Achieving Cross-Lab Reproducibility in Immunological Assays: A Framework for Standardization, Validation, and Best Practices
This article provides a comprehensive framework for researchers, scientists, and drug development professionals aiming to improve the reproducibility of immunological assays across different laboratories.
Achieving Cross-Lab Reproducibility in Immunological Assays: A Framework for Standardization, Validation, and Best Practices
Abstract
This article provides a comprehensive framework for researchers, scientists, and drug development professionals aiming to improve the reproducibility of immunological assays across different laboratories. It explores the foundational challenges and sources of variability, details methodological best practices and standardized protocols for key assays like the DC maturation assay and flow cytometry, offers troubleshooting strategies for critical parameters such as cell fitness and reagent validation, and establishes a rigorous approach for assay validation and comparative analysis. By synthesizing current research and multi-institutional efforts, this guide aims to equip scientists with the knowledge to generate reliable, comparable, and clinically translatable immunological data.
Understanding the Reproducibility Crisis in Immunological Testing
Reproducibility forms the cornerstone of scientific validity, particularly in biomedical research where immunological assays provide critical data for vaccine development and therapeutic interventions. The consistency of experimental results—whether within a single laboratory, across multiple facilities, or when different methodologies are applied—directly impacts the reliability of scientific conclusions and the success of clinical translation. In immunological research, the challenges of achieving reproducible data are compounded by complex assay requirements, reagent variability, and the need for standardized protocols. This guide examines the multifaceted nature of reproducibility through the lens of recent interlaboratory studies and methodological validations, providing researchers with comparative data and frameworks to enhance the reliability of their experimental findings.
The Three Dimensions of Reproducibility
Intra-laboratory Precision
Intra-laboratory precision, also known as intermediate precision, measures the consistency of results within a single laboratory under varying conditions such as different analysts, equipment, or days. This dimension of reproducibility captures the inherent variability of an assay when performed within one facility.
A study evaluating a multiplex immunoassay for Group B streptococcus (GBS) capsular polysaccharide antibodies demonstrated exceptional within-laboratory precision. Across five participating laboratories, the relative standard deviation (RSD) was generally below 20% for all six GBS serotypes when factoring in variables like bead lots, analysts, and testing days [1]. Similarly, a microneutralization assay for detecting anti-AAV9 neutralizing antibodies reported intra-assay variations of 7-35% for low positive quality controls [2].
Table 1: Intra-laboratory Precision Metrics Across Assay Types
| Assay Type | Target | Precision Metric | Reported Value | Key Variables Tested |
|---|---|---|---|---|
| Multiplex Immunoassay | GBS CPS Serotypes | Relative Standard Deviation (RSD) | <20% | Bead lot, analyst, day [1] |
| Microneutralization Assay | Anti-AAV9 NAbs | Intra-assay Variation | 7-35% | Low positive QC samples [2] |
| Microneutralization Assay | Anti-AAV9 NAbs | Inter-assay Variation | 22-41% | Low positive QC samples [2] |
| MEASURE Assay | fHbp Surface Expression | Total RSD | ≤30% | Multiple operators/runs [3] |
Inter-laboratory Reproducibility
Inter-laboratory reproducibility represents the ability of different laboratories to produce consistent results using the same method. This is particularly crucial for multi-center clinical trials and global health initiatives where data must be comparable across sites.
The GBS multiplex immunoassay study demonstrated remarkable cross-laboratory reproducibility, with RSD values below 25% for all six serotypes across five different laboratories [1]. This consistency was achieved despite the participating facilities being located in different countries (USA, England, and South Africa), highlighting the effectiveness of standardized protocols and reagents.
In the validation of a meningococcal MEASURE assay, three independent laboratories achieved >97% agreement when classifying 42 MenB test strains based on a predetermined fluorescence intensity threshold [3]. This high level of concordance is significant as the MEASURE assay predicts strain susceptibility to vaccine-induced antibodies, a critical determination for vaccine efficacy assessment.
Table 2: Inter-laboratory Reproducibility in Recent Studies
| Assay Type | Participating Laboratories | Reproducibility Metric | Performance | Significance |
|---|---|---|---|---|
| GBS Multiplex Immunoassay | 5 (Pfizer, UKHSA, CDC, St. George's, Witwatersrand) | Cross-lab RSD | <25% all serotypes | Enables data comparison across studies [1] |
| MEASURE Assay | 3 (Pfizer, UKHSA, CDC) | Classification Agreement | >97% | Consistent prediction of vaccine susceptibility [3] |
| Microneutralization Assay | 3 (Beijing laboratories) | % Geometric Coefficient of Variation | 23-46% | Supports clinical trial application [2] |
| Malaria Multiplex Immunoassay | 2 (MSD, Jenner Institute) | Correlation of Clinical Samples | Statistically significant (all antigens) | Validated for Phase 3 clinical trial use [4] |
Methodological and Analytical Challenges
Methodological challenges encompass issues related to protocol standardization, reagent characterization, and data analysis approaches that impact reproducibility regardless of where an assay is performed.
The antibody characterization crisis represents a significant methodological challenge, with an estimated 50% of commercial antibodies failing to meet basic characterization standards [5]. This deficiency costs the U.S. research community an estimated $0.4-1.8 billion annually in irreproducible research [5].
In artificial intelligence applications for biomedical data science, reproducibility faces unique challenges from inherent non-determinism in AI models, data preprocessing variations, and substantial computational requirements that hinder independent verification [6]. For complex models like AlphaFold3, the computational cost alone presents a significant barrier to reproducibility, with the original AlphaFold requiring 264 hours of training on specialized Tensor Processing Units [6].
Standardized Experimental Protocols for Enhanced Reproducibility
GBS Multiplex Immunoassay Protocol
The standardized GBS multiplex immunoassay (MIA), adopted by the GASTON consortium, exemplifies a robust protocol designed for cross-laboratory reproducibility [1]:
- Bead Coupling: MagPlex microspheres are coupled with GBS capsular polysaccharide Poly-L-Lysine conjugates following standardized coating procedures
- Assay Setup: Each 96-well plate includes an 11-point human serum reference standard dilution series, quality control samples, and test serum samples diluted in assay buffer (0.5% BSA in 10 mM PBS/0.05% Tween-20/0.02% NaN3, pH 7.2)
- Incubation: Test serum samples are tested in duplicate at 1:500, 1:5,000, and 1:50,000 dilutions with overnight incubation
- Detection: Plates are washed using a standardized protocol, followed by addition of R-Phycoerythrin-conjugated goat anti-human IgG secondary antibody
- Analysis: Plates are read on a Luminex 200 reader using Bio-Plex Manager, with signal output expressed as mean fluorescence intensity (MFI)
Microneutralization Assay for Anti-AAV9 Antibodies
The optimized microneutralization assay for detecting anti-AAV9 neutralizing antibodies incorporates critical quality controls [2]:
- Sample Pre-treatment: Serum or plasma samples are heat-inactivated at 56°C for 30 minutes
- Virus Neutralization: 50 μL of 2-fold serially diluted serum (starting at 1:20) is incubated with 2×10^8 vg of rAAV9-EGFP-2A-Gluc in 50 μL DMEM with 0.1% BSA for 1 hour at 37°C
- Cell Infection: The mixture is added to HEK293-C340 cells (20,000 cells/well) and incubated for 48-72 hours
- Detection: Gaussian luciferase activity is measured using a luciferase assay system with coelenterazine substrate
- Quality Control: System QC requires inter-assay titer variation of <4-fold difference or geometric coefficient of variation <50%
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Their Functions in Reproducible Immunoassays
| Reagent/ Material | Function | Reproducibility Considerations | Examples from Literature |
|---|---|---|---|
| Qualified Bead Lots | Solid phase for antigen immobilization | Lot-to-lot variability must be <20% RSD; qualification against reference lot required [1] | GBS CPS-PLL coated beads [1] |
| Human Serum Reference Standard | Quantification standard for IgG antibodies | Enables comparison across laboratories and studies; weight-based IgG assignments [1] | GBS human serum reference standard [1] |
| Quality Control Samples (QCS) | Monitoring assay performance | Pools of immune human serum samples; tested in each run [1] | GBS QCS from immune human serum pools [1] |
| rAAV Vectors with Reporter Genes | Virus neutralization target | Empty and full virus particles separated; <10% empty capsids [2] | rAAV9-EGFP-2A-Gluc [2] |
| Anti-AAV Neutralizing Monoclonal Antibody | System suitability control | Used for quality control; defines acceptable variation thresholds [2] | Mouse neutralizing monoclonal antibody in human negative serum [2] |
| Secondary Antibodies | Detection | Conjugated for specific detection methods; lot consistency critical [1] [4] | R-Phycoerythrin-conjugated goat anti-human IgG [1] |
Factors Influencing Reproducibility Across Dimensions
The pursuit of reproducibility in immunological assays requires systematic attention to intra-laboratory precision, inter-laboratory consistency, and methodological rigor. The case studies examined demonstrate that carefully standardized protocols, qualified reagents, and appropriate statistical approaches can achieve remarkable reproducibility across multiple laboratories, with relative standard deviations frequently below 25% and classification agreements exceeding 97%. The continued development of standardized assays like the GBS GASTON assay and the MEASURE assay, coupled with increased attention to antibody characterization and computational reproducibility, provides a roadmap for enhancing reliability in immunological research. As the field progresses, adherence to these principles will be essential for generating translatable findings that successfully bridge basic research and clinical application.
Reproducibility is a cornerstone of scientific research, yet immunological assays are particularly prone to variability that can compromise data reliability and cross-study comparisons. This guide objectively compares sources of variability and their impact on assay performance across different laboratory settings. Evidence from multi-site proficiency testing and methodological comparisons reveals that variability arises at every stage of the experimental workflow, from sample collection to final data interpretation [7]. Understanding and managing these sources is crucial for researchers, scientists, and drug development professionals who rely on precise and reproducible immunological data for critical decisions in therapeutic development and clinical applications.
Sample Collection and Handling
The pre-analytical phase introduces significant variability before formal testing begins. Sample stability is profoundly affected by handling conditions. Multi-site studies demonstrate that cytokine measurements in serum can vary by 10-25% based solely on freeze-thaw cycles or duration of sample storage at room temperature [7]. The matrix effect—where samples are diluted in serum, plasma, or artificial buffers—also substantially impacts recovery rates, particularly in immunoassays where sample composition interferes with antibody binding [8].
Reagents and Biological Materials
Reagent quality and consistency are fundamental to assay reproducibility. Critical reagents such as capture antibodies, detection antibodies, and analyte standards exhibit lot-to-lot variations that directly impact assay performance. Table 1 summarizes the effects of key reagent-related variables.
Table 1: Impact of Reagent Variability on Assay Performance
| Variable | Impact on Assay | Evidence |
|---|---|---|
| Antibody affinity/ specificity | Alters sensitivity, dynamic range | Affinity-purified antibodies reduce non-specific binding [8] |
| Coating buffer composition | Affects immobilization efficiency | Comparison of carbonate-bicarbonate vs. PBS buffers [8] |
| Blocking buffer formulation | Changes background signal, noise | Casein-based blockers reduce non-specific binding vs. BSA [8] |
| Conjugate enzyme stability | Impacts detection sensitivity | HRP vs. alkaline phosphatase substrate kinetics [8] |
Biological materials present additional challenges. Use of misidentified, cross-contaminated, or over-passaged cell lines compromises experimental validity and reproducibility [9]. Long-term serial passaging can alter gene expression, growth rates, and physiological responses, generating significantly different results across laboratories using supposedly identical cellular models [9].
Assay Execution and Platform Differences
Technical execution contributes substantially to variability. In bead-based cytokine assays, procedural differences in washing steps, incubation timing, and temperature control account for approximately 15-30% of inter-laboratory variation [7]. Instrument selection introduces another layer of variability, with different plate readers and flow cytometers producing systematically different readouts despite identical samples [10] [7].
Substantial inter-assay differences emerge even when measuring the same analyte. For example, two different pseudovirus-based SARS-CoV-2 neutralization assays (Duke and Monogram) showed statistically significant differences in measured antibody titers when testing identical samples, with the Monogram assay consistently reporting higher values [11]. These differences necessitate statistical bridging methods to compare or combine data across platforms.
Quantitative Evidence from Multi-Laboratory Studies
Multi-site proficiency testing provides the most compelling evidence of variability in real-world conditions. The External Quality Assurance Program Oversight Laboratory (EQAPOL) multiplex program, conducting 22 rounds of proficiency testing over 12 years with over 40 laboratories, offers comprehensive data on inter-laboratory variability [7].
Table 2: Inter-Laboratory Variability in Cytokine Measurements from EQAPOL Program
| Cytokine | Concentration (pg/mL) | Inter-lab CV (%) | Major Source of Variability |
|---|---|---|---|
| IL-2 | 50 | 15-25% | Bead type, detection antibody |
| IL-6 | 100 | 12-20% | Standard curve fitting |
| IL-10 | 75 | 18-30% | Matrix effects, sample dilution |
| TNF-α | 50 | 10-22% | Instrument calibration |
| IFN-γ | 100 | 20-35% | Bead type, sample handling |
The data reveal that variability is analyte-dependent, with some cytokines exhibiting consistently higher coefficients of variation (CV) across laboratories. The switch from polystyrene to paramagnetic beads early in the program significantly reduced average inter-laboratory CVs by approximately 8-12%, highlighting how single technological improvements can enhance reproducibility [7]. However, proficiency scores stabilized after initial improvements, suggesting fundamental limits to technical standardization.
Similar variability was observed in T-cell immunophenotyping across five laboratories, where interlaboratory differences were statistically significant for all T-cell subsets except CD4+ cells, ranging from minor to eightfold for CD25+ subsets [10]. Notably, the date of analysis was significantly associated with values for all cellular activation markers within laboratories, emphasizing the impact of temporal drift even in established assays [10].
Experimental Protocols for Assessing Variability
Variance Component Analysis
Formal statistical approaches are essential for quantifying variability. Variance component analysis, consistent with USP 〈1033〉, partitions total variability into its constituent sources [12]. The recommended practice involves:
- Logarithmic Transformation: Apply base e logarithm to relative potency results to reduce variance heterogeneity with increasing potency [12].
- Experimental Design: Execute studies with multiple analysts over several days, with two assays performed by each analyst daily.
- Variance Calculation: Use statistical software to estimate variance components for each source (e.g., analyst, day, inter-assay).
- Percentage Calculation: Convert variance components to more interpretable %CV or %GCV using the formulas:
- %CV = 100√{exp(Vc) - 1}
- %GCV = 100(exp(√Vc) - 1) where Vc is the variance component estimate [12].
This approach enables practitioners to identify whether variability stems predominantly from analyst-to-analyst differences, day-to-day variation, or inter-assay effects, allowing targeted improvement efforts.
Bridging Different Assay Platforms
When combining data from different assays, statistical bridging methods are essential. The left-censored multivariate normal model accommodates differences in both measurement error and lower limits of detection (LOD) between assays [11]. The protocol involves:
- Paired Sample Collection: Obtain samples measured by both assays (e.g., Duke and Monogram nAb assays).
- Model Establishment: Assume (Xâ‚, Xâ‚‚) follow a bivariate normal distribution, where Xâ‚ and Xâ‚‚ represent measurements from two different assays.
- Parameter Estimation: Account for left-censoring due to different LODs in each assay.
- Calibration: Use established relationships to convert measurements between assays or combine data for meta-analysis [11].
This method prevents misleading conclusions when comparing immunogenicity between vaccine regimens or evaluating correlates of risk using data from different assays [11].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Their Functions in Immunoassays
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Solid Surfaces | Greiner high-binding plates, Nunc plates | Optimal antigen/antibody immobilization with minimal lot-to-lot variability [8] |
| Coating Buffers | 50mM sodium bicarbonate (pH 9.6), PBS (pH 8.0) | Maximize binding efficiency of capture antibodies or antigens to solid phase [8] |
| Blocking Buffers | 1% BSA in TBS, Casein-based blockers, Heterophilic blocking reagents | Reduce non-specific binding to minimize background signal [8] |
| Wash Buffers | PBST (0.05% Tween-20), TBST | Remove unbound reagents while maintaining assay integrity [8] |
| Detection Systems | HRP/TMB, Alkaline phosphatase/pNPP | Generate measurable signal with optimal signal-to-noise ratio [8] |
| Reference Materials | Authenticated, low-passage cell banks, Characterized serum pools | Provide standardization across laboratories and over time [13] [9] |
| H-Phe-Trp-OH | H-Phe-Trp-OH, CAS:24587-41-5, MF:C20H21N3O3, MW:351.4 g/mol | Chemical Reagent |
| NSC 16590 | NSC 16590, CAS:62-57-7, MF:C4H9NO2, MW:103.12 g/mol | Chemical Reagent |
Strategies for Managing Variability
Measurement Assurance Framework
A systematic measurement assurance framework identifies, minimizes, and monitors variability throughout the experimental process [13]. This approach includes:
- Clearly Defined Measurands: Precisely specify what physical property is being measured (e.g., "number of cells fluorescently labeled with a membrane-impermeant dye" for viability counting) [13].
- Fit-for-Purpose Validation: Qualify assays for sensitivity, limits of detection, linearity, specificity, accuracy, precision, and robustness [13].
- In-Process Controls: Implement controls at each step to monitor variability during sample preparation, data collection, and analysis [13].
- Reference Materials: Use authenticated biological reference materials with documented performance characteristics to calibrate measurements across instruments and laboratories [13].
Statistical and Design Approaches
Robust experimental design significantly reduces variability. Design of Experiment (DOE) methodologies systematically evaluate the sensitivity of assays to changes in experimental parameters, establishing acceptable performance ranges for critical factors such as enzymatic treatment times, reagent concentrations, and incubation conditions [13]. Pre-registering studies, including detailed methodologies, helps standardize approaches across laboratories and reduces selective reporting [9]. Publishing negative data is equally valuable, as it helps interpret positive results and prevents resource waste on irreproducible findings [9].
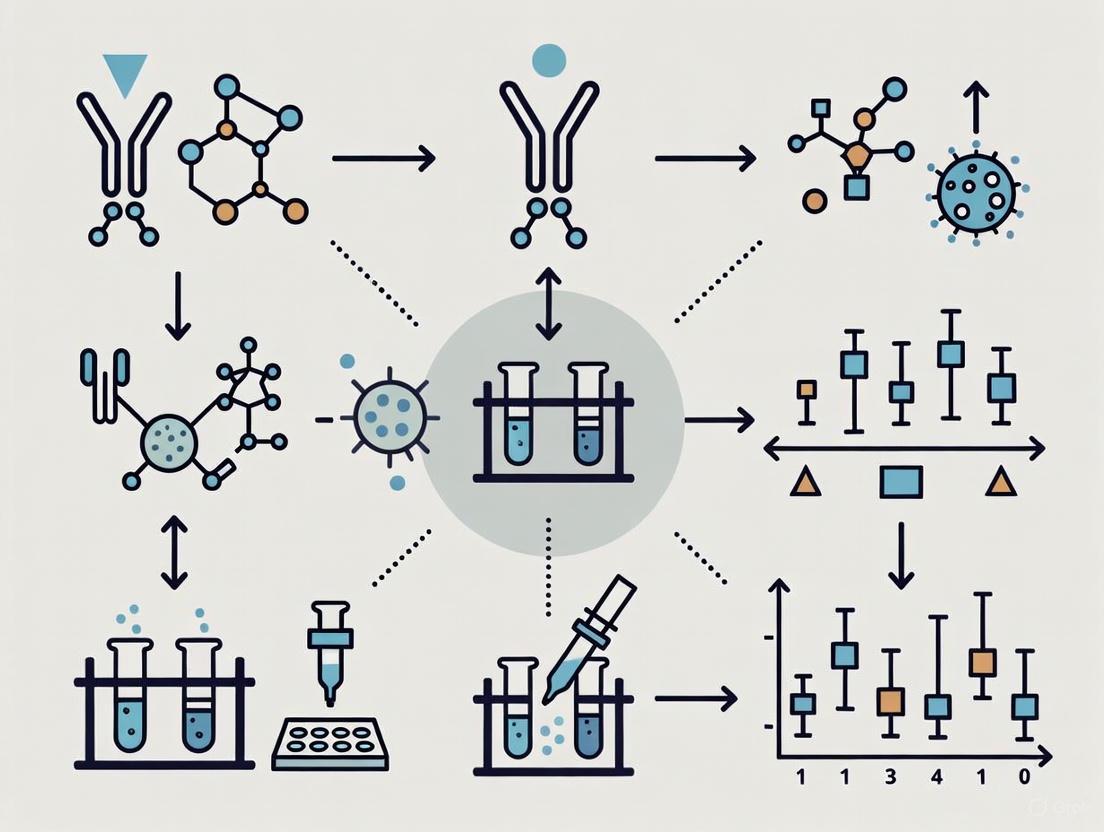
The above diagram illustrates a systematic framework for managing variability throughout the measurement process, incorporating specific assurance tools at each experimental stage.
Variability in immunological assays arises from interconnected technical and biological sources spanning the entire experimental workflow. Evidence from multi-laboratory studies demonstrates that consistent implementation of measurement assurance strategies—including standardized protocols, validated reagents, appropriate statistical bridging, and reference materials—significantly improves reproducibility. While some variability is inherent to complex biological systems, systematic approaches to its identification and management enable more reliable data interpretation and cross-study comparisons, ultimately accelerating drug development and scientific discovery.
Immunogenicity—the unwanted immune response to therapeutic biologics or vaccines—poses a significant challenge throughout the drug development pipeline. For protein-based therapeutics, immunogenicity can trigger the development of anti-drug antibodies (ADAs) that reduce efficacy, alter pharmacokinetics, and potentially cause severe adverse events [14]. Similarly, vaccine development requires careful assessment of immunogenicity to ensure consistent protection against targeted pathogens. The reproducibility of immunological assays across different laboratories is therefore paramount for accurately evaluating product performance, enabling meaningful comparisons between platforms, and ensuring regulatory compliance.
This guide objectively compares experimental approaches for immunogenicity and vaccine assessment, focusing on interlaboratory reproducibility data. We examine case studies across therapeutic classes, provide detailed methodological protocols, and present quantitative comparisons of assay performance to support scientific and regulatory decision-making.
Comparative Analysis of Immunological Assay Reproducibility
Reproducibility of the Meningococcal MEASURE Assay
The Meningococcal Antigen Surface Expression (MEASURE) assay was developed by Pfizer as a flow-cytometry-based method to quantify surface-expressed factor H binding protein (fHbp) on intact meningococci. This assay addresses limitations of the traditional serum bactericidal antibody using human complement (hSBA) assay, which is constrained by human sera and complement requirements [15].
Table 1: Interlaboratory Reproducibility of the MEASURE Assay
| Performance Metric | Pfizer Laboratory | UKHSA Laboratory | CDC Laboratory | Overall Agreement |
|---|---|---|---|---|
| Strain Classification Agreement | Reference | >97% concordance | >97% concordance | >97% across all sites |
| Precision (Total RSD) | ≤30% | ≤30% | ≤30% | All sites met criteria |
| Key Threshold | Mean fluorescence intensity <1000 indicates susceptibility to MenB-fHbp-induced antibodies | |||
| Number of MenB Strains Tested | 42 strains encoding sequence-diverse fHbp variants | |||
| Study Design | Intermediate precision within each laboratory; pairwise comparisons between laboratories |
This interlaboratory study demonstrated that MEASURE assay results were highly consistent across three independent laboratories (Pfizer, UKHSA, and CDC), with >97% agreement in classifying strains above or below the critical threshold for predicting susceptibility to vaccine-induced antibodies [15]. Each laboratory met precision criteria of ≤30% total relative standard deviation, establishing the MEASURE assay as a robust and reproducible platform for meningococcal vaccine assessment.
Reproducibility of Anti-HPV ELISA Isotype Detection
A comprehensive study evaluated the reproducibility of enzyme-linked immunosorbent assays (ELISAs) for detecting different anti-human papillomavirus (HPV) immunoglobulin isotypes in samples from the Costa Rica HPV Vaccine Trial [16].
Table 2: Reproducibility Performance of Anti-HPV16 L1 Isotype ELISAs
| Assay Isotype | Inter-Technician CV (%) | Inter-Day CV (%) | Overall CV (%) | Detectability in Vaccinated Participants | Intraclass Correlation Coefficient (ICC) |
|---|---|---|---|---|---|
| IgG1 | 12.8 | 6.2 | 7.7 | >86.3% | >98.7% |
| IgG3 | 22.7 | 30.6 | 31.1 | 100% | >98.7% |
| IgA | 16.2 | 19.4 | 19.8 | >86.3% | >98.7% |
| IgM | 15.8 | 25.3 | 26.4 | 62.1% | >98.7% |
| Assay Cut-off (EU/mL) | IgG1: 12; IgG3: 1.25; IgA: 0.48; IgM: 4.79 |
The data revealed that IgG1 exhibited the highest precision (lowest coefficients of variation), while IgM showed the greatest variability. IgG3 was detected in all vaccinated participants, whereas IgM had limited detectability (62.1%). All assays demonstrated excellent reliability with ICC values exceeding 98.7% [16]. Correlation analyses showed significant relationships between IgG subclasses and IgA, but not with IgM, informing interpretation of humoral immune responses to HPV vaccination.
Experimental Protocols for Immunological Assays
Three-Tiered Immunogenicity Testing Approach for Biologics
The FDA recommends a three-tiered testing approach for detecting anti-drug antibodies (ADAs) against therapeutic proteins during drug development [14]:
Tier 1: Screening Assay
- Purpose: Maximize sensitivity to minimize false-negatives
- Methodology: Ligand-binding immunoassay format
- Procedure:
- Dilute patient samples in appropriate buffer
- Incubate with immobilized therapeutic protein
- Wash to remove unbound components
- Detect bound antibodies using labeled secondary antibodies
- Compare signals to predetermined cut point (typically based on negative control population)
Tier 2: Confirmatory Assay
- Purpose: Establish specificity and minimize false-positives
- Methodology: Competitive inhibition format
- Procedure:
- Split positive samples from Tier 1 into two aliquots
- Pre-incubate one aliquot with excess soluble therapeutic protein
- Pre-incubate second aliquot with buffer only
- Process both aliquots through Tier 1 method
- Calculate percentage inhibition: [1 - (Signal with inhibitor/Signal without inhibitor)] × 100%
- Samples exceeding predetermined inhibition cut point (e.g., >50%) are confirmed positive
Tier 3: Characterization Assays
- Purpose: Determine ADA titer, isotype, and neutralizing capacity
- Methodologies:
- Titer Determination: Serial dilution of confirmed positive samples until signal falls below cut point
- Isotyping: Use of isotype-specific secondary antibodies
- Neutralizing Antibody Assays: Cell-based or competitive ligand-binding formats to assess interference with therapeutic protein function
A significant limitation of this approach is the reliance on positive controls created in non-human species, which may not accurately represent human ADA responses [14].
MEASURE Assay Protocol
The MEASURE assay protocol for quantifying fHbp expression on meningococcal surfaces consists of the following key steps [15]:
Bacterial Culture Preparation:
- Grow MenB strains to mid-logarithmic phase in appropriate media
- Standardize bacterial density using optical density measurements
Antibody Staining:
- Incubate bacteria with primary anti-fHbp antibody
- Wash to remove unbound antibody
- Incubate with fluorochrome-conjugated secondary antibody
- Include isotype controls for background determination
Flow Cytometry Analysis:
- Acquire data on flow cytometer using standardized instrument settings
- Gate on bacterial population based on light scatter properties
- Analyze minimum of 10,000 events per sample
- Report results as mean fluorescence intensity (MFI)
Data Interpretation:
- Compare MFI values to established threshold of 1000
- Strains with MFI < 1000 are considered susceptible to MenB-fHbp-induced antibodies
HPV Isotype ELISA Protocol
The detailed protocol for anti-HPV16 L1 isotype ELISAs includes these critical steps [16]:
Plate Coating:
- Coat 96-well plates with HPV16 L1 virus-like particles (VLPs) at 50 ng/well in PBS
- Incubate overnight at 4°C
- Block with PBS containing 1% bovine serum albumin and 0.05% Tween-20
Sample and Standard Preparation:
- Prepare serum standard pools from vaccinated individuals at predetermined dilutions (IgG1: 1:4200; IgG3: 1:3150; IgA: 1:200; IgM: 1:300)
- Create standard curves using 2-fold serial dilutions
- Include quality control samples at low, medium, and high concentrations
- Test clinical samples at optimal dilutions determined during assay development
Assay Procedure:
- Add standards and samples to coated plates in duplicate
- Incubate for 2 hours at room temperature
- Wash plates extensively
- Add isotype-specific horseradish peroxidase-conjugated detection antibodies at optimized concentrations (IgG1: 150 ng/mL; IgG3: 233 ng/mL; IgA: 67 ng/mL; IgM: 40 ng/mL)
- Incubate for 1 hour at room temperature
- Develop with tetramethylbenzidine substrate
- Stop reaction with sulfuric acid
- Read optical density at 450 nm with reference wavelength at 620 nm
Data Analysis:
- Generate standard curves using 4-parameter logistic regression
- Apply cut-off values determined from naive samples (3 standard deviations above geometric mean)
- Calculate intra- and inter-assay coefficients of variation
- Determine intraclass correlation coefficients for reproducibility assessment
Immunogenicity Pathways and Testing Workflows
Figure 1: Immunogenicity Cascade Pathway. This diagram illustrates the sequential immune events following biologic administration, from initial innate immune activation to potential clinical consequences of anti-drug antibody production. Route of administration influences immunogenicity risk [14]. ADA: anti-drug antibody; PK: pharmacokinetics.
Figure 2: Three-Tiered Immunogenicity Testing Workflow. This workflow depicts the sequential approach for anti-drug antibody detection and characterization, as recommended by FDA guidance [14]. Each tier serves a distinct purpose in ensuring accurate immunogenicity assessment.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Immunogenicity Assessment
| Reagent/Category | Function/Application | Examples/Specifications |
|---|---|---|
| Positive Controls | Semiquantitative assay calibration; quality control | Polyclonal ADAs from immunized non-human species; critical for assay standardization [14] |
| Isotype-Specific Detection Antibodies | Differentiation of immune response profiles | HRP-conjugated anti-human IgG1, IgG3, IgA, IgM; optimized concentrations for each assay [16] |
| Virus-Like Particles (VLPs) | Antigen source for vaccine immunogenicity assays | HPV16 L1 VLPs for plate coating in ELISA; maintain conformational epitopes [16] |
| Flow Cytometry Reagents | Surface antigen quantification | Anti-fHbp antibodies, fluorochrome-conjugated secondaries; standardized for bacterial staining [15] |
| Assay Standards | Quantitative comparison across laboratories | Pooled immune sera with assigned arbitrary units (EU/mL); enables normalization [16] |
| Cell-Based Reporter Systems | Innate immune response profiling | THP-1 and RAW-Blue reporter cell lines; detect immunogenicity-risk impurities [17] |
| Eplivanserin | Eplivanserin, CAS:130579-75-8, MF:C19H21FN2O2, MW:328.4 g/mol | Chemical Reagent |
| Fluvastatin Lactone | Fluvastatin Lactone, CAS:94061-83-3, MF:C24H24FNO3, MW:393.4 g/mol | Chemical Reagent |
The case studies presented demonstrate that robust, reproducible immunological assays are achievable across multiple laboratories when standardized protocols, calibrated reagents, and validated analysis methods are implemented. The MEASURE and HPV isotype ELISA platforms show how precise quantification of vaccine antigens and immune responses enables reliable product characterization and comparison.
Reproducibility challenges persist, particularly regarding positive control preparation for ADA assays and interpretation of results across different assay platforms [14]. Emerging approaches, including quantitative systems pharmacology models and computational prediction of immunogenic epitopes, show promise for enhancing immunogenicity risk assessment during early drug development [14] [18]. As biologic therapeutics and novel vaccine platforms continue to evolve, standardized assessment of immunogenicity will remain crucial for ensuring product safety, efficacy, and comparability.
The Role of International Consortia and Standardization Initiatives
The reproducibility of immunological assays across different laboratories is a cornerstone of reliable biomedical research and drug development. Variability in assay protocols, reagents, and interpretation criteria can significantly compromise data comparability, potentially delaying diagnostic advancements and therapeutic innovations. International consortia and standardization initiatives have emerged as essential forces in addressing these challenges by establishing harmonized protocols, developing reference materials, and implementing quality assurance programs. These collaborative efforts provide the critical framework needed to ensure that experimental results are consistent, comparable, and transferable from research settings to clinical applications, ultimately strengthening the scientific foundation upon which diagnostic and therapeutic decisions are made.
The absence of analytical standards can lead to startling discrepancies in critical diagnostic tests. For example, a study of estrogen receptor (ER) testing across accredited laboratories revealed that while one laboratory's assay could detect 7,310 target molecules per cell, another required 74,790 molecules—a tenfold difference in analytical sensitivity—to produce a visible result, despite both laboratories passing national proficiency testing [19]. Such inconsistencies underscore the vital role that standardization bodies play in aligning methodological sensitivity and ensuring that assays performed in different settings yield clinically equivalent results.
Major International Standardization Initiatives
Several prominent organizations and consortia have established frameworks to improve the accuracy and reproducibility of immunological assays across laboratories worldwide. These initiatives range from broad regulatory standards to focused technical consortia targeting specific methodological challenges.
Consortium for Analytic Standardization in Immunohistochemistry (CASI)
Established with funding from the National Cancer Institute, CASI addresses a fundamental gap in immunohistochemistry (IHC) testing—the lack of analytical standards. Its mission centers on integrating analytical standards into routine IHC practice to improve test accuracy and reproducibility [19]. CASI operates under two primary mandates: experimentally determining analytical sensitivity thresholds (lower and upper limits of detection) for selected IHC assays, and educating IHC stakeholders about what analytical standards are, why they matter, and how they should be used [19].
CASI promotes the use of quantitative IHC calibrators composed of purified analytes conjugated to solid-phase microbeads at defined concentrations traceable to the National Institute of Standards and Technology (NIST) Standard Reference Material 1934 [19]. This approach allows laboratories to objectively measure their assay's lower limit of detection (LOD) and align it with the analytical sensitivity of original clinical trial assays, thereby creating a crucial link between research validation and diagnostic implementation.
External Quality Assurance Programs
External quality assurance (EQA) programs, also known as proficiency testing, serve as practical tools for assessing and improving interlaboratory consistency. The Spanish Society for Immunology's GECLID program represents a comprehensive example, running 13 distinct EQA schemes for histocompatibility and immunogenetics testing [20]. Between 2011 and 2024, this program collected and evaluated over 1.69 million results across various assay types, including anti-HLA antibody detection, molecular typing, chimerism analyses, and crossmatching [20].
These programs enable ongoing performance monitoring and harmonization across participating laboratories. The success rates reported by GECLID demonstrate the effectiveness of such initiatives, with molecular typing schemes achieving 99.2% success, serological typing at 98.9%, crossmatches at 96.7%, and chimerism analyses at 94.8% [20]. Importantly, in 2022, 61.3% of participating laboratories successfully passed every HLA EQA scheme, while 87.9% of annual reports were rated satisfactory, indicating generally strong performance with targeted areas for improvement [20].
International Assay Comparison Studies
Collaborative studies across multiple laboratories have played a pivotal role in understanding sources of variability and establishing standardized approaches. A landmark international collaborative study published in 1990 involving 11 laboratories comparing 14 different methods for detecting HIV-neutralizing antibodies demonstrated that excellent between-laboratory consistency was achievable [21]. This study identified the virus strain used as the most important variable, while factors such as cell line, culture conditions, and endpoint determination method proved less impactful [21].
Similar approaches have been applied to influenza serology. A 2020 comparison of influenza-specific neutralizing antibody assays found that while different microneutralization (MN) assay readouts (cytopathic effect, hemagglutination, ELISA, RT-qPCR) showed good correlation, the agreement of nominal titers varied significantly depending on the readouts compared and the virus strain used [22]. The study identified the MN assay with ELISA readout as having the highest potential for standardization due to its reproducibility, cost-effectiveness, and unbiased assessment of results [22].
Comparative Analysis of Standardization Initiatives
The table below summarizes key international standardization initiatives, their focal areas, and their documented impacts on assay reproducibility.
Table 1: Comparison of Major International Standardization Initiatives in Immunological Assays
| Initiative/Program | Primary Focus | Key Metrics | Impact on Reproducibility |
|---|---|---|---|
| Consortium for Analytic Standardization in Immunohistochemistry (CASI) [19] | Developing analytical standards for IHC assays | • Lower/upper limits of detection• Quantitative calibrators traceable to NIST | Addresses 10-30% discordance rates in IHC testing; enables standardized method transfer from clinical trials to diagnostics |
| GECLID External Quality Assurance [20] | Proficiency testing for immunogenetics laboratories | • 1.69+ million results evaluated• 13 specialized schemes• 99.2% success rate for molecular typing | Identifies error sources (nomenclature, risk interpretation); ensures homogeneous results across different methods and laboratories |
| International HIV Neutralization Assay Comparison [21] | Method comparison for HIV antibody detection | • 11 laboratories• 14 methods compared• Virus strain identified as key variable | Demonstrated excellent between-laboratory consistency; established that standardization is readily achievable |
| Influenza MN Assay Standardization Study [22] | Identifying optimal readout for influenza neutralization assays | • 4 MN readouts compared• ELISA readout showed highest reproducibility• Correlation with HAI titers | Recommended standardized MN protocol with ELISA readout to minimize interlaboratory variability |
Experimental Protocols and Methodologies
Standardization initiatives rely on rigorous experimental approaches to evaluate and harmonize assay performance. The following section details key methodologies employed by these programs.
IHC Calibrator Protocol for Determining Limits of Detection
The CASI consortium has pioneered the use of calibrators to determine the analytical sensitivity of IHC assays [19]. The experimental workflow proceeds through several critical stages:
Figure 1: IHC Calibrator Workflow for Detection Limits
- Calibrator Preparation: Purified analytes are conjugated to clear cell-sized (7-8 µm) glass microbeads at up to 10 defined concentration levels, with values traceable to NIST Standard Reference Material 1934 [19].
- Parallel Processing: Calibrators undergo identical processing as tissue samples, including deparaffinization, hydration, and antigen retrieval [19].
- Visual Detection Threshold Determination: The lowest calibrator level that produces visible color after IHC staining establishes the lower limit of detection (LOD) [19].
- Analytic Response Characterization: Higher analyte concentrations typically show an initial linear increase in stain intensity followed by a plateau at maximum response [19].
- Quantitative Reporting: The LOD is expressed as the number of analyte molecules per cell equivalent, providing a standardized metric for comparing assay sensitivity across laboratories [19].
External Quality Assurance (EQA) Assessment Methodology
The GECLID program follows a rigorous protocol for administering and evaluating EQA schemes [20]:
Figure 2: External Quality Assurance Assessment Process
- Sample Selection and Distribution: Programs obtain peripheral blood (buffy coats) and sera from biobanks, with minimal processing to maintain samples representative of routine clinical specimens [20].
- Participant Analysis: Laboratories process samples using their standard protocols, including both commercial kits and laboratory-developed tests, reflecting real-world practice [20].
- Result Collection: Participants report results through standardized web forms, capturing data on methodology, reagents, and interpretation criteria [20].
- Consensus Value Assignment: Using algorithms specified in ISO 13528, the program analyzes all reported results to determine assigned values for each parameter [20].
- Performance Evaluation: Individual laboratory results are compared against consensus values using scoring systems aligned with European Federation for Immunogenetics (EFI) standards [20].
- Reporting: Comprehensive reports detail overall performance metrics alongside individualized feedback, identifying specific areas requiring improvement [20].
International Method Comparison Protocol
The international HIV neutralization assay study established a model for multi-laboratory method comparisons [21]:
- Panel Design: A blinded panel of 10 coded sera plus positive and negative controls was distributed to all participating laboratories [21].
- Parallel Testing: Each laboratory tested the panel using their established neutralization assay methods (14 different methods across 11 laboratories) [21].
- Data Collection: Laboratories reported both methodological details (virus strain, cell line, culture conditions, endpoint determination) and experimental results [21].
- Correlation Analysis: Results were analyzed for within-laboratory and between-laboratory consistency, identifying key variables contributing to variability [21].
- Recommendation Development: Based on findings, the study identified the virus strain as the most critical variable requiring standardization for improved reproducibility [21].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of standardized immunological assays requires specific reagent solutions and reference materials. The following table outlines key components used in standardization initiatives.
Table 2: Essential Research Reagent Solutions for Assay Standardization
| Reagent/Resource | Function in Standardization | Application Examples |
|---|---|---|
| Primary Reference Standards [19] | Fully characterized materials with known analyte concentrations from accredited agencies (NIST, WHO) | Serve as metrological foundation for traceability; used by companies preparing secondary reference standards |
| Secondary Reference Standards (Calibrators) [19] | Materials with assigned analyte concentrations derived from primary standards | IHC calibrators with defined molecules/cell equivalent; enable quantitative sensitivity measurements |
| International Standard Sera [21] [22] | Well-characterized antibody preparations for interlaboratory normalization | WHO reference anti-HIV-1 serum; standard sera for influenza neutralizing antibody comparisons |
| Stable Control Materials [20] | Quality control samples mimicking clinical specimens | Peripheral blood and serum samples distributed in EQA schemes; ensure representative testing conditions |
| Matched Antibody Pairs [23] [24] | Optimized antibody combinations for specific capture and detection | Sandwich ELISA kits; ensure consistent recognition of target epitopes across laboratories |
| Erythrivarone A | Erythrivarone A, MF:C20H18O5, MW:338.4 g/mol | Chemical Reagent |
| Bullatantriol | Bullatantriol, CAS:99933-32-1, MF:C15H28O3, MW:256.38 g/mol | Chemical Reagent |
Impact Assessment and Future Directions
Standardization initiatives have demonstrated measurable benefits for assay reproducibility and reliability. The incorporation of analytical standards in other clinical chemistry fields offers instructive precedents: the National Glycohemoglobin Standardization Program dramatically improved hemoglobin A1c testing, while standardization of cholesterol testing reduced error rates from 18% to less than 5%, with estimated healthcare savings exceeding $100 million annually [19].
For immunohistochemistry, the integration of calibrators and analytical standards is expected to enable three key advancements: (1) harmonization and standardization of IHC assays across laboratories; (2) improved test accuracy and reproducibility; and (3) dramatically simplified method transfer of new IHC protocols from published literature or clinical trials to diagnostic laboratories [19].
The evolving regulatory landscape, including the EU In Vitro Diagnostic Device Regulation, now requires appropriateness evaluation for laboratory-developed tests, further emphasizing the importance of standardized approaches and participation in proficiency testing schemes [20]. Future directions will likely include expanded reference material availability, harmonized reporting standards, and the integration of new technologies such as digital pathology and artificial intelligence for more objective result interpretation.
International consortia and standardization initiatives provide indispensable frameworks for ensuring the reproducibility and reliability of immunological assays across research laboratories and clinical diagnostics. Through the development of reference materials, establishment of standardized protocols, and implementation of quality assurance programs, these collaborative efforts address critical sources of variability and create the foundation for robust, comparable data generation. As biomarker discovery advances and personalized medicine evolves, the role of these standardization bodies will become increasingly vital in translating research findings into clinically actionable information that improves patient care and therapeutic outcomes.
Implementing Standardized Protocols for Common Immunoassays
Best Practices for the Dendritic Cell (DC) Maturation Assay
The dendritic cell (DC) maturation assay is a critical tool in the non-clinical immunogenicity risk assessment toolkit during drug development. It evaluates the ability of a therapeutic candidate to induce maturation of immature monocyte-derived DCs (moDCs), serving as an indicator of factors that may initiate an innate immune response and contribute to an adaptive immune response [25]. As therapeutic modalities increase in structural and functional complexity, ensuring the reproducibility and robustness of this assay across different laboratories has become paramount for meaningful data comparison and candidate selection [25] [26]. This guide outlines best practices, standardized protocols, and comparative data to achieve reliable and reproducible DC maturation assays.
Purpose and Application of the DC Maturation Assay
The primary objective of the DC maturation assay is to assess the adjuvanticity potential of biotherapeutics, which can contribute to the risk of developing anti-drug antibodies (ADA) [25]. The assay enables the ranking of different drug candidates based on their capacity to trigger DC maturation.
Key applications include:
- Candidate Screening: Comparing and ranking variants of molecules during development processes [25].
- Impact Assessment of Product Attributes: Investigating the effects of critical quality attributes (CQAs) such as protein aggregates, host cell proteins, or formulation components [25] [27].
- Mechanistic Studies: Understanding stimulatory effects mediated by target engagement, candidate payloads, or specific impurities under defined conditions [25].
It is crucial to note that the absence of observed DC maturation does not imply the absence of T-cell epitopes in the therapeutic product. Therefore, this assay should be used alongside other preclinical immunogenicity assays, such as MHC-associated peptide proteomics (MAPPs) and T-cell activation assays, to obtain a comprehensive risk assessment [25].
Core Signaling Pathways in DC Maturation
The maturation of DCs is a fundamental process linking innate and adaptive immunity. The following diagram illustrates the key signaling pathways involved in DC maturation and subsequent T-cell activation.
Figure 1: Signaling Pathway in DC Maturation and T-Cell Activation. Immature DCs (iDCs) recognize pathogenic stimuli or drug product impurities via Pattern Recognition Receptors (PRRs). This triggers a maturation process, leading to upregulated surface expression of costimulatory molecules (CD80, CD86, CD83, CD40) and HLA class II molecules. The mature DC (mDC) then activates naive CD4+ T cells by providing two essential signals: Signal 1 (TCR engagement with HLA-peptide complexes) and Signal 2 (co-stimulation via CD80/CD86 binding to CD28) [25].
Best Practices for a Reproducible Assay
Achieving inter-laboratory reproducibility requires standardization of key parameters. The European Immunogenicity Platform Non-Clinical Immunogenicity Risk Assessment working group (EIP-NCIRA) has provided recommendations to improve assay robustness and comparability [25].
Cell Source and Culture Standardization
- Cell Source: Use peripheral blood mononuclear cells (PBMCs) from healthy donors as the starting material. PBMCs should be obtained from reputable blood donation centers with appropriate ethical consent [25] [27].
- Monocyte Isolation: Isolate CD14+ monocytes from PBMCs via immunomagnetic positive selection using systems like CliniMACS or MiniMACS technology [28] [27].
- DC Differentiation and Maturation: Differentiate monocytes into immature DCs (iDCs) by culturing them for 5-6 days in the presence of GM-CSF (50 ng/mL) and IL-4 (50 ng/mL) [28] [27]. Induce maturation by adding a pro-inflammatory cytokine cocktail, typically including TNF-α, IL-1β, IL-6, and PGE2 [28].
Critical Assay Controls
Including the appropriate controls is vital for meaningful data interpretation. The table below summarizes the essential controls and their acceptance criteria.
Table 1: Essential Controls for the DC Maturation Assay
| Control Type | Purpose | Examples | Acceptance Criteria |
|---|---|---|---|
| Negative Control | Defines baseline maturation of iDCs. | Cell culture medium alone [25]. | Low expression of maturation markers (e.g., CD80, CD83, CD86). |
| Positive Control | Verifies DCs' capacity to mature. | 100 ng/mL Lipopolysaccharide (LPS) [27]. | Significant upregulation of maturation markers and cytokine production. |
| Reference Control | Provides a benchmark for comparison. | A clinically validated benchmark molecule or a known immunogenic antibody (e.g., aggregated infliximab) [25] [27]. | Consistent response profile across multiple assay runs. |
Key Readouts and Quality Control
A robust assay employs multiple readouts to comprehensively assess the maturation state.
- Phenotypic Analysis via Flow Cytometry: This is the primary readout. Measure the increased surface expression of CD80, CD83, CD86, CD40, and HLA-DR on mature DCs compared to immature DCs [25] [28] [27]. Adherence to flow cytometry standardization efforts, such as those by the Euroflow consortium, is recommended to minimize inter-laboratory variation [26].
- Cytokine Secretion Profile: Quantify the production of pro-inflammatory cytokines such as IL-1β, IL-6, IL-8, IL-12, TNF-α, CCL3, and CCL4 in the culture supernatant using techniques like cytometric bead array (CBA) or ELISA [27].
- Quality Control (QC) of Cells: Prior to assay setup, iDCs should undergo QC. Viability must be maintained above 90% to ensure functional competence [28] [29]. The immature state should be confirmed by low expression of maturation markers.
Experimental Data and Protocol Comparison
To illustrate the practical application and outcomes of the DC maturation assay, the following table summarizes experimental data generated using different therapeutic antibodies.
Table 2: Comparative DC Maturation Response to Therapeutic Antibodies and Aggregates
| Therapeutic Antibody | Humanization Status | Stress Condition | Phenotypic Changes (CD83/CD86) | Cytokine Signature | Phospho-Signaling |
|---|---|---|---|---|---|
| Infliximab | Chimeric | Heat stress (aggregates) | Marked increase | IL-1β, IL-6, IL-8, IL-12, TNF-α, CCL3, CCL4 ↑ | Syk, ERK1/2, Akt ↑ |
| Natalizumab | Humanized | Native / Stressed (non-aggregating) | No activation | No significant change | No significant change |
| Adalimumab | Fully Human | Heat stress (aggregates) | Slight variation | Slight parameter variation | Slight parameter variation |
| Rituximab | Chimeric | Heat stress (aggregates) | Slight variation | Slight parameter variation | Slight parameter variation |
Data adapted from a multi-laboratory study [27]. The results demonstrate that the propensity to activate DCs is molecule-dependent and influenced by factors like aggregation state.
Detailed Experimental Protocol
The following workflow outlines the core steps for performing a standardized DC maturation assay, integrating recommendations from multiple sources [25] [28] [27].
Figure 2: DC Maturation Assay Workflow. The process begins with the isolation and differentiation of immature DCs (iDCs), followed by a critical quality control step. iDCs are then exposed to the test articles and controls before being harvested for multiparameter analysis.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and materials required to establish a reproducible DC maturation assay.
Table 3: Essential Reagent Solutions for the DC Maturation Assay
| Reagent / Material | Function / Purpose | Examples / Notes |
|---|---|---|
| CD14+ Microbeads | Immunomagnetic isolation of monocytes from PBMCs. | Clinically graded kits (e.g., Miltenyi Biotec CliniMACS) ensure reproducibility [28]. |
| Cytokines (GM-CSF, IL-4) | Induces monocyte differentiation into immature DCs (iDCs). | Use pharmaceutical-grade cytokines and replenish on day 3 of culture [28] [27]. |
| Maturation Cocktail | Induces final maturation of antigen-loaded DCs. | Typically includes TNF-α, IL-1β, IL-6, and PGE2 [28]. |
| Flow Cytometry Antibodies | Phenotypic analysis of maturation markers. | Antibodies against CD80, CD83, CD86, CD40, and HLA-DR. Standardized panels improve cross-lab comparability [26]. |
| Cytokine Detection Kit | Quantification of secreted cytokines in supernatant. | Cytometric Bead Array (CBA) flex sets or ELISA kits for IL-1β, IL-6, IL-12, TNF-α, etc. [29] [27]. |
| Positive Control | Assay validation and system suitability. | LPS (100 ng/mL) or a known immunogenic aggregated antibody (e.g., infliximab) [27]. |
| Piribedil N-Oxide | Piribedil N-Oxide, CAS:53954-71-5, MF:C16H18N4O3, MW:314.34 g/mol | Chemical Reagent |
| 9-PAHPA | 9-PAHPA, CAS:1636134-70-7, MF:C32H62O4, MW:510.8 g/mol | Chemical Reagent |
The DC maturation assay is a powerful predictive tool for assessing the innate immunogenicity risk of biotherapeutics. Its successful implementation and the ability to compare data across different projects and laboratories hinge on the adoption of standardized best practices. This includes careful attention to cell source, culture conditions, a defined set of controls, and multiple readout parameters. By adhering to these guidelines and utilizing the essential reagent toolkit, researchers can generate robust, reproducible, and meaningful data to inform candidate selection and de-risk drug development.
Flow cytometry remains a powerful, high-throughput methodology for multiparameter single-cell analysis, but its utility in multi-center research and drug development is heavily dependent on standardized procedures. The reproducibility crisis in immunological assays stems from multiple variables, including instrument configuration, antibody reagent performance, sample preparation protocols, and data analysis approaches. Recent studies have demonstrated considerable variability in flow cytometric measurements between different laboratories analyzing identical samples, limiting the comparability of data in large-scale clinical trials [30]. This comparison guide evaluates current standardization methodologies across technological platforms, antibody panel development, and procedural workflows to provide researchers and drug development professionals with evidence-based strategies for enhancing reproducibility.
Comparative Performance of Flow Cytometry Platforms
Technology Benchmarking and Detection Limits
Different flow cytometry platforms offer varying capabilities for detection sensitivity, multiparameter analysis, and reproducibility. A 2021 benchmark study systematically compared conventional, high-resolution, and imaging flow cytometry platforms using nanospheres and extracellular vesicles (EVs) to characterize detection abilities [31].
Table 1: Performance Comparison of Flow Cytometry Platforms
| Platform Type | Lower Detection Limit | Key Technological Features | Reported Applications | Sensitivity Limitations |
|---|---|---|---|---|
| Conventional Flow Cytometry (e.g., BD FACSAria III) | 300-500 nm (best case: ~150 nm) | Standard photomultiplier tubes (PMTs), fluidics optimized for cells (2-30 µm) | Immunophenotyping, cell cycle analysis | Unable to detect abundantly present smaller EVs; swarm detection of multiple particles as single events |
| High-Resolution Flow Cytometry (e.g., Apogee A60 Micro-PLUS) | <150 nm | PMTs on scatter channels, reduced wide-angle forward scatter/medium-angle light scatter, higher power lasers, decreased flow rates | EV characterization, nanoscale particle analysis | Improved but limited for smallest biological particles |
| Imaging Flow Cytometry (e.g., ImageStream X Mk II) | ~20 nm | Charge-coupled device (CCD) cameras with larger dynamic range, time delay integration (TDI), slow sheath/sample flow rates | EV characterization, submicron particle analysis | Longer acquisition times, complex data analysis |
The study found that conventional flow cytometers have a lower detection limit between 300-500 nm, with an optimized minimal detection limit of approximately 150 nm, thereby excluding abundantly present smaller extracellular vesicles from analysis [31]. Additionally, conventional instruments suffer from "swarm detection" where multiple EVs are detected as single events due to fluidics optimized for cell-sized particles (2-30 μm) [31].
High-resolution flow cytometers incorporate modifications such as changing photodiodes to PMTs on light scatter channels, adding reduced wide-angle forward scatter collection, installing higher-power lasers, and decreasing sample and sheath flow rates [31]. These modifications enable detection limits below those of conventional flow cytometers, making them increasingly prevalent in extracellular vesicle research.
Imaging flow cytometers demonstrate significantly enhanced sensitivity, detecting synthetic nanospheres as small as 20 nm, largely due to CCD cameras with greater dynamic range and lower noise than PMTs, combined with time delay integration that allows longer signal integration times for each particle [31].
Inter-Instrument Variability in Multicenter Studies
A 2020 multicenter study investigating standardization procedures for flow cytometry data harmonization revealed significant variability across eleven instruments from different manufacturers (Navios, Gallios, Canto II, Fortessa, Verse, Aria) [30]. When analyzing the same blood control sample across all platforms, researchers found frequency variation coefficients ranging from 2.3% for neutrophils to 17.7% for monocytes, and mean fluorescence intensity (MFI) variation coefficients ranging from 10.9% for CD3 to 30.9% for CD15, despite initial harmonization procedures [30].
Table 2: Inter-Instrument Variability in Multicenter Flow Cytometry Study
| Measurement Parameter | Cell Population/Marker | Coefficient of Variation Range | Impact on Data Interpretation |
|---|---|---|---|
| Population Frequencies | Neutrophils | 2.3% | Minimal impact |
| Population Frequencies | Monocytes | 17.7% | Substantial impact for precise immunomonitoring |
| Marker Expression (MFI) | CD3 | 10.9% | Moderate impact for low-expression markers |
| Marker Expression (MFI) | CD15 | 30.9% | Substantial impact for quantitative comparisons |
The study further identified that lot-to-lot variations in reagents represented a significant source of variability, with three different antibody lots used during the 4-year study period showing marked variations in MFI when the same samples were analyzed [30].
Standardization of Antibody Panels and Reagents
Antibody Titration and Validation
Proper antibody titration is fundamental for generating reproducible flow cytometry data. Using incorrect antibody concentrations leads to either non-specific binding (with excess antibody) or weak signals (with insufficient antibody) [32]. The optimal concentration must be determined for each new antibody lot and specific cell type through systematic titration.
A recommended titration protocol involves preparing a series of antibody dilutions and staining identical control samples [32]. The optimal concentration provides the maximum signal-to-noise ratio—the brightest specific signal with the lowest background. This process ensures both scientific rigor and cost-effective reagent use [32].
For complex panels, particularly in spectral flow cytometry, careful antibody selection and staining optimization are crucial. As panel complexity increases, so does potential data variability from non-biological factors [33]. In a 30-color spectral flow cytometry panel development, researchers performed iterative refinements with careful consideration of antibody selection, staining optimization, and stability analyses to minimize non-biological variability [33].
Ad Hoc Antibody Panel Modifications
In clinical laboratories, unforeseen situations may necessitate ad hoc modifications to validated antibody panels. The 2025 guidance from the European Immunogenicity Platform recommends that such modifications should be limited—such as substituting or adding one or two antibodies—while maintaining assay integrity [34]. These modifications are intended for rare clinical situations and are not substitutes for full validation protocols.
Key considerations for ad hoc modifications include assessing impacts on fluorescence compensation, antibody binding, assay sensitivity, and overall performance [34]. Proper documentation with review and approval by laboratory medical directors is essential to mitigate risks associated with these modifications. The guidance emphasizes that these are temporary adaptations, not permanent changes to validated assays [34].
Instrument Setup and Quality Control Procedures
Daily Quality Control and Standardization
Implementing robust quality control procedures is essential for instrument stability. The PRECISESADS study developed a standardized operating procedure using 8-peak beads for daily QC to preserve intra-instrument stability throughout their 4-year project period [30]. They established targets during initial harmonization and monitored performance regularly.
Researchers developed an R script for normalization of results over the study period for each center based on initial harmonization targets to correct variations observed in daily QC [30]. This script applied normalization using linear regression with determined parameters, using MFI values of 8-peak beads obtained during initial calibration as reference. Validation experiments demonstrated that this approach could correct intentionally introduced PMT variations of 10-15%, reducing coefficients of variation to less than 5% [30].
Standardized Startup and Shutdown Procedures
Core facilities typically implement strict protocols for instrument operation to ensure consistency and maintenance. The Houston Methodist Flow Cytometry Core provides detailed SOPs for startup and shutdown procedures [35]:
Start-up Procedure:
- Check sheath level and ensure sufficient supply for the experiment
- If sheath tank needs filling, empty waste tank
- Turn on the instrument and computer
- Set up data-acquisition protocols
- Prime instrument once
- Let instrument warm up 15 minutes prior to use [35]
Shut-down Procedure:
- Run a tube with 2 mL of 10% bleach
- Move swing arm to aspirate 1 mL of bleach
- Return swing arm to center, put instrument on RUN and HIGH for 5 minutes
- Run a tube with 2 mL of distilled water
- Aspirate 1 mL of water, return arm to center
- Put instrument on STANDBY for 5 minutes for laser cooldown
- After 5 minutes, the instrument may be turned off [35]
The Yale Research Flow Cytometry Facility adds that users must empty waste tanks and add 100 mL of bleach after each use, and refill sheath fluid tanks, unless the next user has agreed to perform these tasks [36].
Sample Preparation and Experimental Protocols
Sample Processing Standardization
Proper sample preparation is foundational for reproducible flow cytometry results. Key considerations include:
Single-Cell Suspension: Creating a monodispersed, viable cell suspension is critical. Clumps of cells obstruct the flow path, cause instrument errors, and lead to inaccurate counts [32]. For solid tissues, proper mechanical and enzymatic disaggregation must balance releasing individual cells without compromising viability or altering surface antigen expression [32].
Filtration: Filtering cell suspensions through fine mesh filters (typically 40-70μm) removes cell clumps, debris, and tissue fragments, preventing clogs in the fluidic system and ensuring uniform sample stream [32]. The Yale Facility requires all samples to be filtered at the machine just before running, with specific protocols using Falcon Mesh Top tubes [36].
Viability Assessment: Dead and dying cells pose significant problems through non-specific antibody binding, creating background noise [32]. Viability dyes like propidium iodide or 7-AAD allow differentiation between live and dead cells for subsequent exclusion during analysis. Facilities often mandate fixation of potentially infectious materials before analysis on shared instruments [36].
Controlling for Background and Non-Specific Binding
Background noise from non-specific antibody binding or cellular autofluorescence can obscure true positive signals:
Blocking Reagents: Cells with Fc receptors can bind antibodies non-specifically. Blocking these receptors with FcR blocking solution before adding antibodies is crucial for accurate data [32].
Appropriate Controls: Isotype controls (antibodies with same host species, isotype, and fluorophore but specific to irrelevant antigens) help distinguish true positive staining from background [32]. Unstained samples measure autofluorescence, while fluorescence minus one (FMO) controls are critical for accurate gating in multicolor panels [35].
Data Analysis and Harmonization Approaches
Automated Analysis for Improved Reproducibility
Manual data analysis introduces significant variability in flow cytometry. The PRECISESADS study addressed this by developing supervised machine learning-based automated gating pipelines that replicated manual analysis [30]. Their approach used a two-step workflow: a first step customized for each instrument to address differences in forward and side scatter signals, and a second instrument-independent step for gating remaining populations of interest [30].
Validation comparing automated results with traditional manual analysis on 300 patients across 11 centers showed very good correlation for frequencies, absolute values, and MFIs [30]. This demonstrates that automated analysis provides consistency and reproducibility advantages, especially in large-scale, multi-center studies.
Cross-Laboratory Harmonization Protocols
Recent initiatives have focused on comprehensive harmonization strategies. The Curiox Biosystems Commercial Tutorial at CYTO 2025 highlighted advances in antibody preparation and automation for reliable immune monitoring, emphasizing CLSI H62 and NIST standards for assay validation and harmonization across laboratories [37].
Similarly, the European Immunogenicity Platform's working group on non-clinical immunogenicity risk assessment has provided comprehensive recommendations for establishing robust workflows to ensure data quality and meaningful interpretation [38]. While acknowledging the improbability of complete protocol harmonization, they propose measures and controls that support developing high-quality assays with improved reproducibility and reliability [38].
Essential Research Reagent Solutions
Table 3: Key Reagent Solutions for Standardized Flow Cytometry
| Reagent Category | Specific Examples | Function in Standardization | Implementation Considerations |
|---|---|---|---|
| Reference Standard Beads | VersaComp Capture Beads, 8-peak beads | Instrument calibration, PMT standardization, daily QC | Establish baseline MFI targets; monitor drift over time |
| Viability Dyes | Propidium iodide, 7-AAD, Ghost Dye v450 | Distinguish live/dead cells; exclude compromised cells from analysis | Titrate for optimal concentration; include in all experiments |
| Fc Receptor Blocking Reagents | Human FcR Blocking Solution | Reduce non-specific antibody binding | Pre-incubate before antibody staining; particularly important for hematopoietic cells |
| Stain Buffer | Brilliant Stain Buffer | Manage fluorophore aggregation in multicolor panels | Essential for high-parameter panels with tandem dyes |
| Alignment Beads | Commercial alignment beads (manufacturer-specific) | Laser alignment and performance verification | Regular use according to manufacturer schedule |
| Standardized Antibody Panels | DuraClone dried antibody panels | Lot-to-lot consistency, reduced pipetting errors | Provide stability over time, ease of storage |
Standardization of flow cytometry across antibody panels, instrument setup, and SOPs requires a systematic, multifaceted approach. Technological advancements in high-resolution and spectral flow cytometry have expanded detection capabilities but introduced new standardization challenges. Successful multicenter studies implement comprehensive strategies including initial instrument harmonization, daily quality control, standardized sample processing, automated analysis pipelines, and careful reagent validation. As flow cytometry continues to evolve toward higher-parameter applications in both research and clinical trials, the adoption of these standardization practices will be essential for generating reliable, comparable data across laboratories and over time. The scientific community's increasing emphasis on reproducibility, evidenced by new guidelines and standardization initiatives, promises to enhance the robustness of flow cytometric data in immunological research and drug development.
Experimental Workflow Diagrams
Standardization Workflow - This diagram illustrates the comprehensive flow cytometry standardization process from panel design through data analysis, highlighting critical control points.
Multicenter Approach - This diagram shows the key components for achieving reproducible flow cytometry results across multiple research centers.
Multiplexed Immunofluorescence (mIF) and Multi-institutional Verification
Multiplexed immunofluorescence (mIF) has emerged as a transformative technology in spatial biology, enabling the simultaneous visualization and quantification of multiple protein targets within a single formalin-fixed paraffin-embedded (FFPE) tissue section [39] [40]. By preserving critical spatial context within the tumor microenvironment (TME), mIF provides insights into cellular phenotypes, functional states, and cell-to-cell interactions that are lost in dissociated cell analyses [41]. This spatial information has proven particularly valuable in immuno-oncology, where the spatial organization of immune cells within tumors often correlates more strongly with patient response to immunotherapy than other biomarker modalities [42] [43].
Despite its powerful capabilities, the transition of mIF from a research tool to a clinically validated methodology faces significant challenges in reproducibility and standardization across institutions. The Society for Immunotherapy of Cancer (SITC) has highlighted that mIF technologies are "maturing and are routinely included in research studies and moving towards clinical use," but require standardized guidelines for image analysis and data management to ensure comparable results across laboratories [42]. This review examines current verification frameworks, compares analytical pipelines, and provides best practices for achieving robust multi-institutional mIF data.
Comparative Analysis of mIF Analysis Platforms and Their Performance
Multiple platforms and computational pipelines have been developed to address the analytical challenges of mIF data. The table below compares four prominent solutions used in multi-institutional settings.
Table 1: Comparison of mIF Analysis Platforms and Verification Performance
| Platform/Pipeline | Technology Basis | Key Verification Metrics | Multi-institutional Validation | Reference Performance Data |
|---|---|---|---|---|
| SPARTA Framework | Platform-agnostic with AI-enabled segmentation | Standardized processing across imaging systems (Lunaphore Comet, Akoya PhenoImager, Zeiss Axioscan) | Cross-platform consistency in data processing and analysis | Consistent cell segmentation and classification across platforms [41] |
| MARQO Pipeline | Open-source, user-guided automated analysis | Composite segmentation accuracy (>60% centroid detection across stains), validated against pathologist curation | Tested across multiple sites and tissue types; compatible with CIMAC-CIDC networks | 91.3% concordance with manual pathologist segmentation in HCC validation [44] |
| SITC Best Practices | Guidelines for mIHC/IF analysis | Image acquisition standards, cell segmentation verification, batch effect correction | Multi-institutional harmonization efforts across academic centers and pharmaceutical companies | Established framework for cross-site comparability; AUC >0.8 for predictive biomarkers [42] |
| ROSIE (AI-based) | Deep learning (ConvNext CNN) | Pearson R=0.285, Spearman R=0.352 for protein expression prediction from H&E | Trained on 1,300+ samples across multiple institutions and disease types | Sample-level C-index=0.706 for biomarker prediction [45] |
The performance variation across these platforms highlights both the progress and challenges in mIF verification. The SPARTA framework addresses pre-analytical and analytical variability through standardized workflows across different imaging systems [41]. MARQO demonstrates that iterative segmentation approaches leveraging multiple nuclear stains can achieve pathologist-level accuracy (>90% concordance) while enabling whole-slide analysis [44]. The SITC guidelines emphasize that proper validation must extend beyond technical performance to encompass analytical validity for specific research questions, particularly as mIF biomarkers show potential as companion diagnostics with AUCs exceeding 0.8 [42].
Experimental Protocols for Multi-institutional mIF Verification
Specimen Processing and Staining Standardization
Robust mIF verification begins with standardized specimen handling and staining protocols. The customized affordable mIF protocol demonstrates that using commercially available stripping reagents for sequential antibody staining enables comprehensive marker panels while controlling costs [39]. Critical steps include:
- Tissue Preparation: Consistent use of FFPE tissue sections cut at 5μm thickness with appropriate antigen retrieval methods tailored to specific antibody clones [39] [46].
- Antibody Validation: Each antibody must be individually optimized and validated using monoplex chromogenic IHC before multiplex panel development, testing multiple clones and concentrations to establish optimal conditions [46].
- Fluorophore Selection: Strategic assignment of fluorophores to markers based on abundance and spectral overlap, with careful balancing of signal intensities across all channels to minimize bleed-through artifacts [46].
- Autofluorescence Control: Implementation of autofluorescence quenching protocols, particularly critical for damaged tissues or those with inherent autofluorescence like brain tissue [39].
Image Acquisition and Analysis Workflows
Standardized image acquisition and analysis are fundamental to reproducible multi-institutional mIF data. The SITC task force recommends:
- Whole-Slide Imaging: Preference for whole-slide imaging over region of interest (ROI) selection to minimize sampling bias, with a minimum of five high-power fields (0.33-0.64 mm² each) when ROI selection is necessary [42].
- Spectral Unmixing: Implementation of validated spectral unmixing algorithms to properly separate fluorophore signals, with quality control metrics for separation efficiency [42] [43].
- Cell Segmentation: Use of composite segmentation approaches that leverage multiple nuclear stains where available, with consensus detection thresholds (e.g., centroid detection within 3μm across ≥60% of iterative stains) [44].
- Batch Effect Correction: Implementation of normalization protocols to address inter-institutional and batch-to-batch technical variability, including reference standards and control samples [42].
Table 2: Key Experimental Reagents and Solutions for mIF Verification
| Reagent Category | Specific Examples | Function in mIF Workflow | Verification Application |
|---|---|---|---|
| Signal Amplification | Tyramide Signal Amplification (TSA) | Enhances detection sensitivity for low-abundance targets | Standardization of detection limits across platforms [43] [46] |
| Antibody Stripping | SDS-Tris-HCl-β-mercaptoethanol solution | Enables sequential staining cycles by removing antibodies | Validation of stripping efficiency and epitope preservation [39] [47] |
| Autofluorescence Control | Commercial autofluorescence quenching reagents | Reduces tissue autofluorescence background | Standardization of signal-to-noise ratios across institutions [39] |
| Nuclear Counterstains | DAPI, hematoxylin | Enables cell segmentation and registration | Consistent segmentation performance across analysis platforms [44] [47] |
| Reference Standards | Well-characterized control tissues (tonsil, liver) | Platform performance monitoring and normalization | Inter-institutional reproducibility assessment [42] [43] |
Visualization of mIF Verification Workflows
The diagram below illustrates the critical pathway for establishing verified multi-institutional mIF data, from experimental design through cross-site validation.
Multi-institutional mIF Verification Pathway
The verification pathway emphasizes the staged approach necessary for robust mIF implementation, beginning with rigorous single-site validation before progressing to multi-institutional assessment.
Analytical Framework for Cross-Platform mIF Data
Image Analysis and Data Management Standards
The computational pipeline for mIF data requires standardized approaches to ensure reproducible results. The SITC guidelines emphasize several critical components:
- Color Deconvolution/Spectral Unmixing: Separation of overlapping signals through validated algorithms that accurately assign marker expression to specific cellular compartments [42].
- Cell Segmentation: Nuclear segmentation using consensus methods, with MARQO demonstrating that composite segmentation across multiple iterative stains improves accuracy compared to single-stain approaches [44].
- Phenotyping Algorithms: Transparent rules for cell type identification, with preference for unsupervised clustering followed by expert-guided annotation to maintain biological relevance [44].
- Spatial Analysis: Standardized metrics for cell-cell proximity, neighborhood analysis, and compartment identification that can be replicated across institutions [42] [43].
Emerging Technologies and Future Directions
Artificial intelligence approaches are creating new pathways for mIF verification and accessibility. ROSIE demonstrates that deep learning can predict protein expression patterns from H&E images alone, providing a potential bridge for comparing mIF data with historical samples [45]. Similarly, mSIGHT uses generative adversarial networks to create virtual mIF from H&E stains, showing significant associations between predicted CD8+ T-cell density and treatment response in breast cancer [47]. While these computational approaches do not replace physical mIF assays, they offer promising methods for augmenting verification efforts and expanding the scope of multi-institutional comparisons.
The successful implementation of multiplexed immunofluorescence across multiple institutions requires a comprehensive approach to verification that addresses pre-analytical, analytical, and post-analytical variables. Frameworks like SPARTA and MARQO demonstrate that platform-agnostic analysis pipelines and robust segmentation algorithms can achieve greater than 90% concordance with pathologist interpretation [41] [44]. The SITC guidelines provide a critical foundation for standardizing image analysis and data management practices across sites [42]. As the field progresses toward clinical application, continued emphasis on reference materials, inter-laboratory comparison studies, and transparent reporting will be essential for establishing mIF as a reproducible and reliable technology for translational research and diagnostic applications.
Peripheral Blood Mononuclear Cells (PBMCs) are foundational to immunology, oncology, and cell therapy research, serving as critical starting materials for functional assays, vaccine development, and discovery-stage therapeutic studies [48]. The quality of PBMCs, dictated by their source, isolation, and handling, directly impacts data accuracy and reproducibility in immunological assays across laboratories [48] [49]. This guide objectively compares key products and methodologies, providing supporting experimental data to inform researchers, scientists, and drug development professionals.
PBMC Suppliers and Source Quality
The choice of supplier is a critical pre-analytical variable, influencing the consistency of starting material for multi-center studies. Suppliers differ in product type, quality, and logistical support [48].
Table 1: Comparison of Key PBMC Suppliers for 2026
| Supplier | PBMC Type | Grade | Average Viability | Fresh Lead Time | Regions Served | Key Strengths |
|---|---|---|---|---|---|---|
| CGT Global | Fresh & Cryopreserved | Research-use-only | ≥95% fresh / ≥90% cryo | 24-48 hours | US Nationwide | Fast turnaround, live chat support [48] |
| AllCells | Cryopreserved | Research | ≥90% | 3-5 days | US & EU | Scalable inventory, batch consistency [48] |
| Discovery Life Sciences | Cryopreserved | Research | ≥92% | 3-5 days | Global | Data-rich donor profiles, international reach [48] |
| BioIVT | Cryopreserved | Research | ≥90% | 3-5 days | US & EU | Reliable for translational research [48] |
| STEMCELL Technologies | Cryopreserved | RUO | ≥90% | 3-5 days | Global | Optimized for proprietary assay workflows [48] |
Standardizing donor quality is essential for reducing variability. Verified donor programs with documented health screening, collection parameters, and traceable metrics help ensure consistency in cell recovery and performance from the outset [50].
PBMC Isolation Techniques
The method chosen for isolating PBMCs from whole blood or leukapheresis product can significantly impact cell yield, purity, and, most importantly, functionality [51].
Table 2: Comparison of PBMC Isolation Techniques
| Method | Principle | Advantages | Disadvantages | Impact on Reproducibility |
|---|---|---|---|---|
| Density Gradient Centrifugation | Separation based on cell density using media like Ficoll-Paque [51]. | Simple, cost-effective, processes large volumes [51]. | Requires skill; risk of cell activation or damage; sensitive to temperature and sample age [51] [50]. | High operator dependency can lead to inter-lab variability in purity and viability. |
| Magnetic-Activated Cell Sorting (MACS) | Uses antibody-coated magnetic beads to target specific cell types [51]. | High specificity and purity for cell subsets [51]. | Expensive; beads may interfere with cell surface receptors [51]. | Standardized kits improve reproducibility, but bead binding may affect downstream functional assays. |
| Fluorescence-Activated Cell Sorting (FACS) | Sorts cells based on fluorescent antibody labeling and light scattering [51]. | Highest specificity and multi-parameter sorting [51]. | Very expensive, technically demanding, slow, and can induce cell stress [51]. | Yields highly pure populations, but stress from sorting may inconsistently impact cell function. |
| Microbubble Technology (Akadeum) | Gentle buoyancy-based separation floats unwanted cells for removal [51]. | Gentle, high viability, simple, scalable, and "untouched" target cells [51]. | Relatively new technology; may not be as widely validated [51]. | Simplicity and gentleness may reduce a key variable in cell functionality, enhancing cross-lab consistency. |
Experimental Workflow for PBMC Processing
The following diagram outlines a generalized workflow for processing blood into isolated and cryopreserved PBMCs, highlighting key steps where variability can be introduced.
Cryopreservation Protocols and Media Comparison
Cryopreservation is crucial for long-term storage and batch analysis in clinical trials, but it exposes cells to extreme conditions [52]. The choice of freezing medium and protocol is vital for preserving viability and function.
Experimental Protocol for Long-Term Storage Assessment
A comprehensive study evaluated the viability and functionality of PBMCs cryopreserved in various animal-protein-free media compared to a traditional FBS-supplemented medium over two years [52].
- Sample Collection & Processing: PBMCs were isolated from 11 healthy volunteers using a lymphocyte density gradient medium (Lymphoprep) and washed in Hanks' Balanced Salt Solution buffer [52].
- Freezing Media Tested: The reference medium was FBS10 (90% FBS + 10% DMSO). Tested alternatives included the CryoStor family (CS2, CS5, CS7.5, CS10), NutriFreez D10, SF-CFM D10, Bambanker D10 (all with 10% DMSO), and DMSO-free media Stem-Cellbanker D0 and Bambanker D0 [52].
- Freezing Protocol: Cell aliquots were dispensed into cryovials, transferred to CoolCell containers, and placed into a -80°C freezer for 1–7 days before transfer to vapor-phase liquid nitrogen storage [52].
- Assessment Time Points: Cells were evaluated at 3 weeks (M0), 3 months (M3), 6 months (M6), 1 year (M12), and 2 years (M24) post-freezing. Assessments included viability, yield, phenotype, and functionality (e.g., cytokine secretion, T and B cell FluoroSpot) [52].
Comparative Data on Cryopreservation Media
Table 3: Viability and Functionality of PBMCs in Different Freezing Media Over 2 Years
| Freezing Medium | DMSO Concentration | Key Findings (Over 2 Years) | Conclusion for Reproducibility |
|---|---|---|---|
| FBS10 (Reference) | 10% | Maintained high viability and functionality across all timepoints [52]. | Robust but has ethical, batch variability, and pathogen transmission risks [52]. |
| CryoStor CS10 | 10% | Maintained high viability and functionality, comparable to FBS10 [52]. | A robust, serum-free alternative, eliminating FBS-related variability. |
| NutriFreez D10 | 10% | Maintained high viability and functionality, comparable to FBS10 [52]. | A robust, serum-free alternative, eliminating FBS-related variability. |
| Bambanker D10 | 10% | Comparable viability but tended to diverge in T cell functionality vs. FBS10 [52]. | May introduce functional variability in T-cell assays. |
| Media with <7.5% DMSO | 2%-5% | Showed significant viability loss and were eliminated after initial assessment [52]. | Not suitable for long-term storage; high risk of inconsistent cell yield. |
The Impact of Cryopreservation on Transcriptomic Profiles
Beyond viability and simple functionality, advanced studies using single-cell RNA sequencing (scRNA-seq) have investigated the effects of cryopreservation on the transcriptome profile of PBMC subsets.
- Experimental Protocol: PBMCs from healthy donors were cryopreserved using an optimized procedure with Recovery cell Culture Freezing Medium and a controlled-rate freezer. Cells were stored in liquid nitrogen for 6 and 12 months, then compared to fresh cells via scRNA-seq [53].
- Key Findings:
- Cell Population: Six major immune cell types (monocytes, dendritic cells, NK cells, CD4+ T cells, CD8+ T cells, and B cells) were identified in both fresh and cryopreserved samples, with relatively stable viability and population composition over 12 months [53].
- Transcriptome Profile: The transcriptome profiles of cryopreserved samples did not show substantial perturbation. However, a few key genes involved in the AP-1 complex, stress response, or response to calcium ions exhibited significant change, albeit at a very small scale (< two folds) [53].
- Technical Note: A reduction in scRNA-seq cell capture efficiency was observed after 12 months of cryopreservation [53].
Key Cellular Pathways Affected by Cryopreservation
The following diagram summarizes the primary stress pathways in cells that can be subtly altered during the freeze-thaw process, based on transcriptomic findings.
Quality Control and Best Practices
Consistent quality control (QC) is the cornerstone of reproducible PBMC-based research across laboratories. Key parameters must be checked post-isolation and post-thaw.
Table 4: Essential Research Reagent Solutions for PBMC Workflows
| Reagent / Solution | Function in PBMC Workflow | Key Considerations for Reproducibility |
|---|---|---|
| Anticoagulants (e.g., EDTA, Heparin) | Prevents blood clotting during and after collection [50]. | Type of anticoagulant can affect downstream assays; must be consistent across sites. |
| Density Gradient Medium (e.g., Ficoll-Paque) | Separates PBMCs from other blood components based on density [51] [54]. | Must be at room temperature for optimal separation; brand and batch should be standardized [50]. |
| Cryoprotectant (DMSO) | Prevents intracellular ice crystal formation during freezing [50] [55]. | Cytotoxic at room temperature; standardize exposure time (work quickly) and concentration (≥7.5%) [50] [52]. |
| Serum (FBS) or Serum-Free Media | Base component of freezing media; provides nutrients and stability. | FBS has batch-to-batch variability and ethical concerns. Serum-free alternatives (e.g., CryoStor CS10) provide more consistency [52]. |
| Viability Stain (Trypan Blue) | Distinguishes live (unstained) from dead (blue) cells for counting [54]. | Standardized counting methods (manual or automated) are needed to ensure consistent viability calculations between labs. |
Standardized Thawing and Recovery Protocol
A poorly executed thaw can undo the benefits of optimal cryopreservation. An optimized and standardized protocol is critical [53].
- Thawing: Remove vial from storage and thaw quickly in a 37°C water bath until only a small ice crystal remains [53].
- Dilution: Gently transfer the cell suspension to a tube containing 10 mL of pre-warmed complete medium (e.g., RPMI-1640 with 10% FBS) [53].
- Washing: Centrifuge at 500 x g for 5 minutes at room temperature to remove the DMSO-containing supernatant [53].
- Resuspension: Gently break the pellet and resuspend in fresh, warmed complete medium. A second wash is often recommended [53].
- Resting: For functional assays, allowing PBMCs to "rest" for several hours or overnight in culture medium before stimulation can improve responsiveness and reduce assay variability.
Achieving reproducibility in immunological assays across different laboratories hinges on rigorous standardization of PBMC source and handling. Key takeaways for researchers and drug development professionals include:
- Source Control: Utilize suppliers with verified donor programs and comprehensive CoAs to minimize pre-analytical variability [48] [50].
- Technique Selection: Choose isolation methods that balance yield, purity, and preservation of functionality for your specific application, noting that gentler methods may enhance cross-lab consistency [51].
- Protocol Standardization: Adopt controlled-rate freezing and standardized thawing protocols to maintain cell integrity. Serum-free, 10% DMSO media like CryoStor CS10 and NutriFreez D10 are viable, consistent alternatives to FBS-based media for long-term storage [52] [55].
- Quality Tracking: Implement rigorous QC at every stage, monitoring viability, recovery, and cell composition. Acknowledging subtle transcriptomic changes post-thaw can inform the interpretation of sophisticated assays [53] [49].
By systematically addressing these variables in PBMC isolation, cryopreservation, and quality control, the research community can significantly improve the reliability and comparability of data in both basic research and clinical trials.
Strategies for Overcoming Technical Pitfalls and Enhancing Assay Robustness
In biomedical research and drug development, establishing robust minimum cell fitness criteria is fundamental for ensuring the reliability and reproducibility of experimental data. This is particularly critical in immunology, where cellular function directly influences study outcomes. Assessing cell fitness requires a multifaceted approach, focusing on three fundamental pillars: viability (the proportion of living cells), apoptosis (the rate of programmed cell death), and metabolic activity (a measure of cellular health and function). The challenge for researchers lies not only in accurately measuring these parameters but also in understanding how assay selection influences results, especially across different laboratory settings. This guide provides an objective comparison of current methodologies and technologies, supported by experimental data, to help establish standardized, reproducible criteria for evaluating cell fitness in immunological research.
Comparative Analysis of Cell Viability Assays
Cell viability is a primary and critical quality attribute measured throughout the manufacturing process of cellular products, from starting materials to final product release [56]. Selecting an appropriate assay is complicated by product complexity, sample quantity limitations, and the need for rapid results.
Key Viability Assay Technologies
A 2023 study systematically compared the accuracy and precision of four commonly used viability assays on fresh and cryopreserved cellular therapy products, including peripheral blood stem cell (PBSC) apheresis samples, purified PBMCs, and cultured engineered T-cell products [56]. The results provide a quantitative basis for selection.
Table 1: Comparison of Common Cell Viability Assay Performance
| Assay Method | Principle | Key Advantages | Key Limitations | Reported Viability (%) (Fresh / Cryopreserved) | Reproducibility (Precision Assessment) |
|---|---|---|---|---|---|
| Manual Trypan Blue (TB) | Dye exclusion via membrane integrity [56] | Simple, cost-effective, versatile [56] | Subjectivity, small event count, no audit trail [56] | ~95% / ~85% (Variable among assays) [56] | Accurate and reproducible for fresh products [56] |
| Flow Cytometry (7-AAD/PI) | Nucleic acid staining in membrane-compromised cells [56] | Objective, high-throughput, multi-parameter analysis [56] | Requires expensive instrumentation [56] | ~95% / ~85% (Variable among assays) [56] | Accurate and reproducible for fresh products [56] |
| Image-based (Cellometer AO/PI) | Fluorescent staining of live (AO, green) and dead (PI, red) cells [56] | Automated, rapid, provides cell images [56] | Platform-specific reagent costs | ~95% / ~85% (Variable among assays) [56] | Accurate and reproducible for fresh products [56] |
| Vi-Cell BLU Analyzer | Automated trypan blue exclusion [56] | Standardizes TB method, reduces operator bias [56] | Based on traditional TB principle | ~95% / ~85% (Variable among assays) [56] | Accurate and reproducible for fresh products [56] |
Experimental Protocol: Viability Assay Comparison
The comparative study followed a standardized protocol to ensure a fair evaluation [56]:
- Specimens: Eighteen fresh and twenty-six cryopreserved cellular products (PBSC apheresis, purified PBMCs, cultured CAR/TCR-T cells).
- Sample Processing: All samples were processed within 1.5 hours, with measurements performed in triplicate by a single operator.
- Viability Standard: A pre-mixed live/dead cell standard was used to assess the accuracy of each method.
- Analysis: For flow cytometry, viable cells were gated as the 7-AAD/PI-negative population. For manual TB and Vi-Cell BLU, viability was calculated as (number of viable cells / total cells) × 100.
Critical Findings on Viability Assessment
The study concluded that while all methods provided accurate and reproducible data for fresh cellular products, cryopreserved products exhibited significant variability among the tested assays [56]. This highlights that viability assay performance is highly dependent on sample history. Furthermore, when analyzing specific immune cell subsets within cryopreserved PBSC products, T cells and granulocytes were found to be more susceptible to the freeze-thaw process, showing decreased viability compared to other cell types [56]. This underscores the need for a "fit-for-purpose" assay selection, especially for complex, heterogeneous immune cell products.
Viability Assay Comparison Workflow
Apoptosis Assay Market and Technologies
Apoptosis assays detect and quantify programmed cell death, a process fundamental to both immune system function and the pathogenesis of many diseases. The global apoptosis assay market, valued at USD 6.5 billion in 2024 and projected to reach USD 14.6 billion by 2034, reflects their critical importance [57].
Market Drivers and Key Players
The high prevalence of chronic diseases is a primary driver of market growth. Dysregulated apoptosis is implicated in cancer, neurodegenerative diseases, and autoimmune disorders, making these assays vital for understanding disease progression and developing therapies [58]. The market is led by established players with distinct competitive strategies:
- Thermo Fisher Scientific holds a leading 28.5% market share, maintained through a comprehensive, vertically integrated portfolio that offers end-to-end solutions from reagents to flow cytometry systems and cloud-based data analysis tools [57].
- Danaher leverages a diversified platform approach through its subsidiaries, offering integrated solutions that combine imaging, flow cytometry, and assay technologies, with a focus on innovation and automation [57].
- Merck KGaA capitalizes on an expansive library of validated apoptosis reagents and assay kits, emphasizing assay reproducibility and scientific rigor for both academic and commercial research [57].
Apoptosis Assay Segmentation and Trends
Table 2: Apoptosis Assay Market Analysis by Segment and Application
| Segment | Dominant Category & Market Share | Key Trends and Growth Projections | Representative Technologies |
|---|---|---|---|
| By Product Type | Consumables (Kits, Reagents) - Largest share in 2024 [57] [58] | Fastest growth (CAGR 8.9%, to USD 8.2B by 2034); driven by demand for high-performance, scalable reagents [57] | Annexin V conjugates (e.g., Bio-Rad's StarBright Dyes), caspase substrates, TUNEL assay reagents [57] [58] |
| By Application | Drug Discovery & Development - Largest share in 2024 [58] | Used for target validation, lead compound screening, mechanism of action studies, and safety assessment [58] | High-content screening platforms, multiplexed flow cytometry panels |
| By Technology | Flow Cytometry - Market size USD 4.9B in 2022 [57] | Evolving towards high-throughput, multi-color immunophenotyping and integration with AI-powered automated gating [57] [58] | Integrated flow cytometers with automated sample handling |
A major trend is the development of automated solutions to improve efficiency, reliability, and scalability. For instance, Nanolive's LIVE Cell Death Assay offers an automated, label-free approach for cytotoxicity analysis [58]. Furthermore, advancements in detection reagents, such as Bio-Rad's 2024 launch of Annexin V conjugated to eight new StarBright Dyes, provide researchers with more options for sensitive, multiplexed apoptosis detection via flow cytometry [58].
Assessing Metabolic Activity for Cell Fitness
Metabolic activity is a crucial, functional indicator of cell fitness that often provides earlier and more sensitive detection of stress or pathology than simple viability measures.
Experimental Protocol: Breath Alcohol Analysis for CYP2E1 Metabolic Activity
A 2025 study established a non-invasive method to assess cytochrome P450 2E1 (CYP2E1) metabolic activity in a rat model of immune-mediated liver injury, demonstrating its sensitivity as a fitness biomarker [59].
- Principle: The rate of alcohol metabolism reflects CYP2E1 metabolic activity, particularly at blood alcohol concentrations >15-20 mg% where the CYP2E1 pathway dominates [59].
- Method Validation: The breath alcohol analysis method was rigorously validated for:
- Reproducibility: Nine repeated measurements of a standard alcohol solution showed a high coefficient of variation.
- Linearity: A strong concentration-response curve was established across dilutions.
- Experimental Procedure:
- Rats were administered 5 mL/kg of 56% (v/v) alcohol via gavage.
- The animal was placed in a gas collection bottle, and after 10 minutes, exhaled air was collected using a 550 mL syringe.
- Alcohol concentration was measured with a breath alcohol analyzer, which automatically converted the value to blood alcohol concentration.
- Measurements were taken every 20 minutes until concentration reached zero to plot a concentration-time curve.
- Pharmacokinetic parameters (AUC, MRT, CLz/F) were calculated using DAS 3.0 software.
Key Findings on Metabolic Activity Dynamics
The study revealed that in a BCG-induced immune liver injury model, CYP2E1 metabolic activity was most severely impaired on day 6 post-stimulation and showed a gradual recovery at days 10 and 14 [59]. Crucially, alterations in metabolic activity were detected earlier and were more pronounced than changes in CYP2E1 protein expression, highlighting metabolic readouts as a leading indicator of cellular dysfunction. These dynamic changes paralleled activation of the hepatic NF-κB inflammatory and MAPK oxidative stress pathways [59].
Metabolic Activity Assessment Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the right reagents and tools is fundamental to obtaining reliable data in cell fitness studies. The following table details essential solutions based on the cited research and market analysis.
Table 3: Essential Research Reagent Solutions for Cell Fitness Assays
| Product Category | Key Function | Example Products & Vendors | Application Notes |
|---|---|---|---|
| Viability Assay Kits | Distinguish live/dead cells based on membrane integrity. | Manual TB (Lonza); 7-AAD/PI staining kits (BD Biosciences, ThermoFisher); AO/PI kits (Cellometer) [56] | For heterogeneous immune cell samples, flow-based kits allow simultaneous phenotyping and viability assessment [56]. |
| Apoptosis Assay Kits | Detect key apoptotic events: phosphatidylserine exposure, caspase activation, DNA fragmentation. | Annexin V conjugates (Bio-Rad StarBright Dyes); caspase activity kits (Merck, Thermo Fisher) [57] [58] | Multiplexing Annexin V with cell surface markers enables apoptosis analysis in specific immune cell subsets. |
| Metabolic Assay Reagents | Measure metabolic pathway activity and mitochondrial function. | CYP2E1 substrates (e.g., chlorzoxazone); metabolic dyes (e.g., MTT, AlamarBlue); breath alcohol analyzers [59] | Functional metabolic assays can detect cellular stress earlier than viability or protein expression assays [59]. |
| Cell Culture Consumables | Provide optimized environment for maintaining cell fitness in vitro. | Specialized culture media (Thermo Fisher, Bio-Rad); culture vessels [60] [61] | Media formulation (e.g., energy substrates, amino acids) critically influences basal metabolic activity and health [61]. |
| Validated Antibody Panels | Enable immunophenotyping and analysis of cell population-specific fitness. | Fluorochrome-labeled antibodies for immune cell markers (CD3, CD14, CD16, CD19, CD45, CD56, etc.) from BD, BioLegend [56] | Essential for assessing fitness in specific immune cell subsets from complex samples like PBMCs or apheresis products [56]. |
| Hispidanin B | Hispidanin B, MF:C42H56O6, MW:656.9 g/mol | Chemical Reagent | Bench Chemicals |
| Darotropium bromide | Darotropium bromide, CAS:850607-58-8, MF:C24H29BrN2, MW:425.4 g/mol | Chemical Reagent | Bench Chemicals |
Establishing minimum cell fitness criteria requires a multi-parametric approach that rigorously assesses viability, apoptosis, and metabolic activity. Experimental data confirms that assay choice significantly impacts results, particularly for sensitive or cryopreserved immune cell samples [56]. While viability provides a basic fitness snapshot, apoptosis assays reveal dynamic cell death pathways, and metabolic activity serves as a sensitive, early indicator of functional decline [59] [58]. The growing integration of automation, multiplexing, and AI-driven data analysis in these platforms is enhancing throughput and reproducibility [57]. For researchers, a "fit-for-purpose" strategy that aligns assay selection with sample type, specific immune cell populations of interest, and the intended use of the data is paramount. By adopting a standardized, multi-faceted framework for defining cell fitness, the scientific community can significantly improve the consistency and reliability of immunological data across laboratories.
In the landscape of immunological assays, antibody validation and lot-to-lot variability represent a fundamental challenge to experimental reproducibility and reliable drug development. Inconsistent reagent performance across laboratories undermines research integrity, with studies indicating that poor antibody specificity contributes significantly to the reproducibility crisis in biomedical science [62]. For researchers and drug development professionals, implementing robust qualification processes is not merely optional but essential for generating trustworthy data.
This guide examines the core issues surrounding critical reagent qualification, providing standardized experimental protocols, comparative performance data, and practical mitigation strategies to enhance reproducibility across laboratories. We focus specifically on immunological assays, where the complex nature of antibody-antigen interactions makes them particularly vulnerable to lot-to-lot variance (LTLV) [63].
Root Causes of Lot-to-Lot Variation
Lot-to-lot variation arises from multiple sources throughout the reagent lifecycle. Understanding these sources is the first step toward effective management:
Raw Material Fluctuations: Approximately 70% of an immunoassay's performance is determined by raw material quality [63]. Biological components like antibodies sourced from hybridomas exhibit inherent variability that is difficult to regulate. Key issues include aggregation, fragmentation, and unpaired antibody chains that can lead to high background noise, signal leap, and inaccurate analyte concentration measurements [63].
Manufacturing Process Deviations: The remaining 30% of performance is attributed to production processes, including buffer recipes and reagent formulation [63]. Even slight alterations in the binding of antibodies to solid phases during manufacturing can create detectable differences between lots.
Epitope Instability and Recognition: Antibodies generated against synthetic peptides may not recognize native protein conformations, while those generated against purified proteins may fail to detect denatured targets [62]. This becomes particularly problematic in fixed tissue samples where epitope accessibility may change.
Clinical and Research Consequences
Undetected lot-to-lot variation has direct consequences on experimental and clinical outcomes:
Inconsistent Patient Results: Documented cases include HbA1c reagent lot changes causing 0.5% average increases in patient results, potentially leading to incorrect diabetes diagnoses [64].
Cumulative Analytical Drift: Studies monitoring insulin-like growth factor 1 (IGF-1) over several years revealed progressive increases in reported values despite acceptable individual lot-to-lot comparisons, demonstrating how small, acceptable shifts can accumulate into clinically significant drifts [65].
Compromised Research Findings: Non-reproducible antibodies have been shown to produce staining patterns with no correlation (R² = 0.038) between different lots of the same antibody clone, fundamentally undermining research validity [62].
Experimental Protocols for Assessment
Establishing Acceptance Criteria
Before evaluating new reagent lots, establish acceptance criteria based on clinical requirements, biological variation, or professional recommendations rather than arbitrary percentages [64]. For tests with single, well-defined applications (e.g., BNP), this is relatively straightforward, while multiplex tests require more complex consideration [65].
Performance specifications should follow updated Milan criteria for defining analytical performance instead of historical arbitrary percentages [64]. These criteria ensure that lot acceptance aligns with the intended use of the assay.
CLSI-Based Evaluation Protocol
The Clinical and Laboratory Standards Institute (CLSI) provides a standardized protocol for reagent lot evaluation [64]. The general workflow encompasses sample selection, testing, and statistical analysis to determine lot acceptability:
Key protocol steps:
Sample Selection: Use 10-20 native patient samples spanning the analytical measurement range, with emphasis on medical decision limits. Avoid relying solely on quality control materials due to commutability issues [64].
Testing Procedure: Analyze all samples with both current and new reagent lots using the same instrument, operator, and testing conditions to minimize extraneous variables.
Statistical Analysis: Compare paired results using appropriate statistical methods with sufficient power to detect clinically significant differences.
Modified Risk-Based Approach
For resource-constrained environments, a categorized approach developed by Martindale et al. offers a practical alternative [65]:
Table 1: Risk-Based Reagent Evaluation Categories
| Category | Description | Examples | Evaluation Protocol |
|---|---|---|---|
| Group 1 | Unstable analytes or laborious tests | ACTH, fecal fats, tissue copper | Initial QC measurement only (4 measurements/level) |
| Group 2 | Minimal historical lot variation | General chemistry tests | Patient comparison only if QC rules violated |
| Group 3 | History of significant variation | hCG, troponin, IGF-1 | Mandatory 10-patient sample comparison |
Comparative Performance Data
Documented Lot-to-Lot Variance Across Assays
Empirical studies reveal substantial variation across different immunoassay types. Research analyzing five common immunoassay items demonstrated considerable differences between reagent lots [66]:
Table 2: Observed Lot-to-Lot Variation in Immunoassays
| Analyte | % Difference Range | Maximum D:SD Ratio | Clinical Context |
|---|---|---|---|
| AFP | 0.1% to 17.5% | 4.37 | Cancer monitoring |
| Ferritin | 1.0% to 18.6% | 4.39 | Iron status assessment |
| CA19-9 | 0.6% to 14.3% | 2.43 | Pancreatic cancer marker |
| HBsAg | 0.6% to 16.2% | 1.64 | Hepatitis B diagnosis |
| anti-HBs | 0.1% to 17.7% | 4.16 | Immunity verification |
The difference-to-standard deviation ratio (D:SD ratio) represents the degree of difference between lots compared to daily measurement variation, with higher values indicating more significant lot changes [66].
Reproducibility Assessment in ELISA Platforms
Recent studies evaluating anti-HPV16 L1 immunoglobulin detection demonstrate the variable reproducibility across different isotypes [16]:
Table 3: ELISA Reproducibility Across Antibody Isotypes
| Isotype | Inter-Technician CV | Inter-Day CV | Overall CV | Detectability |
|---|---|---|---|---|
| IgG1 | 12.8% | 6.2% | 7.7% | >86.3% |
| IgG3 | 13.5% | 7.9% | 8.4% | 100% |
| IgA | 14.2% | 8.1% | 9.3% | >86.3% |
| IgM | 22.7% | 30.6% | 31.1% | 62.1% |
Coefficient of variation (CV) data demonstrates that IgM detection shows substantially higher variability compared to IgG subclasses and IgA, highlighting the importance of considering analyte-specific characteristics when establishing acceptance criteria [16].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Antibody Validation Studies
| Reagent/Solution | Function | Key Specifications |
|---|---|---|
| Native Patient Samples | Gold standard for comparison | Cover medical decision points and reportable range |
| SEC-HPLC | Assess antibody purity and aggregation | Purity >95%, minimal aggregates |
| CE-SDS | Detect impurity proteins and fragments | <5% impurity for consistent performance |
| Commutable QC Materials | Monitor long-term performance | Demonstrate correlation with patient samples |
| Stable Reference Standards | Calibrate across lots | Lyophilized for improved stability |
Advanced Monitoring and Mitigation Strategies
Moving Average Monitoring
Traditional lot-to-lot comparison protocols frequently fail to detect cumulative shifts in patient results over time [64]. Implementing moving average (MA) monitoring provides real-time detection of systematic errors:
This statistical process control method calculates a running average of patient results, updating with each new value while dropping the oldest. Significant deviations from the established historical average trigger investigations, potentially identifying problematic reagent lots that passed initial validation [65].
Vendor Selection and Quality Assessment
Choosing reputable antibody providers significantly impacts lot consistency. Market analyses indicate researchers increasingly prioritize vendor trust, validation rigor, and product transparency [67]. Key considerations include:
Recombinant Antibody Technologies: Demonstrate superior batch-to-batch consistency compared to hybridoma-derived monoclonal antibodies [63].
Comprehensive Validation Data: Prioritize vendors providing extensive application-specific validation rather than basic functionality data [68].
Shared Quality Metrics: Emerging platforms enable data-sharing between laboratories and manufacturers, creating collective intelligence for detecting problematic lots [64].
Managing critical reagent qualification requires a systematic, multifaceted approach combining rigorous initial validation with ongoing monitoring. The experimental protocols and comparative data presented here provide researchers and drug development professionals with evidence-based strategies to enhance reproducibility across laboratories.
By implementing structured evaluation protocols, establishing clinically relevant acceptance criteria, and employing advanced monitoring techniques, laboratories can significantly reduce the impact of lot-to-lot variation on research and diagnostic outcomes. The resulting improvement in assay reproducibility strengthens research validity and ultimately accelerates reliable drug development.
Immunological assays are fundamental tools for evaluating immune responses in research and drug development. However, their utility in multi-center studies and their ability to generate reproducible data depend critically on the stringent standardization of key parameters, chief among them being incubation times and reagent concentrations. Inconsistencies in these parameters represent a significant source of technical variability that can obscure biological signals and compromise the comparability of data across different laboratories [10] [69]. A foundational study investigating immunological tests for multiple chemical sensitivity syndrome highlighted that while intralaboratory reproducibility can be excellent, statistically significant interlaboratory differences are common, often linked to variations in analytical methods and timing [10] [69]. This guide objectively compares the performance of different assay configurations by examining experimental data, with the goal of providing a framework for optimizing critical parameters to enhance the reliability of immunological data.
Comparative Analysis of Assay Performance: The Impact of Incubation Conditions
The choice of incubation conditions—specifically time and temperature—directly influences the binding efficiency between antibodies and antigens, thereby affecting the assay's sensitivity, dynamic range, and background signal. The following data, consolidated from rigorous comparative studies, illustrates how these parameters impact various assay platforms.
Table 1: Impact of Incubation Conditions on Multiplex Bead-Based Serological Assays
| Assay Type | Incubation Condition | Key Performance Findings | Experimental Context |
|---|---|---|---|
| P. falciparum Antibody Multiplex (qSAT) [70] | 4°C overnight | Highest magnitude for IgG & IgG1-4 responses No increase in unspecific binding (vs 37°C) | IgG, IgG1–4, IgM, IgE against 40 P. falciparum antigens |
| 37°C for 2 hours | Lower specific signal for most Ig types | Customized positive control pools & WHO reference reagent | |
| Room Temp for 1 hour | Inferior performance compared to 4°C overnight | ||
| Multiplex Bead Assays (Cytokines) [71] | Standardized per mfr. | Significant variation in standard curves across labs and kit lots Use of common reference standards enabled cross-comparison | 17 cytokines/chemokines; kits from 4 manufacturers tested in 3 labs |
| T-Cell Activation Marker Flow Cytometry [10] | Lab-specific protocols | Excellent intra-lab reproducibility (≤3% difference) Significant inter-lab differences for CD25, CD26, CD38, HLA-DR | T-cell surface markers in MCS, healthy, and autoimmune cohorts |
The data from the P. falciparum study demonstrates that a longer, colder incubation (4°C overnight) provides an optimal equilibrium for antibody-antigen binding, maximizing the specific signal without increasing background noise [70]. In contrast, the cross-laboratory evaluation of cytokine bead assays reveals that even when following manufacturer protocols, inherent kit-to-kit and lab-to-lab variations exist. This underscores the necessity of including common reference standards to calibrate results and allow for meaningful comparisons between different studies and laboratories [71].
Detailed Experimental Protocols for Parameter Optimization
To ensure reproducibility, it is critical to document and adhere to detailed methodologies. Below are condensed protocols from the cited studies that directly investigate the optimization of incubation and other key parameters.
This protocol systematically tests how incubation time and temperature affect the measurement of multiple antibody isotypes and subclasses.
- 1. Plate Preparation: Couple carboxylated magnetic microspheres (e.g., MagPlex) with purified antigens of interest using standard carbodiimide chemistry (e.g., Sulfo-NHS and EDC). Block beads with PBS containing 1% BSA.
- 2. Assay Setup:
- Use a standardized positive control pool (e.g., the WHO reference reagent 10/198 for malaria, potentially enriched for specific antigens if necessary).
- Include a negative control (e.g., naive serum or sample diluent).
- 3. Experimental Incubation: Aliquot antigen-coupled beads and incubate with sample sera under the following test conditions in parallel:
- Condition A: 4°C overnight (≈16-18 hours), protected from light.
- Condition B: 37°C for 2 hours.
- Condition C: Room temperature for 1 hour.
- 4. Detection & Analysis: Wash beads and incubate with phycoerythrin (PE)-conjugated detection antibodies specific for the human Ig isotype/subclass (e.g., anti-IgG, IgG1-4, IgM, IgE). Measure median fluorescence intensity (MFI) on a flow-based multiplex reader (e.g., Luminex).
- 5. Optimal Condition Selection: Compare the MFI signals and signal-to-noise ratios across the three conditions. The condition yielding the highest specific signal (from the positive control) without elevating the negative control signal is optimal. For the tested P. falciparum assays, this was 4°C overnight.
This protocol outlines a framework for evaluating the inter-laboratory reproducibility of a multiplex assay, focusing on the critical role of standardized reagents.
- 1. Reagent Design: Procure kits from multiple manufacturers and, importantly, multiple lots from each manufacturer.
- 2. Common Reference Standards: Prepare and distribute identical sets of samples to all participating laboratories. These must include:
- Spiked Samples: With known concentrations of analytes.
- Biological Samples: Relevant to the study context (e.g., vaccine responses).
- Newly Developed Reference Standards: A common pool of serum or culture supernatant to be used as a running control.
- 3. Assay Execution: Each laboratory performs the multiplex assay according to its standard operating procedure or the manufacturer's instructions.
- 4. Data Analysis & Harmonization: Collect all raw data files. Use a uniform algorithm (e.g., a logistic function for standard curve analysis) to calculate analyte concentrations across all labs. Statistically determine the major sources of variation (e.g., lab, kit lot, analyst).
The Scientist's Toolkit: Essential Reagents for Reproducible Immunoassays
Standardized, high-quality reagents are the foundation of any reproducible assay. The table below lists key solutions used in the featured experiments.
Table 2: Key Research Reagent Solutions for Assay Optimization
| Reagent / Solution | Critical Function | Application Example |
|---|---|---|
| International Reference Standards (e.g., WHO) [72] [70] | Provides a universal benchmark for quantifying analyte levels, enabling cross-study and cross-lab data comparison. | Calibrating a multiplex bead assay for vaccine antibodies (e.g., anti-diphtheria, tetanus) [72]. |
| Customized Positive Control Pools | Enriches for specific, low-abundance analytes not adequately present in commercial standards, improving assay sensitivity. | Creating a control with high anti-CSP antibodies for malaria vaccine studies [70]. |
| Carboxylated Magnetic Beads | Solid-phase matrix for covalent coupling of antigens or capture antibodies in multiplex bead assays. | Coupling pertussis, diphtheria, and tetanus antigens for a multiplex serological assay [72]. |
| Carbodiimide Coupling Chemistry (EDAC/sulfo-NHS) | Activates carboxylated beads to form stable amide bonds with primary amines in proteins (antigens/antibodies). | Covalently linking P. falciparum antigens to MagPlex microspheres [70]. |
| Third-Party Universal Detection Reagent | Eliminates variability introduced by different detection antibodies included in commercial kits. | Harmonizing signal detection across multiplex kits from different manufacturers in a cross-lab study [71]. |
Visualizing the Workflow for Incubation Parameter Optimization
The following diagram outlines the logical workflow for determining the optimal incubation conditions for an immunological assay, as derived from the experimental protocols.
Diagram: Workflow for Optimizing Assay Incubation Conditions. This process involves testing key parameters in parallel to identify the condition that yields the most robust and reliable result.
The experimental data clearly demonstrates that the optimization of incubation times and concentrations is not merely a procedural step but a fundamental determinant of an immunoassay's reproducibility and analytical robustness. The consistent finding of significant inter-laboratory variability, even with standardized kits [10] [71], underscores that protocol harmonization must extend beyond simple adherence to manufacturer instructions. Future efforts in immunological monitoring should prioritize the universal adoption of common reference standards [71] [72] and the detailed reporting of optimized parameters like 4°C overnight incubation for serological assays [70]. By systematically validating and documenting these critical assay parameters, the scientific community can enhance the reliability of data, facilitate direct comparisons across studies, and accelerate discoveries in immunology and drug development.
The reproducibility of immunological assays across different research laboratories is a cornerstone of reliable scientific discovery and drug development. Flow cytometry, a pivotal technology in immunology, faces significant challenges in data analysis consistency, primarily due to the subjective, labor-intensive nature of manual gating. This process, where analysts visually identify cell populations by drawing boundaries on plots, introduces substantial inter-operator variability, complicating the comparison of results across multicenter studies [73].
Automated gating and machine learning approaches have emerged as powerful solutions to overcome these limitations, promising enhanced objectivity, throughput, and reproducibility. This guide provides a comparative evaluation of leading automated gating technologies, assessing their performance, experimental validation, and practical implementation within the critical context of harmonizing immunological data analysis across laboratories.
Comparative Performance Evaluation of Automated Gating Solutions
The following table summarizes the key performance metrics of several automated gating solutions as validated in recent studies, providing a direct comparison of their accuracy, efficiency, and data requirements.
Table 1: Performance Comparison of Automated Gating and Machine Learning Approaches
| Technology / Tool | Reported Performance (F1 Score) | Training Data Required | Analysis Speed | Key Advantages |
|---|---|---|---|---|
| BD ElastiGate [73] | 0.82 to >0.93 (across multiple cell types and assays) | Minimal (1 pre-gated sample) | High (batch processing) | Accessible plugin for FlowJo/FACSuite; based on visual pattern recognition. |
| GateNet [74] | 0.910 to 0.997 (human-level performance) | ~10 samples | 15 microseconds/event (GPU) | Fully end-to-end automated gating with built-in batch effect correction. |
| flowDensity [73] | Used as a comparator in studies | Variable, requires computational expertise | Not Specified | A leading tool for automating analysis using pre-established gating hierarchy. |
| Cytobank Automatic Gating [73] | Used as a comparator in studies | Not Specified | Not Specified | Cloud-based analysis platform. |
The quantitative data reveals that both BD ElastiGate and GateNet achieve high accuracy, comparable to expert manual gating. GateNet demonstrates exceptional data efficiency, requiring only approximately ten samples to reach human-level performance, making it suitable for studies with limited sample sizes [74]. Its integrated batch effect correction is a significant advantage for multi-center studies. Conversely, BD ElastiGate's strength lies in its practical integration into widely used commercial software suites (FlowJo and BD FACSuite), allowing for easier adoption by biologists without deep computational expertise [73].
Detailed Experimental Protocols and Methodologies
Protocol for Validating Automated Gating Tools
The validation of automated gating tools relies on rigorous benchmarking against manually gated datasets, often with consensus from multiple experts. The following workflow outlines a standard protocol for such validation studies.
Title: Automated Gating Validation Workflow
The methodology typically involves several critical stages. First, Sample Collection and Manual Ground Truth Establishment is performed. For instance, one GateNet study utilized over 8,000,000 events from 127 peripheral blood and cerebrospinal fluid samples, each independently labeled by four human experts to create a robust consensus ground truth [74]. Similarly, BD ElastiGate validation used datasets from CAR-T cell manufacturing, tumor immunophenotyping, and cytotoxicity assays, with manual gating performed by several expert analysts [73].
Next, in the Algorithm Training and Execution phase, the automated tool is trained on a subset of this data. A key differentiator is the amount of data required; ElastiGate can function with a single pre-gated sample as a template [73], whereas GateNet requires around ten samples to achieve peak performance [74].
Finally, Performance Quantification is conducted using statistical metrics. The F1 score—the harmonic mean of precision and recall—is the standard metric for comparing algorithm-generated gates against the manual ground truth. This process evaluates not just accuracy but also the reduction in inter-operator variability, which is fundamental for inter-laboratory reproducibility [73] [74].
Broader Context: Harmonization of Immunological Assays
The challenge of variability is not unique to flow cytometry. Inter-laboratory comparisons of other immunological assays reveal similar issues, underscoring the need for standardized protocols. For example, a 2025 study comparing an anti-FGFR3 autoantibody ELISA across centers in France and Germany found that while overall concordance was substantial (81%), optical densities differed significantly between sites, necessitating laboratory-specific cut-off values [75]. Another 2024 study on a microneutralization assay for detecting anti-AAV9 antibodies highlighted that standardized protocols, including defined cell lines, virus particles, and quality controls, were crucial for achieving reproducible results across laboratories [2]. These examples from related fields highlight that harmonization requires both technological solutions (like automated gating) and strict procedural standardization.
Essential Research Reagent Solutions and Materials
Successful implementation of automated gating and assay harmonization depends on access to specific, high-quality reagents and platforms. The following table details key materials used in the featured experiments and the broader field.
Table 2: Key Research Reagent Solutions for Flow Cytometry and Assay Harmonization
| Item / Reagent | Function / Application | Example Use-Case |
|---|---|---|
| Flow Cytometers | Platform for acquiring single-cell data. | DxFLEX vs. FACS Canto II cross-platform validation [76]. |
| Fluorescent Quantitation Beads | Calibrating cytometer fluorescence scale & quantifying antigen density. | Used in ElastiGate benchmarking for gating multiple bead populations [73]. |
| Standardized Cell Lines | Reproducible cellular substrate for functional assays. | HEK293 cell lines used in inter-lab microneutralization assay for AAV9 NAbs [2]. |
| rAAV Vectors (e.g., rAAV9-EGFP-2A-Gluc) | Viral tools for cell-based neutralization assays. | Critical reagent in standardized MN assay for detecting anti-AAV9 neutralizing antibodies [2]. |
| Reference Sera & Controls | Positive/Negative controls for assay calibration and quality control. | Used in inter-lab ELISA and MN studies to determine cut-off values and monitor performance [75] [2]. |
| Validated Antibody Panels | Phenotyping and identifying specific immune cell subsets. | Refined B-cell panels incorporating CD21 for better subset stratification [77]. |
The integration of these reagents with automated analysis platforms is key to modernizing workflows. As noted in trend analyses for 2025, unified lab informatics platforms (sometimes called "Lab-in-a-Loop") are essential for ingesting and centralizing data from diverse sources like instruments and assays, which is a prerequisite for deploying effective AI and machine learning models [78].
The harmonization of data analysis across immunological laboratories is an achievable goal through the adoption of automated gating and machine learning. Technologies like BD ElastiGate and GateNet demonstrate that it is possible to achieve human-level accuracy while drastically improving consistency and throughput. The choice between solutions often involves a trade-off between the seamless integration and user-friendliness of commercial plugins and the advanced, end-to-end automation with built-in batch correction offered by novel neural network architectures.
A holistic approach to harmonization is critical. It requires not only selecting a robust analytical algorithm but also a commitment to standardizing experimental protocols, using calibrated reagents, and implementing controlled data management systems. As the field moves towards increasingly multimodal research, platforms that support flexibility and data interoperability will be vital for training the next generation of AI models, ultimately driving more reproducible and reliable drug development.
Robust Validation Frameworks and Comparative Assay Analysis
Immunoassay validation provides the documented evidence that an analytical method is fit for its intended purpose, ensuring the reliability of data used in clinical diagnostics and drug development [79] [80]. The validation process confirms through examination that the method's performance characteristics—including precision, trueness, and limits of quantitation (LOQ)—meet predefined requirements for their specific application [80]. In regulated environments such as pharmaceutical development, method validation is not merely good scientific practice but a mandatory compliance requirement with standards set by regulatory bodies like the FDA and through international guidelines such as ICH Q2(R1) [81] [82].
The fundamental principle underlying method validation is that the extent of validation should be determined by the method's intended use [79] [80]. For instance, a method developed as an in-house research tool may require different validation parameters than one used for quality control of a commercial therapeutic product. When evaluating immunological assays across multiple laboratories, understanding the hierarchy of precision—from repeatability to reproducibility—becomes particularly critical for interpreting data generated from multicenter studies [83]. This guide examines the core validation parameters with a specific focus on their application in assessing the reproducibility of immunological assays across research laboratories, providing both theoretical frameworks and practical experimental approaches.
Core Validation Parameters: Precision, Trueness, and LOQ
Precision: Repeatability, Intermediate Precision, and Reproducibility
Precision is defined as "the closeness of agreement between independent test results obtained under stipulated conditions" [79] [80]. The precision of an analytical method is evaluated at three distinct levels, each introducing additional sources of variability, as illustrated in Figure 1.
Repeatability (intra-assay precision) represents the smallest possible variation in results, obtained when the same sample is analyzed repeatedly over a short time period using the same measurement procedure, operators, instruments, and location [81] [83]. In practice, repeatability is assessed through a minimum of nine determinations across a minimum of three concentration levels covering the specified range (e.g., three concentrations with three replicates each) [81]. Results are typically reported as the percent relative standard deviation (%RSD), with acceptance criteria depending on the assay type and its intended use.
Intermediate precision (within-lab reproducibility) incorporates additional variability factors encountered within a single laboratory over an extended period, including different analysts, equipment, reagent lots, and calibration standards [81] [83]. Because intermediate precision accounts for more sources of variation than repeatability, its standard deviation is consequently larger [83]. Experimental designs for intermediate precision should systematically vary these factors to isolate their individual and combined effects on measurement variability.
Reproducibility (between-lab reproducibility) represents the highest level of variability, assessed through collaborative studies between different laboratories [81] [83]. Reproducibility is essential when analytical methods are transferred between sites or used in multicenter studies, as it captures the additional variability introduced by different laboratory environments, equipment, and personnel [83].
Figure 1: Hierarchy of precision measurement encompassing repeatability, intermediate precision, and reproducibility.
Trueness and Recovery
Trueness refers to "the closeness of agreement between the average value obtained from a large series of test results and an accepted reference value" [79]. It represents the systematic error component of measurement uncertainty and is typically assessed through recovery experiments [79]. In these experiments, known quantities of the analyte are added to a sample matrix, and the measured value is compared to the theoretical expected value. Recovery is calculated as the percentage of the known added amount that is recovered by the assay [79] [81].
The experimental approach for documenting trueness involves collecting data from a minimum of nine determinations over a minimum of three concentration levels covering the specified range [81]. The data should be reported as the percent recovery of the known, added amount, or as the difference between the mean and the true value with confidence intervals (e.g., ±1 standard deviation) [81]. For drug substances, accuracy measurements may be obtained by comparison to a standard reference material or a second, well-characterized method [81].
Limits of Quantitation (LOQ)
The limit of quantitation (LOQ) is defined as "the lowest concentration of an analyte in a sample that can be quantitated with acceptable precision and accuracy under the stated operational conditions of the method" [81]. The LOQ represents the lower boundary of the method's quantitative range and is distinct from the limit of detection (LOD), which represents the lowest concentration that can be detected but not necessarily quantified with acceptable precision [81].
Two primary approaches are used for determining LOQ:
- Signal-to-noise ratio: Using a ratio of 10:1 for LOQ [81]
- Standard deviation and slope method: Calculated using the formula LOQ = K(SD/S), where K is a constant (typically 10 for LOQ), SD is the standard deviation of response, and S is the slope of the calibration curve [81]
It is important to note that determining these limits is a two-step process: initial calculation followed by experimental verification through analysis of an appropriate number of samples at the limit to fully validate method performance [81].
Experimental Protocols for Validation Parameters
Protocol for Precision Assessment
A comprehensive precision assessment should evaluate all three levels of precision (repeatability, intermediate precision, and reproducibility) using a standardized experimental design.
Sample Preparation and Experimental Design:
- Prepare quality control (QC) samples at three concentrations (low, medium, high) covering the assay range
- For repeatability: Analyze each QC level in a minimum of six replicates in a single run by one analyst using the same equipment and reagents [81] [16]
- For intermediate precision: Analyze each QC level in duplicate across multiple runs (different days, different analysts, different equipment, different reagent lots) [81]. A typical design involves two analysts each preparing and analyzing replicate sample preparations using different HPLC systems [81]
- For reproducibility: Expand the intermediate precision design to include multiple laboratories, with each site following the same standardized protocol [10] [83]
Data Analysis:
- Calculate mean, standard deviation, and %RSD for each QC level at each precision level
- For intermediate precision, compare results between analysts using statistical tests (e.g., Student's t-test) to determine if significant differences exist [81]
- For reproducibility across laboratories, report standard deviation, %RSD, and confidence intervals, and perform statistical analysis to assess interlaboratory variability [10]
Table 1: Example Precision Acceptance Criteria Based on Industry Standards
| Precision Level | Sample Design | Acceptance Criteria | Statistical Output |
|---|---|---|---|
| Repeatability | Minimum of 9 determinations (3 concentrations, 3 replicates) | %RSD < 2-5% depending on assay type | Standard deviation, %RSD |
| Intermediate Precision | Two analysts, duplicate preparations, different instruments | % difference in means < 5% | Student's t-test, %RSD |
| Reproducibility | Collaborative study with multiple laboratories | Based on study objectives, typically %RSD < 10-15% | Interclass correlation coefficient, %RSD |
Protocol for Trueness (Recovery) Evaluation
The recovery experiment evaluates the method's ability to accurately measure the analyte of interest across the validated range.
Sample Preparation:
- Prepare a blank matrix (e.g., serum, plasma) that is free of the analyte
- Spike known concentrations of the analyte into the blank matrix to create samples at a minimum of three concentration levels (low, medium, high) covering the quantitative range
- Include a minimum of three replicates at each concentration level [81]
Experimental Procedure:
- Analyze each spiked sample using the validated method
- Include calibration standards and quality controls in each run to ensure proper method performance
- Calculate the measured concentration for each spiked sample based on the calibration curve
Data Analysis:
- Calculate percent recovery for each sample: (Measured Concentration / Theoretical Concentration) × 100
- Calculate mean recovery and %RSD for each concentration level
- Acceptance criteria typically require mean recovery of 85-115% (80-120% at LOQ) with %RSD < 15% (20% at LOQ), though these may vary based on the method's intended use [81]
Protocol for LOQ Determination
Two complementary approaches should be used to determine LOQ, with verification of the final value through experimental testing.
Signal-to-Noise Method:
- Prepare samples at progressively lower concentrations near the expected LOQ
- Inject each sample and measure the signal-to-noise ratio (S/N)
- LOQ is the lowest concentration where S/N ≥ 10:1 [81]
Standard Deviation and Slope Method:
- Use the formula: LOQ = 10 × (SD/S)
- Where SD is the standard deviation of the response (y-intercept) and S is the slope of the calibration curve [81]
- This approach is particularly useful for chromatographic methods with baseline noise
LOQ Verification:
- Prepare and analyze a minimum of six replicates at the determined LOQ concentration
- Demonstrate that the precision (%RSD) at LOQ is ≤20% and accuracy (mean recovery) is 80-120% [81]
- Establish that the analyte response at LOQ is recognizable, discrete, and reproducible [81]
Case Studies in Immunoassay Reproducibility
Multicenter Study of T-Cell Activation Markers
A comprehensive study evaluating the reproducibility of immunological tests for multiple chemical sensitivity (MCS) syndrome provides valuable insights into interlaboratory variability [10] [69]. The study analyzed replicate blood samples from 19 healthy volunteers, 15 persons with MCS, and 11 persons with autoimmune disease across five laboratories for T-cell surface activation markers (CD25, CD26, CD38, and HLA-DR) [10].
Key Findings:
- Intralaboratory reproducibility was excellent, with 90% of replicates analyzed in the same laboratory differing by ≤3% [10] [69]
- Interlaboratory differences were statistically significant for all T-cell subsets except CD4+ cells, ranging from minor to eightfold for CD25+ subsets [10] [69]
- The date of analysis within laboratories was significantly associated with values for all cellular activation markers, highlighting the importance of temporal factors in assay performance [10]
- Shipping effects on measurements, while sometimes statistically significant, were very small, supporting the reliability of shipped samples for multicenter studies [10]
Table 2: Interlaboratory Variability of T-Cell Subset Measurements in Multicenter Study
| T-Cell Subset | Intralaboratory Reproducibility | Interlaboratory Variability | Key Influencing Factors |
|---|---|---|---|
| CD25+ | ≤3% difference between replicates | Up to eightfold differences between laboratories | Methodological differences, analysis date |
| CD26+ | ≤3% difference between replicates | Statistically significant differences | Laboratory-specific protocols |
| CD38+ | ≤3% difference between replicates | Statistically significant differences | Instrument calibration, reagent lots |
| HLA-DR+ | ≤3% difference between replicates | Statistically significant differences | Analysis date, personnel technique |
Multiplexed Immunoassay for Malaria Vaccine Development
The validation of a multiplexed immunoassay for immunological analysis of pre-erythrocytic malaria vaccines demonstrates approaches to addressing reproducibility challenges in vaccine development [4]. The assay was designed to measure antibodies specific to four antigens representing components of the R21 immunogen and was validated for use in a Phase 3 clinical trial across five sites in four African countries [4].
Validation Approach:
- Inter-laboratory variability was assessed by comparing standards and QC samples between the developer's laboratory (Meso Scale Discovery) and the end-user laboratory (Jenner Institute) [4]
- Intra-run variability was evaluated by comparing two plates run by the same operator on the same day [4]
- The multiplex assay demonstrated a strong linear relationship with the singleplex ELISA reference method, with rho values of 0.89 and 0.88 for two separate clinical trials (both p < 0.0005) [4]
Performance Metrics:
- For standard curve samples, the mean coefficient of variation (CV) was 2.5% across all antigens [4]
- QC samples showed increasing variation with increased dilution: mean CV of 14.1% for QC1 (high), 17.3% for QC2 (medium), and 21.7% for QC3 (low) [4]
- Clinical trial sample measurements were positively correlated between laboratories, with statistical significance for all antigens [4]
ELISA Reproducibility for Anti-HPV Antibody Isotypes
A recent study evaluated the reproducibility of enzyme-linked immunosorbent assays (ELISAs) for detecting anti-HPV16 L1-specific IgG1, IgG3, IgA, and IgM antibodies, highlighting the variability across different immunoglobulin isotypes [16].
Experimental Design:
- Seventy-two serum samples from participants in the Costa Rica HPV Vaccine Trial were used for reproducibility assessment [16]
- Measurements were performed across different technicians and days to evaluate multiple sources of variability [16]
- Intraclass correlation coefficients (ICCs) and coefficients of variation (CVs) were calculated to quantify reproducibility [16]
Reproducibility Findings:
- CVs between technicians ranged from 12.8-22.7%, while CVs across days ranged from 6.2-30.6% [16]
- Overall CVs ranged from 7.7-31.1%, with IgM ELISA showing higher variability (15.8-31.1%) than IgG1, IgG3, and IgA (6.2-22.7%) [16]
- All ICC values were >98.7%, indicating excellent reliability despite the observed variability in CVs [16]
Table 3: Reproducibility Metrics for Anti-HPV16 L1 Antibody Isotype ELISAs
| Antibody Isotype | Inter-Technician CV (%) | Inter-Day CV (%) | Overall CV (%) | Detectability in Samples |
|---|---|---|---|---|
| IgG1 | 12.8-22.7 | 6.2-30.6 | 7.7-31.1 | >86.3% |
| IgG3 | 12.8-22.7 | 6.2-30.6 | 7.7-31.1 | 100% |
| IgA | 12.8-22.7 | 6.2-30.6 | 7.7-31.1 | >86.3% |
| IgM | 15.8-31.1 | 15.8-31.1 | 15.8-31.1 | 62.1% |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful immunoassay validation requires careful selection and standardization of key reagents and materials. The following table outlines essential components and their functions in validation experiments.
Table 4: Essential Research Reagent Solutions for Immunoassay Validation
| Reagent/Material | Function in Validation | Critical Considerations |
|---|---|---|
| Reference Standards | Establish calibration curve; quantify analyte | Purity, stability, commutability with patient samples |
| Quality Control Materials | Monitor assay performance over time | Three levels (low, medium, high); commutable; stable |
| Matrix-Matched Samples | Evaluate specificity, recovery, and matrix effects | Should match patient sample matrix (serum, plasma, etc.) |
| Detection Antibodies | Signal generation for analyte quantification | Specificity, affinity, lot-to-lot consistency |
| Solid Phase Supports | Immobilization of capture reagents | Binding capacity, uniformity, low non-specific binding |
| Assay Buffer Systems | Maintain optimal assay conditions | pH, ionic strength, blocking agents, stabilizers |
| Secondary Reagents | Signal amplification and detection | Enzyme conjugates, labels, detection substrates |
Implementation in Regulated Environments
Cross-Validation Between Methods and Laboratories
When combining data from different methods or laboratories for regulatory submissions, cross-validation becomes essential to demonstrate comparability [84]. The ICH M10 guideline emphasizes the assessment of bias between methods, though it does not stipulate specific acceptance criteria [84]. Recent approaches to cross-validation include:
- Statistical assessment of bias using Bland-Altman plots, Deming regression, and Concordance Correlation Coefficient [84]
- Sample selection with n>30 samples spanning the concentration range [84]
- Two-step equivalency assessment: initial evaluation of whether the 90% confidence interval of the mean percent difference of concentrations is within ±30%, followed by assessment of concentration-dependent bias trends [84]
The debate continues regarding appropriate acceptance criteria for cross-validation, with some experts arguing that pass/fail criteria are inappropriate and that statistical experts should be involved in designing cross-validation plans and interpreting results [84].
Robustness Testing and Method Transfer
Robustness is "the ability of a method to remain unaffected by small variations in method parameters" [79] [80] [81]. Robustness testing should identify critical parameters in the procedure (e.g., incubation times, temperatures) and systematically evaluate the impact of small variations on method performance [79] [80].
The experimental approach for robustness testing includes:
- Identifying critical method parameters
- Performing the assay with systematic changes to these parameters, one at a time
- Using the same set of samples at each occasion to isolate the effect of each parameter
- Incorporating acceptable parameter ranges into the final method protocol [79] [80]
Figure 2: Immunoassay validation workflow showing sequential assessment of key parameters.
The validation of immunoassays for precision, trueness, and LOQ provides the foundation for generating reliable data in research and regulated environments. The case studies presented demonstrate that while intralaboratory precision can be excellent (≤3% difference for cellular markers), interlaboratory variability presents ongoing challenges that require systematic assessment and control [10] [69] [16]. Successful method validation requires not only technical competence but also rigorous experimental design, appropriate statistical analysis, and thorough documentation.
As immunoassay technologies advance and their applications expand into novel biomarkers and personalized medicine approaches, the principles of method validation remain constant: objective evidence must demonstrate that a method fulfills the requirements for its intended use [79] [80]. By adhering to these principles and implementing the protocols outlined in this guide, researchers can ensure the quality and reproducibility of immunological data across laboratories, ultimately supporting robust scientific conclusions and regulatory decision-making.
Assessing Parallelism, Recovery, and Selectivity in Complex Matrices
In the development and validation of ligand-binding assays (LBAs) for biological compounds, demonstrating reliable performance in complex matrices like serum or plasma is paramount. For researchers, scientists, and drug development professionals, three parameters are particularly critical for assessing assay accuracy and reliability: parallelism, recovery, and selectivity. These parameters evaluate how an assay performs when measuring an endogenous analyte in its natural, complex biological environment, as opposed to a simple buffer. Parallelism experiments are, in fact, an essential experiment characterizing relative accuracy for an LBA [85]. They serve to assess the effects of dilution on the quantitation of endogenous analyte(s) in matrix, thereby evaluating selectivity, matrix effects, the minimum required dilution, endogenous levels in healthy and diseased populations, and the lower limit of quantitation (LLOQ) in a single, comprehensive experiment [85].
The core scientific challenge in biomarker measurement, as opposed to traditional drug assays, is the presence of the endogenous molecule itself. This complexity means that simple spike-and-recovery experiments used for drug concentration assays are insufficient [86]. When measuring endogenous molecules, scientists face challenges that spike recovery alone cannot address. The central question shifts from simple recovery to demonstrating that the critical reagents recognize both the standard calibrator material and the endogenous analyte in a consistent and comparable manner [86]. This article provides a comparative guide to the experimental methodologies and performance data for assessing these key parameters, framed within the broader thesis of evaluating the reproducibility of immunological assays across research laboratories.
Experimental Protocols for Key Parameters
Protocol for Parallelism Assessment
Parallelism tests whether the dilution-response curve of an endogenous sample runs parallel to the standard curve prepared in the assay matrix. This indicates that the assay reagents recognize the endogenous analyte and the reference standard similarly.
Detailed Methodology:
- Sample Selection: Identify a study sample with a high endogenous concentration of the analyte of interest.
- Sample Dilution: Prepare a series of dilutions (e.g., 1:2, 1:4, 1:8, etc.) of the study sample using the assay dilution buffer. The dilution range should cover the quantifiable range of the standard curve.
- Standard Curve Preparation: Prepare the standard curve per the assay protocol by serially diluting the reference standard material in the same matrix used for the standard curve (often a surrogate or stripped matrix).
- Assay Run: Analyze all diluted study samples and the standard curve in the same run using the validated immunoassay protocol (e.g., ELISA or multiplex immunoassay).
- Data Analysis: Calculate the apparent concentration of the analyte in each diluted study sample by interpolating from the standard curve.
- Result Interpretation: Multiply the apparent concentration by the dilution factor for each point. If the diluted samples are parallel to the standard curve, the calculated concentrations (after correction for dilution) should be consistent across the dilution series. A lack of parallelism suggests interference from the matrix or differences in the properties of the endogenous analyte versus the reference standard [85] [86].
Protocol for Recovery Assessment
Recovery experiments determine the accuracy of the assay by measuring the ability to recover a known amount of reference standard spiked into the study matrix.
Detailed Methodology:
- Baseline Measurement: Analyze the native study matrix (e.g., serum from a healthy donor) to determine the baseline level of the endogenous analyte.
- Spike Preparation: Spike the reference standard at multiple concentrations (e.g., low, mid, and high) into aliquots of the study matrix. The spiked concentrations should be within the assay's quantitative range.
- Control Preparation: Prepare matching standard concentrations in the ideal matrix (e.g., buffer or stripped matrix) used for the standard curve.
- Assay Run: Analyze the spiked study matrix samples, the control samples, and the standard curve in the same run.
- Data Analysis:
- Calculate the measured concentration in the spiked study matrix.
- Calculate the endogenous concentration from the unspiked matrix.
- The percent recovery is calculated as:
[(Measured concentration in spiked matrix - Endogenous concentration) / Known spiked concentration] × 100%.
- Result Interpretation: Consistent recovery (typically 80-120%, depending on the assay's validated criteria) across the spiked concentrations indicates minimal matrix interference and good assay accuracy [86].
Protocol for Selectivity Assessment
Selectivity is the ability of the assay to measure the analyte unequivocally in the presence of other components that might be expected to be present in the sample, such as similar proteins, metabolites, or binding proteins.
Detailed Methodology:
- Sample Collection: Obtain individual matrix samples (e.g., serum or plasma) from a sufficient number of normal and disease-state donors (e.g., 10 or more).
- Sample Analysis: Measure the endogenous analyte levels in these individual samples.
- Spiking and Recovery in Individual Matrices: Spike the analyte at a low concentration (e.g., near the LLOQ) into each of the individual matrix samples and measure the recovery.
- Data Analysis: Calculate the percent recovery for each individual donor matrix as described in the recovery protocol.
- Result Interpretation: The assay is considered selective if the recoveries across the different individual matrices fall within pre-defined acceptance criteria (e.g., ±25% of the nominal concentration). This demonstrates that the assay performance is consistent across the biological diversity encountered in the target population [86].
The logical relationship and purpose of these three key experiments in validating an assay's performance in a complex matrix are summarized in the following workflow.
Performance Data Comparison Across Assay Formats
The reproducibility and robustness of an assay are ultimately quantified through specific performance metrics. These metrics allow for the objective comparison of different assay formats and their suitability for use in regulated studies. The following table summarizes key quantitative performance data from interlaboratory studies and validation reports for various immunological assay formats.
Table 1: Comparative Performance Metrics from Interlaboratory Studies
| Assay Format / Target | Key Performance Parameter | Reported Result | Context & Study Details |
|---|---|---|---|
| Multiplex Immunoassay (MIA)Anti-GBS CPS IgG [1] | Within-laboratory Intermediate Precision | Generally < 20% RSD | Across 5 laboratories, 44 human sera, 6 serotypes. Factors: bead lot, analyst, day. |
| Cross-laboratory Reproducibility | < 25% RSD for all 6 serotypes | Demonstrated consistency across different laboratory settings. | |
| Microneutralization (MN) AssayAnti-AAV9 Neutralizing Antibody [2] | Intra-assay Variation (low positive QC) | 7–35% | Cell-based assay. |
| Inter-assay Variation (low positive QC) | 22–41% | Cell-based assay. | |
| Inter-laboratory Reproducibility (blind samples) | %GCV of 23–46% | Method transferred to and compared across 3 laboratories. | |
| Rapid ImmunoassaysHeparin-Induced Thrombocytopenia (HIT) [87] | Within-run Imprecision (CV) | Met < 10% criterion | Based on 10 within-run repetitions. |
| Day-to-day Imprecision (CV) | Met < 10% criterion | Based on 5 day-to-day repetitions. |
Beyond the core parameters of precision and reproducibility, other statistical measures are vital for evaluating the overall robustness of an assay, especially in a screening environment. The Z' factor is a key statistical score that incorporates both the assay dynamic range (Signal-to-Background) and the data variation (Standard Deviation) [88]. An assay with a Z' score between 0.5 and 1.0 is considered of good-to-excellent quality and suitable for high-throughput screening, while a score below 0.5 indicates a poor-quality assay that is unreliable for screening purposes [88].
The Scientist's Toolkit: Essential Reagents & Materials
The successful execution of the aforementioned experiments and the attainment of reliable data depend on the use of standardized, high-quality reagents. The following table details key research reagent solutions and their critical functions in method development and validation.
Table 2: Essential Research Reagents for Validation Experiments
| Reagent / Material | Function in Validation | Application Example from Literature |
|---|---|---|
| Antigen-Coated Beads | Solid phase for capturing target analyte in multiplex assays. Lot-to-lot qualification is essential. | Used in the standardized GBS multiplex immunoassay; qualified in side-by-side comparisons using a reference serum panel [1]. |
| Human Serum Reference Standard | Calibrator with assigned antibody concentrations to enable quantitative interpolation of unknown samples. | Served as the primary standard in the interlaboratory GBS study, allowing comparison of results across six serotypes and five laboratories [1]. |
| Quality Control (QC) Samples | Monitors assay precision and performance over time. Typically a pool of known positive samples. | Used in both the GBS and AAV9 studies to ensure system suitability and control inter-assay variation [1] [2]. |
| Critical Antigen Conjugates | The purified antigen (e.g., CPS-PLL) used to coat beads or plates, defining assay specificity. | GBS CPS-PLL conjugates for all six serotypes were centrally prepared and distributed to participating laboratories to ensure consistency [1]. |
| Secondary Antibody (Labeled) | Detection reagent; its specificity and label (e.g., R-Phycoerythrin) are key for sensitivity. | A standardized R-Phycoerythrin-conjugated goat anti-human IgG was used in the GBS MIA [1]. |
| Assay Buffer & Blockers | Minimizes non-specific binding and matrix effects, crucial for recovery and selectivity. | Assay buffers (e.g., PBS with BSA and Tween) are used universally to dilute samples and reagents [1] [89]. |
| System Suitability Controls | Confirms the assay is performing as expected before results are accepted. | The AAV9 MN assay required a virus control to cell control ratio >10 for a valid run [2]. |
The rigorous assessment of parallelism, recovery, and selectivity is not merely a regulatory checkbox but a fundamental scientific requirement for ensuring that immunological assays generate reliable and meaningful data in complex biological matrices. As demonstrated by interlaboratory studies, the use of standardized protocols, critical reagents, and a systematic approach to validation enables a high degree of reproducibility across different laboratory settings [1] [2]. This reproducibility is the bedrock upon which credible biomarker discovery, vaccine evaluation, and diagnostic development are built. By adhering to detailed experimental protocols for these key parameters and critically evaluating performance metrics, researchers and drug developers can have greater confidence in their data, facilitating robust comparisons across studies and accelerating the translation of scientific findings into clinical applications.
The evaluation of immunological assays presents a fundamental trade-off between simplicity and comprehensiveness. On one hand, simpler assay formats, often based on single metrics like binary serostatus or total IgG, offer streamlined protocols and straightforward data interpretation. On the other, complex serological analyses, such as systems serology, provide a multidimensional view of immune responses by interrogating antibody isotypes, subclasses, and effector functions. This comparison is framed within a critical thesis: assessing the reproducibility of these assays across different laboratories and research settings. Reproducibility is not merely a technical concern but a foundational requirement for generating reliable scientific knowledge and robust public health insights [90] [10]. As serological data becomes increasingly central to understanding infectious disease dynamics and vaccine efficacy, the choice between simple and complex assays carries significant implications for both research validity and clinical application [90] [91]. This guide objectively compares the performance of these divergent approaches through experimental data, methodological protocols, and analytical frameworks.
The table below summarizes the core characteristics, performance data, and optimal use cases for simpler and complex serological assay formats.
Table 1: Comparative Overview of Serological Assay Formats
| Feature | Simpler Assay Formats | Complex Serological Analyses |
|---|---|---|
| Core Metrics | Binary serostatus (positive/negative), total antigen-specific IgG/IgM [90] | Multiple antibody isotypes (IgG1-4, IgA1-2, IgE, IgM), Fc receptor binding (FcγRIIA/B, FcγRIIIA), effector functions (ADCD, ADCP, ADNP) [91] |
| Typical Platforms | Conventional ELISA, Lateral Flow Immunoassays (LFI) [92] | Multiplex protein arrays, customized ligand binding assays, systems serology platforms [91] [92] |
| Throughput | High | Medium to Low |
| Data Complexity | Low (single-dimensional) | High (multidimensional) |
| Key Performance Data | Diagnostic specificity ≥95% is crucial for population screening [92] | Identifies distinct immune signatures (e.g., adjuvants AS01/AS03 vs. Alum induce different Fc-profiles) [91] |
| Inter-laboratory Reproducibility | Can show statistically significant, sometimes major (e.g., eightfold) differences for cellular markers [10] | Requires stringent standardization; cell fitness (>70% live, apoptosis-negative) critical for reliable PBMC-based assays [93] |
| Best Applications | Large-scale serosurveys, progress monitoring towards elimination, initial screening [90] | Deep immunoprofiling, correlates of protection studies, vaccine adjuvant evaluation [90] [91] |
Experimental Protocols for Method Comparison
Protocol for a Comparison of Methods Experiment
A standardized "Comparison of Methods" experiment is critical for objectively assessing the systematic error (inaccuracy) between a new test method and a established comparative method using real patient specimens [94].
- Specimen Selection and Number: A minimum of 40 different patient specimens should be selected to cover the entire working range of the method and represent the spectrum of diseases expected in routine application. The quality of specimens, providing a wide range of results, is more critical than a large number [94].
- Experimental Timeline and Replication: The experiment should be conducted over a minimum of 5 days, analyzing 2-5 patient specimens per day, to minimize systematic errors from a single run. While single measurements are common, performing duplicate measurements on different sample aliquots is ideal to identify sample mix-ups or transposition errors [94].
- Data Analysis and Graphical Interpretation: Data should be graphed at collection for visual inspection. A difference plot (test result minus comparative result on the y-axis versus the comparative result on the x-axis) is used for methods expected to show one-to-one agreement. A comparison plot (test result vs. comparative result) is used for methods not expected to agree perfectly. Linear regression statistics (slope, y-intercept, standard error of the estimate) are calculated to estimate systematic error at medically important decision concentrations [94].
Protocol for a Systems Serology Analysis
Systems serology provides a high-dimensional, functional profile of the humoral immune response, moving beyond simple antibody titers [91].
- Assay Configuration: A suite of ligand binding assays is configured to measure a comprehensive panel of antibody features from serum or plasma.
- Immunoglobulin Profiling: Use an Fc-binding protein array to quantify antigen-specific levels of total IgG, IgM, IgA, and their subclasses (IgG1-4, IgA1-2) [91].
- Fc Receptor Binding: Measure the ability of antigen-specific antibodies to bind to various activating and inhibitory Fc gamma receptors (FcγRIIA, FcγRIIB, FcγRIIIA, FcγRIIIB), as well as FcRn and FcAR [91].
- Functional Effector Assays: Quantify the capacity of antibodies to recruit innate immune effector functions, including:
- Antibody-Dependent Cellular Phagocytosis (ADCP) using THP-1 cells or monocyte-derived dendritic cells (ADDCP).
- Antibody-Dependent Neutrophil Phagocytosis (ADNP).
- Antibody-Dependent Complement Deposition (ADCD).
- Antibody-Dependent NK Cell Activation (ADNKA) [91].
- Data Integration and Analysis: The data from the ~24 different antibody features are integrated. Univariate analysis highlights robust responses in different groups (e.g., by adjuvant), and multivariate statistical analyses (e.g., dimensionality reduction) are used to identify clusters of features that distinguish between groups and define unique immune signatures [91].
Visualizing Workflows and Logical Relationships
Assay Selection Decision Pathway
Systems Serology Analytical Workflow
Essential Research Reagent Solutions
The table below details key reagents and materials essential for conducting the serological assays discussed, particularly the complex analyses.
Table 2: Key Research Reagent Solutions for Serological Assays
| Reagent/Material | Function in Assay | Application Context |
|---|---|---|
| Recombinant Antigens | The target molecule immobilized on a plate or bead to capture specific antibodies from a sample [90] | Foundational for both simple and complex serological assays |
| Fc Receptor Proteins | Recombinant proteins used to measure the ability of antibodies to engage innate immune cells [91] | Critical for complex systems serology profiles |
| Reference Standards | Calibrated samples (e.g., international standards) used to normalize quantifications across labs and time [95] [92] | Vital for improving inter-laboratory reproducibility |
| Viability/Cell Fitness Kits | Assays to measure metabolic activity and early apoptosis (beyond simple permeability stains) in cell-based functional assays [93] | Essential for reliable ADCP, ADNP, and other cellular assays |
| Multiplex Bead Arrays | Microspheres with distinct spectral addresses to simultaneously measure multiple antibody features in a single sample [91] | Enables high-information-density complex analyses |
The choice between simpler metrics and complex serological analyses is not a matter of selecting the objectively superior method, but rather the appropriate tool for the research question and context. Simpler assays provide an efficient, high-throughput, and cost-effective means for large-scale epidemiological studies and diagnostics where a primary, binary outcome is sufficient [90] [92]. Their primary challenge lies in ensuring reproducibility across laboratories, as variations in methods and reagents can lead to statistically significant and clinically relevant differences [10]. Complex serological analyses offer an unparalleled depth of biological insight, revealing functional immune signatures that simple titers cannot capture, as demonstrated in adjuvant studies [91]. Their adoption, however, demands rigorous standardization, careful attention to cell fitness [93], and sophisticated data analysis pipelines. The ongoing development of innovative technologies, such as immunoaffinity proteomics and improved multiplex platforms, promises to enhance the specificity, reproducibility, and depth of serological diagnostics, ultimately bridging the gap between these two paradigms [92]. A well-validated, fit-for-purpose assay, whether simple or complex, remains the cornerstone of reproducible immunological research.
Leveraging Open-Access Data Repositories for Cross-Validation and Meta-Analysis
The evaluation of reproducibility in immunological assays across different laboratories presents a significant challenge in biomedical research. Inconsistent results can stem from multiple sources, including pre-analytical variables, reagent quality, and differences in data analysis protocols. A core issue is the antibody characterization crisis, where an estimated 50% of commercial antibodies fail to meet basic characterization standards, contributing to financial losses of $0.4–1.8 billion annually in the United States alone and generating unreliable data in numerous publications [5]. This problem is compounded by inadequate control experiments in many studies and insufficient understanding among researchers about how data quality depends on properly validated reagents.
Open-access data repositories offer a powerful solution to these challenges by enabling cross-validation and meta-analysis approaches. These resources allow researchers to test findings across diverse populations, methodologies, and experimental conditions, thereby strengthening the evidence for any discovered biomarker or biological relationship. When datasets are generated using different antibodies, assays, or platforms, cross-dataset validation provides a robust mechanism for verifying results and assessing their generalizability beyond a single laboratory's methodology.
The Value of Data Repositories for Cross-Validation
Documented Disparities in Major Repositories
Comparative analyses between large-scale data repositories reveal substantial variations that highlight the importance of cross-validation. A 2024 study comparing the All of Us (AoU) medical database and BigMouth dental repository found striking differences in reported health metrics across similar demographic groups [96]:
Table 1: Documented Variations Between All of Us and BigMouth Repositories
| Metric | Demographic Group | All of Us | BigMouth |
|---|---|---|---|
| Alcohol use | Hispanic/Latino | 80.6% | 16.8% |
| Alcohol use | Female | 87.9% | 26.0% |
| Diabetes prevalence | Female | 8.8% | 21.6% |
| Health literacy | Hispanic/Latino | 49.2% | 3.2% |
| Satisfactory health status | Hispanic/Latino | 70.1% | 98.3% |
These substantial disparities likely result from different recruitment approaches, participant demographics, and healthcare access patterns among the populations sampled in each repository [96]. Such findings underscore that data from any single source may contain systematic biases, making cross-repository validation essential for establishing robust conclusions.
Standardized Meta-Analysis Frameworks
Dedicated computational tools have been developed specifically for cross-study meta-analysis of complex biological data. The SIAMCAT (Statistical Inference of Associations between Microbial Communities And host phenoTypes) machine learning toolbox enables robust meta-analysis of microbiome datasets while addressing common pitfalls in cross-study comparisons [97].
SIAMCAT implements specialized workflows to handle challenges inherent to meta-analysis, including:
- Data normalization methods adapted for compositional microbial data
- Confounder analysis to identify and account for technical and biological batch effects
- Control augmentation strategies to improve disease specificity of models transferred across studies
- Standardized performance evaluation using area under the receiver operating characteristic curve (AUROC)
This toolbox has demonstrated capability to reproduce findings from major meta-analyses of metagenomic datasets, generating models with similar accuracy (within 95% confidence intervals) across diverse studies [97].
Experimental Approaches for Cross-Repository Validation
Standardized Protocols for Dataset Comparison
The methodological framework for comparing the All of Us and BigMouth repositories provides a template for rigorous cross-repository validation [96]. The protocol involves several key stages:
Data Extraction and Harmonization
- Create isolated computational workspaces for analysis
- Build comparable cohorts using consistent demographic criteria
- Develop unified concept sets for variables of interest (e.g., tobacco use, diabetes status, health literacy)
- Apply consistent inclusion/exclusion criteria across datasets
- Harmonize variable definitions and response categories
Statistical Analysis
- Conduct descriptive statistics for all variables
- Perform bivariate analyses across demographic strata
- Calculate odds ratios with 95% confidence intervals
- Compute effect sizes using Cohen's D for significant comparisons
- Implement appropriate multiple testing corrections
This approach facilitates direct comparison of disease prevalence, health behaviors, and socioeconomic factors across repositories, enabling researchers to identify consistent patterns versus repository-specific findings.
Meta-Analysis of Crohn's Disease Microbiome Studies
SIAMCAT has been applied to conduct a meta-analysis of fecal shotgun metagenomic data from five independent studies of Crohn's disease, demonstrating a practical framework for cross-study validation [97]. The methodology includes:
Data Preprocessing
- Unified taxonomic profiling using standardized reference databases
- Unsupervised abundance and prevalence filtering
- Cross-study normalization to account for technical variation
Machine Learning Pipeline
- Non-parametric association testing (Wilcoxon test) with generalized fold change
- Multiple normalization methods suitable for sparse compositional data
- Cross-validation schemes that account for study-specific effects
- Regularized regression (LASSO, Elastic Net) and random forest algorithms
- Model interpretation and feature importance analysis
Performance Assessment
- Evaluation of within-study prediction accuracy
- Assessment of cross-study generalizability
- Control augmentation to improve disease specificity
- Confounder analysis to identify potential batch effects
This approach revealed that when naively transferred across studies, machine learning models lost both accuracy and disease specificity, highlighting the importance of specialized methods for cross-study validation [97].
Quality Assessment in Immunological Assays
Regulatory Frameworks and Quality Standards
Immunoassays used in clinical and research contexts must meet established quality standards, with regulatory frameworks providing specific performance requirements:
Table 2: Selected CLIA 2025 Proficiency Testing Criteria for Immunological Assays
| Analyte | Acceptance Criteria |
|---|---|
| IgA, IgG, IgM, IgE | Target value (TV) ± 20% |
| Complement C3 | TV ± 15% |
| Complement C4 | TV ± 5 mg/dL or ± 20% (greater) |
| C-reactive protein (high sensitivity) | TV ± 1 mg/L or ± 30% (greater) |
| Alpha-1-antitrypsin | TV ± 20% or positive/negative |
| Autoantibodies (ANA, ASO, RF) | TV ± 2 dilutions or positive/negative |
These standards provide benchmarks for assessing analytical performance across laboratories [98]. The Six-Sigma methodology offers another framework for evaluating assay quality, calculating sigma metrics as (TEa - bias)/CV, where TEa represents total allowable error, bias measures systematic error, and CV represents coefficient of variation [99]. Assays with sigma values ≥6 are considered "world-class," while those between 3-6 are "good," and values <3 are "unacceptable" [99].
Standardization Challenges for Immunodeficiency Testing
The diagnosis of inborn errors of immunity (IEI) faces particular challenges in assay standardization. Despite the importance of accurate diagnosis for patient care, several IEI-relevant immunoassays lack standardization, including standardized protocols, reference materials, and external quality assessment programs [100]. Well-established reference values remain undetermined, especially for pediatric populations where severe conditions often manifest.
Immunoassays present unique standardization challenges because they frequently assess heterogeneous molecules, such as serum polyclonal antibodies, that share characteristics but represent distinct analytes with individual features [100]. This complexity often necessitates parallel testing of healthy control samples, particularly problematic for young patients whose results are typically compared to adult reference ranges.
Visualizing Cross-Repository Validation Workflows
Meta-Analysis Pipeline for Microbiome Studies
Meta-Analysis Pipeline for Microbiome Studies - This workflow illustrates the SIAMCAT framework for cross-study meta-analysis of microbiome data, incorporating specialized steps for handling compositional data and confounder assessment [97].
Cross-Repository Data Harmonization Process
Cross-Repository Data Harmonization Process - This diagram outlines the workflow for comparing datasets across repositories like All of Us and BigMouth, highlighting the importance of standardized variable definitions and statistical approaches [96].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Cross-Repository Validation Studies
| Resource | Function | Application in Validation |
|---|---|---|
| SIAMCAT R Package | Machine learning toolbox for comparative metagenomics | Standardized meta-analysis of microbiome datasets across studies [97] |
| Open-Source Antibodies | Well-characterized antibodies with publicly available sequences | Improves reagent transparency and research reproducibility [101] |
| All of Us Researcher Workbench | Secure cloud-based analysis environment for multimodal data | Enables cross-domain validation (medical, behavioral, environmental) [96] |
| BigMouth Dental Repository | Integrated EHR data from dental schools | Facilitates oral-systemic health relationship studies [96] |
| PATH Biorepository | Open-access biological specimens | Provides reference materials for diagnostic validation [102] |
| Research Resource Identifiers (RRIDs) | Unique identifiers for research resources | Tracks reagent usage across studies and publications [5] |
Leveraging open-access data repositories for cross-validation and meta-analysis represents a powerful approach to addressing reproducibility challenges in immunological research. By implementing standardized workflows like those demonstrated in the SIAMCAT toolbox and following rigorous data harmonization protocols, researchers can distinguish robust biological signals from method-specific artifacts. The documented disparities between major repositories like All of Us and BigMouth highlight both the necessity and value of cross-repository validation approaches. As the field continues to grapple with the antibody characterization crisis and other sources of variability, the integration of diverse data sources through carefully designed meta-analyses will be essential for advancing reproducible immunology research and developing reliable diagnostic and therapeutic approaches.
Conclusion
Achieving robust reproducibility in immunological assays across laboratories is an attainable goal that demands a systematic approach encompassing standardized protocols, rigorous validation, and continuous collaboration. The key takeaways highlight the non-negotiable need for defined cell fitness criteria, the success of multi-institutional consortia in standardizing complex techniques like flow cytometry and multiplex immunofluorescence, and the critical role of context-specific validation. Future efforts must focus on developing and adopting certified reference materials, expanding the use of open-data platforms like ImmPort for broader validation, and integrating advanced computational tools for data analysis. By embracing these strategies, the immunology community can significantly enhance the reliability of preclinical data, accelerate the translation of biomarkers into clinical use, and ultimately improve the development of safer and more effective biologics and vaccines.
References
- 1. Interlaboratory comparison of a multiplex immunoassay that ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11018077/]
- 2. Methodological Validation and Inter-Laboratory ... [https://www.mdpi.com/1999-4915/16/10/1512]
- 3. PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278967/]
- 4. Validation of a multiplexed immunoassay for ... [https://www.nature.com/articles/s41541-024-01039-z]
- 5. Science Forum: Antibody characterization is critical to ... [https://elifesciences.org/articles/100211]
- 6. Challenges of reproducible AI in biomedical data science [https://pmc.ncbi.nlm.nih.gov/articles/PMC11724458/]
- 7. Sources of variability in Luminex bead-based cytokine ... [https://www.sciencedirect.com/science/article/abs/pii/S002217592400084X]
- 8. Immunoassay Methods - Assay Guidance Manual - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK92434/]
- 9. Six factors affecting reproducibility in life science research ... [https://www.nature.com/articles/d42473-019-00004-y]
- 10. Reproducibility of Immunological Tests Used To Assess ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC262428/]
- 11. Comparing and combining data from immune assays ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9790822/]
- 12. Certain Approaches to Understanding Sources of Bioassay ... [https://www.bioprocessintl.com/assays/certain-approaches-to-understanding-sources-of-bioassay-variability]
- 13. Understanding and managing sources of variability in cell ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/451/Understanding-and-managing-sources-of-variability-in-cell-measurements]
- 14. Immunogenicity in Clinical Practice and Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC7070797/]
- 15. Interlaboratory study to assess precision and ... [https://pubmed.ncbi.nlm.nih.gov/40517645/]
- 16. Reproducibility Assessment of Enzyme-Linked ... [https://www.mdpi.com/2076-393X/12/10/1108]
- 17. Understanding preclinical and clinical immunogenicity ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1151888/full]
- 18. Immunogenicity of Protein-based Therapeutics [https://www.fda.gov/vaccines-blood-biologics/science-research-biologics/immunogenicity-protein-based-therapeutics]
- 19. A Consortium for Analytic Standardization in ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11681772/]
- 20. Analysis of immunogenetics interlaboratory comparisons ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1268728/full]
- 21. International Collaborative Study to Compare Assays for ... [https://pubmed.ncbi.nlm.nih.gov/2390334/]
- 22. Comparison of influenza-specific neutralizing antibody ... [https://www.sciencedirect.com/science/article/pii/S0264410X20301419]
- 23. Enzyme-linked immunosorbent assay (ELISA) [https://www.immunology.org/public-information/bitesized-immunology/experimental-techniques/enzyme-linked-immunosorbent-assay]
- 24. Enzyme Linked Immunosorbent Assay - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK555922/]
- 25. Dendritic cell maturation assay for non-clinical ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1704045/full]
- 26. International Reproducibility Efforts in Clinical Flow ... [https://www.clinicallab.com/international-reproducibility-efforts-in-clinical-flow-cytometry-26666]
- 27. Evaluation of in vitro Assays to Assess the Modulation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.00601/full]
- 28. Safe and Reproducible Preparation of Functional Dendritic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4572908/]
- 29. The Design of a Multistage Monitoring Protocol for ... [https://www.mdpi.com/1422-0067/26/12/5444]
- 30. Standardization procedure for flow cytometry data ... [https://www.nature.com/articles/s41598-020-68468-3]
- 31. Conventional, High-Resolution and Imaging Flow Cytometry [https://www.mdpi.com/2227-9059/9/2/124]
- 32. Sample Preparation Tips for Accurate Flow Cytometry ... [https://www.labx.com/resources/sample-preparation-tips-for-accurate-flow-cytometry-results/5521]
- 33. Advanced immunophenotyping of lymphocyte and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1577206/full]
- 34. Ad hoc antibody modification of a validated flow cytometric ... [https://pubmed.ncbi.nlm.nih.gov/40952067/]
- 35. Flow Cytometry Core: Standard Operating Procedures [https://www.houstonmethodist.org/academic-institute/research/cores/flow-cytometry/standard-operating-procedures/]
- 36. Flow cytometry: rules for analyzers | Yale Research [https://research.yale.edu/flow-cytometry-rules-analyzers]
- 37. On-Demand: Standardizing Flow Cytometry [https://www.curiox.com/videos/standardizing-flow-cytometry/]
- 38. MAPPs assays for non-clinical immunogenicity risk ... [https://pubmed.ncbi.nlm.nih.gov/41142823/]
- 39. A customized affordable multiplexed immunofluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452037/]
- 40. SITC 2025 - Research Use Only (RUO) Validation of 'Off ... [https://dls.com/resources/sitc-2025-ruo-validation-of-off-the-shelf-mif-panels/]
- 41. A Framework for Multiplex Immunofluorescence Analysis [https://cellcarta.com/science-hub/mif-analysis-framework/]
- 42. Society for Immunotherapy of Cancer - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11749220/]
- 43. Multiplex Immunofluorescence and Multispectral Imaging [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2021.674747/full]
- 44. Multiparametric cellular and spatial organization in cancer ... [https://www.nature.com/articles/s41551-025-01475-9]
- 45. ROSIE: AI generation of multiplex immunofluorescence ... [https://www.nature.com/articles/s41467-025-62346-0]
- 46. Design and Validation of Multiplex Immunofluorescence ... [https://www.leicabiosystems.com/us/life-science-solutions/webinars/design-optimization-and-validation-of-multiplex-immunofluorescence-panels/]
- 47. Virtual multiplex immunofluorescence identifies lymphocyte ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547128/]
- 48. Top PBMC Suppliers for 2026: Fresh, Cryopreserved, and ... [https://cgt.global/top-pbmc-suppliers-for-2026-fresh-cryopreserved-and-gmp-grade-options-compared/]
- 49. CYTO 2025 Tutorials: Do you know your ABCs of PBMCs? ... [https://learning.isac-net.org/products/cyto-2025-tutorials-do-you-know-your-abcs-of-pbmcs-a-critical-evaluation-of-pre-analytical-variables]
- 50. Optimizing PBMC Viability and Recovery: Updated Best ... [https://cgt.global/pbmc-viability-and-recovery/]
- 51. Why Separate Peripheral Blood Mononuclear Cells [https://www.akadeum.com/blog/pbmc-isolation-methods-isolation-white-blood-cells/?srsltid=AfmBOoofRhip8z8KSbOBVJ7Yqcre9XjkYHdMFEQy5Pd2584oN6y7rTNd]
- 52. Evaluation of the viability and functionality of human ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1627973/full]
- 53. Frontiers | The effects of cryopreservation on PBMCs transcriptome... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1690316/full]
- 54. Stepwise Protocol for Efficient PBMC Extraction and ... [https://www.protocols.io/view/stepwise-protocol-for-efficient-pbmc-extraction-an-hb9jb2r4p.html]
- 55. Storage - PBMC & Controlled-Rate Freezing Cryopreservation [https://researchdonors.co.uk/2025/02/18/the-importance-of-cryopreservation-solutions-and-controlled-rate-freezing-in-pbmc-storage/]
- 56. Assessment and Comparison of Viability Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10872314/]
- 57. Apoptosis Assay Market Size Report, 2025 – 2034 [https://www.gminsights.com/industry-analysis/apoptosis-assay-market]
- 58. Apoptosis Assays Market Size, Share, Trends and Industry ... [https://www.consegicbusinessintelligence.com/apoptosis-assays-market]
- 59. Dynamic CYP2E1 expression and metabolic activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12176122/]
- 60. Top Cell Viability Assays Companies & How to Compare ... [https://www.linkedin.com/pulse/top-cell-viability-assays-companies-sxewf]
- 61. The quest for metabolic biomarkers of IVF outcomes [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1640807/full]
- 62. Antibody validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3891910/]
- 63. Lot-to-Lot Variance in Immunoassays—Causes, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10252387/]
- 64. Lot-to-Lot Variation - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6223607/]
- 65. Managing Reagent Lot to Lot Variability [https://myadlm.org/science-and-research/clinical-chemistry/clinical-chemistry-trainee-council/pearls-of-laboratory-medicine-in-english/2015/managing-reagent-lot-to-lot-variability]
- 66. Analysis of Reagent Lot-to-Lot Comparability Tests in Five ... [http://www.annclinlabsci.org/content/42/2/165.full]
- 67. Trust and Transparency Rule: How Scientists Choose ... [https://www.prnewswire.com/news-releases/trust-and-transparency-rule-how-scientists-choose-antibodies-in-2025-302581225.html]
- 68. Top Anti-NeuN Antibody Companies & How to Compare ... [https://www.linkedin.com/pulse/top-anti-neun-antibody-companies-how-compare-them-itahc/]
- 69. Reproducibility of immunological tests used to assess multiple ... [https://pubmed.ncbi.nlm.nih.gov/14607863/]
- 70. of Optimization conditions of Plasmodium falciparum... incubation [https://malariajournal.biomedcentral.com/articles/10.1186/s12936-018-2369-3]
- 71. Cross-laboratory evaluation of multiplex bead assays ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0201205]
- 72. Frontiers | Quantitative bead–based multiplex assay for simultaneous... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1587567/full]
- 73. Automation of flow cytometry data analysis with elastic ... [https://www.nature.com/articles/s41598-025-99118-1]
- 74. GateNet: A novel neural network architecture for automated ... [https://www.sciencedirect.com/science/article/pii/S0010482524009053]
- 75. Inter-laboratory comparison of a serum fibroblast growth ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1604456/full]
- 76. ICCS 2025 [https://cytometry.org/public-admin/mobile/show_presentation.php?abstractno=70]
- 77. B-Cell Populations in Focus: A New Flow Cytometry Assay ... [https://cellcarta.com/science-hub/bcell-flow-cytometry-autoimmune-research/]
- 78. 3 Customer Trends We're Watching in 2025 [https://www.dotmatics.com/blog/3-customer-trends-in-2025]
- 79. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 80. A Practical Guide to Immunoassay Method Validation [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2015.00179/full]
- 81. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 82. Analytical Method Development and Validation in ... [https://resolvemass.ca/analytical-method-development-and-validation-in-pharmaceuticals/]
- 83. 4.1. Repeatability, intermediate precision and reproducibility [https://sisu.ut.ee/lcms_method_validation/41-precision-trueness-accuracy/]
- 84. Cross-Validations in Regulated Bioanalysis [https://labs.iqvia.com/blog/cross-validations-in-regulated-bioanalysis]
- 85. Parallelism experiments to evaluate matrix effects ... [https://pubmed.ncbi.nlm.nih.gov/28737442/]
- 86. Understanding Biomarker Method Validation: Specificity & ... [https://www.linkedin.com/pulse/understanding-biomarker-method-validation-dm9qe]
- 87. Rapid immunoassays for diagnosis of heparin-induced ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0178289]
- 88. Understanding Assay Performance Metrics [https://indigobiosciences.com/understanding-assay-performance-metrics/]
- 89. Improved immunoassay sensitivity and specificity using ... [https://www.nature.com/articles/s41467-022-32796-x]
- 90. Serodynamics: A primer and synthetic review of methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11649536/]
- 91. Systems serology-based comparison of antibody effector ... [https://www.nature.com/articles/s41541-023-00613-1]
- 92. Redefining serological diagnostics with immunoaffinity ... [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-023-09431-y]
- 93. Improving Reliability of Immunological Assays by Defining ... [https://pubmed.ncbi.nlm.nih.gov/39248805/]
- 94. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 95. Assay Formats: Recommendation for Best Practices and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3933581/]
- 96. Comparing two large data repositories to understand the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11653124/]
- 97. Microbiome meta-analysis and cross-disease comparison ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02306-1]
- 98. 2025 CLIA Acceptance Limits for Proficiency Testing [https://www.westgard.com/clia-a-quality/quality-requirements/2024-clia-requirements.html]
- 99. The Evaluation of Analytical Performance of Immunoassay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6294088/]
- 100. A Critical Review on the Standardization and Quality ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.721289/full]
- 101. Open-source antibodies as a path to enhanced research ... [https://www.sciencedirect.com/science/article/pii/S1871678425000421]
- 102. From biorepositories to data repositories: Open-access ... [https://journals.plos.org/globalpublichealth/article?id=10.1371/journal.pgph.0002044]