vitro T-cell assays then experimentally validate these predictions using blood samples from diverse naïve human donors to compare T-cell responses to the active pharmaceutical ingredient versus its impurities [1]. This combination represents a powerful orthogonal strategy as the computational and cellular approaches operate on fundamentally different principles yet should yield concordant results if the risk assessment is accurate.
Table 1: Key Assay Platforms for Orthogonal Immunogenicity Assessment
| Assay Category | Specific Methods | Key Output Measures | Utility in Risk Assessment |
|---|---|---|---|
| In Silico Prediction | HLA-binding prediction algorithms | Binding affinity scores, epitope mapping | Identifies potential T-cell epitopes in peptide sequences and impurities |
| In Vitro Cellular | Naïve T-cell activation assays | IFN-γ ELISPOT, cytokine secretion (IL-2, TNF-α) | Measures actual T-cell responses to peptides in human donor cells |
| In Vitro Binding | MHC-associated peptide proteomics (MAPPs) | Peptide elution profiles, HLA-peptide complexes | Directly identifies peptides presented by antigen-presenting cells |
| Serological | Anti-drug antibody (ADA) assays | Antibody titers, isotype profiling | Detects humoral immune responses to peptide therapeutics |
Advanced Analytical Techniques for Physicochemical Characterization
Beyond biological immunogenicity assays, orthogonal analytical methods provide essential characterization of product-related impurities that may influence immunogenicity potential.
- Reversed-phase high-performance liquid chromatography (RP-HPLC) offers superior resolution for separating target antigens from host cell protein impurities in process intermediates and final drug substances [86].
- When combined with mass spectrometry and microcapillary electrophoresis, this orthogonal approach enables precise identification of both product-related and process-related impurities [86].
- The integration of Simple Wes automated Western analysis provides orthogonal confirmation of protein identity and integrity across collected fractions [86].
For vaccine development specifically, these techniques facilitate rapid characterization of antigen variants and support accelerated process development timelines without compromising assessment rigor [86].
Experimental Protocols for Key Assays
IFN-γ ELISPOT for T-cell Response Evaluation
The IFN-γ ELISPOT assay serves as a cornerstone technique for measuring T-cell responses in immunogenicity assessment. The protocol typically involves:
- Lymphocyte Isolation: Prepare single-cell suspensions from spleen and lymph nodes of immunized animals or human donors [87].
- Peptide Stimulation: Incubate lymphocytes with individual peptides or peptide pools (typically at 1-10μg/mL) in ELISPOT plates pre-coated with IFN-γ capture antibody [87].
- Development and Quantification: After 24-48 hours incubation, develop spots using biotinylated detection antibody, enzyme conjugate, and substrate solution [87].
- Data Analysis: Count spot-forming units (SFUs) using an automated ELISPOT reader and calculate stimulation indices (SI) relative to negative controls. A positive response is typically defined as SI ≥ 2 with statistical significance of p < 0.05 [87].
This protocol was effectively employed in evaluating measles peptide vaccines, where it identified four immunogenic peptides (from an initial 13 candidates) that induced significant IFN-γ responses in transgenic mouse models [87].
Multiplex Bead-Based Flow Cytometry for Humoral Immunity
For comprehensive assessment of humoral immune responses, multiplex bead-based flow cytometry enables simultaneous detection of multiple antibody isotypes:
- Bead Preparation: Covalently immobilize target antigens (e.g., SARS-CoV-2 spike RBD) onto differentially barcoded fluorescent beads of varying sizes (5μm and 8μm) and APC fluorescence intensities [88].
- Serum Incubation: Incubate diluted serum samples with the mixed bead array to allow antibody binding [88].
- Detection: Add fluorochrome-conjugated detection antibodies against human IgM, IgG, and IgA (conjugated with R-PE, V450, and B488, respectively) [88].
- Flow Cytometric Analysis: Analyze using standard flow cytometry, gating on different bead populations based on size and APC fluorescence, then measuring detection antibody fluorescence in appropriate channels [88].
This approach allows high-throughput screening of 624 samples within 2 hours, with intra-plate coefficients of variation ranging from 3.16% to 6.71%, demonstrating excellent reproducibility for large-scale immunogenicity studies [88].
Diagram 1: Orthogonal immunogenicity assessment workflow integrating computational, cellular, and analytical methods.
Comparative Performance Data of Assay Platforms
Case Study: Peptide Vaccine Immunogenicity Assessment
A comprehensive evaluation of measles-derived peptides demonstrates the value of orthogonal assessment. Following identification of 13 HLA-DRB1*03:01-binding peptides from measles virus-infected cells, researchers employed multiple assays to evaluate immunogenicity [87]:
- IFN-γ ELISPOT screening revealed that only 4 of 13 peptides (#4, #7, #11, and #12) induced significant T-cell responses with stimulation indices ranging from 2.05 to 28.43 [87].
- Cytokine profiling of culture supernatants provided orthogonal confirmation, detecting significant levels of IFN-γ, IL-2, and TNF-α specifically in response to these immunodominant peptides [87].
- Viral challenge studies in transgenic mice demonstrated functional protection, with vaccinated mice maintaining 96-98% of initial weight compared to 89% in unvaccinated controls, validating the immunogenicity predictions [87].
Table 2: Comparison of Methodologies for Cytokine Measurement
| Methodology | Sample Volume Requirement | Multiplexing Capacity | Throughput | Key Applications |
|---|---|---|---|---|
| ELISA | Significant volume per analyte | Single analyte at a time | Lower throughput, labor intensive | Quantification of specific cytokines in supernatant |
| Flow Cytometry | Minimal volume for multiple analytes | High multiplex capacity | 624 samples in 2 hours | Simultaneous detection of multiple antibody isotypes or intracellular cytokines |
| Multiplex Bead Array | Small volume for multiple analytes | Moderate to high multiplexing | High throughput with automation | Comprehensive cytokine profiling or antibody isotype detection |
Statistical Considerations for Method Comparison
When implementing orthogonal methodologies, appropriate statistical analysis is crucial for interpreting concordance between methods. While regression analysis has traditionally been used to compare methodologies, the Bland-Altman plot provides superior assessment of agreement between methods [89]. This approach:
- Calculates the mean difference between two methods and the standard deviation of these differences
- Establishes "limits of agreement" (mean difference ± 1.96 SD) to visually assess methodological concordance [89]
- Identifies systematic biases that correlation analysis might overlook
For instance, a comparison of ELISA and flow cytometry for cytokine measurement demonstrated good correlation for IL-1β, IL-6, and TNF-α via regression analysis, but Bland-Altman plots revealed dissimilarity in IL-1β and TNF-α measurements, highlighting the importance of orthogonal verification [89].
Research Reagent Solutions for Implementation
Table 3: Essential Research Reagents for Orthogonal Immunogenicity Assessment
| Reagent Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| HLA Transgenic Mouse Models | HLA-DR3 transgenic mice crossed with human CD46 transgenic mice [87] | Preclinical vaccine immunogenicity testing | Provides human-relevant HLA molecules for T-cell response evaluation |
| Adjuvant Systems | CpG 1826, R848, poly(I:C) with IFA [87] | Enhancing peptide vaccine immunogenicity | Promotes Th1-biased immune responses for better T-cell activation |
| Detection Antibodies | Anti-human IgM Fc5μ, IgG Fcγ, IgA ɑ-chain [88] | Multiplex serological analysis | Enables simultaneous detection of multiple antibody isotypes |
| Barcoded Bead Arrays | RayPlex Multiplex Beads with varying sizes and APC intensities [88] | High-throughput antibody screening | Facilitates simultaneous analysis of multiple analytes in single samples |
| Cell Lines for Validation | RT4, MCF7 (high expressors); HDLM-2, MOLT-4 (low expressors) [85] | Antibody and assay validation | Provides controlled systems for specificity testing across expression levels |
Orthogonal methodologies represent the gold standard for comprehensive immunogenicity risk assessment of peptide-based vaccines and therapeutics. By integrating multiple independent assays spanning computational, cellular, molecular, and analytical approaches, researchers can develop a robust understanding of immunogenic potential that no single method could provide alone. The mandatory implementation of orthogonal assessment in regulatory pathways like ANDA underscores its critical importance in ensuring product safety [1].
Future developments in orthogonal assessment will likely focus on increasing throughput and automation while expanding the multiplexing capacity of individual assays. The integration of public data resources like the Human Protein Atlas, Cancer Cell Line Encyclopedia, and DepMap Portal will further strengthen orthogonal validation by providing extensive antibody-independent reference data [85]. Additionally, advanced statistical approaches like Bland-Altman analysis will improve methodological comparisons, ensuring that orthogonal approaches provide truly complementary information rather than simple verification [89]. As peptide therapeutics and vaccines continue to expand, orthogonal methodologies will remain essential for balancing accelerated development timelines with rigorous safety assessment.
Bridging In Vitro Results to Clinical Outcomes: Validation and Comparative Analysis
Correlating In Vitro Assay Data with In Vivo Protection Models
In the development of modern vaccines, particularly peptide-based platforms, a central challenge lies in establishing a reliable correlation between data generated from controlled in vitro assays and the ultimate in vivo protection observed in living organisms. The ability to predict in vivo immunogenicity and efficacy through in vitro testing is paramount for accelerating vaccine development, reducing costs, and adhering to the ethical principles of the 3Rs (Replacement, Reduction, and Refinement) in animal research [90] [91]. For peptide vaccines, which can suffer from poor immunogenicity and rapid in vivo degradation, this correlation is especially critical [92]. The scientific and regulatory push is toward developing robust in vitro potency assays that can serve as reliable proxies for the complex immune responses elicited in vivo, thereby streamlining lot release testing and potentially reducing the dependency on animal models for batch-to-batch quality control [90] [91]. This guide objectively compares the performance, applications, and limitations of these two foundational approaches in immunogenicity assessment.
Comparative Analysis: In Vitro vs. In Vivo Models
The following table summarizes the core characteristics, advantages, and limitations of in vitro and in vivo models in vaccine development.
Table 1: Core Characteristics of In Vitro and In Vivo Models
| Aspect | In Vitro Models | In Vivo Models |
|---|---|---|
| Experimental Context | Controlled laboratory environment outside living organisms [93] | Within living organisms (e.g., mice, primates) [93] |
| Physiological Relevance | Limited; examines isolated components [93] | High; captures systemic complexity and interactions [93] [94] |
| Typical Assay Examples | Cell-based transfection, ELISA, molecular integrity tests (e.g., CGE) [90] [91] | Vaccine challenge assays, immunogenicity studies (antibody & T-cell measurement) [90] [91] |
| Throughput & Cost | High throughput, cost-effective [91] [93] | Low throughput, resource-intensive [91] |
| Assay Variability | Lower variability (%CV often <10%) [91] | High variability (%CV can range from 34% to 125%) [91] |
| Key Advantages | Controlled conditions, mechanistic insights, faster turnaround, reduced ethical concerns [91] [93] | Holistic view of immune response, long-term effect studies, identifies unexpected outcomes [91] [93] |
| Major Limitations | May oversimplify biology, cannot fully replicate immune system crosstalk [93] [94] | Ethical considerations, species-specific differences, long duration [90] [91] |
Establishing Correlation: Experimental Methodologies
Establishing a predictive link between in vitro and in vivo data requires a systematic and deliberate experimental strategy. The workflow below outlines the key stages in this process.
Diagram 1: Workflow for Correlating In Vitro and In Vivo Data. Short Title: Correlation Workflow
Step 1: Generation of Vaccine Samples with Varied Potency
The foundation of a robust correlation study is the creation of vaccine samples that exhibit a gradient of biological activity. This is typically achieved through controlled stress studies [90].
- Protocol: Accelerated Thermal Stress: Incubate samples of the peptide vaccine or its delivery system (e.g., lipid nanoparticles) at elevated temperatures (e.g., 25°C, 40°C) for varying durations (e.g., 0, 1, 3, 7 days). This process gradually destabilizes the product's structure, creating a series of samples with potencies ranging from 100% down to 0% [90].
- Application Example: For an mRNA-LNP vaccine encoding the RSV pre-fusion F (RSVpreF) protein, thermal stress was used to degrade the mRNA, leading to a quantifiable loss of intact mRNA and a corresponding decrease in protein expression in vitro [90].
Step 2: In Vitro Characterization of Stressed Samples
The stressed samples are first subjected to a battery of in vitro tests designed to measure key Critical Quality Attributes (CQAs).
Structural Integrity Assay:
- Method: Capillary Gel Electrophoresis (CGE). This technique separates biomolecules based on size and can quantify the percentage of intact, full-length mRNA in a vaccine sample [90].
- Data Output: A plot of "% Intact mRNA" versus "Time under Stress" provides a quantitative measure of primary structure degradation [90].
Cell-Based Potency Assay:
- Method: Cell Transfection and Quantitative Imaging. Select a relevant mammalian cell line (e.g., HepG2) and transfer with the stressed vaccine samples. The expressed protein antigen is detected using fluorescently labeled, antigen-specific antibodies, and quantified via high-content imaging [90].
- Data Output: Half-maximal effective concentration (EC50) values are calculated, representing the in vitro relative potency of each sample [90].
Step 3: In Vivo Immunogenicity Testing
In parallel, the same set of stressed samples is administered to animal models to measure the functional immune response.
- Protocol: Mouse Immunization and Serum Analysis:
- Immunization: Administer stressed and control vaccine samples to groups of mice (e.g., intramuscular injection) [90] [92].
- Serum Collection: Draw blood after a set period to collect serum [91].
- Humoral Response: Measure antigen-specific total IgG levels using Enzyme-Linked Immunosorbent Assay (ELISA). This assesses the magnitude of the antibody response [90].
- Functional Response: Perform a pseudovirus neutralization assay (e.g., Fluorescent Focus Assay). This critical test evaluates the quality of the antibody response by measuring the serum's ability to neutralize a pseudotyped virus, reported as a neutralization titer or half-maximal effective dose (ED50) [90].
Step 4: Data Correlation and Analysis
The final step is to statistically correlate the in vitro data with the in vivo outcomes.
- Analysis: Plot the in vitro relative potency (EC50) against the in vivo antibody titers or neutralization titers (ED50). A statistically significant correlation indicates that the in vitro assay can predict the in vivo immunogenic performance [90].
- Case Study: For an RSVpreF mRNA-LNP vaccine, a significant correlation was found between the in vitro cell-based potency (EC50) and the in vivo pseudovirus neutralization potency (ED50), whereas the correlation with total antibody titers was less clear. This underscores that the choice of in vivo endpoint is crucial [90].
Case Studies in Vaccine Development
Case Study 1: mRNA Lipid Nanoparticle (LNP) Vaccines
A pivotal study established correlation for an mRNA-LNP vaccine against Respiratory Syncytial Virus (RSV) [90].
- Experimental Data:
- In Vitro: Loss of intact mRNA (via CGE) and loss of in vitro protein expression (in HepG2 cells) were observed with increasing thermal stress.
- In Vivo: Mice immunized with the stressed samples showed reduced anti-RSV antibody titers and lower pseudovirus neutralization capacity.
- Correlation Outcome: The in vitro protein expression data showed a statistically significant correlating trend with the in vivo neutralization potency, demonstrating the predictive power of the cell-based assay [90].
Case Study 2: Peptide Delivery Systems
Research on peptide antigens encapsulated in Synthetic Spore Husk-Encased Lipid (SSHEL) particles highlights the importance of formulation.
- Experimental Data:
- In Vitro: Particle size and antigen presentation (surface-attached vs. encapsulated) profoundly influenced cross-presentation of the SIINFEKL model epitope on MHC-I in dendritic cells. Five hundred-nanometer particles with encapsulated peptide were vastly superior to liposomes or free peptide [92].
- In Vivo: Immunization with the optimized SSHELEncPep construct in a mouse melanoma model elicited robust antigen-specific CD8+ T cell expansion, reduced tumor size, and increased survival [92].
- Correlation Outcome: The superior in vitro cross-presentation directly predicted stronger in vivo T-cell responses and therapeutic efficacy, validating the in vitro model for screening peptide vaccine formulations [92].
The Scientist's Toolkit: Essential Research Reagents
Successful correlation studies depend on specific, high-quality reagents and tools. The following table details key solutions for evaluating peptide vaccines.
Table 2: Essential Research Reagents for Peptide Vaccine Evaluation
| Research Reagent / Solution | Function in Evaluation | Application Example |
|---|---|---|
| Antigen-Specific Monoclonal Antibodies (mAbs) | Critical reagents for in vitro immunoassays; must recognize conformational epitopes linked to neutralizing immune responses [90]. | Used in sandwich ELISA to quantify antigen expression and conformational integrity for RSV F protein [90]. |
| Stable Cell Lines for Transfection | Reproducible cellular system for measuring protein expression and antigen functionality from nucleic acid (DNA/mRNA) vaccines [90]. | HepG2 cells selected for robust protein expression from mRNA-LNP RSV vaccines [90]. |
| Toll-like Receptor (TLR) Assays | In vitro systems to assess the intrinsic adjuvant properties of a vaccine candidate by measuring interaction with innate immune receptors [95] [36]. | Molecular docking and dynamics simulations used to predict vaccine construct binding affinity to TLR2 and TLR4 [95] [36]. |
| Relevant Animal Models | In vivo systems to study the complex, integrated immune response, including humoral and cellular immunity, that cannot be fully replicated in vitro [91] [93]. | Mice used for immunogenicity studies; challenge models to demonstrate protective efficacy [90] [92]. |
| AI-Powered Epitope Prediction Tools (e.g., MUNIS, NetMHCpan) | In silico platforms that use deep learning to accurately predict immunogenic T-cell and B-cell epitopes, streamlining antigen selection [96] [95]. | Used in multi-epitope vaccine design to filter candidate peptides for high antigenicity and low allergenicity prior to synthesis [95] [36]. |
Challenges and Future Directions
Despite advances, correlating in vitro and in vivo data remains challenging. A significant hurdle is high variability in in vivo assays, with percent coefficients of variation (%CV) documented from 34% to as high as 125%, compared to often less than 10% for in vitro methods [91]. Furthermore, species-specific differences in immune responses can limit the translatability of animal data [90] [94].
The future of this field is being shaped by several key developments. Artificial Intelligence (AI) and advanced in silico models are improving the prediction of epitope immunogenicity and optimizing antigen design, as demonstrated by tools like Graph Neural Networks (GNNs) [96]. There is also a growing emphasis on developing more sophisticated cell-based assays that better mimic in vivo conditions, such as 3D organoid or co-culture systems. Finally, the push for regulatory acceptance of in vitro assays for product lot release continues to drive the need for robustly correlated methods, reinforcing the application of the 3Rs in biotechnology [90] [91].
Benchmarking Against Reference Standards and Regulatory Guidelines
The global market for therapeutic peptides has experienced substantial growth and is projected to reach US$86.9 billion by 2032 [2]. As of 2025, over 100 therapeutic peptide products encompass hormone analogs, growth factors, neurotransmitters, and anti-infectives [2]. Evaluating immunogenicity—the unwanted immune response to therapeutic peptides—is an integral component of peptide development programs, particularly for next-generation epitope-based vaccines designed to combat antibiotic-resistant pathogens [2] [97].
Immunogenicity risk arises from a complex interplay of product-related, patient-related, and treatment-related factors [2]. For researchers developing peptide-based vaccines, rigorous in vitro benchmarking against established regulatory standards provides the foundation for assessing clinical immunogenicity risk before proceeding to costly clinical trials. This guide establishes a standardized framework for comparing peptide vaccine candidates against critical reference standards and outlines detailed experimental protocols aligned with current regulatory thinking.
Key Regulatory Standards and Quality Attributes
Analytical Characterization Benchmarks
Regulatory guidance for therapeutic peptides emphasizes comprehensive characterization of critical quality attributes (CQAs) that impact immunogenicity [2]. The following table summarizes key reference standards and their analytical benchmarks for peptide-based vaccines:
Table 1: Key Analytical Benchmarks for Peptide-Based Vaccines
| Quality Attribute Category | Specific Analytical Benchmarks | Regulatory Reference/Threshold | Impact on Immunogenicity |
|---|---|---|---|
| Product-Related Impurities | Peptide-related substances (insertions, deletions, substitutions, racemization) | Case-by-case determination; ICH Q3A/Q3B principles [2] | Modulates immune response; may increase immunogenicity risk |
| Aggregates, oligomers, fibrils | No broadly applicable thresholds; justified per product [2] | Can enhance immunogenicity and promote immune-related adverse events | |
| Process-Related Impurities | Host cell proteins, DNA (recombinant peptides) | ICH Q6B guidance [2] | Potential immunogenicity risk |
| Biochemical modifications (deamidation, oxidation) | Controlled via manufacturing process validation [2] | May alter immune recognition | |
| Container Closure System | Extractables/leachables | Based on compatibility studies [2] | May promote higher order structure or product degradation |
Immunogenicity Risk Assessment Framework
Regulatory assessment of immunogenicity risk occurs throughout the peptide drug lifecycle [2]:
- Candidate Selection: Initial sequence selection for low immunogenicity risk using in silico and in vitro tools
- Manufacturing: Control of impurities introduced during synthesis and storage
- Pre-clinical Stage: Animal studies to qualify impurities for immunotoxicity
- Clinical Stage: Anti-drug antibody (ADA) assays evaluating impact on pharmacokinetics, pharmacodynamics, efficacy, and safety
- Post-marketing Stage: Monitoring for rare immune-related adverse events
For follow-on peptide products under 505(j) and 505(b)(2) pathways, manufacturers must bridge differences in impurities through comparative analytical methods, as these differences may increase immunogenicity risk compared to the reference product [2].
Experimental Design for In Vitro Immunogenicity Assessment
Target Antigen Selection and Epitope Prediction
The development workflow for epitope-based vaccines begins with bioinformatics-driven target antigen selection [97]. The following experimental protocol establishes a standardized approach for benchmarking antigen selection:
Table 2: Research Reagent Solutions for Antigen Selection
| Research Reagent | Manufacturer/Source | Function in Experimental Protocol |
|---|---|---|
| VaxiJen Software | University of Aberdeen | Alignment-independent prediction of protective antigens using machine learning algorithms [97] |
| Vaxign2 Platform | Virginia Commonwealth University | Reverse vaccinology and machine learning for protective antigen prediction [97] |
| BLASTp Database | National Center for Biotechnology Information | Assessment of host protein homologs to mitigate autoimmunity risk [97] |
| UniProtKB Database | UniProt Consortium | Source of protein sequences for antigenicity analysis [97] |
Experimental Protocol: Target Antigen Selection
- Protein Screening: Apply VaxiJen with threshold antigenicity score >0.4 for initial classification of protective antigens [97]
- Localization Analysis: Predict subcellular localization prioritizing cell wall-associated, extracellular, secreted, and membrane-associated proteins over cytoplasmic/intracellular proteins
- Safety Assessment: Evaluate allergenicity and toxicity using Vaxign2 complementary analysis
- Homology Assessment: Perform BLASTp analysis against human proteome to exclude antigens with significant homology to human proteins
- Conservation Verification: Confirm antigen conservation across bacterial strains using multiple sequence alignment
Figure 1: Target Antigen Selection Workflow
Epitope Prediction and Immunogenicity Assays
Experimental Protocol: Epitope Prediction and Selection
- B-Cell Epitope (BCE) Prediction:
- Linear epitopes: Utilize BepiPred, ABCpred, or IEDB B-cell epitopes tools with 15-22 amino acid window [97]
- Conformational epitopes: Apply ElliPro or DiscoTope for discontinuous epitopes (note technical challenges in reproduction)
T-Cell Epitope (TCE) Prediction:
- Cytotoxic T lymphocyte epitopes (CTLs): Predict binding affinity to MHC I molecules
- Helper T lymphocyte epitopes (HTLs): Predict binding affinity to MHC II molecules
In Vitro Immunogenicity Assay:
- Utilize HLA-DR transgenic mouse splenocytes for T-cell proliferation assays
- Measure interferon-γ (IFN-γ) production via ELISA as indicator of cellular immune response
- Assess epitope-specific antibody production in BALB/c mice models
Table 3: Epitope Prediction Tools and Their Applications
| Tool Category | Specific Tools | Epitope Type Detected | Key Output Parameters |
|---|---|---|---|
| Linear B-Cell Epitopes | BepiPred, ABCpred, IEDB B-cell | Linear B-cell epitopes (LBLs) | Antigenicity score, residue position |
| Conformational B-Cell Epitopes | ElliPro, DiscoTope | Conformational B-cell epitopes (CBLs) | Structural amino acids, proximity score |
| T-Cell Epitopes | MHC I & II binding predictors | Cytotoxic (CTL) & Helper (HTL) epitopes | Binding affinity (IC50), percentile rank |
Figure 2: Epitope Prediction and Selection Workflow
Comparative Immunogenicity Assessment Framework
In Vitro Potency and Immunogenicity Assays
Experimental Protocol: Comparative T-cell Activation Assay
- Human PBMC Isolation: Isolate peripheral blood mononuclear cells from healthy donors (n≥10) using Ficoll density gradient centrifugation
- Peptide Stimulation: Culture PBMCs with reference standard and test peptide vaccines at concentrations of 1μg/mL, 5μg/mL, and 10μg/mL
- Cytokine Profiling: After 72-hour incubation, measure IFN-γ, IL-2, and IL-4 production via multiplex ELISA
- Flow Cytometry Analysis: Stain for CD4+ and CD8+ T-cell activation markers (CD69, CD25)
- Benchmarking Analysis: Compare test peptide response to reference standard using normalized response ratio (NRR) = (Test peptide response)/(Reference standard response)
Experimental Protocol: B-cell Activation and Antibody Production
- Mouse Immunization: Administer reference standard and test peptides to BALB/c mice (n=6 per group) on days 0, 14, and 28
- Serum Collection: Collect serum samples on days 0, 14, 28, and 42
- ELISA Analysis: Measure epitope-specific IgG, IgG1, and IgG2a titers against target antigen
- Neutralization Assay: For pathogen-targeting vaccines, perform in vitro neutralization assay with appropriate cell lines
Table 4: Comparative Immunogenicity Assessment Parameters
| Assessment Parameter | Experimental Method | Benchmarking Criteria | Acceptance Threshold |
|---|---|---|---|
| Cellular Immune Response | IFN-γ ELISpot, Flow cytometry | ≥2-fold increase over negative control | p<0.05 vs. control |
| Humoral Immune Response | Antigen-specific ELISA | Serum titer ≥1:1000 dilution | Statistical significance vs. reference |
| T-cell Proliferation | CFSE dilution assay | Stimulation index ≥2.5 | p<0.01 vs. unstimulated control |
| Cytokine Profile | Multiplex cytokine array | Th1/Th2 cytokine ratio >1.5 | Balanced Th1/Th2 response preferred |
Stability and Impurity Profiling
Experimental Protocol: Accelerated Stability Studies
- Stress Conditions: Incubate peptide formulations at 40°C±2°C/75%RH±5%RH for 1, 3, and 6 months
- Analytical Monitoring: Assess peptide content, related substances, and higher order structures monthly
- Forced Degradation: Expose to oxidative (0.01% H2O2), thermal (60°C), and photolytic (1.2 million lux hours) stress conditions
- Immunogenicity Correlation: Test degraded samples in T-cell activation assays to identify degradation products with enhanced immunogenicity potential
Data Interpretation and Regulatory Decision-Making
The immunogenicity risk assessment for peptide-based vaccines must demonstrate comparability to reference standards or previously approved products, particularly for follow-on products [2]. Significant gaps remain in understanding how specific product quality attributes impact immunogenicity, particularly for impurity qualification [2].
When benchmarking against regulatory standards, consider that current FDA guidance does not establish broadly applicable qualification thresholds for peptide-related impurities [2]. Limits and controls are determined case-by-case based on manufacturing experience, batch data, stability data, and toxicology data [2]. For synthetic peptides, ICH Q3A and Q3B principles may be considered applicable, while recombinant peptides fall under ICH Q6B guidance [2].
The integrated data from these standardized experimental protocols provides a comprehensive framework for regulatory submissions, supporting the transition from in vitro characterization to clinical development with robust immunogenicity risk assessment.
Comparative Potency Assessment of Multi-Peptide Cocktails and Vaccine Formulations
The development of peptide-based vaccines represents a promising strategy in immunotherapy for infectious diseases and cancer. These vaccines utilize minimal antigenic components to elicit targeted immune responses, offering advantages in safety and specificity over whole-pathogen or whole-cell approaches [97]. A critical challenge in the field is understanding the factors that determine the immunogenicity and efficacy of multi-peptide formulations. This guide provides a comparative analysis of different peptide vaccine strategies, supported by experimental data and detailed methodologies, to inform researchers and drug development professionals.
Comparative Performance Data of Peptide Vaccine Formulations
The immunogenicity and protective efficacy of peptide-based vaccines vary significantly based on their design, including epitope selection, adjuvant use, and inclusion of T-helper components. The table below summarizes quantitative outcomes from various experimental and clinical studies.
Table 1: Comparative Immunogenicity and Efficacy of Peptide Vaccine Formulations
| Vaccine Target / Type | Key Components | Immune Readout | Efficacy / Survival Outcome | Study Reference |
|---|---|---|---|---|
| Melanoma (Clinical) | 12MP (CTL peptides) + 6MHP (cognate helper peptides) + Cyclophosphamide | CD8+ T-cell responses | Median OS: Not reached; 15-year OS: 61% | [98] |
| Melanoma (Clinical) | 12MP (CTL peptides) + Tetanus toxoid helper peptide (non-cognate) | CD8+ T-cell responses | Median OS: 12.9 years; 15-year OS: 45% | [98] |
| HIV (Clinical) | 4 hybrid T-helper-CTL peptides (MEP) + RC529-SE adjuvant ± GM-CSF | IFN-γ ELISPOT | Response Rate: 6/80 (7.5%); transient responses | [99] |
| Brucella spp. (Preclinical) | Multi-epitope protein (Poly B) + Poly I:C adjuvant | IgG2a (Th1) > IgG1 (Th2); High IFN-γ | Protection vs 16M: ~1.5 log CFU reduction in spleen | [100] |
| Brucella spp. (Preclinical) | Multi-epitope protein (Poly B) alone | Lower IgG2a & IFN-γ | Protection vs 16M: ~0.8 log CFU reduction in spleen | [100] |
| Group A Streptococcus (Clinical) | J8/P*17 & K4S2 epitopes conjugated to CRM197 carrier + Alum | Opsonophagocytic antibodies; High avidity | Antibodies killed bacteria in vitro; 100% seroconversion | [101] |
Detailed Experimental Protocols and Methodologies
Immunogenicity Assessment via ELISPOT
The Enzyme-Linked Immunospot (ELISPOT) assay is a cornerstone for quantifying antigen-specific T-cell responses in peptide vaccine studies [99].
- Protocol: Peripheral blood mononuclear cells (PBMCs) are isolated from vaccinated subjects via density gradient centrifugation. Cells are typically plated at a density of 2-4 x 10^5 cells per well in pre-coated IFN-γ antibody plates. They are then stimulated with the vaccine peptide pools (e.g., individual MEP peptides A, B, C, J) [99]. Controls include cells alone (negative control) and cells stimulated with a mitogen like phytohemagglutinin (positive control). After a 24-48 hour incubation, cells are removed, and a biotinylated detection antibody is added. Following incubation with streptavidin-enzyme conjugate and a precipitating substrate, spot-forming units (SFUs) representing individual cytokine-releasing cells are counted using an automated ELISPOT reader.
- Data Analysis: The results are expressed as SFUs per million cells. A positive response is often defined as a statistically significant increase over the mean of negative control wells, with a minimum threshold (e.g., >50 SFUs/million and at least twice the background) [99].
In Vivo Protection Models
Preclinical vaccine efficacy is frequently evaluated in animal challenge models.
- Brucella Challenge Model: Mice are immunized subcutaneously with the multi-epitope vaccine formulation (e.g., 100 µg of Poly B protein) emulsified in an adjuvant such as Poly I:C [100]. After two boosts, mice are challenged intraperitoneally with a virulent strain like B. melitensis 16M. To quantify protection, spleens are aseptically removed from the mice, weighed, and homogenized. Serial dilutions of the homogenate are plated on Brucella-selective agar plates. After several days of incubation, the number of bacterial colonies (CFU) is counted. The log protection is calculated by comparing the mean log CFU in the spleens of vaccinated mice versus unvaccinated control mice [100].
Humoral Immunogenicity Analysis
The quality and magnitude of antibody responses are critical for many peptide vaccines.
- Protocol: Sera are collected from immunized subjects at various time points. Antibody titers are typically measured using Enzyme-Linked Immunosorbent Assay (ELISA), where plates are coated with the vaccine peptide or target antigen. Serial serum dilutions are applied, and bound antibodies are detected with enzyme-conjugated secondary antibodies specific to different isotypes (e.g., IgG1, IgG2a) [100]. The endpoint titer is often defined as the highest serum dilution that gives an absorbance value greater than a pre-defined cut-off.
- Functional Assays: For bacterial vaccines like the Strep A candidate, functional opsonophagocytic assays (OPA) are performed. This involves incubating the target bacteria with vaccinated subject sera and complement, followed by the addition of phagocytic cells (e.g., differentiated HL-60 cells). The mixture is incubated, plated on agar, and bacterial survival is quantified. A reduction in CFU indicates functional, opsonic antibodies [101]. Antibody avidity can be further assessed by including a washing step with a chaotrope (e.g., urea) in the ELISA to dissociate low-affinity antibodies [101].
Signaling Pathways and Immunological Mechanisms
Peptide vaccines initiate a cascade of immune activation events. The following diagram illustrates the key pathways from antigen presentation to the development of effector and memory responses.
Diagram Title: Immune Activation Pathway of Peptide Vaccines
The Scientist's Toolkit: Essential Research Reagents
Successful evaluation of peptide vaccines relies on a specific set of reagents and assays. The following table details key materials and their functions in vaccine research and development.
Table 2: Essential Reagents for Peptide Vaccine Research
| Reagent / Material | Primary Function in Research | Key Application Example |
|---|---|---|
| Synthetic Peptides | Serve as the vaccine antigen; contain defined T-cell and/or B-cell epitopes. | 12MP (melanoma), MEP peptides (HIV), J8/P*17 (Strep A) [99] [98] [101] |
| Adjuvants (e.g., Poly I:C, RC529-SE) | Enhance immunogenicity by activating innate immunity (e.g., via TLR3), promoting APC maturation. | Poly I:C used with Brucella multi-epitope protein to boost Th1 response [100]. |
| ELISPOT Kits (IFN-γ) | Quantify the frequency of antigen-specific T cells by detecting cytokine secretion. | Measuring CD8+ T-cell responses to 12MP vaccine in melanoma patients [99] [98]. |
| Flow Cytometry Antibodies | Phenotype and characterize immune cells (e.g., CD4, CD8, memory markers). | Analyzing T-cell differentiation and activation status post-vaccination. |
| Recombinant Carrier Proteins (e.g., CRM197) | Enhance immunogenicity of small peptides by providing T-helper epitopes. | J8 and P*17 epitopes conjugated to CRM197 for Strep A vaccine [101]. |
| In Vivo Animal Models | Preclinical evaluation of vaccine safety, immunogenicity, and protective efficacy. | Mouse challenge models with Brucella melitensis 16M [100]. |
The comparative data and methodologies presented in this guide underscore that the potency of multi-peptide vaccines is not a function of a single component but a synergy of rational design. Critical factors for success include the use of long or multi-epitope peptides to broaden HLA coverage and engage CD4+ help, the selection of appropriate adjuvants to drive a robust and durable Th1-skewed response, and the strategic inclusion of cognate T-helper epitopes to support cytotoxic T-cell memory and enhance long-term clinical outcomes, as demonstrated in melanoma trials [97] [98] [100]. Overcoming the challenges of HLA restriction and the immunosuppressive microenvironment remains a central focus. Future advancements will likely rely on personalized neoantigen vaccines, innovative delivery platforms, and combination immunotherapies to unlock the full potential of peptide-based vaccination.
The evaluation of immunogenicity is a critical step in vaccine development and therapeutic peptide assessment. This guide systematically compares the predictive value of a suite of in vitro and in silico assays across three distinct immunological challenges: measles virus immunity, cancer peptide vaccines, and universal influenza vaccine development. By synthesizing recent experimental data and validation protocols, we provide a framework for researchers to select appropriate assays based on the specific immune parameters of interest—humoral response durability, T-cell priming efficiency, or cross-reactive epitope prediction. The integration of advanced machine learning models with traditional immunological assays emerges as a transformative approach for enhancing predictive accuracy in immunogenicity risk assessment.
Predicting immunogenicity is paramount for developing effective vaccines and therapeutic peptides. The core challenge lies in accurately forecasting the complex interplay between antigen presentation, T-cell and B-cell activation, and the resulting durable protection in a heterogeneous human population. Traditional in vitro assays have long provided the foundation for these assessments, but their predictive value can be limited by the complexity of the entire immune system. Recent advances are addressing this gap through two key approaches: the refinement of bioassays to better mimic in vivo conditions (e.g., lymph node trafficking) and the integration of sophisticated AI-driven epitope prediction tools that learn from expansive immunological datasets [57]. This review objectively compares the performance of these evolving methodologies through the lens of three pressing case studies, providing researchers with validated experimental protocols and a clear analysis of the strengths and limitations of each predictive tool.
Comparative Analysis of Predictive Assays: Performance Data
The table below summarizes the quantitative performance and key applications of various predictive assays discussed in this review.
Table 1: Comparative Performance of Immunogenicity Predictive Assays
| Assay / Model | Primary Application | Key Performance Metric | Reported Value | Key Advantage | Experimental Validation |
|---|---|---|---|---|---|
| Machine Learning Outbreak Model [102] | Measles case prediction (County-level) | Sensitivity (2019 data) | 72% | Identifies high-risk outbreak areas | Comparison with actual 2019 measles cases |
| IgG Titer (CLIA) [103] | Measles humoral immunity | Seroprotection rate (Vaccinated vs. Natural infection) | 80% vs. 94% | Direct measure of circulating antibody | Chemiluminescence immunoassay (LIAISON) |
| Amph-Vaccine T-cell Priming [104] | Cancer peptide vaccines | Enhanced T-cell responses | Significant increase (vs. soluble peptide) | Improved lymph node drainage and stability | Mouse models, human DC processing assays |
| AI: B-cell Epitope Prediction [57] | Universal vaccine design | Prediction Accuracy (AUC) | 87.8% (AUC=0.945) | Outperforms traditional tools by ~59% (MCC) | Benchmarking against established methods |
| AI: MUNIS (T-cell Epitope) [57] | Universal vaccine design | Performance vs. prior algorithms | 26% higher | Identifies novel, validated epitopes | HLA binding & T-cell assays (EBV model) |
| In vitro Immunogenicity Assays [105] | Generic peptide drug risk | Adaptive & Innate response profiling | N/A (Qualitative) | Assesses impact of impurities | Immune cell-based assays, HLA genotypes |
Case Study 1: Measles – Durability of Humoral vs. Cellular Immunity
Experimental Data on Antibody Persistence
A critical aspect of measles immunology is the long-term persistence of protective immunity. A 2021 serological study provides crucial quantitative data on the comparative durability of humoral responses, summarized in the table below [103].
Table 2: Comparative Long-term Immunogenicity: Measles Vaccination vs. Wild Infection
| Immunity Group | Study Cohort (n) | Proportion with Protective IgG | Geometric Mean Titer (GMT) |
|---|---|---|---|
| Two MMR Doses | 410 | 80% | 92.2 |
| History of Measles Infection | 201 | 94% | 213.3 |
This study demonstrated a statistically significant (p < .0001) difference in both seroprotection rates and antibody levels, indicating that natural infection induces a more robust and durable humoral response compared to vaccination with two doses of the MMR vaccine [103]. The experimental protocol involved:
- Participant Cohort: 611 medical students and residents.
- IgG Measurement: Semi-quantitative chemiluminescence immunoassay (CLIA) using the LIAISON platform.
- Cut-off: >16.5 AU/mL (equivalent to 175 mIU/mL per WHO standard) [103].
T-cell Epitope Mapping and Viral Escape
While antibodies are a key correlate of protection, T-cell immunity is crucial for clearing infected cells. A 2025 study investigated whether circulating measles virus (MeV) genotypes could escape vaccine-induced T-cell immunity [106].
- Experimental Protocol: An immunoinformatics pipeline predicted 83 universal CD4+ T-cell epitope candidates from the vaccine MeV strain. Polyclonal T-cell lines were generated from PBMCs of vaccinated and convalescent individuals. T-cell responsiveness was measured via IFN-γ ELISPOT and a flow cytometry panel assessing CD154 expression and intracellular IFN-γ [106].
- Key Finding: The study identified 37 functional CD4+ T-cell epitopes. Strikingly, 73% (27/37) of these epitope regions contained sequence variations in wild-type viruses (genotypes B3, D4, D8, H1). Functional assays confirmed that specific mutations in epitopes from the H and F proteins disrupted the ability of vaccine-induced CD4+ T cells to respond to circulating viruses [106]. This highlights a potential mechanism for immune escape that is not detected by standard antibody assays.
Diagram 1: Workflow for Predicting and Validating T-cell Epitope Escape in Measles.
Case Study 2: Cancer – Enhancing Peptide Vaccine Immunogenicity
The Amphiphile-Vaccine (Amph-Vaccine) Platform
A significant hurdle for therapeutic peptide vaccines in oncology is their poor delivery to lymph nodes (LNs) and short in vivo half-life, leading to suboptimal T-cell priming [104]. Research has demonstrated that modifying peptides with an albumin-binding moiety, 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-PEG (DSPE-PEG), directly addresses this challenge [104].
- Mechanism: Conjugation promotes binding to endogenous albumin, facilitating "hitchhiking" to the draining LNs. This enhances lymphatic trafficking and increases peptide stability in serum [104].
- Experimental Workflow: The critical steps for evaluating such enhancements are summarized below.
Diagram 2: Experimental workflow for evaluating amph-vaccine conjugates, from synthesis to functional T-cell assessment.
Key Predictive Assays and Reagents
The assessment of amph-vaccine efficacy relies on a defined set of research reagents and assays to quantify lymphatic delivery and immunogenicity [104].
- LN Trafficking and Persistence: Amph-peptides showed trafficking beyond immediate draining LNs to distal nodes. Antigen presentation was detectable for at least a week in vivo, whereas presentation from soluble peptide quickly decayed [104].
- T-cell Priming Requirement: The enhanced immunogenicity of amph-vaccines was found to be dependent on Batf3-dependent dendritic cells, a key subset for cross-presentation, but was not altered in mice deficient in the neonatal Fc receptor (FcRn) [104].
Table 3: Research Reagent Solutions for Peptide Vaccine Immunogenicity Testing
| Research Reagent / Assay | Function in Evaluation | Key Experimental Readout |
|---|---|---|
| DSPE-PEG-NHS / Maleimide | Chemistries for covalent peptide-lipid conjugation | Successful conjugate synthesis (LC-MS) |
| Mouse Models (e.g., Batf3-KO) | Define cellular mechanisms of immune priming | Requirement for cross-presenting DCs |
| IFN-γ ELISPOT | Quantify antigen-specific T-cell frequency | Spot-forming units (SFUs) per million cells |
| Activation-Induced Marker (AIM) Assay | Identify functional T cells (e.g., CD154+) | Flow cytometry: % CD154+ IFN-γ+ CD4+ T cells |
| Human DC Processing Assay | Confirm human immune cell compatibility | Equivalent processing vs. unmodified peptide |
Case Study 3: Universal Influenza Vaccine – AI-Driven Epitope Prediction
The Limitations of Traditional Assays and the Rise of AI
The development of a universal influenza vaccine (UIV) is hampered by the virus's high mutation rate, particularly in the immunodominant head region of the hemagglutinin (HA) protein. Current seasonal vaccines often have an effectiveness ranging from 10% to 60%, which can drop significantly during vaccine mismatches [107]. Traditional epitope identification methods, such as motif-based searches or peptide microarrays, are often low-throughput, costly, and achieve limited accuracy (~50-60% for B-cell epitopes) [57]. AI-driven approaches are transforming this field by learning complex sequence-structure patterns from large immunological datasets.
Benchmarking AI Models Against Traditional Methods
Recent AI models have demonstrated substantial improvements in predictive performance, as detailed in Table 1. For instance:
- MUNIS (T-cell epitope prediction): This model showed a 26% higher performance than the best prior algorithm. It successfully identified known and novel CD8+ T-cell epitopes from a viral proteome, which were experimentally validated through HLA binding and T-cell assays [57].
- B-cell Epitope Prediction (CNN-based): One deep learning model achieved 87.8% accuracy (AUC = 0.945), outperforming previous state-of-the-art methods by about 59% in Matthews correlation coefficient (MCC), a more robust metric for imbalanced datasets [57].
Practical Workflow for AI-Guided UIV Development
The integration of AI into the vaccine development pipeline provides a powerful strategy for prioritizing candidates.
- Actionable Workflow:
- Broad In Silico Screening: Use an AI platform (e.g., Vaxign-ML, MUNIS) to scan the entire influenza proteome for conserved, immunogenic epitopes, including non-surface proteins like nsp3 [57].
- Prioritize Conserved Epitopes: Focus predictions on the conserved stalk region of HA, neuraminidase (NA), or the extracellular domain of M2 (M2e) to circumvent antigenic drift [107].
- Validate Structurally: Leverage tools like AlphaFold to generate high-quality structural models for AI-optimized antigen variants, ensuring enhanced antibody binding is structurally plausible [57].
- Experimental Confirmation: Synthesize top AI-prioritized candidates and test them in a cascade of assays, beginning with in vitro HLA binding and human DC presentation assays, followed by T-cell activation and neutralizing antibody assays, before moving to in vivo challenge models [57] [106].
The Scientist's Toolkit: Essential Reagents and Assays
This table consolidates key materials and methods critical for the immunogenicity assays discussed in this guide.
Table 4: Essential Research Toolkit for Immunogenicity Assessment
| Category | Reagent / Assay | Specific Function | Context of Use |
|---|---|---|---|
| Humoral Immunity | LIAISON Measles IgG CLIA | Quantify protective antibody titers | Measles seroprotection studies [103] |
| Cellular Immunity | IFN-γ ELISPOT | Measure T-cell frequency and response | Amph-vaccine T-cell priming; MeV epitope validation [104] [106] |
| Cellular Immunity | Activation-Induced Marker (AIM) Assay | Identify polyfunctional antigen-specific T cells | High-resolution CD4+ T-cell epitope mapping (e.g., CD154) [106] |
| Antigen Presentation | HLA Binding Assays | Determine peptide affinity for MHC molecules | Validating AI-predicted T-cell epitopes [57] [106] |
| In Silico Tools | MUNIS, NetBCE, GraphBepi | AI-driven B-cell and T-cell epitope prediction | Universal influenza vaccine antigen selection [57] |
| Specialized Reagents | DSPE-PEG Conjugates | Enhance peptide lymphatic delivery and stability | Improving immunogenicity of cancer peptide vaccines [104] |
| Cell Models | Batf3-dependent DCs | Critical for cross-presentation to CD8+ T cells | Mechanistic studies of amph-vaccine action [104] |
The predictive value of immunogenicity assays is maximized when a holistic, multi-parametric approach is employed. The case studies examined herein demonstrate that:
- For measles, assessing both humoral durability and T-cell epitope conservation is critical for understanding long-term protection and potential immune escape.
- For cancer peptide vaccines, assays that predict and measure lymphatic delivery and antigen persistence (e.g., using amph-vaccine platforms) are more predictive of robust T-cell priming than simple in vitro binding assays.
- For universal influenza vaccines, AI-driven in silico prediction has become an indispensable tool, dramatically increasing the speed and accuracy of conserved epitope identification, but its predictions must be bridged to traditional in vitro and in vivo validation assays.
The future of immunogenicity risk assessment lies in the intelligent integration of high-performance computational predictions with carefully selected, mechanistically informative biological assays. This synergistic approach provides the most robust framework for de-risking the development of next-generation vaccines and therapeutic peptides.
Conclusion
In vitro immunogenicity assessment is an indispensable component of peptide-based vaccine development, providing a controlled and predictive means to evaluate candidate vaccines before costly clinical trials. A holistic approach that combines foundational knowledge of immune epitopes with robust methodological application, strategic troubleshooting, and rigorous validation is key to success. Future directions will be shaped by the integration of high-throughput technologies like immunoarrays, advanced nanoparticle delivery systems, and sophisticated in silico predictions. These innovations, coupled with evolving regulatory frameworks for orthogonal assessment, promise to enhance the predictive power of in vitro assays, ultimately accelerating the development of safer and more effective peptide vaccines for infectious diseases, cancer, and beyond.
References
- 1. Immunogenicity of Generic Peptide Impurities - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159091/]
- 2. Immunogenicity of therapeutic peptide products: bridging ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1608401/full]
- 3. Eliciting antitumor immunity via therapeutic cancer vaccines [https://www.nature.com/articles/s41423-025-01316-4]
- 4. Identification of immunogenic KIF5B-RET fusion neopeptides ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611928/]
- 5. C > U mutations generate immunogenic peptides in SARS- ... [https://www.nature.com/articles/s41467-025-65251-8]
- 6. Peptide Mapping for Sequence Confirmation of ... [https://www.mdpi.com/1422-0067/26/20/9962]
- 7. A multi-adjuvant personal neoantigen vaccine generates ... [https://www.sciencedirect.com/science/article/abs/pii/S0092867425006853]
- 8. Fundamentals and Methods for T- and B-Cell Epitope ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5763123/]
- 9. Introduction to T and B lymphocytes - Autoimmunity - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK459471/]
- 10. The Relative Positioning of B and T Cell Epitopes Drives ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9413633/]
- 11. B Cells vs T Cells: 7 Key Differences and Functions ... [https://int.livhospital.com/b-cells-vs-t-cells-7-key-differences-and-functions-explained/]
- 12. T Cells: Types and Function [https://my.clevelandclinic.org/health/body/24630-t-cells]
- 13. Antibody class switching differs among SJL, C57BL/6 and 129 ... [https://pubmed.ncbi.nlm.nih.gov/17329233/]
- 14. T cell independent antibody responses with class switch ... [https://www.nature.com/articles/s41541-024-00902-3]
- 15. Understanding how biologics trigger immune responses: T ... [https://www.bioanalysis-zone.com/understanding-how-biologics-trigger-immune-responses-t-cell-dependent-vs-t-cell-independent-pathways/]
- 16. Adjuvanted Protein Vaccines Boost RNA-Based ... [https://www.mdpi.com/2076-393X/13/8/797]
- 17. Peptide vaccines: an innovative therapeutic approach ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1567584/full]
- 18. Cell-Based Assays to Detect Innate Immune Response Modulating Impurities: Application to Biosimilar Insulin | The AAPS Journal [https://link.springer.com/article/10.1208/s12248-024-00983-x]
- 19. Detection of innate immune response modulating impurities (IIRMI) in therapeutic peptides and proteins: Impact of excipients - PubMed [https://pubmed.ncbi.nlm.nih.gov/36148237/]
- 20. Advances in nanotechnology-enabled adjuvants for ... [https://www.sciopen.com/article/10.26599/NR.2025.94907534]
- 21. Systematic review and meta-analysis of the effectiveness of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603288/]
- 22. Immunogenicity risk mitigation of therapeutic proteins with ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354925003223]
- 23. Single dose of foot-and-mouth disease peptide vaccine ... [https://www.nature.com/articles/s41541-025-01274-y]
- 24. ELISA versus ELISpot: Which assay is right for your ... [https://www.mabtech.com/knowledge-hub/elisa-versus-elispot-which-assay-right-your-research]
- 25. ELISpot vs. ICS: Optimizing Immune Monitoring in Clinical ... [https://cellcarta.com/science-hub/elispot-vs-ics/]
- 26. Comparison of interferon gamma release assays and ... [https://pubmed.ncbi.nlm.nih.gov/41087415/]
- 27. Comparison between enzymeâ€linked immunospot assay and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9449588/]
- 28. Comparison of Immunologic Assays for Detecting Immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944467/]
- 29. Alternative Evaluation of an ELISPOT Assay Using ... [https://ar.iiarjournals.org/content/41/8/3825]
- 30. Optimizing Microneutralization and IFN-γ ELISPOT Assays ... [https://www.mdpi.com/2076-393X/13/1/27]
- 31. Improving the diagnostic performance for prior COVID-19 ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1675605/full]
- 32. An overview of ELISA: a review and update on best laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808753/]
- 33. Cross-comparison study of three ELISA methodologies to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570479/]
- 34. ELISA: The Complete Guide [https://www.antibodies.com/applications/elisa]
- 35. In silico design and in vitro validation of a multi-epitope ... [https://pubmed.ncbi.nlm.nih.gov/40626008/]
- 36. In silico design and in vitro validation of a multi-epitope ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1611991/full]
- 37. ELISA (Enzyme-linked Immunosorbent Assay) Test Results ... [https://www.cellsignal.com/applications/elisa/analyzing-results-from-elisa?srsltid=AfmBOopaqq6ESbNVTycrJTswfGFwceqio8HAiafPuf-BVVAyX4g2aEqf]
- 38. How to Analyze ELISA Data and Calculate Results [https://www.bosterbio.com/blog/post/how-to-analyze-elisa-data-and-calculate-results-step-by-step-guide-with-troubleshooting-tips?srsltid=AfmBOoqB85WARu6v56rKCQMuLp2M-vSBuqF9MNn5IEURcgN-6l-2FpA2]
- 39. ELISA Data Analysis | Thermo Fisher Scientific - ES [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-data-analysis.html]
- 40. MHC-Associated Peptide Proteomics (MAPPs) as a Tool ... [https://www.chromatographyonline.com/view/mhc-associated-peptide-proteomics-mapps-as-a-tool-for-assessment-of-immunogenicity-risk-potential-of-therapeutic-monoclonal-antibodies]
- 41. MAPPs assays for non-clinical immunogenicity risk assessment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12549661/]
- 42. Applying MAPPs Assays to Assess Drug Immunogenicity [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.00698/full]
- 43. MHC-Associated Peptide Proteomics: Immunogenicity and ... [https://abzena.com/articles/feature-articles/mhc-associated-peptide-proteomics-immunogenicity-and-vaccine-design-2/]
- 44. Assessing MAPPs assay as a tool to predict the ... [https://www.life-science-alliance.org/content/7/1/e202302095]
- 45. The MHC Associated Peptide Proteomics assay is a useful ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10616951/]
- 46. MHC-Associated Peptide Proteomics: Immunogenicity and ... [https://www.biopharminternational.com/view/mhc-associated-peptide-proteomics-immunogenicity-and-vaccine-design]
- 47. A universal monoallelic human leukocyte antigen class II ... [https://www.nature.com/articles/s42003-025-08692-7]
- 48. HLAIIPred: cross-attention mechanism for modeling the ... [https://www.nature.com/articles/s42003-025-08500-2]
- 49. Peptide libraries: from epitope mapping to in-depth high- ... [https://pubmed.ncbi.nlm.nih.gov/38724411/]
- 50. EPIphany—A Platform for Analysis and Visualization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9581008/]
- 51. High-resolution Mapping of Linear Antibody Epitopes ... [https://www.sciencedirect.com/science/article/pii/S153594762033471X]
- 52. Comparison of eight commercial, high-throughput ... [https://pubmed.ncbi.nlm.nih.gov/32942137/]
- 53. Comparison of Elisa with other commonly used Immunoassa [https://www.mybiosource.com/learn/comparison-of-elisa-with-other-commonly-used-immunoassa/]
- 54. Comparative Analysis of Multiple Immunoassays for ... [https://www.sciencedirect.com/science/article/pii/S2472555222066473]
- 55. Utilizing murine dendritic cell line DC2.4 to evaluate the... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10925716/]
- 56. IEDBâ€3D 2.0: Structural data analysis within the Immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10022491/]
- 57. AI-driven epitope prediction: a systematic review ... [https://www.nature.com/articles/s41541-025-01258-y]
- 58. Dendritic Cell Markers [https://www.antibodies.com/primary-antibodies/cell-markers/immune-cell-markers/dendritic-cell-markers]
- 59. Mature dendritic cells enriched in immunoregulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9937888/]
- 60. CD83: Activation Marker for Antigen Presenting Cells and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.01312/full]
- 61. Incorporating immune cell surrogates into a full-thickness ... [https://www.nature.com/articles/s41598-024-81014-9]
- 62. Cell shape sensing licenses dendritic cells for homeostatic ... [https://www.nature.com/articles/s41590-024-01856-3]
- 63. Challenges and opportunities on achieving an adequate ... [https://www.sciencedirect.com/science/article/pii/S0169409X25001607]
- 64. Next-Generation Vaccine Platforms: Integrating Synthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12197771/]
- 65. Development of a Spherical Nucleic Acid Nanovaccine for ... [https://www.dovepress.com/denv-peptides-delivered-as-spherical-nucleic-acid-constructs-enhance-a-peer-reviewed-fulltext-article-IJN]
- 66. Rational vaccinology with spherical nucleic acids - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6535021/]
- 67. Vaccine adjuvants: mechanisms and platforms [https://www.nature.com/articles/s41392-023-01557-7]
- 68. Advances in vaccine adjuvant development and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180328/]
- 69. Engineering STING Nanoadjuvants for spatiotemporally ... [https://www.nature.com/articles/s41467-025-60927-7]
- 70. Development and Efficacy Evaluation of a Novel Nano ... [https://www.mdpi.com/2079-4991/12/22/3934]
- 71. Methodological approach to identify immunogenic epitopes candidates for vaccines against emerging pathogens tailored to defined HLA populations - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1476927125000490]
- 72. The Use of a Rapid ELISPOT Assay to Analyze Peptide ... [https://pubmed.ncbi.nlm.nih.gov/11129322/]
- 73. A Mathematical Framework for the Selection of an Optimal Set of Peptides for Epitope-Based Vaccines | PLOS Computational Biology [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1000246]
- 74. Cell-Based Assays for Immunogenicity and Immunotoxicity [https://bioscience.lonza.com/lonza_bs/CH/en/introduction-to-immunogenicity-assay]
- 75. Use of In Vitro Assays to Assess Immunogenicity Risk ... [https://pubmed.ncbi.nlm.nih.gov/27494246/]
- 76. Adaptable antigen matrix platforms for peptide vaccination ... [https://www.sciencedirect.com/science/article/pii/S0142961220305883]
- 77. Peptide Solubility Limits: Backbone and Side-Chain Interactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC5909690/]
- 78. Peptide stability, storage and solubilisation [http://www.innovagen.com/peptide-stability-storage-and-solubilisation]
- 79. Thermal stability of self-assembled peptide vaccine materials [https://pmc.ncbi.nlm.nih.gov/articles/PMC4821069/]
- 80. Stability of Multi-Peptide Vaccines in Conditions Enabling ... [https://link.springer.com/article/10.1007/s10989-024-10620-y]
- 81. Enantiomeric purity of synthetic therapeutic peptides [https://pubmed.ncbi.nlm.nih.gov/38448043/]
- 82. Enantiomeric purity analysis of synthetic peptide ... [https://www.sciencedirect.com/science/article/abs/pii/S157002322300048X]
- 83. Immunogenicity of therapeutic peptide products: bridging the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213570/]
- 84. Structure and Immunogenicity of a Peptide Vaccine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3945320/]
- 85. Antibody Validation Essentials: Orthogonal Strategy - CST Blog [https://blog.cellsignal.com/hallmarks-of-validation-orthogonal-strategy]
- 86. Accelerated vaccine process development by orthogonal ... [https://www.nature.com/articles/s41598-025-96642-y]
- 87. Immunogenicity of a peptide-based vaccine for measles [https://www.nature.com/articles/s41598-024-69825-2]
- 88. A Novel Flow Cytometry Array for High Throughput ... [https://www.mdpi.com/2076-393X/13/10/1063]
- 89. Comparison of ELISA and flow cytometry for measurement ... [https://www.degruyterbrill.com/document/doi/10.1515/tjb-2017-0164/html?lang=en&srsltid=AfmBOormgBTOuFEoTWNXre-C000YNHIY7OfKH3DeXIfyrj4LRUIiGzgA]
- 90. Establishing correlation between in vitro potency and in ... [https://www.nature.com/articles/s41541-025-01181-2]
- 91. In Vitro vs In Vivo Potency Assays: Modern Vaccine Batch ... [https://www.quantics.co.uk/blog/in-vitro-vs-in-vivo-potency-assays-modern-vaccine-batch-release/]
- 92. Immunization with peptide encapsulated within synthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505882/]
- 93. In Vitro vs In Vivo: Complete Comparison + Selection Guide [https://www.assaygenie.com/in-vitro-vs-in-vivo-complete-comparison-selection-guide-research-methods/?srsltid=AfmBOoo3zqtMEs2chNw5GDIt2fWr5UsGVm5wTTTuhRm5ZeCRnOnoGWlK]
- 94. The merits of in vitro versus in vivo modeling ... [https://www.sciencedirect.com/science/article/abs/pii/S1382668905001158]
- 95. Multi-Epitope-Based Peptide Vaccine Against Bovine ... [https://www.mdpi.com/2306-7381/12/11/1074]
- 96. AI-driven epitope prediction: a systematic review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398602/]
- 97. Epitope-Based Vaccines: The Next Generation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11946261/]
- 98. Multipeptide vaccines for melanoma in the adjuvant setting [https://www.nature.com/articles/s41467-024-46877-6]
- 99. Safety and Immunogenicity of a CTL Multiepitope Peptide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2692338/]
- 100. Evaluation of immunogenicity of novel multi-epitope ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576919314754]
- 101. Phase I Trial of a Peptide-Based Vaccine to Prevent Group ... [https://www.mdpi.com/2504-3900/124/1/26]
- 102. Prediction of measles cases in US counties: A machine ... [https://www.sciencedirect.com/science/article/pii/S0264410X2400971X]
- 103. Long-term immunogenicity after measles vaccine vs. wild ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8189124/]
- 104. Enhancement of peptide vaccine immunogenicity by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6247902/]
- 105. In Vitro Immunogenicity Assays for Evaluating Generic ... [https://www.fda.gov/science-research/fda-science-forum/in-vitro-immunogenicity-assays-evaluating-generic-peptide-drug-products]
- 106. Impact of genotypic variability of measles virus T-cell ... [https://www.nature.com/articles/s41541-025-01088-y]
- 107. Recent Advances, Approaches and Challenges in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10957243/]