Beyond Animal Models: How New Approach Methods (NAMs) Are Revolutionizing Immunology Research and Drug Development
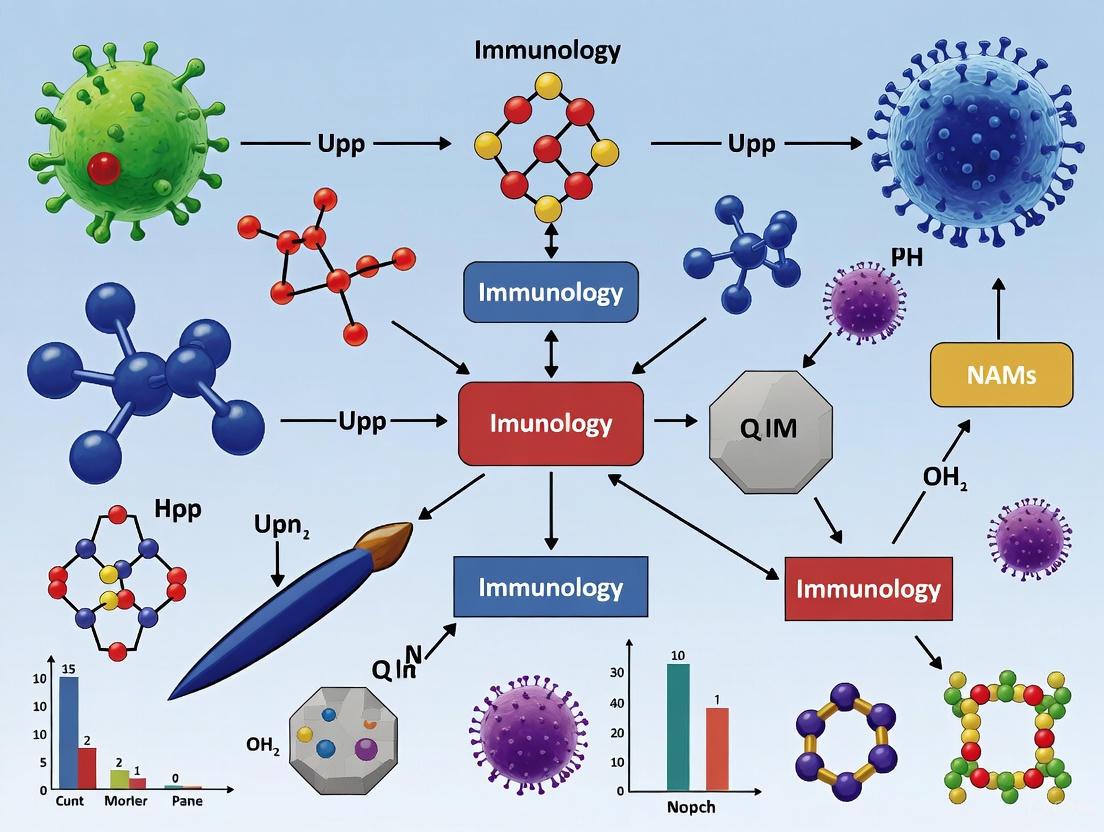
This article provides a comprehensive overview of the paradigm shift towards New Approach Methods (NAMs) in immunology.
Beyond Animal Models: How New Approach Methods (NAMs) Are Revolutionizing Immunology Research and Drug Development
Abstract
This article provides a comprehensive overview of the paradigm shift towards New Approach Methods (NAMs) in immunology. Driven by ethical imperatives, economic pressures, and the significant translational gap between animal studies and human clinical outcomes—often called the 'valley of death'—NAMs offer human-relevant alternatives. We explore the scientific and regulatory foundations of this movement, detail cutting-edge methodological applications from organ-on-chip systems to in silico modeling, address key challenges in implementation and optimization, and analyze pathways for regulatory validation. Designed for researchers, scientists, and drug development professionals, this resource synthesizes current initiatives from the FDA and NIH, showcases state-of-the-art technologies, and outlines a strategic framework for integrating NAMs into immunology research to enhance predictive accuracy and accelerate therapeutic discovery.
The Urgent Shift: Scientific and Regulatory Drivers for Adopting NAMs in Immunology
FAQs: Understanding the Translational Gap
What is the "Valley of Death" in translational immunology?
The "Valley of Death" refers to the critical gap where promising discoveries from laboratory research, often using animal models, fail to become effective human therapies [1]. In immunology, this is driven by the poor predictive value of traditional animal models for human immune responses, leading to a high failure rate of drugs in clinical trials [2] [3].
Why do animal models often fail to predict human immune responses?
Animal models, particularly rodents, have significant evolutionary divergences from human immunology. These include differences in immune cell subset heterogeneity, cytokine/chemokine biology, Toll-like receptor function, and vascular-immune cross-talk [3]. Approximately 1,600 immune-response genes in mice do not directly match their human equivalents, complicating the extrapolation of results [4].
What are New Approach Methods (NAMs) and how can they help?
New Approach Methods (NAMs) are non-animal, human-relevant research tools that include organ-on-chip systems, 3D organoids, advanced in silico modelling, and human-based immune cell cultures [2] [5]. These methods are driven by ethical, economic, and scientific motivations, and are designed to better mimic human physiology, thereby helping to bridge the translational gap [2].
Are there situations where animal models are still indispensable?
Yes, animal models remain valuable for studying complex, multi-organ immune processes that current NAMs cannot yet fully replicate. This includes investigating the dynamic cross-talk between a diseased tissue, peripheral blood, lymph nodes, and other organs, which is crucial for understanding overall immune response in areas like cancer immunotherapy [3].
Troubleshooting Guides: Addressing Common Experimental Challenges
Challenge 1: Poor Translational Outcomes in Preclinical Studies
Problem: Your therapeutic shows efficacy in animal models but fails in human trials.
| Recommended Action | Rationale | Specific Tools & Methods |
|---|---|---|
| Incorporate Humanized Models | Use THX mice or other advanced humanized mouse models that mount a more robust, human-like antibody response [4]. | THX mice: Created by injecting human stem cells; develop human lymph nodes, antibodies, and T/B cells [4]. |
| Adopt a Reverse Translation Approach | Start with human clinical data ("big data") to identify evolutionarily conserved immune phenotypes before testing in animals [3]. | Multi-omics profiling: Integrate transcriptomic, epigenomic, and proteomic data from human patients to guide animal model selection [6] [3]. |
| Integrate Organ-on-Chip Systems | Model human organ-level interactions and immune responses more accurately than in isolated animal tissues [4] [5]. | Multi-organ-on-chip (multi-OoC): Systems that replicate systemic immunological processes by integrating various human tissues and immune cells [2]. |
Challenge 2: Modeling the Complexity of Human Inflammatory Diseases
Problem: It is difficult to recapitulate the heterogeneity and progression of human inflammatory diseases (e.g., sepsis) in a controlled lab setting.
| Recommended Action | Rationale | Specific Tools & Methods |
|---|---|---|
| Refine Animal Models with Comorbidities | Standard, healthy animal models do not reflect the clinical reality of patients with underlying conditions [6]. | MQTiPSS Guidelines: Follow Minimum Quality Threshold in Pre-Clinical Sepsis Studies guidelines; incorporate chronic stress, diabetes, or other comorbidities into animal models [6]. |
| Use Human Ex Vivo Models | Leverage postmortem human tissues or advanced cell cultures that maintain native immune cell characteristics [2]. | Postmortem Tissue Studies: Viable human tissues can be used for immunological studies within 8-14 hours of death [2]. 3D Full-Thickness Skin Models: Immunocompetent models with integrated dendritic cells for studying inflammatory responses [2]. |
| Focus on Late-Acting Mediators | In diseases like sepsis, targeting early mediators like TNF has failed. Shift focus to later-acting mediators with wider therapeutic windows [6]. | Target HMGB1 & pCTS-L: These later-acting mediators offer a more promising therapeutic window than early cytokines like TNF [6]. |
Research Reagent Solutions
The following table details key reagents and models essential for modern, human-relevant immunology research.
| Reagent / Model | Function & Application | Key Feature |
|---|---|---|
| THX Mouse Model [4] | A humanized mouse model for vaccine research and studying human immune responses to pathogens like HIV and COVID-19. | Mounts a strong antibody response to mRNA vaccines; does not require complicated tissue engraftments. |
| Organ-on-Chip / Organoid Systems [4] | Miniature models of human organs (gut, liver, lung) for studying disease mechanisms and drug responses without animals. | Provides a more accurate model of human biology than animal models; endorsed by FDA and NIH for drug safety trials. |
| scRNA-seq with CITE-seq [4] | Single-cell RNA sequencing combined with protein surface marker detection to map immune cell types and functions in high resolution. | Uncover specific immune cell types (e.g., three main types of NK cells) and their roles in cancer and other diseases. |
| 3D Full-Thickness Skin Model [2] | An in vitro model with integrated dendritic cells for testing skin sensitization and inflammatory responses to compounds. | Effectively mimics immune responses to sensitizers and can be used to test anti-inflammatory compounds. |
| 24-Color Flow Cytometry Panel [2] | A high-throughput panel for comprehensive immunophenotyping of human peripheral blood cells to screen chemical effects. | Facilitates the identification of affected immune cell types and signaling pathways in response to stimuli. |
Experimental Protocols & Workflows
Protocol 1: Implementing a Reverse Translation Workflow
This protocol outlines a strategy to bridge the evolutionary gap between animal models and human immunology by starting with human data.
1. Generate Human Patient 'Big Data': Collect and integrate multi-omics data (transcriptomic, proteomic) from human patients with their clinical response variables [3]. 2. Computational Bridging: Use multi-dimensional computational approaches to identify evolutionarily conserved immune pathways and targets between humans and animal models [3]. 3. Tailored Animal Modeling: Select or create animal models (e.g., humanized mice, models with comorbidities) that most closely mirror the context of the human disease-immune cross-talk identified in Step 2 [6] [3]. 4. Forward Translation: Test novel immunotherapies or biomarkers in the tailored models before proceeding to human clinical trials [3].
Reverse Translation Workflow
Protocol 2: Developing an Immunocompetent Organ-on-Chip Model
This methodology details the creation of a microfluidic platform to model human vascular inflammation, a key process in many immune diseases [2].
1. Platform Setup: Use a scalable microfluidic platform with 64 parallel channels, each lined with human endothelial cells [2]. 2. Real-Time Measurement: Integrate a system for real-time measurement of endothelial barrier function via transendothelial electrical resistance (TEER) [2]. 3. Introduce Immune Stimuli: Apply cytokines or immune cells to the system to induce an inflammatory response [2]. 4. Monitor Key Parameters: Measure changes in barrier function, adhesion molecule expression (e.g., ICAM-1, VCAM-1), and immune cell migration in real-time [2]. 5. Drug Screening Application: Use the calibrated platform to screen potential anti-inflammatory drugs by assessing their ability to normalize the measured parameters [2].
Quantitative Limitations of Traditional Animal Models
| Limitation | Data / Evidence | Impact on Translation |
|---|---|---|
| Genetic Divergence | Over 1,600 immune-response genes in mice lack direct human equivalents [4]. | Poor prediction of drug efficacy and toxicity in humans. |
| Antibody Response | Most humanized mice fail to mount a strong antibody response to vaccines [4]. | Hampers vaccine and infectious disease research. |
| Species-Specific Biology | Fundamental differences in NK cell biology, T-cell repertoire, and cytokine networks exist [3]. | Mechanisms of action discovered in animals may not hold in humans. |
| Model Homogeneity | Animal models use genetically identical subjects with standardized insults, unlike heterogeneous human populations [6]. | Fails to predict treatment outcomes across diverse human patients. |
Comparison of Advanced Research Models
| Model | Key Advantage | Primary Application | Key Quantitative Finding |
|---|---|---|---|
| THX Mice [4] | Strong human-like antibody response. | Vaccine research, B-cell biology. | Mounted a strong immune response to an mRNA COVID-19 vaccine. |
| Organ-on-Chip (Vascular) [2] | Real-time monitoring of barrier function. | Vascular inflammation, drug screening. | Enabled real-time TEER measurement in 64 parallel microfluidic channels. |
| 3D Skin Model with DCs [2] | Mimics native tissue immune response. | Skin sensitization, toxicity testing. | Integrated dendritic cells responded to sensitizers by upregulating maturation markers. |
| Postmortem Tissue Studies [2] | Direct access to human tissue immune responses. | Tuberculosis, tissue-specific immunology. | Maintained cell viability for immunological studies up to 14 hours postmortem. |
Foundational Concepts: The 3Rs and New Approach Methodologies (NAMs)
What are the 3Rs? The 3Rs are a guiding principle for the ethical use of animals in science. Established over 65 years ago, they provide a framework for humane animal research [7]:
- Replace: Substituting animal use with non-animal systems like computer models, biochemical assays, or less-developed animal species.
- Reduce: Using the minimum number of animals necessary to achieve research objectives.
- Refine: Modifying procedures to eliminate or minimize pain and distress and to enhance animal well-being.
What are New Approach Methodologies (NAMs)? NAMs are innovative, human-relevant tools that do not rely solely on traditional animal testing [7] [8]. They are designed to provide more predictive data for human safety and efficacy. Key categories include:
- In chemico: Experiments on biological molecules (e.g., proteins, DNA) outside of cells.
- In silico: Experiments using computational platforms, including mathematical modeling, simulation, and artificial intelligence (AI).
- In vitro: Experiments on cells outside the body, including advanced models like organoids and organs-on-chips.
Frequently Asked Questions for the Practicing Scientist
Q1: We must provide animal data for regulatory submissions. Can we still use NAMs? Yes. Recent U.S. legislation and regulatory guidance actively encourage the use of NAMs. The FDA Modernization Act 2.0 (Dec 2022) removed the mandatory requirement for animal testing for drugs and explicitly defined "nonclinical tests" to include human biology-based methods like cell-based assays, microphysiological systems (MPS), and computer models [9] [10]. You are now authorized to submit data from these methods. Furthermore, the FDA's 2025 roadmap outlines a plan to phase out routine animal testing, making animal studies "the exception rather than the rule" [9] [10]. For specific contexts of use, engage with agency pilot programs like the FDA's ISTAND to qualify your novel drug development tool [9] [10].
Q2: Our complex immunology research involves systemic responses. Can NAMs truly replace animal models for this? For complex, multi-organ processes, a complete replacement is currently challenging. However, NAMs serve as powerful complementary tools. While some argue that whole living systems are still necessary to capture the complexity of interconnected organs [11], advanced Microphysiological Systems (MPS), such as multi-organ chips, are being developed to model interconnected human systems. A pragmatic approach is to use NAMs to reduce and refine animal use. For instance, use human-based in vitro models to prioritize the most promising drug candidates or to elucidate mechanistic pathways, thereby reducing the number of animals needed and refining the experiments that are ultimately conducted [8].
Q3: How do we validate a new NAM in our lab to ensure regulatory and scientific acceptance? Validation is a critical, multi-step process:
- Define a Clear Context of Use: Specify the exact purpose and application of your NAM.
- Generate Robust, Reproducible Data: Assess the method's reliability within your lab.
- Establish Human Relevance: Demonstrate that the NAM accurately predicts human biology or toxicology, for example, by using human primary cells or stem cell-derived tissues.
- Utilize Public Data Resources: Leverage tools like the Integrated Chemical Environment (ICE) to compare your results with existing reference data [7].
- Engage Early with Regulators: For drug development, consult with the FDA about the appropriateness of your NAM data for a specific application [8] [10].
- Seek Qualification Programs: Pursue formal qualification through pathways like the FDA's ISTAND pilot program, which accepted the first organ-on-a-chip (a Liver-Chip for DILI prediction) in 2024 [9].
Q4: What are the most immediate "low-hanging fruit" applications for NAMs in immunology? You can start integrating NAMs today in several areas:
- Early Safety Screening: Use high-throughput in vitro assays (e.g., from the Tox21 program) to screen for immunotoxicity or cytokine release syndrome risk, eliminating unsafe compounds before they ever reach an animal [7].
- Mechanistic Studies: Employ patient-derived organoids or immune cell-coated chips to study specific human immune pathways in a controlled environment.
- Disease Modeling: Utilize human peripheral blood mononuclear cells (PBMCs) or macrophages in 3D culture systems to model human-specific inflammatory diseases.
Q5: Our grant funding requires animal use. Are there funding opportunities for NAMs development? Yes, funding priorities are shifting significantly. The NIH Complement-ARIE program is a major initiative to speed the development and use of human-based NAMs [7]. Critically, as of July 2025, the NIH announced that proposals relying exclusively on animal data will no longer be eligible for agency support. Your grant applications must now integrate at least one validated human-relevant method [9].
Experimental Protocols: Integrating NAMs into Your Workflow
Protocol 1: Implementing a Human Liver-Chip for Preclinical Hepatotoxicity Screening
This protocol outlines how to integrate a microphysiological system to reduce animal use in drug safety testing.
- Objective: To predict drug-induced liver injury (DILI) using a human-relevant in vitro model prior to rodent or non-rodent studies.
- Background: A landmark study demonstrated that a human Liver-Chip showed 87% sensitivity and 100% specificity in predicting DILI for a set of drugs, outperforming animal models [9].
- Methodology:
- Cell Seeding: Seed a microfluidic chip with primary human hepatocytes, hepatic stellate cells, and Kupffer cells to recreate the liver sinusoid.
- Perfusion Culture: Maintain the chip under physiological fluid flow to provide shear stress and nutrient exchange.
- Dosing: Introduce the drug candidate into the perfusion medium at a range of clinically relevant concentrations.
- Endpoint Analysis:
- Biomarker Assays: Measure albumin, urea, and ALT/AST levels in the effluent daily.
- Immunofluorescence: Stain for tight junction proteins (ZO-1) and bile canaliculi to assess structural integrity.
- RNA Sequencing: Analyze transcriptomic changes to uncover mechanisms of toxicity.
- Integration with Animal Studies: Data from the Liver-Chip can be used to prioritize which drug candidates advance to in vivo studies and to inform dosing levels, reducing the number of animals required and refining the study design [9].
Protocol 2: An In Silico Workflow for Reducing Animal Use in Immunogenicity Risk Assessment
This protocol uses computational tools to reduce the need for animal immunogenicity studies.
- Objective: To predict the potential immunogenicity of a biologic drug candidate (e.g., a monoclonal antibody) using in silico tools.
- Background: AI/ML approaches can analyze complex datasets to identify sequences with a high risk of eliciting an anti-drug antibody (ADA) response.
- Methodology:
- Sequence Analysis: Input the protein sequence of the biologic into an in silico tool (e.g., from the CATMoS framework or similar platforms) to identify T-cell and B-cell epitopes that match common human HLA alleles [10].
- Aggregation Propensity Prediction: Use tools like TANGO or PASTA to predict regions prone to aggregation, as aggregates can increase immunogenicity.
- Glycosylation Pattern Analysis: Predict glycosylation sites and potential non-human glycan structures.
- Data Integration and Risk Scoring: Combine the outputs from the various in silico analyses to generate a composite immunogenicity risk score for the candidate molecule.
- Outcome: Candidates with a high predicted immunogenicity risk can be re-engineered or deprioritized before any in vivo immunogenicity studies are initiated in transgenic mice or other animal models, leading to a significant reduction in animal use.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 1: Essential Materials for Advanced In Vitro and In Silico Research
| Item | Function/Application | Example Use Case |
|---|---|---|
| Primary Human Cells | Provides human-relevant biological data; sourced from donors or stem cells. | Creating patient-specific disease models in organoids or chips [8]. |
| Organ-on-a-Chip (MPS) | Microfluidic devices that emulate human organ physiology and function. | Predicting drug-induced liver injury (DILI) with high accuracy [9]. |
| 3D Organoids | Miniature, simplified 3D tissue structures grown from stem cells. | Modeling human intestinal or lung tissue for infection or toxicity studies [7]. |
| AI/ML Analytics Software | Analyzes complex 'omics datasets and generates predictive models of toxicity or efficacy. | Building a model to prioritize chemicals for testing based on structural similarity [7] [8]. |
| High-Throughput Screening Assays | Allows for rapid testing of thousands of compounds using automated, cell-based systems. | Tox21 program screening of ~10,000 chemicals for biological activity [7]. |
Regulatory and Workflow Diagrams
Regulatory Paths: Traditional vs. NAMs-Integrated
NAM Development and Regulatory Ecosystem
The landscape of biomedical research is undergoing a fundamental transformation. Driven by the recognition that animal models often fail to predict human outcomes, major U.S. regulatory and research agencies are actively shifting the field toward human-relevant, non-animal methods [12] [13] [14]. This change is embodied in two pivotal initiatives: the U.S. Food and Drug Administration's (FDA) 2025 "Roadmap to Reducing Animal Testing" and the National Institutes of Health's (NIH) plan to establish the Office of Research Innovation, Validation, and Application (ORIVA) [12] [15] [14]. This technical support center is designed to help you, the researcher, navigate this transition by providing practical guidance on implementing New Approach Methodologies (NAMs) in your work, with a focus on immunology and drug development.
The Regulatory Framework
What are the key objectives of the FDA's 2025 Roadmap and NIH's ORIVA initiative?
The FDA's Roadmap and the NIH's ORIVA initiative represent a coordinated effort within the Department of Health and Human Services to reduce and eventually eliminate the reliance on animal testing in biomedical research and drug development [14].
FDA's 2025 Roadmap: This strategic document outlines a plan to phase out animal testing requirements, starting with monoclonal antibodies (mAbs) and eventually expanding to other biological molecules and new chemical entities [15] [14]. Its key objectives include:
- Promoting NAMs: Encouraging the use of advanced tools like organ-on-a-chip systems, computational modeling, and advanced in vitro assays for safety and efficacy evaluations [15] [14].
- Regulatory Incentives: Offering streamlined reviews and regulatory relief to sponsors who submit strong NAMs data [15] [16].
- Pilot Programs: Launching pilot programs allowing selected developers to use primarily non-animal-based testing strategies [15].
- Long-Term Vision: The FDA's stated goal is to make animal studies the exception, not the norm, within 3-5 years [17].
NIH's ORIVA Initiative: The new Office of Research Innovation, Validation, and Application (ORIVA) will coordinate NIH-wide efforts to integrate human-based science [12]. Its core functions are:
- Coordination: Serving as a hub for developing, validating, and scaling non-animal approaches across the NIH's research portfolio [12].
- Funding and Training: Expanding funding opportunities and training programs focused on NAMs [12].
- Bias Mitigation: Providing training for grant review staff to address potential bias towards animal studies and integrating experts on alternative methods into study sections [12].
What is the evidence supporting this shift away from animal models?
The regulatory shift is driven by significant scientific and economic evidence highlighting the limitations of animal models and the promise of human-based methods.
Table 1: Documented Limitations of Animal Models
| Category | Specific Example | Impact/Consequence |
|---|---|---|
| Safety Failures | Fialuridine: No significant toxicity in mice, rats, or dogs; caused fatal hepatic failure in humans [13]. | Late-stage clinical failure, patient harm. |
| Safety Failures | Troglitazone: Safe in animals; withdrawn from market due to human liver failure [13]. | Drug withdrawal, public health risk. |
| Safety Failures | Rofecoxib: No safety signals in animals; increased risk of heart attack and stroke in humans [13]. | Post-market safety issues. |
| Immunology Disconnect | TGN1412 mAb: Appeared safe in monkey studies; caused life-threatening cytokine release syndrome in humans [18] [17] [16]. | Clinical trial crisis, near-fatalities. |
| Immunology Disconnect | Ipilimumab: Minimal safety concerns in NHPs; highest incidence of immune-related adverse events among early immunotherapies in clinic [18]. | Poor prediction of human immune toxicity. |
| Efficacy Failures | Over 90% of drugs that appear safe/effective in animals fail in human trials due to lack of efficacy or unexpected safety issues [13] [14] [17]. | High R&D attrition, costing billions of dollars. |
Table 2: Quantitative Economic Impact of Traditional mAb Testing
| Metric | Traditional Animal-Centric Approach | Potential NAM Impact |
|---|---|---|
| Animal Use | ~144 non-human primates (NHPs) per program [17] [16]. | Significant reduction; goal to waive studies [17]. |
| Cost per Animal | Up to $50,000 per NHP [16]. | Reduced animal costs. |
| Timeline | Up to 9 years per therapeutic [17]. | Accelerated development. |
| Total Program Cost | \$650-\$750 million [17]. | Potential for significant reduction. |
Implementing NAMs: Core Technologies & Protocols
This section provides detailed methodologies for key NAMs relevant to immunology research.
FAQ: What are the core NAM technologies, and how do I choose?
New Approach Methodologies (NAMs) encompass a suite of human-based tools. Selecting the right one depends on your research question and the required context of use (COU) [18] [19].
Table 3: Core NAM Technologies and Their Applications
| Technology Category | Key Examples | Primary Research Applications |
|---|---|---|
| In Vitro Models | Organoids, Spheroids, Organ-on-a-Chip [12] [19] | Disease modeling (e.g., cancer, inflammatory conditions), capture patient-specific characteristics, toxicity screening [12] [17]. |
| In Silico Models | AI/ML predictive models, PBPK models, QSP models [12] [18] [19] | Predicting drug toxicity, pharmacokinetics, and human immunogenicity; simulating complex biological systems [15] [13]. |
| Omics Technologies | Transcriptomics, Proteomics, Metabolomics [19] | Mechanistic insights, biomarker discovery, pathway analysis aligned with Adverse Outcome Pathways (AOPs) [19]. |
| Integrated Strategies | IATA (Integrated Approaches to Testing and Assessment), ITS (Integrated Testing Strategies) [19] | Combining data from multiple NAMs (e.g., in vitro + in silico) for a weight-of-evidence safety assessment [19]. |
Experimental Protocol 1: Establishing a 3D Immune-Competent Organoid Co-culture for Cytokine Release Syndrome (CRS) Assessment
Background: This protocol is designed to model TGN1412-like cytokine release syndrome using a human-based system, providing a more predictive safety assessment than non-human primates [18] [17] [16].
Workflow Overview:
Step-by-Step Methodology:
Cell Sourcing and Preparation:
- Primary Human Immune Cells: Isolate peripheral blood mononuclear cells (PBMCs) from healthy donor blood using density gradient centrifugation (e.g., Ficoll-Paque). Alternatively, use cryopreserved PBMCs.
- Target Tissue Cells: Source human primary endothelial cells (e.g., HUVECs) or hepatocytes (for liver-chip models). Alternatively, use relevant human induced pluripotent stem cell (iPSC)-derived cell types [17] [16].
- Culture Media: Maintain cells in their respective optimized media prior to co-culture.
3D Matrix Embedding:
- Prepare a basement membrane matrix (e.g., Matrigel or a synthetic hydrogel) on ice.
- Mix the target tissue cells (endothelial/hepatocytes) with the matrix at a predetermined density.
- Plate the cell-matrix mixture in a 96-well plate or on the chip channel of an organ-on-a-chip device. Allow polymerization at 37°C for 30-60 minutes [17].
Co-culture Establishment:
- Gently add immune cells (PBMCs) in suspension to the top of the polymerized 3D structure or introduce them into the adjacent channel in a microfluidic device.
- Use a co-culture medium that supports both cell types. For microfluidic systems, initiate perfusion to mimic blood flow and enable immune cell recruitment [17] [19].
Compound Dosing:
- After a stabilization period (e.g., 24-48 hours), expose the co-culture to the therapeutic mAb or biologic.
- Include controls: a negative isotype control antibody and a positive control known to cause CRS (e.g., anti-CD28 superagonist).
- Test a range of concentrations relevant to predicted clinical exposure.
Assay and Analysis:
- Time Course Sampling: Collect supernatant from the culture at 0, 6, 24, and 48 hours post-dosing.
- Cytokine Profiling: Use a multiplex immunoassay (e.g., Luminex) to quantify a panel of pro-inflammatory cytokines (e.g., IL-6, IL-2, IFN-γ, TNF-α).
- Viability Assessment: At endpoint, perform a cell viability assay (e.g., Calcein-AM/EthD-1 live/dead staining) on the tissue cells.
- Imaging: Use confocal microscopy to visualize immune cell adhesion and infiltration into the tissue layer (using fluorescently labeled immune cells).
Experimental Protocol 2: Leveraging AI/ML and QSP Modeling for First-in-Human (FIH) Dose Prediction
Background: This in silico protocol integrates NAM-derived data with mechanistic modeling to inform FIH dose selection, reducing reliance on animal pharmacokinetic and pharmacodynamic studies [18].
Workflow Overview:
Step-by-Step Methodology:
Data Input and Curation:
- Internal NAM Data: Input data from in vitro assays, such as:
- Target affinity (e.g., KD from surface plasmon resonance).
- Cellular potency (e.g., EC50 from a cell-based reporter assay).
- Human hepatocyte data for clearance prediction.
- External/Public Data: Curate large-scale datasets for model training. This includes:
- Internal NAM Data: Input data from in vitro assays, such as:
AI/ML Model Training:
- Feature Engineering: Identify critical parameters influencing human PK/PD (e.g., molecular weight, charge, in vitro clearance, target expression).
- Model Selection: Train a machine learning model (e.g., gradient boosting or random forest) using data from approved therapeutics to predict human clearance, volume of distribution, and ultimately, clinical exposure profiles [18].
QSP Model Development:
- Build or adapt a existing QSP platform that mathematically represents the biological system relevant to your drug's mechanism (e.g., a T cell engager QSP model for a bispecific antibody).
- Calibrate the model using the in vitro NAM data (e.g., incorporating on-target effect and cytokine release data from Protocol 1) [18].
Model Integration and Simulation:
- Integrate the outputs of the AI/ML-predicted PK with the QSP model's PD components.
- Run thousands of virtual trials using the integrated model to simulate a range of dosing scenarios and predict efficacy and toxicity margins in a diverse virtual human population [18].
FIH Dose Recommendation:
- Based on the simulations, identify a safe starting dose (e.g., a dose expected to achieve 10% of the maximum effect with a high safety probability) and a dose-escalation scheme for the clinical trial [18].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Reagent Solutions for Human-Based Immunology NAMs
| Reagent/Material | Function/Application | Example & Notes |
|---|---|---|
| Primary Human Cells | Provide species-relevant biology; source for organoids and co-cultures. | PBMCs, primary hepatocytes, HUVECs. Use donor-matched sets for consistent results. iPSCs offer a scalable alternative [17]. |
| 3D Culture Matrices | Provide a physiologically relevant scaffold for 3D cell growth and signaling. | Basement membrane extracts (e.g., Matrigel), synthetic hydrogels (e.g., PEG-based). Select based on stiffness and composition for your tissue type [17]. |
| Specialized Culture Media | Support the complex metabolic needs of multi-cell type co-cultures. | Commercially available organoid media or custom formulations. Avoid serum to reduce variability. Include key cytokines for immune cell survival [17]. |
| Cytokine Detection Kits | Quantify immune activation and cytokine release syndrome (CRS) in response to therapeutics. | Multiplex bead-based immunoassays (e.g., Luminex). Essential for safety assessment of immunotherapies [16]. |
| Microfluidic Devices | Enable organ-on-a-chip cultures with perfusion, mechanical stress, and tissue-tissue interfaces. | Commercially available liver-chips, immune-chips. Recreate key aspects of human physiology not possible in static wells [17] [19] [16]. |
| AI/ML & Modeling Software | Analyze high-dimensional NAM data, build predictive models, and simulate human physiology. | PBPK platforms (e.g., GastroPlus, Simcyp), QSP software, and general data science tools (e.g., Python/R with ML libraries) [18] [19]. |
Troubleshooting Common NAMs Challenges
FAQ: My NAMs data is highly variable. How can I improve reproducibility?
Variability is a major challenge in early NAMs adoption. Standardization is key to regulatory acceptance [18] [13].
- Define a Clear Context of Use (COU): Early in development, precisely define what question the NAM is intended to answer. This focuses the model's complexity on clinically relevant outcomes and guides standardization efforts [18].
- Standardize Protocols: Use standardized, commercially available platforms where possible. For in-house protocols, document and rigorously adhere to detailed SOPs for cell sourcing, passage number, matrix lot, and media formulation [13] [17].
- Incorporate Robust Controls: Always include benchmark compounds (both positive and negative controls) in every experiment. This allows for cross-experiment and cross-laboratory data normalization and validation [18].
- Utilize Centralized Resources: Leverage new infrastructure like the NIH's $87 million Standardized Organoid Modeling (SOM) Center, which is specifically designed to address reproducibility by creating standardized protocols and models [17].
FAQ: How can I gain regulatory acceptance for NAMs data in my IND submission?
Engaging with regulators early and building a robust scientific rationale is critical.
- Engage Early via FDA INTERACT Meetings: For innovative programs, the FDA's INTERACT meeting provides informal, early feedback on your proposed use of NAMs, helping to align your strategy with regulatory expectations [20].
- Adopt a "Weight-of-Evidence" Approach: Regulators are more likely to accept NAMs data when it is part of an Integrated Testing Strategy (IATA). Combine data from multiple complementary NAMs (e.g., in vitro cytokine release + in silico PBPK/QSP modeling) to build a compelling case [18] [19].
- Generate Retrospective Validation Data: If possible, demonstrate that your NAM can correctly predict the clinical outcomes of known drugs (both safe and toxic). The Emulate Liver-Chip, for example, was validated by correctly identifying 87% of known hepatotoxic drugs [16].
- Participate in Pilot Programs: The FDA is actively seeking "pilot cases" where sponsors propose to waive animal studies based on strong NAM data. Volunteering for these programs provides a pathway for acceptance and helps shape future policy [15] [17].
FAQ: My NAM is complex but doesn't directly predict clinical doses. What should I do?
Rich mechanistic data from complex NAMs often needs translation to be clinically useful.
- Integrate with Mechanistic Models: Bridge the gap by feeding NAM outputs into Quantitative Systems Pharmacology (QSP) or Physiologically Based Pharmacokinetic (PBPK) models. For instance, in vitro efficacy data from an organoid can be used to parameterize a QSP model, which then simulates human dose-response relationships [18].
- Focus on Comparative Assessment: For next-in-class drugs, use your NAM to compare your candidate to a clinically approved benchmark. Demonstrating a comparable or improved safety/efficacy profile in the human-based system provides strong supportive evidence for your FIH dose strategy [18].
- Use for De-risking, Not Just Approval: Even if not used as a primary justification for a clinical dose, NAMs are powerful for internal decision-making. They can help prioritize the best candidate molecule, identify potential safety liabilities early, and guide clinical monitoring strategies [16].
FAQ: Troubleshooting Guide for Immunotoxicity Risk Assessment
Q1: Our therapeutic monoclonal antibody passed all standard in vitro and animal model safety tests. How can we better assess the risk of a "cytokine storm" in humans before first-in-human trials?
A: The TGN1412 tragedy demonstrated critical gaps in traditional testing. A modern, robust risk assessment should include the following troubleshooting steps and advanced protocols:
Problem: Standard cell suspension assays fail to detect superagonist activity.
- Solution: Implement a solid-phase assay where the therapeutic antibody is immobilized on a surface. Serendipitous research following the TGN1412 incident found that while the antibody caused no activation in liquid suspension, it provoked a massive cytokine release when coated onto plastic plates [21]. This mimics the cell-surface binding conditions more accurately.
Problem: Animal models do not predict human-specific immune responses.
- Solution: Utilize humanized in vitro systems. For TGN1412, a key difference was found in the expression of CD28 on CD4+ effector memory T-cells between humans and non-human primates, despite high sequence homology [22]. Prioritize tests on human peripheral blood mononuclear cells (PBMCs) or other human-derived immune cell cultures.
Problem: Inadequate characterization of cytokine release profile.
- Solution: Employ multiplex cytokine arrays to quantify a broad panel of pro- and anti-inflammatory cytokines. Research correlating with the TGN1412 disaster severity specifically identified the level of IL-2 release as a key differentiator from other mAbs [22]. Flow cytometry can further identify the specific immune cell subsets (e.g., Th1, Th2, Th17) responsible for cytokine production [22].
Q2: What are the critical New Approach Methodologies (NAMs) for de-risking immunomodulatory biologics?
A: The field of immunology is increasingly adopting human-relevant NAMs to bridge the translational gap. Key methodologies include [2]:
- Advanced In Vitro Models: 3D tissue models (e.g., full-thickness skin models with integrated immune cells), human organ-on-chip systems (e.g., microfluidic platforms for modeling vascular inflammation), and the use of primary human immune cells in defined co-cultures.
- In Silico Modeling: Mechanistic computational models, including agent-based models, to simulate complex immune responses and predict inflammatory cascades without using animals.
- High-Throughput Immunophenotyping: Comprehensive, multi-color flow cytometry panels (e.g., 24-color) for high-throughput screening of chemicals and biologics on human PBMCs to identify affected cell types and signaling pathways.
Experimental Protocols for Enhanced Preclinical Safety
Protocol: Solid-Phase T-Cell Activation Assay
This protocol is designed to detect the superagonistic activity of immunomodulatory antibodies, which may be missed in conventional assays [21] [22].
1. Key Research Reagent Solutions
| Item | Function |
|---|---|
| Human PBMCs | Source of primary human T-cells for a physiologically relevant response. Isolate from healthy donors. |
| Anti-CD28 mAb (Test Article) | The immunomodulatory agent being investigated (e.g., TGN1412). |
| Control mAbs | Include an isotype control (negative) and a known T-cell mitogen like anti-CD3 (positive). |
| 96-Well Plate | Solid surface for immobilizing the antibody. |
| Cytokine Multiplex Array | For quantifying a broad panel of cytokines (e.g., IFN-γ, TNF-α, IL-2, IL-4, IL-5, IL-6, IL-10, IL-17). |
| Flow Cytometer | For immunophenotyping activated T-cell subsets and intracellular cytokine staining. |
2. Methodology
- Step 1: Antibody Immobilization. Prepare the test and control antibodies in a suitable coating buffer. Add the solutions to the wells of a 96-well plate and incubate overnight at 4°C. Subsequently, block the plates with a protein-based buffer to prevent non-specific binding [21].
- Step 2: Cell Seeding and Stimulation. Isolate PBMCs from human donors. Seed the cells into the antibody-coated wells. Include control wells with cells only and mitogen-stimulated cells. Incubate for 24-48 hours at 37°C and 5% CO₂ [22].
- Step 3: Supernatant and Cell Harvesting. Carefully collect the supernatant from each well and store at -80°C for cytokine analysis. Harvest the cells for flow cytometric analysis.
- Step 4: Analysis.
- Cytokine Release: Use the multiplex array to measure cytokine concentrations in the supernatant. A significant release of IL-2, IFN-γ, and TNF-α is a major red flag for a potential "cytokine storm" [22].
- Immunophenotyping: Stain the cells for surface markers (e.g., CD4, CD8, CD25) and intracellular cytokines (e.g., IL-2) to identify the specific T-cell populations being activated.
Protocol: Cross-Species CD28 Expression and Function Analysis
This protocol assesses critical species-specific differences that may invalidate animal models for a particular drug candidate [23] [22].
1. Methodology
- Step 1: Cell Sourcing. Obtain PBMCs or purified T-cells from humans and relevant preclinical species (e.g., cynomolgus monkey, rhesus monkey).
- Step 2: Flow Cytometric Analysis. Stain cells with fluorescently labeled anti-CD28 antibodies and antibodies against T-cell subsets (e.g., CD4, CD8, CD45RO for memory T-cells). Analyze the percentage of CD28-positive cells and the receptor density (Mean Fluorescence Intensity) on different T-cell subsets, particularly CD4+ effector memory T-cells [22].
- Step 3: Functional Assay. Perform the solid-phase T-cell activation assay (as described in Protocol 2.1) in parallel using cells from each species. Compare the magnitude and profile of cytokine release.
2. Data Interpretation
- A negative or weak response in animal cells alongside a strong response in human cells indicates a critical species difference, as was the case with TGN1412. This finding should trigger extreme caution in extrapolating animal safety data to humans.
The following tables consolidate key quantitative findings from the TGN1412 case and related research.
Table 1: Comparison of TGN1412 Effects in Preclinical vs. Clinical Studies
| Parameter | Preclinical (Non-Human Primates) | Clinical (Human Volunteers) |
|---|---|---|
| Max Tolerated Dose | 50 mg/kg (NOAEL) [23] | Life-threatening at 0.1 mg/kg (500x lower) [23] |
| Primary Symptom | Well-tolerated, moderate cytokine increase [23] | Cytokine storm, multi-organ failure [24] |
| T-cell Response | Proliferation and expansion [23] | Severe and rapid depletion (lymphopenia) [24] |
| Key Cytokines | Moderate, transient increase in IL-2, IL-5, IL-6 [23] | Massive, rapid release of TNF-α, IFN-γ, IL-2, IL-6 [24] [22] |
| CD28+ Expression on CD4+ Effector Memory T-cells | Low or absent [22] | High [22] |
Table 2: Cytokine Release Profile of TGN1412 vs. Other mAbs in Solid-Phase Assay [22]
| Therapeutic mAb | IL-2 Release (pg/ml) | IFN-γ Release | Key T-cell Subsets Activated |
|---|---|---|---|
| TGN1412 | 2894 - 6051 | Significant | Th1, Th2, Th17, Th22 |
| Muromonab (OKT3) | 62 - 262 | Significant | Polyclonal T-cells |
| Alemtuzumab | Not Significant | Not Significant | - |
| Bevacizumab | Not Significant | Not Significant | - |
Visualizing the Mechanistic Failure and New Testing Paradigm
The diagram below illustrates the immunological mechanism behind the TGN1412 tragedy and how modern assays detect this risk.
The Scientist's Toolkit: Essential Reagents for Immunotoxicity Testing
Table 3: Key Research Reagent Solutions for Advanced Immunotoxicity Assessment
| Reagent / Material | Function in Assay |
|---|---|
| Human PBMCs from Multiple Donors | Provides a genetically diverse source of primary human immune cells for assessing inter-individual variability. |
| Cryopreserved Human Immune Cell Subsets | Enables specific study of isolated cell types (e.g., CD4+ T-cells, regulatory T-cells). |
| Recombinant Human Proteins & Antibodies | Positive and negative controls for assay validation (e.g., anti-CD3 for T-cell activation). |
| Multiplex Cytokine Detection Kits | Allows simultaneous, quantitative measurement of a wide array of cytokines from a small sample volume. |
| Flow Cytometry Panels (12+ colors) | Enables deep immunophenotyping of cell surface and intracellular markers to identify responding cell populations. |
| 3D Human Tissue Constructs | Provides a more physiologically relevant microenvironment for studying immune cell migration and function. |
| Microfluidic Organ-on-Chip Platforms | Models systemic immune responses and inter-organ communication in a human-relevant context [2]. |
The Unique Challenges of Modeling the Human Immune System for NAM Development
Troubleshooting Guides
Guide 1: Addressing Lack of Standardization in Human Immune NAMs
A primary hurdle in adopting New Approach Methodologies (NAMs) for immunology is the lack of standardized, reproducible protocols across different laboratories. The recent launch of the NIH's $87 million Standardized Organoid Modeling (SOM) Center directly addresses this by funding efforts to create robust, high-throughput platforms capable of delivering regulatory-ready data [17].
- Problem: High inter-laboratory variability in immune NAMs (e.g., organoids, organ-on-chip) due to non-standardized protocols.
- Symptoms: Inconsistent results between batches or labs; regulatory reluctance to accept data; difficulty comparing studies.
- Solution: Develop a clearly defined Context of Use (COU) for your NAM. The FDA encourages sponsors to propose specific cases, such as for monoclonal antibodies targeting human-specific receptors, where animal studies can be waived based on a strong scientific rationale and robust NAM data [17] [18].
- Preventative Steps:
- Utilize foundational models and shared decoders to align data types, as demonstrated in top-performing machine learning challenges for immunology [25].
- Implement a fit-for-purpose approach. Start with simpler, well-defined assays (e.g., 2D T-cell cytotoxicity assays) that have a clear path to regulatory acceptance for specific endpoints, before moving to more complex systems [18].
Guide 2: Incorporating Critical Immune Components
The 2025 Nobel Prize highlighted that immune tolerance is actively maintained by regulatory T cells (Tregs), not merely the absence of activation. This underscores the need for immune-competent models that capture such dynamic balances [26].
- Problem: Models lack key immune populations or interactions, failing to recapitulate essential processes like active tolerance or cytokine storms.
- Symptoms: Inability to predict immunotoxicity (e.g., drug-induced liver injury); poor translation of efficacy from model to human; missing key adverse events like cytokine release syndrome.
- Solution: Integrate immune components to model the full immune cycle. This can be achieved by:
- Example Protocol: Generating a 3D full-thickness skin model with integrated dendritic cells [2].
- Culture a full-thickness human skin equivalent.
- Incorporate dermal dendritic cell surrogates (e.g., derived from THP-1 cells) into the model.
- Apply the test compound (e.g., sensitizer) topically.
- Assay by measuring dendritic cell activation markers (e.g., CD86, CD54) via flow cytometry and cytokine secretion via ELISA.
Guide 3: Translating Complex NAM Data to Clinical Outcomes
A key strength of in vitro NAMs is generating human-relevant mechanistic data, but these rich datasets (e.g., transcriptomics, spatial imaging) are often difficult to correlate directly with clinical outcomes [18].
- Problem: Inability to translate high-dimensional NAM data (e.g., transcriptomic changes) into predictions for first-in-human (FIH) dose or safety margins.
- Symptoms: "Data-rich, but information-poor" outcomes; uncertainty in how NAM results inform clinical trial design.
- Solution: Integrate NAMs with computational modeling and AI.
- Leverage AI/ML: Use artificial intelligence to analyze deep phenotypic readouts from NAMs and anchor them to known clinical outcomes of benchmark drugs [18].
- Employ Mechanistic Models: Use Physiologically Based Pharmacokinetic (PBPK) models to extrapolate drug disposition from multi-organ-chip systems, or Quantitative Systems Pharmacology (QSP) models to translate in vitro efficacy/toxicity into clinical exposure predictions [17] [18].
The workflow below illustrates this integrated approach.
Frequently Asked Questions (FAQs)
Q1: My NAM is working perfectly in-house, but other labs can't reproduce my findings. What should I focus on? A1: Reproducibility issues often stem from a lack of standardized protocols. Focus on defining a precise Context of Use and documenting every aspect of your protocol, including cell source, culture conditions, and assay readouts. Engaging with initiatives like the NIH's SOM Center, which aims to create standardized organoid models, can provide valuable guidelines and resources [17] [18].
Q2: For a new immunotherapy target with no animal model, what's the best NAM-driven strategy to gain regulatory approval for a first-in-human trial? A2: Build a compelling weight-of-evidence package using multiple human-relevant NAMs. This should include:
- In vitro functional data from immune-competent 3D models demonstrating the intended mechanism of action and preliminary efficacy [27].
- Integration with in silico models (PBPK/QSP) to predict human pharmacokinetics and pharmacodynamics, informing first-in-human dosing [18].
- Leverage existing datasets (e.g., Human Protein Atlas) to validate target expression and safety profile in human tissues. The FDA has shown openness to such integrated approaches for justifying waivers for animal studies [17] [18].
Q3: How can I model complex systemic immune reactions, like a cytokine storm, in an in vitro system? A3: Use a human-based multi-organ-on-chip (multi-OoC) system that connects different tissue models (e.g., liver, immune, vascular) through microfluidic circulation. For example, an in vitro human liver chip integrated with immune cells can specifically evaluate and detect cytokine release syndrome far more accurately than non-human systems. These platforms are designed to replicate systemic immunological processes and can capture organ-organ crosstalk critical for such reactions [17] [2].
Q4: What are the biggest pitfalls when incorporating AI into my immunology NAM workflow, and how can I avoid them? A4: Key pitfalls include:
- Poor Quality Data: AI models are only as good as the data they're trained on. Ensure your NAM data is high-quality, well-annotated, and biologically relevant [28].
- Lack of Interpretability ("Black Box"): Regulators and scientists need to understand the AI's reasoning. Use methods like Retrieval-Augmented Generation (RAG) to integrate external knowledge sources and improve factual accuracy, or prioritize models that provide explanatory insights [29].
- Algorithmic Bias: Be aware that AI can inherit biases from its training data. Actively work to include diverse biological data (e.g., from donors of different ages, sexes, and ethnicities) to make your models more generalizable and equitable [27].
Data Presentation
Table 1: Quantifying the Translational Gap in Immunology Models
This table summarizes the documented limitations of traditional animal models and the corresponding capabilities of advanced NAMs.
| Challenge Area | Documented Limitation in Animal Models | NAM Capability & Advantage |
|---|---|---|
| Predictive Safety | Over 90% of drugs appearing safe in animals fail in human trials due to safety/effi cacy issues [17]. TGN1412 caused cytokine storm in humans after being safe in monkeys [17] [18]. | Human in vitro liver models with immune cells can better predict cytokine release syndrome [17]. |
| Species Specificity | Ipilimumab showed minimal safety concerns in NHPs but has high irAE incidence in humans. Pembrolizumab raised safety concerns in NHPs but has a favorable human profile [18]. | Use of human 3D immune-competent models (e.g., organoids) captures human-specific biology and cell responses [26] [27]. |
| Modeling Human Diversity | Animal models are often inbred, single-sex, and kept in sterile environments, failing to capture human population diversity [27]. | Biobanks of tissue from diverse donors (age, sex, ethnicity) used to create immune organoids preserve donor-specific immune responses [27]. |
Table 2: Research Reagent Solutions for Immune NAMs
Essential materials and tools for developing and analyzing sophisticated immunological New Approach Methodologies.
| Reagent / Tool | Function in Immune NAMs | Key Considerations |
|---|---|---|
| Primary Human Immune Cells (e.g., PBMCs, T cells, macrophages) | Provide a genetically and functionally diverse, human-relevant source of immune components for co-culture models [26] [2]. | Source from diverse donors to capture population variability. Use fresh or properly cryopreserved cells to maintain viability and function. |
| 3D Scaffolds & Matrices (e.g., MatriDerm, collagen-elastin) | Provide the structural and biochemical foundation for 3D tissue models (e.g., full-thickness skin, organoids) that support immune cell integration and function [2]. | Choose a matrix that supports cell viability, infiltration, and mimics the native tissue environment. |
| Flow Cytometry Panels (e.g., 24+ color panels) | Enable high-throughput, multiparametric immunophenotyping of complex co-cultures to identify multiple cell types and their activation states simultaneously [2]. | Panel design is critical. Requires careful fluorochrome selection and compensation controls to ensure data quality. |
| Spatial Transcriptomics Kits | Allow for mapping of gene expression within the context of tissue architecture in a NAM, revealing localized immune responses [25]. | Integration with histopathology images via AI can predict gene expression patterns, maximizing data from a single sample [25]. |
| AI/ML Modeling Platforms | Analyze high-dimensional NAM data (transcriptomics, imaging), predict immune responses, and generate hypotheses by integrating diverse datasets [28] [18] [29]. | Model interpretability and validation with robust biological datasets are essential for regulatory acceptance and scientific insight [29]. |
Experimental Protocols
Protocol 1: Establishing a Microfluidic Platform for Modeling Vascular Inflammation
This protocol, based on the work of Ehlers et al., enables real-time measurement of endothelial barrier function and immune cell migration in a high-throughput manner [2].
1. System Setup:
- Utilize a 64-channel parallel microfluidic platform.
- Seed human endothelial cells (e.g., HUVECs) into the microfluidic channels and culture until a confluent monolayer is formed. Monitor confluence and barrier integrity via Transendothelial Electrical Resistance (TEER).
2. Inflammation Induction & Immune Cell Recruitment:
- Introduce a pro-inflammatory cytokine (e.g., TNF-α, IL-1β) into the channels to activate the endothelium.
- In parallel, isolate primary human immune cells (e.g., PBMCs or monocytes) from blood and label them with a fluorescent cell tracker dye.
3. Real-Time Analysis:
- TEER Measurement: Continuously monitor TEER values across all channels to quantify the breakdown of the endothelial barrier in response to inflammation.
- Immune Cell Migration Assay: Perfuse the fluorescently labeled immune cells through the channels. Use live-cell imaging to track their adhesion to and migration through the endothelial layer.
- Endpoint Immunostaining: Fix the cells and stain for adhesion molecules (e.g., ICAM-1, VCAM-1) to confirm endothelial activation.
Protocol 2: Functional Assessment of a Peptide-Based Vaccine Candidate Using Dendritic Cells
This in vitro protocol, adapted from Lu et al., provides a method to screen vaccine immunogenicity before moving to animal studies [2].
1. Dendritic Cell Culture & Antigen Exposure:
- Culture the DC2.4 dendritic cell line or generate dendritic cells from primary human or mouse bone marrow precursors.
- Expose the dendritic cells to the peptide-based vaccine candidate. Include a known immunogenic peptide as a positive control and an untreated group as a negative control.
2. Measurement of Dendritic Cell Activation:
- Uptake Assay: Use a fluorescently tagged version of the peptide and measure internalization via flow cytometry or confocal microscopy after a set incubation period.
- Maturation Marker Analysis: After 24-48 hours, harvest cells and stain for surface maturation markers (e.g., CD80, CD86, MHC-II). Analyze using flow cytometry.
- Cytokine Secretion: Collect cell culture supernatant and measure the concentration of key cytokines (e.g., IL-12) using an ELISA kit.
3. T Cell Activation Assay:
- Co-culture the peptide-pulsed dendritic cells with naïve T cells isolated from a compatible donor.
- After several days, measure T cell proliferation (e.g., via CFSE dilution) and activation (e.g., via CD69 expression or IFN-γ release).
Next-Generation Tools: A Practical Guide to NAM Technologies for Immune System Modeling
The field of immunology is undergoing a transformative shift, moving away from traditional animal models toward more human-relevant New Approach Methodologies (NAMs). Microphysiological systems (MPS), commonly known as Organ-on-Chip (OoC) technology, represent a pivotal advancement in this transition. These microfluidic devices contain engineered or natural miniature tissues designed to replicate the functional units of human organs, providing unprecedented control over cellular microenvironments and enabling the maintenance of tissue-specific functions [30].
The incorporation of immune components is critical for bringing OoC models to the next level and enabling them to mimic complex biological responses to infection, disease, and therapeutic interventions [31]. As the scientific community acknowledges the limitations of animal models—including poor translatability to humans, low reproducibility rates, high costs, and ethical concerns—MPS offer a promising alternative that bridges the gap between conventional cell cultures and human physiology [32]. This technical resource center provides practical guidance for researchers navigating the implementation of immunocompetent MPS, with a specific focus on modeling immune cell recruitment and inflammatory processes.
Technical Support Center: FAQs and Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: Why should I use MPS instead of well-established animal models for immunology research? MPS offer several advantages for immunology research: they provide human-relevant data that often translates better to clinical outcomes than animal studies; they enable precise control over the cellular microenvironment; they allow for real-time, high-resolution imaging of immune processes; and they align with regulatory shifts toward NAMs. Notably, around 90% of drug trials pre-screened in animals fail in humans due to differences in drug efficacy and toxicity, highlighting the translational gap that MPS aim to bridge [32].
Q2: What are the key considerations when designing an MPS model to study immune cell recruitment? Successful modeling of immune cell recruitment requires recreating the multi-step extravasation cascade. Key considerations include: (1) Incorporating a functional endothelial barrier that expresses appropriate adhesion molecules (e.g., E-selectin, P-selectin, ICAM-1, VCAM-1); (2) Establishing a stable chemotactic gradient of cytokines or chemoattractants; (3) Applying physiological flow conditions to mediate cell rolling and adhesion; and (4) Including a 3D hydrogel-based extracellular matrix (ECM) to model the interstitial space through which immune cells migrate after transmigration [31].
Q3: Which immune cells are most commonly integrated into MPS, and what are the associated challenges? Innate immune cells (neutrophils, monocytes, macrophages) are most frequently integrated due to their central role in initial inflammatory responses and less complex activation requirements. Integrating adaptive immune cells (T cells, B cells) is more challenging because it often requires HLA-matching of all cell types in the system to prevent graft-versus-host-like reactions, which presents a significant cell-sourcing limitation [32].
Q4: My immune cells are not transmigrating effectively. What could be wrong? Ineffective transmigration can stem from several factors. Review the activation status of your endothelium—ensure it is properly activated with cytokines like TNF-α or IL-1β to upregulate adhesion molecules. Verify the integrity and stability of your chemokine gradient. Check the physiological relevance of your flow rates, as excessive shear stress can prevent cell arrest and adhesion. Finally, assess the composition and density of your hydrogel ECM, as an overly dense matrix can physically impede cell migration [31] [32].
Q5: Are there commercially available MPS platforms that support immunology research? Yes, several commercial platforms are widely used. The Emulate system (including Zoë-CM2 and the new AVA Emulation System) and the Mimetas OrganoPlate are both popular choices cited in recent research. The CN Bio PhysioMimix system is another validated platform. These systems offer various features, such as perfusion, imaging compatibility, and multi-organ capabilities, which can be leveraged for immune-focused studies [33] [34] [32].
Q6: What does the recent regulatory shift mean for my use of MPS in preclinical work? Recent regulatory changes significantly bolster the value of MPS data. The FDA Modernization Act 2.0 (2022) removed the mandatory requirement for animal testing for new drugs and explicitly recognized MPS as valid nonclinical test models. Furthermore, the FDA's 2025 roadmap outlines a plan to phase out routine animal testing, and the NIH now prioritizes funding for research that incorporates human-relevant methods like MPS. This means data from qualified MPS are not just acceptable but are increasingly expected by regulators [9].
Troubleshooting Common Experimental Issues
The table below outlines common problems, their potential causes, and recommended solutions when working with immunocompetent MPS.
Table 1: Troubleshooting Guide for Immunocompetent MPS Experiments
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Poor Immune Cell Recruitment | - Insufficient endothelial activation.- Unstable or weak chemotactic gradient.- Non-physiological flow rate (too high). | - Characterize expression of adhesion molecules (e.g., ICAM-1, VCAM-1) on endothelium after cytokine stimulation.- Use hydrogels or controlled perfusion to maintain gradient stability. Validate with dye tests.- Optimize flow rate to allow for immune cell rolling and arrest; typical venous shear stresses range from 0.5 to 5 dyne/cm² [31] [32]. |
| Loss of Tissue Barrier Integrity | - High shear stress damaging the cell layer.- Cytokine-induced barrier disruption.- Incorrect cell seeding density. | - Measure Transepithelial/Transendothelial Electrical Resistance (TEER) regularly to monitor barrier health.- Use perfusion systems that allow for ramping up flow gradually after barrier formation.- Perform functional permeability assays (e.g., with fluorescent dextran) to quantify integrity [35] [32]. |
| Low Viability of Primary Immune Cells | - Lack of necessary survival signals in media.- Shear-induced activation or damage.- Interaction with incompatible cell types (for adaptive cells). | - Supplement media with appropriate cytokines (e.g., GM-CSF for monocytes).- Introduce immune cells under low-flow or static conditions initially.- For T cell studies, use HLA-matched cell types from a single donor or iPSC source to prevent alloreactivity [32]. |
| High Background in Apical/Basal Sampling | - Cross-contamination between channels.- Non-specific binding to chip materials (e.g., PDMS). | - Verify the integrity of the separating membrane before seeding cells.- Pre-treat channels with blocking agents like BSA. Consider using non-PDMS, low-binding chips (e.g., Emulate's Chip-R1) for analyte collection [34]. |
| Difficulty Reproducing Complex Inflammation | - Lack of key resident immune cells (e.g., macrophages).- Failure to recapitulate tissue-specific pathophysiology. | - Pre-seed tissue-resident immune cells during the initial model establishment.- Incorporate patient-derived or disease-specific cells (e.g., from organoids) to build a more physiologically relevant model [35] [34]. |
Essential Experimental Protocols and Workflows
Protocol for Establishing a Basic Immune Cell Recruitment Assay
This protocol outlines the key steps for creating a simplified MPS model to study immune cell transmigration across an endothelial barrier, a foundational process in inflammation.
Table 2: Key Research Reagents for Immune Cell Recruitment Assays
| Reagent / Material | Function / Explanation | Example |
|---|---|---|
| Microfluidic Chip | Provides the scaffold with micro-channels for fluid flow and cell culture. Often features a porous membrane to separate compartments. | Mimetas OrganoPlate (3-lane channel), Emulate Chip-S1 [32]. |
| Endothelial Cells | Forms the vascular barrier that regulates immune cell transit. | Human Umbilical Vein Endothelial Cells (HUVECs), Primary Human Microvascular Endothelial Cells (HMVECs). |
| Extracellular Matrix (ECM) Hydrogel | Mimics the interstitial tissue space and basement membrane. Provides structural support and biochemical cues for cell migration. | Collagen I, Matrigel, Fibrin, or composite hydrogels [31] [35]. |
| Chemoattractant | Creates a chemical gradient that directs immune cell migration. | Chemokines (e.g., IL-8, CCL2, CXCL12), bacterial peptide (fMLP), or complement component (C5a). |
| Cytokine for Activation | Activates the endothelium to upregulate adhesion molecules. | Tumor Necrosis Factor-alpha (TNF-α) or Interleukin-1 beta (IL-1β), typically used at 1-100 ng/mL. |
| Immune Cells | The circulating cells being studied for recruitment. | Primary human neutrophils, monocytes, or conditionally immortalized cell lines. |
Workflow Steps:
- Chip Preparation and ECM Coating: Sterilize the chip (e.g., UV light). Prepare the ECM solution (e.g., collagen I) on ice and introduce it into the designated tissue or ECM channel. Allow it to polymerize at 37°C for 30-60 minutes [35].
- Endothelial Barrier Seeding: Trypsinize and resuspend endothelial cells at a high density (e.g., 10-20 million cells/mL). Seed the cell suspension into the vascular (bottom) channel. Let the cells adhere under static conditions for a period (e.g., 1-2 hours) before initiating a low flow to remove non-adherent cells.
- Barrier Maturation: Culture the chip under continuous perfusion with endothelial growth medium for 2-4 days to form a confluent, tight monolayer. Monitor barrier integrity via TEER or permeability assays if possible.
- Endothelial Activation: Introduce a pro-inflammatory cytokine (e.g., TNF-α at 10 ng/mL) into the vascular channel via the perfusion medium. Incubate for 4-24 hours to activate the endothelium and induce adhesion molecule expression.
- Establishing a Chemotactic Gradient: After activation, introduce a chemoattractant into the tissue compartment (opposite side of the membrane from the endothelium) or into the ECM hydrogel. This establishes a concentration gradient that will guide the immune cells.
- Immune Cell Introduction and Assay: Resuspend fluorescently labeled immune cells in cell culture medium without serum. Introduce the immune cell suspension into the vascular channel under a defined, physiological flow rate. Allow cells to interact with the endothelium for the desired timeframe.
- Imaging and Analysis: Fix the cells at the endpoint and stain for actin (e.g., Phalloidin), nuclei (e.g., Hoechst), and specific markers (e.g., CD45 for leukocytes). Use confocal microscopy to capture z-stacks. Quantify the number of adhered and transmigrated cells using image analysis software (e.g., ImageJ/Fiji) [31] [35].
The following diagram visualizes the core experimental setup and the biological process being modeled.
Visualizing the Immune Cell Extravasation Cascade
The process of immune cell migration from the vasculature into tissues, known as the extravasation cascade, is a multi-step process that can be effectively modeled in MPS. The following diagram details these key steps, which your MPS setup aims to replicate.
The Regulatory and Commercial Landscape for MPS
The drive to adopt MPS is strongly supported by a shifting regulatory and commercial environment. As noted in the troubleshooting section, the FDA Modernization Act 2.0 was a landmark change, legally recognizing MPS as valid tools for drug development [9]. This has been followed by concrete actions:
- The FDA's ISTAND pilot program accepted its first Organ-on-a-Chip (a Liver-Chip for predicting drug-induced liver injury) in September 2024, creating a formal pathway for qualifying these systems [9] [34].
- In April 2025, the FDA released a roadmap outlining a phased plan to reduce and eventually replace routine animal testing, prioritizing MPS data and AI-driven models [9].
- The NIH has shifted its funding priorities to favor grants that incorporate human-based technologies, and as of July 2025, it no longer funds proposals that rely exclusively on animal data [9] [36].
Commercially, the market offers robust platforms that simplify adoption. The Emulate AVA Emulation System launched in 2025 as a high-throughput 3-in-1 platform for running 96 chips in parallel, significantly expanding experimental scale [34]. CN Bio's PhysioMimix system is noted for its ease of use, PDMS-free consumables, and validated performance in single- and multi-organ configurations [33]. These advancements lower the barrier to entry, allowing researchers to focus on biology rather than device fabrication. When selecting a platform, consider factors such as throughput needs, compatibility with your desired readouts (e.g., imaging, -omics), and availability of validated protocols for your organ system of interest.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Core Concepts and Applications
Q1: How do PBPK modeling and Agent-Based Models (ABMs) directly contribute to the reduction of animal models in immunology research?
These in silico approaches create virtual populations and simulate complex biological interactions, reducing the need for animal studies. Their specific contributions are outlined in the table below.
| Method | Primary Contribution to Animal Model Reduction | Key Application Example |
|---|---|---|
| PBPK Modeling [37] [38] [39] | Predicts drug/vaccine pharmacokinetics (PK) in diverse human populations (pediatric, geriatric, pregnant) where animal data translation is poor and clinical trials are ethically challenging. | Simulating drug exposure in pediatric populations, avoiding unnecessary clinical trials or extensive animal testing in these sensitive groups [37] [39]. |
| Agent-Based Models (ABMs) [40] | Simulates complex, emergent interactions within the immune system (e.g., between cells, cytokines, antigens) to predict immunogenicity and efficacy, which is difficult to model in animals. | Predicting the immunogenicity of biological compounds and vaccines, such as simulating infection dynamics and host immune system interactions for COVID-19 [40]. |
| AI/ML Integration [41] [42] [43] | Analyzes large multimodal datasets to predict immune responses, toxicity, and identify vaccine targets, slashing the time and cost of preclinical animal research. | Using tools like AlphaFold for de novo vaccine antigen discovery and predicting biomolecular interactions to accelerate immunotherapeutic design [41]. |
Q2: What are the most common technical challenges and solutions when integrating PBPK models with AI for immunogenicity prediction?
Integrating PBPK with AI, while powerful, presents specific technical hurdles. The table below details common issues and recommended solutions.
| Technical Challenge | Underlying Cause | Troubleshooting & Solution Strategies |
|---|---|---|
| Parameter Uncertainty & Large Parameter Space [43] | PBPK models for complex entities like antibodies or nanoparticles require many parameters (e.g., blood flow, enzyme expression, binding constants) that are often unknown or vary widely. | Use AI/ML for parameter estimation and to reduce the complexity of the parameter space. Perform sensitivity analyses to identify the most critical parameters requiring precise estimation [43]. |
| Limited Data Availability [43] | A lack of high-quality, tissue-specific drug concentration data or human-relevant in vitro data for training AI models limits predictive accuracy. | Leverage AI to mine existing datasets and integrate Real-World Data (RWD). Use QSAR models informed by AI to predict parameters from a drug's physicochemical properties where data is scarce [37] [43]. |
| Model Validation & Regulatory Acceptance [44] | Concerns about the credibility of integrated models for regulatory decision-making beyond established areas like drug-drug interactions. | Adopt a "predict-learn-confirm" cycle. Follow regulatory guidance (e.g., FDA credibility assessment framework) and engage early with agencies like the EMA and FDA to align on model development and validation standards [39] [44]. |
Q3: What steps can be taken to validate an Agent-Based Model for vaccine immune response prediction when human data is scarce?
When human data is limited, a multi-faceted validation strategy is required.
- Utilize the Universal Immune System Simulator (UISS): Employ established platforms like UISS, which have been successfully applied to model various diseases and immune responses. Using a validated framework provides a solid foundation [40].
- Leverage All Available Preclinical Data: Calibrate and validate the ABM using high-quality, well-designed animal study data. Ensure the animal studies incorporate randomization, blinding, and proper power calculations to improve data reliability and translational value [41].
- Incorporate Human In Vitro Data: Integrate data from human-relevant New Approach Methodologies (NAMs) such as organoids or organs-on-chips. These systems provide direct human biological data for validating specific model components [12] [8].
- Perform Virtual Population Studies: Run the model across a wide range of virtual patients to ensure it can reproduce known population-level immunological outcomes and behaviors, even if individual-level data is missing [37].
Technical Troubleshooting
Q4: Our PBPK model predictions for a nanoparticle-based vaccine in geriatric populations do not match initial clinical data. What could be wrong?
This discrepancy often arises from failing to account for key physiological and biological changes in the elderly. Focus on these parameters:
- Verify Physiological Parameters: Ensure the virtual population accurately reflects age-dependent decreases in hepatic and renal function, which can impair clearance and prolong half-life [37].
- Check for Disease-Associated Changes: The geriatric population often has comorbidities. Confirm if the model accounts for specific disease states that may alter organ function or volume [38].
- Review Nanoparticle-Specific Processes: For nanoparticles, key processes like uptake by the mononuclear phagocytic system can show high inter-patient variability. Ensure your model's parameters for these processes are calibrated for age-related changes in immune function [43].
- Conduct Sensitivity Analysis: Perform a sensitivity analysis on all parameters related to geriatric physiology and nanoparticle disposition to identify which have the largest impact on your model's output and require refinement [39] [43].
Q5: An AI model trained on existing datasets for T-cell epitope prediction is performing poorly for a novel pathogen. How can this be addressed?
This is typically a problem of data bias or model applicability.
- Retrain with Pathogen-Specific Data: Fine-tune the model using any available, even if limited, experimental data specific to the novel pathogen. This helps the model adapt to the new biological context [41].
- Explore Alternative AI Architectures: If the current model is consistently wrong, consider using a different AI approach. For instance, for predicting protein-antibody complexes, tools like ZDOCK may sometimes provide more accurate docking orientation predictions than AlphaFold 3, which might not capture dynamic conformational changes during binding [41].
- Augment Training Data: Use data augmentation techniques or integrate multi-omics data (genomics, proteomics) to broaden the model's feature set and improve its generalizability [41] [8].
- Validate with In Vitro Models: Use patient-derived organoids or other NAMs to generate human-relevant data for key predictions, creating a feedback loop to retrain and improve the AI model [12] [8].
Essential Research Reagent Solutions
The table below lists key reagents, software, and technologies essential for implementing the in silico and AI-driven approaches discussed.
| Tool Name | Category | Primary Function in NAMs Research |
|---|---|---|
| GastroPlus [40] | PBPK Software Platform | Simulates and predicts the pharmacokinetics of drugs and formulations in various human populations. |
| Simcyp Simulator [40] | PBPK Software Platform | A widely accepted platform for PBPK modeling, particularly for evaluating drug-drug interactions and population variability. |
| PK-Sim [40] | PBPK Software Platform | An open-source tool for whole-body PBPK modeling, supporting the development and validation of models. |
| Universal Immune System Simulator (UISS) [40] | Agent-Based Model Platform | Models the immune system to predict the immunogenicity of vaccines and biological compounds. |
| AlphaFold [41] | AI/Structural Biology Tool | Predicts the 3D structure of proteins and biomolecular complexes to aid in antigen and antibody design. |
| Organoids [12] [8] | In Vitro NAM | Provides a 3D, patient-derived in vitro model to study human biology and validate in silico predictions. |
| Organ-on-a-Chip [12] [8] | In Vitro NAM | Microfluidic devices that emulate human organ physiology for more translatable efficacy and toxicity testing. |
Workflow and Signaling Pathway Visualizations
Diagram: AI-Augmented PBPK Model Development Workflow
Diagram: Integrated Workflow for Vaccine Immunogenicity Prediction
The field of immunology and drug development is undergoing a significant transformation, driven by a strategic shift toward human-relevant, predictive New Approach Methodologies (NAMs). This movement aims to Replace, Reduce, and Refine (the 3Rs) the use of animal models in research [7]. Advanced in vitro assays, particularly high-throughput flow cytometry and complex 3D tissue models, are at the forefront of this change. They provide more accurate human-specific data, overcome the limited predictive power of traditional animal models, and align with recent regulatory modernizations like the FDA Modernization Act 2.0, which explicitly recognizes microphysiological systems (MPS) as valid nonclinical test methods [9]. This technical support center is designed to help you implement these powerful technologies, troubleshoot common challenges, and contribute to the paradigm shift in biomedical research.
Troubleshooting Guides and FAQs
High-Throughput Flow Cytometry Panels
FAQ: What are the most common issues causing weak or no signal in my flow cytometry data?
Weak fluorescence signals can stem from multiple sources in the experimental workflow. The table below outlines common causes and their solutions.
| Problem Cause | Recommended Solution | Additional Notes |
|---|---|---|
| Insufficient Target Induction | Optimize treatment conditions; use fresh PBMCs over frozen when possible [45]. | Include appropriate controls: unstimulated, isotype, unstained, positive [45]. |
| Poor Fixation/Permeabilization | For intracellular targets, use appropriate protocol; add formaldehyde immediately post-treatment to inhibit phosphatases [45]. | Test extracellular epitope sensitivity to fixative; use ice-cold methanol for permeabilization [45]. |
| Dim Fluorochrome for Low-Density Target | Pair brightest fluorochrome (e.g., PE) with lowest density target (e.g., CD25) [45]. | Consider fluorochrome size/stability for intracellular staining [45]. |
| Incorrect Laser/PMT Settings | Ensure laser wavelength and PMT settings match fluorochrome excitation/emission spectra [45]. | Use calibration beads to check instrument performance [46]. |
| Instrument Clogging | Run 10% bleach for 5-10 min, followed by dH₂O for 5-10 min to unclog [45]. | Follow manufacturer's instructions [45]. |
FAQ: How can I resolve high background fluorescence and poor population separation?
High background can obscure your results and lead to inaccurate data interpretation. Key solutions are summarized below.
| Problem Cause | Recommended Solution |
|---|---|
| Fc Receptor-Mediated Binding | Block with BSA, Fc receptor blockers, or normal serum prior to staining [45]. |
| Presence of Dead Cells | Use a viability dye (e.g., PI, 7-AAD, fixable dyes) to gate out dead cells [45] [46]. |
| Excessive Antibody | Titrate antibodies to find the optimal concentration; avoid over-staining [45] [46]. |
| Autofluorescence | Use red-shifted fluorochromes (e.g., APC) or very bright fluorophores in problematic channels [45]. |
| Poor Compensation | Use bright, single-stained controls (cells or beads); ensure >5,000 positive events for control [46] [47]. |
| Tandem Dye Breakdown | Protect samples from light; fix samples promptly after staining; check tandem dye integrity [47]. |
FAQ: My compensation looks incorrect, with skewed populations and negative events. What should I do?
Incorrect spillover compensation is a common error manifesting as skewed signals and correlation (or anti-correlation) between channels [47].
- Diagnose the Cause: This often occurs due to differences between single-color controls and samples (e.g., fixation, staining duration, pipetting time), improper controls (e.g., using beads instead of cells), poor positive signal, or autofluorescence interference [47].
- Implement Fixes:
- For Future Experiments: Use better, cell-based single-color controls. Run Fluorescence-Minus-One (FMO) controls for critical markers. Acquire more events for controls to better define positive and negative populations [47].
- For Existing Data: Check your single-color controls and re-compensate using software tools. Compare your data to an FMO control if available. For spectral flow cytometry, check autofluorescence unmixing and consider using a targeted identification method [47].
- Avoid Manual Matrix Editing: Manually editing compensation matrices is generally not recommended, as it can introduce unseen errors in other dimensions of your data [47].
3D Immune-Competent Tissue Models
FAQ: Why are my 3D bioprinted constructs failing to yield a single-cell suspension for flow cytometry analysis?
A key challenge in analyzing 3D models is the gentle but complete dissolution of the scaffold to create a high-quality single-cell suspension.
- For Alginate-Based Bioinks: A validated protocol involves using a de-gelation solution containing sodium citrate to chelate the calcium ions cross-linking the alginate. After de-gelation, cells are fixed, permeabilized with ice-cold methanol, and can then be stained for flow cytometry [48].
- Optimization is Critical: The de-gelation process must be optimized for timing and agitation to maximize cell yield and viability while ensuring complete scaffold breakdown [48].
FAQ: My nanoparticle therapeutics work in 2D cultures but fail in 3D models. What are the potential barriers?
3D tissue models introduce extracellular barriers that are absent in traditional monolayer cultures, providing a more realistic prediction of in vivo performance [49].
- Hindered Diffusion: The extracellular matrix (ECM) in 3D models has restrictive pore sizes and high tortuosity. Studies using multicellular spheroids show nanoparticle penetration is significantly hindered for particles ≥ 100 nm [49].
- Binding Site Barriers: Vector surface charge affects distribution. Liposomes with high surface charge can be confined to outer cell layers due to non-specific binding to ECM components, demonstrating a "binding site barrier" [49].
- Cell Phenotype Differences: Cells in 3D cultures often regain more in vivo-like phenotypes, which can alter their response to therapeutics and exhibit multicellular drug resistances not seen in 2D [49].
FAQ: How can I design a better nanoparticle for delivery into 3D tissue models?
Insights from 3D culture systems can directly inform nanoparticle design.
- Size Matters: Design nanoparticles with diameters less than 100 nm for improved tissue penetration [49].
- Surface Chemistry: PEGylation (adding polyethylene glycol) can reduce non-specific binding to ECM components and increase diffusion rates [49].
- Particle Shape: Some studies suggest that extending nanoparticles into flexible, worm-like structures may allow for more effective tissue penetration compared to spherical carriers [49].
Experimental Workflows and Protocols
Workflow for Flow Cytometry Analysis of 3D Bioprinted Constructs
This workflow diagrams the key steps for preparing 3D bioprinted samples for flow analysis, based on a model using an alginate-based bioink [48].
Protocol: Dissolution and Staining of 3D Alginate Constructs
This protocol is adapted from a study using INS-1E cells in an alginate-based bioink [48].
- Post-Printing Cross-Linking: After printing the cell-laden bioink, cross-link the alginate scaffold using ionic gelation (e.g., with a calcium chloride solution).
- Dissolution (De-gelation): Incubate the 3D construct in a sodium citrate solution (e.g., 100 mM, pH 7.4) to chelate cross-linking ions and dissolve the scaffold. Gently agitate for a predetermined time (e.g., 10-15 minutes) to ensure complete de-gelation without damaging cells.
- Cell Harvesting: Centrifuge the cell suspension to pellet the cells and carefully remove the supernatant.
- Fixation: Resuspend the cell pellet in a fixation buffer (e.g., PBS supplemented with 3.6% formaldehyde) and incubate for a defined period [48].
- Permeabilization: Chill cells on ice. Permeabilize by adding ice-cold 90% methanol drop-wise to the cell pellet while gently vortexing to ensure homogeneous permeabilization and prevent hypotonic shock [45].
- Staining: Proceed with standard intracellular or cell surface staining protocols for flow cytometry. Include a viability dye to account for any cell death during the process.
Workflow for a Systematic Flow Cytometry Troubleshooting Approach
Adopt a methodical approach to diagnose and resolve flow cytometry issues efficiently.
The Scientist's Toolkit: Essential Research Reagents and Materials
| Item | Function/Application |
|---|---|
| Sodium Citrate Solution | Chelating agent for dissolving ionically cross-linked alginate scaffolds in 3D bioprinting (de-gelation) [48]. |
| Fixable Viability Dyes | Distinguish live from dead cells in fixed samples, crucial for gating and eliminating non-specific background [45] [46]. |
| Fc Receptor Blocking Reagent | Reduces non-specific antibody binding, lowering background fluorescence in flow cytometry [45] [46]. |
| Methanol (Ice-cold) | A vigorous permeabilization agent for intracellular staining, particularly suitable for nuclear antigens [45] [46]. |
| Compensation Beads | Antibody-capture beads used to create consistent and bright single-stain controls for accurate spillover compensation [46]. |
| CellTrace Violet | A fluorescent cell proliferation dye that dilutes with each cell division, used for tracking cell division in 3D cultures [48]. |
| Saponin / Triton X-100 | Detergents for mild cell permeabilization, used for intracellular staining of cytoplasmic or near-membrane targets [45] [46]. |
The field of immunology is undergoing a significant transformation with the advent of New Approach Methodologies (NAMs), defined as any technology, methodology, or approach that can replace, reduce, or refine the use of animals in research [50]. This shift is driven by ethical considerations and the critical need to bridge the translational gap between animal studies and human clinical trials—often referred to as the 'valley of death' [51]. Animal models often fail to accurately replicate the human immune system's complexity due to 90 million years of evolutionary divergence [51].
Immunology presents special challenges for traditional models due to the immune system's intricate complexity, spatial and temporal dynamics, genetic variability among individuals, involvement of multiple organs, and responsiveness to environmental factors [51]. Ex vivo human tissue models, particularly precision-cut tissue slices and tissues from postmortem donations, have emerged as powerful NAMs that preserve human tissue architecture, cellular diversity, and functional responses, offering more physiologically relevant platforms for studying human immunology and developing therapeutics.
Ex Vivo Tissue Slice Models
Precision-cut tissue slices (PCTS) are thin sections of fresh human tissue that maintain the original tissue architecture, stromal components, and cellular populations of the tumor microenvironment (TME) [52]. This ex vivo platform accurately recapitulates the high intratumoral complexity found in vivo and offers several advantages over traditional models:
- Preservation of native architecture: Retains the 3D structure, cell-to-cell interactions, and spatial relationships of the original tissue [53] [52]
- Maintenance of tumor microenvironment: Contains cancer cells, immune cells, endothelial cells, and stromal components in their natural configuration [52] [54]
- Rapid establishment: Can be quickly prepared from fresh tissue samples with limited cost [53]
- Patient-specific modeling: Enables study of individual patient responses to therapies [52]
Compared to other models, PCTS address significant limitations: 2D cell cultures lack 3D structure and cell-to-cell signaling; 3D spheroids lack tumor heterogeneity; patient-derived organoids (PDOs) lack the complete tumor microenvironment; and patient-derived xenograft (PDX) models are costly, time-consuming, and lack a human immune system [52].
Experimental Protocols for Tissue Slice Culture
Protocol for Precision-Cut Tumor Slice Generation and Culture
Tissue Acquisition and Preparation:
- Obtain fresh tumor tissue from surgical resection specimens, collected within 20 minutes of surgical removal [54]
- Place tissue in ice-cold transport medium (e.g., Hank's Balanced Salt Solution with Ca²⁺ and Mg²⁺, supplemented with antibiotics) [54]
- Sample tissue pieces of approximate dimensions 7×5×5 mm using sterile techniques [54]
Slice Generation:
- Fix tissue to a metal buffer tray with tissue adhesive and submerge in ice-cold transport medium [54]
- Cut 300-350 μm thick slices using a vibrating-blade microtome (vibratome) with settings: speed 0.05-0.15 mm/s; amplitude 1.30 mm [53] [54]
- Alternative instruments: Compresstome (reduces tissue damage and shearing, 5x faster than traditional vibratomes) [52]
- Transfer slices carefully with a thin brush to culture dishes [54]
Culture Conditions:
- Use CMRL 1066 medium supplemented with 2.5% human serum, HEPES, sodium pyruvate, insulin-transferrin-sodium selenite, and antibiotics [54]
- Rest slices on membrane inserts (0.4 μm pore size) in culture dishes with medium both below and above the slice to keep it submerged [54]
- Maintain cultures at 37°C in a humidified incubator with 41% oxygen tension to prevent hypoxia [54]
- Exchange culture medium every 24 hours with fresh pre-conditioned medium [54]
Viability Assessment:
- Maintain slices in culture for at least 4-5 days with preserved viability [54]
- Assess viability through morphological analysis, immunohistochemistry, and functional assays [54]
- For tumor slices, luminescence measurements can confirm maintained viability over 96 hours [53]
Research Reagent Solutions for Tissue Slice Cultures
Table: Essential Reagents for Ex Vivo Tissue Slice Culture
| Reagent/Category | Specific Examples | Function/Purpose |
|---|---|---|
| Transport Media | Hank's Balanced Salt Solution (HBSS) with Ca²⁺ and Mg²⁺, PBS, MACS tissue storage buffer, Belzer UW Cold Storage Solution | Maintain tissue viability during transport from surgery to laboratory [52] [54] |
| Culture Media | CMRL 1066 medium, DMEM | Base nutrients for tissue maintenance; CMRL 1066 shows better viability for pancreatic tissue [54] |
| Media Supplements | Human serum AB (2.5%), HEPES buffer, sodium pyruvate, insulin-transferrin-sodium selenite, zinc sulfate, diphenyl diselenide, antibiotics (PenStrep) | Provide essential growth factors, buffer pH, provide antioxidants, and prevent microbial contamination [54] |
| Viability Assays | Propidium iodide, ethidium homodimer, ATP measurements, immunohistochemistry (PCNA, Ki-67) | Assess and quantify tissue viability, cell death, and proliferation rates [53] [54] |
| Specialized Equipment | Vibratome (Leica VT1200S), Compresstome, membrane inserts (0.4μm pore size) | Generate precise tissue slices and provide support during culture [52] [54] |
Postmortem Tissue Donation for Immunological Research
Postmortem Tissue Donation Programs
Postmortem tissue donation, particularly through rapid autopsy programs, enables collection of comprehensive tissue samples from multiple metastatic sites promptly after death, providing invaluable resources for studying advanced disease states [55]. These programs address the critical limitation of sample availability for metastatic cancer research, where single biopsies cannot capture the full spectrum of intra-patient tumor heterogeneity [55].
Key initiatives include:
- UPTIDER Program: A breast cancer post-mortem tissue donation program that samples a median of 31 metastases (range: 5-90) and 5-8 liquid biopsies per patient [55]
- Gift from a Child: Focuses on pediatric brain tumor donations, with tissue going to the Children's Brain Tumor Network, the world's largest pediatric brain tumor biorepository [56]
- Brain Donor Project: Facilitates brain tissue donation for neurological research [56]
These programs have demonstrated that RNA quality and transcriptional profiles remain stable with increasing time after death, especially when organs are cooled, making postmortem tissues suitable for various molecular and immunological studies [55].
Experimental Protocols for Postmortem Tissue Studies
Protocol for Rapid Autopsy and Tissue Processing
Program Setup and Logistics:
- Establish a multidisciplinary team including clinical oncologists, pathologists, forensic medicine specialists, and palliative care teams [55]
- Develop electronic case report forms (eCRF) and laboratory information management systems (LIMS) for sample tracking [55]
- Secure 24/7 transport services for patients passing away at home or in hospice [55]
- Install necessary processing infrastructure (centrifuges, -80°C freezers) in the morgue [55]
Patient Consent and Pre-mortem Preparation:
- Approach patients with metastatic disease during later lines of treatment using the term "tissue donation program" rather than "autopsy" to improve acceptance [55]
- Obtain written informed consent prior to death [56]
- Perform inclusion sampling of easy-access liquid biopsies (blood, urine, saliva) when possible [55]
- Prepare a patient-specific "tissue donation plan" based on latest imaging and research interests [55]
Postmortem Procedures:
- Notify the research team immediately upon patient death (ideally within 1 hour) [56]
- Transport the body to the processing facility with minimal delay [55]
- If feasible, perform whole-body MRI before autopsy to guide sampling [55]
- Collect all body fluid types first, storing as supernatant aliquots and cell pellets [55]
- Examine organs in patient-specific order, sampling all identified metastases and selected non-tumor tissues [55]
- Process samples for multiple downstream analyses (fresh frozen, formalin-fixed, organoid generation) [55]
Timeline Considerations:
- Complete autopsy and tissue processing within 8 hours of death while maintaining cell viability for up to 14 hours [51]
- Most researchers prefer tissue donated within 24 hours, though timing flexibility accommodates family needs [56]
Research Reagent Solutions for Postmortem Studies
Table: Essential Reagents for Postmortem Tissue Research
| Reagent/Category | Specific Examples | Function/Purpose |
|---|---|---|
| Sample Registration | LabCollector-based platforms, REDCap electronic case report forms (eCRF), barcode/QR code systems | Manage patient data and track hundreds of samples per autopsy with unique identifiers [55] |
| Liquid Biopsy Processing | EDTA blood collection tubes, sterile urine containers, saliva collection kits | Collect and process liquid biopsies for circulating tumor cells, cell-free DNA, and other biomarkers [55] |
| Nucleic Acid Preservation | RNAlater, PAXgene Tissue systems, TRIzol reagents | Preserve RNA and DNA integrity for genomic, transcriptomic, and epigenomic analyses [55] |
| Cell Culture Models | Matrigel, specialized organoid media, basement membrane matrices | Generate ex vivo models including organoids and cell lines from donated tissues [56] [55] |
| Histology & Imaging | Formalin, paraffin, hematoxylin and eosin (H&E) stains, immunohistochemistry antibodies | Process tissue for pathological evaluation and spatial analysis of immune cells [54] [55] |
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions
Q: What is the maximum time window for collecting viable tissue after death? A: Studies show that tissue viability can be maintained for up to 14 hours postmortem, with optimal results when autopsies are completed within 8 hours of death [51]. RNA quality and protein expression remain stable with increasing time after death, particularly when organs are cooled promptly [55].
Q: Does brain tissue donation interfere with funeral arrangements? A: In most cases, no. The donation procedure is performed from the back of the head to prevent disfigurement, allowing for open casket viewings. The brain bank coordinates with the funeral home to ensure arrangements proceed as planned [56].
Q: Can patients donate both organs for transplantation and tissues for research? A: In some cases, yes. Recovery teams can coordinate so both donations can take place. However, patients with brain tumors may face challenges donating organs for transplantation [56].
Q: How does the oxygen tension affect tissue slice viability? A: Research on pancreatic ductal adenocarcinoma slices shows that cultures maintained at 41% oxygen tension better prevent hypoxia in the inner layers of slices, which lack blood circulation. However, comparative studies show viable cultures can also be maintained at 21% oxygen [54].
Q: What thickness is optimal for precision-cut tissue slices? A: Typical thickness ranges from 300-350 μm. Thicker slices better preserve tissue architecture but may develop necrotic cores due to limited nutrient diffusion. Thinner slices may compromise structural integrity [53] [54].
Q: Can ex vivo tissue slices be used to test immunotherapies? A: Yes, PCTS preserve the native tumor immune microenvironment, including T cells, macrophages, and other immune populations. This makes them suitable for testing various immunotherapies, including immune checkpoint inhibitors and CAR-T cell therapies [52].
Troubleshooting Common Experimental Issues
Table: Troubleshooting Guide for Ex Vivo Tissue Studies
| Problem | Potential Causes | Solutions |
|---|---|---|
| Poor tissue viability in slices | Extended time between resection and culture; improper storage; incorrect slicing technique | Transport tissue in ice-cold storage buffers; process within 1-2 hours of resection; optimize vibratome settings; use antioxidants in media [52] [54] |
| Necrotic centers in tissue slices | Slice too thick; insufficient oxygen tension; inadequate nutrient diffusion | Reduce slice thickness to 200-350 μm; increase oxygen tension to 41%; ensure medium contact on both sides of slice [54] |
| Low postmortem tissue donation acceptance | Terminology concerns; family objections; logistical barriers | Use "tissue donation program" instead of "autopsy"; train physicians in compassionate communication; arrange 24/7 transport services [55] |
| Inconsistent drug responses in slices | Heterogeneous tissue composition; variable slice thickness; poor compound penetration | Include multiple slices per condition; standardize slicing protocol; verify drug penetration with markers; extend treatment duration [53] [52] |
| Rapid deterioration of tissue architecture | Excessive mechanical stress during preparation; suboptimal culture conditions; microbial contamination | Use Compresstome instead of traditional vibratome to reduce shearing; validate culture medium composition; add antibiotics to media [52] [54] |
Comparative Analysis of Model Systems
Quantitative Comparison of Preclinical Models
Table: Comparison of Preclinical Models for Immunological Studies
| Model System | Preservation of Tumor Microenvironment | Time Required for Establishment | Cost Considerations | Immunocompetence | Key Advantages | Major Limitations |
|---|---|---|---|---|---|---|
| 2D Cell Cultures | None | Days | Low | None | Simple, scalable, high-throughput | Lacks 3D architecture and cellular interactions [52] |
| 3D Tumor Spheroids | Limited | Days | Low-moderate | None | 3D architecture, better drug resistance modeling | Lacks heterogeneous TME components [53] [52] |
| Patient-Derived Organoids (PDOs) | Partial (epithelial compartment only) | Weeks | Moderate | None | Patient-specific, retains some tumor heterogeneity | Lacks full TME including immune cells [52] |
| Patient-Derived Xenografts (PDX) | Partial (murgeonized stroma) | Months | High | None (immune-deficient mice) | In vivo context, maintains tumor histology | Costly, time-consuming, no human immune system [52] |
| Precision-Cut Tissue Slices (PCTS) | High (preserves native TME) | Hours-days | Low-moderate | Fully immunocompetent | Maintains architecture and immune cells, rapid setup | Limited lifespan (5-7 days), requires fresh tissue [53] [52] |
| Postmortem Tissues | High (complete native environment) | Hours (after death) | Variable | Fully immunocompetent | Access to multiple metastases, complete disease picture | Logistically challenging, limited time window [55] |
Visualization of Model Systems and Workflows
Comparative Advantages of Ex Vivo Models
Comparative Translation Potential of Research Models
Precision-Cut Tissue Slice Workflow
Precision-Cut Tissue Slice Experimental Workflow
Postmortem Tissue Donation Pathway
Postmortem Tissue Donation and Research Pathway
New Approach Methodologies (NAMs) are revolutionizing immunology research by providing innovative, human-relevant testing strategies that reduce reliance on animal models. These approaches include in vitro assays, microphysiological systems, and in silico modeling that collectively enable a more predictive assessment of human immune responses [57]. The drive toward NAMs stems from ethical considerations, economic factors, and the significant "translational gap" between results obtained in animal studies and clinical outcomes in humans [58] [59]. This technical support center provides comprehensive guidance for implementing integrated NAMs strategies to achieve a holistic view of immune function while advancing the critical goal of reducing animal use in immunology research.
Key In Vitro Immunization (IVI) Platforms: A Comparative Analysis
Several advanced IVI platforms have been developed to recapitulate the complexity of human immune responses. The table below compares three prominent systems used in immunology research.
Table 1: Comparison of Key In Vitro Immunization (IVI) Platforms
| Platform | Advantages | Limitations | Best Use Cases |
|---|---|---|---|
| Whole Blood Assay (WBA) | High number of viable immune cells; Presence of all immune cell populations; Low cost; Minimal sample processing [60] | Short shelf-life (must be used immediately); Low dendritic cell percentage (<1%); No spatial/temporal features of immune interactions [60] | Initial vaccine candidate screening; Cost-effective preliminary immunogenicity assessment |
| Monocyte-Derived DC with DC-T cell Interface (MoDC + DTI) | Cryopreservation capability; Conservation of DC phenotypic/functional characteristics; Incorporates temporal features of immune interactions [60] | Low throughput; Time-consuming (up to 10 days); Expensive compared to WBA; No spatial features of immune system [60] | Detailed analysis of antigen presentation and T-cell activation; Gold standard for balanced complexity and experimental control |
| Microphysiological Human Tissue Construct (HTC) | High physiological relevance with spatial/temporal immune interactions; DC differentiation without exogenous cytokines; Cryopreservation possible [60] | Very low throughput; Most expensive option; Time-consuming (10-11 days); High expertise required [60] | Advanced therapeutic development where human physiological relevance is critical |
Experimental Protocols for Key NAMs Platforms
Whole Blood Assay (WBA) Protocol
Methodology:
- Immune Cell Isolation: Collect fresh human whole blood using anticoagulant tubes (heparin or EDTA). Process immediately to maintain granulocyte functionality [60].
- Antigen Stimulation: Dilute whole blood 1:5-1:10 in appropriate cell culture medium. Add vaccine candidate or antigen at optimized concentrations. Include positive controls (e.g., LPS) and negative controls [60].
- Incubation: Culture for 24-48 hours at 37°C with 5% CO₂ based on desired readouts.
- Immune Response Readout: Collect supernatant for cytokine analysis (ELISA/MSD). Analyze cell pellets by flow cytometry for activation markers [60].
Technical Considerations: WBAs require minimal sample processing but have a short shelf-life and must be used immediately after collection [60].
MoDC + DTI Assay Protocol
Methodology:
- PBMC Isolation: Isolate PBMCs from whole blood via density gradient centrifugation. Cryopreserve if necessary for later use [60].
- MoDC Differentiation: Isolate CD14+ monocytes by magnetic sorting. Differentiate into immature MoDCs using GM-CSF and IL-4 for 5-7 days [60].
- Antigen Pulsing and Maturation: Pulse immature MoDCs with antigen for 4-24 hours. Add maturation stimulus (e.g., LPS) for final 24 hours [60].
- T Cell Co-culture: Isolate autologous T cells and co-culture with matured MoDCs at optimized ratios for 3-5 days [60].
- Readout: Measure T cell proliferation (CFSE dilution), cytokine production, and activation markers [60].
Technical Considerations: This 10-day protocol preserves autologous DC-T cell interactions but requires significant expertise and resources [60].
Troubleshooting Guides and FAQs
Common Technical Challenges and Solutions
Table 2: Troubleshooting Guide for NAMs in Immunology
| Problem | Potential Causes | Solutions |
|---|---|---|
| High variability between replicates | Inconsistent cell quality; Improper assay conditions; Donor variability | Implement strict QC for primary cells; Use standardized protocols; Consider donor pooling for screening [61] |
| Weak immune response | Suboptimal antigen concentration; Improper DC maturation; Low cell viability | Titrate antigens and adjuvants; Validate maturation markers; Check viability before assay [60] |
| Poor T cell activation | Insufficient co-stimulation; Inadequate antigen presentation; Wrong T cell:APC ratio | Verify expression of CD80/CD86 on DCs; Optimize antigen loading; Test different T cell:DC ratios [60] |
| Low data reproducibility | Unvalidated models; Equipment calibration issues; Inconsistent protocols | Implement model validation; Regular equipment calibration; Use detailed SOPs [61] |
Frequently Asked Questions
Q: How can I ensure my NAMs data will be acceptable for regulatory submissions? A: Engage with regulatory agencies early in development, use validated methods where available, and provide robust scientific data to support your approach. The FDA is increasingly encouraging inclusion of NAMs data in submissions, particularly for monoclonal antibodies and other biologics [57].
Q: What are the key validation requirements for NAMs in immunology? A: Demonstrate scientific validity, reliability, and relevance for your specific context. This includes biological relevance, sensitivity, specificity, and consistency across different test runs [61]. For regulatory use, consider Defined Approaches that combine multiple data sources with fixed interpretation procedures [59].
Q: How do I handle donor variability in human-based NAMs? A: Plan for sufficient donor replication (typically n=3-5 minimum), characterize donor demographics, and consider using cryopreserved PBMCs from characterized donors to maintain consistency across experiments [60].
Q: Can NAMs completely replace animal models in immunology research? A: While complete replacement remains a longer-term goal, NAMs already effectively replace specific tests and reduce animal use. Current strategies focus on using integrated NAMs approaches for screening and mechanistic studies, reserving animal models for later validation when necessary [59].
Signaling Pathways in Immune Activation
The diagram below illustrates the critical signaling pathway between dendritic cells and T cells that must be properly replicated in NAMs to generate physiologically relevant immune responses.
Diagram 1: Three-Signal Model of T Cell Activation. This pathway must be successfully replicated in NAMs to generate physiologically relevant immune responses [60].
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Immunology NAMs
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Source of human immune cells for in vitro assays | Can be cryopreserved; Maintain phenotypic/functional characteristics with proper handling [60] |
| Cell Culture Media | Support immune cell viability and function | Must be optimized for specific cell types; Include necessary cytokines and supplements [60] |
| Cryopreservation Medium | Long-term storage of primary cells | Enables flexibility in experimental timing; Maintain cell viability and function [60] |
| Cytokines/Growth Factors | Direct immune cell differentiation and function | Critical for DC maturation (GM-CSF, IL-4) and T cell polarization [60] |
| ELISpot/MSD Kits | Measure cytokine secretion at single-cell level | High sensitivity for detecting low-frequency responding cells [60] |
| Flow Cytometry Antibodies | Characterize immune cell phenotypes | Enable detailed immunophenotyping of multiple cell populations simultaneously [60] |
Integrated Experimental Workflow
The following diagram outlines a comprehensive workflow for implementing integrated NAMs strategies in immunology research.
Diagram 2: Integrated NAMs Workflow for Immunology Research. This strategic approach enables researchers to select the appropriate platform based on their specific research goals and resource constraints [60].
Integrated testing strategies combining multiple NAMs platforms offer a powerful approach to obtain a holistic view of immune responses while significantly reducing reliance on animal models. By strategically implementing WBA, MoDC-DTI, and HTC assays according to specific research needs, immunologists can generate more human-relevant data with improved predictive accuracy for clinical outcomes. The ongoing development and validation of these approaches, supported by regulatory agencies, continues to advance the field toward more ethical, efficient, and human-predictive immunology research.
Overcoming Implementation Hurdles: Strategies for Optimizing NAMs in Immunology Workflows
Frequently Asked Questions (FAQs)
FAQ 1: What are the main limitations of animal models in immunology that NAMs aim to address? Animal models, particularly rodents, often fail to accurately replicate the complexity of the human immune system due to ~90 million years of evolutionary divergence. This creates a significant "translational gap" or "valley of death" between animal studies and human clinical trials [51]. Key limitations include:
- Genetic and Functional Variability: The immune system exhibits significant individual variability, which is poorly captured by inbred animal strains [51].
- Differences in Immune Responses: The intricate interplay of innate and adaptive human immunity, with its specific spatial and temporal dynamics, is not fully replicated in animals [51].
- Ethical Considerations: Animal studies, especially infection challenges, often involve severe suffering, driving the need for more humane alternatives [51].
FAQ 2: How can I model the connection between innate and adaptive immunity in a human-based system? Incorporating dendritic cells (DCs) is crucial as they are professional antigen-presenting cells that bridge innate and adaptive immunity. One method involves generating functional, tissue-specific macrophages (derived from innate immunity) from a 3D culture of stromal vascular cells, which have been shown to mirror in vivo phenotypic and functional traits [51]. For initiating an adaptive response, DCs can be co-cultured with naive T cells. A detailed protocol for generating enhanced immunostimulatory dendritic cells from bone marrow using a specific cocktail of small molecule inhibitors (YPPP) is available, which has shown improved T cell activation capabilities [51].
FAQ 3: My in vitro immune model lacks physiological structure. What advanced platforms can provide a more tissue-relevant environment? 3D organoid and organ-on-chip (OoC) technologies are designed to address this exact issue.
- 3D Tissue Models: For skin immunology, full-thickness skin models incorporating dermal dendritic cell surrogates or peripheral blood-derived monocytes and T cells can effectively mimic immune responses to sensitizers and burn injuries [51].
- Multi-Organ-on-Chip (Multi-OoC): These systems integrate various human tissues (e.g., lung, skin, intestine) and immune components in a controlled environment to replicate systemic immunological processes and organ-level interactions [51]. A specific microfluidic platform also exists for modeling human vascular inflammation, allowing real-time measurement of endothelial barrier function and immune cell migration [51].
FAQ 4: How can I assess the diverse repertoire of T cell and B cell receptors in my human culture system? The field relies heavily on high-throughput sequencing and computational analysis.
- Method: Single-cell RNA sequencing (scRNA-seq) can be employed to profile the T cell receptor (TCR) and B cell receptor (BCR) repertoire from cells in your culture.
- Analysis: Specialized computational methods are available to analyze immune repertoire sequencing data. Tools like sciCSR can even use transcriptomic data to model B cell dynamics by predicting the direction of class-switch recombination [62].
FAQ 5: What in vitro methods can reduce animal use in vaccine potency and toxicity testing? Several New Approach Methods are being validated for this purpose.
- Vaccine Immunogenicity: An in vitro assay using the DC2.4 dendritic cell line to measure uptake, maturation, and cytokine production in response to peptide-based vaccine candidates has shown good correlation with in vivo results [51].
- Vaccine Toxicity: For Clostridium perfringens veterinary vaccines, a cell-based assay with THP-1 cells has been developed and validated as an alternative to mouse-based tests for toxicity assessment [51].
Troubleshooting Guides
Issue 1: Poor T Cell Activation in a Human 3D Co-culture Model
Problem: Antigen-presenting cells (APCs) in the co-culture are failing to robustly activate naive T cells.
Solution: Follow this systematic troubleshooting guide.
| Step | Checkpoint | Action & Recommendation |
|---|---|---|
| 1. APC Maturity | Confirm APCs are adequately mature. Immature DCs induce T cell tolerance. | Use a validated maturation stimulus (e.g., cytokine cocktail: TNF-α, IL-1β, PGE2). Check for surface expression of CD80, CD83, and CD86 via flow cytometry [63]. |
| 2. Antigen Load | Ensure antigen is present at an optimal concentration. | Titrate the antigen dose. Consider using a positive control like superantigen SEB to bypass the need for antigen processing/presentation. |
| 3. Co-stimulation | Verify the presence of co-stimulatory signals. | Ensure APCs express B7 family ligands. The interaction of CD28 on T cells with B7 on APCs is a critical secondary signal for full T cell activation [63]. |
| 4. MHC Matching | Confirm MHC restriction. | Use APCs and T cells from a matched donor or use a system where APCs are engineered to express a compatible MHC allele. |
| 5. Readout Assay | Validate the sensitivity of the activation readout. | Use a combination of methods: CFSE dilution to measure proliferation and flow cytometry to detect early (CD69) and late (CD25) activation markers, plus cytokine secretion (e.g., IL-2) [62]. |
Issue 2: Inconsistent Barrier Function in a Vascular Inflammation-on-Chip Model
Problem: The transendothelial electrical resistance (TEER) readings are unstable, making it difficult to assess immune cell migration.
Solution:
| Step | Checkpoint | Action & Recommendation |
|---|---|---|
| 1. Cell Confluence | Confirm a confluent endothelial monolayer. | Allow adequate time for the endothelial cells to form a tight barrier before initiating experiments. Measure baseline TEER; a stable, high baseline is essential [51]. |
| 2. Medium & Factors | Check growth medium and supplements. | Use specialized endothelial cell growth medium. Avoid repeated freeze-thaw cycles of growth factors. Ensure the presence of agents like cAMP and phosphodiesterase inhibitors to promote barrier stability. |
| 3. Perfusion & Shear Stress | Verify that flow conditions are stable and physiological. | Calibrate the microfluidic pumps. Ensure consistent, pulsation-free flow. Physiological shear stress is critical for endothelial health and barrier function [51]. |
| 4. Contamination | Rule out microbial or cellular contamination. | Test for mycoplasma. Ensure no other cell types (e.g., fibroblasts) are contaminating the endothelial culture. |
Issue 3: Failure to Recapitulate a Systemic Immune Response in a Multi-Organ-on-Chip System
Problem: Immune cells are not trafficking between different organ compartments as expected.
Solution:
| Step | Checkpoint | Action & Recommendation |
|---|---|---|
| 1. Circulatory Flow | Confirm the "circulatory" flow is not biased. | Check the design of the microfluidic channels for unintended traps or pressure differentials that may prevent cells from entering certain compartments. Use computational modeling to simulate cell flow [51]. |
| 2. Chemokine Gradients | Verify the establishment of chemotactic gradients. | Prime the target organ compartment with an appropriate inflammatory cytokine (e.g., TNF-α) to induce expression of adhesion molecules and chemokines. Ensure the flow rate is slow enough to allow stable gradient formation [63]. |
| 3. Immune Cell Phenotype | Check that the immune cells are in a correct state for trafficking. | Use primary human peripheral blood mononuclear cells (PBMCs) or isolated T cells. Avoid using immortalized cell lines that may have altered homing receptor expression. Validate the expression of relevant homing receptors (e.g., L-selectin, integrins) on the immune cells [51]. |
Research Reagent Solutions
This table details key reagents and their functions for building advanced immune models.
| Reagent / Material | Function in the Experimental System |
|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Source of primary human immune cells (T cells, B cells, monocytes, NK cells) for building autologous or allogeneic immune-competent models [51]. |
| THP-1 Cell Line | A human monocytic cell line that can be differentiated into macrophage-like or dendritic-like cells, used as a surrogate for innate immune cells in toxicity and sensitization testing [51]. |
| Collagen-Elastin Matrix (e.g., MatriDerm) | A scaffold used to create 3D full-thickness skin equivalents that can be populated with immune cells to model burn wounds and inflammatory processes [51]. |
| Small Molecule Inhibitor Cocktail (YPPP) | A defined cocktail used to generate dendritic cells from mouse bone marrow with enhanced maturation, IL-12 production, and T cell activation capabilities for cancer immunotherapy research [51]. |
| Cytokine Cocktails (e.g., TNF-α, GM-CSF, IL-4) | Used to differentiate and mature primary immune cells, such as driving monocyte-to-dendritic cell differentiation or inducing endothelial cell activation [51] [63]. |
Experimental Workflow & Signaling Pathways
Adaptive Immune Response Initiation Workflow
This diagram outlines the key cellular steps in initiating an adaptive immune response within a New Approach Method.
T Cell Activation Signaling Pathway
This diagram illustrates the critical signaling interactions between an Antigen Presenting Cell and a T cell during activation.
Foundational Principles: Why Human Diversity is Central to Modern Immunology
1.1 Why is there a pressing need to shift from animal models to human-focused immunology research?
Decades of heavy reliance on animal models, particularly inbred mice, have created significant translational challenges in immunology. While these models were foundational for understanding basic immunology, they often failed to lead to effective human treatments because of fundamental genetic, anatomical, and physiological differences between species. These differences are especially pronounced in the immune system, leading to inconclusive results for human diseases like Alzheimer's and cancer [64] [12]. The field is now undergoing a paradigm shift toward direct study of human immunity, accelerated by new technologies that enable high-quality, in-depth human data collection. This human-based approach is considered critical for accelerating innovation, improving healthcare outcomes, and delivering more effective treatments [64] [12].
1.2 What is meant by "biological variability" in human immunology, and why is it a feature to design for, not a problem to eliminate?
Biological variability in human immunology refers to the vast differences in immune system function and composition between individuals. This diversity is not random noise but is shaped by a complex interplay of factors. The table below summarizes the key contributors to this variability.
Table: Key Drivers of Human Immune System Diversity
| Factor | Key Aspect of Diversity | Primary Influence |
|---|---|---|
| Genetics | Presence of thousands of weakly associated genetic loci; archaic human gene introgressions (e.g., Neanderthal alleles); variations in HLA and KIR systems [65] [66]. | Up to half of observed immune variation; provides substrate for disease susceptibility and pathogen defense [65]. |
| Sex | Escape of immune-related genes (e.g., TLR7) from X-chromosome inactivation; suppressive role of testosterone in vaccine response [65]. | Leads to sex-specific differences in type I IFN responses and transcriptional responses to immune challenges like LPS [65]. |
| Age | Myeloid-biased hematopoietic stem cells; impaired early T follicular helper cell differentiation; thymic output variation [65]. | Shapes immune system composition and response capacity across the lifespan [65]. |
| Ancestry & Environment | Population-specific HLA, TCR, and immunoglobulin germline alleles; environmental exposures; microbiome; socioeconomic factors [66] [67]. | Impacts disease susceptibility, autoimmune disorder prevalence, and cancer risk across different populations [67]. |
Troubleshooting Guides: Addressing Common Challenges in Diverse Human Systems
2.1 FAQ: Our team is new to human immunology. What is the first practical step to account for genetic diversity in our study design?
The most critical first step is to ensure your research cohort includes individuals from diverse genetic ancestries. Most immunogenomics studies, including Adaptive Immune Receptor Repertoire (AIRR-seq) studies, have historically focused on individuals of European descent, severely limiting the generalizability of findings [66]. Actively including non-European populations will enhance the discovery of novel genetic traits and improve understanding of how pathogens have exerted selective pressures on immune-related genes in different human populations [66].
2.2 FAQ: We are getting unexpected negative results in our AIRR-seq analysis. What is a common source of error?
A frequent source of error is an incomplete or non-population-specific germline gene database. The process of V(D)J recombination in T and B cells creates vast receptor diversity, and the first analytical step—assigning sequences to their germline gene origins—requires a reliable, comprehensive database of germline V(D)J alleles [66]. The widely used IMGT database is invaluable but lacks a comprehensive set of human TCR and immunoglobulin alleles representing diverse populations worldwide [66]. Using a database that does not reflect the ancestry of your study population can lead to misassignment and failed analyses.
- Troubleshooting Steps:
- Repeat the analysis using newly available, more diverse germline databases like the Open Germline Receptor Database or VDJbase, which are being built by the AIRR Community (AIRR-C) to curate population-level data [66].
- Consider whether the experiment actually failed or is revealing genuine, previously uncharacterized diversity. Studies in South African and Papua New Guinea populations have discovered many novel immunoglobulin alleles not in IMGT [66].
- Document everything and consider submitting newly inferred germline sequences to the Inferred Allele Review Committee (IARC) for validation and inclusion in public databases to aid the wider community [66].
2.3 FAQ: Our immunohistochemistry (or other cell staining) results show a dim signal. How should we systematically troubleshoot this?
A dim signal in protocols like immunohistochemistry can stem from multiple variables. A systematic approach is key to resolving the issue.
- Troubleshooting Steps:
- Repeat the experiment: Unless cost-prohibitive, simply repeating the protocol can catch simple mistakes in reagent volumes or steps [68].
- Verify your controls: Ensure you have included a positive control. If the positive control also shows a dim signal, the problem is likely with the protocol or reagents. If only your experimental sample is dim, the result may be biologically accurate (e.g., low protein expression) [68].
- Check equipment and materials: Inspect reagents for improper storage or expiration. Verify that primary and secondary antibodies are compatible [68].
- Change one variable at a time: Isolate and test individual variables. Generate a list of potential issues and test the easiest ones first [68].
- Fixation time: Possibly too short.
- Antibody concentration: Possibly too low for primary or secondary antibody.
- Washing steps: Possibly too many or too vigorous.
- Microscope settings: Incorrect light settings are a quick check [68].
The Scientist's Toolkit: Research Reagent Solutions
When working with human models, having the right tools is essential. The table below details key reagents and their functions in immunology research.
Table: Essential Research Reagents for Human Immunology
| Reagent / Material | Function / Application |
|---|---|
| Human Immune Monitoring Center Tools | A suite of advanced immunological assays (e.g., high-parameter flow cytometry, multiplexed cytokine analysis) used for "systems immunology" - the integrated, large-scale analysis of human blood and tissue samples [64]. |
| AIRR-seq Technologies | High-throughput sequencing techniques specifically designed to capture the vast diversity of recombined, expressed T cell and B cell receptor repertoires from human samples [66]. |
| Human Organoids & Tissue Chips | In vitro 3D systems that model human disease and capture human-specific variability and patient-specific characteristics, serving as a key New Approach Method (NAM) [12]. |
| T Cell Characterization Kits | Reagents for the isolation (e.g., magnetic selection for CD4+ CD25+ regulatory T cells) and characterization of specific human T cell subsets (e.g., Th1, Th2, Th17) from PBMC or splenocyte preparations [69]. |
| Computational Models | Algorithms and software that simulate complex human biological systems, disease pathways, and drug interactions, reducing the reliance on animal models for initial screening [12]. |
Experimental Protocols: Key Methodologies for Human Immunology
4.1 Protocol: Isolation and Characterization of Human T Cell Subsets from Peripheral Blood
Background: This protocol is fundamental for studying human T cell responses in health and disease, allowing for direct assessment of human immune function without inference from animal models.
Detailed Methodology:
- Cell Source: Start with Peripheral Blood Mononuclear Cells (PBMCs) isolated from fresh human blood samples using density gradient centrifugation [69].
- Isolation: Use magnetic selection kits to isolate specific T cell populations. For example, use a CD4+ T Cell Isolation Kit to negatively select total CD4+ T cells. From this population, further isolate CD4+ CD25+ Regulatory T Cells (Tregs) using positive selection for CD25 [69].
- Characterization: Differentiate naive T cells into specific helper T cell subsets using cytokine cocktails:
- Human Th1 Cells: Differentiate with IL-12 and an anti-IL-4 antibody.
- Human Th2 Cells: Differentiate with IL-4 and an anti-IFN-γ antibody.
- Human Th17 Cells: Differentiate with TGF-β, IL-6, IL-1β, and antibodies against IFN-γ and IL-4 [69].
- Validation: Confirm successful differentiation by analyzing lineage-specific cytokine production (e.g., IFN-γ for Th1, IL-4 for Th2, IL-17 for Th17) using intracellular staining for flow cytometry or ELISA [69].
4.2 Protocol: Adaptive Immune Receptor Repertoire Sequencing (AIRR-seq)
Background: AIRR-seq allows for the comprehensive profiling of the diversity of B and T cell receptors in a human sample, directly capturing the genetic blueprint of an individual's adaptive immune response.
Detailed Methodology:
- Sample Preparation: Isolve RNA from human immune cells (B or T cells) from blood or tissue [66].
- cDNA Synthesis & Amplification: Use 5' RACE PCR to amplify T cell receptor (TCR) or immunoglobulin (B cell receptor) cDNA. This method is preferred for its ability to capture full-length variable regions without bias [66].
- High-Throughput Sequencing: Sequence the amplified libraries using a next-generation sequencing platform to generate millions of receptor sequences [66].
- Bioinformatic Analysis: Process the raw sequence data through a standardized pipeline:
- Pre-processing: Quality control and filtering of raw reads.
- Germline Gene Assignment: Map sequences to a database of V, D, and J genes (e.g., IMGT). This step is highly dependent on the completeness of the database [66].
- Clonotype Definition: Cluster sequences that are derived from the same original B or T cell.
- Diversity Analysis: Calculate metrics of repertoire diversity, clonality, and somatic hypermutation (for B cells) [66].
Technical Support Center
Troubleshooting Guides
Issue 1: High Inter-Laboratory Variability in Results Problem: Different laboratories reporting conflicting results for the same NAMs-based assay. Solution:
- Standardize Protocols: Develop and implement detailed Standard Operating Procedures (SOPs) for all critical steps, from sample collection to data analysis [70].
- Calibrate Equipment: Ensure all instruments across sites are calibrated using the same reference standards and maintenance schedules [71].
- Use Common Reagents: Source key reagents from a single manufacturer or implement quality checks to ensure consistency [71].
- Cross-Lab Validation: Perform initial ring trials where all laboratories analyze identical reference samples to identify and correct for systematic biases [70].
Issue 2: Low Fluorescent Signal in 3D Organoid Imaging Problem: Dim or absent fluorescence signal when visualizing protein targets in organoid cultures. Solution:
- Confirm Assay Validity: First, verify that your target protein is expressed at detectable levels in the organoid type [68].
- Check Antibody Compatibility: Ensure primary and secondary antibodies are compatible and have not degraded due to improper storage [68].
- Optimize Staining Parameters: Systematically test variables one at a time, starting with the simplest:
- Include Controls: Always run a positive control (e.g., a organoid line known to express the target) to confirm the protocol is working [68].
Issue 3: Inconsistent Machine Learning Model Performance Problem: An ML model trained on data from one automated platform performs poorly when applied to data from another lab. Solution:
- Harmonize Data Generation: Use automated, robotic workcells for sample preparation and analysis to eliminate operator-induced variability [72].
- Multi-Instrument Training: Train models using data generated from multiple identical instruments across different facilities to make the model robust to instrument-specific noise [72].
- Feature Engineering: Incorporate domain knowledge to select features that are biologically relevant and less sensitive to technical variation [72].
Frequently Asked Questions (FAQs)
What quality control (QC) measures are essential for reproducible NAMs research? High-quality NAMs research relies on a multi-layered QC system [70]:
- Internal Standards: Use isotopically labeled compounds (e.g., 13C, 15N) added during sample preparation to correct for extraction efficiency and instrument drift [70].
- Pooled QC Samples: Create a sample from a small aliquot of every study sample and analyze it at regular intervals (e.g., every 8-10 injections) to monitor system stability [70].
- Technical Replicates: Perform multiple analyses of the same sample to quantify analytical precision. Aim for a coefficient of variation (CV%) below 15% for targeted analysis and below 30% for untargeted screens [70].
How can we reduce reliance on animal models through NAMs without sacrificing data quality? New Approach Methodologies (NAMs), such as organoids, microphysiological systems, and computational models, are designed to be complementary and potentially replacement tools for animal research [73]. To ensure data quality:
- Robust Validation: Rigorously validate NAMs by benchmarking their responses against known clinical outcomes or existing, limited animal data where necessary [73].
- AI-Enhanced Standardization: Use generative AI to create optimized, standardized protocols that capture critical details often overlooked in manual documentation, ensuring consistent implementation across different research teams [74].
- Cross-Model Correlation: Establish a strong correlation between data from different NAMs platforms (e.g., different organoid lines, different computational models) to build confidence in their predictive value [73].
What are the key steps in validating a new analytical method for NAMs? Method validation is critical for generating high-confidence data [70].
- Test Repeatability & Reproducibility: Analyze QC samples across multiple batches and days to confirm consistency [70].
- Assess Linearity & Limits: Establish the dynamic range of quantification and the lowest detectable amount of analyte [70].
- Evaluate Recovery & Matrix Effects: Measure how efficiently the method extracts the analyte and whether the sample background enhances or suppresses the signal [70].
- Cross-Platform Validation: Compare results with those from a different analytical technique (e.g., LC-MS vs. NMR) to ensure consistency [70].
How can AI and automation improve reproducibility? Generative AI and automated platforms address reproducibility crises by [74] [72]:
- Protocol Standardization: AI can analyze successful experiments to generate hyper-detailed, standardized protocols that eliminate ambiguity.
- Intelligent Quality Control: AI systems can monitor experiments in real-time, detecting deviations from the protocol and alerting researchers before the experiment is compromised [74].
- Eliminating Human Variability: Remotely programmed, robotic synthesis and analysis ensure that the exact same procedure is executed every time, regardless of location or operator [72].
- Automated Documentation: AI-driven lab notebooks can automatically record every parameter (reagent lot numbers, equipment settings, environmental conditions), creating a perfect record for replication [74].
Standardized Experimental Protocols
Protocol 1: Cross-Laboratory Validation of an Organoid-Based Assay
Objective: To ensure an organoid assay yields reproducible results across multiple research sites.
Materials:
- Cultured organoids (from a central, validated source)
- Standardized culture medium (pre-formulated or created from a master mix)
- Assay reagents (e.g., cytokines, dyes, antibodies) from single lots
- Multi-well plates and automated liquid handlers (e.g., Hamilton Liquid Handler) [72]
- Plate reader or imaging system (e.g., CLARIOstar spectrometer) [72]
Methodology:
- Protocol Distribution: All participating labs receive an identical, detailed SOP covering organoid handling, dosing, and endpoint measurement.
- Reagent Harmonization: Centralized distribution of key reagents (e.g., organoid lines, assay kits) to all sites to minimize variability [71].
- Instrument Calibration: Each site verifies calibration of its equipment against provided reference standards before starting [71].
- Blinded Analysis: Sites analyze a set of blinded samples, including positive/negative controls and unknown test compounds.
- Data Collection & Analysis: Raw data is collected in a standardized format and analyzed using a central, pre-defined statistical model to calculate inter-laboratory CV%.
Protocol 2: Machine Learning-Guided Optimization of a Microphysiological System
Objective: To use an ML-driven, automated workflow to optimize culture conditions for a liver-on-a-chip model.
Materials:
- Microphysiological system chips
- Primary human hepatocytes or iPSC-derived hepatocytes
- Robotic liquid handling workcell (e.g., Hamilton Microlab STAR) [72]
- In-line absorbance/fluorescence spectrometer [72]
- ML software platform (e.g., Wolfram Mathematica) [72]
Methodology:
- Experimental Design: Use a sampling method (e.g., Latin Hypercube Sampling) to define an initial set of 20-40 experiments that vary key parameters (e.g., shear stress, cell seeding density, cytokine concentration) [72].
- Automated Execution: Program and execute the experiments remotely on a robotic workcell, ensuring precise control over all fluid additions, timings, and environmental conditions [72].
- Real-Time Monitoring: Use in-line spectrometers to collect high-frequency data on key output metrics (e.g., albumin secretion, urea production) [72].
- Model Training & Prediction: Train a machine learning model (e.g., Random Forest, Gradient Boosted Trees) on the collected data to predict the combination of parameters that will maximize desired organ function [72].
- Validation: Run the model-predicted optimal conditions in the automated system to validate the improvement.
Data Presentation
Key Quality Control Metrics for Reproducible Research
Table 1: Essential QC metrics and their targets for ensuring data reproducibility.
| Metric | Purpose | Target/Best Practice |
|---|---|---|
| Coefficient of Variation (CV%) | Measures intra- and inter-batch precision [70]. | <15% for targeted analysis; <30% for untargeted [70]. |
| Internal Standards | Corrects for instrument drift and matrix effects [70]. | Use isotopically labeled analogs of target analytes [70]. |
| Pooled QC Samples | Monitors system stability over time [70]. | Analyze every 6-10 study samples; track retention time and signal intensity [70]. |
| Certified Reference Standards | Calibrates instruments for accurate quantification [70]. | Use for establishing a calibration curve [70]. |
| Proficiency Testing | Assesses laboratory performance against peers [71]. | Regular participation in external quality assurance programs [71]. |
Research Reagent Solutions for NAMs
Table 2: Key materials and their functions in establishing reproducible NAMs.
| Reagent/Material | Function in NAMs Research |
|---|---|
| Basement Membrane Extract (BME) | Provides a 3D scaffold for the culture of organoids, mimicking the in vivo extracellular matrix [69]. |
| Defined Differentiation Kits | Directs stem cells to differentiate into specific cell lineages (e.g., hepatocytes, neurons) with high consistency [69]. |
| Cytokine & Growth Factor Panels | Used to simulate disease states or specific immune responses in microphysiological systems [69]. |
| Isotopically Labeled Internal Standards | Enables precise quantification of metabolites in LC-MS/MS assays, critical for metabolomics-based safety assessments [70]. |
| Viability Assay Kits (e.g., 7-AAD) | Provides a standardized method to assess cell health and compound toxicity in complex 3D cultures [69]. |
Workflow Visualization
Diagram 1: Cross-Lab Validation Workflow
Diagram 2: AI-Enhanced Reproducibility System
For researchers pioneering New Approach Methodologies (NAMs), defining the Context of Use (COU) is a critical, foundational step for regulatory acceptance and scientific validity. A clearly articulated COU provides a concise description of how a specific tool—such as a biomarker or a novel in vitro assay—will be used within drug development, and under what specific conditions it can be relied upon [75] [76]. As regulatory agencies like the FDA and NIH prioritize a shift toward human-based research technologies to reduce reliance on animal models, a well-defined COU ensures that these innovative methods are evaluated against clear, relevant criteria [12] [8]. This technical support center is designed to help you, the researcher, successfully navigate the process of defining and applying the COU to your NAMs, facilitating their integration into the regulatory landscape.
Frequently Asked Questions (FAQs)
What exactly is a Context of Use (COU)?
A Context of Use is a concise description of a tool's specified application in drug development. According to the FDA, it consists of two core components: the BEST biomarker category and the tool's intended use in drug development [75]. It is generally structured as: [BEST biomarker category] to [drug development use] [75].
Examples of COU include [75]:
- Predictive biomarker to enrich for enrollment of a sub-group of asthma patients who are more likely to respond to a novel therapeutic in Phase 2/3 clinical trials.
- Safety biomarker for the detection of acute drug-induced renal tubule alterations in male rats.
- Prognostic biomarker to enrich the likelihood of hospitalizations during the timeframe of a clinical trial.
Why is defining the COU so critical for NAMs?
Defining the COU is critical for NAMs for several key reasons:
- Regulatory Qualification: For a Drug Development Tool (DDT) like a NAM assay, qualification is a conclusion that within the stated COU, the tool can be relied upon to have a specific interpretation and application in drug development and regulatory review [76]. It defines the boundaries within which the available data justify the tool's use [76].
- Facilitates Widespread Adoption: Once a DDT is qualified for a specific COU, it becomes publicly available for use in any drug development program for that qualified purpose, potentially without needing further re-evaluation in every IND, NDA, or BLA submission [76].
- Guides Evidence Generation: A precise COU focuses your validation efforts. It tells you exactly what performance characteristics need to be measured and what scientific evidence needs to be generated to support the tool's intended use, making the development process more efficient.
What is the process for getting a COU qualified by a regulatory agency?
The FDA's Drug Development Tool (DDT) qualification process is a multi-stage pathway established by the 21st Century Cures Act [76]. While complex, it generally involves:
- Submission of a Qualification Plan: This is a comprehensive document outlining the proposed COU and the development plan for the tool. The FDA has published a revised outline for these plans to assist requestors [76].
- Agency Interactions and Collaboration: The process is designed for early engagement and scientific collaboration with the FDA to facilitate tool development [76].
- Data Generation and Review: Submission of data that supports the qualified use of the tool within the specific COU.
The mission of this program is to encourage innovation, expedite drug development, and create a shared learning environment [76].
Troubleshooting Guides
Problem: My assay's results are inconsistent, leading to questions about its reliability for regulatory submission.
Issue: High variability in experimental outputs makes it difficult to define a stable performance profile for the COU.
Diagnosis and Solution: Applying a structured troubleshooting methodology can help isolate and resolve the root cause. The following workflow outlines a systematic approach to diagnosing reliability issues, from initial understanding to implementing a permanent fix.
Best Practices for Resolution:
- Ask Targeted Questions: Probe for specific details. "Does the variability occur between different operators, or between different lots of a key reagent?" [77] [78].
- Change One Variable at a Time: Systematically test potential causes (e.g., reagent lot, cell passage number, equipment) without introducing other changes. This is the only way to definitively identify the root cause [77].
- Compare to a Working Baseline: If available, compare your inconsistent results to data generated from a previously validated and stable method to help spot differences [77].
- Document Everything: Keep a detailed log of all tests, changes, and results during the investigation. This documentation will be crucial for your eventual regulatory submission.
Problem: My validation data does not seem to support the proposed Context of Use.
Issue: A disconnect exists between the data generated from your NAM assay and the claims you are making about its use in the COU.
Diagnosis and Solution: This problem often stems from a COU that is too broad or vague. The solution is to refine the COU and ensure your experimental design directly validates its specific claims.
Best Practices for Resolution:
- Narrow the Scope: Instead of "predicting human toxicity," define a COU like "identifying compounds that induce phospholipidosis in human hepatocytes." A narrower COU is easier to validate [75] [76].
- Engage Regulators Early: Discuss your proposed COU and supporting validation plan with the FDA through the appropriate qualification pathway. Their feedback is invaluable for ensuring your approach is aligned with regulatory expectations [76] [8].
- Build Evidence Incrementally: It is often practical to start by using your NAM alongside traditional animal models, building evidence of its predictive value before seeking qualification as a full replacement [8].
Research Reagent Solutions for NAMs Assay Development
The following table details key materials and their functions in building robust NAMs assays.
| Research Reagent / Tool | Function in NAMs Assay Development |
|---|---|
| 2D & 3D Cell Culture Systems | Provides the foundational biological model; 3D systems like organoids better mimic human tissue architecture and function compared to traditional 2D cultures [8]. |
| Organoids | Enables precision culture using patient-derived cells, allowing for the study of human-specific disease biology and patient variability [12] [8]. |
| Organs-on-a-Chip | Microphysiological systems that mimic human organ function and can be linked to model inter-organ interactions, providing a more holistic view of drug effects [12] [8]. |
| Specialized Media & Growth Factors | Critical for maintaining the health, function, and phenotypic stability of complex cell cultures like organoids over time [8]. |
| Omics Reagents (Genomics, Proteomics) | Tools for deep molecular profiling to uncover biomarkers of response and mechanism of action, strengthening the biological rationale of your COU [8]. |
| Computational & AI/ML Analytics | Software and algorithms to integrate and analyze complex datasets from NAMs, identifying predictive patterns and simulating toxicity pathways [12] [8]. |
Experimental Protocol: Key Steps for Validating a COU for a Novel NAM
This protocol outlines the critical stages for generating the evidence required to support a specific Context of Use.
Objective: To generate robust, reproducible data that validates the performance of a New Approach Methodology for its specified Context of Use.
Workflow Overview:
Detailed Methodologies:
Draft the COU Statement:
Design the Validation Study:
- Define a Compound Panel: Select a set of reference compounds with known mechanisms and effects relevant to your COU (e.g., known hepatotoxins for a liver injury biomarker assay).
- Include Appropriate Controls: Ensure your study design includes positive, negative, and vehicle controls to account for assay variability.
- Establish Acceptance Criteria: Pre-define the performance metrics (e.g., sensitivity >80%, specificity >70%, high intra- and inter-assay precision) that your assay must meet to be considered successful for the COU.
- Plan for Statistical Power: Ensure the study is designed with sufficient replicates and sample sizes to generate statistically sound conclusions.
Execute and Analyze:
- Conduct assays in a blinded manner where possible to minimize bias.
- Measure key performance parameters: Accuracy (how close results are to the known truth), Precision (repeatability and reproducibility), Robustness (resistance to small, deliberate changes in protocol), and Specificity/Sensitivity.
- Compare the results directly against the claims made in the COU.
Document and Submit:
- Compile all data, standard operating procedures (SOPs), and statistical analyses into a comprehensive report.
- This body of evidence forms the core of a Qualification Plan submission to a regulatory agency like the FDA, seeking official recognition of the DDT for its specified COU [76].
Troubleshooting Guides & FAQs
Common Multi-OMICs Integration Failures
1. Unmatched Samples Across Omics Layers
- Problem: RNA, ATAC, proteomics, or methylation data come from different, unmatched sample sets, leading to confusing and unreliable correlation results.
- Solution: Begin with a matching matrix to visualize sample overlap across all modalities. Perform analyses only on the subset of samples with data across all layers, avoiding forced integration of unmatched data [79].
2. Misaligned Data Resolution
- Problem: Attempting to integrate data from different resolutions, such as bulk RNA-seq with single-cell ATAC-seq, without accounting for compositional differences and missing cellular anchors.
- Solution: Evaluate resolution compatibility first. Use reference-based deconvolution for bulk data or infer cell type signatures to create a compatible bridge between data layers [79].
3. Improper Normalization Across Modalities
- Problem: Each omics type uses different normalization (e.g., library size for RNA-seq, TMT ratios for proteomics, β values for methylation), causing one modality to dominate integrated analysis if not harmonized.
- Solution: Apply comparable scaling such as quantile normalization, log transformation, or centered log-ratio (CLR) to each layer. Test modality contributions post-integration to ensure no single layer skews the results [79].
4. Batch Effects That Compound Across Layers
- Problem: Batch effects present in individual omics layers are amplified upon integration, creating patterns driven by technical artifacts rather than biology.
- Solution: Inspect batch structure both within and across omics layers. Apply cross-modal batch correction methods after initial alignment and verify that biological signals dominate the final integrated structure [79].
5. Overinterpreting Weak Correlations
- Problem: Expecting and reporting high correlations between layers like RNA and protein, when biological regulation often leads to divergence.
- Solution: Analyze regulatory links only when supported by additional evidence like genomic distance, enhancer maps, or TF binding motifs. Report confidence levels and build integration from mechanistic logic rather than raw correlation [79].
High-Content Screening (HCS) Optimization
6. Ensuring Assay Quality and Reproducibility
- Problem: HCS data quality is variable, leading to unreliable results and poor reproducibility.
- Solution: Use the Z' factor as a key statistical parameter for assessing assay quality. An assay with a Z' factor > 0.4 is considered robust for screening, though > 0.6 is preferred. Include pharmacological controls within each assay to monitor quality [80].
7. Minimizing Fluorescent Bleed-Through
- Problem: Significant bleed-through between fluorescent probes due to broad excitation/emission spectra, leading to cross-talk and inaccurate data.
- Solution: Choose wavelengths and emission filters by reviewing filter specifications to minimize cross-talk. Optimize the optical setup to match the peak properties of the fluorescent targets used [80].
8. Managing Edge Effects in Multi-Well Plates
- Problem: "Edge effects" in plate-based assays cause over- or under-estimation of cellular responses in outer wells due to evaporation or temperature gradients.
- Solution: For fluorescent assays, use solid black polystyrene microplates to reduce well-to-well cross-talk and background signal. When possible, avoid using only the first and last columns for controls [80].
Experimental Protocols & Data Standards
Multi-OMICs Data Preprocessing Workflow
Adhering to a standardized preprocessing workflow is critical for successful data integration and for reducing the need for repeated animal experiments [81] [79].
Detailed Methodologies:
Modality-Specific Normalization: Apply appropriate normalization for each data type.
- RNA-seq: Normalize by library size (e.g., TPM, FPKM) or using a robust method like DESeq2's median of ratios.
- Proteomics: Normalize by TMT ratios or spectral counts.
- ATAC-seq: Normalize by total peaks or use binning approaches.
- DNA Methylation: Use β-values or M-values [79].
Standardization & Harmonization: Convert all datasets into a unified format, typically an n-by-k samples-by-feature matrix. This often involves mapping data onto shared biochemical networks or using domain-specific ontologies to ensure compatibility [81] [82].
Cross-Modal Batch Effect Correction: Inspect for batch effects within and across data layers. Use multivariate linear modeling or tools like Harmony with batch covariates to correct these effects jointly across all modalities, not just individually [79].
Biology-Aware Feature Selection: Move beyond simple variance-based filtering. Apply biology-aware filters to remove uninformative features:
- Remove mitochondrial or ribosomal genes from RNA-seq data.
- Exclude blacklist genomic regions from ATAC-seq data.
- In proteomics, focus on high-confidence, consistently detected proteins to ensure pathway-level coherence [79].
Assay Quality Control for High-Content Screening
Implementing rigorous QC protocols ensures HCS data is reliable and reproducible, maximizing information gained from each experiment.
Table: HCS Quality Control Metrics and Standards
| Parameter | Target/Standard | Implementation in NAMs |
|---|---|---|
| Z' Factor | > 0.4 (minimum), > 0.6 (preferred) [80] | Statistical measure of assay robustness; use for every plate. |
| Controls | Positive & negative controls in every assay [80] | Essential for defining valid assay response and baseline. |
| Replicates | Minimum of duplicates for primary screening [80] | Reduces false positives/negatives; confirms hits. |
| Cell Line Validation | Genotyping (e.g., STR analysis) [80] | Confirms cellular model identity and functionality for reliable results. |
| Liquid Handling | Regular calibration and verification [80] | Ensures dispensing accuracy and reproducibility in automated platforms. |
The Scientist's Toolkit
Table: Essential Research Reagent Solutions for Multi-OMICs & HCS
| Category | Specific Tool / Solution | Function in NAMs |
|---|---|---|
| Bioinformatics Tools | mixOmics (R) [81], INTEGRATE (Python) [81], MOFA+ [79] | Performs integrative analysis of multiple omics data types. |
| Cell Line Quality Control | Short Tandem Repeat (STR) Analysis [80] | Authenticates cell lines, ensuring model fidelity and reducing experimental variability. |
| HCS Fluorescent Probes | SCREEN-WELL libraries, CELLESTIAL probes [80] | Enable multiplexed, phenotypic readouts in live or fixed cells. |
| Data Harmonization | Conditional Variational Autoencoders (e.g., for RNA-seq) [81], Domain-specific ontologies [81] | Aligns data from different sources/platforms to a common standard, enabling integration. |
| Statistical QC | Z' Factor Calculation [80] | Provides a standard metric to validate the quality and robustness of each HCS assay run. |
Advanced Integration & Analysis
Successfully preprocessed data can be integrated using advanced analytical frameworks to extract biologically meaningful insights relevant to immunology.
Implementation Guide:
- Network Integration: Map multiple omics datasets onto shared biochemical networks. This connects analytes (genes, proteins, metabolites) based on known interactions (e.g., a transcription factor to the transcript it regulates) to improve mechanistic understanding [82].
- AI/ML for Pattern Detection: Leverage machine learning and deep learning to detect intricate patterns and interdependencies within high-dimensional multi-omics datasets that are beyond human capability to discern, facilitating biomarker discovery and patient stratification [82] [83].
- Tool Selection: Choose integration-aware tools like MOFA+ or DIABLO that can weight modalities separately, rather than standard PCA, to prevent one data type from dominating the analysis [79].
From Proof-of-Concept to Regulatory Acceptance: Validating and Qualifying NAMs
FAQs: Core Concepts and Troubleshooting
FAQ 1: What is the fundamental difference between retrospective and prospective validation for New Approach Methodologies (NAMs)?
Retrospective validation uses existing datasets from previously completed clinical studies to test a model's predictive power. This approach is more feasible and timely but requires high-quality, well-annotated historical data from randomized controlled trials to avoid confounding factors [84]. In contrast, prospective validation is the gold standard, where a model's predictions are tested in a new, planned clinical study or within a predefined clinical workflow. This provides the strongest evidence for regulatory acceptance but requires more time and resources [84] [85].
FAQ 2: Our computational model performed well in retrospective validation but failed prospectively. What are the most common reasons for this?
This is a frequent challenge. Common pitfalls include:
- Overfitting: The model is too complex and captures noise from the training data rather than the underlying biological signal, leading to poor performance on new data [86].
- Cohort Shift: The patient population or healthcare setting in the prospective study differs significantly from the retrospective data used for development, affecting model generalizability [86] [85].
- Inadequate Bias Assessment: The model was not properly assessed for algorithmic bias across different racial, gender, or ethnic subgroups before prospective deployment [85].
- Workflow Integration Failure: The model's output does not integrate seamlessly into the clinical or experimental workflow, leading to misinterpretation or misuse, even if the prediction is accurate [85].
FAQ 3: What are the key regulatory considerations for using a validated NAM to replace an animal study?
Regulatory agencies like the FDA encourage a scientifically justified approach. Key steps include:
- Engage Early: Utilize programs like the FDA's Model-Informed Drug Development (MIDD) Paired Meeting Program to discuss your NAM strategy and context of use [87].
- Provide Strong Rationale: Justify why the NAM is more human-relevant, especially for targets with poor cross-species translatability (e.g., a monoclonal antibody targeting a human-specific receptor) [17].
- Submit Parallel Data: Initially, submit NAM data (e.g., from organoids or in silico models) alongside traditional animal data as supportive evidence to build regulatory confidence [17].
- Demonstrate Standardization: Use standardized, reproducible protocols for your NAMs, as variability has been a major historical hurdle to adoption [17].
FAQ 4: How can we assess the "translational relevance" of a NAM before committing to a large prospective clinical trial?
Computational frameworks can evaluate translatability by focusing on conserved biological pathways rather than individual genes. One method involves:
- Pathway Enrichment Analysis: Convert gene expression data from both your NAM and human disease samples into pathway enrichment scores.
- Identify Translatable Pathways: Use machine learning (e.g., sparse PCA) to identify phenotype-defining biological pathways that are consistently dysregulated in both your NAM and human datasets.
- Qualification Testing: Test the framework's predictive validity by seeing if it can correctly predict the outcomes of known clinical successes or failures based solely on preclinical NAM data [88].
Quantitative Data and Performance Benchmarks
The following tables summarize key performance metrics from real-world examples of model validation, providing benchmarks for your own work.
Table 1: Prospective Validation Performance of an ML Model for Predicting ED Visits in Oncology Patients [85]
| Metric | Retrospective Evaluation | Prospective Evaluation |
|---|---|---|
| Cohort Size | 28,433 encounters | 1,236 patients |
| Observed Event Rate | 10% | 7% |
| Positive Predictive Value (PPV) | 26% | 22% |
| Negative Predictive Value (NPV) | 91% | 95% |
| Odds Ratio (High vs. Low Risk) | 3.5 (95% CI: 3.4–3.5) | 5.4 (95% CI: 2.6–11.0) |
| Key Outcome | Model identified high-risk patients. | 76% of model-flagged patients were confirmed as high-risk by clinicians. |
Table 2: Framework for Assessing Translatability of Alzheimer's Disease Animal Models [88]
| Preclinical Model | Presence of Translatable Pathways | Identified Translatable Pathways | Predictive Validity |
|---|---|---|---|
| APP/PS1 | No | None Identified | Not Demonstrated |
| 3×Tg | No | None Identified | Not Demonstrated |
| 5×FAD | Yes | SREBP control of lipid synthesis; Cytotoxic T-lymphocyte activity | Accurately predicted clinical failure of ibuprofen |
Experimental Protocols for Key Validation Experiments
Protocol 1: Workflow for a Prospective, Real-World Clinical Validation Study
This protocol is based on a successful implementation of an ML tool for predicting emergency department visits in cancer patients [85].
- Define Clinical Aim: Clearly state the clinical quality improvement goal (e.g., "Identify patients at high risk for a 60-day ED visit for eligibility in a home-based acute care program").
- Model Development & Retrospective Validation:
- Use a dedicated training dataset to develop the model.
- Test the model on a held-out retrospective validation cohort to establish baseline performance (PPV, NPV, calibration).
- Bias Assessment:
- Perform a fairness analysis by calculating calibration factors for different demographic subgroups (e.g., by race, gender, ethnicity).
- Ensure that the bootstrapped 95% confidence interval for the calibration factor includes 0 for all groups, indicating no significant miscalibration [85].
- Prospective Pilot Validation:
- Integrate the model into the live clinical workflow.
- For a set period, have the model screen all eligible patients and flag "high-risk" individuals.
- Have clinical experts (e.g., nurse practitioners) review the EHRs of flagged patients to confirm eligibility for the intervention, without being blinded to the model's output.
- Track the concordance rate between the model and clinician assessment.
- Outcome Tracking & Analysis:
- Track the actual clinical outcome (e.g., ED visit within 60 days) for all patients.
- Compare the model's prospective performance (PPV, NPV, Odds Ratio) against its retrospective performance and against the baseline event prevalence.
Protocol 2: A Computational Workflow to Assess NAM Translatability
This protocol uses a machine learning approach to evaluate how well a preclinical model recapitulates human disease pathways, based on an assessment of Alzheimer's disease models [88].
- Data Selection & QC:
- Obtain transcriptomic data (e.g., microarray, RNA-seq) from your NAM under diseased and control conditions.
- Obtain comparable human transcriptomic data from post-mortem tissue or clinical biopsies.
- Ensure data originates from analogous biological contexts (e.g., same brain region, cell type). Use a database like GEMMA to assign a data quality score (≥0.4 is acceptable) [88].
- Gene Set Enrichment Analysis (GSEA):
- Independently for each dataset (NAM and human), calculate fold-change expression for each gene versus control.
- Perform pre-ranked GSEA using a tool like the
fgseaR package to generate Normalized Pathway Enrichment Scores (NES) for each sample. Use pathway gene sets (e.g., BIOCARTA) [88].
- Sparse Principal Component Analysis (sPCA):
- Power-transform the NES data to normalize.
- Construct an sPCA model for the NAM data to identify the principal components (PCs) that capture the maximum variance driven by the experimental phenotype.
- Machine Learning Classification:
- Use a support vector machine (SVM) classifier on the sPCA results to identify the PCs that best distinguish the NAM's diseased state from its control state.
- Projection and Translatability Assessment:
- Project the human data into the NAM's sPCA space.
- Pathways that are significantly enriched in both the NAM and human data within this PCA space are considered "translatable pathways." A model with no translatable pathways has poor translational relevance [88].
Visualized Workflows and Signaling Pathways
Prospective Clinical Validation Workflow
NAM Translatability Assessment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for NAM Development and Validation
| Resource / Reagent | Function / Application | Key Consideration |
|---|---|---|
| Standardized Organoids | 3D in vitro models that mimic human organ complexity for toxicity and efficacy testing [17]. | Prioritize kits with high reproducibility and validated protocols to ensure regulatory-grade data. |
| PBPK Modeling Software | In silico platforms for simulating the absorption, distribution, metabolism, and excretion of compounds in humans [89] [17]. | Models must account for ontogeny (organ maturation) in specific populations like pediatrics [89]. |
| BIOCARTA/Gene Set Databases | Curated collections of biological pathways used for Gene Set Enrichment Analysis (GSEA) [88]. | Essential for shifting from single-gene to pathway-level analysis, improving cross-species translatability. |
| FDA MIDD Meeting Program | A regulatory pathway for sponsors to get FDA feedback on their modeling and simulation plans [87]. | Critical for de-risking development and aligning NAM strategy with regulatory expectations. |
| Immune-Competent Co-culture Systems | Organoid or tissue models that include human immune cells to study immunology and immuno-oncology [17]. | Overcomes a major limitation of animal models, which have different immune systems. |
| Historical Clinical Trial Data | Datasets from previous RCTs, essential for retrospective validation of predictive biomarkers [84]. | Must be from a well-conducted RCT with available samples from a large majority of patients to avoid bias [84]. |
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: What is the fundamental goal of benchmarking a NAM against an animal model? The goal is not to perfectly recapitulate every aspect of the animal test, but to determine if the NAM can provide information of equivalent or superior human relevance for a safety decision, often by capturing key biological pathways or mechanisms of action [59]. The aim is improved human safety assessment, not merely replicating the animal response [59].
FAQ 2: My NAM results are inconsistent. What could be the cause? Variability in NAMs can stem from the biological donor-to-donor variability of human cells, which can be a strength if managed correctly [58] [51]. Ensure strict quality control measures, including:
- Using standardized cell culture protocols.
- Thoroughly characterizing cell sources (e.g., primary vs. cell line).
- Implementing appropriate positive and negative controls in every experiment run [90].
FAQ 3: How do I handle a situation where my NAM data contradicts historical animal study data? A discrepancy does not automatically mean the NAM is wrong. First, investigate the scientific basis:
- Species Differences: The animal model may not be human-relevant for that specific endpoint. Rodents, for example, have a documented poor predictivity rate (40-65%) for human toxicity [59].
- Exposure Conditions: Re-evaluate if the exposure concentrations and durations in your NAM are physiologically relevant compared to the in vivo situation [59].
- Mechanistic Insight: Use the NAM to investigate the underlying mechanism; this can provide a powerful scientific argument for the validity of your results [59].
FAQ 4: What are the key considerations when incorporating AI or machine learning with NAM data? Effective data integration and analysis are crucial [90]. Ensure you have:
- High-Quality, Curated Data: AI models are only as good as the data they are trained on.
- Clear Objectives: Define the specific question the model is meant to answer (e.g., classification, potency prediction).
- Interdisciplinary Collaboration: Work with data scientists to leverage appropriate analytical techniques and avoid overfitting models [90].
FAQ 5: How can I build confidence in my NAM for regulatory submission? Start by using your NAM alongside traditional methods for specific, well-defined questions. Generating data using a Defined Approach (DA)—a fixed combination of information sources and a data interpretation procedure—can facilitate regulatory acceptance, as seen with OECD Test Guidelines for skin sensitization [59]. Proactively engaging with regulatory agencies early in the process is also highly recommended [90].
Detailed Experimental Protocols for Key NAMs
The following protocols represent advanced NAMs used in immunology research, reflecting the state-of-the-art as of late 2024.
Protocol 1: Microfluidic Platform for Modeling Vascular Inflammation [51]
- Objective: To create a human-relevant model for real-time measurement of endothelial barrier function and immune cell migration in response to inflammatory stimuli.
- Key Materials:
- Human endothelial cells (e.g., HUVECs)
- A 64-channel parallel microfluidic platform (e.g., from commercial suppliers)
- Microfluidic chips coated with collagen or fibronectin
- Transendothelial Electrical Resistance (TEER) measurement system integrated into the platform
- Inflammatory cytokines (e.g., TNF-α, IL-1β) and/or human immune cells (e.g., monocytes)
- Cell culture medium and appropriate supplements
- Methodology:
- Chip Preparation: Coat the microfluidic channels with an extracellular matrix protein (e.g., collagen I) and sterilize.
- Cell Seeding: Introduce a suspension of human endothelial cells into the microfluidic channels and allow them to form a confluent, tight monolayer over 2-3 days. Monitor confluence visually and via TEER values.
- Barrier Integrity Baseline: Measure a stable, baseline TEER value, indicating the formation of a functional endothelial barrier.
- Inflammatory Challenge: Perfuse the channels with a medium containing pro-inflammatory cytokines or introduce human immune cells into the flow.
- Real-Time Monitoring:
- Continuously monitor TEER for a period of 6-24 hours. A drop in TEER indicates increased barrier permeability and a successful inflammatory response.
- Optionally, sample effluent for cytokine analysis (e.g., via ELISA) or fix cells at endpoint for immunostaining of adhesion molecules (e.g., ICAM-1, VCAM-1).
- Data Analysis: Quantify the rate and extent of TEER reduction. Correlate with cytokine data and/or immune cell adhesion/migration counts.
Protocol 2: Generating a 3D Immunocompetent Full-Thickness Skin Model for Sensitization Testing [51]
- Objective: To develop a human skin equivalent containing functional immune cells to assess the response to chemical sensitizers and irritants.
- Key Materials:
- Human dermal fibroblasts
- Human keratinocytes
- THP-1 cell line (as a surrogate for dermal dendritic cells)
- Cell culture inserts for air-liquid interface culture
- Type I collagen matrix
- Test chemicals (sensitizers and non-sensitizers)
- Dexamethasone (for suppression control)
- Flow cytometry antibodies (e.g., against CD86, CD54, HLA-DR)
- Methodology:
- Dermal Equivalent Fabrication: Mix human dermal fibroblasts with a collagen I matrix and allow it to contract and mature in a cell culture insert for several days.
- Immune Cell Integration: Differentiate THP-1 cells into a dendritic cell-like phenotype and incorporate them into the dermal equivalent.
- Epidermal Development: Seed human keratinocytes on top of the dermal layer. After reaching confluence, raise the construct to an air-liquid interface to promote the formation of a stratified, cornified epidermis. This process typically takes 2-3 weeks.
- Model Validation: Confirm the presence of key skin structures (stratified epidermis, dermis) histologically and verify dendritic cell surrogate localization and viability.
- Chemical Exposure: Topically apply the test chemicals to the surface of the skin model for a defined period (e.g., 24-48 hours).
- Endpoint Analysis:
- Cell Activation: Digest the model to extract cells and analyze the expression of dendritic cell maturation markers (e.g., CD86, CD54) via flow cytometry.
- Cytokine Secretion: Measure pro-inflammatory cytokines (e.g., IL-8, IL-1β) in the culture medium using ELISA.
- Histology: Fix and section the model to assess tissue viability and morphology.
- Data Interpretation: A positive sensitization response is indicated by a statistically significant upregulation of maturation markers and cytokine secretion compared to vehicle controls. Suppression of this response by dexamethasone confirms the model's functionality.
Quantitative Data on NAM Performance vs. Animal Studies
Table 1: Comparison of Predictive Performance for Human Toxicity
| Model Type | Reported Human Toxicity Predictivity Rate | Key Advantages | Key Limitations |
|---|---|---|---|
| Traditional Animal Models (Rodents) | 40% - 65% [59] | Whole-system biology; established historical data [58] | High cost, ethical concerns, significant species differences [58] [59] |
| Organ-on-a-Chip Systems | ~80% accuracy (for replicating human physiology) [91] | Human cells; dynamic flow; can model barrier function [51] [91] | High complexity; can lack full immune components; standardization ongoing [51] |
| Defined Approaches (DAs) for Skin Sensitization | Outperforms the murine Local Lymph Node Assay (LLNA) in specificity [59] | Human-relevant mechanisms; OECD-approved; reduces animal use [59] | Applicable to specific endpoints only; requires validation for new areas [59] |
Table 2: Key Research Reagent Solutions for NAMs in Immunology
| Reagent / Material | Function in Experiment | Example Application |
|---|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Source of primary human immune cells (T cells, B cells, monocytes, NK cells) for in vitro assays [51] | Immunophenotyping, cytokine release assays, antigen-specific response studies [51] |
| THP-1 Cell Line | A human monocytic cell line that can be differentiated into macrophage- or dendritic cell-like states [51] | Acting as antigen-presenting cells in 3D skin models or in vitro immunogenicity assays [51] |
| Microfluidic Chips | Provide a miniaturized system with fluid flow to mimic blood vessels and organ-level interactions [51] | Modeling vascular inflammation, immune cell extravasation, and multi-organ interactions [51] [91] |
| Recombinant Inflammatory Cytokines (e.g., TNF-α, IL-1β) | Used to stimulate immune responses in vitro and mimic inflammatory conditions [51] | Triggering endothelial activation in vascular models or maturation of dendritic cells [51] |
| Collagen I Matrix | A major component of the extracellular matrix providing a 3D scaffold for cell growth and tissue structure [51] | Forming the dermal layer in 3D skin models or providing a basement membrane in organ-chips [51] |
Workflow and Signaling Pathway Visualizations
NAM Benchmarking Workflow
Inflammatory Signaling in NAMs
The FDA's Innovative Science and Technology Approaches for New Drugs (ISTAND) and the European Medicines Agency's (EMA) Scientific Advice and Qualification procedures are regulatory pathways designed to support innovative drug development, including New Approach Methodologies (NAMs) that can reduce reliance on animal models [92] [93] [94]. The table below summarizes their core characteristics.
Table 1: Key Characteristics of FDA ISTAND and EMA Regulatory Pathways
| Feature | FDA ISTAND | EMA Scientific Advice & Qualification |
|---|---|---|
| Primary Focus | Qualification of novel Drug Development Tools (DDTs) not covered by other pathways [92] | Scientific advice on drug development strategy & qualification of novel methodologies [93] [94] |
| Key Outcome | Qualified DDT for a specific Context of Use (COU) [92] | CHMP Qualification Opinion or Advice; Letter of Support for promising methods [94] |
| Regulatory Scope | Tools (methods, materials, measures) independent of a specific drug [92] [95] | Advice on a specific medicine or qualification of a novel method [93] [94] |
| Binding Nature | Qualified DDT can be used in INDs, NDAs, BLAs without reconsideration [92] | Scientific advice is not legally binding for future marketing authorization [93] |
| Transparency | Public database of qualified DDTs [92] | Qualification opinions and some letters of support are published [94] |
Table 2: Typical Review Timelines for Regulatory Procedures
| Procedure | Median Review Time | Key Steps Included in Timeline |
|---|---|---|
| FDA ISTAND | Pilot program launched in 2020; permanent program established recently [95] | Multi-step process: Letter of Intent, Qualification Plan, Full Qualification Package [96] |
| EMA Scientific Advice | Review time longer than FDA for standard procedures [97] | Time from Marketing Authorization Application to European Commission decision [97] |
| FDA Expedited Programs | Shorter review times compared to EMA standard procedures [97] | Time from Investigational New Drug (IND) application to first FDA approval [97] |
Decision Pathways: Choosing the Right Regulatory Route
Navigating the correct regulatory pathway is crucial for the efficient development and endorsement of NAMs. The following workflow helps determine the most appropriate route.
Application Processes: A Step-by-Step Guide
FDA ISTAND Submission Workflow
The ISTAND program follows a defined, multi-stage submission process for qualifying a Drug Development Tool.
EMA Scientific Advice and Qualification Procedure
The EMA's process for scientific advice and qualification involves multiple steps with input from various committees and experts.
Table 3: EMA Scientific Advice and Qualification Steps
| Step | Key Actions | Stakeholders Involved |
|---|---|---|
| Registration & Request | Developer registers with EMA and submits request via IRIS portal [93] | Medicine Developer, EMA |
| Validation & Appointment | EMA validates questions; appoints two SAWP coordinators [93] | Scientific Advice Working Party (SAWP) |
| Assessment | Coordinators form teams, prepare reports, may request meetings [93] | SAWP, Assessment Teams |
| Consultation | SAWP consults other committees, working parties, and patients [93] | CAT, COMP, Patients, Experts |
| Final Response | SAWP consolidates response, adopted by CHMP and sent to developer [93] | CHMP, SAWP, Medicine Developer |
Practical Application for NAMs Research
Case Studies: Regulatory Successes for NAMs
- Organ-on-a-Chip Technology: The FDA's ISTAND program accepted its first organ-on-a-chip technology, a liver-chip model designed to predict human drug-induced liver injury (DILI), as a non-clinical drug development tool [92]. This represents a significant milestone for NAMs in replacing traditional animal models for specific toxicity tests.
- AI and Digital Health Technologies: Both ISTAND and EMA's qualification process have shown openness to AI-based tools and Digital Health Technologies. ISTAND has accepted multiple AI-based tool submissions and recognizes the use of AI for novel endpoints [92] [95]. The EMA has also published a Q&A document on qualifying digital technology-based methodologies [94].
- Non-Animal Safety Testing: ISTAND explicitly includes "novel nonclinical pharmacology/toxicology assays" and tools that assess preclinical safety without using animals as examples of suitable submissions [92] [95], directly supporting the thesis of reducing animal models.
Troubleshooting Common Regulatory Challenges
FAQ 1: What if my novel tool doesn't neatly fit the definition of a biomarker or clinical outcome assessment? The ISTAND program was specifically created for such situations. It is designed to qualify DDTs that are "out of scope for existing DDT qualification programs," including novel methodologies like tissue chips (microphysiological systems) and novel nonclinical assays [92]. The first step is to submit a Letter of Intent to ISTAND@fda.hhs.gov describing your tool and its proposed Context of Use [96].
FAQ 2: How can I get regulatory feedback early in the development of a promising NAM when I don't have full validation data? The EMA offers a mechanism for this scenario through a "Letter of Support." This is an option when a novel methodology is promising but not yet ready for full qualification. The Letter of Support encourages data generation and sharing to facilitate eventual qualification [94]. For product-specific questions, EMA Scientific Advice can provide early guidance on your development plan, including the use of novel methods [93].
FAQ 3: We are an academic group with limited regulatory experience. Which pathway is more accessible? The EMA explicitly states that scientific advice is particularly useful for developers with limited regulatory knowledge, such as academic groups [93]. You can request a preparatory meeting to familiarize yourself with the process. For tool qualification (as opposed to product-specific advice), the structured, multi-step nature of ISTAND can also provide a clear roadmap [96].
FAQ 4: Is compliance with Scientific Advice or a Qualified DDT a guarantee of regulatory approval for my drug? No. It is critical to understand that scientific advice is not legally binding [93]. Similarly, a qualified DDT, while acceptable for its specific Context of Use, does not guarantee the overall success of a drug application. The final assessment always looks at the complete evidence for the drug's benefit-risk profile, regardless of any prior advice or tool qualification [93].
Essential Research Reagent Solutions for NAMs Development
Table 4: Key Research Reagents and Materials for NAMs Development
| Reagent/Material | Function in NAMs Development | Application Example |
|---|---|---|
| Organoid Culture Media | Provides necessary nutrients and signaling molecules for the growth and maintenance of 3D organoids [73] | Developing microphysiological systems (organ-on-a-chip) [92] |
| Specialized Extracellular Matrix (ECM) | Mimics the in vivo cellular microenvironment for 3D cell culture in models like organ-on-a-chip [73] | Creating biomimetic tissue models for safety/efficacy testing [92] |
| Cell Line Sources (e.g., iPSCs) | Provides a reproducible and human-relevant cell source for constructing in vitro models [73] | Populating microphysiological systems and tissue models [92] |
| Computational Modeling Software | Enables the creation of in silico models to simulate biological processes and drug effects [73] | AI-based algorithms for patient evaluation or novel endpoints [92] |
Frequently Asked Questions (FAQs) on Regulatory Strategy for NAMs
Q1: What is a 'Safe Harbour' Data Submission? A "Safe Harbour" data submission is a regulatory mechanism that allows researchers to submit preliminary or exploratory data generated by New Approach Methodologies (NAMs) without immediate regulatory consequences. This concept encourages the early and transparent sharing of data with regulators to build confidence in novel tools, fostering a collaborative environment for assessing the validity and utility of NAMs before their formal use in pivotal safety or efficacy studies.
Q2: Why are pilot programs important for transitioning away from animal models? Pilot programs are crucial because they provide a controlled, real-world testing ground for NAMs. They allow researchers and regulators to:
- Generate Robust Evidence: Collect data on a NAM's performance, reproducibility, and predictive value.
- Identify Limitations: Understand a model's boundaries and the contexts in which it is fit-for-purpose.
- Build Collective Experience: Create a shared knowledge base across industry and regulatory bodies, which is essential for establishing qualified, standardized methods.
Q3: How do regulatory bodies currently view non-animal models? Major regulatory agencies are actively encouraging the development and use of NAMs. The U.S. National Institutes of Health (NIH) now prioritizes funding for studies that use human-based technologies over those relying solely on animal models [4]. Furthermore, the U.S. Food and Drug Administration (FDA) has published a roadmap to phase out animal testing in favor of human cell cultures, organoids, and other NAMs for drug safety trials, noting that animal models have been poor predictors of drug success for many diseases [4]. The central shift is toward accepting human-relevant data as the gold standard.
Q4: What are the common hurdles in getting regulatory acceptance for a new NAM? Common challenges you might encounter include:
- Lack of Standardization: Inconsistent protocols and performance metrics between labs.
- Technical Complexity: Sophisticated models like organ-on-chip systems can be difficult to build and reproduce across different laboratories [4].
- Demonstrating Predictive Power: Providing sufficient evidence that the NAM accurately predicts human physiology and clinical outcomes.
- Data Quality and Completeness: Submitting insufficient or poorly characterized data that fails to demonstrate the NAM's reliability.
Q5: What type of data is most critical to include in a pilot program submission to a regulator? Focus on providing comprehensive, well-documented data that demonstrates:
- Robustness and Reproducibility: Data showing consistent performance within and across your lab.
- Context of Use: A clear definition of what the NAM is intended to predict (e.g., specific drug-induced liver injury).
- Benchmarking Data: Direct comparisons to existing, accepted models (including animal data or known clinical outcomes) to establish predictive validity.
- Standardized Protocols: Detailed, step-by-step methodologies that others can follow.
Troubleshooting Guide: Common Issues with Advanced NAMs
This guide addresses specific technical challenges you may face when working with advanced NAMs, framed within the strategy of generating high-quality data for regulatory submissions.
Issue 1: Poor Reproducibility in Complex In Vitro Models (e.g., Organoids, Organs-on-Chip)
- Potential Cause: Inconsistent cell sourcing, protocol drift, or environmental fluctuations.
- Solution:
- Standardize Reagents: Use well-characterized, commercial cell lines or primary cells from reputable sources. Implement strict batch-tracking for all critical reagents.
- Document Rigorously: Maintain a detailed lab journal that records all protocol deviations, passage numbers, and environmental conditions (e.g., CO₂, humidity).
- Implement QC Checkpoints: Establish routine quality control measures, such as imaging to confirm 3D structure or testing for key biomarkers, to ensure model fidelity before starting an experiment.
Issue 2: Inadequate Representation of Human Immune System in Animal Models
- Potential Cause: Using traditional "humanized" mouse models that do not fully recapitulate the human immune response.
- Solution: Consider adopting next-generation models like the THX mouse. Unlike earlier models, THX mice are created by injecting human stem cells that develop into functional human lymph nodes, T cells, and B cells. They have been shown to mount a strong antibody response to vaccines like COVID-19, a significant improvement over previous models that failed to generate robust antibody responses [4]. This model is noted for being relatively cheap and less labour-intensive to produce [4].
Issue 3: Difficulty Capturing Complex Systemic Drug Effects (e.g., Multi-organ Toxicity)
- Potential Cause: Single-organ or 2D cell cultures cannot model inter-organ communication.
- Solution: Utilize interconnected organ-on-chip systems. These platforms can model the interaction between different human organs, such as the gut, liver, and lung, providing a snapshot of how a disease or drug affects multiple systems [4]. This is vital for predicting complex adverse events, such as those seen with CAR T-cell immunotherapies, which can cause toxicities affecting multiple organs including the brain [11].
Issue 4: Incomplete Profiling of Cellular Responses in a Heterogeneous Sample
- Potential Cause: Bulk analysis techniques mask the distinct signatures of individual cells.
- Solution: Integrate single-cell RNA sequencing (scRNA-seq) into your workflow. This method determines which genes are being transcribed in individual cells, allowing you to map specific immune cell types and pinpoint key differences in gene activity [4]. For even deeper insights, combine it with:
Key Research Reagent Solutions for Immunology NAMs
Table: Essential research reagents and models for advanced immunology research.
| Reagent/Model Name | Type | Primary Function in NAMs |
|---|---|---|
| THX Mouse Model [4] | Transgenic Animal Model | Provides a more accurate in vivo system for studying human immune responses, vaccine efficacy, and B-cell/T-cell biology. |
| Organ-on-Chip / Organoids [4] | In Vitro Human Model | Creates miniature, functional versions of human organs (e.g., gut, liver) to study disease mechanisms, drug toxicity, and inter-organ crosstalk. |
| scRNA-seq & CITE-seq [4] | Sequencing Tool | Enables deep profiling of heterogeneous cell populations at the single-cell level, mapping cell types, states, and surface protein expression simultaneously. |
| Perturb-seq [4] | Functional Genomics Tool | Uncover causal mechanisms by linking genetic perturbations (via CRISPR) to changes in gene expression profiles across thousands of single cells. |
| Naturalized Mice [11] | Animal Model | Mice exposed to diverse environmental factors to develop more "human-like" immune systems, improving the prediction of drug effects for immune diseases. |
Experimental Protocols for Key NAMs
Protocol 1: Differentiating and Characterizing Regulatory T-Cells (Tregs) in a 3D In Vitro Model The 2025 Nobel Prize in Physiology or Medicine highlighted the critical role of Tregs in maintaining immune tolerance [98] [99]. Modeling their function in vitro is a key NAM.
- Isolate Naive CD4+ T-cells: Isolate naive CD4+ T-cells from human peripheral blood mononuclear cells (PBMCs) using a magnetic bead-based cell separation kit.
- 3D Co-culture Setup: Seed the naive T-cells into a pre-established 3D immune-competent model, such as a liver or tumor spheroid that contains autologous dendritic cells.
- Treg Differentiation: To induce Treg differentiation, add recombinant human TGF-β and IL-2 to the culture medium. Include a control group with no cytokines.
- Characterization via Flow Cytometry: After 5-7 days, harvest cells from the 3D model and analyze for Treg markers using antibody staining against CD4, CD25, and FOXP3 (intracellular staining required). The expression of the transcription factor FOXP3 is the master regulator of Treg development and function [98] [26].
- Functional Suppression Assay: Co-culture the generated Tregs with fluorescently labeled, activated effector T-cells (Teffs). Measure the proliferation rate of the Teffs via flow cytometry to confirm the suppressive function of the Tregs.
Protocol 2: Utilizing THX Mice for Human Antibody Response Studies
- Model Sourcing: Acquire THX mice from a licensed provider. This model is generated by injecting human stem cells that develop into human immune components like lymph nodes and B cells [4].
- Vaccination/Immunization: Administer the vaccine or antigen of interest to the mice via an appropriate route (e.g., intramuscular, subcutaneous).
- Immune Monitoring: At designated time points post-vaccination, collect blood samples to monitor the development of a humoral immune response.
- Analysis: Use ELISA or similar assays to quantify antigen-specific human antibodies in the serum. The key advantage of the THX model is its ability to mount a strong, measurable human antibody response, which was a limitation in earlier humanized mouse models [4].
- Application: This model is particularly valuable for preclinical testing of vaccines and therapies for diseases like HIV, where a strong, specific B-cell response is critical [4].
Protocol 3: Implementing Perturb-seq to Uncover Immune Gene Function
- Design and Synthesize gRNA Library: Design a single-guide RNA (sgRNA) library targeting genes of interest (e.g., immune checkpoint genes) and a set of non-targeting controls.
- Viral Transduction: Produce a lentiviral library containing the sgRNAs and a barcode. Transduce a population of human T-cells at a low MOI to ensure most cells receive only one sgRNA.
- Selection and Expansion: Select successfully transduced cells using an antibiotic (e.g., puromycin) and allow them to expand for several days.
- Single-Cell Partitioning: Harvest the cells and load them into a single-cell RNA-sequencing platform (e.g., 10x Genomics) to capture individual cells, their native transcriptomes, and the associated sgRNA barcode in the same droplet.
- Bioinformatic Analysis: After sequencing, bioinformatically link each cell's gene expression profile to the specific genetic perturbation it received. This allows you to map the causal role of each gene on global gene expression patterns in immune cells [4].
Pathways and Workflows for Regulatory Confidence
The following diagrams illustrate the logical workflow for integrating NAMs into regulatory strategy and the key signaling pathway involved in immune tolerance.
FAQs: Navigating Global NAM Data Standards
1. What are the main objectives of global harmonization for NAM data standards? The primary objectives are to establish a collaborative platform connecting biopharma companies, researchers, regulatory bodies, and academics to standardize the measurement of assay performance, ensure consistent reporting of assay results, and harmonize the provenance of assay metadata. This aims to create a sustainable approach to reducing, replacing, and refining preclinical in vivo studies. [100]
2. What are the common hurdles faced when adopting NAMs across different organizations? Organizations validating NAM platforms often face hurdles including:
- Lack of standardization in performance qualification and method ontology.
- Absence of universal validation standards and data management frameworks.
- Poor annotation of assay metadata.
- Difficulties in integrating data sets for use in AI/ML applications. [100]
3. How do harmonized standards benefit regulatory submissions? Regulatory agency reviewers will better understand data from NAM methods when submitted in regulatory applications. Standardized data reporting simplifies the process for all parties and increases the likelihood of regulatory acceptance, potentially leading to more applications containing in vitro NAM data. [100]
4. What stakeholders are involved in developing these global standards, and how do they benefit? Key stakeholders include:
- Program leaders: Find it easier to find and evaluate human-relevant tests.
- CROs: Benefit from an industry standard that simplifies data reporting to clients.
- Assay developers: Receive clear guidance on expectations of assay users and regulators.
- Pharmaceutical companies: Reduce time and resources spent on reformatting data. [100]
5. How can researchers assess the impact of these standardization efforts? Impact can be quantified through surveys measuring researchers' willingness to use in vitro NAMs before and after project deliverables. Long-term, success can be measured by increased sales of NAM services from participating CROs or a rise in regulatory applications containing in vitro NAM data. [100]
Troubleshooting Guides for NAM Experiments
Troubleshooting Immunological Assay Performance
Problem: Inconsistent results in immune cell functional assays using primary human cells.
| Step | Action & Purpose | Technical Tips |
|---|---|---|
| 1 | Define Problem: Identify specific inconsistency (e.g., high variability in cytokine secretion, low cell viability). | Clearly outline the issue, specifying the cell type (e.g., PBMCs, T cells), the readout (e.g., ELISA, flow cytometry), and the point of failure. [101] |
| 2 | Verify Cell Source & Handling: Confirm cell viability and functionality are not compromised by isolation or shipping. | Use fresh Peripheral Blood Mononuclear Cells (PBMCs) and maintain cell viability by processing quickly; one study established feasibility within 8 hours of death with viability maintained up to 14 hours. [51] |
| 3 | Standardize Stimulation Conditions: Eliminate variability from activating agents or culture media. | Use positive controls (e.g., LPS for monocytes) and titrate stimuli concentrations. In whole blood assays (WBA), account for individual donor variability. [102] |
| 4 | Validate Key Reagents: Ensure consistency of critical reagents like cytokines and antibodies across batches. | Use multicolor flow cytometry panels with validated antibodies. A 24-color panel for human immunophenotyping facilitates high-throughput screening. [51] |
| 5 | Implement Assay Controls: Include both positive and negative controls to contextualize results and identify technical failure. | Use a reference compound or control sample in each experiment to normalize data and monitor assay performance over time. [102] |
Troubleshooting Complex In Vitro Model Systems
Problem: Failure to recapitulate systemic immune responses in multi-organ-on-chip (multi-OoC) systems.
| Step | Action & Purpose | Technical Tips |
|---|---|---|
| 1 | Define Problem: Identify the specific failure (e.g., lack of expected immune cell migration, absence of cytokine signaling). | Determine if the issue lies with a single organ model or the integrated systemic crosstalk. [101] |
| 2 | Characterize Individual Modules First: Ensure each tissue module (e.g., liver, skin) is functional before integration. | Validate individual tissue function. For example, ensure a skin model with dermal dendritic cell surrogates responds correctly to sensitizers before linking it to a lymph node module. [51] |
| 3 | Optimize Circulatory Media & Flow: Confirm the media composition and flow rates support all integrated cell types and enable cell trafficking. | Use a physiologically relevant circulation medium and flow rates that support immune cell viability and function without causing undue shear stress. [51] |
| 4 | Verify Immune Cell Competence: Ensure immune cells introduced into the system remain functional and responsive. | Source immune cells (e.g., from PBMCs) appropriately and introduce them in a way that allows for trafficking. Functional assays should confirm their activity post-culture. [51] |
| 5 | Monitor System-Level Readouts: Implement real-time, non-destructive monitoring to capture dynamic interactions. | Use transendothelial electrical resistance (TEER) in endothelial barriers to monitor integrity and real-time cytokine sampling to track immune signaling. [51] |
Key Experimental Protocols in Immunological NAMs
Protocol: Generating a 3D Immune-Competent Full-Thickness Skin Model
Purpose: To create an in vitro human skin model containing functional immune cells for assessing sensitization and inflammatory responses, reducing the need for animal skin testing. [51]
Methodology:
- Step 1: Prepare the dermal equivalent. Seed human dermal fibroblasts into a collagen-based matrix (e.g., MatriDerm) and culture until a connective tissue layer forms.
- Step 2: Incorporate immune cells. Differentiate THP-1 cells or isolate primary monocytes and seed them into the dermal equivalent as dendritic cell surrogates.
- Step 3: Form the epidermal layer. Seed human primary keratinocytes onto the dermal-immune cell construct and lift to the air-liquid interface to promote stratified epidermis formation.
- Step 4: Model application and analysis. Expose the mature model to test compounds. Assess immune activation by measuring:
- Cell viability (e.g., MTT assay).
- Dendritic cell maturation markers (e.g., CD83, CD86 via flow cytometry).
- Cytokine secretion profiles (e.g., IL-1β, IL-8 via ELISA). [51]
Protocol: Microfluidic Platform for Modeling Vascular Inflammation
Purpose: To enable real-time, high-throughput measurement of human endothelial barrier function and immune cell migration in response to inflammatory stimuli. [51]
Methodology:
- Step 1: Device preparation. Use a microfluidic platform with 64 parallel channels containing integrated electrodes for Transendothelial Electrical Resistance (TEER) measurement.
- Step 2: Endothelial cell culture. Seed human endothelial cells (e.g., HUVECs) into the microfluidic channels and culture until a stable, confluent barrier is formed, confirmed by a stable, high TEER value.
- Step 3: Inflammatory challenge. Introduce pro-inflammatory cytokines (e.g., TNF-α, IL-1β) or immune cells (e.g., monocytes, neutrophils) into the circulation.
- Step 4: Real-time monitoring and endpoint analysis.
- Continuous TEER monitoring tracks barrier integrity.
- Microscopy visualizes immune cell adhesion and transmigration.
- Endpoint immunofluorescence assesses adhesion molecule expression (e.g., ICAM-1, VCAM-1).
- Collection of effluent for cytokine analysis. [51]
Data Presentation: NAM Assay Performance Metrics
Quantitative Data from Featured NAM Studies
Table 1. Performance metrics of selected immunological NAMs from recent literature.
| NAM Platform | Key Measured Endpoint | Result / Sensitivity | Correlation with In Vivo/Clinical Data | Reference |
|---|---|---|---|---|
| 3D Skin Model with DCs | Upregulation of CD86 in response to sensitizers | Demonstrated significant increase; detected suppression by dexamethasone | Effectively mimics immune responses to known sensitizers | [51] |
| Microfluidic Vascular Model | Change in TEER after cytokine exposure | Detected significant barrier disruption in real-time across 64 channels | Platform captures key aspects of human vascular inflammation | [51] |
| In vitro DC immunogenicity assay | DC uptake, maturation, cytokine production | Good correlation with previously reported in vivo results for peptide vaccines | Useful for screening vaccine candidates before animal testing | [51] |
| Flow cytometry panel for immunotoxicity | Modulation of T cell, NK cell, B cell activation | Detected immunomodulatory effects of various chemicals; high-throughput | Uses primary human cells, offering a more human-relevant alternative | [51] |
Visualizing Workflows and Relationships
NAM Data Standardization Workflow
Multi-organ-on-chip System for Immunology
The Scientist's Toolkit: Research Reagent Solutions
Table 2. Essential reagents and materials for implementing standardized immunological NAMs.
| Item | Function & Application in NAMs | Key Considerations |
|---|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | Primary human immune cells for assays; source for deriving other immune cell types. | Use fresh isolates or well-characterized cryopreserved batches; account for donor variability. [51] |
| 3D Scaffolding Matrices (e.g., MatriDerm, collagen) | Provide structural support for 3D tissue models like skin and multi-organ systems. | Select based on pore size, stiffness, and biocompatibility to support specific cell types. [51] |
| Multicolor Flow Cytometry Antibody Panels | High-content immunophenotyping of multiple cell types and activation states from a single sample. | Panel design must account for fluorophore brightness and spillover; validation is critical. [51] |
| Microfluidic Devices with TEER Electrodes | Foundation for organ-on-chip models; enable real-time monitoring of barrier tissue integrity. | Ensure channel design matches biological question; select materials (e.g., PDMS) with low compound absorption. [51] |
| Recombinant Human Cytokines & Growth Factors | Direct cell differentiation (e.g., generating dendritic cells) and simulate inflammatory signals. | Use carrier-protein-free formulations where possible; determine optimal concentrations via titration. [51] [102] |
Conclusion
The integration of New Approach Methods into immunology represents a fundamental and necessary evolution in biomedical research. The collective insights from foundational drivers, advanced methodologies, optimization strategies, and validation frameworks underscore that NAMs are no longer futuristic concepts but are viable, often superior, tools for understanding human immune responses. The recent, decisive action from regulatory bodies like the FDA and NIH signals a permanent shift in the preclinical landscape. For researchers and drug developers, the path forward involves strategic investment in these human-relevant platforms, active participation in validation studies, and engagement with regulatory dialogue. While challenges in fully replicating the immune system's complexity remain, the accelerated development of multi-organ chips, sophisticated in silico models, and integrated testing strategies promises a future where drug development is faster, safer, more cost-effective, and fundamentally more predictive of human outcomes. Embracing this transition is critical for bridging the translational 'valley of death' and delivering the next generation of immunotherapies, vaccines, and treatments to patients.
References
- 1. Translational Therapeutics Accelerator [https://c-path.org/program/translational-therapeutics-accelerator/]
- 2. Editorial: New approach methods in immunology [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1488534/full]
- 3. the key to increasing the clinical success of immunotherapy? [https://www.nature.com/articles/s41435-023-00217-8]
- 4. Four game-changing immunology tools to watch [https://www.nature.com/articles/d41586-025-03335-7]
- 5. Day of Immunology 2025 [https://www.linkedin.com/pulse/day-immunology-2025-petasao-x2ruc]
- 6. Value of animal sepsis research in navigating the ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1593342/full]
- 7. Alternatives to Animal Testing [https://www.niehs.nih.gov/health/topics/science/sya-iccvam]
- 8. New Approach Methodologies (NAMs) in Drug Development [https://www.thermofisher.com/blog/biotechnology/new-approach-methodologies-nams-in-drug-development/]
- 9. A Recent Timeline of U.S. Actions to Reduce and Replace ... [https://emulatebio.com/alternatives-to-animal-testing-in-drug-development/]
- 10. Regulatory Applications of 3Rs - National Toxicology Program [https://ntp.niehs.nih.gov/whatwestudy/niceatm/accept-methods/apps]
- 11. Modern animal models for biomedical research ... - STAT News [https://www.statnews.com/2025/11/07/animal-research-mice-models-invaluable-biomedical-discovery/]
- 12. NIH to prioritize human-based research technologies [https://www.nih.gov/news-events/news-releases/nih-prioritize-human-based-research-technologies]
- 13. The FDA's Roadmap to Reducing Animal Testing ... [https://cytel.com/perspectives/the-fdas-roadmap-to-reducing-animal-testing-in-preclinical-safety-studies/]
- 14. FDA and NIH Announce Initiatives to Reduce Animal ... [https://www.lw.com/en/insights/fda-and-nih-announce-initiatives-to-reduce-animal-testing-and-encourage-alternative-methodologies]
- 15. FDA Announces Plan to Phase Out Animal Testing ... [https://www.fda.gov/news-events/press-announcements/fda-announces-plan-phase-out-animal-testing-requirement-monoclonal-antibodies-and-other-drugs]
- 16. FDA NAMs Roadmap: Economic and Scientific Impact ... [https://www.4dcell.com/post/fdanamsroadmap]
- 17. Human-Centric 3D Models: The NIH and FDA Push [https://insphero.com/human-centric-drug-testing/]
- 18. New Approach Methodologies: What Clinical Pharmacologists ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404678/]
- 19. New Approach Methodologies (NAMs): The Future of ... [https://emulatebio.com/new-approach-methodologies-nams-the-future-of-toxicology-and-safety-testing/]
- 20. IMMUNOLOGY - Innovation Gathers Momentum Amid New ... [https://drug-dev.com/immunology-innovation-gathers-momentum-amid-new-scientific-technological-breakthroughs/]
- 21. TGN1412 – learning from a clinical trials disaster [https://nibsc.org/about_us/worldwide_impact/tgn1412.aspx]
- 22. Severity of the TGN1412 trial disaster cytokine storm ... [https://pubmed.ncbi.nlm.nih.gov/23701319/]
- 23. TGN1412: From Discovery to Disaster - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2964774/]
- 24. New England journal report describes unique features of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1569962/]
- 25. Machine Learning Teams Push the Boundaries of Virtual ... [https://www.ericandwendyschmidtcenter.org/updates/machine-learning-teams-push-the-boundaries-of-virtual-spatial-biology-in-global-autoimmune-disease-challenge]
- 26. Nobel 2025: Immune Tolerance and 3D In Vitro Models [https://insphero.com/nobel2025-celebrating-discoveries-in-immune-tolerance/]
- 27. Why a human-first approach is the future of drug discovery [https://www.drugdiscoverynews.com/why-a-human-first-approach-is-the-future-of-drug-discovery-16647]
- 28. Systems immunology: When systems biology meets immunology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447193/]
- 29. Artificial intelligence for autoimmune diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552663/]
- 30. A guide to the organ-on-a-chip [https://www.nature.com/articles/s43586-022-00118-6]
- 31. Integration of immune cells in organs-on-chips: a tutorial - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10267470/]
- 32. In vitro immunity: an overview of immunocompetent organ- ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1373186/full]
- 33. PhysioMimix® Core Microphysiological System MPS [https://cn-bio.com/physiomimix-core/]
- 34. Expanding the Frontiers of Human Biology with Organ-on-a ... [https://emulatebio.com/expanding-the-frontiers-of-human-biology-with-organ-on-a-chip-technology-highlights-from-the-2025-mps-world-summit/]
- 35. Protocol for generating and analyzing organ-on-chip using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11066468/]
- 36. NIH, FDA plan to reduce animal testing draws mixed reactions ... [https://www.statnews.com/2025/07/25/nih-fda-alternatives-to-animal-testing-new-rules-breakdown/]
- 37. Leveraging In Silico and Artificial Intelligence Models to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180087/]
- 38. Physiologically-based Pharmacokinetic Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC5204363/]
- 39. PBPK Modeling & Simulation in Drug Development [https://www.allucent.com/resources/blog/pbpk-modeling-and-simulation-drug-development]
- 40. In Silico Studies to Support Vaccine Development [https://www.mdpi.com/1999-4923/15/2/654]
- 41. Artificial intelligence-, organoid-, and organ-on-chip-powered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615408/]
- 42. Artificial intelligence in preclinical research: enhancing ... [https://www.sciencedirect.com/science/article/pii/S135964462500073X]
- 43. Opportunities for machine learning and artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12573771/]
- 44. Development of Best Practices in Physiologically Based ... [https://www.fda.gov/drugs/news-events-human-drugs/development-best-practices-physiologically-based-pharmacokinetic-modeling-support-clinical]
- 45. Flow Cytometry Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/flow-cytometry-troubleshooting-guide?srsltid=AfmBOopG8mVv84vgcCJhKG4-120FeD6Te-SLD5AkSmnbS_O6WA-fEOWU]
- 46. Flow Cytometry Troubleshooting Guide [https://www.novusbio.com/support/support-by-application/flow-cytometry/troubleshooting?srsltid=AfmBOoopQjF9LT2SK35NWt1VI0PktsABonx8pRKvhiMViAK0QrsifW4A]
- 47. Identifying and fixing errors in flow data [https://www.colibri-cytometry.com/post/identifying-and-fixing-errors-in-flow-data]
- 48. 3D bioprinting – Flow cytometry as analytical strategy for ... [https://www.sciencedirect.com/science/article/abs/pii/S2405886618300034]
- 49. 3-D tissue culture systems for the evaluation and optimization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2652657/]
- 50. New Approach Methodologies (NAMs) [https://www.washington.edu/aco3rs/2025/07/18/nams-2/]
- 51. Editorial: New approach methods in immunology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11445123/]
- 52. Precision-Cut Tumor Slices (PCTS) as an Ex Vivo Model in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9036232/]
- 53. Ex-Vivo Treatment of Tumor Tissue Slices as a Predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7016787/]
- 54. Ex vivo organotypic culture system of precision-cut slices ... [https://www.nature.com/articles/s41598-019-38603-w]
- 55. the UPTIDER post-mortem tissue donation program [https://www.nature.com/articles/s41523-024-00637-3]
- 56. Brain Tissue Donation Explained: Answers to Frequently ... [https://braintumor.org/news/brain-tissue-donation-explained-answers-to-frequently-asked-questions/]
- 57. New Approach Methodologies (NAMs): Advances in ... [https://www.axionbiosystems.com/new-approach-methodologies-nams-advances-preclinical-safety-studies]
- 58. New Approach Methods in Immunology [https://www.frontiersin.org/research-topics/55518/new-approach-methods-in-immunology/magazine]
- 59. New approach methodologies (NAMs): identifying and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10964841/]
- 60. Methods integrating innate and adaptive immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12133800/]
- 61. 7 Tips for Navigating the Complexities of NAMs [https://www.altasciences.com/resource-center/blog/7-tips-navigating-complexities-vitro-nams-studies]
- 62. Investigating immunity | Nature Methods [https://www.nature.com/articles/s41592-024-02286-7]
- 63. Adaptive immune system [https://en.wikipedia.org/wiki/Adaptive_immune_system]
- 64. 5 Questions: Mark Davis on why immunology research needs ... [https://med.stanford.edu/news/all-news/2022/070/mark-davis-5-questions.html]
- 65. Human immune diversity: from evolution to modernity [https://www.nature.com/articles/s41590-021-01058-1]
- 66. Diversity in immunogenomics: the value and the challenge [https://pmc.ncbi.nlm.nih.gov/articles/PMC8842483/]
- 67. Human immune system: Exploring diversity across ... [https://www.sciencedirect.com/science/article/pii/S2405844025002166]
- 68. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 69. Protocols & Troubleshooting Guides [https://www.rndsystems.com/resources/protocols-troubleshooting-guides]
- 70. Metabolomics Quality Control, Reproducibility & Validation [https://www.arome-science.com/metabolomics-faqs/metabolomics-quality-control-reproducibility-method-validation-guide/]
- 71. Assessing the reproducibility of diagnostic tests across different... [https://editverse.com/assessing-the-reproducibility-of-diagnostic-tests-across-different-laboratories-and-settings/]
- 72. - Cross of machine learning models for copper... laboratory validation [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d5dd00335k]
- 73. New Approach Methodologies [https://oacu.oir.nih.gov/new-approach-methodologies]
- 74. Generative AI Enhancing Reproducibility in Pharma Experiment [https://www.pharmaadvancement.com/market-moves/generative-ai-enhancing-reproducibility-in-pharma-experiments/]
- 75. Context of Use [https://www.fda.gov/drugs/biomarker-qualification-program/context-use]
- 76. Drug Development Tool (DDT) Qualification Programs [https://www.fda.gov/drugs/development-approval-process-drugs/drug-development-tool-ddt-qualification-programs]
- 77. The Art of Troubleshooting for Customer Support ... [https://www.helpscout.com/helpu/art-of-troubleshooting-support/]
- 78. The complete guide to customer service troubleshooting [https://devrev.ai/blog/customer-service-troubleshooting]
- 79. Why Multi-Omics Data Integration Often Fails [https://www4.accurascience.com/blogs_44_0.html]
- 80. 10 Tips for Successful High Content Screening (HCS) Assays [https://www.enzo.com/note/10-tips-for-successful-high-content-screening-hcs-assays/]
- 81. Ten quick tips for avoiding pitfalls in multi-omics data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10325053/]
- 82. 2025 Trends: Multiomics [https://www.genengnews.com/topics/omics/2025-trends-multiomics/]
- 83. Advancing drug discovery through multiomics [https://www.ddw-online.com/advancing-drug-discovery-through-multiomics-37448-202510/]
- 84. Clinical Trial Designs for Predictive Biomarker Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2734400/]
- 85. A machine learning framework supporting prospective ... [https://www.nature.com/articles/s41746-022-00660-3]
- 86. Developing clinical prediction models: a step-by-step guide [https://pmc.ncbi.nlm.nih.gov/articles/PMC11369751/]
- 87. Model-Informed Drug Development Paired Meeting Program [https://www.fda.gov/drugs/development-resources/model-informed-drug-development-paired-meeting-program]
- 88. Translatability of Animal Models for Alzheimer's Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603623/]
- 89. Modelling and simulation: questions and answers [https://www.ema.europa.eu/en/human-regulatory-overview/research-and-development/scientific-guidelines/clinical-pharmacology-pharmacokinetics/modelling-simulation-questions-answers]
- 90. New Approach Methodologies (NAMs) and Important Tips [https://www.herox.com/blog/1115-new-approach-methodologies-nams-and-important-tips]
- 91. Non-Animal & Human-Relevant Research News [https://riseforanimals.org/news/sci-news-sept-2025/]
- 92. ISTAND Program [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/innovative-science-and-technology-approaches-new-drugs-istand-program]
- 93. Scientific advice and protocol assistance [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-advice-protocol-assistance]
- 94. Qualification of novel methodologies for medicine development [https://www.ema.europa.eu/en/qualification-novel-methodologies-medicine-development]
- 95. FDA Advances Drug Development Innovation by ... [https://www.fda.gov/news-events/fda-voices/fda-advances-drug-development-innovation-establishing-istand-permanent-qualification-program]
- 96. ISTAND Program Submission Process [https://www.fda.gov/drugs/innovative-science-and-technology-approaches-new-drugs-istand-program/innovative-science-and-technology-approaches-new-drugs-istand-program-submission-process]
- 97. Food and Drug Administration vs European Medicines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6983504/]
- 98. Research identifying immune system regulators wins ... [https://www.healio.com/news/rheumatology/20251008/research-illuminating-powerful-regulators-of-the-immune-system-wins-nobel-prize]
- 99. Nobel honours discovery of regulatory T cells, and other ... [https://www.weforum.org/stories/2025/10/health-news-immune-tcells-nobel-covid/]
- 100. In Vitro NAM Data Standards [https://www.pistoiaalliance.org/project/in-vitro-nam-data-standards/]
- 101. What Is a Troubleshooting and 6 Steps to Create... Guide [https://clickhelp.com/clickhelp-technical-writing-blog/troubleshooting-guide-definition-importance-and-tips-for-creating/]
- 102. New approach methodologies to assess wanted and ... [https://www.sciencedirect.com/science/article/pii/S2666027X25000088]