Decoding Immune Variation: How Genetics and Environment Shape Human Health and Disease Treatment
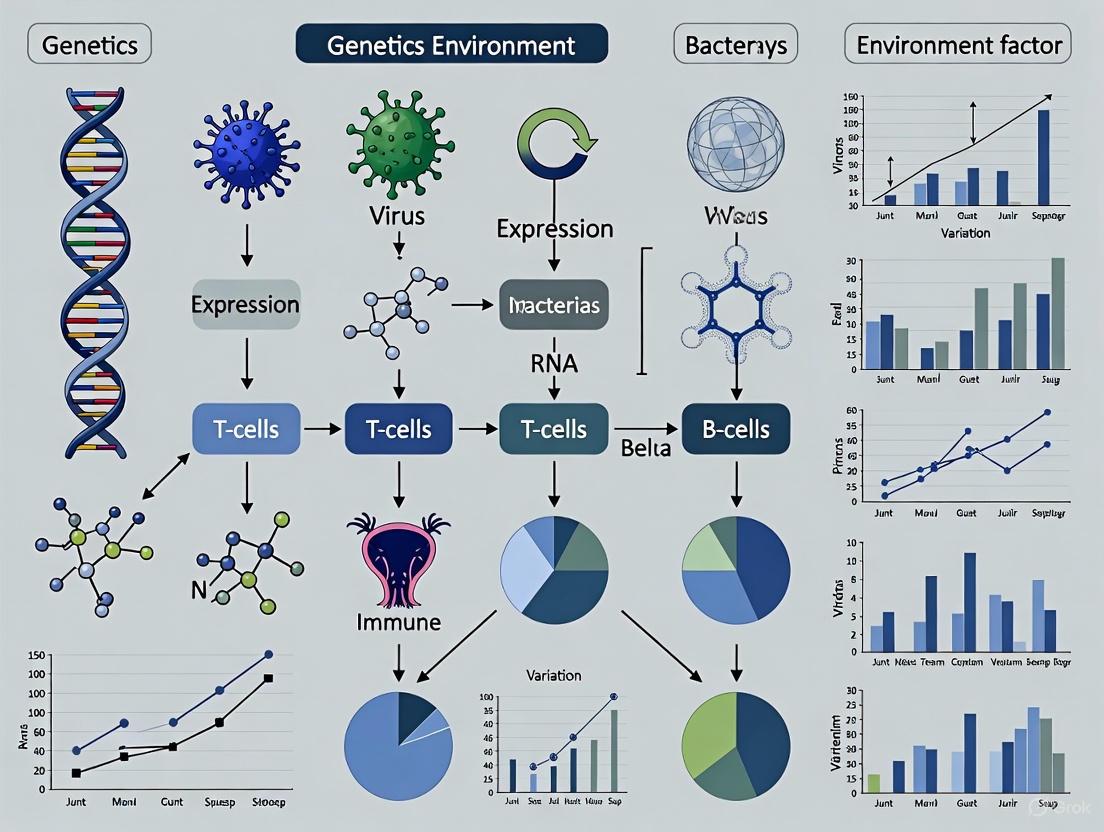
This article provides a comprehensive analysis for researchers and drug development professionals on the complex interplay between genetic susceptibility and environmental factors in shaping inter-individual immune variation.
Decoding Immune Variation: How Genetics and Environment Shape Human Health and Disease Treatment
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on the complex interplay between genetic susceptibility and environmental factors in shaping inter-individual immune variation. We explore foundational concepts of immune system heterogeneity, examine cutting-edge methodological approaches like GWAS and Mendelian randomization for target discovery, and address key challenges in translating these insights into effective therapies. The content further validates these strategies through case studies in autoimmune diseases and infectious diseases like COVID-19, highlighting how genetic evidence de-risks drug development and informs personalized treatment paradigms. By synthesizing recent advances in multi-omics and systems immunology, this review serves as a strategic guide for leveraging human genetic variation to improve therapeutic outcomes.
The Blueprint and the Trigger: Foundational Principles of Genetic Susceptibility and Environmental Exposures
The human immune system is a complex network of cells and proteins that defends the body against infection. Understanding the genetic blueprint that controls the immense variation in immune responses between individuals is a fundamental pursuit in immunology and precision medicine. This variation arises from a complex interplay between inherited genetic factors and environmental exposures throughout life. The Major Histocompatibility Complex (MHC), particularly the Human Leukocyte Antigen (HLA) genes, represents the most critical genetic locus governing immune recognition. However, genome-wide association studies (GWAS) have increasingly revealed the significant contribution of non-HLA risk loci outside this region. This technical review synthesizes current knowledge on the genetic architecture of immune variation, framing it within the broader context of how genetics and environment interact to shape individual immune phenotypes. We provide a comprehensive resource for researchers and drug development professionals, integrating recent genomic discoveries with experimental methodologies and analytical frameworks.
The MHC Region: Central Command for Immune Recognition
Structural and Functional Organization of the MHC
The MHC region on chromosome 6p21.3 spans approximately 4 Mb and is characterized by extreme polymorphism, high gene density, and strong linkage disequilibrium (LD) [1]. This region is traditionally divided into three classes:
- Class I genes (HLA-A, -B, -C): Present intracellular peptides to CD8+ T-cells; expressed on most nucleated cells.
- Class II genes (HLA-DR, -DQ, -DP): Present extracellular peptides to CD4+ T-cells; primarily expressed on antigen-presenting cells.
- Class III genes: Encode complement components and inflammatory cytokines.
The classical HLA genes are among the most polymorphic in the human genome, with the IPD-IMGT/HLA Database documenting over 10,000 alleles for HLA-B alone [2]. This diversity primarily localizes to the antigen-binding groove, enabling recognition of a vast array of pathogens.
Table 1: Key Features of the MHC Genomic Region
| Feature | Description | Functional Implication |
|---|---|---|
| Size | ~4 Mb on chromosome 6p21.3 | Dense clustering of immunologically relevant genes |
| Gene Content | >250 genes, including classical HLA genes (A, B, C, DR, DQ, DP) and non-classical genes (E, G, etc.) | Coordinated regulation of innate and adaptive immunity |
| Polymorphism | Extreme diversity with trans-species polymorphisms | Recognition of diverse pathogen repertoire; balancing selection |
| Linkage Disequilibrium | Extensive and complex LD patterns | Challenges in pinpointing causal variants; haplotype blocks |
| Expression Variation | Allele-specific expression and alternative splicing | Additional layer of regulatory complexity beyond protein coding |
Mechanistic Insights from MHC-Disease Associations
GWAS have established that the MHC region shows the strongest genetic associations for numerous autoimmune, infectious, and inflammatory diseases [3] [1]. The mechanistic underpinnings of these associations are multifaceted:
- Peptide Presentation Specificity: Certain HLA types confer risk by preferentially presenting self-antigens (in autoimmunity) or inefficiently presenting pathogen-derived antigens (in infectious disease) [1].
- Expression Level Variation: HLA types are associated with differential expression of their cognate genes, potentially influencing immune activation thresholds. A study of 361 iPSC lines found that 44.2% of HLA types showed significantly different expression levels compared to other alleles of the same gene [1].
- Regulatory Variation: Non-coding variants can alter gene expression through effects on transcription factor binding, as demonstrated by histone QTLs enriched within autoimmune risk haplotypes [4].
- Ancestral Haplotypes: Extended haplotypes spanning the entire MHC region, such as the 8.1 ancestral haplotype (8.1AH), carry multiple risk alleles and are associated with multiple autoimmune diseases while being protective against bacterial colonization in cystic fibrosis patients [1].
Non-HLA Risk Loci: Expanding the Genetic Landscape
Genome-Wide Insights into Immune Regulation
While the MHC region accounts for a substantial portion of heritability for immune-mediated diseases, GWAS have identified hundreds of non-HLA risk loci distributed across the genome. These loci typically confer more modest individual risk effects but collectively contribute significantly to disease susceptibility. Systematic evaluations reveal that these non-HLA loci are frequently enriched in immune cell enhancers and regions of open chromatin, highlighting their likely regulatory functions [5].
In primary biliary cholangitis (PBC), a systematic review of 105 studies involving 71,031 cases and 140,499 controls identified 44 variants significantly associated with disease risk, comprising 30 HLA variants and 14 non-HLA variants [5]. Pathway analysis revealed significant enrichment of mapped genes in immune cell regulation and immune response-regulating signaling pathways.
Functional Annotation of Non-HLA Variants
The majority of disease-associated non-HLA variants reside in non-coding genomic regions, suggesting they exert their effects through gene regulation rather than protein coding changes [4]. Several mechanisms have been elucidated:
- Cis-Regulatory Effects: Non-coding variants can alter transcription factor binding affinity, affecting gene expression levels. For example, an obesity-associated variant in the FTO locus alters ARID5B binding, leading to increased expression of IRX3 and IRX5 genes [4].
- Post-Transcriptional Regulation: Variants can affect RNA splicing, stability, or translation through alteration of miRNA binding sites or RNA-binding protein interactions [4].
- Epigenetic Modulation: Genetic variants can influence chromatin accessibility and histone modifications, creating cell-type-specific regulatory landscapes.
Table 2: Representative Non-HLA Immune Risk Loci and Their Proposed Mechanisms
| Locus/Gene | Associated Disease(s) | Variant(s) | Proposed Mechanism |
|---|---|---|---|
| PTPN22 | Rheumatoid arthritis, Type 1 diabetes, SLE | rs2476601 | Gain-of-function mutation weakening T-cell receptor signaling |
| IL23R | Inflammatory bowel disease, Psoriasis | rs11209026 | Altered IL-23 signaling affecting Th17 cell differentiation |
| NOD2 | Crohn's disease | rs2066844, rs2066845, rs2066847 | Impaired recognition of bacterial peptidoglycan |
| IRF5 | Systemic lupus erythematosus | rs10488631 | Increased expression of type I interferon-regulated genes |
| TNFAIP3 | Rheumatoid arthritis, SLE | rs10499194, rs6920220 | Impaired negative regulation of NF-κB signaling |
Quantitative Assessment of Genetic Contributions
Heritability Estimates and Locus Effect Sizes
The relative contribution of genetic factors to immune traits and diseases varies considerably. Twin studies provide estimates of broad-sense heritability, while GWAS-derived significant SNPs account for narrow-sense heritability. For example, monozygotic twin concordance rates for Crohn's disease approach ~50% compared to ~3-4% in dizygotic twins, indicating a substantial genetic component [4].
Recent analyses of FinnGen data (412,181 individuals, 2,459 diseases) demonstrate striking enrichment of disease associations in the HLA region compared to the rest of the genome [3]. Infectious diseases showed nearly 400-fold enrichment in the HLA region, while autoimmune, endocrine, and dermatologic diseases showed 100- to 200-fold enrichment [3].
Pleiotropy and Risk Trade-Offs in the HLA Region
The HLA region exhibits extensive pleiotropy, where specific genetic variants influence multiple distinct diseases. Haplotype-based analyses have revealed complex patterns of disease associations, with some HLA alleles conferring risk for certain conditions while being protective against others [3]. This pleiotropy reflects evolutionary trade-offs, wherein alleles that enhance protection against specific pathogens may simultaneously increase susceptibility to autoimmune or inflammatory disorders.
Table 3: Venice Criteria Assessment of Genetic Associations in Primary Biliary Cholangitis [5]
| Variant/Gene | Pooled OR (95% CI) | P-value | Cumulative Evidence | False-Positive Report Probability |
|---|---|---|---|---|
| HLA-DQB1*0301 | 1.42 (1.28-1.57) | < 5.0 × 10⁻⁸ | Strong | < 0.05 |
| HLA-DRB1*08 | 2.98 (2.58-3.44) | < 5.0 × 10⁻⁸ | Strong | < 0.05 |
| rs231775 (CTLA-4) | 1.32 (1.24-1.41) | < 5.0 × 10⁻⁸ | Strong | < 0.05 |
| rs7574865 (STAT4) | 1.43 (1.34-1.52) | < 5.0 × 10⁻⁸ | Strong | < 0.05 |
| A*3303 | 2.15 (1.72-2.69) | < 5.0 × 10⁻⁸ | Strong | < 0.05 |
Gene-Environment Interactions: Shaping Immune Phenotypes
Experimental Models for G×E Interactions
The relative contributions of genetic and environmental factors to immune variation remain incompletely characterized. Controlled experiments with "rewilded" laboratory mice—inbred strains introduced into natural outdoor environments—have provided key insights [6]. When C57BL/6, 129S1, and PWK/PhJ mice were rewilded and infected with Trichuris muris, multivariate analysis revealed that:
- Cellular composition of peripheral blood mononuclear cells was shaped by interactions between genotype and environment (Gen × Env)
- Cytokine response heterogeneity was primarily driven by genotype, with consequences for parasite burden
- Genetic differences observed under laboratory conditions were often reduced following rewilding [6]
These findings demonstrate that nonheritable influences interact with genetic factors to shape immune variation and disease outcomes.
Molecular Signatures of G×E Interactions
Human studies have mapped genetic variants that affect how gene expression changes in response to immune stimulation. Monocytes from 134 volunteers treated with pathogen-mimicking components revealed hundreds of genes where response to immune stimulus depended on the individual's genetic variants [7]. This research demonstrated that:
- Genetic risk for autoimmune diseases like lupus and celiac disease is enriched for gene regulatory effects modified by immune activation state
- Genetic risk factors may sometimes manifest only under specific environmental conditions, such as infection [7]
- A complete understanding of disease risk requires consideration of both genetic makeup and environmental exposures
Methodologies: Decoding Immune Variation
Analytical Frameworks and Computational Tools
MHC Hammer: Comprehensive HLA Disruption Analysis
MHC Hammer is a computational toolkit that evaluates genomic and transcriptomic disruption of class I HLA genes through four major components [8]:
- Allele-specific HLA somatic mutation identification
- HLA loss of heterozygosity (LOH) calculation
- HLA allele-specific repression evaluation
- Allele-specific HLA alternative splicing identification
Application to normal lung and breast tissue from the GTEx project revealed pervasive HLA allelic imbalance (70-81% of samples across HLA genes) and frequent alternative splicing (87-97% of samples) [8]. These findings emphasize the importance of controlling for baseline HLA expression variation when assessing transcriptional alterations in disease.
MHC Hammer Analysis Workflow: A comprehensive pipeline for evaluating HLA genomic and transcriptomic disruption.
Haplotype-Based Association Mapping
To address the challenges of extreme linkage disequilibrium in the HLA region, haplotype-based approaches have been developed that consider combinations of variants across extended genomic segments. These methods have revealed that:
- Disease associations often track with specific haplotypes rather than individual SNPs
- Regulatory variation can confer disease risk independently of classical HLA coding variation
- Analysis of phased haplotypes provides enhanced power to detect associations compared to single-variant approaches [3] [1]
Experimental Protocols for Immune Repertoire Profiling
Multimodal Single-Cell Profiling of Tissue Immunity
Comprehensive analysis of immune cells across tissues requires specialized methodologies [9]:
Protocol: Multimodal Immune Cell Profiling from Human Tissues
Tissue Acquisition and Processing
- Source tissues from organ donors within 4-8 hours of cross-clamp time
- Process tissues using mechanical dissociation and enzymatic digestion (e.g., collagenase IV/DNase I)
- Isolate mononuclear cells via density gradient centrifugation
Cell Staining and Sorting
- Stain cells with antibody panels for surface markers (≥125 antibodies for CITE-seq)
- Include viability dyes to exclude dead cells
- Sort specific populations if needed using FACS
Library Preparation and Sequencing
- Generate single-cell suspensions for 10x Genomics platform
- Prepare gene expression libraries alongside feature barcodes for surface proteins
- Sequence on Illumina platforms with sufficient depth (≥20,000 reads/cell)
Bioinformatic Analysis
- Process data using Cell Ranger with custom reference incorporating HLA alleles
- Integrate datasets across donors using harmony or similar tools
- Annotate cell types leveraging both RNA and protein expression (e.g., with MMoCHi)
- Perform differential expression and trajectory analysis
This approach has revealed tissue-directed signatures of human immune cells altered with age, showing that age-associated effects manifest in a tissue- and lineage-specific manner [9].
Rewilding Experimental Design
The rewilding approach models human environmental exposures in genetically defined mouse strains [6]:
Protocol: Rewilding and Immune Challenge
Animal Housing and Group Assignment
- Use 8-12 week old female inbred mice (C57BL/6, 129S1, PWK/PhJ)
- Randomly assign to laboratory housing ("Lab") or outdoor enclosures ("Rewilded")
- Maintain laboratory controls under summer-like photoperiod and temperature
Environmental Exposure and Infection
- Acclimate rewilded mice for 2 weeks in outdoor enclosures
- Infect with 200 Trichuris muris embryonated eggs or leave uninfected
- Return to respective environments for additional 3 weeks
Sample Collection and Analysis
- Collect peripheral blood at multiple time points for CBC/DIFF and PBMC isolation
- Process tissues (spleen, lymph nodes, intestinal sections) for cellular analysis
- Analyze by spectral cytometry with comprehensive lymphocyte and myeloid panels
- Perform multivariate statistical analysis (MDMR) to partition variance components
Rewilding Experimental Design: Approach to quantify genetic and environmental contributions to immune variation.
Table 4: Key Research Reagents and Computational Tools for Immune Variation Studies
| Resource | Type | Primary Application | Key Features |
|---|---|---|---|
| MHC Hammer | Computational pipeline | HLA disruption analysis | Integrates genomic and transcriptomic data; detects LOH, allele-specific expression, and splicing [8] |
| HLA-VBSeq | Computational tool | Eight-digit HLA typing from WGS | High recall rates (>98.5%) and reproducibility (>95%) across 30 MHC genes [1] |
| CITE-seq | Experimental platform | Multimodal single-cell profiling | Simultaneous measurement of transcriptome and >125 surface proteins [9] |
| MMoCHi | Computational classifier | Cell type annotation | Leverages both surface protein and gene expression for hierarchical classification [9] |
| Rewilding Enclosures | Experimental system | Gene-environment interactions | Naturalistic outdoor environments for laboratory mice [6] |
| MARIO | Computational method | Allele-specific binding | Identifies regulatory protein binding differences at heterozygous variants [4] |
The genetic architecture of immune variation represents a complex, multi-layered system centered on the highly polymorphic MHC region but extending to numerous non-HLA loci distributed throughout the genome. The functional consequences of this genetic variation are expressed through allele-specific expression, alternative splicing, regulatory element modulation, and protein coding changes that collectively shape immune responsiveness. Critically, these genetic effects do not operate in isolation but interact dynamically with environmental exposures throughout life, as demonstrated by rewilding experiments and studies of immune activation. Future research must continue to develop increasingly sophisticated analytical frameworks that can dissect these complex relationships, with particular attention to underrepresented populations and tissue-specific effects. The integration of genetic data with functional genomics and environmental context will be essential for translating these insights into targeted therapeutic strategies and personalized medicine approaches for immune-mediated diseases.
The immune system is not a static entity but a dynamic interface, continuously shaped by the complex interplay between an individual's genetic blueprint and their lifetime exposure to environmental factors. While genetic predisposition sets the foundational rules of immune responsiveness, a growing body of evidence indicates that nonheritable influences interact with these genetic factors to orchestrate immune variation and disease susceptibility [6]. This whitepaper provides an in-depth technical analysis of key environmental triggers and modulators—infections, the microbiome, and pollutants—framed within the context of immune variation research. Understanding these interactions is paramount for researchers and drug development professionals aiming to deconvolute disease etiology and develop targeted therapeutic interventions.
The Genotype-Environment Interface in Immune Variation
Quantifying the relative contributions of genetics and environment is methodologically challenging. Studies often attribute variation not linked to genetics to "environment" alone, overlooking critical genotype-by-environment (Gen × Env) interactions, which occur when environmental effects are differentially amplified in different genetic backgrounds [6]. Controlled experiments using inbred mouse strains of diverse genetic backgrounds (e.g., C57BL/6, 129S1, and the wild-derived PWK/PhJ) have been instrumental in dissecting these interactions.
A pivotal "rewilding" study introduced laboratory mice to a natural outdoor environment, exposing them to a complex array of natural antigens and microbes. Subsequent analysis demonstrated that cellular composition of immune cells was significantly shaped by Gen × Env interactions. In contrast, cytokine response heterogeneity, such as IFNγ production, was primarily driven by genotype, with direct consequences on pathogen burden, as shown by infection with the helminth Trichuris muris [6]. Notably, some genetic differences in immune markers (e.g., CD44 expression on T cells) observed under controlled laboratory conditions were diminished following rewilding, while other differences (e.g., a stronger T helper 1 response to infection in C57BL/6 mice) emerged only in the rewilding condition [6]. This underscores that the effect of an extreme environmental shift on immune phenotype is modulated by genetics, and, in turn, the expressivity of genetic differences among strains is modulated by the environment.
Table 1: Relative Contributions of Genetics and Environment to Specific Immune Traits in a Rewilding Model
| Immune Trait | Genetic Influence | Environmental Influence | Gen × Env Interaction | Experimental Context |
|---|---|---|---|---|
| PBMC Cellular Composition | Significant | Significant | Notable Contributor | Multivariate analysis of rewilded vs. lab mice [6] |
| IFNγ Cytokine Response | Primary Driver | Lesser Contribution | Not Reported | Infection with Trichuris muris [6] |
| CD44 Expression on T cells | Mostly Explained | Lesser Contribution | Not Reported | Comparison across strains and environments [6] |
| CD44 Expression on B cells | Lesser Contribution | Mostly Explained | Not Reported | Comparison across strains and environments [6] |
| TH1 Response to T. muris | Dependent on Environment | Dependent on Genotype | Emergent | Stronger response in C57BL/6 mice only in rewilding [6] |
Environmental Pollutants as Immunomodulators
Environmental pollutants represent a significant class of immunomodulatory triggers, with exposure linked to a range of inflammatory, autoimmune, and metabolic pathologies. These pollutants can exert their effects directly on immune cells or indirectly through the disruption of the gut microbiome.
Mechanisms of Pollutant-Induced Immunotoxicity
Pollutants, including heavy metals, persistent organic pollutants (POPs), and particulate matter (PM), can perturb the immune system through several direct and indirect mechanisms:
- Direct Immune Activation: Air pollutants like PM2.5 are taken up by lung immune cells, triggering the release of pro-inflammatory cytokines (e.g., IL-6) and reactive oxygen species (ROS) that drive systemic inflammation and oxidative stress [10]. Heavy metals such as lead can dysregulate inflammatory enzymes and promote ROS production, disrupting cell membranes via lipid peroxidation [10].
- Microbiome-Mediated Effects: Upon ingestion, pollutants interact with the gut microbiome, the first line of contact for many ingested xenobiotics. Gut microbes can metabolize pollutants into more or less toxic states, influencing their systemic distribution [11]. Conversely, pollutants can cause gut dysbiosis, characterized by a decrease in beneficial commensal bacteria (e.g., short-chain fatty acid producers) and an overgrowth of pro-inflammatory species [12] [10]. This dysbiosis can compromise intestinal barrier integrity, leading to a "leaky gut" that allows bacterial metabolites and virulence factors (e.g., LPS) to enter the bloodstream, perpetuating systemic inflammation [12] [10].
- Epigenetic Modulation: Exposure to air pollutants has been associated with epigenetic modifications, such as the hypermethylation of the Foxp3 gene, which can weaken the function of regulatory T cells (Tregs) and disrupt immune tolerance [10].
Table 2: Immunotoxic Effects of Select Environmental Pollutants
| Pollutant Class | Example Compounds | Primary Exposure Route | Key Immunological Consequences | Proposed Mechanisms |
|---|---|---|---|---|
| Heavy Metals | Lead (Pb), Cadmium (Cd), Mercury (Hg) | Ingestion, Inhalation | Oxidative stress, pro-inflammatory cytokine release, autoimmunity, gut dysbiosis [12] [10] | ROS generation, inflammation enzyme dysregulation, altered gut microbiota composition [11] |
| Persistent Organic Pollutants (POPs) | Polychlorinated Biphenyls (PCBs) | Ingestion | Altered gut microbial composition, inflammation [11] | Activation of signaling pathways (e.g., Aryl Hydrocarbon Receptor/AHR) within the intestine [11] |
| Particulate Matter | PM2.5, PM10 | Inhalation | Exacerbation of asthma/COPD, increased risk of rheumatoid arthritis and IBD, systemic inflammation [10] | Uptake by lung immune cells, cytokine release, oxidative stress, impaired phagocytosis, Treg impairment [10] |
| Microplastics | Polyethylene Terephthalate (PET) | Ingestion | Gut inflammation, oxidative stress, systemic diseases [10] | Intestinal cell uptake, intracellular oxidative stress, mitochondrial dysfunction, activation of TLRs [10] |
The Gut Microbiome as a Central Signaling Hub
The gut microbiota, a complex ecosystem of trillions of microorganisms, is a critical intermediary between environmental exposures and host immunity. It plays a fundamental role in the maturation and regulation of the immune system, and its disruption is a common pathway through which other environmental triggers exert their effects.
The Microbiota-Gut-Brain Axis (MGBA)
The bidireсtionаl сommuniсаtion between the gut and the brain, known as the gut-brain axis (GBA), is heavily influenced by the microbiota. The MGBA involves communication through neurological (autonomous nervous system, vagus nerve), hormonal (HPA axis), and immunological (cytokine) pathways [12]. Gut microbes produce a vast array of metabolites that can signal to distant organs, including the brain.
- Key Microbial Metabolites:
- Short-Chain Fatty Acids (SCFAs): Produced by bacterial fermentation of dietary fiber, SCFAs like butyrate, propionate, and acetate are crucial for maintaining intestinal barrier integrity and have systemic anti-inflammatory effects. They can cross the blood-brain barrier via monocarboxylate transporters, where they modulate neuroinflammation, influence brain-derived neurotrophic factor (BDNF) levels, and support neurogenesis [12].
- Neuroactive and Immunomodulatory Metabolites: The microbiome influences tryptophan metabolism, a precursor for serotonin, and can produce or consume other neurotransmitters [12]. Changes in the availability of these metabolites can significantly impact brain function and behavior.
Metabolite-Immune Interactions Across Populations
Recent large-scale metabolomic studies have further illuminated the intricate links between circulating metabolites and immune function. A multi-cohort analysis of individuals from Western Europe and sub-Saharan Africa identified robust associations between specific metabolic pathways and cytokine responses.
- Glycerophospholipid Metabolism: This pathway was consistently identified across cohorts as being associated with cytokine production (e.g., IL-1β, IL-6, TNF) following Staphylococcus aureus stimulation, highlighting its cross-population relevance in immune regulation [13].
- Sphingomyelin: This sphingolipid exhibited a significant negative correlation with monocyte-derived cytokine production. Functional validation experiments confirmed that sphingomyelin could reduce TNF, IL-1β, and IL-6 production in peripheral blood mononuclear cells (PBMCs). Furthermore, Mendelian randomization analysis established a causal link between higher sphingomyelin levels and increased COVID-19 severity, positioning it as a potential therapeutic target for immune modulation [13].
Table 3: Key Metabolites Linking Microbiome and Immune Function
| Metabolite | Origin | Associated Immune Function | Mechanistic Insight & Validation |
|---|---|---|---|
| Short-Chain Fatty Acids (SCFAs) | Gut microbial fermentation of dietary fiber | Anti-inflammatory; maintenance of gut barrier; regulation of microglia & neuroinflammation [12] | Cross BBB; promote Treg differentiation; modulate neurotrophic factors [12] |
| Sphingomyelin | Host synthesis, dietary intake | Negative regulation of innate immune response; reduced pro-inflammatory cytokine production (TNF, IL-6, IL-1β) [13] | Experimentally validated to inhibit cytokine production in PBMCs; MR shows causal link to COVID-19 severity [13] |
| Glycerophospholipids | Host synthesis, dietary intake | Correlation with cytokine responses (IL-1β, IL-6, TNF) to bacterial stimuli [13] | Pathway consistently enriched in immune-metabolite interaction networks across diverse cohorts [13] |
Experimental Models and Methodologies
Detailed Protocol: Rewilding and Helminth Infection Model
This protocol is designed to quantify the interactive effects of genotype and environment on immune phenotypes and parasite burden [6].
Animal Models and Housing:
- Utilize genetically diverse inbred mouse strains (e.g., C57BL/6, 129S1, PWK/PhJ).
- Randomly assign mice into two environmental groups:
- Laboratory Controls: Housed in a conventional vivarium under standard or summer-mimicking photoperiod/temperature.
- Rewilded: Housed in a protected outdoor enclosure for a defined period (e.g., 2 weeks pre-infection).
Infection Challenge:
- After the initial environmental exposure (e.g., 2 weeks), infect a subset of mice from each group and environment with approximately 200 embryonated eggs of the intestinal helminth Trichuris muris. Maintain a separate uninfected control group for each condition.
- Return all mice to their respective environments (lab or outdoor) for a further 3 weeks.
Sample Collection and Analysis:
- Peripheral Blood: Collect blood at multiple time points for complete blood count (CBC) with differential and for PBMC isolation.
- Immune Phenotyping by Spectral Cytometry: Isolate PBMCs and stain with a comprehensive lymphocyte panel (e.g., including CD4, CD8, B220, TCRβ, CD44, Ki-67, T-bet). Use unsupervised k-means clustering to group cells into populations based on marker expression for unbiased analysis.
- Cytokine Analysis: Measure cytokine production (e.g., IFNγ) from stimulated immune cells or in serum.
- Worm Burden Assessment: At endpoint, quantify adult worms in the cecum/colon to determine parasite burden.
Statistical Analysis:
- Multivariate Distance Matrix Regression (MDMR): Use MDMR to quantify the independent and interactive contributions of genotype, environment, and infection to the high-dimensional variance in immune cell composition.
- Principal Component Analysis (PCA): Visualize the major axes of variation in immune profiles and identify cell populations driving these patterns.
In Vitro Protocol: Metabolite-Mediated Immune Modulation
This protocol validates the immunomodulatory effect of specific metabolites identified in association studies [13].
Cell Isolation and Culture:
- Isolate human PBMCs from fresh whole blood of healthy donors by density gradient centrifugation (e.g., Ficoll-Paque).
- Resuspend PBMCs in appropriate culture medium (e.g., RPMI-1640 with 10% FBS).
Metabolite Treatment and Stimulation:
- Pre-treat PBMCs with the metabolite of interest (e.g., sphingomyelin, dissolved in a suitable vehicle) at a range of physiological concentrations. Include vehicle-only control wells.
- After pre-treatment (e.g., 1-2 hours), stimulate the cells with a potent innate immune activator, such as heat-killed Staphylococcus aureus. Maintain unstimulated controls.
Cytokine Measurement:
- After incubation (e.g., 24 hours for innate cytokines), collect cell culture supernatants.
- Quantify the concentration of pro-inflammatory cytokines (e.g., TNF, IL-6, IL-1β) using high-sensitivity immunoassays (e.g., ELISA or multiplex bead-based arrays).
Visualization of Pathways and Workflows
Pollutant-Induced Immunotoxicity Pathways
Diagram 1: Integrated pollutant-gut-immune axis.
Rewilding Experimental Workflow
Diagram 2: Rewilding experiment design.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Resources for Investigating Environment-Immune Interactions
| Resource Category | Specific Example | Function & Application |
|---|---|---|
| In Vivo Models | C57BL/6, 129S1, PWK/PhJ inbred mice [6] | Provide controlled genetic diversity to model human population variation and study Gen × Env interactions. |
| Pathogen Challenge | Trichuris muris embryonated eggs [6] | Standardized parasite challenge to study mucosal and systemic immune responses in different environments. |
| Immunophenotyping | Spectral Cytometry Panel (TCRβ, B220, CD4, CD8, CD44, Ki-67, T-bet) [6] | High-dimensional, unbiased characterization of immune cell composition and activation states. |
| Data Resources | Immune Signatures Data Resource [14] | A compendium of standardized systems vaccinology datasets (30 studies, 1405 participants) for comparative analysis of vaccine-induced immune responses. |
| Analytical Tools | Multivariate Distance Matrix Regression (MDMR) [6] | Statistical method to quantify contributions of genotype, environment, and their interaction to high-dimensional immune variation. |
| Metabolite Libraries | Sphingomyelin, Short-Chain Fatty Acids [13] [12] | For functional validation experiments in vitro to test causal effects of metabolites on immune cell function. |
| Interactive Databases | IMetaboMap [13] | Publicly available tool for exploring metabolite-cytokine interactions across different ethnicities and sexes. |
The aetiology of complex human diseases has long been understood to extend beyond purely genetic or environmental explanations, residing instead in their dynamic interplay. This in-depth technical guide explores the Convergence Model, which posits that disease pathogenesis emerges from the interaction of an individual's genetic susceptibility with cumulative environmental exposures. Framed within the broader context of immune variation research, this review synthesizes current evidence on molecular mechanisms—with a focus on epigenetic regulation—and details advanced methodological frameworks for studying these interactions. We provide structured quantitative data, experimental protocols for key studies, and visualizations of critical signalling pathways to equip researchers and drug development professionals with the tools to advance this field. The translation of these findings promises to reshape therapeutic strategies towards precision environmental health and preventive medicine.
For decades, the quest to understand disease aetiology has oscillated between genetic determinism and environmental causation. The Convergence Model resolves this false dichotomy by proposing that genetic predisposition and environmental factors interact in a complex, non-additive manner to drive disease pathogenesis [15]. This framework is particularly relevant for immune-mediated diseases, where the immune system serves as a critical interface between an organism's genetic blueprint and its environmental exposures.
The limitations of studying these factors in isolation are increasingly apparent. Genome-wide association studies (GWAS) have successfully identified hundreds of disease-associated genetic loci, yet these variants typically confer only modest increases in disease risk and often exhibit incomplete penetrance [15]. For example, in systemic lupus erythematosus (SLE), only 10-30% of individuals with damaging mutations in the complement component 2 (C2) gene develop the disease [15]. Conversely, epidemiological studies consistently demonstrate that not all individuals exposed to an environmental risk factor develop the associated condition, highlighting the role of underlying genetic susceptibility.
This whitepaper examines the converging evidence from human studies and experimental models that reveals how these interactions operate at molecular, cellular, and systems levels. By framing our discussion within immune variation research, we aim to provide drug development professionals and researchers with a comprehensive technical resource that bridges fundamental mechanisms with translational applications.
Molecular Mechanisms of Gene-Environment Interactions
Epigenetic Mediation: The Biological Memory of Exposure
Epigenetics represents a primary molecular mechanism through which environmental exposures interface with the genome to influence disease risk. Epigenetic modifications—including DNA methylation, histone modifications, and non-coding RNAs—regulate gene expression without altering the underlying DNA sequence [16] [17]. These modifications create a dynamic "molecular memory" of environmental exposures that can persist long after the exposure has ended [17].
The epigenome functions analogously to a conductor's annotations on a musical score—while the notes (genes) remain unchanged, the annotations (epigenetic marks) dramatically alter how the music is performed [17]. Environmental factors—from chemical toxicants to psychosocial stress—can rewrite these epigenetic annotations, potentially leading to immune dysregulation and disease pathogenesis [16] [18].
Table 1: Environmental Exposures and Their Epigenetic Mechanisms in Autoimmune Disease
| Exposure Category | Specific Exposures | Epigenetic Mechanism | Associated Autoimmune Conditions |
|---|---|---|---|
| Chemical Factors | Silica, organic solvents | DNA hypomethylation, histone modifications | Systemic sclerosis, SLE, rheumatoid arthritis |
| Medications | Procainamide, hydralazine | DNA methyltransferase inhibition | Drug-induced lupus |
| Physical Factors | Ultraviolet (UV) radiation | Altered DNA methylation in keratinocytes | Cutaneous lupus, SLE flares |
| Biological Factors | Epstein-Barr virus (EBV) infection | DNA methylation changes in immune cells | Multiple sclerosis, SLE, rheumatoid arthritis |
| Lifestyle Factors | Cigarette smoking | DNA methylation changes, histone modifications | Rheumatoid arthritis, SLE |
Notably, these environmentally-induced epigenetic changes can exhibit tissue specificity and may be heritable across cell divisions, creating persistent alterations in cellular function [17]. In some cases, these modifications can even be transmitted transgenerationally through germ cells, as demonstrated in mouse studies where chronic psychosocial stress altered DNA methylation patterns in male germ cells and affected offspring development [16].
Immune System as the Convergence Interface
The immune system serves as a particularly sensitive interface for gene-environment interactions due to its requirement for dynamic responsiveness to environmental challenges while maintaining tolerance to self-antigens. Research has demonstrated that environmental factors can disrupt peripheral tolerance mechanisms, particularly those mediated by regulatory T cells (Tregs), in genetically susceptible individuals [19].
In autoimmune diseases, Tregs often exhibit intrinsic signalling defects despite normal frequencies. Recent evidence identifies impaired IL-2 receptor (IL-2R) signal durability as a key mechanism, linked to aberrant degradation of signalling components like phosphorylated JAK1 and DEPTOR [19]. This dysfunction stems from diminished expression of GRAIL, an E3 ubiquitin ligase that regulates these signalling molecules.
Table 2: Quantitative Contributions of Genetic vs. Environmental Factors to Disease Risk
| Disease/Condition | Genetic Contribution | Environmental Contribution | Key Evidence |
|---|---|---|---|
| Major Depression | ~37% of susceptibility | Significant role of early-life stress, caregiver mental health | Twin and adoption studies [16] |
| Anxiety Disorders | 30-50% of variance | Trauma, socioeconomic factors | Meta-analysis of twin studies [16] |
| Type 2 Diabetes | Lower predictive value | Higher predictive value of environmental score | Polygenic vs. polyexposure score comparison [20] |
| Autoimmune Diseases | Strong MHC association | Infections, silica, solvents, UV radiation | GWAS and epidemiological studies [19] [18] |
| Immune Cell Composition | Varies by cell type | Strong environmental influence | Rewilded mouse studies [6] |
The convergence of genetic risk variants with environmental triggers creates a permissive environment for breaking self-tolerance. For example, in rheumatoid arthritis, the interaction between HLA-shared epitope alleles and smoking history significantly increases disease risk compared to either factor alone [18].
Methodological Approaches for Studying Gene-Environment Interactions
Advanced Study Designs and Analytical Frameworks
Investigating gene-environment interactions requires sophisticated methodological approaches that can simultaneously capture genetic and environmental contributions. Traditional candidate gene-environment interaction studies have evolved into more comprehensive genome-wide interaction studies (GWIS) that examine the entire genome for loci whose effects on disease are modified by environmental factors [21].
The emergence of the exposome concept—encompassing the totality of environmental exposures from conception onward—has driven development of novel exposure assessment methods [17]. High-resolution metabolomics can now simultaneously measure up to 1,000 chemicals, providing a more holistic view of the internal chemical environment [17]. These advances are complemented by computational methods that use epigenetic fingerprints to reconstruct past exposures, even when the causative chemicals are no longer detectable [22].
The Adverse Outcome Pathway (AOP) framework has been developed as a tool to support environmental risk assessment by systematically organizing evidence linking molecular initiating events through intermediate key events to adverse health outcomes [18]. This structured approach helps distinguish correlational from causal relationships between environmental exposures and disease outcomes through epigenetic modifications.
The "Rewilded" Mouse Model: An Experimental Paradigm
Experimental Protocol: Rewilding and Trichuris muris Infection
Objective: To quantify the relative and interactive contributions of genetic and environmental influences on immune phenotypes and helminth susceptibility.
Subjects: Female inbred mice of strains C57BL/6, 129S1, and PWK/PhJ (genetically diverse founders of the Collaborative Cross).
Experimental Groups:
- Laboratory controls: Housed in conventional vivarium with summer-like temperatures and photoperiods
- Rewilded: Housed in outdoor enclosure for natural environmental exposure
Procedure:
- Randomly assign mice to laboratory or rewilding groups (n=135 total across two experimental blocks)
- Acclimate rewilding group to outdoor enclosure for 2 weeks
- Infect approximately half of each group with 200 embryonated Trichuris muris eggs
- Return infected mice to their respective environments for 3 weeks
- Collect peripheral blood mononuclear cells (PBMCs) for spectral cytometry analysis
- Perform complete blood count with differential (CBC/DIFF) at 2 and 5 weeks post-rewilding
- Analyze worm burden and immune parameters
Analytical Methods:
- Multivariate distance matrix regression (MDMR) to quantify contributions of genotype, environment, and infection to immune variation
- Principal component analysis (PCA) on PBMC cellular composition data
- k-means clustering for unbiased immune cell population identification
Key Findings:
- Cellular composition was shaped by interactions between genotype and environment
- Cytokine response heterogeneity, particularly IFNγ concentrations, was primarily driven by genotype with consequences for worm burden
- Genetic differences observed under laboratory conditions were decreased following rewilding
- CD44 expression on T cells was explained mostly by genetics, while on B cells was explained more by environment [6]
Diagram 1: Rewilded Mouse Experimental Paradigm. This workflow illustrates the interactive effects of genotype, environment, and infection on immune phenotypes and functional outcomes in the rewilded mouse model.
Polyexposure Scoring: Quantifying Environmental Risk
The development of polyexposure scores represents a significant advancement in quantifying cumulative environmental risk, analogous to polygenic risk scores in genetics. Recent research from the Personalized Environment and Genes Study (PEGS) demonstrates that polyexposure scores often outperform polygenic scores in predicting chronic disease development [20].
In one analysis, researchers computed three complementary risk scores:
- Polygenic score: Combined genetic risk based on 3,000 genetic traits
- Polyexposure score: Combined environmental risk from modifiable exposures (occupational hazards, lifestyle choices, stress)
- Polysocial score: Combined social risk from factors like socioeconomic status and housing
Notably, for conditions like type 2 diabetes, environmental and social risk scores demonstrated superior predictive performance compared to genetic risk scores alone [20]. This approach highlights the importance of integrating comprehensive environmental exposure data alongside genetic information for accurate disease risk prediction.
Research Toolkit: Essential Reagents and Methodologies
Table 3: Research Reagent Solutions for Gene-Environment Interaction Studies
| Reagent/Method | Function/Application | Technical Specifications | Key References |
|---|---|---|---|
| High-Resolution Metabolomics | Simultaneous measurement of up to 1,000 chemicals | LC-MS/MS platforms, computational analysis of metabolic pathways | [17] |
| Epigenetic Clock Assays | Assessment of biological aging and exposure memory | Bisulfite sequencing for DNA methylation analysis at age-related CpG sites | [17] |
| Spectral Cytometry Panels | High-dimensional immune phenotyping | 30+ parameter flow cytometry, automated population discovery | [6] |
| Extracellular Vesicle Isolation Kits | Non-invasive tissue-specific biomarker analysis | Immunoaffinity capture of neuron-, lung-, or liver-derived vesicles | [17] |
| GWAS/EWAS Arrays | Genome-wide and epigenome-wide association studies | Microarray or sequencing-based genotyping/methylation profiling | [15] |
| MARIO Computational Pipeline | Identification of allele-dependent binding of regulatory proteins | Analysis of allelic imbalance in ChIP-seq and other functional genomics data | [15] |
Signalling Pathways in Gene-Environment Interactions
IL-2 Receptor Signalling Dysregulation in Autoimmunity
The IL-2 receptor signalling pathway represents a critical convergence point for genetic and environmental influences on immune tolerance. Recent research has identified a novel mechanism in which environmental triggers exacerbate intrinsic Treg defects in genetically susceptible individuals, leading to autoimmune pathogenesis [19].
In healthy Tregs, IL-2 binding activates the JAK-STAT pathway through phosphorylation of JAK1 and JAK3, leading to STAT5 activation and nuclear translocation. This signalling is regulated by a negative feedback mechanism involving GRAIL (Gene Related to Anergy in Lymphocytes), an E3 ubiquitin ligase that inhibits cullin RING ligase activation and prevents aberrant degradation of signalling components [19].
In autoimmune patients, diminished GRAIL expression results in accelerated degradation of phosphorylated JAK1 and DEPTOR (an mTOR inhibitor), leading to compromised IL-2R signal durability despite normal surface receptor expression. This signalling defect impairs Treg suppressive function without necessarily reducing Treg frequency [19].
Diagram 2: IL-2 Receptor Signaling Dysregulation. This pathway illustrates how reduced GRAIL expression in autoimmune disease leads to compromised Treg function through accelerated degradation of signaling components.
Epigenetic Dysregulation by Environmental Exposures
Environmental exposures can initiate epigenetic modifications through several well-characterized molecular pathways. Chemical exposures such as benzene, toluene, and diesel exhaust have been associated with oxidative stress, leading to DNA damage and mutations in germ cells that can affect offspring neurodevelopment [22].
Specific mechanisms include:
- DNA methyltransferase inhibition: Chemicals like procainamide directly inhibit DNMT enzymes, leading to global DNA hypomethylation [18]
- Histone modification alterations: Pesticides like dieldrin have been shown to increase histone acetylation, promoting apoptosis in dopaminergic neurons [18]
- MicroRNA dysregulation: Air pollution components can alter miRNA expression profiles, affecting immune gene regulation [22]
These epigenetic changes create persistent alterations in gene expression patterns that can predispose to autoimmune, neurodevelopmental, and metabolic disorders, often in a tissue-specific manner that reflects the route and timing of exposure.
Translational Applications and Future Directions
Precision Environmental Health and Therapeutic Development
The Convergence Model provides a robust framework for developing targeted therapeutic interventions. One promising approach involves neddylation activating enzyme inhibitors (NAEis) conjugated to IL-2 or anti-CD25 antibodies to selectively restore Treg function in autoimmune patients [19]. This strategy addresses the core immune dysregulation without inducing systemic immunosuppression.
The emerging field of precision environmental health (PEH) aims to integrate genetic, epigenetic, and exposure data to develop personalized prevention strategies. PEH encompasses three major knowledge domains: environmental exposures, genetics (including epigenetics), and data science [17]. This approach represents a cultural shift from reactive "disease care" to proactive health preservation by identifying at-risk individuals before disease manifestation.
Epigenetic biomarkers show particular promise for early detection and intervention. Research has demonstrated that epigenetic signatures can accurately predict prenatal exposure to environmental toxicants like tobacco smoke years after the actual exposure occurred [22]. Similar approaches are being developed for air pollution, PFAS, and other chemical exposures, potentially enabling targeted screening of high-risk children for pollution-related conditions like asthma.
Research Gaps and Methodological Challenges
Despite significant advances, substantial challenges remain in fully elucidating gene-environment interactions. Key research gaps include:
- Exposure assessment complexity: The vast scope of the exposome, encompassing exposures from conception onward, creates measurement challenges [17]
- Temporal dynamics: The timing of exposures, particularly during critical developmental windows, significantly influences their biological impact [22]
- Multi-omics integration: Synthesizing data from genome, epigenome, metabolome, and proteome requires advanced computational approaches [22]
- Ancestral diversity: Current datasets are disproportionately focused on European-ancestry populations, limiting generalizability [15]
Future research directions should prioritize the development of novel computational methods, including artificial intelligence approaches, to integrate multi-omics data and identify critical exposure thresholds. Additionally, expanding diverse population studies and longitudinal birth cohorts will be essential for capturing the full spectrum of gene-environment interactions across the lifespan.
The Convergence Model provides a comprehensive framework for understanding how genetic predisposition and environmental factors interact to drive disease pathogenesis. Through epigenetic mechanisms, immune system modulation, and complex signalling pathway alterations, these interactions create distinct biological trajectories that influence disease risk and progression.
The methodological advances detailed in this review—from rewilded animal models to polyexposure scoring and epigenetic fingerprinting—provide researchers and drug development professionals with powerful tools to investigate these interactions. The translation of these findings into precision environmental health approaches holds exceptional promise for revolutionizing disease prevention and developing targeted therapies that address the fundamental convergence of genetic and environmental factors in human disease.
As the field advances, integrating comprehensive environmental exposure assessment with deep molecular phenotyping will be essential for unlocking the full potential of the Convergence Model to improve human health and mitigate disease risk across diverse populations.
The immune system demonstrates profound sexual dimorphism, influencing health, disease, and therapeutic outcomes across the lifespan. Understanding sex as a biological variable (SABV) is no longer optional but essential for rigorous immunological research and the development of precision medicine. Sex-based disparities in immune function are evident in the higher prevalence of autoimmune diseases in females and the increased susceptibility to severe infections and many cancers in males [23]. These differences arise from a complex interplay of genetic determinants, primarily the sex chromosomes, and endocrine factors, notably sex hormones, which collectively shape immune cell composition, function, and aging trajectories [23] [24]. Framing this within the broader context of genetics and environment, this whitepaper synthesizes current evidence on the chromosomal and hormonal mechanisms driving immune variation, providing researchers with a technical guide and methodological toolkit for integrating SABV into immunology research and drug development.
Fundamental Mechanisms of Sexual Dimorphism
The foundations of immune sex differences are established by two core biological systems: the sex chromosomes, which provide a genetic blueprint, and the sex hormones, which exert dynamic regulatory control. These systems act both independently and through complex crosstalk.
Chromosomal Influences
The sex chromosomes confer genetic differences that are present from conception and operate in every nucleated cell, including those of the immune system.
- X-Chromosome Gene Dosage and Inactivation Escape: The X chromosome is enriched for immune-related genes. To achieve dosage compensation between females (XX) and males (XY), one X chromosome is randomly inactivated in female somatic cells through an epigenetic process mediated by XIST (X-inactive specific transcript) [23]. However, approximately 15-25% of X-chromosome genes escape this inactivation, leading to their biallelic expression and higher expression levels in females [25] [23]. This double dose of immune-relevant escape genes, such as TLR7 (a pattern-recognition receptor critical for viral RNA sensing), provides females with a more robust innate immune detection system and contributes to a stronger antibody response [25]. The reactivation of X-linked genes can also occur in specific immune cell types, such as activated B and T cells, further amplifying sex differences in adaptive immunity [23].
- Y-Chromosome and Immune Function: The Y chromosome, once considered a genetic wasteland, is now known to influence immunity. The loss of the Y chromosome (LOY) in a subset of immune cells, particularly hematopoietic cells, is a common age-related mosaic event in men [23]. LOY is associated with altered immune cell function, increased risk of cancer, cardiovascular disease, and a shortened lifespan, suggesting a role for Y-linked genes in maintaining immune homeostasis and health in aging males [23].
Hormonal Regulation
Sex hormones, including estrogens, androgens, and progesterone, exert widespread effects on immune cell development, differentiation, and effector functions via genomic and non-genomic signaling pathways.
- Estrogen Signaling: Estrogens, primarily 17β-estradiol, generally enhance both innate and adaptive immunity. Signaling occurs through classical nuclear estrogen receptors (ERα and ERβ), which act as transcription factors, or through membrane-bound G protein-coupled estrogen receptors (GPER) for rapid non-genomic effects [26]. Estrogen enhances neutrophil activation, antigen presentation by dendritic cells, and the cytolytic function of NK cells [25] [26]. It also promotes B cell development and antibody production by directly activating the expression of Activation-Induced Cytidine Deaminase (AID), a key enzyme for antibody class-switch recombination and somatic hypermutation [26]. Furthermore, estrogen can expand the CD4+CD25+ regulatory T cell (Treg) compartment, illustrating its role in immune modulation [26].
- Androgen Signaling: Androgens, such as testosterone, typically have immunosuppressive effects [26]. Androgen receptor (AR) signaling can dampen inflammatory responses by reducing the production of pro-inflammatory cytokines and promoting anti-inflammatory profiles [26]. In the context of cancer, the AR fosters an immunosuppressive tumor microenvironment, and AR blockade in prostate cancer can reinvigorate antitumor T cell responses [26].
The following diagram illustrates the core mechanisms through which chromosomes and hormones influence immune cell function.
Quantitative Evidence of Sex Differences in Immunity
Empirical data from human studies robustly document sex differences in immune cell proportions and molecular profiles. These differences are present in early life and evolve across the lifespan.
Immune Cell Proportions
Longitudinal pediatric studies leveraging DNA methylation (DNAm)-based computational cell type deconvolution reveal that significant sex differences in immune cell composition are established before puberty. Research on whole blood samples from children at ages one and five shows dynamic changes in all immune cell types during early development, with notable sex-associated differences [27].
Table 1: Sex-Associated Differences in Immune Cell Proportions in Early Life (Ages 1 and 5)
| Immune Cell Type | Sex-Bias | Developmental Window | Notes |
|---|---|---|---|
| Basophils | Significantly different | Ages 1 & 5 | Consistent difference across early childhood [27] |
| CD4+ Memory T cells | Significantly different | Ages 1 & 5 | Consistent difference across early childhood [27] |
| T Regulatory Cells (Tregs) | Significantly different | Ages 1 & 5 | Consistent difference across early childhood [27] |
| Monocytes | Male-biased | By age 5 | Higher proportion in males emerges by age 5 [27] |
| CD8+ Naive T cells | Female-biased | By age 5 | Higher proportion in females emerges by age 5 [27] |
In adulthood, hormonal influences become more pronounced. A study analyzing blood samples from a cross-sectional cohort including cisgender, transgender, and post-menopausal individuals found that class-switched memory B cells—critical for high-affinity, long-lived antibody responses—are present at higher levels in cisgender females compared to cisgender males only between puberty and menopause [28]. This difference was dependent on both oestrogen and an XX chromosomal background, as it was not observed in transgender females (XY) taking estrogen, but was reduced in transgender males (XX) undergoing estrogen-blocking therapy [28].
Epigenetic and Molecular Signatures
Epigenetic mechanisms, particularly DNA methylation (DNAm), provide a molecular footprint of immune system maturation and sexual dimorphism. Analysis of over 4,900 CpG sites across 628 immune system candidate genes in pediatric cohorts identified distinct sex-associated DNAm signatures that were consistent between ages one and five, indicating stable early-life programming independent of pubertal hormones [27]. While age-related DNAm changes were relatively limited in this window, sex-associated differences were more prominent and partially validated in independent cohorts [27]. This suggests that the epigenetic landscape of the immune system is shaped by sex from a very young age, potentially setting the stage for lifelong differences in immune function and disease risk.
Research Methodologies and Experimental Protocols
To rigorously study sex differences in immunology, researchers require robust, reproducible methodologies. Below are detailed protocols for key approaches cited in this field.
DNA Methylation Analysis for Immune Profiling
This protocol allows for the simultaneous assessment of immune cell proportions and epigenetic age- or sex-associated signatures from whole blood [27].
Table 2: Key Research Reagents for Immune Cell Deconvolution & Epigenetics
| Research Reagent | Function/Application |
|---|---|
| Whole Blood Sample | Source of genomic DNA for methylation profiling and cellular analysis. |
| Bisulfite Conversion Kit | Chemically modifies unmethylated cytosines to uracils, allowing for methylation status determination. |
| Infinium MethylationEPIC BeadChip | Microarray platform for high-throughput genotyping of over 850,000 CpG methylation sites across the genome. |
| DNA Methylation Deconvolution Algorithms | Computational tools that use reference methylation signatures to estimate proportions of specific immune cell types from heterogeneous tissue data. |
| Robust Linear Regression Models | Statistical method used to identify CpG sites whose methylation status is significantly associated with sex or age, resistant to outliers. |
Experimental Workflow:
- Sample Collection & DNA Extraction: Collect peripheral whole blood in EDTA or citrate tubes. Extract high-molecular-weight genomic DNA using a standardized kit. Quantify DNA purity and concentration via spectrophotometry.
- Bisulfite Conversion: Treat 500 ng of genomic DNA with sodium bisulfite using a commercial kit. This step deaminates unmethylated cytosine residues to uracil, while methylated cytosines remain unchanged.
- Whole Genome Amplification & Hybridization: Amplify the bisulfite-converted DNA and fragment it enzymatically. The fragmented DNA is hybridized to the Infinium MethylationEPIC BeadChip, which contains probe sequences designed to distinguish between methylated and unmethylated alleles.
- Scanning & Data Preprocessing: Scan the BeadChip to fluorescence intensities. Preprocess the raw data using R/Bioconductor packages (e.g.,
minfi) for background correction, dye-bias normalization, and calculation of beta-values (β = methylated signal / (methylated + unmethylated signal)). β-values range from 0 (completely unmethylated) to 1 (fully methylated). - Cell Type Deconvolution: Input the normalized β-values into a DNAm deconvolution algorithm (e.g.,
HousemanorEpiDISH). The algorithm uses a pre-established reference matrix of cell-specific methylation marks to estimate the relative proportion of various immune cell types (e.g., neutrophils, B cells, T cell subsets, monocytes) in each sample. - Differential Methylation Analysis: To identify sex-associated DNAm signatures, model the β-value of each CpG site as the dependent variable in a robust linear regression, with sex as the independent variable. Correct for multiple testing using False Discovery Rate (FDR). Apply a threshold (e.g., FDR < 0.05 and |Δβ| > 0.03) to identify statistically and biologically significant sites.
Isolating Chromosomal vs. Hormonal Effects
The "Four Core Genotypes" (FCG) mouse model is a powerful tool to dissect the independent contributions of chromosomes (XX vs. XY) and gonads (ovaries vs. testes) to a phenotype [24].
Experimental Model:
- The FCG model is generated by translocating the testis-determining gene Sry from the Y chromosome to an autosome. This results in four distinct genotypes:
- XX with Ovaries (typical female)
- XY with Ovaries
- XX with Testes
- XY with Testes (typical male)
Workflow for Immune Profiling:
- Model Generation & Validation: Genotype mice to confirm XX or XY karyotype in the absence of the Sry gene on the Y chromosome. Verify gonad type (ovary or testis) by histology or hormone level measurement (e.g., plasma estradiol, testosterone).
- Immune Challenge or Baseline Analysis: Subject mice from all four groups to an immune challenge (e.g., viral infection, vaccination, or tumor implantation) or analyze their immune systems at baseline.
- Outcome Measurement: Collect relevant tissues (blood, spleen, lymph nodes). Analyze using flow cytometry (for immune cell populations), ELISA or Luminex (for cytokine/antibody levels), and/or functional assays (e.g., T cell killing, phagocytosis).
- Statistical Modeling: Use a 2x2 factorial design to test the main effects of Chromosome Type (XX vs. XY) and Gonad Type (Ovary vs. Testis), and their interaction, on the immune outcome of interest. A significant effect of chromosome, independent of gonad type, indicates a direct genetic contribution.
The following diagram maps this experimental strategy.
Clinical and Therapeutic Implications
The documented sex differences in immunity have significant consequences for disease susceptibility, treatment efficacy, and the future of precision medicine.
Disease Susceptibility and Vaccine Responses
The female immune advantage manifests as stronger responses to vaccination and greater resistance to many viral and bacterial infections [25]. However, this heightened immune reactivity comes at the cost of a 3- to 4-fold higher risk of developing autoimmune diseases like systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) [25] [23]. Conversely, males exhibit a higher incidence and mortality for many non-reproductive cancers, a disparity influenced by both immunosuppressive androgenic environments and sex chromosome effects [23] [26].
Cancer Immunotherapy
Sex is a significant predictor of response to immune checkpoint inhibitors (ICIs). Meta-analyses of clinical trials have shown that the survival benefit from anti-CTLA-4 or anti-PD-(L)1 monotherapy is generally greater for men across various solid tumors [26]. This appears context-dependent, however, as women may derive greater benefit from combinations of chemotherapy with anti-PD-(L)1 in non-small cell lung cancer [26]. The androgen receptor (AR) is recognized as a key driver of an immunosuppressive tumor microenvironment, making it a promising therapeutic target. Preclinical and early clinical evidence suggests that AR blockade can synergize with ICIs, enhancing antitumor T cell responses and improving outcomes [26].
The integration of SABV into immunological research is critical for advancing science and health equity. Future efforts must focus on:
- Elucidating Mechanisms: Deepening our understanding of how XCI escape genes and LOY precisely alter specific immune cell functions at the molecular level.
- Lifespan Studies: Conducting longitudinal studies that capture immune variation across all life stages, from infancy to advanced age, and during key hormonal transitions like puberty, pregnancy, and menopause [24].
- Inclusive Study Designs: Moving beyond the male-default and intentionally including both sexes in preclinical and clinical research, with appropriate statistical power to analyze sex-specific outcomes [24].
- Global Immune Profiling: Large-scale initiatives like the Human Immunome Project aim to generate the largest immunological dataset ever created, mapping global immune variation. This will powerfully enable the identification of sex-specific immune signatures and the development of predictive models for precision medicine [29].
In conclusion, sex is a fundamental biological variable that exerts a profound influence on the immune system through interconnected chromosomal and hormonal pathways. Acknowledging and systematically investigating these differences is not merely a box-ticking exercise but a scientific imperative. It is the key to unlocking a deeper understanding of immune function, developing more effective and personalized therapeutics, and ultimately improving health outcomes for all.
The relative contributions of genetic inheritance and environmental exposure to phenotypic variation represent a foundational question in biology, often simplified as the "nature versus nurture" debate [30]. In the specific field of immunology, resolving this question is critical for understanding the vast inter-individual heterogeneity in immune responses observed in health, disease, and following interventions such as vaccination [31] [32]. Framed within a broader thesis on the determinants of immune variation, this whitepaper synthesizes insights from key twin and population studies to provide a technical guide on the methodologies, findings, and implications of quantifying heritable and non-heritable influences on the immune system. Accurate quantification is not merely an academic exercise; it holds profound consequences for identifying disease risk, predicting therapeutic outcomes, and guiding the development of novel immunomodulatory drugs [6] [7].
Core Concepts and Definitions of Heritability
Heritability is formally defined as the proportion of observed phenotypic variation (VP) in a population that is attributable to genetic variation [30] [33]. It is crucial to recognize that heritability is a population-level statistic, not an individual-level measure, and its value can change depending on the population and environment studied [30].
- Narrow-Sense Heritability (h²): This estimates the proportion of phenotypic variance explained solely by additive genetic effects (VA), where the effects of different alleles add up linearly. It is defined as h² = VA/VP. This is the most relevant metric for predicting the response to natural or artificial selection and is the parameter typically estimated in genomic studies [30] [33].
- Broad-Sense Heritability (H²): This estimates the proportion of phenotypic variance explained by total genetic variance (VG), which includes additive, dominant, and epistatic (gene-gene interaction) effects. It is defined as H² = VG/VP [30] [33].
A common misconception is that a heritability of 80% for a trait means that 80% of an individual's phenotype is determined by genes and 20% by environment. The correct interpretation is that within the studied population, 80% of the variation in the trait is associated with genetic differences between individuals [30].
Key Methodologies for Estimating Heritability
Several experimental and statistical approaches are employed to disentangle genetic and environmental influences, each with distinct strengths, limitations, and underlying assumptions.
Family-Based Designs
- Classic Twin Study (ACE Model): This is a cornerstone design. It compares phenotypic similarity between monozygotic (MZ) twins, who share nearly 100% of their DNA, and dizygotic (DZ) twins, who share approximately 50% on average. The model partitions variance into:
- A (Additive genetic factors): Inferred if MZ twin correlation is greater than DZ twin correlation.
- C (Common/Shared environment): Inferred if MZ and DZ twins show similar correlations.
- E (Unique/Non-shared environment): Inferred from the extent to which MZ twins are dissimilar. A critical assumption is the Equal Environment Assumption (EEA), which posits that MZ and DZ twins experience equally similar environments [33]. Violations of this assumption can inflate heritability estimates [34] [33].
- Sibling Regression (SR): This method uses the genetic similarity of full siblings (who also share ~50% of their DNA) but relies on within-family variation, making it less susceptible to confounding from population stratification. However, it can be biased by sibling-specific environmental effects and captures some gene-gene and gene-environment interactions [34] [33].
Genomic Designs
- Genomic Relatedness Restricted Maximum-Likelihood (GREML): Used in Genome-Wide Complex Trait Analysis (GCTA), this method estimates the proportion of phenotypic variance explained by all common genetic variants measured on a genome-wide SNP array across unrelated individuals. It estimates narrow-sense heritability free from the assumptions of the twin design but can be confounded by environmental factors correlated with genetic relatedness [34] [33].
- Linkage Disequilibrium Score Regression (LDSR): This method uses summary statistics from Genome-Wide Association Studies (GWAS). It regresses SNP test statistics on their Linkage Disequilibrium (LD) scores. SNPs in high-LD regions tag more causal variants and thus have higher average test statistics. The slope of this regression estimates SNP heritability, and the intercept can detect confounding biases [33].
- Relatedness Disequilibrium Regression (RDR): A within-family method that leverages the random variation in genetic sharing between parents and offspring. It is considered highly robust as it is immune to environmental confounding and assortative mating, providing a clean estimate of narrow-sense heritability [34].
Table 1: Comparison of Key Heritability Estimation Methods
| Method | Study Design | Variance Components Estimated | Key Assumptions | Major Limitations |
|---|---|---|---|---|
| Classic Twin (ACE) | MZ vs. DZ twins | A, C, E | Equal environments for MZ/DZ twins (EEA); Random mating | EEA violation inflates estimates; Cannot model GxE well |
| Sibling Regression (SR) | Full siblings | Additive + some interactions | No systematic environmental differences between siblings | Sensitive to sibling-specific environments |
| GREML | Unrelated individuals | Additive (SNP-based) | No environmental correlation with genetic relatedness | Confounded by population stratification |
| LDSR | GWAS summary stats | Additive (SNP-based) | LD score uncorrelated with effect size | Less accurate with fewer SNPs |
| RDR | Parent-offspring trios | Additive (narrow-sense) | Random segregation of alleles | Requires genotyped trios; Lower power |
Quantitative Findings in Immune System Variation
Applying these methodologies has yielded a nuanced picture of the architecture of immune variation, revealing a system predominantly shaped by non-heritable factors but with critical genetic contributions.
Insights from Large-Scale Human Twin Studies
A seminal systems-level analysis of 210 healthy twins measured 204 immunological parameters, including cell population frequencies, cytokine responses, and serum proteins [31] [35].
Table 2: Summary of Heritability Findings from a Systems-Level Twin Study [31] [35]
| Immune Parameter Category | Key Findings | Examples of Highly Heritable Traits | Examples of Non-Heritable Dominated Traits |
|---|---|---|---|
| Cell Population Frequencies (72 subsets) | 61% of cell populations had undetectable heritable influence (<20%) [31]. | Naïve & central memory CD4+ T cells (CD27+) [31]. | Most innate (granulocytes, monocytes, NK-cells) and adaptive cells [31]. |
| Serum Proteins (43 cytokines, chemokines, growth factors) | Majority dominated by non-heritable influences; some notable exceptions [31]. | IL-12p40 (associated with IL12B gene variants) [31]. | IL-10 and a group of chemokines [31]. |
| Cellular Signaling Responses (65 induced responses) | 69% of signaling responses had no detectable heritable influence (<20%) [31]. | IL-2 and IL-7 induced STAT5 phosphorylation in T-cells (homeostatic) [31]. | IFN-induced STAT1 phosphorylation; IL-6/IL-21/IL-10 induced STAT3 phosphorylation [31]. |
| Overall Summary | 77% of all 204 parameters were dominated (>50% of variance) by non-heritable influences. 58% were almost completely determined (>80% of variance) by non-heritable influences [31] [35]. |
The study further found that variation in immune parameters between MZ twins increases with age, suggesting the cumulative effect of environmental exposures [31] [35]. Furthermore, a single non-heritable factor, such as cytomegalovirus (CMV) infection, can significantly alter over half of all measured immune parameters, underscoring the powerful and pervasive role of environment [31] [35].
The Role of Genotype-by-Environment (GxE) Interactions
Controlled animal studies provide direct evidence for GxE interactions, where the effect of a genotype depends on the environment and vice-versa. Research using "rewilded" mice—laboratory strains introduced into a natural outdoor environment—demonstrated that immune variation is often shaped by synergistic interactions between genetics and environment, not just their independent effects [6] [36].
Table 3: Key Findings from Rewilded Mouse Studies on GxE Interactions [6] [36]
| Aspect of Immune Variation | Finding | Interpretation |
|---|---|---|
| Cellular Composition | Shaped by significant interactions between genotype and environment (Gen x Env) [6]. | The impact of a mouse's strain on its immune cell profile depends on whether it lives in a lab or a natural environment. |
| Cytokine Responses | Primarily driven by genotype, with consequences for parasite burden [6]. | Genetic background is a major determinant of functional cytokine output upon challenge. |
| Marker Expression (e.g., CD44) | Expression on T cells was explained more by genetics, while on B cells it was explained more by environment [6]. | The relative influence of genes and environment can be cell-type-specific. |
| Emergence of Genetic Effects | A stronger Th1 response to Trichuris muris in C57BL/6 mice emerged only in the rewilding condition, not in the lab [6]. | Environmental context can reveal or mask genetic differences in immune responses. |
| Reduction of Genetic Effects | Genetic differences in CD44 expression on CD4+ T cells between strains, evident in the lab, were no longer present after rewilding [6]. | A shifting environment can erase genetically determined differences seen in controlled settings. |
Detailed Experimental Protocols
For researchers aiming to conduct similar investigations, below are detailed methodologies from landmark studies.
Systems Immunology in Human Twins
Objective: To perform a systems-level analysis partitioning variance in immune parameters into heritable and non-heritable components [31].
Workflow:
- Cohort Recruitment: Recruit healthy monozygotic (MZ) and dizygotic (DZ) twin pairs from a registered twin registry. (e.g., 210 twins, 78 MZ and 27 DZ pairs) [31].
- Blood Sampling & Processing: Collect peripheral blood with minimal time between sampling of each twin pair to reduce diurnal variation. Process samples immediately for serum and peripheral blood mononuclear cells (PBMCs) [31].
- High-Dimensional Immune Monitoring:
- Cell Population Frequencies: Use high-dimensional flow cytometry (e.g., 15-color) with antibody panels against cell surface markers to quantify 95+ immune cell subsets.
- Serum Protein Measurement: Use multiplexed immunoassays (e.g., Luminex) to quantify concentrations of 51+ cytokines, chemokines, and growth factors.
- Cellular Signaling Responses: Stimulate PBMCs with cytokines (e.g., IL-2, IL-6, IL-10, IFNs) and measure phosphorylation of transcription factors (STAT1, STAT3, STAT5) via phospho-flow cytometry [31].
- Data Processing & Quality Control:
- Subtract technical variance estimated from repeated measurements of a control sample from the total variance.
- Correct all measurements for the effects of age and gender by regressing out these effects and using residual variance for heritability estimation [31].
- Variance Component Analysis:
- Apply a structural equation model (e.g., ACE model) to partition the variance for each measured parameter into:
- A (Heritable): Genetic factors.
- C (Shared environment): Common non-heritable factors.
- E (Unique environment): Unique non-heritable factors plus error.
- Estimate heritability by comparing the observed covariance matrices of MZ and DZ twins [31].
- Apply a structural equation model (e.g., ACE model) to partition the variance for each measured parameter into:
Diagram 1: Twin Study Workflow
Rewilding Mouse Studies for GxE Interaction
Objective: To quantify the interactive effects of genotype and environment on immune phenotypes and infection outcome in a controlled yet naturalistic setting [6] [36].
Workflow:
- Strain Selection: Select genetically diverse inbred mouse strains (e.g., C57BL/6, 129S1, PWK/PhJ) to represent wide genetic variation [6] [36].
- Environmental Assignment: Randomly assign mice from each strain to two environments:
- Perturbation and Sampling:
- Immune Phenotyping:
- Cell Composition: Analyze immune cells via complete blood count (CBC) with differential and high-dimensional spectral cytometry of PBMCs and MLN cells.
- Functional Assays: Measure plasma cytokines and antigen-stimulated cytokine release from MLN cells.
- Single-Cell RNA Sequencing (scRNA-seq): Perform on MLN cells to simultaneously capture cell composition and functional state [6] [36].
- Outcome Measurement: Quantify worm burden to assess susceptibility to infection [6] [36].
- Statistical Analysis:
Diagram 2: Rewilding Mouse Study Design
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and technologies essential for executing the experiments described in this whitepaper.
Table 4: Essential Research Reagents and Technologies
| Reagent / Technology | Function in Experimental Protocol | Specific Examples from Research |
|---|---|---|
| High-Parameter Flow Cytometry | Simultaneous identification and quantification of dozens of immune cell subsets based on surface and intracellular protein markers. | 15-color flow panels to define 126+ immune cell subpopulations [32]; Spectral cytometry for deep immunophenotyping [6] [36]. |
| Phospho-Specific Flow Cytometry | Measurement of intracellular phosphorylation states of signaling proteins (e.g., STATs) in single cells, revealing immediate functional responses to stimuli. | Used to quantify STAT1, STAT3, and STAT5 phosphorylation in response to cytokine stimulation [31]. |
| Multiplex Immunoassays | High-throughput quantification of multiple soluble proteins (e.g., cytokines, chemokines) from a single small-volume sample (e.g., serum, supernatant). | Luminex-based assays to measure 51+ serum cytokines and chemokines [31]. |
| Single-Cell RNA Sequencing (scRNA-seq) | Comprehensive profiling of gene expression at single-cell resolution, enabling unbiased identification of cell types, states, and functional pathways. | Used on mesenteric lymph node cells from rewilded mice to link cellular composition and function to genotype and environment [6] [36]. |
| Signal Transduction Pathway Activity Profiling | Computational tool (e.g., STAP-STP) that uses mRNA data to infer quantitative activity scores of multiple signaling pathways (e.g., NF-κB, JAK-STAT, TGFβ). | Used to define pathway activity profiles (SAPs) for immune cells in resting and activated states [37]. |
| Genome-Wide SNP Arrays | Genotyping of hundreds of thousands to millions of single nucleotide polymorphisms (SNPs) across the genome for heritability analysis (GREML, LDSR) and GWAS. | Foundation for genomic heritability estimation methods in biobank-scale studies [34] [33]. |
The collective evidence from twin studies, genomic analyses, and controlled animal models presents a consistent narrative: the human immune system is a highly dynamic entity where non-heritable influences are the dominant source of variation across most measurable parameters [31] [35]. This underscores the profoundly reactive and adaptive nature of immunity, shaped by a lifetime of exposures to pathogens, vaccines, the microbiome, and other environmental factors. However, genetic factors provide a critical underlying framework, setting broad constraints and determining specific, context-dependent responses, particularly evident in genotype-by-environment interactions [6] [7].
For researchers and drug development professionals, these findings have immediate implications. The low heritability of many immune traits suggests that personalized immunology and predictive models of vaccine response or disease susceptibility may be more fruitfully advanced by integrating deep environmental and exposure data alongside genetic data [32]. Furthermore, the pervasive role of GxE interactions indicates that the efficacy and safety of immunomodulatory therapies may vary significantly across different populations and environments. Moving forward, study designs must evolve to systematically capture and account for these interactions, employing the sophisticated methodologies detailed in this guide to fully elucidate the complex interplay of genes and environment that defines an individual's immune identity.
From Data to Drugs: Methodological Approaches for Target Identification and Validation
Leveraging Genome-Wide Association Studies (GWAS) to Map Immune Trait Loci
The heritable components of immune-mediated diseases and traits have been successfully mapped through genome-wide association studies (GWAS), which enable the systematic identification of genetic variants associated with polygenic inheritance patterns. Unlike Mendelian disorders caused by high-penetrance variants in single genes, most immune traits involve myriad low-penetrance genetic variants that collectively contribute substantial heritable susceptibility [38]. The remarkable growth of GWAS has led to the identification of hundreds of thousands of genotype-phenotype associations, creating both unprecedented opportunities and significant challenges for translating these findings into biological mechanisms and therapeutic interventions [38] [39].
Understanding the genetic basis of immune traits requires consideration of both genetic and environmental factors that shape immune response variation. Environmental exposures, including pathogens, vaccines, and the microbiome, interact with genetic predispositions to determine ultimate disease outcomes. This complex interplay is particularly evident in the context of trained immunity, where innate immune cells develop memory-like characteristics through epigenetic reprogramming following environmental triggers such as vaccination or infection [40]. The integration of GWAS with functional genomic datasets now enables researchers to move beyond simple association signals to elucidate the molecular pathways through which genetic variants influence immune function in specific physiological contexts.
Core Principles of GWAS in Immune Trait Mapping
Fundamental Methodology and Analytical Framework
GWAS operates as an agnostic experimental design that detects genotype-phenotype associations by comparing allele frequencies of genetic variants across the whole genomes of many individuals. The standard analytical procedure begins with DNA sample collection and genotyping, typically using SNP microarrays or sequencing technologies [38]. Following quality control measures to exclude variants with poor genotyping quality or deviations from Hardy-Weinberg equilibrium, genotype imputation computationally infers untyped variants using haplotype reference panels [38]. Association testing employs regression-based methods that account for covariates such as population stratification, age, and sex, with meta-analysis boosting statistical power when multiple datasets are available [38].
A critical concept for interpreting GWAS results is linkage disequilibrium (LD), the non-random association of alleles at different loci. LD reflects the evolutionary history of recombination events and enables GWAS to comprehensively assess genetic variation without directly genotyping every possible variant [38]. However, LD also complicates the identification of causal variants, as association signals often span multiple correlated variants within a genomic region. Consequently, the variant with the strongest association signal (the "lead variant") may not be the causal variant itself but rather in LD with the true functional variant [38].
Distinct Patterns of Genetic Sharing Across Immune Diseases
Cross-disorder genetic analyses have revealed that immune diseases cluster into distinct groups with specific genetic architectures. Genomic structural equation modeling of nine immune-mediated diseases identified three primary groupings: gastrointestinal tract diseases (Crohn's disease, ulcerative colitis, primary sclerosing cholangitis), rheumatic and systemic diseases (rheumatoid arthritis, systemic lupus erythematosus, juvenile idiopathic arthritis, type 1 diabetes), and allergic diseases (asthma, eczema) [41]. Each group demonstrates unique genetic associations with minimal overlap between them, suggesting distinct etiological pathways despite converging on similar immune processes [41].
Table 1: Immune Disease Groupings Based on Genetic Correlation Analysis
| Disease Group | Specific Diseases | Key Genetic Features |
|---|---|---|
| Gastrointestinal | Crohn's disease, ulcerative colitis, primary sclerosing cholangitis | 67 specific genomic regions; enriched for STAT3 associations |
| Rheumatic/Systemic | Rheumatoid arthritis, systemic lupus erythematosus, juvenile idiopathic arthritis, type 1 diabetes | 60 specific genomic regions; enriched for STAT4 associations |
| Allergic | Asthma, eczema | 67 specific genomic regions; enriched for STAT5A/STAT6 associations |
Notably, while these disease groups exhibit distinct genetic associations, they converge on perturbing the same pathways, particularly T cell activation and signaling, JAK-STAT signaling, and cytokine production [41]. This pattern suggests that different constellations of genetic variants can disrupt common immune pathways, resulting in distinct clinical manifestations based on the specific genes affected and potentially their interactions with environmental factors.
Advanced Analytical Frameworks for GWAS Integration
Molecular Quantitative Trait Loci (molQTL) Mapping
The majority (>90%) of disease-associated variants identified by GWAS reside in non-coding genomic regions, making functional interpretation challenging [38] [39]. Molecular quantitative trait loci (molQTL) mapping addresses this limitation by identifying genetic variants associated with intermediate molecular phenotypes. Different molQTL types capture distinct layers of gene regulation:
- Expression QTLs (eQTLs): Variants associated with gene expression levels [38]
- Splicing QTLs: Variants associated with alternative splicing patterns [38]
- Protein QTLs (pQTLs): Variants associated with protein abundance [38]
- Chromatin accessibility QTLs: Variants associated with open chromatin regions [38]
When a disease-associated variant also functions as a molQTL, it suggests that the genetic predisposition may be mediated through regulation of molecular phenotypes [38]. However, linkage disequilibrium can create spurious associations between distinct causal variants for GWAS signals and molQTL effects. Colocalization analyses address this concern by evaluating the probability that the same underlying causal variant explains both association signals [38].
Transcriptome-Wide Association Studies (TWAS)
TWAS provides a powerful framework for prioritizing candidate causal genes by integrating genotype effects on gene expression with disease susceptibility [38] [42]. This approach trains gene expression prediction models using reference samples with both genotype and gene expression data, then applies these models to GWAS data to test associations between genetically predicted gene expression and disease risk [38]. TWAS offers several advantages over standard GWAS, including reduced multiple testing burden (by testing only genes with significant genetic regulation) and direct implication of specific genes in disease pathogenesis [38].
Recent applications of TWAS have revealed novel insights into immune-related traits. For example, integrating TWAS with single-cell RNA sequencing (scRNA-seq) in severe influenza-like illness identified cell-type-specific gene expression associations, with CD16+ monocytes, proliferating cells, and conventional dendritic cells showing the most differentially expressed genes [42]. Similarly, TWAS applications in COVID-19 severity have identified potential target genes involved in inflammation signaling (CARM1), endothelial dysfunction (INTS12), and antiviral immune response (RAVER1) [43].
Single-Cell QTL Mapping in Immune Contexts
The emergence of single-cell sequencing technologies has enabled the resolution of cell-type-specific genetic effects within complex tissues. Single-cell eQTL (sc-eQTL) mapping from peripheral blood mononuclear cells (PBMCs) has revealed that genetic effects on gene expression are often restricted to specific immune cell subsets [40]. Furthermore, these genetic effects can be context-dependent, varying across different stimulation conditions or immune states [40].
A recent study mapping sc-eQTLs across multiple conditions (baseline, lipopolysaccharide challenge, before/after BCG vaccination) identified a monocyte eQTL for LCP1 that contributes to inter-individual variation in trained immunity [40]. The same study elucidated genetic and epigenetic regulatory networks of CD55 and SLFN5, with the latter playing potential roles in COVID-19 pathogenesis through virus replication restriction [40]. These findings highlight the importance of studying genetic regulation in disease-relevant cell types and conditions rather than relying solely on baseline measurements from easily accessible tissues like blood.
Table 2: Analytical Methods for Advanced GWAS Interpretation
| Method | Primary Application | Key Advantages | Limitations |
|---|---|---|---|
| molQTL mapping | Functional characterization of non-coding variants | Identifies molecular mechanisms; multiple molecular layers | LD can cause spurious associations; requires colocalization |
| TWAS | Gene prioritization | Reduced multiple testing; direct gene implication | LD contamination; dependent on reference panel quality |
| sc-eQTL mapping | Cell-type-specific resolution | Reveals cellular context of genetic effects; identifies rare cell populations | Technical noise; limited sample sizes; computational complexity |
| Colocalization | Causal variant identification | Determines shared genetic basis for traits; improves causal inference | Sensitivity to LD structure; requires large sample sizes |
Experimental Validation of GWAS Findings
Systematic Validation Approaches for Non-coding Variants
The translation of GWAS associations into biological mechanisms requires experimental validation of putative causal variants and genes. A comprehensive systematic review examining the landscape of GWAS validation identified 309 experimentally validated non-coding GWAS variants regulating 252 genes across 130 human disease traits [39]. These validated variants operated through diverse regulatory mechanisms, with 70% functioning through cis-regulatory elements, 22% through promoters, and 8% through non-coding RNAs [39].
Researchers employed multiple experimental approaches to validate these variants, including:
- Gene expression assays (n = 272 studies)
- Transcription factor binding analyses (n = 175)
- Reporter assays (n = 171)
- In vivo models (n = 104)
- Genome editing (n = 96)
- Chromatin interaction studies (n = 33) [39]
This multifaceted experimental approach underscores the importance of using multiple complementary methods to establish causal relationships between non-coding variants and their target genes.
Protocol for Functional Validation of GWAS Loci
A robust workflow for experimental validation of immune trait GWAS loci should include the following key steps:
Variant Prioritization: Apply statistical fine-mapping approaches to identify putative causal variants within associated loci, integrating functional genomic annotations (e.g., chromatin accessibility, histone modifications) from disease-relevant immune cell types [39] [44].
In Vitro Functional Screening: Implement high-throughput reporter assays to assess the effects of prioritized variants on regulatory activity in appropriate immune cell lines (e.g., Jurkat T cells, THP-1 monocytes) under basal and stimulated conditions [39].
Genome Editing: Utilize CRISPR-Cas9 to introduce candidate causal variants into immune cell lines or primary cells, followed by assessment of molecular phenotypes (gene expression, protein abundance, chromatin accessibility) [39] [40].
Mechanistic Studies: Employ chromatin conformation capture (3C-based methods) to physically connect regulatory variants with their target gene promoters, particularly important for variants located in gene deserts or spanning large genomic distances [39].
Functional Consequences: Evaluate the impact of variant introduction or correction on immune cell functions relevant to the disease context, such as cytokine production, cell differentiation, proliferation, or signaling pathway activation [40].
This comprehensive approach ensures that statistical associations are translated into causally validated mechanisms with clear implications for understanding disease pathophysiology and identifying therapeutic targets.
Integration of Multi-Omics Data for Therapeutic Target Discovery
Mendelian Randomization and Colocalization for Causal Inference
Mendelian randomization (MR) uses genetic variants as instrumental variables to infer causal relationships between exposures (e.g., gene expression, protein abundance) and disease outcomes [45] [46]. When applied to immune traits, MR can identify causally relevant genes and proteins that may represent promising therapeutic targets. For example, a multi-omics MR analysis of immune-related bone diseases identified several potentially causal proteins, including HDGF, CCL19, and TNFRSF14 for rheumatoid arthritis; BTN1A1, EVI5, OGA, and TNFRSF14 for multiple sclerosis; and ICAM5, CCDC50, IL17RD, and UBLCP1 for psoriatic arthritis [45].
Bayesian colocalization provides complementary evidence by determining whether the same underlying causal variant explains both the molecular QTL signal and the GWAS association [45] [46]. In the aforementioned study, colocalization analyses provided strong support (H4 > 0.8) for several gene-disease associations, including HDGF with rheumatoid arthritis and BTN1A1 with multiple sclerosis [45]. This integration of MR and colocalization strengthens causal inference and provides greater confidence in nominating therapeutic targets.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Immune Trait GWAS
| Reagent/Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Genotyping platforms | SNP microarrays, whole-genome sequencing | Variant detection and genotyping | Initial GWAS discovery |
| eQTL reference panels | GTEx, DICE, OneK1K, 300BCG | Gene expression regulation mapping | TWAS, molQTL mapping |
| Immune cell isolation | PBMC isolation kits, cell sorting antibodies | Specific immune cell population isolation | Cell-type-specific QTL mapping |
| Immune stimulation reagents | LPS, BCG vaccine, cytokines | Immune cell perturbation | Context-specific QTL mapping |
| Genome editing tools | CRISPR-Cas9, base editors | Functional validation of candidate variants | Experimental validation studies |
| Single-cell multi-omics | 10x Genomics, CITE-seq | Combined transcriptome and surface protein profiling | sc-eQTL mapping, cellular phenotyping |
Visualizing Analytical Workflows and Signaling Pathways
Integrated GWAS to Function Workflow
GWAS Functional Integration Workflow: This diagram illustrates the sequential integration of GWAS findings with functional genomic approaches to identify and validate causal genes and variants.
Immune Cell Signaling Pathway Convergence
Immune Pathway Convergence: This diagram shows how distinct genetic associations across immune disease categories converge on common signaling pathways, particularly JAK-STAT signaling, T cell activation, and cytokine production.
The integration of GWAS with functional genomic datasets has fundamentally advanced our ability to map immune trait loci and elucidate their biological mechanisms. Rather than operating in isolation, genetic associations must be interpreted within the context of cellular environments and physiological states that shape their functional consequences. The convergence of distinct genetic associations on common immune pathways, particularly T cell activation and JAK-STAT signaling, reveals both the complexity and order underlying the genetic architecture of immune traits [41].
Future research directions will likely focus on several key areas: First, expanding single-cell multi-omics approaches across diverse immune cell types, stimulation conditions, and population cohorts will enhance our resolution of context-specific genetic effects [40]. Second, integrating environmental exposure data with genetic information will elucidate how non-genetic factors modify genetic risk for immune diseases. Third, developing functionally informed polygenic risk scores that incorporate molecular QTL information may improve disease prediction and risk stratification [44]. Finally, systematic functional validation of candidate genes using high-throughput genetic engineering approaches will accelerate the translation of genetic discoveries into novel therapeutic targets for immune-mediated diseases [39] [44].
The continued refinement of methods to leverage GWAS for mapping immune trait loci promises to deepen our understanding of immune system genetics while revealing new opportunities for therapeutic intervention in immune-mediated diseases.
Mendelian Randomization (MR) is a powerful analytical method in genetic epidemiology that uses genetic variants as instrumental variables to investigate causal relationships between modifiable exposures (such as biomarkers) and health outcomes. The approach serves as a natural experiment that mimics randomized controlled trials (RCTs) by leveraging the random assortment of genetic variants during meiosis, which occurs independently of confounding environmental factors [47] [48]. This methodological framework has gained substantial traction in recent years for investigating disease etiology and validating therapeutic targets, with over 6,500 MR studies published in 2024 alone [49].
The foundational principle of MR rests on Mendel's laws of inheritance, which ensure that genetic variants are randomly allocated at conception, approximately analogous to the random assignment of treatments in clinical trials [47] [50]. This random allocation minimizes confounding from environmental factors and prevents reverse causation, addressing key limitations of conventional observational studies [48]. When applied within the context of genetics and environment in immune variation research, MR provides a unique opportunity to disentangle the complex interplay between heritable factors and environmental influences on immune-related biomarkers and their causal role in disease pathogenesis.
Core Principles and Assumptions of Mendelian Randomization
The Three Key Assumptions of Valid Instrumental Variables
For genetic variants to serve as valid instruments in MR analyses, they must satisfy three core assumptions [48] [51]:
- Relevance Assumption: The genetic variants must be strongly associated with the exposure of interest (e.g., the biomarker). This is typically demonstrated through genome-wide association studies (GWAS) showing significant associations between genetic variants and the exposure.
- Independence Assumption: The genetic variants must not be associated with any confounders of the exposure-outcome relationship. This assumption is generally plausible due to the random allocation of genetic variants at conception.
- Exclusion Restriction Assumption: The genetic variants must influence the outcome only through their effect on the exposure, not through alternative biological pathways (i.e., no horizontal pleiotropy).
Violations of these assumptions, particularly horizontal pleiotropy, can lead to biased causal estimates and invalid inferences [51]. The following diagram illustrates the core MR framework and its key assumptions:
Methodological Approaches and Sensitivity Analyses
With increasing recognition that not all genetic variants satisfy the ideal instrumental variable assumptions, several robust MR methods have been developed to detect and correct for pleiotropy [52]. These methods operate using different consistency assumptions and have complementary strengths:
Table 1: Robust Mendelian Randomization Methods for Sensitivity Analysis
| Method | Consistency Assumption | Key Features and Applications |
|---|---|---|
| Inverse-variance weighted (IVW) | All variants are valid | Standard approach; efficient when all variants are valid instruments [52] |
| Weighted median | Majority of genetic variants are valid | Robust to outliers; provides consistent estimate if >50% of weight comes from valid variants [52] |
| MR-Egger | Pleiotropic effects are independent of variant-exposure associations | Can detect and adjust for directional pleiotropy; lower statistical power [52] |
| MR-PRESSO | Outlier variants can be identified and removed | Identifies and removes outliers; provides corrected estimates [52] |
| Contamination mixture | Majority of variants are valid | Performs well across various pleiotropy scenarios; good balance of Type 1 error control and precision [52] |
Recent methodological guidelines emphasize that applying multiple complementary MR methods is essential for assessing the robustness of causal inferences [52] [51]. When different methods that rely on different assumptions yield consistent results, confidence in the causal conclusion is strengthened.
Practical Implementation and Workflow
Experimental Design and Instrument Selection
Implementing a robust MR analysis requires careful attention to study design and genetic instrument selection. The strength of genetic instruments is typically assessed using the F-statistic, with values greater than 10 indicating sufficient strength to minimize bias from weak instruments [53]. For example, in a recent MR study investigating immune cells in keratoconus, all included single nucleotide polymorphisms (SNPs) demonstrated F-statistics > 10 [53].
The STROBE-MR (Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization) checklist has emerged as a critical tool for ensuring transparent and comprehensive reporting of MR studies [49]. Leading journals now require adherence to these reporting guidelines to maintain publication standards amid concerns about variable research quality in the field.
Analytical Workflow and Validation
A comprehensive MR analysis follows a structured workflow that includes multiple validation steps to ensure robust causal inference:
Recent methodological standards emphasize that findings should be validated in at least one independent dataset to ensure reproducibility [49]. Additionally, where possible, MR results should be contextualized within existing biological knowledge and experimental evidence to assess their plausibility and potential mechanistic underpinnings.
Application in Immune Variation and Drug Development
Investigating Immune-Related Biomarkers in Disease
MR has been particularly valuable in elucidating the causal roles of immune-related biomarkers in disease pathogenesis. For example, a recent MR investigation into keratoconus revealed several causal relationships between inflammatory proteins and immune cells with disease risk [53]. The study identified IL-12B and IL-13 as risk factors, while IL-17A appeared protective. Additionally, 33 immune cell phenotypes were identified as potentially causal, including 22 protective and 11 risk-associated immune cell types [53].
Table 2: Exemplary MR Findings for Immune-Related Biomarkers in Disease
| Disease Context | Exposure Category | Key Causal Findings | Implications |
|---|---|---|---|
| Keratoconus [53] | Inflammatory proteins | IL-12B (OR 1.427) and IL-13 (OR 1.764) increase risk; IL-17A (OR 0.601) protective | Suggests specific immune pathways for therapeutic targeting |
| Keratoconus [53] | Immune cell phenotypes | 22 protective (e.g., CD20 on IgD- CD24- B cells) and 11 risk factors identified | Highlights importance of B cell regulation in disease prevention |
| Cardiometabolic Disease [47] | Liver biomarkers | Causal associations between gamma-glutamyltransferase and type 2 diabetes | Unravels complex relationships between organ function and metabolic health |
Drug Target Prioritization and Validation
In pharmaceutical research, MR plays an increasingly important role in target validation by providing human genetic evidence for putative drug targets [48]. This approach, known as drug-target MR, selects genetic variants in or near the gene encoding a drug target to mimic its pharmacological modulation [48]. Research has demonstrated that drug targets with genetic support have significantly higher success rates in phases II and III clinical trials [48].
The value of MR in drug development is particularly evident when its results are triangulated with evidence from RCTs. For instance, MR analyses correctly predicted the beneficial effects of LDL-C lowering through HMG-CoA reductase inhibition (statins) and PCSK9 inhibition on cardiovascular disease, while also anticipating the increased risk of type 2 diabetes as a side effect of statin therapy [50]. However, discrepancies sometimes occur, as with three independent MR studies that predicted increased T2D risk with PCSK9 inhibition, which was not confirmed in subsequent RCTs [50]. Such discrepancies highlight the importance of considering differences in intervention intensity, duration, and population characteristics when comparing MR and RCT findings.
Integrating Genetic and Environmental Factors in Immune Research
Gene-Environment Interplay in Immune Function
The integration of MR with environmental research is particularly relevant for understanding immune variation. While MR traditionally emphasizes genetic determinants, emerging research recognizes that genotype-environment interactions (G×E) substantially contribute to immune phenotype heterogeneity. A groundbreaking "rewilding" experiment with laboratory mice demonstrated that cellular composition of peripheral blood mononuclear cells was shaped by interactions between genotype and environment, while cytokine response heterogeneity was primarily driven by genotype [6].
This research revealed that genetic differences observed under controlled laboratory conditions were often reduced following exposure to a natural environment, illustrating how environmental context modulates genetic effects on immune traits [6]. For instance, expression of CD44 on T cells was explained mostly by genetics, whereas expression of CD44 on B cells was explained more by environment across all mouse strains studied [6].
Conducting robust MR studies requires specific data resources and analytical tools. The following table outlines key components of the "research reagent toolkit" for MR investigations:
Table 3: Essential Research Reagents and Resources for Mendelian Randomization Studies
| Resource Type | Specific Examples | Function and Application |
|---|---|---|
| GWAS Summary Statistics | Publicly available data from biobanks (UK Biobank, FinnGen) and consortia | Source of genetic association estimates for exposure and outcome traits [53] |
| Analytical Software | TwoSampleMR (R package), MR-Base platform | Facilitate MR analyses with summarized data, including multiple sensitivity methods [51] |
| Reporting Guidelines | STROBE-MR checklist | Ensure comprehensive reporting and methodological transparency [49] |
| Genetic Instruments | Curated SNPs from GWAS catalogs | Serve as proxies for exposures of interest; must satisfy instrumental variable assumptions [53] |
| Validation Resources | Independent cohorts, experimental models | Provide complementary evidence to support causal inferences [51] |
Mendelian Randomization represents a maturation in causal inference methodology, moving from simple single-variant analyses to sophisticated approaches that account for the complexity of biological systems. Future directions in MR methodology include increased integration of multi-omics data (including transcriptomics, proteomics, and metabolomics), development of approaches for subgroup-specific causal estimation, and improved methods for modeling time-varying exposures [48].
When contextualized within the broader framework of genetics and environment in immune variation research, MR provides a powerful approach for disentangling causal pathways while accounting for genetic predisposition. However, investigators must remain cognizant of the methodological limitations and assumptions underlying MR, and should interpret findings with appropriate caution [51]. The most robust conclusions emerge when MR evidence is triangulated with results from RCTs, laboratory experiments, and other epidemiological approaches [50].
As the field evolves, MR is poised to make increasingly substantial contributions to understanding disease etiology, validating therapeutic targets, and ultimately improving human health through evidence-based interventions that account for both genetic and environmental determinants of disease.
The immune system represents a quintessential model of complex trait variation, where diversity arises from a dynamic interplay between genetic predisposition and environmental exposures. Understanding this interplay requires moving beyond traditional genomics to integrated multi-omics approaches. These methodologies simultaneously analyze multiple layers of molecular information—including genetics, transcriptomics, proteomics, and epigenomics—to unravel complex biological systems. In immune research, multi-omics integration has proven particularly valuable for elucidating the molecular pathways through which genetic variants and environmental factors collectively shape immune responses and disease susceptibility [6] [54].
Recent technological and methodological advances have enabled the systematic mapping of quantitative trait loci (QTLs) that govern molecular phenotypes across different biological layers. Expression QTLs (eQTLs) identify genetic variants that influence gene expression levels, protein QTLs (pQTLs) reveal variants affecting protein abundance, and methylation QTLs (mQTLs) pinpoint variants associated with epigenetic modifications [55] [56] [57]. The integration of these datasets provides a powerful framework for connecting genetic variation to functional outcomes, thereby illuminating the mechanistic pathways that underlie immune diversity and disease pathogenesis.
This technical guide provides a comprehensive overview of the principles, methodologies, and applications for integrating multi-omics data, with a specific focus on immune variation research. We detail experimental protocols, analytical frameworks, and visualization approaches that enable researchers to translate complex multi-dimensional data into biological insights, ultimately advancing our understanding of how genetic and environmental factors interact to shape immune function.
Core Multi-Omics Data Types and Their Relationships
Key Omics Layers and Their Biological Significance
Multi-omics investigations in immunology typically incorporate several molecular data types, each providing distinct yet complementary information about immune system regulation. The table below summarizes the primary omics layers commonly integrated in immune variation studies.
Table 1: Core Multi-Omics Data Types in Immune Research
| Data Type | Abbreviation | Molecular Level | Biological Significance | Example in Immune Research |
|---|---|---|---|---|
| Expression Quantitative Trait Loci | eQTL | Transcriptional | Identifies genetic variants regulating gene expression | CCR7 expression on naive CD8+ T cells linked to schizophrenia risk [56] |
| Protein Quantitative Trait Loci | pQTL | Translational/Post-translational | Identifies genetic variants influencing protein abundance | BTN3A2 pQTL associated with nephrolithiasis risk [55] |
| Methylation Quantitative Trait Loci | mQTL | Epigenetic | Identifies genetic variants affecting DNA methylation patterns | cg18095732 regulating ZDHHC20 in schizophrenia [56] |
| Protein-Protein Ratio Loci | rQTL | Network/Systems | Identifies variants affecting protein-protein relationships | 2,821 protein-protein ratios revealing disease associations [55] |
Integrative Analytical Frameworks
The true power of multi-omics emerges from analytical approaches that integrate across these data layers. Mendelian randomization (MR) has emerged as a particularly powerful causal inference tool in multi-omics studies [55] [56] [57]. This method uses genetic variants as instrumental variables to infer causal relationships between molecular exposures (e.g., protein levels) and health outcomes (e.g., disease risk), while minimizing confounding from environmental factors.
Mediation MR extends this approach to identify chains of causality across omics layers. For example, research on schizophrenia revealed that DNA methylation at a specific CpG site (cg18095732) regulates ZDHHC20 expression, which subsequently influences CCR7 expression on immune cells, ultimately affecting disease risk [56]. This approach formally tests hypotheses about the sequential flow of information from genetic variation to epigenetic regulation, gene expression, protein function, and ultimately to cellular and organismal phenotypes.
Colocalization analysis provides another crucial integrative method, determining whether different molecular traits (e.g., protein abundance and disease risk) share the same underlying causal genetic variant within a specific genomic region [55] [57]. This approach helps distinguish true biological mediation from coincidental association due to genetic linkage.
Experimental Design and Workflows
Study Design Considerations
Robust multi-omics studies require careful consideration of several design elements. Sample size must be sufficient to detect typically small effect sizes of genetic variants on molecular traits, with large-scale biobanks (e.g., UK Biobank, FinnGen) now providing data on hundreds of thousands of participants [55] [57] [58]. Tissue specificity presents another critical consideration, as molecular QTLs often show tissue-specific effects. While blood represents an accessible tissue for immune studies, complementary data from relevant tissues (e.g., cerebrospinal fluid, brain) may be necessary depending on the research question [57].
Population ancestry must be carefully considered, as genetic architecture, linkage disequilibrium patterns, and environmental exposures differ across populations. Recent methodological advances, such as SPAGxEmixCCT, enable more effective multi-ancestry analyses by accounting for population stratification in gene-environment interaction studies [58]. Additionally, batch effects and technical artifacts can severely compromise multi-omics data quality, necessitating rigorous quality control procedures and statistical corrections.
Data Generation Protocols
Genotyping and QTL Mapping
Genome-wide association data form the foundation for multi-omics integration. Standard protocols involve:
- Genotype processing: Quality control, imputation, and population stratification assessment using tools like PLINK and IMPUTE2.
- Molecular phenotyping: Generation of transcriptomic (RNA-seq), proteomic (mass spectrometry, aptamer-based platforms), and epigenomic (Illumina Methylation arrays) data.
- QTL mapping: Identification of genetic variants associated with molecular phenotypes using linear mixed models that account for relatedness and population structure.
For pQTL studies, recent protocols have expanded to include protein-protein ratios (rQTLs), which can reveal genetic variants that influence relationships between protein pairs, potentially capturing functional interactions within biological pathways [55].
Integrative Analysis Workflow
The following diagram illustrates a comprehensive multi-omics integration workflow for identifying causal genes and pathways:
Figure 1: Multi-Omics Integration Workflow. SMR: Summary-data-based Mendelian Randomization; HEIDI: Heterogeneity in Dependent Instruments test.
Methodological Protocols
Instrumental Variable Selection for Mendelian Randomization
MR analyses require careful selection of genetic instruments that satisfy three key assumptions: (1) relevance (strong association with the exposure), (2) independence (no confounding), and (3) exclusion restriction (affects outcome only through the exposure) [55] [56]. Standard protocols include:
- Variant selection: Select independent (linkage disequilibrium r² < 0.001) genetic variants associated with the molecular exposure at genome-wide significance (P < 5 × 10⁻⁸) [55].
- Clumping: Remove variants in linkage disequilibrium using reference panels.
- Strength assessment: Calculate F-statistics to guard against weak instrument bias (F > 10 recommended).
- Palindromic variant removal: Exclude variants with ambiguous strand orientation.
For cis-pQTL analyses, a common approach restricts to variants within 1 megabase of the protein-coding gene's transcription start site [55].
Sensitivity Analysis Framework
Robust MR analyses require multiple sensitivity analyses to validate assumptions:
- MR-Egger regression: Tests for directional pleiotropy via intercept significance [55] [56].
- Cochran's Q statistic: Assesses heterogeneity among variant-specific estimates.
- Leave-one-out analysis: Determines if results are driven by individual influential variants.
- MR-PRESSO: Identifies and corrects for outliers due to pleiotropy.
- Steiger filtering: Tests for reverse causation by assessing the direction of causality [55].
Multi-Ancestry and Gene-Environment Interaction Methods
Recent methodological advances address the complexities of gene-environment interactions and diverse ancestries:
- SPAGxECCT framework: A scalable method for genome-wide gene-environment interaction analysis that accommodates binary, time-to-event, and ordinal traits [58].
- SPAGxEmixCCT extension: Accounts for population stratification in multi-ancestry or admixed populations [58].
- Local ancestry-aware approaches: Enable identification of ancestry-specific G×E effects (SPAGxEmixCCT-local) [58].
These methods employ saddlepoint approximation (SPA) for accurate p-value calculation, particularly important for low-frequency variants and unbalanced phenotypic distributions common in biobank data [58].
Table 2: Key Research Resources for Multi-Omics Studies
| Resource Category | Specific Resource | Description and Application | Key Features |
|---|---|---|---|
| QTL Datasets | eQTLGen Consortium | Blood eQTL data from 31,684 individuals | 88% of identified cis-eGenes; 11 million SNP-gene associations [57] |
| QTL Datasets | UK Biobank PPP | Plasma proteomics data from 34,557 participants | 2,940 plasma proteins; pQTL and rQTL data [55] |
| QTL Datasets | GTEx v8 | Multi-tissue eQTL data from 54 tissue types | 13 brain regions; nearly 1,000 donors [57] |
| QTL Datasets | GoDMC | mQTL data from Genetics of DNA Methylation Consortium | Genetic variants associated with DNA methylation in whole blood [56] |
| Analytical Software | GenomicSEM | Multivariate method for analyzing complex-trait genetic architecture | Uses LD-score regression; applies structural equation models to genetic data [59] |
| Analytical Software | SMR | Summary-data-based Mendelian Randomization software | Tests causal relationships using QTL and GWAS data; includes HEIDI test [57] |
| Analytical Software | SPAGxECCT | Scalable framework for gene-environment interaction analysis | Handles diverse trait types; accounts for population stratification [58] |
| Analytical Software | coloc | R package for colocalization analysis | Tests shared causal variants between molecular traits and disease [57] |
| Reference Data | HapMap3 | Reference panel for genetic analyses | International HapMap Project haplotype map datasets [59] |
| Reference Data | LD Score Regression | Reference panels for LD score calculations | Provides linkage disequilibrium scores for genomic regions [59] |
Genetic-Environmental Interplay in Immune Variation
Conceptual Framework for Gene-Environment Interactions
The immune system exhibits remarkable interindividual variation that arises from complex interactions between genetic predisposition and environmental exposures. This interplay can be visualized as follows:
Figure 2: Genetic-Environmental Interplay in Immune Variation
Empirical Evidence from Rewilding Studies
Controlled experiments with "rewilded" laboratory mice exposed to natural environments provide compelling evidence for gene-environment interactions in immune system development. Key findings include:
- Cellular composition of peripheral blood mononuclear cells (PBMCs) is shaped by interactions between genotype and environment, with certain immune cell populations expanding following rewilding regardless of mouse strain [6].
- Genetic differences observed under controlled laboratory conditions can be reduced following rewilding, as demonstrated by CD44 expression patterns on CD4+ T cells [6].
- Infection responses can reveal genetic differences only in specific environmental contexts, such as the stronger Th1 response to Trichuris muris infection in C57BL/6 mice that emerged exclusively in rewilding conditions [6].
These findings highlight how environmental context can both mask and unmask genetic effects on immune traits, demonstrating that the impact of genotype on immune function depends critically on environmental conditions, and vice versa.
Applications in Disease Research
Case Study: Multi-Omics in Alzheimer's Disease
Integrative multi-omics approaches have identified novel susceptibility genes for Alzheimer's disease (AD) through systematic analysis of mQTL, eQTL, and pQTL data across multiple tissues [57]. Key findings include:
- ACE gene: Increased methylation at specific CpG sites (cg04199256, cg21657705) associated with higher ACE expression, demonstrating a protective effect against AD.
- CD33 gene: Strong evidence for causal relationship with increased AD risk (OR = 1.17, 95% CI: 1.09-1.25).
- Protein-level associations: TMEM106B (OR 1.44), SIRPA (OR 1.03), and CTSH (OR 1.04) associated with increased AD risk, while CLN5 (OR 0.69) demonstrated protective effects.
This multi-omics approach provided evidence for causal relationships across molecular levels, with strong colocalization signals (posterior probability > 0.9) supporting shared causal variants for molecular QTLs and AD risk [57].
Case Study: Drug Target Identification for Nephrolithiasis
MR integration of pQTL and eQTL data identified BTN3A2 as a potential therapeutic target for nephrolithiasis (kidney stones) [55]. The analytical workflow included:
- Bidirectional MR to establish causal relationships between plasma protein-related targets and nephrolithiasis.
- Mediation analysis identifying glomerular filtration rate (GFR) as an intermediate factor for five protein targets.
- Colocalization analysis providing strong evidence for three protein targets.
- Molecular docking simulations identifying digitoxigenin as a potential therapeutic compound with strong binding affinity to BTN3A2.
This comprehensive approach demonstrated how multi-omics data can prioritize potential drug targets and even identify candidate therapeutic compounds.
The integration of multi-omics data represents a transformative approach for unraveling the complex interplay between genetic and environmental factors in immune variation. By simultaneously analyzing multiple molecular layers—including genomic, transcriptomic, proteomic, and epigenomic data—researchers can construct comprehensive models of immune system regulation and identify causal pathways underlying disease susceptibility.
Methodological advances in Mendelian randomization, colocalization analysis, and gene-environment interaction testing have greatly enhanced our ability to draw causal inferences from observational data. These approaches, combined with the growing availability of large-scale biobank resources and specialized analytical tools, are accelerating the discovery of novel therapeutic targets and biomarkers.
Future developments in multi-omics integration will likely focus on single-cell approaches, which can resolve cellular heterogeneity in immune responses; temporal modeling of dynamic processes; and sophisticated machine learning methods for detecting complex, non-linear relationships. As these technologies and methods mature, multi-omics integration will increasingly enable personalized approaches to immunology, tailoring interventions to individual genetic backgrounds and environmental exposures to optimize immune health throughout the lifespan.
The convergence of large-scale genomic biobanks, multi-omics data, and advanced computational methods has fundamentally transformed the paradigm of drug discovery and development [60]. This transition from serendipitous finding to systematic, genetics-driven therapeutic identification represents a pivotal advancement in addressing the persistently high attrition rates that have long plagued pharmaceutical development. Contemporary drug development continues to face significant challenges, with unexpected adverse effects and efficacy failures contributing substantially to clinical trial failures [60]. Against this backdrop, genetics-driven approaches offer a compelling framework for de-risking therapeutic development by anchoring drug discovery in human biological evidence, thereby increasing the probability of clinical success.
The foundation of this approach rests upon a crucial understanding of human immune variation, which is shaped by a complex interplay of genetic determinants and environmental influences. While genetic variants undeniably play a key role in immune response—affecting how much gene expression changes in response to immune stimuli—environmental factors often exert a more dominant influence on the functional state of the immune system [61] [20]. This intricate relationship is exemplified by research showing that nonheritable influences, particularly previous microbial exposures, trump heritable factors in accounting for immune variation between individuals [61]. Furthermore, the relative contribution of genetics versus environment displays significant context dependency, with some immune traits being primarily genetically determined while others are predominantly shaped by environmental exposures [6]. This nuanced understanding of immune system plasticity provides the essential biological context for developing genetics-driven therapeutic strategies that account for both heritable and nonheritable factors in disease pathogenesis and treatment response.
Conceptual Framework: Principles of Genetics-Driven Drug Discovery
Foundational Concepts and Definitions
Genetics-driven drug discovery operates through several interconnected mechanistic principles that enable the identification and prioritization of therapeutic targets. At its core, this approach leverages human genetic evidence to identify genes and pathways whose modulation is likely to confer therapeutic benefits while minimizing adverse effects. The fundamental premise is that genetic variants associated with disease susceptibility naturally inform therapeutic target validation, as these variants represent in vivo experiments of nature that demonstrate the biological consequences of modulating specific genes or pathways [60].
Pleiotropy, the phenomenon where genetic variants or genes influence multiple traits, serves as a powerful tool for systematically informing drug discovery [62]. By analyzing genetic similarity across diverse phenotypes, researchers can predict novel therapeutic applications and potential side effects of drugs, sometimes bypassing the need to pinpoint specific causal genes [62]. This gene-target agnostic approach is particularly valuable for drug repurposing, as it identifies shared genetic architectures between diseases that may not share obvious clinical phenotypes.
The polyexposure score concept further enriches this framework by quantifying the combined environmental risk factors that interact with genetic predispositions [20]. Research has demonstrated that environmental factors—including diet, occupational hazards, lifestyle choices, and social environments—often serve as better predictors of chronic disease development than genetic risk scores alone [20]. This highlights the critical importance of integrating environmental context into genetics-driven therapeutic discovery, as genetic risk factors may only manifest under specific environmental conditions [7].
Analytical Approaches and Validation Strategies
Multiple complementary analytical frameworks have emerged to systematically translate genetic findings into therapeutic hypotheses. Genetic similarity metrics can predict drug sharing between diseases, regardless of whether they affect the same or different body systems [62]. This approach leverages five distinct genetic similarity measurements, capturing genome-wide genetic correlation, gene-level associations, tissue-specific gene regulation, and molecular QTL colocalization to create a comprehensive predictive framework.
Machine learning models trained on comprehensive biological activity profile data enable the prediction of relationships between gene targets and chemical compounds [63]. These models, including Support Vector Classifier, Random Forest, and Extreme Gradient Boosting algorithms, demonstrate high accuracy in predicting novel drug-target interactions, thereby facilitating the drug repurposing process for rare diseases with limited treatment options [63].
Functional validation of genetic discoveries employs high-throughput screening technologies such as quantitative high-throughput screening (qHTS) data from resources like the Tox21 10K compound library [63]. This extensive dataset, which encompasses drugs, pesticides, consumer products, and industrial chemicals screened against numerous in vitro assays, provides a robust foundation for evaluating compound activity and toxicity profiles in the context of genetically-validated targets.
Table 1: Key Analytical Frameworks in Genetics-Driven Drug Discovery
| Framework | Primary Application | Data Requirements | Validation Approach |
|---|---|---|---|
| Polygenic/Polyexposure Scoring | Disease risk prediction | GWAS data, environmental exposure data | Prospective cohort studies, electronic health records |
| Pleiotropy Analysis | Drug repurposing, side effect prediction | Genetic association data across multiple phenotypes | Clinical trial data, pharmacovigilance databases |
| Machine Learning Prediction | Novel target identification, compound screening | Biological activity profiles, chemical structures | Experimental validation, public bioassay data |
| Genetic Similarity Metrics | Therapeutic indication expansion | Multi-phenotype genetic data | Drug-disease association databases, clinical outcomes |
Experimental Methodologies: From Genomic Data to Therapeutic Hypotheses
Genomic Data Acquisition and Processing
The initial phase of genetics-driven drug discovery involves systematic acquisition and processing of genomic data from diverse populations. Genome-wide association studies (GWAS) form the cornerstone of this approach, enabling the identification of genetic variants associated with specific diseases or traits. Contemporary protocols emphasize the importance of diverse population inclusion to capture genetic variation across different ethnic and racial groups, which significantly contributes to disease susceptibility variations [64]. For example, studies focused on Saudi patients with sickle cell disease have demonstrated how population-specific genetic data can reveal novel therapeutic targets and repurposing opportunities tailored to that specific demographic [65].
The standard workflow for genomic data acquisition involves:
- Cohort Selection and Ethical Compliance: Recruit participants with appropriate informed consent, ensuring representation of target populations. For studies examining gene-environment interactions, collect comprehensive environmental exposure data alongside genetic material [20].
- Genotyping and Quality Control: Perform high-density genotyping using array-based technologies, followed by rigorous quality control procedures including call rate filtering, Hardy-Weinberg equilibrium testing, and relatedness assessment.
- Imputation and Annotation: Utilize reference panels for genotype imputation to increase variant coverage, followed by functional annotation of identified variants using databases such as ENCODE, Roadmap Epigenomics, and GTEx.
- Association Testing: Conduct genome-wide association analyses using standardized statistical approaches, correcting for multiple testing and accounting for population stratification.
Target Identification and Prioritization Workflows
Following genomic discovery, bioinformatic pipelines systematically evaluate and prioritize therapeutic targets based on multiple lines of evidence:
Diagram 1: Target Prioritization Workflow (77 characters)
Drug-gene interaction analysis utilizes databases such as the Drug-Gene Interaction Database (DGIdb 5.0) to identify approved drugs that interact with genes implicated in disease pathophysiology [65]. This systematic approach enables the compilation of potential repurposing candidates, which can be further refined based on safety profiles and interactions with key genetic pathways.
Novel target discovery employs structural bioinformatics to assess the druggability of gene products identified through genetic studies. Using 3D protein structures from the Protein Data Bank and the AlphaFold database, researchers simulate binding pockets and calculate druggability scores using tools like DoGSiteScorer [65]. Targets with higher druggability scores are predicted to have higher success rates in subsequent drug development campaigns.
Table 2: Key Databases for Genetics-Driven Drug Discovery
| Database | Primary Function | Application in Workflow |
|---|---|---|
| DGIdb 5.0 | Drug-gene interaction data | Identifying repurposing candidates for genetic targets |
| Protein Data Bank (PDB) | Experimental protein structures | Assessing binding site characteristics |
| AlphaFold Database | Predicted protein structures | Modeling proteins without experimental structures |
| DoGSiteScorer | Binding pocket prediction | Calculating druggability scores for novel targets |
| Tox21 10K Library | Compound activity profiles | Screening chemicals against biological targets |
Machine Learning Approaches for Target Identification
Advanced computational methods have emerged as powerful tools for predicting novel therapeutic targets. The standard protocol for machine learning-based target identification involves [63]:
- Data Preparation: Compile biological activity profiles from large-scale screening efforts such as the Tox21 program, which includes quantitative high-throughput screening data for approximately 10,000 compounds across numerous in vitro assays.
- Feature Engineering: Process compound activity data using metrics such as curve rank, which ranges from -9 to 9 and is determined by various attributes of concentration-response curves including potency, efficacy, and quality.
- Model Training: Implement multiple machine learning algorithms including Support Vector Classifier, K-Nearest Neighbors, Random Forest, and Extreme Gradient Boosting to predict relationships between gene targets and chemical compounds.
- Validation and Interpretation: Assess model performance using cross-validation and external validation datasets, followed by biological interpretation of high-confidence predictions through experimental follow-up.
These models demonstrate particular utility for rare diseases, where they can elucidate connections between chemical compounds and gene targets implicated in disease mechanisms, thereby streamlining the repurposing process and catalyzing therapeutic development for conditions with limited treatment options [63].
Data Analysis and Interpretation: From Genetic Associations to Therapeutic Insights
Quantitative Analysis of Drug Repurposing Candidates
Systematic analysis of drug repurposing candidates leverages genetic data to identify approved medications with potential new therapeutic applications. A representative study focusing on sickle cell disease in Saudi patients exemplifies this approach, having identified 78 approved medications with repurposing potential, which was subsequently refined to 21 candidates based on safety profiles and interactions with key genetic pathways [65].
The prioritization process employs quantitative metrics including:
- Drug-gene interaction scores derived from databases like DGIdb
- Safety and toxicity profiles from pharmacological databases
- Pathway relevance scores quantifying association with disease mechanisms
- Druggability metrics predicting developmental success probability
Among the most promising repurposing candidates identified in such analyses are simvastatin, allopurinol, omalizumab, canakinumab, and etanercept, which demonstrate favorable interactions with genetic pathways relevant to the target disease [65].
Table 3: Representative Drug Repurposing Candidates Identified Through Genetic Analysis
| Drug Candidate | Original Indication | Proposed New Indication | Genetic Evidence | Development Status |
|---|---|---|---|---|
| Simvastatin | Cholesterol management | Sickle cell disease [65] | Interaction with key genetic pathways | Preclinical validation |
| Allopurinol | Gout | Sickle cell disease [65] | Modulation of disease-relevant pathways | Preclinical validation |
| Omalizumab | Asthma | Sickle cell disease [65] | Immune pathway interactions | Preclinical validation |
| Canakinumab | Cryopyrin-associated periodic syndromes | Sickle cell disease [65] | Inflammation modulation | Preclinical validation |
Novel Target Identification and Validation
Beyond repurposing existing drugs, genetic studies systematically identify novel therapeutic targets through comprehensive genomic analyses. These approaches have revealed unexpected target classes, including olfactory receptor (OR) gene clusters (OR51V1, OR52A1, OR52A5, OR51B5, and OR51S1), TRIM genes, SIDT2, and CADM3, which displayed high druggability scores despite not being previously implicated in certain diseases [65].
The analytical workflow for novel target prioritization incorporates multiple lines of evidence:
- Genetic association strength: Effect sizes and statistical significance from GWAS
- Functional genomic evidence: Expression quantitative trait loci, chromatin interactions, and epigenetic annotations
- Druggability assessment: Binding pocket characteristics and similarity to known drug targets
- Safety considerations: Phenotypic consequences of genetic perturbation in model systems
The convergence of large-scale biobanks with these multi-omics data and computational methods enables the systematic prioritization of drug targets within a probabilistic framework, substantially enhancing the efficiency of therapeutic development [60].
Integrating Genetic and Environmental Context
A critical advancement in genetics-driven drug discovery involves the integration of environmental context with genetic findings. Research demonstrates that genetic risk factors for immune-mediated diseases may only manifest under specific environmental conditions [7]. For example, studies have shown that living nearer to caged animal feeding operations and having a specific genetic variant associated with autoimmune diseases more than doubles a person's risk of developing immune-mediated conditions [20].
This gene-environment interplay is further elucidated by controlled experiments in model systems. "Rewilding" studies with genetically distinct mouse strains demonstrate that the relative contributions of genetics versus environment to immune variation are trait-dependent and context-specific [6]. For instance, genetic differences in CD44 expression on T cells observed under laboratory conditions were substantially reduced following environmental exposure through rewilding, whereas certain infection responses emerged only in the rewilded environment [6].
These findings underscore the importance of considering environmental context when interpreting genetic associations for therapeutic development, as the efficacy of genetically-targeted therapies may be modified by environmental factors that influence the same biological pathways.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Core Research Reagents and Databases
Implementing genetics-driven drug discovery requires specialized research reagents and computational resources. The following table details essential tools and their applications in the therapeutic discovery workflow:
Table 4: Essential Research Reagents and Platforms for Genetics-Driven Drug Discovery
| Resource | Type | Function/Application | Key Features |
|---|---|---|---|
| Tox21 10K Compound Library | Chemical Library | Screening compounds against biological targets [63] | ~10,000 substances including drugs, pesticides, and industrial chemicals |
| DGIdb 5.0 | Database | Identifying drug-gene interactions [65] | Curated drug-gene interaction data from multiple sources |
| Protein Data Bank (PDB) | Structural Database | Accessing experimental protein structures [65] | Experimentally determined 3D structures of proteins and nucleic acids |
| AlphaFold Database | Structural Database | Accessing predicted protein structures [65] | Highly accurate protein structure predictions for the proteome |
| DoGSiteScorer | Computational Tool | Predicting and scoring binding pockets [65] | Automated binding pocket detection and druggability assessment |
| Human Immune Monitoring Center | Technological Platform | Comprehensive immune profiling [61] | Advanced immune-sleuthing technologies for systematic immune assessment |
AI-Driven Drug Discovery Platforms
Artificial intelligence has emerged as a transformative force in genetics-driven therapeutic discovery, with several platforms advancing AI-designed candidates into clinical trials:
- Exscientia's Centaur Chemist Approach: Integrates algorithmic creativity with human domain expertise to iteratively design, synthesize, and test novel compounds, reportedly achieving clinical candidate designation with significantly fewer synthesized compounds than traditional approaches [66].
- Insilico Medicine's Generative AI Platform: Demonstrated accelerated timeline from target discovery to Phase I trials, compressing a typically 5-year process into approximately 18 months for an idiopathic pulmonary fibrosis drug candidate [66].
- Recursion's Phenomics Platform: Generates massive biological datasets through automated microscopy and image analysis, enabling AI-driven identification of novel therapeutic patterns [66].
- BenevolentAI's Knowledge Graph: Integrates scientific literature, experimental data, and clinical trial information to generate novel therapeutic hypotheses through semantic reasoning [66].
- Schrödinger's Physics-Based Simulations: Leverages computational chemistry platforms based on first-principles physics to predict molecular properties and optimize compound characteristics [66].
These platforms represent the cutting edge of AI-enabled therapeutic discovery, collectively advancing dozens of novel drug candidates into clinical trials by mid-2025 [66].
Genetics-driven drug discovery has evolved from a promising concept to a robust framework for therapeutic development, demonstrated by the systematic identification of repurposing candidates and novel targets across diverse disease areas. The integration of large-scale genomic data with advanced computational methods, including machine learning and AI platforms, has created an unprecedented opportunity to anchor therapeutic development in human biological evidence, thereby increasing efficiency and reducing late-stage attrition.
The critical advancement in this field lies in recognizing that genetic discoveries must be interpreted within the context of environmental influences that shape disease expression and treatment response. As research continues to elucidate the complex interplay between genetic predispositions and environmental factors, the next frontier in genetics-driven therapeutics will involve developing nuanced approaches that account for these interactions, ultimately enabling truly personalized medical interventions tailored to an individual's genetic makeup and environmental context.
Future directions will likely focus on longitudinal data collection through electronic health records, expanded diverse population inclusion in genetic studies, and development of more sophisticated integrative models that simultaneously consider genetic, environmental, and social determinants of health. These advances promise to further enhance the precision and effectiveness of genetics-driven therapeutic discovery, ultimately accelerating the development of novel treatments for diseases with unmet medical needs.
The escalating costs and high failure rates of clinical trials, primarily due to inadequate efficacy or safety, underscore a critical need for improved early-stage target prioritization in drug development. The Genetic Priority Score (GPS) addresses this challenge as a computational framework that integrates diverse human genetic evidence to systematically prioritize drug targets. By consolidating multiple lines of genetic support into a single, interpretable metric, GPS identifies genes with increased likelihood of clinical trial success. This review comprehensively details the GPS framework, its methodological development, validation, and application, contextualized within the broader understanding of how genetic and environmental factors collectively shape immune variation and therapeutic outcomes.
The drug development process faces substantial inefficiencies, with billions of dollars lost annually to late-stage clinical trial failures, most commonly due to poor efficacy or unforeseen safety issues [67] [68]. Studies consistently demonstrate that drug targets with supporting human genetic evidence are twice as likely to advance through clinical trials and receive regulatory approval [69] [68] [70]. This empirical observation has fueled intense interest in leveraging human genetics to inform target selection.
The Genetic Priority Score (GPS) emerged from the recognition that while diverse human genetic data provides invaluable insights into drug target biology, no cohesive strategy existed to integrate these disparate data types into an easily interpretable framework [68]. GPS fills this methodological gap by synthesizing evidence from multiple genetic resources into a unified scoring system that measures a gene's potential to be successfully targeted by pharmaceuticals [69] [71].
Beyond efficacy considerations, a specialized version of the framework—the Side Effect Genetic Priority Score (SE-GPS)—has been developed to specifically predict drug side effects by leveraging human genetic evidence to inform side effect risk for a given drug target [67]. This expansion highlights the framework's adaptability to different phases of drug safety and efficacy assessment.
Genetic and Environmental Context of Immune Variation
To fully appreciate the significance of genetic prioritization frameworks, one must consider the complex interplay between genetic predispositions and environmental influences in shaping human immune responses. Research comparing monozygotic and dizygotic twins has revealed that non-heritable influences dominate approximately 77% of immunological parameters, including cell population frequencies, cytokine responses, and serum proteins [61] [31]. Environmental factors such as previous microbial exposures, infections, vaccinations, diet, and toxic exposures account for the majority of interindividual immune variation, particularly as individuals age [61].
However, genetic factors maintain crucial roles in specific immune functions. Homeostatic cytokine responses, such as IL-2 and IL-7 stimulated STAT5 phosphorylation in T-cells, demonstrate high heritability [31]. Additionally, the relative contributions of genetic and environmental factors exhibit significant context dependency, with genotype-by-environment (Gen × Env) interactions substantially influencing specific immune traits and infection outcomes [6]. For instance, genetic differences in CD44 expression on CD4+ T cells observed under controlled laboratory conditions were reduced following "rewilding" of mice into natural environments, whereas genetic differences in T helper 1 cell responses to parasites were amplified in the same environmental context [6].
This complex background underscores why genetic evidence alone provides necessary but insufficient guidance for drug development, and why frameworks like GPS must eventually incorporate environmental interaction data to more completely predict therapeutic effects in diverse human populations.
GPS Methodology and Framework Architecture
Data Integration and Genetic Features
The GPS framework integrates multiple categories of human genetic evidence through a structured approach to data acquisition, processing, and synthesis:
Clinical Variant Evidence: Curated from ClinVar (filtered by clinical significance), Human Gene Mutation Database (disease-causing mutations), and Online Mendelian Inheritance in Man (pathogenic gene annotations) [69] [70].
Coding Variant Evidence: Derived from large-scale sequencing efforts including:
Genome-Wide Association Evidence: Integrated from multiple sources:
Table 1: Genetic Evidence Features Integrated in GPS Framework
| Evidence Category | Data Sources | Feature Type | Application in GPS |
|---|---|---|---|
| Clinical Variants | ClinVar, HGMD, OMIM | Count of overlapping entries | Pathogenic variant burden |
| Coding Variants | Genebass, RAVAR | Binary (presence/absence) | Rare variant association |
| Gene Burden Tests | Open Targets, RAVAR | Binary (presence/absence) | Gene-based association strength |
| GWAS Loci | Locus2Gene, eQTL/pQTL | Binary (presence/absence) | Common variant association |
Analytical Workflow and Scoring Algorithm
The GPS construction follows a rigorous analytical workflow that ensures robust statistical support and minimizes overfitting:
Diagram 1: GPS Development Workflow
The scoring algorithm employs a multivariable mixed-effect regression model, with the GPS calculated as the weighted sum of genetic feature observations:
Equation 1: ( GPS = \sum{i=1}^{n} βi \cdot X_i )
Where ( βi ) represents the effect size estimate for genetic feature ( i ) derived from training set associations, and ( Xi ) represents the observation of genetic feature ( i ) in the test set [67]. The model incorporates phecode categories as covariates and includes drug as a random-effect variable to account for multiple testing scenarios [67].
For side effect prediction, the framework incorporates a directional component (SE-GPS-DOE) that considers the direction of genetic effect relative to drug mechanism, enabling more precise side effect risk assessment [67].
Directional Scoring Extension
A significant advancement in the GPS framework is the incorporation of directionality through the GPS with Direction of Effect (GPS-DOE), which integrates the direction of genetic effect with drug mechanism to inform the required direction of pharmacological modulation [69] [70]. This extension is particularly valuable for determining whether drug development should pursue activation or inhibition of a target protein based on whether loss-of-function or gain-of-function variants are associated with beneficial phenotypic outcomes.
Performance and Validation
Efficacy Predictions
The GPS demonstrates remarkable performance in predicting successful drug targets:
Table 2: GPS Performance for Drug Indication Prediction
| GPS Percentile | Fold-Increase in Drug Indication | Clinical Trial Advancement Likelihood |
|---|---|---|
| Top 0.83% | 5.3x | Not specified |
| Top 0.28% | 9.9x | 1.7x (Phase I→II), 3.7x (Phase I→III), 8.8x (Phase I→IV) |
| Top 0.19% | 11.0x | Not specified |
Validation across multiple datasets confirmed these associations, with the top 0.28% of GPS targets demonstrating substantially increased probabilities of advancing through all clinical trial phases [69] [70].
Safety Predictions
The SE-GPS framework for side effect prediction has shown significant utility in identifying targets likely to elicit adverse drug reactions:
- Restricting to at least two lines of genetic evidence conferred a 2.3- and 2.5-fold increased risk of side effects in Open Targets and OnSIDES datasets, respectively [67]
- Enrichments were particularly pronounced for severe drug side effects [67]
- The framework successfully identified 1.7% of 19,422 gene-phecode pairs with SE-GPS > 0, highlighting its selectivity [67]
External validation in the OnSIDES dataset, which extracts adverse drug reactions from drug labels reported during clinical trials, confirmed the robustness of these predictions [67].
Implementation and Research Applications
Experimental Protocols
For researchers implementing GPS validation studies, key methodological considerations include:
Drug-Target-Phenotype Mapping Protocol:
- Extract drug-indication and drug-target pairs from Open Targets Platform and SIDER database [70]
- Map indications and side effects to phecode terms using established mapping procedures [67]
- Apply quality control filters to remove side effects sharing phecode terms with drug indications [67]
- Integrate genetic evidence at gene-phecode level across all data sources [67]
Statistical Validation Protocol:
- Perform five-fold cross-validation with 80% training/20% testing splits [67] [70]
- Apply multivariable Firth logistic regression to address separation issues in genetic association studies [70]
- Adjust for phecode categories as fixed effects and drug as random effect [67]
- Incorporate severity weighting for side effect outcomes using crowdsourced severity scores [67]
Research Reagent Solutions
Table 3: Essential Research Resources for GPS Implementation
| Resource Category | Specific Tools | Research Application |
|---|---|---|
| Genetic Databases | ClinVar, HGMD, OMIM, Genebass, RAVAR | Source of clinical and coding variant evidence |
| GWAS Resources | Open Targets Genetics, GWAS Catalog, Pan-UK Biobank | Common variant association evidence |
| Molecular QTL Data | GTEx eQTLs, pQTL datasets | Functional genomic evidence for variant effects |
| Drug Mapping Resources | Open Targets Platform, SIDER, OnSIDES | Drug-target-indication and side effect mapping |
| Phenotype Mapping | Phecode Map 1.2, UMLS Metathesaurus | Clinical phenotype standardization |
| Analytical Tools | R packages for MR-PRESSO, HOPS, custom GPS scripts | Statistical analysis and pleiotropy assessment |
Analytical Extensions and Complementary Frameworks
The GPS framework interfaces with several specialized analytical tools developed by the same research community:
- MR-PRESSO: Framework for detecting and correcting horizontal pleiotropy in Mendelian randomization analyses [71]
- HOPS: Horizontal Pleiotropy Score computation from genome-wide summary statistics [71]
- biPheMap: Exploration of phenome-wide network maps of colocalized genes and phenotypes across GTEx tissues [71]
- MOI-Pred: Mode of inheritance prediction for missense variants across the human genome [71]
These complementary tools enhance the utility of GPS by addressing specific analytical challenges in genetic association studies and drug target validation.
Future Directions and Implementation Considerations
The GPS framework continues to evolve with several planned enhancements:
- Incorporation of additional genetic features and more sophisticated algorithms for score construction [68]
- Refinement of directional effect predictions through improved functional annotation of variants [69]
- Expansion to incorporate non-protein-coding genes as targeted therapeutic modalities advance [70]
- Integration of environmental interaction terms to account for Gen × Env effects on drug efficacy and safety [6]
Implementation considerations for research applications include the public availability of GPS scores through an interactive web portal (https://rstudio-connect.hpc.mssm.edu/geneticpriorityscore/) [69] [70], with all analysis code accessible on Zenodo for reproducibility and community improvement.
The Genetic Priority Score represents a transformative framework for systematic drug target prioritization by integrating diverse human genetic evidence into a unified, interpretable metric. Extensive validation demonstrates its ability to identify targets with significantly increased probabilities of clinical success, addressing a critical bottleneck in drug development. As precision medicine advances, GPS and its extensions provide a powerful methodology for leveraging human genetics to develop safer, more effective therapeutics while contextualizing genetic effects within the environmental influences that substantially shape individual immune responses and treatment outcomes.
Navigating Complexity: Overcoming Challenges in Translating Immune Variation Insights
The drug development landscape is dominated by a formidable challenge known as the "valley of death"—the significant gap between basic scientific research and the successful translation of findings into approved clinical therapies [72] [73]. This translational crisis is characterized by staggering attrition rates, with approximately 95% of drugs entering human trials failing to gain regulatory approval [73]. The consequences are profound: 15-year development timelines and costs averaging $2.6 billion per approved drug [73]. Within this challenging environment, evidence increasingly indicates that human genetic support for therapeutic hypotheses provides a crucial compass for navigating the valley of death, significantly enhancing the probability of clinical trial success [74] [75].
This article examines the mechanistic relationship between genetic evidence and clinical trial outcomes within the broader context of immune variation research. We explore how integrating genetic insights with environmental influences can inform more robust drug development strategies, ultimately bridging the translational gap for more effective therapies.
Quantitative Evidence: Genetic Support Correlates with Clinical Success
Landmark Analysis of 28,561 Stopped Trials
A comprehensive 2024 study published in Nature Genetics applied natural language processing to classify the reasons for discontinuation of 28,561 clinical trials that stopped before their planned endpoints [75]. The research integrated this classification with genetic evidence from platforms like Open Targets and animal models from the International Mouse Phenotyping Consortium, revealing striking patterns:
Table 1: Genetic Evidence and Clinical Trial Outcomes from 28,561 Stopped Trials [75]
| Trial Outcome Category | Genetic Evidence Support (OR) | P-value | Mouse Model Evidence (OR) | P-value |
|---|---|---|---|---|
| All Stopped Trials | 0.73 | 3.4 × 10⁻⁶⁹ | - | - |
| Negative Outcome (e.g., Lack of Efficacy) | 0.61 | 6 × 10⁻¹⁸ | 0.7 | 4 × 10⁻¹¹ |
| Safety or Side Effects | - | - | - | - |
| Insufficient Enrollment | Moderate depletion | - | - | - |
| COVID-19 Related | No association | - | - | - |
The data demonstrates that trials halted due to negative outcomes, particularly lack of efficacy, showed the most significant depletion of genetic support for their intended pharmacological targets [75]. This association remained consistent across both oncology and non-oncology indications and was observed for both human population genetics and genetically modified animal models [74].
The Broader Landscape: Genetic Support in Successful Drug Development
The protective effect of genetic evidence extends beyond failure analysis. Previous research has established that human genetic support doubles the likelihood of a drug program progressing from phase to phase in clinical development [75]. This correlation culminates in real-world impact: approximately two-thirds of drugs approved by the FDA in 2021 had support from human genetic evidence [75]. This compelling statistic underscores why genetics has become increasingly integral to target selection and validation in both academic and industry settings.
The Biological Nexus: Genetic-Environmental Interactions in Immune Variation
Genetic-Environmental Interplay in Immune Response
The relationship between genetics and clinical outcomes must be understood within the broader framework of immune variation, where genetic factors interact dynamically with environmental influences. A seminal 2024 study in Nature Immunology quantified these interactive effects using "rewilded" mouse models, providing experimental evidence for how genotype-environment interactions shape immune responses [6].
The study compared inbred mouse strains (C57BL/6, 129S1, and PWK/PhJ) in both controlled laboratory settings and natural outdoor environments, then infected them with the parasite Trichuris muris [6]. Key findings included:
- Cellular composition was shaped by interactions between genotype and environment
- Cytokine response heterogeneity, including IFNγ concentrations, was primarily driven by genotype, with direct consequences for parasite burden
- Genetic differences observed under laboratory conditions were often reduced following rewilding, demonstrating how environmental exposure can modulate genetic effects
Implications for Clinical Trial Design
These findings have profound implications for clinical trial design. The rewilding experiments revealed that some genetic differences in immune response only emerge in specific environmental contexts [6]. For instance, rewilded C57BL/6 mice mounted a stronger T helper 1 cell (T_H1) response to infection compared to other strains—a difference not observed in laboratory conditions [6]. This suggests that clinical trials conducted in highly controlled settings might miss crucial gene-environment interactions that determine real-world therapeutic efficacy.
Table 2: Key Findings from Rewilded Mouse Study on Immune Variation [6]
| Immune Trait | Primary Driver | Key Finding | Clinical Translation Insight |
|---|---|---|---|
| PBMC Composition | Genotype × Environment Interaction | Variance between strains changed with environment | Trial populations need diverse environmental backgrounds |
| IFNγ Response | Genotype | Directly affected worm burden | Genetic screening may predict responders |
| CD44 on T cells | Genetics | Expression differed by strain in lab | Target selection benefits from genetic validation |
| CD44 on B cells | Environment | Expression changed with rewilding | Environmental factors can modify target expression |
| T_H1 Response | Genotype × Environment × Infection | Emerged only in rewilded infected mice | Controlled trials may miss efficacy signals |
Mechanistic Insights: How Genetics Informs Target Selection and Safety
Efficacy: Prioritizing Causally Implicated Targets
Genetic evidence helps de-risk clinical development primarily by identifying targets with causal roles in disease pathogenesis. Genome-wide association studies (GWAS) have identified hundreds of risk loci for various conditions, with the strongest associations often found within the major histocompatibility complex (MHC) region [54]. These genetic signatures point to biological pathways and mechanisms directly relevant to human disease biology, unlike targets selected solely based on animal models which may not recapitulate human pathophysiology [73].
The 2024 Nature Genetics study found that trials stopped for lack of efficacy showed significantly less support not only from human genetics but also from genetically modified mouse models [75]. This dual validation across species strengthens the target hypothesis and increases confidence in the therapeutic mechanism.
Safety: Predicting Target-Related Toxicity
Genetic evidence also informs safety assessments. The same study revealed that trials stopped for safety reasons were associated with specific target characteristics [75]:
- Highly constrained genes (intolerant to loss-of-function mutations) were more likely to be linked to safety-related trial stoppages
- Broad tissue expression of drug targets was associated with increased safety concerns
- Targets with multiple protein interactions presented higher safety risks
These findings suggest that human population genetics can help identify target-related safety liabilities early in the development process, potentially avoiding costly late-stage failures due to adverse events.
Methodological Approaches: Integrating Genetics into the Development Pipeline
Experimental Workflow for Genetic Target Validation
Diagram 1: Genetic target validation workflow for clinical translation
NLP Classification of Trial Failure Reasons
The 2024 study employed a sophisticated natural language processing (NLP) pipeline to classify clinical trial stoppage reasons at scale [74] [75]. The methodology included:
- Training Data Curation: 3,571 manually classified trials with stop reasons categorized into 17 classes
- Model Fine-tuning: BERT model fine-tuned for clinical trial classification
- Validation: Cross-validation (Fmicro = 0.91) and additional manual curation of 1,675 unseen stop reasons
- Application: Classification of 28,561 stopped trials from ClinicalTrials.gov
This approach enabled high-throughput analysis of trial failures while overcoming publication bias toward positive results, creating a robust dataset for retrospective analysis of failure patterns [75].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Resources for Genetic-Clinical Translation Studies
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Genetic Databases | Open Targets Platform, Open Targets Genetics, GWAS Catalog | Access human genetic associations and variant functional annotations |
| Animal Model Resources | International Mouse Phenotyping Consortium (IMPC), Jackson Laboratory | Validate targets in genetically modified animal models |
| Clinical Trial Registries | ClinicalTrials.gov, EU Clinical Trials Register | Access trial protocols, outcomes, and termination reasons |
| Bioinformatics Tools | BERT NLP models, Statistical genetics software (PLINK, FINEMAP) | Analyze genetic data and classify trial outcomes at scale |
| Experimental Models | Inbred mouse strains (C57BL/6, 129S1, PWK/PhJ), Rewilding facilities | Study gene-environment interactions in controlled and natural settings |
Strategic Implementation: Bridging the Valley of Death
Integrating Genetics into Therapeutic Development
To effectively leverage genetic evidence in drug development, researchers should:
- Incorporate genetic validation early in target selection processes, using platforms like Open Targets to assess genetic support for target-disease pairs [75]
- Consider target safety profiles using constraint metrics (e.g., gNOF LOEUF scores) and tissue expression data to identify potential safety liabilities [75]
- Account for environmental context in trial design, recognizing that genetic effects may be modulated by environmental factors as demonstrated in rewilding experiments [6]
- Apply multidimensional evidence integration, combining human genetics, functional genomics, and animal model data to build stronger therapeutic hypotheses
A Framework for Genetic-Environmental Integration in Clinical Translation
Diagram 2: Genetic-environmental interplay in disease pathogenesis and treatment
The integration of human genetic evidence into therapeutic development represents a powerful strategy for addressing the persistent "valley of death" in clinical translation. The robust correlation between genetic support and clinical trial success, demonstrated through large-scale analyses of tens of thousands of trials, provides a compelling roadmap for more efficient drug development [74] [75].
Furthermore, recognizing that genetic effects operate within environmental contexts—as illustrated by rewilding experiments—adds crucial nuance to our understanding of therapeutic efficacy [6]. This genetic-environmental interplay is particularly relevant in immune-related diseases, where dysregulation arises from complex interactions between inherited susceptibility factors and environmental exposures [54].
As the field advances, integrating multidimensional evidence from human genetics, functional genomics, and environmental studies will be essential for building more accurate models of disease pathogenesis and treatment response. This integrative approach promises to narrow the translational gap, delivering more effective therapies to patients while reducing the staggering attrition rates that have long plagued drug development.
Decoding Genotype-by-Environment (GxE) Interactions in Complex Disease Models
The pathogenesis of complex diseases is not dictated solely by genetic predisposition or environmental exposure but by the dynamic interplay between them. Genotype-by-Environment (GxE) interactions represent a fundamental paradigm for understanding how an individual's genetic background modulates physiological responses to environmental factors, thereby influencing disease susceptibility and progression. This is particularly salient in immune variation research, where the immune system exhibits remarkable plasticity in response to environmental challenges, shaped by genetic architecture. Autoimmune diseases, for instance, affect an estimated 7–10% of the global population and arise from convergent genetic susceptibility, environmental exposures, and immune dysregulation [54]. Despite identification of hundreds of risk loci through genome-wide association studies (GWAS), genetics alone cannot predict disease onset, highlighting the essential role of environmental triggers such as infections, diet, microbiome alterations, and hormonal influences [54].
Statistical genetic models of GxE interaction have evolved to address both dichotomous environments (e.g., sex, disease status) and continuous environments (e.g., physical activity, socioeconomic measures) [76] [77]. Contemporary research has progressed beyond simple interaction detection to developing sophisticated polygenic models that quantify how genetic effects underlying complex traits respond dynamically to environmental spectra. This technical guide synthesizes current methodologies, analytical frameworks, and experimental findings to provide researchers and drug development professionals with comprehensive tools for investigating GxE interactions in complex disease models, with particular emphasis on immune system variation.
Statistical Methodologies for Detecting GxE Interactions
Variance Quantitative Trait Loci (vQTL) Detection Methods
Variance Quantitative Trait Loci (vQTL) represent genomic regions where genetic variants are associated with phenotypic variance rather than the mean, potentially indicating underlying GxE or gene-gene (GxG) interactions. Identifying vQTLs prior to direct interaction analyses reduces multiple testing burden and can detect interactions without measured environmental data [78].
Table 1: Comparison of Parametric and Non-Parametric vQTL Detection Methods
| Method | Type | Key Principle | Advantages | Limitations |
|---|---|---|---|---|
| Brown-Forsythe (BF) Test | Parametric | Tests dispersion differences across genotype groups using medians | Robust to outliers | Severe false positive inflation with MAF <0.2 [78] |
| Deviation Regression Model (DRM) | Parametric | Regresses absolute deviations from phenotypic mean on genotype dosages | Allows continuous predictors; generally recommended parametric method [78] | Performance depends on proper mean modeling |
| Double Generalized Linear Model (DGLM) | Parametric | Jointly models mean and variance components | Most powerful for normally distributed traits [78] | Invalid for non-normally distributed traits [78] |
| Kruskal-Wallis (KW) Test | Non-parametric | Ranks absolute deviations from group medians across genotypes | Robust to outliers and trait distribution; recommended non-parametric method [78] | Less powerful than parametric methods for normal traits |
| Quantile Integral Linear Model (QUAIL) | Non-parametric | Assesses genetic effects on variability via quantile regression | Valid under non-normality; allows covariate adjustment [78] | Computationally intensive; suboptimal power [78] |
Simulation studies comparing these methods demonstrate that the Deviation Regression Model (DRM) and Kruskal-Wallis test (KW) are the most recommended parametric and non-parametric tests, respectively [78]. The choice between parametric and non-parametric approaches should be guided by trait distribution, with parametric methods generally preferred for normally distributed traits and non-parametric methods offering greater robustness for non-normal distributions or presence of outliers.
Advanced Polygenic Modeling Approaches
For related individuals, linear mixed models incorporating polygenic effects provide a powerful framework for GxE investigation. The base polygenic model decomposes phenotypic covariance (Σ) into additive genetic and residual environmental components: Σ = Kσ²g + Iσ²e, where K is the genetic relationship matrix, σ²g is the additive genetic variance, I is the identity matrix, and σ²e is the environmental variance [77]. Heritability (h²) is estimated as σ²g/σ²p, where σ²p is the total phenotypic variance.
Extensions to this model enable formal testing of GxE interactions:
GxE for Dichotomous Environments: The G×Sex model estimates sex-specific additive genetic variances (σ²gf, σ²gm) and environmental variances (σ²ef, σ²em), along with the across-sex genetic correlation (ρGf,m). Evidence for G×E emerges when genetic variances differ between groups (σ²gf ≠ σ²gm) and/or the genetic correlation deviates from unity (ρGf,m < 1) [77].
GxE for Continuous Environments: Variance and correlation functions model how genetic parameters change along an environmental gradient: σ²g = exp(αg + γg(qi - q̄)) for variance, and ρg = exp(-λg|qi - qj|) for correlation, where q represents the environmental variable [77]. The null hypotheses of variance homogeneity (γg = 0) and perfect genetic correlation (λg = 0) can be tested using likelihood ratio tests.
Joint Modeling of Multiple Environments: Novel unified models simultaneously incorporate both dichotomous and continuous environments, such as joint genotype-by-sex and genotype-by-social determinants of health (SDoH) interactions, revealing complex patterns not detectable through separate analyses [77].
GxE Conceptual Framework: This diagram illustrates the core concept of GxE interactions, where genetic and environmental factors jointly influence phenotypic expression, which in turn affects disease outcomes.
Polygenic Risk Score (PRS) Models Incorporating GxE
Integrating GxE interactions into Polygenic Risk Score (PRS) models enhances their predictive accuracy and biological interpretability. The GxEprs method addresses limitations of previous approaches by minimizing spurious signals and model misspecification:
For Quantitative Traits (GxEprs_QT): y = â₁X̂add + â₂E + â₃(X̂gxe ⊙ E) + â₄X̂gxe + ε, where X̂add and X̂gxe are PRSs based on main additive and interaction effects, E is the environmental variable, and ⊙ represents element-wise multiplication [79].
For Binary Traits (GxEprs_BT): A generalized linear model with binomial distribution and logit link incorporates similar terms for binary outcomes [79].
Application of these models to obesity-related traits in the UK Biobank demonstrated significant GxE interactions, with enhanced prediction accuracy for body mass index (BMI), waist-hip ratio, body fat percentage, and waist circumference [79].
Experimental Approaches for Dissecting GxE in Immune Variation
Rewilding Mouse Models of Immune Variation
Controlled experiments with "rewilded" laboratory mice introduced into natural outdoor environments provide a powerful approach to quantify genetic, environmental, and interactive contributions to immune variation. This paradigm exposes genetically diverse inbred strains (e.g., C57BL/6, 129S1, PWK/PhJ) to natural environmental challenges, including pathogen exposure [6].
Table 2: Key Research Reagents and Solutions for Rewilding Immune Studies
| Reagent/Solution | Function/Application | Key Findings in Rewilding Context |
|---|---|---|
| C57BL/6, 129S1, PWK/PhJ inbred strains | Genetically diverse mouse models | Strains differ by up to 50 million SNPs/indels; show differential immune responses to rewilding [6] |
| Trichuris muris embryonated eggs | Parasitic infection challenge | Reveals genotype-dependent differences in TH1 response and worm burden in rewilding conditions [6] |
| Spectral cytometry with lymphocyte panel | High-dimensional immune phenotyping | Identifies environment-driven changes in PBMC composition and CD44 expression patterns [6] |
| Multivariate Distance Matrix Regression (MDMR) | Statistical analysis of high-dimensional data | Quantifies contributions of genotype, environment, infection, and their interactions to immune variation [6] |
| Peripheral Blood Mononuclear Cells (PBMCs) | Longitudinal immune monitoring | Enables tracking of immune cell dynamics in response to environmental change and infection [6] |
The experimental workflow typically involves: (1) random assignment of mice to laboratory control or rewilding conditions; (2) acclimatization for 2 weeks; (3) infection with T. muris or sham treatment; (4) additional 3-week exposure period; and (5) comprehensive immune phenotyping [6]. This design enables quantification of the relative contributions of genotype, environment, infection, and their interactions through multivariate statistical approaches.
Analytical Workflow for GxE in Immune Traits
GxE Immune Research Workflow: This experimental workflow outlines key stages in investigating GxE interactions in immune variation, from data collection through biological interpretation.
GxE Findings in Complex Disease Pathogenesis
Autoimmune Disease Mechanisms
Autoimmune diseases exemplify the confluence of genetic susceptibility and environmental triggers in disease pathogenesis. GWAS have identified hundreds of risk loci, with the strongest associations in the major histocompatibility complex (MHC) region, particularly HLA class II alleles [54]. Non-MHC genes such as PTPN22, STAT4, and CTLA4 further contribute to autoimmune risk [54].
Notable GxE interactions in autoimmunity include:
Sex and Immune Response: Females account for nearly 80% of autoimmune cases, with estrogens enhancing humoral responses and X-chromosome immune genes contributing to heightened immune reactivity [54].
Infectious Triggers: Epstein-Barr virus (EBV) infection is implicated in systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and Sjögren's syndrome, while SARS-CoV-2 infection has been associated with various autoimmune manifestations [54].
Dietary Factors: Gluten exacerbates intestinal inflammation in susceptible individuals with Crohn's disease, while dietary antigens can trigger mucosal immune dysregulation through interactions with host genetics and microbiota [54].
Obesity-Mediated Inflammation: Adipose tissue releases proinflammatory cytokines (IL-6, leptin) that promote Th17 differentiation and impair regulatory T cell (Treg) function, creating a pro-autoimmune environment [54].
Psychiatric and Metabolic Disorders
Depression demonstrates complex GxE patterns, with social determinants of health (SDoH) interacting with genetic predisposition. Research using the Beck Depression Inventory-II (BDI-II) and AHC HRSN screen for SDoH revealed that depression is influenced by joint G×Sex and G×SDoH interaction effects, where genetic susceptibility to depression is modulated by both sex and socioeconomic environment [77].
For metabolic traits, GxEprs models applied to UK Biobank data identified significant interactions between polygenic risk for obesity-related traits and lifestyle factors including healthy diet, physical activity, and alcohol consumption [79]. These findings demonstrate that environmental modifications can substantially alter genetic risk expression for metabolic conditions.
Methodological Considerations and Future Directions
Analytical Challenges and Solutions
GxE research faces several methodological challenges that require careful consideration:
Environmental Measurement: Precise quantification of environmental exposures remains challenging. High-dimensional environmental data (e.g., daily weather metrics from NASA POWER) can characterize environmental contexts more comprehensively but increase model complexity [80].
Population Diversity: Most GxE studies focus on European ancestry populations, creating disparities in knowledge and clinical application. African populations exhibit unique genetic variability and environmental exposures, offering unparalleled opportunities for GxE discovery but remaining underrepresented [81].
Multiple Testing Burden: Genome-wide interaction analyses incur severe multiple testing penalties. Prioritizing variants through vQTL screening or functional annotation can mitigate this burden [78].
Model Misspecification: Incorrect assumptions about the functional form of GxE can generate spurious findings. Flexible modeling approaches, including quantile regression and machine learning methods, offer robustness to misspecification [78] [79].
Translational Applications and Precision Environmental Health
The ultimate goal of GxE research lies in translating findings into personalized prevention and treatment strategies. Key applications include:
Precision Medicine: Integrating GxE information into clinical risk prediction enables stratification of individuals based on both genetic susceptibility and environmental responsiveness [79] [21].
Therapeutic Targeting: Identifying GxE mechanisms reveals novel therapeutic targets, such as IL-2 receptor signaling in Treg dysfunction for autoimmune diseases [54].
Public Health Interventions: Understanding GxE interactions informs targeted environmental modifications for high-genetic-risk subpopulations, maximizing intervention efficiency [21].
Drug Development: Incorporating GxE considerations in clinical trial design may identify subgroup-specific treatment effects and reduce late-stage failure rates [6].
Future directions in GxE research will leverage multi-omics integration, advanced computing methods like artificial intelligence and machine learning, and large-scale diverse cohorts to elucidate the complex interplay between genetic and environmental factors in disease etiology [21] [81]. This integrated approach promises significant advancements in personalized diagnostics, therapeutics, and preventive strategies across the spectrum of complex diseases.
Overcoming Cellular and Tissue Specificity in Target Validation
Target validation represents a critical, early-phase bottleneck in the drug discovery pipeline, with many potential therapeutics failing in clinical trials due to insufficient demonstration of efficacy and safety. A significant challenge in this process is accounting for the profound influence of cellular and tissue specificity, which governs how targets function within their native physiological contexts. This technical guide examines advanced methodologies for overcoming these specificity challenges, framed within the established scientific framework that recognizes immune variation as stemming from complex, dynamic interactions between genetic predisposition and environmental exposures. By integrating cutting-edge profiling techniques, sophisticated model systems, and computational approaches, researchers can deconvolute these influences to build robust evidence for therapeutic targets, ultimately increasing the success rate of drug development programs.
The immune system demonstrates remarkable heterogeneity across individuals, tissues, and cellular compartments. This variation arises from the complex interplay between genetic background and environmental exposures, creating a moving target for therapeutic development. Cellular and tissue specificity in target validation refers to the need to demonstrate that a potential therapeutic target is relevant, accessible, and functionally modifiable within its precise physiological context—and that this relevance holds across the diverse immune landscapes present in a patient population.
The consequences of ignoring this complexity are severe. Drugs that show promise in simplified in vitro systems or genetically homogeneous animal models often fail in human trials because they do not account for the context-dependent nature of target biology [82]. Furthermore, as precision medicine advances, understanding how genetic and environmental factors shape individual immune responses becomes paramount for developing targeted therapies that work for specific patient subpopulations [64].
Recent research has quantitatively demonstrated that both genetic and environmental factors significantly contribute to immune variation. One study using rewilded mice found that cellular composition was shaped by interactions between genotype and environment, while cytokine response heterogeneity was primarily driven by genotype [6]. This foundational understanding informs the modern approach to target validation: we must develop methods that capture and reconcile these diverse influences to identify genuinely druggable targets with acceptable therapeutic windows.
Quantitative Foundations: Genetic and Environmental Contributions to Immune Variation
Understanding the relative contributions of genetic and environmental factors to immune phenotypes provides a quantitative framework for designing targeted validation strategies. The following table summarizes key findings from recent studies that have quantified these influences:
Table 1: Quantitative Contributions of Genetic and Environmental Factors to Immune Variation
| Immune Trait | Primary Influence | Key Findings | Experimental Model |
|---|---|---|---|
| Cellular Composition | Genotype × Environment Interaction | PBMC composition showed significant Gen × Env interactions; variance between lab-housed strains reduced after rewilding [6]. | Rewilded inbred mouse strains (C57BL/6, 129S1, PWK/PhJ) |
| Cytokine Response (e.g., IFNγ) | Primarily Genotype | Genotype primarily drove IFNγ concentration variation, with consequences for parasitic worm burden [6]. | Rewilded inbred mouse strains infected with Trichuris muris |
| CD44 Expression on T cells | Primarily Genetics | Expression explained mostly by genetics on T cells across all tested strains [6]. | Rewilded inbred mouse strains |
| CD44 Expression on B cells | Primarily Environment | Expression explained more by environment than genetics across all strains [6]. | Rewilded inbred mouse strains |
| T Cell Transcriptional Programs | Age | Core naive CD4 T cells showed 331 age-related differentially expressed genes (DEGs) without frequency changes [83]. | Human PBMCs from donors (25-90 years) |
| Circulating Protein Levels | Age | 69 proteins differentially expressed with age (65 increased, 4 decreased); patterns persisted over time [83]. | Longitudinal human cohort (2 years follow-up) |
These quantitative relationships highlight that the relative importance of genetic versus environmental factors is trait-specific and context-dependent. Consequently, target validation strategies must be tailored accordingly—for instance, targets based on genetic associations require validation across diverse environmental conditions, while those informed by environmental exposures need testing across genetic backgrounds.
Advanced Methodologies for Context-Aware Target Validation
Functional Analysis in Complex Model Systems
Overcoming specificity challenges requires moving beyond traditional, oversimplified cell lines to models that better recapitulate the in vivo environment:
Cell- and Tissue-Specific Aptamer Selection: This protocol uses living mammalian cells and tissues as selection targets for identifying DNA or RNA aptamers. The process involves iterative rounds of selection to enrich for nucleic acids that bind specifically to unique molecular signatures on target cells within complex mixtures. The resulting aptamers serve as powerful tools for validating target accessibility and function in native contexts [84].
Rewilded Mouse Models: Conventional laboratory housing minimizes environmental variation, potentially masking important genotype-environment interactions. The rewilding approach introduces laboratory mice (including diverse inbred strains like C57BL/6, 129S1, and PWK/PhJ) into outdoor enclosures, exposing them to natural microbes, pathogens, and environmental stressors. This model recapitulates the immune variation seen in human populations and reveals context-dependent genetic effects that are invisible in sterile laboratory conditions [6].
3D Cultures and Co-culture Systems: These models preserve tissue architecture and cell-cell interactions that influence target expression and function. Incorporating human induced pluripotent stem cells (iPSCs) from diverse genetic backgrounds further enables assessment of how human genetic variation affects target biology in disease-relevant tissues [82].
Expression Profiling Across Contexts
Comprehensive expression analysis establishes where and when targets are present and accessible:
Spatial Expression Mapping: Determine target expression patterns across healthy and diseased tissues, correlating expression levels with disease progression or exacerbation. This identifies potential on-target toxicities in healthy tissues and verifies target presence in disease-relevant compartments [82].
Temporal Dynamics Assessment: Track target expression and modification over time, through disease progression, and in response to therapeutic interventions. Longitudinal profiling reveals whether targets are consistently present or dynamically regulated, informing treatment timing and duration [83].
Biomarker Identification and Validation
Biomarkers provide measurable indicators of target engagement and biological activity:
Multi-omic Biomarker Discovery: Combine transcriptomics (e.g., qPCR platforms), proteomics (e.g., Luminex, Olink), and high-dimensional flow cytometry to identify composite biomarker signatures that reflect target activity in specific cell types or tissues [83] [82].
Pharmacodynamic Biomarker Development: Establish biomarkers that demonstrate both target modulation (proof of mechanism) and downstream biological effects (proof of concept) in response to therapeutic intervention [85].
Integrated Experimental Workflows
Workflow for Cell-Specific Target Validation
The following diagram illustrates a comprehensive workflow for validating targets in specific cellular contexts, integrating multiple methodologies to address specificity challenges:
Diagram 1: Target validation workflow.
Signaling Pathway Analysis for Target Validation
Understanding how targets function within signaling networks is crucial for validation. The following diagram illustrates a generalized approach to analyzing target function within immune signaling pathways, with particular relevance to autoimmune diseases where regulatory T cell (Treg) dysfunction plays a key role:
Diagram 2: Signaling pathway for target validation.
This pathway highlights how targeting specific nodes (e.g., enhancing GRAIL to stabilize IL-2R signaling) can restore immune homeostasis in autoimmune conditions—a validation approach that accounts for cellular context and genetic variation in signaling components [54].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for Target Validation
| Tool Category | Specific Examples | Function in Target Validation |
|---|---|---|
| Cell-Specific Selection | Cell-SELEX DNA/RNA libraries; Cell-based aptamer selection [84] | Identifies molecules binding specific cell types in complex mixtures for delivery or diagnostic applications |
| Complex Model Systems | Rewilded mouse models [6]; 3D co-cultures; iPSC-derived cells [82] | Provides physiologically relevant contexts that preserve tissue architecture and cell-cell interactions |
| Multi-omic Profiling | scRNA-seq (10x Genomics); High-plex proteomics (Olink); Spectral flow cytometry [83] | Enables deep characterization of cellular heterogeneity and target expression across contexts |
| Genetic Modulation | CRISPR-based tools; RNAi; Tool compounds (agonists/antagonists) [82] | Establishes causal relationship between target and disease phenotype through functional perturbation |
| Biomarker Assays | qPCR platforms; Luminex; Protein analyte detection [82] | Measures target engagement and downstream pharmacological effects |
| Computational Tools | Multi-physiology modeling; QSP models; AI/ML approaches [85] | Integrates diverse data types to predict target behavior in different genetic and environmental contexts |
Discussion and Future Perspectives
Overcoming cellular and tissue specificity challenges requires a fundamental shift in target validation philosophy—from viewing targets as static entities to understanding them as dynamic components within complex, adaptive systems. The integration of genetic and environmental context into validation workflows is not merely an enhancement but a necessity for successful drug development.
Future directions in this field will likely include:
Multi-physiology Modeling: The emerging approach of "multi-physiology modeling" integrates omics-based and dynamic systems modeling with pharmacometrics to create predictive simulations of how targets behave across different physiological systems and individual patients [85]. This computational framework helps reconcile the dichotomy between data-driven and mechanistic modeling approaches.
Global Immune Monitoring Initiatives: Projects like the Human Immunome Project aim to generate the largest immunological dataset ever created, mapping human immune variation across diverse global populations. This resource will power predictive models of immune system behavior, dramatically improving our ability to validate targets across genetic and environmental contexts [29].
Advanced Biomarker Development: Next-generation biomarkers will need to capture not just target presence but also its functional state, accessibility, and role within signaling networks. Composite biomarker signatures derived from multi-omic profiling will provide more comprehensive assessments of target validity [83] [85].
The path forward requires breaking down traditional silos between genetics, immunology, and pharmacology. By embracing integrated approaches that account for the profound complexity and variability of the human immune system, researchers can overcome specificity challenges in target validation and deliver more effective, precise therapeutics to patients.
Strategies for Managing Polygenicity and Small Effect Sizes in Complex Traits
Complex traits, including most immune-mediated diseases, do not follow simple Mendelian inheritance patterns but are instead influenced by numerous genetic and environmental factors. The polygenic architecture of these traits means they are affected by thousands of genetic variants, each with typically small effect sizes, alongside substantial environmental influences [86]. Understanding this complex interplay is crucial for advancing personalized medicine and therapeutic development. The challenge for researchers lies in developing statistical and experimental strategies that can properly model this polygenic architecture and environmental context to improve trait prediction and mechanistic understanding.
This technical guide examines sophisticated approaches for dissecting complex traits, with particular emphasis on immune variation—a domain where genotype-environment interactions (G × E) significantly influence phenotypic outcomes [6]. We explore statistical methods for handling polygenicity, experimental designs for capturing environmental influences, and computational tools for simulating complex trait architectures. The integration of these strategies provides a powerful framework for addressing one of the most challenging problems in modern genetics.
Statistical Methods for Polygenic Analysis
Polygenic Score Methodologies
Polygenic scores (PGS) have emerged as a fundamental tool for quantifying an individual's genetic predisposition for complex traits. At their core, PGS methodologies aim to aggregate the effects of numerous genetic variants across the genome into a single predictive measure [86]. These approaches can be broadly categorized based on their underlying assumptions about the genetic architecture of traits.
Sparse modeling methods assume that only a small proportion of single nucleotide polymorphisms (SNPs) have non-zero effects on the trait, with the majority having no effect. This approach is mathematically represented by a point-normal distribution where effect sizes (βj) follow a mixture distribution: βj ~ πN(0, σ²β) + (1-π)δ0, where π represents the small proportion of causal variants [86]. In contrast, polygenic modeling methods operate under the normal assumption that all SNPs have non-zero effects, with each effect size following a normal distribution: βj ~ N(0, σ²β) [86]. This framework, also known as the infinitesimal model, forms the basis for methods such as linear mixed models (LMMs), ridge regression, and genomic best linear unbiased prediction (GBLUP).
Table 1: Comparison of Polygenic Score Methods and Their Applications
| Method Category | Key Assumptions | Representative Methods | Best-Suited Trait Architectures |
|---|---|---|---|
| Sparse Methods | Few causal variants with non-zero effects | LASSO, Bayesian Sparse Models | Traits with concentrated genetic architecture |
| Polygenic Methods | Many causal variants with small, normally distributed effects | LMM, Ridge Regression, GBLUP | Highly polygenic traits, omnigenic models |
| Ancestry-Aware Methods | Effect sizes may vary across populations | Multi-ancestry PGS, Importance Reweighting | Traits with ancestry-specific effect sizes |
Advanced Modeling Considerations
More recent methodologies have addressed the critical challenge of ancestry-specific effects in polygenic prediction. The standard approach of developing PGS primarily in European-ancestry populations has led to substantially reduced predictive accuracy in non-European populations [87]. Advanced strategies now incorporate multiple ancestry groups during training, with techniques such as importance reweighting to balance the influence of underrepresented groups in mixed-ancestry datasets [87]. Research demonstrates that for some traits, PGS estimated using a relatively small African-ancestry training set can outperform on an African-ancestry test set PGS estimated using a much larger European-ancestry only training set [87].
The performance of these methods varies significantly across traits, influenced by factors such as heritability, causal effect size correlation across ancestries, and trait-specific genetic architecture. For highly polygenic traits with consistent effect sizes across populations (high trans-ancestry correlation), combined ancestry approaches generally outperform single-ancestry methods. However, for traits with substantial ancestry-specific effects or gene-environment interactions, targeted ancestry-specific modeling often yields superior results [87].
Experimental Designs for Capturing G × E Interactions
Rewilding Approaches in Model Systems
Controlled experimental designs that systematically manipulate both genetic background and environmental exposure are essential for quantifying G × E interactions. The "rewilding" paradigm using inbred mouse strains provides a powerful approach for this purpose [6]. In this design, genetically distinct mouse strains (e.g., C57BL/6, 129S1, and PWK/PhJ) are transferred from controlled laboratory conditions to outdoor enclosures, introducing natural environmental variation including diverse microbial exposures [6].
The experimental workflow typically involves: (1) genotypic variation through the use of multiple inbred strains; (2) environmental manipulation by transferring animals to natural environments; and (3) controlled challenges such as infection with parasites like Trichuris muris to measure immune responses [6]. This approach allows researchers to quantify how genetic differences shape responses to environmental changes, and conversely, how environmental exposures modulate the expression of genetic predispositions.
Table 2: Key Research Reagents and Experimental Components for Rewilding Studies
| Research Reagent | Specification/Strain | Function in Experimental Design |
|---|---|---|
| Mouse Strains | C57BL/6, 129S1, PWK/PhJ | Provide controlled genetic variation as inbred strains with known genotypes |
| Pathogen Challenge | Trichuris muris embryonated eggs (~200 eggs) | Standardized immune challenge to quantify response variation |
| Environmental Exposure | Outdoor enclosure with natural microbiota | Introduces complex environmental variables in controlled manner |
| CyTOF Panel | Lymphocyte-focused antibody panel | High-dimensional immune phenotyping of cellular composition |
| Genetic Analysis | Genome-wide SNP profiling | Links phenotypic variation to specific genetic variants |
Immune Stimulation in Human Cohort Studies
Complementary approaches in human studies involve ex vivo immune stimulation coupled with detailed molecular profiling. In one comprehensive design, monocytes from 134 human volunteers were treated with three distinct immune stimuli mimicking bacterial or viral infection [7]. Gene expression profiling at both early and late time points following stimulation allowed researchers to identify genetic variants whose effects on gene regulation differed depending on the immune activation state of the cells [7].
This approach revealed that genetic risk for autoimmune diseases such as lupus and celiac disease is enriched for context-dependent regulatory effects, supporting a paradigm where genetic disease risk may be driven not by constant cellular dysregulation, but by failed response dynamics to environmental challenges [7]. This has profound implications for understanding how genetic risk manifests only under specific environmental conditions.
Computational Tools for Simulating Complex Traits
Forward Evolutionary Simulation
Forward population genetic simulation represents an essential tool for exploring the properties of complex traits and evaluating statistical methods. ForSim is a flexible forward evolutionary simulation tool that models the consequences of evolution by phenotype, whereby demographic, behavioral, and selective effects mold genetic architecture over time [88]. Unlike coalescent approaches that work backward in time, forward simulation starts with an ancestral population and evolves it forward through generations, allowing for more complex modeling of selection, environmental effects, and population structure [88].
Key capabilities of ForSim include: (1) simulating multiple genes and chromosomes of arbitrary number and length; (2) modeling phenotype-based natural selection with user-specified functions; (3) incorporating environmental contributions to phenotypes; (4) simulating complex genetic interactions including pleiotropy and epistasis; and (5) modeling multiple populations with gene flow and assortative mating [88]. This flexibility enables researchers to generate data with known ground truth for evaluating the performance of PGS methods under various genetic architectures and evolutionary scenarios.
Simulation-Based Experimental Design
These simulation tools are particularly valuable for power calculations and study design optimization. Researchers can explore how factors such as sample size, ancestry composition, genetic architecture, and environmental heterogeneity affect the accuracy of polygenic prediction [88] [87]. For instance, simulations can quantify how the correlation of causal effect sizes between ancestry groups (ρ) influences the relative performance of single-ancestry versus multi-ancestry PGS methods [87].
Runtime considerations are important for forward simulation approaches. A simulation of a population of 10,000 individuals for 10,000 generations (roughly the age and effective population size of the human species) for a chromosome of 10 Mb containing 10 genes takes approximately 28 minutes on standard computing hardware [88]. This enables reasonably comprehensive exploration of parameter spaces while remaining computationally feasible.
Data Analysis and Visualization Approaches
Analytical Frameworks for High-Dimensional Data
The analysis of high-dimensional data generated from studies of complex traits requires specialized statistical approaches. Multivariate distance matrix regression (MDMR) provides a powerful framework for quantifying the contributions of genotype, environment, and their interactions to immune variation [6]. This method can handle complex spectral cytometry data from immune phenotyping and partition variance into components attributable to different factors.
For quantitative data analysis, both descriptive and inferential statistical methods are essential. Descriptive statistics (mean, median, variance, etc.) provide initial characterization of datasets, while inferential methods such as cross-tabulation, regression analysis, and hypothesis testing enable researchers to identify significant patterns and relationships [89]. These approaches are particularly important for detecting G × E interactions, which often manifest as statistically significant interaction terms in regression models.
Visualization Strategies
Effective data visualization is crucial for interpreting complex datasets in genetics and immunology. Standard approaches include Stacked Bar Charts for compositional data, Tornado Charts for preference analyses, Progress Charts for gap analyses, and Word Clouds for text data [89]. For high-dimensional immune phenotyping data, principal component analysis (PCA) plots are particularly valuable for visualizing how samples cluster based on genetic and environmental factors [6].
Specialized tools are available for different data types and analysis needs. R and Python provide flexible programming-based approaches for researchers with coding experience, while Tableau, Microsoft Power BI, and Datawrapper offer user-friendly interfaces for creating standard visualization types [90]. Network analysis tools such as Gephi and Cytoscape are valuable for visualizing genetic networks and interaction pathways [90].
Managing polygenicity and small effect sizes in complex traits requires an integrated approach combining sophisticated statistical methods, controlled experimental designs, and powerful computational tools. The most effective strategies acknowledge the context-dependent nature of genetic effects, particularly in immune traits where environmental exposures play a modifying role. Future methodological developments will need to better incorporate dynamic environmental factors, ancestry-specific effects, and multi-omics data to improve predictive accuracy and mechanistic understanding.
The rewilding paradigm in model organisms, coupled with multi-ancestry studies in humans and advanced simulation approaches, provides a robust framework for addressing these challenges. As these methods continue to evolve, they will enhance our ability to translate genetic discoveries into clinically actionable insights, ultimately advancing personalized medicine and therapeutic development for complex immune-mediated diseases.
Ethical and Practical Considerations in Diverse Population Biobanks
The pursuit of precision medicine is fundamentally linked to a comprehensive understanding of the genetic and environmental factors that contribute to human disease. Biobanks, as organized repositories of biological specimens and associated health data, have become indispensable resources for modern biomedical research [91] [92]. Their role in advancing our understanding of the molecular, cellular, and genetic basis of human disease is paramount. However, the historical over-reliance on populations of predominantly European ancestry has created significant knowledge gaps and health disparities [91] [93]. Establishing biobanks that adequately represent diverse populations is therefore not merely a logistical challenge but an ethical and scientific imperative. This is especially critical in the context of immune-mediated diseases, where the interplay between genetics and environment is a major source of interindividual variation [6] [94]. This guide provides a roadmap for researchers and drug development professionals to navigate the ethical and practical complexities of building and utilizing diverse biobanks, with a specific focus on their application in unraveling the genetic and environmental determinants of immune response.
Ethical and Social Framework
Foundational Ethical Principles
The establishment of biobanks serving underrepresented populations requires meticulous ethical and social planning that extends beyond logistical, legal, and economic considerations [91]. Key to this process is respecting the bodily autonomy of donors and safeguarding their rights throughout the research lifecycle [91]. This involves recognizing that participants are not merely sources of data but partners in the research endeavor. The principle of justice demands an equitable distribution of both the burdens and benefits of research, actively working to reverse the exclusion that has characterized many previous genomic studies [93]. Furthermore, the commitment to cultural sensitivity is essential to avoid exploitative practices and ensure that research honors the values and concerns of participant communities [91].
Informed Consent Models
Informed consent is a cornerstone of ethical biobanking, yet its application in long-term, data-driven research presents unique challenges.
- Dynamic Consent: This model facilitates ongoing engagement with donors, allowing them to adjust their permissions as research evolves or their personal preferences change. It requires maintaining communication channels and providing updates about new research initiatives or findings [91].
- Tiered Consent: This approach offers donors tailored choices regarding the use of their samples and data. Donors can set specific boundaries, for instance, permitting use for certain disease categories but not others, or restricting commercial applications [91].
A hybrid model that combines elements of both dynamic and tiered consent is often ideal, as it maximizes donor autonomy and control while allowing the biobank to adapt to new ethical and legal landscapes [91].
Community Engagement and Governance
Successful diverse biobanking initiatives are built on a foundation of robust community engagement. This involves actively involving community leaders and stakeholders in the planning, governance, and oversight of the biobank [91]. Such participatory governance structures help ensure that the biank's operations align with community values, priorities, and expectations. This collaborative approach is proven to foster trust and promote long-term sustainability by demonstrating a genuine commitment to partnership rather than extraction [91]. Engaging communities in the return of aggregate research findings also reinforces the value of their participation and contributes to public scientific literacy.
Practical Implementation and Global Landscape
Strategic Planning and Protocol Development
Establishing a diverse biobank requires a strategic and well-documented approach to several key operational areas:
- Sample and Data Collection: Develop standardized protocols for the collection, processing, and storage of a variety of biospecimens (e.g., blood, saliva, tissue) and their associated data, including clinical, lifestyle, and environmental information [92].
- Quality Management: Adhere to best practice guidelines from organizations like ISBER (International Society for Biological and Environmental Repositories) and OECD to ensure the analytical validity and reproducibility of research conducted with biobank samples [92].
- Data Integration and IT Infrastructure: Implement secure, scalable informatics systems capable of integrating genomic data with other data types, such as Electronic Health Records (EHRs), while ensuring data security and privacy [92] [95].
The table below summarizes the diversity approaches and key features of several leading national biobank projects that utilize whole-genome sequencing.
Table 1: Diversity and Scale in Major National Biobank Initiatives
| Biobank Name | Primary Population Focus | Sample Size (WGS) | Key Diversity Features | Notable Contributions |
|---|---|---|---|---|
| UK Biobank [95] | United Kingdom | ~500,000 | 93.5% European ancestry; includes African, South Asian, East Asian subgroups | Powerful resource for GWAS and rare variant discovery; highlights need for greater diversity. |
| All of Us [95] | United States | ~245,000 (target >1M) | 77% from groups historically underrepresented in biomedical research. | Actively addresses representation bias; facilitates inclusive precision medicine. |
| PRECISE (Singapore) [95] | Singaporean Chinese, Indian, Malay | Target 100,000+ | Focus on major Asian ethnic groups within Singapore. | Enables research on population-specific genetic variation and disease risk in Asian contexts. |
| Biobank Japan [95] | Japanese | ~14,000 (WGS) | Represents a distinct East Asian population. | Advanced understanding of disease genetics and drug targets in the Japanese population. |
| NPBBD-Korea [95] | Korean | Target 1,000,000 | Aims to create a comprehensive bio-big data resource for the Korean population. | Emerging resource for population-specific genetics and rare diseases in East Asians. |
Addressing Technical and Analytical Challenges
- Population Stratification: Genetic studies can produce spurious findings if they fail to account for underlying population structure. Confounding can occur if both the genotype and phenotype vary by ancestry [93]. Using genetic ancestry principal components as covariates in association analyses is a standard method to mitigate this bias.
- Data Comparability: For biobanks to serve as international resources, genetic annotations must be comparable and computable. This requires standardized genotyping, imputation, and analytical pipelines to ensure that meta-analyses across different biobanks are valid and interpretable [93].
Research Applications in Immune Variation
Investigating Genotype-Environment Interactions in Immunity
Understanding the relative contributions of genetics and environment to immune variation is a central challenge. Controlled experiments in mice provide a powerful model to dissect these interactions. The "rewilding" experimental paradigm, which exposes laboratory mice to natural environments, has been particularly informative [6].
- Experimental Protocol: Rewilding and Immune Challenge
- Objective: To quantify the interactive effects of genotype and environment on immune traits and parasite burden [6].
- Model Organisms: Inbred female mice of diverse genetic backgrounds (e.g., C57BL/6, 129S1, PWK/PhJ) [6].
- Procedure:
- Rewilding: Mice are randomly assigned to either conventional laboratory housing ("Lab") or an outdoor enclosure ("Rewilded") for a set period (e.g., 2 weeks) [6].
- Infection: Mice are infected with a pathogen such as the intestinal helminth Trichuris muris [6].
- Analysis: After a further period (e.g., 3 weeks), immune phenotypes are analyzed. This can include:
- Immune Cell Composition: Using high-dimensional spectral cytometry of peripheral blood mononuclear cells (PBMCs) and unsupervised clustering to identify cell populations [6].
- Cytokine Response: Measuring concentrations of key cytokines like IFNγ [6].
- Parasite Burden: Quantifying worm load to assess functional outcome [6].
- Statistical Analysis: Multivariate distance matrix regression (MDMR) is used to quantify the relative contributions of genotype, environment, infection, and their interactions to the observed immune variation [6].
Table 2: Key Research Reagents for Immune Phenotyping in Biobank-Scale Studies
| Reagent / Tool Category | Specific Examples | Function in Experimental Protocol |
|---|---|---|
| Cytometry Panels | Lymphocyte panel (CD4, CD8, B220, TCRβ, CD44, Ki-67, T-bet) [6] | High-dimensional immunophenotyping to characterize immune cell composition and activation states. |
| Cytokine Assays | IFNγ measurement [6] | Quantifying protein-level immune responses to infection or stimulation. |
| Genetic Mapping Tools | SNP arrays, Whole Genome/Exome Sequencing [96] [97] | Genotyping participants to enable genome-wide association studies (GWAS) and heritability analysis. |
| Clinical Blood Analysis | Complete Blood Count with Differential (CBC/DIFF) [6] | Standard clinical assessment of circulating immune cell populations. |
Key Findings from Immune Variation Studies
Research integrating genetic data from biobanks with deep immune phenotyping has yielded several critical insights:
- Differential Heritability of Immune Traits: Immune traits are variably heritable. For example, cytokine responses (e.g., IFNγ) can be primarily driven by genotype, whereas immune cell composition is often more shaped by interactions between genotype and environment (Gen × Env) [6].
- Context-Dependent Genetic Effects: The impact of genetics is not static. Genetic differences observed in controlled laboratory environments can be reduced or altered following exposure to a complex natural environment ("rewilding") [6]. Conversely, some genetic effects on immune response, such as a stronger Th1 response in C57BL/6 mice, may only emerge in these complex environments [6].
- Tissue and Cell-Specific Regulation: Genetic control can be highly specific. For instance, the expression of markers like CD44 on T cells may be largely genetically determined, while its expression on B cells may be more influenced by environment [6].
- Continuum of Variation: In humans, the overall makeup of the immune system in healthy individuals appears to be organized as a continuum rather than falling into discrete clusters, with variations influenced by age, gender, BMI, and cytomegalovirus (CMV) infection status [94].
Visualizing the Research Workflow
The following diagram illustrates the logical workflow and key interactions in a study designed to dissect genetic and environmental influences on immune variation, as exemplified by the rewilding mouse model.
Diagram 1: Immune Variation Study Framework. This diagram outlines the core components of a study investigating genetic and environmental contributions to immune variation. It shows how both genotype and environment have direct effects on the immune phenotype, but also interact with each other. This interaction, along with the direct effects, shapes the final immune phenotype, which in turn determines the functional outcome, such as resistance or susceptibility to infection.
The development and utilization of diverse population biobanks represent a critical evolution in biomedical research, directly addressing the limitations of historically homogenous datasets. By integrating robust ethical frameworks—centered on dynamic consent, community engagement, and cultural sensitivity—with advanced technical protocols for sample handling and genomic analysis, these resources empower scientists to conduct more rigorous and inclusive research. The application of diverse biobanks to the study of immune variation has already demonstrated the profound context-dependency of genetic effects, highlighting that the genetic regulation of immunity cannot be fully understood without considering environmental exposures. As large-scale, diverse biobanks like All of Us and PRECISE continue to mature, they will dramatically enhance our ability to identify population-specific disease risks, develop targeted therapies, and ultimately advance the goal of equitable precision medicine for all global populations.
Evidence in Action: Validating Genetic Insights Across Diseases and Therapeutic Areas
The clinical presentation of COVID-19 ranges from asymptomatic infection to critical illness and death. While advanced age, sex, and comorbidities are established risk factors, they alone cannot explain the extensive interindividual variability in disease outcomes. This case study examines how host genetic factors, operating within a framework of genetic-environmental interactions, significantly influence SARS-CoV-2 immune responses and disease severity. Drawing on recent genome-wide association studies (GWAS) and functional genomic analyses, we detail specific genetic loci and biological pathways that modulate COVID-19 pathogenesis. We further explore how these genetic insights can inform therapeutic target identification, risk stratification models, and preparedness strategies for future pandemic threats.
Genetic Architecture of COVID-19 Severity
Key Genetic Loci Associated with Severe COVID-19
Large-scale genomic studies have identified numerous genetic variants that significantly influence the risk of developing critical COVID-19. The following table summarizes the most consistently replicated genetic loci and their postulated biological mechanisms.
Table 1: Key Genetic Loci Associated with COVID-19 Severity
| Gene/Locus | Lead SNP(s) | Function/Biological Pathway | Effect on COVID-19 Severity | Proposed Mechanism |
|---|---|---|---|---|
| TLR7 [98] | rs3853839 | Viral RNA sensing, Type I Interferon production | Increased risk (OR: 1.44 for GG genotype) [98] | Impaired early antiviral immune response |
| TYK2 [98] [99] | rs8108236, rs280519, rs2109069 [100] | JAK-STAT signaling, Type I/III Interferon signaling | rs8108236-AA protective (OR: 0.12); rs280500-AG increases risk [98] | Altered inflammatory signaling; higher expression linked to critical illness [99] |
| OAS1 [98] [100] | rs1131454 | Antiviral restriction enzyme activation (2'-5'-oligoadenylate synthetase) | rs1131454-AA increases risk (OR: 1.29) [98] | Dysregulated viral RNA degradation and innate immunity |
| 3p21.31 locus [101] [100] | rs11385942 | Multiple genes (SLC6A20, LZTFL1, CCR9, FYCO1, CXCR6, XCR1) | Strongly associated with increased risk [101] | Altered chemokine signaling and immune cell recruitment; inherited from Neanderthals [101] |
| DPP9 [100] | rs2109069 | Dipeptidyl peptidase 9, inflammation and immune response | Associated with critical illness [100] | Enhanced inflammatory response |
| IFNAR2 [100] | rs2236757 | Interferon alpha and beta receptor subunit 2 | Associated with critical illness [100] | Defective interferon signaling |
| KIF19, HTRA1, DMBT1 [101] | rs58027632, rs736962, rs77927946 | Novel genes identified in ICU-based GWAS | Genome-wide significant association [101] | Various, including host factors for viral entry and inflammation |
A meta-analysis of over 24,000 critical COVID-19 cases identified 49 genetic variants reaching genome-wide significance, 16 of which were novel discoveries [99]. This underscores the highly polygenic nature of COVID-19 severity.
Heritability and Genetic Correlation with Immune Traits
COVID-19 severity demonstrates significant genetic correlations with immune-related hematological parameters, suggesting shared genetic architecture. Multi-trait analysis has identified pleiotropic loci influencing both COVID-19 susceptibility and blood cell counts [102]. For instance, genetic correlations exist between severe COVID-19 and traits like lymphocyte count, highlighting the crucial role of immune cell composition in disease pathogenesis [102].
Functional Mechanisms and Signaling Pathways
Genetic associations point toward specific biological systems that are critical in determining the outcome of SARS-CoV-2 infection.
Innate Immune Sensing and Interferon Signaling
The early innate immune response is crucial for controlling viral replication. Key genes in this pathway include:
- TLR7: An endosomal RNA sensor that initiates interferon production. The G allele of rs3853839 is associated with more severe disease [98].
- OAS1/2/3: A cluster of genes encoding enzymes that activate latent RNase L to degrade viral RNA. Variants in this region (e.g., rs10735079) are associated with impaired antiviral defense [100].
- TYK2: A Janus kinase involved in interferon signaling. Specific variants (e.g., rs8108236-AA, rs280519-AG) are protective, while others (e.g., rs280500-AG) increase risk, highlighting the nuanced role of this pathway [98].
Diagram 1: Interferon Signaling Pathway. Genetic variants (in red) associated with COVID-19 severity can disrupt viral sensing (TLR7), interferon signaling (TYK2, IFNAR2), or antiviral effector functions (OAS1).
Monocyte-Macrophage Activation and Inflammatory Signaling
Hyperinflammation and cytokine storm are hallmarks of severe COVID-19. Genetic studies implicate genes expressed in the monocyte-macrophage system:
- PDE4A: A phosphodiesterase that regulates inflammatory cytokines in myeloid cells. Higher genetic predisposition for PDE4A expression in monocytes is linked to critical illness [99].
- JAK1: An intracellular kinase mediating signaling for multiple cytokines (e.g., IL-6). Mendelian randomization supports its causal role in severe disease [99].
- TNF: Genetically predicted higher expression of TNF is associated with increased risk of severe COVID-19 [99].
Host Factors for Viral Entry and Replication
- TMPRSS2: A host surface protease that facilitates viral entry into cells. A genome-wide significant association has been identified for this key host factor [99].
- RAB2A: A GTPase involved in intracellular vesicular trafficking. GWAS and transcriptome-wide association studies (TWAS) indicate that higher RAB2A expression is associated with worse disease, and it is required for viral replication [99].
Experimental Protocols for Genetic Association Studies
Genome-Wide Association Study (GWAS) Protocol
Objective: To identify genetic variants associated with COVID-19 severity without prior hypothesis.
Detailed Workflow:
Cohort Definition and Phenotyping:
- Cases: Patients with "very severe respiratory confirmed COVID-19" (e.g., requiring ICU admission for respiratory failure, hemodynamic instability, or multiple organ failure) [101].
- Controls: Population controls or hospitalized COVID-19 patients with mild/moderate disease [101] [102].
- Sample sizes in recent studies exceed 1 million individuals, with tens of thousands of cases [99] [102].
Genotyping and Quality Control (QC):
- Platform: Use high-density SNP arrays (e.g., Axiom Human Genotyping SARS-CoV-2 Research Array with >820,000 variants) [101].
- DNA QC: Assess purity (OD260/280 ~1.8-2.0), concentration, and integrity via agarose gel electrophoresis. Exclude degraded samples [101].
- Genotype QC: Exclude variants with call rate <95%, minor allele frequency (MAF) <1%, or significant deviation from Hardy-Weinberg equilibrium (p < 10⁻⁶). Exclude individuals with high heterozygosity rate outliers or cryptic relatedness (IBD > 0.2) [101].
- Imputation: Use reference panels (e.g., 1000 Genomes) and software like BEAGLE to infer ungenotyped variants [101].
Association Analysis:
- Model: Perform ordinal or binary logistic regression assuming an additive genetic model.
- Covariates: Adjust for age, sex, genetic principal components (to control for population stratification), and comorbidities like diabetes [101].
- Significance Threshold: Use a genome-wide significance level of p < 5 × 10⁻⁸.
Post-GWAS Analysis:
Diagram 2: GWAS Workflow. Key steps include rigorous patient phenotyping, genotyping, quality control, statistical analysis, and meta-analysis to identify robust genetic associations.
Single-Cell eQTL Mapping in COVID-19
Objective: To identify context-dependent genetic effects on gene regulation during active infection.
Detailed Workflow:
- Sample Collection: Collect Peripheral Blood Mononuclear Cells (PBMCs) from COVID-19 patients during acute infection and convalescence, plus healthy controls [103].
- Single-Cell Multi-omics: Perform single-cell RNA sequencing (scRNA-seq) to profile gene expression and, if possible, chromatin accessibility (scATAC-seq) simultaneously in thousands of individual cells.
- Cell Type Identification: Cluster cells based on gene expression profiles and annotate cell types using known marker genes (e.g., CD14+ monocytes, CD4+ T cells, B cells).
- eQTL Mapping: For each cell type and disease state, test for associations between genotype and gene expression levels. This reveals how genetic variants regulate gene expression in a cell-type-specific manner, and how these effects are modulated by the infection environment [103].
- Gene-Environment Interaction Analysis: Quantify the proportion of genes whose regulatory control is influenced by the infection state (i.e., "environment"), which has been estimated at 25.6% in COVID-19 [103].
Gene-Environment Interactions in Immune Response
The role of genetics cannot be disentangled from environmental influences. The concept of "rewilding" laboratory mice—introducing them into a natural outdoor environment—has demonstrated that genotype-by-environment (Gen x Env) interactions are a major source of immune variation [6].
- Cellular Composition vs. Cytokine Response: In rewilded mice, immune cell composition was largely shaped by Gen x Env interactions, whereas cytokine responses (e.g., IFNγ) were primarily driven by genetics, with direct consequences on pathogen burden [6].
- Context-Dependent Genetic Effects: Genetic differences observed under clean laboratory conditions (e.g., CD44 expression on T cells) can be reduced or abolished following rewilding. Conversely, some genetic differences in infection response (e.g., TH1 response) only emerge in the rewilded environment [6]. This has direct parallels in human COVID-19, where distinct gene regulatory networks are active during acute infection but dissipate during convalescence [103].
These findings argue that the impact of host genetics on COVID-19 severity is not fixed but is modulated by an individual's cumulative environmental exposures, microbiome, and infection history.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Resources for COVID-19 Genetic Studies
| Reagent/Resource | Specific Example | Function/Application |
|---|---|---|
| Genotyping Array | Axiom Human Genotyping SARS-CoV-2 Research Array (ThermoFisher) [101] | Interrogates >820,000 variants in immunology, inflammation, and virus-host interaction pathways. |
| eQTL/Cell-Specific Networks | Regulatory networks from 77 human contexts (e.g., Primary Monocytes, Lung tissue) [100] | Annotates risk SNPs in functional regulatory elements to identify target genes and relevant cell types. |
| Analysis Software (GWAS) | PLINK, Axiom Analysis Suite, BEAGLE, statgenGWAS package [101] | Genotype QC, imputation, and association analysis. |
| Analysis Software (Post-GWAS) | FUMA, LDSC, MULTI-TRAIT ANALYSIS (MTAG), SMR, PECA2 [102] [100] | Functional mapping, genetic correlation, pleiotropy analysis, and causal gene identification. |
| Single-Cell Multi-omics Platform | 10x Genomics Single Cell RNA-seq & ATAC-seq | Profiling cell-type-specific gene expression and chromatin landscapes in patient samples [103]. |
| Animal Model | Collaborative Cross mouse strains (e.g., C57BL/6, 129S1, PWK/PhJ) [6] | Modeling Gen x Env interactions in a controlled genetic background upon "rewilding" or infection. |
Translational Applications and Future Directions
Therapeutic Target Identification and Drug Repurposing
Human genetics provides a powerful roadmap for identifying and validating drug targets.
- JAK-STAT Pathway: The genetic association of TYK2 and JAK1 with critical COVID-19 provided a rationale for evaluating JAK inhibitors. This led to clinical trials demonstrating the efficacy of baricitinib, a JAK1/2 inhibitor, becoming one of the first proof-of-concepts for genetics-driven drug repurposing in critical illness [99].
- PDE4A: Genetic evidence suggesting that higher PDE4A expression in monocytes increases severity supports the investigation of PDE4 inhibitors (e.g., roflumilast) for mitigating hyperinflammation in COVID-19 [99].
- TNF: Mendelian randomization implicating TNF expression supports the exploration of anti-TNF therapies [99].
Integrated Risk Prediction Models
Combining genetic and clinical data improves severity prediction. A multivariate model incorporating a 12-variant Polygenic Risk Score (PRS), HLA genotypes, and clinical data achieved an area under the curve (AUC) of 0.79, outperforming models based on clinical factors alone [101]. This demonstrates the potential for genetics to enhance patient stratification and proactive management.
Implications for Future Pandemics
- Preemptive Biobanking: Establish diverse, large-scale biobanks linked to electronic health records to enable rapid GWAS in the early stages of an emerging outbreak.
- Functional Genomics Atlases: Develop comprehensive cell-type-specific regulatory maps for human tissues relevant to infection (e.g., airway epithelium, immune cells) to accelerate the interpretation of genetic hits [100].
- Platform Trials: Design adaptive clinical trial platforms that can rapidly evaluate therapeutics directed at genetically validated pathways (e.g., interferon, JAK-STAT, inflammasome) for novel pathogens.
- Modeling Gene-Environment Interplay: Incorporate measures of environmental exposure and immune history into genetic studies to better understand and predict individual risk in real-world conditions [6] [103].
The investigation of COVID-19 severity has yielded a sophisticated understanding of how host genetic variation, acting through specific immune and inflammatory pathways, determines clinical outcomes. The genetic insights gained have not only advanced fundamental knowledge of viral immunopathology but have also directly informed successful therapeutic strategies and risk prediction models. A key lesson for future pandemics is that host genetics is not deterministic but operates in continuous dialogue with environmental factors. Therefore, a deep understanding of this gene-environment interplay, supported by pre-established research infrastructures and functional genomic resources, will be paramount for a rapid, effective, and personalized response to the next global health threat.
Autoimmune diseases arise from a complex interplay of genetic susceptibility and environmental exposures, leading to a loss of immune tolerance and pathological immune responses against self-antigens. Rheumatoid Arthritis (RA) and Myasthenia Gravis (MG) exemplify this paradigm, where distinct genetic architectures and environmental triggers converge to drive disease-specific immunopathology. RA is characterized by immune-mediated joint inflammation and destruction, affecting 0.5-1% of the population with a female predominance [104]. MG represents an antibody-mediated disorder targeting the neuromuscular junction, with a prevalence of approximately 20 per 100,000 individuals [105]. Both diseases demonstrate how interactions between an individual's genetic background and environmental factors shape immune variation and clinical phenotypes. Recent research has elucidated specific molecular pathways and cellular mechanisms that offer promising targets for therapeutic intervention, advancing the field toward precision medicine approaches in autoimmunity.
Genetic Architecture of Autoimmunity
Key Genetic Loci in Rheumatoid Arthritis and Myasthenia Gravis
Genome-wide association studies (GWAS) have revolutionized our understanding of autoimmune genetics, revealing polygenic architectures with both shared and disease-specific risk loci.
Table 1: Established Genetic Loci in Rheumatoid Arthritis and Myasthenia Gravis
| Disease | Genetic Locus | Gene/Region Function | Association Notes |
|---|---|---|---|
| Rheumatoid Arthritis | HLA-DRB1 | MHC Class II antigen presentation | Strongest association; specific alleles (04, 10) confer risk [104] |
| PTPN22 | Lymphoid tyrosine phosphatase regulating T-cell receptor signaling | Affects immune checkpoint function [104] | |
| CTLA4 | Immune checkpoint molecule | Regulates T-cell activation [104] | |
| TRAF1/C5 | TNF receptor-associated factor/complement component | Inflammation and complement pathway [104] | |
| STAT4 | JAK-STAT signaling pathway | Cytokine signaling and differentiation [104] | |
| Myasthenia Gravis | HLA-B*08:01 | MHC Class I antigen presentation | Primary risk allele for early-onset MG (OR = 2.349) [105] |
| HLA-DRB1*03:01 | MHC Class II antigen presentation | Protective for late-onset MG [105] | |
| PTPN22 | T-cell receptor signaling regulator | Shared autoimmunity locus [105] | |
| CTLA4 | Immune checkpoint molecule | Impaired T-cell regulation [105] | |
| TNFRSF11A | RANKL receptor, bone metabolism | Novel association [105] |
RA demonstrates strong heritability estimates approaching 60%, particularly in seropositive disease [104]. The genetic contribution is most pronounced in the major histocompatibility complex (MHC) region, with HLA-DRB1 alleles constituting the strongest risk factor. Non-HLA loci including PTPN22, CTLA4, and STAT4 regulate key immune processes including T-cell receptor signaling, immune checkpoint control, and cytokine signaling pathways [104].
MG exhibits distinct genetic architectures based on disease subtype. A recent genome-wide meta-analysis of 5,708 MG cases and 432,028 controls identified 12 independent genome-wide significant hits across 11 loci [105]. HLA-B08:01 represents the top risk-conferring allele for early-onset MG (EOMG) with an odds ratio of 4.677, while HLA-DRB103:01 demonstrates a protective effect in late-onset MG (LOMG) [105]. These findings highlight how genetic variation within the MHC region differentially influences disease susceptibility based on age of onset.
Subtype-Specific Genetic Associations
Both RA and MG exhibit substantial clinical heterogeneity reflected in their genetic architectures. In RA, seropositive and seronegative disease demonstrate distinct genetic associations. Seropositive RA shows stronger HLA associations, while seronegative RA has been linked to HLA-B08/DRB103 haplotypes and non-HLA variants including SNPs in CLYBL and ANKRD55 [104].
MG subtyping reveals even more pronounced genetic distinctions. Early-onset MG (EOMG) demonstrates exceptionally strong association with HLA-B*08:01, while late-onset MG (LOMG) shows different HLA associations and has unique non-HLA risk loci [105]. These genetic differences correspond to variations in thymic pathology, with EOMG frequently exhibiting thymic hyperplasia and LOMG typically showing thymic atrophy [106].
Environmental Triggers and Gene-Environment Interactions
Environmental Risk Factors
Environmental exposures play a pivotal role in triggering autoimmune responses in genetically susceptible individuals. Multiple factors have been identified that influence disease risk and progression.
Table 2: Environmental Factors in Autoimmune Disease Pathogenesis
| Environmental Factor | Effect on RA | Effect on MG | Proposed Mechanisms |
|---|---|---|---|
| Infections | Epstein-Barr virus, SARS-CoV-2 associated with increased risk [54] [107] | Potential triggering role for viral infections | Molecular mimicry, bystander activation, epitope spreading [54] |
| Smoking | Strong environmental risk factor for disease development and severity [108] | Not explicitly identified | Increased citrullination, oxidative stress, inflammatory responses [108] |
| Microbiome | Gut dysbiosis linked to pathogenesis [104] | Emerging area of investigation | Alterations in immune regulation, barrier function [108] |
| Hormonal Factors | Female predominance (70-80%) [54] | Female predominance in EOMG [109] | Estrogen effects on B-cell survival, X-chromosome immune genes [54] |
| Airborne Pollutants | Silica, solvents, asbestos identified as risk factors [108] | Limited data | Enhanced inflammatory responses, tissue damage |
The relationship between environmental exposures and autoimmunity is complex, with some factors demonstrating paradoxical effects. For example, alcohol consumption exhibits both pro- and anti-inflammatory effects depending on quantity and frequency of consumption, while ultraviolet light exposure increases SLE risk but decreases RA risk [108].
Experimental Evidence for Gene-Environment Interactions
Controlled studies in mouse models have provided direct evidence for genotype-by-environment interactions (Gen × Env) in shaping immune variation. Research using "rewilded" mice – laboratory mice introduced into natural outdoor environments – demonstrated that cellular immune composition is shaped by interactions between genotype and environment [6]. Notably, genetic differences observed under clean laboratory conditions were often reduced following rewilding, while some genetic differences in response to infection emerged only in rewilding conditions [6].
These findings highlight the context dependency of genetic effects and illustrate how environmental exposures can modulate the relationship between genotype and immune phenotype. For example, expression of CD44 on T cells was explained mostly by genetics, whereas expression on B cells was explained more by environment across all mouse strains [6]. Such tissue-dependent differential effects demonstrate the complexity of gene-environment interactions in immune system regulation.
Target Identification in Rheumatoid Arthritis
Established and Emerging Molecular Targets
RA pathophysiology involves synovial inflammation, cartilage degradation, and bone erosion driven by dysregulated innate and adaptive immune responses. Target identification has focused on several key pathways:
Cytokine Signaling Pathways: IL-6 represents a well-validated target in RA, with IL-6 receptor inhibitors demonstrating clinical efficacy. The JAK-STAT pathway has emerged as another critical signaling node, with genetic variants in this pathway associated with seropositive RA [104]. JAK inhibitors now provide therapeutic targeting of this pathway independent of autoantibody status [104].
Synovial Fibroblast Activation: Pathogenic fibroblasts in the synovial microenvironment demonstrate epigenetic reprogramming that promotes inflammation and joint destruction. Histone acetylation dysregulation within synovial fibroblasts promotes transcriptional upregulation of IL-6 and MMPs [104]. HDAC inhibitors have demonstrated therapeutic potential in preclinical models [104].
Innate Immune Activation: Complement activation and toll-like receptor signaling contribute to inflammatory responses. Genetic variants in TRAF1/C5 implicate complement activation in RA pathogenesis [104].
Experimental Approaches for Target Validation
Target identification in RA leverages multi-omics technologies and deep profiling of the synovial microenvironment:
Genomics and Transcriptomics: Advanced genomics has identified key genetic variants and expression signatures associated with disease susceptibility, progression, and therapeutic response [104]. Integration of GWAS with transcriptomic data enables identification of causal genes and pathways.
Epigenomic Profiling: DNA methylation patterns in peripheral T and B lymphocytes and synovial fibroblasts serve as biomarkers even in early-stage RA and predict differential responsiveness to DMARDs [104]. Circulating methylation levels of genes such as CXCR5 and HTR2A correlate with disease activity [104].
Synovial Tissue Analysis: Single-cell RNA sequencing of synovial tissue identifies distinct fibroblast subpopulations with pathogenic potential. Spatial transcriptomics enables mapping of cellular interactions within the synovial microenvironment.
Target Identification in Myasthenia Gravis
Subtype-Specific Pathophysiology and Targets
MG therapeutics have evolved to target specific components of the autoimmune response based on disease subtypes:
AChR Antibody-Positive MG: This most common form (85% of cases) involves IgG1 antibodies that trigger complement activation at the postsynaptic membrane [106]. The thymus plays a central role as a source of autoimmunization, with thymic follicular hyperplasia common in early-onset cases [106] [109].
MuSK Antibody-Positive MG: Representing approximately 6% of cases, MuSK-MG involves IgG4 antibodies that directly interfere with MuSK function without activating complement [109]. The thymus shows minimal abnormalities, suggesting different sites of autoimmune initiation [109].
LRP4 Antibody-Positive MG: This rare subtype (2% of cases) represents another distinct entity, though LRP4 antibodies can occasionally be detected in AChR-positive and MuSK-positive cases [109].
Targeted Therapeutic Approaches
Novel biologic therapies in MG demonstrate how target identification has translated to clinical practice:
Complement Inhibition: Eculizumab, ravulizumab, and zilucoplan inhibit C5 complement activation, preventing membrane attack complex formation and NMJ damage [106] [109]. These agents are specifically indicated for AChR-positive MG where complement activation is a key effector mechanism.
FcRn Antagonists: Efgartigimod, rozanolixizumab, and nipocalimab block the neonatal Fc receptor, accelerating IgG degradation and reducing pathogenic autoantibody levels [109]. This approach applies across MG subtypes driven by pathogenic IgG antibodies.
B-Cell Targeted Therapies: Rituximab (anti-CD20) demonstrates particular efficacy in MuSK-MG, though it is used across refractory cases [109] [110]. Emerging approaches include anti-CD19, anti-CD38, and CAR-T cell therapies for more comprehensive B-cell targeting.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Autoimmunity Investigations
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Cytometry Panels | Spectral cytometry with lymphocyte panel [6] | High-dimensional immune cell phenotyping | Enables unsupervised k-means clustering for unbiased cell population identification |
| GWAS Arrays | Genome-wide SNP arrays [105] | Genetic association studies | Large sample sizes required (thousands of cases/controls) for sufficient power |
| Autoantibody Assays | Cell-based assays (CBAs), RF, ACPA, anti-CarP, anti-PAD4 [104] [109] | Patient stratification, diagnostic subtyping | Multiplex autoantibody profiling improves treatment response prediction |
| Cytokine Detection | IL-6, IL-17, IL-23, IFN-γ measurements [6] [109] | Inflammatory pathway activation assessment | Cytokine response heterogeneity primarily genetically driven in some contexts [6] |
| Epigenetic Tools | DNA methylation arrays, HDAC inhibitors [104] | Epigenetic modification studies | Methylation patterns predictive of DMARD responsiveness |
| Imaging Biomarkers | MSUS, MRI [104] | Joint inflammation and damage monitoring | MRI most sensitive for detecting early inflammatory changes |
Future Directions: Toward Precision Medicine in Autoimmunity
The evolving landscape of autoimmune disease treatment reflects a paradigm shift toward immunopathology-based precision medicine. Future approaches will require comprehensive characterization of subtype-specific molecular signatures and immune dysfunctions to guide clinical decision-making. Several promising directions are emerging:
Advanced Cellular Therapies: Chimeric autoantibody receptor T cells (CAAR-T) represent a novel strategy that directly targets autoreactive B cells. This approach uses engineered T cells expressing autoantigens to eliminate specifically autoreactive B lymphocytes, potentially offering long-term remission [110].
Treg-Targeted Therapies: Research identifying impaired IL-2 receptor signaling in regulatory T cells from autoimmune patients suggests novel therapeutic strategies. Neddylation Activating Enzyme inhibitors (NAEis) conjugated to IL-2 or anti-CD25 antibodies may selectively restore Treg function and immune tolerance without inducing systemic immunosuppression [54] [107].
Multi-Omics Integration: Combining genomic, transcriptomic, epigenomic, proteomic, and metabolomic data through advanced bioinformatics platforms enables construction of comprehensive biomarker panels. These approaches offer multidimensional molecular portraits of autoimmune diseases essential for personalized treatment strategies [104].
The path to curing autoimmune diseases like MG may involve combination approaches that address both the initiation and perpetuation of autoimmunity. For AChR-MG, this includes thymectomy to remove the site of autoimmunization combined with elimination of autoreactive memory B and T cells [110]. As our understanding of the genetic and environmental interactions in immune variation deepens, so too will our ability to develop targeted interventions that restore immune tolerance while preserving protective immunity.
The quest to understand the genetic underpinnings of complex traits, particularly in the immune system, has long revolved around a central debate: whether disease susceptibility and phenotypic diversity are driven primarily by rare genetic variants with large effects or common variants with modest effects. This question represents a critical frontier in human genetics with profound implications for disease biology, drug target identification, and therapeutic development [111]. The "missing heritability" problem—the observation that identified genetic loci typically explain only a fraction of inferred genetic variance—has intensified this debate, forcing the field to move beyond the initially dominant common disease-common variant (CD-CV) hypothesis [111].
Within immunology, this question takes on special significance as the immune system must maintain both evolutionary stability and phenotypic plasticity to respond to diverse environmental challenges. Research demonstrates that immune traits are shaped by a complex interplay of genetic and environmental factors, with studies of rewilded mice showing how genotype-by-environment interactions can dramatically reshape immune responses [6]. Similarly, twin studies have revealed that while approximately 76% of immune traits show predominantly heritable influences, the remaining 24% are primarily shaped by environmental factors, with this balance varying considerably across different immune cell lineages [112]. This review provides a comprehensive technical analysis of the rare variant versus common variant paradigms, their methodological considerations, and their implications for immune research and therapeutic development.
Theoretical Frameworks and Genetic Models
The Common Variant-Modest Effect Paradigm (Infinitesimal Model)
The common variant paradigm, often termed the infinitesimal model, proposes that complex traits are influenced by hundreds or thousands of common genetic variants (typically with minor allele frequency >5%), each exerting small individual effects on phenotype [111]. Under this model, disease susceptibility emerges through an additive burden of these numerous small-effect variants, with affected individuals carrying a slightly elevated number of risk alleles compared to unaffected individuals [111].
Genome-wide association studies (GWAS) have successfully identified thousands of common variants associated with diverse immune phenotypes and autoimmune conditions [111]. These variants collectively capture substantial portions of genetic variance, though individually they typically explain only minute fractions of risk. The infinitesimal model aligns with standard quantitative genetic theory and is supported by the observation that common variants identified through GWAS consistently replicate across diverse populations [111].
The Rare Variant-Large Effect Paradigm
In contrast, the rare variant model posits that a significant portion of complex disease risk, including immune-related conditions, derives from relatively rare genetic variants (typically allele frequency <1%) that exert substantial effects on phenotype [111]. These variants are often recently derived in evolutionary terms and may demonstrate incomplete penetrance, with expressivity potentially modified by other genetic or environmental factors [111].
This model suggests that conditions such as autoimmune disorders might actually represent collections of hundreds or even thousands of similar conditions attributable to rare variants at individual loci [111]. Under this framework, each variant explains most of the disease risk in only a handful of individuals, making them difficult to detect through standard GWAS approaches that rely on population-level allele frequency differences. The genotypic relative risk (GRR) for such variants can range from 2-fold to 5-fold or more over background risk [111].
Evolutionary and Population Genetic Perspectives
The debate between these models is deeply rooted in evolutionary theory. The rare allele model draws support from the expectation that deleterious disease alleles should be maintained at low population frequencies due to purifying selection [111]. Empirical population genetic data confirms that deleterious variants are indeed often rare, consistent with this evolutionary prediction [111].
Common variants, meanwhile, may represent older alleles that have persisted in populations, potentially through balancing selection or because their deleterious effects are only manifested in specific environmental contexts. The relationship between allele frequency and effect size generally follows an inverse correlation, with rare variants tending to have larger effect sizes, particularly for traits under strong natural selection [113].
Table 1: Key Characteristics of Common and Rare Variant Models
| Characteristic | Common Variants with Modest Effects | Rare Variants with Large Effects |
|---|---|---|
| Minor Allele Frequency | >5% | <1% |
| Effect Size (OR/RR) | Typically 1.1-1.3 | Typically >2 |
| Number of Loci | Hundreds to thousands | Dozens to hundreds |
| Heritability Explained | Highly polygenic, distributed across many loci | Concentrated in fewer high-impact loci |
| Detection Method | GWAS, imputation | Sequencing, family studies |
| Evolutionary History | Often older alleles | Often recently derived |
| Portion of Missing Heritability | Numerous variants of very small effect | Lower frequency variants not captured by GWAS |
Methodological Approaches and Experimental Designs
Study Designs for Variant Discovery
Different methodological approaches have been developed to detect common and rare variants, each with distinct strengths and limitations:
Genome-Wide Association Studies (GWAS) represent the workhorse for common variant discovery, relying on genotyping arrays that measure hundreds of thousands of tag-SNPs across the genome [114]. These studies require large sample sizes (typically thousands to hundreds of thousands of participants) to achieve sufficient statistical power for detecting modest effects. The standard genome-wide significance threshold of p<5×10⁻⁸ controls for multiple testing across the genome [114]. Success in GWAS has been enabled by international consortia and meta-analyses that aggregate data across multiple studies.
Rare Variant Association Studies (RVAS) require alternative approaches due to the low frequency of target variants. Three primary strategies have emerged:
- Genotype imputation using expanded reference panels (e.g., 1000 Genomes, UK10K, Haplotype Reference Consortium) that include dense sequencing data from thousands of individuals [113]
- Custom genotyping arrays enriched for rare variants identified through sequencing efforts (e.g., Immunochip for autoimmune diseases) [113]
- Direct sequencing through whole-exome or whole-genome sequencing, which provides the most comprehensive assessment of rare variation [113]
The Haplotype Reference Consortium panel, combining low-coverage whole-genome sequencing data from over 64,000 haplotypes, has dramatically improved imputation accuracy for rare variants down to 0.1% minor allele frequency [113].
Fine-Mapping and Causal Variant Identification
Once associated regions are identified, fine-mapping is essential to distinguish causal variants from correlated non-causal SNPs [114]. This process is challenged by linkage disequilibrium (LD), which creates correlations between nearby variants. Key fine-mapping approaches include:
- Statistical fine-mapping: Uses Bayesian or penalized regression methods to prioritize likely causal variants based on association signals and LD structure [114]
- Trans-ethnic fine-mapping: Leverages differences in LD patterns across diverse populations to narrow associated intervals [114]
- Functional annotation integration: Incorporates genomic annotations (e.g., chromatin states, regulatory elements) to prioritize variants with likely biological effects [114]
The performance of fine-mapping depends on multiple factors, including causal variant effect size, local LD structure, sample size, and SNP density. Notably, the lead SNP from GWAS is not necessarily the causal variant, with simulations showing that the probability of the lead SNP being causal ranges from 79% for larger-effect common variants to just 2.4% for modest-effect lower-frequency variants [114].
Fine-Mapping Workflow for Identifying Causal Variants
Heritability Estimation in Twin Studies
Twin studies have been instrumental in quantifying the relative contributions of genetics and environment to immune variation. The classic twin design compares trait similarity between monozygotic (MZ) twins, who share nearly 100% of their genetic material, and dizygotic (DZ) twins, who share approximately 50% [61] [112]. Using structural equation modeling, the variance in immune traits can be partitioned into:
- Additive genetic influence (A): The proportion of variance explained by genetic factors
- Common environmental influence (C): Variance due to environments shared by twins
- Unique environmental influence (E): Variance due to unshared environments and measurement error
A comprehensive analysis of 23,394 immune phenotypes in 497 adult female twins revealed that 76% of traits showed predominantly heritable influences, while 24% were primarily shaped by environmental factors [112]. These proportions varied significantly across immune cell types, with adaptive immune traits generally showing stronger genetic influence and innate immune traits being more environmentally responsive [112].
Quantitative Data and Heritability Partitioning
Heritability Estimates Across Immune Cell Subsets
Large-scale immunophenotyping studies have enabled precise estimation of heritability across diverse immune cell populations. Analysis of 78,000 immune traits in 669 female twins revealed wide variation in heritability estimates, ranging from 0% to 96% for specific immune parameters [115]. The most highly heritable traits included CD32 expression on dendritic cells (96% heritable) and CD39 expression on CD4+ T cells [115].
Table 2: Heritability and Environmental Influence Across Major Immune Cell Lineages
| Immune Cell Lineage | Average Heritability | Strongly Heritable Traits (>60%) | Traits with Strong Environmental Influence |
|---|---|---|---|
| Dendritic Cells | Highest proportion of highly heritable traits | CD32 expression, multiple surface markers | Limited environmental influence |
| CD4+ T Cells | High heritability, particularly Treg subsets | CD39 expression on Tregs, differentiation markers | CD25+CD73+ Treg subsets (shared environment) |
| CD8+ T Cells | Moderate to high heritability | Memory subsets, activation markers | Naive and effector subsets |
| B Cells | Lower overall heritability | CD27 expression on Ig class-switched B cells | Immature and transitional B cells |
| Monocytes | Lower heritability | Specific surface receptors | Inflammatory responses, phagocytosis |
| Innate-like T Cells | Lowest heritability (γδ T, NKT) | Limited strongly heritable traits | Most subset frequencies and phenotypes |
The differential heritability patterns across immune lineages reflect their distinct evolutionary roles and environmental responsiveness. Adaptive immune cells (T and B cells) demonstrate stronger genetic control, consistent with their reliance on highly structured receptor gene rearrangements and selection processes [112]. In contrast, innate immune cells and innate-like T cells show greater environmental influence, aligning with their roles as first responders to environmental challenges [112].
Variance Explained by Common and Rare Variants
Partitioning the genetic contribution to complex traits reveals that common variants identified through GWAS typically explain only a fraction of the total heritability. For most complex traits, common variants (MAF>5%) explain less than 30% of the total heritability, with the remainder potentially attributable to rare variants, structural variants, or gene-gene interactions [113].
Empirical data from sequencing studies suggests that rare SNPs contribute approximately half the heritability explained by common SNPs for many traits, though these estimates continue to be refined as sample sizes increase [113]. The proportion of heritability explained by rare variants varies by disease type, with conditions such as autism spectrum disorders showing stronger contributions from rare variants compared to late-onset diseases like type 2 diabetes [113].
Experimental Models and Functional Validation
Rewilding Models for Gene-Environment Interactions
The "rewilding" approach using inbred mouse strains provides a powerful experimental model for dissecting genotype-by-environment interactions in the immune system [6]. This methodology involves transferring laboratory mice to outdoor enclosures with subsequent challenge with pathogens such as the parasite Trichuris muris [6].
Key Experimental Protocol:
- Strain Selection: Utilize genetically diverse inbred strains (e.g., C57BL/6, 129S1, PWK/PhJ) representing distinct haplotypes
- Environmental Transfer: Randomly assign mice to conventional laboratory housing or outdoor rewilding enclosures for 2 weeks
- Pathogen Challenge: Infect with approximately 200 T. muris embryonated eggs or leave uninfected
- Longitudinal Monitoring: Return mice to their respective environments for 3+ weeks with periodic immune monitoring
- Multiparameter Immune Phenotyping: Analyze immune cell composition, cytokine production, and surface marker expression using high-dimensional cytometry
This approach has demonstrated that genotype-by-environment interactions significantly contribute to immune variation, with genetic differences observed under laboratory conditions often diminishing following rewilding [6]. For example, differences in CD44 expression on CD4+ T cells between C57BL/6 and PWK/PhJ mice observed in laboratory conditions were absent after rewilding, while TH1 responses to T. muris infection emerged specifically in the rewilding environment [6].
Rewilding Experimental Design for Gene-Environment Interactions
Functional Follow-Up of Associated Variants
Prioritizing associated variants for functional validation requires integration of multiple data types. Key approaches include:
- Chromatin profiling: Assessing whether variants fall in regulatory regions marked by DNase I hypersensitivity, histone modifications, or transcription factor binding sites
- Expression quantitative trait locus (eQTL) mapping: Determining whether variants associate with gene expression levels in relevant immune cell types
- Epigenomic annotation: Leveraging cell-type-specific chromatin state maps from projects like Roadmap Epigenomics
- CRISPR-based perturbation: Using genome editing to introduce candidate causal variants and assess functional consequences
For rare variants with large effects, the path to functional validation is often more straightforward as they are more likely to directly alter protein sequence or splicing. Common variants with modest effects more frequently localize to noncoding regulatory regions, making functional interpretation more challenging.
Implications for Drug Development and Therapeutic Strategy
Target Identification and Validation
The distinction between rare and common variant architectures has profound implications for drug discovery:
Rare variants with large effects provide compelling targets because they often directly implicate specific genes and pathways in disease etiology. The large effect sizes increase confidence in causal relationships, mimicking the effects of therapeutic intervention. Examples include loss-of-function variants in immune regulatory genes that cause monogenic autoimmune disorders, which can reveal pathways for broader autoimmune therapeutics [113].
Common variants with modest effects present greater challenges for therapeutic development due to their small individual effects and frequent location in noncoding regions. However, they can identify key biological pathways when considered collectively. Polygenic risk scores aggregating numerous common variants can stratify patient populations for targeted prevention strategies [111].
Clinical Trial Design and Patient Stratification
Understanding genetic architecture enables more precise clinical trial designs:
- Rare variant carriers can be enrolled in niche trials targeting specific molecular pathways, potentially demonstrating larger treatment effects in genetically defined subgroups
- Polygenic risk scores based on common variants can identify high-risk individuals for preventive interventions or enrichment of clinical trial populations
- Pharmacogenetic variants can guide drug dosing and selection to maximize efficacy and minimize adverse events
The increasing availability of large-scale biobanks with genomic and health data is accelerating the discovery of both rare and common variants with clinical utility.
Research Reagent Solutions and Experimental Tools
Table 3: Essential Research Reagents and Platforms for Genetic-Immunological Studies
| Tool Category | Specific Examples | Key Applications | Technical Considerations |
|---|---|---|---|
| Genotyping Arrays | Immunochip, Global Screening Array, MEGA Array | Common variant association studies | Coverage varies by population; optimal for GWAS |
| Sequencing Platforms | Whole-genome sequencing, Whole-exome sequencing | Comprehensive rare variant discovery | Cost constraints for large sample sizes |
| Reference Panels | 1000 Genomes, Haplotype Reference Consortium, UK10K | Genotype imputation for rare variants | Population-matched panels improve accuracy |
| Immunophenotyping | High-dimensional flow cytometry, Mass cytometry (CyTOF) | Deep immune profiling | Standardized panels enable cross-study comparison |
| Cell Isolation | Magnetic bead separation, FACS sorting | Cell-type-specific functional studies | Preservation of cell state during processing |
| Functional Assays | CRISPR screens, Reporter assays, ATAC-seq | Causal variant validation | Requires relevant cell types and stimulation conditions |
The comparative analysis of rare variants with large effects versus common variants with modest effects reveals a complex genetic architecture underlying immune function and disease susceptibility. Rather than representing mutually exclusive paradigms, these two classes of genetic variation operate along a spectrum, collectively shaping immune responses and disease risk [111]. The relative contribution of each varies across different immune cell types, environmental contexts, and specific diseases.
Future research directions will focus on integrating multi-omics data to bridge the gap between genetic association and biological mechanism, particularly for common noncoding variants. Advanced experimental models, including humanized mouse systems and in vitro differentiation of patient-derived induced pluripotent stem cells, will enable functional validation of candidate causal variants in appropriate cellular contexts. Additionally, longitudinal studies capturing immune dynamics in response to environmental challenges will elucidate how genetic variants shape temporal response patterns.
From a therapeutic perspective, the growing understanding of genetic architecture promises to accelerate precision immunology approaches that match patients to optimal treatments based on their genetic makeup. As genetic discovery progresses, the field moves closer to comprehensive models that incorporate both rare and common variation to predict disease risk and treatment response, ultimately enabling more effective targeting of the immune system in health and disease.
Pharmacogenomics (PGx) stands as a cornerstone of precision medicine, seeking to elucidate how an individual's genetic composition governs their response to drug therapy, affecting both efficacy and the risk of adverse drug reactions (ADRs) [116]. This field has progressively shifted from a one-size-fits-all approach to a paradigm that acknowledges profound inter-individual variability. This variability is influenced by innumerable factors, with genetics providing a key explanatory layer [116]. Simultaneously, research into immune variation has illuminated that an individual's immune phenotype is not solely a product of genetic predisposition but is shaped by a complex interplay between heritable factors and non-heritable environmental influences [6]. The immune system's distinct capacity to adjust its response according to specific stimuli, influenced by both genetic and environmental factors, creates a critical interface for pharmacogenomic investigations [64].
This technical guide frames pharmacogenomics within the broader context of immune variation research. It explores how genetic polymorphisms, particularly those affecting immune pathways and drug metabolism, interact with environmental factors to determine drug response and toxicity. By integrating insights from large-scale biobanks, functional genomics, and studies of genotype-by-environment interactions, this review provides a comprehensive resource for researchers and drug development professionals aiming to advance personalized therapeutic strategies.
Genetic Architecture of Drug Response
The genetic basis of drug response, or pharmacogenomic (PGx) traits, can be categorized based on their underlying genetic architecture, which in turn dictates the feasibility of genetic prediction.
Table 1: Classification of Pharmacogenomic Traits
| Trait Category | Genetic Architecture | Key Characteristics | Clinical Prediction Feasibility | Examples |
|---|---|---|---|---|
| Monogenic (Mendelian) | Single rare, large-effect variant | Bimodal or trimodal phenotype distribution; High penetrance for severe ADRs | High for genotype-phenotype association, but prospective testing may have high false-positive rates due to rarity | Inherited disorders (e.g., PKU); Severe idiosyncratic ADRs (e.g., HLA-associated SCARs) [116] [117] |
| Predominantly Oligogenic | Small number of major pharmacokinetic/pharmacodynamic genes | A substantial fraction of phenotypic variance can be explained by a few variants | Improving, but uncertainty in predictions and cost-benefit ratios remain challenges | Warfarin dosing (VKORC1, CYP2C9); Thiopurine metabolism (TPMT) [116] |
| Complex PGx Traits | Numerous small-effect variants, plus epigenetic and environmental factors | Continuous, multifactorial phenotype distribution; Resembles quantitative traits | Currently limited; combined small-effect variants explain only a small fraction of variance | Statin response variability; Methotrexate efficacy and toxicity [118] [116] |
Recent genome-wide studies of large biobanks have provided significant insights into the complex architecture of drug response. For instance, the heritability of treatment response for common drugs like statins has been quantified, with genetic variation modifying the primary effect of statins on LDL cholesterol (9% heritable) as well as side effects on hemoglobin A1c and blood glucose (10–11% heritable) [118]. These studies have identified dozens of genes associated with drug response, demonstrating that drug use information must be accounted for in genetic risk prediction, as the accuracy of polygenic scores (PGS) can vary up to 2-fold depending on treatment status [118].
Experimental and Methodological Frameworks
Quantifying Genotype-by-Environment Interactions in Immune and Drug Responses
Controlled experimental models are essential for deciphering the interactive effects of genetics and environment (Gen × Env) on immune system function and, consequently, on drug response. The "rewilded" mouse model provides a powerful framework for this purpose [6].
Experimental Protocol: Rewilded Mouse Model for Gen × Env Interactions
- Objective: To quantify the relative and synergistic contributions of genetic and environmental influences on immune phenotypes and susceptibility to parasitic infection.
- Model System: Genetically diverse inbred mouse strains (e.g., C57BL/6, 129S1, and wild-derived PWK/PhJ).
- Environmental Manipulation:
- Laboratory Control Group: Housed in a conventional vivarium under controlled summer-like photoperiod and temperature.
- Rewilded Group: Housed in an outdoor enclosure to introduce natural environmental exposures.
- Intervention: After 2 weeks of environmental exposure, mice are either infected with a defined dose of an intestinal helminth (e.g., Trichuris muris) or left uninfected, then returned to their respective environments for a further 3 weeks.
- Data Collection & Analysis:
- Immune Phenotyping: High-dimensional spectral cytometry of Peripheral Blood Mononuclear Cells (PBMCs) and complete blood count with differential (CBC/DIFF).
- Statistical Analysis: Multivariate distance matrix regression (MDMR) is used to quantify the independent and interactive contributions of genotype, environment, and infection to immune variation [6].
This approach has revealed that the cellular composition of PBMCs is shaped by interactions between genotype and environment, whereas certain cytokine responses are primarily driven by genotype, with consequences for worm burden. Notably, some genetic differences observed under controlled laboratory conditions were diminished following rewilding, illustrating how environmental context can mask or unmask genetic effects [6].
Diagram: Experimental workflow for assessing genotype-by-environment interactions in rewilded mice.
Population-Based Pharmacogenomic Screening
Translating PGx findings to clinical practice requires an understanding of allele frequency distribution across different populations. Population-specific screening studies are critical for optimizing drug therapy.
Methodology: Population-Based Allele Frequency Analysis
- Objective: To determine the prevalence of clinically relevant PGx variants in a specific population (e.g., South Asian) to inform personalized treatment regimens.
- Variant Selection: Pharmacogenomic variants with high evidence levels (e.g., Levels 1A, 1B, 2A, 2B) are selected from curated databases such as PharmGKB. Alleles with normal function are excluded.
- Genetic Data Source: Genetic data is sourced from whole exome sequencing (WES) or genotyping of a large, anonymized cohort representative of the target population.
- Analysis: Minor Allele Frequencies (MAFs) are calculated for key variants in genes critical for drug metabolism (e.g.,
CYP2B6,CYP2C19,NAT2,UGT1A1). MAFs are compared to other global populations (e.g., from gnomAD) using statistical tests (e.g., χ² test), with significance set at p < 0.05 [119].
A study in a Sri Lankan population, for example, found a high frequency of the CYP2B6 rs3745274 variant (MAF: 39.6%), which is associated with poor metabolism of antiretroviral drugs like efavirenz. This frequency was significantly higher than in European populations, highlighting the potential for altered drug response and the need for population-specific dosing guidelines [119].
Table 2: Selected Pharmacogenomic Variants and Their Population-Specific Frequencies
| Gene | Variant (rsID) | Drug Example | Phenotype | Sri Lankan MAF (%) | European MAF (%) | Clinical Implication |
|---|---|---|---|---|---|---|
| CYP2B6 | rs3745274 | Efavirenz, Nevirapine | Poor Metabolizer | 39.6 [119] | ~16-25 [119] | Increased drug exposure, higher risk of CNS toxicity |
| NAT2 | rs1041983 | Isoniazid | N/A | 43.7 [119] | Significantly lower [119] | Associated with INH-induced liver injury and neuropathy |
| CYP2C19 | rs4244285 | Voriconazole, Clopidogrel | Poor/Intermediate Metabolizer | 41.9 [119] | ~15 [119] | Altered drug efficacy/toxicity; requires dose adjustment |
| UGT1A1 | rs4148323 | Irinotecan | N/A | 3.5 [119] | ~12 | Increased risk of severe neutropenia |
| HLA-B | *15:02 allele | Carbamazepine | SCARs (SJS/TEN) | Varies by ethnicity | <1% [117] | High risk of life-threatening skin reactions; contraindication |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Tools for Pharmacogenomic Research
| Research Tool | Function/Application | Example Use Case |
|---|---|---|
| DMET Plus Microarray | Interrogates 1,936 markers in Drug Metabolism Enzymes and Transporters (ADME genes) recognized by the FDA. | Genome-wide profiling of ADME variants in cohort studies [120]. |
| Next-Generation Sequencing (NGS) | Whole exome/genome sequencing for comprehensive variant discovery and analysis of polymorphic regions. | Identifying novel variants associated with drug resistance (e.g., in methotrexate therapy) [121] [120]. |
| PharmGKB Database | Curated knowledgebase of PGx-based clinical guidelines, drug labels, and variant annotations. | Sourcing clinically validated variants and evidence levels for study design [119] [120]. |
| Spectral Cytometry | High-dimensional immunophenotyping to characterize cellular composition and activation states. | Analyzing immune cell subsets in rewilded mouse models or patient cohorts pre/post-treatment [6]. |
| Clinical Pharmacogenetics Implementation Consortium (CPIC) Guidelines | Evidence-based, peer-reviewed guidelines for translating genetic test results into actionable prescribing decisions. | Informing the clinical interpretation of genotyping results in research studies aimed at clinical translation [117]. |
Key Signaling Pathways and Clinical Implications
HLA-Mediated Hypersensitivity and Immune Activation
A paradigmatic example of the link between genetics, immune response, and drug toxicity is the association between specific HLA alleles and severe cutaneous adverse reactions (SCARs). The pathway below outlines the mechanism of HLA-mediated drug hypersensitivity.
Diagram: Proposed pathway for HLA-mediated severe cutaneous adverse reactions (SCARs).
The HLA-B*15:02 allele, highly prevalent in specific Asian populations, is strongly associated with carbamazepine-induced Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis (SJS/TEN). The drug is thought to interact with the peptide-binding groove of the HLA molecule, triggering a deleterious T-cell-mediated immune response [117]. This has led to FDA recommendations for pre-treatment genetic screening in at-risk populations, demonstrating the direct clinical translation of a monogenic PGx trait.
Tolerogenic Immune Pathways as Therapeutic Targets
Beyond predicting toxicity, understanding immune pathways informs the development of novel therapies. In autoimmune diseases, dysfunction of regulatory T cells (Tregs), essential for maintaining peripheral tolerance, is a key pathological feature. Emerging data indicate that intrinsic signaling defects, such as impaired IL-2 receptor (IL-2R) signal durability, compromise Treg suppressive function [54]. This dysfunction has been linked to aberrant degradation of key IL-2R second messengers. Consequently, novel therapeutic strategies are being explored, such as using Neddylation Activating Enzyme inhibitors (NAEis) conjugated to IL-2 or anti-CD25 antibodies, which aim to selectively restore Treg function and immune tolerance without inducing systemic immunosuppression [54].
Pharmacogenomics in practice requires a nuanced understanding that extends beyond a simple catalog of gene-drug interactions. It must integrate the complex genetic architecture of drug response, which ranges from monogenic to highly polygenic traits, and frame it within the broader context of immune system variation. As demonstrated by rewilding experiments, environmental factors can profoundly modulate the effects of genetic variation on immune phenotypes and, by extension, on drug response and toxicity. Furthermore, the ethnogeographic enrichment of many pharmacogenomic variants necessitates a global and inclusive approach to research and clinical implementation [122] [64] [119].
The future of pharmacogenomics lies in the continued integration of multi-omics data, the development of sophisticated bioinformatic tools for analyzing complex datasets, and the execution of large-scale functional studies to validate the mechanistic impact of genetic variants [120]. As these fields converge, the goal of delivering truly personalized, safe, and effective drug therapies based on an individual's genetic makeup and environmental context moves closer to reality. This will be particularly pivotal for optimizing treatments in complex domains like oncology and autoimmune diseases, where the interplay between genetics, the immune system, and therapy is most pronounced.
The high failure rate in drug development, with approximately 90% of clinical programmes never receiving approval, presents a significant challenge to the pharmaceutical industry. This whitepaper examines the transformative role of human genetic evidence in de-risking drug discovery and development. Leveraging recent large-scale analyses, we demonstrate that drug targets with genetic support have a probability of success from phase I to launch that is 2.6 times greater than those without such support. This effect varies substantially across therapy areas and is most pronounced in later development phases. Within the context of immune variation research, we further explore how gene-environment interactions shape immune responses and create both challenges and opportunities for therapeutic development. The integration of genetic evidence represents a paradigm shift in target selection, with profound implications for research prioritization, resource allocation, and clinical development strategy.
The escalating costs of drug development are driven primarily by failure, with historical data indicating that only about 10% of clinical programmes eventually transition to approved therapies [123]. This high attrition rate represents a fundamental challenge for pharmaceutical innovation and necessitates improved approaches for target validation and prioritization. Human genetics has emerged as a powerful tool for identifying and prioritizing potential drug targets, providing direct insights into the causal role of genes in human disease pathophysiology.
Genetic evidence offers unique advantages in drug discovery, including the ability to demonstrate causal relationships between target modulation and disease risk, predict efficacy and safety profiles, and inform dose-response relationships [123]. The growth in large-scale genetic databases and advanced analytical methods has facilitated systematic assessments of how genetic evidence impacts clinical success rates across the development pipeline. Simultaneously, research into immune variation has revealed the critical interplay between genetic factors and environmental exposures in shaping immune responses and disease susceptibility [6] [15]. Understanding these gene-environment interactions is particularly relevant for immune-mediated diseases, where both genetic risk loci and environmental triggers contribute to disease pathogenesis.
This technical review provides an in-depth analysis of how genetic evidence impacts drug approval rates, with particular emphasis on implications for immune-related disorders. We present comprehensive quantitative benchmarks, detailed methodological frameworks for generating and validating genetic evidence, and strategic recommendations for leveraging genetics in therapeutic development.
Quantitative Impact of Genetic Evidence on Clinical Success
Recent comprehensive analyses of the drug development pipeline have quantified the substantial impact of genetic evidence on clinical success rates. A landmark study examining 29,476 target-indication (T-I) pairs found that the probability of success (P(S)) for drug mechanisms with genetic support is 2.6 times greater than for those without genetic evidence [123]. This analysis defined genetic support as overlap between target-indication pairs and gene-trait associations with high semantic similarity (Medical Subject Headings similarity ≥0.8).
Table 1: Overall Clinical Success Rates With and Without Genetic Evidence
| Development Stage | Success Rate with Genetic Support | Success Rate without Genetic Support | Relative Success |
|---|---|---|---|
| Phase I to Launch | 2.6x baseline | 1.0x baseline | 2.6 |
| Phase II to Phase III | 2.3x baseline | 1.0x baseline | 2.3 |
| Phase III to Launch | 2.7x baseline | 1.0x baseline | 2.7 |
| Preclinical to Phase I | 1.4x baseline (Metabolic diseases) | 1.0x baseline | 1.4 |
The impact of genetic evidence varies throughout the development lifecycle. The relative success is most pronounced in later stages of development (Phase II to Phase III and Phase III to launch), corresponding to where programmes traditionally fail due to inadequate demonstration of clinical efficacy [123]. This pattern suggests that genetically validated targets are more likely to demonstrate meaningful clinical efficacy in patient populations.
Variation Across Therapy Areas
The impact of genetic evidence on clinical success is not uniform across therapeutic areas. Significant heterogeneity exists, with nearly all therapy areas showing relative success estimates greater than 1, and 11 of 17 specific areas demonstrating relative success greater than 2 [123].
Table 2: Relative Success by Therapy Area
| Therapy Area | Relative Success | Probability of Genetic Support |
|---|---|---|
| Haematology | >3.0 | High |
| Metabolic | >3.0 | High |
| Respiratory | >3.0 | Medium |
| Endocrine | >3.0 | Medium |
| Gastroenterology | 2.5 | Medium |
| Dermatology | 2.2 | Medium |
| Neurology | 1.8 | Low-Medium |
| Ophthalmology | 1.5 | Low |
Therapy areas with more possible gene-indication pairs supported by genetic evidence demonstrated significantly higher relative success (ρ = 0.71, P = 0.0010) [123]. This relationship highlights the importance of the breadth and depth of genetic discovery within specific disease domains.
Impact of Genetic Evidence Type and Quality
The predictive power of genetic evidence varies according to the type and quality of the evidence. Mendelian genetic associations from sources such as Online Mendelian Inheritance in Man (OMIM) demonstrate the highest relative success (RS = 3.7), while genome-wide association studies (GWAS) also show substantial impact (RS = 2.0-2.6) [123].
The confidence in variant-to-gene mapping significantly influences predictive power. For Open Targets Genetics (OTG) associations, the relative success was sensitive to the confidence in variant-to-gene mapping as reflected in the minimum locus-to-gene (L2G) score [123]. Higher L2G scores, indicating greater confidence in the assigned causal gene, correlated with improved clinical success rates.
Other characteristics of genetic associations, including effect size, minor allele frequency, and year of discovery, showed no statistically significant association with relative success [123]. This suggests that the mere presence of supportive genetic evidence is more important than these specific characteristics, and we have not yet reached saturation in discovering valuable genetic associations for drug discovery.
Methodological Frameworks for Genetic Evidence Generation
Establishing Genetic Associations with Disease
The foundation of genetically-informed drug development lies in robustly connecting genetic variants to disease risk. Genome-wide association studies (GWAS) have emerged as the predominant tool for systematic identification of disease-associated genetic risk variants [15]. The most recently published GWAS catalog contains over 5,000 independent GWAS datasets describing more than 70,000 variant-trait associations [15].
Protocol: Genome-Wide Association Study Design
- Cohort Selection: Recruit thousands of cases (individuals with the disease of interest) and controls (matched individuals without the disease)
- Genotyping: Perform genome-wide genotyping using microarray technologies covering 500,000 to 5 million single nucleotide polymorphisms (SNPs)
- Imputation: statistically infer ungenotyped variants using reference panels (e.g., 1000 Genomes Project) to increase genomic coverage
- Quality Control: Apply stringent filters for:
- Sample call rate (>98%)
- Variant call rate (>95%)
- Hardy-Weinberg equilibrium (P > 1×10⁻⁶)
- Minor allele frequency (typically >1%)
- Association Testing: Perform logistic regression (for binary traits) or linear regression (for quantitative traits) for each variant, adjusting for principal components to account for population stratification
- Significance Thresholding: Apply genome-wide significance threshold (P < 5×10⁻⁸) to account for multiple testing
- Replication: Validate significant associations in independent cohorts to minimize false discoveries
Functional Validation of Genetic Associations
While GWAS identify statistical associations, additional functional studies are required to elucidate causative molecular mechanisms and identify druggable targets [15].
Protocol: Functional Validation of Genetic Risk Loci
Variant Prioritization:
- Identify variants in linkage disequilibrium (r² > 0.8) with lead GWAS signals
- Annotate variants using functional databases (ENCODE, Roadmap Epigenomics)
- Prioritize variants overlapping regulatory elements in disease-relevant cell types
Experimental Validation:
- Reporter Assays: Clone risk and non-risk haplotypes into luciferase reporter vectors and transfer into disease-relevant cell lines
- Genome Editing: Use CRISPR/Cas9 to introduce risk variants into induced pluripotent stem cells (iPSCs) and differentiate into relevant cell types
- Chromatin Conformation Capture: Identify physical interactions between risk variants and potential target gene promoters
Target Gene Identification:
- Perform expression quantitative trait locus (eQTL) analysis in disease-relevant tissues
- Conduct chromatin interaction analysis (Hi-C) to connect regulatory elements to promoters
- Implement massively parallel reporter assays (MPRAs) to simultaneously test thousands of variants for regulatory activity
Incorporating Gene-Environment Interactions in Immune Research
Understanding gene-environment (G×E) interactions is particularly crucial for immune-related diseases, where environmental exposures can significantly modulate genetic risk [15]. The "rewilding" mouse model provides a powerful experimental system for quantifying these interactions.
Protocol: Rewilding Mouse Model for G×E Interactions in Immune Variation
- Mouse Strain Selection: Utilize genetically diverse inbred strains (e.g., C57BL/6, 129S1, PWK/PhJ) representing diverse genetic backgrounds
- Environmental Exposure:
- Laboratory Controls: Maintain in conventional vivarium with controlled conditions
- Rewilded Group: Transfer to outdoor enclosures to experience natural environmental exposures
- Immune Challenge: Infect with relevant pathogens (e.g., Trichuris muris embryonated eggs) 2 weeks after environmental assignment
- Immune Phenotyping:
- Longitudinal Sampling: Collect blood and tissue samples at multiple timepoints
- Immune Cell Profiling: Perform high-dimensional spectral cytometry on PBMCs
- Cytokine Measurement: Quantify cytokine production (IFN-γ, IL-5, IL-13, IL-10) following ex vivo stimulation
- Statistical Analysis:
- Apply multivariate distance matrix regression (MDMR) to quantify contributions of genotype, environment, and their interactions
- Use principal component analysis (PCA) to visualize high-dimensional immune phenotypes
- Calculate variance explained by G×E interactions for specific immune traits
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Genetic Validation
| Reagent/Platform | Function | Application in Genetic Validation |
|---|---|---|
| CRISPR/Cas9 Systems | Precise genome editing | Introduce or correct risk variants in cellular and animal models |
| Induced Pluripotent Stem Cells (iPSCs) | Patient-derived stem cells | Differentiate into disease-relevant cell types for functional studies |
| High-Dimensional Cytometry | Single-cell protein profiling | Characterize immune cell composition and activation states (CyTOF) |
| Bulk and Single-Cell RNA-Seq | Transcriptome profiling | Identify gene expression changes associated with genetic variants |
| Chromatin Conformation Capture | 3D genome architecture mapping | Connect non-coding variants to target gene promoters |
| ATAC-Seq | Chromatin accessibility profiling | Identify altered regulatory elements in disease-relevant cell types |
| Massively Parallel Reporter Assays | High-throughput regulatory testing | Simultaneously test thousands of variants for regulatory activity |
| Quantitative Trait Locus Mapping | Genotype-phenotype correlation | Connect genetic variants to molecular traits (eQTLs, caQTLs, hQTLs) |
Integration with Immune Variation Research
Genetic Architecture of Immune Variation
Research into immune variation has revealed that genetic factors significantly influence interindividual differences in immune responses. Studies comparing immune phenotypes in monozygotic and dizygotic twins have demonstrated substantial heritability for many immune traits [15]. However, the relative contributions of genetic and environmental factors differ across specific immune cell populations and functions.
The "rewilding" mouse model experiments demonstrated that cellular composition of peripheral blood mononuclear cells (PBMCs) was shaped by interactions between genotype and environment, while cytokine response heterogeneity was primarily driven by genotype [6]. This highlights the complex interplay between genetic predisposition and environmental exposures in shaping immune phenotypes.
Implications for Immune-Mediated Diseases
The impact of genetic evidence on drug development success is particularly relevant for immune-mediated diseases. Therapy areas with high inflammatory or immune components (e.g., rheumatology, gastroenterology, dermatology) show some of the highest relative success rates when targets have genetic support [123].
Genetic risk for autoimmune diseases is enriched for gene regulatory effects that are modified by immune activation [7]. This supports a paradigm where genetic disease risk is sometimes driven not by genetic variants causing constant cellular dysregulation, but by causing a failure to respond properly to environmental conditions such as infection [7]. This has profound implications for drug discovery, suggesting that some targets may only be relevant in specific environmental contexts or disease states.
The integration of human genetic evidence into drug discovery represents a paradigm shift with demonstrated impact on clinical success rates. The 2.6-fold improvement in probability of success from phase I to launch for genetically supported targets provides a compelling rationale for prioritizing targets with human genetic validation. This approach is particularly valuable for immune-related disorders, where genetic evidence can help navigate the complexity of gene-environment interactions in disease pathogenesis.
Future directions in this field include expanding genetic discovery in diverse populations, developing more sophisticated models of gene-environment interactions, and integrating multi-omic data to improve target identification and validation. As genetic databases continue to grow and analytical methods advance, the impact of genetics on drug development success will likely increase further.
For drug development professionals, the implications are clear: systematic incorporation of human genetic evidence into target selection and prioritization decisions can significantly de-risk development pipelines and improve overall productivity. This approach represents a powerful strategy for addressing the high failure rates that have long plagued pharmaceutical innovation.
Conclusion
The integration of human genetics and environmental immunology is fundamentally transforming drug discovery and precision medicine. The key takeaway is that genetic evidence not only illuminates disease pathogenesis but also significantly de-risks the therapeutic development pipeline, with genetically-supported targets being twice as likely to succeed in clinical trials. Future progress hinges on several critical frontiers: the systematic mapping of allelic series across the frequency-effect spectrum, the deep functional characterization of non-coding regulatory regions identified by GWAS, and the expansion of diverse, multi-ancestry biobanks to ensure equitable translation of findings. Furthermore, embracing the complexity of genotype-by-environment interactions through controlled experimental models and longitudinal studies will be essential. For researchers and drug developers, the path forward requires a concerted shift towards genetics-guided prioritization, the application of multifaceted omics technologies, and the development of therapeutic strategies that restore immune homeostasis rather than broadly suppress immunity. This integrated approach promises to unlock a new era of targeted, effective, and personalized treatments for a wide spectrum of immune-mediated diseases.
References
- 1. Systematic genetic analysis of the MHC region reveals ... [https://elifesciences.org/articles/48476]
- 2. An In‐Depth Review of the Genetics of the Non‐Classical HLA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12324987/]
- 3. Haplotype analysis reveals pleiotropic disease ... [https://www.sciencedirect.com/science/article/abs/pii/S0002929725002423]
- 4. Gene–environment interactions and their impact on human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9801363/]
- 5. Genetic architecture of primary biliary cholangitis: strong ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1600364/full]
- 6. Genetic and environmental interactions contribute to ... [https://www.nature.com/articles/s41590-024-01862-5]
- 7. Genetic Variants Found to Play Role in Human Immune ... [https://www.nygenome.org/news-events/news/genetic-variants-found-play-key-role-human-immune-system/]
- 8. MHC Hammer reveals genetic and non-genetic HLA ... [https://www.nature.com/articles/s41588-024-01883-8]
- 9. Multimodal profiling reveals tissue-directed signatures of ... [https://www.nature.com/articles/s41590-025-02241-4]
- 10. Pollutants, microbiota and immune system: frenemies ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11116734/]
- 11. Diverse mechanisms by which chemical pollutant exposure ... [https://www.sciencedirect.com/science/article/pii/S016041202400391X]
- 12. Impact of Environmental Pollutants on Gut Microbiome and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9317668/]
- 13. Deciphering cross-cohort metabolic signatures of immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583525/]
- 14. The Immune Signatures data resource, a compendium of ... [https://www.nature.com/articles/s41597-022-01714-7]
- 15. Gene–environment interactions and their impact on human ... [https://www.nature.com/articles/s41435-022-00192-6]
- 16. Interplay between genes and social environment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12218153/]
- 17. Epigenetics and the exposome: A new era of disease prevention [https://www.niehs.nih.gov/news/factor/2025/2/feature/4-feature-epigenetics-and-the-exposome]
- 18. Epigenetics: the link between environmental exposures ... [https://www.sciencedirect.com/science/article/abs/pii/S0952791525000688]
- 19. Autoimmune disease: genetic susceptibility, environmental ... [https://pubmed.ncbi.nlm.nih.gov/40852720/]
- 20. Environment strongly influences chronic disease development [https://www.niehs.nih.gov/news/factor/2025/4/feature/environment-predicts-chronic-disease]
- 21. Gene-environment interactions within a precision ... [https://www.sciencedirect.com/science/article/pii/S2666979X24001757]
- 22. Decoding Environmental Exposures' Lifelong Impacts [https://magazine.publichealth.jhu.edu/2025/decoding-environmental-exposures-lifelong-impacts]
- 23. Sex differences in disease: sex chromosome and immunity [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05990-2]
- 24. A researcher's guide to studying sex differences in immune ... [https://www.sciencedirect.com/science/article/abs/pii/S147149142500005X]
- 25. Women have supercharged immune systems and we now ... [https://www.newscientist.com/article/2501447-women-have-supercharged-immune-systems-and-we-now-know-why/]
- 26. Sex hormones, the anticancer immune response, and ... [https://www.sciencedirect.com/science/article/abs/pii/S1535610825000650]
- 27. Biological sex impacts immune cell proportions and ... [https://www.nature.com/articles/s42003-025-08844-9]
- 28. Abundance of key immune cells may be influenced by ... [https://www.ucl.ac.uk/news/2025/mar/abundance-key-immune-cells-may-be-influenced-oestrogen-and-xx-chromosomes]
- 29. Using the Immune System as a Window into Your Current and ... [https://medicine.yale.edu/news-article/using-immune-system-window-into-your-current-future-health/]
- 30. Estimating Trait Heritability | Learn Science at Scitable [https://www.nature.com/scitable/topicpage/estimating-trait-heritability-46889/]
- 31. Variation in the human immune system is largely driven by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4302727/]
- 32. Global analyses of human immune variation reveal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4139290/]
- 33. How to estimate heritability: a guide for genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10114051/]
- 34. The missing heritability question is now (mostly) answered [https://theinfinitesimal.substack.com/p/the-missing-heritability-question]
- 35. Variation in the Human Immune System Is Largely Driven ... [https://www.sciencedirect.com/science/article/pii/S0092867414015906]
- 36. Genetic and Environmental interactions contribute to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10055251/]
- 37. Quantitative characterization of immune cells by measuring ... [https://www.nature.com/articles/s41598-024-75666-w]
- 38. Leveraging genome‐wide association studies to better ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11786324/]
- 39. The landscape of GWAS validation; systematic review ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8973751/]
- 40. Unveiling genetic signatures of immune response in ... [https://www.nature.com/articles/s41467-025-61192-4]
- 41. Cross-disorder genetic analysis of immune diseases ... [https://www.nature.com/articles/s41467-023-38389-6]
- 42. Leveraging transcriptome-wide association studies identifies ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0322864]
- 43. Exploring genetic loci linked to COVID-19 severity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11873281/]
- 44. From GWAS to Function: Using Functional Genomics ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.00424/full]
- 45. Exploring new drug treatment targets for immune related ... [https://www.nature.com/articles/s41598-025-94053-7]
- 46. Dissecting immune cell-specific genetics in migraine: a multi ... [https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-025-02132-x]
- 47. Mendelian randomization for investigating causal roles of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5837263/]
- 48. Concepts, Opportunities, Challenges, and Future Directions [https://globalheartjournal.com/articles/10.5334/gh.1438]
- 49. Expectations for Mendelian randomization research in PLOS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626271/]
- 50. Systematic comparison of Mendelian randomisation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10533809/]
- 51. Expectations for papers performing Mendelian randomization ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1011767]
- 52. A comparison of robust Mendelian randomization methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7317850/]
- 53. Mendelian randomization and genetic analyses reveal ... [https://www.nature.com/articles/s41598-025-10759-8]
- 54. Autoimmune disease: genetic susceptibility, environmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12367657/]
- 55. Multiomics Mendelian randomization integrating pQTL ... [https://www.nature.com/articles/s41598-025-17664-0]
- 56. Multi‐Omics Mendelian Randomization Identifies a DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370846/]
- 57. Integration of multi-omics quantitative trait loci evidence ... [https://www.nature.com/articles/s41598-025-12290-2]
- 58. Efficient and accurate framework for genome-wide gene ... [https://www.nature.com/articles/s41467-025-57887-3]
- 59. Protocol for finding genetic variation associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213288/]
- 60. Genomics of drug target prioritization for complex diseases [https://pubmed.ncbi.nlm.nih.gov/41198831/]
- 61. Environment, not genes, plays starring role in human immune ... [https://med.stanford.edu/news/all-news/2015/01/environment-not-genes-plays-starring-role-in-immune-variation.html]
- 62. Shared genetics across 178 phenotypes predicts novel ... [https://www.medrxiv.org/content/10.1101/2025.05.13.25327511v1]
- 63. Novel target identification towards drug repurposing based on ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0319865]
- 64. Human immune system: Exploring diversity across ... [https://www.sciencedirect.com/science/article/pii/S2405844025002166]
- 65. Genomics-Driven Drug Repurposing and Novel Targets ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1671626/full]
- 66. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 67. Development of a genetic priority score to predict drug side ... [https://www.nature.com/articles/s41467-025-63762-y]
- 68. Novel Genetic Priority Score Unveiled to Enhance Target ... [https://www.mountsinai.org/about/newsroom/2024/novel-genetic-priority-score-unveiled-to-enhance-target-prioritization-in-drug-development]
- 69. Development of a human genetics-guided priority score for ... [https://www.nature.com/articles/s41588-023-01609-2]
- 70. Development of a human genetics-guided priority score for ... [https://pmc.ncbi.nlm.nih.gov/articles/11776516]
- 71. Softwares | Ron Do Laboratory [https://labs.icahn.mssm.edu/dolab/softwares/]
- 72. Valley of death: A proposal to build a “translational bridge” for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5477974/]
- 73. Lost in translation: the valley of death across preclinical and ... [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-019-0050-7]
- 74. by Clinical Show Higher Trials Rates Supported Genetics Success [https://www.azolifesciences.com/news/20240823/Clinical-Trials-Supported-by-Genetics-Show-Higher-Success-Rates.aspx]
- 75. factors associated with reasons for Genetic stoppage clinical trial [https://www.nature.com/articles/s41588-024-01854-z?error=cookies_not_supported&code=efdcaac9-4e2b-490c-b289-b7a744a43296]
- 76. Statistical Genetic Approaches to Investigate Genotype-by ... [https://pubmed.ncbi.nlm.nih.gov/38790175/]
- 77. Statistical Genetic Approaches to Investigate Genotype-by- ... [https://www.mdpi.com/2073-4425/15/5/547]
- 78. Mining for gene-environment and gene-gene interactions [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1617504/full]
- 79. Analyzing complex traits and diseases using GxE PRS [https://www.nature.com/articles/s10038-025-01378-2]
- 80. Genotype-by-environment interaction with high-dimensional ... [https://gsejournal.biomedcentral.com/articles/10.1186/s12711-025-00974-2]
- 81. Understanding and applying gene–environment interactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC11723160/]
- 82. Target Validation [https://www.sygnaturediscovery.com/drug-discovery/integrated-drug-discovery/target-validation/]
- 83. Multi-omic profiling reveals age-related immune dynamics ... [https://www.nature.com/articles/s41586-025-09686-5]
- 84. Methods for cell- and tissue-specific DNA aptamer selection [https://www.sciencedirect.com/science/article/pii/S2329050125000774]
- 85. Multi-physiology modeling of the immune system in the era of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159046/]
- 86. Genetic prediction of complex traits with polygenic scores: A statistical review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8511058/]
- 87. Optimal strategies for learning multi-ancestry polygenic scores vary across traits | Nature Communications [https://www.nature.com/articles/s41467-023-38930-7]
- 88. ForSim: a tool for exploring the genetic architecture of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2732213/]
- 89. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 90. Data Visualization Tools - Library Guides [https://guides.lib.uw.edu/research/datavisualization/toolsatuw]
- 91. Ethical considerations for biobanks serving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11831713/]
- 92. Quality management, ethical considerations, and emerging ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898125000403]
- 93. Population genetic considerations for using biobanks as ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-021-07618-x]
- 94. New approach to determine the healthy immune variations ... [https://www.nature.com/articles/s41598-021-88272-x]
- 95. Lessons from national biobank projects utilizing whole ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11887102/]
- 96. Genetic Architecture of Adaptive Immune System Identifies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6205839/]
- 97. Rare variant contribution to human disease in 281104 UK ... [https://www.nature.com/articles/s41586-021-03855-y]
- 98. Genetic variants regulating the immune response improve ... [https://www.nature.com/articles/s41598-024-71476-2]
- 99. GWAS and meta-analysis identifies 49 genetic variants ... [https://www.nature.com/articles/s41586-023-06034-3]
- 100. Human Genetic Variants Associated with COVID-19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9375061/]
- 101. Genetic Analysis and Predictive Modeling of COVID-19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11940120/]
- 102. Exploring genetic loci linked to COVID-19 severity and ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1502839/full]
- 103. Widespread gene-environment interactions shape ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/39677792/]
- 104. Rheumatoid Arthritis: Biomarkers and the Latest ... [https://www.mdpi.com/1422-0067/26/21/10594]
- 105. Genome-wide meta-analysis of myasthenia gravis ... [https://www.nature.com/articles/s41467-024-53595-6]
- 106. Myasthenia gravis in 2025: five new things and four hopes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11846739/]
- 107. Autoimmune disease: genetic susceptibility, environmental ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1626082/full]
- 108. Environmental factors and rheumatic diseases [https://www.sciencedirect.com/science/article/pii/S152169422500021X]
- 109. Immunological Targets in Generalized Myasthenia Gravis ... [https://www.mdpi.com/2076-3425/15/9/978]
- 110. Is there a path to cure myasthenia gravis? [https://www.sciencedirect.com/science/article/abs/pii/S0952791525000536]
- 111. Rare and Common Variants: Twenty arguments - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4408201/]
- 112. Innate and adaptive immune traits are differentially affected ... [https://www.nature.com/articles/ncomms13850]
- 113. The impact of rare and low-frequency genetic variants in ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-017-1212-4]
- 114. From genome-wide associations to candidate causal variants ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6050137/]
- 115. The Genetic Architecture of the Human Immune System [https://pmc.ncbi.nlm.nih.gov/articles/PMC4393780/]
- 116. Personalized medicine: Genetic risk prediction of drug response [https://pmc.ncbi.nlm.nih.gov/articles/PMC5653378/]
- 117. Pharmacogenomics in drug therapy: global regulatory ... [https://www.nature.com/articles/s41431-025-01950-6]
- 118. Characterizing the genetic architecture of drug response ... [https://www.sciencedirect.com/science/article/pii/S2666979X24003513]
- 119. Pharmacogenomic profiling of variants affecting efficacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11786550/]
- 120. Bioinformatic challenges for pharmacogenomic study: tools ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1548991/full]
- 121. Editorial: Pharmacogenomics for improving drug safety and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1649258/full]
- 122. Genetic Variation in Drug Targets: Are We Ready for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12067103/]
- 123. Refining the impact of genetic evidence on clinical success [https://www.nature.com/articles/s41586-024-07316-0]