Generating Functionally Active Adipose Tissue-Resident Macrophages Using 3D Culture Systems: A Protocol and Review
This article provides a comprehensive resource for researchers and drug development professionals on the generation and application of functionally active adipose tissue-resident macrophages using advanced 3D culture systems.
Generating Functionally Active Adipose Tissue-Resident Macrophages Using 3D Culture Systems: A Protocol and Review
Abstract
This article provides a comprehensive resource for researchers and drug development professionals on the generation and application of functionally active adipose tissue-resident macrophages using advanced 3D culture systems. We explore the foundational biology of adipose tissue macrophages, detail step-by-step methodological protocols for 3D co-culture systems, address common troubleshooting and optimization challenges, and present validation frameworks for comparing 3D models against traditional 2D cultures and in vivo counterparts. This synthesis of current research enables more physiologically relevant study of immunometabolic diseases and drug screening applications.
The Critical Role of Adipose Tissue Macrophages in Health and Disease
Adipose Tissue as an Endocrine and Immune Organ
The understanding of adipose tissue has undergone a fundamental paradigm shift. No longer considered a passive storage depot for excess energy, it is now recognized as a central endocrine and immune organ, crucial in regulating metabolic homeostasis, immune responses, and inter-organ communication [1]. Its dysfunction, often resulting from a chronic positive energy balance, is a hallmark of obesity and is strongly implicated in the pathogenesis of insulin resistance, type 2 diabetes, atherosclerosis, and various cancers [1]. This application note details the experimental frameworks for investigating this complex organ, with a specific focus on the role of adipose tissue-resident macrophages within 3D culture systems that mirror the in vivo microenvironment.
Adipose Tissue as a Secretary Organ
White adipose tissue (WAT) secretes a wide array of bioactive molecules—including adipokines, cytokines, and lipids—that modulate systemic energy balance, insulin sensitivity, and inflammation [1]. The secretory profile changes dramatically in obesity, shifting from an anti-inflammatory to a pro-inflammatory state.
Table 1: Key Adipokines and Their Physiological Roles
| Adipokine | Primary Secretory Source | Major Functions | Dysregulation in Obesity |
|---|---|---|---|
| Leptin | Adipocytes | Signals satiety, regulates energy balance [2] | Increased (leptin resistance) [2] |
| Adiponectin | Adipocytes | Enhances insulin sensitivity, counters inflammation [2] | Decreased [2] |
| Resistin | Adipocytes | Associated with insulin resistance [2] | Increased |
| TNF-α | Macrophages, Adipocytes | Pro-inflammatory cytokine, promotes insulin resistance [3] [2] | Increased |
| IL-6 | Macrophages, Adipocytes | Pro-inflammatory cytokine; ~50% of circulating IL-6 in obesity originates from adipose tissue [3] [2] | Increased |
The Adipose Tissue Immune Niche
Adipose tissue functions as a dynamic immune-endocrine nexus, harboring a complex network of innate and adaptive immune cells [3]. Under physiological conditions, anti-inflammatory immune cells, such as M2-polarized macrophages and regulatory T cells (Tregs), predominate to maintain tissue homeostasis [3] [2]. Obesity induces a profound immunological shift, triggering chronic, low-grade inflammation characterized by the infiltration of pro-inflammatory cells like M1 macrophages, neutrophils, and CD8+ T cells, while suppressing anti-inflammatory regulators [3] [4] [5]. This immune imbalance is a key driver of adipose tissue dysfunction and systemic metabolic disease.
Heterogeneity of Adipose Tissue Macrophages (ATMs)
Adipose tissue macrophages (ATMs) are the most abundant immune cells in WAT and are highly heterogeneous [6] [4]. Single-cell transcriptomics has revealed that the traditional M1/M2 classification represents polarization extremes, with a spectrum of intermediate phenotypes existing in vivo [4] [2].
Table 2: Major Adipose Tissue Macrophage Subpopulations in Obesity
| ATM Subpopulation | Key Markers | Primary Origin | Functional Role in Adipose Tissue |
|---|---|---|---|
| Resident TIM4+ Macrophages | F4/80hi, TIM4+, MHCIIlow |
Embryonic [6] | Tissue homeostasis, lipid buffering [6] |
| CD11c+ Lipid-Associated Macrophages (LAMs) | F4/80hi, CD11c+, TREM2+ [6] |
Bone marrow-derived [6] | Lipid-laden, form crown-like structures (CLS) around dead adipocytes; possess high bioenergetic activity [6] |
MHCIIhi Macrophages |
F4/80hi, MHCIIhi, CD11c- |
Bone marrow-derived [6] | Infiltrate during obesity; specific function under investigation |
Contrary to the long-held belief that all ATMs in obesity are detrimental, recent studies using transgenic mouse models (e.g., CD169-DTR) have revealed that certain resident ATMs protect WAT from excessive pathological remodeling during obesity. These protective functions include maintaining vascular integrity, supporting adipocyte function, and restraining fibrosis [6].
Protocol: 3D Culture of Functional Adipose Tissue-Resident Macrophages
This protocol, adapted from a 2024 study, describes a method to generate and culture functional ATMs from the stromal vascular fraction (SVF) of murine subcutaneous adipose tissue using a 3D spheroid system. This system preserves the inherent properties of resident macrophages without the need for cell sorting [7].
Materials and Reagents
- Source Tissue: Subcutaneous adipose tissue from wild-type C57BL/6 mice.
- Digestion Buffer: Collagenase solution in PBS.
- Culture Medium: DMEM/F12 supplemented with 10% FBS, 1% Penicillin/Streptomycin, and Macrophage Colony-Stimulating Factor (M-CSF).
- Culture Vessels: Ultra-low attachment plates.
- Staining Antibodies: For flow cytometry: anti-F4/80, anti-MHCII, anti-CD11c, anti-CD301, anti-TIM4.
Experimental Workflow
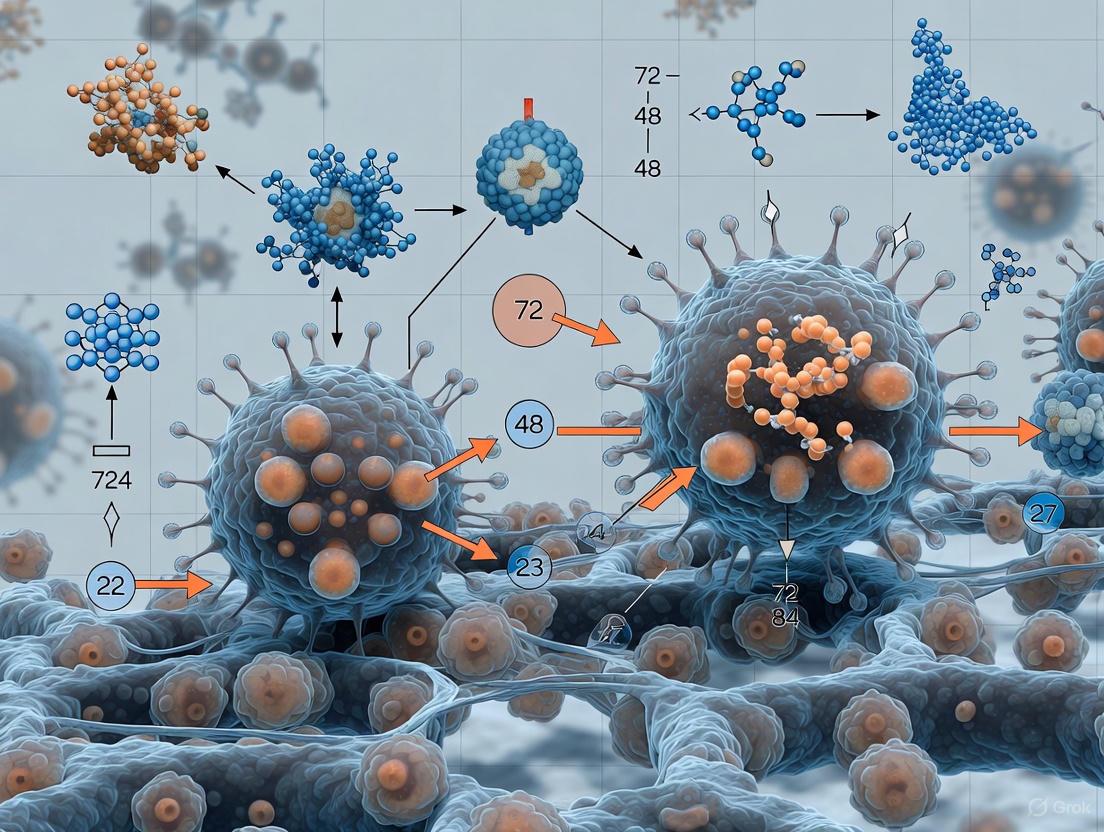
The following diagram illustrates the complete experimental workflow for generating and analyzing adipose tissue macrophages in 3D culture.
Step-by-Step Procedure
- Stromal Vascular Fraction (SVF) Isolation: Mince subcutaneous adipose tissue and digest with collagenase solution (e.g., 1 mg/mL) at 37°C for 30-60 minutes with gentle agitation. Centrifuge the digest to separate the floating adipocytes from the SVF pellet. Lyse red blood cells if necessary.
- 3D Seeding and Spheroid Formation: Resuspend the isolated SVF cells in complete culture medium supplemented with M-CSF (typical concentration: 10-20 ng/mL). Seed the cell suspension into ultra-low attachment multi-well plates. The inability to adhere will promote cell aggregation.
- Culture and Macrophage Generation: Culture the cells for 4 days, during which they will spontaneously aggregate to form spheroids. Continue the culture for an additional 7 days. Over this period, mature macrophages will begin to migrate out of the spheroids and adhere to the surface of the culture plate.
- Harvesting and Characterization: After a total of 11 days, macrophages can be harvested for analysis. Characterization should include:
- Phenotypic Profiling: Flow cytometry to confirm expression of macrophage markers (F4/80, CD11b) and specific subpopulation markers (CD11c, MHCII, TIM4) to validate their resemblance to in vivo resident macrophages [7] [6].
- Functional Assays:
- Phagocytosis: Using fluorescent beads or pHrodo-labeled E. coli particles.
- Polarization: Stimulate with LPS/IFN-γ (M1) or IL-4 (M2) and assess cytokine output via ELISA (e.g., TNF-α, IL-10).
- Metabolic Profiling: Measure extracellular acidification rate (ECAR) and oxygen consumption rate (OCR) via Seahorse Analyzer.
Application: Investigating Macrophage-Adipocyte Crosstalk
The 3D-generated ATMs can be used in co-culture systems to study cell-cell communication. A contact-mode co-culture protocol with adipocytes reveals how immune cells modulate adipose biology [5].
Co-culture Protocol
- Differentiate Adipocytes: Use the 3T3-L1 cell line or primary human pre-adipocytes. Induce differentiation using a standard cocktail (IBMX, dexamethasone, insulin).
- Establish Co-culture: Once adipocytes are fully differentiated, seed the generated 3D ATMs directly onto the adipocyte culture (contact mode).
- Analysis:
- Gene Expression: After 24-48 hours of co-culture, analyze RNA for adipogenesis (PPARγ, C/EBPα) and inflammation markers (TNF-α, IL-6) via qPCR.
- Cytokine Secretion: Collect conditioned media and quantify cytokines/chemokines (e.g., CCL5, CXCL10, TNF-α, IL-1β) using a multiplex Luminex assay or ELISA [5].
- Lipid Accumulation: Fix co-cultured cells and stain with Oil Red O to visualize and quantify lipid content in adipocytes [5].
Key Signaling Pathways in Crosstalk
The diagram below summarizes the key molecular pathways through which macrophages and adipocytes communicate, driving inflammation and metabolic dysfunction in obesity.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Adipose Tissue Macrophage Research
| Reagent / Tool | Function/Application | Example Use Case |
|---|---|---|
| M-CSF (Macrophage Colony-Stimulating Factor) | Promotes survival, proliferation, and differentiation of macrophages from progenitors. | Generation of ATMs from SVF in 3D culture [7]. |
| Ultra-Low Attachment Plates | Prevents cell adhesion, forcing cells to aggregate and form 3D spheroids. | Essential for the 3D culture protocol to generate ATMs [7]. |
| CD169-DTR Transgenic Mice | Enables specific ablation of CD169+ resident macrophages upon diphtheria toxin (DT) administration. | In vivo functional studies to investigate protective roles of resident ATMs [6]. |
| Fluorescent Conjugated Antibodies | Flow cytometric identification and sorting of distinct ATM subpopulations. | Staining for F4/80, CD11c, MHCII, TIM4, TREM2 to characterize heterogeneity [6] [8]. |
| Clodronate Liposomes | Depletes phagocytic cells (e.g., macrophages) upon injection or ex vivo treatment. | Validating the regulatory role of ATMs in processes like adipocyte dedifferentiation [8]. |
Macrophages are crucial immune cells with significant roles in tissue homeostasis, immune defense, and disease pathogenesis. A major advancement in macrophage biology is the recognition of their profound heterogeneity, primarily stemming from two distinct subpopulations: tissue-resident macrophages (TRMs) and bone marrow (BM)-derived macrophages [9]. Understanding the origin, maintenance, and functional characteristics of these subsets is fundamental to dissecting their roles in health and disease, particularly in complex tissues like adipose tissue (AT) [10] [11].
This Application Note provides a detailed framework for defining these macrophage subpopulations, with a specific focus on methodologies relevant for 3D culture systems in adipose tissue research. We present standardized protocols for identifying macrophage origins, detailed procedures for establishing 3D adipose tissue cultures that support resident macrophage populations, and a comprehensive toolkit for researchers and drug development professionals.
Defining Macrophage Subpopulations
Macrophage heterogeneity is influenced by developmental origin, tissue-specific signals, and pathological stimuli. The two primary subpopulations can be distinguished by their origin, maintenance mechanisms, and phenotypic markers.
Table 1: Core Characteristics of Resident vs. Bone Marrow-Derived Macrophages
| Characteristic | Tissue-Resident Macrophages (TRMs) | Bone Marrow-Derived Macrophages |
|---|---|---|
| Developmental Origin | Primarily embryonic yolk sac and fetal liver progenitors [9] [12] | Adult hematopoietic stem cells (HSCs) in the bone marrow [9] |
| Maintenance in Tissue | Self-renewal through local proliferation [13] [11] | Continuous replenishment from circulating monocytes [13] |
| Key Identifying Markers (Mouse) | TIM4, LYVE1, CD206, Folr2 [11] [12] | CCR2 [11] [12] |
| Key Identifying Markers (Human) | CD14, CD163 [13] | CCR2 [13] |
| Primary Research Model | 3D co-culture systems with adipose stromal vascular fraction (SVF) [11] | Bone marrow-derived macrophages (BMDMs) cultured with M-CSF [11] |
The traditional M1/M2 polarization model is increasingly seen as an oversimplification, as in vivo macrophages exist in a continuum of transcriptional states shaped by tissue-specific and disorder-specific cues [14] [12]. In adipose tissue, for instance, single-cell analyses have revealed a complex landscape of up to eight distinct resident macrophage subsets in lean mice, defined by combinations of surface markers like TIM4, CD163, and MHC II [10]. Obesity induces the infiltration of BM-derived macrophages and the appearance of specific disorder-specific subsets, such as TREM2+ lipid-associated macrophages (LAMs), which play a key role in disease pathogenesis [12].
Protocols for Studying Macrophage Heterogeneity in 3D Adipose Tissue Models
Protocol 1: Establishing a 3D Scaffold-Free Adipose Tissue Organoid for Resident Macrophage Generation
This protocol generates functional AT-resident macrophages from a murine subcutaneous AT stroma-vascular fraction (SVF) using ultra-low attachment plates, creating spheroids that mimic the native tissue microenvironment [11].
Workflow Overview:
Materials:
- Animals: 6- to 8-week-old male C57Bl/6J mice [11].
- Reagents: Collagenase (NB4, 1.7 U/ml), Dispase I (2.5 U/ml), RPMI GlutaMAX, Heat-Inactivated Newborn Calf Serum (hiNBSC), Macrophage Colony-Stimulating Factor (M-CSF, 10 ng/ml), antibiotic-antimycotic cocktail [11].
- Equipment: Ultra-low attachment (ULA) 96-well round-bottom plates, cell culture incubator (37°C, 5% CO2) [11].
Procedure:
- SVF Isolation: Harvest subcutaneous AT, remove lymph nodes, and mechanically dissociate. Digest the tissue in collagenase solution for 30 minutes at 37°C with occasional shaking. Filter the cell suspension, centrifuge, and perform red blood cell lysis. Count the isolated SVF cells [11].
- 3D Spheroid Seeding: Seed the SVF cells at a density of 10^5 cells per well into the ULA 96-well plate in culture medium (RPMI supplemented with 10% hiNBSC, 1% antibiotics, and 10 ng/ml M-CSF). Centrifuge the plate briefly to aggregate cells at the well bottom and incubate at 37°C with 5% CO2 [11].
- Spheroid Culture and Macrophage Generation: After 4 days of culture, cells will spontaneously form spheroids. From day 7 onwards, macrophages will begin to migrate out of the spheroids and adhere to the culture plate. These cells can be harvested for analysis from day 13 [11].
- Spheroid Dissociation (Optional): To analyze cells within the spheroid, collect spheroids and dissociate using a cocktail of NB4 collagenase (1.7 U/ml) and Dispase I (2.5 U/ml) for 40 minutes at 37°C, followed by mechanical dissociation and centrifugation [11].
Protocol 2: Flow Cytometry Analysis of Adipose Tissue Macrophage Heterogeneity
This protocol details the procedure for immunophenotyping macrophage subsets from digested AT or 3D cultures using fluorescent flow cytometry, based on markers defined in single-cell proteomics studies [10].
Procedure:
- Cell Preparation: Generate a single-cell suspension from AT (via collagenase digestion) or from 3D cultures (as in Protocol 1, step 4) [10] [11].
- Fc Receptor Blocking: Incubate cells with an anti-CD16/32 antibody (e.g., clone 2.4G2) for 10 minutes at room temperature to block non-specific antibody binding [10].
- Surface Staining: Stain the cells with a panel of fluorochrome-conjugated antibodies for 20 minutes at 4°C. A suggested panel for identifying resident and BM-derived subsets in mice includes:
- Core Macrophage Marker: F4/80
- Resident Macrophage Markers: TIM4, CD163, CD206
- BM-derived Marker: CCR2
- Activation/Maturation Marker: MHC II
- Viability Dye: To exclude dead cells.
- Data Acquisition and Analysis: Acquire data on a flow cytometer (e.g., LSR Fortessa) and analyze using software such as FlowJo. Identify macrophage populations as F4/80+ cells and subsequently gate on subpopulations based on TIM4, CD163, and CCR2 expression [10].
Table 2: Key Surface Markers for Identifying Adipose Tissue Macrophage Subsets
| Macrophage Subset | Surface Marker Profile | Ontogeny & Functional Notes |
|---|---|---|
| TIM4+ CD163+ | F4/80+, TIM4+, CD163+, CD206+ | Embryonic origin; high self-renewal capacity; superior in vivo scavenging [10]. |
| TIM4- CD163+ | F4/80+, TIM4-, CD163+, CD206+ | Largely bone marrow-derived [10]. |
| TIM4- CD163- | F4/80+, TIM4-, CD163-, CD206- | Largely bone marrow-derived [10]. |
| CD206- (Recruited) | F4/80+, CD206-, CCR2+ | Infiltrates during high-fat diet; pro-inflammatory [10]. |
| Lipid-Associated Macrophage (LAM) | F4/80+, TREM2+ | Disorder-specific subset in obesity; involved in lipid metabolism and inflammation [12]. |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for 3D Adipose Tissue Macrophage Research
| Reagent/Material | Function/Application | Example |
|---|---|---|
| M-CSF | Critical cytokine for macrophage survival, differentiation, and proliferation in vitro. Essential for generating both BM-derived and resident-like macrophages [13] [11]. | Recombinant Mouse M-CSF (PeproTech) [13] [11] |
| Collagenase/Dispase | Enzymatic digestion of adipose tissue to isolate the stromal vascular fraction (SVF) containing macrophage precursors and other cells [11]. | Collagenase D (Roche) / NB4 (Sigma-Aldrich) & Dispase I (Sigma-Aldrich) [10] [11] |
| Ultra-Low Attachment (ULA) Plates | Prevents cell adhesion, promoting cell-cell aggregation and spontaneous 3D spheroid formation from SVF cells [11]. | COSTAR ULA 96-well round bottom plates [11] |
| Gellan Gum (GG) | Animal-free, bacteria-derived hydrogel used as a scaffold for 3D co-culture of mature adipocytes and macrophages [15]. | GG Hydrogel [15] |
| PMA/LPS | Activation stimuli used to induce a pro-inflammatory state in macrophage-adipocyte co-culture models [15]. | Phorbol 12-myristate 13-acetate (PMA) & Lipopolysaccharide (LPS) [15] |
| Antibody Panels for Cytometry | Immunophenotyping of macrophage subpopulations based on origin and activation status. | Anti-mouse: F4/80, TIM4, CD163, CD206, CCR2, MHC II [10] |
The precise definition of macrophage heterogeneity is paramount for advancing our understanding of their role in adipose tissue physiology and disease. The protocols and tools outlined in this document provide a standardized approach for researchers to isolate, culture, and characterize distinct resident and BM-derived macrophage subpopulations within physiologically relevant 3D models. Mastering these techniques enables more accurate in vitro modeling of adipose tissue immune function, thereby accelerating the discovery of novel therapeutic targets for obesity and related metabolic disorders.
Within adipose tissue (AT), macrophages are a heterogeneous population pivotal for maintaining tissue homeostasis, orchestrating immune responses, and regulating metabolic processes [16] [9]. Distinct macrophage subsets, notably resident adipose tissue macrophages (ATMs), perform specific functions under physiological and pathological conditions [16] [17]. A significant challenge in immunology and metabolic research has been the accurate identification and study of these resident macrophages in vitro, as traditional isolation and culture methods often alter their inherent properties [16].
The advent of specific cell surface and genetic markers has revolutionized our ability to distinguish resident macrophage subpopulations. Among these, Timd4, Lyve1, Folr2, and CD206 have emerged as a crucial combination for identifying resident macrophages and discriminating them from bone marrow-derived macrophages [16] [18]. This application note details the marker profiles, experimental protocols, and practical applications of these markers within the context of 3D culture systems for functional adipose tissue-resident macrophages, providing researchers with a framework for advanced metabolic and immunological studies.
Marker Profiles and Biological Significance
The discrimination of resident macrophages from other myeloid cells relies on a panel of markers, each conferring specific functional and ontogenetic information.
Table 1: Key Markers for Identifying Resident Adipose Tissue Macrophages
| Marker | Full Name | Primary Function | Expression in Resident ATMs | Significance |
|---|---|---|---|---|
| Timd4 (Tim-4) | T-cell immunoglobulin and mucin domain containing 4 | Phosphatidylserine receptor; mediates phagocytosis of apoptotic cells [18]. | High [18] | Identifies a long-term resident subset; key regulator of post-prandial cholesterol transport [18]. |
| Lyve1 | Lymphatic Vessel Endothelial Hyaluronan Receptor 1 | Receptor for hyaluronan; involved in lymphangiogenesis and cell adhesion [18]. | High [18] | Associates with vasculature; a hallmark of tissue residency in AT and other tissues [17] [18]. |
| Folr2 | Folate Receptor 2 | Binds and internalizes folates; role in one-carbon metabolism [19]. | High [16] [19] | Defines an embryonically-derived, anti-inflammatory resident subset; often co-expressed with Lyve1 [19]. |
| CD206 | Macrophage Mannose Receptor (MRC1) | Phagocytic receptor for glycoproteins; antigen capture and clearance [16]. | High [16] | Identifies resident macrophages in adipose tissue and dermis; associated with homeostatic functions [16]. |
| CCR2 | C-C Chemokine Receptor Type 2 | Receptor for MCP-1; mediates monocyte recruitment from blood [16] [18]. | Low/Negative [16] [18] | Negative marker; identifies bone marrow-derived monocytes/macrophages. |
The combination of these markers allows for the precise identification of resident ATMs (Timd4+ Lyve1+ Folr2+ CD206+ CCR2-) and their distinction from monocyte-derived infiltrates (CCR2+), which are often associated with inflammatory conditions [16] [18]. Single-cell RNA sequencing (scRNA-seq) has been instrumental in validating this profile, confirming that these markers define a transcriptionally distinct cluster of macrophages enriched for genes involved in homeostasis and endocytosis [17] [18].
Experimental Protocols for 3D Culture and Analysis
3D In Vitro System for Generating Functional AT Resident Macrophages
This protocol, adapted from current research, enables the generation of functional mature macrophages that mirror the phenotypic and functional traits of in-vivo AT resident macrophages without the need for physical cell sorting [16].
Key Research Reagent Solutions:
- Ultra-low adherence plates: Essential for spheroid formation.
- Macrophage colony-stimulating factor (M-CSF): Critical for macrophage differentiation and survival (10 ng/mL) [16].
- Collagenase (e.g., NB4): For enzymatic digestion of adipose tissue.
- Dispase I: Used in conjunction with collagenase for spheroid dissociation.
- Antibodies for F4/80, Timd4, Lyve1, Folr2, CD206, CCR2: For flow cytometry and immunohistochemistry validation.
Detailed Methodology:
Isolation of Stromal Vascular Fraction (SVF):
- Harvest subcutaneous adipose tissue (e.g., from C57Bl/6J mice) and remove lymph nodes.
- Mechanically dissociate the tissue and digest using collagenase NB4 (1.7 U/mL) at 37°C for 30 minutes [16].
- Filter the cell suspension and centrifuge to isolate the SVF pellet.
- Perform red blood cell lysis using an appropriate buffer (e.g., NH₄Cl 155 mM, K₂HPO₄ 5.7 mM, EDTA 0.1 mM) and count the cells [16].
3D Spheroid Culture and Macrophage Generation:
- Seed the isolated SVF cells on ultra-low adherence 96-well round bottom plates at a density of 10⁵ cells per well [16].
- Culture the cells in RPMI medium supplemented with Glutamax, 10% Heat-Inactivated Newborn Calf Serum, antibiotics (penicillin/streptomycin/amphotericin), and M-CSF (10 ng/mL).
- Centrifuge the plates briefly to encourage cell contact and incubate at 37°C with 5% CO₂.
- After 4 days, the cells will spontaneously aggregate to form spheroids.
- By day 7, macrophages begin to migrate out of the spheroids and adhere to the culture plate. These cells can be harvested for experiments from day 13 onwards [16].
Spheroid Dissociation for Analysis:
- To characterize cells within the spheroid, collect spheroids at desired time points (e.g., day 7, 13, or 21).
- Dissociate using a cocktail of collagenase NB4 (1.7 U/mL) and dispase I (2.5 U/mL) at 37°C for 40 minutes, with periodic mechanical pipetting [16].
- Centrifuge to obtain a single-cell suspension.
Validation Workflow and Marker Identification
The following workflow ensures the generated macrophages possess the signature of resident ATMs.
Figure 1: Immunohistochemistry workflow for validating macrophage markers.
For flow cytometry, use the dissociated cell suspension from the 3D cultures. Follow standard staining procedures: first, label with a viability dye, then incubate with conjugated antibodies against the panel of markers (F4/80, Timd4, Lyve1, Folr2, CD206, CCR2). Analysis will reveal the co-expression patterns that define the resident population.
Table 2: Functional Characterization of 3D Cultured Resident ATMs vs. Bone Marrow-Derived Macrophages (BMDMs)
| Assay Type | Parameter Measured | 3D Cultured ATMs | BMDMs | Protocol Summary |
|---|---|---|---|---|
| Phagocytosis | Phagocytic capacity | Similar to BMDMs [16] | Baseline | Incubate cells with fluorescent beads (e.g., pHrodo). Measure uptake via flow cytometry or fluorescence microscopy. |
| Metabolic Activity | Metabolic polarization | Specific metabolic profile; distinct from BMDMs [16] | Baseline | Measure extracellular acidification rate (ECAR) and oxygen consumption rate (OCR) using a Seahorse Analyzer. |
| Polarization | Response to IL-4 or IFN-γ | Specific polarization signature [16] | Standard M2/M1 response | Treat cells with IL-4 (10 ng/mL, 24h) for M2 or IFN-γ (50 ng/mL, 24h) for M1. Analyze marker expression (e.g., Arg1, Nos2) via qPCR. |
| Genetic Profile | Transcriptomic signature | Mirrors in-vivo resident ATMs [16] | Distinct signature | Perform single-cell RNA sequencing on F4/80+ sorted cells from 3D cultures and BMDM controls. |
Signaling Pathways and Functional Relevance
Resident ATMs defined by Timd4, Lyve1, Folr2, and CD206 are integral to tissue homeostasis, and their markers are often directly involved in functional pathways.
The phosphatidylserine receptor Timd4 is a key regulator of a crucial metabolic pathway. In lean mice, ingestion of a lipid-rich meal leads to transcriptional activation of resident Lyve1+Timd4+ ATMs. These cells exhibit high lysosomal activity and express ABCA1, a cholesterol transporter. Timd4-mediated signaling is essential for this lysosomal activation, which in turn promotes the release of post-prandial high-density lipoprotein cholesterol (HDLc), a key step in reverse cholesterol transport. Blocking Timd4 inhibits this process, directly linking this resident macrophage marker to systemic lipid metabolism [18].
Figure 2: Timd4 role in post-prandial cholesterol transport.
Furthermore, these resident macrophages are strategically located around blood vessels in adipose tissue [17] [18]. They contribute to protecting the adipose tissue vascular barrier. Dysfunction of these subsets, as observed in conditions like non-alcoholic steatohepatitis (NASH), correlates with a breakdown of vascular integrity and albumin extravasation, perpetuating tissue inflammation [17].
Application in Metabolic Research and Drug Development
The 3D culture model for generating resident-like ATMs provides a powerful tool for investigating macrophage function in metabolic diseases and screening therapeutic compounds.
- Disease Modeling: This system allows for the study of resident ATM dysfunction in contexts such as obesity and NAFLD/NASH. Researchers can expose the 3D cultures to lipotoxic or pro-inflammatory conditions to mimic the pathological environment and investigate how this alters the phenotype and function of the resident macrophages, including their role in maintaining vascular integrity [17].
- Therapeutic Targeting: The distinct pathways active in resident macrophages, such as the Timd4-lysoosomal pathway, represent novel therapeutic targets for treating dyslipidemia and atherosclerosis [18]. The 3D culture system is ideal for high-throughput screening of compounds aimed at modulating these specific pathways to reinstate the protective, homeostatic functions of resident ATMs.
- Adipocyte-Macrophage Crosstalk: This platform can be used to study the paracrine interactions between adipocytes and macrophages. For instance, depletion of resident ATMs in explant cultures leads to increased adipocyte dedifferentiation, a process regulated by signaling pathways like TNFα, highlighting the role of macrophages in maintaining adipocyte homeostasis [8].
The marker profile of Timd4, Lyve1, Folr2, and CD206 provides a robust framework for identifying and studying resident adipose tissue macrophages, a cell population critical for metabolic health and tissue homeostasis. The implementation of the described 3D culture protocol enables the generation of functionally active resident macrophages in vitro that faithfully recapitulate their in-vivo counterparts. This combined approach of precise marker-based identification and physiologically relevant culture models offers researchers a powerful "scientist's toolkit" to delve deeper into the biology of resident macrophages, accelerating discovery in metabolic disease research and drug development.
Adipose tissue (AT) is a vital endocrine and immune organ that plays a critical role in overall metabolic health, communicating with other organs through the release of adipokines and inflammatory factors [20]. Within this tissue, adipose tissue macrophages (ATMs) constitute the predominant immune cell population and exhibit a remarkable functional dichotomy—they are essential for maintaining tissue homeostasis under physiological conditions yet become primary drivers of chronic inflammation in metabolic diseases such as obesity and type 2 diabetes [8] [20]. This paradoxical nature stems from the existence of distinct macrophage subpopulations with opposing functions: resident macrophages typically support metabolic homeostasis, while bone marrow (BM)-derived infiltrating macrophages promote inflammation and insulin resistance [11] [16].
The transition from homeostatic maintenance to inflammatory dysfunction represents a crucial continuum in metabolic disease pathogenesis. In lean, healthy states, ATMs predominantly exhibit an anti-inflammatory M2 phenotype and contribute to tissue remodeling, insulin sensitivity, and adipocyte homeostasis through the secretion of type II cytokines such as IL-4, IL-10, IL-13, and TGF-β [8] [20]. However, obesity triggers a dramatic shift in both the number and function of ATMs, characterized by increased accumulation of pro-inflammatory M1 macrophages that secrete cytokines like TNF-α, leading to chronic low-grade inflammation, insulin resistance, and metabolic dysfunction [20] [21]. Understanding this functional switch and the mechanisms governing ATM plasticity is essential for developing novel therapeutic strategies for metabolic diseases.
The Homeostatic Versus Inflammatory Spectrum of Adipose Tissue Macrophages
Molecular and Functional Characteristics of ATM Subpopulations
The functional dichotomy of ATMs is reflected in their distinct transcriptional, phenotypic, metabolic, and functional characteristics [11] [16]. Resident ATMs, believed to primarily originate from embryonic yolk-sac precursors under normal conditions, express specific markers including Timd4, Folr2, Lyve1, and CD206 [11] [16]. These cells play crucial roles in maintaining AT homeostasis, supporting tissue expansion and remodeling, and facilitating tissue regeneration [11]. In contrast, bone marrow-derived macrophages, which infiltrate AT during obesity, can be identified by Ccr2 expression and negatively impact AT function by promoting inflammation, insulin resistance, and fibrosis [11] [16].
The table below summarizes the key distinguishing features of these two macrophage subpopulations:
Table 1: Characteristics of Adipose Tissue Macrophage Subpopulations
| Feature | Homeostatic (Resident) Macrophages | Inflammatory (BM-Derived) Macrophages |
|---|---|---|
| Origin | Embryonic yolk-sac precursors [11] | Bone marrow-derived monocytes [11] |
| Key Markers | Timd4, Folr2, Lyve1, CD206 [11] [16] | Ccr2 [11] |
| Primary Functions | Tissue homeostasis, expansion, remodeling, regeneration [11] | Promotion of inflammation, insulin resistance, fibrosis [11] [16] |
| Cytokine Profile | IL-4, IL-10, IL-13, TGF-β (Type II cytokines) [8] [20] | TNF-α, IL-1β, MCP-1 (Pro-inflammatory) [20] [21] |
| Metabolic Role | Maintain insulin sensitivity, support adipocyte function [8] [20] | Induce insulin resistance, disrupt adipocyte homeostasis [20] [21] |
| Polarization State | Alternatively activated (M2) [8] | Classically activated (M1) [20] |
Signaling Networks in ATM Homeostasis and Inflammation
The balance between homeostatic and inflammatory ATMs is regulated by complex signaling networks involving multiple immune cell types and stromal components. In physiological conditions, group 2 innate lymphoid cells (ILC2s) respond to IL-33 (produced by adipose tissue-resident mesenchymal stromal cells, or ATSCs) by secreting IL-4, IL-5, IL-9, and IL-13, which subsequently promote the activation and maintenance of homeostatic ATMs and recruit eosinophils [20]. This creates a type 2 immune environment conducive to metabolic health. However, in obesity, this balance is disrupted as elevated TNF-α levels upregulate PD-1 expression on ILC2s, while M1 macrophages expressing PD-L1 increase in number, inhibiting ILC2 function through the PD-1/PD-L1 pathway and perpetuating inflammation [20].
Diagram 1: Signaling networks regulating ATM homeostasis and inflammation. In lean states (green), IL-33 from ATSCs activates ILC2s, which promote M2 macrophage polarization and eosinophil recruitment, maintaining metabolic homeostasis. In obesity (red), TNF-α and PD-1/PD-L1 interactions suppress ILC2 function, enabling M1 macrophage dominance and inflammation.
3D Culture Models for Studying Adipose Tissue Macrophages
Limitations of Traditional Macrophage Culture Systems
Studying resident macrophages in vitro has presented significant challenges because conventional isolation methods and extended 2D culture periods often alter their intrinsic properties [11] [16]. The tissue microenvironment plays a critical role in macrophage imprinting, and preserving their in vivo characteristics in culture has been a difficult task [11]. Furthermore, sorting resident macrophages typically alters their intrinsic properties, complicating the study of their true biological functions [16]. These limitations have hindered progress in understanding the distinct roles of various ATM subsets and their specific contributions to metabolic homeostasis and disease.
Protocol: Generation of Functional ATMs Using 3D Culture Systems
An innovative three-dimensional (3D) culture method has been developed to generate functional mature macrophages that accurately mirror the phenotypic and functional traits of in-vivo AT resident macrophages [11] [16]. This protocol enables the production of ATMs without the need for cell sorting, maintaining their characteristic properties for extended periods.
Materials and Reagents
Table 2: Essential Research Reagents for 3D ATM Culture
| Reagent/Consumable | Function/Application | Specifications |
|---|---|---|
| Ultra-low adherence 96-well plates | Facilitates spheroid formation | Round bottom, non-adherent surface [11] [16] |
| Roswell Park Memorial Institute (RPMI) medium | Base culture medium | Supplemented with Glutamax [11] [16] |
| Heat Inactivated Newborn Calf Serum (hiNBSC) | Serum supplement for cell growth | 10% final concentration [11] [16] |
| Antibiotic-Antimycotic cocktail | Prevents microbial contamination | 1% final concentration (streptomycin, penicillin, amphotericin) [11] [16] |
| Macrophage colony-stimulating factor (M-CSF) | Drives macrophage differentiation | 10 ng/ml [11] [16] |
| Collagenase NB4 | Tissue dissociation enzyme | 1.7 U/ml for spheroid dissociation [11] [16] |
| Dispase I | Tissue dissociation enzyme | 2.5 U/ml for spheroid dissociation [11] [16] |
Step-by-Step Methodology
Isolation of Stromal Vascular Fraction (SVF):
- Harvest subcutaneous adipose tissue (sc-AT) from 6- to 8-week-old male C57Bl6/J mice
- Remove lymph nodes and mechanically dissociate tissue
- Digest with collagenase NB4 (1.7 U/ml) at 37°C for 30 minutes
- Filter and centrifuge to isolate stroma vascular cells
- Perform red blood cell lysis using NH4Cl (155 mM), K2HPO4 (5.7 mM), EDTA (0.1 mM)
- Count cells using an automated cell counter [11] [16]
3D Spheroid Formation:
- Seed SVF cells on ultra-low adherence 96-well round bottom plates at 10^5 cells/well
- Culture in RPMI medium supplemented with Glutamax, 10% hiNBSC, 1% antibiotic-antimycotic cocktail, and M-CSF (10 ng/ml)
- Centrifuge plates briefly and incubate at 37°C with 5% CO₂
- After 4 days, cells spontaneously aggregate to form spheroids [11] [16]
Macrophage Migration and Harvest:
Macrophage Culture and Polarization:
Diagram 2: 3D culture workflow for generating functional adipose tissue macrophages. The process begins with SVF isolation from adipose tissue, progresses through spheroid formation in ultra-low attachment plates, and culminates in macrophage migration and characterization.
Characterization of 3D-Cultured ATMs
ATMs generated through this 3D culture system present distinct genic and phenotypic characteristics compared to bone marrow-derived macrophages, with specific metabolic activity and polarization in response to stimulation, but similar phagocytic capacity [11] [16]. Single-cell analysis confirms that AT-macrophages generated in 3D culture mirror the phenotypic and functional traits of in-vivo AT resident macrophages, making them a valuable resource for exploring ATM differentiation and function in diverse physiological and pathological contexts [11].
Application Notes: Investigating the Functional Dichotomy in Metabolic Disease
Protocol: Assessing Adipocyte-Macrophage Crosstalk in Dedifferentiation
The 3D culture system enables investigation of how ATM functional states influence adipocyte homeostasis and plasticity. Recent research has revealed that resident ATMs play a regulatory role in maintaining the mature adipocyte phenotype and preventing excessive adipocyte dedifferentiation [8]. The following protocol outlines methods to study this crosstalk:
Adipocyte Dedifferentiation Assessment
- Explant Culture Setup: Use epididymal AT explants from lean, chow-fed homozygous AdipoqCreERT2 × ROSA26-CAG-tdTo × CSF1R-EGFP (MacFat) mice
- Microscopic Analysis: Image living explants over 7-10 days to track emergence of stellate-shaped tdTomato+ (tdTo+) cells with small vacuoles and cytoplasmic projections
- Flow Cytometry Quantification: Analyze explants on days 0, 7, and 10 for tdTo+ stromal cells using the following gating strategy:
- Identify viable cells (DAPI-negative) as stromal vascular fraction
- Detect ATMs as GFP+, tdTo- population from SVF
- Quantify dedifferentiated adipocytes as GFP-, tdTo+ population from SVF [8]
Macrophage Depletion Studies
- Pharmacological Depletion: Treat explants with either Plexxicon 5622 or clodronate liposomes to deplete macrophages
- Dedifferentiation Measurement: Compare DFAT cell levels between macrophage-depleted and control explants
- RNA Sequencing: Perform bulk RNA sequencing of macrophage-depleted explants to identify enriched pathways [8]
Data Interpretation and Analysis
Studies using these approaches have revealed that macrophage depletion significantly increases DFAT cell levels, suggesting resident ATMs normally suppress excessive adipocyte dedifferentiation [8]. RNA sequencing of macrophage-depleted explants shows enrichment of the TNFα signaling pathway, and subsequent experiments demonstrate that TNFα stimulation decreases adipocyte dedifferentiation, highlighting the complex role of inflammatory signaling in maintaining adipocyte homeostasis [8].
The table below summarizes key quantitative findings from adipocyte dedifferentiation studies:
Table 3: Temporal Changes in Adipocyte Dedifferentiation and Macrophage Polarization in AT Explants
| Parameter | Day 0 | Day 7 | Day 10 |
|---|---|---|---|
| DFAT Cells (% of SVF) | Baseline | ~2x increase [8] | ~3x increase [8] |
| ATM Polarization (M1 vs M2) | Predominantly M2 (CD11c-; CD301+) [8] | Shift toward M1 [8] | Dominantly M1 (CD11c+; CD301-) [8] |
| Effect of Macrophage Depletion | - | Significant increase in DFAT cells [8] | - |
| TNFα Stimulation Effect | - | Decreased adipocyte dedifferentiation [8] | - |
The 3D culture system for generating functional adipose tissue macrophages represents a significant advancement in obesity and metabolic disease research. By faithfully replicating the in vivo characteristics of ATM subpopulations, this platform enables detailed investigation of the functional dichotomy between homeostatic maintenance and inflammation in metabolic disease. The protocols outlined herein provide researchers with robust methodologies to study ATM biology in conditions that closely mimic the physiological tissue microenvironment, facilitating the discovery of novel therapeutic targets for obesity-related metabolic disorders.
This experimental approach offers particular value for:
- Drug discovery screens targeting specific macrophage subpopulations
- Mechanistic studies of macrophage-adipocyte crosstalk
- Investigation of metabolic memory and trained immunity in ATMs
- Personalized medicine approaches using patient-derived adipose tissue
As research in this field advances, the integration of 3D macrophage culture systems with other sophisticated models such as organ-on-a-chip technologies and humanized mouse models will further enhance our understanding of the intricate relationship between immune function and metabolic homeostasis.
Adipose tissue macrophages (ATMs) are indispensable for maintaining tissue homeostasis, supporting tissue expansion and remodeling, and enabling tissue regeneration under physiological conditions [16]. Their functionality is not intrinsic but is profoundly shaped by a complex tissue microenvironment known as the niche. This niche consists of a specific three-dimensional (3D) architecture, cell-cell interactions, extracellular matrix (ECM), and mechanical cues that collectively imprint macrophages with unique functional identities [22]. In conventional two-dimensional (2D) monolayer cultures, this critical niche is absent, leading to macrophages that lack key phenotypic and functional characteristics of their in vivo counterparts. This application note details the limitations of 2D systems and provides validated protocols for establishing 3D cultures that recapitulate the adipose niche to generate more physiologically relevant macrophages for research and drug development.
The Scientific Basis of Niche Imprinting
Macrophage Heterogeneity and Niche Dependence
In vivo, adipose tissue contains a diverse population of macrophage subsets, each playing distinct roles. Key subsets include:
- Resident Tissue Macrophages (RTMs): Often derived from embryonic precursors, they maintain tissue homeostasis and express markers like LYVE1, FOLR2, and CD206 [22] [23] [16].
- Lipid-Associated Macrophages (LAMs): Also referred to as CD9+ macrophages, these cells accumulate in obesity within crown-like structures (CLS) surrounding dying adipocytes. They exhibit high lipid metabolism and phagocytic activity and express genes like TREM2 and LPL [22] [23].
- Monocyte-Derived Macrophages: Recruited during inflammation, these cells are often CCR2+ and contribute to a pro-inflammatory state [22].
Single-cell RNA sequencing analyses of human adipose tissue have revealed that this heterogeneity is a continuum of activation states shaped by the local environment, far surpassing the traditional M1/M2 dichotomy [22] [23]. The tissue niche is arguably the most important driver of resident macrophage function, determining their transcriptional profile and metabolic activity [22].
Limitations of 2D Culture Systems
Conventional 2D culture systems fail to model this complexity, leading to several critical limitations:
Table 1: Key Limitations of Conventional 2D Macrophage Cultures
| Aspect | In Vivo Niche | Conventional 2D Culture | Functional Consequence |
|---|---|---|---|
| Spatial Architecture | 3D tissue structure with CLS in obesity [22] | Flat, rigid plastic surface | Loss of physiologically relevant cell-cell and cell-ECM interactions |
| Metabolic Programming | Distinct global metabolic activation; high glycolysis, respiration, and lipid metabolism in obesity [23] | Altered, non-physiologic metabolism | Poorly modeling inflammatory diseases like obesity and type 2 diabetes |
| Phenotypic Stability | Stable resident phenotypes maintained by niche signals (e.g., LYVE1, FOLR2) [22] [16] | Phenotypic drift; loss of tissue-specific markers | Reduced predictive value for in vivo therapeutic responses |
| Transcriptomic Profile | Unique transcriptome defined by tissue location [22] | Divergent gene expression | Poor correlation with native macrophage function |
Advanced 3D Models for Preserving Niche Imprinting
3D Spheroid Culture for Adipose Tissue-Resident Macrophages
This protocol generates functional mature macrophages that mirror the phenotypic and functional traits of in-vivo AT resident macrophages from the stromal vascular fraction (SVF) [16].
Experimental Workflow: Generation of 3D Adipose Tissue Macrophage Spheroids
Detailed Protocol:
- Isolation of Stromal Vascular Fraction (SVF):
- Collect subcutaneous adipose tissue from C57Bl/6 mice (6-8 weeks old).
- Remove lymph nodes and mechanically dissociate the tissue.
- Digest the tissue with Collagenase NB4 (1.7 U/mL) at 37°C for 30 minutes.
- Filter the cell suspension through a 70 µm strainer and centrifuge.
- Perform red blood cell lysis using NH₄Cl buffer. Count the isolated SVF cells [16].
- 3D Spheroid Culture:
- Seed the SVF cells at a density of 10^5 cells per well in ultra-low attachment (ULA) 96-well round-bottom plates.
- Culture the cells in RPMI medium supplemented with Glutamax, 10% Heat-Inactivated Newborn Calf Serum, 1% penicillin/streptomycin/amphotericin, and 10 ng/mL Macrophage Colony-Stimulating Factor (M-CSF).
- Centrifuge the plates briefly to aggregate cells at the well bottom and incubate at 37°C with 5% CO₂.
- Within 4 days, cells will spontaneously form spheroids.
- From day 7 onwards, macrophages will begin to migrate out of the spheroids and adhere to the culture plate surface. These can be harvested for experiments [16].
Key Quality Control:
- Immunostaining: Confirm macrophage identity via F4/80 staining [16].
- Flow Cytometry: Verify expression of resident macrophage markers (e.g., CD206) and absence of monocyte-derived markers (e.g., CCR2) [16].
- Functional Assays: Validate phagocytic capacity and metabolic activity [16].
Animal-Free 3D Inflamed Adipose Tissue Model
This system co-cultures human primary mature adipocytes with monocytic cell lines in a fully defined, animal-free environment to model adipose tissue inflammation [15] [24].
Experimental Workflow: Animal-Free 3D Inflamed Adipose Tissue Model
Detailed Protocol:
- 3D Adipocyte Culture:
- Encapsulate human primary mature adipocytes (ACs) in 0.5% (w/v) Gellan Gum (GG) hydrogel. GG is a bacteria-derived, animal-free polysaccharide that is thermosensitive and can be cross-linked with cations [15].
- Use a defined, serum-free medium to maintain the culture, eliminating batch-to-batch variability and confounding factors from animal sera [15].
Macrophage Differentiation and Activation:
- Use human monocytic cell lines MM6 or THP-1.
- Differentiate and activate the monocytes using a combination of Phorbol 12-myristate 13-acetate (PMA) at a low concentration and Lipopolysaccharide (LPS). This combination effectively induces an inflammatory state [15] [24].
- Note: Activated cells will show characteristic clumping and reduced viability/proliferation compared to unstimulated controls [15].
Inflammation Induction and Analysis:
- Co-culture the encapsulated adipocytes with the activated macrophages in the defined medium for up to 72 hours.
- The PMA+LPS stimulation successfully activates the entire co-culture to an inflammatory state, characterized by the release of pro-inflammatory cytokines like IL-6 and TNF-α [15].
- Assess adipocyte functionality by monitoring high viability, intracellular lipid content, and perilipin A expression [15].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for 3D Adipose Tissue Macrophage Models
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| Gellan Gum (GG) | Animal-free hydrogel scaffold for 3D cell encapsulation. Provides a biocompatible, tunable 3D matrix. | Bacteria-derived exopolysaccharide; cross-linkable with cations. Superior to collagen for defined, animal-free setups [15]. |
| Ultra-Low Attachment (ULA) Plates | For scaffold-free spheroid formation. Prevents cell adhesion, forcing 3D self-assembly. | Critical for generating adipose tissue organoids and macrophage spheroids [25] [16]. |
| Macrophage Colony-Stimulating Factor (M-CSF) | Essential cytokine for macrophage survival, proliferation, and differentiation. | Used at 10 ng/mL to generate and maintain macrophages from progenitors in 3D culture [16]. |
| Defined / Serum-Free Medium | Eliminates batch variability and undefined components from Fetal Calf Serum (FCS). Increases experimental reproducibility. | Custom formulations or commercial kits are available. Crucial for animal-free test systems [15]. |
| Collagenase (NB4) | Enzymatic digestion of adipose tissue to isolate the Stromal Vascular Fraction (SVF). | Specific type and concentration (e.g., 1.7 U/mL) are critical for efficient digestion and cell viability [16]. |
| PMA & LPS | Pharmacological activation stimuli to induce a pro-inflammatory state in macrophages and co-cultures. | Combined use (PMA+LPS) is an effective activator for inducing inflammation in 3D co-culture models [15]. |
The "Niche Imprinting Problem" represents a fundamental challenge in macrophage research that cannot be adequately addressed using conventional 2D systems. The protocols outlined herein for generating 3D adipose tissue macrophage spheroids and animal-free inflamed co-cultures provide robust and physiologically relevant tools. By adopting these advanced 3D models, researchers can better elucidate the mechanisms of metabolic disease, improve the predictive accuracy of pre-clinical drug testing, and accelerate the development of novel therapeutics.
Protocols and Applications: Building 3D Adipose Tissue Macrophage Models
Within adipose tissue (AT), macrophage subsets play pivotal and specific roles in upholding tissue homeostasis under both physiological and pathological conditions [16]. Resident AT macrophages are crucial for maintaining AT homeostasis, tissue expansion, and remodeling, while bone marrow (BM)-derived macrophages can promote inflammation and insulin resistance [16] [6]. Studying resident macrophages in vitro presents significant challenges, as traditional isolation and culture methods can alter their inherent properties [16]. This protocol details an innovative three-dimensional (3D) culture system for generating functional mature macrophages from the adipose stromal-vascular fraction (SVF) that mirror the phenotypic and functional traits of in-vivo AT resident macrophages, providing a valuable resource for exploring macrophage function in diverse physiological and pathological contexts [16] [11].
Materials and Methods
Research Reagent Solutions
Table 1: Essential materials and reagents for the 3D culture of adipose tissue macrophages.
| Item | Function/Application |
|---|---|
| Ultra-low attachment 96-well plates | Facilitates spontaneous spheroid formation by preventing cell adhesion [16] |
| Macrophage colony-stimulating factor (M-CSF) | Key cytokine driving macrophage differentiation and survival (10 ng/mL) [16] |
| RPMI medium with Glutamax | Base nutrient medium for cell culture [16] |
| Heat Inactivated Newborn Calf Serum (hiNBCS) | Provides essential growth factors and nutrients for cell viability (10% concentration) [16] |
| Antibiotic-Antimycotic cocktail | Prevents microbial contamination in long-term cultures [16] |
| Collagenase (e.g., NB4) | Enzymatic digestion of adipose tissue to isolate the stromal-vascular fraction [16] |
| Dispase I | Used in combination with collagenase for spheroid dissociation [16] |
Protocol Workflow
The following diagram outlines the complete experimental workflow for generating macrophages from the adipose stromal-vascular fraction.
Isolation of Adipose Stromal-Vascular Fraction
- Harvest Tissue: Collect subcutaneous adipose tissues (sc-AT) from 6- to 8-week-old male C57Bl6/J mice and remove lymph nodes [16] [11].
- Mechanical Dissociation: Sustain mechanical dissociation of sc-AT.
- Enzymatic Digestion: Digest tissue with collagenase NB4 (1.7 U/mL) at 37°C for 30 minutes [16].
- Filtration and Centrifugation: Filter and centrifuge the digestate to isolate stroma vascular cells as previously described [16].
- Red Blood Cell Lysis: Perform red blood cell lysis using NH4Cl (155 mM), K2HPO4 (5.7 mM), and EDTA (0.1 mM) [16].
- Cell Counting: Count isolated SVF cells with a cell counter [16].
3D Culture and Macrophage Generation
- Cell Seeding: Seed adipose SVF cells on ultra-low adherence 96-well round bottom plates at a density of 10^5 cells/well in RPMI medium supplemented with Glutamax, 10% hiNBCS, 1% antibiotic-antimycotic cocktail, and M-CSF (10 ng/mL) [16].
- Centrifugation and Incubation: Briefly centrifuge plates and incubate at 37°C with 5% CO₂ [16].
- Spheroid Formation: After 4 days of culture, cells spontaneously aggregate to form spheroids [16].
- Macrophage Migration: Starting on day 7, cells begin to spread out of the spheroid and adhere to the culture plate [16].
- Spheroid Dissociation (Optional): For analysis at specific timepoints (day 7, 13, or 21), collect and dissociate spheroids with NB4 (1.7 U/mL) and dispase I (2.5 U/mL) at 37°C for 40 minutes, followed by mechanical dissociation and centrifugation [16].
Results and Characterization
Phenotypic and Functional Characteristics
Table 2: Key characteristics of 3D-generated AT macrophages compared to bone marrow-derived macrophages (BMDMs).
| Parameter | 3D AT-Macrophages | Bone Marrow-Derived Macrophages |
|---|---|---|
| Origin | Adipose stromal-vascular fraction | Bone marrow cells [16] |
| Culture System | 3D spheroid culture | 2D culture on non-adherent Petri dishes [16] |
| Differentiation Time | ~7 days until migration | 13 days [16] |
| Markers | Mirror in vivo resident macrophages (CD206+) [16] | Conventional BMDM markers [16] |
| Polarization Response | Specific metabolic activity and polarization in response to stimulation [16] | Conventional polarization response [16] |
| Phagocytic Capacity | Similar to BMDMs [16] | Similar to 3D AT-Macrophages [16] |
| Metabolic Activity | Distinct metabolic characteristics [16] | Different from 3D AT-Macrophages [16] |
Key Cellular Features
The following diagram summarizes the distinct characteristics and validation outcomes for the generated macrophages.
Discussion
This protocol establishes a robust 3D in-vitro system for generating and culturing functional AT-resident macrophages without the need for cell sorting [16]. The generated macrophages present distinct genic and phenotypic characteristics compared to bone marrow-derived macrophages, along with specific metabolic activity and polarization in response to stimulation [16]. Single-cell analysis confirms that AT-macrophages generated in this 3D culture system mirror the phenotypic and functional traits of in-vivo AT resident macrophages [16]. This system enables researchers to maintain the intrinsic properties of resident macrophages during extended culture periods, addressing a significant challenge in macrophage biology research [16]. The ability to faithfully model resident macrophage behavior in vitro provides a valuable platform for investigating their roles in various physiological and pathological contexts, including obesity, metabolic disease, and tissue regeneration [16] [6].
The study of adipose tissue-resident macrophages is crucial for understanding metabolic health, obesity, and related inflammatory diseases. A significant challenge in this field is maintaining macrophages in vitro with phenotypes and functions that accurately reflect their in vivo state. This Application Note details standardized protocols for the 3D culture of functional adipose tissue-resident macrophages, focusing on the essential roles of Macrophage Colony-Stimulating Factor (M-CSF), optimized media formulations, and robust spheroid formation techniques. These methods are designed to provide researchers with reliable tools to generate physiologically relevant models for studying macrophage biology in the context of adipose tissue function and dysfunction [16].
Core Components for Macrophage Culture
The Critical Role of M-CSF
M-CSF is a non-redundant cytokine for the survival, proliferation, and differentiation of macrophages and their progenitors [26]. Recent research has identified bone marrow Adipoq-lineage progenitors as a major cellular source of M-CSF in the bone marrow microenvironment, highlighting a direct link between the adipogenic lineage and myeloid cell homeostasis [26]. For in vitro culture, M-CSF is typically used at a concentration of 10 ng/mL to drive the differentiation of progenitor cells into mature macrophages [16].
Media Formulations and Serum Effects
The choice of culture medium and serum supplementation significantly impacts macrophage morphology, transcriptional profile, and inflammatory responsiveness. Table 1 compares common media formulations used for human monocyte-derived macrophage (hMDM) culture.
Table 1: Comparison of Media Formulations for Human Monocyte-Derived Macrophages
| Media Component | DMEM | RPMI | Macrophage-SFM |
|---|---|---|---|
| Serum Requirement | Typically 10% FBS + 5% human AB serum | Typically 10% FBS + 5% human AB serum | Serum-Free |
| Inflammatory Response to LPS | Robust NF-κB activation and cytokine secretion | Robust NF-κB activation and cytokine secretion (slightly lower than DMEM) | Muted NF-κB activation and cytokine secretion |
| Baseline Phenotype | Pro-inflammatory with higher baseline secretion | Comparable to DMEM | Distinct morphology and dysregulated lipid homeostasis |
| Phagocytic Capacity | High | High | Reduced |
| Key Differentiator | Lacks non-essential amino acids; yields high cytokine output | Contains non-essential amino acids | Designed for specific macrophage culture without serum variables |
Studies demonstrate that hMDMs cultured in DMEM or RPMI, both supplemented with FBS, produce a robust pro-inflammatory response upon LPS stimulation. In contrast, cells cultured in the serum-free M-SFM exhibit a significantly muted inflammatory response. The presence of FBS alone can induce a pro-inflammatory phenotype, underscoring the necessity of carefully matching media formulation to the specific experimental goals [27].
Protocols for 3D Adipose Tissue Macrophage Culture
3D Spheroid Culture of Functional Adipose Tissue Macrophages
This protocol generates functional mature macrophages from murine adipose tissue that closely mirror the phenotypic and functional characteristics of in vivo resident macrophages [16].
Isolation of Stromal Vascular Fraction (SVF):
- Source Tissue: Collect subcutaneous adipose tissue from 6-8 week-old male C57Bl/6J mice.
- Dissociation: Mechanically dissociate the tissue, followed by enzymatic digestion in collagenase NB4 (1.7 U/mL) for 30 minutes at 37°C.
- Processing: Filter the digestate through a cell strainer and centrifuge to obtain a pellet.
- Lysis: Perform red blood cell lysis using NH4Cl (155 mM), K2HPO4 (5.7 mM), and EDTA (0.1 mM).
- Counting: Resuspend the final SVF and count the cells.
Spheroid Formation and Macrophage Generation:
- Seeding: Seed SVF cells on ultra-low attachment 96-well round-bottom plates at a density of 100,000 cells per well in RPMI medium supplemented with Glutamax, 10% heat-inactivated Newborn Calf Serum, 1% penicillin/streptomycin/amphotericin, and M-CSF (10 ng/mL) [16].
- Centrifugation: Briefly centrifuge the plate to aggregate cells at the well bottom.
- Incubation: Incubate cells at 37°C with 5% CO2.
- Spheroid Formation: Cells will spontaneously aggregate into a single spheroid per well within 4 days.
- Macrophage Migration: Around day 7 of culture, macrophages will begin to migrate out of the spheroid and adhere to the plate surface. These cells are mature, functional, and express characteristic macrophage markers like F4/80.
3D Spheroid Culture for Adipose-Derived Stem Cells (ASCs)
This complementary protocol details the formation of 3D spheroids from adipose-derived stem cells, which can serve as a co-culture model or for studying adipocyte-macrophage interactions.
Spheroid Formation via Liquid Overlay Method:
- Cell Source: Use characterized human or bovine Adipose-Derived Stem Cells (ASCs). Bovine ASCs (bASCs) are positive for CD73, CD90, and CD105, and negative for CD56 [28].
- Seeding: Apply a cell suspension in culture medium over a non-adhesive surface (e.g., a plate coated with ELP-PEI copolymer).
- Spheroid Initiation: Spheroids form within 2 days under static culture conditions.
- Enhancement: To improve long-term spheroid retention during media changes, use ELP-PEI copolymer coatings functionalized with RGD peptides, which enhance integrin-mediated adhesion and minimize spheroid loss [29].
Adipogenic Differentiation of ASC Spheroids:
- Differentiation Medium: Use a base medium (e.g., DMEM) supplemented with a simplified cocktail:
- 2.5 µM Rosiglitazone (PPARγ activator)
- 3 µg/mL Insulin
- 1 µM Dexamethasone [28]
- Duration: Differentiate spheroids over 14 days, with medium changes every 2-3 days. Differentiated spheroids will show significant lipid accumulation and expression of markers like PPARγ and Perilipin 1.
Visualization of Culture Workflows and Signaling
3D Spheroid Culture Workflow
The following diagram illustrates the key steps in establishing a 3D spheroid culture for generating adipose tissue-resident macrophages.
M-CSF Signaling in Macrophage Development
This diagram outlines the central role of M-CSF signaling in macrophage development and its functional outcomes, particularly in the adipose and bone marrow niches.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for 3D Adipose Tissue Macrophage Culture
| Reagent/Category | Specific Examples & Functions | Application Context |
|---|---|---|
| Critical Cytokines | M-CSF (10 ng/mL): Essential for myeloid cell differentiation, survival, and proliferation. | Fundamental for all protocols generating macrophages from progenitors. [26] [16] |
| Base Media | RPMI-1640 / DMEM: Standard media for macrophage culture, require serum supplementation. Macrophage-SFM: Serum-free formulation, produces distinct, muted inflammatory responses. | Choose based on need for robust inflammation (RPMI/DMEM) or to avoid serum variables (M-SFM). [27] |
| Serum & Supplements | Fetal Bovine Serum (FBS): Promotes a pro-inflammatory baseline phenotype. Human AB Serum: Often used at 5% for human cell culture. | Serum choice and concentration significantly impact macrophage polarization and function. [27] |
| Adhesion Modifiers | Ultra-Low Attachment (ULA) Plates: Force cell aggregation to form spheroids. RGD-functionalized ELP-PEI Coatings: Enhance spheroid adhesion and retention during long-term culture. | ULA plates are essential for initial spheroid formation. RGD coatings prevent spheroid loss. [29] [16] |
| Differentiation Inducers | Rosiglitazone, Insulin, Dexamethasone: Core cocktail for inducing adipogenic differentiation in ASC spheroids. | For generating adipocyte models to study adipocyte-macrophage crosstalk. [28] |
The study of adipose tissue biology is crucial for understanding metabolic diseases like obesity and type 2 diabetes. Traditional two-dimensional (2D) cell cultures and animal models have significant limitations in replicating human physiology, with low success rates in translating findings from animal experiments to human clinical trials, particularly in inflammation research [30]. This application note details the development and implementation of a advanced three-dimensional (3D) model of vascularized human adipose tissue incorporating functional macrophages. This integrated system more accurately recapitulates the complex cellular crosstalk and tissue physiology of native human adipose tissue, enabling more predictive research in metabolic disease mechanisms and therapeutic development.
Protocol: Establishing Vascularized Adipose Tissue with Macrophages
Cell Sourcing and Isolation
The protocol utilizes human adipose-derived cells to create a personalized, physiologically relevant model.
Human Adipose Stromal Cells (hASC) Isolation: Subcutaneous adipose tissue samples are obtained with ethical approval and patient consent. Tissue is minced and digested with collagenase (2 mg/mL) for 20 minutes at 37°C [30]. The stromal vascular fraction (SVF) is separated via filtration and centrifugation. hASCs are propagated in culture medium containing Dulbecco's Modified Eagle's Medium Nutrient Mixture F-12 (DMEM/F-12), 10% human serum, and 2 mM L-glutamine [30]. Cells are used at passage 2 for experiments.
Adipose Tissue-Derived Endothelial Cell Isolation: Endothelial cells are isolated from the same adipose tissue sample as hASCs using established methods [30]. This allows construction of personalized models. Human umbilical vein endothelial cells (HUVEC) can be used as an alternative source and are propagated in EGM-2 medium [30].
Macrophage Isolation and Differentiation: Primary monocytes are isolated from blood samples and differentiated into macrophages. For personalized models, macrophages can be isolated directly from the same adipose tissue sample as hASCs and endothelial cells [30].
3D Model Assembly and Differentiation
The following workflow outlines the sequential assembly of the vascularized adipose tissue model with integrated macrophages:
Key Steps:
Vascular Network Formation: hASCs and endothelial cells (HUVEC or adipose-derived) are combined in a 3D matrix and cultured for 7-10 days to allow formation of capillary-like structures [30]. The use of natural adipogenesis induction methods like Adipose Tissue Extract (ATE) benefits vascular development compared to chemical cocktails [30].
Adipogenic Differentiation: After vasculature establishment, adipogenesis is induced. We recommend using a natural adipogenesis induction protocol with Adipose Tissue Extract (ATE), which better supports vascular structures, as an alternative to conventional chemical cocktails (insulin, dexamethasone, IBMX, rosiglitazone) [30] [31].
Macrophage Integration: Macrophages are incorporated into the pre-vascularized adipose tissue model. This can be done simultaneously with adipogenesis induction or sequentially after adipocyte differentiation has initiated [30].
Model Characterization and Validation
The developed model requires comprehensive characterization to confirm successful tissue formation:
- Immunocytochemical Analysis: Confirm presence of adipocytes (Perilipin A), endothelial cells (CD31), and macrophages (CD68) [30].
- Functional Assessment: Measure triglyceride accumulation via Oil Red O staining, adipokine secretion (leptin, adiponectin) via ELISA, and glucose uptake assays [30].
- Morphological Evaluation: Verify formation of unilocular lipid droplets in adipocytes and interconnected capillary networks [31].
Key Findings and Data Outputs
Macrophage Impact on Adipogenesis and Inflammation
Experimental data derived from this model demonstrates critical macrophage-adipocyte interactions. Researchers have observed that lipid accumulation in adipocytes is significantly greater in the presence of macrophages [30]. The pro-inflammatory cytokine Interferon-gamma (IFNγ) amplifies this effect, increasing the difference in lipid accumulation between adipocyte-only cultures and adipocyte-macrophage co-cultures [30]. Furthermore, macrophages have a more pronounced effect on protein secretion patterns in non-vascularized models compared to vascularized ones, highlighting the modulating role of vasculature in inflammatory crosstalk [30].
Macrophage Phenotypes Across Adipose Depots
The table below summarizes quantitative findings on macrophage subpopulations in human adipose tissues, which can be replicated and studied using this advanced model:
Table 1: Macrophage Phenotypes in Human Adipose Tissue Depots
| Adipose Tissue Depot | Pro-inflammatory (M1-like) Macrophages | Anti-inflammatory (M2-like) Macrophages | Key Identifying Markers |
|---|---|---|---|
| Subcutaneous (SCAT) | Lower proportion [32] | Higher proportion [32] | CD16+CD36+ (pro-inflammatory); CD16-CD163+ (anti-inflammatory) [32] |
| Visceral (VAT) | ~2x higher than SCAT [32] | Lower proportion [32] | |
| Perivascular (PVAT) | ~2x higher than SCAT [32] | Lower proportion [32] | |
| Vasculature-Associated (VAMs) | Present, adapt to stimuli [33] | Present, adapt to stimuli [33] | High endocytic capacity; associated with blood vessels [33] |
These depot-specific differences are substantially more pronounced in postmenopausal women, potentially linked to increased cardiovascular risk [32]. The developed model allows investigation of these distinct macrophage populations in a controlled setting.
Signaling Pathways in Adipose Tissue Inflammation
The following diagram illustrates key inflammatory signaling pathways operational in the adipose tissue microenvironment that can be studied using this model:
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Vascularized Adipose Tissue Models
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Sources | hASC, Adipose-derived Endothelial Cells, HUVEC, Monocytes/Macrophages [30] | Primary building blocks for constructing 3D models; enable personalized approaches |
| Culture Media | hASC Medium (DMEM/F-12 + Human Serum + L-Glutamine), EGM-2, Macrophage Differentiation Media [30] | Cell propagation and maintenance |
| Differentiation Inducers | Adipose Tissue Extract (ATE), Chemical Cocktail (Insulin, Dexamethasone, IBMX, Rosiglitazone) [30] [31] | Induce adipogenesis from stem/progenitor cells |
| Cytokines & Stimuli | Interferon-gamma (IFNγ), TNFα, LPS, Free Fatty Acids [30] [33] | Model inflammatory conditions and metabolic stress |
| 3D Scaffolds/Matrices | Collagen Type I, Fibrin, Decellularized Adipose ECM, Synthetic Hydrogels (PEG, GelMA) [34] [31] | Provide 3D structural support mimicking native extracellular matrix |
| Analysis Reagents | Oil Red O, Antibodies (Perilipin A, CD31, CD68), ELISA Kits (Leptin, Adiponectin) [30] | Model characterization, functional assessment, and endpoint analysis |
Applications in Disease Modeling and Drug Development
This advanced model system enables numerous research applications with enhanced physiological relevance:
Obesity and Type 2 Diabetes Research: Study the development of insulin resistance in response to lipotoxic conditions, chronic inflammation, and endocrine dysfunction [30] [31]. The model reproduces key features of metabolic syndrome, including adipokine dysregulation (shift in adiponectin-to-leptin ratio) [31].
Cancer Research: Model obesity-associated cancers, particularly breast cancer, where the adipose microenvironment influences tumor progression and chemotherapy resistance [34]. Co-culture with cancer cells creates an inflamed adipose border typical of obese patients.
Drug Efficacy and Toxicity Screening: Serve as a human-relevant platform for preclinical compound testing. 3D adipose models have shown increased resistance to certain chemotherapeutic agents (e.g., paclitaxel) and altered sensitivity to metabolic drugs (e.g., metformin) compared to 2D cultures, better predicting in vivo responses [34] [35].
Personalized Medicine Approaches: Using cells isolated from a single donor allows creation of patient-specific models for evaluating individual treatment responses and studying rare medical conditions [30].
The vascularized adipose tissue model with integrated macrophages represents a significant advancement over traditional 2D cultures and animal models for metabolic research. By incorporating key cellular components—adipocytes, vasculature, and immune cells—within a 3D architecture, this system more faithfully recapitulates human adipose tissue physiology and disease pathologies. The protocols and data presented herein provide researchers with a roadmap for implementing this advanced model system, which promises to enhance our understanding of metabolic diseases and improve the predictive value of preclinical drug development.
Adipose tissue (AT) is a dynamic endocrine organ, and its dysfunction, characterized by chronic low-grade inflammation, is a hallmark of obesity and related metabolic disorders [15] [36]. The metabolic crosstalk between adipocytes and immune cells, particularly macrophages, is central to this process. In lean states, AT macrophages (ATMs) typically exhibit an anti-inflammatory, M2-like phenotype that supports tissue homeostasis [37] [36]. However, during obesity, lipid overload and microenvironmental stress trigger a shift in ATM polarization towards pro-inflammatory states, leading to the secretion of cytokines that impair insulin signaling and promote systemic metabolic dysfunction [36] [5]. Advanced 3D co-culture systems that accurately mimic the human adipose tissue microenvironment are crucial for dissecting this complex cellular communication and for the preclinical testing of therapeutic interventions [15] [38]. This application note details a standardized, animal-free protocol for establishing a human 3D adipocyte-macrophage co-culture model to study metabolic crosstalk.
Establishing a Defined 3D Co-Culture System
The following section outlines the methodology for creating a physiologically relevant, animal-free model of human adipose tissue inflammation.
The experimental process, from cell preparation to analysis, is summarized in the diagram below.
Detailed Experimental Protocol
Materials and Reagent Preparation
- Gellan Gum (GG) Hydrogel: Prepare a sterile, 1.5% (w/v) solution of high-purity gellan gum (e.g., Gelzan, Phytagel) in ultrapure water. Heat until completely dissolved and clear. Maintain at 37°C until cell encapsulation to prevent premature gelling [15].
- Defined Culture Medium: Use a commercially available serum-free medium or formulate in-house. The medium must support the viability of both adipocytes and macrophages. It is critical to avoid fetal calf serum (FCS) to eliminate batch variability and animal-derived components [15].
- Cell Lines: Use human monocytic cell lines THP-1 or Mono Mac-6 (MM6). Primary mature human adipocytes are isolated from adipose tissue samples via collagenase digestion and flotation [15] [38].
- Activation Stimuli: Prepare stock solutions of Phorbol 12-myristate 13-acetate (PMA) and Lipopolysaccharide (LPS) in DMSO and PBS, respectively. Use a combination of PMA (e.g., 100 nM) and LPS (e.g., 100 ng/mL) to activate macrophages and induce a pro-inflammatory state in the co-culture [15].
Step-by-Step Co-culture Assembly
Encapsulate Adipocytes in 3D Hydrogel:
- Gently mix isolated primary human mature adipocytes with the liquefied gellan gum solution at a density of 1-5 x 10^5 cells/mL of hydrogel.
- Pipet the cell-hydrogel mixture into the desired cultureware (e.g., 24-well plate). Allow gelation to occur for 15-30 minutes at room temperature or 4°C, as per the manufacturer's instructions [15].
- Once polymerized, carefully overlay the gels with the defined culture medium.
Differentiate Monocytes into Macrophages:
- Culture THP-1 or MM6 cells in defined medium. Differentiate THP-1 cells by treating with 100 nM PMA for 48 hours. For MM6 cells, follow established differentiation protocols suitable for serum-free conditions [15].
- After differentiation, gently wash the macrophages to remove non-adherent cells and PMA.
Establish Co-culture:
Induce Inflammation and Harvest:
- Challenge the assembled co-culture system with a combination of PMA and LPS for up to 72 hours to induce a robust inflammatory response.
- Post-incubation, collect conditioned media for subsequent analysis (e.g., cytokine profiling). Process the hydrogel and cells for viability assays, RNA/protein extraction, or immunohistochemistry [15].
Key Analytical Outcomes and Data
This co-culture system reliably models key aspects of adipose tissue inflammation, yielding both quantitative and functional data.
Viability and Inflammatory Profile
Upon activation with PMA+LPS, the system maintains high adipocyte viability while inducing a distinct pro-inflammatory cytokine profile from the macrophages.
Table 1: Representative Cell Viability and Cytokine Secretion Post PMA+LPS Activation (72h)
| Cell Type / Parameter | Unstimulated Control | PMA+LPS Stimulated | Measurement Method |
|---|---|---|---|
| THP-1 Macrophages | |||
| Viability | ~83-86% | ~57-58% | Flow cytometry [15] |
| IL-6 Secretion | Low | Significantly Increased | ELISA [15] [39] |
| TNF-α Secretion | Low | Significantly Increased | ELISA [39] [5] |
| Primary Adipocytes in GG Hydrogel | |||
| Viability | High | Maintained High | Live/Dead staining [15] |
| Lipid Content (Perilipin A) | High | Maintained (in untreated models) | Immunofluorescence [15] |
Molecular Pathways of Metabolic Crosstalk
The dialogue between adipocytes and macrophages is mediated by soluble factors and direct contact, activating specific signaling pathways that disrupt metabolic homeostasis. The key molecular interactions are illustrated below.
- Cytokine-Mediated Insulin Resistance: Macrophage-derived IL-6, TNF-α, and IL-1β downregulate the expression of GLUT4 and impair insulin-induced Akt phosphorylation in adipocytes, directly contributing to insulin resistance [39].
- Lipid-Induced Inflammation & Ferroptosis: In obesity, TIPE2 loss in macrophages promotes excessive mitochondrial fission and reduces the delivery of exosomal ferritin to adipose stem cells (ASCs). This results in Fe²⁺ and ROS overload in ASCs, leading to lipid peroxidation and a novel form of cell death called ferroptosis, which contributes to ASC shortage and visceral fat dysfunction [37].
- Functional Impairment: Macrophages from obese AT can fuel adipogenesis and lipid accumulation in pre-adipocytes, while T cells and dendritic cells further amplify the expression of inflammatory chemokines like CCL5 and CXCL10, creating a self-sustaining inflammatory loop [5].
The Scientist's Toolkit
A successful animal-free co-culture experiment relies on key reagents and materials. The following table lists essential solutions.
Table 2: Essential Research Reagents for Animal-Free Adipocyte-Macrophage Co-culture
| Reagent / Material | Function & Application | Specific Example |
|---|---|---|
| Gellan Gum Hydrogel | Animal-free 3D scaffold providing structural support for adipocyte encapsulation, maintaining morphology and function. | Gelzan, Phytagel [15] |
| Serum-Free/Defined Medium | Supports co-culture without animal serum, ensuring reproducibility and eliminating confounding factors from batch variations. | Custom formulation or commercial SFM [15] |
| Human Monocytic Cell Lines | Consistent source for generating human macrophages; THP-1 and MM6 are well-characterized for co-culture studies. | THP-1, Mono Mac-6 (MM6) [15] |
| PMA & LPS | Pharmacological activators used in combination to differentiate monocytes and induce a pro-inflammatory state in macrophages. | Phorbol 12-myristate 13-acetate, Lipopolysaccharide [15] |
| Collagenase, Type I | Enzyme for the digestion of human adipose tissue samples to isolate primary mature adipocytes. | From Clostridium histolyticum [38] |
| FFA Assay Kits | For quantifying free fatty acid transfer between adipocytes and co-cultured cells, a key metabolic readout. | Colorimetric/Fluorometric kits [38] |
The advent of personalized medicine has necessitated the development of advanced in vitro models that accurately recapitulate human disease pathophysiology. This application note details protocols for generating patient-specific functional adipose tissue-resident macrophages within three-dimensional (3D) culture systems. These models serve as powerful tools for exploring metabolic diseases, screening drug candidates, and investigating individual-specific immune-metabolic responses [11] [15]. The 3D microenvironment is critical for maintaining the phenotypic and functional characteristics of resident macrophages, which are often lost in traditional two-dimensional (2D) culture systems [11] [16]. By utilizing patient-derived cells, researchers can create more physiologically relevant models that account for human genetic diversity and disease-specific modifications.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential research reagents for generating 3D adipose tissue-resident macrophage cultures.
| Reagent Category | Specific Product/Type | Function and Application Notes |
|---|---|---|
| Cell Sources | Adipose Stromal Vascular Fraction (SVF) [11] [16] | Provides progenitor cells for generating resident macrophages; maintains tissue-specific imprinting. |
| Simpson-Golabi-Behmel Syndrome (SGBS) preadipocyte cell strain [40] | Human preadipocyte model for co-culture studies; high capacity for adipogenic differentiation. | |
| THP-1 or Mono Mac-6 (MM6) monocytic cell lines [15] | Human monocytic cells for generating macrophages in defined, animal-free systems. | |
| Culture Matrices | Ultra-low attachment plates [11] [16] | Enables scaffold-free spheroid formation for 3D culture. |
| Gellan Gum (GG) hydrogel [15] | Animal-free, bacteria-derived polysaccharide hydrogel for 3D cell encapsulation. | |
| Critical Media Components | Macrophage Colony-Stimulating Factor (M-CSF) [11] [16] | Essential cytokine for macrophage differentiation and survival (10 ng/mL). |
| Defined, serum-free medium [15] | Eliminates batch variability and unknown factors from fetal calf serum. | |
| Activation/Polarization Agents | Interleukin-4 (IL-4) [11] [16] | Induces alternative (M2) macrophage polarization (10 ng/mL). |
| Interferon-γ (IFN-γ) [11] [16] | Induces classical (M1) macrophage polarization (50 ng/mL). | |
| Phorbol 12-myristate 13-acetate (PMA) + Lipopolysaccharide (LPS) [15] | Combined stimulus for monocyte activation and pro-inflammatory cytokine production. |
Comparative Analysis of Macrophage Generation Platforms
Table 2: Platform comparison for generating adipose tissue-resident macrophages.
| Parameter | 3D Murine AT-Macrophage Model [11] [16] | Human SGBS/THP-1 Co-culture [40] | Animal-Free Human Co-culture [15] |
|---|---|---|---|
| Species Origin | Mouse (C57Bl/6J) | Human | Human |
| Core Cell Types | Adipose SVF-derived macrophages | SGBS adipocytes + THP-1 macrophages | Primary mature adipocytes + MM6/THP-1 macrophages |
| Culture Format | Scaffold-free spheroids | 2D direct co-culture or conditioned medium | 3D hydrogel encapsulation (Gellan Gum) |
| Key Macrophage Features | Recapitulates in vivo resident macrophages (Timd4+, Lyve1+); distinct from BM-derived macrophages | Responsive to paracrine signals from adipocytes; produces inflammatory cytokines | Activated with PMA+LPS; produces IL-6, IL-1β, TNFα |
| Differentiation Timeline | ~7 days for initial spread; ~13 days for mature macrophages | ~7 days for SGBS adipogenesis; ~3 days for THP-1 macrophage differentiation | ~72 hours for inflammatory activation |
| Unique Applications | Studying tissue-resident macrophage biology; metabolism and polarization studies | Human-specific adipocyte-macrophage crosstalk; drug screening | Preclinical testing in defined, xeno-free conditions; high reproducibility |
Protocol 1: Generation of Murine Adipose Tissue-Resident Macrophages in 3D Culture
Background and Principle
This protocol adapts a method for generating functionally active resident macrophages from adipose tissue within a 3D environment [11] [16]. The 3D culture system enables the production of mature macrophages that mirror the phenotypic and functional traits of in vivo AT resident macrophages without the need for cell sorting, which often alters intrinsic cellular properties [11]. The generated macrophages display distinct transcriptomic, phenotypic, and metabolic characteristics compared to bone marrow-derived macrophages, making them particularly valuable for studying tissue-specific immune responses [16].
Materials and Reagents
- Animals: 6- to 8-week-old male C57Bl/6J mice [11] [16]
- Digestion Buffer: HBSS with 1.7 U/mL collagenase NB4 and 2.5 U/mL dispase I [16]
- Culture Medium: RPMI supplemented with Glutamax, 10% Heat Inactivated Newborn Calf Serum, 1% penicillin/streptomycin/amphotericin, and 10 ng/mL M-CSF [11] [16]
- Cultureware: Ultra-low adherence 96-well round bottom plates [11]
- Dissociation Solution: NB4 (1.7 U/mL) and dispase I (2.5 U/mL) for spheroid dissociation [16]
Step-by-Step Procedure
Isolation of Stromal Vascular Fraction (SVF):
- Harvest subcutaneous adipose tissue and remove lymph nodes.
- Mechanically dissociate tissue and digest with collagenase NB4 at 37°C for 30 minutes.
- Filter through a 100-μm cell strainer and centrifuge at 500 × g for 5 minutes.
- Resuspend pellet in red blood cell lysis buffer (155 mM NH₄Cl, 5.7 mM K₂HPO₄, 0.1 mM EDTA) for 5 minutes at room temperature.
- Centrifuge, resuspend in culture medium, and count viable cells [11] [16].
3D Spheroid Culture Setup:
- Seed SVF cells at a density of 10⁵ cells/well in ultra-low adherence 96-well round bottom plates.
- Centrifuge plates briefly at 300 × g to encourage cell aggregation.
- Incubate at 37°C with 5% CO₂ [11].
Macrophage Generation and Harvest:
- After 4 days, observe spontaneous aggregation forming spheroids.
- By day 7, macrophages begin to migrate out of spheroids and adhere to the plate.
- For analysis, harvest spheroids between days 7-21.
- Dissociate spheroids with NB4 (1.7 U/mL) and dispase I (2.5 U/mL) at 37°C for 40 minutes with periodic mechanical pipetting [16].
Macrophage Polarization:
Expected Outcomes
- Spheroid Formation: Visible cell aggregates by day 4 of culture.
- Macrophage Migration: Cells spreading from spheroids beginning day 7.
- Macrophage Yield: Functional mature macrophages by day 13.
- Phenotypic Validation: Generated macrophages express resident macrophage markers (Timd4, Lyve1, CD206) and demonstrate specific metabolic activity and polarization responses [11] [16].
Protocol 2: Animal-Free Human 3D Adipocyte-Macrophage Co-culture
Background and Principle
This protocol describes a completely animal-free system for co-culturing human mature adipocytes and macrophages within a 3D environment [15]. The model utilizes gellan gum as a xeno-free hydrogel matrix and a defined culture medium to eliminate batch-to-batch variability associated with fetal calf serum. This system successfully creates an inflamed adipose tissue microenvironment suitable for testing anti-inflammatory therapeutics and studying human-specific disease mechanisms [15]. The setup is particularly valuable for personalized medicine applications, as it can be adapted to incorporate patient-derived primary cells.
Materials and Reagents
- Hydrogel Matrix: Gellan gum (GG) prepared according to manufacturer specifications [15]
- Cell Sources: Primary human mature adipocytes and MM6 or THP-1 monocytic cell lines [15]
- Defined Culture Medium: Serum-free formulation developed in-house [15]
- Activation Stimuli: PMA (phorbol 12-myristate 13-acetate) and LPS (lipopolysaccharide) [15]
Step-by-Step Procedure
Adipocyte Encapsulation:
- Resuspend primary human mature adipocytes in liquid gellan gum solution at 4°C.
- Quickly plate the cell-hydrogel mixture and incubate at 37°C to induce gelation.
- Culture in defined medium for 24 hours before co-culture establishment [15].
Monocyte Activation:
- Culture MM6 or THP-1 cells in defined medium.
- Activate with PMA and LPS combination according to optimized concentrations.
- Confirm activation by observing characteristic cell aggregation and cytokine production [15].
Co-culture Establishment:
- Add activated monocytes to the adipocyte-loaded gellan gum hydrogels.
- Maintain in defined culture medium at 37°C with 5% CO₂.
- The system remains viable and functional for at least 72 hours [15].
Inflammatory Stimulation and Analysis:
- Stimulate with PMA+LPS to induce pro-inflammatory state.
- Monitor viability, intracellular lipid content, and perilipin A expression.
- Quantify inflammatory cytokines (IL-6, IL-1β, TNFα) in supernatant [15].
Expected Outcomes
- Successful Activation: PMA+LPS stimulated monocytes show characteristic aggregation and distinct cytokine profiles.
- Maintained Adipocyte Function: High viability and preserved lipid content in encapsulated adipocytes.
- Inflammatory Phenotype: Activated co-culture secretes pro-inflammatory cytokines including IL-6, IL-1β, and TNFα.
- Model Utility: Reproducible, animal-free test system suitable for pharmacological studies [15].
Key Signaling Pathways in Adipocyte-Macrophage Crosstalk
The interaction between adipocytes and macrophages involves complex signaling pathways that maintain tissue homeostasis or drive inflammation in metabolic diseases. Understanding these pathways is essential for leveraging 3D co-culture models in personalized medicine applications.
TNFα Signaling Pathway
Resident adipose tissue macrophages play a regulatory role in maintaining mature adipocyte phenotype and preventing excessive dedifferentiation [8]. Macrophage depletion experiments have shown enrichment of the TNFα signaling pathway, with direct TNFα stimulation decreasing adipocyte dedifferentiation [8]. This pathway represents a crucial mechanism by which macrophages influence adipose tissue plasticity and function.
Metabolic Integration Pathways
Adipose tissue macrophages demonstrate specific metabolic activities that differ based on their origin and polarization state [11]. Resident macrophages generated through 3D culture show distinct metabolic profiles compared to bone marrow-derived macrophages, reflecting their specialized functions in maintaining tissue homeostasis [11] [16]. These metabolic pathways integrate with inflammatory signaling to coordinate overall tissue response to nutritional status and cellular stress.
Polarization Signaling Networks
Macrophages in 3D adipose cultures respond to polarization stimuli differently than traditional models [11]. The 3D environment influences cytokine response patterns, with IL-4 inducing alternative activation and IFN-γ driving classical activation through distinct signaling cascades that modulate inflammatory output and cellular function [11] [16]. These polarization states significantly impact adipocyte function, creating feedback loops that either maintain homeostasis or drive disease progression.
Troubleshooting and Optimization Guidelines
Table 3: Troubleshooting guide for 3D adipose tissue-macrophage cultures.
| Problem | Potential Causes | Solutions |
|---|---|---|
| Poor spheroid formation | Insufficient cell density; inadequate centrifugation | Increase seeding density to 10⁵ cells/well; ensure proper centrifugation at 300 × g [11] |
| Low macrophage yield | Suboptimal M-CSF concentration; impaired differentiation | Verify M-CSF activity and maintain at 10 ng/mL; confirm tissue digestion efficiency [11] [16] |
| High adipocyte death in 3D | Excessive hydrogel stiffness; oxidative stress | Optimize gellan gum concentration; consider antioxidant supplementation [15] |
| Weak inflammatory response | Inadequate monocyte activation; donor variability | Titrate PMA+LPS concentrations; pre-test monocyte responsiveness [15] |
| Loss of resident macrophage markers | Overly prolonged culture; microenvironment mismatch | Harvest macrophages at earlier time points (days 7-13); verify 3D matrix composition [11] [16] |
Applications in Personalized Medicine and Drug Development
The patient-specific 3D adipose tissue-macrophage models described herein enable researchers to investigate individual variations in disease mechanisms and treatment responses. These systems permit:
- Patient-Specific Disease Modeling: Incorporation of patient-derived adipocytes and macrophages to create individualized disease models [15]
- Drug Screening Platforms: Medium-throughput capability for testing anti-inflammatory compounds in a human-relevant system [40] [15]
- Mechanistic Studies: Investigation of signaling pathways in a controlled yet physiologically relevant environment [11] [8]
- Toxicity Assessment: Evaluation of compound effects on human adipose tissue immune function without species translation concerns [15]
These applications highlight the transformative potential of 3D patient-specific models in advancing personalized medicine for metabolic diseases, inflammation disorders, and immune-metabolic conditions.
Troubleshooting and Optimizing Your 3D Macrophage Culture System
In the field of 3D cell culture research, particularly for the generation of functional adipose tissue-resident macrophages, the development of hypoxic cores within spheroids represents a critical challenge to cell viability and experimental validity. Spheroids that exceed a critical diameter develop diffusion-limited oxygen and nutrient gradients, leading to a necrotic core that compromises cellular function and introduces experimental artifacts [41]. For researchers investigating adipose tissue macrophages (ATMs), which play pivotal roles in maintaining tissue homeostasis under both physiological and pathological conditions, preserving cell viability and function in vitro is paramount [11] [16]. This application note provides detailed, practical methodologies for preventing hypoxic core formation in spheroid cultures, specifically contextualized within adipose tissue-resident macrophage research.
The Hypoxic Core Challenge in Spheroid Research
Physiological Spheroid Organization and Hypoxia Development
Spheroids mimic the complex architecture of solid tissues by developing three distinct cellular zones: an outer layer of highly proliferative cells, an intermediate layer containing quiescent cells, and an inner core characterized by hypoxic and acidic conditions when diffusion limitations occur [41]. This cellular heterogeneity creates critical gradients of oxygen, nutrients, and signaling molecules that significantly impact cell viability and function [41].
In the context of adipose tissue-resident macrophage research, where 3D culture systems enable the generation of functional mature macrophages that mirror the phenotypic and functional traits of in-vivo AT resident macrophages, preventing unintended hypoxia is essential for maintaining physiological relevance [11] [16]. Uncontrolled hypoxia can alter macrophage polarization, metabolic activity, and inflammatory responses, thereby compromising experimental outcomes.
Quantitative Relationship Between Spheroid Size and Hypoxia
Table 1: Spheroid Size Parameters and Their Impact on Viability
| Spheroid Diameter (μm) | Core Viability Status | Oxygen Diffusion | Suitability for ATM Research |
|---|---|---|---|
| 100-200 | Fully viable | Unrestricted | Excellent for uniform cultures |
| 200-300 | Pre-hypoxic state | Limited diffusion | Good with monitoring |
| 300-500 | Hypoxic core developing | Significantly limited | Requires intervention |
| >500 | Necrotic core present | Severely limited | Unsuitable for functional studies |
Research on pancreatic ductal adenocarcinoma (PDAC) spheroids has demonstrated that spheroid size directly correlates with the development of hypoxic cores. In one study, PANC-1 spheroids grew from approximately 500μm to 1,000μm in diameter over 10 days, developing significant central hypoxia, while BxPC-3 spheroids maintained a consistent ~300μm diameter without developing hypoxic cores under the same culture conditions [42]. This quantitative relationship provides critical guidance for establishing appropriate spheroid size parameters in adipose tissue macrophage research.
Experimental Protocols for Hypoxia Prevention
Protocol 1: Size-Controlled Spheroid Production for ATM Research
This protocol adapts the established method for generating functional ATMs from adipose stromal vascular cells (SVCs) while incorporating specific size-control measures [11].
Materials:
- Stromal vascular cells isolated from murine subcutaneous adipose tissue [11]
- Ultra-low adherence 96-well round bottom plates (e.g., COSTAR) [11]
- Roswell Park Memorial Institute (RPMI) medium with Glutamax [11]
- Heat Inactivated Newborn Calf Serum (hiNBCS; 10%) [11]
- Macrophage colony-stimulating factor (M-CSF; 10 ng/ml) [11]
- Antibiotic/antimycotic cocktail (1%) [11]
- Centrifuge with plate adapters
Method:
- Isolate the stromal vascular fraction (SVF) from subcutaneous adipose tissues through mechanical dissociation and enzymatic digestion with collagenase at 37°C for 30 minutes [11].
- After filtration, centrifugation, and red blood cell lysis, resuspend SVF cells in RPMI medium supplemented with 10% hiNBCS, 1% antibiotic/antimycotic, and 10 ng/ml M-CSF [11].
- Seed cells onto ultra-low adherence 96-well round bottom plates at a density of 1×10⁵ cells/well [11].
- Centrifuge plates briefly at 500 × g for 5 minutes to promote initial cell aggregation.
- Incubate at 37°C with 5% CO₂. After 4 days, cells spontaneously aggregate to form spheroids [11].
- Monitor spheroid diameter daily using microscopy. For adipose tissue macrophage cultures, maintain spheroids below 300μm diameter [42].
- If spheroids approach the critical size threshold, gently dissociate and reseed at lower density using enzymatic digestion with NB4 (1.7 U/ml) and dispase I (2.5 U/ml) at 37°C for 40 minutes [11].
- Starting on day 7, macrophages begin to spread out of the spheroid and adhere to the culture plate, where they can be harvested for functional assays [11].
Protocol 2: ECM Optimization to Enhance Oxygenation
Extracellular matrix (ECM) components can significantly influence spheroid compactness and oxygen diffusion. This protocol describes ECM optimization for preventing hypoxia.
Materials:
- Matrigel (for PANC-1:hPSC spheroids) [42]
- Collagen I (15-60 μg/mL) [42]
- PDAC cell lines (PANC-1, BxPC-3) or adipose-derived stromal cells
- Pancreatic stellate cells (hPSCs) for co-culture [42]
Method:
- For PANC-1-based spheroids, supplement culture medium with 2.5% Matrigel to promote formation of smaller, denser spheroids (500μm diameter) rather than large, loosely packed aggregates [42].
- For BxPC-3-based spheroids, use Matrigel-free medium to maintain consistent ~300μm diameter spheroids without hypoxic cores [42].
- As an alternative to Matrigel, test collagen I supplementation at 15-60 μg/mL to improve spheroid uniformity, though note that this may induce invasiveness in some cell types [42].
- For adipose tissue research, optimize ECM composition based on specific research goals—Matrigel for dense, uniform spheroids, or collagen for modeling invasive characteristics.
- Monitor spheroid morphology and size daily, adjusting ECM components accordingly to maintain optimal diameter below 300μm.
Visualization of Experimental Workflows
Spheroid Generation and Hypoxia Prevention Workflow
Diagram 1: Experimental workflow for generating viable spheroids without hypoxic cores
Size-Hypoxia Relationship in Spheroids
Diagram 2: Relationship between spheroid size and hypoxia development
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Hypoxia-Free Spheroid Culture
| Reagent/Category | Specific Product Examples | Function in Spheroid Research | Application Notes |
|---|---|---|---|
| Low-Adhesion Plates | COSTAR ULA 96-well round bottom plates | Prevents cell attachment, promotes 3D aggregation | Critical for consistent spheroid formation [11] |
| Digestive Enzymes | Collagenase NB4, Dispase I | Dissociates oversized spheroids for reseeding | Use at 1.7 U/ml and 2.5 U/ml respectively [11] |
| Growth Factors | Macrophage CSF (M-CSF) | Promoves macrophage differentiation from SVF | Use at 10 ng/ml for ATM generation [11] |
| ECM Components | Matrigel, Collagen I | Modulates spheroid compactness and size | Matrigel at 2.5% for PANC-1; avoid for BxPC-3 [42] |
| Culture Media | RPMI with Glutamax, 10% hiNBCS | Provides nutrient base for cell growth | Supplement with antibiotic/antimycotic cocktail [11] |
| Cell Lines | PANC-1, BxPC-3, adipose SVF | Model systems for spheroid optimization | PANC-1 requires ECM support; BxPC-3 self-aggregates [42] |
Maintaining spheroid viability by preventing hypoxic core formation is achievable through rigorous size control, strategic ECM optimization, and continuous monitoring. For adipose tissue-resident macrophage research, where preserving physiological function is paramount, implementing these protocols will enhance experimental reproducibility and biological relevance. The optimal spheroid diameter of 200-300μm provides sufficient biomass for analysis while avoiding diffusion limitations that compromise cell viability and function.
The study of adipose tissue biology is pivotal for understanding metabolic health and diseases such as obesity and type 2 diabetes. Adipose tissue is now recognized as a dynamic endocrine organ that plays a central role in regulating systemic metabolism, energy balance, and inflammation, rather than merely serving as a passive lipid storage depot [43] [44]. The functional interplay between adipocytes and immune cells—particularly adipose tissue macrophages (ATMs)—creates a complex microenvironment that dictates metabolic outcomes. Recent research has established that glucose metabolism is intrinsically linked to the inflammatory status of macrophages, which in turn plays an integral role in promoting obesity-related insulin resistance [45].
The development of physiologically relevant three-dimensional (3D) adipose tissue models has emerged as a crucial advancement for studying metabolic processes in vitro. These models overcome the limitations of traditional 2D cell culture by better replicating the architectural and functional complexity of native adipose tissue [44]. This Application Note provides detailed protocols for establishing 3D co-culture systems of human adipocytes and macrophages, with specific emphasis on optimizing glucose concentrations to balance lipogenic and lipolytic functions while maintaining physiologically relevant immune-metabolic crosstalk.
Key Principles of Glucose Metabolism in Adipose Tissue Macrophages
Energy metabolism in macrophages fundamentally shapes their inflammatory response and polarization state, particularly in the context of obesity [46] [47]. Glucose serves as a critical fuel substrate that drives macrophage activation and function. Evidence indicates that overexpression of GLUT1, the primary glucose transporter in macrophages, results in elevated glucose uptake and metabolism, creating a hyper-inflammatory state characterized by elevated secretion of MCP-1 and PAI-1 [45]. Conversely, macrophage-specific Glut1 knockout mice fed a high-fat diet demonstrate resistance to obesity, maintained normoglycemia, and blunted inflammation in liver and adipose tissue [45].
Beyond its role as an energy source, glucose can modulate macrophage energy metabolism and inflammatory responses through several mechanisms: feeding into non-oxidative pathways (such as the pentose phosphate pathway), acting as signaling molecules, or mediating post-translational modifications (including O-GlcNAcylation or β-hydroxybutyrylation) [46] [47]. Understanding these metabolic-inflammatory axes is essential for developing targeted therapeutic strategies for obesity-related metabolic disorders.
Table 1: Key Metabolic Pathways Linking Glucose Metabolism to Macrophage Function
| Metabolic Pathway | Key Enzymes/Transporters | Impact on Macrophage Function | Therapeutic Potential |
|---|---|---|---|
| Glycolysis | GLUT1, HK, PFK | Drives pro-inflammatory polarization; Hyper-inflammatory state when enhanced | GLUT1 inhibition reduces inflammation and obesity susceptibility |
| Pentose Phosphate Pathway | G6PD | Generates NADPH for antioxidant defense | May influence redox balance in adipose tissue |
| O-GlcNAcylation | OGT, OGA | Post-translational modification of signaling proteins | Emerging target for metabolic regulation |
| β-hydroxybutyrylation | Ketone-mediated post-translational modification | Links ketone metabolism to epigenetic regulation |
Establishing a 3D Human Adipocyte-Macrophage Co-Culture System
A recently developed completely animal-free 3D co-culture system provides an ideal platform for studying glucose-mediated effects on lipogenesis and lipolysis in a defined environment [15]. This model utilizes human primary mature adipocytes encapsulated in gellan gum (GG) hydrogels co-cultured with human monocytic cell lines (MM6 or THP-1) in serum-free medium. The system successfully replicates key aspects of human adipose tissue inflammation, including macrophage infiltration and pro-inflammatory cytokine release, which are hallmark features of obese adipose tissue [15].
Gellan gum was selected as the scaffold material due to its biocompatibility, non-toxicity, and tunable physical properties. This bacteria-derived exopolysaccharide represents a promising animal-free alternative to traditional extracellular matrix components like collagen or Matrigel [15]. The thermosensitive nature of GG and its cross-linking capability with mono- and divalent cations allows for precise modification of hydrogel stiffness and pore size to mimic native adipose tissue mechanical properties.
Protocol: 3D Adipose Tissue Co-Culture Setup
Materials Required:
- Cells: Human primary mature adipocytes (isolated from lipoaspirates), MM6 or THP-1 monocytic cell lines
- Scaffold Material: Gellan gum (GG)
- Culture Vessels: Ultra-low attachment (ULA) plates or spinner flask systems
- Basal Medium: DMEM/F12
- Differentiation Cocktail: Insulin (1-5 μg/mL), dexamethasone (1 μM), pantothenate (17 μM), biotin (33 μM), 2,3-thiazolidinediones (TZD, 1 μM), 3-isobutyl-1-methylxanthine (IBMX, 100 μM)
- Maintenance Medium: Basal medium supplemented with insulin (1-5 μg/mL) only
- Inflammatory Stimuli: Phorbol 12-myristate 13-acetate (PMA, 10-100 nM) and lipopolysaccharide (LPS, 10-100 ng/mL)
Procedure:
Gellan Gum Hydrogel Preparation:
- Prepare a sterile 1.5% (w/v) gellan gum solution in ultrapure water.
- Heat the solution to 90°C with stirring until completely dissolved.
- Cool to 37°C and mix with cell suspension.
- Transfer to multi-well plates and cross-link by adding calcium chloride solution (50 mM final concentration).
- Incubate for 30 minutes at room temperature to form stable hydrogels.
Adipocyte Encapsulation:
- Isolate human primary mature adipocytes from lipoaspirates via collagenase digestion and centrifugation.
- Resuspend adipocytes in gellan gum solution at a density of 2-5 × 10^6 cells/mL prior to cross-linking.
- Plate 500 μL of the cell-gellan gum mixture per well in 24-well ULA plates.
- Allow complete cross-linking before adding culture medium.
Macrophage Differentiation and Activation:
- Culture MM6 or THP-1 cells in defined serum-free medium.
- Differentiate monocytes to macrophages using PMA (10 nM for 24 hours).
- Activate macrophages with LPS (10-100 ng/mL for 24 hours) to induce pro-inflammatory polarization.
- For co-culture, add activated macrophages to the adipocyte-containing hydrogels at a 1:5 macrophage:adipocyte ratio.
Glucose Optimization:
- Test glucose concentrations ranging from 5 mM (physiological) to 25 mM (high-glucose, simulating hyperglycemia).
- Maintain cultures for up to 72 hours with daily medium changes.
- Monitor cytokine secretion and lipid content to determine optimal glucose concentration that maintains both adipocyte and macrophage functionality.
Table 2: Research Reagent Solutions for 3D Adipose Tissue Models
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Scaffold Materials | Gellan Gum, Silk Fibroin, Collagen, Agarose | Provides 3D structure for cell growth and tissue organization | Gellan gum offers animal-free advantage; silk provides long-term stability [43] [15] |
| Cell Sources | Primary mature adipocytes, ASCs, MM6, THP-1 | Forms adipose tissue and immune components | Primary adipocytes most physiologically relevant; cell lines offer reproducibility [15] |
| Culture Media | Defined serum-free medium, DMEM/F12 basal medium | Supports cell viability and function without animal components | Eliminates batch variability; enables precise component control [15] |
| Differentiation Agents | Insulin, Dexamethasone, IBMX, TZD | Induces adipogenic differentiation from precursors | Standard cocktail enables reproducible adipogenesis [43] [44] |
| Inflammatory Activators | LPS, PMA, Free Fatty Acids | Induces pro-inflammatory state in macrophages | LPS+PMA combination effectively activates co-culture system [15] |
| Analysis Kits | Glycerol quantification, Leptin ELISA, PicoGreen DNA assay | Quantifies metabolic and inflammatory outputs | Enables functional assessment of lipolysis and endocrine function [43] |
Experimental Workflow for Glucose Optimization Studies
The following diagram illustrates the comprehensive workflow for establishing and analyzing the 3D adipocyte-macrophage co-culture system with glucose optimization:
Assessment of Lipogenic and Lipolytic Functions
Lipogenesis Assessment Protocols
Lipid Droplet Staining with Oil Red O:
- Carefully wash 3D constructs with phosphate-buffered saline (PBS).
- Fix with 4% paraformaldehyde for 1 hour at room temperature.
- Wash twice with PBS followed by one wash with 60% isopropanol.
- Incubate with freshly prepared Oil Red O working solution (0.5% in isopropanol) for 1 hour.
- Wash extensively with distilled water until runoff is clear.
- Image using brightfield or fluorescence microscopy.
- For quantification, elute stained Oil Red O with 100% isopropanol and measure absorbance at 520 nm [43].
Triglyceride Content Measurement:
- Homogenize 3D constructs in 1 mL of 5% NP-40 detergent solution.
- Heat samples to 95°C for 5 minutes, then cool to room temperature.
- Repeat heating and cooling cycle twice to ensure complete triglyceride extraction.
- Centrifuge at 10,000 × g for 5 minutes to remove insoluble material.
- Use commercial triglyceride quantification kit following manufacturer's instructions.
- Normalize triglyceride content to total DNA content using PicoGreen assay [43].
Gene Expression Analysis of Lipogenic Markers:
- Extract total RNA from 3D constructs using Trizol reagent.
- Purify RNA using RNeasy Mini Kit with DNase I treatment.
- Synthesize cDNA using reverse transcriptase with oligo(dT) primers.
- Perform quantitative PCR using SYBR Green and primers for key lipogenic genes:
- PPARγ: Master regulator of adipogenesis
- GLUT4: Insulin-responsive glucose transporter
- FABP4: Fatty acid binding protein
- Leptin: Adipokine regulating energy balance
- Normalize expression to housekeeping genes (GAPDH, β-actin) using the 2^(-ΔΔCt) method [43].
Lipolysis Assessment Protocols
Basal and Stimulated Lipolysis Measurements:
- Wash 3D constructs with serum-free medium.
- Pre-incubate for 2 hours in basal medium (containing 2% fatty acid-free BSA).
- For basal lipolysis: Incubate constructs in fresh basal medium for 4 hours.
- For stimulated lipolysis: Incubate constructs in medium containing 1 μM isoproterenol for 4 hours.
- Collect conditioned media and measure glycerol release using commercial glycerol quantification kit.
- Normalize glycerol release to total DNA content [48].
Free Fatty Acid (NEFA) Measurement:
- Use conditioned media from lipolysis experiments.
- Apply commercial NEFA assay kit following manufacturer's protocol.
- Include BSA-only blanks to account for background signal.
- Normalize NEFA values to total DNA content [48].
Temporal Dynamics of Lipolytic Pathways:
- Compare acute (2-4 hour) versus prolonged (24-48 hour) lipolytic responses.
- Utilize pathway-specific inhibitors to dissect contributions:
- Canonical pathway: ATGL inhibitor Atglistatin (10-50 μM)
- Lysosomal pathway: LAL inhibitor Lalistat2 (10-50 μM) or bafilomycin (10-100 nM)
- Assess differential activation of pathways under various glucose concentrations [48].
Table 3: Quantitative Assessment of Lipogenic and Lipolytic Functions
| Functional Assessment | Key Methodologies | Expected Outcomes | Glucose Dependence |
|---|---|---|---|
| Lipogenesis | Oil Red O staining, Triglyceride quantification, Lipogenic gene expression | Increased lipid droplet formation and TG storage under optimal glucose | Maximal at 15-25 mM glucose; reduced below 5 mM |
| Basal Lipolysis | Glycerol release, NEFA measurement in unstimulated state | Low basal lipolysis in insulin-containing medium | Enhanced at low glucose (<5 mM); suppressed at high glucose (>15 mM) |
| Stimulated Lipolysis | Glycerol/NEFA release after isoproterenol stimulation | Robust response to β-adrenergic stimulation | Optimal response at physiological glucose (5-10 mM) |
| Lipolytic Pathways | Pharmacological inhibition (Atglistatin, Lalistat2) | Canonical pathway dominates acute response; lysosomal pathway with prolonged fasting | Glucose availability regulates pathway preference |
| Inflammatory Crosstalk | Cytokine secretion (TNFα, IL-6, IL-1β), Gene expression | Pro-inflammatory state enhances lipolysis; anti-inflammatory promotes storage | High glucose promotes pro-inflammatory macrophage polarization |
Signaling Pathways in Glucose-Mediated Metabolic Regulation
The following diagram illustrates the key signaling pathways through which glucose availability influences macrophage-adipocyte crosstalk and metabolic functions:
Data Analysis and Interpretation
Quantitative Metrics for Glucose Optimization
When analyzing the effects of glucose concentration on the balance between lipogenesis and lipolysis, researchers should track multiple parameters simultaneously to establish the optimal glucose range:
Lipogenesis-Lipolysis Balance Index:
- Calculate the ratio of lipogenic to lipolytic activity under basal conditions
- Determine the dynamic response range (stimulated lipolysis divided by basal lipolysis)
- Assess the glucose concentration that maintains homeostatic balance (approximately 1:1 ratio under basal conditions)
Inflammatory-Metabolic Coupling Coefficient:
- Correlate inflammatory cytokine levels (TNFα, IL-6) with lipolytic rates
- Establish the glucose threshold at which inflammation begins to drive excessive lipolysis
- Identify the optimal glucose concentration that supports metabolic functions without inducing pathological inflammation
Troubleshooting Guide
Table 4: Troubleshooting Common Issues in 3D Adipose Tissue Cultures
| Problem | Potential Causes | Solutions | Preventive Measures |
|---|---|---|---|
| Poor Adipocyte Viability | Nutrient insufficiency, Hypoxia in core, Excessive inflammation | Optimize glucose concentration (5-15 mM), Increase medium exchange frequency, Reduce inflammatory stimulus concentration | Use porous scaffolds (gellan gum), Maintain appropriate cell density, Incorporate endothelial cells for vascularization [43] |
| Inadequate Lipogenic Response | Suboptimal differentiation, Insulin resistance in culture, Incorrect glucose concentration | Verify differentiation cocktail potency, Test insulin sensitivity, Titrate glucose (10-20 mM optimal for lipogenesis) | Use primary mature adipocytes rather than differentiated precursors, Include TZDs in differentiation protocol [43] [15] |
| Excessive Basal Lipolysis | Over-activation of macrophages, Nutrient starvation, Pro-inflammatory cytokine excess | Reduce macrophage:adipocyte ratio, Ensure adequate glucose supply, Add anti-inflammatory cytokines (IL-10) | Maintain physiological glucose (5 mM), Use controlled macrophage activation [15] [48] |
| Loss of 3D Structure | Scaffold degradation, Inadequate cross-linking, Cell-mediated contraction | Optimize gellan gum concentration, Adjust cation cross-linking, Use composite scaffolds | Test scaffold stability before cell culture, Use spinner flask culture for improved nutrient distribution [43] [15] |
The protocols outlined in this Application Note provide researchers with a comprehensive framework for establishing physiologically relevant 3D human adipocyte-macrophage co-cultures optimized for studying glucose-mediated regulation of lipogenesis and lipolysis. The animal-free system utilizing gellan gum hydrogels and defined serum-free medium offers superior reproducibility and translational relevance compared to traditional 2D cultures or animal-derived materials.
Optimal glucose concentration emerges as a critical parameter that balances adipocyte metabolic functions with macrophage inflammatory status, typically falling in the physiological range of 5-10 mM. This optimized system enables detailed investigation of the metabolic-inflammatory crosstalk that underlies adipose tissue dysfunction in obesity and related metabolic disorders, providing a valuable platform for drug discovery and metabolic research.
The selection of an appropriate hydrogel matrix is a critical determinant for the success of in vitro models, particularly for complex co-culture systems such as those involving functional adipose tissue-resident macrophages. The three-dimensional (3D) microenvironment dictates cellular phenotypes, signaling, and intercellular crosstalk, with profound implications for the physiological relevance of the research outcomes. Within the specific context of adipose tissue biology, the choice between natural polymers like fibrin and collagen, and advanced synthetic hydrogels, involves balancing biological recognition against tunability and reproducibility. Fibrin-based matrices demonstrate a pronounced ability to activate angiogenic and immunomodulatory signaling in adipose-derived stem cells (ASCs), promoting the secretion of vascular endothelial growth factor (VEGF) and other cytokines [49]. Collagen hydrogels, a widely used standard, provide a versatile scaffold that supports adipocyte differentiation and can direct the specialization of hematopoietic progenitor cells into unique, chemokine-secreting macrophage subsets [50] [51]. Emerging synthetic and animal-free options, such as polyethylene glycol (PEG)-based and gellan gum hydrogels, offer defined and reproducible mechanical environments, minimizing batch-to-batch variability and enabling precise dissection of cell-matrix interactions [15] [52]. This application note provides a structured comparison of these hydrogel systems and detailed protocols for their use in constructing robust 3D adipose tissue models for macrophage research.
Quantitative Matrix Comparison
The following tables summarize key characteristics and functional outcomes of the different hydrogel matrices to inform selection.
Table 1: Physicochemical and Mechanical Properties of Hydrogels
| Property | Fibrin | Collagen Type I | PEGylated Fibrin (P-Fibrin) | Gellan Gum (GG) |
|---|---|---|---|---|
| Typical Stiffness Range | Weak, degrades rapidly [53] | ~45 Pa (for HPC culture) [50] | Improved vs. fibrin [49] | Tunable with cation content [15] |
| Polymer Concentration | 3.2 mg/mL (common) [49] | 3-4 mg/mL (common) [49] [54] | 4 mg/mL (final) [49] | Varies (animal-free) [15] |
| Crosslinking Method | Enzymatic (Thrombin) [55] | pH/temperature (Self-assembly) [55] | Enzymatic + covalent (PEG) [49] | Ionic (Divalent cations) [15] |
| Key Advantage | High bioactivity, pro-angiogenic [49] | Gold standard, supports adipogenesis [51] | Enhanced stability & mechanical properties [49] [53] | Animal-free, high biocompatibility [15] |
| Key Limitation | Rapid degradation, shrinkage [53] | Batch-to-batch variability [53] | More complex fabrication [49] | Requires optimization for specific cell types [15] |
Table 2: Documented Biological Effects in Adipose and Immune Cell Cultures
| Hydrogel Type | Impact on Adipose/Stromal Cells | Impact on Macrophages/Immune Cells | Key Documented Secretory Profiles |
|---|---|---|---|
| Fibrin | Elongated morphology; Enhanced angiogenic potential [49] | Not specifically reported in results | Higher VEGF secretion at 7 days vs. collagen; Enhanced angiogenic/immunomodulatory cytokines [49] |
| Collagen | Supports visceral adipocyte differentiation [51] | Directs HSC differentiation to "3D-macrophages" expressing Cxcl2, Cd14, Tnf [54] [50] | Specific cluster expresses chemokines (CXCL2) for neutrophil recruitment [54] |
| PEGylated Fibrin | Significantly elongated morphology; High vWF expression [49] | Less pronounced polarization in 3D vs. 2D [52] | VEGF secretion similar to fibrin; distinct cytokine profile [49] |
| Gellan Gum (GG) | High viability and maintained lipid content in mature adipocytes [15] | Supports co-culture; allows LPS-induced inflammatory activation [15] | Production of IL-6, IL-1β, TNFα upon PMA+LPS stimulation [15] |
Experimental Protocols
Protocol: Establishing a 3D Adipocyte-Macrophage Co-Culture in Gellan Gum
This protocol outlines a method for creating a defined, animal-free co-culture system to study adipose tissue inflammation [15].
I. Materials
- Hydrogel Matrix: Gellan gum (GG) powder.
- Crosslinking Solution: Sterile solution of mono-/divalent cations (e.g., MgCl2, CaCl2).
- Cells: Human primary mature adipocytes (ACs) and human monocytic cell lines (MM6 or THP-1).
- Defined Culture Medium: Serum-free medium formulated in-house or commercially available.
- Inflammatory Inducers: Phorbol 12-myristate 13-acetate (PMA) and Lipopolysaccharide (LPS).
II. Procedure
- Hydrogel Preparation: Suspend GG powder in the defined culture medium at the desired concentration (e.g., 0.5-1.5% w/v). Gently heat and stir until the solution is clear and homogeneous. Allow it to cool to a handling temperature (37°C is suitable).
- Adipocyte Encapsulation: Gently mix a suspension of human primary mature adipocytes with the liquid GG solution. Avoid vigorous mixing to prevent cell damage.
- Gelation: Pipette the cell-hydrogel mixture into the desired cultureware (e.g., transwell inserts or multi-well plates). Add the crosslinking solution to the surface or submerge the constructs to initiate ionic gelation. Incubate for 15-30 minutes at 37°C to form stable hydrogels.
- Monocyte Seeding and Activation: After gelation, add defined culture medium to the culture vessel. Seed monocytic cells (MM6 or THP-1) on top of or around the adipocyte-loaded GG hydrogels. To induce an inflammatory state, treat the co-culture with a combination of PMA (e.g., 50 ng/mL) and LPS (e.g., 100 ng/mL).
- Culture Maintenance: Culture the co-cystem for up to 72 hours, refreshing the defined medium as required.
- Analysis: Assess outputs via:
- Viability: Live/dead staining.
- Inflammation: ELISA for cytokines (IL-6, IL-1β, TNFα) in the supernatant.
- Morphology: Histology (e.g., H&E, Oil Red O for lipids).
Protocol: Generating Specialized "3D-Macrophages" from HSCs in Collagen Hydrogels
This protocol describes how the 3D collagen microenvironment can steer hematopoietic stem cell (HSC) differentiation toward a specialized macrophage phenotype [54] [50].
I. Materials
- Hydrogel Matrix: Rat tail type I collagen solution (e.g., 3-5 mg/mL).
- Neutralization Solution: Sterile NaOH and PBS (10x concentration).
- Cells: Freshly isolated mouse bone marrow HSCs (Lineage-, c-Kit+).
- Culture Medium: IMDM supplemented with 10% FBS, SCF (50 ng/mL), TPO (20 ng/mL), and Flt-3 L (20 ng/mL).
II. Procedure
- Hydrogel Preparation: Keep all components on ice to prevent premature gelation. Mix the collagen solution with the cell suspension and 10x PBS. Neutralize the pH to ~7.4 using 1N NaOH.
- HSC Encapsulation: Quickly pipette the neutralized collagen-cell mixture into pre-chilled culture plates.
- Gelation: Transfer the plates to a 37°C, 5% CO2 incubator for 30 minutes to allow complete polymerization.
- Culture: After gelation, gently overlay the hydrogels with complete culture medium. Culture the constructs for 48 hours or as required.
- Cell Harvesting: To retrieve cells from the 3D matrix, carefully digest the hydrogels using type IV collagenase solution.
- Macrophage Isolation: Harvested cells can be incubated with a CD14-PE antibody. The CD14+ population ("3D-macrophages") can then be purified using flow cytometry-based cell sorting for downstream functional assays [54].
Protocol: Modulating ASC Phenotype in PEGylated Fibrin Hydrogels
This protocol leverages PEGylated fibrin to enhance the angiogenic behavior of adipose-derived stem cells (ASCs) [49].
I. Materials
- Hydrogel Components: Human fibrinogen, Succinimidyl glutarate-modified PEG (SG-PEG-SG), Bovine thrombin, CaCl2 solution.
- Cells: Human Adipose-derived Stem Cells (ASCs).
- Culture Medium: Basic growth medium (e.g., DMEM-low glucose with 10% FBS).
II. Procedure
- Solution Preparation: Dissolve fibrinogen in DPBS. In a separate tube, dissolve SG-PEG-SG in DPBS.
- PEGylation: Combine the fibrinogen and SG-PEG-SG solutions in a 1:1 volume ratio.
- Cell Seeding and Gelation: Mix the fibrinogen-PEG solution with an equal volume of ASC suspension. Initiate crosslinking by adding an equal volume of thrombin solution (e.g., 25 U/mL in 40 mM CaCl2). Quickly pipette the mixture into culture plates and incubate at 37°C, 5% CO2 for 10 minutes to form gels.
- Culture and Analysis: After gelation, add culture medium. To assess angiogenic potential:
- Morphology: Use phase-contrast microscopy to observe elongated, vessel-like structures.
- Phenotype: Analyze expression of von Willebrand factor (vWF) via immunostaining.
- Secretion: Quantify VEGF in conditioned media via ELISA after 7 days.
Visualizing Workflows and Signaling
The following diagrams illustrate the core experimental workflows and cell-matrix interactions described in this note.
Diagram 1: A flowchart comparing three primary experimental workflows for different research objectives.
Diagram 2: Key signaling pathways and functional outcomes driven by specific hydrogel matrices in immune-metabolic cultures.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Featured 3D Co-Culture Experiments
| Reagent/Material | Function/Description | Example Application in Protocols |
|---|---|---|
| Gellan Gum (GG) | Animal-free, bacteria-derived polysaccharide hydrogel; crosslinked with ions. | Primary matrix for animal-free adipocyte-macrophage co-culture [15]. |
| Rat Tail Collagen I | Natural ECM protein hydrogel; self-assembles upon neutralization. | Matrix for differentiating HSCs into specialized 3D-macrophages [54] [50]. |
| Fibrinogen & Thrombin | Natural polymer from blood clotting; forms hydrogel upon enzymatic reaction. | Base material for creating PEGylated fibrin gels for ASC culture [49]. |
| SG-PEG-SG | Amine-reactive polyethylene glycol; covalently modifies fibrinogen. | Used to create PEGylated fibrin for enhanced mechanical stability [49]. |
| CD14-PE Antibody | Fluorescently-labeled antibody against macrophage surface marker CD14. | Isolation of "3D-macrophages" from collagen hydrogels via FACS [54]. |
| PMA & LPS | Potent inducers of macrophage activation and pro-inflammatory polarization. | Stimulating inflammation in adipocyte-macrophage co-cultures [15]. |
| Type IV Collagenase | Enzyme for digesting collagen-based hydrogels to recover encapsulated cells. | Harvesting cells from 3D collagen matrices after culture [54]. |
The study of adipose tissue-resident macrophages is pivotal for understanding immunometabolic diseases such as obesity, diabetes, and insulin resistance. These specialized macrophages, which demonstrate distinct genic and phenotypic characteristics compared to their bone marrow-derived counterparts, play critical roles in maintaining adipose tissue homeostasis, regulating inflammation, and coordinating tissue remodeling [11] [16]. Three-dimensional (3D) culture systems have emerged as essential tools in this field, successfully recapitulating the in-vivo microenvironment and generating functionally active resident macrophages that faithfully mirror their in-situ counterparts [11].
While foundational research has predominantly utilized 96-well plate formats, the transition to high-throughput screening (HTS) compatible systems presents significant technical and methodological challenges. This application note details these scalability challenges and provides validated protocols and solutions to enable robust, high-throughput screening for drug discovery applications targeting adipose tissue immunobiology.
Scalability Analysis of 3D Macrophage Culture Platforms
The migration from low-throughput to HTS-compatible formats necessitates careful evaluation of different 3D culture technologies. The table below summarizes the key advantages and limitations of common platforms regarding their HTS suitability.
Table 1: HTS Suitability Analysis of 3D Macrophage Culture Platforms
| 3D Culture Platform | Key Advantages for HTS | Scalability Challenges | Recommended Screening Format |
|---|---|---|---|
| Ultra-Low Attachment (ULA) Plates [11] [35] | - Simple, protocol-friendly- Self-aggregating spheroids- Amenable to automation- High reproducibility | - Spheroid size uniformity- Hypoxic cores in large spheroids- Medium evaporation in edge wells | 384-well for spheroid formation & assay |
| Hanging Drop Plates [35] | - Excellent spheroid uniformity- Minimal surface contact- Low material consumption | - Requires transfer for assays- Liquid handling complexity- Not ideal for long-term culture | 96- or 384-well for formation; requires transfer |
| Magnetic Bioprinting [56] | - Prevents organoid floating- Minimizes handling loss- Positional control | - Specialized equipment needed- Additional reagent (nanoshuttle) | 96- to 384-well with magnetic holders |
| Hydrogel Embedding [15] [31] | - Superior microenvironment- Tunable mechanical properties- Enhanced maturation | - Varying polymerization times- Drug diffusion barriers- Lot-to-lot variability | 96-well for complex co-cultures |
Quantitative HTS Transition Metrics
Successfully transitioning macrophage assays to HTS formats requires optimization of critical parameters that directly impact data quality, operational efficiency, and reagent consumption.
Table 2: Key Parameter Shifts in HTS Transition
| Parameter | 96-Well Format | 384-Well Format | 1536-Well Format |
|---|---|---|---|
| Working Volume | 50-200 µL | 10-50 µL | 5-10 µL |
| Cell Seeding Density | 10^5 cells/well [11] | 2.5 × 10^4 cells/well | 5-8 × 10^3 cells/well |
| Spheroid Diameter | 100-400 µm [31] | 80-150 µm | 50-80 µm |
| M-CSF Concentration | 10 ng/mL [11] | 10 ng/mL | 10-15 ng/mL* |
| Assay Readout Compatibility | Standard plate readers, microscopy | High-content imaging, automated microscopy | Specialized HCS systems |
Note: Potential concentration increase needed to compensate for higher surface-area-to-volume ratio.
Core Protocol: Scalable 3D Adipose Tissue-Resident Macrophage Generation
This protocol adapts the established 3D culture method for generating functional adipose tissue-resident macrophages [11] with specific modifications to enhance HTS compatibility.
Materials and Reagents
Table 3: Essential Research Reagent Solutions
| Reagent/Category | Specific Example | Function in Protocol |
|---|---|---|
| Source Cells | Murine adipose stromal vascular fraction (SVF) [11] | Provides progenitor population for resident macrophages |
| Basal Medium | RPMI with Glutamax [11] | Nutrient support for cell growth and maintenance |
| Critical Supplement | Macrophage Colony-Stimulating Factor (M-CSF; 10 ng/mL) [11] | Drives macrophage differentiation and survival |
| Serum | Heat-Inactivated Newborn Calf Serum (10%) [11] | Provides essential growth factors and adhesion proteins |
| 3D Culture Vessel | Ultra-low attachment (ULA) round-bottom plates [11] [35] | Promotes spontaneous spheroid formation via minimized adhesion |
| Antibiotics | Penicillin/Streptomycin/Amphotericin B cocktail (1%) [11] | Prevents microbial contamination in long-term cultures |
| Dissociation Agents | Collagenase NB4 (1.7 U/mL) + Dispase I (2.5 U/mL) [11] | Liberates macrophages from spheroids for analysis |
Step-by-Step Workflow for HTS Implementation
Adipose Stromal Vascular Fraction (SVF) Isolation
- Excise subcutaneous adipose tissue from C57Bl/6J mice (6-8 weeks old) and remove lymph nodes.
- Mechanically dissociate tissue followed by enzymatic digestion with collagenase NB4 (1.7 U/mL) at 37°C for 30 minutes with agitation.
- Filter through 100-70μm strainers, centrifuge (400 × g, 10 min), and lyse red blood cells using NH₄Cl-based lysing buffer.
- Resuspend SVF pellet in complete medium: RPMI + Glutamax, 10% hiNBCS, 1% antibiotics, and 10 ng/mL M-CSF [11].
Scalable 3D Spheroid Formation
- 96-well format: Seed SVF cells at 10^5 cells/well in 100 μL complete medium into ULA round-bottom plates. Centrifuge briefly (300 × g, 5 min) to aggregate cells at well bottom [11].
- 384-well format: Seed SVF cells at 2.5 × 10^4 cells/well in 25-30 μL complete medium using automated liquid handlers. Centrifuge as above.
- Incubate at 37°C with 5% CO₂. Spheroids typically form within 4 days.
Macrophage Differentiation and Harvest
- Around day 7, macrophages begin to migrate from spheroids and adhere to the plate. Culture typically continues until day 13-21 for full maturation [11].
- For analysis requiring single cells, harvest spheroids and dissociate using collagenase NB4 (1.7 U/mL) + dispase I (2.5 U/mL) at 37°C for 40 minutes with periodic mechanical pipetting [11].
HTS-Compatible Functional Assays
- Phagocytosis: Use pH-sensitive fluorescent beads (e.g., pHrodo) in scaled-down volumes. Measure fluorescence increase upon phagolysosomal internalization.
- Polarization: Stimulate with IL-4 (10 ng/mL) or IFN-γ (50 ng/mL) for 4-24 hours in HTS-compatible plates. Quantify marker expression via high-content imaging or multiplexed cytokine secretion assays [11].
- Metabolic Analysis: Utilize commercial kits adapted to 384-well format to measure glycolytic flux and mitochondrial respiration (Seahorse XFp Analyzer).
Diagram: HTS-Compatible Workflow for 3D Adipose Tissue Macrophage Generation. This diagram outlines the scalable protocol from cell isolation to high-content analysis.
Technical Hurdles and Optimization Strategies
Spheroid Uniformity and Assay Reproducibility
The generation of uniformly sized spheroids is arguably the most critical factor for reproducible HTS outcomes. In ULA plates, spheroid size is primarily controlled by initial seeding density. The transition to higher-density formats requires empirical optimization to maintain the optimal 100-400 μm diameter range, which ensures adequate nutrient diffusion while preventing central hypoxia [31]. Automated liquid handlers with regular nozzle calibration are essential to minimize well-to-well variation in cell number. Incorporating vibration-dampening platforms during the critical centrifugation step further enhances spheroid uniformity across the plate.
Microenvironment Control in Miniaturized Formats
Reduced well volumes in 384- and 1536-well formats exacerbate challenges with evaporation, particularly in edge wells, and nutrient gradient formation. These issues can be mitigated by:
- Using plate seals designed for gas exchange while limiting evaporation.
- Employing environmental chambers in automated incubators to maintain uniform humidity.
- Implementing microplate perfusion systems [31] or semi-automated medium exchange protocols to maintain nutrient and cytokine homeostasis.
- Adding oxygen-sensitive probes to monitor hypoxia in real-time, allowing for culture intervention before artifactual signaling occurs.
Readout Adaptation and Validation
Transitioning established endpoint assays requires rigorous re-validation. High-content imaging systems must be configured with appropriate objectives and z-stacking capabilities to accurately capture 3D structures. Automated image analysis pipelines should be developed to quantify macrophage migration distance from spheroids, a key indicator of functional maturity in this model [11]. For phagocytosis assays, the increased surface-area-to-volume ratio in HTS formats can alter reagent kinetics, necessitating optimization of probe concentration and incubation time.
The migration of 3D adipose tissue-resident macrophage cultures from 96-well to HTS formats, while challenging, is an essential step in leveraging these physiologically relevant models for systematic drug discovery. Success hinges on meticulous optimization of spheroid formation parameters, careful management of the microscale microenvironment, and rigorous adaptation of functional assay readouts. The protocols and solutions detailed herein provide a roadmap for overcoming key scalability challenges, enabling researchers to harness the full potential of these complex immune cell models in high-throughput campaigns aimed at combating metabolic disease. Future advances in automated perfusion systems [31] and sensor-integrated microplates will further dissolve the technical barriers between physiological relevance and screening throughput.
Within the field of immunometabolism and tissue engineering, adipose tissue-resident macrophages (ATMs) play pivotal roles in maintaining tissue homeostasis, regulating inflammation, and supporting adipocyte function [11] [9]. A significant challenge in studying these cells has been the preservation of their inherent properties during extended in vitro culture, as traditional two-dimensional (2D) culture systems often fail to recapitulate the native tissue microenvironment, leading to phenotypic drift and loss of functional characteristics [11] [16]. This Application Note details established and novel methodologies, with a focus on three-dimensional (3D) culture systems, that enable researchers to maintain phenotypic and functional stability of adipose tissue-resident macrophages during long-term culture, thereby providing more physiologically relevant models for investigating adipose tissue biology, obesity, metabolic disorders, and for screening potential therapeutic compounds [11] [15].
Key Challenges in Maintaining ATM Phenotype
The persistence of adipose tissue-resident macrophages in culture is highly dependent on signals from their cellular niche. When removed from this environment and cultured using conventional methods, they often undergo rapid functional alteration and lose their tissue-specific identity [11] [8]. The table below summarizes the primary challenges and their implications for in vitro research.
Table 1: Key Challenges in Long-Term Culture of Adipose Tissue-Resident Macrophages
| Challenge | Impact on Phenotypic Stability | Consequence for Research |
|---|---|---|
| Loss of Tissue Microenvironment [11] | Alters transcriptomic and metabolic profiles; reduces expression of resident macrophage markers (e.g., Timd4, Lyve1, CD206). | Diminished relevance to in vivo physiology. |
| Standard 2D Monolayer Culture [11] | Promotes dedifferentiation and disrupts native cell-cell and cell-matrix interactions. | Loss of specialized functions such as homeostatic regulation. |
| Prolonged Culture Duration [11] | Gradual drift from resident characteristics towards a generic, bone marrow-derived macrophage-like state. | Reduced reproducibility and accuracy in long-term studies. |
| Lack of Physiological Co-culture Systems [15] [8] | Absence of crosstalk with adipocytes and other stromal cells eliminates key regulatory signals. | Inability to model intercellular communication in adipose tissue. |
Established 3D Culture Protocol for Functional ATMs
This protocol, adapted from recent research, describes a robust method for generating and maintaining functional adipose tissue-resident macrophages from the stromal vascular fraction (SVF) of murine subcutaneous adipose tissue using a 3D spheroid system [11] [16].
Materials and Reagents
Table 2: Essential Research Reagents for 3D ATM Culture
| Reagent/Catalog Number | Function in Protocol |
|---|---|
| Ultra-low adherence plates (e.g., COSTAR) | Enables spontaneous spheroid formation by preventing cell attachment. |
| Macrophage Colony-Stimulating Factor (M-CSF) (e.g., PeproTech, 10 ng/ml) | Key cytokine for macrophage survival, proliferation, and differentiation. |
| Collagenase NB4 (e.g., Sigma-Aldrich) | Enzymatically digests adipose tissue to isolate the stromal vascular fraction. |
| Dispase I (e.g., Sigma-Aldrich) | Used in tandem with collagenase for gentle spheroid dissociation. |
| Roswell Park Memorial Institute (RPMI) 1640 Medium | Base culture medium. |
| Heat-Inactivated Newborn Calf Serum (hiNBCS) (10%) | Provides essential nutrients and growth factors for cell growth. |
Step-by-Step Methodology
Isolation of Stromal Vascular Fraction (SVF):
- Harvest subcutaneous adipose tissue from C57Bl/6J mice (6-8 weeks old).
- Mechanically mince the tissue and digest using Collagenase NB4 (1.7 U/mL) in α-MEM medium at 37°C for 30 minutes with agitation.
- Filter the digested tissue through a cell strainer to remove debris and centrifugate.
- Lyse red blood cells using an ammonium chloride solution, wash, and resuspend the SVF pellet in complete medium [11] [16].
3D Spheroid Formation and Culture:
- Seed the isolated SVF cells onto ultra-low adherence 96-well round-bottom plates at a density of 10^5 cells/well in RPMI-1640 medium supplemented with GlutaMAX, 10% hiNBCS, 1% penicillin/streptomycin, and 10 ng/mL M-CSF.
- Centrifuge the plates briefly to aggregate cells at the bottom of wells and incubate at 37°C with 5% CO₂.
- Within 4 days, cells will spontaneously aggregate to form a single spheroid per well [11].
Macrophage Generation and Maintenance:
- Continue culture without disturbance. Around day 7, macrophages will begin to migrate out of the spheroid and adhere to the plate surface.
- Culture can be maintained for several weeks. For subculturing or analysis, spheroids can be collected and dissociated using a combination of Collagenase NB4 (1.7 U/mL) and Dispase I (2.5 U/mL) at 37°C for 40 minutes, followed by gentle mechanical pipetting [11] [16].
Phenotypic Validation
Cells derived from this 3D system should be validated to ensure they recapitulate the key features of in vivo resident ATMs. Key assessments include:
- Flow Cytometry: Confirm expression of resident macrophage markers such as CD206 and absence of high CCR2 expression [11] [16].
- Functional Assays: Demonstrate characteristic metabolic activity and polarization capacity in response to stimuli like IL-4 and IFN-γ, while maintaining strong phagocytic ability [11].
- Transcriptomic Analysis: Single-cell RNA sequencing can be used to verify that the cultured cells mirror the transcriptional profile of in vivo resident ATMs [11].
Advanced Co-culture System for Enhanced Physiological Relevance
To further mimic the adipose tissue niche and study macrophage-stromal cell interactions, a defined, animal-free 3D co-culture system can be implemented [15].
Workflow Diagram
Key System Components and Steps
Adipocyte Compartment Setup:
- Encapsulate human primary mature adipocytes in Gellan Gum (GG), an animal-free hydrogel, to provide a supportive 3D matrix.
- Culture the constructs in a defined, serum-free medium to eliminate batch-to-batch variability and improve reproducibility [15].
Macrophage Compartment Setup:
- Differentiate human monocytic cell lines (e.g., MM6 or THP-1) into macrophages using Phorbol 12-myristate 13-acetate (PMA).
- Activate the macrophages using a combination of PMA and Lipopolysaccharide (LPS) to induce a pro-inflammatory state, modeling adipose tissue inflammation [15].
Co-culture and Analysis:
- Combine the two compartments to establish the 3D co-culture.
- This system maintains high adipocyte viability and intracellular lipid content for at least 72 hours while sustaining an inflammatory response, making it suitable for short-term pharmacological testing of anti-inflammatory compounds [15].
Troubleshooting and Technical Notes
- Minimizing Phenotypic Drift: The 3D spheroid culture method has been shown to preserve transcriptomic and metabolic features of resident ATMs far more effectively than traditional 2D bone marrow-derived macrophage cultures [11]. For studies exceeding 21 days, periodic validation of key markers is recommended.
- Addressing Buoyancy in 3D Cultures: A common issue in 3D adipose cultures is the buoyancy of lipid-laden adipocytes, which disrupts the culture. To counter this, consider using magnetic bioprinting technology with a magnetic holder to restrain organoids, preventing flotation and minimizing handling losses [56].
- Manipulating Macrophage Presence: To investigate the specific role of macrophages in regulating adipocyte behavior (e.g., dedifferentiation), macrophage depletion can be performed within complex culture systems like adipose tissue explants using agents such as Plexxicon 5622 or clodronate liposomes [8].
The protocols detailed herein provide validated strategies for overcoming the historical challenge of phenotypic instability in cultured adipose tissue-resident macrophages. The core 3D spheroid system enables the generation of macrophages that faithfully mirror their in vivo counterparts, while the advanced co-culture model offers a powerful tool for investigating cell-cell communication in a pathophysiologically relevant context. By adopting these methods, researchers can significantly enhance the reliability and translational potential of their studies in immunometabolism and drug development.
Validation and Comparative Analysis: Ensuring Physiological Relevance
The adoption of three-dimensional (3D) culture models for generating functional adipose tissue-resident macrophages represents a significant advancement in recreating physiologically relevant microenvironments in vitro. However, the true utility of these sophisticated models depends entirely on rigorous validation demonstrating that the cultured cells accurately mirror their in vivo counterparts. Single-cell RNA sequencing (scRNA-seq) has emerged as a powerful technology for this validation, enabling unprecedented resolution for comparing cellular identities, heterogeneous subpopulations, and transcriptional states between in vitro systems and living organisms [57] [58].
Within adipose tissue biology, scRNA-seq profiling of murine models provides a crucial opportunity to increase the translatability of findings into clinical applications and to select the most appropriate models for testing novel therapeutics [57]. This application note details comprehensive protocols and analytical frameworks for employing scRNA-seq as a validation tool, specifically framed within the context of 3D cultured adipose tissue-resident macrophage research. By establishing robust transcriptomic validation pipelines, researchers can bridge the critical gap between in vitro observations and in vivo biology, thereby enhancing the reliability of preclinical research in drug development.
Key Analytical Workflow for Transcriptomic Validation
The validation process involves a coordinated series of experimental and computational steps designed to systematically compare in vitro and in vivo transcriptional profiles. The following workflow outlines the core components of this analytical pipeline, with detailed methodologies provided in subsequent sections.
Core Experimental Protocol: Sample Preparation and Sequencing
Generation of 3D Cultured Adipose Tissue-Resident Macrophages
The production of functional mature macrophages from adipose tissue using 3D culture systems enables the generation of cells that closely mirror in vivo resident macrophages without the need for cell sorting, which can alter intrinsic cellular properties [11] [16].
Materials:
- Murine subcutaneous adipose tissue
- Ultra-low adherence 96-well round bottom plates
- RPMI medium supplemented with Glutamax
- Heat-inactivated newborn calf serum (10%)
- Antibiotic/antimycotic cocktail (1%)
- Macrophage colony-stimulating factor (M-CSF; 10 ng/mL)
Methodology:
- Isolate the stromal vascular fraction (SVF) from subcutaneous adipose tissues through mechanical dissociation and enzymatic digestion with collagenase (NB4) for 30 minutes at 37°C [11] [16].
- Following filtration and centrifugation, isolate stromal vascular cells and perform red blood cell lysis.
- Seed SVF cells on ultra-low adherence plates at a density of 10^5 cells/well in supplemented RPMI medium containing M-CSF.
- Centrifuge plates briefly and incubate at 37°C with 5% CO₂.
- Monitor for spheroid formation (typically occurring after 4 days of culture).
- Allow macrophages to spread out of spheroids and adhere to culture plates (beginning approximately on day 7 of culture).
- Harvest cells for scRNA-seq analysis between days 13-21 of culture.
Preparation of High-Quality Single-Cell/Nucleus Suspensions for scRNA-seq
Obtaining high-quality transcriptional profiles from adipose tissue presents unique challenges due to the fragility of adipocytes and the high lipid content of the tissue. Both single-cell and single-nucleus RNA sequencing approaches have specific advantages depending on the research objectives [58].
Single-Cell RNA Sequencing Protocol:
- Process fresh adipose tissue specimens within 1 hour of collection.
- Wash tissue three times in PBS and mince thoroughly with scalpels.
- Digest minced tissue in RPMI supplemented with collagenase I (5 mg/mL) and DNase I (100 µg/mL) for 2.5 hours at 37°C [59].
- Filter digested tissue through a 100-μm cell strainer, wash with PBS, and centrifuge at 800 g.
- Resuspend cell pellet and remove dead cells/debris by sorting 7-AAD-negative population using flow cytometry.
- Resuspend viable cells in appropriate buffer for scRNA-seq platform.
Single-Nucleus RNA Sequencing Protocol (Optimized for Adipose Tissue):
- Homogenize adipose tissue in nucleus isolation buffer supplemented with vanadyl ribonucleoside complex (VRC) to inhibit RNase activity and preserve RNA integrity [58].
- Filter homogenate through cell strainers and centrifuge to isolate nuclei.
- Resuspend nuclei in storage buffer and assess quality using microscopy.
- Count nuclei and adjust concentration for single-nucleus RNA sequencing platform requirements.
Table 1: Critical Reagents for scRNA-seq Sample Preparation
| Research Reagent | Function/Application | Key Considerations |
|---|---|---|
| Collagenase I | Tissue dissociation for cell suspension | Concentration and incubation time must be optimized for different adipose depots [59] |
| Vanadyl Ribonucleoside Complex (VRC) | RNase inhibitor for nuclear RNA preservation | Essential for maintaining RNA quality in adipose tissues prone to degradation [58] |
| Macrophage Colony-Stimulating Factor (M-CSF) | Differentiation and maintenance of macrophages in 3D culture | Critical for generating functional adipose tissue-resident macrophages [11] [16] |
| Ultra-Low Adherence Plates | Facilitate spheroid formation in 3D culture | Enable proper macrophage differentiation and function [11] |
| 7-AAD Viability Dye | Identification and removal of dead cells | Improves scRNA-seq data quality by reducing background noise [59] |
Computational Analysis Framework for Comparative Transcriptomics
Data Processing and Quality Control
The computational analysis of scRNA-seq data requires careful quality control to ensure meaningful biological interpretations. The following steps outline a standardized processing pipeline:
Raw Data Processing:
- Trim raw reads to remove adapter sequences and low-quality bases.
- Align reads to the appropriate reference genome (e.g., GRCh38 for human, GRCm38 for mouse) using STARsolo or similar aligners [59].
- Generate gene expression matrices using cell barcodes and unique molecular identifiers.
Quality Control Metrics:
- Filter out cells with high mitochondrial transcript percentage (>20% suggests compromised cell viability) [59].
- Remove cells with an unusually low or high number of detected genes (potential doublets or empty droplets).
- Exclude cells with low library complexity.
Data Integration:
- Normalize data using variance-stabilizing transformation methods.
- Integrate multiple datasets using harmony, Seurat's CCA, or similar methods to enable comparative analysis.
- Address batch effects between in vitro and in vivo samples to prevent technical artifacts.
Cell Type Identification and Comparative Analysis
The identification of cell populations and their transcriptional comparison forms the core of the validation process:
Dimension Reduction and Clustering:
- Identify highly variable genes for principal component analysis.
- Perform graph-based clustering on significant principal components.
- Visualize clusters using UMAP or t-SNE projections.
Cell Type Annotation:
- Identify cluster-specific marker genes using differential expression testing.
- Annotate cell types based on canonical marker genes and reference datasets.
- Validate cell type identities through expert curation and literature concordance [59].
Comparative Analysis Between in Vitro and in Vivo Cells:
Table 2: Key Marker Genes for Validating Adipose Tissue-Resident Macrophages
| Gene Marker | In Vivo Expression Pattern | Expected Expression in Validated 3D Cultures | Functional Significance |
|---|---|---|---|
| TIMD4 | Resident macrophage marker [16] | Maintained expression | Distinguishes tissue-resident from bone marrow-derived macrophages |
| FOLR2 | Resident macrophage marker [16] | Maintained expression | Identifies embryonic-derived residential populations |
| LYVE1 | Resident macrophage marker [16] | Maintained expression | Associated with homeostatic functions |
| CD206 | Adipose resident macrophage marker [16] | Maintained expression | Marker of alternatively activated macrophages |
| CCR2 | Bone marrow-derived macrophage marker [16] | Low/absent expression | Indicates monocyte-derived macrophage contamination |
Functional Validation of Transcriptomic Findings
Transcriptomic data should be functionally validated to confirm the biological relevance of identified markers and pathways. A multi-tiered validation approach provides the most robust confirmation of 3D culture fidelity.
In Vitro Functional Assays
Phagocytosis Assay:
- Harvest 3D-cultured adipose tissue macrophages and seed on adherent culture plates.
- Incubate cells with fluorescently-labeled particles (e.g., pHrodo E. coli bioparticles, zymosan, or latex beads).
- Measure phagocytic activity using flow cytometry or fluorescence microscopy.
- Compare phagocytic capacity with bone marrow-derived macrophages and, if possible, freshly isolated adipose tissue macrophages [16].
Metabolic and Polarization Assays:
- Treat 3D-cultured macrophages with polarizing stimuli (IL-4, 10 ng/mL; IFN-γ, 50 ng/mL).
- Assess gene expression changes at 4 hours (transcriptional) and 24 hours (protein) post-stimulation.
- Evaluate metabolic activity using Seahorse extracellular flux analyzer or similar platforms.
- Compare polarization responses with control macrophages [16].
Target Validation Pipeline
For identified differentially expressed genes, implement a systematic validation pipeline to confirm functional importance:
Gene Prioritization Using GOT-IT Framework:
- Target-Disease Linkage: Focus on markers specific to the cell type of interest (e.g., tip endothelial cells, residential macrophages) that show conserved expression across species and models [60].
- Target-Related Safety: Exclude markers with genetic links to unrelated diseases or potential safety concerns.
- Strategic Considerations: Prioritize novel targets with minimal previous characterization in the specific biological context.
- Technical Feasibility: Consider availability of perturbation tools, protein localization, and cell type specificity [60].
Functional Assessment:
- Perform knockdown experiments using multiple non-overlapping siRNAs to ensure target specificity.
- Assess phenotypic changes using migration assays (wound healing), proliferation assays (³H-thymidine incorporation), and specialized functional assays (sprouting angiogenesis for endothelial cells) [60].
- Confirm findings at both RNA and protein levels to validate transcriptional observations.
Applications in Drug Development and Disease Modeling
The integration of scRNA-seq validation with 3D culture systems has profound implications for pharmaceutical research and development, particularly in enhancing the translational potential of preclinical findings.
Enhancing Translation Between Models and Human Disease
In inflammatory bowel disease (IBD) research, scRNA-seq has revealed both similarities and differences between human disease and experimental mouse models, enabling researchers to select the most appropriate models for testing specific therapeutic targets [57]. Similarly, in adipose tissue biology, understanding the transcriptional alignment between 3D cultures and in vivo tissues allows for more predictive screening of therapeutic candidates.
Identifying and Addressing in vitro-in vivo Disconnects
Transcriptomic comparison can reveal systematic discrepancies between in vitro and in vivo systems. Statistical frameworks, such as fractional polynomial modeling combined with biclustering algorithms, can identify genes with discordant expression patterns between model systems [61]. These "disconnect signatures" highlight biological pathways that may not be properly recapitulated in vitro and require additional model refinement.
Table 3: Troubleshooting Common scRNA-seq Validation Challenges
| Challenge | Potential Causes | Solutions |
|---|---|---|
| Poor RNA Quality in Adipose Samples | High intrinsic RNase activity [58] | Implement VRC during nucleus isolation; minimize processing time |
| Low Correlation Between in vitro and in vivo Profiles | Inadequate culture conditions; improper cell type matching | Optimize 3D culture duration; ensure appropriate reference population selection |
| Failure to Detect Rare Cell Populations | Insufficient cell sequencing depth; over-clustering | Increase cell numbers; utilize targeted enrichment strategies |
| Technical Batch Effects | Different processing protocols; platform variations | Implement batch correction algorithms; include technical controls |
Single-cell RNA sequencing provides an unparalleled toolkit for validating the transcriptional fidelity of 3D cultured adipose tissue-resident macrophages against their in vivo counterparts. Through rigorous experimental protocols, computational analysis, and functional validation, researchers can establish robust models that faithfully recapitulate key aspects of native tissue biology. This validation framework not only enhances confidence in 3D culture systems but also strengthens the translational potential of findings from these models to clinical applications. As the field advances, continued refinement of these approaches will further bridge the gap between in vitro modeling and in vivo biology, accelerating the development of novel therapeutics for metabolic diseases, cancer, and inflammatory disorders.
Within adipose tissue (AT), resident macrophages are pivotal players in upholding tissue homeostasis under both physiological and pathological conditions [16] [11]. Studying these cells in vitro has posed significant challenges, as traditional isolation and culture methods often alter their inherent properties [16]. The advent of three-dimensional (3D) culture systems has revolutionized this field by enabling the generation of functional mature macrophages that mirror the phenotypic and functional traits of their in-vivo counterparts [16] [44]. This application note details standardized protocols for establishing 3D cultures of adipose tissue-resident macrophages and conducting key functional assays—phagocytosis, metabolic profiling, and polarization capacity—which are essential for advancing research in immunometabolism and drug development.
Generation of Adipose Tissue Macrophages via 3D Culture
This protocol describes the generation of functional resident macrophages from the stromal vascular fraction (SVF) of murine subcutaneous adipose tissue using a scaffold-free, spheroid-based 3D culture system [16] [11].
Materials and Reagents
- Animals: 6- to 8-week-old male C57Bl/6J mice [16] [11].
- Dissection and Digestion:
- 3D Culture Medium:
- Equipment:
Step-by-Step Protocol
- Isolation of Stromal Vascular Fraction (SVF): Harvest subcutaneous adipose tissue, remove lymph nodes, and mechanically dissociate. Digest the tissue with collagenase (e.g., NB4, 1.7 U/mL) at 37°C for 30 minutes. Filter the digest, centrifuge, and lyse red blood cells. Resuspend the final SVF pellet in culture medium and perform a cell count [16] [11].
- Spheroid Seeding and Culture: Seed SVF cells at a density of 10⁵ cells per well into ULA 96-well plates in 3D Culture Medium. Centrifuge the plates briefly to encourage cell aggregation and incubate at 37°C with 5% CO₂ [16] [11].
- Spheroid Formation and Macrophage Generation: After 4 days of culture, cells will spontaneously aggregate to form spheroids. Starting around day 7, macrophages will begin to migrate out of the spheroids and adhere to the culture plate. Mature, functional macrophages are typically available for experimentation from day 13 onwards [16] [11].
Core Functional Assays for Adipose Tissue Macrophages
Table of Key Functional Assays and Readouts
Table 1: Summary of core functional assays for characterizing adipose tissue macrophages.
| Functional Assay | Key Readout | Technique/Equipment | Significance |
|---|---|---|---|
| Phagocytosis | Uptake of fluorescent particles (e.g., zymosan, beads); similar capacity observed between 3D AT-macrophages and BM-derived macrophages [16]. | Flow cytometry, fluorescence microscopy | Assesses capacity for cellular debris clearance and efferocytosis [62]. |
| Metabolic Activity | Extracellular Acidification Rate (ECAR), Oxygen Consumption Rate (OCR); distinct profiles for 3D AT-macrophages vs. BM-derived macrophages [16] [63]. | Seahorse Analyzer (e.g., Agilent) | Reveals metabolic phenotype (glycolysis vs. oxidative phosphorylation) [63]. |
| Polarization Capacity | Gene and protein expression of polarization markers (e.g., CD11c, CD206, CD301); specific response to IL-4 and IFN-γ in 3D AT-macrophages [16] [8] [62]. | qPCR, Flow cytometry, Cytokine array | Determines plasticity and functional response to inflammatory or resolving stimuli [16]. |
| Metabolic Profiling | Expression of nutrient transporters and metabolic enzymes (e.g., GLUT1, ACC1, CPT1A) [63]. | Spectral flow cytometry | Provides high-dimensional, single-cell data on metabolic states in complex populations [63]. |
Detailed Experimental Protocols
Phagocytosis Assay
- Principle: This assay quantifies the ability of macrophages to engulf fluorescently labeled particles, mimicking their fundamental role in clearing cellular debris and pathogens [62].
- Procedure:
- Harvest 3D-cultured AT-macrophages and seed onto adherent plates overnight.
- Incubate cells with pHrodo-labeled zymosan bioparticles (or similar fluorescent particles) according to the manufacturer's instructions for 1-2 hours.
- Terminate phagocytosis by placing cells on ice and extensively washing with cold PBS to remove non-internalized particles.
- Analyze phagocytic activity using flow cytometry to measure the fluorescence intensity of cell populations, or by fluorescence microscopy to visualize particle uptake at a single-cell level.
Metabolic Activity Profiling
- Principle: Macrophage function is critically dependent on cellular metabolism. This assay simultaneously measures the two major metabolic pathways—glycolysis (ECAR) and mitochondrial respiration (OCR)—in real time [63].
- Procedure:
- Seed harvested macrophages onto Seahorse assay plates and allow them to adhere.
- Equilibrate cells in Seahorse XF base medium in a non-CO₂ incubator for 1 hour.
- Load the cartridge with metabolic modulators (e.g., glucose, oligomycin, FCCP, rotenone/antimycin A) for a Mitochondrial Stress Test, or glucose, oligomycin, and 2-DG for a Glycolysis Stress Test.
- Run the assay on the Seahorse Analyzer. The instrument will automatically measure ECAR and OCR after each injection of modulators.
- Analyze the data using Wave software to calculate key parameters like basal and maximal respiration, glycolytic capacity, and glycolytic reserve.
Polarization and Stimulation
- Principle: Macrophages exhibit remarkable plasticity. This assay evaluates their capacity to adopt different functional phenotypes in response to polarizing cytokines [16].
- Procedure:
- Seed harvested macrophages in adherent culture plates.
- Treat the cells with one of the following for specified durations:
- Following stimulation, harvest cells for RNA extraction and subsequent qPCR analysis of polarization markers (e.g., Cd11c, Nos2 for M1; Arg1, Mrc1 for M2), or collect supernatant for cytokine detection via ELISA/ multiplex arrays. Cells can also be analyzed by flow cytometry for surface marker expression (e.g., CD11c, CD206) [16] [8] [62].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key research reagent solutions for the culture and functional analysis of adipose tissue-resident macrophages.
| Reagent / Solution | Function / Application | Example |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Provides a scaffold-free environment for spontaneous 3D spheroid formation from SVF cells [16] [44]. | COSTAR ULA plates [16] |
| Macrophage Colony-Stimulating Factor (M-CSF) | Critical growth factor for the survival, proliferation, and differentiation of macrophages in 3D culture [16] [11]. | Recombinant murine M-CSF (PeproTech) [16] |
| Collagenase & Dispase Enzymes | Enzymatic cocktail for the dissociation of adipose tissue to isolate SVF and for dissociating mature spheroids for analysis [16]. | Collagenase NB4, Dispase I (Sigma-Aldrich) [16] |
| Polarizing Cytokines | Used to stimulate macrophages toward pro-inflammatory (M1-like) or anti-inflammatory (M2-like) states in functional polarization assays [16]. | Recombinant murine IFN-γ and IL-4 (PeproTech) [16] |
| pHrodo-labeled Bioparticles | pH-sensitive fluorescent particles for quantifying phagocytic activity; fluorescence increases upon internalization into acidic phagosomes. | pHrodo Red Zymosan Bioparticles (Thermo Fisher Scientific) |
| Seahorse XF Analyzer Kits | Pre-optimized reagent kits for real-time, live-cell analysis of metabolic function (glycolysis and mitochondrial respiration). | Seahorse XF Glycolysis Stress Test Kit, Mito Stress Test Kit (Agilent) |
| Antibody Panels for Spectral Flow Cytometry | Antibodies against metabolic proteins and surface markers for deep phenotyping of macrophage heterogeneity and metabolic state [63]. | Anti-GLUT1, ACC1, CPT1A, CD11c, CD206, etc. [63] |
Workflow and Signaling Visualization
Workflow for 3D ATM Functional Profiling. This diagram outlines the sequential process from the isolation of the stromal vascular fraction (SVF) through 3D spheroid culture and macrophage generation, to the execution of core functional assays and their corresponding biological readouts.
Macrophage Activation Pathways and Functional Outcomes. This diagram illustrates the primary signaling cues (IFN-γ, IL-4, Fatty Acids) that drive macrophage polarization and metabolic reprogramming, leading to distinct functional capacities. Key metabolic enzymes like ACC1 link fatty acid synthesis to critical functions such as efferocytosis [63] [62].
{article}
Comparative Analysis: 3D vs. 2D vs. Bone Marrow-Derived Macrophages
Macrophages are versatile immune cells central to tissue homeostasis, inflammation, and disease pathogenesis. Their study in vitro relies on models that accurately recapitulate their in vivo functional states. Traditional two-dimensional (2D) cultures of bone marrow-derived macrophages (BMDMs) have been a cornerstone of immunological research. However, a paradigm shift is underway with the development of three-dimensional (3D) culture systems, which better mimic the physiological tissue microenvironment. This is particularly critical in adipose tissue research, where the crosstalk between adipocytes and immune cells is a key driver of metabolic health and disease. This application note provides a comparative analysis of 3D adipose tissue-resident macrophages, traditional 2D BMDMs, and in vivo resident macrophages, offering structured data and detailed protocols to guide researchers in selecting and implementing the most appropriate model for their research objectives.
Comparative Phenotypic and Functional Profiles
The choice of macrophage model significantly influences experimental outcomes, as 2D and 3D systems generate cells with distinct phenotypic, functional, and metabolic characteristics. The table below summarizes the core differences between these models, highlighting how 3D-cultured macrophages more closely mirror the properties of native adipose tissue resident macrophages.
Table 1: Comparative Analysis of Macrophage Models
| Characteristic | 3D Adipose Tissue Macrophages | Traditional 2D BMDMs | In Vivo Adipose Resident Macrophages |
|---|---|---|---|
| Origin / Culture System | Adipose Stromal Vascular Fraction (SVF) in ultra-low attachment plates with M-CSF [7] [11] [16] | Bone marrow progenitors differentiated with M-CSF on plastic surfaces [64] | Embryonic (yolk sac) origin with self-renewal capacity [11] [16] [9] |
| Key Phenotypic Markers | CD206+, F4/80+ [11] [16] | CD11b+, F4/80+, MHC IIhi [64] | TIMD4+, LYVE1+, FOLR2+, CD206+ [11] [16] [23] |
| Transcriptomic Profile | Mirrors the in vivo resident macrophage signature [7] [16] | Distinct from resident macrophages; closer to monocyte-derived inflammatory cells [16] | Unique core signature defined by tissue niche [9] [23] |
| Metabolic Activity | Specific metabolic profile and polarization response [7] [11] | High glycolytic and oxidative capacity; model for metabolic studies [64] | Context-dependent; lipid-associated macrophages show unique flux [23] |
| Proliferative Capacity | Not explicitly detailed | Limited; terminally differentiated, non-proliferative [64] | Self-renewing in tissues [65] [9] |
| Response to Polarization | Altered metabolic activity and gene expression upon IL-4 or IFN-γ stimulation [11] | High plasticity; pronounced M1 (LPS/IFN-γ) and M2 (IL-4/IL-13) polarization [64] | Functional states exist on a continuum beyond M1/M2 [9] [23] |
| Primary Application | Studying adipose tissue immunobiology, metabolic crosstalk, and niche-specific functions [7] [25] | General mechanistic studies of macrophage biology, signaling, and polarization [64] | N/A (gold standard for in vivo validation) |
Beyond phenotypic markers, these models exhibit fundamental differences in functional output. For instance, 3D-cultured macrophages demonstrate a metabolic reprogramming profile that is distinct from their 2D counterparts [7]. Furthermore, in the context of obesity, in vivo studies reveal that adipose tissue macrophages can be broadly categorized into homeostatic tissue-resident macrophages (TRMs) expressing LYVE1 and FOLR2, and lipid-associated macrophages (LAMs) expressing TREM2 and CD9, with the latter population expanding significantly in obesity [23]. This level of functional heterogeneity is challenging to capture fully in traditional 2D BMDM cultures.
Experimental Protocols
Protocol 1: Generation of 3D Adipose Tissue-Resident Macrophages
This protocol describes the generation of functional adipose tissue-resident macrophages from murine subcutaneous fat using a 3D spheroid culture system, adapted from the Frontiers in Immunology study [7] [11] [16].
Materials:
- Animals: 6- to 8-week-old male C57Bl/6J mice.
- Dissection Media: Roswell Park Memorial Institute (RPMI) medium with 1% antibiotics/antimycotics.
- Digestion Enzyme: Collagenase NB4.
- Culture Media: RPMI supplemented with Glutamax, 10% Heat-Inactivated Newborn Calf Serum (hiNBCS), 1% antibiotics/antimycotics, and 10 ng/mL recombinant M-CSF.
- Specialized Plastics: Ultra-low attachment 96-well round-bottom plates.
Procedure:
- Stromal Vascular Fraction (SVF) Isolation: Harvest subcutaneous adipose tissue and remove lymph nodes. Mechanically dissociate the tissue and digest with collagenase NB4 (1-2 U/mL) at 37°C for 30 minutes with agitation. Filter the digest through a cell strainer (e.g., 70 µm) and centrifuge. Lyse red blood cells using an ammonium chloride-based buffer. Resuspend the pellet in culture media to obtain the SVF.
- 3D Spheroid Seeding: Seed the SVF cells at a density of 10^5 cells per well in the ultra-low attachment 96-well plates. Centrifuge the plates briefly (e.g., 300-500 x g for 3 minutes) to aggregate the cells at the bottom of the wells.
- Culture and Differentiation: Incubate the cells at 37°C with 5% CO2.
- Day 4: Cells will spontaneously aggregate to form a single spheroid per well.
- Day 7: Macrophages begin to migrate out of the spheroid and adhere to the culture plate surface.
- Harvesting: Macrophages can be harvested from the culture plate for experimentation from day 7 onwards. To dissociate the spheroid itself for analysis, use a combination of NB4 (1.7 U/mL) and dispase I (2.5 U/mL) at 37°C for 40 minutes, followed by gentle mechanical dissociation.
Protocol 2: Differentiation of Bone Marrow-Derived Macrophages (2D)
This standard protocol for generating BMDMs is a workhorse for immunological research and serves as a baseline for comparison with the 3D model [64].
Materials:
- Bone Marrow Source: Murine femurs and tibias.
- Culture Media: RPMI 1640 or DMEM supplemented with 10% Fetal Bovine Serum (FBS), 1% penicillin/streptomycin, and 20-30% L929-cell conditioned medium (as a source of M-CSF) or 20-50 ng/mL recombinant M-CSF.
- Culture Vessels: Non-treated bacteriologic Petri dishes or plates.
Procedure:
- Bone Marrow Harvest: Flush the marrow from femurs and tibias of euthanized mice using cold PBS. Dissociate the marrow by pipetting or passing through a syringe needle.
- Red Blood Cell Lysis: Pellet the cells and lyse red blood cells using an ammonium chloride solution. Wash and resuspend the cells in complete culture media.
- Plating and Differentiation: Seed the bone marrow cells on non-tissue-culture-treated dishes at a density of 2-5 x 10^5 cells/mL. Culture the cells at 37°C with 5% CO2 for 5-7 days.
- Harvesting: After 5-7 days, adherent BMDMs can be detached using cold PBS or cell dissociation buffers (e.g., containing EDTA) followed by gentle scraping.
Signaling Pathway and Metabolic Reprogramming
The pathophysiological state of macrophages, particularly in the adipose niche, is defined by distinct metabolic and signaling pathways. The following diagram illustrates the core signaling and metabolic reprogramming in Lipid-Associated Macrophages (LAMs), a key population in obese adipose tissue, and how weight loss interventions modulate these pathways.
Figure 1: LAM Signaling and Metabolic Reprogramming.
The Scientist's Toolkit: Research Reagent Solutions
Selecting the appropriate reagents is critical for the successful implementation of the protocols described above. This table lists essential materials and their specific functions in generating and analyzing adipose tissue macrophages.
Table 2: Essential Research Reagents for Adipose Tissue Macrophage Studies
| Reagent / Material | Function / Application | Key Notes |
|---|---|---|
| Ultra-Low Attachment Plates | Enforces scaffold-free 3D spheroid formation by preventing cell adhesion [7] [16] | Critical for the self-assembly of the adipose stromal vascular fraction into organoids. |
| Recombinant M-CSF | Drives differentiation and survival of macrophages from progenitors [7] [64] | Used in both 3D and 2D BMDM protocols at 10-50 ng/mL. |
| Collagenase NB4 | Enzymatic digestion of adipose tissue to isolate the Stromal Vascular Fraction (SVF) [11] [16] | Specific activity and purity are crucial for SVF viability and yield. |
| Flow Cytometry Antibodies | Phenotypic characterization of macrophage subsets [11] [23] | Key targets: F4/80 (pan-macrophage), CD11b, CD206, TIMD4, LYVE1, FOLR2. |
| Polarizing Cytokines | In vitro modulation of macrophage functional states [11] [64] | IFN-γ (50 ng/mL) for M1; IL-4 (10 ng/mL) for M2 polarization. |
The comparative analysis presented herein underscores that 3D-cultured adipose tissue macrophages represent a superior model for investigating adipose-specific immunobiology, as they recapitulate the transcriptomic and functional profile of in vivo resident macrophages more faithfully than traditional 2D BMDMs. The detailed protocols and reagent toolkit provide a robust foundation for researchers to integrate this advanced model into their studies on metabolic disease, drug discovery, and the intricate crosstalk within the adipose tissue niche. The choice of model should be guided by the research question: 2D BMDMs remain a valid tool for general mechanistic studies, while 3D systems are indispensable for niche-specific, translational research.
{/article}
Within the realm of metabolic disease and immunology research, a significant challenge persists: creating in vitro models that truly recapitulate the complex physiological environment of native adipose tissue. This application note addresses this gap by providing detailed protocols for the generation and functional validation of advanced 3D co-culture systems containing adipose-resident macrophages. The fidelity of these models is paramount, and thus we focus specifically on rigorous benchmarking methodologies, using lipidomic and secretory profiles as key quantitative metrics to compare in vitro constructs against native tissue references. This approach provides researchers with a validated framework for developing highly physiological systems suitable for investigating obesity-related metabolic inflammation, evaluating drug efficacy, and advancing therapeutic discovery.
Key Research Reagent Solutions
The following table catalogs essential reagents and materials critical for establishing physiologically relevant 3D adipose tissue models with integrated immune components.
Table 1: Essential Research Reagents for 3D Adipose Tissue-Macrophage Models
| Reagent/Material | Function/Application | Key Characteristics & Rationale |
|---|---|---|
| Gellan Gum (GG) [15] | Animal-free hydrogel matrix for 3D adipocyte encapsulation. | Biocompatible, bacteria-derived exopolysaccharide; provides tunable stiffness and supports adipocyte functionality. |
| Ultra-Low Attachment Plates [11] | Facilitate spontaneous spheroid formation from stromal vascular fraction (SVF). | Promotes 3D self-assembly in the presence of M-CSF, enabling generation of resident-like macrophages. |
| Macrophage Colony-Stimulating Factor (M-CSF) [11] | Differentiation and survival factor for macrophages. | Critical for generating functional mature macrophages from progenitor cells in 3D culture. |
| Defined (Serum-Free) Medium [15] | Animal-free culture medium for co-cultures. | Enhances reproducibility, eliminates batch variability of FCS, and prevents masking of experimental outcomes. |
| Stromal Vascular Fraction (SVF) [11] | Source of adipocyte precursors and resident immune cells. | Contains native cellular heterogeneity, enabling self-organizing adipose organoids with endogenous macrophages. |
| PMA + LPS [15] | Activation stimuli to induce an inflammatory state. | Effectively stimulates pro-inflammatory cytokine production in macrophages, mimicking an obese adipose environment. |
Experimental Protocols for Model Establishment and Benchmarking
Protocol 1: Generation of Functional Macrophages from Adipose Tissue via 3D Spheroid Culture
This protocol enables the in vitro generation of macrophages that mirror the phenotypic and functional traits of in-vivo adipose tissue resident macrophages, providing a critical immune component for co-culture systems [11].
Materials:
- Isolation medium: α-MEM supplemented with collagenase (e.g., NB4, 1.7 U/mL).
- Growth medium: RPMI supplemented with Glutamax, 10% Heat-Inactivated Newborn Calf Serum, 1% penicillin/streptomycin/amphotericin, and 10 ng/mL M-CSF.
- Ultra-low adherence 96-well round-bottom plates.
- Dissociation solution: Collagenase NB4 (1.7 U/mL) and dispase I (2.5 U/mL).
Method:
- Isolate Stromal Vascular Fraction (SVF):
- Collect subcutaneous adipose tissue from mice (C57Bl/6J, 6-8 weeks old).
- Mechanically dissociate tissue and digest with collagenase in α-MEM at 37°C for 30 minutes.
- Filter the digestate through a cell strainer and centrifuge.
- Perform red blood cell lysis on the pellet (SVF) and count cells.
Initiate 3D Spheroid Culture:
- Seed SVF cells at a density of 10^5 cells/well into ultra-low adherence 96-well plates in growth medium.
- Centrifuge plates briefly and incubate at 37°C with 5% CO₂.
- Within 4 days, cells will spontaneously aggregate to form spheroids.
Harvest and Mature Macrophages:
- From day 7 onwards, macrophages will begin to migrate out of the spheroids and adhere to the plate.
- For analysis, spheroids can be collected between days 7-21.
- To dissociate, incubate spheroids with collagenase NB4 and dispase I at 37°C for 40 minutes, followed by mechanical pipetting and centrifugation.
- Differentiated macrophages can be seeded onto adherent plates for functional assays.
Protocol 2: Assembly of an Animal-Free 3D Adipocyte-Macrophage Co-Culture
This protocol details the setup of a defined, serum-free co-culture system to study human adipocyte-macrophage crosstalk in an inflamed microenvironment [15].
Materials:
- Primary human mature adipocytes (ACs).
- Human monocytic cell line (e.g., THP-1 or MM6).
- Gellan Gum (GG) hydrogel.
- Defined, serum-free culture medium.
- Activation stimuli: 1 µg/mL Lipopolysaccharide (LPS) and 10 ng/mL Phorbol 12-myristate 13-acetate (PMA).
Method:
- Encapsulate Adipocytes:
- Resuspend primary human mature adipocytes in a sterile Gellan Gum solution.
- Plate the cell-hydrogel mixture and induce gelation to form a 3D scaffold encapsulating the adipocytes.
Introduce Immune Component:
- Culture THP-1 or MM6 monocytic cells in the same defined medium.
- Add the monocytic cells to the culture system containing the adipocyte-loaded GG hydrogel.
Induce Inflammation:
- Activate the co-culture by adding a combination of PMA and LPS to the defined medium.
- The model sustains a robust inflammatory state for at least 72 hours, suitable for testing anti-inflammatory compounds.
Quantitative Benchmarking Against Native Tissue
Lipidomic Profiling of Native Tissue and Adiposomes
Comprehensive lipidomic analysis of native human adipose tissue and derived adiposomes (adipose tissue-derived extracellular vesicles) reveals specific lipid shifts in obesity, providing a critical benchmark for model validation [66] [67].
Table 2: Lipidomic Shifts in Human Adiposomes: Lean vs. Obese Phenotype
| Lipid Class | Change in Obesity (vs. Lean) | Representative Lipid Species (Change) | Correlation with Clinical Parameters |
|---|---|---|---|
| Ceramides (Cer) | Significantly Increased | Cer-NS d18:1/23:0 (↑) | Positive correlation with insulin resistance (HOMA-IR), systemic inflammation (IL-6, CRP). |
| Free Fatty Acids (FA) | Significantly Increased | - | Associated with impaired vascular function (reduced FMD). |
| Acylcarnitines (Acar) | Significantly Increased | - | Linked to metabolic dysregulation and insulin resistance. |
| Phosphatidylcholine (PC) | Significantly Decreased | - | Negative correlation with BMI and cardiometabolic risk factors. |
| Sphingomyelins (SM) | Significantly Decreased | - | Loss associated with inflammation and vascular impairment. |
| FAHFA | Significantly Decreased | FAHFA 18:0/20:2 (↓) | Anti-inflammatory lipids; reduction exacerbates metabolic dysfunction. |
Key findings from native tissue analysis include:
- Particle Release: Adiposome concentration is 100% higher in individuals with obesity (9.0 × 10¹¹ vs. 4.5 × 10¹¹ particles/mL) [66].
- Pathway Dysregulation: Enrichment analyses highlight dysregulation in glycerophospholipid metabolism, sphingolipid metabolism, and proinflammatory pathways in obesity [66].
- Biomarker Potential: Machine-learning models using adiposome lipid data can classify obesity and predict cardiometabolic conditions with >85% accuracy [66] [67].
Secretory and Functional Profiling of Macrophages
Spatial and single-cell analyses of native adipose tissue reveal a dynamic macrophage landscape during obesity, characterized by distinct functional subsets [68].
Table 3: Secretory and Functional Profiles of Adipose Tissue Macrophage Subsets in Obesity
| Macrophage Subset | Spatial Localization | Secretory & Functional Profile | Proposed Role in Obesity |
|---|---|---|---|
| Proinflammatory Immune Cells | - | Predominance in early obesity. | Initiation of adipose tissue inflammation and dysfunction. |
| Lipid-Associated Macrophage (LAM) Precursor (pre-LAM) | Associated with early obesity Crown-Like Structures (CLS) | Express lipid-handling ligands (Apoe, Lpl, Lrp1, App). | Key role in early CLS formation; intermediary in LAM differentiation. |
| Mature Lipid-Associated Macrophages (LAMs) | Within Crown-Like Structures (CLS) | Engulf lipid droplets; Trem2+ phenotype. | Lipid scavenging in chronically obese tissue; sustained inflammation. |
| Non-resident Anti-inflammatory ATMs | - | Predominate in chronic obesity. | Resolution of inflammation or alternative activation states. |
Signaling Pathways in the Adipose Tissue Niche
Spatial transcriptomics of native adipose tissue in early diet-induced obesity has identified a ligand-receptor signaling network involving monocytes, pre-LAMs, and LAMs, centered on lipid signaling [68]. Key components of this pathway include Apoe, Lrp1, Lpl, and App, suggesting a coordinated mechanism for lipid handling and intercellular communication within the niche.
Diagram 1: Lipid Signaling in Early Obesity. This pathway illustrates the differentiation of monocytes into lipid-associated macrophages (LAMs) via a pre-LAM intermediate within the crown-like structure (CLS) niche, driven by specific lipid-handling ligands [68].
Integrated Experimental Workflow for Model Validation
A robust benchmarking strategy requires an integrated workflow that progresses from model establishment to multi-faceted validation against native tissue standards.
Diagram 2: Benchmarking Workflow. The integrated process for validating 3D adipose tissue models against native tissue lipidomic, secretory, and functional data [66] [15] [11].
Metabolically active adipose tissue is a complex endocrine organ, and its dysfunction is a cornerstone of diseases like type 2 diabetes and obesity. A critical aspect of this dysfunction involves the intricate crosstalk between adipocytes and resident immune cells, particularly macrophages. Research using advanced 3D co-culture systems has revealed that adipose tissue macrophages are not passive bystanders but active participants in regulating both insulin sensitivity and lipolysis—the breakdown of triglycerides into free fatty acids [15]. This application note provides detailed protocols and frameworks for assessing these key metabolic functions within the context of contemporary research on adipose tissue-resident macrophages.
Assessing Insulin Sensitivity
Insulin sensitivity refers to the responsiveness of target tissues (e.g., liver, muscle, adipose) to insulin's glucose-lowering effects. Its quantification is essential for understanding metabolic health.
Reference Standard: Hyperinsulinemic-Euglycemic Clamp
The hyperinsulinemic-euglycemic clamp, developed by Andres and DeFronzo, is the gold standard for directly measuring whole-body insulin sensitivity [69].
- Procedure: After an overnight fast, a primed, constant intravenous infusion of insulin is administered to achieve a steady-state hyperinsulinemic plateau. A variable-rate glucose infusion is simultaneously adjusted based on frequent (5-10 min) blood glucose measurements to "clamp" blood glucose at a normal fasting level (euglycemia). Under steady-state conditions, the glucose infusion rate (GIR) equals whole-body glucose disposal, providing a direct measure of insulin action [69].
- Data Interpretation: The insulin sensitivity index (SIClamp) is calculated as M/(G × ΔI), where M is the steady-state glucose disposal rate (often normalized to body weight or fat-free mass), G is the steady-state blood glucose concentration, and ΔI is the difference between fasting and steady-state plasma insulin levels [69].
Simple Surrogate Indices
For large-scale studies where the clamp is impractical, validated surrogate indices derived from fasting samples are used. Table 1 summarizes the most common indices. The Single-Point Insulin Sensitivity Estimator (SPISE) index has recently gained prominence for its strong correlation with clamp-measured insulin sensitivity and superior performance in predicting metabolic syndrome (MetS), with pooled AUC values reaching 0.86 in meta-analyses [70] [71]. Its formula is non-invasive, relying on common clinical measures.
Table 1: Surrogate Indices for Estimating Insulin Sensitivity/Resistance
| Index Name | Formula | Key Advantages | Reported AUC for MetS |
|---|---|---|---|
| SPISE [70] | ( \frac{600 \times HDL-C^{0.185}}{(TG^{0.2} \times BMI^{1.338})} ) | Does not require insulin measurement; excellent predictive power for MetS [70]. | 0.86 (0.83-0.90) |
| HOMA-IR [69] | (Fasting Glucose × Fasting Insulin) / 22.5 | Widely used, extensive validation data. | Lower than SPISE [70] |
| QUICKI [69] | 1 / (log(Fasting Insulin) + log(Fasting Glucose)) | Good correlation with clamp data. | N/A |
| TG/HDL-C Ratio [71] | Triglycerides / HDL-C | Simple, uses common lipid panel. | Lower than SPISE [71] |
Investigating Lipolytic Function
Lipolysis is a fundamental metabolic process regulated by hormonal signals, including stimulation by catecholamines and inhibition by insulin [72].
Signaling Pathways in Adrenergic-Stimulated Lipolysis
Beta-adrenergic activation in adipocytes initiates a cascade leading to lipolysis. Recent research has uncovered a novel pathway linking this metabolic process to behavior via macrophage signaling. The following diagram illustrates this integrated pathway.
This pathway is critical in physiological (e.g., cold exposure, fasting) and pathological states. Studies show that genetic ablation of adipose triglyceride lipase (ATGL) or β-adrenergic receptors in mice completely blocks the increase in GDF15 following stimulation or restraint stress, confirming the necessity of this lipolytic cascade [73].
Protocol: Assessing Lipolysis in a 3D Adipocyte-Macrophage Co-Culture System
This protocol, adapted from current research, details the setup of an animal-free 3D co-culture to study lipolysis and its interplay with macrophages [15].
- Workflow Overview:
- Detailed Methodology:
- 3D Adipocyte Culture Setup: Encapsulate primary human mature adipocytes in a thermosensitive, animal-free gellan gum (GG) hydrogel. GG concentration and cation content can be tuned to adjust mechanical properties [15].
- Macrophage Component: Use human monocytic cell lines (e.g., MM6 or THP-1). Differentiate and activate them into a pro-inflammatory state using Phorbol 12-myristate 13-acetate (PMA) and Lipopolysaccharide (LPS) in a defined, serum-free medium to avoid confounding effects of serum [15].
- Co-culture and Stimulation: Combine the 3D adipocyte constructs with the activated macrophages. To induce lipolysis, stimulate the system with a β-adrenergic agonist (e.g., 1µM Isoproterenol or CL316,243) for 2-4 hours.
- Lipolysis Quantification: Measure glycerol concentration in the culture medium using a commercial colorimetric or fluorometric assay. This is the gold-standard metric for lipolytic rate. Free fatty acid levels can be measured in parallel. Furthermore, supernatant can be analyzed for GDF15 via ELISA to capture the macrophage response [73].
The Scientist's Toolkit: Essential Research Reagents
Success in these functional assays relies on specific, high-quality reagents. Table 2 lists key materials for setting up the described 3D co-culture and lipolysis experiments.
Table 2: Key Research Reagents for 3D Adipose Tissue Metabolic Studies
| Item | Function/Description | Example Application |
|---|---|---|
| Gellan Gum (GG) | Animal-free, bacteria-derived polysaccharide hydrogel for 3D cell encapsulation; biocompatible and tunable [15]. | Scaffold for 3D adipocyte culture. |
| Defined Serum-Free Medium | Chemically defined medium without animal serum; reduces batch variability and improves experimental reproducibility [15]. | Maintenance of adipocyte-macrophage co-culture. |
| M-CSF | Macrophage Colony-Stimulating Factor; promotes differentiation and survival of macrophage lineages [11]. | Generation of macrophages from bone marrow or monocytic precursors. |
| β-adrenergic Agonists | Receptor agonists (e.g., CL316,243, Isoproterenol) that stimulate the cAMP-PKA pathway to activate lipolysis [73] [72]. | Induction of lipolysis in adipocytes. |
| ATGListatin | A specific inhibitor of Adipose Triglyceride Lipase (ATGL), the rate-limiting enzyme in lipolysis [73]. | Inhibition of lipolysis to confirm pathway specificity. |
| PMA + LPS | Phorbol ester and bacterial endotoxin used in combination to differentiate and robustly activate pro-inflammatory signaling in macrophages [15]. | Activation of macrophages in the co-culture system. |
Understanding metabolic responsiveness in adipose tissue requires robust methods for quantifying insulin sensitivity and lipolytic function. While the hyperinsulinemic-euglycemic clamp remains the reference method, surrogate indices like SPISE offer practical, non-invasive screening tools with high clinical relevance. Furthermore, the development of sophisticated 3D co-culture models that recapitulate the adipocyte-macrophage crosstalk has been instrumental in uncovering novel endocrine pathways, such as the lipolysis-GDF15 axis, which links peripheral metabolism to behavioral responses [73]. These application notes provide a foundational framework for researchers to investigate these critical metabolic processes in a physiologically relevant context.
Conclusion
3D culture systems represent a transformative advancement for studying adipose tissue-resident macrophages, successfully bridging the gap between conventional 2D cultures and in vivo physiology. These models generate macrophages that faithfully replicate the transcriptomic, phenotypic, and functional characteristics of their in vivo counterparts, enabling more accurate investigation of immunometabolic diseases. The integration of vascular components, immune-stromal crosstalk, and patient-specific cells in these platforms paves the way for personalized medicine applications and more predictive pre-clinical drug screening. Future directions should focus on developing perfusable, vascularized systems to overcome diffusion limitations, standardizing protocols across laboratories, and further integrating multi-omics approaches to fully capture the complexity of adipose tissue biology. As these models continue to evolve, they will undoubtedly accelerate the development of novel therapeutics for obesity, diabetes, and related metabolic disorders.
References
- 1. Special Issue “New Insights into Adipose Tissue Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12386224/]
- 2. Immune cell–adipose tissue crosstalk in metabolic ... [https://link.springer.com/article/10.1007/s00125-025-06437-z]
- 3. Adipose tissue: an inflammatory organ that can not be ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1698207/full]
- 4. Adipose tissue macrophage heterogeneity in the single- ... [https://www.sciencedirect.com/science/article/pii/S1016847824000360]
- 5. High-fat diet-induced adipose tissue-resident ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1524544/full]
- 6. Resident macrophages restrain pathological adipose tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8339675/]
- 7. Generation of functionally active resident macrophages ... [https://pubmed.ncbi.nlm.nih.gov/38975341/]
- 8. The Impact of Resident Adipose Tissue Macrophages on ... [https://www.mdpi.com/1422-0067/25/23/13019]
- 9. Tissue macrophages: origin, heterogenity, biological ... [https://www.nature.com/articles/s41392-025-02124-y]
- 10. Single-Cell Proteomics Reveals the Defined Heterogeneity ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.719979/full]
- 11. Generation of functionally active resident macrophages ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1356397/full]
- 12. Functional diversity of disorder-specific macrophages involved ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12487080/]
- 13. Distinct bone marrow-derived and tissue resident ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3842019/]
- 14. Unravelling approaches to study macrophages: from classical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11847493/]
- 15. Animal‐Free Setup of a 3D Mature Adipocyte‐Macrophage Co ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12391635/]
- 16. Generation of functionally active resident macrophages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11224291/]
- 17. Adipose tissue macrophage dysfunction is associated with ... [https://www.sciencedirect.com/science/article/pii/S0168827823052716]
- 18. Role of Tim4 in the regulation of ABCA1 + adipose tissue ... [https://www.nature.com/articles/s41467-021-24684-7]
- 19. FOLR2 + macrophages in cancer: allies or enemies [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02257-1]
- 20. Innate Immune System Orchestrates Metabolic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.702835/full]
- 21. Chronic tissue inflammation and metabolic disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7919414/]
- 22. The Interplay Between Tissue Niche and Macrophage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6987434/]
- 23. Selective remodelling of the adipose niche in obesity and ... [https://www.nature.com/articles/s41586-025-09233-2]
- 24. Animal-Free Setup of a 3D Mature Adipocyte-Macrophage ... [https://pubmed.ncbi.nlm.nih.gov/40538298/]
- 25. 3D Adipose Tissue Models: 10 Impactful Studies [https://www.cherrybiotech.com/scientific-note/10-studies-3d-adipose-tissue-models/]
- 26. Bone marrow Adipoq-lineage progenitors are a major ... [https://elifesciences.org/articles/82118]
- 27. Microenvironmental conditions and serum availability alter ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12239098/]
- 28. Dynamically cultured, differentiated bovine adipose ... [https://www.nature.com/articles/s41467-024-53486-w]
- 29. Extending the Three-Dimensional Culture of Adipocytes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11939550/]
- 30. Development of novel human in vitro vascularized adipose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7547925/]
- 31. Adipose Tissue Organoids: Protocols & Applications [https://www.cherrybiotech.com/scientific-note/adipose-tissue-organoids-protocols-applications-current-limitations/]
- 32. Characterisation and comparison of adipose tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4940901/]
- 33. Vasculature-associated fat macrophages readily adapt to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6446877/]
- 34. Development and characterisation of a novel 3D in vitro ... [https://www.nature.com/articles/s41523-025-00766-3]
- 35. Three-Dimensional Cell Cultures in Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5448717/]
- 36. Diverse Functions of Macrophages in Obesity and ... [https://immunenetwork.org/DOIx.php?id=10.4110/in.2025.25.e12]
- 37. Obesity-associated macrophages dictate adipose stem cell ... [https://www.nature.com/articles/s41467-025-62690-1]
- 38. A novel 3D culture model for human primary mammary ... [https://www.nature.com/articles/s41598-023-31673-x]
- 39. Interactive Changes between Macrophages and Adipocytes [https://pmc.ncbi.nlm.nih.gov/articles/PMC2849320/]
- 40. THP-1 Macrophages and SGBS Adipocytes – A New Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3355855/]
- 41. Mimicking the Complexity of Solid Tumors: How Spheroids ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11987746/]
- 42. A 3D spheroid model for assessing nanocarrier-based ... [https://www.nature.com/articles/s44385-025-00041-x]
- 43. Sustainable Three-Dimensional Tissue Model of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3751318/]
- 44. Generation of immune cell containing adipose organoids ... [https://www.nature.com/articles/s41598-020-78015-9]
- 45. Glucose metabolism is linked to the inflammatory status of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3374262/]
- 46. The Evolving Role of Macrophage Metabolic ... [https://pubmed.ncbi.nlm.nih.gov/40311669/]
- 47. Review The Evolving Role of Macrophage Metabolic ... [https://www.sciencedirect.com/science/article/pii/S0828282X25003204]
- 48. Non-canonical lysosomal lipolysis drives mobilization of ... [https://www.nature.com/articles/s41467-025-56613-3]
- 49. Fibrin-based 3D Matrices Induce Angiogenic Behavior of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4380681/]
- 50. 3D collagen matrices modulate the transcriptional ... [https://www.sciencedirect.com/science/article/pii/S2452199X21004084]
- 51. Three-Dimensional Adipocyte Culture: The Next Frontier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4655218/]
- 52. investigating how macrophage origin influences responses ... [https://www.frontiersin.org/journals/biomaterials-science/articles/10.3389/fbiom.2024.1399448/full]
- 53. Technological advances in fibrin for tissue engineering - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10426312/]
- 54. Macrophages generated in 3D mechanical microenvironment ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04413-3]
- 55. The Effect of Collagen and Fibrin Hydrogels Encapsulated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10858360/]
- 56. Optimized scaffold-free human 3D adipose tissue organoid ... [https://www.sciencedirect.com/science/article/pii/S2472555225000115]
- 57. - Single profiling to improve the translation... cell RNA sequencing [https://pubmed.ncbi.nlm.nih.gov/38179052/]
- 58. Robust single-nucleus RNA sequencing reveals depot ... [https://elifesciences.org/articles/97981]
- 59. - Single analysis of human pleura reveals stromal... cell transcriptomic [https://publications.ersnet.org/content/erj/63/1/2300143]
- 60. Prioritization and functional validation of target genes from ... [https://www.nature.com/articles/s42003-023-05006-7]
- 61. Identification of in vitro and in vivo disconnects using ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-015-1726-7]
- 62. Adipocyte death triggers a pro-inflammatory response and ... [https://www.nature.com/articles/s41419-021-03872-9]
- 63. Metabolic heterogeneity of tissue-resident macrophages in ... [https://www.nature.com/articles/s41467-023-41353-z]
- 64. Comprehensive review of macrophage models: primary ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1640935/full]
- 65. Macrophages with different origins proliferate ex vivo and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159446/]
- 66. Lipidomic profiling of human adiposomes identifies specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226050/]
- 67. Lipidomic profiling of human adiposomes identifies specific ... [https://pubmed.ncbi.nlm.nih.gov/40548377/]
- 68. A lipid-associated macrophage lineage rewires the spatial ... [https://insight.jci.org/articles/view/171701]
- 69. Assessing Insulin Sensitivity and Resistance in Humans [https://www.ncbi.nlm.nih.gov/books/NBK278954/]
- 70. Screening accuracy of Single-Point Insulin Sensitivity ... [https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-025-01957-6]
- 71. Single point insulin sensitivity estimator index for ... [https://www.sciencedirect.com/science/article/abs/pii/S1871403X24000905]
- 72. Multi-omics analysis of thermogenic lipolysis in brown ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12424250/]
- 73. GDF15 links adipose tissue lipolysis with anxiety [https://www.nature.com/articles/s42255-025-01264-3]