Bioengineered Skin with Immune Functions: Revolutionizing Dermatology Research and Drug Testing
This article provides a comprehensive overview of 3D skin constructs engineered to replicate human immunological functions.
Bioengineered Skin with Immune Functions: Revolutionizing Dermatology Research and Drug Testing
Abstract
This article provides a comprehensive overview of 3D skin constructs engineered to replicate human immunological functions. Targeted at researchers and drug development professionals, it explores the foundational biology of skin immunology, details cutting-edge methodologies for constructing immunocompetent models, addresses common challenges in model development and maintenance, and evaluates validation protocols against traditional models. The synthesis offers a roadmap for utilizing these advanced constructs to improve the predictive accuracy of preclinical testing for inflammatory skin diseases, immunotoxicity, and immunotherapy development.
The Living Shield: Deconstructing Skin Immunology for Bioengineering
This technical guide details the principal cellular and molecular components of the skin's immune system, termed skin-associated lymphoid tissues (SALT). Framed within ongoing research to develop immunocompetent 3D skin constructs, this whitpaper provides a foundational overview for scientists engineering tissues that accurately mimic cutaneous immunological functions for drug development and disease modeling.
The skin is a primary barrier and a dynamic immunological interface. Its resident and recruited cells form a sophisticated network for surveillance, tolerance, and defense. Replicating this system in vitro requires precise recapitulation of its architecture and signaling pathways, a core challenge in constructing 3D skin models with full immunological fidelity.
Key Cellular Players
The immunocompetent cells of the skin operate in a spatially organized manner.
Resident Immune Cells
- Keratinocytes: The predominant epidermal cells, acting as non-professional immune sentinels. They express Pattern Recognition Receptors (PRRs) and release antimicrobial peptides (AMPs), cytokines, and chemokines upon damage or pathogen encounter.
- Langerhans Cells (LCs): Dendritic cells (DCs) residing in the epidermis. They sample antigens, migrate to draining lymph nodes, and initiate adaptive immune responses.
- Dermal Dendritic Cells (dDCs): A heterogeneous population in the dermis with superior capacity for CD8+ T cell priming compared to LCs.
- Tissue-Resident Memory T Cells (T~RM~): Long-lived T cells that persist in the skin following antigen exposure, providing rapid local recall responses.
- Dermal Macrophages: Phagocytic cells involved in pathogen clearance, wound healing, and tissue homeostasis.
- Innate Lymphoid Cells (ILCs): Tissue-resident lymphocytes (e.g., ILC2s) that respond to cytokines and secrete effector molecules, regulating inflammation and barrier function.
Recruited Immune Cells
- Recirculating T Cells (CD4+, CD8+): Effector and helper cells recruited during inflammation.
- Neutrophils: First responders to injury or infection, executing phagocytosis and releasing neutrophil extracellular traps (NETs).
- Mast Cells: Granule-containing cells that degranulate in response to allergens via IgE, driving immediate hypersensitivity.
Table 1: Quantitative Distribution of Key Immune Cells in Human Skin
| Cell Type | Primary Location | Estimated Density (cells/mm²) | Key Surface Markers (Human) |
|---|---|---|---|
| Langerhans Cells | Epidermis | 200 - 1000 | CD1a, CD207 (Langerin), MHC-II |
| CD8+ T~RM~ Cells | Epidermis | 50 - 200 | CD8, CD69, CD103 |
| CD4+ T~RM~ Cells | Dermis | 100 - 500 | CD4, CD69, CD49a |
| Dermal DCs | Dermis | Variable | CD11c, MHC-II, CD1c (BDCA-1) |
| Dermal Macrophages | Dermis | 50 - 200 | CD68, CD163, CD11b |
Molecular Mediators and Signaling Pathways
Cellular crosstalk is governed by a complex cytokine and chemokine milieu.
Key Signaling Pathways
a) Keratinocyte Alarmin Response: Damage-associated molecular patterns (DAMPs) from stressed keratinocytes (e.g., IL-1α, IL-33, TSLP) activate dermal immune cells, initiating a type 2/immune-skewing response. b) LC/dDC Antigen Presentation & Migration: Antigen uptake triggers LC maturation (downregulation of E-cadherin, upregulation of CCR7), enabling migration towards CCL19/21 gradients to lymph nodes. c) IL-17/IL-23 Axis in Psoriasiform Inflammation: Dermal DC-derived IL-23 expands IL-17-producing T cells (Th17, γδ T cells), which drive keratinocyte hyperproliferation and AMP production.
Diagram 1: IL-23/IL-17 Inflammatory Pathway in Psoriasis Models
Cytokine and Chemokine Profiles
Table 2: Key Cytokines/Chemokines in Skin Immunity & Their Sources/Targets
| Mediator | Primary Cellular Source | Major Target/Function | Common Assay for Detection |
|---|---|---|---|
| TSLP | Keratinocytes | Activates dDCs (Th2 priming) | ELISA, IHC |
| IL-1β | Keratinocytes, Macrophages | Endothelial activation, fever | Luminex, Western Blot |
| IL-23 | Dermal DCs, Macrophages | Expansion of IL-17-producing cells | Flow Cytometry (intracellular) |
| IL-17A | Th17, γδ T cells, Tc17 | Keratinocyte activation | ELISA, RNA-Seq |
| CCL27 | Keratinocytes | Skin-homing T cells (CCR10+) | Multiplex Immunoassay |
| CCL19/21 | Lymphatic Endothelium | CCR7+ DC & T cell migration | Transwell Migration Assay |
Experimental Protocols for Key Assays in 3D Constructs
Protocol: Measuring Immune Cell Migration in a 3D Skin Construct
Objective: To assess chemotactic recruitment of immune cells into a dermal compartment.
- Construct Setup: Generate a bilayer 3D model with fibroblast-populated collagen dermis and differentiated epidermis.
- Challenge: Apply test compound (e.g., TNF-α, IL-1β) or vehicle to the culture medium at the "basal" side.
- Cell Loading: Label peripheral blood mononuclear cells (PBMCs) or specific immune subsets (e.g., CD4+ T cells) with a fluorescent cell tracker (e.g., Calcein AM).
- Introduction: Add labeled cells to the medium in a compartment separated from the dermis by a porous membrane (e.g., in a transwell setup) or directly into a "vascular" channel in microfluidic chips.
- Incubation: Culture for 24-48 hours.
- Analysis: Fix the construct, section, and stain for fluorescent cells and dermal markers (e.g., anti-CD3, anti-collagen I). Quantify infiltrated cells per dermal area using confocal microscopy and image analysis software (e.g., ImageJ).
Protocol: Evaluating Antigen-Specific Responses in an Epicutaneous Challenge Model
Objective: To model contact hypersensitivity in a 3D construct containing resident antigen-presenting cells.
- Construct Generation: Incorporate monocyte-derived Langerhans cells or DCs into the epidermal layer during airlift.
- Sensitization: Topically apply a hapten (e.g., DNFB at 0.5% in acetone:olive oil) to the stratum corneum for 24h.
- Rest Period: Culture in standard media for 5-7 days to allow for antigen processing and putative memory formation.
- Challenge: Re-apply a lower dose of the same hapten to a different site on the construct.
- Readout: At 24-48h post-challenge, quantify:
- Cytokines: Analyze culture supernatant for IFN-γ, IL-17, IL-22 via multiplex ELISA.
- Epidermal Damage: Measure lactate dehydrogenase (LDH) release.
- Marker Expression: Fix and stain for activation markers (e.g., CD86, HLA-DR) on DCs and T cells (if co-cultured).
Diagram 2: Workflow for 3D Skin Immune Challenge Assay
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for 3D Skin Immunology Research
| Item/Category | Example Product/Description | Function in Research |
|---|---|---|
| 3D Culture Scaffolds | Collagen Type I Matrix, Synthetic Fibrin-Based Hydrogels | Provides a physiologically relevant dermal structure for cell embedding and migration. |
| Immune Cell Media Supplements | Recombinant Human GM-CSF, IL-4, TGF-β, FLT3-L | Differentiates and maintains monocytes into dendritic cells or Langerhans-like cells within constructs. |
| Critical Cytokines/Chemokines | Recombinant Human TSLP, IL-1β, IL-23, CCL19, CCL27 | Used to challenge models and stimulate specific immune pathways for functional readouts. |
| Fluorescent Cell Trackers | CellTrace Violet, CFSE, Calcein AM | Labels immune cells prior to introduction into constructs to track migration and proliferation. |
| Live-Cell Imaging Dyes | Hoechst 33342 (nucleus), CellMask (membrane), pHrodo beads (phagocytosis) | Enables real-time, longitudinal visualization of cellular dynamics in live constructs. |
| Multiplex Immunoassay Panels | 25-Plex Human Cytokine/Chemokine Panel (Luminex-based) | Simultaneously quantifies a broad spectrum of soluble mediators from limited supernatant volumes. |
| Flow Cytometry Antibody Panels | Anti-human: CD1a, CD207, CD11c, HLA-DR, CD3, CD4, CD8, CD69, CD103 | Phenotypes and identifies immune cell populations extracted from dissociated 3D constructs. |
| Immunohistochemistry Antibodies | Anti-human: Loricrin (epidermal), Collagen I (dermal), CD3, CD68, IL-17A | Spatial profiling of structural and immune markers in fixed construct cross-sections. |
Faithfully replicating the skin's immune function in vitro hinges on integrating the precise cellular players and molecular networks described herein into a biomimetic 3D architecture. Current advanced models are incorporating patient-derived cells, spatially defined chemokine gradients, and vascularized channels to study trafficking. The ultimate goal is to generate standardized, immunocompetent skin constructs that predict human clinical responses for autoimmune, allergic, and infectious disease research, as well as for evaluating the immunogenicity of topical therapeutics and biologics.
Why Animal Models and 2D Cultures Fail to Capture Human Skin Immunity
Human skin is a complex immunological organ, featuring a stratified epithelium populated by resident and recruited immune cells that interact within a structured, three-dimensional (3D) microenvironment. Research into human skin immunity has historically relied on animal models and two-dimensional (2D) cell cultures. However, these systems exhibit significant limitations in recapitulating the human-specific architecture, cellular diversity, and dynamic immune responses of native skin. This whitepaper delineates the intrinsic shortcomings of these traditional models and frames the imperative for advanced 3D skin constructs that faithfully mimic human immunological functions, a core thesis in contemporary translational immunology.
Fundamental Limitations of Animal Models
Animal models, primarily mice, are phylogenetically distant from humans, leading to critical divergences in skin anatomy, immune cell composition, and receptor expression.
Table 1: Key Disparities Between Murine and Human Skin Immunity
| Aspect | Murine Skin | Human Skin | Implication for Modeling |
|---|---|---|---|
| Epidermal Thickness | Typically 1-3 cell layers (thin) | 50-100 μm (thick, stratified) | Altered barrier function and penetration kinetics for pathogens/topicals. |
| Immune Cell Repertoire | Dominated by γδ T cells (DETC); Different dendritic cell (DC) subsets. | Rich in αβ T cells; Distinct Langerhans cell and dermal DC networks. | Divergent initiators and effectors of adaptive immune responses. |
| Cytokine/Chemokine Profiles | Often different isoforms, expression levels, and receptor specificities (e.g., IL-8/CXCL8 family). | Human-specific signaling networks. | Inflammatory and chemotactic signals are not directly translatable. |
| Toll-like Receptor (TLR) Distribution | Differential expression patterns across skin layers and cell types. | Cell-type and compartment-specific expression. | Altered recognition of pathogen-associated molecular patterns (PAMPs). |
| Wound Healing | Primarily by contraction (panniculus carnosus muscle). | Primarily by re-epithelialization and granulation tissue. | Models of inflammatory skin healing are poorly representative. |
Experimental Protocol: Cross-Species Immune Response Profiling
- Objective: To quantify differences in cytokine release following a standardized immune challenge.
- Method:
- Sample Preparation: Generate full-thickness skin explants from human donors (surgical discard) and age-matched C57BL/6 mice.
- Challenge: Stimulate explants with 100 ng/mL of synthetic TLR2/TLR6 agonist (Pam2CSK4) or 1 μg/mL of Imiquimod (TLR7 agonist) for 24 hours.
- Analysis: Collect supernatant and perform a multiplex cytokine assay (e.g., Luminex) targeting IL-1β, IL-6, TNF-α, IFN-γ, IL-17A, IL-22, CCL2, and CXCL8.
- Data Normalization: Normalize cytokine concentrations to total explant protein content (BCA assay).
- Expected Outcome: Human skin will show a pronounced CXCL8 response and a distinct T helper cytokine ratio (Th1/Th17/Th22) compared to murine skin, which may show higher levels of IL-12p70 or KC (CXCL1).
Inadequacies of Conventional 2D Cell Cultures
Monolayer cultures of keratinocytes, fibroblasts, or immortalized cell lines lack the physiological context of tissue, leading to altered phenotypes and signaling.
Table 2: Limitations of 2D Cultures in Modeling Skin Immunity
| Parameter | 2D Culture Artifact | In Vivo Skin Reality | Consequence |
|---|---|---|---|
| Cell Morphology & Polarity | Flattened, stretched cytoskeleton; loss of apical-basal polarity. | Stratified, cuboidal to squamous cells with established polarity. | Disrupted intracellular signaling and secretion profiles. |
| Microenvironment | Homogeneous, rigid plastic/glass substrate (Young's modulus >> skin). | Compliant, laminin/collagen-rich ECM with gradient stiffness. | Aberrant mechanotransduction (e.g., via YAP/TAZ) affecting proliferation and inflammation. |
| Cell-Cell Interactions | Limited to same-plane contacts; no physiological 3D spatial organization. | Complex 3D networking via tight junctions, gap junctions, and desmosomes across strata. | Unrepresentative cell signaling and barrier formation. |
| Differentiation | Incomplete, often aberrant terminal differentiation program. | Orderly progression from basal proliferative to suprabasal, spinous, granular, and cornified layers. | Altered expression of antimicrobial peptides (AMPs) and immune mediators (e.g., IL-1 family cytokines). |
| Immune Co-Culture | Difficult to maintain primary immune cells; interactions occur on an unnatural plane. | Immune cells (e.g., T cells, Langerhans cells) reside in specific 3D niches and survey via dendrites. | Fail to model migration, antigen presentation in 3D, and paracrine signaling gradients. |
Experimental Protocol: Transcriptomic Analysis of 2D vs. 3D Keratinocytes
- Objective: To compare global gene expression profiles of human primary keratinocytes cultured in 2D monolayers vs. 3D air-liquid interface (ALI) constructs.
- Method:
- Culture Models:
- 2D: Culture keratinocytes to 80% confluence in submerged conditions with serum-free, low-Ca2+ medium.
- 3D: Seed keratinocytes on a contracted fibroblast-populated collagen lattice. Raise to ALI and culture for 14 days to achieve stratification.
- RNA Sequencing: Isolate total RNA (in triplicate) using a column-based kit with DNase treatment. Assess RNA integrity (RIN > 8.0).
- Library Prep & Sequencing: Prepare stranded mRNA libraries and sequence on an Illumina platform to a depth of ~30 million paired-end reads per sample.
- Bioinformatics: Map reads to the human genome. Perform differential expression analysis (e.g., DESeq2). Conduct gene set enrichment analysis (GSEA) on hallmark and immune signature pathways.
- Culture Models:
- Expected Outcome: 3D constructs will show significant upregulation of genes associated with epidermal differentiation (e.g., FLG, IVL, LOR), barrier lipid synthesis, and key immune mediators (e.g., DEFB4A, IL36G), while 2D cultures will show enrichment for proliferation and stress-response pathways.
The Emergence of 3D Immunocompetent Skin Constructs
Advanced 3D models integrate multiple cell types in a biomimetic scaffold, enabling the study of human-specific immune responses.
The Scientist's Toolkit: Key Reagents for 3D Immunocompetent Skin Models
| Reagent / Material | Function & Rationale |
|---|---|
| Primary Human Keratinocytes | Essential autologous cell source for forming a stratified, differentiated epidermis. Isolated from neonatal foreskin or adult skin biopsies. |
| Primary Human Dermal Fibroblasts | Generate and remodel the dermal ECM, providing crucial mechanical and biochemical cues for epidermal morphogenesis. |
| Type I Collagen (Rat tail or bovine) | The major structural protein of the dermis; forms a hydrogel scaffold for fibroblast embedding and contraction. |
| Air-Liquid Interface (ALI) Culture Media | Specialized, serum-free media (e.g., EpiLife with defined supplements) that promotes terminal differentiation when the epidermis is exposed to air. |
| Immune Cell Additives | CD14+ Monocytes: Differentiate into Langerhans-like cells or macrophages within the construct. Peripheral Blood Mononuclear Cells (PBMCs): Source for T cells. IL-4 & GM-CSF: Cytokines to drive DC differentiation from monocytes. |
| Matrigel or Fibrin Gels | Alternative/complementary matrices to collagen, providing a more complex basement membrane-like environment. |
| Transwell Inserts (e.g., 0.4 μm pore) | Permissible membrane supports that allow separate compartmentalization of dermal and epidermal layers and medium diffusion. |
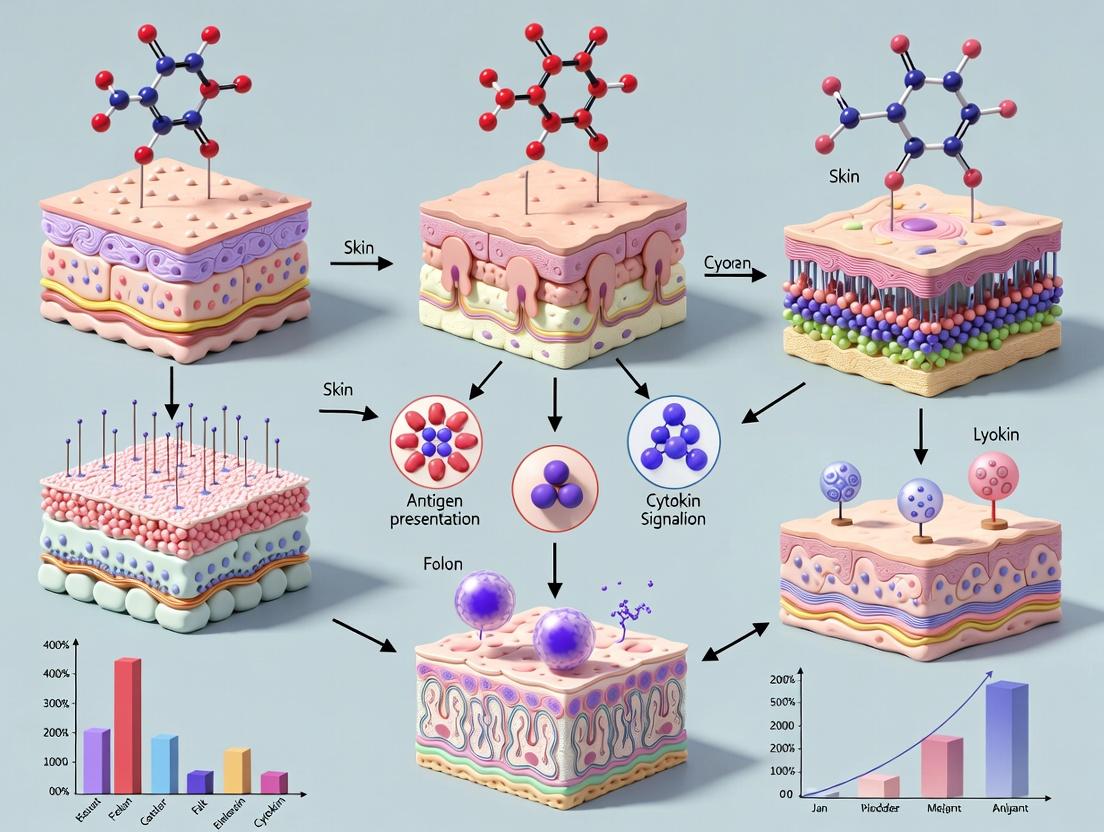
Visualizing Key Concepts and Workflows
Animal models and 2D cell cultures provide foundational but incomplete insights into human skin immunity. Their inherent biological discrepancies and structural oversimplifications, respectively, limit their predictive value for human disease mechanisms and therapeutic efficacy. The development and standardization of sophisticated 3D immunocompetent skin constructs represent a paradigm shift. By incorporating human cells in a biomimetic architecture, these models offer a physiologically relevant platform to dissect human-specific immune pathways, screen novel therapeutics, and advance personalized medicine approaches in dermatology and immunology. This evolution is central to the thesis that future breakthroughs in understanding cutaneous immunity will be driven by models that recapitulate the human tissue context in vitro.
Core Design Principles for an Immunocompetent 3D Skin Construct
Within the broader research thesis on engineering 3D skin constructs that recapitulate immunological functions, this guide details the core design principles required to move beyond structural mimicry to dynamic immunocompetence. The ultimate goal is to create a physiologically relevant in vitro platform for studying cutaneous immunology, testing immunomodulatory therapeutics, and improving skin graft outcomes. This requires integrating the cellular actors, signaling networks, and tissue-level organization that define the skin's immune niche.
Foundational Cellular Components
An immunocompetent construct must incorporate the key residential and transient immune cells of human skin. The resident cells provide constant surveillance and initial response, while the capacity to recruit circulating immune cells adds a critical layer of functionality.
Table 1: Essential Cellular Constituents and Their Functions
| Cell Type | Primary Function in Skin Immunity | Recommended Source for Construct |
|---|---|---|
| Keratinocytes | Barrier; production of antimicrobial peptides (AMPs), cytokines (e.g., IL-1α, TSLP); antigen presentation via MHC-II. | Primary human keratinocytes (HEKn/HEKa) or immortalized lines (HaCaT). |
| Dermal Fibroblasts | Structural support; secretion of extracellular matrix (ECM); production of chemokines (e.g., CXCL12) and cytokines. | Primary human dermal fibroblasts (HDF). |
| Langerhans Cells (LCs) | Epidermal dendritic cells; antigen capture, processing, and presentation; immune regulation. | CD34+ hematopoietic progenitor cell-derived or monocyte-derived LCs. |
| Dermal Dendritic Cells (DDCs) | Antigen presentation in dermis; key link between innate and adaptive immunity. | Monocyte-derived DCs or specific DC subsets. |
| Resident Memory T Cells (TRM) | Long-lived, tissue-resident lymphocytes providing rapid recall responses. | Isolation from human skin or in vitro differentiation and migration into construct. |
| Macrophages | Phagocytosis; cytokine secretion; tissue repair and remodeling. | Primary monocytes (e.g., CD14+) differentiated into M0/M1/M2 phenotypes. |
| Mast Cells | IgE-mediated hypersensitivity; release of pre-formed granules (histamine, tryptase). | CD34+ progenitor-derived or cord blood-derived mast cells. |
Core Architectural and Biochemical Design Principles
Stratified and Compartmentalized Architecture
The construct must physically separate the epidermal and dermal compartments to model their distinct immune microenvironments.
- Dermal Equivalent: A collagen type I hydrogel (e.g., rat tail or bovine) populated with HDFs forms the foundation. Incorporating other ECM components (e.g., elastin, hyaluronic acid) enhances physiological relevance and influences immune cell behavior.
- Epidermal Equivalent: Keratinocytes are seeded on the dermal equivalent and raised to the air-liquid interface (ALI) to induce terminal differentiation, stratum corneum formation, and proper barrier function.
Immune Cell Localization and Niche Engineering
- Epidermal Niche: Langerhans Cells must be incorporated within the stratified epithelium prior to ALI culture. A standard protocol involves seeding LCs with keratinocytes.
- Dermal Niche: Macrophages, DDCs, and TRM cells should be embedded within the dermal equivalent during hydrogel polymerization to ensure even distribution.
Dynamic Soluble Signaling Environment
The construct's medium must be tailored to support both epithelial and immune cell viability without suppressing immune functionality. This often involves a reduction of high-level immunosuppressants like hydrocortisone and use of specific cytokine cocktails (e.g., GM-CSF, IL-4 for DC maintenance).
Key Experimental Protocols for Validation
Protocol: Immune Challenge and Cytokine Profiling
Objective: To assess the construct's functional response to a pathogenic stimulus.
- Stimulation: Apply a Toll-like receptor (TLR) agonist (e.g., 100 ng/mL Lipopolysaccharide (LPS) for TLR4, 1 µg/mL Pam3CSK4 for TLR1/2) to the construct surface or culture medium.
- Sampling: At timepoints (e.g., 6h, 24h, 48h) post-stimulation, collect supernatant.
- Analysis: Use a multiplex bead-based immunoassay (e.g., Luminex) to quantify a panel of pro-inflammatory cytokines (IL-1β, IL-6, IL-8, TNF-α, IFN-γ). Validation: Compare cytokine secretion profiles to those from ex vivo human skin explants under identical stimulation.
Protocol: Antigen-Specific T Cell Activation Assay
Objective: To validate the antigen-presenting capability of dendritic cells within the construct.
- Antigen Loading: Apply a model antigen (e.g., 10 µg/mL Ovalbumin) +/- an adjuvant to the construct surface for 24h.
- T Cell Co-culture: Isolate CD4+ or CD8+ T cells from peripheral blood and label with a cell proliferation dye (e.g., CFSE).
- Interaction: Harvest cells from the construct by enzymatic digestion (dispase/collagenase) and co-culture with autologous CFSE-labeled T cells at a 1:10 (DC:T) ratio for 5 days.
- Readout: Analyze T cell proliferation via CFSE dilution by flow cytometry and measure activation markers (CD25, CD69) and effector cytokines (IFN-γ, IL-2).
Protocol: Barrier Integrity Assessment Post-Immune Challenge
Objective: To correlate immune activation with tissue barrier disruption.
- Challenge: Stimulate constructs as in Protocol 4.1.
- Measurement: Use a transepithelial electrical resistance (TEER) meter or apply fluorescent tracers (e.g., 4 kDa FITC-Dextran) to the apical surface.
- Quantification: Measure TEER (Ω·cm²) over time or quantify the flux of tracer into the basal medium via fluorometry. Table 2: Expected Quantitative Outcomes for a Mature Construct
| Assay | Baseline (Unstimulated) | Post-Stimulation (24h LPS) | Measurement Method |
|---|---|---|---|
| Barrier Integrity (TEER) | >250 Ω·cm² | Decrease of 30-60% | TEER Electrode |
| IL-8 Secretion | 50-200 pg/mL | 10-50 fold increase | Multiplex ELISA |
| LC Migration (to medium) | <5% of total LCs | >20% of total LCs | Flow Cytometry (CD1a+ HLA-DR+) |
| T Cell Proliferation (CFSE Low) | <15% | >40% (with antigen) | Flow Cytometry |
Visualization of Critical Pathways and Workflows
Title: Skin Immune Response to Pathogen Signal
Title: 3D Skin Construct Assembly and Testing Flow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Immunocompetent Skin Model Research
| Reagent/Material | Function | Example Product/Supplier |
|---|---|---|
| Type I Collagen, High Concentration | Forms the foundational dermal hydrogel matrix. | Rat tail collagen I, Corning Matrigel (for basement membrane). |
| Defined Keratinocyte-SFM Media | Supports keratinocyte growth and differentiation with defined components. | Gibco Epilife or KGM-Gold BulletKit. |
| Cytokine Cocktails (GM-CSF, IL-4, IL-1β, M-CSF) | Differentiates and maintains immune cell populations (LCs, DCs, Macrophages) within the construct. | PeproTech or R&D Systems recombinant human proteins. |
| Toll-like Receptor (TLR) Agonists | Standardized pathogen-associated molecular patterns (PAMPs) for immune challenge experiments. | InvivoGen Ultrapure LPS (TLR4), Pam3CSK4 (TLR1/2). |
| Dispase II & Collagenase D | Enzymatic digestion of construct for harvesting embedded cells for flow cytometry. | Roche or Worthington Biochemical. |
| Multiplex Cytokine Assay Kits | Simultaneous quantification of multiple inflammatory mediators from limited supernatant volumes. | Bio-Plex Pro Human Cytokine Assays (Bio-Rad), LEGENDplex (BioLegend). |
| Fluorescent Tracers (FITC-Dextran) | Quantification of paracellular barrier permeability. | Sigma-Aldrich FD4 (4 kDa FITC-Dextran). |
| Transwell Permeable Supports | Physical scaffold for ALI culture and easy access for TEER measurement. | Corning Transwell with polycarbonate membrane. |
The development of advanced 3D skin constructs represents a paradigm shift in dermatological research, toxicology, and immunology. A central challenge is defining the criteria for a successful model that accurately recapitulates human immune responses. This whitepaper delineates two core philosophies: Structural Mimicry, which focuses on replicating the precise cellular and architectural composition of native skin, and Functional Mimicry, which prioritizes the accurate emulation of biological processes and signaling outcomes, even if achieved through alternative cellular mechanisms. The ultimate thesis is that while structural fidelity provides a essential foundation, the definitive validation of a 3D immunocompetent skin model lies in its functional output.
Conceptual Framework and Definitions
- Structural Mimicry: Success is measured by the presence and physical organization of key immune components (e.g., Langerhans cells, dermal dendritic cells, resident memory T-cells, mast cells) within their correct epidermal and dermal compartments. Metrics include cell count, spatial distribution, and marker expression.
- Functional Mimicry: Success is measured by the model's capacity to execute complex immune behaviors. Key readouts include: cytokine/chemokine release profiles upon challenge, antigen presentation efficacy, T-cell activation and recruitment, and the execution of inflammatory or tolerogenic pathways.
Quantitative Data Comparison: Structural vs. Functional Readouts
The following tables summarize benchmark data from recent studies on advanced 3D skin constructs.
Table 1: Structural Metrics for Immune Cell Incorporation
| Immune Cell Type | Target Localization | Typical Density in Native Skin (cells/mm²) | Achieved in Advanced Constructs (cells/mm²) | Method of Incorporation |
|---|---|---|---|---|
| Langerhans Cells (LCs) | Epidermis, Basal/Suprabasal | 200-400 | 50-150 | CD34+ progenitor seeding or post-culture integration |
| Dermal Dendritic Cells | Papillary Dermis | 100-200 | 20-80 | Monocyte-derived DC seeding in dermal layer |
| Resident Memory T Cells (Trm) | Epidermis/Dermis | Variable | Low (<10) | Co-culture with pre-activated T-cell clones |
| Mast Cells | Dermis, perivascular | 40-120 | 10-40 | Seeding of cord blood-derived mast cell progenitors |
Table 2: Functional Response Benchmarks to Standard Challenges
| Challenge Agent (Protocol) | Key Functional Readout | Native Skin/Ex Vivo Response (Peak Concentration) | 3D Construct Response (Peak Concentration) | Time to Peak (Construct) |
|---|---|---|---|---|
| Toll-like Receptor Agonist (e.g., Poly I:C) | CXCL8 (IL-8) Secretion | 500-1500 pg/mL | 200-800 pg/mL | 24-48 hours |
| Allergen (e.g., NiSO₄) | CCL18 Secretion | 100-300 pg/mL | 50-200 pg/mL | 48-72 hours |
| Antigen-Specific T-Cell Activation (OVA model) | IFN-γ Secretion | 1000-3000 pg/mL | 300-1200 pg/mL | 72-96 hours |
| Viral Mimic (HSV-1 Peptide) | Granzyme B Release (CD8+ T-cell) | Detectable Cytotoxicity | Variable, often lower | 96-120 hours |
Experimental Protocols for Key Validations
Protocol 1: Assessing Antigen Presentation Capability (Functional Assay)
- Objective: To evaluate the ability of construct-derived antigen-presenting cells (APCs) to process and present antigen to naïve T-cells.
- Materials: 3D skin construct with integrated LCs/DCs, OVA protein (or model antigen), CFSE-labeled, OVA-specific transgenic CD4+ T-cells (e.g., OT-II).
- Methodology:
- Apply soluble OVA (100 µg/mL) topically to construct air-liquid interface for 24h.
- Isolate migratory APCs from the culture medium (containing cells that have migrated out of the construct) using CD11c+ magnetic bead selection.
- Co-culture isolated APCs with CFSE-labeled OT-II T-cells at a 1:10 APC:T-cell ratio in a 96-well plate for 72-96 hours.
- Analyze T-cell proliferation via CFSE dilution by flow cytometry and measure Th1/Th2 cytokine profiles (IL-2, IFN-γ, IL-4, IL-13) in supernatant by multiplex ELISA.
- Success Metric: Significant CFSE dilution and IFN-γ release compared to constructs without antigen challenge.
Protocol 2: Spatial Mapping of Immune Cells (Structural Assay)
- Objective: To quantify density and distribution of key immune cells in the 3D construct.
- Materials: Cryosectioned 3D construct, antibodies for CD207 (Langerin), CD1a, CD3, CD11c, MHC-II, appropriate fluorescent secondary antibodies.
- Methodology:
- Fix construct in 4% PFA for 2-4 hours, cryoprotect in 30% sucrose, embed in OCT, and section at 10-12 µm thickness.
- Perform multiplex immunofluorescence staining using Opal tyramide signal amplification or similar to allow simultaneous labeling of 4-6 markers.
- Image sections using a confocal microscope with automated tile-scanning.
- Use image analysis software (e.g., QuPath, ImageJ with plugins) to perform cell segmentation based on nuclear stain (DAPI) and quantify marker-positive cells within user-defined epidermal and dermal regions.
- Success Metric: Quantitative data on cell density (cells/mm²) and stratification (epidermal vs. dermal localization) matching reference histology data.
Visualizing the Key Signaling Pathways
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function & Relevance |
|---|---|
| Primary Human Keratinocytes & Fibroblasts | Foundation for constructing the epidermal and dermal layers. Autologous sourcing enables patient-specific models. |
| CD34+ Hematopoietic Progenitor Cells (HPCs) | Critical for de novo generation and integration of Langerhans cells within the epidermis upon differentiation. |
| Monocyte-derived Dendritic Cell (moDC) Precursors | Used to seed the dermal compartment with professional antigen-presenting cells. |
| Chemically Defined ALI Medium | Supports stratification and cornification at the air-liquid interface. Must be cytokine-replete for immune cell viability. |
| Toll-like Receptor (TLR) Agonists (e.g., Poly I:C (TLR3), LPS (TLR4)) | Standardized pathogen mimics to challenge the construct and trigger innate immune pathways. |
| Haptens & Allergens (e.g., NiSO₄, DNCB) | To model allergic contact dermatitis and assess functional sensitization responses. |
| Antigen-Specific T-Cell Clones/Transgenic T-Cells (e.g., OT-I, OT-II) | Essential tools for quantifying antigen-specific, MHC-restricted T-cell activation (functional mimicry gold standard). |
| Multiplex Cytokine Assay Panels (e.g., Luminex, MSD) | Enable simultaneous quantification of a broad panel of pro-inflammatory, Th1, Th2, and regulatory cytokines from limited supernatant volumes. |
| Multi-plex Immunofluorescence Reagents (e.g., Opal TSA) | Allow spatial phenotyping of multiple cell types within a single tissue section, critical for structural validation. |
Building the Model: Techniques for Creating Immune-Reactive Skin Constructs
Within the advanced research field of developing 3D skin constructs that mimic immunological functions, the choice of cellular starting material is a foundational determinant of experimental success and translational relevance. This technical guide provides an in-depth analysis of the three core cell sourcing strategies—primary cells, induced pluripotent stem cells (iPSCs), and immortalized cell lines—framed specifically for applications in immunocompetent skin modeling. The selection directly impacts the construct's physiological accuracy, longevity, scalability, and ability to replicate complex immune-stromal-epithelial crosstalk.
Primary Cells: The Gold Standard for Fidelity
Primary cells, isolated directly from human tissue (e.g., donor skin), offer the highest degree of physiological relevance. For immunocompetent skin models, this includes primary keratinocytes, fibroblasts, and critically, immune cells like Langerhans cells, dermal dendritic cells, and resident memory T cells.
Key Advantages: Native phenotype, correct epigenetic landscape, and authentic functional responses. Major Limitations: Donor variability, finite lifespan, limited expansion capacity, and ethical/logistical constraints for certain immune cell subsets.
Protocol: Isolation of Primary Human Keratinocytes and Dermal Fibroblasts from Skin Biopsy
- Tissue Acquisition: Obtain de-identified human skin samples (e.g., from reconstructive surgery) with IRB approval.
- Disinfection & Processing: Rinse biopsy in 70% ethanol, then in PBS with 1% Antibiotic-Antimycotic. Remove subcutaneous fat.
- Dermal-Epidermal Separation: Incubate tissue overnight at 4°C in Dispase II solution (2.4 U/mL in PBS).
- Epidermal Cell (Keratinocyte) Isolation:
- Peel off the epidermis and place in Trypsin-EDTA (0.25%) for 15 min at 37°C.
- Neutralize with serum-containing medium. Filter through a 70 µm strainer.
- Centrifuge and resuspend in Defined Keratinocyte-SFM.
- Dermal Cell (Fibroblast) Isolation:
- Mince the remaining dermis finely and incubate in Collagenase Type I (1 mg/mL in DMEM) for 4-6 hours at 37°C on a shaker.
- Filter through a 100 µm strainer.
- Centrifuge and culture in Fibroblast Growth Medium (DMEM, 10% FBS, 1% AA).
Induced Pluripotent Stem Cells (iPSCs): Unlimited Potential with Engineered Complexity
iPSCs, reprogrammed from somatic cells, provide a scalable, donor-defined source for generating any cell type, including rare or inaccessible tissue-resident immune cells. This is pivotal for creating genetically diverse or patient-specific disease models.
Key Advantages: Unlimited self-renewal, potential for autologous models, ability to gene-edit and introduce disease-specific mutations. Major Limitations: High cost, lengthy differentiation protocols, potential epigenetic artifacts, and variability in differentiation efficiency.
Protocol: Directed Differentiation of iPSCs to Skin Keratinocytes via Dual-SMAD Inhibition & Epidermal Induction
- Maintenance: Culture iPSCs on Matrigel in mTeSR1 medium.
- Definitive Ectoderm Induction (Days 0-5): At 80% confluence, switch to Ectoderm Induction Medium (DMEM/F12, 1% N2 supplement, 1% non-essential amino acids) containing 10 µM SB431542 (TGF-β inhibitor) and 100 nM LDN193189 (BMP inhibitor). Change medium daily.
- Pre-Placodal Ectoderm Patterning (Days 5-9): Switch to Keratinocyte Induction Medium (KIM: DMEM, 10% FBS, 1% AA) supplemented with 10 ng/mL BMP4 and 10 ng/mL retinoic acid.
- Epidermal Commitment (Days 9-18): Culture cells in KIM only, with media changes every other day. Observe emergence of KRT5/14+ epithelial clusters.
- Purification & Expansion (Day 18+): Manually pick or FACS-sort KRT5/14+ clusters. Plate on collagen IV-coated dishes in Defined Keratinocyte-SFM.
Immortalized Cell Lines: Consistency and Scalability for Screening
Immortalized lines (e.g., HaCaT keratinocytes, THP-1 monocytes) are genetically altered to proliferate indefinitely. They are invaluable for high-throughput mechanistic studies and toxicity screening but have compromised physiological responses.
Key Advantages: Genetic uniformity, infinite expansion, cost-effective scaling. Major Limitations: Altered metabolism, karyotypic abnormalities, and loss of tissue-specific functions and immune competency.
Protocol: Differentiating THP-1 Monocytes into Macrophage-like Cells for Incorporation into 3D Constructs
- Culture: Maintain THP-1 cells in RPMI-1640 with 10% FBS, 0.05 mM 2-mercaptoethanol.
- Differentiation: Seed cells at 5x10^5 cells/mL in culture medium supplemented with 100 ng/mL Phorbol 12-myristate 13-acetate (PMA).
- Incubation: Incubate for 48-72 hours. Cells will adhere and adopt a macrophage-like morphology.
- Resting: Replace medium with fresh RPMI-1640 + 10% FBS (without PMA) and rest for 24 hours to allow cells to return to a resting state.
- Harvesting: Gently scrape adherent cells for downstream incorporation into dermal equivalents.
Comparative Analysis and Application in Immunocompetent Skin Constructs
The strategic application of each sourcing method depends on the research phase. Primary cells are optimal for final validation models, iPSCs for patient-specific disease modeling and genetic studies, and immortalized lines for initial protocol development and large-scale screening.
Table 1: Quantitative Comparison of Cell Sourcing Strategies
| Parameter | Primary Cells | iPSC-Derived Cells | Immortalized Lines |
|---|---|---|---|
| Physiological Relevance | High (Native) | Moderate-High (Depends on differentiation) | Low (Genetically altered) |
| Proliferative Capacity | Low (≤10 passages) | Very High (Unlimited) | Very High (Unlimited) |
| Donor Variability | High | Defined by donor iPSC clone | None (Clonal) |
| Cost per 10^6 Cells | High ($200-$500) | Very High ($500-$2000) | Low (<$50) |
| Time to Experiment | Short (Days) | Long (Weeks to months) | Short (Days) |
| Genetic Manipulability | Low | Very High (CRISPR at iPSC stage) | Moderate |
| Typical Use Case | Final validation of immunocompetent constructs | Modeling genetic diseases, autologous immunity | Pilot studies, high-throughput compound screening |
Table 2: Functional Output in 3D Skin Constructs
| Output | Primary Cells | iPSC-Derived | Immortalized Lines |
|---|---|---|---|
| Barrier Integrity (TEER) | 1,500 - 3,000 Ω*cm² | 800 - 2,000 Ω*cm² | 200 - 500 Ω*cm² |
| Cytokine Secretion (Upon LPS challenge) | Physiologic, donor-dependent | Variable, often elevated | Often blunted or non-physiologic |
| Antigen-Presenting Cell Function | Present & Functional | Can be generated, requires validation | Requires artificial activation (e.g., PMA) |
| Long-term Culture Stability | 2-4 weeks | 4+ weeks (with care) | Indefinite |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Cell Sourcing & 3D Construct Assembly
| Item | Function | Example Product/Catalog |
|---|---|---|
| Defined Keratinocyte-SFM | Serum-free medium for expansion of primary or iPSC-derived keratinocytes without differentiation. | Gibco Defined Keratinocyte-SFM |
| mTeSR1 | Feeder-free, defined medium for maintenance of human iPSCs/ESCs. | STEMCELL Technologies, #85850 |
| Y-27632 (ROCK inhibitor) | Improves survival of dissociated single cells, especially iPSCs and primary keratinocytes. | Tocris, #1254 |
| Collagen Type I, Rat Tail | Major component for forming the dermal equivalent (contracted fibroblast lattice). | Corning, #354236 |
| Dispase II | Neutral protease used for clean separation of epidermis from dermis. | Sigma, D4693 |
| Matrigel/Geltrex | Basement membrane extract for coating plates for iPSC culture or air-liquid interface assays. | Corning Matrigel, #356231 |
| LPS (Lipopolysaccharide) | Toll-like receptor 4 agonist used to challenge and test the immune function of skin constructs. | InvivoGen, tlrl-3pelps |
| LIVE/DEAD Viability/Cytotoxicity Kit | Fluorometric assay to assess cell viability within 3D constructs. | Thermo Fisher, L3224 |
Visualizing Key Workflows and Pathways
The development of 3D skin constructs that accurately mimic native immunological functions is a cornerstone of advanced dermatological research, toxicology testing, and immunomodulatory drug discovery. A critical determinant of success is the scaffold, which provides the structural and biochemical microenvironment necessary for resident and recruited immune cell function. This technical guide examines three pivotal scaffold categories—hydrogels, decellularized matrices, and 3D-bioprinted architectures—detailing their properties, fabrication protocols, and specific utility in engineering immunocompetent skin models.
Hydrogels: Tunable Microenvironments for Immune Signaling
Hydrogels, crosslinked polymer networks with high water content, are ideal for encapsulating skin cells (keratinocytes, fibroblasts) and immune cells (Langerhans cells, macrophages). Their mechanical and biochemical properties can be finely tuned to direct cell behavior and cytokine signaling.
Key Signaling Pathways Modulated by Hydrogel Stiffness: The mechanical properties of hydrogels, typically defined by elastic modulus (Young's modulus), directly influence immune cell activation via mechanotransduction pathways, crucial for mimicking immunological functions in skin.
Diagram 1: Stiffness-mediated immune cell activation pathway.
Protocol: Fabrication of a Tuneable HA-MA Hydrogel for Macrophage Encapsulation
- Objective: Create methacrylated hyaluronic acid (HA-MA) hydrogels of defined stiffness to study macrophage polarization.
- Materials: HA-MA polymer, Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) photoinitiator, UV light (365 nm, 5-10 mW/cm²).
- Steps:
- Dissolve HA-MA in PBS at desired concentration (e.g., 2%, 4%, 6% w/v).
- Add LAP photoinitiator to a final concentration of 0.1% w/v. Protect from light.
- Mix thoroughly and add human monocyte-derived macrophages (e.g., 1x10^6 cells/mL).
- Pipette the cell-polymer mix into a mold.
- Crosslink via UV exposure for 30-60 seconds.
- Culture in supplemented macrophage media, assessing phenotype (M1/M2) via flow cytometry for CD80/CD206 and cytokine ELISA (IL-10, IL-12) at 72 hours.
Decellularized Matrices: Preserving Native Immunomodulatory Cues
Decellularized extracellular matrix (dECM) from human or porcine skin provides a biologically complex scaffold retaining native composition (collagens, glycosaminoglycans, fibronectin) and bound signaling molecules that guide immune cell recruitment and function.
Protocol: Preparation and Recellularization of Human Dermal dECM
- Objective: Generate an immunologically active dermal scaffold for reconstructing a skin model with resident immune cells.
- Materials: Full-thickness human skin (donor), 1% (w/v) Sodium dodecyl sulfate (SDS), DNase I solution, PBS/Antibiotic-Antimycotic.
- Steps:
- Decellularization: Cut skin to 0.5 mm thickness. Agitate in 1% SDS for 48-72 hours (change solution every 24h). Rinse in PBS for 72 hours.
- Enzyme Treatment: Treat with DNase I (100 U/mL) for 6 hours at 37°C to remove residual nucleic acids.
- Sterilization: Rinse extensively. Sterilize in PBS with 5x Antibiotic-Antimycotic for 48h.
- Validation: Confirm decellularization via H&E/DAPI staining and quantify residual DNA (<50 ng/mg tissue).
- Recellularization: Seed human dermal fibroblasts (2x10^5 cells/cm²) onto the dermal side. Culture for 14 days. Subsequently, seed keratinocytes (1x10^5 cells/cm²) on the epidermal side and culture at air-liquid interface for 7-14 days. Introduce Langerhans cell precursors or dendritic cells prior to air-lift.
3D Bioprinting: Architecting Spatial Immune Niches
3D bioprinting enables the precise spatial patterning of multiple cell types and matrix components, allowing the construction of skin models with defined immunological zones (e.g., epidermal Langerhans cell network, dermal macrophage populations).
Bioprinting Workflow for Immunocompetent Skin.
Diagram 2: Multi-material bioprinting workflow for skin.
Protocol: Extrusion Bioprinting of a Stratified Skin Model with Immune Cells
- Objective: Print a tri-layered construct containing fibroblasts, keratinocytes, and Langerhans cell precursors.
- Materials: Thermoplastic gelatin-based bioink, Type I collagen bioink, extrusion bioprinter, 37°C heated stage.
- Steps:
- Bioink Preparation:
- Dermal Layer: Mix human fibroblasts (5x10^6 cells/mL) with neutralized Type I collagen solution.
- Epidermal Layer: Suspend keratinocytes (1x10^7 cells/mL) in a gelatin-based bioink at 28°C.
- Immune Niche Layer: Suspend Langerhans cell precursors (1x10^6 cells/mL) in a gelatin-based bioink.
- Printing: Load bioinks into separate print cartridges. Program a sequential print:
- Layer 1: Print dermal collagen layer in a lattice pattern.
- Layer 2: Print immune niche bioink in a defined pattern on the dermal layer.
- Layer 3: Print a dense, continuous epidermal layer over the previous layers.
- Crosslinking: Gel the construct at 37°C for 30 minutes.
- Maturation: Culture submerged for 3 days, then transfer to air-liquid interface culture for 10-14 days to promote epidermal stratification and immune cell maturation.
- Bioink Preparation:
Comparative Data & The Scientist's Toolkit
Table 1: Quantitative Comparison of Scaffold Modalities for Immunological Skin Models
| Parameter | Synthetic Hydrogels (e.g., PEG, HA-MA) | Natural Hydrogels (e.g., Collagen, Fibrin) | Decellularized ECM (dECM) | 3D Bioprinted Constructs |
|---|---|---|---|---|
| Typical Elastic Modulus | 0.1 - 50 kPa (highly tunable) | 0.5 - 5 kPa (soft) | 1 - 20 kPa (tissue-specific) | 0.5 - 100 kPa (design-dependent) |
| Key Immunological Advantage | Precise control over mechanical & biochemical cues for immune cell mechanobiology studies. | Natural cell adhesion motifs support innate immune cell migration and function. | Preserves native immunomodulatory matrikines and chemoattractants. | Enables precise spatial organization of immune cell populations. |
| Primary Research Application in Thesis | Studying stiffness-induced macrophage polarization or T-cell activation. | Modeling dendritic cell migration through the dermis. | Creating a pro-healing microenvironment for studying chronic inflammation. | Engineering controlled immune cell "niches" for drug screening. |
| Typical Pore Size | 5 - 100 nm (mesh size) | 1 - 20 µm | 50 - 200 µm (native structure) | 100 - 500 µm (designed porosity) |
| Degradation Time (in vitro) | Days to months (engineered) | Days to weeks (enzymatic) | Months (slow, remodeling-dependent) | Days to weeks (bioink-dependent) |
Table 2: The Scientist's Toolkit: Essential Reagents for Scaffold-Based Immune Research
| Research Reagent / Material | Primary Function & Rationale |
|---|---|
| Methacrylated Hyaluronic Acid (HA-MA) | Photo-crosslinkable polymer for creating tunable stiffness hydrogels to study mechano-immunology. |
| Type I Collagen, Rat Tail | Gold-standard natural hydrogel for dermal equivalent formation; supports fibroblast contraction and immune cell infiltration. |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Cytocompatible photoinitiator for visible/UV light crosslinking of bioinks with high cell viability. |
| Recombinant Human Cytokines (e.g., GM-CSF, IL-4, IFN-γ) | To differentiate and polarize immune cells (e.g., monocytes to dendritic cells or macrophages) within scaffolds. |
| Fluorescently-conjugated Anti-human CD markers (CD45, CD3, CD11c, CD68) | For immune cell identification, tracking, and phenotypic analysis via flow cytometry or confocal microscopy in 3D constructs. |
| Matrigel or Similar Basement Membrane Extract | Used to create a keratinocyte-friendly epidermal-dermal junction, influencing Langerhans cell localization. |
| AlamarBlue or CellTiter-Glo 3D | Metabolic and viability assays optimized for 3D scaffold cultures to assess immune cell activity. |
| Transwell or Air-Liquid Interface Inserts | Critical for the maturation of stratified epidermal layers and studying immune cell transmigration. |
The strategic selection of scaffold—whether a tunable hydrogel, a biologically complex dECM, or a spatially precise bioprinted structure—directly dictates the fidelity of the immunological functions that can be modeled in a 3D skin construct. Integrating insights from all three modalities offers the most powerful approach: using dECM as a bioactive base, reinforcing it with printable hydrogel networks, and precisely positioning immune cells via bioprinting to create next-generation models for immunotherapy testing and inflammatory disease modeling.
The development of complex 3D skin constructs that accurately recapitulate immunological functions represents a pivotal advancement in dermatological research, toxicology, and immunomodulatory drug development. The core challenge lies in the precise temporal integration and spatial organization of immune cells within the multi-layered epidermal and dermal architecture. This guide details current methodologies for establishing these critical immune-stromal interactions, moving beyond static models to dynamic systems capable of mimicking innate and adaptive immune responses.
Core Principles of Immune Cell Incorporation
Successful co-culture hinges on two interdependent variables: timeline (the sequence and duration of cell seeding) and spatial arrangement (the physical location of cells within the 3D matrix). The chosen strategy must reflect the physiological recruitment or resident status of the target immune population.
Quantitative Comparison of Co-culture Strategies
The following tables summarize key quantitative data from recent studies on integrating various immune cells into 3D skin constructs.
Table 1: Co-culture Timeline Strategies for Key Immune Cells
| Immune Cell Type | Optimal Seeding Point | Co-culture Duration (Days) | Key Outcome Metrics | Reference Model |
|---|---|---|---|---|
| Primary Human Macrophages | Day 7 (post-fibroblast/keratinocyte seeding) | 7-14 | M1/M2 polarization ratio; Cytokine (IL-1β, TNF-α, IL-10) secretion; Phagocytic activity | Full-thickness model with collagen scaffold |
| Monocyte-derived Dendritic Cells (moDCs) | Day 14 (at air-liquid interface) | 3-7 | Migration rate (% cells to supernatant); Surface markers (CD83, CD86, HLA-DR); T-cell activation capacity | Reconstructed human epidermis (RHE) |
| T Lymphocytes (CD4+/CD8+) | Day 21 (fully stratified epidermis) | 3-5 | Proliferation index; IFN-γ/IL-17 production; Cytotoxic granule release (for CD8+) | Skin-on-a-chip with endothelial barrier |
| Neutrophils (HL-60 differentiated) | Day of challenge (e.g., pathogen, allergen) | 1-2 | NETosis quantification; Myeloperoxidase activity; Transepithelial migration | Wounded 3D epidermis |
| Tissue-Resident Memory T Cells (TRM) | Integrated during fibroblast contraction phase (Day 3-5) | 28+ | Long-term persistence (flow cytometry); Tissue-retention marker expression (CD69, CD103) | De-epidermized dermis (DED) model |
Table 2: Spatial Arrangement Methods & Quantitative Outcomes
| Spatial Method | Technical Description | Immune Cell Type | Resultant Cell Density (cells/mm²) | Functional Advantage |
|---|---|---|---|---|
| Topical Application | Suspension added to stratum corneum surface. | moDCs, Neutrophils | 100-500 | Mimics epicutaneous challenge; easy access for sampling. |
| Intra-epidermal Injection | Micro-injection into specific epidermal layers post-maturation. | TRM | 200-800 | Precise localization; models intra-epithelial lymphocytic infiltrates. |
| Dermal Encapsulation | Immune cells pre-mixed with collagen/ fibrin hydrogel. | Macrophages, Mast cells | 1000-3000 | Models dermal immune stroma; supports long-term viability. |
| Perfusable Vascular Channel | Seeding into engineered endothelial-lined channels. | Monocytes, Neutrophils | Variable by flow | Studies extravasation, rolling, and adhesion in real-time. |
| Stratified Co-culture | Sequential seeding to create distinct immune cell layers. | Langerhans cells (epidermal) + Dermal DCs (dermal) | Epidermal: 50-200Dermal: 400-1000 | Recapitulates anatomically distinct antigen-presenting cell networks. |
Detailed Experimental Protocols
Protocol 4.1: Integrated Macrophage-Dermal Construct for Chronic Inflammation Modeling
Objective: To establish a long-term co-culture of primary human macrophages within a fibroblast-populated dermal matrix.
- Dermal Construct Fabrication: Mix primary human dermal fibroblasts (2 x 10⁵ cells/mL) with acid-soluble rat tail collagen I (3 mg/mL) in neutralization buffer. Plate 1.5 mL/well in a 12-well insert. Allow contraction for 5 days in fibroblast medium.
- Macrophage Differentiation: Isolate CD14+ monocytes from PBMCs using magnetic separation. Differentiate into M0 macrophages with 50 ng/mL M-CSF for 6 days in low-attachment plates.
- Integration: On Day 7, harvest M0 macrophages, resuspend in a minimal volume of collagen I (1 mg/mL). Gently pipette 100 µL of the macrophage-collagen suspension onto the contracted dermal construct in 3-5 discrete "dermal papilla" locations.
- Culture & Polarization: After 24h, add complete medium. For M1 polarization, add 20 ng/mL IFN-γ and 100 ng/mL LPS for 48h. For M2, use 20 ng/mL IL-4 for 48h.
- Analysis: Fix and section for IHC (CD68, iNOS, CD206). Collect conditioned medium for multiplex cytokine assay.
Protocol 4.2: Dynamic T Cell Recruitment in a Skin-on-a-Chip Platform
Objective: To model T cell extravasation and migration toward an inflamed epidermal compartment.
- Device Preparation: Use a tri-channel microfluidic device with a porous membrane separating the top (dermal) and middle (epidermal) channels. Coat all channels with fibronectin.
- Dermal Layer Formation: Seed human dermal microvascular endothelial cells (HDMECs) into the bottom channel at 5 x 10⁶ cells/mL. Perfuse with EGM-2MV medium until a confluent monolayer forms (2-3 days).
- Epidermal Layer Formation: Seed primary human keratinocytes (3 x 10⁶ cells/mL) into the top channel on the opposite side of the membrane. Raise to air-liquid interface (ALI) on Day 3 for stratification (7 days).
- Inflammatory Priming: At ALI Day 7, add 10 ng/mL TNF-α and 10 ng/mL IL-1β to the top channel medium for 24h to mimic epidermal inflammation.
- T Cell Perfusion: Label isolated human CD3+ T cells with CellTracker Green. Resuspend at 1 x 10⁶ cells/mL in perfusion medium and introduce into the vascular (bottom) channel at a flow rate of 0.1 µL/min.
- Real-Time Analysis: Image via time-lapse confocal microscopy over 24h. Quantify adherent cells (per mm² of endothelium) and transmigrated cells (in top chamber) using image analysis software (e.g., ImageJ).
Visualizations
Immune Cell Integration Timeline in 3D Skin Model
T Cell Recruitment Signaling Pathway
Macrophage Integration & Polarization Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent / Material | Supplier Examples | Key Function in Immune-Skin Co-culture |
|---|---|---|
| Type I Collagen, High Concentration | Corning, Advanced BioMatrix, Merck | Provides the primary dermal scaffold for fibroblast and immune cell encapsulation and contraction. |
| Defined Immune Cell Media (Xeno-free) | Gibco, PromoCell, STEMCELL Tech. | Supports specific immune cell viability and function without inducing non-physiological differentiation. |
| Air-Liquid Interface (ALI) Inserts | Corning Transwell, Greiner, Millipore | Enables proper epidermal stratification and topical access for immune cell application or sampling. |
| Human Cytokine/Chemokine Multiplex Assay | Bio-Rad, R&D Systems, Thermo Fisher | Quantifies complex secretory profiles from co-cultures to assess inflammatory status. |
| Cell Tracking Dyes (e.g., CFSE, CellTracker) | Thermo Fisher, BioLegend | Enables visualization and quantification of immune cell migration and proliferation within constructs. |
| Microfluidic Skin-on-a-Chip Devices | Emulate, MIMETAS, in-house fabrication | Provides dynamic, vascularized models for studying immune cell trafficking under flow. |
| De-epidermized Dermis (DED) | Ready-made from tissue banks, or in-house prep. | Biologically derived scaffold retaining native basement membrane for highly authentic cell-matrix interactions. |
| Functional Blocking Antibodies (anti-ICAM-1, anti-CCL2) | BioLegend, R&D Systems | Tools to interrogate specific adhesive or chemotactic pathways in recruitment experiments. |
This whitepaper details the application of advanced 3D skin constructs that incorporate key immunological components (e.g., resident immune cells, cytokine gradients) for modeling complex dermatological and immunological endpoints. This work is situated within a broader thesis arguing that the next generation of in vitro models must transcend passive barrier function to actively recapitulate the dynamic crosstalk between epithelial and immune cells. Such immunocompetent 3D skin constructs are pivotal for mechanistic disease research, safety assessment, and the development of targeted biologics and immunomodulators.
Disease Modeling Applications
Psoriasis (PsO) Model
Psoriasis is a chronic autoimmune disease characterized by keratinocyte hyperproliferation, aberrant differentiation, and a pronounced Th1/Th17 inflammatory milieu.
Key Experimental Protocol: Psoriasis-like Inflammation Induction
- Construct Preparation: Use a full-thickness 3D skin model incorporating dermal fibroblasts and epidermal keratinocytes. Co-culture with CD4+ T cells (naive or pre-polarized) and CD11c+ dendritic cells in the dermal compartment is optimal.
- Cytokine Cocktail: To induce a psoriatic phenotype, supplement the medium in the basal compartment for 6-9 days with a cocktail of:
- IL-17A (50 ng/mL)
- IL-22 (50 ng/mL)
- TNF-α (25 ng/mL)
- IL-1α (10 ng/mL)
- Validation Endpoints:
- Histology: H&E staining for acanthosis (epidermal thickening), loss of granular layer, and parakeratosis.
- Immunohistochemistry: Staining for Keratin 16 (K16, hyperproliferation marker), Ki67, and antimicrobial peptides (LL-37, β-defensin).
- Cytokine Analysis: ELISA/MSD for IL-17, IL-23, IL-8, and TNF-α in supernatant.
- Gene Expression: qPCR for DEFB4, S100A7, IL17C, KRT16.
Atopic Dermatitis (AD) Model
AD is a Th2-skewed inflammatory disease driven by barrier dysfunction, pruritus, and allergic sensitization.
Key Experimental Protocol: AD-like Condition Induction
- Construct Preparation: Utilize a 3D model with a filaggrin-deficient keratinocyte genotype or chemically impair barrier function (e.g., mild SDS treatment).
- Th2 Cytokine Polarization: Expose the model to a Th2 cytokine milieu for 5-7 days:
- IL-4 (25 ng/mL)
- IL-13 (25 ng/mL)
- IL-31 (50 ng/mL) to induce pruritic signaling.
- Optional Allergen Challenge: For a late-phase AD model, topically apply house dust mite extract (Dermatophagoides pteronyssinus) or ovalbumin.
- Validation Endpoints:
- Barrier Function: Measure Transepithelial Electrical Resistance (TEER) or permeability to tracer molecules (e.g., FITC-dextran).
- Histology: Spongiosis (intercellular edema).
- Biomarkers: IHC for filaggrin, loricrin; ELISA for TSLP, IL-4, IL-13, IL-31, CCL26 (eotaxin-3).
- Gene Expression: qPCR for FLG, LOR, TSLP, CCL17, CCL22.
Allergy (Skin Sensitization) Testing
This application assesses the potential of chemicals to cause allergic contact dermatitis (ACD), a key regulatory endpoint (OECD TG 442D/E).
Key Experimental Protocol: Direct Peptide Reactivity Assay (DPRA) & ARE-Nrf2 Luciferase LuSENS Test This protocol describes the integration of key mechanistic events into a 3D construct.
- Molecular Initiating Event (Covalent Binding):
- Incubate test chemical with a synthetic peptide containing lysine or cysteine.
- Analyze via HPLC to quantify peptide depletion (% depletion > threshold indicates sensitizer).
- Keratinocyte Activation in a 3D Model:
- Topically apply the test chemical (non-cytotoxic concentrations) to a reconstructed human epidermis (RHE) model.
- Culture for 24-48 hours.
- Key Event Analysis:
- Gene Expression: Extract RNA for qPCR analysis of the Nrf2-antioxidant response element (ARE) pathway genes (HMOX1, NQO1, GCLM).
- IL-18 Release: Measure IL-18 in culture supernatant by ELISA—a critical cytokine for dendritic cell activation and Th1 polarization.
- Cell Viability: MTT assay to ensure results are not due to general cytotoxicity.
Immunotoxicity Testing
This assesses unintended immunosuppression or hyperactivation of skin immune responses by pharmaceuticals or chemicals.
Key Experimental Protocol: Modality-Specific Immunotoxicity Screening
- Construct: Use an immunocompetent 3D skin model containing keratinocytes, fibroblasts, and integrated monocyte-derived dendritic cells (moDCs) and CD4+ T cells.
- Challenge & Compound Exposure:
- Pre-treat the model with the test compound (e.g., a new topical drug) for 24 hours.
- Challenge the model with a toll-like receptor agonist (e.g., Poly I:C for viral mimicry or LPS for bacterial challenge) or a known sensitizer.
- Endpoint Multiplexing:
- Dendritic Cell Activation: Flow cytometry of recovered moDCs for surface markers CD86, CD83, HLA-DR.
- Cytokine Storm Risk: Luminex/ MSD multi-cytokine panel for pro-inflammatory cytokines (IL-1β, IL-6, TNF-α, IFN-γ).
- Lymphocyte Proliferation: CFSE dilution assay on recovered T cells.
- Tissue Viability: MTT or ATP-based assay.
Summarized Quantitative Data
Table 1: Key Cytokine Profiles in Disease-Mimicking 3D Skin Constructs
| Disease Model | Key Inducing Agents | Characteristic Upregulated Biomarkers (Fold Change vs. Control) | Typical Assay |
|---|---|---|---|
| Psoriasis | IL-17A, IL-22, TNF-α, IL-1α | IL-8 (>10x), hBD-2 (>50x), KRT16 (>20x), S100A7 (>100x) | qPCR, ELISA, IHC |
| Atopic Dermatitis | IL-4, IL-13, IL-31 | TSLP (>15x), CCL26 (>20x), IL-13 (>8x), FLG (↓ >70%) | qPCR, ELISA |
| Allergy (Sensitizer) | Contact allergen (e.g., DNCB) | IL-18 (>5x), HMOX1 (>3x), CD86 on DCs (>2x) | ELISA, qPCR, Flow Cyt. |
| Immunosuppression | Drug + TLR Agonist | CD86 on DCs (↓ >40%), IL-6 secretion (↓ >60%) | Flow Cyt., ELISA |
Table 2: Comparison of 3D Skin Model Types for Immunological Applications
| Model Type | Immune Components | Key Applications | Throughput | Complexity |
|---|---|---|---|---|
| Reconstructed Epidermis (RHE) | Keratinocytes only | Barrier integrity, direct cytotoxicity, basic sensitization (KE3) | High | Low |
| Full-Thickness Model | Keratinocytes + Fibroblasts | Psoriasis/AD morphology, cytokine-mediated studies | Medium | Medium |
| Immunocompetent Co-culture | Keratinocytes + Fibroblasts + Immune Cells (DCs, T cells) | Full ACD pathway, immunomodulation, mechanistic toxicity | Low | High |
Signaling Pathways and Workflows
Diagram 1: Core Psoriasis Inflammatory Loop
Diagram 2: Atopic Dermatitis Pathogenesis Cycle
Diagram 3: Generic Experimental Workflow for 3D Skin Testing
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Immunocompetent 3D Skin Research
| Item / Reagent Solution | Function & Application | Example Vendor/Product |
|---|---|---|
| Normal Human Epidermal Keratinocytes (NHEK) & Fibroblasts (NHDF) | Primary cells for constructing the epidermal and dermal layers. Critical for donor-specific studies. | Lonza, Thermo Fisher, CELLnTEC |
| CD14+ Monocytes / Peripheral Blood Mononuclear Cells (PBMCs) | Source for deriving dendritic cells (moDCs) and other immune cells for co-culture integration. | STEMCELL Technologies, Miltenyi Biotec |
| Cytokine Milieu Cocktails | For disease phenotype induction (e.g., PsO: IL-17A, IL-22, TNF-α; AD: IL-4, IL-13). | PeproTech, R&D Systems |
| Reconstructed Human Epidermis (RHE) or Full-Thickness Kits | Pre-fabricated 3D skin models for higher-throughput screening (e.g., EpiDerm, SkinEthic). | MatTek, Episkin |
| IL-18 ELISA Kit | Quantification of this key cytokine for skin sensitization potency assessment (Key Event 3). | MBL, Invitrogen |
| Multi-plex Cytokine Assay Panels | Simultaneous measurement of dozens of pro/anti-inflammatory cytokines from limited supernatant. | Meso Scale Discovery (MSD), Bio-Rad |
| Cell Recovery Solution (for non-trypsin) | Gentle enzymatic dissociation to extract viable immune cells from the 3D matrix for flow cytometry. | Corning, BD Biosciences |
| Nrf2/ARE Reporter Cell Line | Used in LuSENS-type assays to measure the antioxidant response element activation (Key Event 2). | ATCC, commercial LuSENS assay |
| Filaggrin (FLG) siRNA / CRISPR Kit | To genetically engineer barrier-defective keratinocytes for robust AD modeling. | Horizon Discovery, Sigma-Aldrich |
| Low-Melting Point Agarose/ Collagen Matrix | For creating the dermal equivalent scaffold that supports fibroblast and immune cell embedding. | Corning, Advanced BioMatrix |
This case study is presented within the context of a broader thesis investigating the development and application of immunocompetent 3D skin constructs that recapitulate the native tissue's architecture, cellular heterogeneity, and, crucially, its immunological functions. The central premise is that such advanced in vitro models are indispensable for dissecting complex immune-mediated adverse events (irAEs), such as checkpoint inhibitor-induced dermatitis (CIPD). By mimicking the crosstalk between keratinocytes, resident immune cells (e.g., Langerhans cells, memory T cells), and infiltrating lymphocytes, these constructs provide a human-relevant, ethical, and mechanistically transparent platform for preclinical toxicology and therapeutic discovery.
Pathogenesis & Rationale forIn VitroModeling
Immune checkpoint inhibitors (ICIs), such as anti-PD-1 and anti-CTLA-4 antibodies, disrupt co-inhibitory signaling in T cells, unleashing anti-tumor immunity. However, this systemic immune activation frequently targets the skin, leading to maculopapular rash or lichenoid dermatitis, which are among the most common irAEs. The hypothesized pathogenesis involves:
- Loss of peripheral tolerance in skin-resident memory T cells.
- Enhanced activation and cytokine secretion by T cells upon encountering cutaneous antigens.
- Cytokine-mediated keratinocyte damage (e.g., IFN-γ, TNF-α) and subsequent inflammatory amplification.
Traditional 2D co-cultures fail to capture the 3D tissue microenvironment and spatially organized immune-stromal interactions. Therefore, modeling CIPD requires constructs that incorporate immune cells within a stratified, physiologically relevant epidermal and/or full-thickness skin model.
Table 1: Key Cytokine Profiles in CIPD from Clinical & Preclinical Studies
| Cytokine/Chemokine | Role in Pathogenesis | Reported Fold-Change in CIPD (vs. Control) | Detection Method (Example) |
|---|---|---|---|
| IFN-γ | Th1 polarization, keratinocyte apoptosis, MHC-II upregulation | 5x - 15x increase | ELISA / Luminex |
| TNF-α | Pro-inflammatory, induces keratinocyte cell death | 3x - 10x increase | ELISA / Luminex |
| Granzyme B | Cytotoxic T-cell and NK cell marker | 8x - 20x increase | Immunoassay / IHC |
| IL-6 | Pro-inflammatory, acute phase response | 4x - 12x increase | ELISA / Luminex |
| CXCL10 | Chemoattractant for T cells and monocytes | 10x - 25x increase | ELISA / Luminex |
| IL-17A | Associated with psoriasiform reactions (subset of cases) | 2x - 8x increase | ELISA / Luminex |
Table 2: Comparison of 3D Skin Model Platforms for CIPD Research
| Model Type | Key Components | Advantages for CIPD Modeling | Limitations |
|---|---|---|---|
| Reconstructed Human Epidermis (RHE) with embedded immune cells | NHEK, CD8+ T cells, Langerhans cell precursors | Focus on epidermal events; good for high-throughput compound screening | Lacks dermal compartment and vascular components. |
| Full-Thickness Skin Equivalents (FTSE) | NHEK, NHDF in collagen matrix, immune cells | Includes dermal-epidermal crosstalk; better model for lichenoid infiltrates. | More complex, variable, lower throughput. |
| Organ-on-a-Chip (Skin Chip) | Epidermal and dermal layers, microfluidic perfusion | Dynamic flow allows immune cell recruitment; can integrate endothelial cells. | Technically demanding, not yet standardized. |
| Bioprinted Constructs | Keratinocytes, fibroblasts, immune cells in bioink | High spatial control over cell placement; potential for vascularization. | Early-stage technology; cost-intensive. |
Detailed Experimental Protocol: ICI Challenge in an Immunocompetent FTSE
Objective: To induce and characterize a CIPD-like phenotype in a full-thickness skin equivalent containing autologous T cells and dendritic cells.
Part A: Generation of the Immunocompetent FTSE
Cell Isolation:
- Isolate normal human dermal fibroblasts (NHDFs) from de-identified tissue.
- Isolate peripheral blood mononuclear cells (PBMCs) from the same donor via density gradient centrifugation.
- Isolate CD14+ monocytes (for dendritic cell differentiation) and CD3+ T cells from PBMCs using magnetic-activated cell sorting (MACS).
Immune Cell Priming (Pre-assembly):
- Differentiate monocytes into immature dendritic cells (iDCs) using IL-4 (50 ng/mL) and GM-CSF (100 ng/mL) in RPMI-1640 for 6 days.
- Maintain autologous CD3+ T cells in TexMACS medium with low-dose IL-2 (50 IU/mL).
Dermal Equivalent Formation:
- Mix NHDFs (2 x 10^5 cells/mL) with neutralized rat tail collagen I (3 mg/mL) in DMEM.
- Pipette 1.5 mL of the collagen-fibroblast mix into a cell culture insert (e.g., 24-well format). Allow to polymerize (37°C, 1 hr).
- Add iDCs (5 x 10^4 cells/insert) to the surface of the polymerized dermal layer.
Epidermal Seeding and Stratification:
- Seed normal human epidermal keratinocytes (NHEKs, 5 x 10^5 cells/insert) on top of the dermal layer.
- Culture submerged for 48 hours in keratinocyte growth medium.
- Raise the construct to the air-liquid interface (ALI). Culture for 10-14 days with appropriate medium changes to promote full epidermal stratification.
- On day 7 at ALI, add primed autologous CD3+ T cells (1 x 10^5 cells/insert) onto the stratum corneum; they will migrate into the construct.
Part B: Checkpoint Inhibitor Challenge
Treatment Groups:
- Control: Culture medium only.
- ICI Monotherapy: Add anti-PD-1 antibody (e.g., Nivolumab biosimilar, 10 µg/mL) to the culture medium.
- ICI + Stimulation: Add anti-PD-1 antibody (10 µg/mL) and a low-level T cell stimulant (e.g., anti-CD3 at 0.5 µg/mL, mimicking weak antigenic trigger) to the medium.
- Stimulant Control: Anti-CD3 only (0.5 µg/mL).
Exposure: Treat constructs for 96 hours, refreshing medium and compounds every 48 hours.
Part C: Endpoint Analysis
Histology & Immunohistochemistry:
- Fix constructs in 4% PFA, paraffin-embed, section.
- Stain with H&E to assess epidermal morphology, spongiosis, and lymphocytic infiltration.
- Perform IHC for CD3 (T cells), CD8 (cytotoxic T cells), Granzyme B, and Ki-67 (proliferation).
Cytokine Profiling:
- Collect conditioned media at 48h and 96h.
- Analyze using a multiplex Luminex panel for IFN-γ, TNF-α, IL-6, IL-1β, IL-17A, and CXCL10.
Gene Expression:
- Isolate RNA from separated epidermal and dermal layers.
- Perform qRT-PCR for inflammatory markers (CXCL10, ICAM1, HLA-DRα), apoptosis markers (CASP3), and keratinocyte differentiation genes (FLG, LOR).
Signaling Pathways & Experimental Workflow
Title: CIPD Pathogenesis and In Vitro Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Immunocompetent Skin Model Research
| Reagent / Material | Supplier Examples | Function in CIPD Modeling |
|---|---|---|
| Normal Human Epidermal Keratinocytes (NHEKs) | Lonza, Thermo Fisher, CELLnTEC | Primary epidermal cells for forming the stratified, differentiated barrier. |
| Normal Human Dermal Fibroblasts (NHDFs) | Lonza, ATCC, PromoCell | Primary cells for constructing the dermal collagen matrix. |
| Collagen I, High Concentration (Rat Tail or Bovine) | Corning, Advanced BioMatrix | The major structural protein for forming the 3D dermal scaffold. |
| CD3+ T Cell Isolation Kit (Human) | Miltenyi Biotec, STEMCELL Tech | Isolation of untouched, viable T cells from PBMCs for model incorporation. |
| Recombinant Human IL-4 & GM-CSF | PeproTech, R&D Systems | Cytokines for differentiating monocytes into immature dendritic cells (iDCs). |
| Anti-human PD-1 (Nivolumab) Antibody, BioXCell | Bio X Cell, InvivoGen | The checkpoint inhibitor used to induce the immune-dysregulation phenotype. |
| Air-Liquid Interface Culture Inserts | Corning, Merck Millipore | Permeable supports enabling epidermal stratification at the air interface. |
| Multiplex Cytokine Assay (Human) | R&D Systems, Thermo Fisher | Simultaneous quantification of key inflammatory mediators from conditioned media. |
| Skin Dissociation Kit (for RNA) | Miltenyi Biotec | Gentle enzymatic separation of epidermal and dermal layers for spatial analysis. |
Navigating Complexity: Challenges and Solutions in Immune-Skin Model Development
The development of immunocompetent 3D skin constructs represents a transformative advance for modeling inflammatory skin diseases, testing immunotoxicity, and evaluating immunomodulatory therapeutics. A central thesis in this field posits that the predictive validity of these complex in vitro systems is inherently linked to the sustained, functional presence of key immune populations—such as macrophages, dendritic cells, and T cells—within the epidermal and dermal compartments over physiologically relevant timeframes. The common and critical pitfall undermining this thesis is the rapid loss of immune cell viability, coupled with phenotypic and functional drift, under conventional culture conditions. This guide details the technical challenges and presents evidence-based solutions for long-term immune cell maintenance within 3D skin models.
Core Challenges and Quantitative Data
The primary factors leading to immune cell attrition and dysregulation in 3D skin co-cultures are summarized in the table below, with supporting quantitative data from recent studies.
Table 1: Primary Factors in Immune Cell Attrition & Phenotype Loss in 3D Skin Constructs
| Factor | Impact on Immune Cells | Typical Timeframe of Significant Effect | Key Supporting Metrics (Representative Values) |
|---|---|---|---|
| Inadequate Cytokine/Growth Factor Support | Loss of lineage-specific markers (e.g., CD14, CD11c, CD3), reduced phagocytic/antigen-presenting capacity, apoptosis. | 3-7 days | >80% loss of CD14+ macrophages by day 7 without M-CSF/IL-4 (vs. <20% loss with). [Recent data, 2023] |
| Hypoxia & Metabolic Stress | Shift to pro-inflammatory, hyperactive state (M1-like) followed by necrosis; T cell exhaustion. | 24-72 hours | O2 concentration <2% in construct core leads to 60% reduced viability vs. periphery by day 5. [Recent data, 2024] |
| Lack of Physiologic Soluble Mediator Crosstalk | Dysregulated activation, failure to recapitulate resolution phases of inflammation. | Ongoing | Co-culture with fibroblasts increases monocyte-derived Langerhans cell survival from 40% to 75% at day 10 via GM-CSF secretion. [Recent data, 2023] |
| Mechanical Stress from Stiff Scaffolds | Altered integrin signaling, forced proliferation or anoikis. | 1-14 days | Macrophages on high-stiffness (>50 kPa) hydrogels show 3-fold increase in IL-1β secretion vs. physiologic stiffness (~2-10 kPa). [Recent data, 2024] |
Detailed Experimental Protocols for Long-Term Maintenance
Protocol: Establishing a Long-Term Monocyte-Derived Macrophage (MDM) Population in a Full-Thickness Skin Model
Objective: To incorporate and maintain functional, M2-polarizable macrophages within the dermal compartment of a 3D skin construct for 21 days.
Materials & Reagents:
- Primary human monocytes (CD14+ isolated from PBMCs).
- Fibroblast-populated collagen type I hydrogel (dermal equivalent).
- Normal Human Epidermal Keratinocytes (NHEKs).
- Specialized Macrophage Maintenance Medium (see Section 5 Toolkit).
Methodology:
- Dermal Construct Seeding: Generate a collagen I/fibronectin hydrogel (2 mg/ml collagen, physiological stiffness) containing 2 x 10^5 human dermal fibroblasts/ml. Allow contraction for 48 hours.
- Macrophage Precursor Incorporation: Differentiate isolated CD14+ monocytes into macrophages in situ by seeding 1 x 10^5 cells/construct on top of the contracted dermis in RPMI-1640 supplemented with 50 ng/ml recombinant human M-CSF. Culture for 6 days, with medium changes every 48 hours.
- Epidermal Overlay & Air-Lift: Seed NHEKs onto the macrophage-containing dermis. Culture submerged for 48 hours, then air-lift to stratify the epidermis. At air-lift, switch to a Dual-Cytokine Maintenance Medium: a 1:1 mix of keratinocyte-defined medium and Advanced RPMI, further supplemented with 25 ng/ml M-CSF and 10 ng/ml IL-4 to sustain macrophage viability and promote an M2-polarizable state.
- Long-Term Culture & Analysis: Culture the complete construct for up to 21 days. Change the Dual-Cytokine Maintenance Medium every 2-3 days. Assess macrophage viability and phenotype weekly via:
- Flow Cytometry: Harvest dermal compartment via collagenase digestion. Stain for viability, CD11b, CD14, CD68, CD163, CD206, and HLA-DR.
- Functional Assay (Phagocytosis): Incubate live construct sections with pHrodo E. coli Bioparticles for 2 hours, image via confocal microscopy.
- Cytokine Secretion: Multiplex ELISA of conditioned medium for IL-10, TNF-α, CCL18.
Visualizing Key Signaling Pathways & Workflows
Title: Cytokine Signaling for Macrophage Maintenance
Title: 21-Day 3D Skin Immune Co-Culture Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for Long-Term Immune Cell Maintenance
| Reagent / Material | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Recombinant Human M-CSF (rhM-CSF) | Primary survival and differentiation factor for macrophages. Essential for preventing apoptosis in long-term co-culture. | PeproTech, 300-25; BioLegend, 574806 |
| Recombinant Human IL-4 (rhIL-4) | Promotes alternative (M2) activation and phenotype stability. Used in combination with M-CSF for homeostasis. | R&D Systems, 204-IL-010 |
| Physiologic-Stiffness Hydrogels | Collagen I or hyaluronic acid matrices tuned to ~2-10 kPa elastic modulus to prevent mechano-inflammatory signaling. | Corning Collagen I, rat tail; Advanced BioMatrix, HyStem kits |
| Specialized Co-Culture Media | Chemically defined, cytokine-supplemented media designed to support both stromal/epithelial and immune lineages. | Gibco Immune Cell Serum-Free Media; STEMCELL Technologies, M-CSF Macrophage Media |
| Hypoxia-Mimetic or Gas-Permeable Cultureware | Maintains physiologic O2 tension (2-5%) throughout the 3D construct to prevent necrotic core formation. | Gas-permeable plates (e.g., ZellSafe); Hypoxia chambers (e.g., STEMCELL, HypoxyLab) |
| pHrodo Bioparticles (E. coli or Zymosan) | Fluorescent, pH-sensitive probes for quantitative measurement of phagocytic function within live constructs. | Thermo Fisher Scientific, P35361 |
| Pan-Macrophage & Polarization Antibody Panel | For flow cytometry: CD68 (pan), CD163 (M2), CD80/86 (M1), HLA-DR (activation). | BioLegend, Fluidigm mass cytometry panels |
The development of advanced in vitro 3D skin models that faithfully replicate immunological functions represents a frontier in dermatological research, toxicology, and drug development. A core challenge in constructing these living tissues is the precise recapitulation of the skin's native cellular architecture—specifically, the physiological cell ratios and spatial-chemical gradients that govern immune surveillance, barrier function, and inflammatory responses. This technical guide details the strategies and methodologies essential for achieving this balance, moving beyond mere 3D structure to dynamic, immunocompetent tissue.
Quantitative Landscape of Native Human Skin
Achieving physiological mimicry requires a foundational understanding of the quantitative cellular composition and gradient parameters of native human skin. The following tables consolidate current data from recent single-cell RNA sequencing and spatial profiling studies.
Table 1: Major Cellular Populations in Human Epidermis and Dermis
| Cell Type | Location | Approximate Percentage (%) | Key Immune Function |
|---|---|---|---|
| Keratinocytes | Epidermis (Stratum Basale to Corneum) | 85-90% (of epidermis) | Produce antimicrobial peptides (AMPs); cytokine signaling. |
| Melanocytes | Epidermis (Stratum Basale) | 5-10% (of basal layer) | UV protection; paracrine immunomodulation. |
| Langerhans Cells | Epidermis (Stratum Spinosum) | 2-5% (of epidermis) | Antigen presentation; immune sentinels. |
| Tissue-Resident Memory T Cells | Epidermis & Dermis | 1-2% (of total skin) | Rapid recall response to pathogens. |
| Fibroblasts | Dermis (Papillary & Reticular) | 60-70% (of dermis) | Extracellular matrix (ECM) production; cytokine milieu. |
| Dermal Dendritic Cells | Dermis | 5-10% (of dermal leukocytes) | Antigen capture and presentation to T cells. |
| Macrophages | Dermis | 10-15% (of dermal leukocytes) | Phagocytosis; pro/anti-inflammatory signaling. |
| Endothelial Cells | Dermis (Vasculature) | 5-10% (of dermis) | Leukocyte recruitment; gradient formation. |
| Mast Cells | Dermal perivascular zone | 1-3% | IgE-mediated hypersensitivity; cytokine release. |
Table 2: Critical Biochemical Gradients in Skin
| Gradient Type | Source -> Sink | Approximate Range | Physiological Role |
|---|---|---|---|
| Calcium (Ca²⁺) | Stratum Granulosum -> Basale | Low (0.05 mM) to High (1.4 mM) | Drives keratinocyte differentiation and barrier formation. |
| Oxygen (pO₂) | Dermal vasculature -> Stratum Corneum | ~70 mmHg -> <10 mmHg | Influences metabolism, HIF-1α signaling, wound healing. |
| Chemokine (e.g., CCL27) | Keratinocytes -> Dermal Vasculature | Concentration declines with depth | T-cell homing to the skin. |
| Vitamin D3 | Stratum Corneum (upon UV) -> Vasculature | Synthesized locally | Modulates immune cell function (Treg activation). |
| pH | Stratum Corneum -> Viable Epidermis | 4.5-5.5 -> ~7.4 | Antimicrobial barrier; enzyme activity regulation. |
Core Methodologies for Establishing Ratios and Gradients
Protocol: Sequential Cell Seeding for Stratified Ratios
Objective: To construct a bilayer skin model with physiologically accurate epidermal:dermal and immune cell ratios.
Materials:
- Collagen Type I hydrogel (rat tail, high concentration)
- Primary human dermal fibroblasts (HDFs)
- Primary human keratinocytes (HEKs)
- CD34+ hematopoietic stem cell-derived Langerhans Cell (LC) precursors
- Monocyte-derived dermal dendritic cells (mo-DDCs)
- Defined media: Fibroblast Growth Medium (FGM), Keratinocyte Growth Medium (KGM), Immunocyte Maturation Medium.
Procedure:
- Dermal Construct Formation: Mix HDFs at a density of 1-2 x 10⁵ cells/mL within a neutralized collagen I solution. Polymerize in a transwell insert (37°C, 30 min) to create a contracted gel (≈1-2 mm thick). Culture in FGM for 5-7 days.
- Immune Cell Incorporation: On day 3 of dermal culture, gently inject a suspension containing mo-DDCs (at 2-5% of the HDF number) into the lower dermal region using a micro-injector.
- Epidermal Seeding: Lift the dermal construct to air-liquid interface (ALI). Seed a mixed suspension of HEKs and LC precursors (at a ratio of 50:1 HEKs:LCs) on top at a high density (2-5 x 10⁵ cells/cm²). Submerge culture in KGM for 3 days to allow attachment.
- Stratification & Maturation: Raise to ALI. Culture for 10-14 days, feeding from below. LC precursors will migrate and differentiate within the forming epidermis.
Protocol: Generating a Calcium Gradient for Differentiation
Objective: To establish a vertical Ca²⁺ gradient driving spatially correct keratinocyte differentiation.
Materials:
- Established epidermal layer (day 3 post-ALI).
- Custom diffusion chamber or commercial transwell system.
- "High-Ca²⁺" Medium (1.2-1.4 mM Ca²⁺).
- "Low-Ca²⁺" Medium (0.05-0.1 mM Ca²⁺).
Procedure:
- Place the construct in a two-compartment chamber where the basal medium contacts only the dermal layer.
- Continuously perfuse the basal medium with Low-Ca²⁺ Medium.
- Apply a thin layer of High-Ca²⁺ Medium exclusively to the apical (top) surface for 1 hour daily.
- This creates a stable, time-averaged gradient from the stratum corneum (high Ca²⁺) to the stratum basale (low Ca²⁺), mimicking the in vivo environment and triggering sequential expression of keratin K10, involucrin, and filaggrin.
Protocol: Chemokine Gradient Formation via Microfluidic Integration
Objective: To model immune cell recruitment by establishing a stable chemokine gradient across the dermal compartment.
Materials:
- Perfusion bioreactor with integrated microfluidic channels.
- Pump system for precise flow control.
- Fluorescently tagged chemokine (e.g., CCL19-FITC).
- Primary human T cells or dendritic cells.
Procedure:
- Fabricate a 3D skin construct with a vascularized channel (using endothelial cells) embedded within the dermal layer.
- Integrate the construct into a microfluidic chip where one channel represents a "blood vessel."
- Perfuse the "vascular" channel with medium containing a defined concentration of chemokine (e.g., 100 ng/mL CCL19).
- The chemokine will diffuse into the surrounding dermal matrix, establishing a stable, quantifiable concentration gradient over 24-48 hours.
- Introduce fluorescently labeled immune cells into the "vascular" channel and track their migration speed and directionality up the gradient using time-lapse microscopy.
The Scientist's Toolkit: Key Reagent Solutions
Table 3: Essential Research Reagents for Skin Construct Immunology
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| Primary Human Keratinocytes & Fibroblasts | Foundation for epidermal and dermal layers. | Donor variability impacts immune response; use pooled donors or multiple lines for reproducibility. |
| CD34+ Hematopoietic Progenitor Cells | Source for generating Langerhans cells and other resident immune populations. | Allows for in situ differentiation within the construct for proper localization. |
| Recombinant Human Cytokines (IL-4, GM-CSF, TGF-β, CCL27) | Driving immune cell differentiation and establishing chemotactic gradients. | Batch-to-batch activity variation requires bioassay validation for gradient studies. |
| Decellularized Dermal Matrix (DDM) | Provides a native, complex ECM scaffold for improved cell migration and signaling. | Preserves critical ECM-bound cytokines and growth factors absent in pure collagen gels. |
| Oxygen-Sensitive Nanoparticles / Fluorescent Probes | Real-time, non-destructive mapping of oxygen gradients within 3D constructs. | Essential for validating hypoxic niches that drive specific immune functions (e.g., macrophage polarization). |
| Neutralizing Antibodies (anti-CCL17, anti-IL-1α) | Functional validation of specific gradient/pathway contributions. | Used to block signaling in control constructs to confirm mechanistic roles. |
Visualizing Key Signaling Pathways and Workflows
Title: Calcium Gradient Drives Keratinocyte Differentiation
Title: Langerhans Cell Maturation & Migration Pathway
Title: Workflow for Building an Immunocompetent Skin Model
Within the burgeoning field of engineering 3D skin constructs that mimic immunological functions, the selection of appropriate immunogenic triggers is a critical determinant of experimental validity and translational relevance. This guide provides a technical framework for researchers, scientists, and drug development professionals to choose and apply stimuli—such as cytokines, allergens, microbial products, and haptens—to elicit and study specific immune responses in reconstructed human skin equivalents. The goal is to bridge the gap between simplistic 2D cell culture and in vivo complexity, enabling predictive modeling of skin inflammation, sensitization, and tolerance.
Categories of Immunogenic Triggers and Their Applications
Immunogenic triggers are selected based on the target immunological pathway and the research question (e.g., modeling atopic dermatitis, allergic contact dermatitis, or psoriasis).
Table 1: Major Categories of Immunogenic Triggers for 3D Skin Constructs
| Category | Examples | Primary Target Cells/Receptors | Induced Immune Response | Typical Use Case in 3D Skin |
|---|---|---|---|---|
| Pro-inflammatory Cytokines | TNF-α, IL-1β, IL-6, IL-17A, IL-22 | Keratinocytes, Dermal Fibroblasts, Resident Immune Cells | Acute inflammation, Barrier disruption, Chemokine secretion | Psoriasis-like models, General inflammation studies |
| TH2 Cytokines & Alarmins | IL-4, IL-13, IL-25, IL-31, TSLP | Keratinocytes, Langerhans Cells, Type 2 Innate Lymphoid Cells | Atopic inflammation, IgE class switching, Pruritus, Barrier dysfunction | Atopic dermatitis (eczema) models |
| Allergens & Haptens | DNCB, DNFB, Nickel Sulfate, Fragrance Mix, Ovalbumin | Langerhans Cells, Keratinocytes (via haptenation), T-cells | Allergic contact dermatitis, Sensitization, Dendritic cell maturation | Predictive skin sensitization testing (OECD TG 497) |
| Microbial & Pathogen-Associated Molecular Patterns (PAMPs) | LPS (Gram-negative bacteria), Lipoteichoic Acid (Gram-positive), Poly(I:C) (viral dsRNA mimic) | TLR4 (LPS), TLR2 (LTA), TLR3 (Poly I:C) on Keratinocytes & DCs | Innate immune activation, Antimicrobial peptide production, Mixed inflammatory cytokine profile | Infection modeling, Innate immunity studies |
| Damage-Associated Molecular Patterns (DAMPs) | HMGB1, ATP, Uric Acid Crystals, Extracellular DNA | RAGE, P2X7, NLRP3 Inflammasome | Sterile inflammation, Pyroptosis, Necroinflammation | Irritant dermatitis, Wound healing models |
Quantitative Considerations: Dosage and Temporal Dynamics
Stimulus concentration and exposure time are paramount. Over-stimulation can cause necrotic cell death, masking specific immune signaling, while sub-optimal doses may fail to elicit a measurable response.
Table 2: Exemplary Quantitative Parameters for Common Triggers in 3D Skin Constructs
| Trigger | Typical Concentration Range | Exposure Duration (Acute) | Key Readout Metrics | Notes / References (Recent Studies) |
|---|---|---|---|---|
| TNF-α | 10–100 ng/mL | 24–72 hours | IL-8 secretion (pg/mL), NF-κB nuclear translocation, VCAM-1 expression | Often used in combination with IL-17 or IL-1β for psoriatic phenotype. |
| IL-4 + IL-13 | 10–50 ng/mL each | 48–120 hours | CCL26 (eotaxin-3) secretion, Filaggrin/Loricrin downregulation (qPCR), STAT6 phosphorylation | Core cytokines for establishing a TH2-skinned microenvironment. |
| DNCB (Sensitizer) | 5–50 µM (sensitization phase) | 24 hours (followed by 5-7 day maturation) | CD86/ CD54 expression on dendritic cells, IL-18 secretion, CCR7 upregulation | Key agent in in vitro skin sensitization tests like h-CLAT or U-SENS. |
| Poly(I:C) (HMW) | 1–25 µg/mL | 6–48 hours | IFN-β, CXCL10 secretion, MDA-5/RIG-I expression, Keratinocyte hyperproliferation | Mimics viral infection; dose-dependent induction of type I & III IFNs. |
| LPS (E. coli) | 100 ng/mL – 1 µg/mL | 6–24 hours | TNF-α, IL-1β, IL-6 secretion, TLR4 surface expression | High purity (<1% protein) recommended to avoid confounding TLR2 activation. |
Experimental Protocols for Key Applications
Protocol: Inducing a Psoriasis-Like Phenotype
Objective: To generate a hyperproliferative, pro-inflammatory state mimicking psoriatic skin. Materials: Full-thickness 3D skin construct (epidermis + dermis), culture media, recombinant human cytokines. Procedure:
- Pre-conditioning: Maintain constructs at air-liquid interface for minimum 7 days for barrier maturation.
- Stimulus Cocktail Preparation: Prepare fresh medium containing TNF-α (50 ng/mL), IL-17A (50 ng/mL), and IL-22 (25 ng/mL). IL-1β (10 ng/mL) can be added for a more severe phenotype.
- Application: Gently aspirate maintenance medium from the basal compartment. Add the cytokine cocktail medium to the basal compartment. Avoid direct apical flooding.
- Incubation: Incubate constructs for 48-72 hours, with a medium change at 24 hours.
- Harvest & Analysis:
- Histology: Fix in formalin, section, stain with H&E for acanthosis (epidermal thickening) and Munro's microabscesses.
- qPCR: Isolate RNA from epidermal layer. Assess DEFB4, S100A7, IL-36G, KRT16 expression.
- Cytokine Array: Collect conditioned medium, analyze for IL-8, CCL20, LL-37 via ELISA.
Protocol: Skin Sensitization Potency Assessment (OECD TG 497 Alignment)
Objective: To classify a chemical as a skin sensitizer and predict its potency (extreme, strong, moderate, weak). Materials: Reconstructed human epidermis (RhE) model (e.g., EpiDerm, SkinEthic), test chemical, positive controls (DNCB, NiSO4), MTT assay kit, ELISA for IL-18. Procedure:
- Dose-Finding (Cytotoxicity): Expose RhE to a range of chemical concentrations for 48h. Perform MTT assay. Determine the concentration that causes 20% cytotoxicity (CV75) and 50% cytotoxicity (CV50).
- Main Sensitization Exposure: Apply non-cytotoxic concentrations (especially CV75) of the test chemical, vehicle control, and positive control to the apical surface of duplicate RhE tissues for 48h.
- Biomarker Measurement:
- IL-18 Secretion: Collect culture medium at 48h. Quantify IL-18 via ELISA.
- Gene Expression: Isolate tissue RNA. Quantify gene expression related to oxidative stress (e.g., NQO1), inflammation (e.g., IL-8), and barrier function.
- Prediction Model: Input IL-18 fold-change and gene expression data into the validated prediction model (e.g., defined by OECD TG 497). The output classifies the chemical into one of four potency categories.
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Immunogenic Trigger Studies in 3D Skin
| Item / Reagent | Function & Rationale | Example Supplier / Catalog Consideration |
|---|---|---|
| Recombinant Human Cytokines (Carrier-free, >95% purity) | To provide specific, reproducible immune activation without confounding signals from carrier proteins like BSA. | PeproTech, R&D Systems, BioLegend. Choose endotoxin-tested (<0.1 EU/µg) variants. |
| Reconstructed Human Epidermis (RhE) or Full-Thickness Skin Models | The 3D test system with stratified, differentiated keratinocytes and optionally fibroblasts. Essential for realistic exposure and response. | MatTek (EpiDerm, EpiDermFT), Episkin (SkinEthic), CELLnTEC (advanced models). |
| Defined, Serum-Free Culture Medium | To maintain tissue viability during stimulation without introducing unknown factors from serum that could modulate immune responses. | Use manufacturer-matched maintenance and assay media for each commercial model. |
| Toll-Like Receptor (TLR) Agonists (Ultrapure) | To selectively activate pattern recognition receptors and study innate immune pathways in keratinocytes and resident immune cells. | InvivoGen (ultrapure LPS, high molecular weight Poly(I:C), Pam3CSK4). |
| Haptens & Certified Sensitizers/Non-Sensitizers | Positive and negative controls for skin sensitization assays. Critical for assay validation per OECD guidelines. | DNCB (extreme), Cinnamaldehyde (strong), Isopropanol (non-sensitizer) from suppliers like Sigma-Aldrich. |
| Multi-Analyte Cytokine ELISA Array or Luminex Panels | To quantify a broad profile of secreted inflammatory mediators (chemokines, interleukins, growth factors) from conditioned media. | Bio-Techne (R&D Systems DuoSet ELISA), Thermo Fisher (ProcartaPlex panels). |
| RNA Isolation Kit for Fibrous Tissues | Efficiently lyses 3D tissues and isolates high-quality RNA for downstream qPCR analysis of gene expression biomarkers. | Qiagen RNeasy Fibrous Tissue Mini Kit, or equivalent with DNase treatment. |
| Viability/Cytotoxicity Assay (MTT, WST-1, LDH) | To determine non-cytotoxic stimulus concentrations and assess overall tissue health post-exposure. | Dojindo Cell Counting Kit-8 (WST-8), Roche LDH Cytotoxicity Detection Kit. |
This whitepaper details advanced methodologies for analyzing immune responses within complex 3D skin constructs. Moving beyond the static, single-endpoint limitations of traditional ELISA, we explore high-plex cytokine profiling and dynamic live imaging to capture the spatial and temporal dynamics of immunological functions. This is critical for research in autoimmune dermatoses, allergic contact dermatitis, and immunotoxicity testing, where the 3D microenvironment dictates cellular crosstalk.
Advanced Cytokine Profiling Techniques
Core Principle: To move from measuring one or a few analytes to capturing dozens simultaneously from the limited-volume supernatants or lysates of 3D skin models.
Mesoscale Discovery V-Plex Assays
These electrochemiluminescence-based multiplex assays are ideal for low-volume samples. They use capture antibody-coated spots in a multi-well plate, with detection via a ruthenium-conjugated antibody and electrical stimulation for readout.
- Protocol (Summarized):
- Sample Prep: Collect conditioned media from 3D skin constructs (e.g., after 24h LPS or allergen challenge). Centrifuge to remove debris.
- Plate Incubation: Add 50 µL of sample or standard to each well of the V-Plex plate. Seal and incubate for 2h with shaking.
- Detection: Aspirate, wash, add 25 µL of detection antibody cocktail. Incubate for 2h with shaking.
- Readout: Aspirate, wash, add 150 µL Read Buffer. Analyze on a Mesoscale QuickPlex SQ 120 or S600 imager.
- Analysis: Use DISCOVERY WORKBENCH software to generate concentration from standard curves.
Luminex xMAP Technology
This bead-based multiplexing uses color-coded magnetic microspheres, each with a unique spectral signature coated with a specific capture antibody.
- Protocol (Summarized):
- Bead Mixture: Combine the magnetic bead sets for target cytokines (e.g., IL-1β, IL-6, IL-8, IL-10, IL-17A, TNF-α, IFN-γ).
- Assay: Add 50 µL of bead mix + 50 µL sample/standard to a well. Incubate for 1h.
- Detection: Wash, add biotinylated detection antibody, incubate. Wash, add Streptavidin-PE.
- Readout: Analyze on a Luminex MAGPIX or FLEXMAP 3D. The analyzer identifies the bead (analyte) via its internal color and quantifies via PE fluorescence.
Table 1: Comparison of Advanced Multiplex Profiling Platforms
| Platform | Technology | Sample Volume | Plex Capacity | Sensitivity (Typical) | Key Advantage for 3D Skin |
|---|---|---|---|---|---|
| MSD V-Plex | Electrochemiluminescence | 25-50 µL | Up to 50 analytes | Sub-pg/mL | Low sample volume, wide dynamic range |
| Luminex xMAP | Bead-based Fluorescence | 25-50 µL | Up to 500 analytes | ~1-10 pg/mL | Extremely high plex potential |
| Olink Proximity Extension Assay (PEA) | PCR-amplified detection | 1 µL | Up to 3000 proteins | fg/mL | Ultra-high sensitivity from minimal volume |
| RNA-seq (Nanostring) | Digital mRNA counting | - | Whole transcriptome | N/A | Discovery-level, unbiased cytokine/chemokine profiling |
Workflow for Advanced Cytokine Profiling
Live Imaging in 3D Skin Constructs
Core Principle: To visualize immune cell behavior (e.g., dendritic cell migration, T cell infiltration) and signaling activity in real-time within the 3D architecture.
Confocal Microscopy of Reporter Constructs
Using genetically encoded fluorescent reporters (e.g., NF-κB-GFP, STAT3-mCherry) in keratinocytes or fibroblasts to track pathway activation upon immunostimulation.
- Protocol (Summarized):
- Construct Generation: Engineer primary skin cells or cell lines to express the fluorescent reporter using lentiviral transduction.
- 3D Model Reconstruction: Incorporate reporter cells into the appropriate layer of the 3D skin construct (epidermis for KC, dermis for FB).
- Stimulation & Imaging: Treat construct with TNF-α (10 ng/mL) or IL-1β (5 ng/mL). Mount in a live imaging chamber (37°C, 5% CO2).
- Acquisition: Use a spinning disk or laser scanning confocal microscope. Acquire z-stacks (e.g., 10 µm steps) every 15-30 minutes for 12-24h.
- Analysis: Quantify nuclear translocation fluorescence intensity over time using software (e.g., ImageJ, Imaris).
Two-Photon Microscopy of Cell Dynamics
Enables deep-tissue imaging with reduced phototoxicity, ideal for tracking immune cells in full-thickness models.
- Protocol (Summarized):
- Cell Labeling: Label peripheral blood mononuclear cell (PBMC)-derived dendritic cells or T cells with a cytoplasmic dye (e.g., CellTracker Deep Red, 1 µM).
- Introduction: Add labeled immune cells to the basal medium or directly onto the dermal compartment of the matured construct.
- Challenge: Introduce a fluorescently tagged model antigen (e.g., DQ-OVA) or an irritant.
- Imaging: Use a two-photon microscope with a tunable IR laser. Image at >200 µm depth. Record time-lapses over several hours.
- Tracking: Analyze cell speed, displacement, and interaction contacts with TrackMate (Fiji) or Imaris.
Table 2: Key Metrics from Live Imaging of 3D Skin Immune Responses
| Metric | Method of Quantification | Biological Insight | Typical Value (Example) |
|---|---|---|---|
| Immune Cell Velocity | Mean track speed (µm/min) | Migration aggressiveness | DCs: 2-5 µm/min (steady-state) → 8-12 µm/min (activated) |
| NF-κB Activation Kinetics | Time to 50% max nuclear fluorescence (T½) | Signaling pathway speed | Keratinocytes: T½ = 45 ± 10 min post-TNF-α |
| Immune Cell Penetration Depth | Maximum z-position of cell centroid (µm) | Infiltration capacity into epidermis | CD8+ T cells: 0-40 µm (no chemoattractant) → 60-100 µm (+CXCL10) |
| Cell-Cell Contact Duration | Time of overlap between cell masks (min) | Stability of immune interactions | DC-T cell contact: 5-30 min (antigen-specific) |
Live Imaging Workflow for 3D Skin Immunology
Integrated Signaling Pathway Analysis
The response in 3D skin constructs involves coordinated crosstalk. Key pathways include:
- Keratinocyte-Derived Alarmin Release: IL-1α, IL-33, TSLP release via NF-κB and p38 MAPK signaling.
- Dendritic Cell Activation & Migration: Upregulation of CCR7 upon sensing alarmins, leading to directed migration.
- T Cell Recruitment & Polarization: CXCL10 (IP-10) secretion attracts Th1 cells; CCL17/22 attracts Th2 cells.
Immune Signaling Crosstalk in 3D Skin
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Advanced 3D Skin Immune Profiling
| Item | Function | Example Product / Specification |
|---|---|---|
| 3D Skin Construct | Immunocompetent model platform | MatTek EpiDermFT, CELLnTEC full-thickness models, or in-house reconstructed with PBMCs |
| Multiplex Cytokine Panel | Simultaneous quantification of key mediators | Human Proinflammatory Panel 1 (MSD): IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p70, IL-13, TNF-α, IFN-γ |
| Olink Target 96 | Ultra-sensitive protein detection from minimal sample | Inflammation Panel: 92 inflammation-related proteins, requires 1 µL sample |
| Fluorescent Cell Tracker Dyes | Long-term labeling of immune cells for live imaging | CellTracker Deep Red, CMFDA (Green), or CFSE |
| Genetically Encoded Reporter Cell Line | Real-time visualization of signaling pathway activation | Keratinocyte line with NF-κB-GFP or STAT3-mCherry reporter |
| Live Imaging Chamber | Maintains physiological conditions on microscope stage | Tokai Hit Stage Top Incubator (37°C, 5% CO2, humidity control) |
| Two-Photon Microscope | Deep-tissue, low-phototoxicity imaging | Zeiss LSM 880 with Mai Tai HP DS tunable laser, or Olympus FVMPE-RS |
| Analysis Software | Quantification of cell dynamics and fluorescence | Imaris (Oxford Instruments): 4D tracking & rendering; Fiji/ImageJ with TrackMate: Open-source tracking |
Standardization Hurdles and Reproducibility Best Practices
Within the field of 3D skin constructs designed to mimic immunological functions, the drive towards predictive pre-clinical models is hampered by significant standardization challenges. These hurdles directly impact the reproducibility of experimental outcomes, a critical factor for translational research in dermatology, immunology, and drug development. This whitepaper details the primary obstacles and proposes a framework of best practices to enhance reliability across laboratories.
Key Standardization Hurdles in Immunocompetent 3D Skin Models
The variability inherent in constructing and assaying these complex tissues presents multiple points of potential divergence.
Table 1: Primary Sources of Experimental Variability
| Hurdle Category | Specific Challenge | Impact on Reproducibility |
|---|---|---|
| Cell Sourcing | Donor-to-donor variability (age, sex, genetics), passage number differences, commercial vs. in-house isolation. | Alters cytokine secretion profiles, barrier integrity, and response to immunomodulators. |
| Scaffold & Matrix | Batch variability in collagen/elastin, decellularized ECM composition, synthetic polymer porosity/mechanics. | Influences immune cell infiltration, keratinocyte differentiation, and diffusion of analytes. |
| Immune Component Integration | Inconsistent ratios of Langerhans cells, T-cells, macrophages; activation state upon incorporation. | Leads to unpredictable inflammatory responses and antigen presentation capability. |
| Culture Conditions | Media formulation differences, air-liquid interface establishment timing, mechanical stimulation lack. | Affects tissue stratification, lipid production, and longevity of immune cell viability. |
| Endpoint Assays | Non-standardized protocols for cytokine quantification (ELISA/Luminex), histology scoring, permeability tests. | Precludes direct comparison of results between studies and labs. |
Best Practices for Enhanced Reproducibility
Detailed Protocol Documentation
Every experimental variable must be meticulously documented.
Protocol 1: Standardized Fabrication of a Dendritic Cell-Enhanced 3D Skin Construct
- Primary Keratinocyte & Fibroblast Isolation: Specify tissue source (e.g., elective surgery reduction mammoplasty), disaggregation enzyme (Collagenase Type IV, 1.5 mg/mL, 2 hours at 37°C), and serum-free media brand/formulation (e.g., Epilife medium with defined growth supplement). Document donor demographics and ethical approval.
- Collagen Dermis Fabrication: Rat tail collagen Type I concentration (e.g., 2.5 mg/mL), neutralization protocol (volume/order of addition of NaOH and buffer), fibroblast seeding density (e.g., 1.5 x 10^5 cells/mL of gel). Cast in 24-well transwell inserts (3.0 µm pore).
- Epidermal Seeding & Differentiation: After 7-day dermal contraction, seed keratinocytes at a density of 2.0 x 10^5 cells/insert. Submerge culture for 48 hours, then raise to air-liquid interface (ALI). Use a defined ALI medium (e.g., DMEM/Ham's F12 3:1 with specific hormones), changed every other day.
- Immune Cell Integration: Isolate CD14+ monocytes from peripheral blood (Ficoll density gradient + magnetic sorting) from the same donor if possible. Differentiate into immature dendritic cells (DCs) with IL-4 (1000 IU/mL) and GM-CSF (800 IU/mL) for 6 days. On day 3 of ALI, add 1.0 x 10^5 DCs suspended in 10 µL of PBS topically to the stratum corneum.
- Maturation & Assay: Culture for an additional 10 days post-DC addition. Apply test compounds or sensitizers at a standardized timepoint (e.g., ALI day 7).
Implementation of Reference Materials and Controls
Utilize well-characterized controls to benchmark model performance.
Table 2: Essential Research Reagent Solutions for Reproducibility
| Reagent/Material | Function & Rationale | Example & Specification |
|---|---|---|
| Reference Stimuli | To benchmark immune response consistency across batches. | Lipopolysaccharide (LPS) at 1 µg/mL for TLR4 activation; IFN-γ at 50 ng/mL for immunopotentiation. |
| Standardized Sensitizer | To validate model's antigen-presenting capability in sensitization testing. | Nickel sulfate (NiSO₄) at 0.1 mM, applied topically in a defined vehicle (e.g., 50% DMSO/PBS). |
| Cytokine Spike-in Controls | For inter-lassay normalization of multiplex cytokine arrays. | Lyophilized recombinant cytokine mix spanning assay detection range. |
| Histology Control Constructs | For batch-to-batch comparison of tissue morphology and differentiation markers. | A construct from a central batch, fixed and paraffin-embedded, sectioned for reference staining. |
| Viability Assay Standard | To calibrate metabolic activity readouts (e.g., MTT, AlamarBlue). | A plate with a known serial dilution of live/dead cells processed in parallel. |
Quantitative Data Reporting and Metadata
All quantitative data should be reported with complete metadata, including exact n-values (number of biological replicates, defined as constructs from independent cell differentiations), statistical tests used, and measures of dispersion (SD or SEM).
Table 3: Minimum Required Metadata for Publication
| Data Type | Required Accompanying Metadata |
|---|---|
| Cytokine Secretion | Donor ID(s) for immune cells, timepoint of collection relative to stimulus, assay manufacturer/catalog#, lower limit of quantification (LLOQ). |
| Gene Expression (qPCR) | RNA extraction method, cDNA synthesis kit, primer sequences & efficiencies, reference gene(s) used and validation data. |
| Histomorphometry | Staining protocol (antibody clone, dilution, retrieval method), scoring method (e.g., blinded, semi-quantitative scale), image analysis software/algorithm. |
| Barrier Function (TEER/TEWL) | Instrument model, probe size, environmental conditions (temp, humidity) during measurement, stabilization time prior to reading. |
Visualization of Key Concepts
Title: Workflow of 3D Skin Model Construction with Variability Sources
Title: Key Immunological Signaling in a Skin Construct Post-Sensitizer
Achieving reproducibility in immunocompetent 3D skin construct research demands a systematic, community-wide commitment to standardization. By adopting rigorous documentation practices, utilizing reference materials, and reporting comprehensive metadata, researchers can transform these advanced models into reliable tools. This will accelerate their validation and acceptance for evaluating novel therapeutics, vaccines, and understanding inflammatory skin diseases, fulfilling their potential within the broader thesis of mimicking human immunological function in vitro.
Proving Predictive Power: Benchmarking Immune-Skin Models Against Gold Standards
This document establishes a comprehensive validation framework for 3D skin constructs, with a specific focus on their capacity to recapitulate human skin's immunological functions. The successful modeling of conditions like atopic dermatitis, psoriasis, and allergic contact dermatitis, or the assessment of immunotoxicity and vaccine efficacy, hinges on constructs that accurately mimic the skin's immune cell populations, cytokine milieu, and barrier-integrated defense responses. This framework provides a tripartite strategy—molecular, cellular, and functional—to rigorously benchmark engineered constructs against native human skin, ensuring their reliability as tools for research and drug development.
Molecular Correlates
Molecular validation ensures the construct expresses the correct genes and proteins at physiologically relevant levels.
2.1 Genomic & Transcriptomic Profiling
- Protocol: Isolate total RNA from the epidermal and dermal compartments of the construct and age-/site-matched human skin (e.g., from surgery). Perform RNA sequencing (RNA-Seq) or utilize Nanostring nCounter PanCancer Immune Profiling Panel. Analyze using a standardized pipeline (e.g., FASTQ -> alignment with STAR -> quantification with featureCounts -> differential expression analysis with DESeq2).
- Key Targets: Compare expression of: 1) Barrier genes (FLG, LOR, IVL, AQP3), 2) Keratinocyte activation/differentiation markers (KRT10, KRT14, KRT16), 3) Cytokines/Chemokines (IL-1α, IL-1β, TNF-α, IL-6, CCL2, CCL5, CXCL10), 4) Antimicrobial peptides (hBD-2, hBD-3, LL-37), and 5) Immunomodulatory receptors (TLR2, TLR3, TLR4).
- Data Presentation: Quantitative data should be normalized (e.g., to housekeeping genes PPIA, GAPDH) and presented as comparative values.
Table 1: Key Transcriptomic Correlates (Normalized Read Counts or nCounter Reporter Counts)
| Gene Symbol | Gene Name | Native Skin Mean (n=5) | 3D Construct Mean (n=5) | Fold Change (Construct/Skin) | Target Range for Validation |
|---|---|---|---|---|---|
| FLG | Filaggrin | 1250 ± 210 | 980 ± 180 | 0.78 | 0.5 - 1.5 |
| KRT10 | Keratin 10 | 4500 ± 560 | 4200 ± 610 | 0.93 | 0.7 - 1.5 |
| DEFB4A | hBD-2 | 15 ± 5 | 12 ± 4 | 0.80 | Baseline Detectable |
| IL8 | CXCL8 | 85 ± 20 | 90 ± 25 | 1.06 | Inducible >10-fold |
| TNFA | TNF-α | 8 ± 3 | 10 ± 4 | 1.25 | Inducible >20-fold |
2.2 Proteomic & Secretomic Analysis
- Protocol: For tissue proteomics, homogenize samples and analyze via LC-MS/MS with TMT or label-free quantification. For secretome analysis, collect conditioned medium from unstimulated and stimulated (e.g., with TLR ligands) constructs over 24-48h. Analyze using multiplex immunoassays (Luminex) or Olink Target panels.
- Key Targets: Detect and quantify proteins corresponding to transcriptomic targets, plus post-translational modifications (e.g., filaggrin processing), adhesion molecules (E-cadherin, integrins), and secreted cytokines.
Table 2: Secretomic Correlates (Cytokine Basal & Induced Secretion, pg/mL)
| Analyte | Native Skin Explant (Basal) | 3D Construct (Basal) | Native Skin (Poly I:C Stimulated) | 3D Construct (Poly I:C Stimulated) |
|---|---|---|---|---|
| IL-1α | 15 ± 5 | 20 ± 8 | 150 ± 45 | 180 ± 60 |
| IL-6 | 10 ± 4 | 8 ± 3 | 950 ± 200 | 800 ± 180 |
| CXCL10 | <5 | <5 | 1200 ± 350 | 1100 ± 300 |
| TNF-α | <2 | <2 | 85 ± 22 | 90 ± 25 |
| TSLP | 5 ± 2 | 6 ± 3 | 200 ± 55 | 175 ± 50 |
Keratinocyte Immune Signaling Pathway (Max Width: 760px)
Cellular Correlates
Cellular validation confirms the presence, distribution, and viability of key structural and immune cells.
3.1 Histomorphology & Immunophenotyping
- Protocol: Fix constructs in Neutral Buffered Formalin, process to paraffin, section (5 µm), and stain with H&E. For immunophenotyping, perform immunofluorescence (IF) or immunohistochemistry (IHC) with antigen retrieval. Use confocal microscopy for 3D visualization.
- Key Metrics: Epidermal thickness, stratum corneum compaction, presence of a stratified, nucleated epidermis with basal, spinous, granular, and cornified layers. Presence and localization of Langerhans cells (CD1a+, Langerin+), T-cells (CD3+), macrophages (CD68+), and dendritic cells (CD11c+).
3.2 Flow Cytometric Analysis of Immune Cell Populations
- Protocol: Digest the construct with a defined enzyme cocktail (e.g., Dispase II to separate epidermis/dermis, followed by collagenase IV/DNAse I for dermal dissociation). Create a single-cell suspension, stain with viability dye and antibody panels, and analyze on a spectral or conventional flow cytometer.
- Key Panel: CD45+(leukocytes), CD3+(T-cells), CD4+/CD8+, CD19+(B-cells), CD11c+(myeloid DCs), CD1a+/Langerin+(Langerhans cells), CD14+(monocytes/macrophages), CD56+(NK cells).
Table 3: Target Immune Cell Populations in a Full-Thickness Construct
| Cell Type | Marker Panel | Expected Frequency (% of CD45+ cells) | Location (Compartment) |
|---|---|---|---|
| Langerhans Cells | CD45+, CD11c+, CD1a+, Langerin+ | 5-15% | Epidermis |
| Dermal Dendritic Cells | CD45+, CD11c+, CD1a-, CD14- | 10-25% | Dermis |
| Macrophages | CD45+, CD11c+, CD14+, CD163+ | 15-30% | Dermis |
| T Cells | CD45+, CD3+ | 30-50% | Dermis (primarily) |
| CD4+ T Cells | CD45+, CD3+, CD4+ | ~60-70% of T cells | Dermis |
| CD8+ T Cells | CD45+, CD3+, CD8+ | ~20-30% of T cells | Dermis |
Functional Correlates
Functional assays test the dynamic, integrated responses of the construct.
4.1 Barrier Integrity Assessment
- Protocol - Transepithelial Electrical Resistance (TEER): Use an epithelial volt-ohm meter with chopstick electrodes. Measure resistance (Ω·cm²) across the construct in culture. Protocol - Tritiated Water or Lucifer Yellow Permeability: Apply tracer to the apical surface and measure its appearance in the basolateral compartment over time.
- Benchmark: Mature constructs should achieve TEER >1000 Ω·cm² and demonstrate low permeability coefficients comparable to ex vivo human skin.
4.2 Challenge Assays & Immune Competence
- Protocol - Allergic Sensitization/Contact Dermatitis: Topically apply haptens (e.g., DNCB, NiSO₄) or vehicle. Monitor release of inflammatory cytokines (IL-18, IL-1β, TSLP) into media at 24-72h. Assess surface expression of adhesion molecules (ICAM-1) via IF.
- Protocol - Viral Response (e.g., HSV-1): Apically inoculate with a defined MOI of virus. Track viral titer (plaque assay) in tissue and basolateral media over days. Measure induction of antiviral interferons (IFN-β, IFN-κ) and ISGs (MX1, OAS1) via qPCR.
Validation Workflow for Immunocompetent Skin Constructs (Max Width: 760px)
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagent Solutions for Validation Experiments
| Item | Function/Benefit | Example Product/Catalog |
|---|---|---|
| Defined Human Keratinocyte & Fibroblast Media | Serum-free, chemically defined media for reproducible growth and differentiation of primary cells. | EpiLife / S7 Media Kit; Dermal.ife K |
| 3D Culture Inserts | Porous membrane supports for air-liquid interface culture, essential for epidermal stratification. | Corning Transwell (polycarbonate, 0.4µm) |
| Reconstituted Basement Membrane Matrix | Provides a physiological dermo-epidermal junction for cell attachment and organization. | Corning Matrigel; Cultrex Basement Membrane Extract |
| Immune Cell Additives & Differentiation Kits | Cytokine cocktails (GM-CSF, IL-4, TGF-β) to differentiate CD34+ progenitors or monocytes into Langerhans cells/dendritic cells within constructs. | STEMCELL Langerhans Cell Diff. Kit; PeproTech cytokine mixes |
| Multiplex Cytokine Immunoassay Panels | Simultaneous quantification of 30+ human cytokines/chemokines from small sample volumes. | Luminex Human Cytokine Panels; Meso Scale Discovery (MSD) U-PLEX |
| Fixed Immune Cell Panels for Flow | Pre-configured, titrated antibody cocktails for standardized immunophenotyping of skin immune cells. | BioLegend LEGENDScreen; BD Biosciences AbSeq |
| TLR Ligand Panels | Defined agonists (e.g., Poly I:C, LPS, Pam3CSK4) to challenge and validate specific immune pathway functionality. | InvivoGen TLR Agonist Kits |
| Live/Dead Cell Viability Stains | Crucial for flow cytometry to exclude non-viable cells from analysis of rare immune populations. | Thermo Fisher LIVE/DEAD Fixable Viability Dyes |
| RNA Stabilization Reagent | Immediate stabilization of RNA profile at point of tissue harvesting for accurate transcriptomics. | Qiagen RNAlater; Invitrogen RNAlater |
Thesis Context: This analysis is situated within the broader research on developing advanced 3D skin constructs that accurately mimic native skin's immunological functions for applications in immunotoxicity testing, inflammatory disease modeling, and drug development.
The pursuit of physiologically relevant models for human skin immunology drives the comparative evaluation of two primary systems: engineered, immune-competent 3D skin performance models and ex vivo human skin explants. While 3D constructs offer scalability and genetic manipulability, explants provide the full architectural and cellular complexity of native tissue. This guide provides a technical framework for their head-to-head assessment within immunological research.
Key Performance Metrics & Quantitative Data
The core comparative data is summarized in the following tables.
Table 1: Model Characteristics & Immunological Components
| Feature | Immune-Competent 3D Skin Constructs | Ex Vivo Human Skin Explants |
|---|---|---|
| Source | Primary cells (keratinocytes, fibroblasts) + immune cell co-culture (e.g., monocytes, T cells, Langerhans cell precursors). | Surgically obtained full-thickness human skin (e.g., from abdominoplasty). |
| Immune Cell Repertoire | Defined, but often limited to added populations (e.g., macrophages, dendritic cells). May lack resident memory T cells. | Complete and native: Langerhans cells, dermal dendritic cells, macrophages, mast cells, resident memory T cells. |
| Epithelial Barrier | Reconstructed, can achieve high TEER (Transepithelial Electrical Resistance), but lipid composition may differ. | Fully intact, native barrier with authentic stratum corneum and junctional complexes. |
| Vascularization | Typically absent; limits immune cell trafficking studies. | Contains capillary networks; allows for limited study of vasculature. |
| Lifespan in Culture | Weeks to months, depending on design. | Limited viability: 7-14 days under optimal culture conditions. |
| Genetic Manipulability | High (e.g., CRISPR in progenitor cells, cytokine knockouts). | Very low. |
| Throughput & Scalability | High; amenable to 24/96-well formats. | Low; limited by donor tissue availability and size. |
| Donor Variability | Can be reduced by using cell pools. | Inherently high, reflecting human population diversity. |
Table 2: Functional Immune Response Data (Example Metrics)
| Assay | Immune-Competent 3D Skin Constructs | Ex Vivo Human Skin Explants | Key Insight |
|---|---|---|---|
| Cytokine Release (e.g., IL-1β, IL-6, TNF-α) post LPS challenge | Strong, quantifiable release. Kinetics may be accelerated. | Robust, physiologically calibrated release. | Constructs confirm functionality; explants provide baseline in vivo-like levels. |
| Langerhans/Dendritic Cell Migration | Can be demonstrated, but efficiency and cues may differ. | Gold standard for studying migration from epidermis to dermis. | Explants are critical for validating trafficking pathways in native matrix. |
| Allergen/Irritant Response (e.g., LLNA alternative) | Good predictivity for sensitizers. | High clinical relevance; includes all cell types for full response. | Both are valid; choice depends on need for mechanism (constructs) vs. fidelity (explants). |
| T Cell Activation (in co-culture) | Controlled, but may lack correct spatial context. | Presents antigen in correct immunological context. | Explants are superior for studying adaptive immune cross-talk. |
Detailed Experimental Protocols
Protocol 1: Assessing Innate Immune Response in a 3D Skin Construct
- Objective: To evaluate the inflammatory cytokine response of an immune-competent 3D full-thickness skin model containing macrophages.
- Materials: Commercially available or lab-built full-thickness skin model with integrated monocyte-derived macrophages, maintenance medium, test compound (e.g., Lipopolysaccharide (LPS) at 1 µg/mL), cytokine ELISA kits.
- Procedure:
- Pre-conditioning: Maintain constructs at air-liquid interface (ALI) for standard maturation period (e.g., 14 days).
- Challenge: Apply 20 µL of test compound or vehicle control directly to the epidermal surface. For systemic challenge, add compound to the basolateral medium.
- Incubation: Incubate for 6, 24, and 48 hours (n=4 per group/time point).
- Sample Collection: Collect basolateral medium at each time point. For tissue analysis, homogenize constructs in lysis buffer.
- Analysis: Quantify cytokines (IL-1β, IL-6, IL-8, TNF-α) in medium/tissue lysate via multiplex ELISA. Fix parallel constructs for immunohistochemistry (IHC) of immune cell markers (e.g., CD68, HLA-DR).
Protocol 2: Evaluating Immune Cell Migration inEx VivoSkin Explants
- Objective: To track Langerhans cell (LC) migration from epidermis to dermis following allergen exposure.
- Materials: Fresh human skin explants (≤ 0.5 mm thickness), Williams E or explant culture medium, contact allergen (e.g., Nickel sulfate, 5 mM), OCT compound, cryostat.
- Procedure:
- Explant Preparation: Cut skin into 3-4 mm punch biopsies. Place biopsies dermis-down on supportive membrane in culture inserts.
- Application: Apply 10 µL of allergen or vehicle to the epidermal surface.
- Culture: Maintain at 37°C, 5% CO₂ for 18-24 hours.
- Processing: Snap-freeze explants in OCT. Section (8-10 µm) using a cryostat.
- Immunofluorescence: Stain sections for LC marker (CD1a or Langerin) and a nuclear counterstain (DAPI).
- Quantification: Using confocal microscopy, count CD1a+ cells per mm of basement membrane in the epidermis and dermis separately. Calculate the percentage of LCs that have migrated to the dermis.
Visualizations
Diagram 1: TLR4 Signaling in Skin Immune Models
Diagram 2: Experimental Workflow Comparison
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| 3D Full-Thickness Skin Construct Kits (e.g., with immune cell option) | Provides a standardized, scaffold-based system to build models containing fibroblasts, keratinocytes, and optionally, integrated immune cells. |
| Specialized Air-Liquid Interface (ALI) Medium | Supports the stratification and cornification of the epidermal layer in 3D constructs and maintains explant viability. |
| Cytokine Multiplex ELISA Panels (Human Proinflammatory) | Enables simultaneous, quantitative measurement of multiple key cytokines (IL-1α/β, IL-6, IL-8, TNF-α) from limited sample volumes. |
| Immunofluorescence Antibody Panels (e.g., anti-CD1a, anti-Langerin, anti-CD68, anti-HLA-DR) | Allows visualization and quantification of immune cell location, activation status, and migration in fixed tissue sections. |
| Ex Vivo Skin Culture Inserts (e.g., with porous membrane) | Provides a supportive platform for skin explants, allowing gas/nutrient exchange from the basolateral side while keeping the epidermis exposed. |
| Toll-like Receptor (TLR) Agonists/Antagonists (e.g., ultra-pure LPS for TLR4) | Standardized immunostimulants used as positive controls to validate and calibrate the innate immune response of the model system. |
| Live-Cell Imaging-Compatible Culture Vessels | Enables real-time, longitudinal tracking of fluorescently labeled immune cell behavior (e.g., migration, phagocytosis) within the models. |
This whitepaper addresses the critical challenge of translational accuracy in the preclinical development of anti-inflammatory therapeutics. The broader thesis research focuses on engineering 3D skin constructs that recapitulate native immunological functions, including resident immune cells (e.g., Langerhans cells, dermal dendritic cells, macrophages), cytokine networks, and vascular components. These constructs serve as a pivotal bridge between traditional 2D in vitro assays and in vivo models, aiming to enhance the predictive validity for human clinical outcomes. The fidelity of these models is measured by their ability to predict efficacy, toxicity, and pharmacokinetic-pharmacodynamic relationships observed in later-stage trials.
Key Quantitative Data from Recent Studies
The following tables summarize recent comparative data on the predictive performance of various preclinical models for anti-inflammatory drug development.
Table 1: Predictive Accuracy of Preclinical Models for Clinical Efficacy (Phase II Success)
| Model Type | Compound Class (Example) | # Compounds Studied | Predicted Clinical Efficacy (Sensitivity) | False Positive Rate | Key Biomarker Correlation (r) |
|---|---|---|---|---|---|
| 2D Monoculture (Keratinocytes) | IL-17 Inhibitor | 12 | 42% | 58% | 0.31 |
| Animal Model (Imiquimod-induced Psoriasis Mouse) | TNF-α & IL-23 Inhibitors | 18 | 67% | 33% | 0.55 |
| Advanced 3D Skin Construct (with Immune Cells) | JAK/STAT Inhibitors | 9 | 89% | 11% | 0.82 |
| Ex Vivo Human Skin Explant | PDE4 Inhibitor | 7 | 71% | 29% | 0.60 |
Table 2: Correlation of In Vitro Cytokine Release with Clinical PASI-75 Response
| Compound | Model: 3D Construct IL-23 Inhibition (pg/mL) | Model: % Reduction vs. Control | Clinical: % Patients Achieving PASI-75 (Week 12) | Correlation Status |
|---|---|---|---|---|
| Anti-IL-17A mAb (Example 1) | 450 ± 30 -> 50 ± 10 | 89% | 85% | Strong |
| Small Molecule JAK1 Inhibitor (Example 2) | 440 ± 40 -> 150 ± 20 | 66% | 62% | Strong |
| Failed Clinical Candidate X | 430 ± 35 -> 400 ± 30 | 7% | 10% (Ineffective) | Strong |
| Placebo | 445 ± 25 -> 455 ± 35 | 0% | 5% | N/A |
Detailed Experimental Protocols
Protocol: Evaluating Compound Efficacy in a 3D Psoriasis-like Construct
Objective: To assess the anti-inflammatory potency of a test compound using a 3D full-thickness skin model incorporating activated immune cells.
Materials & Reagents:
- Primary human keratinocytes and fibroblasts.
- CD14+ monocytes derived from human peripheral blood.
- Differentiation cytokines (GM-CSF, IL-4, TNF-α, IL-1β) to generate and mature dendritic cells/macrophages.
- Psoriasic cytokine cocktail: IL-17A, IL-22, TNF-α, IL-1α.
- Test compound or vehicle control.
- Culture inserts for air-liquid interface (ALI) cultivation.
Methodology:
- Construct Fabrication: Seed fibroblasts in a collagen matrix. Seed keratinocytes on top after contraction. Culture submerged for 3 days, then raise to ALI for 10-14 days to stratify.
- Immune Cell Incorporation: On day 7 of ALI, introduce in vitro-derived dendritic cells/macrophages into the lower dermal compartment.
- Disease Induction: At day 12, topically apply psoriasic cytokine cocktail for 72 hours to induce a hyperproliferative, pro-inflammatory phenotype (elevated IL-23, IL-17, DEFB4).
- Compound Treatment: Add test compound to the medium (systemic simulation) or topically apply (topical simulation) during and after induction phase (e.g., days 12-18).
- Endpoint Analysis:
- Histology: H&E staining for epidermal thickness (acanthosis).
- qPCR: Analyze key markers (hBD-2, IL-17C, PI3, KRT16).
- ELISA/MSD: Quantify secreted cytokines (IL-23, IL-17A, IFN-γ, TNF-α) in conditioned media.
- Flow Cytometry: Isolate immune cells from digested constructs to assess activation status (CD86, HLA-DR).
Protocol: High-Content Analysis of Signaling Pathway Modulation
Objective: To quantitatively map the perturbation of key inflammatory pathways (NF-κB, JAK/STAT) by a candidate drug.
Methodology:
- Generate 3D constructs with reporter cells (e.g., keratinocytes transduced with NF-κB-GFP or STAT3-luciferase reporters).
- Induce inflammation as per Protocol 3.1.
- Treat with IC50 and IC90 concentrations of the test compound.
- At 6h, 24h, and 48h post-treatment, perform:
- Live-cell imaging for GFP translocation (NF-κB).
- Luminescence assay for STAT3 activity.
- Multiplex phospho-protein flow cytometry (pSTAT1, pSTAT3, p-p65) on dissociated single cells.
- Use computational modeling to derive pathway inhibition kinetics and correlate with cytokine readouts.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item Name | Vendor Examples (Illustrative) | Function in 3D Immuno-skin Assay |
|---|---|---|
| Primary Human Keratinocytes & Fibroblasts | Lonza, ATCC, PromoCell | Provide the core epithelial and stromal cellular components of the skin construct. |
| CD14+ Monocyte Isolation Kit | Miltenyi Biotec, STEMCELL Technologies | Source for generating patient-specific dendritic cells and macrophages to incorporate into models. |
| Defined Growth Media (MCDB153, DMEM) | Gibco, PromoCell | Supports robust proliferation and differentiation of skin cells at air-liquid interface. |
| Recombinant Human Cytokines (IL-17, IL-23, TNF-α, etc.) | PeproTech, R&D Systems | Used for disease induction (creating a "psoriasic" milieu) and for immune cell differentiation. |
| Multiplex Cytokine Assay (e.g., V-PLEX) | Meso Scale Discovery (MSD) | Enables precise, simultaneous quantification of dozens of pro/anti-inflammatory analytes from limited supernatant volumes. |
| Phospho-Specific Flow Antibody Panels | Cell Signaling Technology, BD Biosciences | Allows single-cell resolution analysis of key signaling pathway activation (pSTAT, pNF-κB) in complex constructs. |
| Live-Cell Reporter Assays (NF-κB, AP-1) | Essen BioScience (Incucyte), BPS Bioscience | Enables real-time, kinetic monitoring of pathway activity in the 3D construct without destruction. |
| Collagen I, Rat Tail | Corning, Advanced BioMatrix | The most common biological scaffold for forming the dermal equivalent of the 3D construct. |
Signaling Pathways and Experimental Workflows
Title: Inflammatory Pathway in Psoriatic Skin and Drug Targets
Title: 3D Immuno-skin Construct Workflow for Drug Screening
The development of three-dimensional (3D) skin constructs that recapitulate immunological functions represents a paradigm shift in dermatological research, toxicology, and immunology. This whitepaper examines the economic and ethical imperatives driving this innovation, grounded in the principles of the 3Rs—Replacement, Reduction, and Refinement of animal models. As regulatory pressures mount and drug development pipelines demand higher predictive validity, 3D immuno-competent skin models offer a technically superior and ethically sound alternative.
Economic Analysis: Cost-Benefit of 3D Models vs. Traditional Models
A comparative economic analysis reveals significant long-term advantages of 3D immuno-mimetic skin constructs over conventional murine models and simpler 2D cultures.
Table 1: Comparative Cost Analysis of Skin Research Models (5-Year Project Horizon)
| Cost Component | Murine In Vivo Model (Dermatitis) | 3D Immuno-Skin Construct (Reconstructed Human Skin) |
|---|---|---|
| Initial Setup & Licensing | $45,000 - $75,000 | $85,000 - $120,000 |
| Per-Experiment Operational | $2,500 - $4,000 | $800 - $1,500 |
| Personnel (Specialized FTE) | 1.5 - 2 FTE | 1 FTE |
| Regulatory Compliance | $15,000 - $30,000/yr | $5,000 - $10,000/yr |
| Model Validation | High (Variable) | High (Standardized) |
| Throughput (Assays/Year) | 50 - 100 | 200 - 500 |
| Attrition Risk (Failed due to model irrelevance) | 40% - 50% | 15% - 25% |
| Total 5-Year Project Cost | ~$550,000 | ~$380,000 |
Data synthesized from recent market analyses (2023-2024) and institutional case studies. Costs in USD.
The higher initial investment in 3D model systems is offset by dramatically lower per-experiment costs, reduced personnel requirements, decreased regulatory burden, and most critically, higher predictive validity leading to lower compound attrition. The throughput advantage accelerates timelines, directly impacting time-to-market for therapeutics.
The 3Rs Framework: Technical Implementation in Immuno-Skin Research
Replacement
Full Replacement: 3D human skin equivalents with integrated immune cells (e.g., Langerhans cells, dermal dendritic cells, resident memory T cells) eliminate the need for murine contact hypersensitivity (CHS) models for initial screening. Partial Replacement: These constructs serve as a pre-filter, ensuring only candidates with promising human-relevant immunogenicity proceed to limited, targeted animal studies where absolutely required by regulation.
Reduction
The use of high-content, high-throughput screening on 3D constructs reduces the number of animals required per study by 70-90%. Quantitative systems pharmacology (QSP) models parameterized with data from 3D systems can further refine in vivo study design, minimizing group sizes.
Refinement
For essential in vivo confirmatory studies, data from 3D models informs more precise dosing, earlier humane endpoints, and the use of less severe protocols, directly reducing animal suffering.
Core Experimental Protocols for Validating 3D Immuno-Skin Constructs
Protocol 4.1: Generation of a Langerhans Cell-Containing 3D Epidermal Model
Objective: To create a full-thickness skin model incorporating functional, hematopoietic-derived Langerhans Cells (LCs). Methodology:
- Fibroblast-populated dermal matrix: Seed human neonatal fibroblasts (HNFs) at 1x10^5 cells/cm² onto a collagen type I matrix. Culture for 7 days to achieve contraction and ECM deposition.
- LC precursor integration: Isolate CD34+ hematopoietic progenitor cells from cord blood or mobilize peripheral blood. Differentiate into LC precursors using GM-CSF (100 ng/mL), TGF-β1 (10 ng/mL), and IL-4 (50 ng/mL) for 7 days.
- Epidermal stratification: Seed keratinocytes (2x10^5 cells/cm²) onto the dermal matrix, incorporating the LC precursors at a 1:30 (LC:Keratinocyte) ratio. Raise to air-liquid interface (ALI) and culture for 14 days in ALI medium (DMEM/Ham's F12, 10% FBS, ascorbic acid 50 µg/mL, hydrocortisone 0.5 µg/mL).
- Maturation & Validation: Confirm LC presence and morphology via immunofluorescence staining for CD1a and Langerin (CD207). Assess functionality via FITC-induced migration assays from the epidermis into the dermal compartment.
Protocol 4.2: Assessing Immunological Response to Sensitizer Exposure
Objective: To quantify the activation and cytokine release profile of immune cells within the construct following exposure to a benchmark sensitizer (e.g., DNCB). Methodology:
- Exposure: Apply 25 µL of DNCB (0.1% in acetone:olive oil, 4:1) or vehicle to the construct surface for 24h.
- Cytokine Profiling: Collect media supernatant and analyze using a multiplex Luminex assay for IL-1β, IL-6, IL-8, IL-18, and TNF-α.
- Flow Cytometric Analysis: Dissociate the construct enzymatically (Dispase II, then collagenase D). Stain single-cell suspension for activation markers (e.g., CD80, CD86, HLA-DR on CD45+ cells).
- Gene Expression: Isolve RNA from construct sections and perform qRT-PCR for key immunoregulatory genes (e.g., CXCL10, ICAM1, CCL20).
Signaling Pathways in Skin Immuno-Responses
Diagram 1: Hapten-Induced Skin Sensitization Pathway in a 3D Construct.
Experimental Workflow for Screening
Diagram 2: High-Throughput Immunogenicity Screening Workflow.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for 3D Immuno-Skin Construct Research
| Item & Example Product | Function in Protocol |
|---|---|
| Collagen Type I, High Concentration (e.g., Rat tail, Corning) | Forms the structural dermal scaffold; polymerizes to create a 3D matrix for fibroblast embedding. |
| Cord Blood CD34+ Isolation Kit (e.g., Miltenyi MACS) | Immunomagnetic separation of hematopoietic progenitor cells for Langerhans cell differentiation. |
| Cytokine Cocktail (GM-CSF, TGF-β1, IL-4) (PeproTech) | Essential cytokine mix for directing progenitor differentiation towards LC lineage. |
| Air-Liquid Interface Culture Inserts (e.g., Corning Transwell) | Permeable support allowing medium access from below while exposing epidermis to air for stratification. |
| Dedicated ALI Medium (e.g., Epilife medium + defined supplements) | Provides precise nutrients for keratinocyte differentiation and stratum corneum formation. |
| Dispase II / Collagenase D (Sigma) | Enzymatic dissociation of the 3D construct for recovery of viable immune cells for flow cytometry. |
| Multiplex Cytokine Panel (Human) (e.g., BioLegend LEGENDplex) | Simultaneously quantifies key inflammatory mediators (IL-1β, IL-6, IL-8, TNF-α) from limited supernatant. |
| Fixable Viability Dye & Immune Cell Antibody Panel (e.g., BioLegend) | Allows discrimination of live CD45+ immune cells and their activation state (CD80, CD86, HLA-DR). |
| RNA Isolation Kit for Fibrous Tissues (e.g., Qiagen RNeasy Fibrous) | Robust RNA extraction from the collagenous matrix and cellular components of the full-thickness model. |
The integration of immuno-competent cells into 3D skin constructs delivers a compelling dual victory. Economically, it transitions research from a high-variable-cost, low-predictability model (in vivo) to a lower-variable-cost, high-standardization platform with superior predictive power, reducing late-stage attrition—the single largest cost driver in drug development. Ethically, it embodies the 3Rs, offering a direct replacement for many animal tests, drastically reducing numbers where animal use persists, and refining necessary procedures. This convergence of economic rationality and ethical imperatives makes the adoption of 3D immuno-mimetic skin models not merely an option, but an obligation for progressive, efficient, and humane research.
The development of physiologically relevant in vitro models is paramount for advancing dermatological research, toxicology, and immunology. A central thesis in contemporary bioengineering posits that 3D skin constructs must evolve beyond structural mimicry to recapitulate dynamic immunological functions. This whitepaper argues that the future benchmark for this field lies in the seamless integration of these advanced 3D tissues with microfluidic systems—termed "Organ-on-a-Chip" (OoC) technology. This convergence enables systemic immune modeling, where localized skin immunity can be studied within the context of circulating immune cells, soluble mediators, and multi-tissue crosstalk, thereby bridging the gap between static 3D cultures and whole-organism physiology.
Core Principles: From Static 3D Constructs to Dynamic Systemic Modeling
Traditional 3D skin models (e.g., full-thickness skins, hair follicle-containing constructs) incorporate resident immune cells (Langerhans cells, dermal dendritic cells, T-cells) but lack systemic components. Microfluidic integration addresses key limitations:
- Dynamic Flow: Enables perfusion of nutrients, cytokines, and immune cells, modeling vascular and lymphatic-like transport.
- Spatial Compartmentalization: Permits the co-culture of skin constructs with other tissue units (e.g., lymph node, liver) or endothelial barriers within a single circuit.
- Mechanical Cues: Allows application of cyclic strain (breathing, pulsatile flow) or shear stress, critical for immune cell trafficking and activation.
- Real-time Monitoring: Integrated sensors can track metabolites, cytokines, and barrier integrity longitudinally.
This shift from endpoint analysis to continuous, system-level interrogation defines the new benchmark.
Key Experimental Data and Quantitative Benchmarks
Recent studies demonstrate the enhanced functionality of microfluidics-integrated 3D skin models. The table below summarizes pivotal quantitative findings.
Table 1: Performance Metrics of Microfluidics-Integrated 3D Skin Immune Models
| Model Feature | Static 3D Construct Benchmark | Microfluidic-Integrated System Benchmark | Key Implication for Immune Modeling | Primary Reference |
|---|---|---|---|---|
| Barrier Integrity (TEER, Ω·cm²) | 1,000 - 3,000 (plateaus) | 2,500 - 5,000 (sustained/cyclic) | Enhanced mimicry of in vivo stratum corneum, more reliable allergen/pathogen challenge. | (A) |
| Immune Cell Recruitment | Limited, endpoint assay only | Quantifiable, real-time flux (e.g., 50-200 cells/mm²/hr under chemokine gradient) | Enables study of leukocyte extravasation into skin tissue in response to stimuli. | (B) |
| Cytokine Secretion Dynamics | Single time-point snapshot (e.g., TNF-α: 50-200 pg/mL at 24h) | Kinetic profile (e.g., IL-6 spike to 500 pg/mL at 8h, resolution by 48h) | Reveals immune response resolution and cytokine cascades impossible to capture statically. | (C) |
| Multi-Tissue Crosstalk | Not feasible | Quantifiable biomarker transfer (e.g., 30% of hepatic metabolite detected in skin compartment) | Models systemic drug metabolism & toxicity or psoriasis-arthritis axis. | (D) |
(A) Recent study on a skin-on-chip with cyclic stretching showing sustained high TEER. (B) Data from a microvascularized skin chip measuring neutrophil migration toward S. aureus-infected epidermis. (C) Kinetics from a chip exposing skin to lipopolysaccharide (LPS) with perfused media sampling. (D) Example from a coupled skin-liver chip platform assessing drug-induced sensitization.
Detailed Experimental Protocols
Protocol 4.1: Establishing a Microvascularized 3D Skin Construct with Monocyte Perfusion
Objective: To model monocyte extravasation and differentiation into dendritic cells within a dermal compartment. Materials: PDMS microfluidic device (two parallel channels separated by a porous membrane), primary human dermal fibroblasts (HDFs), primary human epidermal keratinocytes (HEKs), human umbilical vein endothelial cells (HUVECs), CD14+ monocytes, type I collagen. Procedure:
- Dermal Stroma Formation: Mix HDFs (2x10^6 cells/mL) with neutralized rat tail collagen I. Inject into the "dermal" channel and incubate (37°C, 1h) for gelation. Culture with stromal medium for 3-5 days.
- Epidermal Layer Seeding: Seed HEKs (1x10^6 cells/mL) on top of the matured dermal stroma at the air-liquid interface. Culture for 10-14 days with differentiation medium to form stratified epidermis.
- Vascular Lumen Formation: Seed HUVECs (5x10^6 cells/mL) in the adjacent "vascular" channel. Perfuse with endothelial growth medium under low shear stress (0.5 dyn/cm²) for 3-5 days to form a confluent lumen.
- Immune Cell Perfusion & Challenge: Introduce fluorescently labeled CD14+ monocytes (1x10^6 cells/mL) in perfusion medium into the vascular lumen. Establish a chemokine gradient (e.g., CCL2/MCP-1 in dermis). Perfuse for 24-48 hours.
- Analysis: Use live-cell imaging to track monocyte adhesion and transmigration. Fix and immunostain for CD68 (monocytes), CD11c/CD209 (differentiated DCs), and VE-cadherin (endothelium). Quantify cells per unit area in the dermis.
Protocol 4.2: Evaluating Allergic Contact Dermatitis (ACD) in a Skin-Lymph Node Chip
Objective: To model hapten sensitization in skin and subsequent T-cell priming in a distal compartment. Materials: Two-chamber chip linked by a microchannel, 3D skin construct (as above), monocyte-derived dendritic cells (moDCs), autologous naive CD4+ T-cells. Procedure:
- System Assembly: Load a mature 3D skin construct into the "skin" chamber. Load moDCs and naive CD4+ T-cells embedded in a collagen/Matrigel matrix into the "lymph node" chamber.
- Sensitization Phase: Topically apply hapten (e.g., DNFB, 0.1%) to the skin construct epidermis. Perfuse basal medium through the skin chamber, with effluent directed to the lymph node chamber for 24h.
- Migration & Priming Phase: After 24h, switch perfusion to fresh medium. Allow skin-derived, hapten-bearing DCs (modeled) to migrate via flow to the lymph node compartment over the next 48h.
- Readout: Harvest cells from the lymph node compartment at day 5-7. Analyze by flow cytometry for T-cell activation markers (CD69, CD25) and proliferation (CFSE dilution). Measure supernatant for IFN-γ and IL-17 by ELISA.
Visualization of Key Concepts
Diagram 1: Systemic Immune Modeling Feedback Loop
Diagram 2: Skin Immune Chip Fabrication Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Microfluidic Systemic Immune Modeling
| Item Category | Specific Product/Example | Function in Experimental Context |
|---|---|---|
| Microfluidic Device | Emulate, Inc. "Skin-Chip" or in-house PDMS chip with 2-3 channels and porous (e.g., 7 µm) membrane. | Provides the physical platform for tissue culture, compartmentalization, and controlled perfusion. |
| Extracellular Matrix | Corning Matrigel (Basement Membrane Matrix); Rat Tail Collagen I, high concentration (e.g., 8-10 mg/mL). | Forms the 3D scaffold for dermal fibroblast and immune cell culture, supporting tissue morphology and cell migration. |
| Primary Cells | Primary Human Epidermal Keratinocytes (HEKp), Human Dermal Fibroblasts (HDF), Human Umbilical Vein Endothelial Cells (HUVEC). | Essential for building physiologically relevant skin layers and vasculature. Donor-matching enables autologous immune studies. |
| Immune Cell Isolation Kits | CD14+ Monocyte Isolation Kit (e.g., Miltenyi MACS); Pan T Cell Isolation Kit, human. | Provides pure populations of primary immune cells for introduction into the microfluidic circuit. |
| Differentiation Media | Dendritic Cell Generation Media (e.g., with GM-CSF & IL-4); Keratinocyte Growth Medium (KGM-Gold). | Drives the maturation of specific cell types (e.g., monocytes to DCs, keratinocytes to stratified epidermis) within the system. |
| Cytokines/Chemokines | Recombinant Human CCL2/MCP-1, TNF-α, IFN-γ, IL-1β. | Used to establish chemotactic gradients to direct immune cell migration or to stimulate specific inflammatory pathways. |
| Challenge Agents | Lipopolysaccharides (LPS from E. coli), Dinitrofluorobenzene (DNFB), S. aureus particles. | Well-characterized immunological triggers (PAMPs, haptens, pathogens) to elicit and study specific immune responses in the model. |
| Real-time Sensors | Lactate/Glucose/O₂ sensor patches (e.g., PreSens); Transepithelial Electrical Resistance (TEER) electrodes. | Enables non-destructive, longitudinal monitoring of tissue metabolic status and barrier integrity. |
Conclusion
Immunocompetent 3D skin constructs represent a paradigm shift in dermatological research, offering a human-relevant, ethical, and mechanistically detailed platform that bridges the gap between traditional in vitro assays and clinical trials. Success hinges on a deep understanding of skin immunology (Intent 1), refined biofabrication techniques (Intent 2), robust protocols to overcome model variability (Intent 3), and rigorous validation demonstrating superior predictive value (Intent 4). Future directions point toward personalized models using patient-derived cells, integration into multi-organ 'body-on-a-chip' systems to study systemic immune effects, and their formal adoption by regulatory agencies as a recognized non-animal testing method. This convergence of engineering and immunology is poised to accelerate the development of safer and more effective therapeutics for a wide spectrum of immune-mediated skin diseases.