Decoding Tissue Immunity: Insights from Human Postmortem Studies
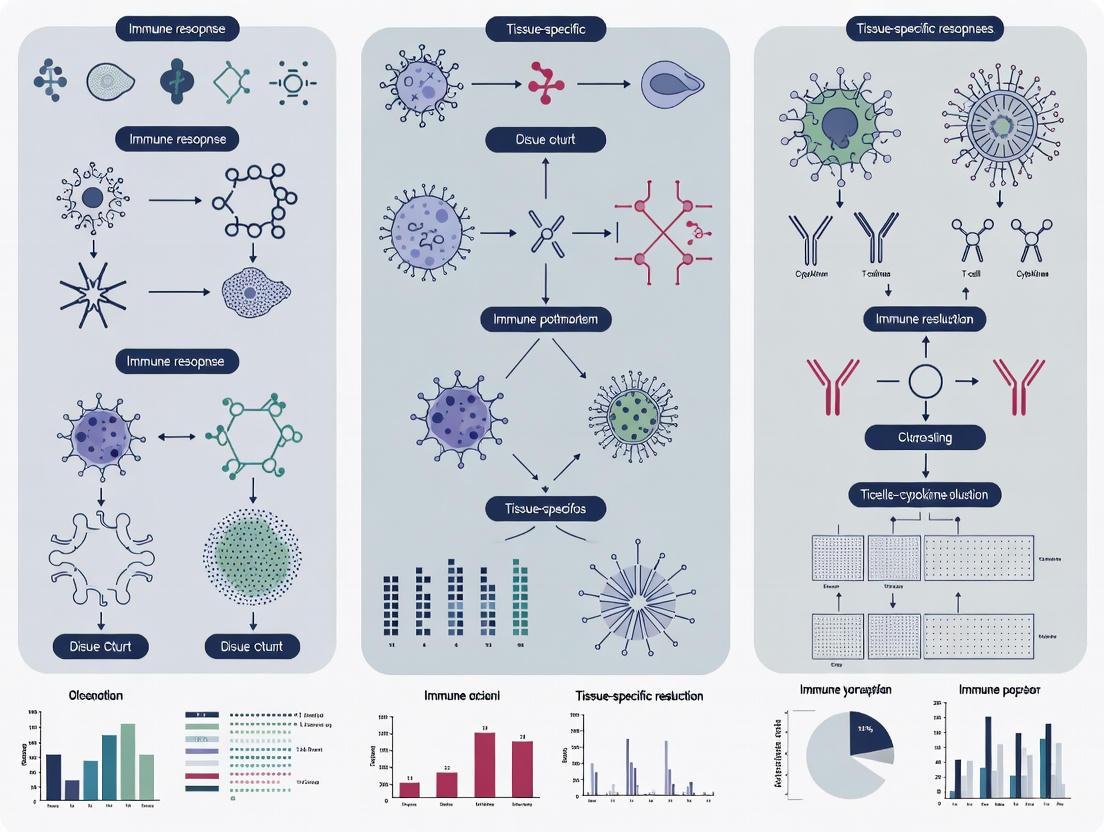
This article synthesizes recent advances in our understanding of tissue-specific immune responses, with a particular focus on insights gained from human postmortem studies.
Decoding Tissue Immunity: Insights from Human Postmortem Studies
Abstract
This article synthesizes recent advances in our understanding of tissue-specific immune responses, with a particular focus on insights gained from human postmortem studies. It explores the foundational principles of localized immunity, detailing the critical roles of tissue-resident memory T cells (TRM) and other specialized populations. The content covers cutting-edge methodological approaches, including multi-color flow cytometry and AI-driven single-cell RNA sequencing, for analyzing immune cells within their native tissue context. It further addresses the unique challenges and optimization strategies in postmortem tissue research, and provides a comparative analysis of how this human-based evidence validates or challenges findings from animal models. Aimed at researchers, scientists, and drug development professionals, this review highlights the translational potential of these findings for vaccine design, cancer immunotherapy, and the treatment of autoimmune and inflammatory diseases.
The Landscape of Localized Defense: Principles of Tissue-Specific Immunity
The immune system employs a dynamic network of cells distributed throughout the body to defend against infections, regulate inflammation, and repair tissue damage. Within this network, tissue-resident immune cells (TRICs) constitute a specialized compartment that resides within specific tissues without recirculating, forming a critical first line of defense and playing essential roles in maintaining tissue homeostasis [1]. Unlike their circulating counterparts, TRICs are endowed with distinct capabilities shaped by their local tissue environments, allowing for highly specialized immune surveillance and response [1]. Recent advances in single-cell technologies and human tissue studies have revolutionized our understanding of TRIC heterogeneity, development, and function across different organs. This whitepaper provides a comprehensive technical guide to defining tissue-resident immune cells, with a specific focus on their characteristics, research methodologies, and implications for human postmortem studies within the context of tissue-specific immune responses.
Defining Characteristics and Classification of TRICs
Core Definition and Key Properties
Tissue-resident immune cells are defined by their persistent localization within specific tissues without re-entering the circulation under steady-state conditions [1]. This fundamental characteristic distinguishes them from circulating leukocytes and endows them with unique functional capabilities. The residency of TRICs is maintained through complex interactions with local tissue niches and expression of specific retention molecules that inhibit their egress into lymphatic or blood vessels [1].
Key defining properties of TRICs include:
- Long-term tissue persistence: TRICs can reside in tissues for extended periods, in some cases throughout the lifespan of the organism.
- Limited recirculation: Unlike circulating immune cells, TRICs do not routinely traffic through blood or lymphatic vessels.
- Tissue-specific adaptation: TRICs undergo phenotypic and functional reprogramming to meet the specific demands of their tissue environment.
- Self-renewal capacity: Many TRIC populations maintain themselves through local proliferation rather than continuous replacement from circulating precursors.
Major TRIC Populations and Their Markers
TRICs encompass multiple lineages from both innate and adaptive immunity. The table below summarizes the major TRIC populations, their key identifying markers, and primary tissue distributions based on recent multimodal profiling studies [2] [1].
Table 1: Major Tissue-Resident Immune Cell Populations and Their Characteristics
| TRIC Population | Key Surface Markers | Transcription Factors | Primary Tissue Locations | Main Functions |
|---|---|---|---|---|
| Tissue-resident memory T cells (TRM) | CD69, CD103, CD49a | Blimp1, Hobit, Runx3 | Skin, lung, intestine, liver [2] | Rapid local protection, cytokine production |
| Tissue-resident macrophages | F4/80, CD11b (variable), TIMD4, LYVE1 | Ahr, Nfatc1, Nfatc2, Irf9 [3] | Kidney, liver, brain, lung [4] [3] | Phagocytosis, tissue repair, homeostasis |
| Tissue-resident B cells (BRM) | CD69, CD73 | Not specified | Lung, intestine [1] | Local antibody production |
| Tissue-resident NK cells (trNK) | CD49a, CD69, CD103 | T-bet, Eomes | Liver, salivary gland, uterus [1] | Cytokine production, cytotoxicity |
| Tissue-resident ILCs | CD127, CD161, CD69 | GATA3, RORγt, T-bet | Mucosal tissues, liver [2] | Tissue repair, cytokine production |
| Tissue-resident neutrophils (TRN) | CD11b, Ly6G | Not specified | Spleen, lung [1] | Pathogen clearance, immunoregulation |
The expression of canonical tissue-residency markers varies significantly across different tissue environments. For instance, CD103 is predominantly expressed by TRICs in mucosal tissues, while CD69 and/or CD49a are more commonly expressed in non-mucosal tissues [1]. This heterogeneity reflects the remarkable adaptability of TRICs to their local microenvironment.
Table 2: Tissue-Specific Variations in Human TRIC Populations Based on Multimodal Profiling
| Tissue Site | Dominant TRIC Populations | Tissue-Specific Features |
|---|---|---|
| Lung (BAL/parenchyma) | Alveolar macrophages, CD8+ TRM, CD4+ TRM [2] | Enhanced disease tolerance mechanisms [4] |
| Jejunum (epithelium/lamina propria) | CD8+ TRM, CD4+ TRM, ILC1, ILC3 [2] | High CD103 expression, IgA+ plasma cells [2] |
| Kidney | TLF+ macrophages (TIMD4+ LYVE1+ FOLR2+) [3] | CX3CR1/CX3CL1 axis for maintenance [3] |
| Skin | CD8+ TRM, γδ T cells, Langerhans cells [1] | CD49a expression predominates over CD103 [1] |
| Lymphoid organs | TRM, resident B cells, macrophages | CD69+ memory B cells, MHC IIhi macrophages [2] |
Origins, Development, and Maintenance
Developmental Origins of TRICs
TRICs originate through diverse developmental pathways that vary by cell lineage and tissue location. The schematic below illustrates the major developmental origins of different TRIC populations:
Figure 1: Developmental origins of major TRIC populations. TRICs can originate from embryonic precursors, adult hematopoietic stem cells, or circulating immune cells that acquire tissue-resident properties.
Some TRICs, including certain tissue-resident macrophages and mast cells, trNK cells, tissue-resident ILCs, and γδ T cells, establish tissue residency during embryogenesis [1]. For example, kidney TRMs (KTRMs) originate from both embryonic yolk sac erythro-myeloid progenitors and the fetal liver, demonstrating the capacity for self-renewal independent of bone marrow hematopoiesis [3]. In contrast, other TRICs such as tissue-resident memory T (TRM) and B (BRM) cells postnatally establish tissue residency during effector phases of immune responses [1].
Maintenance Mechanisms
The maintenance of TRIC populations in tissues involves both self-renewal and limited replenishment from circulating precursors. Tissue-resident macrophages and ILCs predominantly maintain themselves through local self-renewal, with varying requirements for bone marrow-derived progenitor input across different tissues [1]. For instance, alveolar macrophages in the lung and microglia in the brain are primarily self-maintaining, while certain intestinal macrophage populations require continuous replacement from circulating monocytes [4].
Key maintenance mechanisms include:
- CX3CR1/CX3CL1 axis: Critical for maintaining kidney TRMs through in situ proliferation [3].
- IL-4 signaling: Promotes self-renewal and accumulation of TRMs [3].
- Fatty acid metabolism: Mediated by FABP5, essential for differentiation of bone marrow-derived TRMs into KTRMs [3].
- Local tissue niches: Provide specific signals that support TRIC survival and function.
Research Methodologies for TRIC Investigation
Experimental Approaches for Identifying TRICs
Several specialized methodologies have been developed to identify and characterize TRICs, each with distinct advantages and limitations:
Parabiosis surgery remains the gold standard for identifying TRICs, where the circulatory systems of two genetically identical mice are surgically joined. Circulating cells establish equilibrium in both mice, while tissue-resident cells do not exchange between partners [1]. This approach has identified TRM cells, ILCs, trNKs, BRM cells, tissue-resident macrophages, tissue-resident iNKT, MAIT cells, and TRNs [1].
Intravascular labeling employs fluorescently conjugated antibodies administered intravenously to distinguish blood-borne cells (which are labeled) from tissue-resident cells (which remain unlabeled) [1]. This method is particularly useful for identifying TRM and BRM cells without requiring surgical procedures.
Advanced single-cell technologies including scRNA-seq and CITE-seq (Cellular Indexing of Transcriptomes and Epitopes) enable comprehensive profiling of TRIC phenotypes and functions across tissues [2] [1]. These approaches have revealed remarkable heterogeneity in TRIC populations across different tissue sites and have identified novel TRIC subsets in both homeostatic and disease conditions.
Detailed Methodological Protocols
Parabiosis Protocol for TRIC Identification
Surgical procedure: Select age- and sex-matched mice with compatible CD45 alleles (e.g., CD45.1 and CD45.2). Anesthetize mice and shave their lateral aspects. Make matching skin incisions from elbow to knee joint on each mouse. Join the olecranon and knee joints using suture material. Sutures the dorsal and ventral skin flaps to complete the union.
Post-operative care: Administer analgesics for 72 hours and antibiotics for 7-10 days. Allow 2-4 weeks for circulatory exchange to reach equilibrium before experiments.
Analysis: Harvest tissues of interest and prepare single-cell suspensions. Analyze cell populations by flow cytometry using CD45 allelic markers to distinguish host-derived (tissue-resident) from partner-derived (circulatory) cells.
Interpretation: TRICs are identified as cells predominantly derived from the host mouse, with minimal contribution from the parabolic partner.
Intravascular Staining Protocol
Antibody preparation: Dilute fluorescently conjugated anti-CD45 antibody or other pan-leukocyte markers in sterile PBS. Typically, 2-5 µg of antibody in 100-200 µL volume is administered intravenously.
Administration: Inject antibody solution via the tail vein or retro-orbital sinus. Allow 3-5 minutes for circulation to ensure complete labeling of blood cells.
Perfusion and tissue collection: Euthanize mice and perfuse extensively with 20-30 mL of PBS through the left ventricle to flush out blood vessels. Harvest tissues of interest and process for flow cytometry.
Analysis: Identify intravascular (labeled) versus tissue-resident (unlabeled) leukocytes by flow cytometry.
Multimodal Single-Cell Profiling Workflow
The following diagram illustrates the integrated workflow for multimodal TRIC characterization using CITE-seq:
Figure 2: CITE-seq workflow for multimodal TRIC profiling. This approach simultaneously captures transcriptomic and proteomic data from single cells.
Human Postmortem Studies for TRIC Research
Postmortem tissue studies provide a unique opportunity to investigate human TRICs across multiple organs from individual donors. A recent study demonstrated the feasibility of this approach for tuberculosis research, establishing that postmortem procedures and tissue processing could be completed within 8 hours of death while maintaining cell viability for up to 14 hours [5]. This work found good acceptance from next-of-kin for tissue donation, providing a valuable resource for understanding tissue-specific immune responses in humans.
Key considerations for postmortem TRIC studies:
- Time window: Process tissues within 8 hours of death for optimal cell viability.
- Tissue processing: Use established protocols for mononuclear cell isolation from multiple tissues [2].
- Multimodal profiling: Combine CITE-seq with scRNA-seq for comprehensive TRIC characterization.
- Data integration: Leverage computational tools like multi-resolution variational inference (MrVI) to harmonize variation between cell states across samples [2].
Signaling Pathways and Functional Programs
Key Signaling Pathways in TRIC Biology
TRIC development, maintenance, and function are regulated by specific signaling pathways and metabolic programs. Recent studies using quantitative signal transduction pathway activity profiling have revealed characteristic pathway activation patterns in different immune cell types [6].
Table 3: Key Signaling Pathways in TRIC Biology and Their Functions
| Signaling Pathway | Key Components | Role in TRICs | Experimental Assessment |
|---|---|---|---|
| CX3CR1/CX3CL1 | CX3CR1, CX3CL1 | Maintenance of kidney TRMs through in situ proliferation [3] | Flow cytometry, scRNA-seq |
| TGF-β signaling | TGF-β, SMADs | Induction of CD103 expression on TRMs [1] | STAP-STP technology, phospho-flow [6] |
| Fatty acid metabolism | FABP5, PPARs | Differentiation of bone marrow-derived TRMs [3] | Metabolic profiling, inhibitor studies |
| JAK-STAT signaling | JAKs, STAT1/2, STAT3 | TRM development and function [6] | STAP-STP technology, phospho-flow [6] |
| PI3K-FOXO signaling | PI3K, FOXO | Regulation of TRIC survival and metabolism [6] | STAP-STP technology [6] |
| Type 1 IFN signaling | IFNAR, STAT1/2 | Establishment of trained immunity in alveolar macrophages [4] | STAP-STP technology, inhibitor studies [6] |
Trained Innate Immunity in Tissue-Resident Macrophages
Tissue-resident macrophages can develop trained innate immunity (TII), representing a form of innate immune memory characterized by long-lasting functional modifications following initial immunological exposure [4]. This training involves epigenetic reprogramming and metabolic rewiring that enhances responsiveness to subsequent challenges.
Key features of trained immunity in TRICs:
- Duration: Persistent modifications that outlast the initial stimulus.
- Mechanisms: Epigenetic changes and metabolic reprogramming.
- Specificity: Can enhance responses to heterologous challenges.
- Outcomes: Either protective (enhanced pathogen clearance) or maladaptive (exacerbated inflammation).
The schematic below illustrates the induction and maintenance of trained immunity in tissue-resident macrophages:
Figure 3: Induction and maintenance of trained immunity in tissue-resident macrophages. Initial exposure to immunological stimuli triggers epigenetic and metabolic changes that establish a long-lasting trained state.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Key Research Reagent Solutions
Table 4: Essential Research Reagents and Platforms for TRIC Investigation
| Reagent/Platform | Specific Examples | Application in TRIC Research |
|---|---|---|
| Antibody panels | 24-color flow cytometry panels [5] | Comprehensive immunophenotyping of human TRICs |
| Cell isolation kits | Tissue dissociation systems | Isolation of viable immune cells from multiple tissues |
| Single-cell platforms | 10X Genomics, CITE-seq | Multimodal profiling of TRIC transcriptomes and surface proteins [2] |
| Cell culture systems | 3D full-thickness skin models [5] | Study of TRIC function in tissue-like environments |
| Computational tools | MrVI, MMoCHi classifier [2] | Data integration and cell annotation for multimodal datasets |
| Signal transduction assays | STAP-STP technology [6] | Quantitative measurement of pathway activity in immune cells |
| In vivo models | Parabiosis surgery, intravascular staining [1] | Definitive identification of tissue-resident versus circulating cells |
| Microneedle patches | Hydrogel-coated MN arrays [7] | Minimally invasive sampling of skin TRICs |
| 5-Oxodecanoic acid | 5-Oxodecanoic acid, CAS:624-01-1, MF:C10H18O3, MW:186.25 g/mol | Chemical Reagent |
| Benzoylacetone | Benzoylacetone, CAS:93-91-4, MF:C10H10O2, MW:162.18 g/mol | Chemical Reagent |
Emerging Technologies and Model Systems
Immune organoid systems have emerged as powerful tools for studying human immune responses in vitro. These systems provide sophisticated insights about tissue architecture and functionality in miniaturized organs, overcoming limitations of animal models that inadequately represent complex human-specific interactions [8]. Immune organoids established from patient-derived lymphoid tissues can reflect human adaptive immunity with more physiologically relevant aspects than traditional models [8].
Microneedle (MN) patch technology provides a minimally invasive approach to sample immune cells and soluble factors from the skin [7]. Recent advancements include hydrogel-coated MN patches that can recover thousands of live antigen-specific lymphocytes as well as innate immune cells from skin sites where TRMs have been restimulated [7]. This technology is particularly valuable for longitudinal monitoring of TRIC responses in human subjects.
Humanized mouse models and multiorgan-on-chip systems are being developed to better recapitulate human immune responses. These advanced platforms enable study of systemic immunological processes by integrating various immune cells and tissues in a controlled in vitro environment [5].
Tissue-resident immune cells represent a critical component of the immune system, with specialized functions tailored to specific tissue environments. The definitive identification and characterization of TRICs requires specialized methodologies, including parabiosis, intravascular staining, and multimodal single-cell profiling. Recent advances in single-cell technologies, human postmortem studies, and engineered model systems have dramatically expanded our understanding of TRIC heterogeneity, development, and function across different tissues. The integration of these approaches provides unprecedented opportunities to investigate human tissue-specific immune responses and develop targeted therapeutic strategies that leverage the unique properties of TRICs. As these technologies continue to evolve, they will undoubtedly yield further insights into the complex roles of TRICs in health and disease, potentially revolutionizing our approach to vaccine development, immunotherapy, and treatment of inflammatory disorders.
The immune system is not a homogeneous entity but a complex network of specialized cells distributed across distinct tissue niches throughout the body. Traditional immunology, heavily reliant on peripheral blood studies, has given way to a more nuanced understanding that immune cell function, maintenance, and response are profoundly shaped by their specific tissue microenvironment [2]. This paradigm shift has been accelerated by the detailed analysis of human tissues, with postmortem studies providing an unparalleled window into the spatial architecture of immunity in health and disease. Such research has definitively shown that immune responses are not uniform but are instead tailored to the unique challenges and functional requirements of each organ [9].
The concept of the immune niche refers to anatomically defined compartments that support the residence and function of immune cells, facilitating interactions with structural cells, cytokines, and signaling molecules that collectively orchestrate local immunity [10]. Understanding these niches—including the lung, lymphoid organs like the spleen and lymph nodes, and barrier surfaces such as the gut—is critical for deciphering the pathogenesis of infectious, inflammatory, and autoimmune diseases. This guide synthesizes findings from recent human postmortem studies to provide a technical overview of the key immune niches, detailing their cellular composition, functional specializations, and the experimental approaches used to profile them.
Profiling Key Immune Niches in Human Tissues
Advanced single-cell technologies have enabled high-resolution mapping of the immune landscape across the human body. The table below summarizes quantitative findings on immune cell distribution and age-related changes from a comprehensive multimodal study profiling over 1.25 million cells from multiple donors [2].
Table 1: Immune Cell Composition and Age-Associated Changes Across Key Tissue Niches
| Tissue Niche | Dominant Immune Cell Subsets | Key Tissue-Resident Features | Noted Age-Associated Changes |
|---|---|---|---|
| Lung & Airways | - CD8+ and CD4+ Tissue-Resident Memory T (TRM) cells- Mature CD56dimCD16+ NK cells- Alveolar Macrophages | - TRM cells expressing CD69, CD103, and/or CD49a- Strategic positioning for rapid response [9] | - Functional and metabolic changes in macrophages- Alterations in CD8+ T cell function |
| Lymph Nodes (Various) | - CD4+ Naive T (TN) cells- CD4+ Central Memory T (TCM) cells- Germinal Center B cells- Regulatory T (Treg) cells | - Enriched Treg population- CD69+ memory B cells denoting tissue residency | - Significant changes in B cell composition |
| Spleen | - CD8+ Terminal Effector (TEMRA) cells- Mucosal-Associated Invariant T (MAIT) cells- CD11c+ T-bet+ "Atypical" B cells | - Enriched TEMRA and MAIT cells | - Changes in B cell composition |
| Mucosal Barrier (Jejunum) | - CD4+ and CD8+ TRM cells- CD16‑NCR2+IL7R‑ ILC1s- IgA+ Plasma Cells | - Highest frequency of TRM cells- ILC1s with high CD69, CD49a, CD103 expression | - Changes in macrophage signatures |
Deep Dive into Niche-Specific Architecture and Function
Lung: A Frontline Defense Nexus
The lung's immune architecture is organized to respond to a constant barrage of inhaled antigens while maintaining gas exchange. Its homeostasis is maintained by a coordinated effort between alveolar epithelial cells (AECs) and macrophages [11]. AEC II cells are immunologically active, producing cytokines and chemokines, and can act as antigen-presenting cells [11].
The innate defense is coordinated by a network of cells including alveolar macrophages, dendritic cells (DCs), and recruited neutrophils. A key adaptive player is the tissue-resident memory T (TRM) cell population. Recent research reveals that lung TRM cells are not uniform; their function is dictated by their precise location within the lung's architecture [9]. These cells are strategically positioned to provide a swift, localized response to reinfection, orchestrating a broader immune response while minimizing damaging inflammation [9]. In severe pulmonary infections like COVID-19, postmortem studies have identified a hallmark of myeloid activation coupled with lymphocyte suppression. Activated myeloid cells (CD80/83+ CD206+ macrophages and BDCA2+/BATF3+ DCs) are found proximal to viral antigens, while lymphocytes, particularly CD8+ T cells and NK cells, are suppressed and distally located [12].
Lymph Nodes and Spleen: Hubs of Adaptive Immunity
As secondary lymphoid organs, the lymph nodes (LNs) and spleen are specialized for initiating adaptive immune responses and maintaining immune memory.
- Lymph Nodes: LNs are critical sites for antigen presentation and lymphocyte activation. Multimodal profiling shows LNs are enriched for naive T cells (TN), central memory T cells (TCM), and germinal center B cells, which are essential for generating high-affinity antibodies [2]. A key feature is the significant enrichment of regulatory T cells (Treg), highlighting the role of LNs in maintaining immune tolerance [2]. Furthermore, the presence of CD69-expressing memory B cells indicates a population of tissue-resident B cells that contribute to long-term local immunity [2].
- Spleen: The spleen acts as a blood filter and is a major site for immune responses against blood-borne pathogens. It is characterized by an abundance of terminally differentiated CD8+ TEMRA cells and Mucosal-Associated Invariant T (MAIT) cells [2]. The spleen also harbors a unique subset of CD11c+ T-bet+ "atypical" B cells, which are associated with chronic inflammatory conditions and age-related immune changes [2].
Barrier Surfaces: The Gut as a Model
Barrier surfaces like the gut interface directly with the external environment. The jejunum, for instance, demonstrates a profoundly tissue-tailored immune system. It contains the highest frequency of CD4+ and CD8+ TRM cells across all tissues studied, identified by their expression of residency markers CD69, CD103, and CD49a [2]. The gut niche also supports specialized innate lymphoid cells (ILCs), particularly NCR2+IL7R− ILC1s, which also exhibit a strong tissue-resident signature [2]. Finally, the lamina propria is enriched with IgA+ plasma cells, underscoring the niche's focus on producing mucosal antibodies that neutralize pathogens without provoking excessive inflammation [2].
Table 2: Key Surface Markers for Identifying Tissue-Resident Immune Cells
| Cell Type | Core Defining Markers | Function & Significance |
|---|---|---|
| TRM (General) | CD69, CD103 (αE integrin), CD49a | Non-recirculating, sentinel function in tissues; rapid local response [13]. |
| Circulating Memory T Cells | CCR7, CD62L (L-selectrin) | Recirculate between blood and secondary lymphoid organs [13]. |
| CD8+ TEMRA | CD45RA, KLRG1 | Terminally differentiated effector cells; enriched in spleen and blood [2]. |
| CD4+ Treg | FOXP3, CD25 | Immunosuppressive function; enriched in lymph nodes [2] [10]. |
| Atypical B Cell | CD11c, T-bet (TBX21) | Associated with chronic infection and age; enriched in spleen [2]. |
Methodologies for Mapping Tissue Niches in Postmortem Studies
The insights gleaned from tissue niches rely on sophisticated experimental protocols. The following workflow and toolkit detail the key approaches.
Diagram 1: Experimental workflow for tissue immune profiling.
Core Experimental Protocols
1. Tissue Acquisition and Single-Cell Suspension Preparation:
- Source: Tissues (blood, lymphoid organs, lungs, intestines) are obtained from organ donors or postmortem patients [2] [14].
- Processing: Tissues are dissociated using established mechanical and enzymatic protocols to create viable single-cell suspensions while preserving cell surface epitopes [2].
- Critical Consideration: Rapid processing is essential to maintain RNA integrity and protein expression for downstream assays.
2. Multimodal Single-Cell Profiling (CITE-seq):
- Principle: Cellular Indexing of Transcriptomes and Epitopes by Sequencing (CITE-seq) simultaneously measures single-cell transcriptomes and over 100 surface proteins using antibody-derived tags (ADTs) [2].
- Procedure: Cells are stained with a panel of DNA-barcoded antibodies. Single cells are then encapsulated into droplets with barcoded beads for RNA and ADT capture, followed by library preparation and next-generation sequencing [2].
- Advantage: Resolves cell states that are indistinguishable by transcriptomics alone (e.g., distinguishing naive from central memory T cells via CD45RA) [2].
3. Spatial Validation using Multiplex Immunohistochemistry (mIHC) and Digital Spatial Profiling (DSP):
- Principle: Confirms the spatial relationships and protein expression identified in single-cell data within the intact tissue architecture.
- mIHC Protocol: Sequential staining of formalin-fixed paraffin-embedded (FFPE) tissue sections with antibodies conjugated to fluorescent dyes or metal tags, followed by high-resolution imaging [12] [15].
- DSP Protocol: FFPE sections are stained with oligonucleotide-barcoded antibodies. Regions of interest are selected and irradiated with UV light to release barcodes for quantification, allowing correlation of protein expression with tissue morphology [12].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Tissue Niche Profiling
| Reagent / Technology | Function in Experimental Pipeline |
|---|---|
| Panels of DNA-Barcoded Antibodies (CITE-seq) | Enable simultaneous quantification of >100 cell surface proteins alongside transcriptome in single cells [2]. |
| Multiplex Immunohistochemistry/Optical Clearing Kits | Allow visualization of multiple protein targets on a single tissue section, preserving spatial context [12] [15]. |
| Hash Tag Oligonucleotides (HTOs) | Enable sample multiplexing by labeling cells from different donors/tissues with unique barcodes, reducing batch effects and costs [14]. |
| Bioinformatic Tools (MrVI, MMoCHi, Seurat) | MrVI: Integrates data across samples and models technical variation [2]. MMoCHi: Uses protein and RNA data for automated cell classification [2]. Seurat: Standard toolkit for single-cell data analysis [14]. |
| AL-438 | AL-438, CAS:239066-73-0, MF:C23H25NO2, MW:347.4 g/mol |
| Boc-NH-PEG12-NH-Boc | Boc-NH-PEG12-NH-Boc, MF:C36H72N2O16, MW:789.0 g/mol |
The shift from a blood-centric to a tissue-centric view of immunology, powered by postmortem studies and advanced technologies, has revealed that immune protection is a local phenomenon orchestrated by specialized niches. The lung, lymph nodes, spleen, and barrier surfaces each maintain a unique ecosystem of resident immune cells whose function is dictated by their tissue microenvironment. This refined understanding is paving the way for a new generation of niche-specific therapeutic strategies, such as vaccines designed to induce protective TRM cells in barrier tissues or immunotherapies that target exhausted T cells within the tumor microenvironment. Future research will continue to decode the molecular signals that establish and maintain these niches, offering unprecedented opportunities for precise manipulation of immunity in human health and disease.
The immune system is a dynamic network of specialized cells distributed throughout the body to defend against infections, regulate inflammation, and repair tissue damage. Rather than functioning as a homogeneous system, immune cells exhibit remarkable functional specialization based on their tissue location. Understanding how the tissue microenvironment shapes immune cell identity, composition, and function represents a critical frontier in immunology with profound implications for therapeutic development. This technical guide examines the mechanisms of functional adaptation, drawing on evidence from human postmortem studies that provide unprecedented access to tissue-resident immune populations across the human body.
Tissue-Specific Immune Cell Profiling
Comprehensive Mapping of Immune Landscapes
Groundbreaking research utilizing single-cell multimodal profiling has revolutionized our understanding of tissue-specific immunity. A landmark 2025 study published in Nature Immunology comprehensively profiled over 1.25 million immune cells from blood, lymphoid, and mucosal tissues from 24 organ donors aged 20-75 years [2]. Using cellular indexing of transcriptomes and epitopes (CITE-seq) to simultaneously profile transcriptomes and >125 surface proteins, researchers identified dominant site-specific effects on immune cell composition and function across lineages [2].
Table 1: Tissue-Specific Enrichment of Immune Cell Subsets
| Immune Cell Subset | Enriched Tissue Sites | Key Identifying Markers | Primary Functions |
|---|---|---|---|
| CD4+ and CD8+ Tissue-Resident Memory T (TRM) cells | Jejunum (JEL, JLP), Lungs, Spleen, LN | CD69, CD103, CD49a [2] | Long-term tissue surveillance, rapid response to local pathogens |
| CD4+ Naive T (TN) cells | Blood, Multiple Lymph Nodes | CD45RA+ [2] | Antigen-naive precursors to effector/memory populations |
| CD8+ TEMRA cells | Bone Marrow, Spleen | CD45RA+, KLRF1, GZMB [2] | Terminally differentiated effectors with cytotoxic capability |
| CD56dimCD16+ NK cells | Blood, Bone Marrow, Lungs | KLRF1, GZMB [2] | Mature cytotoxic function |
| CD11c+ Memory B cells | Spleen, Bone Marrow | TBX21 (T-BET) [2] | "Atypical" B cell subset with specialized effector functions |
| IgA+ Plasma Cells | Jejunum Lamina Propria (JLP) | SDC1 (CD138) [2] | Mucosal antibody production |
| ILC1 | Jejunum | CD16-NCR2+IL7R-, CD69, CD49a, CD103 [2] | Tissue-resident innate immunity |
The distribution of T cell subsets varies dramatically across tissue sites. CD4+ naive T (TN) and central memory T (TCM) cells are predominantly enriched in blood and lymph nodes, while CD4+ and CD8+ tissue-resident memory T (TRM) cells prevail in jejunum and are present at lower frequencies in lungs, spleen, and lymph nodes [2]. CD8+ TEMRA cells, which exhibit terminally differentiated effector phenotypes, are primarily found in bone marrow and spleen [2].
Innate lymphoid populations also demonstrate tissue-specific patterning. Mature CD56dimCD16+ natural killer (NK) cells expressing cytolytic markers (KLRF1, GZMB) are enriched in blood, bone marrow, and lungs, while CD16-NCR2+IL7R- innate lymphoid cell 1 (ILC1) subsets with high expression of tissue residency markers (CD69, CD49a, CD103) are predominantly localized to jejunum [2].
B cell subset distribution is largely restricted to lymphoid organs, with notable tissue-specific specialization. CD11c+ memory B cells expressing TBX21 (encoding T-BET) resemble "atypical B cells" and localize primarily to spleen and bone marrow, while IgA+ plasma cells are uniquely enriched in jejunal lamina propria [2].
Table 2: Age-Associated Changes in Tissue-Specific Immune Populations
| Tissue Site | Immune Population | Age-Associated Changes |
|---|---|---|
| Mucosal Sites | Macrophages | Functional and compositional alterations [2] |
| Lymphoid Organs | B Cells | Compositional and functional shifts [2] |
| Blood & Tissues | CD8+ T cells | Functional, signaling, and metabolic changes [2] |
| Circulating Compartment | T cells and NK cells | Functional alterations across blood and tissues [2] |
Impact of Aging on Tissue-Specific Immunity
Aging exerts distinct effects on immune populations that vary by tissue site and lineage. While tissue-specific immune cell composition is largely maintained with age, significant functional, signaling, and metabolic alterations occur in specific subsets and locations [2]. Macrophages in mucosal sites, B cells in lymphoid organs, and circulating T cells and natural killer (NK) cells across blood and tissues demonstrate particular susceptibility to age-associated changes [2]. This age-related immunological decline, termed immunosenescence, involves progressive deterioration of both innate and adaptive immunity, though not all components are affected equally [16].
Experimental Approaches for Studying Tissue Immunity
Postmortem Tissue Processing and Cell Isolation
The study of human tissue immunity requires specialized methodologies for tissue acquisition and cell isolation. Postmortem tissues obtained from organ donors with appropriate ethical approvals and informed consent provide invaluable access to multiple tissue sites from individual donors [2] [17].
Diagram 1: Tissue Processing Workflow
For solid tissues such as lung, enzymatic digestion combined with mechanical dissociation is employed. The process involves cutting tissue into small pieces followed by incubation with an enzyme mixture typically containing collagenase D (1 mg/ml) and DNase I (1 μg/ml) [18]. Physical disintegration using instruments such as the gentleMACS Octo Dissociator with specific programs (e.g., "Lung Program 1" and "Lung Program 2") enhances cell yield [18]. The resulting suspension is sequentially filtered through 70μm and 40μm filters to remove debris and obtain a single-cell suspension [18].
Immunopanning provides an alternative approach for prospective purification of specific glial cells from human postmortem brain tissue [17]. This method uses cell type-specific antibodies coated on petri dishes to selectively isolate microglia, oligodendrocytes, and astrocytes from cortical gray matter [17].
Multimodal Single-Cell Profiling
Cellular indexing of transcriptomes and epitopes (CITE-seq) enables simultaneous profiling of transcriptomes and surface proteins at single-cell resolution [2]. This methodology allows for comprehensive immune cell annotation using tools such as MultiModal Classifier Hierarchy (MMoCHi), which leverages both surface protein and gene expression to hierarchically classify cells into predefined categories [2].
Diagram 2: Multimodal Profiling Pipeline
For data integration, multi-resolution variational inference (MrVI) is particularly valuable for cohort studies as it harmonizes variation between cell states while accounting for differences between samples [2]. Visualization with uniform manifold approximation and projection (UMAP) enables comparison across donors, sequencing technologies, and donor covariates such as sex and viral serostatus [2].
Ex Vivo Tissue Models
Advanced ex vivo models have been developed to study human immune responses in preserved tissue contexts. A hydrogel-based lymph node slice platform enables extended culture of patient-derived LN tissues, maintaining architecture, viability, and immune responsiveness for at least 7 days [19]. This system reduces cell egress and preserves LN cellular composition, phenotype, and spatial architecture, allowing evaluation of antitumoral and vaccine responses [19].
Technical Considerations and Limitations
Impact of Postmortem Interval
The postmortem interval (PMI) - the time between death and tissue preservation - represents a critical variable in postmortem tissue studies. Research indicates that even a 3-hour PMI can diminish detection of disease-specific transcriptomic signatures in brain tissues [20]. Basic quality control metrics such as the number of genes and reads per cell, total nuclei counts, and RNA integrity number may remain consistent, but differential gene expression between experimental conditions can be obscured [20].
PMI induces distinct transcriptional changes across cell types. In neurons, upregulated genes are involved in DNA repair, immune response, and stress pathways, while non-neuronal cell types show alterations in genes associated with cell-cell adhesion processes [20]. These effects highlight the importance of standardized PMI documentation and consideration in experimental design.
Methodological Constraints
Tissue-specific immune studies face several methodological challenges:
- Cell viability: Rapid processing is essential to maintain cell viability and preserve native transcriptional states [17].
- Representation of rare populations: Low-abundance immune subsets may be underrepresented in standard processing workflows.
- Spatial context loss: Single-cell dissociation methods disrupt native tissue architecture and cell-cell interactions.
- Technical variability: Differences in tissue collection, processing, and analysis protocols can introduce batch effects.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Tissue Immune Studies
| Reagent/Equipment | Application | Function | Example Specifications |
|---|---|---|---|
| Collagenase D + DNase I | Tissue dissociation | Enzymatic digestion of extracellular matrix | 1 mg/ml Collagenase D, 1 μg/ml DNase I [18] |
| gentleMACS Octo Dissociator | Tissue dissociation | Mechanical disintegration of solid tissues | Programmed protocols (e.g., "Lung Program 1") [18] |
| Anti-CD11b, Anti-O4, Anti-HepaCAM | Immunopanning | Isolation of microglia, oligodendrocytes, astrocytes | Coated on polystyrene Petri dishes [17] |
| CITE-seq Antibody Panels | Multimodal profiling | Simultaneous protein and transcript detection | >125 surface protein targets [2] |
| HA Hydrogels | Ex vivo culture | Preservation of tissue architecture in LN slices | Support viability for ≥7 days [19] |
| 10X Genomics Chromium | Single-cell sequencing | Single-cell partitioning and barcoding | 3' Gene Expression Kit v3.1 [20] |
| Pybg-tmr | Pybg-tmr, MF:C40H35N7O5, MW:693.7 g/mol | Chemical Reagent | Bench Chemicals |
| Fmoc-Cys-Asp10 | Fmoc-Cys-Asp10, MF:C58H67N11O34S, MW:1494.3 g/mol | Chemical Reagent | Bench Chemicals |
Immune cells demonstrate remarkable functional adaptation to their tissue microenvironments, exhibiting distinct compositional, phenotypic, and transcriptional profiles across different organs. The integration of advanced methodologies including multimodal single-cell profiling, sophisticated computational integration, and ex vivo tissue models provides unprecedented insight into these tissue-specific immune signatures. While technical challenges remain, particularly regarding postmortem interval effects and methodological standardization, ongoing technological innovations continue to enhance our understanding of how tissue microenvironments shape immune identity and function. This knowledge provides critical foundations for developing targeted therapeutic interventions that account for tissue-specific immune responses.
The immune system represents a clear example of an evolutionary arms race, constantly adapting under pressure from pathogens to maintain effective host defense. While the role of protein-coding genes in this process has been studied, a critical gap exists in understanding how adaptation manifests within the specific cellular contexts of human barrier tissues—the primary interfaces facing external pathogens. Recent advances in single-cell technologies and the development of comprehensive tissue atlases now enable the investigation of immune adaptation at unprecedented cellular resolution. This whitepaper synthesizes evidence from human postmortem studies to elucidate the distinct evolutionary pressures shaping immune cells in barrier tissues, providing a framework for understanding tissue-specific adaptation and its implications for therapeutic development.
Evidence of Adaptation in Barrier Tissue Immune Cells
Cellular Resolution of Immune Adaptation
Table 1: Key Evidence of Immune Cell Adaptation in Barrier Tissues
| Evidence Type | Key Finding | Experimental Approach | Citation |
|---|---|---|---|
| Cellular adaptation rate | Tissue-resident T and NK cells in adult lung show significantly increased adaptation rates | ABC-MK test on Human Cell Atlas data | [21] |
| Spatial distribution | Immune cells at tissue compartments directly facing external challenges show highest adaptation | Spatial transcriptomics from Lung Cell Atlas | [21] |
| Temporal patterns | Progenitor cells during development and adult cells in barrier tissues harbor increased adaptation | Developmental and Adult Immune Cell Atlas analysis | [21] |
| Functional specialization | Tissue-resident memory T cells (TRM) show distinct adaptation signatures | Single-cell RNA sequencing with differential gene expression | [21] [2] |
| Aging effects | Tissue residence may protect against immunosenescence in mucosal sites | Radiocarbon dating and turnover measurements | [22] |
Analysis of data from the Human Cell Atlas reveals abundant cell types, including progenitor cells during development and adult cells in barrier tissues, harbor significantly increased adaptation rates [21]. Research confirms the particular adaptation of tissue-resident T and NK cells in the adult lung located in compartments directly facing external challenges, such as respiratory pathogens [21]. This spatial organization of adaptation highlights how evolutionary pressures have shaped immune cells based on their functional positioning within tissue architectures.
Methodological Framework for Detecting Adaptation
The detection of adaptation in immune cells relies on sophisticated population genetics approaches applied to transcriptomic data. The primary method involves:
ABC-MK Test Implementation:
- Data Input: Top 500 differentially expressed genes (DEGs) per cell population (FDR < 1×10-4, logFC > 1)
- Statistical Framework: Approximate Bayesian Computation extension of McDonald-Kreitman test
- Adaptation Metrics: Proportion of adaptive non-synonymous substitution (α) and rate of adaptive non-synonymous substitution (ωa)
- Null Distribution: 1000 control datasets matching immune gene subset size [21]
This approach accounts for weakly selected polymorphisms and background selection, which can bias traditional tests of positive selection. By modeling multiple distributions of fitness effects alongside background selection, ABC-MK provides more accurate inference of adaptation parameters in heterogeneous genomic datasets [21].
Figure 1: Workflow for detecting immune cell adaptation in barrier tissues using single-cell data and population genetics approaches.
Tissue-Specific Immune Responses and Adaptation
Barrier Tissue Immune Niches
Human barrier tissues maintain distinct immune niches with specialized functional adaptations. Multimodal profiling of over 1.25 million immune cells from blood, lymphoid, and mucosal tissues reveals dominant site-specific effects on immune cell composition and function across lineages [2]. The tissue environment exerts a powerful influence on immune cell phenotypes, with mucosal sites such as the gut and lungs exhibiting unique immune signatures distinct from lymphoid organs or circulation.
Table 2: Tissue-Specific Immune Cell Distribution and Adaptation
| Tissue Site | Dominant Immune Cell Types | Key Adapted Functions | Age-Related Changes |
|---|---|---|---|
| Lung parenchyma & BAL | CD8+ TRM (CD69+CD103+), CD56dimCD16+ NK cells | Pathogen recognition, early response to respiratory pathogens | Macrophage functional alterations [2] |
| Jejunum (intestinal epithelium) | CD4+ and CD8+ TRM, CD16−NCR2+IL7R− ILC1s | Mucosal surveillance, barrier maintenance | Stable TRM maintenance with age [22] |
| Mesenteric lymph nodes | CD4+ Treg cells, germinal center B cells, ILC3s | Immune regulation, tolerance induction | B cell composition changes [2] |
| Skin | Tissue Tregs, resident macrophages | Wound healing, tissue repair | Not comprehensively studied [23] |
Tissue-resident memory T (TRM) cells demonstrate particularly strong signatures of adaptation. These cells are strategically positioned at barrier sites and exhibit enhanced functionality against previously encountered pathogens. In the lungs, TRM cells located at mucosal surfaces directly interfacing with the environment show the highest adaptation rates, reflecting their position at the frontline of host defense [21].
Structural Immunity and Barrier Reinforcement
The concept of "structural immunity" has emerged as an important adaptation in barrier tissues. This paradigm posits that the first line of immune defense involves the physical reinforcement of tissue barriers, a task directly or indirectly regulated by immune cells [24]. Several leukocyte subtypes help build protective barriers, either by depositing matrix components themselves or through interactions with structural cells and the extracellular matrix.
This structural function challenges traditional compartmentalization of mammalian tissue organization and immune defense. Immune cells acting as architects of tissue barriers represent an evolutionary adaptation that physically prevents pathogen entry, complementing traditional immunological recognition and elimination mechanisms [24].
Experimental Approaches and Methodologies
Human Tissue Processing and Cell Isolation
Tissue Acquisition and Processing Protocol:
- Source: Multiorgan donors (ages 2-93) through organ procurement organizations
- Tissues: Blood, lung, jejunum, spleen, lung-associated and mesenteric lymph nodes
- Processing: Mechanical dissociation followed by enzymatic digestion with Liberase TM (0.25 mg/ml)
- Cell Isolation: Density gradient centrifugation for mononuclear cell separation [22] [2]
Critical Considerations:
- Postmortem intervals minimized to maintain cell viability
- Exclusion criteria: chronic infection, cancer, overt inflammatory disease
- Demographic matching for age and sex comparisons [22] [2]
Single-Cell Multimodal Profiling
Advanced single-cell technologies enable comprehensive immune characterization:
CITE-seq (Cellular Indexing of Transcriptomes and Epitopes) Protocol:
- Cell Preparation: 1.28 million immune cells from 10+ tissue sites
- Antibody Panel: 127 surface protein markers
- Sequencing: Single-cell RNA sequencing with feature barcoding
- Data Integration: Multi-resolution variational inference (MrVI) for harmonization
- Cell Annotation: MultiModal Classifier Hierarchy (MMoCHi) leveraging both surface protein and gene expression [2]
Figure 2: Experimental workflow for multimodal profiling of human tissue immune cells from acquisition to adaptation analysis.
Lineage Tracing and Cellular Aging Studies
Retrospective Birth Dating of Human T Cells:
- Methodology: Radiocarbon (14C) dating based on atmospheric nuclear bomb testing
- Measurement: Determination of genomic DNA incorporation timing
- Lifespan Calculations: Integration with cellular turnover measurements [22]
Key Findings on T Cell Longevity:
- Blood and lymph node T cells: 1-2 years lifespan
- Splenic T cells: 3-10 years lifespan
- Tissue-resident memory T cells exhibit distinct aging dynamics with reduced senescent markers compared to circulating counterparts [22]
The Scientist's Toolkit
Table 3: Essential Research Reagents and Resources
| Reagent/Resource | Application | Function | Example Implementation |
|---|---|---|---|
| Liberase TM | Tissue dissociation | Enzymatic digestion of extracellular matrix | 0.25 mg/ml for 30-60 min at 37°C [25] [2] |
| CITE-seq antibody panels | Multimodal profiling | Simultaneous protein and RNA measurement | 127-surface protein panel [2] |
| Human Cell Atlas data | Reference mapping | Comprehensive transcriptome reference | Developmental and Adult Immune Cell Atlases [21] |
| ABC-MK algorithm | Adaptation rate calculation | Quantifying positive selection | Inference of α and ωa parameters [21] |
| MrVI (Multi-resolution Variational Inference) | Data integration | Harmonizing single-cell data across samples | Integration of datasets from multiple donors [2] |
| MMoCHi (MultiModal Classifier Hierarchy) | Cell annotation | Automated cell type classification | Leveraging protein and RNA for subset identification [2] |
| Fosfenopril-d7 | Fosfenopril-d7 | Fosfenopril-d7 is a deuterated internal standard for accurate LC/MS or GC/MS quantification of Fosinopril. For Research Use Only. Not for human use. | Bench Chemicals |
| hCAXII-IN-1 | hCAXII-IN-1|CA XII Inhibitor|For Research Use | hCAXII-IN-1 is a selective hCAXII inhibitor for cancer research. This product is for Research Use Only (RUO) and not for human use. | Bench Chemicals |
Discussion and Therapeutic Implications
The evidence of accelerated adaptation in barrier tissue immune cells underscores the evolutionary prioritization of defense at host-environment interfaces. These findings have significant implications for vaccine development, immunotherapies, and treatment of inflammatory diseases. Therapeutic strategies targeting tissue-resident immune populations may enhance protection against pathogens while avoiding systemic immune activation.
Future research directions should include:
- Comprehensive mapping of adaptation across more tissue sites and immune subsets
- Investigation of how adaptive signatures correlate with response to infection, vaccination, and immunotherapy
- Development of tissue-targeted delivery systems that leverage adapted immune mechanisms
- Exploration of how modern environmental changes affect ongoing adaptation in barrier immunity
The integration of evolutionary genetics with tissue immunology provides a powerful framework for understanding the design principles of human immune defense and for developing next-generation therapeutic approaches that work in harmony with evolved tissue-specific immunity.
The human immune system is a complex, dynamic network distributed throughout the body, with specialized functions tailored to specific tissue environments. For decades, immunological monitoring has predominantly relied on peripheral blood samples due to their accessibility, creating a fundamental gap in our understanding of localized immune responses. While blood provides a convenient window into systemic immunity, it fails to capture the specialized immune populations, functional states, and cellular interactions within tissues where diseases actually occur. This limitation is particularly critical in the context of infectious diseases, cancer immunotherapy, and autoimmune disorders, where tissue-specific immune dynamics determine clinical outcomes.
Recent advances in high-dimensional spatial profiling and multimodal single-cell analysis of postmortem tissues have revolutionized our capacity to investigate tissue-specific immunity, revealing profound functional specializations that are undetectable in circulation. This technical guide synthesizes cutting-edge methodologies and findings from human postmortem studies to demonstrate why comprehensive immune profiling must extend beyond blood to understand physiological and pathological immune responses truly.
Compelling Evidence: Tissue-Specific Immunity Revealed Through Postmortem Studies
Distinct Immune Compartmentalization in Severe COVID-19
Postmortem immune profiling of COVID-19 decedents has provided unprecedented insights into the spatial organization of immune responses during severe infection. A comprehensive high-dimensional analysis of 22 COVID-19 decedents from Wuhan, China, revealed TIM-3-mediated and PD-1-mediated immunosuppression as a hallmark of severe disease, particularly in male patients [26]. This exhaustive study, which employed digital spatial profiling (DSP) and multiplex immunohistochemistry (mIHC) across multiple organs, discovered that lymphocytes were systematically distal from SARS-CoV-2 viral antigens, while activated myeloid cells were consistently proximal, indicating prevalent infection of myeloid cells across multiple organs [26].
Crucially, the study demonstrated significant sexual dimorphism in immune responses, with male patients showing higher expression of inhibitory receptors (TIM-3, PD-1, CD39, BTLA) and lower expression of immune activation markers (Ki-67, CD69) in lung tissue [26]. This tissue-specific immunosuppressive signature was more pronounced in men and correlated with shorter survival duration, highlighting a pathological mechanism that would be impossible to decipher from peripheral blood studies alone [26].
Table 1: Key Tissue-Specific Immune Findings in Severe COVID-19 from Postmortem Studies
| Finding | Experimental Method | Tissue Localization | Significance |
|---|---|---|---|
| Myeloid cell infection | Multiplex IHC, Spatial profiling | Lung, Liver, Kidney, Spleen | Myeloid cells proximal to viral antigen; lymphocytes distal |
| Sex-specific immunosuppression | Bulk RNA-seq, mIHC | Lung, Kidney, Heart | TIM-3/PD-1 upregulation in males across organs |
| Viral load correlation | DSP, RNA-seq | Multiple organs | Positive correlation with immunosuppression and DC markers |
| Organ-specific NK cell activity | Spatial cell profiling | Lung vs. Liver | NK cells proximal to virus in liver but distal in lung |
Age and Tissue Microenvironment Interactions
A landmark 2025 study profiling over 1.25 million immune cells from blood, lymphoid, and mucosal tissues from 24 organ donors aged 20-75 years provided comprehensive evidence of tissue-directed immune signatures that vary with age [2]. Using cellular indexing of transcriptomes and epitopes (CITE-seq) to simultaneously profile transcriptomes and >125 surface proteins, researchers demonstrated that immune cell composition and function are predominantly determined by tissue site rather than circulation [2].
The study revealed that age-associated effects manifest specifically by tissue site and lineage: macrophages in mucosal sites, B cells in lymphoid organs, and circulating T cells and natural killer cells across blood and tissues showed distinct aging patterns [2]. For instance, memory B cells in lymphoid organs expressed CD69, denoting tissue residency, while plasma cells expressing IgA were enriched in the jejunal lamina propria, and IgG+ plasmablasts were enriched in lymphoid organs [2]. These findings establish that aging exerts highly specific effects on immune populations depending on their tissue localization, information completely masked in blood-only analyses.
Table 2: Tissue-Specific Immune Cell Distributions Revealed by Multimodal Profiling
| Immune Cell Type | Tissue-Specific Enrichment | Functional Significance |
|---|---|---|
| CD4+/CD8+ TRM cells | Jejunum, Lungs, Spleen, LN | Tissue-resident memory positioned for rapid local response |
| CD8+ TEMRA cells | Bone Marrow, Spleen | Terminally differentiated effectors in lymphoid reservoirs |
| MAIT cells | Spleen, BM, Lungs | Mucosal-associated invariant T cells at barrier sites |
| IgA+ Plasma cells | Jejunal Lamina Propria | Specialized for mucosal antibody production |
| CD56dimCD16+ NK cells | Blood, BM, Lungs | Cytolytic effectors at infection sites |
| CD11c+ Memory B cells | Spleen, BM | T-bet+ "atypical" B cells in lymphoid organs |
Methodological Framework: Postmortem Tissue Immune Profiling
Technical Considerations for Postmortem Studies
Postmortem tissue studies present unique methodological challenges that must be addressed to ensure data quality and interpretability. Confounding factors including sex, age at death, medication history, agonal state, postmortem interval (PMI), tissue storage duration, tissue pH, and RNA integrity number (RIN) significantly impact gene expression profiles [27]. A 2025 systematic assessment demonstrated that pH and RIN values particularly affect genes involved in energy production, immune system function, and DNA repair pathways [27].
The postmortem interval critically influences molecular integrity, with studies showing progressive RNA degradation over time. Research in rat models demonstrates that brain tissue morphology remains stable at 4°C for up to 21 days, while at 26°C, cytoplasmic and cell destruction becomes evident after 14 days [28]. Among housekeeping genes, Gapdh and 5S rRNA show high stability across extended PMIs, making them suitable reference genes for molecular analyses [28].
Advanced Spatial Profiling and Tissue Clearing Techniques
The development of SHARD (SHIELD, antigen retrieval, and delipidation) has dramatically improved capacity for three-dimensional immunostaining in long-term formaldehyde-fixed postmortem human brain tissue [29]. This method combines tissue stabilization, antigen retrieval, and lipid removal to enable high-resolution visualization of cellular morphology and spatial relationships in tissues with PMIs ranging from 10 to 72 hours [29].
For multiplexed protein detection, mass cytometry-based systems like the Maxpar Direct Immune Profiling System enable simultaneous measurement of 37+ immune cell types using metal-tagged antibodies, providing exceptional stability for multicenter studies [30]. When combined with spatial techniques like digital spatial profiling, researchers can achieve comprehensive molecular and spatial characterization of immune responses directly in tissues [26].
Diagram 1: Comprehensive Workflow for Postmortem Tissue Immune Profiling
Integrated Framework for Tissue Analysis
An effective organ-specific immunity research framework incorporates multiple complementary approaches. A 2023 study established a tissue analysis framework that combines digital pathology with molecular profiling to investigate local immune responses, emphasizing the importance of studying mucosal lymphoid tissues, macrophages, and dendritic cells in their native tissue context [31]. This integrated approach enables researchers to correlate specific immune cell populations with tissue injury patterns and pathogen localization, providing mechanistic insights into disease pathogenesis.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Tissue-Based Immune Profiling
| Reagent/Platform | Function | Application in Postmortem Studies |
|---|---|---|
| Maxpar Direct Immune Profiling Assay | High-parameter metal-tagged antibody panel | Standardized immunophenotyping of 37+ immune cell types in tissue digests |
| CITE-seq | Simultaneous transcriptome and surface protein profiling | Multimodal single-cell analysis of immune cell identity and function |
| SHARD Clearing Method | Tissue clarification and antigen retrieval | 3D immunostaining in long-term formaldehyde-fixed tissue |
| Digital Spatial Profiling | Spatially-resolved whole transcriptome analysis | Mapping immune cell localization relative to pathogens or pathology |
| Multiplex IHC | Simultaneous detection of multiple protein markers | Spatial characterization of immune cell populations and states |
| RNA Stabilization Reagents | Preservation of RNA integrity | Maintain molecular quality despite postmortem delays |
| IHCH-3064 | IHCH-3064, MF:C25H21N9O2, MW:479.5 g/mol | Chemical Reagent |
| H-Lys(Z)-OH-d3 | H-Lys(Z)-OH-d3, MF:C14H20N2O4, MW:283.34 g/mol | Chemical Reagent |
Experimental Protocols for Key Methodologies
SHARD Protocol for Tissue Clearing and Staining
The SHARD method enables robust three-dimensional imaging in challenging postmortem human brain tissue. The optimized protocol includes [29]:
- Tissue Stabilization: Incubate 200-μm tissue sections in SHIELD Epoxy Solution (LifeCanvas Technologies) for 48 hours at 4°C to stabilize macromolecules.
- Antigen Retrieval: Perform citrate-based antigen retrieval by incubating tissue in sodium citrate buffer (pH 9.0) at 80°C for 30 minutes to reverse formaldehyde cross-linking.
- Lipid Removal: Treat tissue with 0.1% sodium dodecyl sulfate (SDS) for 24-48 hours with gentle agitation to remove lipids and achieve optical clarity.
- Immunostaining: Incubate cleared tissue with primary antibodies for 48-72 hours, followed by fluorophore-conjugated secondary antibodies for 24-48 hours.
- Refractive Index Matching: Mount tissue in SHIELD Mounting Medium (LifeCanvas Technologies) for 24 hours before imaging.
This method successfully processes tissues with PMIs ranging from 10-72 hours across various neurodegenerative conditions and controls, making it particularly suitable for human brain bank samples [29].
High-Dimensional Immune Profiling Workflow
A comprehensive tissue-based immune profiling workflow incorporates both single-cell and spatial techniques [26] [2]:
- Tissue Digestion: Mechanically dissociate and enzymatically digest fresh tissue using collagenase/DNase cocktail to generate single-cell suspensions while preserving surface epitopes.
- Multimodal Single-Cell Profiling:
- Stain cells with CITE-seq antibody panels (127+ surface markers) with barcoded oligonucleotides
- Partition single cells using droplet-based microfluidics (10X Genomics)
- Prepare sequencing libraries for both transcriptome and surface protein detection
- Spatial Transcriptomics:
- Process adjacent tissue sections for spatial transcriptomics using Visium platform (10X Genomics)
- Correlate single-cell data with spatial localization patterns
- Multiplex Immunohistochemistry:
- Stain consecutive sections with validated antibody panels for immune activation (CD69, IFN-γ, granzyme B) and suppression markers (TIM-3, PD-1, BTLA)
- Quantify cell densities and spatial distributions using automated image analysis
Diagram 2: Tissue-Specific Immune Dysregulation Pathway in Severe COVID-19
The evidence from sophisticated postmortem tissue studies unequivocally demonstrates that peripheral blood provides an incomplete and often misleading representation of immune responses. Tissue-specific immune signatures, spatial organization of immune populations, and localized functional states critically determine pathological outcomes in infectious diseases, cancer, and inflammatory disorders. The integrated methodological framework presented here—combining multimodal single-cell analysis, spatial transcriptomics, and advanced tissue clearing techniques—enables comprehensive characterization of immune responses in their native tissue context.
For drug development professionals, these findings highlight the limitations of blood-based biomarkers and emphasize the necessity of developing tissue-targeted therapeutic strategies and localized immunomonitoring approaches. As immunology advances beyond its blood-centric legacy, embracing tissue-informed paradigms will be essential for developing next-generation immunotherapies and precision medicine approaches that account for the spatial dimension of immune responses.
Tools of the Trade: Profiling Immune Responses in Postmortem Tissues
Postmortem tissue samples are an indispensable resource for studying the molecular underpinnings of human health and disease, particularly for organs like the brain that cannot be sampled in living individuals. However, the validity of findings from these tissues hinges on recognizing and controlling for the profound effects of postmortem interval (PMI)—the time between death and tissue preservation—on molecular integrity. Research demonstrates that PMI is not merely a logistical variable but a biological process that actively alters the tissue's molecular landscape. A landmark study from Mount Sinai's Living Brain Project revealed "unequivocal evidence that brain tissue from living people has a distinct molecular character" compared to postmortem samples, with over 60% of proteins and 95% of RNA types showing differential expression or processing [32]. These findings necessitate a rigorous framework for tissue collection and processing that minimizes artifacts and preserves biological signals, especially when investigating delicate processes like tissue-specific immune responses.
This technical guide provides a comprehensive framework for postmortem tissue collection and processing, with particular emphasis on maintaining the integrity of immune signatures. We synthesize recent evidence on PMI-induced molecular changes, present optimized protocols for tissue preservation and nuclei isolation, and provide quantitative data on molecular degradation timelines to inform experimental design in translational research and drug development.
Molecular Consequences of Postmortem Interval
Transcriptomic and Proteomic Alterations
The postmortem period triggers rapid and extensive molecular changes that can obscure disease-specific signatures if not properly accounted for. Single-nucleus RNA sequencing studies in mouse models demonstrate that even a 3-hour PMI significantly diminishes the detection of disease-associated transcriptomic signatures, particularly in neuronal populations [20]. Comparative proteomic analyses between human and mouse models of amyotrophic lateral sclerosis (ALS) further reveal that PMI affects the representation of key biological processes, with human postmortem tissues showing prominent upregulation of immune processes and downregulation of mitochondrial function—patterns not consistently recapitulated in immediately processed animal models [33].
Table 1: Quantitative Molecular Changes Following Postmortem Interval
| Molecular Component | Experimental System | PMI Duration | Key Changes | Citation |
|---|---|---|---|---|
| RNA splicing & processing | Human prefrontal cortex | Variable (living vs postmortem) | 95% of tested RNA transcripts showed differences in splicing, primary RNA levels, or mature RNA levels | [32] |
| Protein expression | Human prefrontal cortex | Variable (living vs postmortem) | >60% of proteins differentially expressed between living and postmortem tissue | [32] |
| Disease-specific gene expression | PS19 tauopathy mouse model | 3 hours | Diminished number of genes differentially expressed between disease and WT models | [20] |
| Mitochondrial transcripts | Rat skeletal muscle | 48 hours | Significant upregulation of mt-ATP6, mt-ATP8, and mt-CO3 (FC > 7.78) | [34] |
| Vascular & metabolic pathways | Rat skeletal muscle | 48 hours | Upregulated nitric oxide transport; downregulated mitochondrial activity | [34] |
Cell-Type-Specific Vulnerabilities
Different cell populations exhibit distinct vulnerabilities to postmortem degradation processes. Neuronal gene expression signatures appear particularly susceptible to PMI effects, with studies showing that "PMI can obscure disease-related gene expression changes, especially in neurons" [20]. In contrast, glial-specific gene expression may demonstrate greater resilience to postmortem degradation. Analysis of postmortem interval effects at single-nucleus resolution identified PMI-induced upregulation of genes involved in DNA repair, immune response, and stress pathways in neurons and interneurons, while alterations in non-neuronal cell types were associated with cell-cell adhesion processes [20].
Practical Protocols for Tissue Processing and Analysis
Optimized Nuclei Isolation from Postmortem Primate Brain Tissue
The isolation of high-quality nuclei from postmortem frozen tissue is a critical first step for single-cell sequencing and other genomic applications. The following protocol has been specifically optimized for challenging postmortem primate brain tissue and addresses common issues including high debris, reduced RNA integrity, and autofluorescence [35]:
Tissue Preparation: Microdissect frozen cerebral cortex tissue on dry ice using a 2mm biopsy punch, yielding 25-50mg tissue samples. Maintain tissue frozen throughout dissection to prevent thawing.
Nuclei Isolation: Use the 10X Genomics Chromium Nuclei Isolation Kit with RNase Inhibitor with optimized lysis time (adjust based on tissue quality; typically 10-15 minutes). Include additional filtration using Flowmi cell strainers (70μm) to reduce debris. Perform extra wash steps with nuclei extraction buffer to improve purity.
Quantification and Quality Control: Quantify nuclei suspensions using automated cell counters with fluorescent viability stains (Acridine Orange/Propidium Iodide). Successful isolations typically show >70% double-stained or PI-labeled nuclei. Assess RNA integrity number (RINe) when possible, though this may be unreliable in significantly degraded samples [20].
Immunostaining for Neuronal Enrichment: Incubate nuclei with primary antibody for neuronal marker NeuN (1:100 dilution) for 30 minutes on ice. Remove unbound antibody by centrifugation (400 rcf for 5 minutes). Add fluorescent secondary antibody and incubate 15 minutes in dark on ice. Wash twice to reduce background fluorescence.
Fluorescent-Activated Nuclei Sorting (FANS): Analyze samples using a cell sorter (e.g., Sony SH800Z) with appropriate laser configuration. Establish gates using unstained and secondary antibody-only controls. Sort DAPI-positive nuclei above background fluorescence threshold for neuronal populations. Collect sorted nuclei in chilled blocking buffer for downstream applications.
Cell Death Analysis in Complex Tissue Organoids
For disease modeling and drug screening applications, glioblastoma organoids (GBOs) represent a valuable platform that preserves tumor heterogeneity. The following flow cytometry protocol enables quantitative cell death analysis in these complex, dense structures [36]:
Organoid Dissociation: Generate single-cell suspensions from GBOs through combined enzymatic and mechanical dissociation. Use gentleMACs Octo Dissociator with heaters running appropriate dissociation programs.
Cell Permeabilization and Staining: Permeabilize cells with 0.1% Triton X-100 for 15 minutes at 4°C. Stain with propidium iodide (PI, 50μg/mL) for 30 minutes in the dark. PI intercalates into fragmented DNA of dying cells.
Flow Cytometry Analysis: Analyze samples using a flow cytometer with 488nm excitation and 617nm emission detection. Identify hypodiploid cells (sub-G1 peak) as a measure of cell death. Include debris and doublet exclusion gates for accurate quantification.
Validation Methods: Confirm treatment-induced effects using complementary methods including Hoechst 33258 staining, lactate dehydrogenase (LDH) release assays, and measurements of organoid diameter changes.
Table 2: Essential Research Reagents for Postmortem Tissue Analysis
| Reagent/Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Nuclei Isolation Kits | 10X Genomics Chromium Nuclei Isolation Kit | Isolation of intact nuclei from frozen tissue | Optimize lysis time; add extra filtration steps for debris-heavy tissue |
| RNase Inhibitors | Promega RNase Inhibitor | Prevent RNA degradation during processing | Use in all buffers and wash steps (0.2 U/μL final concentration) |
| Viability Stains | Acridine Orange/Propidium Iodide; DAPI | Nuclei quantification and viability assessment | AO/PI for general assessment; DAPI for flow sorting applications |
| Cell Type Markers | Anti-NeuN Antibody | Neuronal nuclei identification and enrichment | Validate staining with positive/negative control populations |
| Dissociation Reagents | Miltenyi Nuclei Extraction Buffer | Tissue dissociation and nuclei release | Supplement with RNase inhibitors; maintain cold temperatures |
| Cell Death Assays | Propidium Iodide; LDH Assay Kits | Quantification of apoptosis/necrosis in tissue models | Combine with mechanical dissociation for dense organoids |
Immune Response Dynamics in Postmortem Tissues
Special Considerations for Neuroimmune Studies
The investigation of immune responses in postmortem neural tissues requires particular attention to PMI effects, as immune activation signatures may be especially vulnerable to postmortem alterations. Studies indicate that "PMI altered the transcriptome in the central nervous system (CNS) and blood, dysregulating pathways involved in immune response" [20]. This has profound implications for research on neuroinflammatory conditions such as Alzheimer's disease, multiple sclerosis, and neurodegenerative disorders.
Recent research has identified specific molecular regulators of blood-brain barrier function and immune cell infiltration that may be sensitive to PMI effects. For instance, the scaffold protein IQGAP2 has been identified as a key regulator of brain endothelial cell immune privilege, with loss of IQGAP2 associated with increased leukocyte infiltration and inflammatory signatures in brain endothelial cells [37]. Alzheimer's disease tissue analyses further reveal disease-associated reductions in hippocampal IQGAP2, suggesting this molecule may represent a sensitive marker of neuroimmune status vulnerable to improper tissue processing [37].
Framework for Preserving Immune Signatures
To accurately capture immune dynamics in postmortem tissues, researchers should implement the following practices:
Standardized PMI Documentation: Record precise death-to-preservation intervals for all samples and include as covariate in statistical models. Consider stratifying analyses by PMI when possible.
Validation with Fresh Tissue Comparisons: Where feasible, validate key findings in freshly processed tissue models or surgical specimens to confirm PMI resilience of observed immune signatures.
Multi-omics Corroboration: Support transcriptomic findings of immune activation with proteomic analyses of corresponding cytokines, chemokines, and immune cell markers to distinguish transcriptional changes from protein-level immune responses.
Cell-Type-Specific Resolution: Employ single-cell or nuclei sorting approaches to resolve immune signatures in specific cell populations, as bulk tissue analyses may mask cell-type-specific effects of PMI on immune gene expression.
The reliability of research findings from postmortem tissues depends critically on implementing a standardized framework that acknowledges and mitigates the substantial effects of postmortem interval on molecular integrity. Based on current evidence, the following best practices are recommended:
Minimize PMI Whenever Possible: While not always feasible, efforts to reduce death-to-preservation intervals below 3 hours can significantly improve detection of disease-specific signatures, particularly for neuronal and immune transcripts.
Implement Rigorous Quality Control: Establish minimum quality thresholds for RNA integrity, nuclei viability, and immunostaining specificity. Document and report these metrics for all experiments.
Account for PMI in Study Design: Match comparison groups by PMI, include PMI as a covariate in statistical models, and consider PMI-matched control tissues for disease studies.
Select Appropriate Preservation Methods: For immune and transcriptional studies, prioritize rapid freezing at -80°C or colder with RNase protection for bulk analyses, or immediate nuclei isolation for single-cell applications.
Validate Key Findings: Where possible, corroborate findings from postmortem tissues with living tissue models, animal studies, or human surgical specimens to ensure biological validity.
As research methodologies advance, the integration of standardized PMI-aware processing frameworks will enhance the translational potential of postmortem tissue studies, particularly in the realm of neuroimmunology and neurodegenerative disease research.
High-parameter flow cytometry represents a transformative advancement in single-cell analysis, enabling researchers to unravel extraordinary cellular diversity and heterogeneity within the immune system. By simultaneously measuring dozens of parameters, these technologies have revolutionized our understanding of complex biological systems, particularly in the context of tissue-specific immune responses. The implementation of 29-color panels represents a significant methodological achievement that balances comprehensive marker coverage with technical feasibility, allowing for deep immunophenotyping of rare cell populations in limited human tissue samples [38]. This technical guide explores the application of high-parameter flow cytometry within human postmortem studies, providing researchers and drug development professionals with the experimental frameworks necessary to investigate tissue-resident immunity across different anatomical sites.
The transition from conventional flow cytometry to high-parameter platforms has been driven by the recognition that immune cell identity and function are dictated by complex combinations of surface receptors, transcription factors, and functional markers. Where traditional flow cytometry might identify broad cell lineages, 29-color panels can reveal subtle phenotypic changes associated with tissue residency, cellular differentiation, and functional specialization [39]. This is particularly valuable in human postmortem studies, where tissue samples from organ donors provide a unique opportunity to investigate immune cell distribution and function across multiple anatomical sites from the same individual, creating a comprehensive picture of systemic immunity [2].
Technological Foundations of High-Parameter Flow Cytometry
Instrumentation Capabilities
Modern high-parameter flow cytometers are engineering marvels designed to resolve complex fluorescence signatures. The successful implementation of a 29-color panel, as described in the human liver NK cell study, requires an instrument such as the BD FACSymphony A5, equipped with five lasers (UV, violet, blue, yellow/green, and red) and 50 detectors [38]. This configuration provides the necessary optical flexibility to measure multiple fluorescence parameters simultaneously while maintaining the sensitivity required to detect low-abundance markers.
The fundamental difference between conventional and spectral flow cytometry becomes particularly relevant when designing high-parameter panels. Conventional flow cytometers employ a "one detector–one fluorophore" approach using complex systems of dichroic mirrors and bandpass filters to direct specific wavelength ranges to corresponding detectors [40]. In contrast, spectral flow cytometers capture the full emission spectrum of each fluorophore using a prism or diffraction grating, scattering the emitted light across an array of highly sensitive detectors [40]. This spectral unmixing approach significantly increases the number of markers that can be analyzed in a single panel and provides superior resolution for fluorophores with overlapping emission spectra.
Panel Design and Fluorophore Selection
The design of a 29-color panel requires careful consideration of antigen density, fluorophore brightness, and instrument configuration. The panel developed for human tissue-resident NK cell analysis exemplifies this strategic approach, incorporating markers across multiple functional categories [38] [39]:
- Lineage and identification markers: CD3, CD19, CD14, CD56, CD16
- Tissue-residency markers: CD69, CD103, CD49a, CD49e, CXCR6
- Activating and inhibitory receptors: NKG2D, NKG2A, DNAM-1
- Differentiation markers: CD57, CD27, CD11b
- Chemokine receptors: CCR5, CCR7, CXCR3
- Transcription factors: T-bet, Eomes
Fluorophore selection must account for relative brightness and potential spectral overlap. The human liver NK cell study utilized BD Horizon Brilliant dyes and supplemented all staining steps with BD Horizon Brilliant Stain Buffer Plus to minimize staining artifacts commonly observed when several BD Horizon Brilliant dyes are used together [38]. This attention to technical detail is essential for achieving clean, reproducible results in high-parameter workflows.
Table 1: Key Instrumentation Platforms for High-Parameter Flow Cytometry
| Instrument | Laser Configuration | Detection Channels | Max Parameters | Technology |
|---|---|---|---|---|
| BD FACSymphony A5 | 5 lasers (355, 405, 488, 561, 637 nm) | 50 detectors | 50 parameters | Conventional |
| Cytek Aurora | 5 lasers (355, 405, 488, 561, 640 nm) | 64 fluorescent channels | 40 parameters | Spectral |
| Sony ID7000 | Up to 7 lasers | 184 fluorescent channels | 44+ parameters | Spectral |
| Agilent NovoCyte Opteon | Up to 5 lasers | 73 fluorescent channels | 45 parameters | Spectral |
Experimental Design for Tissue-Based Studies
Sample Acquisition and Processing
Human postmortem studies utilizing organ donor tissues provide an unparalleled opportunity to investigate tissue-specific immune responses across multiple anatomical sites from the same individual. This approach was effectively demonstrated in a comprehensive multimodal profiling study that analyzed over 1.25 million immune cells from blood, lymphoid, and mucosal tissues from 24 organ donors aged 20–75 years [2]. The integrity of cell surface epitopes is paramount for successful high-parameter flow cytometry, making standardized sample processing protocols essential.
For solid tissues, mechanical dissociation followed by enzymatic processing is typically required. The liver NK cell study employed a three-step perfusion protocol with enzymatic processing using collagenase XI to isolate mononuclear liver cells from the tumor non-affected area of liver tissue [38]. Similarly, the multimodal profiling study used established protocols to isolate mononuclear cells from blood, bone marrow, spleen, lymph nodes, lungs, and jejunum [2]. Consistent processing across all tissues minimizes technical variability and ensures comparable results between different anatomical sites.
Staining Protocol for High-Parameter Panels
The complexity of 29-color panels necessitates meticulous staining protocols to ensure optimal antibody binding while minimizing fluorescence spillover. The established methodology for the tissue NK cell panel follows a sequential approach [38] [39]:
Cell Preparation: Cryopreserved mononuclear cell suspensions are thawed rapidly at 37°C, washed twice in complete cell medium, resuspended in FACS buffer (PBS with 2 mM EDTA and 2% FBS), filtered through a 40 μm strainer, and counted.
Surface Antigen Staining: Cells are incubated with antibodies against surface antigens diluted in 50 μl FACS buffer for 20 minutes at room temperature in the dark, followed by two washes with 150–200 μl FACS buffer.
Viability Staining and Streptavidin Conjugates: In a second staining step, cells are stained with LIVE/DEAD Fixable Aqua Dead Cell Stain and fluorescently conjugated streptavidin for 20 minutes, followed by two washes.
Fixation and Permeabilization: Samples are fixed for 45 minutes in freshly prepared fixation/permeabilization working solution from eBioscience Foxp3/Transcription Factor Staining Buffer set.
Intracellular Staining: After fixation, cells are washed once in 1× permeabilization buffer and stained with antibodies against intracellular antigens (including transcription factors) diluted in 1× permeabilization buffer for 30 minutes.
Acquisition: Samples are washed twice in 1× permeabilization buffer, resuspended in 200 μl FACS buffer, filtered through a 35 μm strainer cap, and acquired on a calibrated flow cytometer.
Throughout the staining process, BD Horizon Brilliant Stain Buffer Plus is supplemented at a 1:5 ratio to minimize staining artifacts [38]. Single-stained compensation beads are used according to manufacturer's instructions to prepare compensation controls for all fluorescently conjugated antibodies.
Data Analysis Strategies for High-Dimensional Datasets
Computational Approaches for High-Parameter Data
The analysis of high-parameter flow cytometry data requires specialized computational approaches that circumvent traditional Boolean gating strategies. As noted in the mass cytometry guide, "analyzing mass cytometry data requires a major shift in how to approach these data, moving away from user-defined, Boolean gating strategies to automated identification of cell clusters and phenotypes" [41]. This principle applies equally to high-parameter flow cytometry data, where the complexity exceeds practical manual analysis.
Several algorithms have been developed specifically for high-dimensional cytometry data analysis:
viSNE (t-Distributed Stochastic Neighbor Embedding): A dimensionality reduction technique that projects high-dimensional data into two or three dimensions for visualization while preserving local structure [41].
PhenoGraph: A clustering algorithm that automatically identifies communities of similar cells in high-dimensional space, effectively defining cell populations without manual gating [41].
SPADE (Spanning-tree Progression Analysis of Density-normalized Events): Constructs a minimum spanning tree to visualize relationships between cell populations and can reveal continuous differentiation trajectories [41].
Citrus (Cluster Identification, Characterization, and Regression): Identifies stratifying cell populations between experimental groups by correlating cluster abundance with sample metadata [41].
In the human liver NK cell study, dimensionality reduction techniques were crucial for unraveling NK cell repertoire diversity. When applied to lymphocytes across multiple tissues, these methods ordered events primarily according to lineage rather than tissue of origin. However, when the analysis was narrowed specifically to the NK cell lineage, subsets separated according to tissue, enabling detailed phenotypic characterization of tissue-specific subpopulations [38].
Identification of Tissue-Resident Populations
The application of high-dimensional analysis to human tissue samples has revealed remarkable specialization of immune cells based on their tissue microenvironment. In the comprehensive multimodal study, tissue-resident memory T cells (TRM) were distinguished from circulating memory subsets based on surface expression of CD69, CD103, and/or CD49a [2]. These TRM cells were predominantly found in jejunum and present at lower frequencies in lungs, spleen, and lymph nodes, demonstrating distinct tissue distribution patterns.
Similarly, the liver NK cell study identified CD49e as a key marker for identifying liver-resident NK cell subsets [38]. This finding emerged from the integrated analysis of multiple tissue sites and exemplifies how high-parameter flow cytometry can resolve controversies in the literature regarding tissue-resident cell phenotypes by simultaneously evaluating dozens of potential markers.
Table 2: Key Markers for Identifying Tissue-Resident Immune Cells
| Cell Type | Tissue-Residence Markers | Tissue Distribution | Functional Characteristics |
|---|---|---|---|
| Liver-resident NK cells | CD49e-, CXCR6+, EomeshiT-betlo | Liver (30-40% of lymphocytes) | Antigen-specific memory, cytolytic activity [38] |
| CD8+ TRM cells | CD69+, CD103+, CD49a+ | Jejunum, lungs, spleen, LN | Rapid response to local antigen re-exposure [2] |
| CD4+ TRM cells | CD69+, CD103±, CD49a± | Jejunum, lungs, spleen, LN | Local cytokine production, helper functions [2] |
| Mucosal B cells | CD69+, CD27+ | Lymphoid organs, mucosal sites | Local antibody production, IgA class switching [2] |
Applications in Tissue-Specific Immune Responses
Insights from Human Postmortem Studies
Human postmortem studies utilizing high-parameter flow cytometry have revealed fundamental principles of tissue immunity. The multimodal profiling of over 1.25 million immune cells from multiple tissues demonstrated that "immune cell subset composition is specific to the tissue" [2]. This tissue-specific imprinting was observed across lineages, with distinct microenvironmental signatures defining cell composition and function in gut, lungs, and lymphoid organs.
The power of high-parameter analysis to resolve complex tissue-specific signatures is particularly evident in the characterization of human liver NK cells. Traditional approaches might have identified broad NK cell populations, but the 29-color panel revealed extraordinary diversity within liver NK cells and enabled the identification of previously unrecognized subsets [38]. This deep phenotyping approach provides a template for investigating tissue-specific immunity across other organ systems.
Age-Related Changes in Tissue Immunity
High-parameter flow cytometry applied to human postmortem samples across a wide age range (20-75 years) has revealed how aging differentially affects immune populations in various tissues. The comprehensive multimodal study found that "age-associated effects were manifested by site and lineage for macrophages in mucosal sites, B cells in lymphoid organs, and circulating T cells and natural killer cells across blood and tissues" [2]. This nuanced understanding of how aging impacts distinct immune compartments would not be possible without the multi-tissue, high-parameter approach.
Interestingly, despite age-associated changes in specific subsets and sites, the overall tissue-specific immune cell composition was largely maintained throughout the lifespan [2]. This preservation of tissue immunity architecture suggests robust homeostatic mechanisms that maintain tissue immune landscapes even as individual cell functions may be altered with age.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Reagents for 29-Color Flow Cytometry Panels
| Reagent Category | Specific Examples | Function/Purpose | Considerations |
|---|---|---|---|
| Brilliant Staining Buffer | BD Horizon Brilliant Stain Buffer Plus | Minimizes staining artifacts with multiple Brilliant dyes | Use at 1:5 dilution in all staining steps [38] |
| Viability Dyes | LIVE/DEAD Fixable Aqua Dead Cell Stain | Distinguishes live from dead cells | Critical for excluding compromised cells from analysis [38] |
| Fixation/Permeabilization Kits | eBioscience Foxp3/Transcription Factor Staining Buffer Set | Enables intracellular staining for transcription factors | Freshly prepare working solution for consistent results [38] |
| Compensation Beads | UltraComp eBeads Compensation Beads | Create single-color controls for compensation | Incubate with each fluorescent antibody used in panel [38] |
| Cell Staining Media | FACS Buffer (PBS + 2mM EDTA + 2% FBS) | Provides optimal staining environment | EDTA prevents cell clumping; serum reduces non-specific binding [38] |
| Surface Antibodies | CD16, CD56, CD3, CD19, CD14, CD69, CD103, CCR5, etc. | Cell surface phenotyping | Titrate antibodies for optimal signal-to-noise ratio [38] [39] |
| Intracellular Antibodies | T-bet, Eomes, Ki-67, etc. | Detection of intracellular proteins | Requires fixation/permeabilization before staining [38] |
| Antitumor agent-65 | Antitumor agent-65, MF:C18H17NO10, MW:407.3 g/mol | Chemical Reagent | Bench Chemicals |
| (R)-Linezolid-d3 | (R)-Linezolid-d3, MF:C16H20FN3O4, MW:340.36 g/mol | Chemical Reagent | Bench Chemicals |
Future Perspectives and Concluding Remarks
High-parameter flow cytometry represents a cornerstone technology in the age of single-cell biology, providing unprecedented resolution for investigating tissue-specific immune responses. The implementation of 29-color panels, as exemplified by the human liver NK cell study, demonstrates how carefully designed and validated high-parameter approaches can resolve biological questions that were previously intractable with conventional methods [38]. When integrated with human postmortem studies that provide access to multiple tissues from the same donor, these techniques enable comprehensive mapping of the human immune system across anatomical compartments.
The future of high-parameter flow cytometry will likely involve increased integration with other single-cell technologies, such as CITE-seq (Cellular Indexing of Transcriptomes and Epitopes by Sequencing), which simultaneously profiles transcriptomes and surface proteins [2]. As the field progresses toward even higher parameter measurements, computational approaches for data analysis will become increasingly important for extracting biological insights from these complex datasets [41]. Nevertheless, the 29-color panel represents a sweet spot in the trade-off between comprehensiveness and technical feasibility, providing sufficient parameters for deep immunophenotyping while remaining accessible to well-equipped research laboratories.
For researchers and drug development professionals, high-parameter flow cytometry offers a powerful tool for understanding tissue-specific immunity in health, disease, and throughout the human lifespan. The methodologies and applications described in this technical guide provide a foundation for designing studies that leverage the full potential of this transformative technology.
The accurate identification of immune cell types represents a fundamental challenge and opportunity in modern biomedical research, particularly in the context of human postmortem studies investigating tissue-specific immune responses. Single-cell RNA sequencing (scRNA-seq) has revolutionized our ability to analyze gene expression profiles at unprecedented resolution, enabling detailed characterization of cellular heterogeneity at the individual cell level. However, the complex and hierarchical relationships of immune cell types have made accurate classification particularly challenging using conventional computational approaches [42]. Traditional methods often treat cell types as flat categories without leveraging the known biological hierarchies of immune cell lineages, potentially missing crucial biological insights relevant to understanding neuroimmune interactions in postmortem tissues.
The emergence of sophisticated artificial intelligence frameworks has begun to transform this landscape. Among these, scHDeepInsight represents a significant advancement by integrating deep learning with biologically informed hierarchical classification architectures. This technical guide examines the core architecture, experimental protocols, and practical applications of scHDeepInsight within the context of tissue-specific immune responses in human postmortem studies, providing researchers with a comprehensive framework for implementing this powerful methodology in their investigative workflows.
scHDeepInsight: Core Architecture and Technical Innovation
Hierarchical Classification Framework
scHDeepInsight extends the previous scDeepInsight model by implementing a biologically informed classification architecture that explicitly incorporates the hierarchical relationships among immune cell types. Unlike conventional "flat" classification approaches that treat all cell types as independent categories, scHDeepInsight employs a structured multilevel classification process that mirrors established immune cell lineage relationships [42]. This hierarchical organization preserves biological continuity among related subtypes while maintaining clear separation between major immune lineages.
The framework's architecture processes scRNA-seq data through several sophisticated computational stages. Initially, gene expression vectors undergo transformation into two-dimensional images using the DeepInsight methodology, followed by random masking to enhance robustness. These processed images are then fed into a Convolutional Neural Network (CNN) based on the EfficientNet-B5 architecture for feature extraction. The core innovation lies in the hierarchical classification component, which implements a two-stage prediction process: first identifying primary immune cell types (base-types), then refining these predictions to specific subtypes within each lineage [42].
Adaptive Hierarchical Focal Loss (AHFL)
A critical technical innovation within scHDeepInsight is the Adaptive Hierarchical Focal Loss function, which dynamically balances training priorities across different levels of the cell type hierarchy. The AHFL extends the focal loss framework to optimize classification performance simultaneously at both base-type and subtype levels, automatically adjusting the weights of base-type and subtype focal losses according to their relative performance during training [42]. This approach effectively addresses the class imbalance commonly observed in single-cell RNA-seq datasets, where rare immune cell subtypes can be underrepresented by orders of magnitude compared to abundant populations.
The mathematical formulation of the AHFL ensures that the model maintains predictive accuracy across different granularity levels while preserving the biological relationships between cell types. By explicitly modeling the hierarchical structure of immune cell populations, scHDeepInsight achieves an average accuracy of 93.2% across seven diverse tissue datasets, surpassing contemporary methods by 5.1 percentage points and successfully distinguishing 50 distinct immune cell subtypes with high accuracy [42].
Computational Workflow and Methodological Protocols
Data Preprocessing and Image Transformation
The scHDeepInsight framework implements a sophisticated pipeline for converting high-dimensional scRNA-seq data into CNN-compatible two-dimensional image representations. This process employs the pyDeepInsight tool to map each gene to a specific pixel location, with pixel intensity reflecting the corresponding gene expression level [42]. Manifold techniques, including t-SNE and Uniform Manifold Approximation and Projection (UMAP), project the data into a 2D space using optimized perplexity settings, positioning genes with similar expression patterns in close proximity.
To ensure an optimal gene-to-pixel assignment and eliminate potential collisions where multiple genes would be mapped to the same pixel location, a Linear Sum Assignment algorithm is applied. The resulting 2D representations (224 × 224 × 3) are then utilized by the EfficientNet-B5 CNN for feature extraction and cell type classification. Considering that query datasets may lack certain genes present in the reference atlas used for training, random masking is introduced to the generated images, thereby injecting controlled noise to enhance robustness against missing gene features in query data [42].
Table 1: Key Components of scHDeepInsight Workflow
| Component | Implementation | Function |
|---|---|---|
| Image Transformation | DeepInsight framework with t-SNE/UMAP | Converts gene expression vectors to 2D images |
| Feature Extraction | EfficientNet-B5 CNN | Extracts hierarchical features from gene expression images |
| Hierarchical Classification | Multi-level architecture with AHFL | Classifies cells at base-type and subtype levels |
| Batch Correction | Harmony integration | Corrects technical variations across datasets |
| Interpretability | SHAP analysis | Quantifies gene contributions to classification decisions |
Model Training and Validation Protocol
The training phase of scHDeepInsight utilizes a comprehensive reference dataset constructed from over 460,000 cells from healthy donors across multiple tissues, including blood, lung, intestine, liver, and bone marrow. This integrated reference atlas encompasses 15 base immune cell types and more than 50 subtypes, centered on the top 5,000 highly variable genes extracted via Scanpy from the reference datasets [42]. The data integration pipeline follows a systematic workflow from initial study selection through quality control, normalization, and batch correction using STACAS-based harmonization.
During training, the model undergoes optimization through the adaptive hierarchical focal loss function, which balances performance across the hierarchy levels. The framework employs a probability-based detection mechanism for rare cell identification that analyzes discrepancy patterns between base-type and subtype prediction confidences. For validation, independent query datasets sourced from various public databases covering different tissues and cell types are processed through the trained model, with performance metrics calculated at both base-type and subtype levels to ensure comprehensive evaluation [42].
Applications in Tissue-Specific Immune Response Research
Integration with Postmortem Neurodegenerative Studies
The scHDeepInsight framework offers particular utility for investigating tissue-specific immune responses in human postmortem studies, especially in the context of neurodegenerative diseases. Recent research has revealed that APOE ε4 carriers share consistent pro-inflammatory immune signatures across neurodegenerative diseases including Alzheimer's disease, frontotemporal dementia, and Parkinson's disease dementia [43]. These signatures are characterized by enrichment in specific immune pathways and cells, including monocytes, T cells, and natural killer cells, detectable across brain, cerebrospinal fluid, and plasma compartments.
Single-cell RNA sequencing analysis of immune cell populations in these contexts can benefit substantially from hierarchical classification approaches. For instance, comprehensive post-mortem analyses have demonstrated that APOE ε4 carriage exacerbates the accumulation of phosphorylated tau and amyloid pathology, with glial activation measured by Iba1 (microglia) and GFAP (astrocytes) demonstrating amyloid-specific correlation [44]. The ability to accurately classify immune cell subtypes involved in these neuroinflammatory processes enables researchers to disentangle the complex immune mechanisms contributing to neurodegenerative pathology.
Pan-Cancer Immunological Analysis
Beyond neurodegenerative research, scHDeepInsight has demonstrated significant utility in cancer immunology, particularly in characterizing the tumor immune microenvironment. Studies investigating Gasdermin D (GSDMD), a key executor of pyroptosis, have revealed its role as a predictive biomarker for immunotherapy response across multiple cancer types [45]. Pan-cancer analyses have shown that GSDMD expression correlates with tumor mutational burden, microsatellite instability, and immune checkpoint expression, with high GSDMD expression associated with increased infiltration of pro-inflammatory immune cells.
The application of scHDeepInsight to such datasets enables refined characterization of immune cell populations within the tumor microenvironment, potentially identifying rare immune subtypes that influence therapeutic response. Single-cell RNA sequencing analysis of tumor-infiltrating immune cells has revealed distinct cellular communities and communication patterns that vary based on GSDMD expression status, highlighting the framework's utility in dissecting complex immune-cancer cell interactions [45].
Table 2: Research Reagent Solutions for scRNA-seq Immune Cell Analysis
| Research Reagent | Application | Function in Experimental Protocol |
|---|---|---|
| 10× Genomics 3' v2/v3 | scRNA-seq library preparation | Captures 3' gene expression profiles with cell barcoding |
| MARS-seq | scRNA-seq library preparation | Provides highly specific transcriptome profiling |
| CIBERSORT algorithm | Computational cell quantification | Estimates immune cell fractions from bulk gene expression |
| SOMAScan assay | Proteomic profiling | Measures 6,340 proteins per sample in biofluids |
| CellMarker 2.0 | Cell type annotation | Database of cell-specific marker genes for annotation |
| Seurat v5 | scRNA-seq analysis | R toolkit for single-cell data preprocessing and analysis |
Experimental Design and Implementation Guidelines
Sample Processing and Quality Control
Implementing scHDeepInsight for tissue-specific immune response studies requires careful experimental design beginning with sample acquisition and processing. For postmortem studies, rapid tissue preservation is critical for maintaining RNA integrity, particularly when analyzing tissues with varying postmortem intervals. Research has demonstrated that significant transcriptomic changes occur as early as 48 hours postmortem, with 3,873 differentially expressed mRNAs identified in rat skeletal muscle tissue, including downregulation of mitochondrial activity genes and upregulation of vascular processes [34]. These findings underscore the importance of controlling for postmortem interval in experimental design and interpretation.
Quality control measures should include rigorous assessment of RNA integrity, though traditional metrics like RNA integrity number may require adaptation for postmortem samples. In degraded samples, qualitative assessment by agarose gel electrophoresis showing distinct 28S and 18S rRNA bands indicates high-quality RNA in controls, though this assessment becomes less reliable with significant degradation expected at extended postmortem intervals [34]. For scRNA-seq experiments, cell viability thresholds should be established based on tissue type and postmortem interval, with consideration for potential effects on immune cell populations of interest.
Computational Implementation and Benchmarking
Successful implementation of scHDeepInsight requires appropriate computational resources and benchmarking against established methods. The framework's training typically utilizes large-scale reference datasets, with the original implementation trained on over 460,000 cells from healthy donors across multiple tissues [42]. Researchers should ensure adequate GPU resources for efficient model training and inference, particularly when working with large datasets encompassing multiple samples or conditions.
Benchmarking should include comparison with both flat classification approaches and other hierarchical methods to establish performance improvements in specific experimental contexts. Evaluation metrics should encompass not only overall accuracy but also performance on rare cell populations and biologically meaningful subtypes. The interpretability features of scHDeepInsight, particularly SHAP-based analysis of gene contributions to classification decisions, provide valuable biological validation beyond traditional performance metrics [42].
Visualization and Data Interpretation
Workflow Diagram
scHDeepInsight Classification Workflow
Hierarchical Classification Architecture
Hierarchical Model Architecture
The scHDeepInsight framework represents a significant advancement in cell type annotation by integrating hierarchical biological knowledge with deep learning methodologies. Its application to tissue-specific immune responses in human postmortem studies offers unprecedented resolution for dissecting neuroimmune interactions in health and disease. As single-cell technologies continue to evolve, approaches like scHDeepInsight will play an increasingly vital role in extracting biologically meaningful insights from complex transcriptional data.
Future developments will likely focus on expanding hierarchical classifications to incorporate spatial transcriptomics data, integrating multi-omic measurements, and developing more sophisticated approaches for modeling cellular dynamics and interactions. The continued refinement of these AI-powered analytical frameworks promises to deepen our understanding of tissue-specific immune responses and accelerate therapeutic development for neurodegenerative diseases, cancer, and other immune-mediated conditions.
Spatial transcriptomics (ST) has emerged as a transformative technology that bridges high-throughput transcriptomic profiling with spatially contextualized tissue architecture, enabling researchers to investigate gene expression patterns while preserving crucial spatial location information [46]. This technology effectively combines traditional histological techniques with RNA sequencing to visualize and quantitatively analyze the transcriptome with spatial distribution in tissue sections [46]. For immunology research, particularly in the context of human postmortem studies, ST provides unprecedented insights into the spatial organization of immune cells within tissues, revealing how their positional relationships and microenvironments influence tissue-specific immune responses.
The fundamental advantage of ST lies in its ability to overcome the critical limitation of single-cell RNA sequencing (scRNA-seq), which requires tissue dissociation that inevitably destroys spatial context [46]. ST technologies preserve the spatial information of RNA in tissue sections by mapping transcripts to specific spatial locations before sequencing, thus maintaining the architectural integrity essential for understanding immune cell interactions, localization, and function within native tissue environments [46]. This capability is particularly valuable for investigating the spatial dynamics of immune responses in human tissues, where the precise positioning of immune cells relative to structural elements and other cell types often determines functional outcomes in health and disease.
Core Spatial Transcriptomics Technologies and Methodologies
Technological Platforms and Their Applications
Spatial transcriptomics technologies can be broadly categorized into two complementary approaches: imaging-based and sequencing-based platforms, each with distinct strengths for immunological research [47]. Imaging-based technologies utilize iterative hybridization of fluorescently labeled probes followed by sequential imaging to profile gene expression in situ at single-molecule resolution, while sequencing-based approaches employ spatially barcoded arrays to capture polyadenylated RNA for subsequent high-throughput sequencing [48].
Table 1: Comparison of High-Throughput Spatial Transcriptomics Platforms with Subcellular Resolution
| Platform | Technology Type | Resolution | Target Genes | Key Advantages for Immune Studies |
|---|---|---|---|---|
| Xenium 5K [48] | Imaging-based | Subcellular (<10 μm) | 5,001 genes | Superior sensitivity for marker genes; optimized for FFPE tissues |
| CosMx 6K [48] | Imaging-based | Subcellular | 6,175 genes | High-plex protein co-detection capability |
| Visium HD FFPE [48] | Sequencing-based | 2 μm | 18,085 genes | Whole transcriptome coverage; compatible with archival tissues |
| Stereo-seq v1.3 [48] | Sequencing-based | 0.5 μm | Whole transcriptome | Highest spatial resolution; minimal transcript diffusion |
For human postmortem studies, platform selection depends on specific research objectives. When comprehensive immune gene panels are required, targeted imaging approaches like Xenium and CosMx provide exceptional resolution, while discovery-based studies benefit from the whole transcriptome coverage of Stereo-seq and Visium HD [48]. Recent benchmarking studies demonstrate that Xenium consistently outperforms other platforms in detection sensitivity for multiple marker genes, a critical consideration for identifying rare immune cell populations [48].
Experimental Workflow for Human Postmortem Tissues
The standard workflow for spatial transcriptomics in human postmortem tissue analysis involves several critical steps that ensure data quality and biological relevance, particularly for investigating tissue-specific immune responses.
Diagram 1: Experimental workflow for spatial transcriptomics in human postmortem studies
Tissue Processing and Quality Control: For human postmortem tissues, optimal cutting temperature (OCT) compound-embedded fresh-frozen blocks or formalin-fixed paraffin-embedded (FFPE) blocks are prepared following standardized protocols [48]. The choice between preservation methods depends on experimental priorities: frozen tissues typically yield higher RNA quality, while FFPE preservation offers superior morphological preservation and compatibility with clinical archives [48]. Serial tissue sections of 5-10 μm thickness are generated using a cryostat (for frozen tissues) or microtome (for FFPE tissues) and mounted on specific capture areas depending on the platform used.
Spatial Library Preparation and Sequencing: For sequencing-based approaches like Visium HD, tissue sections are permeabilized to release RNA molecules that are then captured by spatially barcoded poly(dT) oligonucleotides [48]. After reverse transcription, cDNA libraries are constructed with incorporated spatial barcodes that preserve location information. For imaging-based platforms like Xenium, custom gene panels encompassing immune markers are hybridized with fluorescently labeled probes through multiple rounds of hybridization, imaging, and stripping [48]. The resulting data consists of spatial coordinates matched with gene expression counts, enabling reconstruction of spatial expression patterns during analysis.
Analytical Frameworks for Spatial Immune Profiling
Identifying Spatially Variable Genes and Domains
A fundamental step in spatial transcriptomics analysis is detecting spatially variable genes (SVGs), which are genes exhibiting non-random, informative spatial patterns [47]. For immune studies, SVGs often reveal localized immune activation, specialized immune microenvironments, and spatial gradients of immune cell infiltration. Computational methods for SVG detection can be categorized into three classes based on their biological interpretations:
Table 2: Categories of Spatially Variable Gene Detection Methods
| SVG Category | Biological Meaning | Example Methods | Applications in Immune Research |
|---|---|---|---|
| Overall SVGs [47] | Genes with spatial patterns independent of cell types | SpatialDE, SPARK, BOOST-GP | Identifying spatial immune gradients and tissue-wide polarization |
| Cell-Type-Specific SVGs [47] | Genes with spatial variation within a cell type | C-SIDE, cell2location | Revealing immune cell functional states across locations |
| Spatial-Domain-Marker SVGs [47] | Marker genes for predefined spatial domains | SpaGCN, BayesSpace | Annotating immune niches and territories |
In practice, a comprehensive analysis often employs multiple methods. For instance, researchers investigating the human dentate gyrus across lifespan used BayesSpace for unsupervised spatial clustering to identify distinct spatial domains, followed by differential expression analysis to identify domain-specific markers [49]. This approach revealed age-associated increases in neuroinflammation-related gene expression in glial-enriched regions, demonstrating the spatial compartmentalization of immune responses [49].
Integrating Multiple Datasets and Resolutions
The integration of multiple spatial transcriptomics datasets presents significant computational challenges due to batch effects, different spatial resolutions, and technical variations across platforms. Methods like Tacos (multiple spatial Transcriptomics data integration using community-enhanced graph contrastive learning) have been developed specifically to address these challenges [50]. Tacos employs a graph contrastive learning framework that constructs spatial graphs for each slice based on spatial coordinates, then uses communal attribute voting and edge dropping strategies to generate augmented graph views that enhance integration performance [50].
For immunology studies comparing control and diseased tissues, or tissues across different developmental stages, such integration methods enable the identification of conserved and context-specific spatial immune patterns. When applied to datasets from different platforms (e.g., integrating 10x Visium and Slide-seqV2 data), Tacos successfully aligns shared tissue structures while preserving platform-specific features, including rare immune cell niches that may be captured differently across technologies [50].
Applications in Human Postmortem Immunology Research
Mapping Neuroimmune Interactions Across the Lifespan
Spatial transcriptomics has proven particularly valuable for investigating the spatial dynamics of immune responses in human postmortem brain tissues. A recent study of the human dentate gyrus across four life stages (infant, teen, adult, and elderly) revealed striking spatial and temporal patterns in neuroimmune regulation [49]. Researchers performed transcriptome-wide spatial gene expression mapping and identified age-associated molecular signatures, discovering that genes associated with activated microglia and reactive astrocytes were downregulated in infant and teen groups but upregulated in adult and elderly groups [49].
This analysis revealed an inverse relationship between proliferative potential and glial inflammatory activity that changes with the onset of adulthood, with GO terms for immune processes showing pronounced spatial enrichment in specific hippocampal subdomains [49]. The study demonstrated increased BBB permeability and ischemic response signatures in the elderly group, particularly in glial- and neuropil-enriched regions, providing spatial context for age-associated neuroinflammation ("inflammaging") in human brain tissues [49].
Analyzing Large Tissues and Whole-Slide Architectures
Conventional ST platforms are constrained by limited capture areas (typically 6.5×6.5 mm for standard Visium), making comprehensive analysis of large tissue sections challenging [51]. Recent methodological advances address this limitation through computational approaches that predict spatial gene expression across extensive tissue areas. The iSCALE (inferring Spatially resolved Cellular Architectures in Large-sized tissue Environments) framework leverages the relationship between gene expression and histological features learned from small training ST captures to predict expression across entire large tissue sections [51].
Diagram 2: iSCALE workflow for large tissue analysis
When applied to a large gastric cancer sample, iSCALE accurately reconstructed tissue architecture at cellular resolution and identified key immune features such as tertiary lymphoid structures (TLS) [51]. These structures are crucial in antitumor immunity and prognostic assessment, demonstrating how large-scale spatial analysis can reveal clinically relevant immune patterns that would be missed with conventional small-capture approaches [51].
Inferring Cell-Cell Communication from Spatial Data
A particularly powerful application of spatial transcriptomics in immunology is the inference of spatially constrained cell-cell communication. Methods like SpaOTsc (Spatial Optimal Transport for single-cell) leverage spatial metrics to reconstruct signaling networks between immune and non-immune cells within tissues [52]. The approach relies on structured optimal transport to recover spatial properties of scRNA-seq data by utilizing spatial measurements of a relatively small number of genes [52].
The SpaOTsc framework first constructs a spatial metric for cells in scRNA-seq data by integrating it with spatial data using optimal transport, then uses this spatial metric to establish an optimal transport plan from a probability distribution of "sender cells" to "receiver cells" [52]. This approach mimics the physical processes of ligand release by signal senders and consumption by potential receivers, generating spatially constrained cell-cell communication networks that more accurately reflect biological reality compared to non-spatial inference methods [52].
For human postmortem studies, this capability enables researchers to reconstruct immune signaling networks within archival tissues, revealing how immune cells communicate with parenchymal cells and each other in specific tissue locations. By incorporating spatial constraints, these methods significantly reduce false-positive predictions common in non-spatial cell-cell communication inference approaches.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Platforms for Spatial Transcriptomics
| Reagent/Platform | Function | Application Notes for Immune Studies |
|---|---|---|
| 10x Visium HD [48] | Whole transcriptome spatial mapping | Ideal for discovery-phase immune studies; identifies novel immune markers |
| Xenium 5K Gene Panel [48] | Targeted subcellular spatial imaging | Customizable panels focusing on immune cell markers and cytokines |
| CODEX Multiplexed Protein Profiling [48] | Protein co-detection for validation | Confirms protein-level expression of identified immune markers |
| Palo Color Optimization [53] | Spatially-aware color palette assignment | Enhances visualization of neighboring immune cell clusters |
| Tacos Integration Tool [50] | Multiple dataset integration | Aligns immune patterns across multiple samples and conditions |
| SpaOTsc [52] | Cell-cell communication inference | Reconstructs spatially constrained immune signaling networks |
Spatial transcriptomics has fundamentally transformed our ability to investigate immune gene expression within its native architectural context, particularly in human postmortem tissues where spatial relationships are preserved. The integration of increasingly high-resolution spatial technologies with sophisticated computational methods has enabled unprecedented insights into the spatial organization of immune responses across different tissue types, developmental stages, and disease states.
As the field advances, key challenges remain in further improving resolution and sensitivity while reducing costs to enable larger-scale studies [51]. Computational methods for integrating multi-omics spatial data, including spatial proteomics and epigenomics, will provide more comprehensive views of immune cell states and functions within tissues [48]. For human postmortem studies specifically, standardized protocols for tissue preservation and processing will enhance data quality and comparability across different brain banks and tissue repositories.
The application of spatial transcriptomics to investigate tissue-specific immune responses in human postmortem tissues holds particular promise for understanding neurodevelopmental disorders, aging-related neuroinflammation, and the spatial dynamics of neuroimmune interactions in health and disease. By preserving the architectural context that shapes immune function, these approaches will continue to reveal fundamental principles of tissue immunity and identify novel therapeutic targets for immune-mediated conditions.
The integration of specialized analytical software is paramount for deciphering the complexity of the human immune system. This technical guide outlines a robust analytical workflow leveraging FlowJo for high-dimensional flow cytometry analysis and GraphPad Prism for statistical interrogation and data visualization, with a specific focus on tissue-specific immune responses in human postmortem studies. Framed within the context of broader thesis research on compartmentalized immunity, we provide detailed methodologies, structured data summaries, and visualization tools to standardize the analysis of tissue-resident immune cells, enabling researchers to generate reproducible, biologically significant discoveries in infectious disease and immunology research.
The immune system functions in a highly compartmentalized manner, with tissue-specific niches dictating unique cellular phenotypes and functions. Understanding diseases like tuberculosis (TB), which is initiated in the lung, requires a deep analysis of the immune landscape at the site of infection, rather than relying solely on peripheral blood measurements [54]. Postmortem studies provide an unparalleled opportunity to compare immune cells across multiple tissues—such as lung, lymph nodes, and spleen—from the same individual, offering a holistic view of immune responses that is impossible to obtain from living subjects [54] [18].
However, the analytical path from raw data generated in these complex studies to biological discovery is fraught with challenges. These include high-dimensional flow cytometry data management, the need for appropriate statistical models to compare multiple tissues and donor groups, and the correct interpretation of results within a tight biological context. This whitepaper establishes a standardized, end-to-end analytical pipeline using FlowJo and GraphPad Prism to overcome these hurdles, providing a framework for rigorous, data-driven immunology.
Experimental Workflow for Postmortem Tissue Immune Profiling
Tissue Collection and Cell Isolation
The foundation of any robust immunological study is the quality of the starting material. In postmortem studies, speed and sterile technique are critical.
- Ethics and Consent: The workflow begins with ethical approval and sensitive consent acquisition from next-of-kin by trained personnel [54] [18].
- Postmortem Interval: Studies have demonstrated that immune cells from tissues including lung, lymph nodes, and spleen remain viable and functional for up to 14 hours post-death, allowing for a practical window for sample collection [54].
- Multisite Tissue Collection: A full postmortem is performed to collect target tissues. A standard protocol includes:
- Lung tissue and bronchoalveolar lavage (BAL)
- Draining lymph nodes (e.g., Hilar Lymph Nodes)
- Systemic sites (e.g., spleen, peripheral lymph nodes, blood) [18]
- Cell Isolation from Solid Tissues:
- Lung Tissue: Mechanically dissected and subjected to enzymatic digestion using a mixture of Collagenase D (1 mg/ml) and DNase I (1 µg/ml), followed by mechanical dissociation using a gentleMACS Octo Dissociator with predefined "Lung" programs. The resulting cell suspension is filtered through 70 µm and 40 µm filters [54] [18].
- Lymph Nodes and Spleen: Cleaned of surrounding fat, mechanically dissociated, and filtered. Residual red blood cells are lysed using ACK lysis buffer [18].
- Cell Counting: Isolated cells are counted using an automated cell counter (e.g., BioRad TC20) before staining for flow cytometry [54].
High-Dimensional Flow Cytometry Staining
A 29-color flow cytometry panel is used to deeply phenotype T and B cells, enabling the identification of naive, memory, and tissue-resident subsets based on markers like CD45RA, CCR7, CD27, and CD69 [18]. Standard protocols for antibody titration, Fc receptor blocking, and viability dye staining should be followed to ensure data quality.
Core Analytical Workflow: FlowJo & GraphPad Prism Integration
The following diagram illustrates the integrated analytical pathway from raw data to statistical discovery.
Data Preprocessing and Population Identification in FlowJo
FlowJo serves as the central hub for initial data quality control and cell subset identification.
- Quality Control: Begin by examining scatter profiles (FSC-A vs. SSC-A) to identify the intact cell population. Use FSC-A vs. FSC-H to exclude doublets.
- Gating Strategy for Tissue T Cells: The following sequential gating strategy is employed to identify key T cell subsets in tissues like the lung:
- Singlets (FSC-H vs. FSC-A)
- Live cells (Viability dye negative)
- Lymphocytes (FSC-A vs. SSC-A)
- CD3+ T cells
- CD4+ or CD8+ subsets
- Memory Subsets: Naive (CCR7+ CD45RA+), Central Memory (CCR7+ CD45RA-), Effector Memory (CCR7- CD45RA-), and Terminally Differentiated Effector (CCR7- CD45RA+) [18].
- Key Population: Tissue-Resident Memory T (TRM) Cells: Identified as CD69+ CD4+ or CD8+ T cells within the live, singlet, lymphocyte, CD3+ gate. Their frequency is often calculated as a percentage of the parent CD4+ or CD8+ population.
- Data Export: For each sample, export the population statistics (e.g., frequency of TRM cells as a percentage of CD4+ T cells) and, if needed, the median fluorescence intensity (MFI) of specific markers (e.g., KLRG1) into a format compatible with GraphPad Prism, typically a .csv or .txt file.
Statistical Analysis and Visualization in GraphPad Prism
GraphPad Prism transforms the exported quantitative data into statistically rigorous, publication-ready figures.
- Data Table Selection: For comparing population frequencies across multiple tissues and donor groups, a Grouped table is the most appropriate format. This table type is designed for data organized by two grouping variables (e.g., Tissue and IGRA Status) and is analyzed using two-way ANOVA [55].
- Core Statistical Analyses:
- Two-way ANOVA: Used to determine the main effects of factors like "Tissue" and "Donor Group" (e.g., IGRA+ vs. IGRA-) and whether there is a significant interaction between them. For example, this test can reveal if the increase in CD4+ TRM cells in the lungs of IGRA+ individuals is statistically significant and specific to the lung tissue [18].
- Multiple Comparison Post-tests: Following a significant two-way ANOVA, post-tests (e.g., Tukey's or Sidak's) are applied to compare specific groups of interest, such as comparing Lung vs. Spleen within the IGRA+ group.
- t-tests: For simpler comparisons, such as analyzing the expression level of a single marker (e.g., KLRG1 MFI) between two groups in one tissue, an unpaired t-test is suitable.
- Data Visualization:
- Grouped Bar Graphs: Ideal for displaying the mean ± SEM of cell frequencies across different tissues and donor groups, with statistical significance denoted by asterisks and bars.
- Violin Plots: Available in Prism, these plots show the distribution of data points and are excellent for illustrating the spread and density of values in each group [55].
Table 1: Key Statistical Analyses in GraphPad Prism for Immunology Data
| Analysis Goal | Recommended Test in Prism | Example Use Case |
|---|---|---|
| Compare means across 2 groups | Unpaired or paired t-test | Compare KLRG1 expression on lung CD4 T cells between IGRA+ and IGRA- donors [18]. |
| Compare means across >2 groups | One-way ANOVA | Compare CD4+ TRM frequency across three or more tissues within one donor group. |
| Analyze effects of two factors | Two-way ANOVA | Determine the effect of Tissue (Lung, Spleen, LN) and IGRA Status (+/-) on TRM frequency [55]. |
| Model a binary outcome | Simple/Multiple Logistic Regression | Model the probability of disease status based on immune cell predictors [55]. |
| Survival analysis | Kaplan-Meier curves with log-rank test | Compare patient survival curves based on immune cell infiltration levels [56] [55]. |
Case Study: Analyzing TB-Specific Tissue Immunity
A study profiling T cell responses in Mycobacterium tuberculosis (M.tb)-uninfected individuals exemplifies this workflow. Researchers compared T and B cell phenotypes in postmortem tissues from IGRA-positive and IGRA-negative road traffic accident victims [18].
- Finding: Analysis in FlowJo and subsequent statistical comparison in GraphPad Prism revealed that IGRA+ individuals exhibited a significantly higher frequency of CD4+ tissue-resident memory T (TRM) cells in the lungs, but not in the spleen or lymph nodes. Furthermore, these CD4+ T cells in the lungs showed increased expression of KLRG1, a marker of terminal differentiation [18].
- Interpretation: This tissue-specific finding, enabled by the FlowJo/Prism pipeline, suggests that prior M.tb exposure drives localized immune adaptation and T cell differentiation specifically at the primary site of infection. This could not have been deduced from blood analysis alone.
Essential Research Reagent Solutions
The following reagents and tools are critical for the successful execution of the postmortem tissue immunology workflow.
Table 2: Essential Research Reagents and Tools for Postmortem Tissue Immunology
| Reagent / Tool | Function / Application |
|---|---|
| Collagenase D & DNase I | Enzymatic digestion cocktail for liberating immune cells from solid lung tissue matrix [54] [18]. |
| gentleMACS Octo Dissociator | Standardized mechanical dissociation of tissue samples, ensuring reproducibility and cell viability [54]. |
| Ficoll-Paque PLUS | Density gradient medium for the isolation of peripheral blood mononuclear cells (PBMCs) from heparinized blood [18]. |
| ACK Lysis Buffer | Lyses residual red blood cells in cell pellets obtained from tissues like spleen and lymph nodes [18]. |
| 29-color Flow Cytometry Panel | High-parameter phenotyping of T and B cell memory, activation, and tissue-residency subsets [18]. |
| FlowJo Software | Industry-standard platform for high-dimensional flow cytometry data analysis, visualization, and population gating. |
| GraphPad Prism Software | Integrated tool for statistical analysis, curve fitting, and creation of publication-quality graphs from quantitative data [55]. |
The synergistic use of FlowJo for deep cellular phenotyping and GraphPad Prism for rigorous statistical testing and visualization creates a powerful, accessible pipeline for uncovering tissue-specific immune biology. This structured workflow, when applied to precious samples from human postmortem studies, provides a standardized method to move from complex, high-dimensional data to biologically meaningful and statistically sound discoveries. By detailing these protocols and analytical frameworks, this guide empowers researchers to rigorously investigate the compartmentalized nature of the human immune system, accelerating progress in vaccine development and therapeutic interventions for diseases like tuberculosis.
Navigating Challenges: Best Practices in Postmortem Immunology Research
Ensuring Tissue Vidity and Cell Integrity Postmortem
The study of human tissue-specific immune responses is fundamental to advancing our understanding of neuroimmunology, oncology, and infectious diseases. Human postmortem tissues provide an invaluable resource for this research, allowing direct investigation of the human immune system within its native architectural context [2]. However, the utility of these tissues is entirely dependent on maintaining tissue viability and cell integrity after death. The postmortem interval (PMI)—the time between death and tissue preservation—is a critical variable that directly impacts cellular viability, RNA integrity, and protein functionality [57] [58]. This technical guide outlines evidence-based protocols and considerations for maximizing tissue quality for postmortem studies, with particular emphasis on applications in human immunology research.
Tissue Source Considerations and Viability Assessment
Tissue Source Comparison
The selection of appropriate tissue sources represents the first critical decision point in postmortem research design. The two primary sources—surgical resections and postmortem donations—offer distinct advantages and limitations that must be balanced against research objectives.
Table 1: Comparison of Human Tissue Sources for Research
| Tissue Source | Advantages | Limitations | Primary Research Applications |
|---|---|---|---|
| Surgical Resections(e.g., from epilepsy, tumor surgery) [57] | • Enhanced viability and functional activity• Superior preservation of native cellular architecture and microenvironment• Ideal for electrophysiological studies and long-term cultures | • Limited availability dependent on surgical schedules• Often from patients with specific pathologies (e.g., epilepsy, tumors)• May limit generalizability of findings | • Human organotypic brain slice cultures (HBSCs)• Functional electrophysiology• Tumor microenvironment studies• Long-term therapeutic screening |
| Postmortem Donations [57] [59] | • Greater accessibility and larger tissue quantities• Availability from individuals without neurological disease• Enables studies across different ages and conditions | • Variable viability dependent on postmortem interval (PMI)• Potential degradation of RNA, proteins, and cellular structure• Altered physiology due to lack of blood flow and oxygen | • Biobanking for genomic studies• Multimodal immune cell profiling [2]• Establishing patient-derived cell cultures [59]• Disease progression modeling |
Quantitative Viability Assessment
Systematic assessment of tissue and cell viability is essential for validating experimental suitability. Multiple complementary methods provide robust evaluation across different viability dimensions.
Table 2: Viability Assessment Methods and Standards
| Assessment Method | Measurement Principle | Key Indicators of Viability | Typical Acceptance Thresholds |
|---|---|---|---|
| Trypan Blue Exclusion [58] | Membrane integrity: viable cells exclude dye | Percentage of unstained (viable) cells | >60% viability for successful culture establishment [58] |
| Electrophysiological Recordings(patch-clamp, multielectrode arrays) [57] | Functional capacity: sustained neuronal firing and synaptic responses | Presence of action potentials, postsynaptic currents | Robust electrical activity for multiple weeks in vitro [57] |
| Biochemical Viability Assays(live/dead cell staining, LDH release) [57] | Metabolic and enzymatic activity | Proportion of living cells; minimal cell death | High culture fidelity with minimal cell death [57] |
| Mitotic Index Analysis [58] | Proliferative capacity in culture | Number of metaphases per cell | Varies by cell type; higher index indicates better proliferative health |
Experimental Workflows and Protocols
Core Postmortem Tissue Processing Workflow
The following diagram illustrates the critical pathway from tissue acquisition to established culture or analysis, highlighting key decision points and quality control checks.
Protocol for Establishing Postmortem Cell Cultures
Based on established methodologies for difficult-to-culture tissues including brain tumors and deer skin fibroblasts, the following protocol ensures maximal cell viability [59] [58].
A. Pre-Collection Preparation
- Ethical Compliance: Obtain all necessary institutional review board approvals and informed consent from donors or families prior to tissue collection [59].
- Collection Kit Preparation: Prepare sterile kits containing cold shipping media (Hibernate-A or McCoy's medium), high-concentration antibiotics/antimycotics (e.g., 500 mg/L gentamicin, 20 mg/L amphotericin B), and sterile collection tools [59] [58].
- Temperature Control: Ensure access to wet ice or cold packs for immediate temperature control after collection. Do not freeze samples [59].
B. Tissue Collection and Transport
- Sterile Technique: Maintain sterility during collection by changing gloves after handling non-sterile surfaces and using sterile instruments once the tissue source is exposed [59].
- Rapid Processing: Collect small tissue chunks (approximately 1-2 cm²) and immediately immerse in cold, antibiotic-supplemented media [59] [58].
- Continuous Cooling: Maintain samples on wet ice throughout transportation to the laboratory. Shipping should occur overnight on wet ice, not dry ice [59].
C. Laboratory Processing and Culture
- Mechanical Dissociation: Under sterile laminar flow, wash tissue with PBS and mince finely into ~1 mm³ pieces using sterile razor blades or scalpels, removing obvious blood vessels or meninges [59] [58].
- Enzymatic Dissociation: Incubate minced tissue in enzymatic digestion solution (e.g., collagenase I/II and dispase at 25 μg/mL, deoxyribonuclease I at 50 μg/mL in HBSS with calcium and magnesium) at 37°C for 30 minutes with periodic agitation [59] [58].
- Cell Separation: Centrifuge the digested suspension at 200× g for 5 minutes, discard supernatant, and resuspend the cell pellet in appropriate culture medium [58].
- Viability Assessment: Mix a 50 μL aliquot of cell suspension with 50 μL of 0.4% Trypan Blue. Count viable (unstained) and non-viable (blue-stained) cells using a Neubauer chamber [58].
- Culture Establishment: Plate viable cells at appropriate density in specialized media. For neural cultures, use tumor stem media (TSM) with growth factors (EGF, FGF, PDGF). For fibroblasts, use DMEM or McCoy's medium with serum [59] [58].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Postmortem Tissue Research
| Reagent / Material | Function / Purpose | Example Formulations / Notes |
|---|---|---|
| Hibernate-A Medium [59] | Specialized shipping and storage medium designed to maintain tissue viability during transport. | Often supplemented with high-dose antibiotics/antimycotics to prevent microbial contamination. |
| Antibiotic-Antimycotic Cocktails [58] | Control microbial growth in non-sterile postmortem samples. | High concentrations: 500 mg/L gentamicin + 20 mg/L amphotericin B [58]. |
| Enzymatic Dissociation Mix [59] | Break down extracellular matrix to release individual cells while preserving viability. | Collagenase I/II (25 μg/mL) + dispase (25 μg/mL) + DNase I (50 μg/mL) in HBSS with calcium/magnesium [59]. |
| Trypan Blue Stain [58] | Differentiate viable (unstained) from non-viable (blue) cells based on membrane integrity. | 0.4% solution, typically used at 1:1 dilution with cell suspension [58]. |
| Specialized Culture Media [59] | Support growth of specific cell types (e.g., neural cells, fibroblasts). | Tumor Stem Media (TSM): Neurobasal-A/DMEM-F12 base with B27, growth factors (EGF, FGF, PDGF-AA/BB), heparin [59]. |
| S1PR1-specific Radioligands [60] | Quantitative imaging and analysis of specific receptor expression in pathological studies. | [3H]CS1P1 or [11C]CS1P1 for autoradiography and PET imaging of S1PR1 in neuroinflammation [60]. |
Tissue-Specific Applications in Immune Research
Multimodal Immune Cell Profiling
The integration of postmortem tissues with advanced single-cell technologies has revolutionized our understanding of human immunology. A landmark study profiled over 1.25 million immune cells from blood, lymphoid, and mucosal tissues from 24 organ donors aged 20-75 years using CITE-seq (cellular indexing of transcriptomes and epitopes) to simultaneously analyze transcriptomes and 127 surface proteins [2]. This approach revealed that immune cell composition and function are predominantly shaped by tissue site rather than donor age, with distinct signatures identified for gut, lungs, and lymphoid organs [2]. This research underscores the critical importance of tissue context in human immune studies and provides a foundational atlas for understanding tissue-specific immunity.
Neuroimmunology and Multiple Sclerosis
Postmortem CNS tissues have been instrumental in validating novel therapeutic targets and imaging strategies. Quantitative autoradiography of S1PR1—a target for multiple sclerosis drugs like fingolimod—in postmortem MS tissues revealed statistically significant elevation of S1PR1 in MS lesions compared to non-lesion areas and healthy controls [60]. This finding was confirmed using the specific radioligand [3H]CS1P1, demonstrating the utility of postmortem tissues for validating targets and developing diagnostic imaging approaches [60].
Tumor Biology and Therapeutic Development
Postmortem tissues have enabled critical advances in modeling difficult-to-treat cancers. For diffuse intrinsic pontine glioma (DIPG), a lethal childhood brain tumor, rapid autopsy protocols have facilitated the establishment of patient-derived cell cultures and xenograft models that preserve the genetic and biological characteristics of the original tumors [59]. These models have been essential for identifying characteristic histone mutations (H3F3A, HIST1H3B) and screening potential therapeutic compounds, highlighting how postmortem tissues can accelerate research on otherwise inaccessible human diseases [59].
Ethical Considerations and Donor Consent in Postmortem Studies
Postmortem human tissues are an indispensable resource for advancing our understanding of human biology and disease pathogenesis, particularly in the realm of tissue-specific immune responses [31]. Research utilizing these tissues has proven crucial for elucidating the pathophysiology of neurological disorders, infectious diseases like COVID-19, and immune-mediated conditions such as multiple sclerosis [61] [60] [15]. However, this research domain is built upon a foundational ethical imperative: the necessity of informed donor consent and robust ethical oversight. The ethical framework governing postmortem studies not only protects donor autonomy and dignity but also ensures the scientific validity and social acceptability of the research. Within the specific context of investigating local immune responses, the ethical considerations become even more pronounced, as studies often require detailed analysis across multiple organs and employ advanced techniques like imaging mass cytometry and spatial transcriptomics [31] [15]. This guide provides a comprehensive overview of the ethical considerations, consent models, and practical protocols that researchers must navigate to conduct this vital work responsibly.
Core Ethical Principles and Legal Frameworks
The ethical conduct of postmortem research is guided by a set of core principles and variable legal frameworks that researchers must adhere to.
Fundamental Ethical Principles
- Autonomy and Respect for Persons: The cornerstone of ethical postmortem research is respecting the known wishes of the deceased individual. This principle underpins the requirement for informed consent, ensuring that donation is a voluntary act based on comprehension of the research's purpose, procedures, and potential uses of tissues [62] [63].
- Beneficence and Social Value: Research must be designed to maximize potential benefits to society, such as the development of new therapies for conditions like multiple sclerosis or COVID-19, while minimizing any potential harms or disrespect to the donor's body [60] [15].
- Justice: The benefits and burdens of research participation should be distributed fairly. This includes ensuring equitable access to the opportunity to donate and preventing the exploitation of vulnerable populations.
Consent Models in Practice
Globally, the approach to obtaining legal consent for donation varies, which directly impacts donor recruitment strategies and rates.
Table 1: International Organ and Tissue Donation Consent Models
| Country | Consent Model | Key Features | Impact on Donation Rates |
|---|---|---|---|
| Italy | "Opt-out" (Presumed Consent) | Citizens are considered donors unless they register opposition [63]. | Law not fully implemented, leading to disruption and ~8,000 patients on transplant waiting lists [63]. |
| Kazakhstan | "Opt-in" (Explicit Consent) | Individuals must actively register their consent, often via an e-government portal [62]. | Low registration rates; as of 2024, only 7,200 citizens had consented to donation [62]. |
| Australia | Varies by State/Territory | Complex interplay of laws for treatment, research, and ante-mortem interventions [64]. | Legal uncertainty can be a barrier to donation and related research interventions [64]. |
Special Ethical Challenges: Ante-Mortem Interventions
A significant ethical and legal challenge involves ante-mortem interventions (AMIs). These are procedures performed on a potential donor before death solely to improve organ or tissue viability for transplantation or research. Examples include non-therapeutic intubation, bronchoscopy, or blood tests for tissue matching [64]. The central ethical dilemma is that these interventions offer no therapeutic benefit to the donor and may carry risks or burdens. In many Australian jurisdictions, for instance, the legality of substitute decision-makers authorizing such non-therapeutic procedures is uncertain, creating a substantial barrier to donation [64]. Reforms in regions like Victoria and New South Wales, which now have dedicated laws for AMIs, provide a clearer, consent-based pathway for these critical interventions [64].
Implementing Ethical Practices: Protocols and Procedures
Translating ethical principles into actionable research protocols is critical. This involves standardized tissue handling, precise sampling, and the application of advanced analytical techniques.
Standardized Postmortem Tissue Procurement and Processing
Standardized protocols are essential to minimize technical variability and ensure that research data reflects biology rather than artifacts of processing. This is particularly crucial for small, complex structures like the brainstem.
A study on standardizing human brainstem processing highlights a protocol designed to account for inter-specimen structural heterogeneity [61]. Key steps include:
- Tissue Fixation: Brainstems are harvested and fixed in 4% paraformaldehyde for two weeks, followed by cryoprotection in sucrose solution [61].
- Systematic Sectioning: Tissues are sectioned transversely at 50μm thickness in a plane perpendicular to the floor of the 4th ventricle using a cryostat. Sections are collected in series with a 750μm interval between consecutive sections in a series [61].
- Staining and Imaging: Sections are stained with cresyl violet for anatomical visualization and digitized at high resolution using slide scanners (e.g., Hamamatsu NanoZoomer) for subsequent analysis [61].
This approach, based on internal anatomical landmarks, allows for reproducible sampling across different donors, which is a key ethical requirement for generating valid and comparable scientific data [61].
Advanced Techniques for Investigating Tissue-Specific Immunity
Cutting-edge technologies are enabling unprecedented insights into local immune responses within postmortem tissues.
- Imaging Mass Cytometry (IMC): This technique allows for the simultaneous detection of over 35 epitopes on paraffin-embedded tissue sections using antibodies tagged with metal isotopes and mass spectrometry detection. IMC was used to profile immune cells and cytokines in multiple organs (lungs, intestine, liver, kidneys, spleen) from COVID-19 patients, revealing organ-specific immune dysregulation [15]. The workflow involves antibody panel design, tissue section probing, laser ablation, and time-of-flight mass spectrometry detection, followed by high-dimensional bioinformatic analysis [15].
- Spatial Transcriptomics and Digital Pathology: As part of a tissue analysis framework for investigating local immunity to SARS-CoV-2, these techniques allow for the mapping of gene expression patterns within the tissue architecture, correlating immune responses with specific tissue niches [31].
- Quantitative Autoradiography: This methodology quantifies the distribution and density of specific receptors. In multiple sclerosis research, a S1PR1-specific radioligand, [3H]CS1P1, was used in saturation autoradiography studies to quantitatively demonstrate elevated S1PR1 expression in MS lesions compared to non-lesion areas, providing crucial pathophysiological insights [60].
Table 2: Key Research Reagent Solutions for Postmortem Immune Studies
| Research Reagent / Material | Function in Experimental Protocol | Specific Application Example |
|---|---|---|
| Metal-tagged Antibody Panel | Multiplexed detection of cell markers and cytokines via Imaging Mass Cytometry [15]. | Profiling immune cell infiltration (monocytes, macrophages, DCs, NKT cells) and cytokine production (IL-10, TNF-α) in COVID-19 affected organs [15]. |
| S1PR1-specific Radioligand ([³H]CS1P1) | Quantitative assessment of S1PR1 receptor expression and binding affinity via autoradiography [60]. | Measuring dysregulated S1PR1 expression in lesions of postmortem CNS tissues from Multiple Sclerosis cases [60]. |
| Cresyl Violet Stain | Histological counterstain for anatomical visualization and orientation of neural structures [61]. | Defining anatomical landmarks and rostrocaudal levels in postmortem human brainstem sections [61]. |
| PBS with Azide | Preservation solution for storing fixed postmortem tissues to prevent microbial growth [61]. | Long-term storage of brainstem specimens prior to sectioning and analysis [61]. |
Workflow for Ethical and Technical Integration
The diagram below outlines the integrated workflow from donor consent to data analysis, highlighting key ethical and technical steps.
Enhancing Donor Consent Through Education and Dialogue
The ethical procurement of postmortem tissues is inherently linked to public understanding and willingness to donate. Research demonstrates that educational interventions are highly effective in bridging the gap between general positive attitudes and active consent registration.
- Impact of Knowledge: Studies consistently show that knowledge is a critical predictor of willingness to donate organs after death [62]. A study in Kazakhstan found that a single 60-minute educational lecture significantly increased students' knowledge about organ donation and, crucially, the number of participants willing to donate rose from 27 to 56 [62]. Furthermore, greater knowledge gain was a significant predictor of a shift toward consent among initially ambivalent participants [62].
- Addressing Barriers: Key barriers to consent include informational deficits (e.g., uncertainty about how to express consent), mistrust in the healthcare system, and religious or cultural misconceptions [62] [63]. Targeted education that transparently addresses these concerns, including procedural aspects and legal safeguards, can reduce indecision [62].
- The Role of Dialogue: An Italian study found that facilitated open group dialogues (focus groups) involving diverse stakeholders (healthcare professionals, citizens, registry office employees) significantly strengthened positive attitudes toward donation [63]. This underscores that communication is not merely about transmitting information but also about building trust and addressing emotional and social concerns.
Table 3: Quantitative Impact of Educational Interventions on Donation Attitudes
| Intervention Study | Pre-Intervention Willingness to Donate | Post-Intervention Willingness to Donate | Key Predictive Factors for Positive Shift |
|---|---|---|---|
| Kazakhstan University Lecture [62] | 27 out of 97 participants | 56 out of 97 participants (p < 0.001) | Greater knowledge gain, female gender, lower perceived barriers. |
| Italian Focus Groups [63] | Mean attitude score: 6.45/7 | Mean attitude score: 6.56/7 (p < 0.001) | Higher education, familiarity with donation, being registered with donation-related associations. |
The integration of rigorous ethical standards with sophisticated methodological protocols is paramount for the future of postmortem studies on tissue-specific immunity. As research continues to reveal complex, organ-specific immune responses in diseases like COVID-19 and multiple sclerosis, the reliance on high-quality, ethically sourced human tissues will only grow [31] [60] [15]. The path forward requires a sustained commitment to:
- Transparent Public Engagement: Building trust through education and open dialogue is essential for fostering a culture of donation [62] [63].
- Clear and Adaptive Legal Frameworks: Laws must evolve to provide clarity on complex issues like ante-mortem interventions, facilitating research while protecting donor rights [64].
- Standardized and Reproducible Science: Ethical research obligates the use of robust, standardized protocols to ensure that the data generated from donated tissues is of the highest quality and utility [61].
By upholding these principles, the scientific community can honor the gift of donation, ensure the ethical integrity of its work, and accelerate the translation of postmortem tissue research into meaningful clinical advances.
Overcoming Autofluorescence and Background in Fixed Tissues
In the realm of human postmortem studies researching tissue-specific immune responses, autofluorescence presents a significant barrier to achieving clear and biologically accurate results. This inherent tissue fluorescence, caused by endogenous pigments such as lipofuscin and heme, is particularly problematic in fluorescence microscopy, where it manifests as background noise that can obscure specific signals from labeled biomarkers [65]. The challenge is especially pronounced in human tissue research, where autofluorescence is more intense relative to tissues from small animal models, and in studies of aging or diseased tissues where interfering pigments accumulate over time [66]. For researchers investigating immune cell populations and their spatial distribution in tissues like the myocardium, brain, or lymphoid organs, this background interference can compromise data quality, reduce signal-to-noise ratios (SNR), and limit imaging depth, ultimately hindering the reliable quantification of microvascular networks or immune cell subsets that are crucial for understanding disease mechanisms [65] [2]. Overcoming these technical hurdles is therefore essential for advancing our understanding of human immunology directly in relevant tissue contexts.
Autofluorescence in biological tissues originates from several endogenous molecules, each with distinct spectral properties and tissue distributions. Understanding these sources is critical for selecting appropriate countermeasures.
- Lipofuscin: This is a highly cross-linked aggregate of oxidized lipids, proteins, sugars, and metal ions that accumulates in lysosomes with age. It exhibits broad fluorescence emission across the visible spectrum, interfering with many common fluorophores. Lipofuscin is particularly problematic in neuronal tissues, including the central and peripheral nervous systems, where it can occupy up to 80% of visible neuronal cytoplasm in structures like dorsal root ganglia [66].
- Heme: Richly present in tissues with high vascularization like the myocardium, heme is another strong autofluorescent pigment that contributes significantly to background noise, especially in fluorescence imaging of microvasculature [65].
- Crosslinked Proteins: The process of paraformaldehyde (PFA) fixation, commonly used in tissue preservation, can itself generate fluorescent crosslinks that add to background noise [65].
The interference from these autofluorescent compounds is not uniform across all tissue types or experimental conditions. For instance, in myocardial tissues, both lipofuscin and heme contribute significantly to background, whereas in brain tissues from Alzheimer's disease patients, lipofuscin accumulation is particularly pronounced [65] [66]. The impact of these confounding factors is especially relevant in postmortem studies, where tissue quality metrics like pH and RNA integrity number (RIN) can significantly influence molecular analyses [27].
Table 1: Major Sources of Autofluorescence in Fixed Tissues
| Source | Chemical Nature | Spectral Characteristics | Tissue Localization |
|---|---|---|---|
| Lipofuscin | Cross-linked aggregate of oxidized lipids, proteins, sugars, and metal ions | Broad emission across visible spectrum | Lysosomes, accumulates with age; particularly high in neuronal tissues |
| Heme | Iron-containing porphyrin compound | Multiple fluorescence peaks | Highly vascularized tissues (myocardium, spleen, liver) |
| Fixation-induced Crosslinks | Protein crosslinks from aldehyde fixation | Varies with fixative and tissue type | Throughout fixed tissue matrix |
Technical Approaches to Reduce Autofluorescence
Chemical Quenching Methods
Chemical quenching employs specific reagents to reduce autofluorescence through chemical interactions with endogenous fluorophores. Several agents have been systematically evaluated for their efficacy in different tissue contexts.
- TrueBlack and Sudan Black B: These lipofuscin quenching dyes generally improve SNR at the tissue surface but may diminish overall imaging depth in thick tissue sections. In myocardial tissue studies, these agents showed trends of reduced imaging depth compared to controls without quencher incubation [65].
- TrueVIEW and Glycine: These quenching agents did not significantly impact SNR values in myocardial tissue and showed potential for improved SNR and imaging depth, making them worth consideration for certain applications [65].
- Trypan Blue: This agent also did not significantly affect SNR values in validation studies, suggesting it may be compatible with certain tissue types and imaging modalities [65].
The effectiveness of chemical quenchers can vary considerably depending on tissue type, fixation methods, and the specific autofluorescence sources present. For myocardial tissues, which contain high levels of both heme and lipofuscin, the optimization of quenching protocols must be carefully validated against potential tradeoffs between improved surface SNR and diminished imaging depth [65].
Photobleaching Techniques
Photobleaching represents an alternative physical approach to reducing autofluorescence that can be highly effective, particularly for lipofuscin-rich tissues.
- White-Light Photobleaching: A recent study describes a straightforward, scalable, pre-staining method using high-intensity white LED light to near-totally reduce lipofuscin autofluorescence. This technique improves signal detection across the color spectrum without negatively impacting multiplex fluorescence detection assays. It is effective for both peripheral and central nervous system structures, as well as pathological tissue such as Alzheimer's disease brain, which contains high levels of autofluorescent interference [66].
This photobleaching approach offers particular advantages for translational investigations in humans, as it provides a low-cost procedure that can be rapidly implemented into existing research programs to increase the accessibility of high-plex fluorescent microscopy methodologies [66].
Tissue Clearing Methods
Tissue clearing techniques improve light penetration and extend imaging depth by correcting refractive index mismatches in highly heterogeneous tissues. The CUBIC (Clear, Unobstructed Brain/Body Imaging Cocktails and Computational analysis) protocol has been successfully applied to myocardial tissues with optimized delipidation stages [65].
- CUBIC Protocol: This method involves delipidation and refractive index matching to render tissues transparent. For myocardial tissues, optimal image quality was obtained with 24-hour CUBIC Reagent I incubation times. The protocol has demonstrated success for imaging depths of up to 150 μm in myocardial tissues using confocal microscopy [65].
- Compatibility with Quenching: The integration of autofluorescence quenching with tissue clearing protocols requires careful optimization, as some quenching agents may interact with clearing reagents or affect the clearing efficiency itself.
Table 2: Comparison of Autofluorescence Reduction Techniques
| Technique | Mechanism of Action | Best Suited Applications | Advantages | Limitations |
|---|---|---|---|---|
| Chemical Quenching | Chemical reduction of fluorophores | Surface and thin-section imaging; myocardial tissues | Wide range of available reagents; easily incorporated into standard protocols | May reduce imaging depth; variable efficacy across tissue types |
| Photobleaching | Light-induced degradation of fluorophores | Lipofuscin-rich tissues (CNS, PNS, aged tissue) | High efficacy on lipofuscin; cost-effective; minimal impact on antigenicity | Requires specialized equipment; optimization needed for different tissues |
| Tissue Clearing | Refractive index matching and delipidation | Deep tissue imaging; 3D reconstruction | Enables volumetric imaging; improves light penetration | May require extended processing times; can affect some epitopes |
Experimental Protocols for Autofluorescence Reduction
White-Light Photobleaching Protocol for Lipofuscin Reduction
This protocol describes a method for reducing lipofuscin autofluorescence in human nervous system tissue, including pathological specimens like Alzheimer's disease brain tissue [66].
- Tissue Preparation: Cut frozen tissue sections at desired thickness (5-20 μm) and mount on slides. Air dry sections for 30 minutes.
- Photobleaching Setup: Place slides under a high-intensity white LED light source. The optimal distance between light source and slides should be determined empirically but is typically 10-15 cm.
- Exposure: Expose sections to continuous white light for 30-60 minutes. The duration may be optimized based on tissue type and autofluorescence intensity.
- Verification: Check autofluorescence reduction by imaging untreated and treated sections under the same acquisition settings.
- Staining: Proceed with standard multiplex fluorescence staining protocols after photobleaching treatment.
This simple yet powerful advance enables future anatomical investigations in human tissues with minimal infrastructure requirements [66].
Integrated Immersion-Based Labeling and Clearing Protocol for Myocardial Tissue
This protocol combines vascular labeling with tissue clearing for 3D visualization of myocardial microvasculature, with optimization of delipidation and quenching stages [65].
Tissue Collection and Fixation:
- Collect myocardial tissue samples (300-μm sections) from left ventricular free wall.
- Fix tissues in 4% paraformaldehyde for 24 hours at 4°C.
Vascular Labeling:
- Incubate tissues with tomato lectin (1:100 dilution in PBS) for 48 hours at 4°C with gentle agitation.
- Rinse tissues with PBS to remove unbound lectin.
Autofluorescence Quenching (Optional):
- Incubate tissues with selected quenching agent (TrueVIEW, Glycine, TrueBlack, Sudan Black B, or Trypan Blue) according to manufacturer's recommendations.
- Note: TrueBlack and Sudan Black B may reduce imaging depth.
Tissue Clearing with CUBIC Reagents:
- Incubate tissues in CUBIC Reagent I for 24 hours at 37°C with gentle agitation.
- Rinse tissues with PBS for 6 hours.
- Incubate tissues in CUBIC Reagent II for 24 hours at 37°C with gentle agitation.
Image Acquisition:
- Image cleared tissues using confocal microscopy.
- For myocardial tissues, imaging depths of up to 150 μm can be achieved with this protocol.
This immersion-based approach provides enhanced practicality when processing tissues from larger animal models or when only small tissue sections are available, as is often the case in human postmortem studies [65].
Research Reagent Solutions and Essential Materials
The following table details key reagents and materials used in the featured protocols for overcoming autofluorescence in fixed tissues.
Table 3: Essential Research Reagents for Autofluorescence Management
| Reagent/Material | Function/Purpose | Example Applications |
|---|---|---|
| TrueBlack | Lipofuscin quenching agent | Reduces lipofuscin autofluorescence in surface imaging of myocardial and brain tissues |
| Sudan Black B | Lipofuscin quenching agent | Chemical reduction of lipofuscin autofluorescence; may reduce imaging depth |
| TrueVIEW | Autofluorescence quenching agent | Compatible with myocardial tissue clearing; minimal impact on imaging depth |
| Glycine | Autofluorescence quenching agent | Potential for improved SNR and imaging depth in various tissues |
| Trypan Blue | Autofluorescence quenching agent | Compatible with various tissue types; minimal SNR impact |
| CUBIC Reagent I | Delipidation and initial clearing | Removes lipids and initiates refractive index matching in tissue clearing protocols |
| CUBIC Reagent II | Refractive index matching | Finalizes tissue clearing process for optimal light penetration |
| Tomato Lectin | Vascular labeling | Microvascular network visualization in immersion-based labeling approaches |
| High-Intensity White LED | Photobleaching light source | Non-chemical reduction of lipofuscin autofluorescence in human tissues |
Workflow Visualization and Experimental Design
The following diagram illustrates a comprehensive workflow for managing autofluorescence in fixed tissue studies, integrating multiple approaches described in this technical guide:
Diagram 1: Autofluorescence Management Workflow
The advancement of human postmortem studies researching tissue-specific immune responses critically depends on robust methods for overcoming autofluorescence and background interference in fixed tissues. The techniques outlined in this guide—including chemical quenching, photobleaching, and tissue clearing—provide researchers with a comprehensive toolkit for enhancing signal-to-noise ratios and enabling clearer visualization of biological structures. Particularly for immunological studies examining tissue-resident immune cells, microvascular networks, and cellular interactions in complex tissue environments, these methods facilitate the acquisition of high-quality data that accurately reflects the in vivo state. As multimodal profiling approaches continue to reveal the intricate details of human immune cell function across tissues and ages [2], the implementation of effective autofluorescence reduction strategies will remain essential for generating reliable, interpretable results that advance our understanding of human immunology in health and disease.
Standardizing Protocols Across Multiple Tissues and Donors
Research on human postmortem tissues is indispensable for deciphering the molecular architecture of diseases, particularly for investigating tissue-specific immune responses in conditions such as COVID-19 [67] and psychiatric disorders [27]. However, the validity and reproducibility of findings from such studies are heavily dependent on the standardization of protocols across diverse tissues and donors. The fundamental assumption that postmortem tissue accurately reflects living biology was recently challenged by the Landmark Living Brain Project, which demonstrated that nearly 80% of genes show significant expression differences between living and postmortem brain tissues [32] [68]. This revelation underscores the profound impact of pre-analytical and analytical variables on research outcomes. This technical guide provides a comprehensive framework for standardizing protocols across multiple tissues and donors, with a specific focus on investigating tissue-specific immune responses. By addressing key confounding factors and implementing rigorous standardization procedures, researchers can significantly enhance the reliability, reproducibility, and translational potential of their findings in human tissue studies.
Molecular Differences Between Living and Postmortem Tissues
Evidence from the Living Brain Project
Mount Sinai's Living Brain Project conducted a large-scale investigation comparing brain tissue from living people and postmortem donors, revealing substantial molecular differences [32] [68]. The study analyzed approximately 300 brain tissue samples from living patients obtained during deep brain stimulation surgery, applying transcriptomics and proteomics to systematically compare them to standard postmortem samples.
Table 1: Key Molecular Differences Between Living and Postmortem Brain Tissue
| Molecular Feature | Findings from Living Brain Project | Research Implications |
|---|---|---|
| Gene Expression | ~80% of genes significantly differentially expressed (17,186 genes) [68] | Challenges accuracy of postmortem gene expression signatures for living states |
| Protein Expression | >60% of proteins differentially expressed [32] | Protein-level biology is substantially altered postmortem |
| RNA Processing | 95% of RNA transcripts showed differences in splicing or maturity [32] | RNA splicing and processing mechanisms are disrupted |
| Pathway Relationships | Altered RNA-protein co-expression patterns [32] | Fundamental biological relationships are not preserved |
These findings do not negate the value of postmortem samples but emphasize that living samples offer complementary value for understanding real-time molecular processes [32]. The scale and consistency of differences across RNA and protein data highlight the necessity of accounting for the postmortem effect in study design and interpretation.
Implications for Immune Response Research
The molecular differences between living and postmortem tissues have particular significance for immune response research. A comprehensive multimodal profiling study of immune cells from blood, lymphoid, and mucosal tissues from organ donors revealed that tissue-specific effects dominate immune cell composition and function across lineages, with age-associated effects manifesting specifically in certain sites and cell types [2]. For instance, macrophages in mucosal sites and B cells in lymphoid organs showed distinct age-associated changes, highlighting the importance of tissue context in immune studies [2].
Critical Confounding Factors in Postmortem Tissue Research
Technical and Molecular Confounders
Systematic analysis of confounding factors in postmortem brain studies has identified several critical variables that significantly impact gene expression profiles, particularly in psychiatric disorder research [27].
Table 2: Impact of Confounding Factors on Gene Expression in Postmortem Brain Tissue
| Confounding Factor | Impact on Gene Expression | Recommended Control Measures |
|---|---|---|
| Tissue pH | 35,386 mRNA variants significantly correlated; affects cell cycle, energy production, and immune pathways [27] | Measure and match pH across comparison groups; include as covariate in statistical models |
| RNA Integrity Number (RIN) | 11,373 mRNA variants significantly correlated; affects RNA processing, energy production, and immune pathways [27] | Set minimum RIN threshold (e.g., ≥6); include as continuous covariate in analyses |
| Postmortem Interval (PMI) | 99 mRNA variants significantly correlated [27]; impacts RNA splicing and protein expression [32] | Record precise PMI; match across groups; include as covariate in statistical models |
| Tissue Storage Duration | 13,414 mRNA variants significantly correlated [27] | Document storage time; balance across comparison groups |
| Sex | 139 mRNA variants significantly correlated [27] | Match sex distribution; include as biological variable in experimental design |
| Age at Death | 87 mRNA variants significantly correlated [27] | Match age across groups; include as continuous covariate |
| Medication History | Affects gene expression patterns, particularly antipsychotics [27] | Document medication use; consider in patient selection and statistical models |
The study demonstrated that pH and RIN showed the strongest associations with gene expression changes, affecting crucial pathways including metabolic processes, immune function, and energy production [27]. These factors must be carefully controlled through study design and statistical analysis to ensure valid interpretation of results.
Tissue-Specific Considerations
Different tissues present unique challenges for standardization. Research on severe COVID-19 lungs revealed that spatial context profoundly influences immune-stromal interactions, with activated adventitial niches serving as crucial microenvironments that orchestrate prolonged lung immunopathology through chemokines CCL18 and CCL21 [67]. This highlights the importance of accounting for tissue microstructure in addition to molecular confounding factors.
Standardized Protocols for Tissue Collection and Processing
Pre-Analytical Variables and Quality Control
Implementing standardized protocols for tissue collection, processing, and quality assessment is essential for minimizing technical artifacts and ensuring reproducible results across multiple donors and tissues.
Quality Control Protocol for Postmortem Tissues:
- Tissue pH Measurement: Homogenize ~20mg frozen tissue in nuclease-free water (5× volume) and measure pH using a calibrated pH meter [27]
- RNA Integrity Assessment: Extract total RNA using standardized kits (e.g., AllPrep DNA/RNA/Protein Mini Kit), remove genomic DNA with RNase-free DNase I, and determine RIN using Bioanalyzer [27]
- Housekeeping Gene Validation: Verify consistent expression of reference genes (GAPDH, ACTB, HPRT1, RPL13A, B2M, SDHA, TBP, UBC, HMBS) across sample groups [27]
- Spatial Transcriptomics Quality Control: For spatial studies, combine histopathology with molecular analysis using consecutive slides to maintain spatial context [67]
Multimodal Profiling Approaches
Advanced multimodal approaches enable comprehensive characterization of immune responses while controlling for technical variability. A study profiling over 1.25 million immune cells from multiple tissues implemented an integrated workflow including:
- CITE-seq: Simultaneous profiling of transcriptomes and >125 surface proteins [2]
- Multimodal Cell Annotation: Using MultiModal Classifier Hierarchy (MMoCHi) to leverage both surface protein and gene expression for hierarchical cell classification [2]
- Data Integration: Applying multi-resolution variational inference (MrVI) to harmonize variation between cell states while accounting for differences between samples [2]
Standardizing Immune Cell Characterization and Assays
Signal Transduction Pathway Activity Profiling
Quantitative characterization of immune cell functional states can be achieved through Signal Transduction Pathway Activity Profiling (STAP-STP) technology, which enables simultaneous measurement of multiple signal transduction pathways based on mRNA analysis [6]. This approach generates an STP Activity Profile (SAP) consisting of nine pathway activity scores:
Core Signal Transduction Pathways for Immune Characterization:
- PI3K-FOXO Pathway: Inverse relationship between FOXO activity score and PI3K pathway activity
- MAPK Pathway: Regulates cell growth, differentiation, and survival
- JAK-STAT1/2 and JAK-STAT3 Pathways: Mediate cytokine and growth factor signaling
- NFκB Pathway: Central regulator of inflammation and immune responses
- TGFβ Pathway: Modulates immune cell differentiation and function
- Notch Pathway: Influences cell fate decisions in immune cells
- Estrogen Receptor (ER) and Androgen Receptor (AR) Pathways: Hormone-mediated immunoregulation
This technology has been applied to define characteristic SAPs for various immune cell types in resting and activated states, providing a quantitative framework for comparing immune functional states across tissues and donors [6].
Assay Calibration and Cross-Platform Standardization
When combining data from multiple assays or laboratories, statistical methods must be implemented to adjust for differences between assays with respect to measurement error and limits of detection [69]. Methods based on left-censored multivariate normal models assuming common assay differences across settings can integrate external paired-sample data to achieve two key objectives:
- Comparing immunogenicity between vaccine regimens when immune responses are measured by different assays
- Evaluating correlates of risk based on efficacy and biomarker data combined from multiple studies utilizing different assays
For COVID-19 research, calibration between different neutralization assays (e.g., Duke and Monogram Biosciences assays) has been particularly important, as they differ in pseudovirus preparation, cell lines, plate layouts, dilution schemes, and measurement error [69].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Standardized Tissue Immune Profiling
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| Anti-SARS-CoV-2 Nucleocapsid Protein Antibody | IHC detection of SARS-CoV-2 in FFPE tissues [70] | Affinity-purified rabbit IgG; 0.02 µg/mL working concentration |
| Anti-SARS-CoV-2 Spike S1 Glycoprotein Antibody | IHC detection of spike protein in FFPE tissues [70] | Affinity-purified rabbit IgG; 1.0 µg/mL working concentration |
| CITE-seq Antibody Panels | Simultaneous protein and transcriptome measurement at single-cell level [2] | 127+ surface protein targets with oligonucleotide barcodes |
| Multiplex Immunofluorescence Panels | High-parameter spatial phenotyping of immune cells in tissue [67] | 44-parameter MELC panel for immunofluorescence histology |
| Target Retrieval Solution (Low pH) | Antigen retrieval for IHC applications [70] | EnVision FLEX Target Retrieval Solution Low pH (50×) |
| RNA Preservation Solutions | Stabilize RNA during tissue processing and storage | RNAlater or similar commercial stabilization solutions |
| Quality Control Reference RNAs | Assess RNA integrity and sequencing library quality | RIN standards; external RNA controls consortium (ERCC) spikes |
Spatial Transcriptomics and Tissue Niche Analysis
Spatial transcriptomics has emerged as a powerful approach for understanding tissue-specific immune responses within their structural context. In severe COVID-19 lungs, ST analysis identified activated adventitial niches as crucial microenvironments contributing to prolonged immunopathology through up-regulation of CCL21 and CCL18, associated with endothelial-to-mesenchymal transition and tissue fibrosis [67]. The standardized workflow for spatial analysis includes:
This spatial approach enables researchers to identify distinct tissue microenvironments with unique transcriptional signatures and understand how immune-stromal interactions within these niches drive disease pathology [67].
Standardizing protocols across multiple tissues and donors requires a systematic approach that addresses both technical and biological variables. The integration of quality control measures, multimodal profiling technologies, appropriate statistical methods for data integration, and spatial analysis frameworks provides a comprehensive foundation for generating robust, reproducible data on tissue-specific immune responses. As research continues to reveal the complex interplay between tissue microenvironment, immune function, and disease pathology, implementing these standardized approaches will be crucial for advancing our understanding of human biology and developing effective therapeutic interventions. By carefully controlling for confounding factors and leveraging advanced technologies, researchers can overcome the challenges inherent in working with postmortem tissues and generate meaningful insights into the human immune system across diverse tissue contexts.
Road Traffic Accident (RTA) victims provide a critical source of control tissues for human postmortem studies investigating tissue-specific immune responses. Unlike tissues from diseased individuals, RTA-derived tissues typically originate from otherwise healthy individuals with no underlying chronic pathologies or pre-existing immune dysregulation, offering a unique window into baseline human immunology. This whitepaper details standardized methodologies for the collection, processing, and analysis of control tissues from RTA victims, framing these practices within the broader context of advancing human immunology research. We provide comprehensive experimental protocols, quantitative data on tissue viability, and essential resources to enable researchers to incorporate high-quality control tissues into their study designs, thereby strengthening conclusions about disease-specific immune perturbations in conditions like tuberculosis, Alzheimer's disease, and other disorders with significant immune components.
Human postmortem tissues provide an indispensable resource for validating findings from animal models and in vitro systems, yet accessing healthy control tissues presents a significant challenge in medical research. Tissues from Road Traffic Accident (RTA) victims represent a scientifically valuable source of control samples because they typically originate from individuals without protracted illnesses that might alter tissue architecture or immune cell composition. The use of these tissues enables direct comparison with diseased tissues, allowing researchers to distinguish pathological immune processes from normal physiological variation.
The immune system displays remarkable tissue-specific specialization, with unique immune cell populations and functional states in different organs. While blood is commonly used as a proxy for systemic immunity, it does not fully reflect the immune landscape at tissue sites where infections often establish and diseases manifest [54]. Postmortem studies using RTA-derived tissues allow for comprehensive mapping of immune cells across multiple organs—including lungs, lymph nodes, and spleen—from the same donor, providing a holistic view of human immune system organization under normal conditions [54]. This approach is particularly valuable for investigating difficult-to-treat diseases such as tuberculosis, where the initial site of infection is the lungs, but obtaining lung tissues from healthy living individuals is ethically and practically challenging [54].
Furthermore, traumatic injury from RTAs itself initiates a defined immune response characterized by pro-inflammatory and counter-inflammatory phases, providing insights into how the immune system responds to acute tissue damage [71] [72]. Understanding this response is crucial for properly interpreting data derived from RTA tissues and distinguishing trauma-related changes from baseline immune states.
Methodological Framework for RTA Tissue Studies
Ethical Considerations and Donor Recruitment
Ethical procurement of postmortem tissues from RTA victims requires rigorous protocols and sensitive engagement with next of kin. Studies must obtain approval from multiple relevant ethics bodies before commencement [54]. The consent process should be conducted by trained grief counselors who can sensitively approach next of kin during this difficult time [54]. Uganda law, for instance, requires consent from next of kin for postmortem procedures and tissue donation for medical research [54]. Research indicates good acceptability of next-of-kin consent for tissue donation when the process is handled with care and professionalism [54].
Documentation should include consent for:
- Full postmortem examination to establish cause of death
- Tissue donation for immediate medical research
- Future use of tissues for research purposes
- Access to previous medical records for clinical correlation
Donor selection criteria typically include:
- Adults above 18 years of age
- Absence of obvious underlying morbidity or chest involvement at time of death
- No evidence of chronic infectious diseases
- Clear cause of death related to trauma
Tissue Collection and Processing Timeline
Maintaining strict timelines during postmortem procedures is critical for preserving tissue integrity and cellular viability. The entire process from death to tissue processing should ideally be completed within 8-14 hours [54]. Research demonstrates that immune cells remain viable and functional for up to 14 hours after death when proper procedures are followed [54].
Table: Postmortem Tissue Processing Timeline
| Processing Stage | Time Window | Critical Parameters |
|---|---|---|
| Postmortem Interval | 0-8 hours | Shorter intervals preserve better cell viability |
| Tissue Collection | 1-2 hours | Systematic sampling of multiple tissue types |
| Transportation | 1-2 hours | Room temperature in preservation media |
| Tissue Processing | 2-4 hours | Enzymatic digestion and mechanical dissociation |
| Cell Isolation | 1-2 hours | Density centrifugation and washing |
| Cryopreservation | Immediate | Controlled rate freezing in DMSO solutions |
Multisite Tissue Collection Protocol
A comprehensive approach to tissue collection from RTA victims involves harvesting multiple tissue types to enable comparative analysis of immune responses across different anatomical sites.
Lung Tissue Processing:
- Cut lung tissue into small pieces using fine scissors and forceps in a sterile petri dish
- Place tissue in gentleMACS C tubes with enzyme mixture (collagenase D at 1mg/ml and DNase I at 1g/ml)
- Load tubes on gentleMACS Octo Dissociator and run using Lung Program 1
- Incubate tubes in CO2 incubator for 25 minutes
- Run gentleMACS using Lung Program 2
- Filter sample through 70µm followed by 40µm filters
- Centrifuge at 600 rcf for 5 minutes to obtain cell pellet
- Lyse residual red blood cells using ACK lysis buffer
- Wash cells in RPMI and count using automated cell counter [54]
Lymph Node Processing:
- Clean lymph nodes by teasing tissue from surrounding fat using forceps and scissors
- Cut into small pieces using fine scissors and forceps in a sterile petri dish
- Mix with RPMI media
- Filter resultant mixture through 70µm followed by 40µm filters
- Centrifuge at 600 rcf for 5 minutes to obtain cell pellet
- Lyse red blood cells using ACK lysis buffer
- Wash pellet with RPMI and count using automated cell counter [54]
Bronchoalveolar Lavage (BAL) Collection:
- Perform BAL washing of both left and right lungs with PBS
- Collect effluent for analysis of airway immune cells [54]
Blood Collection:
- Collect arterial blood from carotid artery into heparin tubes (arteries preferred due to venous collapse after death)
- Isolate PBMCs by diluting heparinized blood with RPMI media and layering manually on Ficoll-Paque PLUS media
- Harvest buffy coat after density centrifugation
- Lyse red blood cells in pellet, then wash and count cells [54]
All sample tubes should be tightly capped, placed in racks in sealable cool boxes, and transported to the appropriate laboratory at room temperature. Processing under appropriate biosafety conditions (e.g., BSL3 for potentially infectious tissues) is essential.
Quantitative Assessment of Tissue Quality
Donor Demographic Data
Comprehensive donor characterization enables researchers to account for potential confounding variables in their analyses. The following table represents collated demographic data from a typical study utilizing RTA victims as tissue donors [54].
Table: Donor Demographics in RTA Tissue Studies
| Parameter | RTA Donors (n=47) | Percentage |
|---|---|---|
| Gender | ||
| Male | 37 | 78.7% |
| Female | 10 | 21.3% |
| Age Range | ||
| 18-35 years | 26 | 55.3% |
| 36-55 years | 12 | 25.5% |
| ≥56 years | 9 | 19.1% |
| HIV Status | ||
| Positive | 6 | 12.8% |
| Negative | 41 | 87.2% |
| Cause of Death | ||
| Head trauma | 35 | 74.5% |
| Abdominal trauma | 8 | 17.0% |
| Gunshot | 1 | 2.1% |
| Other | 3 | 6.4% |
Tissue Quality Metrics
Multiple parameters influence postmortem tissue quality and must be carefully documented to ensure experimental validity [73].
Table: Critical Tissue Quality Parameters
| Parameter | Acceptable Range | Impact on Research |
|---|---|---|
| Postmortem Interval | <14 hours | Shorter intervals preserve cell viability and function [54] |
| Tissue pH | >6.0 | Higher pH indicates better preservation of molecular integrity [73] |
| RNA Integrity Number (RIN) | >7 for microarray, >5 for RT-PCR | Measures RNA quality; affects transcriptomic studies [73] |
| Cell Viability | >70% | Essential for functional immune assays [54] |
| Agonal State | Documented | Physiological stress before death affects molecular profiles [73] |
| Preterminal Medication | Documented | Drugs can alter immune cell function and gene expression [73] |
Table: Key Research Reagent Solutions for RTA Tissue Studies
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| Collagenase D (1mg/ml) | Tissue digestion | Enzymatic breakdown of extracellular matrix for cell isolation [54] |
| DNase I (1g/ml) | Prevents clumping | Degrades DNA released by damaged cells [54] |
| gentleMACS Octo Dissociator | Mechanical tissue dissociation | Standardized programmatic dissociation (Lung Program 1 & 2) [54] |
| Ficoll-Paque PLUS | Density gradient medium | PBMC isolation from blood [54] |
| RPMI medium | Tissue transport and cell culture | Maintains cell viability during processing [54] |
| ACK lysis buffer | Red blood cell lysis | Removes contaminating erythrocytes from tissue cell suspensions [54] |
| Fetal Bovine Serum (FBS) | Cryoprotectant and nutrient | 20% FBS in RPMI for tissue transport [54] |
| Iba1 antibody | Microglial marker | Detection of microglia in neural tissues [73] |
| Automated cell counter (TC20, Biorad) | Cell quantification | Standardized cell counting for reproducibility [54] |
Immune Responses to Traumatic Injury
Understanding the immunological consequences of traumatic injury is essential for proper interpretation of data derived from RTA tissues. Trauma induces a complex cascade of immune events that begins within minutes to hours after injury [71] [72].
The initial pro-inflammatory phase, known as Systemic Inflammatory Response Syndrome (SIRS), is driven primarily by innate immune cells including macrophages and neutrophils [71] [72]. This phase is characterized by:
- Activation of inflammasome pathways in injury-site draining lymph nodes within 2 hours, spreading systemically [71]
- Enhanced Toll-like receptor (TLR) reactivity observed as early as 1 day after injury, persisting for at least 7 days [71]
- Predominant involvement of macrophages in these enhanced responses [71]
- Release of damage-associated molecular pattern molecules (DAMPs) and alarmins from damaged tissues [72]
This pro-inflammatory phase is followed by a counter-inflammatory response (Compensatory Anti-inflammatory Response Syndrome or CARS) mediated primarily by T cells, particularly regulatory T cells (Tregs) [71]. Key features include:
- Reduced T cell pro-inflammatory phenotype and higher counter-inflammatory cytokine production by 7 days after injury [71]
- Augmented regulatory T cell activity that can control excessive inflammation [71]
- Suppressed Th1-type immune responses with promotion of Th2-type responses [71]
The diagram below illustrates the sequential immune responses following traumatic injury:
This sequential immune activation pattern has important implications for research utilizing RTA-derived tissues. The timing of tissue collection relative to the injury will significantly influence the immune cell profiles observed. Studies aiming to establish baseline immune parameters should account for these trauma-induced alterations when interpreting results.
Experimental Workflow for Tissue Processing and Analysis
The following diagram outlines a comprehensive workflow for processing and analyzing RTA-derived tissues, from donor identification to data generation:
Applications in Disease Research
RTA-derived control tissues have enabled significant advances across multiple disease domains:
Infectious Diseases: In tuberculosis research, RTA tissues have provided crucial insights into lung immune responses. Studies comparing TB-infected lung tissues with healthy RTA-derived lung tissues have revealed disease-specific alterations in immune cell populations and function [54]. The ability to examine multiple tissues from the same donor—including lung, lymph nodes, and spleen—has enabled comprehensive mapping of TB-specific immune responses across different anatomical compartments [54].
Neurodegenerative Disorders: In Alzheimer's disease research, control brain tissues from RTA victims have been instrumental in validating findings from animal models and distinguishing disease-specific neuroinflammatory changes from normal aging processes [73]. The analysis of microglial activation states and inflammatory mediator expression in control versus diseased tissues has refined our understanding of immune contributions to neurodegeneration [73].
Trauma Immunology: RTA tissues themselves provide valuable insights into the fundamental mechanisms of immune responses to tissue damage. Studies have revealed that traumatic injury activates inflammasome pathways in injury-site draining lymph nodes within 2 hours, with activation spreading systemically thereafter [71]. This priming of the innate immune system may represent an evolutionary adaptation to enhance antimicrobial defense following injury, though it can also contribute to the "two-hit" phenomenon in severely injured patients [72].
Tissues from Road Traffic Accident victims represent an invaluable resource for establishing baseline human immune parameters across multiple tissues. The standardized methodologies outlined in this whitepaper provide a framework for collecting, processing, and analyzing these tissues in a manner that preserves cellular viability and function. When properly integrated into research designs, RTA-derived control tissues strengthen conclusions about disease-specific immune perturbations and enable validation of findings from model systems.
The comprehensive approach to tissue collection—spanning multiple organs from the same donor—facilitates systems-level analyses of human immunology that are not possible using blood alone. As single-cell technologies continue to advance, these carefully procured tissue resources will undoubtedly yield further insights into human immune function in health and disease. Researchers are encouraged to incorporate these standardized protocols to enhance reproducibility and comparability across studies investigating tissue-specific immune responses in human postmortem research.
Human Data in Context: Validating Models and Driving Translation
Abstract The pursuit of understanding human immunology faces a fundamental challenge: the primary sources of biological data, namely postmortem human tissues and animal models, each present significant limitations that contribute to the "valley of death" in translating research to clinical applications [74]. Postmortem tissues undergo molecular alterations during the postmortem interval (PMI), while animal models, despite their utility, often fail to fully recapitulate the complexity of human immune responses [32] [75]. This whitepaper details the specific nature of these limitations, presents current data on the molecular disparities between living and postmortem states, and outlines advanced experimental protocols and reagent solutions designed to bridge this translational gap for researchers and drug development professionals.
1. Fundamental Challenges in Translational Immunology
The immune system's complexity, characterized by intricate cellular interactions, spatial-temporal dynamics, and significant inter-individual variability, makes it particularly susceptible to translational failures [74]. Research relies on two primary tissue sources, each with inherent constraints:
- Postmortem Human Tissues: These samples are the current standard for deep molecular studies of the human brain and other tissues. However, their collection involves an unavoidable PMI, a period during which significant molecular degradation and alteration occur [32] [20]. A foundational study from the Living Brain Project provides unequivocal evidence that brain tissue from living people has a distinct molecular character, with over 60% of proteins and 95% of RNA types being differentially expressed or processed in living versus postmortem tissue [32] [76]. These changes can obscure disease-specific signatures, as demonstrated in tauopathy mouse models where a 3-hour PMI diminished the detection of differential gene expression between diseased and wild-type animals [20].
- Animal Models: Mice have been instrumental in immunological breakthroughs but are imperfect surrogates. Approximately 90 million years of evolutionary divergence from humans have resulted in physiological and genetic differences that can limit predictive value [74] [75]. For instance, the transcriptional response to inflammatory perturbations in mice has been shown to poorly mimic that in humans [75]. Furthermore, standard laboratory husbandry, such as specific pathogen-free (SPF) conditions, creates an immunological naivete that does not reflect the diverse infectious history typical of most humans [75].
Table 1: Key Limitations of Traditional Research Models
| Model | Key Limitations | Impact on Research |
|---|---|---|
| Postmortem Human Tissues | - Significant alterations in RNA splicing and protein expression [32] [76]- Degradation of disease-specific transcriptional signatures [20]- Activation of stress and immune response pathways postmortem [20] | - Molecular snapshots may not reflect the living state- Risk of false negatives in disease research |
| Mouse Models | - Evolutionary divergence (∼65-75 million years) [75]- Poor correlation in transcriptional response to inflammation [75]- SPF husbandry does not reflect human immune history [75]- Species-specific pathogen interactions (e.g., herpes viruses, MTb) [75] | - Failed clinical translations (e.g., TGN1412) [77]- Models may study diseases intrinsic only to the model [75] |
2. Methodological Considerations and Experimental Protocols
2.1. Procuring and Validating Postmortem Tissues The fidelity of research using postmortem tissues hinges on rigorous standardization and understanding PMI effects. Key protocols include:
- Rapid Tissue Processing: Studies establishing the feasibility of postmortem tissue for immunology completed procedures and tissue processing within 8 hours of death while maintaining cell viability [74]. This rapid processing is critical for preserving RNA integrity and cellular function.
- snRNA-seq Workflow for PMI Assessment: To systematically evaluate PMI effects, a single-nucleus RNA sequencing (snRNA-seq) protocol can be employed [20]. Brains from wild-type and disease model mice are collected either immediately (0h PMI) or after a defined period (e.g., 3h PMI) with corpses kept at 4°C to mimic human brain bank conditions. Nuclei are isolated using a specialized extraction buffer supplemented with RNase inhibitor, followed by debris removal. Libraries are prepared using platforms like the 10X Genomics 3' Gene Expression Kit and sequenced. Bioinformatic analysis then reveals PMI-induced transcriptional changes in specific cell types.
2.2. Advanced Non-Animal Method (NAM) Technologies To circumvent the limitations of animal models, New Approach Methods (NAMs) are being rapidly developed.
- 3D Immune-Competent Tissue Models: These models aim to mimic the in vivo microenvironment. One protocol involves generating a full-thickness human skin model by integrating dendritic cell surrogates derived from THP-1 cells into a collagen-elastin matrix (e.g., MatriDerm) [74]. The functionality of immune cells is then tested by exposing the model to sensitizers and measuring the upregulation of maturation markers (e.g., CD86, HLA-DR) via flow cytometry. Cytokine secretion in the culture medium can be quantified using ELISA.
- Multi-Organ-on-Chip (Multi-OoC) Systems: These systems replicate systemic immunological processes by interconnecting tissue-specific compartments (e.g., lung, gut, lymph nodes) via microfluidic channels [74]. A key protocol involves a scalable microfluidic platform lined with human endothelial cells to model vascular inflammation. Real-time measurement of endothelial barrier function is achieved using transendothelial electrical resistance (TEER). The system can then be used to study immune cell migration and the effects of anti-inflammatory drugs by applying cytokines and perfusing immune cells through the channels.
Table 2: Quantitative Molecular Differences Between Living and Postmortem Brain Tissue
| Molecule Type | Finding | Technical Method | Biological Implication |
|---|---|---|---|
| Protein Expression | 61% of proteins differentially expressed [32] [76] | Liquid chromatography-mass spectrometry (LC-MS) | Altered protein networks critical for cell signaling and metabolism |
| RNA Transcripts | >95% of tested RNA transcripts showed differences in primary RNA levels, splicing, or mature RNA levels [32] | Bulk RNA Sequencing | Fundamental gene expression and regulation patterns are not preserved |
| RNA Splicing | >9,000 RNA transcripts had higher splicing rates in living brain; >5,000 higher in postmortem brain [76] | Analysis of primary vs. mature RNA transcripts | Postmortem tissue has disrupted RNA processing machinery |
3. Comparative Analysis and Integrative Approaches
3.1. Cross-Species Immune Profiling A systematic comparison of immune responses across species is crucial for validating models. One approach uses mass cytometry with extensive antibody cross-reactivity screening to create universal phenotyping and signaling panels for humans, non-human primates, and mice [77]. In a proof-of-principle study, whole blood from these species was treated with 15 immune stimuli, and signaling responses in 12 immune cell populations were measured. This method revealed conserved and divergent signaling pathways, such as species-specific Fcγ receptor (CD16) interactions and granulocyte responses to Bacillus anthracis antigen [77].
3.2. Leveraging Human Tissue Atlas Data Recent large-scale efforts have generated comprehensive atlases of human immune cells across blood, lymphoid, and mucosal tissues from organ donors aged 20-75 years [2]. This multimodal profiling (CITE-seq) of over 1.25 million cells defines tissue-specific immune signatures and age-associated effects. This resource provides a critical baseline from which to evaluate the physiological relevance of both animal models and in vitro NAMs.
4. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Resources for Cross-Species Translational Immunology
| Reagent / Resource | Function & Application | Key Considerations |
|---|---|---|
| Cross-Reactive Antibody Panels (Mass Cytometry) [77] | Simultaneous immunophenotyping and signaling analysis across humans, NHPs, and mice. | Must be validated for cell-type specific staining in each species (e.g., CD16 stains granulocytes in humans but not macaques). |
| MatriDerm or Similar Scaffolds [74] | 3D collagen-elastin matrix for constructing immunocompetent full-thickness skin and burn wound models. | Supports integration of peripheral blood-derived monocytes and T cells to study inflammatory processes. |
| Microfluidic OoC Platforms [74] | Devices with microchannels and chambers to co-culture multiple human tissue types and study systemic immune effects. | Enables real-time measurement of endothelial barrier function (TEER) and immune cell migration. |
| CITE-seq Antibody Panels [2] | Oligonucleotide-tagged antibodies to simultaneously profile transcriptome and >125 surface proteins at single-cell resolution. | Critical for identifying immune subsets in human tissues that are not resolved by transcriptomics alone (e.g., Tcm vs. Tnaive). |
| NIH Non-Human Primate Reagent Database [77] | Online resource (nhpreagents.org) reporting cross-reactivity of commercial antibodies with 13 NHP species. | A starting point, but requires experimental validation due to incomplete cell-type specificity data. |
5. Conclusion The translational gap in immunology is not an insurmountable chasm but a problem that can be addressed through a refined understanding of model system limitations and the adoption of advanced, human biology-focused tools. A multi-pronged strategy is essential: rigorously controlling for and quantifying PMI effects in human tissues, using cross-species profiling to define the boundaries of animal model relevance, and aggressively integrating sophisticated NAMs that more accurately mimic human tissue immunity. By leveraging the protocols and resources detailed in this whitepaper, researchers can de-risk drug development and build a more predictive and clinically relevant understanding of the human immune system.
This case study is situated within a broader thesis investigating tissue-specific immune responses in human post-mortem studies. The central premise of this research is that local immune responses within organs are pivotal to understanding the full spectrum of human immunity, a concept supported by analytical frameworks developed for studying pathogens like SARS-CoV-2 [78]. While peripheral blood provides a accessible window into systemic immunity, it may not accurately reflect the complex immune dynamics within tissues, particularly at the primary sites of infection or exposure.
This study focuses on tissue-resident memory T cells (TRM) in the lungs following exposure to Mycobacterium tuberculosis (M.tb). Interferon-gamma release assays (IGRAs), such as the T-SPOT.TB, are standard clinical tools used to detect immune memory to M.tb by measuring T-cell release of IFN-γ in response to M.tb-specific antigens in blood samples [18]. However, the relationship between a positive IGRA test result and the localized, tissue-based immune response in the lung remains poorly characterized. By utilizing a unique post-mortem tissue collection framework, this research aims to bridge this critical knowledge gap and validate lung TRM profiles as a more nuanced indicator of localized immune memory.
Experimental Design and Methodology
Study Cohort and Ethical Considerations
The investigation employed a carefully designed post-mortem tissue collection protocol [18].
- Participants: The study recruited 52 deceased, apparently healthy, HIV-negative road traffic accident victims from the Surgical Emergency Unit of Mulago National Referral Hospital, Kampala, Uganda. The cohort was divided into two groups: IGRA-positive (TSPOT+) and IGRA-negative (TSPOT-) individuals, based on the T-SPOT.TB assay.
- Ethical Approval: The study obtained ethical approval from five independent ethics bodies, including the Makerere University School of Biomedical Sciences Research and Ethics Committee and the Uganda National Council of Science and Technology [18].
- Informed Consent: Trained grief counselors sensitively obtained informed consent from the next-of-kin for a full post-mortem and tissue donation for research.
Post-Mortem Tissue Collection and Processing
A full post-mortem was conducted on all subjects to establish the cause of death and identify any underlying conditions. Tissues were collected and processed under Biosafety Level 3 (BSL3) conditions [18].
The table below summarizes the tissues collected and the methods used for cell isolation.
Table 1: Summary of Collected Tissues and Cell Isolation Methods
| Tissue Type | Examples | Cell Isolation Method |
|---|---|---|
| Lung | Lung parenchyma | Enzymatic digestion with collagenase D and DNase I, followed by physical disintegration using a gentleMACS Octo Dissociator. |
| Lymphoid Tissues | Hilar Lymph Nodes (HLNs), Spleen, Peripheral Lymph Nodes (PLNs) | Physical teasing of tissue from surrounding fat. |
| Bronchoalveolar Lavage (BAL) | Washes from left and right lungs | Performed with PBS. |
| Blood | Arterial blood from the carotid artery | Density gradient centrifugation to isolate Peripheral Blood Mononuclear Cells (PBMCs). |
Immune Phenotyping by Flow Cytometry
Immune cell characterization was performed using high-parameter flow cytometry [18].
- Staining Panel: A comprehensive 29-color flow cytometry panel was used to deeply phenotype T and B cell populations.
- Key Markers: The panel included markers for:
- General T cell identification: CD3, CD4, CD8
- Memory T cell subsets: defined by CCR7 and CD45RA expression
- Tissue-resident memory (TRM) markers
- Differentiation marker: KLRG1 (a marker of terminal differentiation)
- Data Analysis: Acquired data were analyzed using FlowJo software. Statistical analysis and graphing were performed using GraphPad Prism.
Key Quantitative Findings
The flow cytometry analysis revealed distinct immune signatures, particularly within the lung compartment.
The study first established that the overall frequencies of major immune cell populations were similar between TSPOT+ and TSPOT- individuals across all tissues [18].
Table 2: Summary of Similar Immune Cell Frequencies Between TSPOT+ and TSPOT- Individuals
| Immune Cell Population | Observation |
|---|---|
| CD3+, CD4+, CD8+ T cells | Similar overall frequencies. |
| CD19+ B cells | Similar overall frequencies. |
| Memory T cell subsets (defined by CCR7/CD45RA) | Similar overall frequencies. |
| Memory B cell subsets (defined by IgD/CD27) | Similar overall frequencies. |
Tissue-Specific CD4+ TRM and Differentiation Profiles
The critical findings emerged from the detailed analysis of tissue-resident populations and their differentiation states [18].
Table 3: Significant Immune Phenotype Differences in Lung Tissue
| Immune Parameter | Tissue | Finding in TSPOT+ Individuals | Biological Implication |
|---|---|---|---|
| CD4+ TRM Frequency | Lung | Significantly Higher | Enhanced localized memory at the primary site of M.tb exposure. |
| KLRG1 Expression | Lung (on mature CD4+CD27- T cells) | Significantly Increased | Indicator of terminal T cell differentiation. |
| CD4+ TRM / KLRG1 Phenotype | Lymph Nodes, Spleen | Not Observed | Effect was specific to the lung compartment. |
These results indicate that IGRA positivity is associated with a highly differentiated CD4+ TRM population specifically within the lungs, the primary site of M.tb infection.
The Scientist's Toolkit: Research Reagent Solutions
The following table details the key reagents and materials central to this research, which can serve as a guide for replicating or designing similar studies.
Table 4: Essential Research Reagents and Materials
| Reagent / Material | Function / Application | Specific Example / Note |
|---|---|---|
| T-SPOT.TB Assay | In vitro ELISPOT test to determine IGRA status by detecting M.tb-specific T cells via IFN-γ release. | Used to classify participants as TSPOT+ or TSPOT- [18]. |
| Flow Cytometry Panel | High-parameter phenotyping of T and B cell populations, memory subsets, and differentiation states. | A 29-color panel was used for deep immune profiling [18]. |
| Cell Isolation Enzymes | Enzymatic digestion of solid tissues (e.g., lung) to obtain single-cell suspensions for analysis. | Collagenase D (1 mg/ml) and DNase I (1 µg/ml) mixture [18]. |
| GentleMACS Octo Dissociator | Automated instrument for the standardized physical disintegration of tissue samples. | Used with specific programs (e.g., Lung Program 1 & 2) for consistent processing [18]. |
| Ficoll-Paque PLUS | Density gradient medium for the isolation of Peripheral Blood Mononuclear Cells (PBMCs) from whole blood. | Standard manual density centrifugation method [18]. |
| Analysis Software | Data analysis is crucial for transforming raw data into meaningful biological insights. | FlowJo for flow cytometry data; GraphPad Prism for statistical analysis and graphing [18]. |
Discussion and Interpretation
The findings of this case study validate the hypothesis that IGRA positivity is linked to a distinct tissue-level immune signature. The increased frequency of CD4+ TRM cells and their terminal differentiation (KLRG1+) specifically within the lungs of TSPOT+ individuals provides strong evidence that a positive blood-based IGRA reflects prior immune engagement that has left a localized mark at the primary portal of infection [18].
This aligns with the broader thesis that tissue-specific analyses are indispensable for a complete understanding of immune responses. The results suggest that the lungs of IGRA-positive individuals maintain a population of battle-ready, antigen-experienced T cells, poised for a rapid response upon re-encounter with M.tb. This localized, tissue-resident memory is not captured by simply quantifying circulating T cell frequencies.
The implications of these findings are significant for public health and clinical practice, particularly in TB-endemic settings. They raise important questions about the long-term consequences of harboring a highly differentiated T cell population in the lungs and how this might influence an individual's susceptibility to future TB infection or progression to active disease. Future research should focus on correlating these specific TRM profiles with clinical outcomes to assess their predictive value. Furthermore, these validated markers and methodologies could be instrumental in evaluating new TB vaccines and therapies aimed at inducing or modulating protective tissue-resident memory.
The immune system represents a dynamic network of specialized cells distributed across the body, orchestrating defense mechanisms against pathogens, regulating inflammation, and maintaining tissue homeostasis. While circulating immune cells have been extensively characterized, particularly in human peripheral blood, understanding immunity at the tissue level has remained challenging due to limited access to human tissue samples. Cross-species immunology has emerged as a critical discipline for bridging this knowledge gap, leveraging comparative analyses to dissect conserved biological principles and species-specific adaptations. This whitepaper examines the current state of cross-species immunology research, focusing on tissue-specific immune responses revealed through human postmortem studies and comparative animal models, with implications for therapeutic development and disease modeling.
Recent technological advances in single-cell profiling have enabled unprecedented resolution in mapping immune cell heterogeneity across tissues and species. These approaches have revealed that tissue microenvironment exerts a dominant influence on immune cell composition and function, potentially surpassing the effects of age or other variables in shaping localized immunity [2]. Furthermore, cross-species analyses have identified both conserved inflammatory responses and divergent regenerative capacities that underlie differential disease outcomes between species [79]. This growing knowledge base provides a foundation for refining animal models to better recapitulate human immunity and for developing more predictive in vitro systems.
Quantitative Analysis of Tissue-Specific Immune Distributions
Human Tissue Immunity Revealed by Postmortem Studies
Large-scale profiling of immune cells from organ donors has generated comprehensive maps of human tissue immunity, revealing specialized immune niches across the body. These studies leverage multimodal single-cell profiling to simultaneously capture transcriptomic and proteomic information from viable immune cells isolated from multiple tissues from individual donors [2]. The resulting datasets enable systematic comparison of immune cell composition, functional states, and tissue-specific adaptations across anatomical sites.
Table 1: Human Immune Cell Distribution Across Tissues Based on Organ Donor Studies
| Cell Type | Subset | Blood | Lymph Nodes | Bone Marrow | Lung | Jejunum |
|---|---|---|---|---|---|---|
| T Cells | CD4+ Naive | Enriched | Present | Low | Low | Low |
| CD8+ Naive | Enriched | Present | Low | Low | Low | |
| CD4+ Treg | Low | Enriched | Low | Low | Low | |
| CD8+ TEMRA | Low | Low | Enriched | Moderate | Low | |
| CD4+/CD8+ TRM | Low | Low | Low | Present | Enriched | |
| B Cells | Naive B cells | Low | Enriched | Low | Low | Low |
| Memory B cells | Low | Enriched | Low | Low | Low | |
| Plasma cells | Low | Present | Enriched | Low | IgA+ enriched | |
| Innate Lymphoid | CD56dim NK | Enriched | Low | Enriched | Enriched | Low |
| ILC1 | Low | Low | Low | Low | Enriched | |
| ILC3 | Low | Present | Low | Low | Present | |
| Myeloid | Alveolar Macrophages | Low | Low | Low | Enriched | Low |
| Classical Monocytes | Enriched | Low | Enriched | Present | Low | |
| Dendritic Cells | Low | Enriched | Low | Present | Present |
Analysis of over 1.25 million immune cells from blood, lymphoid, and mucosal tissues from donors aged 20-75 years demonstrated that immune cell composition exhibits remarkable tissue specificity [2]. T cell subsets showed distinct distribution patterns, with naive T cells enriched in blood and lymph nodes, regulatory T cells (Tregs) particularly abundant in lymph nodes, and tissue-resident memory T (TRM) cells predominating in mucosal sites such as the jejunum [2]. Similarly, B cell subsets were largely confined to lymphoid organs, with plasma cells exhibiting tissue-specific adaptation evidenced by IgA+ plasma cell enrichment in the jejunal lamina propria [2].
Myeloid cells demonstrated perhaps the most profound tissue specialization, with site-specific macrophage populations such as alveolar macrophages in the lung exhibiting distinct transcriptional profiles and functional capacities [80]. These tissue-imprinted identities appear to be largely maintained throughout the lifespan, though age-associated functional changes occur in specific subsets and locations [2].
Conserved and Divergent Immune Responses Across Species
Comparative analyses of immune responses to injury reveal both deeply conserved pathways and species-specific adaptations that inform our understanding of human disease mechanisms. A cross-species single-cell RNA-seq study directly compared inflammatory responses to heart injury in zebrafish (which possess remarkable cardiac regenerative capacity) and mice (which develop fibrotic scarring similar to humans) [79].
Table 2: Cross-Species Comparison of Cardiac Injury Responses
| Parameter | Zebrafish (Regenerative) | Mouse (Fibrotic) | Human Relevance |
|---|---|---|---|
| Macrophage Response | Transient fibrosis; Scar resolution | Persistent inflammation; Fibrotic scarring | Human responses mirror murine pattern |
| Systemic Inflammation | Limited and resolved | Chronic multi-organ engagement | Post-MI inflammation in humans parallels mice |
| Cardiomyocyte Fate | Proliferation and regeneration | Hypertrophy; Minimal proliferation | Adult humans show minimal regeneration |
| Immune Cell Kinetics | Rapid neutrophil clearance; Macrophage transition | Sustained granulocyte recruitment; Inflammatory macrophages | Human MI shows sustained inflammation |
| Extracardiac Effects | Limited peripheral tissue involvement | Liver and kidney inflammation; Immune activation | Human MI associates with multi-organ dysfunction |
This comparative analysis revealed that while both species recruit similar classes of immune cells to the injured heart, the temporal dynamics and functional programs of these cells differ dramatically [79]. In regenerative zebrafish, macrophage populations transition swiftly from a pro-inflammatory to a pro-reparative state, facilitating scar resolution and cardiomyocyte proliferation. In contrast, mice exhibit sustained engagement of inflammatory macrophages that promote fibrotic deposition rather than tissue regeneration [79]. These divergent responses highlight the importance of immune cell plasticity in determining tissue repair outcomes and suggest that modulating human immune responses toward a more "zebrafish-like" state could potentially improve recovery after myocardial infarction.
Beyond the heart, cross-species comparisons have illuminated conserved principles in tissue-specific immunity. Both humans and model organisms demonstrate that tissue residence imprints unique functional signatures on immune cells, with specialized macrophage populations adapted to the specific requirements of their tissue niche [80]. These conserved features validate the use of model systems for understanding fundamental aspects of human tissue immunity while highlighting the need for caution when extrapolating specific mechanistic insights.
Experimental Approaches and Methodologies
Human Postmortem Tissue Processing and Immune Cell Isolation
The study of human tissue immunity relies critically on optimized protocols for processing postmortem tissues and isolating viable immune cells for downstream analysis. The following workflow represents established methodology from recent multi-tissue studies:
Tissue Acquisition and Processing:
- Tissues are obtained from deceased organ donors within approved postmortem intervals (typically 2-8 hours after circulatory death) [2] [80].
- Tissues are transported in cold preservation solution (e.g., University of Wisconsin solution or RPMI with antibiotics) to maintain cellular viability.
- Tissues are mechanically dissociated using gentleMACS Dissociator or similar systems with optimized enzyme cocktails (e.g., Liberase TM plus DNase I) [80].
- Single-cell suspensions are filtered through 70μm strainers and washed in cold PBS with 2% fetal bovine serum.
Immune Cell Enrichment:
- Mononuclear cells are isolated by density gradient centrifugation using Ficoll-Paque or Lymphoprep [2].
- For some applications, specific immune populations are enriched using magnetic-activated cell sorting (MACS) with antibody panels targeting lineage-specific surface markers [80].
- Cell viability is assessed using trypan blue exclusion or automated cell counters, with typical viability thresholds >80% for sequencing applications.
Cryopreservation:
- Cells are resuspended in freezing medium (90% FBS with 10% DMSO) at controlled concentrations.
- Controlled-rate freezing is employed before transfer to liquid nitrogen for long-term storage.
- Post-thaw viability is assessed after rapid thawing and DNase treatment to prevent clumping.
Multimodal Single-Cell Profiling
State-of-the-art immune profiling combines transcriptomic and proteomic measurements from the same single cells, providing complementary information for comprehensive cell annotation:
Cellular Indexing of Transcriptomes and Epitopes by Sequencing (CITE-seq):
- Cells are stained with oligonucleotide-conjugated antibodies (TotalSeq reagents) targeting up to 200 surface proteins [2].
- After staining and washing, cells are loaded on single-cell platforms (10X Genomics Chromium) for partitioning and barcoding.
- Libraries are prepared for both transcriptome and surface protein detection following manufacturer protocols.
- Sequencing is performed on Illumina platforms with recommended read depths of ≥20,000 reads per cell for gene expression and ≥5,000 reads per cell for antibody-derived tags (ADTs).
Data Processing and Integration:
- Raw sequencing data are processed using Cell Ranger or similar pipelines to generate feature-barcode matrices.
- Data integration across donors and tissues employs specialized algorithms such as multi-resolution variational inference (MrVI) to harmonize biological variation while preserving tissue-specific signals [2].
- Cell type annotation leverages multimodal classifiers (e.g., MMoCHi) that simultaneously utilize RNA and protein expression for hierarchical classification [2].
Cross-Species Integration Methods
Comparing immune responses across species presents computational challenges due to genetic and compositional differences:
Orthologous Gene Mapping:
- One-to-one orthologs are identified using Ensembl Compara or similar databases.
- Genes without clear orthology relationships are excluded from cross-species comparisons.
Anchor-Based Integration:
- The Seurat integration workflow or similar approaches are used to identify "anchors" between species datasets.
- Canonical correlation analysis identifies shared correlation structures across species.
- Mutual nearest neighbors (MNNs) correct for species-specific batch effects while preserving biological signals.
Cell Type Alignment:
- Cell types are initially annotated independently within each species using reference datasets.
- Cross-species correspondence is established through marker gene conservation and functional similarity.
- Cluster-based alignment validates consistent cell type definitions across species.
Advanced Model Systems for Human Immunology
Humanized Mouse Models
Humanized MHC (hMHC) murine models have emerged as valuable platforms for studying human-specific immune responses:
Model Generation:
- Endogenous murine β2-microglobulin and H2-Ab1 loci are modified via embryonic stem cell targeting [81].
- Human HLA-A*02:01 and HLA-DR1 genes are transgenically introduced [81].
- Successful humanization is verified by Western blot for HLA expression and peptide binding assays [81].
Applications in Infectious Disease:
- hMHC mice enable study of human T cell responses to viral pathogens including SARS-CoV-2 [81].
- These models demonstrate enhanced immunological activation relative to wild-type controls, particularly in IFN-γ signaling pathways that parallel human immune responses [81].
- hMHC mice provide a platform for vaccine antigen testing and evaluation of human-restricted immune recognition.
Limitations and Considerations:
- Despite humanized MHC, other aspects of the immune system remain murine, potentially affecting integrated immune responses.
- The tissue microenvironment in mice may not fully recapitulate human tissue immunity due to differences in stromal cells and tissue architecture.
Immune Organoids
Three-dimensional immune organoids represent emerging platforms for modeling human adaptive immunity in vitro:
Tonsil Organoids:
- Derived from discarded tonsil tissue following tonsillectomy [82].
- Recapitulate germinal center reactions including somatic hypermutation, antigen-specific antibody production, and class switching [82].
- Enable study of human B cell responses to vaccines and pathogens in a controlled system.
Multi-Organ Integration:
- Microfluidic chips connect distinct organoid modules to simulate systemic immunity [82].
- Enable tracking of immune cell migration between simulated tissue compartments.
- Provide platforms for studying tissue-specific immune responses and peripheral tolerance.
Applications in Vaccine Development:
- Immune organoids enable high-throughput screening of vaccine candidates and adjuvants [82].
- Model age-related differences in immune responses by incorporating cells from donors of different ages.
- Facilitate identification of correlates of protection through controlled manipulation of immune cell composition.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Platforms for Cross-Species Immunology
| Category | Specific Reagent/Platform | Application | Considerations |
|---|---|---|---|
| Single-Cell Technologies | 10X Genomics Chromium | Single-cell RNA-seq and CITE-seq | Enables multimodal profiling of up to 10,000 cells/sample |
| TotalSeq Antibody Panels | Oligonucleotide-conjugated antibodies for CITE-seq | Requires optimization of staining concentrations | |
| Computational Tools | CellTypist | Automated cell type annotation | Trained on pan-tissue immune cell references [80] |
| Seurat Integration | Cross-species data alignment | Corrects for technical and biological batch effects | |
| Humanized Models | hMHC Mice | Human-restricted antigen presentation | HLA-transgenic on murine MHC-deficient background [81] |
| Immune Organoids | 3D modeling of human immune responses | Preserves tissue architecture and cell-cell interactions [82] | |
| Tissue Processing | Liberase TM | Tissue dissociation for immune cell isolation | Gentler than traditional collagenase; preserves surface epitopes |
| GentleMACS Dissociator | Automated tissue processing | Standardized mechanical dissociation across samples |
Cross-species immunology has entered a transformative period, fueled by advanced single-cell technologies and innovative model systems. The integration of human postmortem studies with comparative analyses in model organisms has revealed both fundamental principles of tissue immunity and species-specific adaptations that critically inform translational research. The dominant influence of tissue microenvironment on immune cell identity and function emerges as a conserved feature across species, highlighting the importance of studying immunity in its physiological context rather than relying solely on circulating cells [2] [80].
Future progress in the field will likely focus on several key areas: First, the development of more sophisticated humanized models that incorporate human stromal components to better recreate tissue-specific immune niches. Second, the integration of spatial transcriptomics with single-cell profiling to preserve architectural context in analyses of tissue immunity. Third, the application of cross-species comparisons to additional tissue sites and disease states to identify generalizable principles of immune regulation. Finally, the leveraging of conserved immune responses to identify novel therapeutic targets with broad translational potential.
As these technologies and approaches mature, cross-species immunology will continue to bridge the gap between model organism research and human immunology, accelerating the development of novel immunotherapies and vaccines while deepening our understanding of the fundamental principles governing immune protection across tissues and species.
Correlating Tissue Findings with Clinical Histories and Disease Outcomes
The integration of tissue-specific findings with clinical histories represents a cornerstone of modern biomedical research, particularly for understanding human disease and developing new therapeutics. For researchers studying the human immune system, this correlation is paramount, as immune responses are highly specialized within different tissue environments. Postmortem tissues from organ donors provide an unparalleled opportunity to study these tissue-specific immune landscapes at a systems level across the entire human body. However, this approach introduces significant methodological challenges, primarily concerning the postmortem interval (PMI)—the time between death and tissue preservation—which can induce molecular changes that obscure genuine disease-specific signatures [83] [20] [84]. This technical guide outlines advanced protocols and analytical frameworks for correlating tissue findings with clinical histories, with a specific focus on preserving the fidelity of tissue-specific immune responses in human postmortem studies for robust research and drug development.
Quantitative Concordance Between Diagnostic Modalities
The accurate correlation of tissue findings with clinical presentation relies on multiple, often independent, diagnostic methods. Understanding the rates of agreement between these methods is critical for interpreting data and building validated experimental models. The table below summarizes concordance rates from key studies in different pathological contexts.
Table 1: Concordance Rates Between Diagnostic and Histopathological Methods
| Pathology Context | Comparison | Overall Concordance Rate | Notes on Discordance | Source Study |
|---|---|---|---|---|
| Oral & Maxillofacial Lesions [85] | Clinical vs. Histopathological Diagnosis | 72.2% (2167/3001 cases) | Lowest concordance for pigmented lesions and lesions on the gingiva. | Retrospective analysis of biopsy specimens. |
| Skin & Soft Tissue Infections (SSTIs) [86] | Histopathology vs. Tissue Culture | 76.1% (355 cases) | Lowest concordance for suspected bacterial infections identified by histopathology (61.9%). | Single-center retrospective study. |
| Necrotizing Fasciitis [87] | Novel Histopathologic Staging vs. Mortality | Stage I: 7.1% MortalityStage III: 47% Mortality | Histopathologic stage based on neutrophilic response and bacterial presence significantly correlated with clinical outcome. | Retrospective study of 63 cases. |
Experimental Protocols for Tissue-Specific Immune Cell Profiling
The following section provides detailed methodologies for the comprehensive profiling of immune cells from human postmortem tissues, as utilized in recent landmark studies.
Multimodal Single-Cell RNA and Protein Sequencing (CITE-seq)
This protocol enables the simultaneous quantification of transcriptomes and surface protein expression from single-cell suspensions, allowing for high-resolution immune cell annotation [2].
- Tissue Acquisition & Cell Isolation: Mononuclear cells (MNCs) are isolated from blood, lymphoid organs (bone marrow, spleen, lymph nodes), and mucosal sites (lungs, jejunum) using established density gradient centrifugation and enzymatic digestion protocols. For solid tissues, dissociate using the gentleMACS Octo Dissociator with heaters and specific programs (e.g., "Lung Program 1" and "2" for lung tissue) in the presence of an enzyme mixture (e.g., Collagenase D and DNase I) [2] [18].
- Cell Staining and Library Preparation:
- Create a single-cell suspension and stain with a panel of 127 DNA-barcoded antibodies (TotalSeq-B from BioLegend) for surface protein detection.
- Load the stained cells onto a 10X Genomics Chromium Controller using the 3' Single Cell Gene Expression Kit to generate Gel Bead-In Emulsions (GEMs).
- Perform reverse transcription within GEMs to barcode cDNA.
- Break emulsions, purify cDNA, and amplify by PCR.
- Execute library construction for both gene expression (from cDNA) and surface protein (from antibody-derived tags) sequencing.
- Sequencing and Data Processing: Sequence libraries on an Illumina platform. Process raw data using Cell Ranger (10X Genomics) to align reads and generate feature-barcode matrices. Subsequent analysis, including data integration and harmonization across donors, can be performed using tools like multi-resolution variational inference (MrVI) [2].
- Cell Annotation: Classify cells hierarchically into major lineages (T cells, B cells, myeloid cells) and subsets using a MultiModal Classifier Hierarchy (MMoCHi) that leverages both gene expression and surface protein data for superior accuracy [2].
High-Dimensional Flow Cytometry for T Cell Phenotyping
This protocol is used for deep immunophenotyping of T cell populations across various tissues from organ donors [18].
- Sample Collection: Collect post-mortem tissues (lung, lymph nodes, spleen) and perform bronchoalveolar lavage (BAL). Transport samples in RPMI medium with fetal bovine serum (FBS) at room temperature.
- Cell Isolation from Tissues:
- Lung/Lymph Node Processing: Mechanically tease apart tissues and digest using the gentleMACS Octo Dissociator with collagenase/DNase enzyme mixture.
- Filter the resulting suspension through 70 μm and 40 μm cell strainers.
- Centrifuge to obtain a cell pellet and lyse residual red blood cells using ACK lysis buffer.
- Wash cells and count using an automated cell counter (e.g., BioRad TC20).
- PBMC Isolation: Dilute heparinized blood with RPMI and layer over Ficoll-Paque PLUS. Centrifuge to isolate the PBMC buffy coat by density gradient centrifugation.
- Cell Staining and Acquisition:
- Incubate cells with a pre-optimized 29-color flow cytometry panel including antibodies against CD3, CD4, CD8, CD45RA, CCR7, CD69, CD103, KLRG1, and CD27.
- Acquire data on a high-parameter flow cytometer (e.g., Cytek Aurora).
- Analyze data using FlowJo software and perform statistical analysis in GraphPad Prism.
Workflow Visualization of Key Methodologies
Multimodal Immune Profiling Workflow
Postmortem Tissue Study Considerations
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their applications for successfully executing the protocols described in this guide.
Table 2: Essential Research Reagents for Tissue-Based Immune Profiling
| Reagent / Kit | Primary Function | Application in Protocol |
|---|---|---|
| gentleMACS Octo Dissociator [2] [18] | Automated mechanical and enzymatic tissue dissociation. | Standardized digestion of solid tissues (lung, lymph node, jejunum) to generate single-cell suspensions. |
| Collagenase D & DNase I Enzyme Mixture [18] | Enzymatic breakdown of extracellular matrix and DNA. | Used during tissue dissociation to prevent cell clumping and improve yield of viable immune cells. |
| 10X Genomics 3' Single Cell Kit [2] [20] | Single-cell RNA-seq library preparation. | Generating barcoded cDNA libraries from single cells for transcriptome and surface protein (CITE-seq) analysis. |
| TotalSeq-B Antibody Panel [2] | Multiplexed surface protein detection. | Antibodies conjugated to DNA barcodes enable simultaneous protein quantification with transcriptome in CITE-seq. |
| Ficoll-Paque PLUS [18] | Density gradient medium. | Isolation of peripheral blood mononuclear cells (PBMCs) from whole blood by density centrifugation. |
| 29-Color Flow Cytometry Panel [18] | High-parameter surface and intracellular protein detection. | Deep immunophenotyping of T cell subsets (e.g., Naive, TCM, TEM, TRM) across tissues. |
| Miltenyi Nuclei Extraction Buffer [20] | Lysis buffer for nuclei isolation. | Extraction of intact nuclei from frozen tissue for single-nucleus RNA sequencing (snRNA-seq). |
| RNase Inhibitor [20] | Inhibition of RNase activity. | Added to all buffers during nuclei isolation to preserve RNA integrity and prevent degradation. |
Critical Consideration: The Impact of Postmortem Interval
A critical factor in correlating postmortem tissue findings with clinical histories is accounting for the Postmortem Interval (PMI). Evidence shows that even short PMIs can significantly alter molecular readouts:
- Gene Expression: A 3-hour PMI in mouse models was sufficient to diminish the number of differentially expressed genes between diseased (PS19 tauopathy) and wild-type mice, thereby obscuring disease-specific transcriptomic signatures [20].
- Molecular Fidelity: Large-scale comparisons between living and postmortem human brain tissue reveal distinct molecular characters, with over 60% of proteins and 95% of RNA types being differentially expressed or processed [32]. Pathways involved in DNA repair, immune response, and stress are upregulated postmortem [20].
- Best Practices: To mitigate these effects, researchers should minimize PMI wherever possible, record PMI meticulously for use as a covariate in statistical models, and consider single-nucleus RNA sequencing from frozen tissues, as nuclear RNA can be more stable than cytoplasmic RNA over extended intervals [83] [20].
In the pursuit of understanding human disease and developing novel therapeutics, human postmortem tissue represents an indispensable, yet historically underutilized, resource. While animal and in vitro models provide foundational insights, they often fail to recapitulate the full complexity of human pathophysiology arising from genetic heterogeneity, environmental influences, and the chronic nature of human diseases [73]. The genome-wide association studies in Alzheimer's disease, for instance, highlighted inflammation as a driver of the disease rather than a consequence, a finding that required validation in human tissue to confirm its relevance to human pathology [73]. Postmortem studies enable researchers to directly observe disease processes in the affected tissues, providing an unparalleled window into the spatial organization of disease, cell-type-specific responses, and the molecular networks dysregulated in human conditions.
The mid-20th century saw the emergence of organized brain banking to systematically archive, collect, and distribute human brain samples, facilitating access for researchers worldwide [73]. Today, networks like BrainNet Europe and the NIH NeuroBioBank operate under stringent ethical frameworks to provide high-quality tissue for research [73]. This guide details how these precious tissues are leveraged to inform diagnostic biomarker discovery and therapeutic development, with a specific focus on tissue-specific immune responses.
Key Applications in Disease Research and Therapy Development
Unraveling Neuroinflammatory Pathways in Alzheimer's Disease
Research on postmortem brain tissue has been instrumental in delineating the neuroinflammatory components of Alzheimer's disease (AD). Studies validate in vivo and model-based observations by quantitatively assessing microglial activation states and inflammatory mediators in the human brain. The marker Iba1 (ionized calcium-binding adaptor molecule 1) is widely acknowledged as a reliable marker for microglia in the human brain, independent of their functional state, with increased expression noted during neuroinflammation [73]. Furthermore, the known genetic risk factor APOE genotype has been associated with differential microglial activation in AD brains, influencing the expression of inflammatory molecules and highlighting how genetic context shapes the neuroimmune response [73].
Table 1: Key Microglial and Immune Markers in Postmortem Neuroinflammation Research
| Marker | Cell Type/Process | Significance in Human Postmortem Studies |
|---|---|---|
| Iba1 | Microglia | Reference marker for microglial density and morphology; expression increases with activation [73] |
| CD68 | Macrophages/Microglia | Identifies phagocytic activity; used to characterize infiltrates in COVID-19 and other CNS pathologies [88] |
| CD3, CD4, CD8 | T Lymphocytes | Characterizes T-cell subsets in neuroinflammatory infiltrates; spatial analysis reveals proximity to pathology [88] |
| TIM-3, PD-1 | Immune Exhaustion | High-dimensional profiling links these inhibitory receptors to immunosuppression in severe infections like COVID-19 [89] |
| TTF-1, Cytokeratin | Alveolar Epithelium | In lung studies, helps identify SARS-CoV-2 viral cytopathic effects and pneumocyte hyperplasia [88] |
High-Dimensional Immune Profiling in Severe COVID-19
The COVID-19 pandemic underscored the critical role of postmortem analysis in understanding a novel disease. Comprehensive high-dimensional transcriptional and spatial immune profiling of tissues from COVID-19 decedents revealed distinct patterns of immunosuppression and immunoactivation [89]. A key finding was that lymphocyte suppression and myeloid activation occurred concurrently but independently. Notably, activated myeloid cells (macrophages and dendritic cells) were found proximal to SARS-CoV-2 viral antigens, while suppressed lymphocytes were distal, suggesting a mechanism of immune evasion [89]. This spatial relationship, discernible only through tissue-based analysis, provides a direct rationale for targeting specific immune compartments differently in therapy.
Defining Ancestry-Associated Immune Signatures in the Brain
Recent work has illuminated the significant impact of genetic ancestry on brain immune gene expression. An analysis of the postmortem brain tissue of neurotypical Black Americans revealed thousands of ancestry-associated differentially expressed genes (DEGs) [90]. These DEGs were notably enriched for genes related to the immune response and vascular tissue, but not neurons, and explained a substantial fraction of the heritability for Alzheimer's disease (up to 30%), Parkinson's disease (up to 27%), and ischemic stroke (up to 26%) [90]. This research demonstrates how postmortem studies can uncover population-specific disease vulnerabilities and provides a biological basis for health disparities, guiding the development of more inclusive and effective diagnostics and therapeutics.
Methodological Framework: From Tissue Acquisition to Data Analysis
Tissue Acquisition, Quality Control, and Ethics
The utility of postmortem data hinges on rigorous tissue quality control. Standard practice in prospective brain banks involves fixing one hemisphere for histology and freezing the other for molecular analyses [73]. Key pre- and post-mortem factors that impact tissue integrity must be meticulously recorded and controlled for in analyses. These include the post-mortem interval (PMI), agonal status, age, gender, genetic background, preterminal medication, and concomitant diseases [73].
Table 2: Critical Factors for Quality Control in Postmortem Tissue Studies
| Factor | Impact on Tissue | Quality Assessment Metrics |
|---|---|---|
| Post-Mortem Interval (PMI) | Degradation of RNA, proteins, and metabolites; should ideally be <24-72 hours [73] | Shorter PMI correlates with better macromolecule preservation. |
| Agonal Status | Influences tissue pH and RNA integrity [73] | pH, RNA Integrity Number (RIN) [73] |
| Tissue Fixation | Over-fixation can mask epitopes for antibody binding; standardizing time is crucial [73] | Time in fixative; antigen retrieval optimization required. |
| Concomitant Disease | Systemic inflammation or infection can alter the tissue's immune profile [73] | Review of medical records and post-mortem reports. |
Ethical oversight is paramount. Reputable brain banks operate under licenses from regulatory bodies (e.g., the Human Tissue Authority in the UK) and provide ethical coverage for approved research projects, streamlining the administrative process for researchers [73].
Analytical Techniques for Immune Profiling
A multi-modal approach is essential for a comprehensive understanding of the tissue immune landscape.
- Histology and Immunohistochemistry (IHC): Traditional IHC on fixed paraffin-embedded or free-floating sections allows for the qualitative and quantitative assessment of protein markers. This includes determining the presence, absence, cellular localization, and morphology of immune cells (e.g., ramified vs. amoeboid microglia) [73]. Quantitative data can be collected as cell counts per field, protein load (percentage of stained area), or semi-quantitative scoring systems [73]. Multiplex IHC (mIHC) and digital spatial profiling (DSP) further enable the characterization of multiple markers simultaneously within their spatial context [89].
- Molecular Analyses on Frozen Tissue: Frozen tissue is suitable for bulk RNA-sequencing to define transcriptional profiles and pathway alterations [89]. It also allows for T cell receptor (TCR) sequencing to assess clonality and immune repertoire, which has predictive value in oncology and infectious disease [91]. DNA methylation and other epigenetic analyses can reveal the regulatory mechanisms behind observed gene expression changes [90].
- Cell Type Enrichment and Spatial Analysis: Bioinformatic tools can deconvolute bulk RNA-seq data to estimate cell type abundance [90]. Spatial transcriptomics and proteomics preserve the architectural context of the tissue, allowing researchers to correlate molecular findings with specific histological regions or cell populations, such as analyzing CD3+-rich versus CD68+-rich regions separately [89].
Diagram 1: Postmortem tissue analysis workflow
Table 3: Research Reagent Solutions for Postmortem Immune Profiling
| Reagent/Resource | Function | Application Example |
|---|---|---|
| Iba1 Antibody | Labels microglia regardless of activation state; essential for quantifying microglial response in neurodegeneration [73] | Differentiating homeostatic vs. activated microglia density in Alzheimer's disease brain sections. |
| CD3/CD68 Antibodies | Pan-T cell and macrophage/microglia markers, respectively; used for basic immune cell phenotyping [88] [89] | Characterizing lymphocytic vs. myeloid infiltrates in COVID-19 lung tissue. |
| Oncomine TCR Pan-Clonality Assay | Targeted NGS assay for TCRβ/γ CDR3 regions; works well with FFPE-derived DNA [91] | Sequencing the T-cell repertoire from lung cancer FFPE samples to predict immunotherapy response. |
| Digital Spatial Profiler (DSP) | Allows for multiplexed, spatially resolved quantification of protein or RNA from predefined tissue regions [89] | Profiling immune exhaustion markers (PD-1, TIM-3) in CD3+ vs. CD68+ regions of infected tissues. |
| Brain Bank Networks | Centralized portals for accessing quality-controlled, well-characterized human postmortem tissue (e.g., NIH NeuroBioBank, BrainNet Europe) [73] | Sourcing matched disease and control brain tissue for a study on genetic ancestry and immune gene expression. |
Postmortem human tissue research remains the gold standard for validating disease mechanisms discovered in model systems and for generating novel, human-relevant biological insights. The integration of high-dimensional spatial and molecular techniques with traditional histopathology unlocks unprecedented detail about the tissue-specific immune response in human disease. As methods continue to advance, the strategic use of this irreplaceable resource will be pivotal in de-risking therapeutic targets, explaining treatment failures, and ultimately guiding the development of next-generation diagnostics and personalized immunotherapies.
Conclusion
Human postmortem studies provide an unparalleled, direct window into the spatial organization and functional state of the immune system within its native tissue contexts. They have been instrumental in defining the critical role of tissue-resident memory T cells in sites like the lung, revealing localized immune adaptations, and highlighting the limitations of extrapolating from blood-based assays or animal models alone. The integration of advanced tools—from high-dimensional flow cytometry to AI-driven transcriptomic analysis—is rapidly accelerating this field. The future of tissue-specific immunology lies in building even more comprehensive atlases of health and disease, leveraging these insights to develop next-generation vaccines that induce robust tissue-resident memory, and designing precisely targeted immunotherapies for cancer, autoimmunity, and transplantation that modulate local rather than systemic immunity. This human-tissue-centric approach is poised to fundamentally refine our understanding of immune protection and pathology.
References
- 1. Tissue-resident immune cells: from defining characteristics ... [https://www.nature.com/articles/s41392-024-02050-5]
- 2. Multimodal profiling reveals tissue-directed signatures of ... [https://www.nature.com/articles/s41590-025-02241-4]
- 3. Tissue-resident macrophages and renal diseases [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1548053/full]
- 4. Resident memory macrophages and trained innate immunity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537008/]
- 5. Editorial: New approach methods in immunology [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1488534/full]
- 6. Quantitative characterization of immune cells by measuring ... [https://www.nature.com/articles/s41598-024-75666-w]
- 7. Leveraging tissue-resident memory T cells for non-invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11957092/]
- 8. Engineering human immune organoids for translational ... [https://www.sciencedirect.com/science/article/pii/S2452199X24004547]
- 9. New research reveals how location influences how our ... [https://alleninstitute.org/news/new-research-reveals-how-location-influences-how-our-immune-system-fights-disease/]
- 10. new insights in crosstalk between immune niches and CNS [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1604987/full]
- 11. A four-part guide to lung immunology [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1119564/full]
- 12. high-dimensional Postmortem ... | Nature Communications immune [https://www.nature.com/articles/s41467-021-27723-5?error=cookies_not_supported&code=16ba9c9a-3417-42e6-b549-647e40ab5fae]
- 13. Review The roles of tissue-resident memory T cells (TRMs) ... [https://www.sciencedirect.com/science/article/abs/pii/S0264410X25009028]
- 14. Single-nucleus transcriptome analysis of human brain immune ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-021-00933-8]
- 15. Frontiers | Imaging Mass Cytometric Analysis of Postmortem Tissues... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.600989/full]
- 16. Immunoinflammation and post-translational modifications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355846/]
- 17. Enrichment of Glial Cells From Human Post-mortem Tissue ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2021.772011/full]
- 18. Tissue-specific T cell profiles in Mycobacterium ... [https://www.frontiersin.org/journals/tuberculosis/articles/10.3389/ftubr.2025.1535945/full]
- 19. Extended human lymph node explants for evaluation of ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779925003026]
- 20. Postmortem Interval Leads to Loss of Disease-Specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11913402/]
- 21. Adaptation in human immune cells residing in tissues at ... [https://www.nature.com/articles/s41467-024-54603-5]
- 22. Asynchronous aging and turnover of human circulating ... [https://www.sciencedirect.com/science/article/abs/pii/S1074761325003103]
- 23. The emerging role of tissue regulatory T cells in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1640113/full]
- 24. immune cells as architects of tissue barriers [https://pubmed.ncbi.nlm.nih.gov/41152441/]
- 25. Conserved and tissue-specific immune responses to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12306723/]
- 26. high-dimensional Postmortem of severe COVID-19... immune profiling [https://www.nature.com/articles/s41467-021-27723-5?error=cookies_not_supported&code=616adb30-a822-4445-89cd-96941432e0c5]
- 27. Impact of Confounding Factors in Human Postmortem Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12416912/]
- 28. Postmortem Changes in mRNA Expression and Tissue ... [https://www.mdpi.com/1422-0067/26/15/7059]
- 29. Frontiers | SHARD: an improved method for staining and visualizing... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1474617/full]
- 30. Maxpar Direct Human System | Standard BioTools Immune Profiling [https://www.standardbio.com/area-of-interest/immune-profiling/maxpar-direct-immune-profiling-system]
- 31. A tissue analysis framework for investigating local immune ... [https://www.sciencedirect.com/science/article/pii/S221112472301224X]
- 32. Two Mount Sinai Research Papers Present Evidence of ... [https://www.mountsinai.org/about/newsroom/2025/two-mount-sinai-research-papers-present-evidence-of-distinct-molecular-differences-between-brain-tissue-from-living-people-and-tissue-collected-after-death]
- 33. Proteomic analysis of brain and spinal cord tissue reveals ... [https://www.nature.com/articles/s41598-025-11466-0]
- 34. Transcriptomic analysis at 48 h postmortem: a proof of concept ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540568/]
- 35. For All the Primate FANS: Optimized Isolation of Nuclei ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204041/]
- 36. Flow cytometry protocol for cell death analysis in glioblastoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456761/]
- 37. IQGAP2 regulates blood-brain barrier immune dynamics [https://www.sciencedirect.com/science/article/pii/S2589004225002548]
- 38. 29-Color Flow Cytometry: Unraveling Human Liver NK Cell ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.02692/full]
- 39. 29-Color Flow Cytometry: Unraveling Human Liver NK Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6878906/]
- 40. Spectral Flow Cytometry: The Current State and Future of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193525/]
- 41. A Beginner's Guide To Analyzing and Visualizing Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5765874/]
- 42. scHDeepInsight: a hierarchical deep learning framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502058/]
- 43. APOE ε4 carriers share immune-related proteomic ... [https://www.nature.com/articles/s41591-025-03835-z]
- 44. The impact of apolipoprotein E, type ∊4 allele on Alzheimer's ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0303486]
- 45. GSDMD is a novel predictive biomarker for immunotherapy ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1570901/full]
- 46. Spatial Transcriptomics: A Powerful Tool in Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11103497/]
- 47. Categorization of 34 computational methods to detect ... [https://www.nature.com/articles/s41467-025-56080-w]
- 48. Systematic benchmarking of high-throughput subcellular ... [https://www.nature.com/articles/s41467-025-64292-3]
- 49. Spatiotemporal analysis of gene expression in the human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12353348/]
- 50. Integrating multiple spatial transcriptomics data using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11990772/]
- 51. Scaling up spatial transcriptomics for large-sized tissues [https://www.nature.com/articles/s41592-025-02770-8]
- 52. Inferring spatial and signaling relationships between cells ... [https://www.nature.com/articles/s41467-020-15968-5]
- 53. spatially aware color palette optimization for single-cell and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9272793/]
- 54. Feasibility and acceptability of undertaking postmortem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10734300/]
- 55. Prism [https://www.graphpad.com/features]
- 56. Statistics in Immunology [https://www.graphpad.com/series/statistics-in-immunology]
- 57. Human brain slice cultures: translational applications and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511760/]
- 58. Cell Viability of Skin Tissue Collected from Postmortem ... [https://www.mdpi.com/2673-5636/6/2/31]
- 59. A Protocol for Rapid Post-mortem Cell Culture of Diffuse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5409295/]
- 60. Quantitative Analysis of S1PR1 Expression in the Postmortem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11037862/]
- 61. Standardization of postmortem human brainstem along the ... [https://www.nature.com/articles/s41598-025-20016-7]
- 62. From Uncertainty to Consent: Educational Intervention Effects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524708/]
- 63. Open group dialogue on post-mortem organ donation ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1631504/full]
- 64. Anteâ€mortem interventions for deceased donation: legal ... [https://www.mja.com.au/journal/2025/223/5/ante-mortem-interventions-deceased-donation-legal-barriers-and-uncertainty]
- 65. Immersionâ€Based Clearing and Autofluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589860/]
- 66. Efficient removal of naturally-occurring lipofuscin ... [https://www.sciencedirect.com/science/article/pii/S1526590025005863]
- 67. Distinct tissue niches direct lung immunopathology via ... [https://www.nature.com/articles/s41467-023-36333-2]
- 68. A study of gene expression in the living human brain [https://www.nature.com/articles/s41380-025-03163-1]
- 69. Comparing and combining data from immune assays ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9790822/]
- 70. Sensitive and Specific Immunohistochemistry Protocol for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8293419/]
- 71. Immune response to traumatic injury: harmony and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5997205/]
- 72. Trauma equals danger—damage control by the immune system [https://pmc.ncbi.nlm.nih.gov/articles/PMC3427603/]
- 73. Post-mortem analysis of neuroinflammatory changes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4405851/]
- 74. Editorial: New approach methods in immunology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11445123/]
- 75. Using Mice to Understand Human Immunology [https://pmc.ncbi.nlm.nih.gov/articles/PMC5512602/]
- 76. Deceased and Live Brains Modify RNA and Express Protein ... [https://www.the-scientist.com/deceased-and-live-brains-modify-rna-and-express-protein-differently-73750]
- 77. A Comprehensive Atlas of Immunological Differences ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.867015/full]
- 78. Organ-specific immunity: A tissue analysis framework for ... [https://pubmed.ncbi.nlm.nih.gov/37792533/]
- 79. Cross-species single-cell RNA-seq analysis reveals ... [https://www.nature.com/articles/s42003-024-07315-x]
- 80. Cross-tissue immune cell analysis reveals tissue-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7612735/]
- 81. Transcriptomic profiling reveals SARS-CoV-2-infected ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12353716/]
- 82. Immune organoids: emerging platforms for modeling and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1632117/full]
- 83. Current Understanding and Future Research Direction for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346081/]
- 84. Redefining postmortem interval estimation: the need for ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1646907/full]
- 85. Correlation between Clinical and Histopathological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9124151/]
- 86. Diagnostic concordance of clinical diagnosis, tissue culture ... [https://www.sciencedirect.com/science/article/pii/S2352647520301337]
- 87. Correlation of histopathologic findings with clinical ... [https://pubmed.ncbi.nlm.nih.gov/15668865/]
- 88. An Insight into the Role of Postmortem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8584583/]
- 89. Postmortem high-dimensional immune profiling of severe ... [https://www.nature.com/articles/s41467-021-27723-5]
- 90. Analysis of gene expression in the postmortem brain ... [https://www.nature.com/articles/s41593-024-01636-0]
- 91. Tissue and peripheral T cell receptor repertoire predicts ... [https://www.nature.com/articles/s41598-025-21612-3]