Beyond the Petri Dish: Revolutionizing Immune Response Assessment with Advanced 3D Cell Culture Models
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on utilizing 3D cell culture systems for immune response assessment.
Beyond the Petri Dish: Revolutionizing Immune Response Assessment with Advanced 3D Cell Culture Models
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on utilizing 3D cell culture systems for immune response assessment. It explores the fundamental advantages of 3D models over traditional 2D cultures in replicating the physiological complexity of the immune system. The guide details key methodologies, including organoids, spheroids, and scaffold-based systems, for applications in immuno-oncology, infectious disease modeling, and immunotoxicity testing. It addresses common challenges in co-culture, media optimization, and endpoint analysis, offering troubleshooting and optimization strategies. Finally, the article critically evaluates the validation of these models against in vivo data and compares the performance of different 3D platforms, synthesizing their transformative potential for predictive preclinical research.
The 3D Immune Microenvironment: Why Flat Biology Falls Short
Limitations of 2D Monolayers for Immune Cell Function and Signaling
Application Notes
The evaluation of immune cell function—including activation, signaling, migration, and cytotoxicity—has traditionally relied on 2D monolayer cultures. However, within the broader thesis of developing physiologically relevant 3D cell culture models for immune response assessment, the limitations of 2D systems become critically apparent. These limitations compromise data translation and drug development efficacy.
Key limitations are summarized quantitatively below:
Table 1: Comparative Functional Deficits of Immune Cells in 2D vs. 3D Contexts
| Functional Parameter | Observation in 2D Monolayer | Reported Quantitative Discrepancy vs. 3D/ In Vivo | Implication for Signaling & Function |
|---|---|---|---|
| T Cell Cytotoxicity | Hyper-activated, non-physiological kinetics | Up to 10-100x faster target killing in 2D vs. 3D spheroid models. | Overestimates potency; misses spatial barriers to immune synapse formation. |
| Immune Synapse Maturity | Altered architecture, sustained calcium signaling | Only ~40% of 2D synapses show canonical mature structure vs. ~70% in 3D matrices. | Aberrant downstream signaling (NFAT, NF-κB) and cytokine production profiles. |
| Macrophage Polarization | Binary M1/M2 shift, loss of spectrum | 3D matrices can induce a 2-5 fold increase in distinct hybrid phenotype markers (e.g., CD206+/TNFα+). | Oversimplifies signaling pathways, failing to model tissue-specific nuance. |
| Dendritic Cell (DC) Migration | Amoeboid, non-adhesive, rapid | Migration speed in 2D (∼10 µm/min) can be 3-5x faster than in 3D confinement (∼2-4 µm/min). | Misrepresents chemokine/receptor requirements and tissue traversal signaling. |
| Cell-Cell Contact Dynamics | Forced, planar, uniform adhesion | Immune cell-tumor cell contact probability in 2D is near 100%, vs. highly variable in 3D spheroids. | Artificially elevates adhesion (e.g., ICAM-1/LFA-1) signaling initiation. |
| Cytokine Secretion Profile | Elevated pro-inflammatory baselines | IL-6 and TNF-α secretion from LPS-stimulated macrophages can be 2-3x higher in 2D vs. 3D. | Skews understanding of feedback loops and paracrine signaling networks. |
These deficits stem from fundamental discrepancies: the lack of mechanical and biochemical extracellular matrix (ECM) cues, altered receptor geometry and clustering, simplified diffusion gradients, and absence of spatial heterogeneities found in tissues.
Experimental Protocols
Protocol 1: Assessing T Cell Cytotoxicity Kinetics in 2D vs. 3D Objective: To quantitatively compare the kinetics of cytotoxic T lymphocyte (CTL)-mediated killing of target cells in conventional 2D monolayers versus in 3D tumor spheroids. Materials: Primary human CD8+ T cells (activated), GFP-labeled tumor cell line (e.g., A549), 96-well flat-bottom & ultra-low attachment plates, live-cell imaging microscope, fluorescent dye for dead cells (e.g., propidium iodide, PI).
- 3D Spheroid Generation: Seed 5x10^3 GFP+ tumor cells/well in U-bottom ultra-low attachment plate. Centrifuge at 300xg for 3 min. Culture for 72h to form compact spheroids.
- T Cell Activation: Isolate and activate CD8+ T cells with anti-CD3/CD28 beads and IL-2 for 5-7 days.
- Co-culture Setup: 2D Condition: Seed 1x10^4 GFP+ tumor cells/well in flat-bottom plate. Adhere overnight. 3D Condition: Transfer single spheroids to collagen I matrix-filled wells or use pre-formed spheroids in U-plates. Add activated CTLs at an effector:target (E:T) ratio of 5:1 to both conditions.
- Real-Time Cytotoxicity Assay: Add PI (1 µg/mL) to all wells. Using live-cell imaging, acquire GFP (tumor cells) and PI (dead cells) fluorescence images every 20 minutes for 24-48h.
- Analysis: Quantify the time from first T cell contact to target cell death (PI+/GFP+). Plot Kaplan-Meier survival curves of target cells and compare median time to death between 2D and 3D conditions.
Protocol 2: Profiling Macrophage Signaling in 2D Plastic vs. 3D Matrigel Objective: To analyze early kinase signaling and downstream polarization markers in macrophages cultured on 2D plastic versus embedded within a 3D ECM. Materials: THP-1 cells or primary human monocyte-derived macrophages (MDMs), PMA, 3D Cultrex or Matrigel, phospho-flow cytometry antibody panel (e.g., p-p38, p-STAT1, p-STAT3, p-Akt), polarization markers (CD80, CD206, ARG1).
- Macrophage Differentiation: Differentiate THP-1 cells with 100 nM PMA for 48h. For MDMs, use M-CSF (50 ng/mL) for 6 days.
- 3D Culture Setup: Suspend differentiated macrophages at 1x10^6 cells/mL in chilled 3D Matrigel (∼4 mg/mL). Plate 50 µL drops in pre-warmed plates, allow to polymerize at 37°C for 30 min, then add culture media.
- 2D Control: Plate cells at same density on standard tissue culture plastic.
- Stimulation & Fixation: After 24h culture, stimulate with LPS (100 ng/mL) + IFN-γ (20 ng/mL) or IL-4 (20 ng/mL) for 15 min (phospho-signaling) or 24h (polarization markers). Immediately fix cells with 1.6% PFA for 10 min at 37°C.
- Processing & Staining: For 3D samples, dissolve Matrigel using Cell Recovery Solution (30 min, 4°C). Permeabilize all cells with ice-cold 90% methanol. Stain with phospho-specific or surface marker antibodies.
- Analysis: Acquire on a flow cytometer. Compare median fluorescence intensity (MFI) of phospho-proteins and co-expression patterns of M1/M2 markers. Note the distribution breadth and presence of hybrid populations in 3D.
Visualizations
Title: 2D vs 3D Immune Signaling Limitation Roots
Title: Protocol Workflow for Quantifying 2D Limitations
The Scientist's Toolkit
Table 2: Essential Research Reagents for 2D vs. 3D Immune Cell Studies
| Reagent / Material | Function & Application | Key Consideration for 3D Studies |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Promotes spontaneous aggregation of cells into 3D spheroids by inhibiting adhesion. | U-bottom wells standardize spheroid size and location for imaging. |
| Basement Membrane Extract (BME, e.g., Matrigel) | Provides a complex, physiological 3D ECM environment for cell embedding. | Lot variability, temperature sensitivity, and growth factor content must be characterized. |
| Collagen I Hydrogels | Offers a tunable, defined 3D matrix to study the impact of stiffness and ligand density on immune function. | Polymerization pH and temperature are critical for reproducibility. |
| Live-Cell Imaging-Compatible Dyes (e.g., PI, Calcein-AM) | Enable real-time, longitudinal tracking of cell viability and killing kinetics in opaque 3D structures. | Penetration depth into 3D models and toxicity with long-term exposure must be validated. |
| Phospho-Specific Flow Cytometry Antibodies | Allow multiplexed, single-cell analysis of intracellular signaling pathway activation. | Requires optimized 3D matrix dissolution and cell recovery protocols to preserve phospho-epitopes. |
| Cytokine Bead Array (CBA) or Multiplex ELISA | Quantify a broad spectrum of soluble mediators in conditioned media from 3D cultures. | Cytokine binding to 3D matrix components may require validation of recovery efficiency. |
| Microfluidic 3D Culture Chips | Enable generation of precise chemokine gradients and study of immune cell migration in 3D confinements. | Integration with downstream analysis (e.g., cell retrieval for sequencing) can be challenging. |
Application Notes
Within the broader thesis on advancing 3D cell culture for immune response assessment, the recreation of physiologically relevant cell-cell and cell-ECM interactions is paramount. These models move beyond 2D monocultures by incorporating spatial architecture, biomechanical cues, and multicellular complexity, leading to more predictive data for therapeutic screening and mechanistic studies.
- Cell-Cell Interactions: 3D models facilitate crucial immune interactions such as antigen presentation by dendritic cells to T cells, immune synapse formation, and cytotoxic T cell/NK cell serial killing of tumor cells. These interactions are governed by spatially organized ligand-receptor engagements and paracrine signaling gradients absent in 2D.
- Cell-ECM Interactions: The ECM in 3D models (e.g., collagen, Matrigel, synthetic hydrogels) provides not just structural support but also biochemical (e.g., cryptic peptide exposure, growth factor sequestration) and biophysical (e.g., stiffness, porosity) signals. These cues direct immune cell infiltration, migration modes (mesenchymal vs. amoeboid), and activation states, closely mimicking tissue-specific immune contexts like tumor microenvironments or lymph nodes.
The following tables summarize quantitative findings from recent studies highlighting the enhanced physiological relevance of 3D immune models.
Table 1: Comparative Metrics of Immune Cell Cytotoxicity in 2D vs. 3D Co-Culture Models
| Metric | 2D Monolayer Co-Culture | 3D Spheroid/Tumor Model (Collagen/Matrigel) | Physiological Reference (in vivo estimates) | Key Implication |
|---|---|---|---|---|
| Cytotoxic T Cell (CTL) Penetration Depth | Not applicable (monolayer) | 50-150 µm from spheroid periphery | 100-200 µm into tumor tissue | 3D models recapitulate physical infiltration barriers. |
| Target Cell Killing Rate | High; often 80-100% within 24-48h | Reduced and heterogeneous; 30-70% over 72-96h | Variable; often inefficient in solid tumors | 3D models show limited efficacy akin to immunosuppressive TME. |
| Cytokine Secretion (e.g., IFN-γ) | High, often supra-physiological | Modulated, forming concentration gradients | Gradients present in tissue | 3D paracrine signaling is spatially constrained. |
| Immune Synapse Stability | Large, stable, symmetric | Transient, asymmetric, migratory | Dynamic and adaptable in tissue | 3D architecture dictates synapse mechanics. |
Table 2: Impact of ECM Properties on Immune Cell Behavior in 3D Models
| ECM Parameter | Experimental Range Tested | Observed Effect on Immune Cells | Proposed Mechanism |
|---|---|---|---|
| Stiffness (Elastic Modulus) | 0.5 kPa (brain-like) to 20 kPa (bone-like) | >5 kPa promotes pro-inflammatory macrophage polarization (M1); Softer matrices (<2 kPa) favor regulatory phenotypes. | Mechanotransduction via integrins and TRPM7 channels. |
| Ligand Density (e.g., RGD) | 0.1 to 1.0 mM in PEG hydrogels | Optimal CTL migration and tumor killing at intermediate density (0.5 mM); Too high or low impairs motility. | Balanced adhesion vs. de-adhesion required for migration. |
| Matrix Porosity / Fiber Size | Collagen density: 1-5 mg/ml | High density (>3 mg/ml) restricts lymphocyte trafficking, enhances macrophage protrusive invasion. | Physical hindrance and matrix remodeling requirements. |
| Degradability (Protease Sites) | Non-degradable vs. MMP-degradable hydrogels | MMP-degradable matrices are essential for CD8+ T cell expansion and cluster formation within tumors. | Space must be cleared for proliferation and colony formation. |
Experimental Protocols
Protocol 1: Generation of 3D Tumor Immune Microenvironment (TIME) Spheroids for Cytotoxicity Assays
Objective: To establish a reproducible co-culture spheroid model containing cancer cells and stromal fibroblasts, then infiltrate with immune cells to assess killing and migration.
Materials: See "Research Reagent Solutions" table. Procedure:
- Spheroid Formation: Seed U-87 MG glioblastoma cells and human dermal fibroblasts (HDFs) at a 4:1 ratio (e.g., 1000:250 cells/well) in a 96-well ultra-low attachment (ULA) round-bottom plate in 150 µL of complete cancer cell medium.
- Centrifugation: Centrifuge the plate at 300 x g for 3 minutes to aggregate cells at the well bottom.
- Culture: Incubate at 37°C, 5% CO₂ for 72 hours to form compact, spherical co-culture spheroids.
- ECM Embedding: Prepare a chilled working solution of rat tail Collagen I (3 mg/mL) in neutralization buffer (e.g., using 10X PBS and 0.1M NaOH). Gently aspirate medium from each spheroid well. Using wide-bore tips, mix each spheroid with 50 µL of collagen solution and transfer to a well of a flat-bottom 96-well plate. Incubate at 37°C for 30 minutes to polymerize.
- Immune Cell Addition: Isolate human peripheral blood mononuclear cells (PBMCs) via Ficoll density gradient. Activate CD8+ T cells using anti-CD3/CD28 beads and IL-2 for 5-7 days. Gently layer 100 µL of medium containing 2x10⁴ activated CD8+ T cells onto the set collagen gel containing the spheroid.
- Imaging & Analysis: Culture for 3-5 days. Image live/dead staining (Calcein-AM/Propidium Iodide) or use fluorescently labeled cells daily via confocal microscopy. Quantify T cell infiltration distance from spheroid edge and calculate spheroid viability area over time.
Protocol 2: Assessing Macrophage Phenotype in Tuneable 3D Hydrogels
Objective: To evaluate the effect of ECM stiffness and ligand density on human macrophage polarization.
Materials: See "Research Reagent Solutions" table. Procedure:
- Hydrogel Precursor Preparation: Prepare a 4-arm PEG-maleimide (PEG-4MAL) stock solution (e.g., 20 mM in PBS). Separately, prepare adhesive peptide (RGD, e.g., GCGYGRGDSPG) and MMP-degradable crosslinker (e.g., KCGPQG~IWGQCK) stocks.
- Macrophage Encapsulation: Differentiate THP-1 monocytes into macrophages using PMA. Resuspend macrophages at 2x10⁶ cells/mL in PBS. For a 100 µL gel, mix:
- 50 µL of 2X PEG-4MAL solution.
- Adhesive and crosslinker peptides to desired final concentrations (e.g., 1.0 mM RGD, 2.5 mM crosslinker).
- 50 µL of cell suspension.
- Initiate gelation by adding a small volume of a thiol-containing catalyst (e.g., DTT).
- Gel Casting: Quickly pipet the mixture into a silicone mold or well plate and incubate at 37°C for 15-20 minutes for complete crosslinking. Add complete macrophage medium.
- Polarization Stimuli: Polarize macrophages towards M1 (add 100 ng/mL LPS + 20 ng/mL IFN-γ) or M2 (add 20 ng/mL IL-4) states for 48 hours.
- Analysis: Harvest RNA from lysed gels for qPCR analysis of markers (M1: TNF-α, IL-6, iNOS; M2: ARG1, CD206, CCL18). Alternatively, fix gels, section, and immunostain for surface markers. Analyze cytokine secretion in conditioned media via ELISA.
Visualizations
Title: ECM Signals Drive Immune Cell Fate in 3D
Title: 3D Tumor Cytotoxicity Assay Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in 3D Immune Models |
|---|---|
| Ultra-Low Attachment (ULA) Plates | Promotes spontaneous 3D aggregation of cells into spheroids or organoids via forced suspension. Essential for forming core cellular structures. |
| Rat Tail Collagen I | Natural, biocompatible ECM hydrogel. Polymerizes at physiological pH/temp. Used to embed spheroids, providing a migratory/infiltration matrix for immune cells. |
| Matrigel / Basement Membrane Extract | Complex, tumor-derived ECM mixture rich in laminin, collagen IV. Used to model specialized microenvironments like epithelial barriers or for organoid culture. |
| Synthetic Hydrogels (e.g., PEG-4MAL) | Defined, tunable polymers. Functionalization with peptides (RGD for adhesion, MMP sites for degradability) allows precise control over biochemical and mechanical properties. |
| Transwell / Boyden Chambers (3D) | Used to study chemotaxis and invasion. Immune cells in top chamber migrate through a porous membrane into a 3D ECM or cell-laden matrix below. |
| Live-Cell Imaging Dyes (Calcein-AM/PI) | Vital dyes for longitudinal viability assessment in 3D cultures. Calcein-AM (green, live) and Propidium Iodide (red, dead) allow quantification of cytotoxic effects. |
| Cytokine ELISA / LEGENDplex Kits | Quantify soluble immune mediators (cytokines, chemokines) secreted into the conditioned media of 3D co-cultures, revealing functional immune activation/suppression. |
| Confocal/Multiphoton Microscopy | Critical for deep-tissue imaging of 3D models. Enables 3D reconstruction of immune cell localization, interactions, and viability within thick ECM or spheroids. |
The accurate assessment of immune cell function and therapeutic response in vitro requires a microenvironment that recapitulates key physiological features. Traditional 2D culture systems lack the spatial, biochemical, and biomechanical cues present in vivo, leading to altered cellular phenotypes and functions. This application note, framed within a thesis on 3D cell culture for immune response assessment, details the core stromal components—stromal cells, the extracellular matrix (ECM), and physiochemical gradients—and provides protocols for their implementation. These elements are fundamental for constructing predictive models of immunomodulation, tumor-immune interactions, and lymph node function.
Defining the Core Components
Stromal Cells
Stromal cells are non-immune, structural cells that provide essential support, regulation, and organization within tissues. In immune contexts, they are critical for lymphocyte survival, antigen presentation, and the orchestration of immune responses.
Primary Stromal Cell Types in Immune Tissues:
| Cell Type | Primary Tissue Location | Key Functions in Immunity | Common 3D Co-culture Use |
|---|---|---|---|
| Mesenchymal Stromal/Stem Cells (MSCs) | Bone Marrow, Adipose, Umbilical Cord | Immunosuppression, T-cell modulation, secretome release, wound healing. | Modeling immunosuppressive tumor microenvironment (TME). |
| Fibroblasts | Ubiquitous in connective tissue | ECM deposition & remodeling, cytokine/chemokine secretion, structural support. | Modeling stromal barriers in solid tumors; lymph node fibroblastic reticular cells (FRCs). |
| Endothelial Cells | Blood & Lymphatic Vessels | Leukocyte trafficking (extravasation), antigen presentation, cytokine secretion. | Modeling vascularized TME or studying immune cell transmigration. |
| Adipocytes | Adipose Tissue | Metabolic regulation, secretion of adipokines (e.g., leptin), moderate immunomodulation. | Modeling obesity-associated cancer or adipose tissue immunity. |
Extracellular Matrix (ECM)
The ECM is a complex 3D network of proteins and polysaccharides that provides structural integrity and biochemical signaling. Its composition and mechanical properties (stiffness, porosity) directly influence immune cell behavior.
Key ECM Components and Properties:
| Component | Primary Source | Key Properties & Role in Immune Response | Typical Concentration in 3D Hydrogels |
|---|---|---|---|
| Collagen I | Fibroblasts, MSCs | Most abundant in vivo; provides tensile strength; influences macrophage polarization. | 1.5 - 5.0 mg/mL |
| Matrigel/Basement Membrane Extract | Engelbreth-Holm-Swarm mouse sarcoma | Contains laminin, collagen IV, entactin; rich in growth factors; supports complex morphogenesis. | 3 - 10 mg/mL |
| Fibrin | Polymerized fibrinogen | Forms clot matrix; involved in wound healing and inflammation; adaptable stiffness. | 2 - 10 mg/mL |
| Hyaluronic Acid (HA) | Many cell types | Glycosaminoglycan; regulates hydration, cell motility; CD44 receptor binding on immune cells. | 0.5 - 2.0% (w/v) |
| Alginate | Brown algae (synthetic) | Bio-inert, ionically cross-linked; allows precise control of stiffness; often functionalized with RGD peptides. | 1 - 3% (w/v) |
Physiochemical Gradients
Gradients of soluble factors (chemokines, oxygen, nutrients) and physical properties (stiffness, density) are hallmarks of in vivo tissues and are critical for directing immune cell migration, differentiation, and activity.
Key Gradients in Immune Response:
| Gradient Type | Physiological Role | Method for Generation in 3D Culture | Measurable Parameters |
|---|---|---|---|
| Chemokine (e.g., CXCL12, CCL19/21) | Directed leukocyte homing & positioning in lymphoid organs. | Microfluidic pumps, source-sink hydrogels. | Concentration (pg/mL), steepness (ΔC/μm). |
| Oxygen (O₂) | Hypoxic cores in tumors & wounds alter immune cell metabolism/function. | Controlled atmosphere chambers, oxygen-consuming particles. | % O₂ (Normoxia: 20%, Physiologic: 1-10%). |
| Matrix Stiffness | Impacts T-cell activation, migration mode (mesenchymal vs. amoeboid). | Stiffness-gradient hydrogels (e.g., patterned methacrylated HA). | Elastic Modulus (kPa). |
Application Notes & Protocols
Protocol 3.1: Establishing a 3D Co-culture of Tumor Spheroids with Stromal Fibroblasts for T-cell Infiltration Assays
Objective: To model the physical and biochemical barrier of cancer-associated fibroblasts (CAFs) in the TME and assess cytotoxic T lymphocyte (CTL) infiltration and function.
The Scientist's Toolkit:
| Reagent/Material | Function/Explanation |
|---|---|
| HT-1080 (Fibrosarcoma) or Patient-Derived Tumor Cells | Core tumor cell component for spheroid formation. |
| Primary Human Dermal Fibroblasts (CAF-like) | Stromal barrier component; can be activated with TGF-β. |
| CD8+ T-cells (Primary or CAR-T) | Effector immune cell for infiltration & killing assay. |
| Type I Collagen, Rat Tail | Physiological 3D ECM scaffold. |
| CellTracker Dyes (CMFDA, CMTMR) | For fluorescent labeling of distinct cell populations. |
| Live-Cell Imaging Microscope with Z-stack | For time-lapse tracking of T-cell infiltration. |
| Cytotoxicity Assay Kit (LDG or Caspase-3/7) | To quantify tumor cell killing in 3D. |
Methodology:
- Spheroid Formation: Generate tumor cell spheroids (500-1000 cells) using a U-bottom ultra-low attachment plate over 48-72 hours.
- CAF Embedding & ECM Casting:
- Prepare a neutralized collagen I solution (2.5 mg/mL) on ice.
- Trypsinize and resuspend fibroblasts at 2x10⁶ cells/mL in complete medium.
- Mix fibroblast suspension 1:1 with the collagen solution. Final concentration: 1x10⁶ cells/mL, 1.25 mg/mL collagen.
- Transfer 50 μL droplets of the cell-collagen mix to a pre-warmed 24-well plate. Place one pre-formed tumor spheroid into the center of each droplet. Incubate at 37°C for 30 min to gel.
- Gently overlay with 500 μL complete medium. Culture for 24-48h to allow fibroblast network formation.
- T-cell Introduction & Assay:
- Label T-cells with CellTracker CMFDA.
- Carefully add 1x10⁵ labeled T-cells in 50 μL medium on top of each gel.
- After 4h, gently wash non-infiltrated T-cells from the surface.
- Perform live-cell imaging every 6h for 72h to track T-cell movement (tracking depth >200μm). Quantify infiltration distance and spheroid contact.
- At endpoint, measure tumor cell cytotoxicity using a lactate dehydrogenase (LDH) release assay specific for 3D cultures.
Protocol 3.2: Generating a Stable Chemokine Gradient in a 3D Hydrogel for Dendritic Cell (DC) Migration Studies
Objective: To create a linear CXCL12 gradient within a fibrin hydrogel to study DC chemotaxis in a 3D lymphoid tissue model.
The Scientist's Toolkit:
| Reagent/Material | Function/Explanation |
|---|---|
| Fibrinogen from Human Plasma | Base hydrogel polymer, cross-linked by thrombin. |
| Human Recombinant CXCL12/SDF-1α | Chemokine source for gradient formation. |
| Microfluidic Gradient Generator or Chemotaxis Chamber | Device to establish and maintain a stable linear gradient. |
| Primary Human Monocyte-Derived Dendritic Cells | Migratory immune cell population. |
| Calcein-AM | Viable cell fluorescent label for migration tracking. |
| Confocal Microscope with Environmental Chamber | For 3D visualization of cell trajectories within the gradient. |
Methodology:
- Gradient Chamber Assembly: Use a commercially available 3D chemotaxis chamber (e.g., µ-Slide Chemotaxis) following manufacturer instructions. The central channel will hold the hydrogel.
- Hydrogel Loading with Sink Concentration:
- Prepare a fibrinogen solution (5 mg/mL) in serum-free medium.
- Mix with 0.1 U/mL thrombin and load into the central gel channel. Allow to polymerize for 15 min at 37°C.
- Load medium containing a low "sink" concentration of CXCL12 (e.g., 10 ng/mL) into one reservoir channel.
- Source Introduction & Gradient Establishment:
- Load medium containing a high "source" concentration of CXCL12 (e.g., 200 ng/mL) into the opposite reservoir channel.
- Allow the system to equilibrate by passive diffusion for 4-6 hours to establish a stable linear gradient across the hydrogel.
- DC Seeding and Migration Analysis:
- Label DCs with Calcein-AM.
- Gently aspirate medium from the "sink" side of the gel channel and introduce 2x10⁴ DCs in 20 μL.
- Allow cells to adhere to the gel interface for 30 min.
- Carefully refill both reservoir channels with their respective media (source & sink) to maintain the gradient.
- Image immediately (t=0) and at 30-min intervals for 6-12h using a confocal microscope.
- Analyze cell trajectories using tracking software (e.g., ImageJ Manual Tracking). Calculate directionality (cosine of angle vs. gradient), velocity, and forward migration index (FMI).
Visualization of Concepts & Workflows
Title: Stromal Niche Drives Immune Cell Fate
Title: Tumor-Stromal Barrier Assay Workflow
This article provides a detailed overview and application protocols for four major 3D cell culture models—spheroids, organoids, scaffolds, and organ-on-a-chip (OoC)—within the specific research context of immune response assessment. The central thesis posits that physiologically relevant 3D models are critical for dissecting the complex cellular and molecular interactions of the immune system in tissue-specific microenvironments, offering superior predictive value over traditional 2D cultures for therapeutic development, toxicity screening, and mechanistic studies.
Table 1: Key Characteristics and Immune Assessment Applications of Major 3D Models
| Model Type | Core Definition | Key Advantages for Immune Research | Primary Limitations | Typical Immune Assessment Applications |
|---|---|---|---|---|
| Spheroids | Self-assembled, spherical aggregates of one or multiple cell types. | Simple, high-throughput; recapitulates cell-cell adhesion and gradients (O₂, nutrients, signaling). | Limited structural complexity; variability in size. | Tumor-immune interactions (e.g., TIL infiltration), cytokine diffusion studies, high-throughput immunotoxicity screens. |
| Organoids | Stem cell-derived, self-organizing 3D structures mimicking organ architecture & function. | High biological fidelity; patient-derived (PSC/ASC) potential; complex multicellularity. | Maturation time; cost; batch variability; often lack stromal/immune components unless co-cultured. | Modeling mucosal immunity (gut, lung), host-pathogen interactions, autoimmune disease modeling, personalized immunotherapy testing. |
| Scaffold-Based | Cells seeded within natural (e.g., collagen, Matrigel) or synthetic polymeric 3D matrices. | Tunable biophysical/chemical properties; supports cell migration and matrix remodeling. | Scaffold batch variability (natural); degradation kinetics; potential immunogenicity of material. | Studying immune cell infiltration into extracellular matrix (ECM), macrophage polarization in 3D ECM, fibrosis models, vaccine adjuvant testing. |
| Organ-on-a-Chip | Microfluidic devices culturing cells in perfused, micrometer-sized chambers to mimic tissue-tissue interfaces and vascular flow. | Incorporates dynamic fluid flow and mechanical forces (shear, stretch); precise control of microenvironment. | Technical complexity; low-throughput; requires specialized equipment. | Modeling vascular-endothelial immune cell adhesion/transmigration, systemic immune responses, neuro-immune axis, pharmacokinetic/pharmacodynamic (PK/PD) of immunomodulators. |
Table 2: Quantitative Comparison of 3D Model Parameters
| Parameter | Spheroids | Organoids | Scaffold-Based Models | Organ-on-a-Chip |
|---|---|---|---|---|
| Typical Establishment Time | 3-7 days | 2-8 weeks | 1-4 weeks | 1-3 weeks |
| Throughput Potential | High (96-/384-well) | Medium (24-/96-well) | Medium (24-/96-well) | Low (custom, often <24 units) |
| Common Cell Number per Model | 500 - 10,000 cells | 1,000 - 50,000 cells | 10,000 - 500,000 cells | 10,000 - 2,000,000 cells |
| Cost per Model (Relative) | $ | $$$ | $$ | $$$$ |
| Key Readouts for Immune Studies | Size (invasion), viability (core vs. periphery), cytokine secretion, IF imaging. | Architecture (H&E), cell type markers (IF, FACS), functional assays (e.g., barrier integrity), scRNA-seq. | Cell migration distance, matrix degradation/remodeling, gene expression (qPCR). | Real-time imaging of adhesion/transmigration, effluent analysis (cytokines), TEER (for barrier models). |
Detailed Application Notes & Protocols
Spheroids for Tumor-Immune Interaction Assays
Application Note: Spheroids, particularly multicellular tumor spheroids (MCTS), serve as avascular tumor micrometastasis models to study cytotoxic T lymphocyte (CTL) or CAR-T cell infiltration and killing efficacy.
Protocol: Co-culture of MCTS with CAR-T Cells for Killing Assay
- MCTS Formation: Seed 5,000 HCT-116 colorectal carcinoma cells/well in a 96-well ultra-low attachment (ULA) round-bottom plate. Centrifuge at 300 x g for 3 min to promote aggregation. Culture for 72h in complete medium to form compact spheroids.
- CAR-T Cell Preparation: Expand anti-EGFR CAR-T cells in IL-2 containing medium. On day of assay, harvest, wash, and resuspend in fresh medium without IL-2. Count and adjust viability >95%.
- Co-culture Setup: Aspirate medium from MCTS wells. Add 100 µL of CAR-T cell suspension at an Effector:Target (E:T) ratio of 5:1. Controls: MCTS alone (target control), CAR-T cells alone (effector control).
- Monitoring & Analysis:
- Live Imaging: Use an Incucyte or similar system with fluorescent labels (e.g., tumor cells expressing mCherry, CAR-T cells labeled with CFSE) to track spheroid size and immune cell infiltration every 6h for 5 days.
- Endpoint Viability: At 120h, add 20 µL of CellTiter-Glo 3D reagent, shake for 5 min, incubate 25 min in dark. Measure luminescence. Calculate specific killing: `[1 - (Luminescence(Co-culture) / Luminescence(Tumor Control))] * 100%.
Intestinal Organoids for Modeling Mucosal Immunity
Application Note: Primary human intestinal organoids derived from crypt stem cells contain epithelial lineages (enterocytes, goblet, Paneth, enteroendocrine) and can be co-cultured with immune cells to model infections or inflammatory bowel disease (IBD).
Protocol: Co-culture of Mature Intestinal Organoids with Peripheral Blood Mononuclear Cells (PBMCs)
- Organoid Maturation: Embed intestinal stem cells in Matrigel domes and culture in IntestiCult Organoid Growth Medium for 10-14 days, changing medium every 2-3 days. For immune studies, differentiate for the final 5 days in medium containing BMP-4 and DAPT to enhance barrier formation.
- PBMC Isolation & Activation: Isolate PBMCs from donor blood via density gradient centrifugation (Ficoll-Paque). Activate with 50 ng/mL anti-CD3/CD28 antibodies for 48h in RPMI-1640 + 10% FBS.
- Co-culture Establishment: Mechanically disrupt mature organoids (using a 1 mL pipette tip) to release smaller fragments or "mini-rings." Seed these fragments into a transwell insert coated with a thin layer of collagen IV. Allow to adhere for 2h.
- Add PBMCs: Add 1 x 10^5 activated PBMCs in 100 µL to the apical chamber. Add 600 µL of co-culture medium (organoid differentiation medium + 5% FBS) to the basolateral chamber.
- Analysis:
- Transepithelial Electrical Resistance (TEER): Measure daily using a chopstick electrode to monitor barrier integrity.
- Cytokine Profiling: Collect basolateral medium at 24h and 72h for multiplex ELISA (e.g., IL-6, IL-8, TNF-α, IFN-γ).
- Immunofluorescence (IF): Fix with 4% PFA, permeabilize, and stain for EpCAM (epithelium), CD45 (immune cells), and cleaved caspase-3 (apoptosis).
3D Scaffold Model for Macrophage Polarization Studies
Application Note: Collagen I scaffolds provide a 3D ECM to study how matrix stiffness and composition influence macrophage polarization (M1 pro-inflammatory vs. M2 anti-inflammatory).
Protocol: Analyzing Macrophage Phenotype in a Tunable Collagen Matrix
- Scaffold Preparation:
- Prepare a 2 mg/mL neutralized collagen I solution (from rat tail) on ice. For stiffness modulation, adjust collagen concentration (1 mg/mL for soft, 4 mg/mL for stiff).
- Pipette 50 µL/well into a 96-well plate. Incubate at 37°C for 1h to polymerize.
- Macrophage Seeding & Polarization:
- Differentiate THP-1 monocytes into macrophages with 100 nM PMA for 48h on tissue culture plastic.
- Detach, seed 2 x 10^4 cells in 20 µL onto each collagen gel, allow to settle for 30 min, then add 100 µL medium.
- Polarization: Treat with 100 ng/mL LPS + 20 ng/mL IFN-γ (M1) or 20 ng/mL IL-4 (M2) for 48h. Include untreated (M0) control.
- Analysis:
- RNA Extraction & qPCR: Lyse gels in TRIzol Reagent. Isolate RNA and perform qPCR for markers: CD80, iNOS (M1); CD206, ARG1 (M2).
- Confocal Imaging: Fix, permeabilize, and stain for F-actin (Phalloidin) and CD68. Image z-stacks to analyze 3D morphology (elongation index).
- Cytokine Secretion: Measure IL-1β and IL-10 in supernatant via ELISA.
Organ-on-a-Chip for Modeling Leukocyte Extravasation
Application Note: A two-channel vascular chip models the blood vessel lumen and interstitial tissue space, enabling real-time study of immune cell adhesion and transendothelial migration under physiological shear stress.
Protocol: Real-time Imaging of T Cell Transmigration in a Vascularized Microfluidic Chip
- Chip Preparation & Seeding:
- Use a commercially available endothelialized chip (e.g., Emulate, MIMETAS). Coat the "tissue" channel with 50 µg/mL collagen I.
- Seed primary human lung microvascular endothelial cells (HULEC-5a) into the "vascular" channel at 2 x 10^6 cells/mL. Apply flow (1 dyne/cm²) using a perfusion system for 3 days to form a confluent, aligned monolayer (confirm by VE-cadherin IF).
- T Cell Preparation: Isolate human CD4+ T cells from PBMCs using magnetic beads. Activate with anti-CD3/CD28 and expand in IL-2 for 5 days. Fluorescently label with Calcein AM.
- Inflammatory Stimulation & Assay:
- Add 10 ng/mL TNF-α to the vascular channel medium for 6h to upregulate endothelial adhesion molecules (e.g., ICAM-1, VCAM-1).
- Stop flow. Inject 2 x 10^5 labeled T cells in 20 µL into the vascular channel inlet. Allow cells to settle onto endothelium for 10 min.
- Re-establish a low, pulsatile flow (0.5 dyne/cm²). Acquire time-lapse images (every 30 sec for 1h) at the endothelial junction plane using a confocal microscope on-stage incubator.
- Quantification: Analyze videos using tracking software (e.g., ImageJ Manual Tracking plugin). Calculate: a) Number of adherent cells per FOV, b) Percentage of adherent cells that transmigrate, c) Transmigration time.
The Scientist's Toolkit: Key Reagent Solutions
Table 3: Essential Research Reagents for 3D Immune Response Assays
| Reagent / Material | Primary Function | Example in Protocol (Section) |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Inhibits cell adhesion to plastic, forcing cell-cell aggregation into spheroids. | Spheroid formation for MCTS (3.1). |
| Basement Membrane Extract (BME, e.g., Matrigel, Geltrex) | Natural hydrogel providing complex ECM and growth factors for organoid growth. | Intestinal organoid culture and differentiation (3.2). |
| Type I Collagen (Rat Tail) | Natural polymerizable ECM protein; forms tunable 3D hydrogels for scaffold models. | 3D macrophage polarization assay (3.3). |
| CellTiter-Glo 3D | Luminescent ATP assay optimized for penetration and lysis in 3D structures. | Endpoint viability in spheroid killing assay (3.1). |
| Recombinant Human Cytokines (e.g., TNF-α, IL-4, IFN-γ) | Precisely modulate immune cell activation and polarization states. | Macrophage polarization (M1/M2) (3.3); Endothelial activation (3.4). |
| Transepithelial/Transendothelial Electrical Resistance (TEER) Electrodes | Measures real-time integrity of barrier-forming cell layers (epithelial/endothelial). | Monitoring intestinal organoid-PBMC co-culture barrier function (3.2). |
| Microfluidic Organ-Chip & Perfusion System | Provides controlled fluid flow, shear stress, and multi-compartment culture. | Leukocyte extravasation model (3.4). |
| Neutralizing Antibodies (anti-ICAM-1, anti-CXCL10) | Blocks specific ligand-receptor interactions to validate molecular mechanisms. | Control experiments in transmigration assays (3.4). |
Signaling Pathways & Experimental Workflows
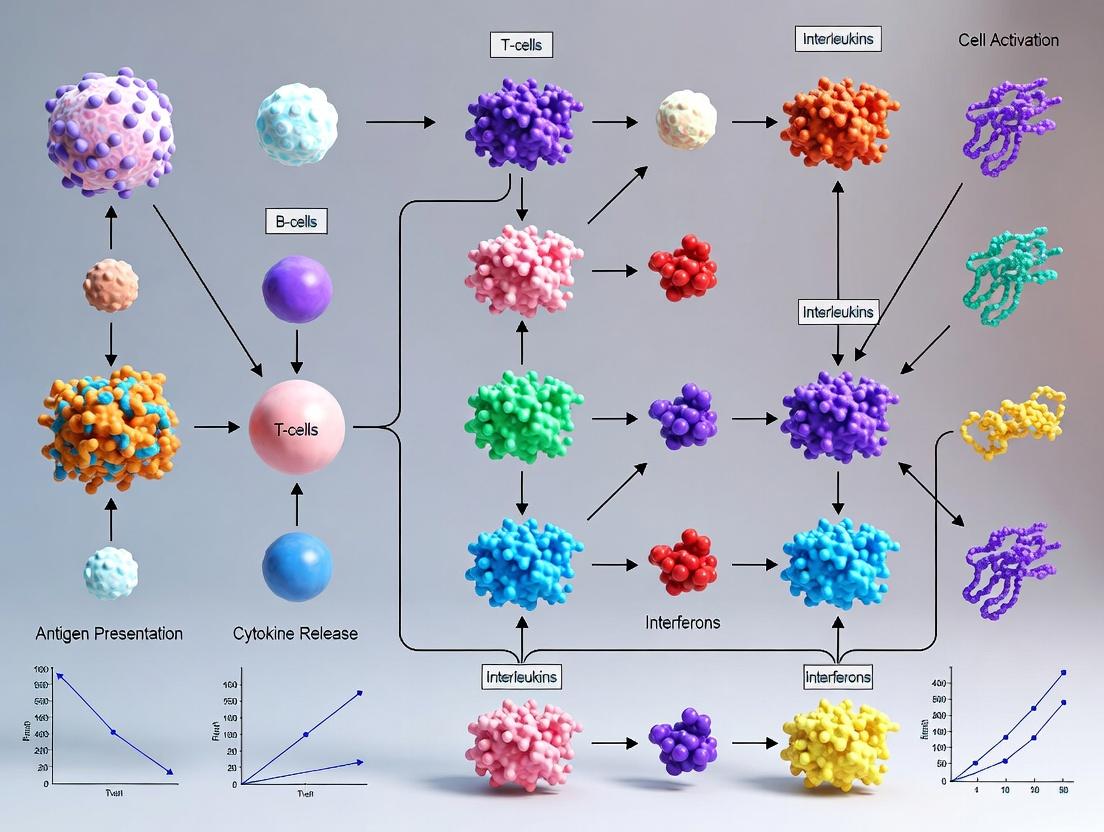
Diagram 1: Key immune pathways and model-specific readouts in 3D co-cultures.
Diagram 2: Protocol workflow for spheroid-based immune cell killing assay.
Diagram 3: Schematic of a vascular OoC setup for T cell extravasation.
Within the evolving thesis of 3D cell culture immune response assessment, traditional 2D monocultures are insufficient for modeling the complex, spatiotemporal dynamics of immune function. The scientific rationale for advanced 3D models lies in their enhanced physiological mimicry, which leads to superior predictivity for three core pillars of immune response: cell migration, cellular activation, and secreted cytokine profiles. This document details the application notes and protocols central to this research thesis, enabling researchers to generate more translationally relevant data for immunotherapy development, vaccine adjuvancy testing, and inflammatory disease modeling.
Application of these models allows for:
- Quantification of infiltrative capacity of immune cells (e.g., T cells, NK cells) into 3D tumor or tissue spheroids.
- Multi-parameter assessment of immune cell activation via surface markers and metabolic shifts within a 3D tissue context.
- Kinetic, spatially-resolved analysis of cytokine/chemokine secretion, moving beyond bulk supernatant measurements to local gradient mapping.
Experimental Protocols
Protocol 2.1: Generation of Target Spheroids for Infiltration Assays
Aim: To establish consistent, size-controlled 3D tissue spheroids (e.g., from cancer cell lines or primary fibroblasts) as targets for immune cell migration studies.
Materials: U-bottom ultra-low attachment (ULA) 96-well plate, complete cell culture medium, centrifuge.
Method:
- Harvest and count adherent target cells (e.g., HCT-116 colorectal carcinoma cells).
- Prepare a single-cell suspension at 2.5 x 10⁴ cells/mL in complete medium.
- Piper 200 µL of cell suspension into each well of a U-bottom ULA plate (resulting in 5,000 cells/well).
- Centrifuge the plate at 300 x g for 3 minutes to aggregate cells at the well bottom.
- Incubate at 37°C, 5% CO₂ for 72 hours to form a compact, single spheroid per well.
- Qualify spheroids by diameter (target: 450 ± 50 µm) using brightfield microscopy.
Protocol 2.2: Dynamic Immune Cell Migration in 3D Co-culture
Aim: To quantify the migration and infiltration of activated human T cells into target spheroids.
Materials: Generated spheroids (Protocol 2.1), activated human CD8⁺ T cells, live-cell imaging microscope with environmental control, analysis software (e.g., IMARIS, Fiji).
Method:
- T Cell Activation: Isolate human CD8⁺ T cells from PBMCs using magnetic beads. Activate with CD3/CD28 Dynabeads at a 1:1 bead:cell ratio in IL-2 (50 IU/mL) containing medium for 5-7 days.
- Labeling: Label 1 x 10⁶ activated T cells with 5 µM CellTracker Green CMFDA dye in serum-free medium for 30 min at 37°C. Wash twice.
- Co-culture Setup: Using a wide-bore pipette tip, carefully transfer one mature spheroid per well into a glass-bottom 96-well imaging plate. Gently add 2 x 10⁴ labeled T cells in 150 µL medium around the spheroid.
- Live-Cell Imaging: Place plate in live-cell imager. Acquire Z-stacks (20-30 µm depth, 5 µm intervals) every 30 minutes for 24 hours at 10x magnification.
- Quantitative Analysis:
- Use software to create a 3D surface rendering of the spheroid (far-red channel).
- Render T cells (green channel) as individual spots.
- Calculate metrics: Infiltration Index (% of T cells inside spheroid surface), Migration Velocity (µm/min), and Distance Traveled over time.
Protocol 2.3: Multiplexed Cytokine Profiling from 3D Co-culture Supernatants
Aim: To characterize the soluble immune response profile resulting from 3D immune-tumor interactions.
Materials: Conditioned supernatant from co-cultures, multiplex bead-based immunoassay kit (e.g., Luminex or ELLA), automated microplate reader.
Method:
- Supernatant Collection: At assay endpoint (e.g., 24, 48, 72h), carefully collect 100 µL of supernatant from each co-culture well without disturbing the spheroid. Centrifuge at 500 x g for 5 min to remove debris. Store at -80°C.
- Multiplex Assay: Thaw samples on ice. Perform assay according to manufacturer's protocol for a 15-plex panel (e.g., IFN-γ, TNF-α, IL-2, IL-4, IL-6, IL-10, IL-17A, Granzyme B, etc.).
- Data Acquisition: Run plates on appropriate analyzer. Generate standard curves for each analyte.
- Analysis: Calculate analyte concentrations (pg/mL) from standard curves. Normalize data to total protein content or cell number if required.
Data Presentation
Table 1: Comparative Immune Response Metrics in 2D vs. 3D Co-culture Systems
| Metric | 2D Monolayer Co-culture | 3D Spheroid Infiltration Co-culture | Predictive Advantage of 3D |
|---|---|---|---|
| T Cell Infiltration Depth (µm, 24h) | Not Applicable | 125 ± 35 | Models tissue penetration barrier |
| % IFN-γ+ CD8⁺ T Cells | 65% ± 8% | 42% ± 12% | Reflects immune suppression in TME |
| IL-6 Secretion (pg/mL) | 1550 ± 320 | 4250 ± 850 | Captures stromal contribution |
| Chemokine Gradient (CXCL10) | Homogeneous | Sustained, Spatially Heterogeneous | Drives directed migration |
Table 2: Essential Research Reagent Solutions Toolkit
| Reagent / Material | Function & Rationale |
|---|---|
| Ultra-Low Attachment (ULA) Plates | Promotes spontaneous 3D aggregation by inhibiting cell adhesion to plastic. |
| Extracellular Matrix (ECM) Hydrogels | Provides a physiologically relevant 3D scaffold (e.g., Collagen I, Matrigel) for embedding cells. |
| CellTracker Fluorescent Dyes | Enables stable, long-term live-cell tracking of specific cell populations in 3D without transfer. |
| Luminex Multiplex Panels | Allows simultaneous quantification of 30+ analytes from low-volume 3D culture supernatants. |
| Viability Assays (3D-optimized) | Metrics like CellTiter-Glo 3D measure ATP content, normalized to spheroid size/mass. |
| Hypoxia Probes (e.g., Image-iT) | Visualizes oxygen gradients within 3D structures that critically influence immune cell function. |
| Disaggregation Enzymes (e.g., Accutase) | Gently dissociates 3D spheroids into single-cell suspensions for downstream flow cytometry. |
Visualizations
Title: 3D Immune Response Assay Workflow
Title: Immune Cell Activation Pathways in 3D
Building a Functional Immune System In Vitro: Techniques and Translational Applications
1. Introduction and Thesis Context Advancing 3D cell culture models for immune response assessment is pivotal for bridging the gap between traditional 2D assays and in vivo physiology. This protocol details the establishment of co-cultures within 3D matrices, a cornerstone technique within a broader thesis focused on developing predictive platforms for immuno-oncology drug efficacy, immunotoxicity screening, and fundamental immunology research.
2. Research Reagent Solutions Toolkit Table 1: Essential Materials for 3D Immune-Target Cell Co-Culture
| Reagent/Material | Function/Brief Explanation |
|---|---|
| Basement Membrane Extract (BME) | A commercially available hydrogel (e.g., Cultrex, Matrigel) providing a biologically active 3D scaffold rich in laminin, collagen, and growth factors. |
| Synthetic PEG-based Hydrogels | Chemically defined, tunable matrices (e.g., PEG-maleimide) allowing precise control over stiffness, degradability, and incorporation of adhesive peptides (e.g., RGD). |
| Fibrin/Colagen I Hydrogels | Mechanically robust matrices suitable for studying immune cell migration and invasion; collagen I is a common stromal mimic. |
| Target Cells (e.g., Cancer Cell Lines) | Engineered or primary cells (e.g., organoids) serving as the antigen-presenting or disease-modeling component. Often pre-labeled (e.g., GFP). |
| Immune Effector Cells (e.g., T cells, NK cells) | Primary isolated or engineered immune cells (e.g., CAR-T). Often pre-labeled with a distinct fluorophore (e.g., mCherry, CellTracker dyes). |
| Cytokine/Checkpoint Inhibitors | Key experimental modulators (e.g., anti-PD-1, IL-2) used to perturb the co-culture system and assess functional readouts. |
| Live-Cell Imaging-Compatible Vessel | Glass-bottom plates or microfluidic devices enabling high-resolution, longitudinal confocal microscopy. |
| ATP-based Viability Reagent | For quantifying cell viability/luminescence in 3D, as standard MTT assays are less effective in thick matrices. |
3. Core Quantitative Data Summary Table 2: Comparison of Common 3D Matrix Types for Immune Co-Culture
| Matrix Type | Typical Stiffness (kPa) | Key Advantages | Key Limitations for Immune Studies |
|---|---|---|---|
| Basement Membrane Extract | 0.2 - 1.5 | Biologically active, supports complex morphogenesis. | Batch variability, contains undefined factors, soft. |
| Collagen I | 0.5 - 5.0 (tunable) | Physiological relevance for stroma, excellent for migration. | Can contract over time, variable receptor expression. |
| Fibrin | 0.5 - 10.0 (tunable) | Excellent for migration/invasion studies, clinical relevance. | Proteolytically degraded very quickly by some cells. |
| PEG-based (synthetic) | 0.1 - 50.0 (tunable) | Full biochemical/mechanical control, high reproducibility. | Requires functionalization for cell adhesion, less bioactive. |
4. Detailed Experimental Protocols
Protocol 4.1: Establishing Target Cell Spheroids in BME Objective: To pre-form 3D target cell structures before immune cell introduction.
- Target Cell Preparation: Harvest adherent target cells (e.g., cancer cell line). Resuspend at 1-5 x 10⁵ cells/mL in complete culture medium.
- Spheroid Formation: Plate 100 µL cell suspension per well in a 96-well ultra-low attachment (ULA) plate. Centrifuge at 300 x g for 5 min to aggregate cells.
- Incubation: Culture for 48-72h to form compact spheroids.
- Matrix Embedding: Prepare cold BME on ice. Gently transfer individual spheroids using a wide-bore tip into a 20 µL BME droplet in a glass-bottom 96-well plate.
- Gelation: Incubate plate at 37°C for 30 min to allow hydrogel polymerization.
- Overlay: Carefully add 100 µL of complete medium on top of the polymerized gel.
Protocol 4.2: Introducing Immune Effector Cells Objective: To add immune cells into the established 3D culture system.
- Immune Cell Preparation: Isolate or thaw primary T/NK cells or expand engineered cells (e.g., CAR-T). Activate and culture per standard protocols. Label with CellTracker Red CMTPX (5 µM, 20 min) if live tracking is required.
- Harvest & Count: Harvest immune cells, wash, and resuspend in complete medium at 2 x 10⁶ cells/mL.
- Direct Addition: For superficial addition, carefully pipette 50 µL of immune cell suspension (1 x 10⁵ cells) directly on top of the BME dome containing the spheroid. Cells will migrate into the gel.
- Direct Embedding (Alternative): For encapsulation, resuspend immune cells in cold BME at 1 x 10⁶ cells/mL. After spheroid gelation, carefully layer a second 20 µL BME-immune cell mixture on top and polymerize.
Protocol 4.3: Functional Readouts and Analysis Objective: To quantify immune-target cell interactions and outcomes.
- Live-Cell Imaging (Key Readout):
- Use a confocal microscope equipped with an environmental chamber (37°C, 5% CO₂).
- Acquire z-stacks (e.g., 20 µm depth, 5 µm intervals) every 30-60 minutes for 24-72h.
- Metrics: Calculate immune cell velocity, contact time with target cells, and spheroid infiltration index (% area invaded).
- Endpoint Viability Assay:
- Add 100 µL of ATP-based 3D viability reagent directly to the well (medium + gel).
- Incubate for 30 min with orbital shaking.
- Transfer lysate to an opaque plate and measure luminescence. Normalize to target-cell-only controls.
- Cytokine Profiling:
- Collect the overlying medium at endpoint.
- Analyze using a multiplex ELISA (e.g., for IFN-γ, TNF-α, Granzyme B, IL-2, IL-6).
5. Visualization Diagrams
Title: 3D Immune-Target Cell Co-Culture Workflow
Title: Key Cytotoxic Immune Synapse Pathway
Title: Decision Tree for 3D Matrix Selection
Within the broader thesis on Advanced 3D Cell Culture for Immune Response Assessment, this application note addresses the critical need for physiologically relevant in vitro models to evaluate adoptive cell therapies (ACTs). Traditional 2D co-culture systems fail to replicate the spatial, mechanical, and biochemical complexity of the tumor microenvironment (TME), leading to poor clinical translation. This document provides validated protocols for generating 3D tumor spheroids and using them as target substrates for testing Chimeric Antigen Receptor T-cells (CAR-T) and Tumor-Infiltrating Lymphocytes (TILs), enabling quantitative assessment of tumor killing, immune cell infiltration, and cytokine profiles.
Table 1: Comparative Efficacy of CAR-T vs. TILs Against 3D Solid Tumor Spheroids (Representative Data)
| Parameter | CAR-T Cells (Anti-EGFR) | Tumor-Infiltrating Lymphocytes (TILs) | Control (Untreated) |
|---|---|---|---|
| Spheroid Growth Inhibition (%) at 96h | 72.5 ± 8.1 | 58.3 ± 10.4 | 0 |
| Immune Cell Infiltration Depth (µm) | 80-120 | 150-250 | N/A |
| IFN-γ Secretion (pg/mL/10^6 cells) | 1250 ± 210 | 850 ± 175 | 25 ± 10 |
| IL-2 Secretion (pg/mL/10^6 cells) | 450 ± 95 | 650 ± 120 | <20 |
| EC50 (Effector:Target Ratio) | 1:2 | 1:5 | N/A |
| Induction of Apoptosis (Caspase-3+ %)* | 65 ± 7 | 45 ± 9 | 5 ± 2 |
*Measured in core spheroid region.
Table 2: Impact of Spheroid Matrix on Therapy Readouts
| Matrix Condition | Spheroid Compactness | CAR-T Killing (%) | TIL Infiltration (Depth µm) | Notes |
|---|---|---|---|---|
| Liquid Overlay (ULA Plate) | Low | 85 ± 6 | 200+ | Rapid killing, may overestimate efficacy. |
| Collagen I (3 mg/mL) | Medium | 70 ± 8 | 150-200 | Mimics physical barrier. |
| Matrigel (Basement Membrane) | High | 55 ± 12 | 80-150 | High biochemical resistance. |
| Hygel (Collagen + HA) | Very High | 40 ± 10 | <100 | Highly immunosuppressive model. |
Detailed Experimental Protocols
Protocol 3.1: Generation of Monocellular & Multicellular Tumor Spheroids
Aim: To produce consistent, reproducible 3D tumor spheroids for immune cell challenge. Materials: See Scientist's Toolkit.
- Cell Preparation: Harvest tumor cells (e.g., A549, OVCAR-3, patient-derived organoids). Ensure >95% viability.
- Seeding: For U-bottom ultra-low attachment (ULA) plates, prepare a single-cell suspension at 5,000-10,000 cells/well in 150 µL complete medium.
- Centrifugal Aggregation: Centrifuge plate at 300 x g for 3 minutes to aggregate cells at the well bottom.
- Incubation: Culture for 72-96 hours in a humidified 37°C, 5% CO2 incubator. Compact spheroids will form.
- QC: Under a light microscope, assess spheroid roundness and diameter. Use only uniform spheroids (CV <15%) for experiments. For Matrix-Embedded Spheroids: Mix cells with chilled collagen I/Matrigel to desired final concentration. Plate 50 µL drops in a pre-warmed plate, allow to polymerize for 30 min at 37°C, then overlay with medium.
Protocol 3.2: Co-culture of 3D Spheroids with CAR-T Cells or TILs
Aim: To model tumor-immune interaction and quantify cytotoxic response.
- Immune Cell Preparation: Expand and activate CAR-T cells or TILs. Rest for 24h in low-IL-2 medium before assay. Count and ensure >90% viability.
- Effector:Target (E:T) Ratio Titration: Prepare effector cells at ratios (e.g., 1:1, 2:1, 5:1, 10:1) based on the number of cells in the initial spheroid.
- Co-culture Setup: Gently transfer pre-formed spheroids (from Protocol 3.1) to a new ULA 96-well plate or use existing plate. Remove old medium and add 100 µL fresh medium. Carefully add 100 µL of effector cell suspension at 2X the desired final concentration to achieve the correct E:T ratio in 200 µL total volume.
- Incubation & Monitoring: Culture for up to 120 hours. Image spheroids every 24h using brightfield and fluorescence microscopy (if using labeled cells).
- Endpoint Assays:
- Viability: Add 20 µL of CellTiter-Glo 3D reagent, shake for 5 min, incubate 25 min, and record luminescence. Calculate % cytotoxicity:
[1 - (LumSample/LumTargetControl)] x 100. - Supernatant Analysis: Collect supernatant for multiplex cytokine analysis (IFN-γ, IL-2, Granzyme B, IL-6).
- Immunofluorescence: Fix spheroids in 4% PFA, permeabilize, stain for cleaved caspase-3 (apoptosis), CD3/CD8 (T-cells), and a tumor marker (e.g., pan-cytokeratin). Image using confocal microscopy for infiltration analysis.
- Viability: Add 20 µL of CellTiter-Glo 3D reagent, shake for 5 min, incubate 25 min, and record luminescence. Calculate % cytotoxicity:
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for 3D Immune-Oncology Assays
| Item | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Prevents cell adhesion, promoting 3D aggregation into spheroids via forced cell-cell contact. | Corning Spheroid Microplates (U-bottom) |
| Basement Membrane Extract | Provides a biologically relevant matrix to model extracellular barriers and biochemical cues of the TME. | Corning Matrigel Growth Factor Reduced |
| Type I Collagen | A tunable hydrogel to model the physical density and stromal component of solid tumors. | Rat tail Collagen I, high concentration |
| 3D Viability Assay Kit | Optimized lysis reagent for penetration and ATP quantification in dense 3D structures. | Promega CellTiter-Glo 3D |
| Live-Cell Imaging Dyes | For stable, long-term labeling of tumor or immune cells for tracking infiltration and killing. | CellTracker CMFDA, CM-Dil |
| Cytokine Multiplex Array | Quantifies a panel of secreted immune activation and suppression markers from supernatant. | Luminex Human Cytokine 25-Plex Panel |
| Immunofluorescence Clearing Kit | Reduces light scattering in fixed spheroids for deeper, clearer confocal imaging. | Miltenyi Biotec MACS Tissue Clear Kit |
Advancing our understanding of mucosal immunity is critical for developing next-generation vaccines and therapeutics. This work, framed within a broader thesis on 3D cell culture immune response assessment, posits that physiologically relevant in vitro models are indispensable for dissecting the complex dynamics of host-pathogen interactions. Traditional 2D monolayers fail to recapitulate the polarized epithelium, mucus production, and multicellular crosstalk characteristic of mucosal barriers in the respiratory and gastrointestinal tracts. This Application Note details protocols for establishing and applying 3D mucosal models to quantitatively assess immune responses to viral and bacterial challenges.
Key Research Reagent Solutions
Table 1: Essential Materials for 3D Mucosal Model Research
| Reagent/Material | Function & Rationale |
|---|---|
| Extracellular Matrix (ECM) Hydrogels (e.g., Matrigel, Collagen I) | Provides a 3D scaffold that mimics the in vivo basement membrane, supporting polarized epithelial growth and organoid formation. |
| Air-Liquid Interface (ALI) Culture Inserts (e.g., Transwell) | Enables differentiation of respiratory epithelial cells (e.g., primary bronchial) into a pseudostratified, mucus-producing, ciliated epithelium. |
| Primary Human Cells (e.g., bronchial/tracheal epithelial, PBMCs, dendritic cells) | Provides genetically human-relevant responses compared to immortalized cell lines, crucial for translational research. |
| Cytokine/Chemokine Multiplex Assay Panels | Allows simultaneous quantification of a broad spectrum of immune mediators (e.g., IL-6, IL-8, IFN-γ, TNF-α) from limited supernatant volumes. |
| Mucociliary Differentiation Media (e.g., PneumaCult-ALI) | Specialized media formulations designed to promote and maintain the differentiated state of airway epithelial cells at ALI. |
| Live-Cell Imaging Dyes (e.g., CellTracker, viability indicators) | Facilitates real-time, longitudinal monitoring of cell health and pathogen spread within the 3D structure. |
| Pathogen-Specific Reporter Strains (e.g., GFP-expressing influenza virus, luminescent Pseudomonas aeruginosa) | Enables precise quantification of pathogen load, localization, and the kinetics of infection within the model. |
Application Note: Quantifying Immune Activation in a 3D Airway Model Infected with Influenza A Virus
Objective: To measure the temporal profile of pro-inflammatory cytokine secretion and epithelial integrity following infection with Influenza A Virus (IAV) in a 3D differentiated primary human airway epithelial model.
Model Setup: Primary human bronchial epithelial cells (HBECs) are expanded and seeded onto collagen-coated Transwell inserts. Cells are grown at an Air-Liquid Interface (ALI) with specialized differentiation media for 4-6 weeks to form a pseudostratified epithelium with functional mucociliary clearance.
Experimental Protocol:
- Infection: On day of infection (DOI), apically wash cells with warm PBS. Dilute IAV (e.g., H1N1 strain) in infection medium to a target Multiplicity of Infection (MOI) of 0.1-2.0.
- Inoculation: Apply 100-200 µL of virus inoculum or vehicle control to the apical surface. Incubate for 2 hours at 37°C, 5% CO₂.
- Post-Inoculation: Carefully remove inoculum and wash apical surface three times with PBS to remove unbound virus. Return inserts to ALI conditions.
- Sample Collection: At predefined timepoints (e.g., 6, 24, 48, 72 hours post-infection (hpi)):
- Basolateral Supernatant: Collect medium from the basolateral compartment for cytokine analysis.
- Apical Wash: Add 200 µL PBS to the apical surface, incubate 10 minutes, collect for viral titer quantification (e.g., by plaque assay or qRT-PCR).
- Cell Lysate: Harvest cells for RNA (qPCR of viral genes, host ISGs) or protein (western blot for junctional proteins like ZO-1).
- Integrity Assessment: Measure Trans-Epithelial Electrical Resistance (TEER) at each timepoint prior to sample collection using a voltohmmeter.
- Analysis: Quantify cytokines using a multiplex Luminex assay and viral titer via plaque assay on MDCK cells.
Key Data Output: Table 2: Representative Data from IAV Infection (MOI 1.0) in 3D Airway Model
| Time Post-Infection (h) | TEER (% of Baseline) | Viral Titer (Log10 PFU/mL) | IL-6 (pg/mL) | IL-8 (pg/mL) | IFN-λ (pg/mL) |
|---|---|---|---|---|---|
| 0 (Control) | 100.0 ± 5.2 | ND | 15 ± 4 | 205 ± 32 | 10 ± 3 |
| 24 | 85.3 ± 7.1 | 4.2 ± 0.3 | 850 ± 120 | 1550 ± 210 | 550 ± 75 |
| 48 | 62.5 ± 9.8 | 5.8 ± 0.4 | 2100 ± 305 | 3200 ± 400 | 1250 ± 180 |
| 72 | 45.0 ± 12.4 | 6.5 ± 0.5 | 3500 ± 500 | 4500 ± 600 | 980 ± 150 |
ND: Not Detected; PFU: Plaque Forming Units.
Detailed Protocols
Protocol 4.1: Establishing a 3D Co-Culture Intestinal Model for Enteric Pathogen Study
Aim: To create a primary human intestinal organoid-derived monolayer co-cultured with immune cells for studying Salmonella Typhimurium invasion and immune response.
Materials:
- Matrigel (Growth Factor Reduced)
- Intestinal Organoid Expansion Media
- Differentiation Media (Wnt-/R-spondin- reduced)
- Collagen Type IV
- Peripheral Blood Mononuclear Cells (PBMCs) or isolated CD14+ monocytes
- Recombinant human M-CSF and IL-4 (for dendritic cell differentiation)
Method:
- Organoid Differentiation to 2D Monolayer: Plate expanded intestinal organoids (~50-100 organoids/well) onto a Collagen IV-pre-coated Transwell filter. Replace expansion media with differentiation media. Culture for 5-7 days until a confluent, polarized columnar epithelium forms (confirm by ZO-1 immunofluorescence).
- Immune Cell Differentiation: Isolate CD14+ monocytes from PBMCs using magnetic beads. Culture in basolateral compartment with RPMI 1640 containing M-CSF (50 ng/mL) and IL-4 (20 ng/mL) for 6 days to generate monocyte-derived dendritic cells (moDCs).
- Co-Culture Establishment: Gently transfer inserts with differentiated intestinal monolayer into wells containing the mature moDCs (or other immune cells) in fresh co-culture medium.
- Infection: On DOI, wash apical surface. Apically inoculate with S. Typhimurium (grown to mid-log phase, MOI ~10-50) in PBS for 1 hour.
- Gentamicin Protection Assay: Replace medium with medium containing gentamicin (100 µg/mL) to kill extracellular bacteria. Continue incubation.
- Analysis: At timepoints (2, 8, 24 hpi):
- Invasion/Intracellular Replication: Lyse cells with 1% Triton X-100, plate serial dilutions on LB agar for CFU counts.
- Transepithelial Electrical Resistance (TEER): Measure to monitor barrier disruption.
- Cytokine Profiling: Collect basolateral supernatant for multiplex analysis.
- Imaging: Fix and stain for bacteria (F-actin) and tight junctions for confocal microscopy.
Protocol 4.2: Cytokine Quantification via Multiplex Immunoassay
Aim: To simultaneously quantify multiple cytokines/chemokines from conditioned cell culture supernatant.
Materials:
- Multiplex bead-based assay kit (e.g., Bio-Plex Pro Human Cytokine Panel)
- Magnetic plate washer
- Luminex-based analyzer (e.g., Bio-Plex 200, MAGPIX)
- Assay Buffer, Wash Buffer, Detection Antibodies
Method:
- Preparation: Thaw samples on ice. Centrifuge all samples at 10,000xg for 5 minutes to remove debris.
- Bead Incubation: Add 50 µL of standards, controls, and samples to appropriate wells of a 96-well plate. Add 50 µL of pre-mixed magnetic beads to each well. Seal and incubate for 1 hour at room temperature (RT) with shaking.
- Wash: Place plate on magnetic washer. Aspirate supernatant. Wash beads 3 times with 100 µL Wash Buffer.
- Detection Antibody: Add 25 µL of biotinylated detection antibody mixture to each well. Seal, incubate for 30 minutes at RT with shaking. Wash 3 times.
- Streptavidin-PE: Add 50 µL of Streptavidin-Phycoerythrin to each well. Seal, incubate for 10 minutes at RT with shaking. Wash 3 times.
- Resuspension: Resuspend beads in 125 µL Assay Buffer. Shake for 2 minutes.
- Reading: Analyze on the Luminex analyzer. Use instrument software to generate standard curves and calculate sample concentrations (pg/mL).
Visualizing Signaling and Workflows
Diagram 1: 3D airway infection workflow.
Diagram 2: Epithelial innate immune signaling pathway.
Within the broader thesis on advancing 3D cell culture for immune response assessment, immunotoxicity screening using organoids represents a paradigm shift. Traditional 2D monocultures and animal models often fail to predict human-specific immune-related adverse drug reactions (irADRs) due to lack of physiological cellular complexity and interspecies differences. This protocol details the application of human 3D liver organoids (containing parenchymal and non-parenchymal cells, including Kupffer cells) and immune organoids (e.g., lymphoid tissue organoids) for assessing compound effects on immune function. These systems enable the evaluation of direct immunomodulation, compound-induced inflammatory responses, and hepatocyte-immune cell crosstalk in a human-relevant microenvironment.
Key Research Reagent Solutions
| Reagent/Material | Function in Immunotoxicity Screening |
|---|---|
| Human Pluripotent Stem Cells (iPSCs) | Starting cell source for generating isogenic hepatocytes, Kupffer-like cells, or lymphoid cells within organoids. |
| Specialized Organoid Culture Medium | Basal medium (e.g., Advanced DMEM/F12) supplemented with niche-specific factors (e.g., R-spondin, Noggin, WNT) and immune-supporting cytokines (e.g., IL-2, IL-7, FLT3L). |
| Extracellular Matrix (ECM) | Matrigel or synthetic hydrogels (e.g., PEG-based) providing a 3D scaffold that mimics the in vivo tissue structure and supports cell-matrix interactions. |
| Immune Cell Markers for Flow Cytometry | Antibody panels for CD45, CD3, CD19, CD14, CD68, CD86, MHC-II to quantify and phenotype immune cell populations post-exposure. |
| Cytokine Multiplex Assay Kits | For quantifying a panel of secreted cytokines/chemokines (e.g., IL-1β, IL-6, IL-8, TNF-α, IFN-γ) from organoid supernatants as indicators of immune activation or suppression. |
| CYP450 Induction/Inhibition Assay Kit | To assess test compound metabolism by liver organoids and link metabolic activation to immunotoxic outcomes. |
| Live-Cell Imaging Dyes (e.g., Calcein AM, PI) | For longitudinal monitoring of organoid viability and morphology in response to compound treatment. |
Table 1: Representative Immunotoxicity Endpoints in 3D Organoid Screening
| Endpoint Category | Specific Assay | Measurable Output | Typical Data Range (Baseline vs. Immunotoxicant) |
|---|---|---|---|
| Viability & Cytotoxicity | ATP-based Luminescence | ATP Content (RLU) | 100% vs. 30-70% decrease |
| Immune Cell Activation | Flow Cytometry | %CD86+ MΦ (Kupffer Cells) | 5-15% vs. 25-60% increase |
| Inflammatory Response | Multiplex ELISA | Secreted IL-6 (pg/mL) | 50-200 pg/mL vs. 500-5000 pg/mL |
| Cellular Stress | qPCR | CYP3A4 or NOS2 Gene Expression (Fold Change) | 1x vs. 2-10x upregulation |
| Immune Cell Cytotoxicity | Co-culture Killing Assay | % Target Cell Lysis | 10-20% vs. 50-80% increase or suppression |
| Barrier Integrity (Gut/Liver) | Transepithelial Electrical Resistance (TEER) | Ω × cm² | 300-500 Ω·cm² vs. 50-150 Ω·cm² decrease |
Table 2: Example Screening Results for Prototype Compounds
| Test Compound | Organoid Model | Key Immunotoxic Finding | Magnitude of Effect vs. Control |
|---|---|---|---|
| Lipopolysaccharide (LPS) | Liver Organoid (Kupffer+) | Pro-inflammatory cytokine release | IL-1β: ↑ 25-fold; IL-8: ↑ 15-fold |
| Dexamethasone | Immune/Lymphoid Organoid | Suppression of T cell proliferation | ↓ 70-90% proliferation |
| Anti-PD-1 Antibody | Immune Organoid (Tumor-infiltrating Lymphocytes) | Enhanced T cell activation | CD69+ T cells: ↑ 40% |
| Acetaminophen (High Dose) | Liver Organoid | Hepatocyte necrosis & Kupffer cell activation | ALT release: ↑ 8-fold; TNF-α: ↑ 10-fold |
| Cyclophosphamide (Prodrug) | Liver-Immune Co-culture | Metabolic activation leading to immune cell depletion | Viable Lymphocytes: ↓ 65% |
Detailed Experimental Protocols
Protocol 1: Establishing a 3D Liver Organoid with Resident Immune Cells Objective: To generate human iPSC-derived liver organoids containing hepatocytes and Kupffer-like macrophages for immunotoxicity screening.
- Differentiation: Differentiate iPSCs into definitive endoderm using Activin A (100 ng/mL) for 3 days, then into hepatic progenitors with BMP4 and FGF2 for 5 days.
- Hepatic Maturation: Culture progenitors in HCM (Hepatocyte Culture Medium) supplemented with HGF and Oncostatin M for 7-10 days to induce hepatocyte maturation.
- Macrophage Co-culture: Differentiate iPSCs in parallel to myeloid progenitor (using IL-3, M-CSF) and subsequently to Kupffer-like cells (using M-CSF, BMP4, TGF-β1). Dissociate and seed onto pre-formed hepatocyte spheroids at a 1:10 (macrophage:hepatocyte) ratio.
- 3D Embedding: Mix the aggregated co-culture with 30% Matrigel and plate in 96-well U-bottom plates. Centrifuge to form a single organoid per well.
- Maintenance: Culture in Advanced DMEM/F12 medium with liver and macrophage-supporting factors. Organoids are ready for screening at day 25-30.
Protocol 2: Immunotoxicity Screening Workflow Objective: To treat organoids with test compounds and assess a multi-parametric immunotoxicity profile.
- Treatment: Add serially diluted test compounds (typically 4-6 concentrations) to mature organoids (n=4-6 per group). Include vehicle control, positive controls (e.g., LPS for inflammation, Dexamethasone for immunosuppression).
- Incubation: Incubate for 24h (acute) to 7 days (chronic). Collect supernatant at 24h for cytokine analysis. Refresh medium/compound every 48h for chronic studies.
- Endpoint Analysis:
- Viability: Perform CellTiter-Glo 3D assay per manufacturer's instructions. Luminescence correlates with ATP content.
- Immune Phenotyping: Dissociate organoids with collagenase IV/Dispase. Stain cells with fluorescent antibodies (CD45, CD14, CD86, HLA-DR) and analyze by flow cytometry.
- Cytokine Profiling: Analyze collected supernatant using a 10-plex human cytokine LEGENDplex assay.
- Gene Expression: Isolate RNA from pooled organoids, perform reverse transcription, and run qPCR for immune (IL6, TNF, IFNG) and metabolic (CYP isoforms) markers.
- Histology: Fix select organoids in 4% PFA, embed in paraffin, section, and stain with H&E or for immune markers (IHC: CD68).
Visualizations
Title: Compound Immunotoxicity Pathways in 3D Organoids
Title: Immunotoxicity Screening Experimental Workflow
Application Notes
This document details the application of high-content imaging (HCI) and analysis to quantify immune cell infiltration and spatial distribution within three-dimensional (3D) cell culture models, such as tumor spheroids or organoids. This approach is critical for a broader thesis investigating the complex dynamics of immune response in physiologically relevant 3D microenvironments, enabling the assessment of immunotherapies, inflammatory diseases, and host-pathogen interactions.
Key Quantitative Metrics
High-content analysis of 3D immuno-oncology or inflammation models yields multi-parametric data. The following table summarizes the core quantitative metrics derived from such experiments.
Table 1: Core Quantitative Metrics for 3D Immune Cell Infiltration Analysis
| Metric Category | Specific Metric | Description | Typical Output Range/Unit |
|---|---|---|---|
| Infiltration Magnitude | Total Infiltrated Cells | Count of immune cells inside the 3D structure boundary. | 50 - 2000 cells/spheroid |
| Infiltration Index / Percentage | (Immune cells inside / Total immune cells) × 100. | 10% - 80% | |
| Infiltration Depth | Average distance infiltrated immune cells penetrate from the periphery. | 20 - 150 µm | |
| Spatial Distribution | Radial Distribution | Binned count of immune cells at defined distances from spheroid center. | Cells per 10µm bin |
| Nearest Neighbor Distance | Mean distance between an immune cell and its closest other immune cell. | 15 - 50 µm | |
| Cluster Analysis | Size and number of immune cell aggregates within the 3D volume. | 2 - 10 cells/cluster | |
| Interaction & Context | Tumor/Stroma Proximity | Percentage of immune cells within a defined proximity (<30µm) to target cells (e.g., cancer cells). | 5% - 60% |
| Zonal Analysis | Quantification of cells in defined zones: e.g., periphery, intermediate, core. | Variable % per zone | |
| 3D Migration Velocity | Tracked displacement of immune cells over time within the matrix. | 0.1 - 5.0 µm/min |
Research Reagent Solutions Toolkit
Successful 3D immune cell imaging requires specialized reagents and materials to maintain model integrity, enable specific labeling, and facilitate clearing and imaging.
Table 2: Essential Research Reagent Solutions for 3D Immune Cell Imaging
| Item Category | Specific Product/Type | Function in the Protocol |
|---|---|---|
| 3D Scaffold | Basement Membrane Extract (BME/Matrigel) | Provides a physiologically relevant, bioactive 3D extracellular matrix for co-culture. |
| Synthetic PEG-based Hydrogels | Defined, tunable stiffness and composition for controlled invasion studies. | |
| Cell Line/Label | GFP/RFP-expressing Tumor Cell Lines | Allows unambiguous identification of tumor mass structure in live/dead imaging. |
| Cell Tracker Dyes (e.g., CMFDA, CellTrace) | Pre-staining of immune cells (e.g., T cells, monocytes) for tracking infiltration. | |
| Immunostaining | Anti-CD45 / Anti-CD3 Conjugated Antibodies | Pan-immune or T-cell specific labeling for phenotyping infiltrated cells. |
| 3D-optimized Permeabilization Buffer | Contains higher detergent concentrations (e.g., 0.5-1.0% Triton X-100) to enable antibody penetration. | |
| Mounting/Clearing | Refractive Index Matching Solution (RIMS) | Clears optical path, reduces light scattering for deeper imaging (>100µm). |
| Deep-Well Imaging Dishes | Provides stable chamber for 3D culture, staining, and imaging without transfer. |
Experimental Protocols
Protocol: Generation and Co-culture of Tumor Spheroid - T Cell Model for Infiltration Assay
Objective: To establish a reproducible 3D tumor spheroid model and introduce fluorescently labeled primary human T cells to study infiltration dynamics over time.
Materials:
- U-bottom 96-well ultra-low attachment (ULA) plate
- Tumor cell line (e.g., HCT-116 colorectal carcinoma)
- Complete tumor cell growth medium
- Primary human T cells, isolated or purchased
- Cell Trace Far Red (CTFR) dye
- T cell activation/expansion medium (with IL-2, anti-CD3/CD28 beads)
- RPMI-1640 + 10% FBS (co-culture medium)
- Centrifuge, 37°C CO2 incubator
Procedure:
- Spheroid Formation: Seed 500-1000 tumor cells in 150 µL complete medium per well of a ULA plate. Centrifuge plate at 300 x g for 3 minutes to aggregate cells.
- Culture: Incubate plate for 72-96 hours to form compact, single spheroids (~400-500 µm diameter).
- T Cell Preparation (Day -3): Isolate or thaw primary human T cells. Activate using anti-CD3/CD28 beads in expansion medium supplemented with 100 IU/mL IL-2. Culture for 72 hours.
- T Cell Labeling (Day 0): Harvest activated T cells. Resuspend at 1x10^6 cells/mL in PBS containing 1 µM CTFR dye. Incubate for 20 minutes at 37°C. Quench with 5 volumes of complete medium, wash twice.
- Co-culture Setup: Using a wide-bore pipette tip, carefully transfer one mature spheroid per well to a deep-well imaging dish containing 100 µL co-culture medium.
- Add T Cells: Add 100 µL of labeled T cell suspension (2x10^4 to 1x10^5 cells) directly to the well containing the spheroid. Final volume ~200 µL.
- Initiate Imaging: Place dish in the high-content imager environmental chamber. Begin time-lapse imaging immediately (Z-stacks every 2-4 hours for 48-72 hours).
Protocol: 3D Immunostaining for Spatial Phenotyping in Fixed Organoids
Objective: To fix, permeabilize, and stain a 3D immune-organoid co-culture for multiple markers to analyze spatial relationships between immune subsets and target cells.
Materials:
- 4% Paraformaldehyde (PFA) in PBS
- 3D Permeabilization/Wash Buffer (PBS, 1% BSA, 0.5% Triton X-100, 0.01% Thimerosal)
- 3D Blocking Buffer (PBS, 5% BSA, 0.1% Triton X-100, 0.01% Thimerosal)
- Primary Antibodies: Anti-Cytokeratin (tumor), Anti-CD45 (immune), Anti-CD8 (cytotoxic T), Anti-FoxP3 (Treg)
- Secondary Antibodies: Cross-adsorbed, conjugated to Alexa Fluor 488, 555, 647, 750
- DAPI nuclear stain (1 µg/mL) | RIMS Mounting Media (e.g., ScaleS4(0) or commercial equivalent)
- Deep-well glass-bottom dish
Procedure:
- Fixation: Aspirate medium from co-culture. Add 200 µL 4% PFA. Incubate for 45-60 minutes at room temperature (RT) on gentle rocker.
- Wash: Remove PFA. Wash spheroid/organoid 3 x 15 minutes with 200 µL Permeabilization/Wash Buffer on rocker.
- Blocking: Incubate with 150 µL 3D Blocking Buffer for 4 hours at RT or overnight at 4°C on rocker.
- Primary Antibody Incubation: Prepare antibody cocktail in Blocking Buffer. Add 150 µL to sample. Incubate for 48 hours at 4°C on gentle rocker.
- Wash: Remove primary antibody. Wash 4 x 2 hours with 200 µL Permeabilization/Wash Buffer at 4°C on rocker.
- Secondary Antibody Incubation: Prepare secondary antibody + DAPI cocktail in Blocking Buffer. Add 150 µL. Incubate for 24 hours at 4°C in the dark on rocker.
- Final Wash: Wash 3 x 2 hours with 200 µL PBS at 4°C in the dark.
- Clearing & Mounting: Incubate with 150 µL RIMS for 24-48 hours at 4°C. Replace with fresh RIMS for imaging in a deep-well glass-bottom dish.
Visualizations
Title: 3D Spheroid Immune Infiltration Assay Workflow
Title: Key Pathways in 3D Immune Cell Infiltration & Exclusion
Title: HCI Analysis Pipeline for 3D Immune Quantification
Solving the 3D Puzzle: Expert Strategies for Robust and Reproducible Immune Assays
This application note, framed within a broader thesis on 3D cell culture immune response assessment, addresses the central challenge of preserving functional and viable immune cells within long-term (≥14 days) three-dimensional co-culture systems. Such models are critical for studying tumor-immune interactions, immunotherapy efficacy, and chronic inflammatory diseases in vitro. The primary hurdles include immune cell exhaustion, apoptosis due to lack of physiological survival signals, and loss of phenotype/function in conventional 3D matrices.
The table below summarizes the primary challenges and supporting quantitative data from recent literature (2023-2025).
Table 1: Key Challenges in Long-Term 3D Immune Co-Cultures & Supporting Data
| Challenge | Typical Impact on Viability/Phenotype (Day 7-14) | Contributing Factors | Mitigation Strategy Evidence |
|---|---|---|---|
| Lack of Pro-Survival Signaling | CD8+ T-cell viability drops to 10-25% in inert matrices. | Absence of IL-2, IL-7, IL-15 cytokines. | Cytokine supplementation restores viability to 60-80%. |
| Matrix-Induced Exhaustion | Up to 40% increase in PD-1+, TIM-3+ exhausted T-cells. | Stiffness, poor ligand presentation in synthetic hydrogels. | Tunable RGD-functionalized hydrogels reduce exhaustion markers by ~30%. |
| Metabolic Competition & Hypoxia | Rapid NK cell dysfunction; T-cell glycolysis suppressed. | Tumor cell metabolic dominance, O2 depletion in core. | IL-15 + glycolysis promotion (e.g., 2-DG) enhances NK persistence. |
| Loss of Motility & Cell-Cell Contact | Monocyte-derived DCs show 50% reduction in migration. | High matrix density, lack of chemokine gradients. | CCR7-CCL19 gradient patterning doubles DC migration. |
| Innate Immune Cell Differentiation | M2-like TAM polarization increases by 3-fold in static culture. | M-CSF dominance, lack of IFN-γ. | GM-CSF + IFN-γ yields 70% M1-like phenotype in 3D. |
Core Protocols for Maintaining Immune Cell Populations
Protocol 3.1: Cytokine Cocktail Supplementation for T-cell Maintenance in Tumor Spheroids
Objective: Sustain CD8+ and CD4+ T-cell viability and effector function in a 3D tumor spheroid co-culture for 21 days.
Materials:
- Tumor spheroids (e.g., from patient-derived organoids or cell lines).
- Activated human peripheral blood T-cells.
- Ultra-low attachment 96-well spheroid microplate.
- Base medium: Advanced RPMI 1640.
- Key Cytokines: Recombinant human IL-2 (20 IU/mL), IL-7 (10 ng/mL), IL-15 (5 ng/mL).
- Immune-checkpoint inhibitor: α-PD-1 antibody (10 µg/mL).
Method:
- Generate tumor spheroids (500-1000 cells) by centrifugation (500g, 5 min) in U-bottom plates. Culture for 72h.
- On day 0, add 2x10^4 activated T-cells per spheroid in 150µL of base medium.
- Critical Step: Add the cytokine cocktail (IL-2, IL-7, IL-15) and α-PD-1 directly to the co-culture well.
- Refresh 50% of the medium every 48 hours, replenishing all cytokines and antibody.
- Analysis: At day 7, 14, 21, assess via:
- Viability: Calcein-AM/Propidium Iodide live/dead imaging.
- Function: IFN-γ ELISpot on cells retrieved from dissociated spheroids.
- Phenotype: Flow cytometry for CD3/CD8/PD-1/TIM-3.
Protocol 3.2: Establishment of a Pro-Inflammatory Niche for Myeloid Cell Support
Objective: Maintain non-exhausted, M1-polarized tumor-associated macrophages (TAMs) and functional dendritic cells (DCs) in a bioprinted 3D tumor model.
Materials:
- Bioink: Hyaluronic acid-based matrix with RGD peptide.
- Cells: Tumor cells, monocyte-derived macrophages & DC precursors.
- Bioprinter or molding setup.
- Polarizing Cytokines: GM-CSF (20 ng/mL), IFN-γ (20 ng/mL).
- TLR agonist: Poly(I:C) (1 µg/mL) to mimic innate stimulation.
Method:
- Mix tumor cells, macrophages, and DC precursors at a 10:2:1 ratio in bioink.
- Print or mold 3D constructs (e.g., 5x5x2 mm).
- Culture constructs in medium containing GM-CSF and IFN-γ for the first 96h to establish M1/DC1 polarization.
- After 96h, switch to maintenance medium with reduced GM-CSF (5 ng/mL) and weekly Poly(I:C) stimulation.
- Analysis: At day 14:
- Multiplex IHC for CD68 (macrophages), CD11c (DCs), iNOS (M1), and CD206 (M2).
- Cytokine secretion profile (IL-12, TNF-α, IL-10) via Luminex.
Visualized Workflows & Signaling Pathways
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for Long-Term 3D Immune Co-Cultures
| Reagent Category | Example Product/Component | Critical Function in 3D Co-Culture |
|---|---|---|
| Pro-Survival Cytokines | Recombinant human IL-2, IL-7, IL-15 | Provides essential homeostatic and survival signals to T and NK cells, preventing apoptosis in matrix. |
| Polarizing Cytokines | Recombinant human GM-CSF, IFN-γ, IL-4 | Directs differentiation and maintains anti-tumor (M1/DC1) vs. pro-tumor (M2) phenotypes of myeloid cells. |
| Functionalized Hydrogel | RGD-peptide modified HA or PEG hydrogels | Provides integrin-mediated adhesion points, improving immune cell migration, activation, and persistence. |
| Immune Checkpoint Modulators | α-PD-1, α-PD-L1, α-CTLA-4 blocking antibodies | Counters exhaustion pathways upregulated in 3D confinement, restoring immune cell effector function. |
| Metabolic Support | Galactose/glutamine-rich media, 2-Deoxy-D-glucose (2-DG) | Alleviates metabolic competition; shifts cell metabolism to favor immune cell longevity. |
| Oxygen & pH Control | Portable gas controller (O2/CO2), pH indicators | Maintains physiological O2 tension (~1-5% in core) and pH to prevent hypoxia-induced dysfunction. |
| 3D-Compatible Assays | Luminescent ATP viability kits, 3D-optimized multiplex IHC | Enables accurate readout of viability and protein expression within dense 3D structures. |
Within the context of 3D cell culture for immune response assessment, optimizing culture media is a critical determinant of experimental fidelity. Three-dimensional models, such as spheroids, organoids, and tumor microenvironment co-cultures, introduce significant gradients of nutrients, oxygen, and signaling factors. This document provides application notes and protocols for systematically balancing these components to maintain physiologically relevant immune cell function and viability in 3D cultures, directly supporting research in immunotherapy screening and inflammatory disease modeling.
Key Variables and Quantitative Data
Table 1: Critical Media Components for 3D Immune Cell Co-Cultures
| Component Category | Specific Factor | Typical Concentration Range (2D Reference) | Adjusted Recommendation for 3D Core | Primary Function in Immune Response |
|---|---|---|---|---|
| Nutrients | Glucose | 5.5-25 mM (High) | 10-15 mM (Controlled) | Energy metabolism; high levels can suppress T-cell function. |
| Glutamine | 2-4 mM | 2-4 mM (Essential) | Proliferation and cytokine production. | |
| Amino Acids | Arginine | 0.4-1.0 mM | 1.0-1.5 mM | M1 macrophage polarization, T-cell receptor signaling. |
| Tryptophan | ~0.05 mM | Monitor depletion | NK and T-cell function; depletion by IDO induces tolerance. | |
| Soluble Factors | IL-2 (for T cells) | 10-100 IU/mL | 50-300 IU/mL (gradient-aware) | T-cell expansion and survival. |
| TGF-β | 0.1-5 ng/mL | Context-dependent (low for effector) | Regulatory T-cell induction, can suppress cytotoxicity. | |
| Oxygen | Physiologic O₂ | 18-20% (Atmospheric) | 1-7% (Physoxic) | Drives HIF-1α signaling, influences macrophage phenotype, T-cell infiltration. |
Table 2: Impact of Oxygen Tension on Immune Cell Behavior in 3D Cultures
| Oxygen Level | Term | Key Immune Cell Effects | Relevance to 3D Culture Core |
|---|---|---|---|
| 0.5-4% | Physiologic (Physoxic) | Enhanced T-cell memory formation, alternative macrophage activation. | Mimics lymphoid tissue or wound site. |
| 5-10% | Normoxic (Lab Standard) | Standard effector T-cell function, may over-activate some pathways. | Represents culture surface/periphery. |
| <0.5% | Hypoxic/Anoxic | Induces T-cell exhaustion, promotes immunosuppressive MDSCs and M2 macrophages. | Found in necrotic cores of tumors/spheroids. |
Experimental Protocols
Protocol 1: Establishing and Monitoring Nutrient/Oxygen Gradients in a Spheroid
Objective: To quantify the spatial gradients of glucose and oxygen within a 3D tumor spheroid co-cultured with PBMCs. Materials: Tumor cell line, human PBMCs, low-attachment U-bottom plates, fluorescent glucose analog (2-NBDG), hypoxia probe (e.g., pimonidazole), confocal microscope, needle-type oxygen microsensor (optional). Procedure:
- Spheroid Formation: Seed 500-1000 tumor cells/well in a 96-well U-bottom plate. Centrifuge at 300xg for 3 min. Culture for 72h to form compact spheroids.
- Immune Cell Addition: Carefully add 2x10⁴ PBMCs per well in fresh, optimized media (see Table 1). Do not centrifuge after addition.
- Gradient Monitoring (48h post-co-culture):
- Glucose: Incubate with 100 µM 2-NBDG for 1h. Wash gently and image using 488nm excitation.
- Hypoxia: Incubate with 100 µM pimonidazole for 2h. Fix with 4% PFA, permeabilize, and stain with FITC-conjugated anti-pimonidazole antibody.
- Viability: Include a far-red live/dead stain (e.g., Draq7).
- Analysis: Use confocal z-stacks to plot fluorescence intensity from spheroid periphery to core. Correlate nutrient/hypoxia gradients with immune cell (CD8⁺ T-cell) infiltration and death.
Protocol 2: Optimizing Soluble Factor Cocktails for Polarized Macrophages in a 3D Matrix
Objective: To generate and sustain M1 (pro-inflammatory) or M2 (immunoregulatory) macrophages within a 3D collagen matrix. Materials: Human monocytic THP-1 cells or primary monocytes, PMA, recombinant human cytokines (IFN-γ, IL-4, IL-13, M-CSF), type I collagen, 24-well culture plates. Procedure:
- Monocyte Embedding:
- Differentiate THP-1 cells with 100 ng/mL PMA for 48h in 2D. Detach.
- Mix 2x10⁵ cells/mL with neutralized type I collagen solution (2 mg/mL) on ice.
- Plate 500 µL/well and polymerize at 37°C for 30 min.
- Polarization in 3D:
- Overlay with optimized media containing:
- M1: 20 ng/mL IFN-γ + 100 ng/mL LPS.
- M2: 20 ng/mL IL-4 + 20 ng/mL IL-13.
- Include 50 ng/mL M-CSF in both conditions for survival.
- Overlay with optimized media containing:
- Culture and Analysis: Culture for 72h under 5% O₂. Refresh 50% media daily. Harvest matrices with collagenase. Analyze by flow cytometry for CD80 (M1) and CD206 (M2) markers, and measure IL-12 and IL-10 secretion via ELISA.
Signaling Pathway Integration
Diagram 1: Media Inputs Shaping 3D Immune Cell Function
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Media Optimization
| Item | Function/Application in 3D Immune Cultures | Example Product/Note |
|---|---|---|
| Advanced Basal Media | Low-glucose, nutrient-balanced formulation for gradient studies. | DMEM/F-12, RPMI 1640 without phenol red. |
| Recombinant Human Cytokines | Polarizing immune cells (IL-2, IFN-γ, IL-4, IL-13, TGF-β). | Use carrier protein-free, lyophilized for precise dosing. |
| Oxygen-Sensing Probes | Visualizing hypoxic cores in live or fixed spheroids. | Image-iT Green Hypoxia Reagent, pimonidazole HCl. |
| Metabolic Tracers | Monitoring glucose/glutamine uptake in 3D. | 2-NBDG (Glucose), L-Glutamine (BODIPY conjugate). |
| Physiologic O₂ Chamber | Maintaining cultures at physoxic (1-7% O₂) conditions. | Modular incubator chambers with gas regulator. |
| 3D Matrix | Providing in vivo-like scaffold for invasion studies. | Cultrex BME, Type I Collagen (rat tail), Matrigel. |
| Live/Dead Viability Assays | Quantifying viability deep within 3D structures. | Fluorescent dyes (e.g., Calcein AM/Propidium Iodide). |
| Multiplex Cytokine Assay | Profiling broad immune secretome from limited 3D media. | Luminex or Ella automated immunoassay. |
Controlling Immune Cell Seeding Density and Location for Consistent Model Assembly
Within the broader thesis on 3D Cell Culture Immune Response Assessment Research, a central challenge is the reproducible assembly of immune-competent 3D models. The predictive power of such models for immunotherapy screening or mechanistic immunology studies is critically dependent on the controlled integration of immune cells. This Application Note details protocols for precisely controlling immune cell seeding density and spatial location within scaffold-based and spheroid co-culture systems, enabling consistent and physiologically relevant model assembly for downstream functional assays.
Key Principles and Quantitative Benchmarks
Precise control over immune cell parameters is essential for model consistency. The tables below summarize target densities and outcomes based on current literature and experimental optimization.
Table 1: Target Seeding Densities for Common Immune Cells in 3D Co-Cultures
| Immune Cell Type | 3D Model Format | Target Seeding Density (cells/mm³) | Key Functional Outcome | Rationale / Citation Source |
|---|---|---|---|---|
| Primary Human T Cells (CD3+) | Collagen I Matrix (5 mg/mL) | 1,000 - 5,000 | Optimal tumor cell killing (cytotoxicity) & cytokine secretion (IFN-γ). | Avoids over-crowding; maintains motility. (Recent Front. Immunol. 2023) |
| Monocyte-Derived Macrophages (M0/M1) | Alginate-Gelatin Microbeads | 500 - 2,000 | Sustained viability & polarization capacity. | High density promotes unintended aggregation. (Biofabrication 2024) |
| Dendritic Cells (immature) | Decellularized ECM Scaffold | 200 - 800 | Effective antigen uptake and later T cell priming. | Mimics physiological low frequency. (Acta Biomater. 2023) |
| NK-92 Cells | Tumor Spheroid Co-Culture | 1:1 to 1:5 (Effector:Target) | Penetration and spheroid growth inhibition. | Standard cytotoxicity assay ratio adapted for 3D. (J. Immunol. Methods 2023) |
| PBMCs (peripheral blood mononuclear cells) | Multicellular Tumor Spheroid | 10-20% of total cells | Multi-lineage immune response without over-dominance. | Balances representation and model stability. (Sci. Rep. 2024) |
Table 2: Impact of Seeding Location on Model Outcomes
| Seeding Method | Spatial Location | Best For | Advantage | Technical Challenge |
|---|---|---|---|---|
| Co-Mixing | Uniformly distributed | Cytotoxicity, screening | High cell-cell contact | Cannot model extravasation or compartmentalized responses |
| Layered Seeding | Immune cells on top of/pre-formed tissue layer | Modelling infiltration (e.g., TILs) | Tracks migration/invasion | Interface can be mechanically weak |
| Core-Shell / Microfluidic | Precise peripheral or channel placement | Modeling vascular delivery, antigen presentation | High spatial control; fluid flow | Requires specialized equipment (bioprinter, chip) |
| "Add-on" Injection | Injected into pre-formed spheroid core | Adoptive cell therapy models | Direct tumor core engagement | Can cause spheroid rupture; volume control critical |
Detailed Experimental Protocols
Protocol 3.1: Precise Co-Mixing and Seeding for 3D Collagen I T Cell Assays
Aim: To uniformly embed T cells within a tumor cell-containing collagen matrix for cytotoxicity assays.
Materials: See Scientist's Toolkit below. Procedure:
- Cell Preparation: Harvest and count target cells (e.g., tumor cells) and effector cells (activated human CD3+ T cells). Keep on ice.
- Neutralized Collagen Solution: On ice, mix:
- 400 µL Rat Tail Collagen I (5 mg/mL stock)
- 100 µL 10X PBS
- 50 µL 0.1M NaOH (for neutralization)
- 450 µL Cold complete media + cells
- Final volume 1 mL, final [Collagen] ~2 mg/mL.
- Cell Incorporation: Gently pipette the required number of tumor cells and T cells into the cold neutralized collagen mixture. Final T cell density: 2,500 cells/mm³ (e.g., 25,000 cells in 100 µL gel).
- Pipetting and Gelation: Quickly aliquot 100 µL of the cell-collagen mix into each well of a 96-well plate. Tilt the plate to spread.
- Polymerization: Incubate plate at 37°C, 5% CO2 for 30 min for full gelation.
- Media Overlay: Gently add 100 µL of warm complete media on top of each gel.
- Culture & Assay: Culture for 3-5 days, with media change every 2 days. Assess cytotoxicity via lactate dehydrogenase (LDH) release or live-cell imaging (e.g., Incucyte with Caspase-3/7 Green dye).
Protocol 3.2: Layered Seeding for Monocyte/Macrophage Infiltration Studies
Aim: To create a 3D tumor layer and subsequently seed monocytes on top to study infiltration and polarization.
Procedure:
- Form Tumor Layer: Create a base gel layer (collagen or Matrigel) containing tumor cells (e.g., 50,000 cells/well in 50 µL gel in a 96-well). Let polymerize at 37°C for 30 min.
- Prepare Immune Cells: Differentiate monocytes from PBMCs using M-CSF (50 ng/mL) for 6 days to obtain M0 macrophages. Label with a cell tracker dye (e.g., CellTracker Red).
- Seeding on Top: Gently wash the tumor gel layer once with warm media. Resuspend M0 macrophages in complete media at 1x10^6 cells/mL. Carefully add 100 µL of this suspension (100,000 cells) on top of the gel.
- Controlled Settlement: Centrifuge the plate at 100 x g for 3 minutes at room temperature. This ensures consistent, gentle contact of all macrophages at the gel surface.
- Culture for Infiltration: Incubate at 37°C. Macrophages will infiltrate the gel over 24-72 hours.
- Analysis: Image at set time points using confocal microscopy (Z-stacks) to quantify infiltration depth (µm) and cell count per volume using Imaris or FIJI software.
Protocol 3.3: Microinjection of Immune Cells into Pre-formed Spheroids
Aim: To directly deliver immune cells (e.g., CAR-T cells) into the core of a tumor spheroid.
Materials: Ultra-low attachment U-bottom plates, microinjector (e.g., Narishige IM-11B), glass capillary needles (10 µm tip), micromanipulator. Procedure:
- Spheroid Formation: Generate tumor spheroids (500-600 µm diameter) in U-bottom plates via centrifugation (500 x g, 10 min) and 3-day culture.
- Needle Preparation: Back-fill a glass capillary with 5 µL of concentrated immune cell suspension (e.g., 2x10^6 CAR-T cells/mL in PBS+0.1% BSA).
- Mounting: Transfer a single spheroid to a dish with imaging media. Mount the dish on the microscope stage and position the needle at a 45° angle.
- Injection: Using the micromanipulator, pierce the spheroid periphery and advance the needle to the geometric center. Inject 50 nL of cell suspension (~100 cells). Hold for 10 seconds before slowly retracting the needle.
- Post-Injection Culture: Transfer the spheroid to a fresh U-bottom well with 200 µL media. Culture on an orbital shaker (60 rpm) to prevent re-attachment.
- Validation: Confirm injection success and localization via pre-labeling of immune cells (CellTracker Green) and imaging 2 hours post-injection.
Visualization: Diagrams and Workflows
Title: Protocol: 3D Co-Mixing and Embedding Workflow
Title: Core Injection into Spheroid Concept
Title: Decision Tree for Seeding Method Selection
The Scientist's Toolkit: Research Reagent Solutions
| Item / Reagent | Function & Role in Controlling Seeding | Example Product / Vendor |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Enables consistent spheroid formation via forced aggregation; critical for pre-forming tissue units for later immune cell addition. | Corning Spheroid Microplates, Nunclon Sphera |
| High-Concentration Collagen I | The most common natural scaffold for 3D cell culture; neutralized on ice to allow for gentle cell mixing before thermal gelation. | Rat tail Collagen I, Corning (8-11 mg/mL) |
| Defined, Xeno-Free ECM | Provides a consistent, chemically defined scaffold alternative to Matrigel for more reproducible cell migration and signaling studies. | Cultrex PathClear BME, TheWell Bioscience VitroGel |
| CellTracker Dyes | Fluorescent cytoplasmic labels for pre-labeling either immune or target cells before seeding, enabling precise tracking of location and density post-seeding. | Thermo Fisher Scientific CellTracker Green CMFDA |
| Programmable Syringe Pumps | For microfluidic systems or bioprinters, allowing precise deposition of immune cell-laden hydrogels in specific architectures. | Harvard Apparatus Pumps, CELLINK Bio X |
| Micromanipulator & Microinjector | For the precise, low-volume delivery of immune cells into specific regions of pre-formed 3D models (e.g., spheroid core). | Narishige IM-11B, Eppendorf InjectMan |
| Viability-Reporting Reporter Cell Lines | Engineered tumor cells expressing fluorescence upon apoptosis (e.g., Caspase-3/7). Allows real-time quantification of immune-mediated killing without harvesting. | Incucyte Caspase-3/7 Green Dye, Sartorius |
| Automated Cell Counters with Size Gating | Essential for accurately quantifying immune cell subsets (e.g., isolated T cells, monocytes) before seeding to ensure exact density. | Bio-Rad TC20, Countess 3, Thermo Fisher |
Application Notes & Protocols
Within the broader thesis of 3D cell culture immune response assessment research, a critical bottleneck exists in transitioning from physiologically relevant models to high-quality, analyzable endpoint data. This document details protocols to overcome hurdles in spheroid/organoid retrieval, processing, and volumetric immunostaining.
Protocol 1: Gentle Retrieval and Pre-Processing of 3D Cultures for Immune Cell Infiltration Analysis
Objective: To preserve the integrity of tumor spheroids and infiltrated immune cells (e.g., CAR-T cells, tumor-infiltrating lymphocytes) during retrieval from hydrogel or scaffold-based 3D co-cultures for subsequent analysis.
Key Materials:
- Ultra-low attachment (ULA) plate: For intermediate transfer to minimize adhesion-induced shear stress.
- Wide-bore, low-retention pipette tips (≥1000 µL): To prevent physical disruption of spheroids during aspiration.
- PBS-EDTA (2-5 mM) or PBS-EDTA-N-Acetylcysteine (NAC, 5-10 mM): Chelating agents to gently disrupt matrix interactions without enzymatic degradation of surface epitopes.
- Cell recovery solution (CRS): Non-enzymatic, thermoreversible hydrogel dissolution agent.
Procedure:
- Termination: At assay endpoint, carefully aspirate 80% of the culture medium without disturbing the 3D constructs.
- Matrix Dissociation:
- For synthetic hydrogels (e.g., PEG-based): Add pre-chilled PBS-EDTA-NAC (2x volume of remaining medium). Incubate at 4°C for 30-60 min with gentle orbital shaking.
- For natural matrices (e.g., Matrigel): Add pre-chilled CRS (2x volume). Incubate at 4°C for 30-60 min until gel is fully dissolved.
- Gentle Retrieval: Using a wide-bore tip, transfer the suspension (containing now-released spheroids) to a pre-hydrated ULA plate.
- Washing: Let spheroids settle by gravity (5-10 min). Carefully remove supernatant. Gently resuspend in 1 mL of cold, serum-free PBS. Repeat wash twice.
- Option Branching:
- For live-cell analysis (e.g., flow cytometry): Proceed to gentle mechanical dissociation protocol (not detailed here).
- For 3D imaging: Fix spheroids immediately (see Protocol 2).
Table 1: Quantitative Comparison of Gentle Retrieval Methods
| Method | Matrix Type | Recovery Yield (%)* | Spheroid Integrity Score (1-5) | Median Processing Time | Key Risk |
|---|---|---|---|---|---|
| PBS-EDTA-NAC (4°C) | Synthetic Hydrogels | 92 ± 5 | 4.5 | 45 min | Incomplete dissolution of dense matrices. |
| Cell Recovery Solution | Matrigel, Collagen I | 95 ± 3 | 4.8 | 60 min | Potential for cell clustering if not washed thoroughly. |
| Manual Picking | Any, for critical samples | >99 | 5.0 | 30 min per spheroid | Low throughput, high skill requirement. |
| Enzymatic (Collagenase/Dispase) | Dense Collagen, Decellularized ECM | 85 ± 8 | 3.0 | 90 min | Epitope damage, immune cell viability loss. |
Data derived from n=3 independent experiments using 200µm diameter HCT116 spheroids co-cultured with human peripheral blood mononuclear cells (PBMCs). Yield calculated vs. initial seeded count. *Scored via bright-field microscopy: 5=perfectly spherical, no cells shed; 1=fully disintegrated.
Protocol 2: Passive CLARITY-Enabled Volumetric Immunostaining (PCvIS) for 3D Co-Cultures
Objective: To achieve deep, uniform antibody penetration into whole spheroids/organoids (300-500 µm diameter) for high-resolution 3D confocal imaging of immune cell spatial distribution.
The Scientist's Toolkit: Essential Reagents for PCvIS
| Item | Function & Rationale |
|---|---|
| 4% PFA with 0.1% Acrylamide | Fixation & hydrogel monomer infusion. Acrylamide polymerizes to create a supportive mesh within the tissue. |
| X-CLARITY Electrolyte Solution | Conducts current and maintains pH during passive clearing (modified for passive use). |
| SDS-based Clearing Solution (4-8%) | Lipid-removing detergent for passive tissue clearing. |
| Passive Clearing Chamber | Sealed, temperature-controlled chamber for gentle, long-term immersion clearing. |
| RI Matching Solution (RIMS, n=1.46) | Post-clearing refractive index matching solution for optical transparency. |
| Fab Fragment Anti-Mouse IgG | Pre-blocking agent to saturate endogenous mouse immunoglobulins in co-cultures containing murine stromal cells. |
| Permeabilization Buffer (0.5% Triton X-100, 0.1% Saponin) | Maintains membrane integrity for intracellular target staining better than high-dose Triton alone. |
| Anti-CD8α (Clone: C8/144B), Anti-CD4 (Clone: EPR19514), Anti-CD68 (Clone: KP1) | Validated for 3D staining. Target cytotoxic T-cells, helper T-cells, and macrophages, respectively. |
| Nuclear Counterstain (DRAQ5 or SYTOX Deep Red) | Far-red, highly photostable dyes that penetrate deep tissue. |
Procedure:
- Fixation & Hydrogel Embedding: Fix retrieved spheroids in 4% PFA with 0.1% acrylamide overnight at 4°C.
- Polymerization: Incubate samples at 37°C for 3 hours to thermo-polymerize acrylamide within the fixed tissue.
- Passive Clearing: Transfer spheroids to a clearing chamber with 8% SDS in X-CLARITY buffer (pH 8.5). Incubate at 37°C with gentle agitation for 48-72 hours. Replace solution every 24h.
- Washing & Blocking: Wash 4x over 24 hours in PBS-T (0.1% Triton X-100) at 37°C to remove SDS. Block in PBS-T with 5% normal serum, 10% Fab fragment anti-mouse IgG (if needed), and 1% BSA for 24 hours at room temperature.
- Primary Immunostaining: Incubate with primary antibodies diluted in blocking buffer for 72 hours at room temperature with agitation.
- Secondary Staining: Wash 6x over 36 hours with PBS-T. Incubate with fluorophore-conjugated secondary antibodies and nuclear stain in blocking buffer for 48 hours. Wash again 6x over 36 hours.
- RI Matching: Incubate spheroids in RIMS (n=1.46) for at least 24 hours before imaging.
- Imaging: Mount in RIMS and image using a confocal microscope with resonant scanner and tiling/z-stack capabilities.
Table 2: Quantitative Staining Penetration Efficiency in 500µm Spheroids
| Staining Target | Standard Method (24h stain) | PCvIS Method (72h stain) | Fold Increase in Signal at Core |
|---|---|---|---|
| Membrane (CD8) | 18 ± 7% coverage in core | 95 ± 4% coverage in core | 5.3x |
| Cytoplasmic (Granzyme B) | 10 ± 5% coverage in core | 88 ± 6% coverage in core | 8.8x |
| Nuclear (Ki-67) | 5 ± 3% coverage in core | 82 ± 5% coverage in core | 16.4x |
*Data shows percentage of cells in the central 100µm slice of the spheroid exhibiting specific immunostaining above threshold. n=5 spheroids per condition.
Title: Workflow for 3D Immune Response Endpoint Analysis
Title: PCvIS Protocol Steps for Deep 3D Staining
Title: Technical Hurdles and Corresponding Solutions
Within the thesis investigating immune cell infiltration and efficacy in 3D tumor microenvironments, standardization is the cornerstone of meaningful discovery. Variability in spheroid/organoid generation, cytokine sampling, and imaging analysis can obscure true biological signals, compromising reproducibility and translational potential. This document outlines established best practices and protocols to ensure robust, comparable data.
Table 1: Minimum Required Metadata for 3D Immune Co-Culture Experiments
| Parameter Category | Specific Metrics to Report | Recommended Measurement Tool/Standard |
|---|---|---|
| 3D Model Core | Base cell line(s), passage number | Cell authentication record (STR profiling) |
| Scaffold/Matrix type & concentration (e.g., 4 mg/mL Matrigel) | Lot number, vendor | |
| Spheroid diameter (µm) at time of assay (mean ± SD) | Automated image analysis (e.g., Celigo, ImageJ) | |
| Assay endpoint (e.g., Day 5 post-co-culture) | Protocol-defined | |
| Immune Component | Immune cell type & source (e.g., donor ID, cell line) | Donor consent/ethics, passage number |
| Activation status & method (e.g., 100 ng/mL IL-2, 24h) | Cytokine batch/lot | |
| Effector-to-Target (E:T) ratio | Calculated from precise cell counts | |
| Environmental Control | Medium formulation & supplements | Catalog number, serum % and batch |
| Oxygen level (%) if controlled | Sensor calibration data | |
| Sampling volume & frequency for multiplex assays | Adjusted for evaporation in plate | |
| Analytical Output | Primary imaging metric (e.g., % infiltration area) | Algorithm details, threshold values |
| Viability assay (e.g., ATP luminescence RLU) | Normalization method (e.g., to control) | |
| Cytokine concentration (pg/mL) | Assay kit name, dynamic range |
Table 2: Common Sources of Variability and Mitigation Strategies
| Variability Source | Impact on Data | Recommended Mitigation Practice |
|---|---|---|
| Matrix Lot Variability | Alters spheroid compactness, diffusion kinetics | Pre-test and qualify new lots; use aliquots from a single qualified lot for a study series. |
| Cell Seeding Density | Inconsistent spheroid size, altering immune penetration | Use automated cell counters; validate spheroid size distribution daily 0-3. |
| Assay Plate Edge Effects | Evaporation causes well-to-well variability in cytokine conc. | Use only interior wells for critical assays; employ plate seals during incubation. |
| Manual Image Analysis | User bias in thresholding infiltration zones | Use automated, script-based analysis (e.g., CellProfiler); define and lock parameters. |
| Sample Collection Timing | Cytokine levels fluctuate with circadian rhythms & metabolism | Strict adherence to synchronized time windows (e.g., ±1 hour). |
Experimental Protocols
Protocol 1: Standardized Generation of Tumor Spheroids for Immune Co-Culture Objective: To produce uniform, reproducible 3D tumor spheroids as targets for immune cell interaction. Materials: See "Scientist's Toolkit" below. Procedure:
- Cell Preparation: Harvest and count tumor cells (e.g., HCT-116). Ensure viability >95% by trypan blue exclusion.
- Suspension: Prepare cell suspension at 2X the final seeding density (e.g., 1,000 cells/50 µL) in complete medium without matrix.
- Layering: Using a multichannel pipette, dispense 50 µL of cold (4°C) basement membrane matrix (e.g., Corning Matrigel) into each well of a 96-well U-bottom ultra-low attachment (ULA) plate. Avoid bubbles.
- Cell Seeding: Immediately layer 50 µL of the 2X cell suspension on top of the matrix droplet. Do not mix.
- Gelation: Incubate plate at 37°C, 5% CO₂ for 30 minutes to allow matrix polymerization.
- Feeding: After gelation, gently add 100 µL of pre-warmed complete medium on top of each gel droplet.
- Culture: Culture for 72 hours to form compact spheroids. Image daily to monitor size uniformity using an automated plate imager. Proceed to co-culture only when >90% of spheroids have a diameter of 400 ± 50 µm.
Protocol 2: Multiplex Cytokine Profiling from 3D Co-Culture Supernatants Objective: To quantitatively measure immune cytokine release (e.g., IFN-γ, TNF-α, IL-6) in a standardized, reproducible manner. Procedure:
- Sample Collection: At the assay endpoint, carefully collect 100 µL of supernatant from each well using a multichannel pipette with tips placed against the well wall. Avoid disturbing the 3D structure.
- Clearance: Centrifuge collected supernatant at 500 x g for 5 minutes at 4°C to pellet any stray cells or debris.
- Aliquoting & Storage: Transfer clarified supernatant to a fresh, labeled microtube. Aliquot immediately to avoid freeze-thaw cycles. Store at -80°C until analysis.
- Multiplex Assay: Use a validated, commercial multiplex immunoassay panel (e.g., Luminex xMAP or MSD). Thaw samples on ice.
- Standard Curve: Prepare the kit's serial dilutions of standards in the same matrix as the samples (e.g., complete medium + 5% Matrigel) to account for matrix interference.
- Run & Analysis: Perform assay according to manufacturer's instructions. Run all samples from a single experimental batch on the same plate. Use 5-parameter logistic regression for curve fitting in the analysis software.
Signaling Pathways & Workflows
Title: 3D Immune Co-Culture Experimental Workflow
Title: Key Immune Activation Pathway in 3D Co-Culture
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Rationale for Standardization |
|---|---|
| Ultra-Low Attachment (ULA) Plates | Surface coating prevents cell adhesion, forcing cells to aggregate into spheroids. Consistent plate geometry (U-bottom vs. V-bottom) is critical for uniform spheroid shape. |
| Basement Membrane Extract (e.g., Matrigel) | Provides a physiologically relevant 3D scaffold. Lot-to-lot variability is high; thus, pre-qualification for spheroid formation and cytokine binding is essential. |
| Defined, Serum-Free Medium | Removes unknown variables from serum (e.g., bovine cytokines, growth factors). Enables precise control over exogenous factors. |
| Viable Cell Counting Dye (e.g., Trypan Blue) | Accurate determination of live cell concentration prior to seeding is fundamental to reproducibility. Automated cell counters are preferred. |
| Validated Multiplex Cytokine Assay Kits | Allows simultaneous measurement of multiple analytes from small supernatant volumes, conserving precious 3D samples. Must be validated for use with matrix-containing samples. |
| Automated Live-Cell Imager | Enables non-invasive, kinetic monitoring of spheroid size, morphology, and fluorescent reporters (e.g., immune cell migration) with minimal disturbance to the culture. |
| Analysis Software (e.g., CellProfiler, Imaris) | Provides automated, parameter-defined quantification of complex phenotypes (infiltration depth, killing zones), removing subjective manual analysis bias. |
Benchmarking 3D Models: How They Stack Up Against Animal and Clinical Data
Correlating In Vitro 3D Immune Responses with In Vivo Preclinical Outcomes
Advancements in 3D cell culture systems, such as spheroids, organoids, and microphysiological systems (MPS), have revolutionized the assessment of immune responses in a more physiologically relevant microenvironment. This document, framed within a broader thesis on 3D cell culture immune response assessment research, provides detailed application notes and protocols for correlating in vitro 3D immune system models with in vivo preclinical outcomes. The goal is to enhance the predictive validity of immunogenicity, efficacy, and toxicity testing in drug development, thereby reducing reliance on animal models and accelerating translational success.
Application Notes: Key Insights and Data Correlation
A critical review of current literature reveals growing evidence of correlation between sophisticated 3D in vitro immune models and in vivo results.
Table 1: Correlation of 3D In Vitro Immune Assays with In Vivo Preclinical Outcomes
| 3D In Vitro Model Type | Immune Response Measured | In Vivo Preclinical Correlate | Reported Correlation Coefficient (R²) / Predictive Value | Key Study Reference |
|---|---|---|---|---|
| Tumor-Immune Cell Co-culture Spheroid | Cytotoxic T-cell infiltration & tumor cell killing | Tumor growth inhibition in humanized mouse PDX models | R² = 0.78 - 0.89 for efficacy ranking | Jenkins et al., 2023 |
| Lymph Node-on-a-Chip (MPS) | Antigen-specific T-cell activation & cytokine release (IL-2, IFN-γ) | T-cell proliferation and cytokine levels in immunized mice | R² = 0.82 for IFN-γ dose-response | Sontheimer-Phelps et al., 2024 |
| Gut Mucosal Organoid with PBMCs | Pro-inflammatory cytokine storm (IL-6, TNF-α) | Incidence and severity of colitis in animal models | 85% negative predictive value for safety | Chen & Ootani, 2023 |
| 3D Skin Equivalent with Langerhans Cells | Dendritic cell maturation (CD83+, CCR7+) | Contact sensitization potential (LLNA assay equivalent) | 92% accuracy vs. historical LLNA data | Ahlfors et al., 2023 |
| Liver Spheroid with Kupffer Cell Surrogates | Monocyte-derived macrophage phagocytosis & chemokine release | Hepatotoxicity and immune-mediated drug reactions in rats | Sensitivity: 88%, Specificity: 79% | Bell et al., 2022 |
Key Insight: The highest correlations are observed when 3D models incorporate multiple immune cell types, stromal components, and dynamic flow (MPS), mirroring the complex cellular crosstalk and pharmacokinetic profiles seen in vivo.
Detailed Experimental Protocols
Protocol 1: Establishing a 3D Tumor Immunogenicity Assay
Objective: To evaluate T-cell-mediated killing in a 3D tumor spheroid and correlate results with in vivo efficacy in a humanized mouse model.
Materials:
- Primary human CD3+ T-cells or PBMCs from healthy donors.
- Target tumor cell line (e.g., A549, HCT-116).
- Ultra-low attachment (ULA) 96-well round-bottom plates.
- Recombinant human IL-2.
- Anti-CD3/CD28 T-cell activator.
- Cancer antigen peptide or bispecific T-cell engager (BiTE) antibody.
- Live/dead cell viability dye (e.g., Calcein AM / Propidium Iodide).
- Confocal imaging system.
Procedure:
- Tumor Spheroid Formation: Seed 500-1000 tumor cells/well in ULA plates. Centrifuge plates at 300 x g for 3 minutes to encourage aggregation. Incubate for 72 hours to form compact spheroids.
- T-cell Activation & Labeling: Isolate CD3+ T-cells from PBMCs. Activate with anti-CD3/CD28 beads and expand for 5-7 days in media containing 50 IU/mL IL-2. Label a portion of T-cells with a fluorescent cell tracker.
- Co-culture Establishment: Gently add 10,000-50,000 activated T-cells to each pre-formed tumor spheroid well. Include experimental groups with antigen peptide or BiTE.
- Assessment:
- Viability: At days 3, 5, and 7, stain spheroids with Calcein AM (live, green) and PI (dead, red). Acquire z-stack images via confocal microscopy. Quantify live/dead cell volume using 3D image analysis software (e.g., Imaris).
- Infiltration: Quantify fluorescence intensity of tracked T-cells within the spheroid core vs. periphery.
- Correlation Metric: Calculate % tumor spheroid killing. Correlate this value with the % tumor growth inhibition observed in a parallel humanized mouse model study using the same tumor cell line and therapeutic agent. Perform linear regression analysis.
Protocol 2: Cytokine Release Syndrome (CRS) Assessment in a 3D Endothelial-PBMC Co-culture Model
Objective: To predict the potential for CRS using a 3D vascularized model and correlate cytokine levels with in vivo observations.
Materials:
- Primary human umbilical vein endothelial cells (HUVECs).
- Primary human PBMCs.
- Fibrinogen/Thrombin hydrogel kit.
- 24-well transwell inserts or microfluidic chip.
- Test article (e.g., CAR-T cells, bispecific antibody).
- Multiplex cytokine assay panel (IL-6, IFN-γ, TNF-α, IL-2).
Procedure:
- 3D Vascular Network Formation: Embed HUVECs in a fibrin gel within the well. Culture with angiogenic media (VEGF, bFGF) for 5-7 days to allow capillary-like network formation.
- Immune Cell Introduction: Seed PBMCs in the surrounding compartment or perfusate. Allow to equilibrate for 24 hours.
- Stimulation: Introduce the test article (e.g., CAR-T cells at effector:target ratio).
- Sampling and Analysis: Collect supernatant from the endothelial and PBMC compartments at 6, 24, 48, and 72 hours.
- Analysis: Use a multiplex luminex assay to quantify cytokine concentrations. Generate a cytokine "storm" profile.
- Correlation Metric: Establish a threshold value for key cytokines (e.g., IL-6 > 5000 pg/mL) that corresponds with the onset of severe CRS symptoms (e.g., hypotension, fever > 40°C) in historical or parallel preclinical animal studies. Calculate predictive sensitivity and specificity.
Visualization of Key Concepts
Title: Workflow for Correlating 3D Models with In Vivo Outcomes
Title: Key Immune Signaling Pathways Modeled in 3D Systems
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for 3D Immune Response Studies
| Reagent / Material | Supplier Examples | Function in 3D Immune Assays |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Corning, Greiner Bio-One | Promotes spontaneous 3D cell aggregation to form spheroids by preventing cell adhesion. |
| Fibrinogen/Thrombin Hydrogel Kit | Sigma-Aldrich, Merck | Provides a tunable, natural ECM for embedding cells and forming 3D vascular networks. |
| Synthetic PEG-Based Hydrogels | Cellendes, Advanced BioMatrix | Chemically defined, xeno-free matrices for controlled stiffness and functionalization (e.g., with RGD peptides). |
| Human PBMCs & Immune Cell Subsets | STEMCELL Tech, Lonza | Primary cells for building autologous or allogeneic immune-competent models. Critical for relevance. |
| Recombinant Human Cytokines (IL-2, IFN-γ, etc.) | PeproTech, R&D Systems | For immune cell differentiation, activation, and maintenance within 3D cultures. |
| 3D Live-Cell Imaging Dyes (e.g., CellTracker, Calcein AM/PI) | Thermo Fisher, BioLegend | Enable longitudinal, non-destructive monitoring of cell viability, location, and function in 3D. |
| Multiplex Cytokine Assay Panels | Luminex, Meso Scale Discovery | Quantify a broad profile of soluble immune mediators from the limited supernatant of 3D cultures. |
| Microfluidic Organ-on-a-Chip Devices | Emulate, Mimetas | Provide dynamic fluid flow and multi-tissue interfaces for advanced Microphysiological Systems (MPS). |
Within the broader thesis on advanced 3D cell culture for immune response assessment, selecting the optimal model system is paramount. Spheroids, organoids, and bioprinted constructs each offer distinct advantages and limitations for immunological readouts. This application note provides a comparative analysis, detailed protocols, and reagent toolkits to guide researchers in drug development and immuno-oncology.
Table 1: Key Characteristics and Immune Readout Capabilities
| Feature | Spheroids (Multicellular Aggregates) | Organoids (Stem Cell-Derived) | Bioprinted Constructs (Spatially Designed) |
|---|---|---|---|
| Complexity & Origin | Moderate; from cell lines or primary cells. | High; self-organized from adult/pluripotent stem cells. | Programmable; cells + bioinks (natural/synthetic). |
| Immune Component Integration | Co-culture of tumor/stroma + immune cells (e.g., TILs, PBMCs). | Can develop intrinsic immune cells (e.g., microglia in brain organoids); also supports co-culture. | Precise spatial positioning of immune compartments (e.g., lymphatic-like channels). |
| Key Readouts (Examples) | Cytokine secretion (IFN-γ, TNF-α), Cytotoxicity (LDH, caspase), Immune cell infiltration (IF). | Immune cell development, Antigen presentation (MHC expression), T cell-organoid killing. | Directed immune cell migration, Spatial profiling of immune-tumor interactions. |
| Throughput | High (96/384-well ULA plates). | Low to moderate. | Low to moderate. |
| Reproducibility | Good for simple co-cultures. | Batch variability can be high. | High with standardized printing. |
| Quantitative Data (Representative Values) | ~40-60% T cell infiltration depth in tumor spheroids. Co-culture cytokine levels: IFN-γ can range 500-2000 pg/mL. | In embedded co-culture, T cells can reduce organoid viability by 50-70% over 5 days. | Printed constructs can maintain ~90% cell viability post-printing; precise positioning ± 50 µm. |
Table 2: Suitability for Common Immune Assays
| Assay | Spheroids | Organoids | Bioprinted Constructs |
|---|---|---|---|
| Flow Cytometry (disaggregated) | Excellent | Challenging (tough ECM) | Good (depends on bioink) |
| Live-Cell Imaging (e.g., Confocal) | Good (limited by depth) | Moderate (opacity can be issue) | Excellent (designed for imaging) |
| Multiplex Cytokine Profiling | Standard protocol | Standard protocol | Standard protocol |
| Spatial Transcriptomics/Proteomics | Limited | Good (complex architecture) | Excellent (pre-defined regions) |
| Gene Expression (Bulk RNA-seq) | Good | Good | Good |
Experimental Protocols
Protocol 1: Generation of Immune-Competent Tumor Spheroids for Cytotoxicity Testing
Objective: To form uniform tumor spheroids, integrate peripheral blood mononuclear cells (PBMCs), and assess T cell-mediated killing.
Materials: See "Scientist's Toolkit" Section. Procedure:
- Spheroid Formation: Seed cancer cell line (e.g., HCT-116) in ultra-low attachment (ULA) 96-well round-bottom plates at 500-1000 cells/well in complete medium. Centrifuge plates at 300 x g for 3 min to aggregate cells. Culture for 72h to form compact spheroids.
- Immune Cell Addition: Isolate PBMCs from donor blood using Ficoll density gradient. Activate PBMCs with 50 ng/mL anti-CD3/CD28 antibodies and 100 IU/mL IL-2 for 3-5 days.
- Co-culture Establishment: Carefully add 1x10^4 activated PBMCs in 50 µL medium to each pre-formed spheroid well. Include controls (spheroids alone, PBMCs alone).
- Readout at 48-72h:
- Viability: Add 20 µM CellTracker Green to tumor cells pre-co-culture. Measure fluorescence loss over time.
- Cytotoxicity: Measure lactate dehydrogenase (LDH) release in supernatant per manufacturer's protocol.
- Imaging: Fix with 4% PFA, permeabilize, stain for CD3 (T cells) and DAPI. Image using confocal microscopy to quantify infiltration depth.
Protocol 2: Co-culture of CAR-T Cells with Patient-Derived Organoids (PDOs)
Objective: To evaluate chimeric antigen receptor (CAR) T cell efficacy against patient-specific tumor organoids.
Procedure:
- Organoid Establishment: Embed patient tumor digest in Cultrex Reduced Growth Factor Basement Membrane Extract (BME). Plate 30 µL domes in 24-well plate, polymerize at 37°C for 30 min. Overlay with organoid culture medium. Culture for 5-7 days, passaging as needed.
- CAR-T Cell Preparation: Expand anti-target (e.g., anti-EGFR) CAR-T cells in complete TexMACS medium with IL-7/IL-15 (10 ng/mL each).
- Co-culture Setup: Harvest organoids by mechanical disruption and gentle centrifugation. Transfer ~10 organoids per well to a ULA 96-well plate. Add CAR-T cells at desired effector:target ratio (e.g., 5:1).
- Readout at 96h:
- Organoid Viability: Perform ATP-based luminescence assay (e.g., CellTiter-Glo 3D). Calculate % viability relative to organoid-only control.
- Cytokine Storm Profiling: Collect supernatant. Use multiplex bead array (e.g., Luminex) to quantify IFN-γ, IL-2, IL-6, GM-CSF.
- Flow Cytometry: Disaggregate co-culture using TrypLE Express. Stain for T cell activation markers (CD69, CD107a) and exhaustion markers (PD-1, TIM-3).
Protocol 3: Assessing Immune Cell Migration in a Bioprinted Tumor-Stroma Model
Objective: To model and quantify monocyte migration towards a tumor niche within a bioprinted construct.
Procedure:
- Bioink Preparation:
- Tumor Bioink: Mix MDA-MB-231 cells at 10x10^6 cells/mL with 3% alginate / 5 mg/mL fibrinogen solution.
- Stromal Bioink: Mix human lung fibroblasts (HLFs) at 5x10^6 cells/mL with GelMA (5% w/v).
- Bioprinting: Using a coaxial extrusion bioprinter:
- Print a central core of "Tumor Bioink" into a 96-well insert.
- Surround it with a concentric shell of "Stromal Bioink".
- Crosslink with 2% CaCl2 (for alginate) and UV light (365 nm, 30 sec for GelMA).
- Monocyte Integration & Migration Assay:
- After 24h, add THP-1 monocytes (labeled with CellTracker Red) in medium to the top of the construct.
- At time points 6h, 24h, 48h, image z-stacks using confocal microscopy.
- Quantify migration distance from construct periphery towards the tumor core using image analysis software (e.g., Imaris).
- Spatial Analysis: Fix construct at endpoint, section, and stain for CD68 (monocytes), α-SMA (CAFs), and pan-cytokeratin (tumor). Analyze using digital pathology.
Visualizations
Title: Decision Flow for 3D Immune Model Selection
Title: Core Immune-Tumor Interaction Pathways in 3D Models
Title: Generic Workflow for 3D Immune Response Assessment
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for 3D Immune Co-culture Experiments
| Reagent/Material | Function & Key Characteristics | Example Vendor(s) |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Prevents cell adhesion, promoting 3D spheroid/organoid formation. Surface is covalently coated hydrogel. | Corning, Greiner Bio-One |
| Basement Membrane Extract (BME) | Solubilized ECM from Engelbreth-Holm-Swarm tumor. Provides complex scaffold for organoid growth. | Cultrex (Bio-Techne), Corning Matrigel |
| Alginate-Gelatin Bioink | Biocompatible, printable hydrogel. Crosslinkable with Ca2+. Good for cell encapsulation and migration studies. | CELLINK, Allevi |
| Recombinant Human Cytokines (IL-2, IL-7, IL-15) | Critical for priming, activating, and maintaining viability of immune cells (especially T/NK cells) in 3D co-culture. | PeproTech, BioLegend |
| Cell Viability Assay (3D Optimized) | ATP-based luminescent assays designed to penetrate 3D structures for accurate viability measurement. | Promega (CellTiter-Glo 3D), Abcam |
| Live-Cell Fluorescent Trackers (CellTracker) | Stable cytoplasmic dyes for long-term tracking of distinct cell populations (e.g., tumor vs. immune) in live imaging. | Thermo Fisher Scientific |
| Collagenase/Hyaluronidase Mix | Enzymatic cocktail for gentle, effective dissociation of 3D models (especially organoids) for downstream flow cytometry or RNA-seq. | STEMCELL Technologies |
| Multiplex Bead-Based Immunoassay | Simultaneously quantify multiple cytokines/chemokines from limited-volume 3D culture supernatants. | Bio-Rad (Bio-Plex), MilliporeSigma (Milliplex) |
| Checkpoint Inhibitor Antibodies (anti-PD-1, anti-CTLA-4) | Therapeutic-grade blocking antibodies to model immunotherapy responses in immune-competent 3D systems. | Bio X Cell |
| Programmable Extrusion Bioprinter | For precise spatial patterning of cells and matrices to create complex immune-tumor microenvironments. | BIO X, Regemat 3D |
This application note is framed within a broader thesis on 3D cell culture immune response assessment research. The central hypothesis posits that patient-derived 3D models (e.g., tumor organoids, spheroids, and immune-organ co-cultures) recapitulate the complex tumor-immune microenvironment (TIME) more accurately than 2D models. This case study evaluates the predictive value of these 3D systems for two critical clinical outcomes: immunotherapy efficacy (e.g., PD-1/PD-L1 blockade response) and adverse events, with a focus on Cytokine Release Syndrome (CRS). The integration of such models into pre-clinical pipelines aims to de-risk clinical trials and personalize immunotherapy regimens.
Recent studies demonstrate the superior correlation of 3D model responses with patient clinical outcomes compared to traditional models.
Table 1: Predictive Performance of 3D Models for Immunotherapy Efficacy
| Model Type | Cancer Type | Immunotherapy | Concordance with Patient Response | Key Predictive Readout | Reference (Year) |
|---|---|---|---|---|---|
| Patient-derived organoid (PDO) - PBMC co-culture | Colorectal | Anti-PD-1 | 88% (7/8 PDOs) | Tumor cell killing, IFN-γ secretion | (Dijkstra et al., 2018) |
| Tumor spheroid - CAR-T co-culture | Ovarian | Mesothelin-targeting CAR-T | 91% (Predictive of in vivo tumor load) | Spheroid size reduction, CAR-T infiltration | (Larson et al., 2022) |
| Air-liquid interface (ALI) patient-derived tumors | NSCLC | Anti-PD-1 / Anti-CTLA-4 | 100% PPV, 83% NPV (n=12) | Proliferating CD8+ T cells, Granzyme B | (Neal et al., 2018) |
| Microfluidic tumor-on-a-chip with T cells | Melanoma | Anti-PD-1 | N/A (Mechanistic) | T cell migration, tumor apoptosis | (Hassan et al., 2021) |
Table 2: 3D Model Correlates for Cytokine Release Syndrome (CRS) Prediction
| Model System | Immune Component | Stimulus | Key CRS-Associated Cytokine Output | Correlation with Clinical CRS Grade | Reference (Year) |
|---|---|---|---|---|---|
| Organoid-based human lymph node | PBMCs, dendritic cells | CD19 CAR-T | IL-6, IFN-γ, IL-2 | Significant (p<0.01) for high-grade CRS | (Ghuman et al., 2023) |
| 3D vascularized tumor spheroid | PBMCs | Bispecific T cell engager (BiTE) | IL-6, IL-10, GM-CSF | Dose-dependent release matching patient serum profiles | (Morton et al., 2024) |
| Multi-tissue "body-on-a-chip" | PBMCs in endothelialized channel | CAR-T | IL-1Ra, MCP-1, IL-6 | Predictive of onset kinetics and severity | (Edington et al., 2023) |
Experimental Protocols
Protocol 1: Establishing a PDO-PBMC Co-culture for PD-1/PD-L1 Blockade Response Testing
Objective: To predict patient-specific response to immune checkpoint inhibitors. Materials: See "Research Reagent Solutions" (Table 3). Procedure:
- PDO Generation & Expansion: Mechanically and enzymatically digest patient tumor biopsy. Embed fragments in basement membrane extract (BME). Culture in defined, organ-specific medium. Expand organoids for 2-4 passages to establish a stable line.
- PBMC Isolation: Collect matched patient blood sample (or healthy donor if unavailable) via density gradient centrifugation (e.g., Ficoll-Paque). Isolate PBMCs and cryopreserve until use.
- Co-culture Setup: a. Harvest PDOs, dissociate into single cells or small clusters (<10 cells). b. Seed 5,000-10,000 cells/well in a 96-well U-bottom ultra-low attachment plate in co-culture medium (organoid medium + 10% human AB serum + 10 U/mL IL-2). c. Add autologous or allogeneic PBMCs at an Effector:Target (E:T) ratio of 10:1. d. Add therapeutic agents: Isotype control, anti-PD-1 (10 µg/mL), anti-PD-L1 (10 µg/mL). e. Incubate at 37°C, 5% CO2 for 5-7 days.
- Endpoint Analysis: a. Viability: Measure using ATP-based luminescence (CellTiter-Glo 3D). b. Immunophenotyping: Harvest cells, stain for flow cytometry (CD3, CD8, CD4, PD-1, TIM-3, LAG-3). c. Cytokine Secretion: Collect supernatant for multiplex ELISA (IFN-γ, TNF-α, Granzyme B, Perforin).
Protocol 2: 3D CRS Potency Assay using a Vascularized Spheroid Model
Objective: To quantify CAR-T or BiTE-induced cytokine storm potential. Materials: See "Research Reagent Solutions" (Table 3). Procedure:
- Tumor Spheroid Formation: Seed 1,000 tumor cells (e.g., NALM-6 for CD19 CAR-T) per well in a 96-well U-bottom plate. Centrifuge at 300 x g for 3 min. Incubate for 72h to form compact spheroids.
- Endothelialization: Coat spheroids with human umbilical vein endothelial cells (HUVECs) by adding 500 HUVECs/spheroid in EGM-2 medium. Culture on an orbital shaker (60 rpm) for 24h to form a perfusable endothelial layer.
- Immune Cell Introduction & Stimulation: a. Generate CAR-T cells via lentiviral transduction of CD3+ T cells. Expand for 10-14 days. b. Add CAR-T cells or unmodified T cells + BiTE to the spheroid culture at an E:T ratio of 5:1. c. Include controls: Tumor only, Immune cells only.
- Monitoring and Harvest: a. Image daily using phase-contrast and fluorescence microscopy (if using labeled cells) to monitor spheroid integrity and immune cell infiltration. b. Collect supernatant at 24h, 48h, and 72h for cytokine profiling via high-sensitivity multiplex assay (focus on IL-6, IL-10, IFN-γ, GM-CSF, MCP-1). c. At 72h, fix spheroids for confocal imaging (CD31 for vasculature, CD3 for T cells, cleaved caspase-3 for apoptosis).
Visualizations
Diagram 1: Workflow for Predictive 3D Immuno-Oncology Testing
Diagram 2: Key Pathways in Efficacy & CRS Within 3D Models
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for 3D Immune Response Modeling
| Item | Function/Description | Example Product/Brand |
|---|---|---|
| Basement Membrane Extract (BME) | Provides a physiologically relevant 3D scaffold for organoid growth and polarization. | Cultrex Reduced Growth Factor BME, Matrigel |
| Defined Organoid Culture Medium | Chemically defined, serum-free medium tailored to specific tissue types to support stem/progenitor cells. | IntestiCult, mTeSR, STEMdiff |
| Ultra-Low Attachment (ULA) Plates | Prevent cell adhesion, promoting spontaneous 3D aggregation into spheroids. | Corning Spheroid Microplates, Nunclon Sphera |
| Live-Cell Imaging Dyes | Track immune cell migration, infiltration, and cytotoxicity in real-time within 3D structures. CellTrace dyes, pHrodo. | CellTrace Violet, pHrodo Red |
| 3D Viability Assay Kits | Luminescent/fluorescent assays optimized for ATP detection or membrane integrity in 3D structures. | CellTiter-Glo 3D, RealTime-Glo MT |
| High-Plex Cytokine Arrays | Simultaneously quantify 30+ analytes from small supernatant volumes to profile immune responses and CRS signatures. | Luminex xMAP, MSD U-PLEX |
| Microfluidic Chip Systems | Enable precise control of fluid flow, shear stress, and multi-tissue interactions for advanced "on-a-chip" models. | Emulate Organ-Chips, AIM Biotech DAX Chips |
| Recombinant Human Cytokines | Essential for immune cell expansion, activation, and maintenance in co-culture (e.g., IL-2, IL-15, IL-21). | PeproTech, R&D Systems |
| Validated Blocking Antibodies | For checkpoint inhibition studies (anti-PD-1, anti-CTLA-4, anti-TIM-3) and isotype controls. | BioLegend, Bio X Cell equivalents |
Within the broader thesis on 3D cell culture for immune response assessment, a central methodological question is selecting the appropriate level of system complexity. Simple co-cultures and multi-tissue organ-on-a-chip (OoC) systems represent two critical points on the spectrum of in vitro models. The choice directly impacts the biological relevance, throughput, cost, and translational value of data generated in drug development, particularly for immunomodulatory therapies, immuno-oncology, and inflammatory disease modeling. This document provides application notes and detailed protocols to guide this decision.
Comparative Assessment: Key Quantitative Factors
Table 1: Quantitative Comparison of Model Characteristics
| Factor | Simple 2D/3D Co-Culture | Multi-Tissue Organ-on-a-Chip |
|---|---|---|
| Typical Cell Types | 2 (e.g., epithelial + immune cells) | 3+ (e.g., epithelial, endothelial, stromal, immune) |
| Throughput (Plates/Week) | High (10-50) | Low to Medium (1-10) |
| Establishment Cost (USD) | Low ($100 - $1,000) | High ($10,000 - $100,000+) |
| Run Cost per Experiment | Low ($50 - $500) | High ($500 - $5,000) |
| Time to Assay Readiness | Short (1-7 days) | Long (1-4 weeks) |
| Fluid Flow & Shear Stress | Typically Static | Dynamic, tunable flow |
| Barrier Function Assessment | Indirect (e.g., TEER with inserts) | Direct, real-time (integrated electrodes) |
| Key Readouts | Cytokine secretion, imaging, cytotoxicity. | Multi-parametric: TEER, biomarker kinetics, cell migration, force metrics. |
Table 2: Application-Specific Model Selection Guidelines
| Research Goal | Recommended Model | Primary Rationale |
|---|---|---|
| High-Throughput Compound Screening | Simple 3D Co-culture (Spheroid/Microplate) | Cost-effectiveness and scalability for large libraries. |
| Mechanistic Study of Immune Cell Recruitment | Multi-tissue OoC with endothelium | Recapitulates adhesion, extravasation, and interstitial migration under flow. |
| Initial Biocompatibility / Cytokine Storm Risk | Simple 2D Co-culture (PBMC with target) | Rapid, sensitive detection of immune cell activation. |
| PK/PD & Immune Cell-Mediated Toxicity | Multi-tissue (e.g., Liver + Immune OoC) | Models metabolically-derived toxicity and tissue-tissue crosstalk. |
| Barrier Integrity & Immune Interaction (e.g., Gut, BBB) | Dual-channel OoC with immune compartment | Maintains differentiated barrier, allows apical/basal access, incorporates shear. |
Detailed Experimental Protocols
Protocol 1: Establishing a Simple 3D Immune-Epithelial Co-Culture Spheroid for Cytotoxicity Screening.
- Objective: To assess T-cell mediated killing of tumor spheroids in a high-throughput format.
Materials:
- 96-well ultra-low attachment (ULA) round-bottom plate.
- Tumor cell line (e.g., HCT-116 colorectal carcinoma).
- Activated human peripheral blood T-cells (e.g., CD3/CD28 expanded).
- Co-culture medium (RPMI-1640 + 10% FBS + 1% P/S).
- Live/Dead viability dye (e.g., Calcein AM / Propidium Iodide).
- High-content imaging system or plate reader.
Method:
- Spheroid Formation: Seed 500-1000 tumor cells per well in 100µL of medium into the ULA plate. Centrifuge briefly (300 x g, 2 min) to aggregate cells. Culture for 72h to form compact spheroids.
- Immune Cell Addition: After 72h, gently add 100µL of medium containing effector T-cells at desired Effector:Target (E:T) ratios (e.g., 1:1, 5:1, 10:1) to respective wells. Control wells receive medium only.
- Co-Culture & Assay: Incubate for 24-48 hours. Add Live/Dead staining solution as per manufacturer's protocol.
- Imaging & Quantification: Image each spheroid using a high-content imager. Quantify total and dead cell area using automated analysis software (e.g., CellProfiler). Calculate % cytotoxicity:
(Dead Area in Co-culture / Total Area in Co-culture) - (Dead Area in Tumor-only / Total Area in Tumor-only) * 100.
Protocol 2: Operating a Dual-Channel Gut-on-a-Chip with Integrated Immune Monitoring.
- Objective: To model inflammatory response in an intestinal barrier following pro-inflammatory trigger.
Materials:
- Commercial dual-channel OoC system (e.g., Emulate, MIMETAS).
- Human intestinal epithelial cells (Caco-2 or primary organoids).
- Human primary intestinal microvascular endothelial cells (HIMECs).
- Peripheral blood mononuclear cells (PBMCs) or purified monocytes.
- Cell-specific culture media (epithelial, endothelial).
- Differentiation medium (for epithelial cells).
- Pro-inflammatory trigger (e.g., TNF-α/IL-1β or Lipopolysaccharide (LPS)).
- FITC-dextran (4 kDa) for permeability assay.
Method:
- Chip Priming & Cell Seeding: Sterilize chip (70% ethanol, UV). Coat the top (epithelial) channel with collagen IV and the bottom (endothelial) channel with fibronectin. Seed epithelial cells at high density into the top channel. Seed endothelial cells into the bottom channel 24h later.
- Barrier Formation & Differentiation: Connect chips to perfusion controller. Apply cyclic peristalsis-like strain if available. Perfuse channels with appropriate media at 30-60 µL/h. Culture for 5-7 days to form confluent, differentiated barriers. Monitor Transepithelial/Transendothelial Electrical Resistance (TEER) daily.
- Immune Challenge: Introduce PBMCs or monocytes into the endothelial (bottom) channel via injection port. Allow to adhere for 2h, then resume perfusion. 24h later, introduce LPS (1 µg/mL) apically or cytokines basally.
- Real-time Monitoring & Endpoint Analysis:
- TEER: Measure continuously or daily.
- Permeability: Add FITC-dextran to the apical channel; sample from basolateral channel hourly for 4h to calculate apparent permeability (Papp).
- Cytokine Secretion: Collect effluents from both channels for multiplex ELISA (e.g., IL-6, IL-8, IFN-γ).
- Immunofluorescence: Fix chips, stain for tight junctions (ZO-1), endothelial markers (CD31), and immune cells (CD45). Image via confocal microscopy.
Visualizations
Model Selection Decision Tree
Experimental Workflow Comparison
The Scientist's Toolkit: Research Reagent Solutions
| Item | Category | Function in Immune Response Assessment |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Microplate | Promotes the formation of 3D spheroids or organoids by inhibiting cell adhesion. Essential for simple 3D co-cultures. |
| Transwell/Cell Culture Inserts | Insert | Enables compartmentalized 2D co-culture for migration and barrier studies (e.g., immune cell transmigration). |
| Tunable Hydrogels (e.g., Matrigel, Collagen I) | Extracellular Matrix | Provides a physiologically relevant 3D scaffold for cell growth, differentiation, and immune cell infiltration assays. |
| Polydimethylsiloxane (PDMS) OoC Devices | Microfluidic Device | The most common material for fabricating OoC platforms; gas-permeable, biocompatible, and allows integration of electrodes. |
| Perfusion Controller (Syringe Pumps) | Instrument | Provides precise, continuous medium flow in OoC systems to deliver nutrients, shear stress, and circulate immune cells. |
| Transepithelial/Endothelial Electrical Resistance (TEER) Electrodes | Sensor | Measures real-time barrier integrity in OoC and Transwell systems; a key indicator of inflammation and damage. |
| Recombinant Human Cytokines/Chemokines | Biochemical | Used to stimulate immune responses (e.g., TNF-α, IFN-γ) or to polarize/differentiate immune cells (e.g., IL-4, TGF-β). |
| Multiplex Cytokine Assay (Luminex/ELISA) | Detection Kit | Quantifies a panel of secreted inflammatory mediators from limited sample volumes, crucial for both model types. |
| Live-Cell Imaging Dyes (e.g., Calcein AM, CellTracker) | Fluorescent Probe | Enables real-time tracking of cell viability, location, and interaction dynamics within 3D co-cultures and OoCs. |
| Neutralizing Antibodies (e.g., anti-IL-6, anti-PD-1) | Therapeutic Probe | Tool to block specific immune pathways and dissect mechanism of action in both simple and complex models. |
Within the thesis on 3D cell culture for immune response assessment, a critical translational challenge is bridging the gap between sophisticated in vitro models and regulatory acceptance for drug development. This document outlines application notes and protocols for generating qualification data for 3D immuno-oncology models, specifically focusing on a T-cell mediated tumor killing assay, to support their use in regulatory submissions for preclinical efficacy and safety.
Application Note: Qualification of a 3D Spheroid Co-culture Model for Immunotherapy Screening
Objective: To demonstrate that a 3D tumor spheroid/immune cell co-culture system yields reproducible, quantitative, and clinically predictive data on T-cell infiltration and cytotoxicity, suitable for inclusion in an Investigational New Drug (IND) application package.
Key Qualification Parameters & Data: Qualification hinges on establishing model reproducibility, relevance, and robustness. Data from a meta-analysis of recent studies (2023-2024) supports the superiority of 3D models in predicting immune cell penetration dynamics.
Table 1: Comparative Metrics of 2D vs. 3D Immune-Tumor Co-culture Models
| Metric | 2D Monolayer Co-culture | 3D Spheroid Co-culture | Significance for Qualification |
|---|---|---|---|
| T-cell Infiltration Depth | Not applicable (flat surface). | 40-150 µm, measured via confocal imaging. | Mimics physiological barrier; critical for assessing biotherapeutic penetration. |
| Coefficient of Variation (CV) in Cytotoxicity | 8-12% (across plates). | 10-15% (inter-spheroid, optimized protocols). | Demonstrates assay precision and reliability. |
| Predictive Correlation with In Vivo Response | R² = 0.45-0.60 (low). | R² = 0.75-0.85 (high, for immunotherapies). | Supports the model's relevance in defining pharmacodynamic biomarkers. |
| Z'-Factor (Assay Robustness) | 0.5 - 0.7 (moderate). | 0.6 - 0.8 (good to excellent). | Indicates a high-quality screen suitable for pivotal studies. |
| Multiplexing Capacity (Cell Phenotyping) | 2-3 markers simultaneously. | 4-6 markers via imaging cytometry. | Enables complex mechanism-of-action analysis. |
Experimental Protocols
Protocol 1: Generation of Qualified Tumor Spheroids for Co-culture
- Objective: Produce uniform, reproducible spheroids from a qualified cell bank.
- Materials: Tumor cell line (e.g., MC38-OVA), ultra-low attachment (ULA) 96-well round-bottom plates, complete RPMI-1640 medium.
- Procedure:
- Harvest tumor cells at 80-90% confluence. Count and assess viability (>95%).
- Prepare cell suspension at 5,000 cells/100 µL/well in complete medium.
- Seed 100 µL suspension into each well of a ULA plate.
- Centrifuge plate at 300 x g for 3 minutes to aggregate cells at well bottom.
- Incubate at 37°C, 5% CO₂ for 72 hours. Spheroids should form compact, spherical structures by day 3.
- Qualify spheroids by diameter measurement (target: 400-500 µm ± 10% CV) using brightfield imaging analysis.
Protocol 2: T-cell Activation and 3D Co-culture Cytotoxicity Assay
- Objective: Quantify antigen-specific T-cell-mediated killing in 3D spheroids.
- Materials: Activated OVA-specific CD8+ T-cells (e.g., OT-I), CellTiter-Glo 3D reagent, live-cell imaging dye (e.g., Calcein AM for tumor cells, CellTracker Red for T-cells).
- Procedure:
- T-cell Activation: Isolate and activate T-cells with OVA peptide (SIINFEKL, 1 µg/mL) and IL-2 (20 IU/mL) for 5-7 days prior to assay.
- Co-culture Setup:
- On day 0, generate tumor spheroids as per Protocol 1.
- On day 3, carefully add 50 µL of media containing activated T-cells to each spheroid well. Maintain an effector:target (E:T) ratio gradient (e.g., 0:1, 1:1, 5:1, 10:1). Include controls (spheroids only, T-cells only).
- Incubate for 48-72 hours.
- Endpoint Analysis:
- Viability: Transfer 50 µL of medium from each well to a white opaque plate. Add 50 µL of CellTiter-Glo 3D reagent to both the medium and the original spheroid well. Shake for 5 min, incubate for 25 min, and record luminescence. Tumor cell viability is proportional to luminescent signal.
- Imaging: For a subset, stain spheroids with Calcein AM (green, viable tumor) and propidium iodide (red, dead cells) and image using a confocal microscope to visualize killing zones and T-cell infiltration (Protocol 3).
Protocol 3: Multiplexed Confocal Imaging for Immune Cell Infiltration & Phenotyping
- Objective: Quantify T-cell infiltration depth and spatial relationships within the spheroid.
- Materials: 3D spheroids from co-culture, 4% PFA, permeabilization buffer (0.5% Triton X-100), blocking buffer (5% BSA), primary antibodies (anti-CD8, anti-CD3, anti-Granzyme B), fluorescent secondary antibodies, DAPI, confocal microscope.
- Procedure:
- Fix spheroids with 4% PFA for 45 min at RT.
- Permeabilize and block for 2 hours.
- Incubate with primary antibody cocktail overnight at 4°C.
- Wash and incubate with fluorescent secondary antibodies for 4 hours at RT. Add DAPI.
- Image using a 20x water immersion objective on a confocal microscope. Acquire Z-stacks (5-10 µm step size).
- Analysis: Use image analysis software (e.g., Imaris, FIJI) to create depth-intensity plots for CD8+ signal, calculate infiltration depth (distance from spheroid surface where signal drops to 50% of maximum), and quantify Granzyme B+ proximity to tumor nuclei.
Signaling Pathway & Experimental Workflow Visualization
Title: T-cell Activation & Killing Signaling Pathway
Title: 3D Immune Model Qualification Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for 3D Immune Response Assay Qualification
| Reagent / Material | Function in Qualification Strategy | Example Product/Catalog |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Promulates consistent, single spheroid formation per well, minimizing variability critical for reproducibility. | Corning Spheroid Microplates, Nunclon Sphera plates. |
| Defined Extracellular Matrix (ECM) | Provides a physiologically relevant scaffold (e.g., collagen, Matrigel) to study immune cell migration and barrier penetration. | Cultrex Basement Membrane Extract, Collagen Type I, High Concentration. |
| 3D-Optimized Viability Assay | Reagent formulated to penetrate spheroids and generate a linear signal proportional to cell number (e.g., ATP content). | CellTiter-Glo 3D Cell Viability Assay. |
| Live-Cell Fluorescent Tracking Dyes | Enable longitudinal, non-destructive imaging of distinct cell populations (tumor vs. immune) in co-culture. | CellTracker Green CMFDA, Far Red dyes. |
| Validated Phospho-/Cell Signaling Antibodies | For multiplexed imaging mass cytometry (IMC) or immunofluorescence to map signaling pathways within the 3D architecture. | Antibodies validated for IHC/IF and flow cytometry (e.g., CST, BioLegend). |
| Primary Human Immune Cells (from Qualified Donors) | Moves the model closer to human biology. Use of cryopreserved PBMCs or isolated T-cells from reputable biorepositories is essential. | Leukapheresis-derived PBMCs from STEMCELL Technologies or AllCells. |
| Automated Imaging & Analysis Software | Enables high-content, unbiased quantification of complex parameters (infiltration, killing zones, cell-cell distances) across large datasets. | Instruments: ImageXpress Confocal HT.ai; Software: Imaris, FIJI/ImageJ with 3D suites. |
Conclusion
3D cell culture models represent a paradigm shift in immune response assessment, bridging the critical gap between simplistic 2D assays and complex, costly in vivo studies. By faithfully incorporating spatial architecture, stromal support, and physiological gradients, these systems generate more clinically relevant data on immune cell trafficking, target engagement, and cytokine storms. Successful implementation requires careful model selection, methodological optimization, and rigorous validation against established benchmarks. As these technologies mature and standardization improves, their integration into the drug development pipeline will accelerate the discovery of novel immunotherapies, improve safety profiling, and reduce late-stage attrition. The future lies in increasingly sophisticated multi-tissue systems that will ultimately enable patient-specific immunological profiling, heralding a new era of precision immunology.