Developing a Robust 3D Human Airway Model Protocol for Advanced Viral Pathogenicity and Drug Screening Studies
This protocol provides a comprehensive guide for researchers to establish, maintain, and apply advanced in vitro 3D human airway models for studying viral pathogenicity.
Developing a Robust 3D Human Airway Model Protocol for Advanced Viral Pathogenicity and Drug Screening Studies
Abstract
This protocol provides a comprehensive guide for researchers to establish, maintain, and apply advanced in vitro 3D human airway models for studying viral pathogenicity. It details the foundational biology of airway epithelium, step-by-step methodologies for model generation from primary cells or induced pluripotent stem cells (iPSCs), and optimized culture conditions using air-liquid interface (ALI) systems. The article addresses common troubleshooting issues, benchmarks the model's performance against traditional 2D cultures and animal models, and validates its application for quantifying viral infection kinetics, host immune responses, and therapeutic efficacy. This resource is essential for virologists and translational scientists seeking physiologically relevant platforms for respiratory virus research and antiviral development.
Why 3D Airway Models? Understanding the Biology and Superiority for Viral Infection Studies
The Limitations of 2D Cell Lines and Animal Models in Respiratory Virology
Application Notes
Critical Limitations of Conventional Models
The study of respiratory viruses has historically relied on two-dimensional (2D) immortalized cell lines (e.g., A549, Vero E6, MDCK) and animal models (e.g., ferrets, mice, Syrian hamsters). While invaluable, these systems exhibit significant shortcomings that compromise their predictive value for human disease and therapeutic response.
1.1.1 Limitations of 2D Cell Lines:
- Lack of Physiological Architecture: Monolayers lack the pseudostratified, mucociliary epithelium of the human airway. This omits crucial biological barriers and cell-cell interactions.
- Altered Cell State: Immortalization alters innate immune responses, metabolic activity, and receptor expression profiles.
- Absence of a Mucociliary Escalator: Critical for understanding viral entry, particle trapping, and clearance.
- Simplified Polarity: Most 2D cultures have incomplete apical-basal polarity, skewing viral entry studies.
1.1.2 Limitations of Animal Models:
- Species-Specific Differences: Key receptors (e.g., ACE2 for SARS-CoV-2) may have different expression patterns or binding affinities.
- Divergent Immune Responses: Innate and adaptive immune pathways differ from humans, affecting pathogenesis readouts.
- Inability to Model Human-Specific Symptoms: Animals often do not develop the full spectrum of clinical disease (e.g., complex cough, anosmia in COVID-19).
- Ethical and Cost Constraints: High-cost, low-throughput, and increasing ethical concerns limit scalability.
Quantitative Comparison of Model Systems
Table 1: Comparative Analysis of Respiratory Virology Models
| Feature | 2D Cell Lines | Animal Models | 3D Human Airway Models |
|---|---|---|---|
| Physiological Relevance | Low | Moderate to High | High |
| Human-Specific Immunity | Very Low | Low | High (if derived from primary cells) |
| Throughput & Cost | High throughput, Low cost | Low throughput, High cost | Moderate throughput, Moderate cost |
| Genetic Manipulability | High | Low to Moderate | Moderate (depends on base cells) |
| Mucociliary Function | Absent | Present but species-specific | Present (human) |
| Lifetime/Duration | Essentially unlimited | Weeks to months | 4-8 weeks (for primary cell-based) |
| Key Limitation | Non-physiological architecture | Species divergence | Variable donor-to-donor reproducibility |
Table 2: Example Data Highlighting Model Discrepancies for SARS-CoV-2
| Viral Parameter | Vero E6 (2D) | Syrian Hamster | Human Primary Airway Epithelium |
|---|---|---|---|
| Primary Entry Receptor (ACE2) Expression Level | Low/Non-native | Moderate | High (apical, native context) |
| TMPRSS2 Protease Expression | Low | High | High (native localization) |
| Peak Viral Titer (Typical log10 TCID50/mL) | 7-8 | 5-6 (lung homogenate) | 6-7 (apical wash) |
| Pro-inflammatory Cytokine Response (e.g., IL-6) | Attenuated/Abnormal | Strong but species-specific | Human-specific, robust |
| Sensitivity to Interferon Pre-treatment | High (defective IFN genes) | Moderate | Variable, donor-dependent |
Experimental Protocols
Protocol: Establishing a Primary Human 3D Airway Epithelial Model at Air-Liquid Interface (ALI)
Title: Differentiation of Primary Human Bronchial Epithelial Cells at Air-Liquid Interface.
Principle: Primary human bronchial epithelial cells (HBECs) are expanded and then differentiated on permeable membrane supports at an air-liquid interface (ALI) to form a pseudostratified, mucociliary epithelium.
Materials (Research Reagent Solutions):
- Primary HBECs: Sourced from donor lungs or bronchi. Essential for retaining native genetics and differentiation potential.
- PneumaCult-Ex Plus or BEGM: Expansion medium for proliferating basal cells.
- PneumaCult-ALI or ALI Differentiation Medium: Specialty medium containing factors (e.g., retinoic acid) to induce mucociliary differentiation.
- Transwell Permeable Supports (0.4 μm pore, polyester): Provides a porous substrate for polarized culture and ALI establishment.
- Coating Matrix (Collagen IV/ Fibronectin): Enhances cell attachment to the Transwell membrane.
- Dimethyl Sulfoxide (DMSO) & FBS: For cryopreservation of primary cells.
- Phosphate Buffered Saline (PBS) w/ Ca2+/Mg2+: For washing apical surfaces without disrupting tight junctions.
- TRIzol or RLT Lysis Buffer: For downstream RNA/DNA extraction from the 3D epithelium.
- 4% Paraformaldehyde (PFA): For fixing tissues for histology.
Procedure:
- Thawing and Expansion: Rapidly thaw cryopreserved HBECs. Seed cells in T-flasks with pre-warmed expansion medium. Change medium every 48 hours until ~80% confluent.
- Transwell Seeding: Coat Transwell inserts with diluted matrix (e.g., 30 μg/mL Collagen IV) for 1-2 hours at 37°C. Aspirate coating. Trypsinize expanded HBECs and seed at high density (e.g., 2.5-5.0 x 10^4 cells/cm²) onto the apical chamber of the coated insert. Add medium to both apical and basolateral chambers for the first 24-48h to allow attachment.
- Air-Liquid Interface Initiation: After 48-72 hours, or when a confluent monolayer forms, aspirate medium from the apical chamber only. Feed cells exclusively from the basolateral chamber with ALI differentiation medium. This marks Day 0 of ALI.
- Differentiation and Maintenance: Change basolateral medium every 48-72 hours. Gently wash the apical surface with 200-300 μL of PBS (with Ca2+/Mg2+) weekly to remove accumulated mucus.
- Maturity Validation: The epithelium typically matures in 4-6 weeks. Assess via:
- Transepithelial Electrical Resistance (TEER): Measure weekly using a volt-ohm meter. Mature cultures often have TEER >500 Ω·cm².
- Histology: Fix inserts in 4% PFA at week 4-5, paraffin-embed, section, and stain with H&E or Alcian Blue/PAS for goblet cells and cilia.
- Ciliary Beat Frequency: Visualize via phase-contrast microscopy.
Protocol: Viral Pathogenicity and Infection Kinetics in 3D ALI Models
Title: Apical Infection of 3D ALI Cultures with Respiratory Virus.
Principle: Virus is inoculated onto the apical (air-facing) surface of the mature ALI culture to mimic natural infection, allowing measurement of replication kinetics and host response.
Materials:
- Mature 3D ALI Cultures: ≥28 days post-ALI.
- Virus Inoculum: Respiratory virus of interest (e.g., SARS-CoV-2, RSV, IAV) titered on relevant cells.
- Infection Medium: Serum-free basal medium (e.g., DMEM/F12).
- Apical Wash Collection Buffer: Infection medium with a defined protein source (e.g., 0.1% BSA).
- RNA/DNA Extraction Kit: For viral genome quantification.
- Plaque Assay or TCID50 Reagents: For infectious virus titration.
- Cytokine ELISA/MSD Kits: For quantifying human cytokine secretion.
Procedure:
- Pre-infection Wash: Gently wash the apical surface of each ALI culture with 200 μL of warm PBS (with Ca2+/Mg2+) to remove excess mucus. Aspirate.
- Virus Inoculation: Dilute virus stock in serum-free infection medium. Apply 100-200 μL of inoculum directly to the apical surface. Incubate at 37°C, 5% CO2 for 1-2 hours, gently tilting the plate every 15 minutes to ensure even coverage.
- Removal of Inoculum: Carefully aspirate the apical inoculum. Wash the apical surface once with 200 μL of PBS to remove unbound virus. Aspirate completely.
- Maintenance Post-Infection: Return cultures to the incubator, maintaining the ALI condition. Add fresh medium to the basolateral chamber.
- Sample Collection (Time Course):
- Apical Viral Shedding: At each time point (e.g., 24, 48, 72, 96 hpi), add 200 μL of collection buffer to the apical surface. Incubate for 10 minutes at 37°C, pipette up and down, and collect the wash. Aliquot for:
- Infectious titer (Plaque Assay/TCID50 on permissive cells).
- Viral genome load (qRT-PCR/qPCR).
- Basolateral Medium: Collect for analysis of secreted cytokines/chemokines (e.g., IL-6, IL-8, IFN-λ) via ELISA.
- Cell Lysate: At terminal time points, lyse cells in RLT/TRIzol buffer for host transcriptomic analysis (RNA-seq) or western blot.
- Apical Viral Shedding: At each time point (e.g., 24, 48, 72, 96 hpi), add 200 μL of collection buffer to the apical surface. Incubate for 10 minutes at 37°C, pipette up and down, and collect the wash. Aliquot for:
- Endpoint Analysis: Fix inserts for immunohistochemistry to visualize viral antigen distribution (e.g., nucleoprotein) relative to cell markers (e.g., acetylated α-tubulin for cilia, MUC5AC for goblet cells).
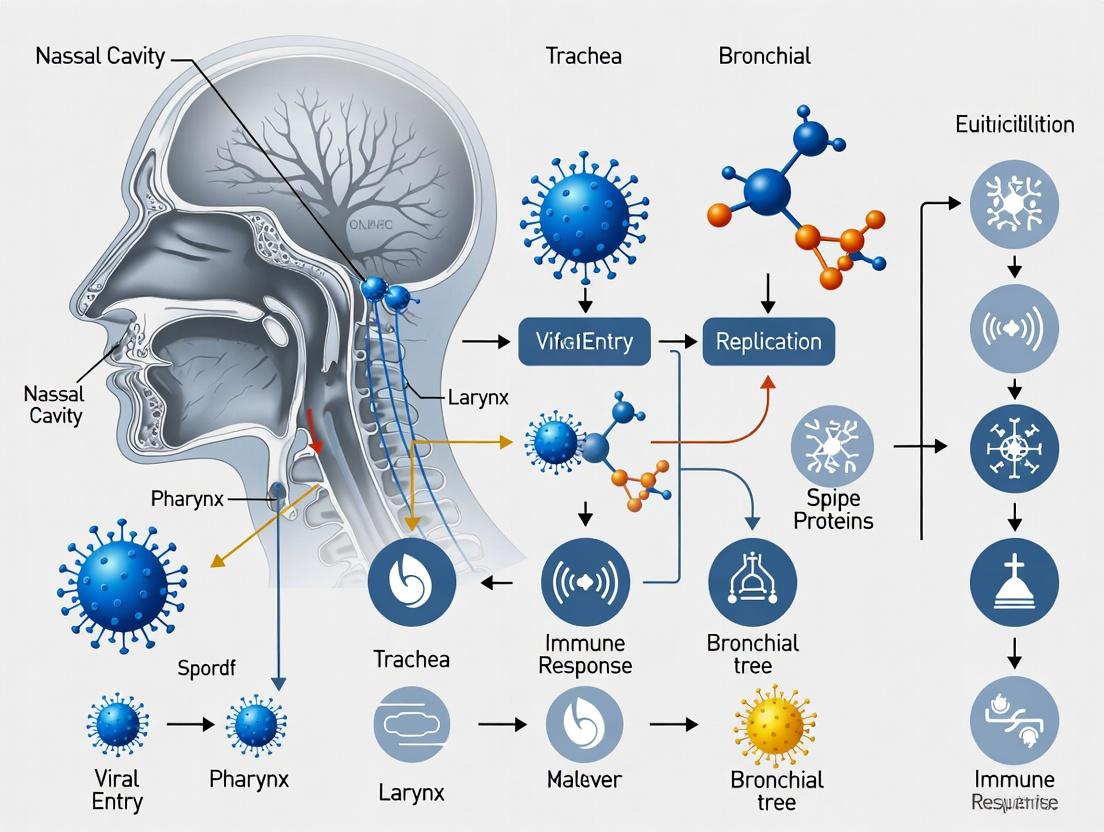
Signaling Pathway & Workflow Visualizations
Title: 3D Airway Model Differentiation Workflow
Title: Viral Infection Pathway in 3D Airway Epithelium
The Scientist's Toolkit: Essential Reagents for 3D Airway Virology
Table 3: Key Research Reagent Solutions for 3D Airway Model Studies
| Reagent/Material | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Primary Human Bronchial Epithelial Cells (HBECs) | Foundation of the model. Retain donor genetics, proper differentiation capacity, and native receptor expression. | Lonza CC-2540; Epithelix MucilAir; MatTek EpiAirway. |
| ALI Differentiation Medium | Specialized, defined medium containing factors (e.g., retinoic acid) to drive formation of ciliated and goblet cells. | STEMCELL PneumaCult-ALI; Epithelix MucilAir Medium. |
| Permeable Transwell Supports | Physical scaffold allowing polarized cell growth and establishment of the critical air-liquid interface. | Corning Costar 3470 (polyester, 0.4 µm). |
| Transepithelial Electrical Resistance (TEER) Meter | Quantitative, non-destructive measurement of epithelial barrier integrity and tight junction formation. | EVOM3 with STX2 chopstick electrode. |
| qPCR Assay for Viral Load | Sensitive, quantitative measurement of viral genomic copies from apical washes or cell lysates. | CDC SARS-CoV-2 N1/N2 assay; IDT PrimeTime assays. |
| Cytokine Detection Assay | Quantification of human-specific host immune response (e.g., IL-6, IL-8, IFN-λ) in basolateral media. | R&D Systems DuoSet ELISA; Meso Scale Discovery (MSD) U-PLEX. |
| Mucociliary Staining Antibodies | Validation of model maturity: Acetylated α-Tubulin (cilia), MUC5AC (goblet cells). | Proteintech 66200-1-Ig (α-Tubulin); Abcam ab19870 (MUC5AC). |
| Neutralizing Antibodies/ Antivirals | Positive controls for infection inhibition studies in the physiologically relevant system. | Remdesivir; SARS-CoV-2 neutralizing antibody (e.g., S309). |
Application Notes
This document details the in vivo cellular architecture of the human airway epithelium, providing the biological benchmark for developing physiologically relevant 3D human airway models. These models, including air-liquid interface (ALI) cultures and organoids, are essential for studying viral pathogenesis and screening antiviral therapeutics.
Core In Vivo Cellular Composition: The pseudostratified epithelium of the proximal conducting airways consists of diverse, specialized cell types. A summary of key quantitative data is provided in Table 1.
Table 1: Quantitative Cellular Composition of Human Bronchial Epithelium
| Cell Type | Approx. Abundance (%) | Primary Function(s) | Key Molecular Marker(s) |
|---|---|---|---|
| Ciliated Cells | 50-60% | Muccciliary clearance, innate defense | FOXJ1, β-IV-tubulin, DNAH5 |
| Secretory (Club & Goblet) Cells | 20-30% | Mucus production, immune modulation, regeneration | SCGB1A1 (Club), MUC5AC/B (Goblet) |
| Basal Cells | 30-40% | Progenitor/stem cells, epithelial integrity | TP63 (p63), KRT5, NGFR |
| Pulmonary Neuroendocrine Cells (PNECs) | <1% | Sensory chemoreception, immune signaling | CGRP, Synaptophysin, ASCL1 |
| Ionocytes | ~1% | Regulation of airway surface liquid, CFTR expression | FOXI1, CFTR, ASCL3 |
| Tuft Cells | Rare | Type 2 immune sensing | PLCG2, TRPM5, IL-25 |
Relevance to 3D Models: Faithful recapitulation of this cellular diversity, particularly the stem/progenitor function of basal cells and the proper differentiation into ciliated and secretory lineages, is critical for modeling viral entry, replication, host response, and barrier function. Recent single-cell RNA sequencing (scRNA-seq) studies confirm the presence of these populations and reveal subtle transcriptional states influenced by disease.
Protocols
Protocol 1: Isolation and Expansion of Primary Human Bronchial Epithelial Cells (HBECs) for 3D Model Establishment
Objective: To isolate basal progenitor cells from human airway tissue for generating ALI cultures or organoids.
Materials:
- Research Reagent Solutions:
- Pronase Solution (1-2% in PBS): Enzymatic digestion to dissociate epithelial sheets from connective tissue.
- Fetal Bovine Serum (FBS): To neutralize protease activity post-digestion.
- Bronchial Epithelial Growth Medium (BEGM): Complete medium with supplements (BPE, Retinoic Acid, etc.) for proliferative expansion of basal cells.
- Y-27632 (ROCK inhibitor): Added to initial culture to inhibit anoikis and enhance survival of seeded single cells.
- Fibronectin/Collagen-coated Flasks: For selective attachment and growth of basal epithelial cells over fibroblasts.
Procedure:
- Obtain fresh human bronchial tissue under approved IRB protocols. Rinse in cold PBS with antibiotics.
- Incubate tissue overnight at 4°C in Pronase solution.
- The next day, gently scrape the epithelial layer from the submucosa using a sterile scalpel. Transfer cell suspension to a tube containing FBS to halt digestion.
- Filter through a 100µm cell strainer and centrifuge.
- Resuspend pellet in BEGM + 10µM Y-27632. Seed onto coated flasks.
- Culture at 37°C, 5% CO₂, changing medium every 48 hours. Passage at ~80% confluence. Expand cells to desired number (Passage 2-4 recommended for differentiation).
Protocol 2: Differentiation at Air-Liquid Interface (ALI) to Reconstitute the In Vivo Epithelium
Objective: To differentiate expanded HBECs into a pseudostratified, mucociliary epithelium.
Materials:
- Research Reagent Solutions:
- ALI Differentiation Medium: Typically, a 50:50 mix of DMEM and BEGM base, without BPE or other proliferative agents, but with retinoic acid.
- PneumaCult-ALI or Similar Commercial Medium: Defined, optimized formulations for robust differentiation.
- Transwell Inserts (0.4µm pore, polyester): Porous supports allowing medium access only from the basolateral side.
- Matrigel/Collagen IV Coating: Provides a basement membrane matrix for cell attachment and polarization.
Procedure:
- Coat Transwell inserts with a thin layer of Matrigel or Collagen IV. Allow to set.
- Seed expanded HBECs at high density (~2.5-3.0 x 10⁵ cells/cm²) in BEGM onto the apical surface of the coated insert. Add medium to the basolateral chamber only.
- Once cells reach 100% confluence (2-3 days), initiate differentiation by removing apical medium and switching the basolateral medium to ALI Differentiation Medium. This establishes the Air-Liquid Interface.
- Maintain cultures for 28-35 days, changing the basolateral medium every 2-3 days.
- Quality Control: Assess differentiation from week 4 onwards via:
- Transepithelial Electrical Resistance (TEER): Measure with volt-ohm meter (>500 Ω·cm² indicates tight junction formation).
- Immunofluorescence: Stain for β-IV-tubulin (ciliated cells), MUC5AC (goblet cells), and KRT5/TP63 (basal cells).
- Periodic Acid-Schiff (PAS) Stain: Histochemical detection of glycoproteins in secretory cells.
Diagrams
The Scientist's Toolkit: Essential Reagents for Airway Epithelium Research
| Reagent / Material | Function / Application |
|---|---|
| PneumaCult-ALI Medium (StemCell Tech) | Defined, serum-free medium optimized for robust differentiation of primary cells into pseudostratified airway epithelium at ALI. |
| Ultroser G Serum Substitute | Chemically defined serum replacement used in BEGM formulations for enhanced growth of primary airway epithelial cells. |
| Human Type IV Collagen | Coating substrate for cultureware to promote attachment and polarization of epithelial cells, mimicking the basement membrane. |
| Y-27632 dihydrochloride (ROCK Inhibitor) | Critical for enhancing survival and cloning efficiency of primary human epithelial cells, especially post-thaw or post-sorting. |
| Recombinant Human FGF-10 & KGF (FGF-7) | Growth factors that promote proliferation and maintenance of basal progenitor cells during expansion phases. |
| All-Trans Retinoic Acid (ATRA) | Essential signaling molecule that drives differentiation towards a ciliated cell fate and inhibits squamous differentiation. |
| DAPT (γ-Secretase Inhibitor) | NOTCH pathway inhibitor used experimentally to skew differentiation towards secretory lineages over ciliated. |
| Cell Recovery Solution (Corning) | For gentle, enzymatic-free detachment of cells or organoids cultured on Matrigel matrix. |
| MucilAir/SmallAir (Epithelix) | Ready-to-use, commercially produced primary human airway epithelial models for standardized screening applications. |
Application Notes
Within viral pathogenicity research, traditional 2D monocultures fail to recapitulate the complex physiology of the human airway. Advanced 3D human airway models, particularly air-liquid interface (ALI) cultures derived from primary cells or induced pluripotent stem cells (iPSCs), provide a transformative platform by emulating three critical in vivo features:
- Mucociliary Clearance: 3D ALI cultures develop a coordinated, beating ciliary apparatus covered by a secreted mucus layer. This active physiological defense mechanism is a primary barrier to inhaled pathogens. Models quantifying ciliary beat frequency (CBF) and mucin composition enable studies on how viruses (e.g., influenza, RSV, SARS-CoV-2) disrupt clearance to establish infection.
- Barrier Function: The models form tight junctions (e.g., ZO-1, occludin) and generate robust transepithelial electrical resistance (TEER), typically ranging from >500 to >2000 Ω·cm². This selective barrier regulates viral entry and paracellular flux, allowing for precise investigation of viral-induced barrier breakdown and the efficacy of therapeutic interventions.
- Relevant Cell Diversity: Unlike single-cell-type models, 3D airway epithelia contain basal cells (progenitors), secretory goblet cells, ciliated columnar cells, and occasionally pulmonary neuroendocrine or club cells. This diversity is critical for studying cell-type-specific viral tropism, host response, and the contribution of rare cell populations to disease progression.
The integration of these features creates a physiologically relevant system for quantifying viral replication kinetics, assessing cytopathic effects, and evaluating antiviral drug and prophylactic efficacy in a human-relevant context.
Table 1: Quantitative Metrics of Key Advantages in 3D Airway Models
| Advantage | Key Measurable Parameters | Typical Values in Mature 3D ALI Models | Relevance to Viral Pathogenicity Studies |
|---|---|---|---|
| Mucociliary Clearance | Ciliary Beat Frequency (CBF) | 5 - 15 Hz | Virus-induced ciliostasis measured via high-speed video microscopy. |
| Mucus Layer Thickness | 5 - 30 µm | Pathogen trapping and penetration assays; mucin (MUC5AC, MUC5B) secretion quantified by ELISA. | |
| Barrier Function | Transepithelial Electrical Resistance (TEER) | 500 - 3000 Ω·cm² | Real-time, non-invasive monitoring of viral-induced barrier disruption. |
| Paracellular Flux (e.g., FITC-Dextran) | Permeability Coefficient (Papp) < 2.0 x 10⁻⁶ cm/s | Quantification of barrier integrity post-infection. | |
| Cell Diversity | Percentage of Ciliated Cells | 30% - 60% (Immunostaining for β-IV Tubulin/Acetylated α-Tubulin) | Identifies target cells for infection (e.g., influenza). |
| Percentage of Goblet Cells | 10% - 30% (Immunostaining for MUC5AC) | Assesses virus-induced mucus hypersecretion and metaplasia. | |
| Presence of Basal Cells | 20% - 40% (Immunostaining for p63/KRT5) | Evaluates progenitor cell impact on epithelial regeneration post-infection. |
Protocols
Protocol 1: Establishing a Primary Human Bronchial Epithelial Cell (HBEC) ALI Culture for Viral Studies
Objective: To differentiate primary HBECs into a pseudostratified, mucociliary epithelium at ALI for viral infection experiments.
Research Reagent Solutions & Materials:
| Item | Function |
|---|---|
| PneumaCult-ALI Medium | A defined, serum-free medium specifically formulated to support mucociliary differentiation at ALI. |
| Corning Transwell inserts | Permeable polyester membrane supports (0.4 µm pore, 6.5 mm or 12 mm diameter) for establishing ALI. |
| Primary HBECs | Isolated from human bronchial tissue, typically passage 2-4, containing the necessary basal progenitor cells. |
| Hydrating Solution (DMEM/F12) | Used to hydrate the apical surface post-seeding without differentiation cues. |
| Dispase II | Enzyme used to recover differentiated cells from the insert membrane for downstream analysis. |
| TEER Voltohmmeter | Device with chopstick electrodes for non-invasive barrier integrity measurement. |
Procedure:
- Seeding: Thaw and expand primary HBECs in expansion medium. Seed cells at a density of 1.0-2.5 x 10⁵ cells per Transwell insert in expansion medium applied to both apical and basolateral chambers.
- Confluence & Initiation of ALI: Once cells reach 100% confluence (typically 2-3 days post-seeding), aspirate the apical medium. Add differentiation medium (e.g., PneumaCult-ALI) only to the basolateral chamber, establishing the ALI. This day is designated as Day 0 of ALI.
- Differentiation & Maintenance: Incubate at 37°C, 5% CO₂. Carefully aspirate any apical mucus accumulation every 48-72 hours. Replace basolateral differentiation medium entirely every 2-3 days.
- Maturation: Cultures typically mature, displaying coordinated ciliary beating and stable TEER, between Days 21-35 post-ALI. Monitor TEER weekly.
- Pre-infection Validation: Prior to viral challenge, confirm maturity by measuring TEER (>500 Ω·cm²) and observing ciliary motion via light microscopy.
Protocol 2: Quantifying Viral-Induced Barrier Dysfunction via TEER and Permeability
Objective: To monitor and quantify the disruption of airway epithelial barrier integrity following viral infection.
Procedure:
- Baseline Measurement: For mature ALI cultures, measure and record the baseline TEER using a voltohmmeter.
- Viral Inoculation: Dilute virus stock in infection medium (e.g., basolateral ALI medium without supplements). Gently wash the apical surface with warm PBS. Apply the viral inoculum (e.g., 50-100 µL for a 6.5 mm insert) to the apical surface. Incubate at 37°C for the desired adsorption period (e.g., 2 hours).
- Post-Inoculation: Aspirate the inoculum and wash the apical surface with PBS to remove unbound virus. Return cultures to ALI conditions.
- Longitudinal TEER Monitoring: Measure TEER at 24, 48, 72, and 96 hours post-infection (hpi). Express data as a percentage of the baseline (uninfected control) TEER.
- Paracellular Permeability Assay (Endpoint): At a selected timepoint (e.g., 72 hpi), prepare a solution of fluorescent tracer (e.g., 100 µg/mL FITC-dextran, 4 kDa) in PBS. Add the tracer to the apical chamber. After 1-4 hours incubation at 37°C, collect 100 µL from the basolateral chamber.
- Quantification: Measure the fluorescence in the basolateral sample (ex/em: 492/518 nm). Calculate the apparent permeability coefficient (Papp) using the formula:
Papp (cm/s) = (dQ/dt) / (A * C₀), where dQ/dt is the flux rate, A is the membrane surface area, and C₀ is the initial apical tracer concentration.
Protocol 3: Immunofluorescence Analysis of Cell Diversity and Viral Antigens
Objective: To visualize cell-type composition and viral tropism within the 3D epithelium.
Procedure:
- Fixation: At the desired timepoint, wash inserts with PBS. Fix cells with 4% paraformaldehyde (apical and basolateral) for 20 min at room temperature.
- Processing: Permeabilize and block with a solution of 0.3% Triton X-100 and 5% normal serum in PBS for 1 hour.
- Staining: Incubate with primary antibodies diluted in blocking solution overnight at 4°C. Use cocktails to identify:
- Cell Diversity: Anti-β-IV Tubulin (ciliated cells), Anti-MUC5AC (goblet cells), Anti-p63 (basal cells).
- Viral Antigens: Virus-specific antibody (e.g., anti-Influenza NP, anti-SARS-CoV-2 nucleocapsid).
- Tight Junctions: Anti-ZO-1.
- Visualization: Wash and incubate with appropriate fluorophore-conjugated secondary antibodies and nuclear stain (e.g., DAPI) for 1-2 hours at RT.
- Imaging: Excise the membrane from the insert and mount on a slide. Acquire Z-stack images using a confocal microscope to capture the 3D structure.
Visualizations
Title: Workflow for Differentiating a 3D Airway Model at ALI
Title: Viral Pathogenesis Disrupts Airway Barrier Pathways
Application Notes
The 3D human airway epithelial (HAE) model, derived from primary cells cultured at an air-liquid interface (ALI), represents a transformative tool for studying respiratory virus pathogenicity. These models accurately recapitulate the pseudostratified epithelium, mucociliary clearance, and innate immune functions of the human proximal airway, overcoming critical limitations of immortalized cell lines. Within the context of a thesis on 3D airway models for viral studies, these systems enable the integrated analysis of the entire viral life cycle and host response in a physiologically relevant environment. Key applications include quantifying viral entry through specific receptors (e.g., ACE2 for SARS-CoV-2), tracking replication kinetics, assessing cytopathogenesis (cilia beating dysfunction, barrier integrity loss, cell death), and profiling the innate immune response (pattern recognition receptor signaling, interferon-stimulated gene induction, cytokine/chemokine secretion). These models are indispensable for evaluating the efficacy of novel antiviral drugs and neutralizing antibodies, and for investigating the pathogenic mechanisms of emerging virus variants.
Table 1: Comparative Viral Kinetics in 3D HAE Models
| Virus | Primary Receptor | Time to Peak Titer (Hours Post-Inoculation) | Peak Titer (Log10 PFU/mL or TCID50/mL) | Major Cytopathic Effect(s) |
|---|---|---|---|---|
| SARS-CoV-2 (ancestral) | ACE2 | 48-72 | 6.0 - 7.5 | Cilia loss, epithelial thinning, sloughing |
| Influenza A/H1N1 (pdm09) | α2,6-linked sialic acid | 24-48 | 5.5 - 7.0 | Club cell hypertrophy, deciliation |
| Respiratory Syncytial Virus (RSV) | Heparan sulfate / nucleolin | 72-96 | 4.5 - 5.5 | Syncytia formation, mucus hypersecretion |
| Human Rhinovirus-16 (HRV-16) | ICAM-1 | 48-72 | 4.0 - 5.0 | Minimal cytopathology |
Table 2: Innate Immune Response Profiles in Infected 3D HAE Models
| Immune Parameter | SARS-CoV-2 | Influenza A | RSV | Assay Method |
|---|---|---|---|---|
| IFN-λ1 (pg/mL) | 150-500 (delayed) | 1000-3000 (robust) | 500-1500 | ELISA (Apical wash) |
| CXCL10/IP-10 (pg/mL) | 2000-8000 | 1000-4000 | 500-2000 | Multiplex Luminex |
| ISG15 mRNA Fold-Change | 10-50x | 100-500x | 50-200x | qRT-PCR |
| MxA Protein Expression | Moderate | High | Moderate | Immunofluorescence |
Experimental Protocols
Protocol 1: Viral Infection and Replication Kinetics in 3D HAE Models
Objective: To quantify viral entry, replication kinetics, and progeny virus release from 3D HAE models.
Materials:
- Differentiated 3D HAE cultures (e.g., Epiairway, MucilAir, or in-house ALI cultures, ≥4 weeks old).
- Virus stock of known titer.
- Infection medium (e.g., Dulbecco’s Modified Eagle Medium (DMEM) without serum).
- Phosphate-Buffered Saline (PBS), pre-warmed.
- Cell scraper.
- Apical wash collection apparatus.
Method:
- Apical Wash & Pre-inoculation: Aspirate the basolateral medium and replace with fresh. Gently wash the apical surface with 200 µL of pre-warmed PBS to remove accumulated mucus. Collect and retain as the "0-hour" apical wash sample.
- Viral Inoculation: Apply 100 µL of virus inoculum (diluted in infection medium to desired MOI or dose, typically 0.1-1.0 MOI based on cell count) directly to the apical surface. Incubate at 37°C, 5% CO2 for 2 hours to allow viral entry.
- Post-Inoculation Wash: Carefully remove the apical inoculum and wash the apical surface 3 times with 200 µL of PBS to remove unbound virus. Pool these washes as the "Input/Unbound" sample.
- Maintenance & Sample Collection: Return cultures to the incubator. At designated time points (e.g., 2, 24, 48, 72, 96 hours post-inoculation - hpi):
- Collect apical washes by adding 200 µL of PBS to the apical surface, incubating for 10 minutes at 37°C, and then carefully aspirating.
- Replace the basolateral medium and retain the old medium as the "basolateral" sample for that time point.
- Harvesting Whole Lysates (Terminal): At selected terminal time points, wash apical and basolateral surfaces with PBS. Lyse the entire epithelial layer using 350 µL of RLT buffer (with β-mercaptoethanol) and a cell scraper. Store lysates at -80°C for subsequent RNA extraction.
- Titration: Determine viral titers in apical wash and basolateral medium samples by plaque assay (PFU/mL) or TCID50 assay on permissive cell lines (e.g., Vero E6 for SARS-CoV-2, MDCK for influenza).
Protocol 2: Profiling the Innate Immune Response via qRT-PCR
Objective: To quantify the expression of interferon-stimulated genes (ISGs) and cytokines in infected 3D HAE models.
Materials:
- RNA lysates from Protocol 1, Step 5.
- RNA extraction kit (e.g., RNeasy Micro Kit, Qiagen).
- DNase I treatment kit.
- cDNA synthesis kit (e.g., High-Capacity cDNA Reverse Transcription Kit, Applied Biosystems).
- TaqMan or SYBR Green qPCR master mix.
- Primers/probes for target genes (e.g., ISG15, MxA, IFIT1, IFN-λ1, CXCL10, GAPDH).
Method:
- RNA Extraction: Extract total RNA from RLT lysates according to the manufacturer's protocol, including an on-column DNase I digestion step. Quantify RNA concentration and purity (A260/A280 ~2.0).
- cDNA Synthesis: Reverse transcribe 500 ng - 1 µg of total RNA into cDNA in a 20 µL reaction.
- Quantitative PCR: Perform qPCR in triplicate using 1-2 µL of diluted cDNA per reaction. Use a standard two-step cycling protocol.
- Housekeeping Genes: GAPDH, β-actin, RPLP0.
- Target Genes: Select a panel relevant to antiviral defense.
- Data Analysis: Calculate the ΔΔCt values relative to mock-infected controls and housekeeping genes. Present data as fold-change in gene expression.
Protocol 3: Assessment of Epithelial Barrier Integrity (TEER & FITC-Dextran Permeability)
Objective: To quantitatively measure virus-induced disruption of epithelial barrier function.
Materials:
- Epithelial voltohmmeter (EVOM) with STX2 chopstick electrodes.
- Fluorescein isothiocyanate (FITC)-labeled dextran (4 kDa), 1 mg/mL in PBS.
- Fluorescence plate reader.
Method:
- Transepithelial Electrical Resistance (TEER):
- Pre-warm PBS and basolateral medium to 37°C.
- Gently wash the apical surface with PBS.
- Add fresh PBS to the apical compartment and medium to the basolateral compartment.
- Sterilize electrodes in 70% ethanol, then rinse in PBS. Insert electrodes into apical and basolateral compartments. Record the resistance (Ω).
- Calculate TEER (Ω·cm²) by subtracting the resistance of a blank insert and multiplying by the membrane surface area. Monitor at 24-hour intervals post-infection.
- FITC-Dextran Paracellular Permeability Assay:
- At the desired time point, prepare FITC-dextran solution.
- Remove apical PBS and add 100 µL of FITC-dextran solution to the apical surface.
- Incubate at 37°C for 2 hours.
- Collect 100 µL from the basolateral compartment. Measure fluorescence (excitation 485 nm, emission 535 nm).
- Calculate the percentage of FITC-dextran that translocated to the basolateral side compared to a standard curve. Higher fluorescence indicates loss of barrier integrity.
Visualizations
Viral Study Workflow in 3D HAE Models
Innate Immune Signaling in Infected Airway Cells
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for 3D HAE Viral Pathogenesis Studies
| Reagent / Material | Primary Function & Application | Example Product / Vendor |
|---|---|---|
| Differentiated 3D HAE Model | Provides physiologically relevant human airway epithelium for infection studies. Can be commercially sourced or cultured in-house from primary cells. | Epiairway (MatTek), MucilAir (Epithelix), PREDICT96-ALI (ATCC). |
| ALI Culture Medium | Specialized medium optimized for long-term maintenance of mucociliary differentiation and barrier function at the air-liquid interface. | PneumaCult-ALI (StemCell Tech), proprietary media from model vendors. |
| Transepithelial Electrical Resistance (TEER) Meter | Quantifies the integrity of the epithelial barrier by measuring electrical resistance across the cell layer. A decrease indicates pathogen-induced damage. | EVOM3 with STX2 electrodes (World Precision Instruments). |
| qRT-PCR Assays for ISGs/Cytokines | Quantifies host gene expression changes in response to viral infection (e.g., IFNs, ISG15, MxA, CXCL10). Critical for profiling innate immune response. | TaqMan Gene Expression Assays (Thermo Fisher), PrimePCR panels (Bio-Rad). |
| Multiplex Cytokine Assay Kits | Simultaneously measures the concentration of multiple pro-inflammatory cytokines and chemokines secreted apically or basolaterally. | Luminex Discovery Assays (R&D Systems), LEGENDplex (BioLegend). |
| Fluorescent Conjugates for Permeability | Assesses paracellular barrier integrity by measuring the flux of a fluorescently labeled molecule (e.g., 4 kDa FITC-dextran) across the epithelium. | FITC-Dextran, 4 kDa (Sigma-Aldrich). |
| Cell Fixation for Imaging | Preserves cellular architecture and antigenicity for subsequent histological analysis (e.g., immunofluorescence for viral antigens, tight junctions). | 4% Paraformaldehyde (PFA) in PBS. |
| RNAlater Stabilization Solution | Stabilizes and protects cellular RNA in intact tissues/cells at the moment of harvest, preventing degradation prior to extraction. | RNAlater (Thermo Fisher). |
Within the broader objective of establishing a robust 3D human airway model for viral pathogenicity studies, the selection of the cellular starting material is a foundational and critical decision. This application note provides a detailed comparison between primary human bronchial/tracheal epithelial cells (HBECs/HTECs) and induced pluripotent stem cell (iPSC)-derived airway epithelial cells, including protocols and key considerations for researchers.
Table 1: Quantitative and Qualitative Comparison of Starting Materials
| Parameter | Primary HBECs/HTECs | iPSC-Derived Airway Cells |
|---|---|---|
| Physiological Relevance | High; directly isolated from human tissue. | Moderate to High; depends on differentiation protocol efficiency. |
| Donor-to-Donor Variability | Inherent; reflects human genetic diversity. | Can be minimized using master cell lines; allows isogenic control generation. |
| Proliferative Capacity | Limited (5-10 passages). | Essentially unlimited. |
| Time to 3D Model | ~4-6 weeks for full differentiation at air-liquid interface (ALI). | ~8-12+ weeks (includes reprogramming, expansion, and differentiation). |
| Cost per Experiment | High (recurring cost for cell isolation/purchase). | Lower long-term cost after initial iPSC line establishment. |
| Genetic Manipulation Potential | Low; difficult to transfert and clone. | High; amenable to CRISPR/Cas9 editing at pluripotent stage. |
| Availability & Sourcing | Dependent on tissue donors; commercial sources available. | Unlimited from established lines; patient-specific lines possible. |
| Key Best Application | Studies requiring immediate, high-fidelity human biology. | Large-scale studies, genetic disease modeling, and high-throughput screening. |
Experimental Protocols
Protocol 1: Expansion and Differentiation of Primary HBECs for 3D ALI Culture
Objective: To cultivate and differentiate primary HBECs into a pseudostratified, mucociliary epithelium at the air-liquid interface.
Materials:
- PneumaCult-Ex Plus Medium (STEMCELL Technologies) or similar.
- PneumaCult-ALI Medium (STEMCELL Technologies).
- Collagen IV-coated transwell inserts (e.g., Corning, 0.4 µm pore, 6.5 mm or 24 mm).
- Dispase solution (for cell sheet harvest).
- DMEM/F-12 basal medium.
Method:
- Thawing & Expansion: Thaw cryopreserved primary HBECs rapidly at 37°C. Seed cells at 1-3 x 10⁴ cells/cm² in a tissue culture flask pre-coated with collagen IV in expansion medium. Change medium every 48 hours.
- Transwell Seeding: Once ~80% confluent, dissociate cells with TrypLE. Seed cells onto collagen IV-coated transwell inserts at a density of 1-2 x 10⁵ cells/cm² in expansion medium. Feed from both apical and basolateral sides.
- Air-Liquid Interface Induction: Upon reaching 100% confluence (typically 2-4 days post-seeding), remove apical medium and feed cells only from the basolateral compartment with ALI differentiation medium.
- ALI Culture Maintenance: Maintain cultures at the ALI for 4-6 weeks, changing the basolateral medium every 48-72 hours. Monitor transepithelial electrical resistance (TEER) weekly.
- Characterization: Assess differentiation at week 4-6 via immunocytochemistry (Acetylated α-Tubulin for cilia, MUC5AC for goblet cells), histology (H&E for stratification), and TEER measurement (>500 Ω·cm²).
Protocol 2: Directed Differentiation of Human iPSCs to Airway Epithelial Cells
Objective: To generate basal-like airway epithelial cells from iPSCs via definitive endoderm and anterior foregut endoderm intermediates for ALI culture.
Materials:
- mTeSR1 or equivalent iPSC maintenance medium.
- RPMI 1640, B-27 Supplement (minus insulin).
- Recombinant human proteins: Activin A, CHIR99021, Noggin, KGF (FGF7), FGF2, Retinoic Acid.
- DMEM/F-12 with HEPES for basal cell expansion.
Method:
- Definitive Endoderm (DE) Induction (Days 1-3): Differentiate confluent iPSCs in monolayers using 100 ng/mL Activin A and 3 µM CHIR99021 in RPMI/B-27 minus insulin for 24h, followed by 48h with Activin A alone. Confirm SOX17/FOXA2 expression via flow cytometry (>80% efficiency target).
- Anterior Foregut Endoderm (AFE) Induction (Days 4-6): Treat DE cells with 10 µM SB431542 (TGF-β inhibitor) and 200 ng/mL Noggin in DMEM/F-12/B-27 for 72 hours to pattern towards AFE (NKX2.1+).
- Lung Progenitor Specification (Days 7-20): Pattern AFE cells towards lung lineage using 10 ng/mL FGF2, 10 ng/mL BMP4, and 10 µM CHIR99021 for 48h, then 10 ng/mL KGF and 10 nM Retinoic Acid for 10-14 days. Expand in KGF (50 ng/mL) and FGF2 (10 ng/mL) for another week.
- Airway Epithelial Maturation & ALI: Dissociate lung progenitor spheres and seed onto transwell inserts at high density in "PneumaCult-ALI" or specialized medium containing Notch pathway inhibitors (e.g., DAPT) to promote basal cell fate (TP63+). Switch to ALI conditions as in Protocol 1 for 6-8 weeks to achieve mucociliary differentiation.
Signaling Pathways and Workflows
Diagram 1: Cell Source Differentiation Paths
Diagram 2: Decision Logic for Cell Selection
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for 3D Airway Model Development
| Reagent/Material | Supplier Examples | Function in Protocol |
|---|---|---|
| PneumaCult-ALI Medium | STEMCELL Technologies | Supports differentiation and long-term maintenance of primary cells at ALI. Contains factors for mucociliary differentiation. |
| Air-Liquid Interface (ALI) Inserts | Corning, Millipore | Permeable membrane supports allowing apical air exposure and basolateral media feeding. Crucial for polarization. |
| Collagen IV, Human | Sigma-Aldrich, Corning | Extracellular matrix coating for cell attachment and expansion, mimicking the basement membrane. |
| Recombinant Human KGF (FGF7) | PeproTech, R&D Systems | Key growth factor for promoting proliferation and differentiation of airway basal cells. |
| Y-27632 (ROCK Inhibitor) | Tocris Bioscience | Enhances survival of dissociated primary and iPSC-derived cells during seeding (anoikis inhibition). |
| Cell Recovery Solution | Corning | For gentle dissociation of cells from Matrigel during iPSC differentiation steps. |
| TEER Voltohmmeter | World Precision Instruments | Measures transepithelial electrical resistance to quantify barrier integrity non-invasively. |
| DAPT (γ-Secretase Inhibitor) | Cayman Chemical | Notch pathway inhibitor used in iPSC protocols to promote basal cell fate over secretory. |
Step-by-Step Protocol: Building and Infecting Your 3D Airway Model at the Air-Liquid Interface
Within the context of developing robust 3D human airway models for viral pathogenicity studies, the generation of a fully differentiated, mucociliary epithelium is paramount. This protocol provides a comprehensive overview, from the resuscitation of cryopreserved primary human bronchial epithelial cells (HBECs) to the establishment of an air-liquid interface (ALI) culture that recapitulates the in vivo airway epithelium. Such models are critical for investigating virus-host interactions, tropism, and the evaluation of novel antiviral therapeutics.
Key Research Reagent Solutions
Table 1: Essential Materials and Reagents
| Reagent/Material | Function | Example Product/Catalog |
|---|---|---|
| Primary Human Bronchial Epithelial Cells (HBECs) | The foundational cell type for generating physiologically relevant airway epithelia. | Lonza CC-2540S, ATCC PCS-300-010 |
| Air-Liquid Interface (ALI) Media | Biphasic medium system supporting basal proliferation and apical differentiation. | PneumaCult-ALI (StemCell Tech, 05001), BronchiaLife ALI (Lifeline Cell Tech, LL-0023) |
| Transwell Permeable Supports | Porous membrane inserts enabling the establishment of the ALI and epithelial polarization. | Corning Costar (e.g., 3460, 0.4 µm pore, 6.5 mm diameter) |
| Cell Recovery Solution (DMSO-Free) | Thaws cryopreserved cells while minimizing osmotic stress and DMSO cytotoxicity. | STEMCELL Technologies, 100-0736 |
| Dispase II Solution | Proteolytic enzyme for detaching differentiated epithelia as intact sheets for analysis. | Sigma-Aldrich, D4693 |
| Mucociliary Differentiation Supplements | Typically includes retinoic acid, growth factors (e.g., EGF, FGF), and hormones to drive ciliogenesis and goblet cell differentiation. | Included in commercial ALI media kits. |
Detailed Protocol
Phase 1: Cell Thawing and Expansion
- Thawing: Rapidly thaw a cryovial of primary HBECs in a 37°C water bath. Immediately transfer cells into a tube pre-filled with 9 mL of pre-warmed, complete expansion medium.
- Centrifugation: Spin at 300 x g for 5 minutes. Aspirate supernatant.
- Resuspension & Seeding: Resuspend cell pellet in expansion medium. Seed cells into a collagen I-coated T-75 flask at a density of 2,500 – 3,000 cells/cm².
- Expansion Culture: Incubate at 37°C, 5% CO₂. Change medium every 48 hours until cells are 80-90% confluent (typically 5-7 days). Passage using trypsin/EDTA.
Table 2: Cell Seeding Quantitative Benchmarks
| Stage | Vessel | Seeding Density | Medium Volume | Time to Confluence |
|---|---|---|---|---|
| Post-Thaw Expansion | T-75 Flask | 2,500 – 3,000 cells/cm² | 15 mL | 5 – 7 days |
| ALI Seeding | 6.5 mm Transwell | 3.0 – 5.0 x 10⁴ cells/insert | 200 µL (apical), 500 µL (basolateral) | 2 – 3 days |
Phase 2: Air-Liquid Interface (ALI) Establishment and Differentiation
- Transwell Seeding: Trypsinize expanded HBECs. Count and resuspend in expansion medium. Plate 3.0-5.0 x 10⁴ cells per 6.5 mm Transwell insert. Add 200 µL medium to the apical chamber and 500 µL to the basolateral chamber.
- Basal Proliferation: Culture submerged for 2-3 days, changing medium daily, until 100% confluent.
- ALI Induction: On the day of confluence, aspirate apical medium completely. Feed basolateral chamber with 500 µL of pre-warmed ALI differentiation medium. This creates the air-liquid interface.
- Differentiation Maintenance: Feed cultures exclusively from the basolateral compartment with ALI medium every 48-72 hours for 21-35 days. Apical surfaces are gently washed with PBS every 7-10 days to remove accumulated mucus.
Phase 3: Quality Control and Validation
A successfully differentiated epithelium is validated by:
- Transepithelial Electrical Resistance (TEER): Measurements >600 Ω·cm² indicate tight junction formation.
- Histology (H&E): Visual confirmation of a pseudostratified epithelium.
- Immunofluorescence: Staining for acetylated α-tubulin (cilia), MUC5AC (goblet cells), and ZO-1 (tight junctions).
- Functional Assay: Measurement of mucociliary clearance or cytokine secretion in response to stimuli.
Signaling Pathways in Mucociliary Differentiation
Key Signaling Pathways in Airway Cell Fate
Experimental Workflow for Model Generation
Workflow: From Thawed Cells to Differentiated Airway Model
Application Notes
The development of physiologically relevant 3D human airway models for viral pathogenicity studies relies on a precise combination of critical materials. These in vitro systems, typically cultured at the air-liquid interface (ALI), aim to recapitulate the pseudostratified mucociliary epithelium of the human bronchus. Their accuracy is contingent upon the optimized formulation of culture media, the inclusion of specific biological supplements, and the use of permeable Transwell inserts that enable proper cellular differentiation and polarization. The following notes detail the application of these core components.
Culture Media: A dual-phase media system is employed. A proliferation phase utilizes submersion culture with a rich basal medium (e.g., DMEM/F-12) supplemented with growth factors (EGF, insulin, transferrin) and antibiotics to expand primary human bronchial epithelial cells (HBECs). The differentiation phase switches to an ALI format using a specialized, serum-free medium (e.g., PneumaCult-ALI or BEGM/DMEM-based mixtures) that withdraws proliferative signals and provides cues for mucociliary differentiation, often involving corticosteroids like hydrocortisone and retinoids.
Critical Supplements: Key supplements dictate cell fate and function. Retinoic acid is indispensable for the development of ciliated cells. Growth factor cocktails (e.g., BPE, EGF) are carefully titrated. In models incorporating fibroblasts or immune cells, additional tailored media are required. The choice of supplements directly impacts the model's susceptibility to viral infection and its inflammatory response profile.
Transwell Inserts: The porous membrane of Transwell inserts (typically 0.4 µm or 1.0 µm pore size, polyester or collagen-coated) provides the structural and functional foundation. It allows for basolateral media feeding, establishes the critical ALI, and enables the formation of tight junctions and epithelial polarity. The insert's pore size and coating influence cell attachment, barrier function (measured by Trans Epithelial Electrical Resistance - TEER), and the ability of viruses to access the basolateral side.
Key Research Reagent Solutions
| Reagent / Material | Primary Function in 3D Airway Model |
|---|---|
| PneumaCult-ALI Medium | A commercially optimized, serum-free medium specifically formulated for the differentiation and long-term maintenance of primary human airway epithelial cells at ALI. Promotes formation of ciliated and goblet cells. |
| DMEM/Ham's F-12 Basal Mix | A common basal medium for custom ALI media formulations. Provides essential nutrients, vitamins, and salts. Often supplemented with the "BEGM" singlequots kit or similar components. |
| Retinoic Acid (All-trans) | A critical differentiation supplement. Drives the development of ciliated cell phenotypes. Typically used at low concentrations (e.g., 10-50 nM) in the differentiation medium. |
| Hydrocortisone | A glucocorticoid used in both proliferation and differentiation media. Enhances epithelial barrier function and cell survival. |
| Collagen IV-Coated Transwell Inserts | Porous membrane inserts (6.5 mm, 24-well format common) pre-coated with collagen IV to enhance attachment and growth of primary HBECs. The 0.4 µm pore size is standard for ALI culture. |
| Primary Human Bronchial/Tracheal Epithelial Cells (HBECs) | The core cellular component. Donor-derived cells retaining in vivo characteristics. Cultured from passage 2-4 for optimal differentiation capacity at ALI. |
| Phosphate-Buffered Saline (PBS) + 0.5 mM EDTA | Used for the gentle dissociation of cells during subculture or for apical washes to collect secreted mucus and released viruses for analysis. |
Table 1: Comparison of Common ALI Media Formulations for HBEC Differentiation
| Medium Formulation | Key Components | Typical Ciliation (% of apical surface) | Typical TEER Range (Ω·cm²) | Time to Full Differentiation |
|---|---|---|---|---|
| PneumaCult-ALI | Proprietary, serum-free, includes hydrocortisone, heparin, BSA | 40-60% | 600-1200 | 28-35 days |
| Custom BEGM/DMEM | DMEM/F-12 + BPE + EGF + Insulin + Transferrin + RA + Hydrocortisone + etc. | 30-50% | 400-800 | 28-42 days |
| ULTRACULTURE + Supplements | Ultraceulture base + RA + Hydrocortisone + Growth Factors | 25-45% | 300-700 | 35-45 days |
Table 2: Transwell Insert Specifications for ALI Culture
| Parameter | Specification | Impact on Model |
|---|---|---|
| Membrane Material | Polyester (PET) or Polycarbonate (PC) | PET offers better clarity for imaging; coating adhesion varies. |
| Pore Size | 0.4 µm, 1.0 µm, 3.0 µm | 0.4 µm standard, prevents fibroblast migration in co-culture; 3.0 µm allows immune cell migration. |
| Surface Coating | Collagen I, Collagen IV, Matrigel, Uncoated | Collagen IV most common for HBECs; enhances polarization and barrier integrity. |
| Insert Size (Typical) | 6.5 mm, 12 mm, 24 mm diameter | 6.5 mm (24-well plate) conserves precious primary cells; 24 mm allows more material for analysis. |
Detailed Experimental Protocols
Protocol 1: Establishing a 3D Human Airway Model at ALI
Objective: To differentiate primary HBECs into a pseudostratified, mucociliary epithelium on Transwell inserts for viral infection studies.
Materials:
- Primary HBECs (P2-P4)
- Proliferation Medium (e.g., PneumaCult-Ex Plus or BEGM)
- ALI Differentiation Medium (e.g., PneumaCult-ALI)
- Collagen IV-coated Transwell inserts (0.4 µm pore, 6.5 mm)
- 24-well culture plates
- PBS, Trypsin/EDTA
Procedure:
- Cell Expansion: Culture HBECs in T-flasks with proliferation medium until ~80% confluent. Passage using trypsin/EDTA.
- Seeding: Resuspend HBECs in proliferation medium. Seed onto the apical side of collagen-coated Transwell inserts at a high density (e.g., 2.5-5.0 x 10⁴ cells per 6.5 mm insert). Add 500 µL of proliferation medium to the basolateral chamber and 150 µL to the apical chamber.
- Submersion Growth: Culture submerged for 5-7 days, changing the medium in both chambers every 48 hours, until 100% confluent.
- Air-Liquid Interface Initiation: Aspirate apical medium completely. Feed cells only from the basolateral side with 500 µL of pre-warmed ALI Differentiation Medium. This is designated as Day 0 of ALI.
- Differentiation & Maintenance: Feed cells basolaterally with fresh ALI medium every 48 hours. Gently wash the apical surface with 100 µL of PBS every 7 days to remove excess mucus.
- Maturation: Culture at ALI for a minimum of 28 days. Monitor TEER weekly (plate values once stable >500 Ω·cm²). The model is ready for infection when a well-differentiated layer with beating cilia (observed via phase-contrast microscopy) is established.
Protocol 2: Viral Pathogenicity Infection Assay on Mature ALI Cultures
Objective: To inoculate the differentiated airway model with a respiratory virus (e.g., Influenza A, SARS-CoV-2) and quantify infectivity and host response.
Materials:
- Mature ALI cultures (≥Day 28)
- Virus stock (titered)
- Infection Diluent (e.g., serum-free DMEM or PBS++ with Ca²⁺/Mg²⁺)
- Apical wash collection tubes
- Cell lysis buffer (for qPCR/immunoblot)
Procedure:
- Pre-inoculation Wash: Gently wash the apical surface of each insert with 100 µL of warm PBS to remove accumulated mucus. Aspirate.
- Virus Inoculation: Dilute virus stock in infection diluent to desired MOI (e.g., 0.1-5.0 for influenza). Apply 50-100 µL of inoculum directly to the apical surface. Ensure even coverage.
- Adsorption: Incubate inserts at 37°C, 5% CO₂ for 1-2 hours. Tilt plate gently every 15 minutes to redistribute inoculum.
- Post-inoculation Wash: Aspirate inoculum. Gently wash apical surface 2-3 times with 100 µL PBS to remove unbound virus. Aspirate completely.
- Post-infection Incubation: Return inserts to ALI conditions. Continue feeding basolaterally with ALI medium.
- Sample Collection:
- Apical Virus Shedding: At defined timepoints (e.g., 24, 48, 72h post-infection), add 100 µL of diluent to the apical surface, incubate 10 min, pipette mix, and collect for plaque assay or qPCR.
- Host Response: Collect basolateral medium for cytokine analysis (ELISA). For cell-associated analysis, wash inserts, lyse cells directly on membrane for RNA/protein extraction.
- Endpoint Analysis: Fix inserts for immunohistochemistry (e.g., viral antigen, cleaved caspase-3) or process for TEM to examine ultrastructural changes.
Visualizations
Diagram 1 Title: Workflow for 3D Airway Model Differentiation and Viral Infection
Diagram 2 Title: Key Supplement Signaling in Airway Differentiation
Within the broader thesis on developing a standardized 3D human airway model protocol for viral pathogenicity studies, establishing a robust, reproducible timeline for cellular seeding, expansion, and Air-Liquid Interface (ALI) induction is critical. This protocol outlines the key morphological and functional checkpoints necessary to generate physiologically relevant pseudostratified, mucociliary differentiated epithelial cultures suitable for modeling host-pathogen interactions.
The following table summarizes the core timeline, critical actions, and target morphological outcomes.
Table 1: Primary Human Airway Epithelial Cell (hAEC) Culture Timeline and Checkpoints
| Phase | Day Range | Key Action/Checkpoint | Target Quantitative Metric | Purpose in Viral Studies |
|---|---|---|---|---|
| Seeding & Attachment | Day 0 | Seeding of P0-P2 hAECs on transwells | 2.5-3.5 x 10^5 cells/cm² | Ensure confluent monolayer foundation |
| Day 1-2 | Media change; confirm attachment | >95% confluent monolayer | Remove non-adherent cells; confirm establishment | |
| Proliferative Expansion | Day 2-7 | Submerged culture in expansion media | TEER > 300 Ω·cm² | Promote proliferation and tight junction formation |
| Day ~7 | Pre-ALI confluency check | 100% visual confluency, cuboidal morphology | Ready for differentiation cue | |
| ALI Induction & Differentiation | Day 0 (ALI) | Apical media removal (ALI induction) | N/A | Initiate differentiation |
| Week 1-2 (ALI) | Basal media switch to differentiation media | Emergence of cilia (beating observed) | Promote ciliogenesis | |
| Week 2-4 (ALI) | Mucin production & stratification | TEER > 600 Ω·cm²; goblet cells visible (≥15% by PAS stain) | Functional mucociliary barrier | |
| Week 4+ (ALI) | Fully Differentiated Model | CBF: 5-15 Hz; mucus layer present; pseudostratified morphology | Ready for viral challenge studies |
Detailed Protocols
Protocol: Seeding and Initial Expansion of Primary hAECs
Objective: To establish a confluent, proliferative monolayer on collagen-IV coated transwell inserts. Materials: See Scientist's Toolkit (Section 5). Procedure:
- Pre-coating: Apply 300 µL of collagen-IV solution (30 µg/mL in PBS) to the apical side of a 6.5 mm transwell insert (0.4 µm pore). Incubate for 2 hours at 37°C. Aspirate and wash once with PBS.
- Cell Preparation: Thaw a cryovial of primary human bronchial epithelial cells (P0-P2) rapidly at 37°C. Resuspend in 10 mL of pre-warmed Expansion Medium (e.g., PneumaCult-Ex Plus). Centrifuge at 300 x g for 5 min. Resuspend pellet in fresh medium and count.
- Seeding: Adjust cell density to 2.5-3.5 x 10^5 cells/cm². Add 100 µL of cell suspension to the apical chamber of the coated insert. Add 500 µL of Expansion Medium to the basal chamber.
- Initial Culture (Day 1-3): Place plate in a 37°C, 5% CO₂ incubator. After 24 hours, carefully aspirate apical medium, leaving the submerged basal medium. Replace basal medium every 48 hours.
- Checkpoint (Day 3-4): Confirm >95% confluency via light microscopy. Cells should exhibit a uniform, cobblestone epithelial morphology.
Protocol: Air-Liquid Interface (ALI) Induction and Differentiation
Objective: To induce differentiation into a pseudostratified, mucociliary epithelium. Procedure:
- Pre-ALI Check (Day ~7): Verify complete confluence and a transepithelial electrical resistance (TEER) > 300 Ω·cm².
- ALI Induction (Day 0): Carefully aspirate the apical medium. Add 500 µL of fresh Differentiation Medium (e.g., PneumaCult-ALI) to the basal chamber only, ensuring the apical surface is exposed to air.
- Differentiation Phase:
- Replace basal Differentiation Medium every 48-72 hours.
- Gently wash the apical surface with 200 µL of PBS every 7 days to remove excess mucus.
- Weekly Checkpoints:
- Week 2 (ALI): Observe developing cilia via phase-contrast microscopy (200-400x). Beating should become apparent.
- Week 3-4 (ALI): Measure TEER (should stabilize or peak >600 Ω·cm²). Assess mucin production via periodic acid-Schiff (PAS) staining of fixed inserts.
- Week 4+ (ALI): The model is mature. Quantify ciliary beat frequency (CBF) and mucus thickness if required for study validation.
Signaling Pathways and Workflow Diagrams
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for hAEC ALI Culture
| Item | Function in Protocol | Example Product/Component |
|---|---|---|
| Primary Human Airway Cells | Source of basal stem/progenitor cells for culture. | Lonza CC-2540S, Epithelix MucilAir donors |
| Collagen IV | Extracellular matrix coating to enhance cell attachment and polarization. | Corning Collagen IV (from human placenta) |
| Airway Epithelial Expansion Medium | A specialized, low-Ca²⁺ medium containing growth factors (e.g., FGF, EGF) to promote proliferation while inhibiting premature differentiation. | STEMCELL PneumaCult-Ex Plus, PromoCell Airway Epithelial Cell Growth Medium |
| ALI Differentiation Medium | A growth factor-defined, serum-free medium that induces and sustains mucociliary differentiation upon ALI establishment. Typically contains retinoic acid. | STEMCELL PneumaCult-ALI, ALI-SFM (Thermo Fisher) |
| Transwell Inserts | Permeable supports allowing independent access to apical and basal compartments, essential for ALI culture. | Corning Costar polyester, 0.4 µm pore, 6.5 mm diameter |
| Transepithelial Electrical Resistance (TEER) Meter | To quantitatively monitor tight junction formation and barrier integrity during expansion and differentiation. | EVOM3 with chopstick electrode (World Precision Instruments) |
| Ciliary Beat Frequency (CBF) Analysis System | To validate functional ciliogenesis; can use high-speed video microscopy with analysis software. | Sisson-Ammons Video Analysis (SAVA) system |
| Mucin Staining Kit | To identify and quantify goblet cell differentiation and mucin production. | Periodic Acid-Schiff (PAS) Staining Kit (Abcam) |
Within the broader thesis on developing standardized 3D human airway model protocols for viral pathogenicity studies, robust monitoring of cellular differentiation is paramount. The establishment of a functional mucociliary phenotype, characterized by active ciliogenesis and mucus production, alongside the development of robust transepithelial electrical resistance (TEER), serves as the primary benchmark for model validity. These metrics directly determine the physiological relevance of the model for studying viral entry, replication, and host response. This document provides detailed application notes and protocols for assessing these critical differentiation endpoints.
Key Differentiation Metrics & Quantitative Benchmarks
Successful differentiation of primary human bronchial epithelial cells (HBECs) at air-liquid interface (ALI) results in predictable physiological metrics. The following table summarizes target quantitative values from published literature and established protocols.
Table 1: Quantitative Benchmarks for a Differentiated Human Airway Epithelium Model
| Metric | Assessment Method | Target Benchmark (Fully Differentiated) | Typical Timeframe (Post-ALI) | Significance for Viral Studies |
|---|---|---|---|---|
| Transepithelial Electrical Resistance (TEER) | Voltmeter/Electrode System | > 500 Ω·cm² | Peaks ~Days 7-14, stabilizes >Day 21 | Indicates tight junction formation; barrier integrity critical for viral tropism studies. |
| Ciliogenesis | Immunofluorescence (IF) for β-tubulin IV | > 50% apical surface coverage with cilia | Visible from ~Day 14, mature by Day 28-35 | Primary site for influenza, RSV, and SARS-CoV-2 attachment; essential for mucociliary clearance. |
| Mucus Production | Periodic Acid-Schiff (PAS) Staining / MUC5AC ELISA | Strong apical PAS+ staining; MUC5AC > 500 ng/mL per insert (culture supernatant) | Detectable ~Day 7, abundant by Day 21-28 | Viral particle trapping; modulator of infection kinetics and immune response. |
| Cell Layer Morphology | Histology (H&E) | Pseudostratified columnar epithelium, 4-6 cell layers thick | Established by Day 14-21 | Recapitulates in vivo architecture, providing relevant cell types for infection. |
Detailed Experimental Protocols
Protocol: Monitoring TEER During ALI Culture
Purpose: To non-invasively track the formation and maturation of epithelial tight junctions throughout differentiation. Materials: Epithelial Voltohmmeter (EVOM2 or equivalent), STX2 "chopstick" electrodes, 37°C incubator, PBS (warmed).
Procedure:
- Equipment Calibration: Calibrate the voltohmmeter according to manufacturer instructions. Sterilize electrode tips by immersion in 70% ethanol for 15 minutes, followed by air drying in a biosafety cabinet.
- Measurement Preparation: Transfer ALI culture inserts to a sterile, laminar flow hood. Gently aspirate the apical and basolateral media. Rinse the apical surface carefully with 500 µL of warm PBS to remove accumulated mucus, which can insulate the electrode.
- Measurement: a. Add 500 µL of fresh warm PBS to the apical compartment. b. Place the insert into a sterile 24-well plate containing pre-warmed basolateral medium. c. Insert the shorter (apical) electrode into the apical PBS and the longer (basolateral) electrode into the basolateral medium, ensuring no contact with the insert membrane. d. Record the resistance value (in Ω). Subtract the background resistance of a blank insert with PBS/media. e. Calculate TEER (Ω·cm²): TEER = (Measured Resistance - Blank Resistance) × Effective Membrane Area (cm²).
- Frequency: Measure TEER weekly during the first two weeks, then bi-weekly until stabilization. Maintain sterility throughout.
- Data Interpretation: A steady increase followed by a plateau indicates successful barrier formation. A sudden drop may signify contamination or differentiation failure.
Protocol: Immunofluorescence Assessment of Ciliogenesis
Purpose: To visualize, quantify, and qualify cilia formation on the apical surface of the differentiated epithelium. Materials: Differentiated ALI inserts, 4% PFA, PBS, Triton X-100 (0.2%), blocking buffer (5% BSA in PBS), primary antibody (Anti-Acetylated α-Tubulin or β-Tubulin IV), fluorescent secondary antibody, DAPI, mounting medium, confocal microscope.
Procedure:
- Fixation: Aspirate media and rinse inserts gently with PBS. Fix cells by adding 500 µL of 4% PFA to the apical side and 1 mL to the basolateral side for 20 minutes at room temperature (RT). Wash 3x with PBS.
- Permeabilization & Blocking: Permeabilize with 0.2% Triton X-100 in PBS (apical/basolateral) for 10 minutes at RT. Wash. Add blocking buffer (apical/basolateral) for 1 hour at RT.
- Antibody Staining: a. Primary Antibody: Dilute anti-acetylated α-tubulin (1:1000) in blocking buffer. Add 250 µL to the apical surface. Incubate overnight at 4°C in a humidified chamber. Wash 3x with PBS. b. Secondary Antibody & Counterstain: Add fluorophore-conjugated secondary antibody (e.g., Alexa Fluor 488, 1:500) and DAPI (1:1000) in blocking buffer to the apical side. Incubate for 2 hours at RT protected from light. Wash 3x with PBS.
- Mounting & Imaging: Carefully cut the membrane from the insert using a scalpel. Mount on a glass slide with antifade mounting medium. Image using a confocal microscope (z-stack recommended for 3D structure). Acquire multiple random fields for quantification.
- Quantification: Use image analysis software (e.g., ImageJ) to calculate the percentage of the apical surface area positive for acetylated tubulin.
Protocol: Quantification of Mucus Production via PAS Staining and ELISA
Purpose: To histologically visualize and biochemically quantify mucin (specifically MUC5AC) production.
Part A: Periodic Acid-Schiff (PAS) Staining Materials: Differentiated ALI inserts, Carnoy's fixative (or 4% PFA), Periodic Acid, Schiff's Reagent, Hematoxylin, graded ethanol, xylene, mounting medium. Procedure:
- Fix inserts with Carnoy's fixative (preferred for mucin retention) for 30 minutes at RT. Process for paraffin embedding. Section at 5 µm thickness.
- Deparaffinize and rehydrate slides to water.
- Oxidize in 1% Periodic Acid solution for 5 minutes. Rinse in distilled water.
- Place in Schiff's Reagent for 15 minutes (develops magenta color). Rinse in lukewarm tap water for 5 minutes.
- Counterstain nuclei with Hematoxylin for 1 minute. Rinse, blue in Scott's tap water.
- Dehydrate, clear, and mount. Score staining intensity (0-3+) in a blinded manner.
Part B: MUC5AC ELISA Materials: Apical wash samples (collected in PBS with protease inhibitors), human MUC5AC ELISA kit. Procedure:
- Sample Collection: At designated time points, gently wash the apical surface of the ALI culture with 300 µL of PBS containing protease inhibitors. Collect and store at -80°C.
- Perform ELISA according to the manufacturer's protocol. Typically involves: a. Coating wells with capture antibody. b. Blocking. c. Adding samples and standards. d. Adding detection antibody, then enzyme conjugate. e. Adding substrate and measuring absorbance.
- Interpolate MUC5AC concentration from the standard curve. Normalize to total protein content or insert membrane area.
Signaling Pathways & Experimental Workflow
Title: Key Signaling in Airway Differentiation
Title: ALI Culture and Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Airway Model Differentiation & Assessment
| Item Name | Supplier Examples | Function in Protocol |
|---|---|---|
| PneumaCult-ALI Medium | STEMCELL Technologies | Specialized, defined medium for robust differentiation of HBECs at ALI, supporting ciliogenesis and mucus production. |
| Human Bronchial/Tracheal Epithelial Cells | Lonza, ATCC, STEMCELL | Primary cells from donor tissue, essential for creating physiologically relevant models. |
| Corning Transwell Permeable Supports | Corning Inc. | Collagen-coated polyester membranes providing the physical scaffold for 3D polarized epithelial growth. |
| EVOM2 Epithelial Voltohmmeter with STX2 Electrodes | World Precision Instruments | Gold-standard instrument for accurate, non-invasive TEER measurement. |
| Anti-Acetylated α-Tubulin Antibody | Sigma-Aldrich, Abcam | High-specificity antibody for labeling stable microtubules in cilia axonemes via immunofluorescence. |
| Human MUC5AC ELISA Kit | MyBioSource, Abcam | Quantitative immunoassay for measuring secreted mucin 5AC levels in apical washes. |
| Periodic Acid-Schiff (PAS) Staining Kit | Abcam, Sigma-Aldrich | Complete reagent set for histological detection of neutral and acidic mucins in paraffin sections. |
| Fluoroshield with DAPI | Abcam, Sigma-Aldrich | Antifade mounting medium with nuclear counterstain, ready-to-use for fluorescence microscopy. |
Within the broader thesis on establishing standardized 3D human airway model protocols for viral pathogenicity and therapeutic intervention studies, the apical inoculation step is critical. This application note details optimized protocols for depositing viral inoculum onto the apical surface of air-liquid interface (ALI) cultures to maximize infection reproducibility and physiological relevance, mimicking natural respiratory infection routes.
Key Quantitative Parameters for Apical Inoculation
Table 1: Comparative Inoculation Parameters for Common Respiratory Viruses
| Virus (Example) | Recommended Inoculum Volume (µl/cm²) | Apical Contact Time | Temperature | Diluent/Medium | Typical Viral Titer (PFU/ml) Range for Infection |
|---|---|---|---|---|---|
| Influenza A (H1N1) | 25-50 µl/cm² | 1-2 hours | 33-35°C (simulating upper airway) | PBS or Infection Medium (serum-free) | 1x10⁵ – 1x10⁶ |
| SARS-CoV-2 | 20-40 µl/cm² | 1.5-2 hours | 33-35°C (upper) or 37°C (lower) | PBS or Infection Medium | 1x10⁴ – 1x10⁵ |
| RSV | 30-60 µl/cm² | 2-3 hours | 33-35°C | Serum-free Maintenance Medium | 1x10⁵ – 1x10⁶ |
| hMPV | 25-50 µl/cm² | 2 hours | 33°C | Opti-MEM or equivalent | 1x10⁵ – 1x10⁶ |
| Rhinovirus | 15-30 µl/cm² | 1 hour | 33°C | PBS with Ca²⁺/Mg²⁺ | 1x10⁶ – 1x10⁷ |
Table 2: Optimization Variables and Their Impact on Infection Efficiency
| Variable | Tested Range | Optimal Value (General) | Primary Impact on Infection |
|---|---|---|---|
| Inoculum Volume | 10-100 µl/cm² | 25-50 µl/cm² | Coverage vs. shear stress; volume must suffice to cover epithelial folds without causing wash-off. |
| Inoculation Time | 15 min - 6 hours | 1-2 hours | Balancing viral attachment/entry and preserving epithelial integrity/viability. |
| Incubation Temperature | 33°C vs. 37°C | 33°C (Upper Airway Models) | Influences viral fusion kinetics and innate immune response; 33°C often reflects natural nasal environment. |
| Diluent pH | 6.8 - 7.6 | 7.0-7.4 | Affects viral particle stability and receptor binding. |
| Pre-inoculation Wash | PBS vs. No Wash | Gentle Wash with Warm PBS | Removes excess mucus that may non-specifically bind virus, improving reproducibility. |
Detailed Experimental Protocol: Optimized Apical Inoculation
Protocol 1: Standardized Viral Inoculation for 3D Airway Epithelial Models
This protocol is designed for use with well-differentiated human primary bronchial or nasal epithelial cells cultured at ALI for ≥28 days.
Materials Required:
- Differentiated 3D airway epithelial model (e.g., 24-well transwell insert).
- Virus stock, titered.
- Appropriate dilution medium (e.g., PBS++ or serum-free ALI medium).
- Sterile pipettes and tips.
- Humidified incubator at desired temperature (33°C or 37°C) with 5% CO2.
- Biosafety cabinet appropriate for the virus.
- Aspiration vacuum system or pipette for liquid removal.
Procedure:
Pre-Inoculation Preparation (Day of Infection): a. Warm dilution medium and PBS to 33°C or 37°C, as per experimental design. b. In a biosafety cabinet, carefully aspirate the basolateral medium from each well of the culture plate. Replace with fresh, pre-warmed ALI maintenance medium (e.g., 500-700 µl for a 24-well plate). This ensures nutrient availability during infection. c. Apical Wash: Gently add 200-300 µl of pre-warmed PBS to the apical surface of each insert. Tilt the plate slightly to ensure complete coverage. Incubate at the desired temperature for 10 minutes to loosen and equilibrate the surface mucus layer. d. Carefully aspirate the PBS from the apical surface using a fine-tip pipette, angling the insert to remove all liquid. Do not touch or scrape the epithelial surface.
Virus Inoculum Preparation: a. Thaw virus stock rapidly on ice. b. Prepare the desired multiplicity of infection (MOI) or viral dose in pre-chilled dilution medium. Keep the inoculum on ice until application. Vortex gently if necessary.
Apical Inoculation: a. Apply the calculated volume of inoculum dropwise onto the center of the apical surface. For a 6.5mm insert (0.33 cm²), a volume of 10-20 µl (≈30-60 µl/cm²) is typical. Ensure the liquid spreads evenly across the surface without spilling over the edges. b. Place the infected culture plate in a humidified incubator set at the target temperature (e.g., 33°C) with 5% CO₂. c. Allow the virus to adsorb for the predetermined time (e.g., 2 hours). Gently rock the plate every 30 minutes to redistribute the inoculum and prevent localized drying.
Post-Inoculation Wash & Maintenance: a. After the adsorption period, carefully aspirate the inoculum from the apical surface. b. Perform a single, gentle apical wash with 200-300 µl of pre-warmed PBS to remove unbound virus. Aspirate completely. c. Return the inserts to the original plate with fresh, pre-warmed basolateral medium. d. Continue incubation at ALI conditions. Monitor cultures daily for cytopathic effect (CPE) and collect apical wash (for viral yield) or tissue lysates (for genomics/proteomics) at defined time points post-infection.
Protocol 2: High-Throughput Inoculation for Drug Screening
A modified protocol for 96-well format ALI cultures, emphasizing parallel processing.
Key Modifications:
- Use automated liquid handlers for apical washing and inoculum dispensing to ensure consistency.
- Reduce apical wash and inoculum volumes proportionally to the surface area (e.g., ~5-10 µl for a 96-well ALI insert).
- Use multichannel pipettes for basolateral medium changes.
- Include control columns on each plate for uninfected (vehicle-only) and cytotoxicity controls.
Diagram: Experimental Workflow for Apical Inoculation
Workflow for Apical Viral Infection
Diagram: Viral Entry Pathways in Airway Epithelium
Viral Entry Pathways at the Apical Surface
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Apical Infection Studies
| Item/Category | Example Product/Description | Primary Function in Protocol |
|---|---|---|
| Differentiated 3D Airway Models | MatTek EpiAirway, Epithelix MucilAir, or lab-grown primary HAE cultures. | Physiologically relevant substrate with functional cilia, mucus production, and tight junctions. |
| Air-Liquid Interface (ALI) Medium | PneumaCult-ALI, Ultroser G supplemented DMEM/F12, or custom formulations. | Supports long-term differentiation and maintenance of mucociliary phenotype. |
| Viral Dilution Medium | Dulbecco's Phosphate-Buffered Saline (DPBS) with calcium & magnesium (PBS++). | Provides ionic stability for viral particles without inhibiting attachment. Serum-free options reduce non-specific binding. |
| Infection Enhancers | Polybrene (hexadimethrine bromide), DEAE-dextran. | Cationic polymers that reduce charge repulsion between virus and cell membrane, potentially increasing infection efficiency for some viruses. Use with optimization. |
| Protease Inhibitors (for certain viruses) | TPCK-trypsin, exogenous proteases (e.g., for influenza HA cleavage). | Required to prime some viral surface proteins for fusion-capable conformation. |
| Mucolytic Agents (Pre-treatment) | Recombinant human DNase I (Pulmozyme), N-Acetylcysteine (low conc.). | Can reduce viscosity of the apical mucus layer pre-inoculation, improving viral access to epithelium. Requires careful titration to avoid damage. |
| Neutral Red or Crystal Violet | Viability staining solutions. | Used post-infection to quantify cytopathic effect (CPE) via dye uptake or plaque assays. |
| Cell Viability Assays | MTT, WST-8, LDH Cytotoxicity Assay Kits. | To monitor compound cytotoxicity or virus-induced damage in tandem with infection assays. |
| Viral Titer Quantification | Plaque Assay (Agarose overlay), TCID50, Immunostaining (Focus Forming Assay), qRT-PCR. | Essential for standardizing inoculum dose and measuring viral output post-infection. |
| Transwell Inserts | Permeable supports (e.g., Corning Costar, polyester or polycarbonate membrane). | Physical scaffold for ALI culture, allowing separate access to apical and basolateral compartments. |
Within the context of a thesis on 3D human airway model protocols for viral pathogenicity studies, quantifying viral infection outcomes is paramount. Downstream assays such as viral titer determination, plaque assays, and molecular analyses via qPCR and RNA-seq provide critical, complementary data on viral replication, infectivity, and host responses. This application note details protocols and considerations for implementing these assays using samples derived from advanced 3D airway cultures, such as air-liquid interface (ALI) differentiated primary cells or organoids.
Key Research Reagent Solutions
The following table lists essential reagents and kits for performing downstream viral assays from 3D airway models.
| Item | Function & Application | Example Product/Kit |
|---|---|---|
| Viral Transport Medium | Stabilizes viral particles from apical washes/samples for titer quantification. | Copan UTM (Universal Transport Medium) |
| Cell Lines for Plaque Assays | Permissive monolayer cells (e.g., Vero E6, MDCK) for quantifying infectious viral particles. | Vero E6 (ATCC CRL-1586) |
| Avicel/Methylcellulose Overlay | Semi-solid overlay for plaque assay; confines spread, enables clear plaque visualization. | 2.4% Avicel RC-591 in maintenance media |
| Crystal Violet Stain | Fixes and stains monolayer cells; visualizes clear plaques (unstained areas). | 1% Crystal Violet in 10% Ethanol |
| RNA Extraction Kit | Isolates high-quality total RNA (viral & host) from infected 3D model lysates or apical washes. | Qiagen RNeasy Mini Kit |
| Reverse Transcription Kit | Synthesizes cDNA from RNA for downstream qPCR analysis. | High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems) |
| qPCR Master Mix | Contains enzymes, dNTPs, for quantitative PCR with probes or intercalating dyes. | TaqMan Fast Advanced Master Mix |
| Viral Target Primers/Probes | Sequence-specific assays for quantifying viral genomic RNA/cDNA. | 2019-nCoV CDC qPCR Probe Assay (IDT) |
| RNA-seq Library Prep Kit | Prepares stranded RNA libraries for next-generation sequencing. | Illumina Stranded Total RNA Prep |
| DNase I | Removes genomic DNA contamination during RNA isolation. | RNase-Free DNase I (Qiagen) |
Protocols & Application Notes
Quantifying Viral Titer from 3D Airway Model Apical Washes
Application Note: Apical washes (e.g., with 200-300 µL PBS) of 3D airway models non-destructively sample released virions. Titers indicate total viral particle production.
Protocol:
- Sample Collection: At designated time points post-infection, gently wash the apical surface of the 3D airway model with 200 µL of cold PBS + 0.1% BSA. Collect the wash into a microcentrifuge tube.
- Clarification: Centrifuge at 500 x g for 5 min at 4°C to remove cellular debris. Transfer supernatant to a new tube.
- Storage: Aliquot and immediately store at -80°C. Avoid freeze-thaw cycles.
- Titer Determination: Use clarified supernatant in plaque assays or TCID₅₀ assays (detailed below).
Plaque Assay for Infectious Virus Quantification
Application Note: The gold standard for quantifying infectious virus particles (PFU/mL). Requires a permissive cell monolayer.
Detailed Protocol:
- Prepare Monolayers: Seed appropriate cells (e.g., Vero E6 for SARS-CoV-2) in 12- or 24-well plates to reach 90-95% confluency at assay time.
- Virus Inoculation:
- Thaw apical wash samples on ice.
- Aspirate media from cell monolayers.
- Perform ten-fold serial dilutions of viral sample in infection medium (e.g., DMEM + 2% FBS, 1% Pen/Strep).
- Inoculate monolayers in duplicate with 100-200 µL of each dilution. Rock plates every 15 min for 1 hour at 37°C.
- Add Overlay:
- Prepare a 2X concentration of your chosen overlay (e.g., Avicel or Methylcellulose) in warm 2X maintenance medium.
- After adsorption, gently add an equal volume of overlay to each well (final volume: e.g., 500 µL per well of a 24-well plate). Ensure even distribution.
- Incubate plates at 37°C, 5% CO₂ for the appropriate number of days (e.g., 2-3 for many respiratory viruses).
- Fix and Stain:
- Carefully aspirate overlay.
- Fix cells with 10% Formalin in PBS for 30 min-1 hour at room temperature.
- Aspirate fixative and stain with 1% Crystal Violet solution (in 10% ethanol) for 20 min.
- Rinse plates gently with tap water to reveal clear plaques.
- Count and Calculate: Count distinct plaques. Calculate plaque-forming units per mL (PFU/mL) using the formula: PFU/mL = (Number of plaques) / (Dilution factor x Inoculum volume (mL))
qPCR for Viral Genome Quantification
Application Note: qPCR rapidly quantifies viral genomic RNA (or cDNA) copies, reflecting both infectious and non-infectious particles. Essential for kinetics studies.
Detailed Protocol (One-Step RT-qPCR):
- RNA Extraction: Isolate total RNA from infected 3D model lysates or apical wash supernatants using a dedicated kit (e.g., QIAamp Viral RNA Mini Kit for supernatants, RNeasy for lysates). Include a DNase I treatment step.
- Assay Setup:
- Use a validated primer/probe set for the target virus (e.g., N gene for SARS-CoV-2).
- Prepare reactions on ice in a 96-well plate: 5 µL RNA template, 10 µL 2X One-Step RT-qPCR Master Mix, 1 µL primer/probe mix (final concentration 400 nM/200 nM), 4 µL nuclease-free water.
- Include a standard curve of known copy number (e.g., 10⁷ to 10¹ copies of synthetic RNA standard) and no-template controls.
- Run qPCR:
- Cycling conditions (example): Reverse Transcription: 50°C for 15 min; Initial Denaturation: 95°C for 2 min; 40 cycles of: 95°C for 5 sec, 60°C for 30 sec (acquire fluorescence).
- Data Analysis: Plot the standard curve (Ct vs. log₁₀ copy number). Use the curve's equation to calculate the genomic copy number in each sample. Report as copies per mL of apical wash or per µg of total RNA from lysates.
Table 1: Comparative Data from Downstream Assays (Hypothetical SARS-CoV-2 Infection in 3D Airway Model)
| Time Post-Infection (hpi) | Plaque Assay (PFU/mL) | qPCR (Genome Copies/mL) | Ratio (Copies:PFU) |
|---|---|---|---|
| 24 | 1.5 x 10³ | 5.2 x 10⁶ | 3.5 x 10³ |
| 48 | 8.7 x 10⁴ | 3.1 x 10⁸ | 3.6 x 10³ |
| 72 | 2.1 x 10⁵ | 9.8 x 10⁸ | 4.7 x 10³ |
RNA-seq for Host Transcriptomic Profiling
Application Note: RNA-seq provides an unbiased, genome-wide view of the host response in the 3D airway model, identifying pathways of inflammation, antiviral defense, and cellular injury.
Workflow Protocol:
- Sample Preparation: Lyse infected and mock-infected 3D airway models directly in well plates using TRIzol or a lysis buffer compatible with your RNA extraction kit. Pool replicates if necessary for sufficient RNA yield.
- RNA Extraction & QC: Extract total RNA, treat with DNase I. Assess quantity (Qubit) and integrity (RIN > 8.0 on Bioanalyzer).
- Library Preparation: Use a stranded total RNA library prep kit that includes ribosomal RNA depletion. Follow manufacturer's instructions precisely.
- Sequencing: Sequence on an Illumina platform (e.g., NovaSeq) to a depth of 20-40 million paired-end reads per sample.
- Bioinformatic Analysis: Align reads to a combined host (e.g., human GRCh38) and viral genome. Perform differential gene expression analysis (e.g., using DESeq2). Pathway analysis (GO, KEGG) reveals perturbed biological processes.
Visualized Workflows & Relationships
Title: Downstream Assay Workflow from 3D Airway Model
Title: Integrating Assay Data for Pathogenicity Insights
Application Notes
Within the broader thesis on developing a standardized 3D human airway model protocol for viral pathogenicity studies, these advanced applications bridge the gap between basic infection modeling and clinically predictive systems. Primary human airway epithelial cells (hAECs) differentiated at the air-liquid interface (ALI) into pseudostratified, mucociliary epithelium form the foundational model. These advanced modules enable the study of complex host-pathogen-immune interactions, chronic infection dynamics, and therapeutic interventions.
1. Co-culture with Immune Cells: Recapitulating the airway's immune landscape is critical for evaluating viral immunopathology and the cascade of inflammatory responses. Integrating peripheral blood mononuclear cells (PBMCs), monocyte-derived macrophages, or dendritic cells into the basal compartment or on the apical surface allows for the study of immune cell recruitment, cytokine storm induction, and antigen presentation. 2. Long-term Infection Models: Many respiratory viruses establish persistent infections or cause chronic sequelae. Extending infection timelines in 3D airway models beyond standard acute phases (e.g., 7-14 days to 4-8 weeks) facilitates investigation of viral latency, intermittent shedding, epithelial remodeling, and long-term damage. 3. Drug Efficacy Testing: These physiologically relevant models serve as a premium platform for preclinical antiviral and anti-inflammatory drug testing. They allow for efficacy assessment under conditions that mimic the human airway, including barrier integrity, mucus production, and innate immune responses, providing superior predictive value over monolayer cultures.
Table 1: Comparative Outputs from Advanced 3D Airway Model Applications
| Application | Key Readout Parameters | Typical Measurement Timepoints | Example Quantitative Data Range (Model-Dependent) |
|---|---|---|---|
| Immune Co-culture | Transepithelial electrical resistance (TEER) drop, Cytokine release (e.g., IL-6, IL-8, IFN-λ), Immune cell migration count, Viral titer (TCID₅₀) | 24, 48, 72 hours post-infection (hpi) | IL-8 secretion: 500-5000 pg/mL increase; Monocyte migration: 5-25% of added cells; TEER reduction: 40-80% |
| Long-term Infection | Viral RNA copy number (qRT-PCR), Histopathology score, Cilia beating frequency, Mucin (MUC5AC) gene expression, LDH release | Weekly up to 60 days post-infection (dpi) | Persistent viral RNA: 10³-10⁵ copies/µg RNA at 28 dpi; Cilia beating reduction: 30-60% at 14 dpi |
| Drug Efficacy Testing | IC₅₀/EC₅₀, Viral load reduction (log₁₀), TEER preservation (%), Cytokine modulation (%), Cytotoxicity (CC₅₀) | 48-96 hpi (treatment pre- & post-infection) | EC₅₀ for novel antivirals: 0.1-5 µM; Viral titer reduction: 2-4 log₁₀; TEER preservation: 60-90% of uninfected control |
Detailed Experimental Protocols
Protocol 1: Integration of Monocyte-Derived Macrophages in a 3D Airway Co-culture Model Objective: To establish a co-culture system for studying macrophage responses to viral infection in a 3D airway epithelium. Materials: 24-well ALI plate, differentiated 3D airway model (day 28+), CD14+ human monocytes, Macrophage colony-stimulating factor (M-CSF), virus inoculum. Procedure:
- Macrophage Differentiation: Isolate CD14+ monocytes from human PBMCs using magnetic separation. Culture in RPMI-1640 medium with 10% FBS and 50 ng/mL M-CSF for 6-7 days to differentiate into macrophages.
- Co-culture Establishment: Gently rinse the basal compartment of the 3D airway model. Add 1 x 10⁵ differentiated macrophages in 500 µL of co-culture medium (PneumaCult ALI basal medium + 10% FBS) to the basal chamber.
- Infection & Monitoring: After 24h of macrophage integration, inoculate virus apically. Monitor TEER daily. Collect basal medium supernatant at 24, 48, 72 hpi for cytokine analysis (e.g., via Luminex) and viral titer. Fix models for confocal microscopy (e.g., staining for viral antigen and macrophage marker CD68).
Protocol 2: Establishing a Long-term Respiratory Syncytial Virus (RSV) Infection Model Objective: To model persistent RSV infection and its impact on epithelial integrity and function over 4 weeks. Materials: Differentiated 3D airway model, RSV A2 strain expressing GFP, dedicated incubator. Procedure:
- Low MOI Infection: Infect models apically with RSV at a low multiplicity of infection (MOI=0.1) in a minimal volume for 2 hours.
- Maintenance & Sampling: Post-inoculation, return to ALI conditions. Replace basal medium twice weekly. Perform weekly, non-destructive sampling: collect apical wash for viral RNA extraction/qRT-PCR and collect 100 µL basal medium for LDH/citokine assay.
- Terminal Analyses: At predetermined endpoints (e.g., 14, 28, 42 dpi), sacrifice replicates for: (a) Histology (H&E, Alcian blue/PAS) for morphology and goblet cell hyperplasia, (b) Immunofluorescence for ciliated cell marker (β-IV tubulin) and viral protein, (c) TEM for cilia ultrastructure.
Protocol 3: Antiviral Drug Efficacy Testing in an Infected 3D Airway Co-culture Objective: To evaluate the efficacy and toxicity of a candidate antiviral compound in a virus-infected airway model with immune components. Materials: Co-culture model (as per Protocol 1), candidate antiviral compound, DMSO vehicle control, validated virus stock. Procedure:
- Experimental Groups: Establish groups: Uninfected, Infected+Vehicle, Infected+Drug (multiple doses), Drug-toxicity control (uninfected+drug).
- Treatment Regimen: Add the compound to the basal medium 2 hours pre-infection. Infect apically with virus (MOI=0.5). Refresh basal medium with drug/vehicle every 48 hours.
- Endpoint Analysis (96 hpi):
- Apical wash: Titrate virus by plaque assay or TCID₅₀.
- Basal supernatant: Multiplex cytokine panel, LDH assay for cytotoxicity.
- Epithelial Cells: Lysc for RNA (host gene expression: IFNs, ISGs, mucins) and protein.
- Calculate EC₅₀ (half-maximal effective concentration) from dose-response curve of viral titer reduction and CC₅₀ (half-maximal cytotoxic concentration) from LDH/ATP data to determine Selectivity Index (SI = CC₅₀/EC₅₀).
Visualizations
Immune Co-culture Experimental Workflow
Immune-Epithelial Crosstalk Signaling Pathway
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for Advanced 3D Airway Studies
| Reagent/Material | Supplier Examples | Function in Protocol |
|---|---|---|
| PneumaCult ALI Medium | STEMCELL Technologies | Maintenance and differentiation of primary human bronchial epithelial cells at ALI. Provides optimized factors for mucociliary differentiation. |
| Human CD14 MicroBeads | Miltenyi Biotec | Isolation of CD14+ monocytes from PBMCs for subsequent macrophage differentiation in co-culture setups. |
| Recombinant Human M-CSF | PeproTech | Differentiation factor required to drive monocytes into a macrophage phenotype over 6-7 days. |
| LIVE/DEAD Viability/Cytotoxicity Kit | Thermo Fisher Scientific | Quantifies compound cytotoxicity (CC₅₀) by measuring lactate dehydrogenase (LDH) release or via calcein AM/ethidium homodimer staining. |
| Luminex Multiplex Assay Panels | R&D Systems, Bio-Rad | Simultaneous quantification of multiple cytokines/chemokines (e.g., IL-6, IL-8, TNF-α, IFN-γ) from limited basal supernatant volumes. |
| Epithelial Voltohmmeter (EVOM) | World Precision Instruments | Measures transepithelial electrical resistance (TEER) as a non-destructive, quantitative readout of epithelial barrier integrity pre- and post-infection/treatment. |
| qRT-PCR Assays for Viral Load | ATCC, IDT | TaqMan probe-based assays for absolute quantification of viral RNA copies (e.g., RSV, Influenza, SARS-CoV-2) from apical washes or cell lysates. |
Troubleshooting Your 3D Airway Model: Solving Common Issues in Differentiation, Infection, and Assays
1. Introduction Within the broader thesis on establishing a robust 3D human airway model protocol for viral pathogenicity studies, a primary challenge is the generation of a fully differentiated, pseudostratified epithelium with functional mucociliary clearance. This phenotype is dependent on the coordinated action of basal, secretory, and ciliated cells. Poor differentiation or a lack of cilia directly compromises the physiological relevance of the model for studying viral entry, replication, and host response. These deficits are most frequently attributed to suboptimal culture media composition and extracellular matrix (ECM) support. This document provides application notes and detailed protocols for optimizing these two critical components.
2. Research Reagent Solutions: Essential Toolkit
| Reagent/Category | Function in Airway Model Differentiation |
|---|---|
| PneumaCult-ALI Medium | A specialized, serum-free medium designed to promote the proliferation and subsequent differentiation of human airway basal cells into a mucociliary epithelium at the air-liquid interface (ALI). |
| Ultroser G Serum Substitute | A chemically defined serum substitute used in differentiation phases to provide hormones, growth factors, and attachment factors that support ciliogenesis. |
| Retinoic Acid (All-Trans) | A critical morphogen derived from Vitamin A. It is essential for inducing and maintaining the differentiation of secretory cells into ciliated cells. |
| ROCK Inhibitor (Y-27632) | Enhances the survival and plating efficiency of primary basal cells during initial seeding, preventing anoikis. |
| Collagen IV from Human Placenta | A key ECM component for coating Transwell inserts, providing a biologically relevant scaffold that promotes basal cell polarization and differentiation. |
| Matrigel (GFR, Phenol Red-free) | A reconstituted basement membrane matrix rich in laminin, collagen IV, and growth factors. Used thinly or in combination with collagen to enhance initial cell attachment and signaling. |
| Recombinant Human Noggin | A BMP pathway inhibitor. Adding Noggin to early differentiation stages can help direct progenitor cells toward a ciliated cell fate by suppressing alternative differentiation pathways. |
| DAPT (γ-Secretase Inhibitor) | A Notch pathway inhibitor. Transient inhibition can promote ciliogenesis by increasing the number of progenitor cells available to become ciliated cells, rather than secretory cells. |
3. Media Optimization Protocol: Sequential Feeding for Enhanced Ciliogenesis Objective: To drive basal stem cells through a proliferative phase, followed by a differentiation phase that maximizes ciliated cell yield.
3.1. Materials
- Primary human bronchial epithelial cells (HBECs) at passage 2-4.
- PneumaCult-Ex Plus Medium (or equivalent expansion medium).
- PneumaCult-ALI Medium.
- Retinoic Acid (RA) stock solution (1 mM in DMSO).
- Dimethyl sulfoxide (DMSO), sterile.
- UltraPure DNase/RNase-Free Distilled Water.
- 24-well or 12-well plate format Transwell inserts (0.4 μm pore, polyester membrane).
- Collagen IV-coated inserts (see Section 4.1).
3.2. Procedure
- Expansion Phase (Days -7 to 0): Seed HBECs at 5.0 x 10⁴ cells/cm² on coated inserts in expansion medium. Feed every 48 hours until 100% confluent.
- ALI Initiation (Day 0): Aspirate medium from the apical chamber to establish the air-liquid interface (ALI). Replace basal medium with PneumaCult-ALI Medium supplemented with 50 nM Retinoic Acid.
- Differentiation Phase (Days 0-28): Feed cultures from the basal chamber only, replacing medium with fresh ALI + 50 nM RA every 48 hours for the first 14 days, then every 72 hours thereafter.
- Optional - Pathway Modulation (Days 0-7): To boost ciliogenesis, supplement the ALI medium during the first week with 100 ng/mL Recombinant Human Noggin and/or 10 μM DAPT. Withdraw after day 7.
- Monitoring: Assess cilia formation via immunofluorescence for α-Tubulin (cilia) and FOXJ1 (ciliated cell transcription factor) weekly from day 14 onwards.
4. Matrix Optimization Protocol: Combinatorial Coating for Polarization Objective: To create an ECM microenvironment that supports basal cell adhesion, polarization, and provides correct signaling cues for differentiation.
4.1. Materials
- Rat tail Collagen I (3-4 mg/mL).
- Human Collagen IV (50 μg/mL in 0.25% acetic acid).
- Growth Factor Reduced (GFR) Matrigel, on ice.
- Sterile 0.02M Acetic Acid.
- Phosphate-Buffered Saline (PBS), without Ca²⁺/Mg²⁺.
- Transwell inserts.
4.2. Procedure: Collagen IV/Matrigel Composite Coating
- Dilution: On ice, prepare a coating solution of 30 μg/mL Collagen IV and 150 μg/mL (~1:40 dilution) GFR Matrigel in cold PBS.
- Coating: Add enough solution to cover the membrane of each Transwell insert (e.g., 150 μL for a 12-well insert).
- Incubation: Incubate inserts at 37°C for a minimum of 2 hours.
- Preparation: Carefully aspirate the coating solution immediately before seeding cells. Do not let the membrane dry. Rinse once with warm PBS or culture medium.
5. Data Presentation: Optimization Impact
Table 1: Effect of Media and Matrix Conditions on Differentiation Outcomes (Hypothetical Data from Typical Experiments)
| Condition | Media Formulation | Matrix Coating | % Ciliated Cells (Day 28) | MUC5AC+ Secretory Cells | TEER (Ω*cm²) | Notes |
|---|---|---|---|---|---|---|
| 1 (Suboptimal) | Basic ALI, no RA | Collagen I only | 8.2% ± 2.1 | Low | 450 ± 80 | Poor ciliogenesis, patchy epithelium. |
| 2 (Standard) | ALI + 50 nM RA | Collagen IV | 22.5% ± 4.3 | Moderate | 650 ± 95 | Functional model, moderate cilia coverage. |
| 3 (Enhanced) | ALI + 50 nM RA + Noggin (D0-7) | Collagen IV | 35.1% ± 5.6 | Moderate | 620 ± 75 | Significant cilia increase, BMP inhibition effective. |
| 4 (Optimized) | ALI + 50 nM RA + DAPT (D0-7) | Collagen IV/Matrigel Composite | 41.8% ± 6.2 | High | 800 ± 110 | Highest ciliation & barrier integrity. Notch inhibition + composite matrix synergize. |
Table 2: Troubleshooting Guide for Poor Differentiation
| Observed Issue | Potential Cause in Media | Potential Cause in Matrix | Recommended Action |
|---|---|---|---|
| Low or No Cilia | Retinoic Acid omitted or degraded; High serum contaminants; Incorrect differentiation timing. | Overly thick or gel-like matrix; Pure Matrigel inhibits ciliogenesis. | Fresh RA aliquot; Use serum-free media; Verify ALI timing. Switch to thin collagen IV or composite coating. |
| Poor Barrier Function (Low TEER) | Microbial contamination; Excessive medium change volume causing shear. | Incomplete or non-uniform coating; Membrane damage. | Test for mycoplasma; Standardize feeding volumes. Ensure even coating; inspect membrane integrity. |
| Overabundant Mucus, Few Cilia | Notch signaling overly active, favoring secretory fate. | Matrix may contain high TGF-β. | Add DAPT (γ-secretase inhibitor) early in differentiation. Use defined, GFR Matrigel. |
| Patchy or Detached Epithelium | ROCK inhibitor not used post-seeding; pH fluctuations. | Coating matrix degraded or insufficient for initial attachment. | Add Y-27632 for first 48h post-seeding. Optimize coating concentration and incubation time. |
6. Visualized Workflows and Pathways
Sequential Media Protocol for Airway Differentiation
Pathway Inhibition to Boost Ciliogenesis
Within the context of developing a robust 3D human airway model protocol for viral pathogenicity studies, consistent and high transepithelial electrical resistance (TEER) is a non-negotiable benchmark. It quantifies the integrity of the tight junction-sealed epithelial barrier, a critical factor for modeling physiological infection and inflammatory responses. Inconsistent or low TEER readings compromise the model's validity, leading to unreliable data on viral entry, replication, and host-pathogen interactions. This application note details systematic troubleshooting protocols to diagnose and rectify barrier integrity issues.
Common Causes & Diagnostic Table
The following table summarizes primary causes of low/inconsistent TEER, associated symptoms, and recommended diagnostic checks.
Table 1: Troubleshooting Guide for Low/Inconsistent TEER
| Cause Category | Specific Issue | Typical TEER Symptom | Diagnostic Check |
|---|---|---|---|
| Cell Culture Health | Low cell viability/passage number | Consistently low, fails to peak | Check viability (>95%), use low-passage cells (P2-P5). |
| Mycoplasma contamination | Erratic, declining over time | Perform mycoplasma PCR/assay. | |
| Seeding Protocol | Sub-optimal seeding density | Low peak value, slow development | Optimize density (e.g., 1-2.5e5 cells/cm² for Calu-3). |
| Inconsistent cell suspension | High well-to-well variability | Use uniform, single-cell suspension; seed multiple inserts in one batch. | |
| Culture Conditions | Incomplete polarization/differentiation | Premature plateau, low max TEER | Extend air-liquid interface (ALI) culture time (≥14 days). Verify ALI establishment. |
| Inconsistent medium supply | Fluctuating daily readings | Standardize feeding schedule & volume. Ensure apical surface is completely drained. | |
| Measurement Artifacts | Electrode/Chamber Damage | Sudden drops, zero readings | Inspect electrodes for cleanliness/kinks. Confirm chamber integrity. |
| Temperature & CO2 Fluctuations | Reading drift during measurement | Pre-warm media, perform measurements quickly in a stable environment (37°C, 5% CO2 if possible). | |
| Edge Damage & Meniscus Effects | Inconsistency between replicates | Handle inserts carefully. Ensure consistent media levels in basolateral compartment. | |
| Biological Assay | Cytotoxicity from test articles | Acute drop post-treatment | Run parallel viability assays (LDH, MTT). Include vehicle controls. |
Core Protocols for Barrier Integrity Assessment
Protocol 3.1: Standardized TEER Measurement for Airway Models
Objective: To obtain consistent and accurate TEER readings from human airway epithelial cells cultured at ALI. Materials:
- EVOM2 or equivalent voltohmmeter with chopstick electrodes.
- EndOhm or similar measurement chamber (for 24-well inserts).
- 37°C pre-warmed, CO2-equilibrated culture medium.
- Sterile PBS (warmed to 37°C).
- ALI-cultured human airway epithelial cell inserts (e.g., primary, Calu-3, MucilAir).
Procedure:
- Preparation: Turn on the meter and allow it to stabilize. Sterilize electrodes by immersion in 70% ethanol for 15 minutes, then rinse thoroughly in sterile PBS.
- Equilibration: Transfer inserts to a new plate. Carefully aspirate apical surface mucus/condensate. Add pre-warmed medium to the basolateral chamber to the standard level (e.g., 500 µL for 24-well insert). Add a small, consistent volume of pre-warmed PBS (e.g., 100 µL) to the apical surface to form a liquid bridge for measurement.
- Measurement:
- For Chopstick Electrodes: Place the shorter electrode in the apical compartment and the longer in the basolateral, ensuring they do not touch the membrane. Hold steady until reading stabilizes (~5-10 seconds). Record value (Ω).
- For EndOhm Chamber: Fill chamber with pre-warmed medium per manufacturer's instructions. Insert cell culture insert, ensuring no air bubbles. Close chamber and take reading.
- Calculation: Subtract the average resistance of a cell-free insert (blank) from the sample reading. Multiply by the effective surface area of the insert (e.g., 0.33 cm² for 24-well). Report as Ω·cm².
- Return to Culture: Aspirate apical PBS and return insert to original culture plate with correct media volumes. Return to incubator promptly.
Protocol 3.2: Paracellular Flux Assay (Complementary to TEER)
Objective: Functionally validate barrier integrity by measuring the passage of a small molecular weight tracer. Materials:
- Fluorescein isothiocyanate-dextran (FITC-dextran, 4 kDa), 1 mg/mL stock in PBS.
- Transport buffer (e.g., HBSS with 10 mM HEPES, pH 7.4).
- Microplate reader capable of fluorescence detection (Ex/Em: ~490/520 nm).
Procedure:
- Preparation: Wash inserts 2x with warm transport buffer.
- Dosing: Add transport buffer to the basolateral compartment. Add FITC-dextran solution (final conc. 0.5-1 mg/mL) to the apical compartment.
- Incubation: Incubate plate at 37°C on an orbital shaker (low speed) for 1-2 hours.
- Sampling: At desired timepoints (e.g., 60, 120 min), sample 100 µL from the basolateral compartment and replace with fresh buffer.
- Analysis: Measure fluorescence in samples against a standard curve. Calculate the apparent permeability coefficient (Papp) in cm/s using the formula:
Papp = (dQ/dt) / (A * C0)where dQ/dt is the flux rate (mol/s), A is the membrane area (cm²), and C0 is the initial apical concentration (mol/mL).
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Airway Barrier Integrity Research
| Item | Function & Rationale |
|---|---|
| Human Primary Bronchial/Tracheal Epithelial Cells | Gold standard for physiologically relevant models. Require optimized media (e.g., PneumaCult-ALI) for proper differentiation into ciliated and goblet cells. |
| Calu-3 Cell Line | Common immortalized model for bronchial epithelium. Forms stable, high-TEER monolayers suitable for standardized viral studies. |
| ALI Culture Media (e.g., PneumaCult-ALI, UltaGRO-ALI) | Specialized, serum-free formulations designed to promote mucociliary differentiation and sustained barrier function at the air-liquid interface. |
| Permeable Supports (e.g., Transwell inserts) | Collagen IV-coated polyester or polyethylene terephthalate (PET) membranes with 0.4 µm pores are standard for ALI culture and TEER measurement. |
| Epithelial Voltohmmeter (e.g., EVOM2) | Dedicated device for accurate, high-resistance TEER measurements. The STX2 "chopstick" electrodes are suited for quick checks; EndOhm chambers provide higher precision. |
| FITC- or TRITC-Dextran (3-5 kDa) | Paracellular flux tracer. Used in functional integrity assays complementary to TEER. Confirms tight junction competence. |
| Tight Junction Protein Antibodies (ZO-1, Occludin, Claudin) | For immunofluorescence staining. Visual confirmation of continuous, well-localized tight junction strands is critical for validating TEER data. |
| Mycoplasma Detection Kit | Essential for routine screening. Contamination is a common, silent cause of declining cell health and barrier function. |
Visualization: Experimental Workflow and Pathway
Diagram 1: TEER Troubleshooting Workflow
Diagram 2: From Barrier Defect to Research Impact Pathway
Challenges in Apical Viral Inoculation and Wash Optimization
Within the broader thesis on establishing a robust 3D human airway epithelial (HAE) model protocol for viral pathogenicity studies, the apical inoculation and subsequent wash step present critical, often under-optimized, technical challenges. These fully differentiated, mucociliary models recapitulate the in vivo physiology of the human respiratory tract but introduce complexity for viral infection studies. The apical surface is air-exposed and bathed in a mucus layer, creating a barrier that standard inoculation methods must overcome without damaging tissue integrity. Optimizing the viral inoculum volume, contact time, and subsequent wash procedure is paramount for achieving consistent, physiologically relevant infection kinetics and high-quality data.
Table 1: Summary of Apical Inoculation Parameters and Impact
| Parameter | Typical Range | Challenge | Consequence of Poor Optimization |
|---|---|---|---|
| Inoculum Volume | 50-300 µL per insert | Overflow can compromise ALI; Underflow yields uneven coverage. | Variable infection multiplicity of infection (MOI); potential basolateral leakage. |
| Inoculum Contact Time | 1-3 hours | Too short: insufficient viral attachment. Too long: desiccation, loss of viability. | Low infectivity titers; increased experimental variability. |
| Wash Solution Volume | 100-500 µL per wash | Incomplete removal of unbound virus vs. mechanical disruption of epithelium. | High background "input" virus in supernatants; altered infection kinetics. |
| Number of Wash Cycles | 1-3 cycles | Diminishing returns with increased cycles; cumulative tissue stress. | Inconsistent removal of non-internalized virus; damaged ciliary function. |
| Mucus Burden (Variable) | Model-dependent | Traps virus, preventing access to cells; non-specific binding. | Underestimation of infectivity; requires mucolytic pre-treatment (e.g., DTT) which may affect cells. |
Table 2: Comparison of Wash Buffer Compositions
| Buffer Component | Common Formulation(s) | Purpose | Consideration |
|---|---|---|---|
| Base Solution | DPBS, MEM, Optimem | Isotonic vehicle. | DPBS may lack nutrients for prolonged contact. |
| Protein Additive | 0.1-1% BSA, Serum | Reduces non-specific viral binding to plastic/tissue. | May interfere with specific virus-receptor interactions. |
| pH Indicator | Phenol Red (optional) | Visual monitoring of wash completeness. | Potential photosensitivity; may be omitted. |
| Antibiotics/Antimycotics | 1x Pen-Strep, Amphotericin B | Prevents microbial contamination during procedure. | Standard practice but may not be necessary for brief exposure. |
| Mucolytic Agent | 1-5 mM Dithiothreitol (DTT) | Disrupts mucus polymers to expose cell surfaces. | Cytotoxic with prolonged exposure; requires careful optimization and removal. |
Detailed Experimental Protocols
Protocol 1: Standardized Apical Inoculation for 3D HAE Models
Objective: To apply a consistent viral inoculum to the apical surface of a 24-well format HAE model without compromising tissue integrity.
Materials:
- Differentiated 3D HAE model (e.g., Epiairway, MucilAir, or primary cell-derived)
- Virus inoculum, diluted in infection medium (e.g., Optimem)
- Pre-warmed wash buffer (e.g., DPBS + 0.1% BSA)
- Sterile pipettes and tips
- 37°C, 5% CO₂ incubator
Procedure:
- Pre-equilibration: Aspirate the basolateral medium and replace with fresh, pre-warmed maintenance medium. Incubate the model for at least 30 minutes at 37°C, 5% CO₂ prior to infection.
- Apical Wash: Gently add 200 µL of pre-warmed wash buffer to the apical chamber. Incubate for 10 minutes at 37°C to loosen mucus. Carefully aspirate the apical liquid completely.
- Viral Inoculation: Apply the calculated viral inoculum in a minimal volume (typically 100 µL for a 24-well insert) directly onto the apical surface. Ensure even distribution by gently tilting the plate.
- Infection Period: Incubate the model at 37°C, 5% CO₂ for the desired contact period (e.g., 2 hours). Gently rock the plate every 20-30 minutes to redistribute the inoculum and prevent drying.
- Termination of Inoculation: Proceed to Protocol 2 for the wash step.
Protocol 2: Optimized Apical Wash for Unbound Virus Removal
Objective: To effectively remove non-internalized viral particles while preserving epithelial integrity and ciliary function.
Materials:
- Inoculated HAE model from Protocol 1
- Pre-warmed wash buffer (e.g., DPBS + 0.1% BSA), 37°C
- Optional: Mucolytic wash buffer (e.g., DPBS with 3mM DTT)
Procedure:
- Initial Removal: Carefully aspirate the apical inoculum.
- Wash Cycles: Gently add 200 µL of pre-warmed wash buffer to the apical surface. Incubate for 5 minutes at 37°C. Gently swirl the plate and carefully aspirate the buffer completely. Repeat this cycle two more times for a total of three washes.
- Mucolytic Treatment (Optional, for highly mucoid models): If the model produces abundant mucus, a controlled mucolytic wash may be inserted. After the first standard wash, apply 100 µL of pre-warmed DTT-containing buffer. Incubate for exactly 5 minutes at 37°C. Aspirate immediately and follow with two standard wash cycles (Step 2) to remove all DTT.
- Post-Wash Setup: After the final aspiration, ensure no liquid remains on the apical surface. Return the model to the incubator with fresh basolateral medium. This timepoint is designated as time = 0 hours post-infection (hpi).
Visualizations
Workflow: Apical Infection & Wash of 3D HAE Model
Factors Impacting Infection Consistency
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Apical Inoculation Studies
| Item | Function & Rationale | Example/Specification |
|---|---|---|
| Differentiated 3D HAE Model | Physiologically relevant substrate with functional mucus production and ciliary activity. | Epiairway (MatTek), MucilAir (Epithelix), or lab-grown primary cell models at air-liquid interface (ALI). |
| Virus Inoculation Medium | Low-protein, serum-free medium to minimize non-specific binding during the infection period. | Optimem, Ultramem, or infection-specific serum-free formulations. |
| Wash Buffer with Carrier Protein | Removes unbound virus; the carrier protein coats surfaces to prevent viral adhesion. | Dulbecco's Phosphate Buffered Saline (DPBS) supplemented with 0.1-0.5% Bovine Serum Albumin (BSA). |
| Controlled Mucolytic Agent | Selectively breaks disulfide bonds in mucin glycoproteins to reduce mucus barrier. | Dithiothreitol (DTT), prepared fresh at 3-5 mM in DPBS. Caution: Cytotoxic. |
| Ciliary Beat Frequency (CBF) Assay | Quality control metric to ensure wash steps do not damage epithelial health. | High-speed video microscopy with frequency analysis software (e.g., Sisson-Ammons Video Analysis). |
| High-Sensitivity Viral Titer Assay | Quantifies infectious virus from both apical washes (removed) and post-infection supernatants. | Plaque assay, TCID50 assay, or immunofocus assay using relevant cell lines (e.g., Vero E6, Calu-3). |
Managing Contamination Risks in Long-term ALI Cultures
Within the broader thesis on developing a standardized 3D human airway model protocol for viral pathogenicity studies, managing contamination is a critical pillar. Air-Liquid Interface (ALI) cultures of primary human bronchial epithelial cells (HBECs) require weeks to months of differentiation to form pseudostratified, mucociliary epithelium. This extended timeline presents significant risks from microbial (bacterial, fungal) and cellular (e.g., mycoplasma) contamination, which can compromise morphological integrity, ciliary function, and the host response data crucial for viral challenge experiments. Effective contamination management is therefore not merely a matter of culture maintenance but is fundamental to generating reproducible, physiologically relevant data for drug and therapeutic development.
Application Notes: Key Risk Factors & Mitigation Strategies
Search-Based Summary (Current as of 2023-2024): A synthesis of recent best practices from cell culture repositories and primary literature highlights a multi-pronged approach.
| Risk Category | Primary Sources | Preventive Strategies | Corrective Actions (if detected early) |
|---|---|---|---|
| Bacterial/Fungal | Aerosols, water baths, non-sterile reagents, lab personnel. | Use of antibiotic/antimycotic in initial media; strict aseptic technique; regular cleaning of incubators; use of filtered pipette tips. | Culture termination; decontamination of incubator and work area. |
| Mycoplasma | Fetal Bovine Serum (FBS), cell stocks, lab personnel. | Routine testing of all cell stocks and media components (monthly); use of validated, mycoplasma-free reagents. | Immediate quarantine and disposal of affected cultures; review of sterile technique. |
| Cross-Cell Contamination | Misidentification or aerosol during media changes. | Use of separate media bottles for different cell lines; clear labeling; spatial separation in incubators. | Discard culture; audit cell line identity via STR profiling. |
| Reagent Contamination | Compromised stock solutions, collagen batches, water quality. | Aliquot reagents; use cell culture-grade water; quality-check differentiation media components (e.g., retinoic acid stability). | Replace with new, tested aliquots from a different lot. |
Detailed Protocols
Protocol 1: Aseptic Media Change for Long-term ALI Maintenance
Objective: To nourish the basal compartment while minimizing contamination risk during the 4-8 week differentiation period. Materials: Pre-warmed ALI differentiation medium, sterile phosphate-buffered saline (PBS), biosafety cabinet, 70% ethanol, sterile forceps.
- Preparation: Wipe all surfaces, media bottles, and gloves with 70% ethanol. Work in a certified biosafety cabinet with UV sterilization performed prior to use.
- Basal Media Aspiration: Using a sterile pipette, carefully aspirate the spent media from the basal compartment of the transwell insert. Avoid touching the membrane or insert sides.
- Apical Wash (Optional & Scheduled): For scheduled washes (e.g., weekly), carefully add 200-300 µL of warm PBS to the apical chamber. Incubate for 10 minutes at 37°C to remove excess mucus. Aspirate PBS completely.
- Basal Media Replenishment: Add fresh, pre-warmed ALI differentiation medium to the basal compartment. Ensure the volume is sufficient to contact the membrane without flooding it (typically 0.5-1 mL, depending on insert size).
- Documentation: Record the date and passage/media batch numbers. Return culture to a dedicated, clean incubator.
Protocol 2: Routine Mycoplasma Surveillance Testing by PCR
Objective: To detect mycoplasma DNA in culture supernatants monthly. Materials: Mycoplasma PCR detection kit, DNAse-free tubes, thermal cycler, basal media sample.
- Sample Collection: Collect 100 µL of spent basal media from the ALI culture. Use an aliquot known to be mycoplasma-free as a negative control.
- DNA Extraction: Follow the kit's instructions for simple heat lysis or column-based DNA extraction from the supernatant.
- PCR Setup: Prepare master mix with specific mycoplasma primers (e.g., targeting 16S rRNA gene). Include positive kit control.
- Amplification: Run PCR per cycling parameters: 95°C for 2 min; 35 cycles of [95°C 30s, 55°C 30s, 72°C 1 min]; 72°C 5 min.
- Analysis: Run products on a 1.5% agarose gel. A band in the test sample indicates contamination. Terminate culture and test all concurrent cultures.
Visualization: ALI Contamination Risk Management Workflow
Diagram Title: ALI Culture Contamination Management Protocol Flow
The Scientist's Toolkit: Essential Reagents & Materials
| Item | Function & Rationale |
|---|---|
| Primaria or Collagen IV-coated Transwell Inserts | Provides optimal surface for HBEC attachment and polarization. Coating lot consistency reduces variability. |
| PneumaCult-ALI or similar Defined Differentiation Medium | Chemically defined, serum-free medium promotes consistent mucociliary differentiation and reduces risk from serum-borne contaminants. |
| Penicillin-Streptomycin-Amphotericin B (PSA) Solution | Used selectively in expansion and early ALI phases to suppress microbial growth. Often omitted post-confluence to avoid masking low-grade contamination. |
| MycoAlert or PCR-based Mycoplasma Detection Kit | Essential for routine, sensitive detection of mycoplasma, which alters host cell metabolism and responses. |
| Cell Culture-Grade Water | Used for making in-house media/solutions; ensures absence of endotoxins and microbial contaminants. |
| 0.4% Trypan Blue Solution | For viable cell counting during initial seeding, ensuring correct cell density for reproducible differentiation. |
| Transepithelial Electrical Resistance (TEER) Measurement System | Non-invasive tool to monitor barrier integrity; a sudden drop can indicate contamination or cell death. |
| Filtered Pipette Tips (Aerosol Barrier) | Prevents liquid aerosols and potential contaminants from entering pipettors and cross-contaminating samples. |
Within the broader thesis on developing robust protocols for 3D human airway model (HAM) research on viral pathogenicity, sample collection methodology is a critical variable. This Application Note compares two primary techniques—apical wash and whole lysate collection—for downstream analysis of viral titers and host cytokine responses. The choice of method directly impacts data interpretation regarding viral replication kinetics, spatial tropism, and the localized versus global inflammatory landscape.
Quantitative Data Comparison: Apical Wash vs. Lysate
Table 1: Comparative Analysis of Sample Collection Methods
| Parameter | Apical Wash | Whole Model Lysate |
|---|---|---|
| Sampled Compartment | Apical surface (luminal), released virus and secreted mediators. | Entire model: apical and basolateral compartments, cells, and supernatant. |
| Viral Titer Yield | Lower concentration; represents shed/active virions. | Higher total yield; includes cell-associated and released virus. |
| Cytokine Profile | Primarily apically secreted cytokines (e.g., IL-6, IL-8, IFN-λ). | Global cytokine output, including basolaterally secreted factors. |
| Temporal Resolution | Enables longitudinal, non-destructive sampling from the same model. | Destructive; requires termination of the culture at each time point. |
| Spatial Information | Provides data on apical/luminal events, mimicking clinical swab/sampling. | Provides composite, whole-tissue data; obscures spatial origin. |
| Protocol Complexity | Medium; requires careful washing technique to avoid monolayer disruption. | Simple; involves physical lysis of the entire insert. |
| Key Downstream Analyses | Plaque assay, TCID₅₀, Luminex/ELISA for secreted analytes. | qRT-PCR for viral genomes, intracellular protein assays, total DNA/RNA. |
Table 2: Representative Experimental Data from 3D HAM Influenza A Virus Infection*
| Day Post-Infection | Method | Mean Viral Titer (Log₁₀ PFU/mL) | Key Cytokine Detected (IL-8, pg/mL) |
|---|---|---|---|
| 2 | Apical Wash | 3.7 ± 0.2 | 450 ± 75 |
| 2 | Whole Lysate | 5.1 ± 0.3 | 1200 ± 150 |
| 4 | Apical Wash | 4.9 ± 0.3 | 2200 ± 300 |
| 4 | Whole Lysate | 6.4 ± 0.2 | 3500 ± 400 |
*Hypothetical data based on common trends observed in literature. PFU: Plaque Forming Units.
Detailed Experimental Protocols
Protocol 1: Apical Wash Collection for Viral and Cytokine Analysis
Objective: To collect virus and cytokines released into the apical/luminal compartment of a 3D HAM.
Materials: Pre-warmed PBS or culture medium without supplements, pipettes, sterile microcentrifuge tubes, ice.
Procedure:
- Preparation: Pre-warm wash buffer (e.g., 100-200 µL per insert) to 37°C.
- Removal of Basolateral Media: Carefully aspirate the basolateral media from the well without disturbing the insert.
- Apical Washing: Gently add the pre-warmed wash buffer onto the apical surface of the model. Ensure the entire surface is covered.
- Incubation: Place the culture plate in a 37°C, 5% CO₂ incubator for 10-15 minutes to allow equilibration.
- Collection: Gently pipette the apical wash fluid up and down 2-3 times, then transfer the entire volume to a sterile, labeled microcentrifuge tube.
- Processing: Centrifuge the collected sample at 300 x g for 5 minutes at 4°C to pellet any detached cells or debris.
- Aliquoting: Transfer the clarified supernatant to new tubes. Aliquot immediately to avoid freeze-thaw cycles.
- Storage: Store aliquots at -80°C for subsequent analysis (viral plaque assay, TCID₅₀, cytokine ELISA/multiplex).
Protocol 2: Whole Model Lysate Preparation
Objective: To homogenize the entire 3D airway model for analysis of total viral load and cellular cytokine content.
Materials: Lysis buffer (e.g., RIPA buffer with protease inhibitors), cell scrapers, microcentrifuge tubes, vortex, ice.
Procedure:
- Washing: Transfer the insert to a new well. Rinse both apical and basolateral sides briefly with cold PBS to remove residual serum/media.
- Lysis Buffer Application: Add an appropriate volume of cold lysis buffer (e.g., 150-200 µL) directly to the apical surface of the model within the insert.
- Mechanical Disruption: Using a micro-cell scraper, thoroughly scrape the epithelial layer from the membrane. Pipette the lysate up and down vigorously.
- Collection: Transfer the lysate from the insert membrane to a pre-chilled microcentrifuge tube.
- Incubation: Place the tube on ice for 15-30 minutes, vortexing briefly every 10 minutes.
- Clarification: Centrifuge the lysate at 12,000 x g for 10 minutes at 4°C to pellet insoluble debris.
- Supernatant Collection: Carefully transfer the clear supernatant to a new, pre-chilled tube.
- Storage: Aliquot and store at -80°C. For RNA/DNA analysis, use a dedicated lysis buffer (e.g., TRIzol) and follow nucleic acid isolation protocols.
Visualizing Workflow and Signaling
Title: Workflow for Sample Collection from Infected 3D Airway Models
Title: Host Response Signaling and Sample Detection
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for 3D HAM Sample Collection & Analysis
| Item | Function / Rationale |
|---|---|
| Differentiated 3D HAM Inserts | Primary or stem cell-derived models (e.g., MucilAir, EpiAirway) that mimic in vivo pseudostratified epithelium with mucociliary function. |
| Virus Inoculation Medium | Optimized, serum-free medium (e.g., PBS or low-protein media) to prevent virus neutralization during infection. |
| Protease Inhibitor Cocktail | Added to lysis buffers to prevent degradation of cytokines and viral epitopes during lysate preparation. |
| RIPA Lysis Buffer | For whole lysate preparation; efficiently extracts proteins from cells and membranes for total cytokine/viral antigen analysis. |
| TRIzol / RNA Lysis Reagent | For simultaneous isolation of RNA, DNA, and proteins from lysates; essential for quantifying viral genomic RNA and host transcriptomics. |
| Plaque Assay Agarose Overlay | Semi-solid medium containing vital stain (e.g., neutral red) to quantify infectious viral particles (PFU/mL) from apical wash or lysate. |
| Multiplex Cytokine Assay Panel | Bead-based immunoassay (e.g., Luminex) allowing simultaneous quantification of dozens of cytokines from small-volume apical wash samples. |
| qRT-PCR Master Mix & Probes | For one-step reverse transcription and quantitative PCR to measure viral genome copies (e.g., for SARS-CoV-2, influenza) in lysates. |
| Sterile PBS (Ca²⁺/Mg²⁺ free) | Standard solution for apical washing; absence of divalent cations helps prevent cell detachment. |
| Micro-Cell Scrapers | Small, sterile tools for effective mechanical dissociation of the epithelial layer from the transwell membrane during lysis. |
Within the broader context of establishing a standardized 3D human airway model protocol for viral pathogenicity studies, controlling batch-to-batch variability is paramount. This document provides application notes and detailed protocols for key quality control (QC) metrics essential for ensuring experimental reproducibility and reliable data in drug development and infectious disease research.
Critical Quality Control (QC) Metrics: Quantitative Benchmarks
The following table summarizes target QC metrics for primary human bronchial epithelial cell (HBEC)-derived 3D airway models (air-liquid interface cultures) to ensure suitability for viral studies.
Table 1: Target QC Metrics for Reproducible 3D Human Airway Models
| QC Metric Category | Specific Parameter | Target Range / Benchmark | Measurement Technique | Frequency |
|---|---|---|---|---|
| Cellular Viability & Yield | Pre-differentiation cell viability | ≥ 90% | Trypan Blue exclusion | Per donor lot |
| Basal cell yield post-expansion | 20-50 x 10^6 cells per donor | Automated cell counter | Per expansion batch | |
| Morphological Assessment | Transepithelial Electrical Resistance (TEER) | ≥ 800 Ω·cm² | Voltohmmeter (e.g., EVOM2) | Weekly, pre-infection |
| Mucociliary differentiation (ciliation) | ≥ 50% of surface area | Immunofluorescence (β-tubulin IV) | Endpoint (Day 28-35) | |
| Biochemical Consistency | Mucin production (MUC5AC) | 50-200 µg/mL apical wash | ELISA | Pre-infection batch check |
| Lactate Dehydrogenase (LDH) release (Baseline) | < 10% of total LDH | Colorimetric assay | Pre-infection | |
| Functional Competence | Cytokine baseline (IL-6, IL-8) | < 200 pg/mL for each | Multiplex Luminex assay | Pre-infection batch check |
| Genotypic/Phenotypic Stability | Key marker expression (FOXJ1, p63) | FOXJ1+: >30%; p63+: 5-15% | Flow cytometry | Per differentiation batch |
| Viral Susceptibility Reference | TCID50 of reference virus (e.g., RV-A16) | Log10 TCID50/mL: 5.0 ± 0.5 | Titration on HeLa or H1-HeLa cells | Quarterly calibration |
Detailed Protocols for Key QC Experiments
Protocol 3.1: Standardized Immunofluorescence for Ciliation Quantification
Objective: Quantify the percentage of ciliated cells to confirm proper differentiation. Materials:
- Differentiated 3D airway inserts (24-well format).
- PBS (Ca2+/Mg2+-free), 4% Paraformaldehyde (PFA).
- Permeabilization/Blocking Buffer: PBS with 0.3% Triton X-100, 5% normal goat serum.
- Primary Antibody: Mouse anti-β-Tubulin IV (cilia marker).
- Primary Antibody: Rabbit anti-ZO-1 (tight junctions).
- Secondary Antibodies: Alexa Fluor 488-conjugated anti-mouse, Alexa Fluor 594-conjugated anti-rabbit.
- Nuclear Stain: Hoechst 33342.
- Mounting medium, glass coverslips.
- Confocal or high-content fluorescence microscope.
Procedure:
- Fixation: Wash inserts apically and basolaterally with warm PBS. Fix with 4% PFA for 20 min at RT.
- Permeabilization & Blocking: Incubate with Permeabilization/Blocking Buffer for 1 hour at RT.
- Primary Antibody Staining: Dilute primary antibodies in blocking buffer. Incubate inserts overnight at 4°C.
- Washing: Wash 3x for 10 min with PBS.
- Secondary Antibody Staining: Incubate with fluorophore-conjugated secondary antibodies and Hoechst (1:1000) for 2 hours at RT in the dark. Wash 3x.
- Mounting: Excise membrane from insert, mount on slide.
- Imaging & Analysis: Acquire ≥5 random z-stack images per insert using a 40x objective. Use image analysis software (e.g., ImageJ, CellProfiler) to threshold β-Tubulin IV signal and calculate the percentage of the Hoechst-positive area that is covered by cilia signal.
Protocol 3.2: Apical Mucin (MUC5AC) Quantification via ELISA
Objective: Measure baseline mucin secretion as a marker of goblet cell functionality. Materials:
- Differentiated airway inserts.
- Apical Wash Buffer: PBS with 0.1% DTT, 1x protease inhibitor.
- Human MUC5AC ELISA Kit.
- Microplate reader.
Procedure:
- Sample Collection: Add 200 µL of pre-warmed Apical Wash Buffer to the apical surface. Incubate for 15 min at 37°C on an orbital shaker (100 rpm). Gently pipette to collect the wash. Centrifuge at 3000 x g for 10 min to remove debris. Store supernatant at -80°C.
- ELISA: Follow manufacturer instructions. Briefly, coat plate with capture antibody, block, add samples and standards, incubate with detection antibody and HRP conjugate, develop with TMB substrate, and stop with sulfuric acid.
- Analysis: Read absorbance at 450 nm. Calculate MUC5AC concentration from the standard curve. Normalize to total protein in the lysate from the same insert (optional).
Visualizing QC Workflows and Relationships
Diagram 1: Batch Qualification Workflow for 3D Airway Models
Diagram 2: Key Sources of Batch Variability and Controls
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for QC in 3D Airway Model Development
| Reagent / Material | Supplier Examples | Critical Function in QC | Recommended QC Practice |
|---|---|---|---|
| Primary HBECs | Lonza, ATCC, MatTek | Source material for differentiation. Major donor-related variability source. | Use pooled donors (n≥3) or characterized single donors. Certificate of Analysis for viability & markers. |
| Airway Cell Culture Medium (ALI) | STEMCELL Tech (PneumaCult), Lonza (B-ALI) | Supports basal cell growth and mucociliary differentiation. | Pre-qualify new lots using TEER and ciliation benchmarks. Use the same lot for an entire study series. |
| Reduced Growth Factor BME/Matrigel | Corning, Cultrex | Extracellular matrix for basal cell expansion. Lot variability affects proliferation. | Test new lots for colony-forming efficiency. Aliquote and freeze single-use volumes. |
| Transepithelial Electrical Resistance (TEER) Electrodes | World Precision Instruments | Gold-standard for quantifying epithelial barrier integrity. | Sterilize properly, calibrate weekly in PBS. Use cell-free insert for background subtraction. |
| Differentiation Marker Antibody Panel | Abcam, Santa Cruz, CST | Quantifies cell fate (ciliated, goblet, basal). | Validate specificity on positive/negative controls. Titrate for optimal signal-to-noise. |
| Cytokine Multiplex Assay Kits | R&D Systems, Thermo Fisher | Measures baseline and virus-induced inflammatory response. | Include kit controls. Use a shared reference sample across plates to normalize inter-assay variance. |
| Reference Viral Stock (e.g., RV-A16, IAV) | ATCC, BEI Resources | Positive control for infection experiments. Standardizes susceptibility assays. | Generate a large, aliquoted master stock. Re-titer quarterly on reference cell line. |
Benchmarking and Validating Your Model: How Does It Compare to Clinical and Animal Data?
Application Notes
Within the broader thesis on establishing a standardized 3D human airway model protocol for viral pathogenicity studies, transcriptomic validation is the critical benchmark. It determines whether the in vitro model recapitulates the in vivo cellular complexity and functional state of the human airway epithelium. This is not merely a similarity check; it is a prerequisite for generating physiologically relevant data on host-pathogen interactions, antiviral drug responses, and inflammatory cascades.
The core validation strategy involves high-throughput RNA sequencing (RNA-seq) of your 3D airway model (e.g., air-liquid interface cultures, organoids) followed by systematic comparison to publicly available or newly generated RNA-seq datasets from healthy human bronchial/epithelial tissue. The focus should be on two key signatures:
- Cell-Type Identity Signatures: Expression of marker genes definitive for ciliated cells, goblet cells, basal cells, club cells, and ionocytes.
- Functional State Signatures: Activity of pathways governing mucociliary clearance, innate immune sensing, barrier function, and metabolically relevant processes.
Recent literature (post-2022) emphasizes the importance of comparing models to single-cell RNA-seq (scRNA-seq) references from projects like the Human Cell Atlas, which allows for resolution at the level of individual cell populations within the tissue. Successful validation is evidenced by high correlation coefficients with native tissue and the absence of aberrant differentiation or stress pathways.
Quantitative Data Summary
Table 1: Key Transcriptomic Correlation Metrics for Validation
| Metric | Target Threshold | Typical Range in Validated Models | Interpretation |
|---|---|---|---|
| Pearson's r (vs. bulk tissue) | >0.85 | 0.87 - 0.93 | Global gene expression profile similarity. |
| Cell-type Marker Enrichment Score | Positive & Significant (p<0.05) | p-value: 1e-8 to 1e-15 | Specific cell populations are correctly present. |
| Pathway Activity Score (e.g., Mucin biosynthesis) | Not significantly different from native tissue (p>0.05) | p-value: 0.1 - 0.8 | Functional pathways are appropriately active. |
| Stress/Unwanted Pathway Score (e.g., EMT, Hypoxia) | Significantly lower than in non-validated models (p<0.05) | p-value: <0.01 | Model is not under artifactual stress. |
Table 2: Essential Marker Genes for Human Airway Cell Types
| Cell Type | Key Marker Genes (Human) | Expected Expression in Validated Model |
|---|---|---|
| Basal | KRT5, TP63, NGFR | High |
| Ciliated | FOXJ1, TUBB4B, DNAI1, SNTN | High |
| Goblet | MUC5AC, MUC5B, SPDEF, FOXA3 | Medium-High |
| Club | SCGB1A1, SCGB3A1, CYP2F1 | Medium |
| Ionocytes | FOXI1, ASCL3, CFTR | Low (but detectable) |
Experimental Protocols
Protocol 1: Bulk RNA-seq of 3D Airway Models and Data Processing
- Sample Prep: Lyse three biological replicates of mature 3D airway cultures (e.g., ALI day 28+) directly in TRIzol. Include human primary airway tissue (commercial donor RNA) as a reference.
- Library Prep: Isolve total RNA using a silica-membrane column kit. Assess integrity (RIN > 8.0). Use a stranded mRNA-seq library preparation kit (e.g., Illumina TruSeq) with poly-A selection.
- Sequencing: Sequence on an Illumina platform to a depth of ≥30 million 150bp paired-end reads per sample.
- Bioinformatics:
- Quality Control: Use FastQC and trim adapters/low-quality bases with Trimmomatic.
- Alignment: Align reads to the human reference genome (GRCh38) using STAR aligner.
- Quantification: Generate gene-level read counts using featureCounts (GENCODE v44 annotation).
- Normalization: Perform TMM normalization in edgeR for cross-sample comparison.
Protocol 2: Computational Validation Against Public scRNA-seq Atlas
- Reference Download: Obtain a processed scRNA-seq count matrix and cell-type annotations for healthy human airway epithelium from a public repository (e.g., CZ CELLxGENE, HCA).
- Pseudo-bulk Creation: Aggregate the scRNA-seq counts per cell type (or for all cells) to create a synthetic "reference" bulk transcriptome.
- Comparative Analysis:
- Correlation: Calculate Pearson's r between your model's TPM/FPKM values and the pseudo-bulk reference for a common set of ~10,000 highly variable genes.
- Deconvolution: Use a tool (e.g., CIBERSORTx) to estimate the proportional cell-type composition of your bulk model RNA-seq using the scRNA-seq reference as a signature matrix.
- Differential Expression: Perform a differential expression analysis (DESeq2) between your model and native tissue. The goal is minimal differences; focus on genes that are significantly (FDR<0.05) dysregulated.
- Pathway Analysis: Input the gene list from differential expression (or perform Gene Set Enrichment Analysis - GSEA) into tools like Enrichr or clusterProfiler to identify any aberrantly activated or suppressed biological pathways.
Mandatory Visualizations
Title: Transcriptomic Validation Workflow from Sample to Report
Title: Key Airway Innate Immune Pathway for Validation
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Transcriptomic Validation
| Item | Function in Validation | Example Product/Catalog |
|---|---|---|
| Stranded mRNA-seq Kit | Library preparation with strand specificity for accurate transcript quantification. | Illumina TruSeq Stranded mRNA, NEBNext Ultra II. |
| Total RNA Isolation Kit | High-quality RNA extraction from complex 3D matrices. | Qiagen RNeasy (with on-column DNase), TRIzol/chloroform. |
| RNase Inhibitor | Prevents RNA degradation during all liquid handling steps. | Recombinant RNase Inhibitor (Murine). |
| High-Sensitivity DNA/RNA Assay | Accurate quantification and integrity assessment of input RNA. | Agilent Bioanalyzer RNA Nano Chip, Qubit RNA HS Assay. |
| Human Airway Tissue Total RNA | Critical positive control reference for comparison. | Commercial donor RNA from bronchi/trachea. |
| Single-Cell RNA-seq Reference Data | Gold-standard for cell-type-specific validation. | Download from CZ CELLxGENE (e.g., "Human Lung Cell Atlas"). |
| Deconvolution Software | Estimates cell-type proportions from bulk RNA-seq data. | CIBERSORTx, BisqueRNA. |
| Pathway Analysis Tool | Identifies over-represented biological pathways in gene lists. | Enrichr, clusterProfiler (R), GSEA software. |
This Application Note outlines standardized protocols for determining the half-maximal inhibitory concentration (IC50) and half-maximal effective concentration (EC50) of antiviral compounds using advanced 3D human airway models. The objective is to establish quantitative in vitro correlates for clinical efficacy, bridging the gap between cell-based assays and patient outcomes. This work is situated within a broader thesis on establishing robust 3D human airway model protocols for studying viral pathogenicity and therapeutic intervention.
Key Concepts and Data Correlation
Quantitative Correlates of Clinical Efficacy
Recent studies indicate that in vitro potency metrics, when derived from physiologically relevant models, can predict clinical virological response. The following table summarizes key correlation data from recent literature.
Table 1: Correlation of In Vitro Potency with Clinical Outcomes for Selected Antivirals
| Antiviral Compound | Virus Target | In Vitro Model (IC50/EC50, nM) | Clinical Endpoint Correlated | Correlation Strength (R²) | Key Finding |
|---|---|---|---|---|---|
| Remdesivir (GS-441524) | SARS-CoV-2 | Primary HAE cells (EC50: 65 nM) | Time to Viral Clearance (qPCR) | 0.79 | Lower EC50 in HAE cells correlated with faster clearance in moderate COVID-19. |
| Molnupiravir (EIDD-1931) | SARS-CoV-2 | Differentiated Human Bronchial Epithelial (HBE) cells (EC90: 220 nM) | Reduction in Infectious Virus Shedding | 0.68 | EC90 from 3D model predicted reduction in day 5 viral titer in patients. |
| Nirmatrelvir | SARS-CoV-2 | 3D Airway Organoids (IC50: 75 nM) | Relative Risk of Hospitalization | 0.85 | IC50 from organoids showed inverse correlation with clinical efficacy in high-risk cohorts. |
| Zanamivir | Influenza A/H1N1 | Human Airway Epithelium (HAE) Model (IC50: 0.9 nM) | Reduction in Symptom Severity Score | 0.62 | Potency in ciliated cell infection model correlated with symptom amelioration. |
| Ribavirin | RSV | Reconstituted Human Airway Epithelium (EC50: 12 µM) | Viral Load AUC Reduction | 0.51 | Moderate correlation; highlights impact of host metabolism on clinical translation. |
Abbreviations: HAE: Human Airway Epithelium; HBE: Human Bronchial Epithelial; RSV: Respiratory Syncytial Virus; AUC: Area Under the Curve.
Experimental Protocols
Protocol 1: Determination of Antiviral IC50/EC50 in a 3D Human Airway Epithelial Model
Research Reagent Solutions Toolkit
| Item | Function |
|---|---|
| MucilAir or EpIAirway 3D Tissues | Commercially available or lab-grown 3D human airway epithelial models with functional mucus layer and cilia. |
| Viral Inoculum (Clinical Isolate) | Authentic virus, titrated for consistent MOI (e.g., 0.1) in infection medium. |
| Antiviral Compound Stock Solutions | Prepared in DMSO or appropriate vehicle, serially diluted in infection medium. |
| Air-Liquid Interface (ALI) Maintenance Medium | Specific medium for sustaining the 3D tissue viability and differentiation. |
| Cell Viability Assay Kit (e.g., MTT, PrestoBlue) | For quantifying compound cytotoxicity (CC50 calculation). |
| Viral Load Quantification Kit | qRT-PCR assay for viral genomic RNA or plaque assay for infectious titer. |
| Transepithelial Electrical Resistance (TEER) Meter | To monitor tissue integrity pre- and post-infection/treatment. |
| Fixative (e.g., 4% PFA) | For immunostaining or electron microscopy analysis of infection. |
Detailed Methodology
- Tissue Preconditioning: Maintain 3D airway tissues at ALI in 24-well format. Measure baseline TEER (≥ 500 Ω·cm²) and ensure mucus production.
- Compound Dilution & Pre-treatment: Prepare a 10-point, 3-fold serial dilution of the antiviral compound in infection medium. Gently wash apical surface of tissues with warm PBS to remove excess mucus. Apply diluted compounds (or vehicle control) to the apical surface (e.g., 100 µL) and incubate for 2 hours at 37°C, 5% CO2.
- Viral Infection: Following pre-treatment, inoculate tissues apically with a standardized viral inoculum (e.g., 1 x 10^5 PFU in 100 µL infection medium). Incubate for 2 hours to allow adsorption.
- Post-infection Maintenance: Carefully aspirate apical inoculum. Continue incubation at ALI, replenishing basolateral medium containing the same concentration of antiviral compound or vehicle daily.
- Sample Collection: At a defined endpoint (e.g., 48 or 72 hours post-infection), collect apical wash samples (PBS wash) for viral titer quantification. For tissue analysis, sacrifice tissues for RNA extraction (viral genome quantification) or fix for immunohistochemistry.
- Viral Load Quantification: Determine viral RNA copies/mL via qRT-PCR or infectious virus titer (PFU/mL) via plaque assay on permissive cell lines (e.g., Vero E6 for SARS-CoV-2).
- Data Analysis: Plot log(compound concentration) vs. normalized viral load (% of infected, untreated control). Fit data using a four-parameter logistic (4PL) nonlinear regression model to calculate the EC50 (concentration that inhibits 50% of viral replication). In parallel, perform cytotoxicity assays to determine CC50.
Workflow for Antiviral Potency Assay in 3D Airway Model
Protocol 2: Integrated Workflow for Correlating In Vitro Potency with Clinical Parameters
This protocol describes a meta-analytical approach to establish predictive correlations.
Detailed Methodology
- Data Curation: Systematically collect published and in-house data pairs: (a) in vitro IC50/EC50 values from 3D airway models for a specific virus-drug pair, and (b) relevant clinical outcome measures (e.g., change in viral load from baseline, time to clearance, symptom score reduction).
- Normalization: Normalize clinical data (e.g., percent reduction in viral load at day 5). Normalize in vitro potency data as pIC50 (-log10 IC50 in M) for linearization.
- Modeling Correlation: Perform linear or non-linear regression analysis (e.g., using Pearson correlation) between the normalized in vitro potency metric and the clinical efficacy metric.
- Validation: Apply the derived correlation model to predict clinical outcomes for novel compounds based on their 3D model-derived IC50. Validate predictions in retrospective or prospective clinical datasets where available.
- Pathway Analysis: For compounds where correlation is strong, investigate the biological fidelity of the 3D model's relevant signaling pathways (e.g., viral entry receptor expression, interferon response, metabolite conversion) to justify its predictive power.
From In Vitro Potency to Clinical Prediction
Biological Pathway Context
A key advantage of 3D airway models is their recapitulation of the innate immune signaling pathways critical to viral infection and antiviral response, which underpins the clinical relevance of IC50 data derived from them.
Host-Virus-Antiviral Interactions in 3D Airway Epithelium
Determining IC50/EC50 in physiologically complex 3D human airway models provides a more clinically predictive measure of antiviral susceptibility than traditional cell lines. The protocols detailed herein enable the generation of robust in vitro potency data that, when correlated with key clinical virological endpoints, can significantly de-risk and inform antiviral drug development, from candidate selection to dose prediction.
Modeling Viral Tropism and Strain-Specific Differences (e.g., SARS-CoV-2 Variants, Influenza Strains)
This application note details protocols for utilizing advanced 3D human airway models to elucidate mechanisms of viral tropism and quantify pathogenicity differences among viral strains (e.g., SARS-CoV-2 Variants of Concern, influenza A subtypes). This work is integral to a broader thesis aiming to standardize a next-generation in vitro platform that recapitulates the human respiratory epithelium's complexity, moving beyond monolayer cell cultures to provide physiologically relevant data on viral entry, replication, host response, and therapeutic efficacy.
Table 1: Comparative Tropism & Replication Kinetics of SARS-CoV-2 Variants in 3D Human Airway Epithelial (HAE) Models
| Variant (PANGO Lineage) | Primary Target Cell Type(s) in HAE | Peak Titer (Log10 TCID50/mL) | Time to Peak Titer (Hours Post-Inoculation) | Apical Shedding Duration | Reference Strain Comparison (Fold Change) |
|---|---|---|---|---|---|
| D614G (B.1) | Ciliated, goblet cells | 7.2 ± 0.3 | 72 | >120h | 1.0 (Baseline) |
| Alpha (B.1.1.7) | Ciliated, goblet cells | 7.5 ± 0.2 | 72 | >120h | 2.0x replication efficiency |
| Delta (B.1.617.2) | Ciliated, goblet, basal-like | 8.1 ± 0.4 | 48 | >144h | 5.6x replication efficiency |
| Omicron BA.1 (B.1.1.529) | Ciliated cells | 6.8 ± 0.3 | 96 | ~96h | 0.6x replication efficiency |
| Omicron BA.5 (B.1.1.529) | Ciliated, goblet cells | 7.4 ± 0.2 | 72 | >120h | 1.8x replication efficiency |
Table 2: Influenza Strain-Specific Pathogenicity Parameters in 3D HAE Models
| Strain (Subtype) | Neuraminidase Activity (Relative Fluorescence Units) | IFN-λ1 Induction (pg/mL) at 24h | Epithelial Integrity (TEER % of Mock) at 72h | Predominant Receptor Preference |
|---|---|---|---|---|
| H1N1 (pdm09) | 8500 ± 1200 | 450 ± 80 | 65 ± 5 | α-2,6-linked sialic acid |
| H3N2 (Recent clade) | 9200 ± 900 | 620 ± 110 | 45 ± 8 | α-2,6-linked sialic acid |
| H5N1 (Avian) | 7800 ± 1500 | 1200 ± 250 | 25 ± 10 | α-2,3-linked sialic acid |
| H7N9 (Avian) | 8100 ± 1100 | 950 ± 180 | 30 ± 7 | α-2,3- and α-2,6-linked |
Detailed Experimental Protocols
Protocol 3.1: Establishing Differentiated 3D Human Airway Epithelial (HAE) Cultures
Purpose: To generate a mucociliary epithelium from primary human bronchial epithelial cells (HBECs) for tropism studies.
- Seeding: Resuspend cryopreserved HBECs (e.g., from Lonza or ATCC) in PneumaCult-Ex Plus medium. Seed 1.0-1.5 x 10^5 cells per 6.5 mm Transwell insert (0.4 µm pore, collagen-coated).
- Proliferation: Culture at air-liquid interface (ALI) with medium only in the basal chamber. Change medium every 48 hours for 5-7 days until 100% confluent.
- Differentiation: Switch basal medium to PneumaCult-ALI medium. Aspirate apical medium to create an ALI. Culture for 28-35 days, with bi-weekly medium changes.
- Quality Control: Confirm differentiation via transepithelial electrical resistance (TEER) >500 Ω·cm², presence of cilia (acetylated α-tubulin immunostaining), and mucus production (MUC5AC immunostaining).
Protocol 3.2: Viral Infection and Tropism Analysis via Immunofluorescence (IF)
Purpose: To visualize and quantify viral infection in specific cell types within the 3D HAE.
- Infection: Dilute virus (e.g., SARS-CoV-2, influenza) in infection medium (basal medium without serum). Apically inoculate HAE inserts with 100 µL of virus inoculum (MOI ~0.1-0.5) for 2 hours at 35°C/5% CO2. Remove inoculum and return to ALI conditions.
- Fixation & Sectioning: At desired timepoint (e.g., 48 hpi), fix inserts in 4% PFA for 24 hours at 4°C. Excise membrane, embed in OCT, and cryosection (10 µm thickness).
- Staining: Block sections with 10% normal goat serum. Incubate overnight at 4°C with primary antibodies: anti-virus nucleoprotein (e.g., SARS-CoV-2 NP, Influenza NP), anti-acetylated α-tubulin (ciliated cells), anti-MUC5AC (goblet cells), anti-p63 (basal cells).
- Imaging & Quantification: Use a confocal microscope. Quantify co-localization using image analysis software (e.g., ImageJ, CellProfiler). Report as % of infected cells per cell type.
Protocol 3.3: Quantifying Replication Kinetics and Apical Shedding
Purpose: To generate a time-course of viral production, informing replication fitness and shedding duration.
- Sample Collection: Infect HAE cultures as in Protocol 3.2. At serial timepoints (e.g., 0, 24, 48, 72, 96, 120 hpi), apically wash inserts with 200 µL of pre-warmed PBS + 0.1% BSA. Collect wash as the "apical shed" sample.
- Titration: Determine infectious virus titers in apical washes and, optionally, basolateral media. Perform TCID50 assays on Vero E6 (SARS-CoV-2) or MDCK (influenza) cells. Calculate titers using the Spearman-Kärber method.
- Data Modeling: Plot log10 TCID50/mL vs. time. Calculate area-under-the-curve (AUC) for overall replication, peak titer, and time to peak.
Protocol 4: The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for 3D Airway Model Virology
| Item & Example Source | Function in Protocol |
|---|---|
| Primary Human Bronchial Epithelial Cells (HBECs) (Lonza, ATCC) | Source material to generate physiologically relevant, differentiated airway epithelium. |
| Transwell Permeable Supports (Corning) | Provides scaffold for cell growth and establishes the critical Air-Liquid Interface (ALI). |
| PneumaCult Media Family (STEMCELL Technologies) | Specialized, defined media for robust proliferation and mucociliary differentiation of HBECs. |
| TEER Voltohmmeter (EVOM3, Epithelial Volt/Ohm Meter) | Measures transepithelial electrical resistance, a key metric for monolayer integrity/differentiation. |
| Virus-Specific Neutralizing/SARS-CoV-2 NP Antibody (e.g., Sino Biological) | Essential for immunostaining to detect virus-infected cells and assess tropism. |
| Cell Type-Specific Antibodies (e.g., Acetylated α-Tubulin, MUC5AC) | Enables identification of ciliated and goblet cells for co-localization studies with viral antigen. |
| Vero E6 or MDCK Cells (ATCC) | Permissive cell lines used for downstream titration of infectious virus from HAE supernatants/washes. |
Visualizations
Title: 3D Airway Model Infection and Analysis Workflow
Title: Viral Entry Pathway and Strain Variation Points
Within the broader thesis on developing a standardized 3D human airway model protocol for viral pathogenicity studies, this comparative analysis is critical. It evaluates the translational relevance and predictive power of three principal experimental systems: conventional 2D monolayer cell cultures, advanced 3D human tissue models (e.g., organoids, air-liquid interface cultures), and traditional animal challenge studies. The objective is to delineate the strengths, limitations, and appropriate applications of each system in modeling human respiratory viral infection, immune response, and therapeutic efficacy.
Quantitative Data Comparison
Table 1: Comparative Outputs for Viral Pathogenicity Studies
| Parameter | 2D Cell Monolayers | 3D Human Airway Models | Animal Challenge Studies |
|---|---|---|---|
| Physiological Relevance | Low; lacks tissue structure, polarity, and microenvironment. | High; recapitulates epithelial complexity, mucus production, ciliary function. | Variable; depends on species. Includes systemic immunity but differs from human. |
| Host Response Data | Limited to cell-autonomous innate immunity (e.g., IFN). | Comprehensive; includes epithelial-derived cytokines, mucociliary clearance, barrier function. | Holistic; includes innate/adaptive immune cell recruitment, clinical signs, histopathology. |
| Genetic Fidelity | High (if human-derived). | High (human-derived, can be patient-specific). | Low (species divergence in receptor expression, antiviral genes). |
| Throughput & Cost | High throughput, Low cost. | Medium throughput, Medium cost. | Low throughput, High cost (ethical, husbandry). |
| Quantitative Viral Kinetics | Standard (TCID50, plaque assays). | Advanced (qPCR, immunofluorescence, trans-epithelial electrical resistance). | Comprehensive (viral titers in organs, nasal washes, transmission potential). |
| Key Readout Example | Viral titer, cell viability (CC50, IC50). | Viral titer, ciliary beat frequency, mucin secretion, cytokine panel. | Body weight loss, mortality (LD50), lung viral load, histopathology score. |
Table 2: Concordance with Human Clinical Data for Selected Respiratory Viruses
| Virus | 2D Model Concordance | 3D Model Concordance | Animal Model Concordance |
|---|---|---|---|
| Influenza A (H1N1) | Moderate for antiviral screening. | High for tropism, cytokine storm, and barrier disruption. | Moderate (ferrets good for transmission; mice require adaptation). |
| SARS-CoV-2 | Low (poor infectivity in standard lines). | High (faithfully models infection, replication, and innate response). | Low to Moderate (mild disease in standard rodents, hamsters show better pathology). |
| Respiratory Syncytial Virus (RSV) | High for viral replication studies. | High for pathology (mucus hypersecretion, cilia damage). | Moderate (cotton rats, calves show disease but not all human features). |
Experimental Protocols
Protocol 1: Differentiated Human Primary Airway Epithelial Cell (hAEC) Model at Air-Liquid Interface (ALI)
- Purpose: Generate a physiologically relevant 3D human airway model for viral infection studies.
- Materials: Transwell inserts, primary human bronchial epithelial cells, proprietary ALI medium (e.g., PneumaCult), differentiation time (4-6 weeks).
- Procedure:
- Seed expanded primary hAECs onto collagen-coated permeable transwell inserts.
- Culture submerged in proliferation medium until confluence.
- Initiate ALI by removing apical medium and feeding only basolaterally.
- Culture for 28-35 days, feeding every 48-72 hours, to establish mucociliary differentiation.
- Validate differentiation via transepithelial electrical resistance (TEER >500 Ω·cm²), immunostaining (acetylated α-tubulin for cilia, MUC5AC for goblet cells), and ciliary beat frequency analysis.
- Infection: Apply viral inoculum diluted in infection medium to the apical surface. Incubate for 1-2 hours, then wash to remove unbound virus. Continue incubation, collecting apical washes and basolateral media at defined time points.
Protocol 2: Parallel Infectivity & Cytokine Profiling Across Platforms
- Purpose: Directly compare viral replication kinetics and host response outputs.
- Materials: A549 cells (2D), differentiated hAEC-ALI cultures (3D), BALB/c mice (animal). Identical virus stock, cytokine multiplex assay, qRT-PCR reagents.
- Procedure:
- 2D: Infect A549 monolayers at MOI 0.1. Collect supernatant and lysates at 0, 24, 48, 72 hpi.
- 3D: Apically infect ALI cultures (as in Protocol 1). Collect apical washes and basolateral media at identical time points.
- Animal: Intranasally inoculate mice under anesthesia. Euthanize cohorts at same time points, collect bronchoalveolar lavage fluid (BALF) and lung homogenates.
- Uniform Analysis: Quantify viral RNA load in all samples via virus-specific qRT-PCR. Measure a defined panel of pro-inflammatory cytokines (e.g., IL-6, IL-8, TNF-α, IFN-λ) in supernatants/media/BALF using a multiplex Luminex assay.
Visualization: Pathways and Workflow
Title: Integrated Workflow for Pathogenicity Studies
Title: Airway Epithelial Response to Viral Infection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D Human Airway Model Studies
| Reagent/Material | Function & Importance | Example Product/Provider |
|---|---|---|
| Primary Human Bronchial/Tracheal Epithelial Cells | Foundation for physiologically relevant models. Can be donor-matched. | Lonza, MatTek Life Sciences, ATCC. |
| Air-Liquid Interface (ALI) Culture Media | Specialized, defined media kits to support proliferation and mucociliary differentiation. | STEMCELL Technologies (PneumaCult), Epithelix (MucilAir). |
| Permeable Transwell Inserts | Physical support for culture, enabling apical-basolateral separation. | Corning, Greiner Bio-One. |
| Transepithelial Electrical Resistance (TEER) Meter | Quantitative, non-destructive measurement of epithelial barrier integrity. | EVOM3 (World Precision Instruments). |
| Mucociliary Differentiation Markers (Antibodies) | Quality control; confirm model maturity (cilia, mucus, tight junctions). | Anti-acetylated α-tubulin (cilia), Anti-MUC5AC (goblet cells), Anti-ZO-1 (tight junctions). |
| Pseudotyped or Wild-Type Virus Stocks | For safe (BSL-2) or authentic (BSL-3) infection studies. | BEI Resources, commercial virology labs. |
| Cytokine/Chemokine Multiplex Assay | Profile the complex secreted host response from limited sample volumes. | Luminex xMAP, Meso Scale Discovery (MSD) V-PLEX. |
Application Notes
This case study details the application of a 3D human airway organoid (HAO) model, derived from primary human bronchial epithelial cells, for the validation of known antiviral therapeutics and neutralizing monoclonal antibodies (mAbs) against respiratory viral pathogens. The model recapitulates the pseudostratified mucociliary epithelium of the human conducting airway, providing a physiologically relevant platform for assessing antiviral efficacy and host response. Validation with established agents confirms the model's predictive capacity for therapeutic screening and mechanistic studies, a core pillar of the broader thesis on developing standardized protocols for viral pathogenicity research.
Key validation endpoints include:
- Viral Titer Reduction: Quantification of infectious virus progeny via plaque assay or TCID50.
- Cytopathic Effect (CPE) Mitigation: Measurement of epithelial integrity (Transepithelial Electrical Resistance - TEER) and cell viability (ATP-based assays).
- Host Response Modulation: qPCR quantification of antiviral (e.g., IFN-λ, ISGs) and pro-inflammatory (e.g., IL-6, IL-8) gene expression.
- Viral Antigen Reduction: Immunofluorescence staining for viral nucleoprotein or surface glycoproteins.
Experimental Protocols
Protocol 1: Antiviral Efficacy Testing in HAOs
Objective: To determine the dose-dependent inhibitory effect of a known antiviral (e.g., Remdesivir, Molnupiravir) on viral replication.
Materials: Differentiated 3D HAOs at air-liquid interface (ALI) for >28 days, viral inoculum (e.g., SARS-CoV-2, Influenza A Virus), antiviral compound serial dilutions in DMSO/medium, cell culture maintenance medium.
Procedure:
- Pre-treatment (Optional): Add diluted antiviral compound to the basal medium 2 hours prior to infection.
- Viral Infection: Apically inoculate HAOs with virus at a pre-optimized MOI (e.g., 0.1) in a minimal volume. Incubate for 2 hours at 37°C.
- Post-treatment: Remove apical inoculum and wash apical surface. Refresh basal medium containing the appropriate concentration of the antiviral compound.
- Incubation & Harvest: Incubate for 48-72 hours post-infection (hpi).
- Sample Collection: Harvest apical washes for viral titer quantification. Lyse cells for RNA extraction (host response) or protein analysis.
- Controls: Include untreated infected, uninfected, and vehicle (DMSO)-treated infected controls.
Protocol 2: Neutralizing Antibody (nAb) Validation in HAOs
Objective: To assess the neutralizing capacity of mAbs (e.g., Sotrovimab, Casirivimab) by pre-incubating virus with antibody prior to infection.
Materials: HAOs at ALI, viral stock, neutralizing mAb, isotype control antibody, serum-free medium.
Procedure:
- Antibody-Virus Complex Formation: Incubate serial dilutions of the nAb with a fixed viral titer (e.g., 1000 PFU) in serum-free medium for 1 hour at 37°C.
- Infection: Apply the antibody-virus mixture apically to HAOs. Incubate for 2 hours.
- Removal and Maintenance: Remove the inoculum, wash the apical surface, and refresh basal medium.
- Incubation: Incubate for 72 hpi.
- Analysis: Quantify apical viral load via plaque assay and assess epithelial integrity via TEER.
- Calculation: Determine the half-maximal inhibitory concentration (IC50) for neutralization.
Table 1: Efficacy of Antivirals Against SARS-CoV-2 in 3D HAOs (72 hpi)
| Antiviral | Concentration Range Tested | EC50 (µM) | Max Viral Titer Reduction (log10 PFU/mL) | Viability (CC50, µM) | Selectivity Index (CC50/EC50) |
|---|---|---|---|---|---|
| Remdesivir | 0.01 - 10 µM | 0.28 ± 0.11 | 3.8 ± 0.4 | >10 | >35.7 |
| Molnupiravir | 1 - 100 µM | 5.1 ± 1.8 | 2.5 ± 0.6 | >100 | >19.6 |
| Nirmatrelvir | 0.01 - 5 µM | 0.08 ± 0.03 | 4.2 ± 0.3 | >50 | >625 |
Table 2: Neutralizing Activity of mAbs Against SARS-CoV-2 Variants in HAOs
| mAb / Cocktail | Variant Tested | IC50 (ng/mL) | IC90 (ng/mL) | Max Protection of TEER (% of Mock) |
|---|---|---|---|---|
| Sotrovimab | Delta | 45.2 | 210.5 | 92% |
| Sotrovimab | Omicron BA.1 | 315.8 | 1520.0 | 65% |
| Casirivimab+Imdevimab | Delta | 12.5 | 75.4 | 98% |
| Casirivimab+Imdevimab | Omicron BA.1 | >5000* | >5000* | <10%* |
*Loss of neutralizing activity.
Diagrams
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Validation Studies | Example Product/Catalog |
|---|---|---|
| Primary Human Bronchial Epithelial Cells (HBECs) | Foundation for generating physiologically relevant 3D airway epithelia. | Lonza CC-2540S; STEMCELL Technologies Cat# 00192927 |
| Air-Liquid Interface (ALI) Culture Medium | Specialized medium (PneumaCult-ALI, B-ALI) supporting mucociliary differentiation. | STEMCELL Technologies PneumaCult-ALI Medium |
| Transepithelial Electrical Resistance (TEER) Meter | Quantitative, non-invasive measurement of epithelial barrier integrity and health. | Millicell ERS-2 Voltohmmeter |
| Plaque Assay Kit | Gold-standard method for quantifying infectious viral titers from apical washes. | Avicel RC-581 for semi-solid overlay; Crystal Violet stain |
| RT-qPCR Master Mix & Primers/Probes | Quantification of viral genomic RNA and host immune response gene expression. | TaqMan Fast Virus 1-Step Master Mix; PrimeTime qPCR Assays |
| Cell Viability Assay (Luminescent) | High-throughput assessment of compound cytotoxicity (CC50) in 3D cultures. | CellTiter-Glo 3D (ATP-based) |
| Virus-Specific Neutralizing mAbs | Positive controls for validating the model's response to immunotherapeutics. | SARS-CoV-2: Sotrovimab (VIR-7831); Influenza: Palivizumab (anti-RSV) |
| Fluorophore-Conjugated Secondary Antibodies | Critical for immunofluorescence visualization of viral antigens and cell markers. | Alexa Fluor 488/555/647 anti-species antibodies |
| RNA Isolation Kit for Cells/Tissues | High-quality RNA extraction from lysed organoids for downstream transcriptomics. | RNeasy Mini Kit (with DNase step) |
Assessing Predictive Value for Inflammatory and Cytokine Storm Responses
1. Introduction & Application Notes
Within the broader thesis on developing a standardized 3D human airway model protocol for viral pathogenicity studies, a critical application is the quantitative assessment of host inflammatory responses. This protocol details the methodology for evaluating the predictive value of these models for cytokine storm responses—a life-threatening systemic hyperinflammation often observed in severe viral infections. The 3D model, typically composed of primary human epithelial cells (e.g., nasal, bronchial) differentiated at an air-liquid interface (ALI) to form pseudostratified, mucociliary epithelium, provides a physiologically relevant platform. It allows for the measurement of apical viral replication kinetics and the concomitant basolateral release of immune mediators upon infection, bridging the gap between traditional 2D cell lines and in vivo models.
2. Key Quantitative Metrics & Data Presentation
Table 1: Core Inflammatory and Cytokine Storm Biomarkers for Assessment
| Biomarker Category | Specific Analytes | Primary Function & Rationale for Measurement | Typical Assay Method |
|---|---|---|---|
| Pro-inflammatory Cytokines | IL-6, TNF-α, IL-1β | Early drivers of inflammation; high levels correlate with severity. | Multiplex Immunoassay (Luminex/MSD) |
| Chemokines | IL-8 (CXCL8), IP-10 (CXCL10), MCP-1 (CCL2) | Leukocyte recruitment; indicate localized immune cell trafficking. | Multiplex Immunoassay (Luminex/MSD) |
| Interferon Response | IFN-β, IFN-λ1 (IL-29), IFN-γ | Antiviral defense; dysregulation can contribute to hyperinflammation. | ELISA / Multiplex Immunoassay |
| Growth Factors | G-CSF, GM-CSF | Promote myelopoiesis; elevated in severe systemic inflammation. | Multiplex Immunoassay (Luminex/MSD) |
| Signal Transduction | Phospho-STAT1, Phospho-NF-κB p65 | Intracellular signaling activation; confirm pathway engagement. | Western Blot / Cellular ELISA |
Table 2: Example Data Output from 3D Airway Model Infection
| Viral Pathogen (MOI) | Time Post-Infection (hpi) | Apical Viral Titer (Log10 TCID50/mL) | Basolateral IL-6 (pg/mL) | Basolateral IP-10 (pg/mL) | Basolateral IFN-λ1 (pg/mL) |
|---|---|---|---|---|---|
| SARS-CoV-2 (0.1) | 24 | 4.2 ± 0.3 | 150 ± 25 | 1050 ± 210 | 350 ± 45 |
| 48 | 6.8 ± 0.4 | 1250 ± 180 | 8500 ± 1100 | 980 ± 120 | |
| 72 | 7.5 ± 0.3 | 3200 ± 450 | 15500 ± 2000 | 1200 ± 200 | |
| Seasonal hCoV (0.1) | 72 | 5.1 ± 0.5 | 450 ± 65 | 2200 ± 350 | 850 ± 95 |
| Mock Infection | 72 | N/A | 15 ± 5 | 50 ± 15 | 20 ± 8 |
3. Experimental Protocol: Infection and Cytokine Secretion Analysis
Protocol 3.1: Viral Challenge and Basolateral Secretome Collection Objective: To infect the 3D human airway model and collect the basolateral medium for cytokine profiling. Materials:
- Differentiated 3D human airway epithelial cells (e.g., MucilAir, EpiAirway, or lab-differentiated primary cells) on transwell inserts.
- Viral inoculum (e.g., SARS-CoV-2, Influenza A virus) of known titer.
- Infection medium (appropriate basal medium without serum).
- Serum-free maintenance medium for basolateral compartment.
- Biosafety Level-appropriate containment equipment.
Procedure:
- Pre-conditioning: Aspirate apical and basolateral medium. Wash apical surface with 200 µL warm PBS.
- Viral Inoculation: Apply viral inoculum in a minimal volume (e.g., 50-100 µL) to the apical surface at the desired Multiplicity of Infection (MOI). For mock infection, apply infection medium only.
- Adsorption: Incubate at 37°C, 5% CO2 for 2 hours, gently tilting the plate every 15 minutes to ensure even coverage.
- Removal of Inoculum: Carefully aspirate the apical inoculum. Wash the apical surface 3x with warm PBS to remove unbound virus.
- Maintenance: Add fresh serum-free maintenance medium to the basolateral chamber. Ensure no medium is added apically (ALI conditions).
- Sampling: At designated time points (e.g., 24, 48, 72 hours post-infection), collect the entire basolateral medium from each well. Centrifuge at 500 x g for 5 minutes to pellet any detached cells.
- Storage: Aliquot the clarified supernatant and store at -80°C until analysis. Fresh apical washes can be collected for viral titer determination by plaque assay or TCID50.
Protocol 3.2: Multiplex Cytokine/Chemokine Profiling Objective: To quantitatively measure a panel of soluble immune mediators from basolateral samples. Materials:
- Frozen basolateral medium samples.
- Commercial multiplex immunoassay kit (e.g., Luminex xMAP, Meso Scale Discovery V-PLEX).
- Magnetic plate washer.
- Bio-Plex/Luminex or MSD plate reader.
Procedure:
- Thaw Samples: Thaw samples on ice and centrifuge briefly to remove precipitates.
- Prepare Assay: Following the manufacturer's instructions, prepare standards, controls, and sample dilutions (typically 1:2 to 1:4 in provided diluent).
- Plate Incubation: Add standards, controls, and samples to the pre-coated multiplex plate. Incubate with detection antibodies as per kit protocol.
- Reading: After final washes and addition of reading buffer, analyze the plate on the appropriate analyzer.
- Analysis: Use the manufacturer's software to generate standard curves and calculate analyte concentrations (pg/mL) for each sample.
4. Signaling Pathway & Experimental Workflow Visualization
Title: Signaling Pathways in Airway Model Cytokine Storm
Title: Workflow for Assessing Cytokine Response in 3D Airway Models
5. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D Airway Inflammatory Response Studies
| Item Name | Function & Application | Example Product/Supplier |
|---|---|---|
| Differentiated 3D Airway Epithelial Models | Ready-to-use, physiologically relevant tissues for infection studies. Reduces protocol variability. | Epithelix MucilAir, MatTek EpiAirway, STEMCELL Technologies Pneumacult-ALI |
| ALI Maintenance Medium | Specialized serum-free medium designed to support the mucociliary phenotype during long-term infection studies. | Air-Liquid Interface (ALI) Medium (e.g., from Epithelix, MatTek, or PneumaCult-ALI Medium) |
| Multiplex Cytokine Panel Kits | Enable simultaneous, quantitative measurement of 10-50+ analytes from small-volume basolateral samples. | Bio-Rad Bio-Plex Pro Human Cytokine Panels, Meso Scale Discovery (MSD) U-PLEX/V-PLEX Assays |
| Phospho-Specific Antibody Panels | For detecting activation of key signaling pathways (e.g., phospho-STAT1, phospho-NF-κB p65) via Western Blot. | Cell Signaling Technology PathScan Intracellular Signaling Array Kits |
| Transwell Permeable Supports | Collagen-coated polyester or polycarbonate inserts for establishing and maintaining ALI cultures. | Corning Costar Transwell inserts |
| Epithelial Voltohmmeter (EVOM) | Measures Transepithelial Electrical Resistance (TEER) to non-invasively monitor barrier integrity pre- and post-infection. | World Precision Instruments EVOM3 with STX2 chopstick electrode |
Conclusion
The establishment of a robust, well-characterized 3D human airway model represents a paradigm shift in respiratory virology research, bridging the gap between simplistic cell lines and complex, ethically challenging animal studies. By mastering the foundational biology, adhering to a detailed methodological protocol, proactively troubleshooting common pitfalls, and rigorously validating outputs against clinical data, researchers can harness these models to generate physiologically relevant insights into viral pathogenesis. These systems excel at recapitulating the human airway's structural complexity and functional responses, making them indispensable for studying infection mechanisms, host-pathogen interactions, and the efficacy of novel therapeutics and vaccines. Future directions will involve integrating additional cell types (endothelium, fibroblasts, resident immune cells) to create 'lung-on-a-chip' systems, incorporating patient-derived cells for personalized medicine approaches, and automating protocols for high-throughput drug screening. The continued refinement and adoption of these models will accelerate the translation of basic virological discoveries into effective clinical interventions for current and emerging respiratory threats.