Harnessing Circadian Rhythms to Manage Intraindividual Variation in Immune Studies
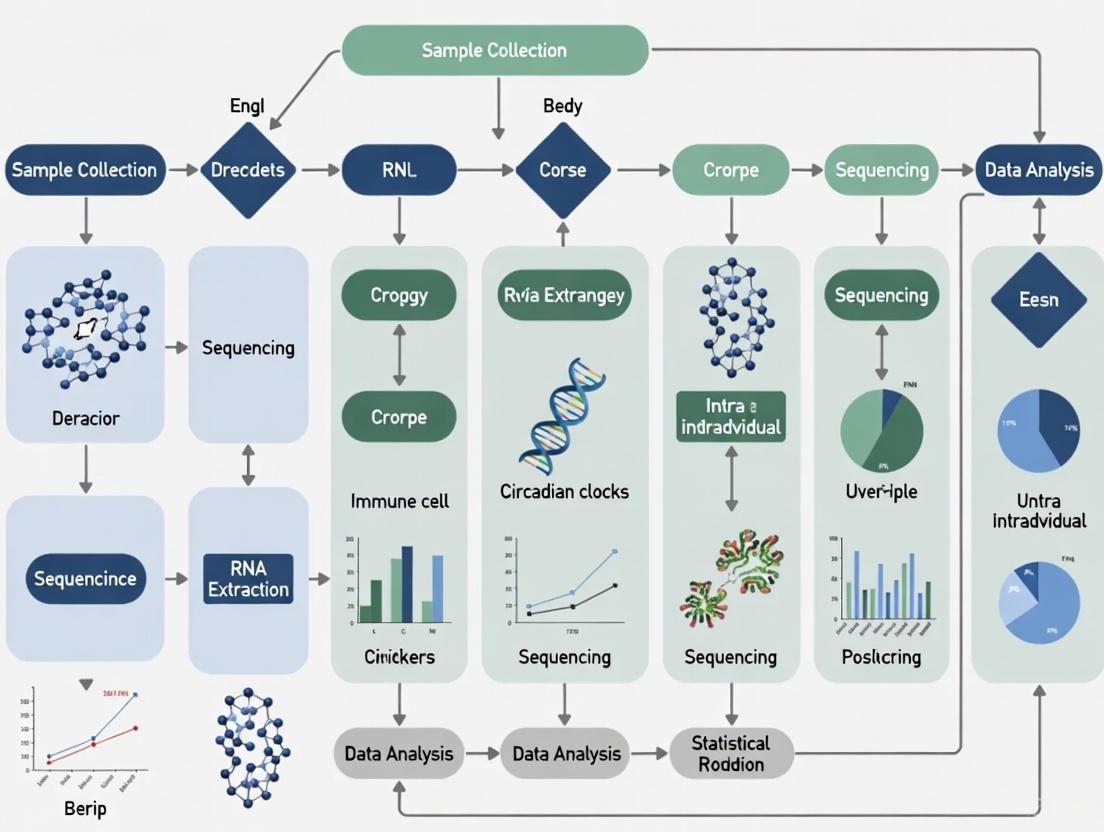
This article provides a comprehensive guide for researchers and drug development professionals on the critical impact of diurnal rhythms on immune function and how to manage the resulting intraindividual variation...
Harnessing Circadian Rhythms to Manage Intraindividual Variation in Immune Studies
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the critical impact of diurnal rhythms on immune function and how to manage the resulting intraindividual variation in biomedical studies. It explores the foundational molecular mechanisms of circadian immunity, presents methodological frameworks for integrating temporal considerations into study design, and offers troubleshooting strategies to mitigate rhythm-induced variability. Drawing on recent evidence from CAR-T cell therapy, vaccine research, and proteomics, the content synthesizes practical approaches for validating findings and optimizing therapeutic timing, ultimately aiming to enhance the precision, reproducibility, and clinical success of immunology research.
The Circadian Immune System: Unraveling Molecular Clocks and Diurnal Variation
FAQ: Core Mechanisms and Experimental Challenges
Q1: What is the core molecular mechanism of the circadian clock and how can its disruption affect immune studies? The core mechanism is a transcription-translation feedback loop (TTFL). The BMAL1/CLOCK heterodimer acts as the central activator, binding to E-box elements to drive the expression of genes including their own repressors, Period (Per) and Cryptochrome (Cry). PER and CRY proteins then form a complex that inhibits BMAL1/CLOCK activity, creating a ~24-hour oscillation cycle [1] [2]. A secondary loop involves nuclear receptors REV-ERBα and ROR, which rhythmically repress and activate Bmal1 transcription, respectively [2]. Disruption of this loop (e.g., via Bmal1 deletion) ablates circadian rhythms and leads to a hyper-inflammatory state in immune cells like macrophages, significantly increasing the production of cytokines like IL-1β [3]. This can introduce profound variability in immune outcomes based on the time of day or the genetic integrity of the clock in your model system.
Q2: Why is understanding intra-individual variation critical for diurnal rhythms research in immunology? The immune system is not static; it exhibits significant rhythmicity over the 24-hour day. Key immune parameters—such as leukocyte trafficking, cytokine release, and the response to pathogens—are all under circadian control [4]. Furthermore, an individual's immune profile is shaped by a combination of heritable and non-heritable factors, including age, sex, and environmental exposures [5] [6]. Failing to account for this temporal and individual variability can lead to inconsistent experimental results, an inability to replicate findings, and a failure to identify true biological effects. Properly managing this variation requires strict standardization of sample collection times and meticulous recording of participant metadata.
Q3: What are the practical consequences of BMAL1/CLOCK disruption in immune cell function? Disruption of the core clock, particularly loss of BMAL1, has a direct impact on immunometabolism, which in turn dictates immune cell function. In macrophages, Bmal1 deficiency causes a metabolic shift toward enhanced glycolysis and mitochondrial respiration [3]. This shift drives inflammation through two primary pathways:
- Succinate Accumulation: Increased flux through the Krebs cycle leads to accumulation of the metabolite succinate. This stabilizes the transcription factor HIF-1α, which promotes Il1b transcription [3].
- PKM2-STAT3 Signaling: BMAL1 normally represses the glycolytic enzyme PKM2. In its absence, increased PKM2 phosphorylates and activates STAT3, which further drives Il1b mRNA expression [3]. Consequently, disruption leads to a consistently heightened pro-inflammatory state.
Troubleshooting Common Experimental Issues
Table 1: Troubleshooting Guide for Circadian Immunology Experiments
| Problem | Potential Cause | Recommended Solution | Key References |
|---|---|---|---|
| High variability in cytokine measurements | Uncontrolled diurnal rhythmicity of immune cells; circadian disruption in animal models. | Standardize time of sample collection across all experimental groups; confirm genetic background and clock gene integrity in transgenic models. | [4] [6] |
| Inconsistent immune cell population counts in flow cytometry | Circadian-driven egress of leukocytes from bone marrow and trafficking to tissues. | Process all samples at the same time of day; include time as a co-variable in statistical analysis. | [4] |
| Unstable circadian oscillations in cell culture | Desynchronization of cellular clocks in vitro; over-confluent cells. | Synchronize cells using a serum shock or dexamethasone treatment; maintain cells at sub-confluent density. | [2] |
| Loss of rhythmic gene expression in Bmal1 KO models | Complete ablation of the core feedback loop. | Use inducible or cell-specific knockout systems to study developmental vs. acute effects; validate knockout efficiency. | [1] [3] |
| Conflicting inflammatory phenotypes in different studies | Use of different global vs. cell-specific knockout models; variations in Zeitgeber Time (ZT) of analysis. | Clearly report the genetic model used and the exact ZT of all experiments and sampling. | [1] |
Table 2: Quantifying Circadian Rhythm Parameters
| Parameter | Description | Experimental Application |
|---|---|---|
| Period | The length of one complete cycle (typically ~24 hours). | Determined by tracking PER2::Luciferase bioluminescence over several days in vitro [7]. |
| Phase | The timing of a specific reference point (e.g., peak, trough) within the cycle. | Used to analyze diurnal body temperature nadir in critically ill patients vs. healthy controls [8]. |
| Amplitude | The magnitude of the difference between peak and trough of the rhythm. | Suppressed temperature rhythm amplitude indicates circadian disruption in ICU patients [8]. |
| Mesor | The rhythm-adjusted mean value around which the oscillation occurs. | CIM patients showed lower temperature rhythm mesors than non-CIM patients [8]. |
Essential Experimental Protocols
Protocol 1: Assessing Circadian Rhythms in Macrophage Immune-Metabolic Function
This protocol is adapted from research investigating BMAL1's role as a metabolic sensor in macrophages [3].
Key Research Reagent Solutions:
- Cells: Bone marrow-derived macrophages (BMDMs) from wild-type and Bmal1^-/-^ mice.
- Synchronization Agent: Dexamethasone (100 nM for 1 hour).
- Stimuli: Lipopolysaccharides (LPS) from E. coli.
- Metabolic Inhibitors: 2-deoxyglucose (2-DG, glycolysis inhibitor), Dimethyl malonate (SDH inhibitor).
- Key Assay Kits: Extracellular Flux Analyzer kit (e.g., Seahorse XF Glycolysis Stress Test), IL-1β ELISA, commercial kits for glucose uptake and lactate production.
Step-by-Step Methodology:
- Cell Culture and Synchronization: Differentiate BMDMs for 6 days. Seed cells for experiments and synchronize the circadian clocks by treating with 100 nM dexamethasone for 1 hour. Replace with fresh media post-treatment.
- Stimulation: At the desired circadian timepoint (e.g., peak of inflammatory response), stimulate cells with LPS.
- Metabolic Phenotyping:
- Glycolysis: Measure the Extracellular Acidification Rate (ECAR) using a Seahorse XF Analyzer.
- Mitochondrial Respiration: Measure the Oxygen Consumption Rate (OCR) using the same instrument.
- Glucose Uptake and Lactate: Quantify using commercial colorimetric/fluorometric assays.
- Inflammatory Output Measurement:
- Harvest cell supernatant and measure IL-1β protein levels via ELISA.
- Analyze gene expression of Il1b and other targets via qPCR.
- Pathway Inhibition: Use pharmacological inhibitors (e.g., 2-DG, dimethyl malonate) to dissect the contribution of specific metabolic pathways to the inflammatory response.
Protocol 2: Pharmacological Modulation of BMAL1 with Small Molecules
This protocol utilizes the recently developed small molecule CCM to directly target BMAL1 [7].
Key Research Reagent Solutions:
- Compound: Core Circadian Modulator (CCM), a selective ligand for the PASB domain of BMAL1.
- Cell Lines: U2OS cells or primary macrophages.
- Validational Assays: Cellular Thermal Shift Assay (CETSA), PER2::Luciferase reporter system.
Step-by-Step Methodology:
- Target Engagement Validation:
- Use a CETSA to confirm CCM binding to BMAL1 in a cellular context. Treat cells with CCM (EC50 ~10.3 µM), heat shock cells at a range of temperatures, and quantify the stabilization of BMAL1.
- Functional Circadian Assay:
- Treat cells carrying a PER2::Luciferase reporter with CCM.
- Monitor bioluminescence rhythms in real-time over several days. CCM treatment will produce dose-dependent alterations in the period and amplitude of PER2::Luc oscillation [7].
- Downstream Immune Phenotyping:
- Treat macrophages with CCM and assess its effect on LPS-induced inflammatory pathways, including the production of IL-1β and phagocytic activity [7].
Signaling Pathways and Workflows
Diagram 1: Core Circadian Feedback Loops. This illustrates the core transcription-translation feedback loops of the molecular clock. The BMAL1/CLOCK heterodimer drives the expression of repressors (PER/CRY) and components of the stabilizing loop (REV-ERB, ROR), which together generate rhythmic gene expression [1] [2].
Diagram 2: BMAL1 Regulates IL-1β via Immunometabolism. This shows the consequences of Bmal1 deletion in macrophages. The loss of BMAL1 removes a metabolic brake, leading to enhanced glycolysis and mitochondrial respiration. This drives pro-IL-1β production via two converging pathways: PKM2-STAT3 signaling and succinate-HIF-1α stabilization [3].
Technical Support Center
Troubleshooting Guides
Problem: Inconsistent Leukocyte Migration Assay Results
| Possible Source of Error | Test or Corrective Action |
|---|---|
| Uncontrolled Circadian Timing | Standardize tissue collection and experimental procedures to a specific Zeitgeber Time (ZT), preferably during the peak migration window (e.g., ZT7 for mouse dermal dendritic cells) [9]. |
| Misaligned Animal Housing | Ensure all experimental animals are maintained under strict, synchronized 12-hour light/12-hour dark (12L:12D) cycles for at least two weeks prior to experimentation [10] [9]. |
| Neglected Chronotype (Human Studies) | In human immune cell studies, assess participant chronotype using questionnaires (e.g., Morningness-Eveningness-Questionnaire), as it can influence the diurnal rhythm of immune parameters [11]. |
| Non-Oscillating In Vitro Cells | Synchronize the intrinsic clocks of cultured immune cells (e.g., Bone Marrow-Derived Dendritic Cells) using a medium containing 50% serum ("serum shock") before conducting migration assays [9]. |
Problem: High Background in Lymphatic Vessel Staining
| Possible Source of Error | Test or Corrective Action |
|---|---|
| High Antibody Concentration | Titrate antibodies against key lymphatic markers (e.g., anti-LYVE-1) to determine the optimal concentration that minimizes non-specific binding [12]. |
| Inadequate Blocking | Implement a blocking step prior to primary antibody incubation using a solution such as 1% bovine serum albumin (BSA) with 10% normal serum from the same species as the secondary antibody [12]. |
| Antigen Retrieval Issues | For fixed tissues, optimize antigen retrieval by empirically testing different treatment times or solutions to restore the immunoreactivity of antigens like CD99 and JAM-A without destroying tissue morphology [12]. |
Frequently Asked Questions (FAQs)
Q1: Why is the time of day I collect blood or tissue samples so critical in immunology research?
A: The immune system is highly rhythmic. The numbers and migratory capacities of leukocytes in the blood and tissues oscillate over 24 hours [13]. For example, inflammatory monocyte recruitment to sites of inflammation is stronger in the afternoon (ZT8 in mice) compared to the morning (ZT0) [10]. If sampling time is not controlled, it introduces significant variation, potentially obscuring true experimental effects or treatments.
Q2: My research involves human participants. How can I account for circadian rhythms?
A: Two key strategies are:
- Standardize Sampling Time: Collect all samples at the same time of day for all participants in a study to minimize variability [11].
- Assess Chronotype: Use standardized questionnaires to determine if a participant's natural sleep-wake cycle (morningness or eveningness) influences your immune readouts. One study found that the IMMAX immune age score decreased during the day in morning-type individuals [11].
Q3: Are the circadian rhythms in immune cell migration just a response to light, or are they built into the cells themselves?
A: Evidence supports both systemic and cell-intrinsic regulation. Immune cells possess their own functional molecular clocks, making their migratory capacity cell-autonomous [10] [14] [9]. This intrinsic rhythm is synchronized by the body's master clock but persists even in constant darkness or in ex vivo conditions, confirming it is a true circadian process and not just a light-driven reaction [10] [9].
Q4: What is the clinical relevance of circadian leukocyte trafficking?
A: Understanding these rhythms is paving the way for "chronotherapy." The efficacy of treatments, including vaccinations and immunotherapies like immune checkpoint blockade and CAR-T cell therapy, can be significantly influenced by the time of day they are administered [10] [14]. Furthermore, disrupted circadian rhythms are linked to exacerbated inflammation in autoimmune diseases [15] [13].
Experimental Protocols & Data
Key Experimental Workflow: Analyzing Rhythmic DC Migration
The following diagram illustrates a key method from research for studying circadian-controlled dendritic cell (DC) migration ex vivo.
Protocol Details: This method demonstrated that DC infiltration into skin lymphatics peaks during the rest phase (ZT7, "day") in mice and is controlled by rhythmic expression of adhesion molecules and chemokines in lymphatic endothelial cells [9]. The rhythm persists in constant darkness, proving it is circadian [9].
Quantifying Circadian Immune Variation
The table below summarizes key quantitative findings on the diurnal variation of different immune parameters, essential for designing and interpreting experiments.
Table 1: Measured Diurnal/Circadian Variations in Immune Parameters
| Immune Cell / Parameter | Observed Rhythm (Model) | Key Change | Potential Molecular Regulator |
|---|---|---|---|
| Dermal Dendritic Cell (DC) Migration | Peaks at ZT7 (day), trough at ZT19 (night) (Mouse) [9] | Increased infiltration into lymphatics during peak [9] | CCL21, LYVE-1, CD99, JAM-A (in LECs) [9] |
| Inflammatory Monocyte Recruitment | Stronger at ZT8 vs ZT0 (Mouse) [10] | Reduced bacterial spread, stronger inflammatory response [10] | BMAL1/CLOCK binding to Ccl2 promoter [10] |
| Neutrophil Aging & Egress | Rhythmic aging and clearance (Mouse/Human) [10] [13] | BMAL1 regulates CXCL2, driving CD62L/CXCR4-dependent aging [10] [13] | CXCL2/CXCR2 axis; CXCL12/CXCR4 axis [10] [13] |
| Circulating Leukocyte Count | Peaks during rest phase (Mouse: day, Human: night) [10] | Oscillating numbers in bloodstream [10] | Glucocorticoids, sympathetic nervous activity [10] [11] |
| IMMAX Immune Age Score | Generally stable, but decreases in morning types (Human) [11] | Score influenced by chronotype over the day [11] | Individual chronotype [11] |
Signaling Pathways in Circadian Immune Trafficking
The core molecular clock and its regulation of key immune trafficking pathways are summarized in the diagram below.
The Scientist's Toolkit
Table 2: Research Reagent Solutions for Circadian Trafficking Studies
| Reagent / Material | Function in Experiment | Example Application |
|---|---|---|
| Anti-LYVE-1 Antibody | Labels lymphatic endothelial vessels for visualization [9]. | Immunofluorescence staining of skin explants to identify lymphatics for DC migration quantification [9]. |
| Anti-CD11c Antibody | Identifies dendritic cells (DCs) [9]. | Staining to track and quantify DC location and migration into LYVE-1+ lymphatics [9]. |
| PER2::Luciferase Reporter | Visualizes and tracks the phase of the intrinsic molecular clock in live cells [9]. | Using BMDCs from PER2-Luc mice to synchronize clocks and test cell-autonomous migration capacity [9]. |
| Zeitgeber Time (ZT) Framework | Standardized experimental time reference based on the light-dark cycle [10]. | Reporting all procedures relative to light onset (ZT0) to ensure reproducibility and cross-study comparison [10] [9]. |
| Serum Shock (50% Serum) | Synchronizes desynchronized cellular clocks in in vitro cultures [9]. | Creating a population of BMDCs with aligned circadian phases to study cell-intrinsic migration rhythms [9]. |
Core Concepts: Understanding Diurnal Rhythms in Immune Function
This section addresses fundamental questions about the impact of daily biological rhythms on immune parameters relevant to experimental research.
FAQ 1: What is the biological basis for diurnal variation in immune function?
The diurnal variations in immune function are governed by the circadian clock, an evolutionarily conserved endogenous time-keeping system. This system operates through transcription-translation feedback loops in immune cells. The core mechanism involves the heterodimerization of the transcription factors CLOCK and BMAL1, which bind to E-box elements in the promoters of clock-controlled genes (CCGs), including their own repressors, Period (PER) and Cryptochrome (CRY). As PER and CRY proteins accumulate, they inhibit CLOCK-BMAL1 activity, eventually degrading to restart the cycle. This molecular oscillator directly regulates the expression of many immune genes, leading to rhythmic changes in immune cell trafficking, cytokine production, and effector functions [16] [17].
FAQ 2: Which key immune parameters exhibit significant diurnal variation that could confound my experimental results?
Multiple immune parameters oscillate over 24 hours. The table below summarizes key oscillating immune components based on recent research:
Table 1: Diurnal Variations in Key Immune Parameters
| Immune Parameter | Observed Diurnal Variation | Peak Time (Acrophase) | Experimental Model |
|---|---|---|---|
| Total White Blood Cells (WBCs) | Nocturnal acrophase [18] | Dark phase | Horse |
| Lymphocytes | Early morning acrophase [18] | Early morning | Horse |
| Neutrophils | Diurnal acrophase [18] | Light phase | Horse |
| CD4+ T Cells | Diurnal acrophase [18] | Light phase | Horse |
| CD8+ T Cells | Diurnal acrophase [18] | Light phase | Horse |
| Interleukin-6 (IL-6) | Early morning acrophase [18] | Early morning | Horse |
| Tumor Necrosis Factor-α (TNF-α) | Diurnal acrophase [18] | Light phase | Horse |
| Interleukin-1β (IL-1β) | Nocturnal acrophase [18] | Dark phase | Horse |
| Circulating T Cells (Human) | Higher percentage in afternoon [19] | 5:00 PM (17:00) | Human |
| Circulating B Cells (Human) | Higher percentage in afternoon [19] | 5:00 PM (17:00) | Human |
| Natural Killer (NK) Cells (Human) | Higher percentage in morning [19] | 8:00 AM | Human |
These rhythms are not merely observational; they are functionally significant. For instance, the response to an immune challenge like lipopolysaccharide (LPS) varies depending on the time of day it is administered, with the intensity of the inflammatory response being time-dependent [16] [17].
Troubleshooting Guides: Managing Diurnal Variation in Your Experiments
This section provides practical solutions to common problems arising from diurnal immune variation.
Problem 1: High Unexplained Variance in Immune Cell Counts and Cytokine Measurements
Potential Cause: Blood or tissue sampling performed at inconsistent times across experimental subjects or groups, capturing different phases of the immune circadian cycle.
Solution:
- Standardize Sampling Time: Conduct all terminal and non-terminal sampling within a strictly defined and narrow time window. Consistency is more critical than the specific time chosen.
- Time-Stamp All Samples: Record the precise time of collection for every sample to enable post-hoc analysis of temporal patterns if variance persists.
- Pilot Time-Course Studies: For critical endpoints, run a small pilot study with sampling at multiple times (e.g., 4-6 time points over 24 hours) to characterize the rhythm of your specific parameter in your model system [18].
Problem 2: Inconsistent Responses to Immune Challenge or Drug Administration
Potential Cause: The intervention is being applied at different circadian times, when the immune system's baseline state and responsiveness are fundamentally different.
Solution:
- Time Interventions Chronotherapeutically: Administer immune challenges, therapeutics, or vaccines at a fixed, documented time of day for all subjects in a cohort.
- Account for Animal Housing Light Cycles: Note that for nocturnal rodents, the "active phase" (dark period) is analogous to the human day. Always report Zeitgeber Time (ZT), where ZT0 is lights-on and ZT12 is lights-off.
- Consider Reverse-Translational Timing: If a treatment is known to be more effective in humans at a certain time of day, consider aligning the timing in animal models to the corresponding phase of the activity-rest cycle [20].
Problem 3: Difficulty Reproducing Published Phenomena Involving Inflammation or Infection
Potential Cause: The original study may have inadvertently been conducted at a time of peak immune susceptibility or resistance, while your replication attempt is not.
Solution:
- Contact the Corresponding Author: Inquire about the time of day key experiments were performed.
- Review Methods Carefully: Scrutinize the original paper's methods section for mentions of a standardized light-dark cycle and time of procedures.
- Systematically Test Timing: If reproduction fails, design an experiment to test the phenomenon across multiple time points (e.g., ZT2, ZT8, ZT14, ZT20) to identify a potential time-dependent effect [16] [17].
Experimental Protocols for Diurnal Immune Studies
Protocol 1: Assessing Diurnal Variation in Circulating Leukocyte Subpopulations
This protocol is adapted from studies in horses and humans, demonstrating conservation across species [18] [19].
Workflow Diagram: Diurnal Leukocyte Analysis
Materials:
- Research-Grade Flow Cytometer: For high-throughput, multi-parameter immunophenotyping.
- Antibody Panels: Specifically designed for identifying leukocyte subpopulations (e.g., anti-CD45 for total leukocytes, anti-CD3 for T cells, anti-CD4, anti-CD8, anti-CD19 for B cells, anti-CD56/16 for NK cells) [19].
- Microvette Tubes (K3 EDTA): For consistent finger-prick or venous blood collection.
- COSINOR Analysis Software: Specialized software or R packages (e.g., 'cosinor', 'circacompare') to statistically validate rhythms and determine acrophase (peak time) and robustness.
Procedure:
- Subject Acclimatization: House subjects under controlled light-dark (LD) conditions (e.g., 12h:12h) for a minimum of two weeks prior to experimentation to entrain circadian clocks.
- Sampling Schedule: Establish a 24-hour sampling schedule with collections at least every 4-6 hours. For mice, sample at ZT2, ZT6, ZT10, ZT14, ZT18, and ZT22 to cover both rest and active phases.
- Blood Collection: Collect blood via a consistent method (venipuncture, tail vein, or cardiac puncture at termination). For repeated sampling in larger animals or humans, an indwelling catheter can minimize stress.
- Cell Staining & Analysis: Process blood samples immediately. Use red blood cell lysis, followed by staining with fluorescently conjugated antibodies according to manufacturer protocols. Analyze using flow cytometry.
- Statistical Analysis: Use COSINOR or similar rhythmometric analyses to fit a cosine curve to the time-series data and determine if a significant rhythm is present.
Protocol 2: Measuring Diurnal Cytokine Production
This protocol outlines methods to track rhythmic cytokine secretion, a key effector function.
Workflow Diagram: Cytokine Rhythm Profiling
Materials:
- ELISA Kits or Multiplex Immunoassay Panels: For specific cytokines of interest (e.g., IL-6, TNF-α, IL-1β, IL-10). Multiplex panels are efficient for measuring multiple analytes simultaneously from a small sample volume [18] [21].
- Cell Stimulation Cocktails: Such as Lipopolysaccharide (LPS) for innate immune activation or PMA/Ionomycin for T cell activation.
- Microplate Reader: For quantifying ELISA results.
Procedure:
- In Vivo Cytokine Measurement: Collect plasma or serum at multiple time points across the 24-hour cycle. Store samples at -80°C until batch analysis to avoid inter-assay variability. Analyze all samples from a single subject in the same assay run.
- Ex Vivo Cytokine Production Capacity:
- Isolate primary immune cells (e.g., PBMCs, splenocytes, peritoneal macrophages) at different times of day.
- Culture a standardized number of cells with or without a potent stimulus like LPS for a defined period (e.g., 4-24 hours).
- Collect the cell culture supernatant and measure cytokine levels using ELISA or a multiplex assay.
- This method disentangles the intrinsic rhythmic capacity of cells to produce cytokines from the rhythmic systemic environment.
Table 2: Research Reagent Solutions for Diurnal Immune Studies
| Reagent/Resource | Function/Application | Key Considerations |
|---|---|---|
| Polychromatic Flow Cytometry Antibody Panels | Immunophenotyping of leukocyte subpopulations from small blood volumes (as low as 25µL) [19]. | Validate antibodies for your specific species. Panel design should minimize spectral overlap. |
| ELISA & Multiplex Bead-Based Assays | Quantification of cytokine concentrations in serum, plasma, and cell culture supernatants [18] [21]. | Multiplex assays conserve precious sample. Ensure dynamic range covers expected values. |
| COSINOR Analysis Software | Statistical package for identifying and characterizing circadian rhythms in time-series data [18]. | Available in R (cosinor2), Python, and dedicated Circadian software suites. |
| Telemetric Temperature Sensors | Continuous, stress-free monitoring of core body temperature as a robust marker of circadian phase [21]. | Validates that experimental manipulations do not disrupt overall circadian physiology. |
| REV-ERB Agonists (e.g., SR9009) / ROR Antagonists | Pharmacological tools to directly target and manipulate the molecular clockwork in vivo or in vitro [16] [20]. | Used to probe causal relationships between the clock and immune functions. |
| LPS (Lipopolysaccharide) | Standardized innate immune challenge to probe time-of-day-dependent inflammatory responses [16] [17]. | Dose and source (e.g., E. coli) must be consistent across all experiments. |
Troubleshooting Common Experimental Challenges
Table 1: Troubleshooting Guide for Diurnal Rhythm Experiments
| Problem Scenario | Potential Underlying Mechanism | Verification Method & Corrective Action |
|---|---|---|
| High variability in lymphocyte counts between samples taken at the same nominal time. | Poorly controlled intraindividual variation due to inconsistent participant sampling times or preparation [19]. | - Verification: Audit sample collection logs.- Corrective Action: Strictly enforce consistent sample collection times (e.g., 8 AM ±15 min) and standardize participant pre-test conditions (fasting, activity). |
| Failure to detect expected diurnal variation in immune cell populations. | - Weak zeitgeber intensity or consistency [22] [23].- Phase misalignment between competing zeitgebers (e.g., light vs. feeding) desynchronizing peripheral clocks [22]. | - Verification: Review participant logs for light exposure and meal timing.- Corrective Action: Implement controlled, time-restricted feeding protocols and instruct participants on consistent light/dark exposure. |
| Inconsistent results from low-volume blood sampling (e.g., finger-prick). | - Technical error in small-volume processing [19].- Local blood flow factors affecting cell concentration. | - Verification: Re-train personnel on the adapted, low-volume protocol [19].- Corrective Action: Apply warm water to fingertips before collection to standardize blood flow [19]. |
| Conflicting entrainment signals in in vitro or animal models. | Peripheral immune cell rhythms are entrained by feeding, not light, creating conflict if cues are misaligned [22]. | - Verification: Check the phase relationship between light/dark and feeding/fasting cycles in the model.- Corrective Action: Align feeding time with the active phase for the model organism to ensure zeitgeber synergy [22]. |
Frequently Asked Questions (FAQs)
Q1: Why is the timing of blood collection so critical in immune studies? The prevalence of circulating immune cells, such as T helper cells and B cells, demonstrates significant diurnal variation. For example, one study found TH cells and B cells showed significantly higher percentages at 5 PM compared to 8 AM [19]. Collecting samples at inconsistent times introduces substantial intraindividual variation, obscuring true biological signals or treatment effects.
Q2: Can I use small-volume blood collection methods, like finger-pricks, for diurnal variation research? Yes. Recent research demonstrates that diurnal variations in lymphocyte prevalence can be reliably detected using small-volume (e.g., 25 µL) finger-prick blood samples, which is a less invasive alternative to traditional venipuncture [19].
Q3: What is the most potent environmental cue for synchronizing the immune system? While light is the primary zeitgeber for the central clock in the brain, feeding/fasting cycles are a more potent synchronizer for peripheral clocks, including those in metabolic organs and likely immune cells [22] [23]. The timing of food intake can entrain these clocks independent of the light cycle.
Q4: What does "phase misalignment" mean, and why is it problematic? Phase misalignment occurs when two major zeitgebers, like the light/dark cycle and feeding/fasting cycle, are out of sync (e.g., eating late at night). This conflict sends conflicting signals to the body's circadian network, which can disrupt robust circadian oscillations in peripheral tissues, including metabolic and immune functions, and is linked to physiological abnormalities [22].
Q5: Which molecular pathways integrate metabolic state with circadian rhythmicity? The nutrient-sensing enzyme Sirtuin 1 (SIRT1) serves as a key integrator. Its activity is regulated by NAD+ levels, which oscillate with feeding rhythms. SIRT1, in turn, influences the core clock machinery (CLOCK/BMAL1 and PER/CRY complexes) through enzymatic activities, thereby translating metabolic state into circadian timing information in peripheral cells [22].
Experimental Protocols & Methodologies
Protocol: Assessing Diurnal Lymphocyte Variation via Low-Volume Blood Sampling
This protocol is adapted for detecting diurnal changes in lymphocyte subsets using finger-prick blood, minimizing participant burden for repeated sampling [19].
1. Participant Preparation & Sampling:
- Recruitment: Recruit healthy volunteers. (Note: The cited study used 8 participants aged 18-25 [19]).
- Sampling Times: Collect blood at two distinct time points on the same day (e.g., 8 AM and 5 PM) [19].
- Standardization: Do not require fasting, but standardize other factors like physical activity before sampling.
- Collection: Apply warm water to fingertips to increase blood flow and allow to dry. Collect a minimum of 225 µL of finger-prick blood using safety lancets into K3 EDTA Microvette tubes [19].
2. Staining & Preparation for Flow Cytometry:
- Reagents: Use a commercial lymphocyte kit (e.g., IMK Simultest: Lymphocyte Kit).
- Low-Volume Adaptation: Scale down reagent volumes to match the reduced blood volume. For a 25 µL blood sample, add 5 µL of the relevant antibody reagent [19].
- Incubation: Stain for 20 minutes at room temperature in the dark.
- Lysis: Lyse red blood cells using 500 µL of lysing solution for 10 minutes at room temperature.
- Wash: Centrifuge (200g, 4°C), discard supernatant, and wash the cell pellet with 500 µL of PBS. Repeat centrifugation and resuspend in an appropriate buffer (e.g., 125 µL of PBS with 2% FBS and 0.1% sodium azide) [19].
3. Flow Cytometry & Analysis:
- Equipment: Use a flow cytometer (e.g., BD FACSVerse).
- Gating Strategy: Analyze using flow cytometry software (e.g., FlowJo v10.8.1). The sequential gating strategy is:
- Lymphocyte Gate: On FSC-A/SSC-A plot.
- Live Cell Gate: Using a live/dead stain (e.g., propidium iodide) on FSC-A/PerCp-Cy5.5 plot.
- Singlet Gate: FSC-H/FSC-W and SSC-H/SSC-W to exclude doublets.
- Cell Subtype Analysis: Use FITC/PE quadrants to identify specific surface markers (CD3, CD19, CD4, CD8, CD16/CD56) for T cells, B cells, helper T cells, cytotoxic T cells, and NK cells [19].
- Statistics: Use a paired, two-tailed t-test to compare morning and afternoon cell prevalence, with a p-value of less than .05 considered significant [19].
Protocol Synopsis: Mathematical Modeling of Light-Feeding Entrainment
For theoretical research, a semimechanistic mathematical model can be employed to study the convoluted effects of light and feeding cues.
- Model Structure: A two-compartment model (central and peripheral) where the central compartment processes light/dark and feeding inputs. The peripheral compartment represents a human hepatocyte, containing the core clock machinery (CLOCK/BMAL1, PER/CRY feedback loops) and the NAD+ salvage pathway influencing SIRT1 activity [22].
- Key Inputs: The model simulates different light-feeding phase relations and intensities [22].
- Key Outputs: The model predicts dynamics of peripheral clock genes and metabolic enzymes, showing that peripheral clocks can entrain completely to feeding rhythms and that the light-feeding phase relationship is critical for robust oscillations [22].
Signaling Pathway & Experimental Workflow Visualizations
Signaling Pathway of Entrainment Cues on Peripheral Immunity
Low-Volume Blood Sampling Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Diurnal Immune Cell Research
| Item | Function & Application | Specific Example |
|---|---|---|
| Safety Lancets & Microvette Tubes | Enables consistent, low-volume blood collection via finger-prick, reducing participant burden and facilitating frequent sampling [19]. | Safety lancets; K3 EDTA 200 µL Microvette tubes (Sarstedt Group) [19]. |
| Polychromatic Flow Cytometry Kit | Allows for the simultaneous identification and quantification of multiple lymphocyte subsets from a single small sample. | IMK Simultest: Lymphocyte Kit (Becton Dickinson). Contains antibodies for CD3, CD19, CD4, CD8, CD16, CD56 [19]. |
| Flow Cytometer & Analysis Software | Instrument and software platform for acquiring and analyzing the stained cell samples to determine cell population percentages. | BD FACSVerse cytometer (Becton Dickinson) with FlowJo v10.8.1 software [19]. |
| Red Blood Cell Lysing Solution | Prepares whole blood for flow cytometry by removing red blood cells, which would otherwise interfere with the analysis of white blood cells. | 10x red blood cell lysing solution (e.g., BD Pharm Lyse) [19]. |
| Propidium Iodide (PI) | A fluorescent DNA dye used as a viability stain. PI is excluded by live cells with intact membranes; thus, PI-positive cells are dead and can be gated out. | Propidium iodide solution [19]. |
A critical, yet often overlooked, variable in biomedical research is the fundamental discrepancy between the nocturnal nature of common laboratory rodents and the diurnal nature of human physiology. This discordance can significantly impact the interpretation and translation of research findings, particularly in immunology and physiology. Research indicates that failing to account for this can hamper reproducibility, reliability, and validity in experimental data [24] [25]. This guide provides troubleshooting advice and protocols to help researchers manage intraindividual variation and effectively navigate the challenges of translating data from nocturnal mice to diurnal humans.
Troubleshooting Common Circadian Translation Issues
FAQ 1: Why does the time of day for testing rodents matter if my lab operates on a standard 9-to-5 schedule?
Testing nocturnal animals during the day (their rest phase) is akin to waking a human in the middle of the night to perform a complex task. Physiological parameters, including immune responses, core body temperature, and hormone levels, exhibit strong daily fluctuations [21] [25]. Conducting tests during the animal's inactive phase may not capture their peak functional capacity and can introduce significant variability, potentially leading to a "floor effect" where true biological differences are masked [25].
FAQ 2: How can I account for circadian rhythms without running my experiments at night?
The most effective method is to reverse the light/dark (LD) cycle of your animal housing facility. House the animals in total darkness during the day and turn on the lights at night. This allows researchers to observe and test the animals during their active phase under simulated "nighttime" conditions during standard work hours [24]. When animals need to be checked during the subjective night, use dim red lighting, as rodents cannot see red light, which prevents disruption of their circadian rhythms [24].
FAQ 3: Our immune cell counts are highly variable between replicates. Could time of day be a factor?
Yes, absolutely. Numerous immune cell populations and inflammatory markers display robust circadian rhythms. For example, in humans, total white blood cells (WBC), neutrophils, and lymphocytes show higher circulating numbers in the afternoon compared to the morning [21]. Similar rhythms are present in rodents but are phase-shifted due to their nocturnal nature. Consistent timing for sample collection is crucial for reducing this source of intraindividual variability.
FAQ 4: We are developing a drug targeting an inflammatory pathway. How relevant is circadian timing for therapy?
Circadian rhythms regulate the core inflammatory machinery, including cytokine secretion and immune cell trafficking [15] [20]. The severity of inflammatory diseases like rheumatoid arthritis often follows a daily pattern, with symptoms like morning stiffness linked to elevated nighttime levels of pro-inflammatory factors [15]. Therefore, administering therapeutics in a time-sensitive manner (chronotherapy) can optimize efficacy and minimize side effects [15].
Key Experimental Protocols & Methodologies
Protocol for Assessing Immune Cell Diurnal Variation
The following protocol, adapted from a 2023 study, demonstrates how to detect diurnal variations in lymphocyte prevalence using small-volume blood samples, relevant for both rodent and human studies [19].
- Objective: To determine diurnal variations in peripheral lymphocyte prevalence.
- Sample Collection:
- Subjects: 8 healthy volunteers (or rodents, with appropriate ethical approval).
- Timing: Collect samples at two distinct time points (e.g., 8 AM and 5 PM).
- Volume & Method: Collect a minimum of 225 µL of finger-prick blood (for humans) or tail-nick blood (for rodents) into K3 EDTA tubes.
- Staining & Analysis:
- Use a polychromatic flow cytometry kit (e.g., IMK Simultest: Lymphocyte Kit).
- Adapt reagent volumes for low blood volume (e.g., 25 µL blood + 5 µL reagent).
- Stain with conjugate antibodies for 20 minutes at room temperature.
- Lyse red blood cells for 10 minutes at room temperature.
- Wash with PBS, centrifuge, and resuspend the pellet for analysis.
- Data Acquisition: Analyze samples on a flow cytometer (e.g., BD FACSVerse).
- Use forward scatter/side scatter to gate on lymphocytes.
- Use live/dead cell staining and singlet gating to ensure analysis of viable, single cells.
- Statistical Analysis: Use a paired Student's two-tailed t-test to compare lymphocyte counts between morning and afternoon samples. A p-value of less than .05 is considered significant [19].
Protocol for Reversed Light/Dark Cycle Housing
Implementing this protocol is fundamental for ensuring rodent data is collected during the appropriate biological time.
- Objective: To house nocturnal rodents on a reversed LD cycle to facilitate daytime testing during their active phase.
- Housing Conditions:
- Maintain the animal room in complete darkness during the human daytime (e.g., 7 AM to 7 PM).
- Switch on the lights during the human nighttime (e.g., 7 PM to 7 AM).
- Procedural Lighting:
- All procedures conducted during the dark (active) phase must be performed under safe lighting.
- Use a miner's light with a red bulb or night-vision goggles when working in the animal room during the subjective night [24].
- Tint room windows with a red film to prevent external light leaks.
- Acclimatization: Allow animals to acclimate to the reversed LD cycle for a minimum of two weeks before initiating any experiments.
- Reporting: When publishing, provide a detailed description of the LD cycle and all measures taken to protect the animals' circadian rhythms during testing [24] [25].
Circadian Regulation of Immunity: Key Data and Pathways
Diurnal Variation in Human Immune Cells and Markers
The table below summarizes the diurnal variations observed in key immune parameters in humans, highlighting the importance of consistent timing for sample collection [21].
| Immune Parameter | Direction of Change | Peak Time (Example) | Notes / Context |
|---|---|---|---|
| Core Body Temperature | Increase | Afternoon (18:00 hs) | More pronounced response to exercise in the morning. |
| Total White Blood Cells (WBC) | Increase | Afternoon (18:00 hs) | Significantly higher concentration post-exercise in the evening. |
| Neutrophils | Increase | Afternoon (18:00 hs) | Higher concentration post-exercise in the evening. |
| Lymphocytes | Increase | Afternoon (18:00 hs) | Higher concentration post-exercise in the evening. |
| IL-6 | Phase response | More pronounced at 18:00 hs | Inflammatory cytokine shows a more pronounced response to stress in the evening. |
| HSP70 | Phase response | More pronounced at 18:00 hs | Heat shock protein response is more pronounced in the evening. |
| TH Cells, B Cells | Increase | Evening (vs. Morning) | Significantly higher percentages found at 5 PM [19]. |
| NK Cells | Decrease | Evening (vs. Morning) | Significantly higher percentage in the morning [19]. |
| Cortisol | Fluctuation | Peaks around 8 AM | Levels rise in the early morning and have a nadir around noon [15]. |
Core Circadian Clock Signaling Pathway
The following diagram illustrates the core transcriptional-translational feedback loop of the mammalian circadian clock, which governs daily rhythms in physiology and immunity [26] [15] [20].
Circadian-Immune System Crosstalk
This diagram outlines the pathway by which environmental light synchronizes the central clock, which in turn regulates rhythmic immune functions, a key consideration for translational research [26] [15] [20].
The Scientist's Toolkit: Key Research Reagents & Materials
The table below lists essential reagents and materials used in the featured protocols for circadian immune research.
| Item Name | Function / Specificity | Example Use Case |
|---|---|---|
| Polychromatic Flow Cytometry Kit (e.g., IMK Simultest) | Simultaneous detection of multiple lymphocyte subsets (T, B, NK cells) via conjugated antibodies [19]. | Phenotyping immune cell subsets in small-volume blood samples over the diurnal cycle [19]. |
| Safety Lancets & Microvette Tubes (K3 EDTA) | Minimally invasive collection of small, precise volumes of peripheral blood. | Repeated sampling from the same subject (e.g., finger-prick in humans) at multiple time points to track diurnal variation [19]. |
| Telemetric Temperature Sensors | Continuous, remote monitoring of core body temperature (e.g., gastrointestinal). | Tracking the circadian rhythm of core body temperature as a physiological marker in unrestrained animals or humans [21]. |
| Red Light Bulbs / Miner's Lights | Provides illumination that is invisible to rodents, preventing circadian rhythm disruption. | Performing animal husbandry, health checks, or experimental procedures during the dark/active phase of a reversed LD cycle [24]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Quantitative measurement of specific proteins (e.g., cytokines, hormones). | Assessing diurnal levels of inflammatory markers like IL-6 or hormones like melatonin or cortisol in serum/plasma [21]. |
| Reverse Light/Dark Cycle Chamber | Environmental chamber programmed to provide a reversed 12h:12h light/dark cycle. | Housing nocturnal rodents to shift their active phase to coincide with researcher working hours for behavioral and physiological tests [24] [25]. |
Implementing Chrono-Methodologies: Practical Frameworks for Temporal Study Design
In immune studies, the biological clock is a fundamental but often overlooked variable. A growing body of evidence reveals that immune cell populations and their functions exhibit significant diurnal fluctuations. For researchers in immunology and drug development, failing to standardize sampling times introduces substantial pre-analytical variability that can obscure true experimental effects, compromise data reproducibility, and lead to erroneous conclusions. This technical support resource provides evidence-based protocols and troubleshooting guidance for managing intraindividual variation driven by circadian rhythms, enabling more robust and reliable immune monitoring in research and clinical applications.
FAQs: Addressing Key Concerns in Diurnal Immune Research
1. Why is standardizing sampling time particularly critical for immune cell analysis?
Circulating immune cell populations demonstrate predictable diurnal variations. For instance, T-helper (TH) cells and B cells show significantly higher percentages in the afternoon (e.g., 5 PM) compared to morning samples (e.g., 8 AM), whereas Natural Killer (NK) cells demonstrate a significantly higher morning prevalence [19]. These endogenous rhythms mean that sampling at inconsistent times of day confounds experimental results by introducing systematic biological noise that is unrelated to the experimental intervention or condition being studied.
2. Can I use small-volume blood samples, like finger-prick collections, to reliably study these diurnal variations?
Yes, recent research confirms that small-volume finger-prick blood samples (e.g., 25 µL) are sufficient to detect significant diurnal variations in lymphocyte subsets using modern analytical platforms like flow cytometry [19]. This validates a less invasive sampling method that can improve participant acceptability and facilitate more frequent time-point collections in longitudinal studies.
3. Beyond immune cells, what other pre-analytical factors should I control for in my study design?
The pre-analytical phase encompasses all steps from sample collection to analysis, each being a potential source of variability. Key factors include [27]:
- Circadian Rhythm and Nutritional Status: Metabolite levels and physiological states fluctuate with time of day and food intake.
- Sample Collection Materials: Additives in collection tubes (e.g., anticoagulants like EDTA, heparin, or citrate) and components like separator gels can leach chemicals and alter metabolomic and lipidomic profiles.
- Sample Processing and Storage: Variations in clotting time (for serum), centrifugation speed, temperature, freeze-thaw cycles, and storage duration can significantly impact analyte stability.
Consistent standardization of these factors across all samples is paramount for data integrity.
Troubleshooting Guide: Common Issues and Solutions
| Problem | Possible Source | Recommended Test or Action |
|---|---|---|
| High Background Noise | Insufficient washing steps during assay procedures. | Increase number of washes; add a 30-second soak step between washes [28]. |
| Poor Duplicates (High variability between technical replicates) | Insufficient or uneven washing; uneven plate coating; reused plate sealers. | Check automatic plate washer ports for obstructions; ensure consistent coating volumes and methods; use fresh plate sealers for each step [28]. |
| Poor Assay-to-Assay Reproducibility | Variations in incubation temperature or protocol; improper calculation of standard curves. | Adhere strictly to recommended incubation temperatures and a consistent protocol; check calculations and use internal controls [28]. |
| Inconsistent Diurnal Data | Non-standardized sampling times; unaccounted for participant activities (meals, exercise). | Collect all samples within a narrow, consistent time window for each participant; record and control for fasting status and physical activity [27] [19]. |
| Unexpected Immune Cell Counts | Contamination of samples; incorrect handling or delays in processing. | Use fresh reagents and buffers; ensure samples are processed immediately according to a standardized protocol [27] [28]. |
Experimental Protocols: A Methodology for Diurnal Variation Assessment
The following protocol, adapted from contemporary research, demonstrates a methodology for detecting diurnal lymphocyte variation using small-volume blood samples [19].
Objective
To assess diurnal variations in peripheral lymphocyte prevalence using finger-prick blood samples and flow cytometry.
Materials and Reagents
- Safety lancets
- K3 EDTA Microvette tubes (e.g., Sarstedt Group)
- Polychromatic antibody kit for lymphocyte immunophenotyping (e.g., IMK Simultest: Lymphocyte Kit)
- Phosphate Buffered Saline (PBS)
- Red blood cell lysing solution
- Flow cytometer with appropriate configuration
Step-by-Step Procedure
- Participant Preparation and Sampling: Recruit participants and obtain informed consent. Collect a minimum of 225 µL of finger-prick blood using safety lancets into K3 EDTA tubes at two distinct time points (e.g., 8 AM and 5 PM) on the same day. Apply warm water to fingertips to increase blood flow prior to collection.
- Staining: Pipette 25 µL of blood into a test tube. Add 5 µL of the appropriate antibody reagent (volumes may be scaled down from manufacturer's instructions). Mix gently and incubate for 20 minutes at room temperature, protected from light.
- Lysis and Washing: Add 500 µL of 10x red blood cell lysing solution to the tube. Vortex and incubate for 10 minutes at room temperature. Centrifuge at 200g for 5 minutes at 4°C and carefully discard the supernatant. Wash the cell pellet with 500 µL of PBS, centrifuge again, and discard the supernatant.
- Resuspension and Analysis: Resuspend the final cell pellet in an appropriate stabilization buffer (e.g., 125 µL of PBS with 2% FBS). Analyze the samples immediately on a flow cytometer.
- Data Analysis: Use flow cytometry analysis software (e.g., FlowJo) for gating and compensation. Identify lymphocyte populations via forward-scatter/side-scatter gating, followed by live/dead cell and singlet gating. Use fluorescence parameters to distinguish specific cell types (T cells, B cells, NK cells, etc.). Employ paired statistical tests (e.g., paired two-tailed t-test) to compare cell prevalence between morning and afternoon samples.
Workflow Visualization
Diagram: Pre-analytical Workflow for Immune Cell Diurnal Studies
Diagram: Circadian-Immune Signaling Pathway
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function & Rationale |
|---|---|
| K3 EDTA Microvette Tubes | For consistent and precise collection of small-volume finger-prick blood samples; EDTA prevents coagulation by chelating calcium [19]. |
| Polychromatic Antibody Panels | Pre-configured antibody kits for immunophenotyping (e.g., identifying T cells, B cells, NK cells) via flow cytometry, enabling comprehensive immune profiling from small samples [19]. |
| Safety Lancets | Enable standardized, minimally invasive capillary blood collection from fingertips, improving participant comfort and facilitating repeated sampling [19]. |
| Red Blood Cell (RBC) Lysing Solution | Lyses red blood cells in whole blood samples without damaging white blood cells (lymphocytes, monocytes, granulocytes), which is a critical sample preparation step for flow cytometric analysis of immune cells [19]. |
| Standardized Collection Tubes | Using the same type and manufacturer of blood collection tubes for an entire study is crucial, as tube additives (e.g., heparin, EDTA, citrate) and separator gels can leach chemicals and variably affect subsequent analytical results [27]. |
Chronovaccination is an emerging field that investigates how the timing of vaccine administration, in alignment with the body's innate 24-hour circadian rhythms, can be used to optimize immunogenicity and effectiveness. This approach represents a low-risk, cost-effective strategy to enhance vaccine-induced protection, which is particularly relevant for higher-risk populations, such as the elderly, who often develop less robust immune responses. This technical support center provides a foundational framework for researchers designing and troubleshooting experiments in this field, with a focus on managing the intraindividual variation inherent in diurnal rhythms research.
FAQs: Core Concepts in Chronovaccination
1. What is the fundamental premise behind chronovaccination? The immune system exhibits strong circadian rhythms, with oscillations observed in cytokine responses, circulating leukocyte counts, and the activity of both innate and adaptive immune cells. These rhythms are controlled by cell-intrinsic circadian clocks. The core premise of chronovaccination is that aligning the time of vaccine administration with peaks in immune cell function and trafficking can enhance the subsequent immune response [29] [30].
2. What is the clinical evidence supporting time-of-day effects on vaccine efficacy? A 2025 systematic review and meta-analysis identified 17 studies investigating vaccination timing for COVID-19, influenza, hepatitis B, hepatitis A, and pneumococcal infection. Eleven of these studies demonstrated statistically significant effects of timing on antibody response, with 10 reporting stronger responses after morning vaccination. The meta-analysis of randomized controlled trials (RCTs) confirmed that morning influenza vaccination elicited a significantly stronger antibody response than afternoon vaccination, with a larger effect size observed in adults aged 65 and older [29] [31].
3. Which populations show the most pronounced benefit from morning vaccination? Current evidence suggests that older adults (aged 60 and above) derive the most consistent benefit from morning vaccination. In the systematic review, five out of six subgroups with an average age of 60+ showed significantly stronger antibody responses following morning vaccination [29]. The effect appears to be more variable and less pronounced in younger populations [31].
4. Are time-of-day effects consistent across all vaccine types? While the principle may be universal, the magnitude of the effect appears to vary. The most robust evidence from RCTs currently exists for influenza and COVID-19 vaccines, as well as the Bacillus Calmette-Guérin (BCG) vaccine. For instance, one study found that morning BCG vaccination led to stronger antigen-specific IFN-γ production and trained innate immunity compared to evening vaccination [30]. More research is needed to characterize effects across a wider range of vaccine platforms.
Troubleshooting Guide: Common Experimental Challenges
Issue 1: Inconsistent or Non-Significant Time-of-Day Effects in Study Data
- Potential Cause: Inadequate control for confounding variables that interact with circadian rhythms, such as participant age, sex, or chronotype (an individual's natural inclination for morning or evening activity).
- Solutions:
- Stratify Recruitment and Randomization: Ensure age and sex are evenly distributed between your morning and afternoon vaccination groups. Consider using chronotype questionnaires to account for this variable.
- Standardize Sample Collection: If collecting longitudinal blood samples for immune monitoring, strictly standardize the time of day for each draw for all participants to avoid confounding by diurnal immune variation.
- Refer to Existing Data: Consult the summary tables below to benchmark your effect sizes against published findings. A lack of effect in a young cohort may be an expected finding.
Issue 2: High Variability in Immune Readouts Within Time Groups
- Potential Cause: High intraindividual variation driven by unmeasured lifestyle factors or imprecise laboratory protocols.
- Solutions:
- Control Pre-Vaccination Activity: Where possible, advise participants to avoid strenuous exercise, significant sleep deprivation, or alcohol consumption in the 24 hours preceding vaccination, as these can independently modulate immune function.
- Standardize Laboratory Assays: Use controlled, validated protocols for processing blood samples and conducting immunoassays. Evidence shows that even small-volume finger-prick blood samples can reliably detect diurnal variations in lymphocyte subsets, offering a less invasive method for repeated measures [19].
Issue 3: Determining the Optimal "Morning" and "Afternoon" Time Windows
- Guidance: Based on successful RCTs, a common and methodologically sound approach is to define "morning" as 9:00 AM – 11:00 AM and "afternoon" as 3:00 PM – 5:00 PM [29] [30]. Adhering to these defined windows, rather than a broad "AM/PM" classification, improves experimental consistency and the ability to compare results across studies.
The following tables consolidate key quantitative findings from recent meta-analyses and studies for easy reference.
Table 1: Summary of Time-of-Day Effects on Antibody Response from a 2025 Systematic Review & Meta-Analysis [29] [31]
| Vaccine Type | Number of Studies | Studies Showing Significant Effect | Direction of Significant Effect | Key Subgroup Findings |
|---|---|---|---|---|
| Influenza | 5 | 2 out of 2 RCTs | Morning > Afternoon | Effect strongest in adults ≥65 years. |
| COVID-19 | 9 | Multiple observational studies | Morning > Afternoon | Improved B-cell and Tfh responses with morning vaccination. |
| Others (Hep A/B, Pneumo) | 3 | Varied | Primarily Morning > Afternoon | More data required for conclusive patterns. |
Table 2: Meta-Analysis Results for Influenza Vaccination by Age Group [29] [31]
| Age Group | Standardized Mean Difference (SMD) | 95% Confidence Interval | Statistical Significance |
|---|---|---|---|
| All Ages | 0.24 | 0.01 – 0.47 | p < 0.05 |
| Adults ≥65 years | 0.32 | 0.21 – 0.43 | p < 0.001 |
| Adults ≤60 years | 0.00 | -0.17 – 0.17 | Not Significant |
Experimental Protocols
Protocol 1: Randomized Controlled Trial for Chronovaccination
This protocol is adapted from the RCTs conducted by Long et al. (2016) and Liu et al. (2022) [29].
- 1. Participant Recruitment:
- Target Population: Define your cohort (e.g., healthy adults ≥65 years). Exclusion Criteria: Immunocompromised state, recent infections, use of immunosuppressant drugs, unstable sleep-wake cycles.
- Stratification: Stratify by sex and age to ensure balanced allocation.
- 2. Randomization & Blinding:
- Randomly assign participants to morning (9:00-11:00) or afternoon (15:00-17:00) vaccination groups. The vaccinator should be blinded to the group assignment where possible.
- 3. Vaccination:
- Administer the standard vaccine (e.g., inactivated influenza vaccine) according to the assigned time window.
- 4. Sample Collection for Immune Monitoring:
- Collect blood samples at baseline (pre-vaccination) and at defined endpoints post-vaccination (e.g., 4 weeks for antibody titers).
- Crucially, all follow-up samples for a given participant should be drawn at the same time of day as their vaccination to control for diurnal variation in immune markers.
- 5. Outcome Measures:
- Primary: Antigen-specific IgG antibody titers, measured via ELISA.
- Secondary: Seroconversion rates, T-cell responses (e.g., ELISpot for IFN-γ), and innate immune parameters.
The workflow for this experimental design is outlined below.
Protocol 2: Assessing Diurnal Immune Variation in Human Blood
This protocol details a method for detecting diurnal changes in lymphocyte populations, adapted from a 2023 study that validated the use of small-volume blood samples [19].
- 1. Participant Preparation:
- Recruit healthy volunteers. Standardize the day prior to sampling (avoid strenuous exercise, alcohol).
- 2. Serial Blood Sampling:
- Collect blood samples at two or more time points (e.g., 8:00 AM and 5:00 PM) on the same day.
- Sample Type: Venous blood or finger-prick blood (≥225 µL collected into K3 EDTA tubes).
- 3. Cell Staining & Flow Cytometry:
- Lysing: Use red blood cell lysing solution.
- Staining: Stain with antibody panels for major lymphocyte subsets:
- T Helper Cells: CD3+, CD4+
- Cytotoxic T Cells: CD3+, CD8+
- B Cells: CD19+
- NK Cells: CD3-, CD16+/CD56+
- Analysis: Run samples on a flow cytometer and analyze using software like FlowJo.
- 4. Expected Results:
- As demonstrated, you should detect significant diurnal variation, such as higher percentages of T-helper and B cells at 5:00 PM and a higher percentage of NK cells in the morning [19].
Circadian Immune Signaling Pathways
The following diagram summarizes the proposed mechanistic pathways linking the central circadian clock to rhythmic immune function and vaccine response.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Chronovaccination and Diurnal Immune Research
| Item | Function / Application | Example / Specification |
|---|---|---|
| Polychromatic Flow Cytometry Panels | Immunophenotyping of rhythmic lymphocyte subsets (T, B, NK cells) and activation markers. | Antibodies against CD3, CD4, CD8, CD19, CD16/56, CD45RA/RO [19]. |
| ELISA Kits | Quantification of antigen-specific antibody titers (IgG, IgM) in serum post-vaccination. | Virus-specific (e.g., Influenza HA, SARS-CoV-2 Spike) kits. |
| ELISpot Kits | Measurement of antigen-specific T-cell responses (e.g., IFN-γ production). | Critical for assessing cellular immune memory. |
| Circadian/Diarunal Study Design Tools | Managing participant scheduling and sample tracking for time-point experiments. | Defined time windows (e.g., 9-11 AM, 3-5 PM); electronic scheduling systems [29] [30]. |
| Small-Volume Blood Collection Systems | Enables frequent, less invasive sampling for dense diurnal kinetics, especially in vulnerable populations. | Finger-prick lancets and micro-containers (e.g., 200µL Microvette tubes) [19]. |
| Validated Temperature Monitoring | Ensuring vaccine potency is not confounded by improper storage, a critical control. | Digital data loggers with continuous monitoring and alert functions [32]. |
Chrono-immunotherapy is the practice of aligning the administration of immune-based cancer treatments with a patient's internal biological clock, or circadian rhythm. This approach aims to enhance treatment efficacy and reduce side effects by leveraging the fact that the immune system's activity, including the ability of killer T-cells to infiltrate tumors, fluctuates predictably over a 24-hour period [33] [34]. The central pacemaker, the suprachiasmatic nucleus (SCN) in the hypothalamus, coordinates these rhythms throughout the body, regulating everything from sleep-wake cycles and hormone secretion (like cortisol) to immune function [34]. Disruption of these rhythms is linked to worse cancer outcomes, while aligning treatment with circadian biology shows promise for improving patient survival [33] [35].
Frequently Asked Questions (FAQs)
Q1: What is the core scientific evidence supporting time-of-day administration for immune checkpoint inhibitors (ICIs)?
Large-scale retrospective clinical studies have consistently shown that patients receiving ICIs earlier in the day experience significantly improved outcomes, including longer progression-free survival (PFS) and overall survival (OS), across multiple cancer types [34]. Mechanistically, this is supported by the circadian regulation of the immune system. Research has revealed that lymphocytes, the professional killer cells activated by immunotherapy, enter and exit tumors in a circadian fashion, with greater infiltration into the tumor occurring in the morning hours [33]. Animal studies confirm that treatment at the start of the active phase elicits a stronger anti-tumor immune response, an effect that is abolished in animals lacking a circadian clock [34].
Q2: How do I account for individual differences in circadian timing among patients?
A patient's innate timing preference, or chronotype, is a crucial factor. A "one-size-fits-all" approach using wall-clock time may be insufficient because individuals have different internal biological times [34]. Chronotype can be assessed using:
- Validated Questionnaires: Such as the Morningness-Eveningness Questionnaire (MEQ) or the Munich Chronotype Questionnaire (MCTQ) [34].
- Wearable Biosensors: Devices that continuously monitor locomotor activity, body temperature, or heart rate can provide objective phase markers of the circadian clock [34].
- Biomolecular Snapshot Methods: Emerging tests like TimeTeller can estimate an individual's circadian phase from a single or limited number of biosamples (e.g., blood, saliva) by analyzing the circadian transcriptome, proteome, or metabolome [34].
Q3: What are the major practical challenges in implementing a circadian-enabled clinical trial?
| Challenge | Description | Potential Mitigation Strategy |
|---|---|---|
| Scheduling | Fitting all patient infusions into a limited morning time window creates logistical bottlenecks [33]. | Explore decentralized administration (e.g., at-home infusion) where safe and feasible [33]. |
| Chronotype Assessment | Integrating individual circadian phase measurement into busy clinical workflows [34]. | Use low-burden methods like validated questionnaires or wearable devices [34]. |
| Standardization | Lack of standardized protocols for measuring circadian rhythms (e.g., cortisol, actigraphy) in clinical cancer settings [35]. | Pre-define and validate measurement protocols in the trial's statistical analysis plan. |
| Prospective Data | Much current evidence is retrospective, which is susceptible to bias [34]. | Design prospective, randomized controlled trials that specifically test timing as an intervention [34]. |
Q4: Can we manipulate the circadian clock to make afternoon treatments more effective?
Yes, this is an active area of research. Potential strategies include:
- Pharmacological Resetting: Investigating drugs that can mimic the daily resetting of the central clock [33].
- Time-Restricted Eating (TRE): Controlling meal times is a powerful non-photic cue that can entrain peripheral clocks. Animal studies show that time-restricted feeding can lower cancer incidence and slow tumor growth [33]. Clinical studies are ongoing to see if TRE improves outcomes for cancer therapies in people [33].
Troubleshooting Common Experimental Issues
Issue 1: High Inter-Patient Variability in Treatment Response
- Potential Cause: Ignoring patient chronotype, leading to treatment at a suboptimal biological time for "evening-type" individuals [34].
- Solution: Stratify patients by chronotype in the trial design and align ICI administration time accordingly. For example, "larks" (morning-types) may receive treatment in the morning, while "owls" (evening-types) may receive it later in the day [34].
Issue 2: Inability to Detect a Significant Time-of-Day Effect
- Potential Cause: Using a fixed "morning" vs "afternoon" window for all patients without accounting for individual circadian phase, diluting the effect [34].
- Solution: Incorporate an objective measure of internal biological time (e.g., from wearables or a biomolecular test) to define treatment windows based on a patient's unique circadian phase rather than the wall clock [34].
Issue 3: Participant Burden in Circadian Rhythm Assessment
- Potential Cause: Requiring frequent sample collection (e.g., for melatonin or cortisol) over multiple days can lead to poor compliance [35] [36].
- Solution: Leverage less invasive and simpler methods, such as saliva sampling for gene expression analysis [36], using wearable activity sensors [34], or employing single-sample biomarker algorithms to estimate circadian phase [34].
Table 1: Observed Time-of-Day Effects in Cancer Therapy
| Therapy / Intervention | Optimal Timing | Observed Effect | Key Supporting Evidence |
|---|---|---|---|
| Immunotherapy (ICIs) | Morning | Improved progression-free and overall survival [33] [34] | Large-scale retrospective clinical studies [34] |
| Radiation Therapy | Morning | Fewer side effects compared to afternoon administration [33] | Clinical observation [33] |
| Chemotherapy | Varies by drug | Improved efficacy and/or reduced toxicity at specific times [33] | Multiple clinical studies [33] |
| Low-Dose Aspirin | Evening | Greater blood pressure reduction [33] | Clinical trials [33] |
| Statins | Night | Highest effectiveness as target enzyme levels peak at night [33] | Clinical trials [33] |
Table 2: Methods for Assessing Circadian Timing in Clinical Trials
| Method | What It Measures | Pros | Cons | Gold Standard Comparison |
|---|---|---|---|---|
| Dim Light Melatonin Onset (DLMO) | Phase of central clock via melatonin secretion | High accuracy | Logistically challenging, requires controlled dim light | Gold Standard itself |
| Core Body Temperature (CBT) | Rhythm of core body temperature | Objective | Affected by activity, food, and sleep | Correlates with DLMO |
| Saliva Gene Expression (e.g., ARNTL1, PER2) | Phase of peripheral clock in oral mucosa | Non-invasive, suitable for home collection [36] | Requires specialized RNA analysis | Correlates with cortisol acrophase and bedtime [36] |
| Wearable Devices (Actigraphy) | Rest-activity cycles | Continuous, real-world data, low patient burden [34] | A proxy measure, not a direct molecular rhythm | Validated against sleep logs and other markers |
| Chronotype Questionnaires (MEQ, MCTQ) | Self-reported diurnal preference | Very low cost, easy to administer [34] | Subjective, does not measure current physiological state | Correlates with DLMO in healthy populations [34] |
Detailed Experimental Protocols
Protocol 1: Assessing Circadian Phase via Saliva Sampling and Gene Expression
This protocol is adapted from recent research demonstrating the feasibility of using saliva for robust circadian rhythm analysis [36].
1. Participant Preparation and Sampling:
- Instruct participants to collect unstimulated whole saliva at 3-4 predefined time points (e.g., 8:00, 14:00, 20:00) over 2 consecutive days.
- Use collection kits containing RNA stabilizer (e.g., RNAprotect). A 1:1 ratio of saliva to stabilizer with a 1.5 mL sample volume has been shown to provide optimal RNA yield and quality [36].
- Samples should be stored at -80°C immediately after collection until RNA extraction.
2. RNA Extraction and Analysis:
- Extract total RNA from saliva samples using a standardized commercial kit suitable for saliva.
- Analyze the expression of core clock genes (e.g., ARNTL1, NR1D1, PER2, PER3) via reverse transcription-quantitative polymerase chain reaction (RT-qPCR). These genes have shown robust, detectable circadian rhythms in saliva and oral mucosa [36].
- Generate circadian phase maps (e.g., acrophase - the time of peak expression) for each participant from the gene expression time series.
3. Data Integration:
- Correlate gene expression acrophases with other circadian markers, such as cortisol levels from the same saliva samples or bedtimes recorded by participants [36]. This validates the molecular data against established rhythms.
Protocol 2: Implementing a Chronotype-Informed Dosing Schedule
1. Chronotype Stratification:
- At trial enrollment, have participants complete the Munich Chronotype Questionnaire (MCTQ) to determine their chronotype (Morning type, Intermediate, Evening type) [34].
- Randomization should stratify patients based on chronotype to ensure balanced groups.
2. Treatment Administration:
- Morning-type ("Larks") and Intermediate-type patients are scheduled to receive their ICI infusions in the morning (e.g., between 08:00 and 11:00).
- Evening-type ("Owls") patients are scheduled to receive their ICI infusions in the late morning or afternoon (e.g., between 11:00 and 14:00). This model is inspired by the successful outcomes of the Treatment in Morning versus Evening (TIME) trial for hypertension [34].
3. Monitoring and Adherence:
- Use clinic logs to strictly record infusion start times.
- Consider using wearable activity trackers throughout the trial to monitor for shifts in rest-activity cycles that might indicate changes in circadian phase [34].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Circadian Clinical Research
| Item / Reagent | Function in Chronotherapy Research | Example Application |
|---|---|---|
| Saliva RNA Collection Kit | Non-invasive collection and stabilization of RNA from saliva for gene expression analysis [36]. | Measuring daily rhythms of core clock genes (e.g., PER2, ARNTL1) in participants [36]. |
| Validated Chronotype Questionnaire (e.g., MCTQ) | Assessing an individual's innate diurnal preference for activity and rest as a proxy for circadian phase [34]. | Stratifying patients in a clinical trial into morning, intermediate, and evening chronotype groups for personalized dosing [34]. |
| Wearable Activity Monitor (Actigraph) | Continuously monitoring rest-activity cycles to objectively characterize a participant's circadian rhythm in their home environment [34]. | Providing a longitudinal proxy measure of circadian stability and sleep-wake patterns during a therapy cycle [34]. |
| Cortisol ELISA Kit | Quantifying cortisol levels in saliva or serum; cortisol is a key circadian hormone with a robust morning peak [35] [36]. | Validating the phase of the central circadian clock and investigating HPA axis dysfunction in cancer patients [35]. |
| TimeTeller or similar algorithm | A computational tool that estimates circadian phase and rhythm disruption from a single or limited number of biosamples using transcriptomic or metabolomic data [34]. | Determining a patient's internal biological time from a single blood draw, reducing the burden of full time-series sampling [34]. |
Visual Workflows and Signaling Pathways
Diagram 1: Circadian Regulation of Anti-Tumor Immunity
Diagram 2: Personalized Chronotherapy Dosing Workflow
Frequently Asked Questions (FAQs)
Q1: Why is it important to account for diurnal rhythms in biomarker discovery studies? The circadian clock exerts strict control over immune function, including the trafficking of leukocytes between tissues and the production of inflammatory mediators. Consequently, the concentration of many immune-related proteins in the blood oscillates over the 24-hour cycle. Failing to standardize sample collection times can introduce significant intraindividual variation, masking true disease-associated signals and reducing the reliability of potential biomarkers [37].
Q2: What are the primary biological drivers of daily variation in the plasma proteome? Two key drivers are:
- The Central Clock: The suprachiasmatic nucleus (SCN) in the hypothalamus, entrained by light-dark cycles, synchronizes rhythms throughout the body via neuropeptides and autonomic innervation [37].
- The Molecular Clock: This cell-autonomous mechanism involves a transcriptional-translational feedback loop. The core components are CLOCK and BMAL1 proteins, which activate genes including their own repressors, PER and CRY. This loop, along with secondary circuits involving REV-ERBα and RORα, generates 24-hour rhythms in gene expression, including those of immune proteins [37].
Q3: Which immune processes are known to be under circadian control? Circadian rhythms govern several key immune functions relevant to biomarker studies:
- Leukocyte Trafficking: The number of circulating immune cells changes dynamically over the day, driven by rhythmic expression of migration factors like CXCL12 and adhesion molecules [37].
- Immune Cell Development: Clock components like NFIL3 and BMAL1 are essential for the development of innate lymphoid cells, B cells, and specific T helper cell subsets [37].
- Inflammatory Responses: The magnitude of immune responses to challenges like vaccination or infection can vary depending on the time of day [37].
Q4: What is a key experimental design consideration for discovering diurnal biomarkers? Longitudinal sampling is crucial. Collecting serial samples from the same individual across multiple time points provides the data density needed to accurately track temporal changes and distinguish true diurnal oscillations from random variation or noise. This is superior to single, cross-sectional measurements [38] [39].
Technical Troubleshooting Guides
Issue 1: High Background in Immunoassays
| Potential Cause | Solution |
|---|---|
| Endogenous Enzymes | Quench endogenous peroxidases by incubating samples with 3% H₂O₂ in methanol or water. Use levamisole to inhibit endogenous phosphatases [40]. |
| Endogenous Biotin | Block with a commercial Avidin/Biotin Blocking Solution prior to adding the avidin-biotin-enzyme complex [40]. |
| Secondary Antibody Cross-reactivity | Increase the concentration of normal serum from the secondary antibody's host species in the blocking buffer to as high as 10% (v/v). Alternatively, reduce the concentration of the secondary antibody [40]. |
| Primary Antibody Issues | Titrate the primary antibody to find the optimal concentration. Reduce nonspecific binding by adding NaCl (0.15M - 0.6M) to the antibody diluent [40]. |
Issue 2: Weak Target Staining in Immunohistochemistry
| Potential Cause | Solution |
|---|---|
| Enzyme-Substrate Reactivity | Ensure buffers do not contain sodium azide (which inhibits HRP) and that the substrate is prepared at the correct pH. Test enzyme activity directly on nitrocellulose [40]. |
| Loss of Primary Antibody Potency | Include a known positive control tissue. Aliquot antibodies to avoid freeze-thaw cycles and store according to the manufacturer's specifications [40]. |
| Secondary Antibody Inhibition | Test decreasing concentrations of the secondary antibody. Excessively high concentrations can paradoxically reduce signal [40]. |
| Antigen Masking | For formalin-fixed paraffin-embedded tissues, perform Heat-Induced Epitope Retrieval (HIER) using a buffer like sodium citrate (pH 6.0) and heating in a microwave or pressure cooker [40]. |
Experimental Protocols for Key Workflows
Protocol 1: Workflow for Longitudinal Plasma/Serum Proteome Profiling
This protocol is adapted from large-scale studies that identified ageing-related proteins and tracked Type 1 Diabetes progression [38] [39].
1. Sample Collection & Study Design
- Collect serial plasma or serum samples from participants at multiple predefined time points.
- For diurnal studies, collect samples across the 24-hour cycle, standardizing conditions (e.g., light-dark, meals).
- Immediately process samples and store at -80°C to preserve protein integrity.
2. High-Abundance Protein Depletion
- Use an immunodepletion column to remove the top 14 most abundant plasma proteins (e.g., albumin, IgG) to enhance detection of lower-abundance proteins.
3. Protein Digestion and Isobaric Labeling
- Denature, reduce, and alkylate depleted proteins.
- Digest proteins with trypsin to create peptides.
- Label peptides from different time points with Tandem Mass Tags (TMT) to enable multiplexed quantitative analysis.
4. Liquid Chromatography and Mass Spectrometry
- Fractionate labeled peptides using high-pH reversed-phase liquid chromatography.
- Analyze fractions via LC-MS/MS on a high-resolution instrument (e.g., Q Exactive HF).
- Use a Data-Independent Acquisition method for comprehensive peptide profiling.
5. Data Analysis
- Process raw data with software to identify and quantify proteins.
- Use statistical trend analysis and linear mixed models to identify proteins with significant temporal or diurnal patterns.
Protocol 2: Verifying a Candidate Protein's Diurnal Rhythm by ELISA
After MS-based discovery, antibody-based assays are used for validation.
1. Sample Preparation
- Use the same longitudinal plasma/serum samples analyzed by MS.
- Dilute samples appropriately within the dynamic range of the ELISA kit.
2. Assay Execution
- Follow the manufacturer's protocol for the target protein's Quantikine ELISA or similar.
- Include all standards and controls in duplicate.
- For a diurnal study, analyze all time-point samples from a single subject on the same plate to minimize inter-assay variation.
3. Data Analysis
- Calculate protein concentrations from the standard curve.
- Plot concentrations against the time of day for each subject.
- Use statistical tests for rhythmicity to determine if the observed temporal pattern is significant.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| Tandem Mass Tags (TMT) | Isobaric chemical labels that enable multiplexed quantitative comparison of up to 16 different proteomic samples in a single LC-MS/MS run [38]. |
| Immunodepletion Column (e.g., MARS-14) | Affinity column that removes highly abundant proteins from plasma/serum, dramatically improving the depth of proteome coverage by allowing detection of lower-abundance proteins [38]. |
| Quantikine ELISA Kits | Ready-to-use, validated immunoassays for the precise quantification of specific protein biomarkers in complex biological fluids like plasma and serum [38]. |
| Sodium Citrate Buffer (pH 6.0) | A common buffer used for Heat-Induced Epitope Retrieval (HIER), a critical step for unmasking antigens in formalin-fixed tissues for IHC analysis [40]. |
| ReadyProbes Avidin/Biotin Blocking Solution | A pre-mixed solution used to block endogenous biotin and avidin, significantly reducing non-specific background staining in IHC and other biotin-based detection methods [40]. |
Core Circadian Signaling Pathway
Understanding the molecular clock is essential for interpreting diurnal protein data. The following diagram illustrates the core transcriptional-translational feedback loop that generates circadian rhythms [37].
Frequently Asked Questions (FAQs)
Q1: Why is the time-of-day a critical factor to consider in immune cell analysis?
Biological rhythms, a form of diurnal variation synchronized with the time of day, are observed across many areas of human physiology and immunology [19]. Circulating blood leukocyte counts demonstrate peak numbers during behavioral rest phases in humans [19]. The same molecular clock mechanism is present in both innate and adaptive human immune cells [19]. Failing to account for these natural fluctuations can introduce significant variance into your dataset, potentially obscuring true experimental effects or leading to inaccurate interpretations.
Q2: What are the practical consequences of ignoring diurnal variation in my experimental design?
Ignoring diurnal variation can reduce the diagnostic precision of your assays and compromise research conclusions [41]. For instance, a study of the human plasma proteome found that 26% of proteins, including 36 clinically utilized biomarkers, exhibited significant diurnal oscillations [41]. This means that a measurement taken in the morning could be significantly different from one taken in the afternoon for the same individual, not due to an experimental treatment but due to the natural daily rhythm. This unaccounted-for variance wastes time, money, and resources [42].
Q3: Can I detect diurnal variations in immune parameters using small blood volumes, such as from finger pricks?
Yes, research demonstrates that diurnal variations in lymphocyte prevalence can be detected using small-volume finger-prick blood samples [19]. One study successfully used 25 µL fingertip blood samples to identify significant diurnal changes in TH cells, B cells, and NK cells [19]. This methodology provides a less invasive sampling technique and improves participant acceptability for studies requiring multiple time-point collections [19].
Q4: Which specific immune cell types are known to exhibit diurnal rhythms?
Research has identified several immune cell types with diurnal patterns. For example, one flow cytometry study found that TH cells and B cells showed significantly higher percentages in the afternoon (5 PM) samples, whereas NK cells demonstrated a significantly higher morning percentage [19]. T cells, leukocytes, and cytotoxic T cells in the same study showed no significant changes over the day [19]. A broader proteomic study suggested diurnal regulation of hemostasis and immune signaling pathways [41].
Q5: What is the best statistical approach for analyzing longitudinal data collected across multiple time points?
Standard statistical methods that assume data points are independent and identically distributed (i.i.d.) are invalid for longitudinal data [42]. Instead, you should use mixed-effects models or generalized estimating equations (GEE) [42]. Mixed-effects models are suitable for smaller sample sizes and quantify both random effects (e.g., baseline differences between organisms) and fixed effects (e.g., differences from your experimental intervention) [42]. These models are statistically stronger than fitting each organism's data set individually and then averaging [42].
Troubleshooting Guide
Problem: High Variance in Immune Cell Counts Between Replicates
Possible Cause: Sample collection occurred at inconsistent times of day, capturing different phases of diurnal rhythms.
Recommendations:
- Standardize Collection Times: Design your experiment so that all samples for a given experimental condition are collected at the same time of day.
- Pilot Study: Conduct a small pilot study to characterize the diurnal variation of your key immune parameters. This will help you choose the most informative and consistent time points for your main experiment.
- Document Time Meticulously: Record the exact time of collection for every sample and include this as a covariate in your statistical models.
Problem: Inconsistent or Weak Signal in Diurnal Rhythm Analysis
Possible Cause: The sampling rate is too low to reliably detect the rhythm.
Recommendations:
- Increase Sampling Frequency: The sampling rate must be at least twice, and preferably more than twice, the frequency of the rhythm you wish to detect [42]. For a 24-hour rhythm, this means sampling at least every 12 hours, though more frequent sampling is needed to determine the waveform accurately [42].
- Ensure Even Spacing: Many rhythmicity analyses assume data are collected at evenly-spaced intervals. If this is not possible, plan for adjustments in your analysis, such as interpolation [42].
Problem: Unclear How to Statistically Model Time-of-Collection Data
Possible Cause: Using statistical tests that assume independence of data points, such as performing individual tests at each time point without correction.
Recommendations:
- Use Longitudinal Models: Apply mixed-effects models to account for the correlation between repeated measurements from the same individual [42].
- Avoid "Cherry-Picking": Never select a single time point from a longitudinal dataset for post-hoc statistical analysis without applying multiple testing corrections, as this dramatically increases the chance of false positives [42]. Pre-specify time points of interest in your experimental hypothesis.
- Check Stationarity: Plot your longitudinal data to check for stationarity—that is, whether the characteristics of the data (e.g., mean, variance) change during the analysis timeframe [42].
Table 1: Experimentally Measured Diurnal Variations in Immune Cell Populations
| Immune Parameter | Change Over Day | Significance (p-value) | Sample Volume Used | Citation |
|---|---|---|---|---|
| TH Cells | Significantly higher at 5 PM | P < 0.05 | 25 µL fingertip blood | [19] |
| B Cells | Significantly higher at 5 PM | P < 0.05 | 25 µL fingertip blood | [19] |
| NK Cells | Significantly higher at 8 AM | P < 0.05 | 25 µL fingertip blood | [19] |
| Cytotoxic T Cells | No significant change | Not Significant (NS) | 25 µL fingertip blood | [19] |
| Human Plasma Proteome | 138 of 523 proteins (~26%) oscillated | FDR-corrected | Standard venipuncture | [41] |
Table 2: Key Statistical Considerations for Longitudinal Immune Data
| Statistical Aspect | Common Mistake | Recommended Approach | Key Reference |
|---|---|---|---|
| Data Independence | Treating repeated measures from one subject as independent data points. | Use mixed-effects models or GEE to account for within-individual correlation. | [42] |
| Multiple Testing | Performing individual statistical tests at each time point without correction. | Pre-specify hypotheses; use longitudinal models or apply strict multiple-testing corrections (e.g., Bonferroni). | [42] |
| Sampling Rate | Sampling too infrequently to capture the rhythm. | Sample at ≥2x the frequency of interest (e.g., every 12h for a 24h rhythm); more for waveform. | [42] |
| Data Structure | Ignoring changes in the data's structure over time (non-stationarity). | Plot data and check for stationarity; use statistical techniques to quantify it. | [42] |
Experimental Protocols
Detailed Methodology: Flow Cytometry for Low-Volume Blood Samples
This protocol is adapted from a study that successfully identified diurnal variations using 25 µL fingertip blood samples [19].
Sample Collection:
- Collect finger-prick blood using safety lancets into K3 EDTA Microvette tubes.
- Apply warm water to fingertips to increase localized blood flow before collection.
- A minimum of 225 µL is recommended to allow for processing.
Staining Protocol (Reduced Volume):
- Use a commercially available lymphocyte kit (e.g., IMK Simultest).
- Adapt volumes: Scale down all reagent volumes to account for the low blood volume. The cited study used a 1:4 reduction, resulting in 25 µL of blood and 5 µL of reagent [19].
- Incubation: Add conjugate antibody and stain for 20 minutes at room temperature.
Lysis and Washing:
- Lyse red blood cells for 10 minutes at room temperature using 500 µL of 10x red blood cell lysing solution.
- Centrifuge at 200g (4°C) and discard the supernatant.
- Wash the sample with 500 µL of phosphate-buffered saline (PBS).
- After a second centrifugation and supernatant discard, resuspend the pellet in 125 µL of an appropriate solution (e.g., PBS with 2% fetal bovine serum).
Flow Cytometry & Analysis:
- Analyze samples on a flow cytometer (e.g., BD FACSVerse).
- Perform gating (lymphocyte, live/dead, singlet) and compensation using standard software (e.g., FlowJo).
- Analyze surface markers using established quadrant gates.
Methodology: Mass Spectrometry-Based Proteomic Analysis for Diurnal Variation
This protocol summarizes the approach used to identify diurnally regulated plasma proteins [41].
Controlled Study Design:
- Participants: Enroll healthy volunteers under strict inclusion criteria to minimize variation.
- Standardization: Control the environment—light exposure, food intake (standardized isocaloric meals), physical activity, and sleep—for 24 hours.
- Sampling: Collect venous blood at regular intervals (e.g., every 3 hours for 24 hours) following a standardized protocol, including patient posture and rest.
Sample Preparation:
- Centrifuge blood tubes to isolate plasma.
- Immediately aliquot and snap-freeze plasma, storing at -80°C.
- Thaw samples and dilute with lysis buffer.
- Reduce and alkylate proteins using reagents like TCEP and Chloroacetamide (CAA).
- Digest proteins into peptides using Trypsin/LysC mix.
LC-MS/MS Analysis:
- Load peptides onto a liquid chromatography system (e.g., Evosep One).
- Separate peptides on an analytical column.
- Analyze eluted peptides using a high-resolution mass spectrometer (e.g., Orbitrap Astral).
Data Analysis and Rhythmicity Assessment:
- Process raw data for protein identification and quantification.
- Filter and impute missing data.
- Assess Rhythmicity: Use Cosinor-based modeling or similar algorithms to fit curves to the longitudinal data and identify oscillating proteins.
- Apply multiple-testing corrections (e.g., Benjamini-Hochberg) to control the false discovery rate.
Workflow Visualization
Diagram 1: Diurnal Data Analysis Workflow
Diagram 2: Statistical Normalization Model
The Scientist's Toolkit
Table 3: Research Reagent Solutions for Diurnal Immune Studies
| Item | Function/Application | Example from Literature |
|---|---|---|
| K3 EDTA Microvette Tubes | Collection and anticoagulation of small-volume finger-prick blood samples. | Used to collect 225 µL of finger-prick blood for lymphocyte diurnal variation studies [19]. |
| Safety Lancets | Minimally invasive blood collection from fingertips. | Employed for participant-friendly, serial blood sampling [19]. |
| Lymphocyte Kit (e.g., IMK Simultest) | Contains pre-titrated antibody cocktails for immunophenotyping by flow cytometry. | Used with scaled-down volumes (5 µL reagent) for low-blood-volume analysis [19]. |
| Trypsin/LysC Mixture | Enzymatic digestion of proteins into peptides for mass spectrometry analysis. | Used in proteomic workflow to prepare plasma samples for LC-MS/MS [41]. |
| Evotips / C18 StageTips | Desalting and purification of peptide mixtures prior to LC-MS/MS injection. | Part of the sample preparation process for high-throughput plasma proteomics [41]. |
| Cosinor-Based Modeling Software | Statistical software package used to identify and characterize rhythms in longitudinal data. | Used to assess significant diurnal oscillation in plasma proteins with Benjamini-Hochberg correction [41]. |
Mitigating Variability: Strategies for Controlling Diurnal Confounders in Immune Research
Key Confounders at a Glance
The table below summarizes the major confounders, their impact on data, and recommended control methods.
| Confounder | Impact on Data | Recommended Control Methods |
|---|---|---|
| Intraindividual Variability (IIV) [43] | Can account for the majority of variance (75-90%) in diurnal parameters like cortisol, overwhelming stable individual differences [43]. | - Use dense repeated measures designs (e.g., 50+ observations per person for net IIV) [43].- Calculate person-specific metrics like intraindividual standard deviation (iSD) or root mean squared error (RMSE) [43]. |
| Chronotype [44] | Misalignment with study schedule (social jet lag) increases risk for obesity, depression, and cardiovascular disease, confounding metabolic and inflammatory markers [45] [44]. | - Classify participants using the Munich Chronotype Questionnaire (MCTQ) [45].- Stratify recruitment and/or schedule assessments to align with individual chronotypes. |
| Light Exposure Timing & Spectrum [46] | Determines circadian phase; morning short-wavelength light induces phase advances, while evening light induces phase delays [45] [46]. | - Monitor with devices like the Daysimeter [45].- Standardize and control light exposure in the lab; use controlled interventions (e.g., blue light/blue-blocking glasses) [45]. |
| Sleep/Wake Schedule Irregularity [47] | Causes irregular sleep patterns, disrupts circadian rhythms, and increases daytime fatigue, affecting physiological measures and cognitive performance [47]. | - Maintain a fixed, advanced sleep/wake schedule during studies [45].- Use actigraphy to verify compliance. |
| Medications & Health Conditions [47] | Many medications (e.g., antidepressants, painkillers) can alter sleep architecture, cause sedation, or affect hormone levels [47]. | - Record all medications and health conditions.- Include as covariates in statistical analysis or use as exclusion criteria. |
Essential Measurement Protocols
Quantifying Intraindividual Variability (IIV)
Intraindividual variability (IIV) refers to short-term, reversible changes within an individual. In diurnal cortisol, for example, stable individual differences account for only 10-25% of the variance, with the majority attributable to IIV [43].
- Key Metrics and Calculation Methods
- Intraindividual Standard Deviation (iSD): The standard deviation of all observations for an individual. It is simple to calculate but captures total variability without disaggregating sources [43].
- Root Mean Squared Successive Difference (rMSSD): Quantifies the variance between successive observations, useful for detecting autocorrelation [43].
- Root Mean Squared Error (RMSE): For cortisol, the iRMSE is the mean of the RMSE from diurnal slopes fit for each day. It represents "net cIIV"—the degree to which individual values deviate from the person's expected diurnal slope [43].
- Data Requirements: For reliable estimates, studies should aim for approximately 10 slopes and 50 residuals per individual [43].
Assessing Chronotype
Chronotype is your body's natural preference for sleep and wake times, closely linked to your circadian rhythm [44].
- Primary Tool: Munich Chronotype Questionnaire (MCTQ) [45]
- This self-report instrument assesses sleep and wake habits on free days and work days.
- It calculates the mid-sleep time on free days (MSFsc), which is a quantitative measure of chronotype [45].
- Classification: Participants can be categorized as early, intermediate, or evening types (sometimes analogized as lions, bears, and wolves) [44].
Monitoring Light Exposure
- Primary Tool: Spectrometer or calibrated light monitor (e.g., Daysimeter) [45]
- Reporting Standards: When reporting light interventions, provide at a minimum the spectral power distribution of the light from the participant's point of view. Illuminance (in lux) and correlated color temperature can also be reported [46].
Measuring Circadian Phase
- Gold Standard: Dim Light Melatonin Onset (DLMO) [45]
- Protocol: Collect salivary samples in the evening under dim light conditions (<10-30 lux).
- Procedure: Samples are typically collected every 30-60 minutes in the hours before habitual sleep onset. DLMO is calculated as the time when melatonin levels consistently exceed a predefined threshold (e.g., 3-4 pg/mL) [45].
Core Biological Pathways
The following diagram illustrates the core pathway through which light entrains circadian rhythms and influences physiological processes, a key relationship in this field of research.
Troubleshooting FAQs
Q1: Our study participants have highly irregular sleep schedules. How can we manage this confounder? Implement a fixed sleep/wake schedule protocol for a period (e.g., 1-2 weeks) before key assessments [45]. Verify compliance using actigraphy watches. During the intervention week, all participants should be placed on the same advanced sleep/wake schedule, with their light exposure carefully controlled to be either congruent or incongruent with the new schedule [45].
Q2: We've measured circadian phase, but the data is noisy. What could be the issue? Ensure strict dim light conditions (<10-30 lux) for at least 2 hours prior to and during DLMO sampling. Inadequate light control is a primary source of error. Also, verify that participants are not using smartphones or tablets, which emit phase-altering short-wavelength light [46].
Q3: How can we account for the large day-to-day swings in our biomarker measurements? This is likely high intraindividual variability (IIV). Instead of relying on single time-point measurements, use a repeated measures design. Calculate person-specific variability metrics like the intraindividual standard deviation (iSD) to quantify this noise, and then determine if the magnitude of variability itself is a meaningful predictor of health outcomes [43].
Q4: Do we need to account for chronotype if all participants follow the same lab protocol? Yes. Forcing evening types to adhere to a morning-oriented protocol induces social jet lag, a chronic misalignment between internal rhythm and external schedule. This state is associated with altered metabolic and stress markers, which can confound your results independently of the experimental manipulation [45] [44]. You should measure chronotype and include it as a covariate in your models.
The Scientist's Toolkit
| Research Reagent / Tool | Function & Application |
|---|---|
| Daysimeter-D [45] | A wearable device for continuous, personal monitoring of light/dark and activity/rest patterns, crucial for quantifying light exposure outside the lab. |
| Munich Chronotype Questionnaire (MCTQ) [45] | A standardized self-report instrument for quantifying an individual's chronotype based on their natural sleep-wake patterns. |
| Short-Wavelength (Blue) Light LEDs [45] | Used as a controlled light intervention in the morning to produce a phase-advancing effect on the circadian clock. |
| Short-Wavelength-Restricting Orange-Tinted Glasses [45] | Worn in the evening to block phase-delaying blue light from artificial sources, helping to maintain an advanced circadian phase. |
| ELISA Kits for VEGF-A, VEGF-C, PLGF [48] | Used for the quantitative measurement of vascular endothelial growth factors in serum or plasma (e.g., CTAD plasma) to study intraindividual variability over time. |
| Actigraphy Watches | Worn on the wrist to objectively monitor sleep-wake cycles and physical activity over extended periods in a participant's natural environment. |
| CTAD Plasma Tubes [48] | Blood collection tubes containing citrate-theophylline-adenine-dipyridamol, which act as platelet inhibitors to provide a more stable sample for measuring plasma VEGF levels. |
FAQs and Troubleshooting Guides
FAQ 1: What defines a "rhythm-stable" versus "rhythm-sensitive" immune parameter?
Answer: The core distinction lies in the parameter's variability over the 24-hour day.
- Rhythm-Sensitive Parameters: These show significant diurnal (daily) variation in their concentration, count, or function. Their values are tied to the time of day, meaning a measurement taken in the morning can be significantly different from one taken in the evening. A prime example is the circulation of specific immune cells, such as helper T cells and B cells, which show higher percentages in the evening (5 PM) compared to the morning (8 AM) [19].
- Rhythm-Stable Parameters: These are immune measures that do not exhibit significant fluctuation throughout the day. Their values remain relatively constant, making them more reliable benchmarks regardless of sampling time. For instance, some studies find that total T cell and cytotoxic T cell percentages do not show significant diurnal changes [19].
FAQ 2: My experimental results for immune cell counts are inconsistent. Could the time of sample collection be a factor?
Answer: Yes, time of collection is a critical and often overlooked confounder. The immune system is under strong circadian control, and the trafficking of leukocytes between the blood, bone marrow, and tissues follows a daily rhythm [37] [49].
- Root Cause: This rhythmic trafficking is regulated by circadian clocks, both within the immune cells themselves (cell-intrinsic) and from the organism's environment (cell-extrinsic), such as rhythmic changes in adhesion molecules and stress hormones [37]. For example, the rhythmic release of factors like CXCL12 from bone marrow stromal cells controls the egress of cells into the periphery [37].
- Solution: Standardize the time of day for all sample collections in your study. If cross-sectional, carefully record the time of collection and account for it as a potential covariate in your analysis. Using a time-stable parameter (like total T cells) as an internal control can help validate your findings.
FAQ 3: How can I identify which of my biomarkers of interest are rhythm-sensitive?
Answer: A systematic approach is required to classify your biomarkers.
- Profile over Time: Conduct a pilot study where you collect samples from the same subjects across multiple time points over a 24-hour period (e.g., every 4-6 hours) under controlled conditions.
- Statistical Analysis: Use statistical tests for rhythmicity (e.g., Cosinor analysis, paired t-tests between peak and trough times) on the data from your pilot study.
- Consult Literature: Refer to existing resources, such as the table below, which summarizes the diurnal behavior of common immune parameters.
Table 1: Diurnal Variation in Common Immune Parameters
| Immune Parameter | Diurnal Variation | Peak Time | Trough Time | Key References |
|---|---|---|---|---|
| Helper T Cells (TH) | Rhythm-Sensitive | Evening (e.g., 5 PM) | Morning (e.g., 8 AM) | [19] |
| B Cells | Rhythm-Sensitive | Evening (e.g., 5 PM) | Morning (e.g., 8 AM) | [19] |
| Natural Killer (NK) Cells | Rhythm-Sensitive | Morning | Evening | [19] |
| Neutrophils | Rhythm-Sensitive | Evening | Morning | [21] |
| Total Leukocytes | Rhythm-Sensitive | Evening | Morning | [21] |
| Cytotoxic T Cells | Rhythm-Stable | N/A | N/A | [19] |
| Total T Cells | Rhythm-Stable | N/A | N/A | [19] |
FAQ 4: I am developing a circadian biomarker for clinical use. What are the major pitfalls in training and validation?
Answer: A common pitfall is developing a biomarker under idealized, stable conditions that fails to perform in real-world scenarios where sleep may be restricted or desynchronized [50].
- Pitfall 1: Overfitting from Small Sample Sizes. Biomarker approaches trained on small sample sizes are prone to poor performance and lack generalizability [50].
- Pitfall 2: Ignoring Protocol Effects. The experimental conditions (e.g., sleep deprivation, forced desynchrony) of the training data significantly impact the selected molecular features and the final biomarker's performance. A biomarker trained on baseline data may not work during shiftwork simulations [50].
- Best Practice: Follow established biomarker-development concepts. Use large, diverse training sets and validate the biomarker's performance across different experimental protocols that mimic the intended real-world application [50].
Experimental Protocols for Diurnal Variation
Protocol 1: Assessing Lymphocyte Diurnal Variation with Low-Volume Blood Collection
This protocol is adapted from a study that successfully identified diurnal changes using only 25 µL finger-prick blood samples [19].
1. Sample Collection:
- Participants: Recruit healthy volunteers. (Original study: n=8, aged 18-25) [19].
- Timing: Collect samples at targeted times (e.g., 8 AM and 5 PM) on the same day.
- Method: Apply warm water to fingertips to increase blood flow. Using safety lancets, collect a minimum of 225 µL of blood into K3 EDTA Microvette tubes.
2. Cell Staining and Preparation:
- Use a commercially available lymphocyte kit (e.g., IMK Simultest: Lymphocyte Kit).
- Scale Down Volumes: Adapt the manufacturer's protocol for low volumes. The cited study used 25 µL of blood and 5 µL of reagent [19].
- Incubate with antibody conjugates for 20 minutes at room temperature.
- Lyse red blood cells for 10 minutes at room temperature.
- Wash cells with PBS, centrifuge, and resuspend in an appropriate buffer for analysis.
3. Flow Cytometry & Analysis:
- Analyze samples on a flow cytometer (e.g., BD FACSVerse).
- Use flow cytometry analysis software (e.g., FlowJo) for gating.
- Gating Strategy:
- Lymphocyte gate on FSC-A/SSC-A plot.
- Live/Dead cell gate using a viability dye (e.g., propidium iodide).
- Singlet gate using FSC-H/FSC-W and SSC-H/SSC-W.
- Analyze fluorescence quadrants to identify specific cell types (T cells, B cells, NK cells, etc.).
4. Statistics:
- Use a paired Student's two-tailed t-test to compare lymphocyte prevalence between morning and afternoon time points. A p-value of less than .05 is typically considered significant [19].
Protocol 2: Evaluating Diurnal Immune Responses to Physiological Stress
This protocol outlines how to investigate the interaction between time of day and an immune challenge, such as intense exercise [21].
1. Study Design:
- Use a crossover randomized design where participants complete the intervention at different times of day (e.g., 09:00 h and 18:00 h), separated by a washout period.
- Conduct the trial in a controlled environment (e.g., an environmental chamber set to 28°C and 70% humidity) [21].
2. Exercise Intervention:
- Participants (e.g., highly trained runners) perform a 10 km time trial on a treadmill.
- Participants should have free control over running speed to mimic a real-world performance test.
3. Data and Sample Collection:
- Physiological Measures: Record core body temperature (via telemetric pill) and heart rate pre-trial, during the trial, and post-trial.
- Blood Samples: Collect venous blood pre-, post-, and 1-hour post-trial.
- Complete Blood Count: Use an automated cell counter to determine total WBC, neutrophil, and lymphocyte counts.
- Serum Biomarkers: Centrifuge blood, aliquot serum, and freeze at -80°C for later analysis of cytokines (e.g., IL-6) via ELISA [21].
4. Statistical Analysis:
- Employ paired t-tests or repeated measures ANOVA to identify significant diurnal differences in immune and physiological parameters in response to the stressor.
Signaling Pathways and Workflows
Circadian-Immune Signaling Network
Circadian Control of Immunity
Biomarker Validation Workflow
Biomarker Development Steps
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Kits for Diurnal Immune Research
| Item / Reagent | Function / Specificity | Example Use Case | Low-Volume Adaptation |
|---|---|---|---|
| IMK Simultest: Lymphocyte Kit | Multiplex flow cytometry panel for T, B, and NK cells | Immunophenotyping from whole blood [19] | Yes (25 µL blood + 5 µL reagent) [19] |
| K3 EDTA Microvette Tubes | Anticoagulant blood collection | Low-volume blood collection from finger-prick or ear [19] | Native use for 200-300 µL draws |
| Safety Lancets | Sterile, disposable finger-prick devices | Minimally invasive micro-sampling [19] | Native use |
| ELISA Kits (e.g., IL-6, HSP70, CC16) | Quantify soluble protein biomarkers in serum/plasma | Measuring inflammatory response to stress [21] | Follow kit specifications; may require sample dilution |
| Red Blood Cell Lysing Solution | Lyses RBCs for WBC analysis | Preparing whole blood for flow cytometry [19] | Scale volume proportionally to blood |
| Propidium Iodide | Viability dye for flow cytometry | Distinguishing live/dead cells during analysis [19] | Scale volume proportionally |
Troubleshooting Guide: Addressing Intraindividual Variation in CAR-T Cell Studies
Common Challenges and Solutions
Issue: Inconsistent therapeutic outcomes between patients
- Potential Cause: Uncontrolled diurnal rhythms in immune cell function and persistence.
- Solution: Standardize CAR-T cell infusion times, prioritizing morning administration. A retrospective study of 670 patients found each hour earlier infusion was associated with significantly higher 90-day overall survival (adjusted OR 0.78, 95% CI 0.66-0.92) and lower rates of severe neurotoxicity [51].
Issue: Delayed treatment initiation
- Potential Cause: Geographic barriers between referring providers and authorized treatment centers.
- Solution: Establish close coordination between referring and treatment centers. Data shows receiving CAR-T therapy in a different geographic area introduces a mean delay of 12 days, growing to 22 days at the 75th percentile [52].
Issue: Variable quality in starting materials
- Potential Cause: Inconsistent leukapheresis product quality from patients with malignancies.
- Solution: Implement rigorous quality control on leukapheresis products, including hemogram and immune cell profiling. Patients pre-treated for malignancies often have lower leukocyte, CD3, and CD4 counts, which can negatively impact manufacturing [53].
Frequently Asked Questions (FAQs)
Q: How significantly does infusion timing affect CAR-T cell efficacy? A: Time of day is a potent modifiable factor. Morning infusions correlate with substantially better survival outcomes and reduced toxicity. Each hour delay in infusion corresponds to a 17% increase in severe neurotoxicity odds (adjusted OR 1.17) and 26% higher likelihood of requiring anakinra prescription [51].
Q: What are the key considerations for leukapheresis product quality? A: Patient health status significantly impacts starting material. Key parameters include:
- Absolute lymphocyte and CD3+ T-cell counts
- CD4/CD8 ratio (often inverted in patients with malignancies)
- Proportion of activated lymphocytes
- Minimal contamination with blasts (in leukemic diseases) [53]
Q: How can I control for diurnal variation in immune cell parameters during sampling? A: Standardize sampling times and use low-volume methods. Research demonstrates diurnal variations in lymphocyte subpopulations can be detected using small-volume (25 µL) finger-prick blood samples, with TH cells and B cells showing significantly higher percentages at 5 PM compared to 8 AM [19].
Q: What strategies optimize CAR-T cell trafficking to solid tumors? A: Mathematical modeling suggests combining CAR-T with tumor microenvironment normalization. A physiologically-based pharmacokinetic model indicates tumor blood vessel normalization can improve CAR-T efficacy and reduce required therapeutic dose approximately fivefold. Local delivery for brain tumors provides equivalent control with fewer cells [54].
Table 1: Impact of CAR-T Cell Infusion Timing on Clinical Outcomes (n=670)
| Outcome Measure | Effect per Hour Delay | Adjusted Odds Ratio | 95% Confidence Interval | P-value |
|---|---|---|---|---|
| 90-Day Overall Survival | Decreased | 0.78 | 0.66-0.92 | 0.004 |
| Severe ICANS (Neurotoxicity) | Increased | 1.17 | 1.01-1.34 | 0.031 |
| Anakinra Prescription | Increased | 1.26 | 1.07-1.49 | 0.006 |
| Severe Cytokine Release Syndrome | No significant association | 0.96 | 0.74-1.23 | 0.73 |
Data derived from retrospective analysis of patients at two geographically distinct hospitals [51]
Table 2: Diurnal Variations in Circulating Lymphocyte Subpopulations
| Cell Type | 8 AM Percentage | 5 PM Percentage | Significance (P<0.05) | Direction of Change |
|---|---|---|---|---|
| TH Cells | Lower | Higher | Yes | Increase |
| B Cells | Lower | Higher | Yes | Increase |
| NK Cells | Higher | Lower | Yes | Decrease |
| T Cells | - | - | No | No significant change |
| Cytotoxic T Cells | - | - | No | No significant change |
| Leukocytes | - | - | No | No significant change |
Data from flow cytometry analysis of 25 µL fingertip blood samples from 8 participants [19]
Experimental Protocols
Detailed Methodology: Assessing Diurnal Lymphocyte Variations
Objective: Determine diurnal variations in peripheral lymphocyte prevalence using small-volume blood samples [19].
Sample Collection:
- Participants: 8 healthy volunteers (5 male, 3 female) aged 18-25
- Sampling times: 8 AM and 5 PM on the same day
- Method: Warm water applied to fingertips to increase blood flow
- Collection: Minimum 225 µL finger-prick blood using safety lancets into K3 EDTA Microvette tubes
- Preference: Single fingertip collection when possible
Flow Cytometry Analysis:
- Blood volume: 25 µL (reduced from standard 100 µL)
- Reagents: IMK Simultest Lymphocyte Kit with volume reduced to 5 µL
- Staining: 20 minutes at room temperature
- Red blood cell lysis: 10 minutes at room temperature
- Centrifugation: 200g at 4°C
- Analysis: BD FACSVerse cytometer with FlowJo software for gating
Statistical Analysis:
- Paired Student 2-tailed t-test for morning vs. afternoon counts
- Significance threshold: P < 0.05
Protocol: Retrospective Analysis of Infusion Timing Outcomes
Study Design: Multicenter retrospective cohort analysis [51].
Patient Population:
- 670 patients from two geographically distinct hospitals
- Timeframe: 2018-2024
- Inclusion: Received CAR-T therapy for B-cell malignancies
Data Collection:
- Primary outcome: 90-day overall survival
- Secondary outcomes: Event-free survival, CRS, ICANS, ICU admission, shock, respiratory failure, infection
- Covariates: Patient characteristics, oncological features, treatment details
Statistical Analysis:
- Multivariable mixed effects logistic regression
- Adjustment for patient, oncological, and treatment characteristics
- Quantification of independent relationship between infusion time and outcomes
Visualizations
Diagram 1: CAR-T Infusion Timing Impact Pathway
Diagram 2: Diurnal Variation Study Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for CAR-T Cell Research
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Leukapheresis Product | Cellular starting material for CAR-T manufacturing | Quality varies in patients with malignancies; assess lymphocyte counts, CD4/CD8 ratio [53] |
| Lentiviral Vectors | Gene delivery for CAR construct | Must include appropriate signaling domains (e.g., 4-1BB, CD3ζ); ensure high transduction efficiency [55] |
| Culture Media (X-Vivo 15) | T-cell expansion and maintenance | Supplement with IL-2 (300 U/mL) for T-cell growth and persistence [55] |
| Cytokines (IL-2) | T-cell activation and expansion | Critical for ex vivo expansion and in vivo persistence of CAR-T cells [55] |
| Flow Cytometry Reagents | Immune cell phenotyping and CAR expression detection | Use lymphocyte-specific antibody panels; small volumes (25µL) sufficient for analysis [19] |
| Lymphodepletion Chemotherapy (Cyclophosphamide/Fludarabine) | Host immune ablation prior to infusion | Creates favorable environment for CAR-T expansion; standard regimen: Cy 500mg/m² ×2d, Flu 30mg/m² ×4d [55] |
Frequently Asked Questions for Researchers
FAQ 1: What are the primary immune biomarkers affected by circadian disruption in human studies? Circadian misalignment, particularly from night-shift work, leads to significant alterations in both cellular and inflammatory immune biomarkers. Key cellular changes include altered counts and diurnal rhythms of lymphocytes (T-helper cells, cytotoxic T-cells, memory B-cells) and natural killer (NK) cells [19] [56]. Inflammatory biomarkers like Interleukin-6 (IL-6) also show disrupted secretion patterns and elevated levels, indicating a heightened pro-inflammatory state [57] [56]. These changes are consistent with a state of immune dysregulation.
FAQ 2: How does social jet lag differ from sleep debt, and how do I measure them in a cohort? Social jet lag and sleep debt are distinct but often concurrent aspects of circadian disruption.
- Social Jet Lag: This is a measure of circadian misalignment, representing the mismatch between biological time (driven by your internal clock) and social time (driven by your schedule). It is calculated as the difference between the mid-sleep time on free days and the mid-sleep time on work days [56] [58].
- Sleep Debt: This is a measure of chronic sleep restriction, calculated as the difference between total sleep time per 24 hours on free days (TST24f) and total sleep time per 24 hours on work days (TST24w) [56]. Multivariate analyses indicate that these factors can have independent and combined effects on immune parameters, particularly in night-shift workers [56].
FAQ 3: What is the evidence that circadian disruption directly impacts immune function, beyond just correlation? Controlled laboratory studies provide direct evidence. For instance, in mice, experimentally induced chronic jet lag (e.g., four consecutive weekly 6-hour phase-advances of the light-dark schedule) led to a dramatically heightened inflammatory response to lipopolysaccharide (LPS), resulting in hypothermia and 89% mortality compared to 21% in control mice [57]. This was linked to a heightened release of pro-inflammatory cytokines. Isolated macrophages from shifted mice maintained this heightened response in vitro, confirming that the circadian disruption directly targets immune cells, independent of sleep loss or stress [57].
FAQ 4: Why is the timing of blood collection so critical in immune studies? The prevalence of most immune cells and cytokines exhibits strong diurnal variation [19] [56] [59]. For example, in day-shifters, lymphocytes like T-helper and B-cells show significantly higher percentages in the evening (5 PM) compared to the morning (8 AM), while NK cells show the opposite pattern [19]. If samples are taken at a single, inconsistent time of day, this biological variation can be misinterpreted as a treatment effect or mask a real one. Standardizing collection times relative to the participant's circadian phase is essential for accurate data interpretation.
FAQ 5: Can I use small-volume blood draws to assess diurnal immune variation? Yes. Recent research demonstrates that diurnal variations in lymphocyte prevalence can be reliably detected using very small blood volumes (e.g., 25 µL from a finger-prick) [19]. This method is less invasive, improves participant acceptability, and is feasible for large-scale or frequent sampling in cohort studies. The detection of expected diurnal patterns with this method has been validated against known biology [19].
Experimental Protocols for Shift Work & Jet Lag Research
Protocol 1: Assessing Immune Rhythms in Night-Shift Workers
This protocol is adapted from a real-world study of hospital healthcare professionals [56].
- Objective: To characterize the impact of permanent night shifts on immune rhythms, sleep debt, and social jet lag.
- Subject Population: Recruit two groups: permanent night-shift workers (e.g., 21:00–07:00) and rotating day-shift workers as a control group.
- Methodology:
- Sleep & Work Diaries: Participants maintain a daily diary for a full work week (7 days), recording all sleep episodes (main sleep and naps) and work schedules. This allows for calculation of Total Sleep Time per 24h on work days (TST24w) and free days (TST24f), sleep debt (TST24f - TST24w), and social jet lag (difference in mid-sleep time between free and work days).
- Blood Sampling: Collect blood samples at the beginning and end of the final shift of the week. For day-shifters, this would be at 7:00 and 14:00 (morning shift) or 14:00 and 21:00 (afternoon shift). For night-shifters, collect at 21:00 and 7:00.
- Immune Biomarker Analysis:
- Flow Cytometry: Use polychromatic flow cytometry to assess circulating counts of immune cells (e.g., total lymphocytes, T-helper cells, cytotoxic T-cells, B-cells, NK cells) [19] [56].
- Inflammatory Markers: Quantify serum levels of IL-6 and C-reactive protein (CRP) using ELISA or a Luminex multiplex assay [57] [56].
- Key Analysis: Compare the 24-hour profile of immune markers between groups. In night-shifters, expect to see inverted or blunted rhythms (e.g., immune markers that are normally low in the morning are high, and vice versa). Use multivariate analysis to model the impact of TST24w, sleep debt, and social jet lag on immune outcomes.
Protocol 2: Modeling Chronic Jet Lag in an Animal System
This protocol is based on studies investigating the innate immune response to circadian disruption [57].
- Objective: To determine the causal effects of chronic circadian disruption on the inflammatory response.
- Animal Model: Adult mice (e.g., C57BL/6 background).
- Chronic Jet Lag Induction:
- Control Group: Maintained on a standard 12-hour light/12-hour dark (12L:12D) cycle.
- Shifted Group: Exposed to a repeating phase-advance schedule. Each week, the light-dark cycle is advanced by 6 hours. This is achieved by shortening the dark period on the day of the shift. This protocol is administered for 4 consecutive weeks [57].
- Immune Challenge:
- On the 7th day after the last photoperiod change, inject mice intraperitoneally with a dose of ultrapure LPS (e.g., 12.5 mg/kg for a lethal model or 5 mg/kg for a sublethal model) at a fixed circadian time (e.g., Zeitgeber Time 3, 3 hours after lights-on) [57].
- Data Collection:
- Survival & Core Temperature: Monitor and record survival and core body temperature for 7 days post-injection.
- Cytokine Measurement: Collect blood via retro-orbital bleeding at 90 minutes and 24 hours post-LPS injection. Separate serum and measure pro-inflammatory cytokines (e.g., IL-6, TNF-α) using a multiplex immunoassay or ELISA [57].
- Macrophage Isolation: Isolate peritoneal macrophages from a separate cohort of shifted and control mice. Challenge the cells with LPS in vitro and measure cytokine production to assess cell-intrinsic effects of the circadian disruption [57].
Quantitative Data on Circadian Disruption and Immune Parameters
Table 1: Diurnal Variation of Key Immune Cells in Healthy Humans (from finger-prick blood, n=8) [19]
| Immune Cell Type | 8:00 AM | 5:00 PM | P-value |
|---|---|---|---|
| T-Helper (TH) Cells | Lower Percentage | Higher Percentage | < 0.05 |
| B Cells | Lower Percentage | Higher Percentage | < 0.05 |
| Natural Killer (NK) Cells | Higher Percentage | Lower Percentage | < 0.05 |
| Cytotoxic T Cells | No Significant Change | No Significant Change | N.S. |
Table 2: Immune & Sleep Characteristics of Hospital Healthcare Professionals (Adapted from [56])
| Parameter | Day Shifters (n=96) | Permanent Night Shifters (n=95) |
|---|---|---|
| Total Sleep Time (Work Days) | ~7.1 hours | 5.4 ± 1.4 hours |
| Sleep Debt | Minimal | 3.2 ± 1.4 hours |
| Social Jet Lag | Minimal | 6.7 ± 2.4 hours |
| IL-6 Rhythm | Normal diurnal pattern | Inverted: Lower at 21:00, higher at 07:00 |
| Lymphocyte Rhythm | Normal diurnal pattern | Inverted: Lower at 21:00, higher at 07:00 |
Table 3: Impact of Chronic Jet Lag on LPS-Induced Lethality in Mice [57]
| Experimental Group | Mortality after LPS (12.5 mg/kg) | Key Immune Finding |
|---|---|---|
| Control (Unshifted) | 21% | Normal cytokine response |
| Chronic Jet Lag (4 shifts) | 89% | Heightened release of pro-inflammatory cytokines |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Circadian Immune Profiling
| Reagent / Kit | Function / Application | Example & Notes |
|---|---|---|
| Polychromatic Flow Cytometry Kit | Immunophenotyping of lymphocyte subsets from small blood volumes. | IMK Simultest: Lymphocyte Kit (BD Biosciences). Volumes can be scaled down for 25 µL blood samples [19]. |
| Multiplex Immunoassay | Simultaneous quantification of multiple cytokines (e.g., IL-6, TNF-α) from a single small sample. | Milliplex MAP Kit (Millipore) on a Luminex xMAP platform [57]. |
| ELISA Kits | Quantification of specific proteins like single cytokines (IL-6) or CRP. | R&D Systems ELISA Kit [57]. |
| Ultrapure Lipopolysaccharide (LPS) | For standardized immune challenge in animal models to study inflammatory pathways. | Ultrapure LPS from E. coli (e.g., Invivogen) [57]. |
| Safety Lancets & Microvette Tubes | For consistent, low-volume blood collection via finger-prick in human studies. | 200-µL Microvette, K3 EDTA tubes (Sarstedt Group) [19]. |
Signaling Pathways and Experimental Workflows
Circadian-IMMUNE AXIS
Shift Work Study Workflow
A core challenge in biological research, particularly in studies involving diurnal rhythms and the immune system, is distinguishing meaningful intraindividual variability from experimental error. Intraindividual variability refers to the natural, transient within-person fluctuations in behavioral or physiological performance [60]. Rather than being mere "noise," such variability can be a significant data source, signaling underlying physiological states, neurological compromise, or ongoing system reorganization and learning [60] [61]. In the context of immune research, this variability is often governed by robust circadian rhythms that control the location, number, and responsiveness of immune cells [37]. This guide provides a diagnostic framework to help researchers troubleshoot unexpected intraindividual variation in their data, enabling them to determine its root cause and refine their experimental designs.
Core Concepts FAQ
Q1: What is intraindividual variability, and why is it significant in immune studies? Intraindividual variability is not merely measurement error. It represents transient within-person fluctuations in performance or physiological measures over time [60]. From a dynamic systems perspective, variability is a potential driving force of development and an indicator of ongoing processes [61]. In immune studies, this is crucial because the immune system exhibits strong diurnal rhythms; the number of circulating immune cells, their migration patterns, and their functional responses change predictably over the 24-hour cycle [37] [62]. Therefore, inconsistent results from samples taken at different times of day may reflect a biologically meaningful, rhythmic process rather than a problem with your assay.
Q2: How can I tell if the variability in my data is biologically meaningful or just noise? Biologically meaningful variability often shows structured patterns, such as:
- Consistency over time: The variability itself can be a stable, trait-like property of the individual for a given measure [60].
- Correlation with other variables: It may be associated with other biological rhythms, such as cortisol levels or core body temperature [62].
- Theoretical predictions: According to dynamic and catastrophe theories, a significant increase in variability can be a harbinger of an impending developmental transition or a "phase shift" in the system, a phenomenon known as anomalous variance [61]. In contrast, pure noise is typically random and uncorrelated with other measured parameters.
Q3: What are the most common sources of unexplained intraindividual variation in immune studies? The primary sources can be categorized as follows:
- Uncontrolled Diurnal Rhythms: Failing to account for the time of sample collection is a major source. Key immune parameters, such as leukocyte counts and cytokine production, fluctuate rhythmically [37] [62].
- Environmental Zeitgebers ("Time Givers"): Inconsistent light-dark cycles, feeding times, or sleep schedules among research subjects (human or animal) can desynchronize internal clocks, leading to increased variability [62].
- Methodological Inconsistency: Varying sample processing protocols or personnel across collection timepoints can introduce technical artifacts.
- Underlying Pathophysiology: Increased behavioral or physiological variability has been linked to various clinical conditions, including dementia, chronic fatigue syndrome, and brain injury [60].
Diagnostic Framework: Isolating the Source of Variation
Use this structured approach to diagnose the cause of unexpected variability in your experiments.
Step 1: Characterize the Variability
Begin by quantifying the nature of the variability in your dataset.
- Calculate Intraindividual Standard Deviation (iSD): Compute the standard deviation of repeated measurements within each individual.
- Examine Patterns: Plot individual trajectories over time to visualize whether fluctuations are random or follow a cyclical pattern.
Step 2: Correlate with Key Experimental Variables
Check for associations between the magnitude of variability and other measured parameters.
- Performance Level: Investigate the relationship between an individual's mean performance level and their variability. A negative correlation (higher performance associated with lower variability) often signals system stability, while a positive correlation can sometimes indicate practice-related learning and strategy exploration [60].
- Time-of-Day: Correlate your primary outcome measures with the precise time of sample collection or behavioral testing.
Step 3: Systematically Control for Major Confounders
If variability correlates with time-of-day, proceed to control for diurnal rhythms.
- Standardize Collection Times: Conduct all sampling at a fixed, biologically relevant time (e.g., 2 hours after lights-on).
- Implement Time-Series Sampling: If resources allow, collect samples across multiple timepoints within the 24-hour cycle to map the rhythm for your specific outcome measure.
Expected Diurnal Variations in Key Immune Parameters
The following table summarizes the diurnal rhythms of various immune cell populations in peripheral blood, as demonstrated in a porcine model (a valuable diurnal model for human immunology) [62]. These rhythms are generally inverted for nocturnal rodents.
Table 1: Diurnal Rhythms in Peripheral Blood Immune Cell Counts
| Immune Cell Population | Peak During Active or Resting Phase? | Notes on Diurnal Rhythm |
|---|---|---|
| Total Leukocytes | Resting Phase | Overall rhythm is present. |
| Neutrophils | Resting Phase | Rhythmic egress from blood vessels is controlled by BMAL1 regulation of CXCR4 and CCL2 [37]. |
| Monocytes | Resting Phase | Trafficking is constrained by BMAL1 [37]. |
| Natural Killer (NK) Cells | Resting Phase | Development depends on the clock protein NFIL3 [37]. |
| T Cells | Resting Phase | Circulating frequencies peak during the resting phase [37]. |
| Cytotoxic T Cells | Resting Phase | Shows clear overall rhythmicity. |
| γδ T Cells | Resting Phase | Shows clear overall rhythmicity. |
| Helper T Cells (Total) | Resting Phase | Shows clear overall rhythmicity. |
| Dendritic Cells | Resting Phase | Shows clear overall rhythmicity. |
| Eosinophils | Resting Phase | Shows clear overall rhythmicity. |
| B Cells | No significant rhythm | No overall diurnal rhythmicity was detected in the study [62]. |
| Antigen-experienced Helper T Cells | No significant rhythm | Did not exhibit overall rhythmicity, unlike total Th cells [62]. |
Experimental Protocols for Controlling Diurnal Variation
Protocol 1: Standardized Sample Collection for Immune Profiling
This protocol is designed to minimize variability introduced by circadian rhythms in immune cell trafficking.
1. Principle: Immune cell migration between the bone marrow, blood, and tissues is under strict circadian control, governed by cell-autonomous clocks and endocrine cues like glucocorticoids [37] [62]. This results in predictable daily oscillations in peripheral blood cell counts.
2. Reagents and Equipment:
- EDTA or Heparin blood collection tubes
- Refrigerated centrifuge
- Flow cytometer with appropriate antibody panels
- -80°C freezer for plasma/serum storage
3. Step-by-Step Procedure:
- Pre-study Acclimatization: House all experimental subjects (animal or human) under a consistent light-dark (LD) cycle (e.g., 12h:12h) for a minimum of two weeks prior to experimentation to entrain circadian clocks.
- Synchronize Zeitgebers: Maintain strict consistency in the timing of light exposure, feeding, and other potential time cues.
- Fix Sample Collection Time: Collect all blood samples at the same time of day within a given study. For cross-study comparisons, the collection time must be identical. The choice of time should be justified based on the biological question (e.g., peak vs. trough of the rhythm).
- Rapid Processing: Process all samples within an identical, short time window after collection (e.g., within 1 hour) to prevent ex vivo changes in cell viability or gene expression.
- Record Time: Meticulously document the exact time of sample collection for every data point.
Protocol 2: Assessing Molecular Clock Function in Immune Cells
If aberrant variability is suspected to stem from a disrupted circadian system, this protocol provides a methodology for assessment.
1. Principle: The core molecular clock is a cell-autonomous transcriptional-translational feedback loop. Key components include the activators BMAL1 and CLOCK and the repressors PER and CRY [37].
2. Reagents and Equipment:
- RNA extraction kit (e.g., Trizol)
- cDNA synthesis kit
- Real-time PCR system
- SYBR Green or TaqMan master mix
- Primers for core clock genes (e.g., BMAL1, PER2, REV-ERBα)
3. Step-by-Step Procedure:
- Time-Series Sampling: Collect samples across at least two timepoints (e.g., 12 hours apart) to capture the oscillatory pattern.
- RNA Extraction: Isolate total RNA from purified immune cell populations (e.g., PBMCs, neutrophils).
- cDNA Synthesis: Synthesize cDNA from equal amounts of RNA.
- qPCR Analysis: Perform quantitative PCR (qPCR) for core clock genes and a housekeeping gene for normalization.
- Data Interpretation: Rhythmic, anti-phasic expression of activator (e.g., BMAL1) and repressor (e.g., PER2) genes indicates a functional clock. Damped or arrhythmic expression suggests circadian disruption.
Visualization of Circadian-Immune System Interactions
The following diagram illustrates the core molecular machinery of the circadian clock and its direct influence on key immune functions, providing a mechanistic basis for understanding diurnal variability.
Diagram 1: The Circadian-Immune System Axis. This figure illustrates how the central clock in the SCN, entrained by light, synchronizes peripheral clocks in immune cells via neural and hormonal signals. The cell-autonomous molecular clock (BMAL1/CLOCK and PER/CRY feedback loop) generates rhythmic gene expression that governs key immune processes. Created based on [37].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating Diurnal Immune Variation
| Reagent / Material | Primary Function in This Context |
|---|---|
| Specific Antibody Panels | Flow cytometric quantification of rhythmically fluctuating immune cell subsets (e.g., neutrophils, monocytes, T cell subsets) [62]. |
| qPCR Reagents | Analysis of rhythmic expression of core clock genes (Bmal1, Per2, Rev-erbα) and clock-controlled immune genes (Cxcl2, Ccr7) [37]. |
| ELISA/Kits for Cortisol/Corticosterone | Quantification of key circadian endocrine mediators that influence immune cell trafficking and function [37] [62]. |
| Environmental Control Chambers | Precise control of light-dark cycles, temperature, and humidity to standardize zeitgebers for animal studies. |
| Luminescence Plate Reader | Real-time monitoring of circadian gene expression dynamics using reporter cell lines (e.g., Per2::Luciferase). |
Advanced Troubleshooting FAQ
Q4: My data shows high intraindividual variability even after controlling for time-of-day. What should I investigate next? Consider these possibilities:
- Practice or Learning Effects: In cognitive or behavioral tasks, higher variability can be positively associated with practice-related gains as individuals explore and consolidate new strategies [60]. Re-analyze your data to see if variability decreases after the first few test sessions.
- Inter-individual Differences: The strength of circadian rhythms can vary between individuals. Analyze your data for "high-variability" and "low-variability" subgroups and check if they differ in other characteristics (e.g., age, genotype, baseline health).
- Clock Gene Polymorphisms: Genetic variations in core clock genes (e.g., CLOCK, BMAL1, PER) can lead to differences in circadian period and amplitude, potentially contributing to variable responses [37].
Q5: How can I experimentally determine if high variability is adaptive (like learning) or maladaptive (like system degradation)? This is a critical distinction. The following diagnostic table can help guide your experimental approach.
Table 3: Differentiating Adaptive vs. Maladaptive Variability
| Feature | Adaptive Variability | Maladaptive Variability |
|---|---|---|
| Temporal Pattern | Often temporary, decreasing as a new stable state is found (e.g., during skill learning) [61]. | Typically persistent or increasing over time. |
| Association with Performance | Positively correlated with long-term performance gains; a precursor to improvement [60] [61]. | Negatively correlated with performance level; associated with declining function [60]. |
| Physiological Correlates | Associated with exploration and neural plasticity. | Linked to neurological compromise, clinical conditions (e.g., dementia, brain injury), or aging [60]. |
| Experimental Test | Introduce a new task or challenge; if variability spikes and then drops as performance improves, it is likely adaptive. | Correlate variability with independent markers of health or system integrity; a negative correlation suggests maladaptation. |
Evidence and Efficacy: Validating Circadian Interventions Across Immune Applications
Frequently Asked Questions (FAQs)
Q1: Why would the time of day (morning vs. evening) affect the outcomes of CAR-T cell therapy? The effectiveness of immune cells, including T cells, is regulated by the body's internal 24-hour clock, known as the circadian rhythm. This rhythm influences key immune processes such as:
- Immune Cell Trafficking: The movement of T cells between the blood, bone marrow, and tissues varies throughout the day. One study found that T-helper cells and B cells showed significantly higher percentages in blood samples taken at 5 PM compared to 8 AM [19].
- Cell-intrinsic Clocks: Immune cells have their own molecular clocks that control their development, differentiation, and function. The transcription factor BMAL1, a core clock component, is essential for the development of certain immune lineages and regulates the expression of molecules that control cell migration [37] [17].
- Inflammatory Responses: The response to inflammatory challenges and the secretion of cytokines can be more or less intense depending on the time of day [37]. This is crucial given that Cytokine Release Syndrome (CRS) is a primary side effect of CAR-T therapy [63] [64] [65].
Q2: Is there any direct clinical evidence showing that CAR-T cell expansion is better at a specific time of day? As of the latest research, no direct clinical studies have been published that prospectively compare morning versus evening CAR-T cell infusion in patients. However, a key 2025 retrospective study provides an important insight: CAR-T cells are capable of robust expansion and can lead to superior outcomes even in patients who have no measurable disease (Complete Response) at the time of infusion [63]. This challenges the old paradigm that a large tumor antigen load is necessary to stimulate expansion and suggests that intrinsic biological factors, which could include circadian rhythms, play a significant role in CAR-T cell kinetics [63].
Q3: What are the key circadian-related variables I should control for in a pre-clinical study on infusion timing? To ensure valid and reproducible results, your experimental design should account for these critical factors:
- Time of Infusion: Strictly control and document the time of cell infusion.
- Light/Dark Cycles: Maintain a standardized light/dark cycle for your animal models (e.g., 12 hours light/12 hours dark) and time all procedures relative to the "zeitgeber" (the primary time cue, like light onset).
- Sample Collection Time: Collect all blood and tissue samples at consistent times to control for natural diurnal variation in cell counts [19] [37].
- Environmental Consistency: Minimize disruptions in noise, temperature, and handler presence during the resting phase.
Q4: What are the primary technical challenges in implementing time-of-day trials for CAR-T therapy? Implementing chronotherapy trials in a clinical setting presents several hurdles:
- Logistical Coordination: Scheduling leukapheresis, manufacturing, lymphodepletion, and infusion within a specific time window requires complex coordination across multiple hospital departments [66] [67].
- Standardization: It is difficult to standardize patient activities (sleep, meals) that can influence their personal circadian rhythms prior to infusion.
- Defining "Morning" and "Evening": There is no consensus on the optimal biological time points for infusion. Definitions may vary based on an individual's chronotype (e.g., "night owl" vs. "early bird").
- Regulatory Considerations: Clinical trial protocols would need to be specifically designed and justified to investigate infusion timing as a variable, which adds a layer of complexity.
Troubleshooting Guides
Issue 1: High Variability in CAR-T Cell Expansion Kinetics
Potential Cause: Uncontrolled diurnal variation in the host's immune environment at the time of infusion. The baseline level and trafficking patterns of key immune cells like T-helper cells and B cells fluctuate significantly between morning and evening [19]. Infusing CAR-T cells into a dynamically changing system can lead to inconsistent engagement and expansion.
Solution:
- Standardize Infusion Time: In your pre-clinical studies, administer all CAR-T cell infusions at a fixed time relative to the animal facility's light cycle (e.g., 2-3 hours after light onset for "morning" or after dark onset for "evening").
- Monitor Circadian Markers: Consider measuring baseline levels of cortisol or melatonin in patients, or using a gene expression assay on blood samples to determine the individual's circadian phase before infusion.
- Analyze by Time Cohort: In clinical data analysis, retrospectively group patients by their actual infusion time and compare outcomes (expansion peaks, CRS incidence, persistence) between morning and evening groups.
Issue 2: Inconsistent Pre-Clinical Results When Replicating CAR-T Studies
Potential Cause: Differences in the time of day when procedures (cell infusion, monitoring, sample collection) are performed across different labs or by different researchers. The migratory and functional capacity of T cells is under direct circadian control via genes like BMAL1 and CLOCK [37] [17].
Solution:
- Document Timing Meticulously: In your lab's Standard Operating Procedures (SOPs), explicitly state the time window for all critical experimental procedures, including the time of day for tumor implantation, CAR-T cell infusion, and blood/tissue collection.
- Control for Zeitgeber Time: Report all experimental times as "Zeitgeber Time" (ZT), where ZT0 is the start of the light cycle and ZT12 is the start of the dark cycle. This standardizes reporting across studies.
- Validate with 24-hour Sampling: In initial experiments, profile CAR-T expansion and related immune markers every 4-6 hours over a 24-hour period to identify the peak expansion time in your specific model.
Data Presentation: Key Circadian Findings in Immunology
Table 1: Diurnal Variations in Key Immune Cell Populations in Human Peripheral Blood Data adapted from a study using 25 µL fingertip blood samples from 8 participants at 8 AM and 5 PM [19].
| Immune Cell Type | Change at 5 PM (vs. 8 AM) | Statistical Significance | Potential Impact on CAR-T Function |
|---|---|---|---|
| T-helper (TH) Cells | Significantly Higher Percentage | Significant | Could influence helper signals for CAR-T expansion and persistence. |
| B Cells | Significantly Higher Percentage | Significant | May indicate a generally more active adaptive immune environment. |
| Natural Killer (NK) Cells | Significantly Lower Percentage | Significant | Reduced competition from innate lymphocytes might favor CAR-T engagement. |
| Cytotoxic T Cells | No Significant Change | Not Significant | Suggests baseline cytotoxic capacity may be stable. |
| Total T Cells | No Significant Change | Not Significant | Indicates a redistribution of subsets, not total numbers. |
Table 2: Core Circadian Clock Genes and Their Documented Roles in Immune Function Synthesized from reviews on circadian rhythm in immunity [37] [17].
| Clock Gene / Factor | Core Function in Circadian Circuit | Documented Role in Immune Cells |
|---|---|---|
| BMAL1 | Forms heterodimer with CLOCK; master transcriptional activator. | Regulates neutrophil and monocyte migration; deficiency impairs B cell development and antibody responses. |
| CLOCK | Forms heterodimer with BMAL1; drives expression of clock-controlled genes. | Influences T-helper 17 (Th17) cell differentiation. |
| PER/CRY | Protein complex that inhibits CLOCK/BMAL1 activity; provides negative feedback. | Inhibits inflammatory mediators in macrophages; deletion increases pro-inflammatory state. |
| REV-ERBα | Represses transcription of BMAL1; stabilizes the feedback loop. | Inhibits macrophage inflammation; agonists can reduce inflammatory gene expression. |
| NFIL3 | Regulates expression of D-box genes in the clock circuit. | Essential for development of Natural Killer (NK) cells and innate lymphoid cells. |
Experimental Protocols
Protocol: Assessing Diurnal Variation in CAR-T Cell Expansion In Vivo
Objective: To determine if the time of day of CAR-T cell infusion impacts its peak expansion, persistence, and anti-tumor efficacy in a mouse model.
Materials:
- Tumor-bearing immunodeficient mice (e.g., NSG).
- Prepared human CAR-T cells.
- Flow cytometer with appropriate antibodies (e.g., anti-human CD3, anti-CAR detection reagent).
- Microvette tubes for small-volume blood collection [19].
Methodology:
- Animal Housing: House mice under a strict 12-hour light/12-hour dark cycle for at least two weeks prior to the experiment. Perform all procedures during the designated time windows.
- Infusion Groups: Randomize mice into two groups:
- Group ZT3: Receive CAR-T cell infusion via tail vein at ZT3 (3 hours after light onset, "morning").
- Group ZT15: Receive CAR-T cell infusion at ZT15 (3 hours after dark onset, "evening").
- Include a control group receiving non-transduced T cells.
- Serial Blood Collection: At multiple time points post-infusion (e.g., days 5, 7, 10, 14), collect small-volume blood samples (e.g., ~25 µL from facial vein) [19]. Crucially, collect all samples from all groups at the same time of day (e.g., ZT4) to control for diurnal variation in sampling.
- Flow Cytometry Analysis: Lyse red blood cells and stain samples to identify and quantify the absolute count of human CAR-T cells in peripheral blood.
- Endpoint Analysis: At the end of the study, analyze tumor volume and harvest tissues (spleen, bone marrow, tumor) to assess CAR-T cell infiltration and persistence.
Protocol: Flow Cytometric Analysis of Low-Volume Blood Samples for Immune Monitoring
Objective: To track lymphocyte populations serially with minimal blood volume, enabling frequent sampling in pre-clinical models or vulnerable patients.
Methodology (Adapted from [19]):
- Blood Collection: Collect 25 µL of blood into a K3 EDTA Microvette tube via finger-prick, ear prick, or tail/retro-orbital bleeding in mice.
- Staining: Transfer 25 µL of blood to a FACS tube. Add 5 µL of the desired antibody cocktail (e.g., CD3, CD4, CD8, CD45, CD19). The volumes of antibody and blood are reduced to 1/4 of typical protocol volumes.
- Incubation: Incubate for 20 minutes at room temperature, protected from light.
- Lysis: Add 500 µL of 1x red blood cell lysing solution. Incubate for 10 minutes at room temperature.
- Wash: Centrifuge at 200g for 5 minutes at 4°C. Discard the supernatant.
- Resuspension: Wash the cell pellet with 500 µL PBS, centrifuge again, and resuspend in 125 µL of a stabilizing solution (PBS with 2% FBS and 0.1% sodium azide) for flow cytometric analysis.
Signaling Pathways and Experimental Workflows
Circadian-Immune Signaling Pathway
CAR-T Timing Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Investigating Circadian Rhythms in CAR-T Cell Therapy
| Item | Function/Application in Research | Example/Note |
|---|---|---|
| Polychromatic Flow Cytometry Panel | To simultaneously identify CAR-T cells and various endogenous immune cell subsets (T, B, NK cells) in low-volume samples. | Antibodies against human/mouse CD3, CD4, CD8, CD19, CD45, CD56, and a CAR detection reagent [19] [68]. |
| K3 EDTA Microvette Tubes | For consistent and reliable collection of small-volume blood samples for serial monitoring. | Enables collection of 25-200 µL volumes, minimizing stress from repeated blood draws in pre-clinical models [19]. |
| Clock Gene Reporter Kits | To visualize and quantify the activity of circadian clock genes (e.g., BMAL1, PER2) in immune cells in vitro. | Includes luciferase constructs or fluorescent reporters under the control of clock gene promoters. |
| Environmental Control Chambers | To house animals under rigorously controlled light, temperature, and humidity conditions, which is fundamental for circadian studies. | Must allow for programmable 12h:12h light/dark cycles and have provisions for "dark" procedures under red light. |
| RT-qPCR Assays for Core Clock Genes | To measure the rhythmic mRNA expression of key circadian regulators (Bmal1, Clock, Per1/2, Cry1/2, Rev-erbα) in isolated cells. | Requires careful timing of sample collection across the 24-hour cycle. |
FAQs and Troubleshooting Guides
FAQ 1: How does the time of day affect COVID-19 vaccine effectiveness?
Answer: Significant diurnal variations in COVID-19 vaccine effectiveness exist. A large-scale retrospective cohort study (n=1,515,754) found the rate of breakthrough infections was lowest when vaccinations were administered between late morning and early afternoon, and highest with evening vaccination [69]. The relationship between vaccination time and breakthrough infection risk was sinusoidal, consistent with an underlying biological rhythm. The peak-to-trough change in hazard ratio (HR) for breakthrough infection was 8.6% to 25%, depending on the vaccine dose [69]. For the second booster dose, morning vaccination was significantly associated with reduced COVID-19 hospitalizations (HR = 0.64, morning vs. evening) [69]. The benefits of daytime vaccination were most pronounced in younger (<20 years) and older (>50 years) individuals [69].
FAQ 2: What is the optimal seasonal timing for influenza and COVID-19 boosters?
Answer: Optimal timing aims to align peak vaccine effectiveness with the period of greatest respiratory virus risk [70]. For COVID-19, a personalized approach is recommended. The best time for a booster depends on geographic location and individual infection history, but generally falls in early autumn for the Northern Hemisphere [71]. Administration in September or October can provide three to four times more protection against infection compared to later boosters [71]. For most at-risk populations, co-administration of COVID-19 and influenza vaccines at a single routine visit ahead of the respiratory virus season is considered optimal [70]. This strategy helps ensure protection is established before the season begins while mitigating the risk of immunity waning before the season ends [70].
FAQ 3: What are the primary methodological challenges in studying vaccination chronoefficacy?
Answer: Key challenges include:
- Confounding Variables: Differences in baseline infection risk, occupation, or household size between groups vaccinated at different times can confound results. Careful statistical adjustment for age, sex, and comorbidities is crucial, and analyzing infection rates prior to vaccine effectiveness (e.g., within 14 days of the first dose) can help rule out baseline risk differences [69].
- Immune Readouts: Using appropriate immune markers is essential. Antibody responses wane more rapidly than T-cell immunity, which may provide more durable protection against severe disease [70]. Studies relying solely on antibody titers as a surrogate may not fully capture the clinical effectiveness modulated by circadian rhythms [69].
- Sample Collection Timing: Diurnal variations in lymphocyte prevalence (e.g., higher TH and B cell percentages at 5 PM vs. 8 AM) can affect immune measurements if sample collection times are not standardized [19]. Using small-volume finger-prick blood collections can improve participant acceptability for multi-timepoint studies [19].
FAQ 4: Which patient factors most influence optimal vaccination timing?
Answer: Age and comorbidity status are the most significant factors.
- Age: Advancing age is the strongest predictor of severe outcomes from COVID-19 and influenza [70]. Older adults (≥75 years) and the immunocompromised may exhibit weaker and more rapidly waning immune responses to vaccination, necessitating tailored timing and dosing strategies [70] [69].
- Comorbidities: Conditions like obesity, diabetes, chronic respiratory, and cardiovascular diseases increase the risk of severe outcomes from respiratory viruses [70]. The presence of comorbidities can be associated with impaired immune responses to vaccination, suggesting these groups may benefit from more precise vaccination timing closer to the virus season [70].
Table 1: COVID-19 Vaccine Effectiveness by Time of Administration
| Vaccine Dose | Comparison Group (Time of Day) | Hazard Ratio (HR) for Breakthrough Infection | Key Outcome Measures |
|---|---|---|---|
| Doses 1 & 2 [69] | Late Morning/Early Afternoon vs. Evening | Sinusoidal HR pattern | Peak-to-trough change in HR: 0.13 (8.6-25% relative change in VE) |
| Dose 3 (First Booster) [69] | Late Morning/Early Afternoon vs. Evening | Sinusoidal HR pattern | Peak-to-trough change in HR: 0.086 |
| Dose 4 (Second Booster) [69] | Morning (800-1159) vs. Evening (1600-1959) | HR = 0.64 | COVID-19-associated hospitalizations (95% CI: 0.43-0.97) |
| Dose 4 (Second Booster) [69] | Late Morning/Early Afternoon vs. Evening | Sinusoidal HR pattern | Peak-to-trough change in HR: 0.25 |
Table 2: Interim 2024-2025 COVID-19 Vaccine Effectiveness (VE)
| Population | Outcome | VE Estimate (95% CI) | Days Post-Vaccination |
|---|---|---|---|
| Adults ≥18 years [72] | COVID-19-associated ED/UC Visit | 33% (28%–38%) | 7–119 days |
| Immunocompetent Adults ≥65 years [72] | COVID-19-associated Hospitalization | 45% (36%–53%) | 7–119 days |
| Immunocompetent Adults ≥65 years [72] | COVID-19-associated Hospitalization | 46% (26%–60%) | 7–119 days |
| Adults ≥65 years with Immunocompromise [72] | COVID-19-associated Hospitalization | 40% (21%–54%) | 7–119 days |
Table 3: Diurnal Variation in Circulating Lymphocyte Prevalence
| Cell Type | 8 AM Sample | 5 PM Sample | Significance |
|---|---|---|---|
| TH cells [19] | Lower Percentage | Higher Percentage | Significant (P < 0.05) |
| B cells [19] | Lower Percentage | Higher Percentage | Significant (P < 0.05) |
| NK cells [19] | Higher Percentage | Lower Percentage | Significant (P < 0.05) |
| Cytotoxic T cells [19] | No significant change | No significant change | Not Significant |
| T cells [19] | No significant change | No significant change | Not Significant |
| Leukocytes [19] | No significant change | No significant change | Not Significant |
Experimental Protocols
Protocol 1: Assessing Diurnal Variation in Lymphocyte Populations Using Small-Volume Blood Collection
Application: This protocol is for tracking diurnal immune cell fluctuations in studies investigating chronoefficacy, using a less invasive method [19].
Detailed Methodology:
- Participant Recruitment and Sampling: Recruit healthy volunteers. Collect a minimum of 225 µL of finger-prick blood using safety lancets into K3 EDTA Microvette tubes at two time points (e.g., 8 AM and 5 PM) on the same day [19].
- Staining for Flow Cytometry: Use a commercial lymphocyte kit (e.g., IMK Simultest). Adapt the manufacturer's protocol for small volumes: use 25 µL of blood and 5 µL of antibody reagent. Add conjugated antibodies and incubate for 20 minutes at room temperature [19].
- Red Blood Cell Lysis and Washing: Lyse red blood cells using 500 µL of 10x lysing solution for 10 minutes at room temperature. Centrifuge at 200g for 5 minutes at 4°C and discard the supernatant. Wash the cell pellet with 500 µL of phosphate-buffered saline (PBS), centrifuge again, and discard the supernatant [19].
- Resuspension and Analysis: Resuspend the final cell pellet in 125 µL of an appropriate solution (e.g., PBS with 2% fetal bovine serum). Analyze samples on a flow cytometer (e.g., BD FACSVerse). Use forward scatter/side scatter to gate on lymphocytes and use fluorescence parameters to identify specific cell subsets (T cells, B cells, NK cells, etc.) [19].
- Statistical Analysis: Analyze paired data (e.g., AM vs. PM from the same participant) using a paired, two-tailed t-test. A p-value of less than 0.05 is typically considered significant [19].
Protocol 2: Analyzing Large-Scale Observational Data for Vaccine Chronoefficacy
Application: This methodology outlines how to use real-world healthcare data to investigate associations between vaccine administration time and clinical outcomes [69].
Detailed Methodology:
- Cohort Definition and Data Source: Define a large retrospective cohort from a healthcare provider database. Include patients with timestamped vaccinations and laboratory-confirmed COVID-19 test results. Exclude immunizations given outside a defined daily window (e.g., 8 AM-8 PM) and those with invalid data [69].
- Exposure and Outcome Definition: The exposure is the time of day of vaccine administration, categorized into bins (e.g., morning: 800-1159; afternoon: 1200-1559; evening: 1600-1959). The primary outcome is a breakthrough infection, defined as a positive SARS-CoV-2 test result ≥7 days after the final vaccine dose in a series. Secondary outcomes can include COVID-19-associated emergency department visits and hospitalizations [69].
- Statistical Analysis: Use Cox proportional hazards regression to model the time to breakthrough infection, adjusting for covariates like age, sex, and number of comorbidities. Model the relationship between vaccination time (as a continuous variable) and the hazard ratio for breakthrough infection to test for a sinusoidal pattern. Perform subgroup analyses by age and vaccine dose [69].
Visualizations
Circadian Rhythm in Vaccine Effectiveness
Diurnal Lymphocyte Sampling Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Chronoefficacy Research
| Item | Function/Application | Specific Example |
|---|---|---|
| Polychromatic Flow Cytometry Kit | Simultaneous identification and quantification of multiple lymphocyte subsets (T cells, B cells, NK cells) from small blood volumes. | IMK Simultest: Lymphocyte Kit (Becton Dickinson) [19] |
| Small-Volume Blood Collection System | Enables repeated, minimally invasive diurnal sampling for immune cell profiling. | K3 EDTA Microvette tubes (e.g., from Sarstedt Group) [19] |
| Safety Lancets | Device for obtaining finger-prick blood samples. | Single-use safety lancets [19] |
| Flow Cytometer | Instrument for analyzing stained cell populations based on light scattering and fluorescence. | BD FACSVerse (Becton Dickinson) [19] |
| Red Blood Cell Lysing Solution | Reagent for removing red blood cells from whole blood prior to flow cytometry. | 10x concentrated lysing solution [19] |
| Real-World Health Data Repository | Large-scale, timestamped data on vaccinations, infections, and clinical outcomes for observational studies of chronoefficacy. | Data from large Health Maintenance Organizations (HMOs) [69] |
What are immune age metrics, and why is their temporal stability important for my research?
Immune age metrics, such as the IMMAX score, are composite measures derived from flow cytometry data that aim to quantify the functional state of an individual's immune system, a process known as immunosenescence. Rather than simply reflecting chronological age, these metrics seek to capture biological age, providing a more accurate indicator of immune health and associated disease risk [73] [74]. In the context of a thesis focused on managing intraindividual variation, the temporal stability of these metrics is paramount. A clinically or scientifically useful metric must demonstrate reliability over time, meaning it should reflect stable, underlying biological traits rather than short-term fluctuations. Understanding its stability directly informs how often you need to measure it to obtain a reliable assessment of an individual's immune status and determines its power to predict long-term health outcomes [75] [76].
Key Concepts and Technical FAQs
FAQ 1: What is the difference between intra-individual and inter-individual variation, and why does it matter?
- Inter-individual variation refers to the differences in a specific immune parameter (e.g., IMMAX score, IL-6 level) between different people in a population. This variation is what allows you to stratify individuals into high-risk or low-risk groups.
- Intra-individual variation refers to the fluctuations in that same immune parameter within a single person over time. These fluctuations can be due to diurnal rhythms, recent infections, exercise, or other transient environmental exposures [76] [77].
Why it matters: Excessive intra-individual variation can obscure true inter-individual differences. If a metric has high intra-individual variation, a single measurement may not accurately represent that person's typical immune status, leading to misclassification in research and clinical settings. Effectively managing this intra-individual "noise" is critical for detecting the true "signal" of stable immune age [77].
FAQ 2: How do diurnal rhythms specifically impact immune measures relevant to immune age?
The human immune system exhibits strong circadian rhythms. Key cell populations and inflammatory mediators show predictable fluctuations throughout the day, which must be controlled for in study design.
- Immune Cells: Studies using small-volume finger-prick blood samples have confirmed that T-helper (TH) cells and B cells show significantly higher percentages in the afternoon (5 PM) compared to the morning (8 AM), while Natural Killer (NK) cells demonstrate a higher percentage in the morning [19].
- Inflammatory Proteins: Core body temperature and immune proteins like IL-6 and HSP70 also show diurnal variation, often peaking in the evening [21].
Troubleshooting Tip: The most effective way to mitigate diurnal variation is to standardize the time of day for all blood sample collections in your longitudinal study, ideally collecting all samples within a narrow time window in the morning.
FAQ 3: Over what timeframes can I expect immune age metrics to be stable?
The stability of biological markers generally decreases as the time between measurements increases. A large meta-analysis on inflammatory markers provides a useful framework for expectations [75]:
| Time Interval | Typical Stability (Correlation Coefficient) | Recommendation for Measurement |
|---|---|---|
| < 6 Months | Strong to Moderate (r = 0.80 - 0.61) | A single measure may be adequate. |
| 6 Months - 3 Years | Modest to Moderate (r = 0.60 - 0.51) | Repeated measures are recommended. |
| > 3 Years | Low (r = 0.39 - 0.30) | Repeated measures are absolutely necessary. |
While this data is for single inflammatory markers, it underscores a fundamental principle: for reliable assessment of stable traits over intervals longer than 6 months, planning for repeated measurements is crucial to account for temporal decay in reliability [75].
Experimental Protocols for Assessing Temporal Stability
Protocol 1: Longitudinal Study Design for Metric Validation
This protocol is designed to empirically test the temporal stability of an immune metric like the IMMAX score in your cohort.
Objective: To determine the test-retest reliability and long-term stability of an immune age metric.
Materials:
- See "Research Reagent Solutions" table below.
- Clinical database for participant metadata.
Methodology:
- Cohort Recruitment: Recruit a cohort of healthy volunteers that reflects the demographic range (age, sex) of your intended study population.
- Baseline Blood Draw: Collect a baseline blood sample via venipuncture under standardized conditions (e.g., morning, after fasting).
- Sample Processing: Isolate Peripheral Blood Mononuclear Cells (PBMCs) using density gradient centrifugation (e.g., Ficoll-Paque) within 2 hours of collection [73] [78].
- Immune Phenotyping: Stain the PBMCs with a pre-optimized panel of fluorescently conjugated antibodies. The panel must include antibodies to identify the T-cell subsets (e.g., CD4, CD8, CD45RA, CD197/CCR7) and other cell populations required to calculate the IMMAX score [73].
- Flow Cytometry Acquisition: Acquire data on a flow cytometer, ensuring consistent instrument settings and performance across all time points using calibration beads.
- Longitudinal Sampling: Repeat steps 2-5 at pre-defined intervals. A robust design includes:
- Short-term stability: Repeat sampling at 1 week and 1 month to assess the impact of minor environmental fluctuations.
- Medium-term stability: Repeat sampling at 6 months and 1 year.
- Long-term stability: Consider sampling at 2+ years [78].
- Data Analysis:
- Calculate the IMMAX score for each participant at each time point.
- Use intraclass correlation coefficients (ICC) to quantify test-retest reliability. ICC values >0.75 are generally considered excellent, 0.60-0.74 good, and below 0.60 indicate poor stability for individual-level assessment [75].
Protocol 2: Controlling for Diurnal Variation in Immune Cell Counts
Objective: To confirm and control for the effect of time-of-day on immune cell subsets in your specific laboratory setup.
Methodology:
- Participant Selection: Recruit a small sub-cohort (e.g., n=8-10).
- Sample Collection: Collect blood samples from each participant at two time points on the same day: once in the morning (e.g., 8 AM) and once in the late afternoon (e.g., 5 PM) [19].
- Sample Processing & Analysis: Process all samples identically and immediately using your standard immune phenotyping protocol.
- Statistical Testing: Use a paired Student's t-test (or non-parametric equivalent) to compare the prevalence of key lymphocyte subsets (T cells, B cells, NK cells) between the morning and afternoon samples. This validates the need for time-standardization in your main study [19].
The following workflow diagram summarizes the key steps for conducting a temporal stability study:
Troubleshooting Guide
| Problem | Potential Cause | Solution |
|---|---|---|
| High intra-individual variability in metric across all participants. | Poorly controlled diurnal rhythms; acute infections; inconsistent sample processing. | Standardize time of blood draw; questionnaire to exclude recent illness; strict SOPs for lab workflow. |
| Low correlation between repeated measures (low ICC). | The metric itself is inherently sensitive to short-term environmental fluctuations; measurement error. | Increase the number of repeated measurements per subject and use the average; validate flow cytometry panel for precision. |
| Unexpected drift in population average metric over time. | Batch effect from reagent lot changes or flow cytometer drift. | Use internal control samples (e.g., frozen PBMCs) across batches; regular instrument calibration. |
| Inability to reproduce published stability findings. | Differences in cohort demographics (age, health status) or technical methods. | Re-calibrate the metric (IMMAX) to your local population and specific lab protocols [73]. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Experiment | Technical Notes |
|---|---|---|
| Fluorochome-conjugated Antibodies | Tag specific cell surface proteins (e.g., CD3, CD4, CD8, CD45RA, CD28) for cell population identification via flow cytometry. | Panel design requires careful compensation controls; validate clones and titers for consistency; be aware of vendor/lot changes [73] [76]. |
| PBMC Isolation Tubes | (e.g., CPT tubes or Ficoll-Paque) Separate mononuclear cells from whole blood via density gradient centrifugation. | Process samples promptly (within 2-4 hours of draw) to maintain cell viability and surface epitopes [73]. |
| Flow Cytometer | Analytical instrument that counts and characterizes individual cells based on fluorescence and light scattering. | Perform daily quality control with calibration beads; ensure consistent laser power and detector settings throughout the study [19] [76]. |
| Variance Components Analysis | A statistical linear mixed-effects model used to partition total variance into technical, intra-individual, and inter-individual components. | Critical for quantifying what proportion of variance is true, stable signal vs. noise [76] [79]. |
| ELISA Kits | Quantify soluble immune markers like IL-6, CRP, or HSP70 in plasma/serum to complement cellular data. | Can be used to add a protein-level dimension to the stability assessment; follow manufacturer protocols precisely [21]. |
The following diagram illustrates the core conceptual relationship between different types of variation and the resulting composite metric:
This technical support article provides a framework for managing intraindividual variation caused by diurnal rhythms in immune studies. We detail common experimental challenges, provide step-by-step protocols for key circadian immune assessments, and visualize critical pathways to enhance research reproducibility across autoimmunity and cancer immunotherapy contexts.
The human immune system demonstrates robust circadian rhythms—biological cycles with a period of approximately 24 hours—that critically influence its function [80]. These rhythms are not merely observed behaviors but are endogenously generated by a molecular clock present in most cells, including immune cells [81] [82]. In the context of disease and treatment, understanding these rhythms is paramount. For example, in cancer, disrupted circadian signaling is an enabling characteristic that tumors use to facilitate their initiation, growth, and progression, including the acquisition of the hallmark of avoiding immune destruction [82]. Conversely, in autoimmunity, the same circadian signals that prime immune responses during the active phase can potentially exacerbate undesirable immune attacks on self-tissues.
This article establishes a technical support framework for researchers grappling with the confounding effects of diurnal variation in immune studies. We provide troubleshooting guides, experimental protocols, and data interpretation tools grounded in the broader thesis that rigorously controlling for and exploiting intraindividual diurnal variation is essential for generating reliable, reproducible data in both basic immunology and translational drug development.
Frequently Asked Questions (FAQs) on Circadian Immunology
Q1: Why is the timing of sample collection so critical in immune studies?
The composition and function of the immune system fluctuate predictably over the 24-hour day. For instance, circulating counts of various lymphocyte subsets show significant diurnal variation [19]. One study found that T helper (TH) cells and B cells showed significantly higher percentages in the afternoon (5 PM) compared to the morning (8 AM), while Natural Killer (NK) cells demonstrated a significantly higher morning percentage [19]. Failing to standardize collection times can therefore introduce substantial variability, masking true treatment effects or creating false positives.
Q2: What is the difference between "diurnal" and "circadian" rhythm?
A diurnal rhythm is a daily rhythm that is synchronized with the time of day, but it may be driven by external cues (e.g., the sleep/wake cycle or feeding) [19] [80]. A circadian rhythm is an endogenous, self-sustaining biological rhythm with a period of approximately 24 hours, which persists even in the absence of external time cues [80]. In practice, most observed daily ("diurnal") rhythms in immune parameters are a combination of the underlying endogenous circadian rhythm and evoked responses from behaviors like sleep and eating [80].
Q3: How can circadian rhythms impact responses to cancer immunotherapy?
Emerging evidence links circadian signals to tumor immunogenicity and response to immune checkpoint inhibitors (ICIs) [82]. For example, in breast cancer patients, distinct circadian rhythm subtypes are associated with different tumor immune microenvironments. A "low circadian rhythm" subtype was characterized by highly enriched immune-related pathways, high immune cell infiltration, and high anti-tumor immunity, suggesting these patients might be more likely to benefit from ICB treatment [83]. Preclinical models also show that chronic circadian disruption can drive metastasis by modulating the immune microenvironment [82].
Q4: What are the key sources of intraindividual variation in circadian immune studies?
Major sources of variation include:
- Time of Day: The primary variable of interest [19] [21].
- Sleep/Wake and Fasting/Feeding Cycles: These behaviors are potent "masking" factors that can obscure the underlying circadian signal if not controlled [80].
- Light Exposure: Light is the primary "zeitgeber" (time-giver) for the central clock in the suprachiasmatic nucleus (SCN). Irregular light exposure can desynchronize rhythms [80] [21].
- Glucocorticoid Levels: These stress hormones, which have a strong circadian rhythm, are powerful immunomodulators [81] [82].
Troubleshooting Guides for Common Experimental Issues
Problem: Inconsistent Immune Cell Counts in Flow Cytometry
| Potential Cause | Solution | Underlying Principle |
|---|---|---|
| Variable Sample Collection Times | Standardize blood draw or tissue collection times across all subjects/cohorts. Record exact time. | Immune cell prevalence in circulation demonstrates high-amplitude circadian rhythmicity [19] [21]. |
| Improper Sample Handling | Process all samples with the same delay after collection. Use consistent lysis and staining protocols. | Cell surface marker expression and viability can degrade over time, potentially at rates influenced by circadian factors. |
| Unaccounted for Subject Chronotype | Record subject sleep/wake schedules using logs or actigraphy. Consider grouping by chronotype. | An individual's chronotype (e.g., "morning lark" vs. "night owl") affects the precise timing of their peak immune rhythms [80]. |
Problem: High Background in Immunohistochemistry (IHC) of Immune Markers
| Potential Cause | Solution | Underlying Principle |
|---|---|---|
| Inadequate Blocking | Use a buffer containing 5-10% normal serum from the host species of the secondary antibody. Ensure blocking time is sufficient (10-30 mins) [84]. | Serum proteins preemptively occupy non-specific binding sites on the tissue, preventing subsequent antibodies from non-specifically adsorbing [84]. |
| Endogenous Enzyme Activity | For HRP-based detection, quench slides in a 3% H2O2 solution for 10 minutes prior to primary antibody incubation [85] [84]. | Tissues like liver and kidney contain endogenous peroxidases that can catalyze the chromogen, creating false-positive signals [85]. |
| Antibody Cross-Reactivity or Over-concentration | Titrate the primary antibody to determine the optimal concentration. Use a validated, IHC-optimized antibody. | Excessive antibody concentration increases the chance of non-specific binding to off-target antigens or structures [84]. |
Detailed Experimental Protocols
Protocol: Assessing Diurnal Variation in Circulating Lymphocytes via Flow Cytometry
This protocol, adapted from [19], allows for the detection of diurnal immune variation using small blood volumes, ideal for longitudinal studies in mice or humans.
Key Research Reagent Solutions:
- Anticoagulant Tubes: K3 EDTA tubes (e.g., Microvette 200 μL) for blood collection.
- Lymphocyte Staining Kit: A pre-configured kit (e.g., IMK Simultest: Lymphocyte Kit) containing fluorochrome-conjugated antibodies against CD3, CD19, CD4, CD8, CD16, CD56.
- Staining Buffer: Phosphate Buffered Saline (PBS) with 2% Fetal Bovine Serum (FBS) and 0.1% sodium azide.
- Lysing Solution: 10x red blood cell lysing solution.
- Viability Stain: Propidium Iodide (PI) or similar.
Methodology:
- Sample Collection:
- Collect finger-prick or venous blood (e.g., 225 μL) at pre-determined circadian times (e.g., 8 AM and 5 PM) into EDTA tubes [19].
- CRITICAL: Maintain consistent collection timing, lighting conditions, and subject fasting state across the entire study.
- Cell Staining:
- Aliquot 25 μL of whole blood into a staining tube.
- Add 5 μL of the pre-mixed antibody cocktail. Vortex gently and incubate for 20 minutes at room temperature in the dark.
- Red Blood Cell Lysis:
- Add 500 μL of 1x red blood cell lysing solution. Vortex and incubate for 10 minutes at room temperature in the dark.
- Centrifuge at 200-250g for 5 minutes at 4°C. Carefully decant the supernatant.
- Wash and Resuspend:
- Wash the cell pellet with 500 μL of staining buffer, centrifuge, and decant the supernatant.
- Resuspend the final pellet in 125-200 μL of staining buffer containing a viability dye like PI.
- Data Acquisition and Analysis:
- Acquire data on a flow cytometer within a few hours.
- Use forward/side scatter to gate on lymphocytes, exclude doublets and dead cells, and then analyze the prevalence of specific immune subsets (e.g., CD3+ T cells, CD19+ B cells, CD16+/CD56+ NK cells) [19].
Protocol: Circadian Immune Phenotyping of Tumor Tissue via IHC
This protocol allows for the spatial analysis of immune cell infiltration in tumor tissue, which can be correlated with circadian time or circadian gene expression in the tissue [83].
Key Research Reagent Solutions:
- Fixative: 10% Neutral Buffered Formalin.
- Antigen Retrieval Buffer: 1x Sodium Citrate buffer, pH 6.0, or Tris-EDTA buffer, pH 9.0.
- Blocking Solution: 1X TBST with 5% Normal Goat Serum (or serum matching the secondary antibody host species).
- Primary Antibodies: Validated, IHC-optimated antibodies against immune markers (e.g., CD8 for cytotoxic T cells, CD4 for helper T cells, CD68 for macrophages) and optionally, circadian proteins (e.g., BMAL1, PER2).
- Detection System: Polymer-based HRP detection system (e.g., SignalStain Boost IHC Detection Reagents) and DAB Substrate Kit [85].
Methodology:
- Tissue Preparation:
- Fix tissue samples in 10% neutral buffered formalin for 18-24 hours at room temperature.
- Process tissue through ethanol dehydration, xylene clearing, and paraffin embedding. Section at 4-5 μm thickness.
- Deparaffinization and Hydration:
- Bake slides at 60°C for 2 hours. Then, pass through fresh xylene (2 changes, 5-10 mins each) and graded ethanol (100%, 95%, 80%, 70%) to deparaffinize and hydrate sections. Rinse in deionized water [84].
- Antigen Retrieval:
- Perform heat-induced epitope retrieval (HIER) by incubating slides in pre-heated sodium citrate buffer (pH 6.0) in a microwave oven, pressure cooker, or water bath until steaming, then maintain sub-boiling temperature for 10-20 minutes [85]. The retrieval method and buffer must be optimized for the specific antibody.
- Immunostaining:
- Peroxidase Quenching: Incubate slides with 3% H2O2 for 10 minutes to block endogenous peroxidase activity.
- Blocking: Incubate with blocking solution for 30 minutes at room temperature.
- Primary Antibody: Apply diluted primary antibody and incubate overnight at 4°C or for 1-2 hours at room temperature.
- Washing: Wash slides 3 times for 5 minutes with TBST or PBS.
- Polymer Detection: Apply polymer-HRP conjugate for 30 minutes at room temperature. Wash again.
- Color Development: Incubate with fresh DAB solution, monitoring color development under a microscope. Stop the reaction by immersing in deionized water once specific staining is clear.
- Counterstaining and Analysis:
- Counterstain with Hematoxylin, dehydrate, clear in xylene, and mount with a coverslip.
- Quantify immune cell infiltration (e.g., number of CD8+ T cells per mm2) using light microscopy and image analysis software.
Data Presentation: Summarizing Quantitative Diurnal Variations
The following table summarizes exemplary quantitative data on diurnal immune variations, as reported in the literature. This can serve as a reference for researchers interpreting their own findings.
Table 1: Exemplary Diurnal Variations in Key Immune Parameters
| Immune Parameter | Morning Level (approx. 8 AM) | Evening Level (approx. 5-6 PM) | Magnitude and Direction of Change | Context / Notes |
|---|---|---|---|---|
| NK Cell Prevalence [19] | Higher Percentage | Lower Percentage | Decrease by afternoon | In healthy human finger-prick blood. |
| T Helper (TH) Cells & B Cell Prevalence [19] | Lower Percentage | Higher Percentage | Increase by afternoon | In healthy human finger-prick blood. |
| Total White Blood Cells (WBC) [21] | Lower Concentration | Higher Concentration | Increase by evening (in athletes post-exercise). | Post-exercise in hot, humid conditions. |
| Plasma IL-6 [21] | Lower Concentration | Higher Concentration | More pronounced increase post-exercise in evening. | Post-exercise in hot, humid conditions. |
| Core Body Temperature [21] | Lower | Higher | Increase by evening; more pronounced response to morning exercise. | A key driver of many physiological rhythms. |
Visualization of Pathways and Workflows
Circadian-Immune Axis in Disease and Therapy
This diagram illustrates the core relationship between the circadian system, immune function, and its implications for autoimmunity and cancer immunotherapy.
Workflow for a Diurnal Variation Immune Study
This workflow outlines the key steps for designing and executing a robust study investigating diurnal immune variation.
Troubleshooting Guides & FAQs
Common Experimental Challenges and Solutions
Problem: High Intraindividual Variability in Immune Cell Counts
- Question: "My flow cytometry data shows high day-to-day variation in leukocyte subsets from the same subject, complicating data interpretation. What could be the cause?"
- Solution: This is a classic sign of unaccounted-for circadian rhythm. Immune cell trafficking and distribution are under strong circadian control [86]. Implement time-stamping for all sample collections. Restrict sample collection to a narrow time window (e.g., within a 2-hour period) for each participant across all study visits to control for diurnal variation.
Problem: Inconsistent Response to Immune Stimulation
- Question: "The response of isolated immune cells to stimulation (e.g., with LPS or PHA) is inconsistent between experiments run on different days."
- Solution: The intrinsic responsiveness of immune cells varies dramatically over the 24-hour cycle [86]. The time of cell isolation and subsequent stimulation is a critical, often overlooked, experimental variable. Isolate and stimulate cells at a standardized circadian time. If working with human samples, collect blood at the same clock time for all stimulation assays.
Problem: Failure to Replicate Animal Immunology Studies
- Question: "We are unable to replicate the findings of a published murine immunology study, despite using the same strain and treatment."
- Solution: The timing of interventions relative to the animals' light/dark cycle is a major confounding factor. Mice are nocturnal; their "day" is our night. Conduct procedures at the same Zeitgeber Time (ZT) in all experiments, where ZT0 is lights-on and ZT12 is lights-off. Always report experimental times as ZT in publications.
Problem: Unstable Biomarker Measurements
- Question: "Measurements of inflammatory cytokines like IL-6 in plasma show high variability, even in healthy, fasted participants."
- Solution: Cytokine production and release are regulated by the circadian clock [86]. Factors like sleep disruption or misaligned meal timing can significantly alter rhythms. Control for lifestyle zeitgebers: enforce consistent sleep-wake schedules and standardized meal times for participants in study protocols to stabilize circadian rhythms and reduce biomarker noise [87].
Frequently Asked Questions (FAQs)
Q1: What is the strongest evidence that circadian optimization has a clinical economic impact? A1: Strong real-world evidence comes from oncology. Multiple retrospective studies have shown that the timing of Immune Checkpoint Inhibitor (ICI) infusions significantly impacts patient survival at no additional drug cost. For instance, in metastatic non-small cell lung cancer (mNSCLC), patients receiving nivolumab infusions before 12:54 had a 4-fold longer overall survival (OS) compared to those treated later in the day [88]. Optimizing infusion schedules is a zero-cost intervention with profound benefits.
Q2: How can I quantify intraindividual circadian variability in my pilot study? A2: For human studies, use actigraphy (wearable activity monitors) to track rest-activity cycles over at least 7-14 days [89]. The variability in the timing of sleep onset/offset or the fragmentation of rhythms can be calculated. In biochemical studies, take sequential samples (e.g., saliva cortisol) to calculate the intraindividual cortisol variability (ICV), which has been shown to be reduced by stress management interventions, indicating a more stable rhythm [90].
Q3: We don't have a chronobiology core facility. What is the simplest first step to implement? A3: The most impactful and simplest step is strict time-stamping. Record the clock time of every biological procedure: sample collection, drug administration, behavioral test, and tissue harvesting. This allows for a post-hoc analysis of time-of-day effects and is the foundational practice of circadian research.
Q4: Are the effects of circadian timing just about sleep? A4: No. While sleep is a key circadian output, the molecular clock operates in virtually every nucleated cell, including immune cells [86]. Effects persist even in the absence of sleep. Circadian rhythms regulate fundamental processes like gene expression (e.g., clock genes like BMAL1 and PER), metabolite availability, and hormone levels (e.g., cortisol and melatonin), all of which independently influence immune function [86] [88].
Table 1: Summary of Clinical Outcomes from Time-of-Day Dependent Immunotherapy
| Cancer Type | Treatment | Optimal Timing | Key Efficacy Finding | Hazard Ratio (HR) [95% CI] |
|---|---|---|---|---|
| mNSCLC [88] | Nivolumab | Before 12:54 | 4x longer Overall Survival (OS) & Progression-Free Survival (PFS) | OS: 0.174 [0.082–0.370] |
| mNSCLC [88] | Pembrolizumab | Before 11:45 (initial infusions) | 2-year survival: 65% (Early) vs. 38% (Late) | OS: 0.28 [0.13–0.64] |
| mNSCLC [88] | Mixed ICIs | Before 11:37 | Median OS: 30.3 months (Early) vs. 15.9 months (Late) | - |
| mNSCLC [88] | Initial 4 ICI infusions | At least one before noon | Median OS: 16.1 months (Early) vs. 7.4 months (Late) | OS: 0.54 [0.35–0.84] |
| Metastatic Melanoma [88] | Ipilimumab (first-line) | Before 16:30 (≤20% after) | 20% improved 5-year OS rate | - |
Table 2: Association Between Rhythm Variability and Health Outcomes
| Condition / Intervention | Variable Measured | Impact of Reduced Variability / Intervention | Citation |
|---|---|---|---|
| Women at risk for breast cancer | Intraindividual Cortisol Variability (ICV) | Cognitive Behavioral Stress Management (CBSM) significantly reduced ICV, suggesting a more stable, healthier rhythm. | [90] |
| Bipolar & Borderline Personality Disorder | Mood & Diurnal Rhythms (Activity/Heart Rate) | Greater variability in objective diurnal physiology was correlated with greater subjective mood instability. | [91] |
| General Population | Positive Affect (PA) & Sleep | More variable sleep quality and duration were linked to more variable and lower positive affect. | [92] |
Detailed Experimental Protocols
Protocol 1: Implementing a Circadian-Optimized Animal Study
Objective: To evaluate a drug's efficacy or immune response while controlling for circadian variation.
Methodology:
- Acclimatization: House animals under a strict 12-hour:12-hour light-dark (LD) cycle for at least two weeks prior to experimentation.
- Zeitgeber Time (ZT): Define ZT0 as the time of lights-on and ZT12 as lights-off. All procedures should be scheduled according to ZT.
- Intervention Timing: Administer the drug or immune challenge at a specific, justified ZT. For example, to model an immune challenge, administer LPS at ZT0 (start of rest phase for mice) when inflammation may be most pronounced.
- Sample Collection: Collect blood or tissues at multiple time points post-intervention, noting the ZT for each sample.
- Analysis: Analyze results with time as a key variable. Compare groups treated at different ZTs to isolate circadian phase-dependent effects.
Protocol 2: Minimizing Intraindividual Variation in Human Immune Studies
Objective: To obtain stable, reproducible immune measures from human participants.
Methodology:
- Participant Screening: Screen for and exclude individuals with extreme chronotypes or irregular sleep schedules (e.g., shift workers). Consider using the Munich ChronoType Questionnaire.
- Pre-Study Stabilization: Instruct participants to maintain a consistent sleep-wake schedule (e.g., ± 30 minutes) for at least one week prior to sampling. Use actigraphy or sleep logs to verify compliance [89].
- Standardized Conditions: Schedule all sample collections at the same individual clock time for each participant (e.g., always at 8:00 AM ± 30 minutes).
- Control Zeitgebers: Implement a standardized pre-test meal and control light exposure in the clinic waiting room (e.g., bright light in the morning, dim light in the evening) [87].
- Time-Stamp and Batch: Clearly label all samples with collection time. Batch analyze samples by participant and time point to control for assay drift.
Signaling Pathways and Workflows
CIR Immune Regulation
Exp Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Circadian Immune Research
| Item | Function / Rationale |
|---|---|
| Actigraphs | Wearable devices to objectively monitor rest-activity rhythms and sleep-wake cycles in humans and animals over long periods. Critical for quantifying intraindividual variability [91] [89]. |
| Portable ECG/HR Monitors | Used to track diurnal rhythms in heart rate, an output of autonomic nervous system activity, which is linked to circadian physiology and mood variability [91]. |
| Light Therapy Lamps/Glasses | To standardize light exposure, a primary zeitgeber. Can be used to enforce a stable circadian phase in participants or to experimentally shift rhythms [87]. |
| Salivary Cortisol/Kits | For non-invasive, frequent sampling of cortisol, a key circadian hormone. Allows calculation of the cortisol awakening response and intraindividual cortisol variability (ICV) [90]. |
| Melatonin Assays (Saliva/Plasma) | The "gold-standard" marker for circadian phase. Measuring dim-light melatonin onset (DLMO) precisely identifies the timing of an individual's internal clock. |
| Custom Smartphone Apps | For Ecological Momentary Assessment (EMA) to collect real-time, high-frequency self-reported data on mood, sleep, and symptoms, minimizing recall bias [91]. |
| Time-Stamping Protocol (SOP) | A standard operating procedure mandating the recording of clock time and/or Zeitgeber Time (ZT) for every biological sample and procedure. The most cost-effective essential. |
Conclusion
The integration of circadian biology into immunology research is no longer a theoretical concept but an empirical necessity for reducing intraindividual variation and enhancing scientific validity. Evidence from CAR-T cell therapy, vaccine development, and proteomics consistently demonstrates that time-of-day is a potent, modifiable factor influencing therapeutic efficacy, toxicity profiles, and biomarker accuracy. Future directions must include the development of standardized reporting guidelines for temporal factors, widespread adoption of chronotherapeutic principles in clinical trial design, and exploration of personalized chrono-medicine based on individual circadian phenotypes. By systematically accounting for diurnal rhythms, researchers can significantly improve the precision, reproducibility, and clinical translation of immunological findings, ultimately leading to more effective and predictable therapeutic outcomes.
References
- 1. Signaling pathway mechanisms of circadian clock gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11772753/]
- 2. Molecular regulations of circadian rhythm and implications ... [https://www.nature.com/articles/s41392-022-00899-y]
- 3. The Circadian Clock Protein BMAL1 Acts as a Metabolic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.700431/full]
- 4. Perfect timing: circadian rhythms, sleep, and immunity [https://pmc.ncbi.nlm.nih.gov/articles/PMC7030790/]
- 5. Harnessing Variability Signatures and Biological Noise ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11488351/]
- 6. Human immune system variation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5328245/]
- 7. Pharmacological targeting of BMAL1 modulates circadian ... [https://www.nature.com/articles/s41589-025-01863-x]
- 8. Distinct diurnal temperature rhythm patterns in critical illness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554853/]
- 9. Circadian clocks guide dendritic cells into skin lymphatics [https://www.nature.com/articles/s41590-021-01040-x]
- 10. Circadian metabolism in myeloid cells - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12203005/]
- 11. Influence of circadian rhythm on the determination ... [https://www.frontiersin.org/journals/aging/articles/10.3389/fragi.2025.1716985/abstract]
- 12. Troubleshooting Guide: Immunohistochemistry [https://www.rndsystems.com/resources/technical/troubleshooting-guide-immunohistochemistry]
- 13. Changes in Circadian Rhythms Dysregulate Inflammation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.673405/full]
- 14. Circadian Clocks and Adaptive Immune Function [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1697854/full]
- 15. Circadian Clock: A Regulator of Immunity in Autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412416/]
- 16. The role of circadian clock in regulating cell functions [https://pmc.ncbi.nlm.nih.gov/articles/PMC10925886/]
- 17. Circadian rhythm regulates the function of immune cells ... [https://www.nature.com/articles/s41420-024-01960-1]
- 18. Circadian Oscillation of Leukocyte Subpopulations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031226/]
- 19. The identification of diurnal variations on circulating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10920974/]
- 20. The circadian clock regulates innate immunity and ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299925008040]
- 21. Diurnal Variation in Physiological and Immune Responses to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5971328/]
- 22. The Synergistic Role of Light - Feeding Phase Relations on Entraining... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5404903/]
- 23. What Is Entrainment ? How It Synchronizes Your Body’s Circadian... [https://goayo.com/glossary/entrainment/]
- 24. Animal studies may not translate to humans without time ... [https://www.sciencedaily.com/releases/2021/06/210610144505.htm]
- 25. Time-of-Day as a Critical Biological Variable - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8504485/]
- 26. Nighttime Light Hurts Mammalian Physiology: What Diurnal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8167723/]
- 27. Recommendations and Best Practices for Standardizing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7344701/]
- 28. Troubleshooting Guide: ELISA [https://www.rndsystems.com/resources/troubleshooting-guide-elisa-development]
- 29. Chrono-optimizing vaccine administration: a systematic review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009823/]
- 30. Chronovaccination: Harnessing circadian rhythms to optimize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9585312/]
- 31. Chrono-optimizing vaccine administration: a systematic ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1516523/full]
- 32. Storage & Handling | Troubleshooting & Follow-Up [http://www.immunize.org/ask-experts/topic/storage-handling/troubleshooting-follow-up/]
- 33. Cancer treatments based on our internal clock could improve ... [https://hub.jhu.edu/2025/10/06/circadian-rhythms-and-cancer-treatments/]
- 34. Personalizing chronotherapy of immune checkpoint blockade [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581061/]
- 35. Editorial: Circadian rhythms and cancer hallmarks [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1571086/full]
- 36. Comprehensive integrative analysis of circadian rhythms in ... [https://www.nature.com/articles/s44323-025-00035-3]
- 37. Circadian rhythms in immunity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7357859/]
- 38. Temporal Expression Profiling of Plasma Proteins Reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5726913/]
- 39. Longitudinal serum proteome mapping reveals biomarkers ... [https://www.nature.com/articles/s42255-024-01185-7]
- 40. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 41. Diurnal rhythm of the human plasma proteome [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-025-09551-7]
- 42. Statistics for Sleep and Biological Rhythms Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC5483995/]
- 43. Intraindividual Variability in Cortisol [https://pmc.ncbi.nlm.nih.gov/articles/PMC5362320/]
- 44. Early bird or night owl? How your chronotype affects ... [https://www.uclahealth.org/news/article/early-bird-or-night-owl-how-your-chronotype-affects-your]
- 45. The effects of chronotype, sleep schedule and light/dark ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8722381/]
- 46. Effects of light on human circadian rhythms, sleep and mood [https://pmc.ncbi.nlm.nih.gov/articles/PMC6751071/]
- 47. Sleep problems and insomnia self-help guide [https://www.nhsinform.scot/illnesses-and-conditions/mental-health/mental-health-self-help-guides/sleep-problems-and-insomnia-self-help-guide/]
- 48. Intra-individual variability and circadian rhythm of vascular ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0184234]
- 49. Circadian immunity from bench to bedside: a practical guide [https://www.jci.org/articles/view/175706]
- 50. Performance of Blood-Based Biomarkers for Human Circadian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572356/]
- 51. Diurnal rhythms in chimeric antigen receptor T cell ... [https://pubmed.ncbi.nlm.nih.gov/40463553/]
- 52. Time to CAR T Infusion in Local Versus Distant Treatment ... [https://www.sciencedirect.com/science/article/abs/pii/S2666636725005524]
- 53. Optimizing CAR-T treatment: A T2EVOLVE guide to raw and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897765/]
- 54. New Model Provides a Roadmap for Optimal CAR-T Cell ... [https://www.massgeneralbrigham.org/en/about/newsroom/articles/new-model-roadmap-for-optimal-car-t-cell-therapy-in-solid-tumors]
- 55. Long-term follow-up of patients with relapsed/refractory ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1650568/full]
- 56. Immune disruptions and night shift work in hospital ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.939829/full]
- 57. DISREGULATION OF INFLAMMATORY RESPONSES BY ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2974025/]
- 58. 3.4 million real-world learning management system logins ... [https://www.nature.com/articles/s41598-018-23044-8]
- 59. Circadian rhythms and immune function [https://www.timeshifter.com/circadian-rhythms/circadian-rhythms-and-immune-function]
- 60. Intraindividual Variability May Not Always Indicate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2908894/]
- 61. Focus on variability: New tools to study intra-individual ... [https://www.sciencedirect.com/science/article/abs/pii/S0163638302001406]
- 62. Diurnal rhythms in peripheral blood immune cell numbers ... [https://www.sciencedirect.com/science/article/abs/pii/S0145305X17305293]
- 63. Robust CAR T-cell expansion and superior outcomes in DLBCL patients in complete response at infusion - PubMed [https://pubmed.ncbi.nlm.nih.gov/40415166/]
- 64. Car T Cell Therapy Side Effects: 10 Key Risks to Watch After Infusion [https://int.livhospital.com/car-t-cell-therapy-side-effects-10-key-risks-to-watch-after-infusion/]
- 65. CAR T-cell Therapy and Its Side Effects [https://www.cancer.org/cancer/managing-cancer/treatment-types/immunotherapy/car-t-cell.html]
- 66. CAR T Cell Therapy: A Guide for Adult Patients & Caregivers [https://www.mskcc.org/cancer-care/patient-education/car-cell-therapy-guide-adult-patients-caregivers]
- 67. Infusion and delivery strategies to maximize the efficacy of CAR-T cell immunotherapy for cancers | Experimental Hematology & Oncology | Full Text [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-024-00542-2]
- 68. Good CAR T-Cell Expansion After Infusion on Day 10 May Predict Response in Patients with Lymphoma | Targeted Oncology - Immunotherapy, Biomarkers, and Cancer Pathways [https://www.targetedonc.com/view/good-car-t-cell-expansion-after-infusion-on-day-10-may-predict-response-in-patients-with-lymphoma]
- 69. Biological rhythms in COVID-19 vaccine effectiveness in an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10231992/]
- 70. Optimal Timing of Vaccination - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12084464/]
- 71. One size doesn't fit all: Best time for COVID-19 booster ... [https://medicine.yale.edu/news-article/one-size-doesnt-fit-all-best-time-for-covid-19-booster-depends-on-where-you-live-infection-history/]
- 72. Interim Estimates of 2024–2025 COVID-19 Vaccine ... [https://www.cdc.gov/mmwr/volumes/74/wr/mm7406a1.htm]
- 73. Calibrating a Comprehensive Immune Age Metric to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9687950/]
- 74. A new method for evaluating biological age and predicting ... [https://www.sciencedirect.com/science/article/pii/S1568163724004719]
- 75. A systematic review and meta-analysis of the stability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9729419/]
- 76. Characterization of biological variation of peripheral blood ... [https://www.nature.com/articles/s41598-019-51294-7]
- 77. Difficulties Posed By Intra-Individual Variation [https://epi.grants.cancer.gov/diet/usualintakes/difficulties.html]
- 78. Multi-omic profiling reveals age-related immune dynamics ... [https://www.nature.com/articles/s41586-025-09686-5]
- 79. Temporal Stability of Epigenetic Markers - Research journals [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0039220]
- 80. Keeping an eye on circadian time in clinical research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9790849/]
- 81. Frontiers | The Impact of Immunotherapy on Sleep and Circadian ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1295267/full]
- 82. The role of the circadian clock in cancer hallmark acquisition and... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-021-01919-5]
- 83. subtyping unveiling distinct Circadian landscapes in... pattern immune [https://link.springer.com/article/10.1007/s00262-023-03495-3]
- 84. Immunohistochemistry (IHC): Experimental Protocols and ... [https://www.antibodysystem.com/archive/387.html]
- 85. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooZyWaI_gE8PFP_k8WXOVyCZrEvOj5qp4pm-MzdiExKZs38iFho]
- 86. Circadian immunity from bench to bedside: a practical guide [https://pmc.ncbi.nlm.nih.gov/articles/PMC10836804/]
- 87. How to Fix & Reset Your Circadian Rhythm in 8 Simple Steps [https://goayo.com/blogs/news/how-to-fix-reset-your-circadian-rhythm-in-8-simple-steps]
- 88. Why does circadian timing of administration matter for ... [https://www.nature.com/articles/s41416-024-02704-9]
- 89. Current Considerations in the Diagnosis and Treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10710539/]
- 90. Stress management reduces intraindividual cortisol variability ... [https://pubmed.ncbi.nlm.nih.gov/26526317/]
- 91. Variability in phase and amplitude of diurnal rhythms is ... [https://www.nature.com/articles/s41598-018-19888-9]
- 92. Associations Between Intraindividual Variability in Sleep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8575675/]