High-Throughput Flow Cytometry Immunophenotyping of Human Blood: A Comprehensive Guide for Robust Pipeline Design and Execution
This article provides a comprehensive guide for researchers and drug development professionals on implementing high-throughput flow cytometry for deep immunophenotyping of human blood.
High-Throughput Flow Cytometry Immunophenotyping of Human Blood: A Comprehensive Guide for Robust Pipeline Design and Execution
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on implementing high-throughput flow cytometry for deep immunophenotyping of human blood. Covering foundational principles to advanced applications, it details robust sample processing pipelines capable of handling thousands of samples, methodological optimizations for 28-color panels, critical troubleshooting strategies to minimize technical variation, and validation frameworks employing automated analysis. By synthesizing recent advancements in standardized protocols and quality control measures, this resource enables precise, reproducible immune monitoring in large cohort studies, clinical trials, and drug discovery pipelines.
Understanding High-Throughput Immunophenotyping: Core Principles and Research Applications
Defining High-Throughput Flow Cytometry in Modern Immunology
High-throughput flow cytometry has revolutionized modern immunology by enabling the multiparametric analysis of thousands of single cells per second from complex mixtures such as human blood [1] [2]. This technology provides quantitative data on cell surface and intracellular markers, allowing researchers to comprehensively decode the human immunome and understand immune responses across the lifespan [2]. The application of high-throughput flow cytometry in immunophenotyping has become indispensable for both basic research and clinical translation, including drug development and immunotherapy monitoring [1] [2]. This Application Note outlines standardized protocols and best practices to ensure the generation of high-quality, reproducible data in high-throughput flow cytometry immunophenotyping of human blood.
Key Principles of High-Throughput Flow Cytometry
Core Technological Advantages
The power of high-throughput flow cytometry in immunology stems from several key capabilities. It allows for multiparametric analysis at the single-cell level, providing a comprehensive view of heterogeneous cell populations [1]. The technology offers exceptional speed and efficiency, analyzing thousands of cells per second to deliver rapid results essential for large-scale studies and timely clinical decisions [1]. Furthermore, it provides precise quantitative assessment of marker expression levels, which is crucial for monitoring subtle immune variations in disease progression, therapy response, and minimal residual disease detection [1] [2].
Emerging Technological Developments
Recent advances have significantly expanded the capabilities of traditional flow cytometry. Mass cytometry (CyTOF) combines flow cytometry with mass spectrometry, using metal-labeled antibodies to enable highly multiplexed measurements of up to 40 cellular parameters without the need for fluorescence compensation [2]. Spectral flow cytometry utilizes full-spectrum fingerprinting and unmixing algorithms to eliminate fluorescence spillover issues, allowing panel complexity to expand to 40 fluorescence parameters and beyond [2]. Imaging mass flow cytometry provides morphological context by analyzing the distribution and interactions of various cells within tissue structures, offering valuable insights into the tumor microenvironment [2]. The integration of artificial intelligence with flow cytometry data has shown remarkable potential in improving diagnostic efficiency, with one model for myelodysplastic syndromes achieving 91.8% sensitivity and 92.5% specificity [2].
Essential Experimental Protocols
Detector Optimization and Voltage Setting
Proper instrument setup is fundamental for obtaining high-quality data. The voltage walk method determines the Minimum Voltage Requirement (MVR) that allows clear resolution of dim fluorescent signals from background instrument noise [3].
Protocol:
- Prepare dimly fluorescent hard-dyed beads according to manufacturer specifications.
- Create a voltage series with increasing increments (e.g., 50 mV steps) for each detector.
- Acquire data at each voltage setting, recording the percent robust Coefficient of Variation (%rCV) and robust Standard Deviation (rSD).
- Plot %rCV and rSD against voltage to identify the inflection point.
- Select the lowest voltage on the %rCV curve before the rSD increases as the optimal setting [3].
This optimization ensures all measurements remain within the detector's linear range while providing the best separation between positive and negative signals [3]. For digital cytometers, the "peak 2" method can be employed, where dim particles are run over a voltage series and the spread of data (CV) is plotted against voltage to identify the inflection point where increased voltage no longer decreases CV [4].
Antibody Titration for Optimal Panel Performance
Antibody titration is critical for minimizing nonspecific binding, increasing signal detection, and reducing spillover spreading [3].
Protocol:
- Begin with the manufacturer's recommended antibody concentration.
- Perform serial 2-fold dilutions in appropriate buffer.
- Incubate cells with each antibody dilution following standard staining protocols.
- Acquire data on a properly calibrated flow cytometer.
- Calculate the Stain Index (SI) for each dilution using the formula: SI = (Mean positive cells - Mean negative cells) / (2 × SD negative cells) [3].
- Plot SI against antibody dilution to identify the separation concentration (providing greatest difference between negative and positive cells) and saturation concentration (where antibody saturates available antigen) [3].
A separation concentration typically provides optimal population resolution, reduces spreading error, and conserves antibody, while saturation concentrations may be necessary for low-abundance antigens but can increase spillover spreading [3].
Fluorophore Selection and Panel Design
Strategic fluorophore selection is crucial for successful multiparametric panels.
Design Principles:
- Pair bright fluorophores with antibodies for low-abundance targets
- Use dim fluorophores with antibodies for highly expressed antigens
- Minimize spectral overlap between fluorophores to reduce spillover
- Use spectrally distinct fluorophores for co-expressed markers
- Group spectrally similar fluorophores for markers expressed on separate cell subpopulations [3]
Visualize potential spillover spreading using single-stained samples or a spillover spread matrix during panel development [3]. The iterative process of panel design requires testing all combinations and reviewing the spillover spread matrix at each iteration [3]. Online tools such as the Invitrogen Flow Cytometry Panel Builder can simplify this process by providing spectral visualization and spillover prediction [3].
Sample Preparation and Staining
Proper sample preparation ensures representative and accurate immunophenotyping results.
Protocol for Human Blood Immunophenotyping:
- Sample Collection: Collect peripheral blood in appropriate anticoagulant tubes (e.g., EDTA, heparin).
- Cell Isolation: Isolate peripheral blood mononuclear cells (PBMCs) using density gradient centrifugation or use whole blood lysis protocols.
- Viability Staining: Incorporate a viability dye (e.g., LIVE/DEAD Fixable Dead Cell Stain) to exclude dead cells that nonspecifically bind antibodies [3] [5].
- FC Receptor Blocking: Incubate cells with FC receptor blocking reagent or human IgG to reduce nonspecific antibody binding.
- Surface Staining: Incubate cells with titrated antibody cocktails for 20-30 minutes at 4°C protected from light.
- Fixation: Fix cells with appropriate fixative (e.g., 1-4% paraformaldehyde) if not proceeding to intracellular staining.
- Intracellular Staining (if required): Permeabilize cells using commercial permeabilization buffers, then incubate with intracellular antibodies.
Note: Maintain single-cell suspension throughout processing, and avoid excessive centrifugation that may cause cell clumping [1].
Essential Controls for Data Integrity
Control Requirements for High-Throughput Applications
| Control Type | Purpose | Preparation Method | Application in Analysis |
|---|---|---|---|
| Unstained Control | Assess autofluorescence | Cells without any fluorescent stains | Baseline fluorescence reference |
| Compensation Controls | Calculate fluorescence spillover | Single-stained beads or cells brightly positive for each fluorophore | Automated compensation calculation during acquisition [4] |
| FMO Controls | Determine positive population boundaries | All antibodies except the one of interest | Gate placement for dim markers and continuum expressions [3] [4] |
| Viability Control | Exclude dead cells | Cells stained with viability dye | Exclusion of dead cells that nonspecifically bind antibodies [3] |
| Biological Controls | Assess experimental variation | Reference samples (e.g., healthy donor PBMCs) | Inter-experimental normalization and quality assessment [4] |
| Isotype Controls | Not recommended due to potential misleading results from unmatched F/P ratios and affinities [4] |
Quality Control and Instrument Monitoring
Implementing experiment-specific QC protocols is essential for detecting variations in instrument performance and staining efficiency [4].
Protocol:
- Daily QC: Run standardized calibration beads (e.g., Spherotech 8-peak beads) each day before sample acquisition to ensure consistent instrument performance.
- Target Values: Establish target values and acceptable variation ranges for key parameters during experimental optimization.
- Levey-Jennings Plotting: Track instrument performance over time using Levey-Jennings plots, which display running averages and ±1-2 standard deviation ranges.
- Troubleshooting: Investigate any data points falling outside quality control levels (±2 SD) before collecting experimental samples [4].
Data Analysis Strategies for High-Throughput Immunophenotyping
Preprocessing and Gating Strategies
Initial data analysis requires careful gating to identify populations of interest while excluding artifacts.
Standard Gating Hierarchy:
- Singlets Gate: Exclude doublets and cell aggregates by plotting FSC-H vs FSC-A [5].
- Live Cells Gate: Exclude dead cells using viability dye staining [3] [5].
- Lymphocyte/Monocyte Gate: Identify broad populations using FSC vs SSC properties [6] [5].
- Subpopulation Gating: Apply lineage-specific markers to identify T-cells, B-cells, monocytes, etc. [6] [5].
When calculating population percentages, remember that nested gates require back-calculation to the total population. For example, if 30.1% of total cells are neutrophils and 14.5% of neutrophils express IL-17a, then 4.36% (30.1 × 0.145) of the total sample are IL-17a-expressing neutrophils [5].
Advanced Analysis Approaches
For high-dimensional data, advanced computational methods enhance population identification and characterization.
Dimensionality Reduction: Techniques such as t-Distributed Stochastic Neighbor Embedding (t-SNE) and Uniform Manifold Approximation and Projection (UMAP) simplify complex datasets while preserving essential characteristics for effective visualization [7].
Clustering Analysis: Automated clustering algorithms (self-organizing maps, partitioning algorithms, density-based clustering) identify cell populations without manual gating bias, either as complete analysis pipelines or for subset identification within manually gated populations [7].
Automated Classification: Artificial intelligence and machine learning approaches, such as gradient boosting machine algorithms, can classify cell populations and predict clinical outcomes with high accuracy [2].
Standardized Immunophenotyping Panels for Human Blood
Recommended Marker Panels for Comprehensive Immune Profiling
The following table summarizes essential immunophenotyping markers for human blood analysis, compiled from standardized clinical panels and research applications [1] [2]:
| Cell Population | Key Defining Markers | Additional Subset Markers | Clinical/Research Utility |
|---|---|---|---|
| T Lymphocytes | CD3, CD4, CD8, CD45 | CD45RA, CD45RO, CCR7, CD25, CD127, CD28 | T-cell maturation, activation, memory subsets [1] |
| Helper T Cells | CD3, CD4 | CXCR5, CD183, CD196, CD25, FoxP3 | Th1/Th2/Th17/Tfh/Treg identification [1] |
| Cytotoxic T Cells | CD3, CD8 | CD45RA, CD27, CD28, CD57, PD-1 | Differentiation, senescence, exhaustion [1] |
| B Lymphocytes | CD19, CD20, CD45 | CD27, CD38, IgD, CD10, CD21 | Maturation, activation, memory B cells [1] |
| NK Cells | CD56, CD16, CD3- | CD57, CD158, NKG2A, CD335 | Cytotoxic potential, education, maturation [1] |
| Monocytes | CD14, CD16, HLA-DR | CD64, CD163, CD80, CD86, CD11b, CD11c | Classical/non-classical subsets, activation [1] |
| Dendritic Cells | HLA-DR, Lineage- | CD11c, CD123, CD141, CD1c | Conventional vs plasmacytoid DC identification [1] |
| Granulocytes | CD15, CD16, CD45 | CD11b, CD66b, CD63, CD14- | Neutrophil activation, maturation [1] |
Application in Hematological Malignancies
Flow cytometry immunophenotyping plays a crucial role in diagnosing and classifying hematological malignancies. The following table outlines standard diagnostic markers based on the WHO classification of haematolymphoid tumors [1]:
| Malignancy Type | Essential Diagnostic Markers | Additional Characteristic Markers |
|---|---|---|
| AML | CD13, CD33, CD34, CD117, HLA-DR | CD14, CD64, MPO [1] |
| B-ALL | CD10, CD19, CD34, TdT | CD20, CD22, CD79a [1] |
| T-ALL | CD1a, CD2, CD3, CD5, CD7, TdT | CD4, CD8, CD45 [1] |
| CLL/SLL | CD5, CD19, CD20, CD23 | CD38, CD43, CD79b, CD200 [1] |
| B-Cell Lymphoma | CD19, CD20, CD22 | CD5, CD10, CD79a, BCL2, Cyclin D1* [1] |
| T-Cell Lymphoma | CD2, CD3, CD5, CD7 | CD4, CD8, CD30, TRBC1/TRBC2 [1] |
*Mantle cell lymphoma [1]
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent Category | Specific Examples | Function in Experiment |
|---|---|---|
| Viability Dyes | LIVE/DEAD Fixable Dead Cell Stains, 7-AAD, DAPI | Distinguish live/dead cells to exclude dead cells with nonspecific binding [3] [5] |
| FC Blocking Reagents | Human FC Receptor Blocking Solution, Human IgG | Reduce nonspecific antibody binding [4] |
| Compensation Beads | Anti-Mouse/Rat Ig Kappa Compensation Beads, ArC Amine Reactive Compensation Bead Kit | Create consistent single-color controls for compensation [4] |
| Cell Preparation Reagents | RBC Lysis Buffer, Ficoll-Paque, DNase I | Process whole blood to isolate target populations [1] |
| Fixation/Permeabilization | Paraformaldehyde, Commercial Intracellular Staining Kits | Preserve samples and enable intracellular marker detection |
| Quality Control Beads | Spherotech 8-Peak Beads, Cyto-Cal Daily QC Beads | Monitor instrument performance over time [4] |
| Standardized Antibody Panels | Pre-configured dried antibody panels | Reduce technical variation in staining [1] |
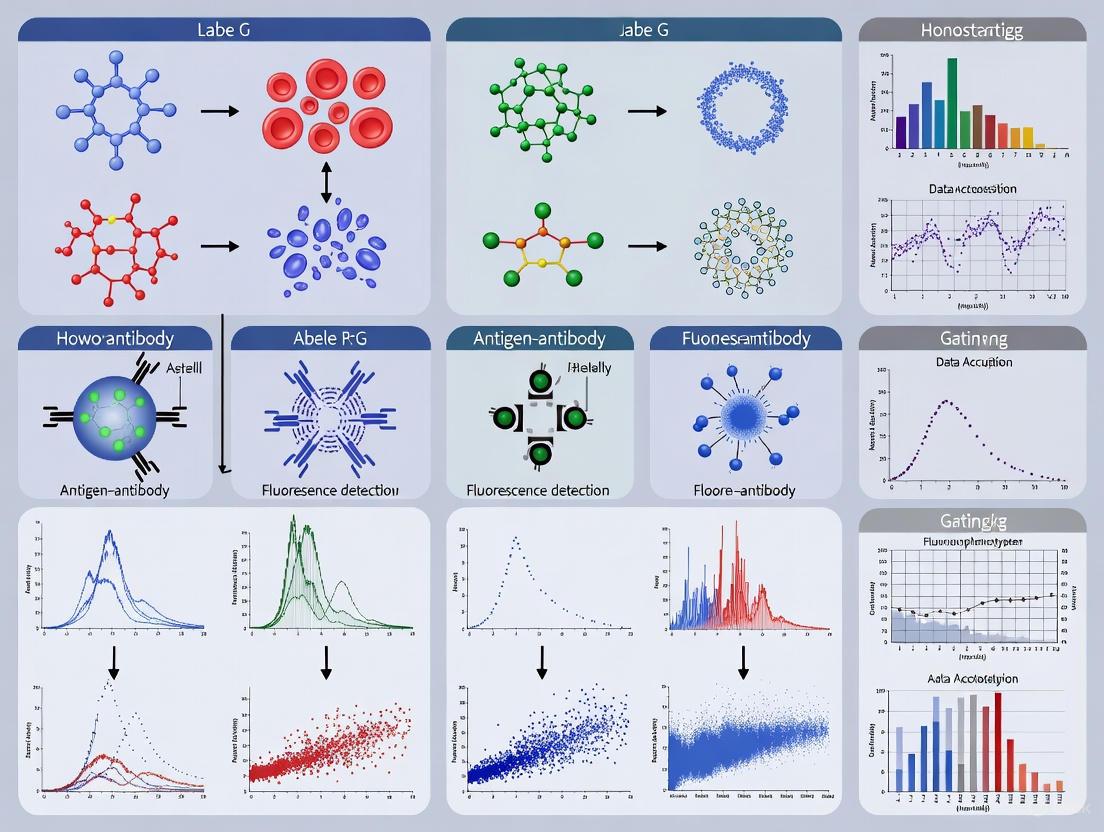
Workflow Visualization
High-Throughput Flow Cytometry Workflow
Troubleshooting Common Challenges
Addressing Technical Variability
Technical variability represents a significant challenge in high-throughput flow cytometry, particularly in multi-center studies. Several approaches can minimize this variability:
Standardization Strategies:
- Implement standardized operating procedures for sample processing, staining, and acquisition
- Use centralized reagent validation and lot testing
- Establish cross-laboratory instrument calibration protocols
- Incorporate reference control samples in each experiment [1] [4]
Data Normalization:
- Use biological reference controls for inter-experimental normalization
- Apply bead-based normalization for instrument performance
- Utilize automated algorithms for batch effect correction [4]
Optimization of High-Parameter Panels
As panel complexity increases, several strategies can maintain data quality:
Spillover Management:
- Regularly review spillover spread matrix during panel development
- Consider bright fluorophores for low-abundance targets and dim fluorophores for highly expressed antigens
- Utilize spectral flow cytometry or CyTOF for highest-parameter panels [3] [2]
Validation Procedures:
- Conduct full-panel validation with FMO controls for all critical markers
- Verify population identities with known biological controls
- Perform reproducibility testing across multiple samples [3] [4]
High-throughput flow cytometry represents a powerful platform for comprehensive immunophenotyping of human blood, with applications spanning basic immunology research, drug development, and clinical diagnostics. The successful implementation of this technology requires careful attention to panel design, instrument optimization, appropriate controls, and standardized protocols. By adhering to the best practices and methodologies outlined in this Application Note, researchers can generate robust, reproducible data that advances our understanding of the human immune system in health and disease. The ongoing integration of artificial intelligence with advanced cytometry technologies promises to further enhance the precision and predictive power of high-throughput flow cytometry in immunology research.
Key Advantages for Large Cohort Studies and Clinical Trials
Large-scale cohort studies represent a cornerstone of modern biomedical research, providing an powerful framework for investigating the complex etiology of chronic diseases and identifying novel risk factors. When integrated with high-throughput flow cytometry for immunophenotyping, these studies unlock profound potential for discovering how the immune system influences health and disease across populations [8]. This approach facilitates the investigation of chronic diseases in relation to a wide spectrum of factors including lifestyle, genetics, socioeconomic status, and environmental exposures [8]. The German National Cohort (GNC), for instance, exemplifies this design by examining 200,000 participants aged 20-69 years to create new strategies for risk assessment, early diagnosis, and prevention of multifactorial diseases [8].
The integration of high-dimensional flow cytometry into these large studies transforms them into platforms for deep immunophenotyping at a population level. This enables researchers to move beyond simple cell counts to detailed characterization of immune cell composition and functional states, capturing thousands of immune cell traits including subset frequencies, ratios, morphologic properties, and surface protein expression levels [9]. The resulting data provides unprecedented insight into immune variation between individuals and its relationship to disease development, progression, and treatment response.
Key Advantages of Large Cohort Studies
Large cohort studies offer distinct methodological advantages over other study designs, particularly for investigating chronic disease etiology and immunological processes. These strengths make them ideally suited for population-level immunology research.
Table 1: Comparative Advantages of Large Cohort Study Designs
| Advantage | Description | Research Impact |
|---|---|---|
| Etiological Investigation | Enables study of multiple disease outcomes in relation to diverse exposures over extended periods [8] [10]. | Identifies complex disease causes and natural history; ideal for chronic disease research [8] [11]. |
| Rare Exposure Assessment | Suitable for observing rare exposures (e.g., new drugs, environmental toxins) due to long duration [10]. | Can detect effects of uncommon exposures that shorter studies would miss. |
| Temporal Relationship Clarification | Prospective nature establishes exposure before outcome development [10] [11]. | Provides stronger evidence for causality than retrospective designs. |
| Multiple Outcome Analysis | Can investigate multiple outcomes associated with single or multiple exposures [11]. | Comprehensive understanding of exposure effects across disease states. |
| High Generalizability | Large sample sizes with standardized recruitment represent broader populations [10]. | Findings have greater external validity and clinical relevance. |
Additional Strategic Benefits
Beyond the core advantages outlined in Table 1, large cohorts provide several strategic benefits that enhance their scientific value:
- Standardization Across Sites: Studies like the GNC implement highly standardized protocols across multiple study centers, ensuring data comparability and quality [8]. This is particularly crucial for immunophenotyping where technical variation can compromise data integrity.
- Biomarker Discovery: The longitudinal design facilitates identification of novel pre-clinical disease markers [8], which is essential for developing early intervention strategies.
- Integration with Omics Technologies: Modern cohorts systematically collect and store biological samples, enabling integration with genomic, proteomic, and other high-dimensional data [12]. This multi-omics approach is transforming our understanding of disease mechanisms.
- Resource for Nested Studies: Large cohorts provide efficient platforms for nested case-control or case-cohort studies focused on specific immunological hypotheses [13].
The Framingham Heart Study exemplifies the long-term impact of such cohort studies, having identified fundamental cardiovascular risk factors and generated predictive models that continue to inform clinical practice decades after its inception [11].
High-Throughput Flow Cytometry Immunophenotyping in Large Cohorts
Standardized Workflow for Large-Scale Immunophenotyping
Implementing high-dimensional flow cytometry in large cohort studies requires rigorous standardization to minimize technical variation and ensure data reproducibility. The following workflow diagram illustrates a robust pipeline for high-content, high-throughput immunophenotyping:
Essential Research Reagent Solutions
The successful implementation of large-scale immunophenotyping requires carefully selected reagents and materials to ensure reproducibility and data quality across thousands of samples.
Table 2: Essential Research Reagents for High-Throughput Immunophenotyping
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Viability Dyes | 7-AAD, DAPI, TOPRO-3, fixable amine-reactive dyes [14] | Distinguishes live from dead cells to exclude nonspecific antibody binding and improve data quality. |
| Blood Collection Tubes | Heparin-coated, EDTA anticoagulant tubes [9] | Preserves sample integrity during transport and processing from multiple collection sites. |
| Lysing Solutions | FACS Lysing Solution, ammonium chloride-based buffers [14] [9] | Removes erythrocytes while preserving leukocyte population for analysis. |
| Fixation/Permeabilization Reagents | Paraformaldehyde (1-4%), methanol, acetone, commercial kits [14] | Preserves cell structure and enables intracellular staining for comprehensive immunophenotyping. |
| Fc Receptor Blocking Agents | Goat serum, human IgG, mouse anti-CD16/CD32 [14] | Reduces nonspecific antibody binding through Fc receptors, improving signal specificity. |
| Validated Antibody Panels | 11-28 color panels with titrated antibodies [15] [9] | Enables simultaneous detection of multiple cell surface and intracellular markers. |
| Calibration Particles | 8-peak Rainbow Calibration Particles, compensation beads [9] | Standardizes instrument performance across time and between different flow cytometers. |
Optimized Staining Protocol for Whole Blood Immunophenotyping
The following detailed protocol is adapted from standardized approaches for deep immunophenotyping of human whole blood [9]:
Sample Preparation (20 minutes)
- Collect fresh human peripheral whole blood in heparin or EDTA anticoagulant tubes.
- Create a single-cell suspension and transfer to a 96-well plate or polystyrene round-bottom tube.
- Incubate with RBC lysis buffer (if needed) according to manufacturer instructions.
- Wash cells with phosphate-buffered saline (PBS) containing 2% FBS.
- Centrifuge at 200 × g for 5 minutes at 4°C
- Carefully aspirate supernatant to avoid cell loss
- Determine cell count and viability (target: 90-95% viability).
- Resuspend cells in ice-cold staining buffer at concentration of 0.5-1 × 10^6 cells/mL.
Viability Staining (Timing varies by dye)
- Incubate cells with viability dye according to manufacturer protocol in the dark at 4°C.
- Select dye with emission spectrum that doesn't overlap with immunostaining fluorophores.
- Wash cells twice with stain buffer (200 × g, 5 minutes, 4°C).
Extracellular Staining (45 minutes)
- Resuspend cell pellet in Fc receptor blocking buffer (e.g., 2-10% goat serum).
- Incubate for 30-60 minutes in the dark at 4°C.
- Wash twice with stain buffer.
- Incubate with titrated antibody mixture for surface markers for 20 minutes at room temperature in the dark.
- Wash twice with stain buffer.
Fixation and Permeabilization (For intracellular targets, 75 minutes)
- Fix cells with 1-4% paraformaldehyde for 15-20 minutes on ice.
- Wash twice with stain buffer.
- Permeabilize cells with detergent solution (e.g., 0.1% Triton X-100) for 10-15 minutes at room temperature.
- Note: Acetone fixation also permeabilizes, making this step unnecessary.
- Wash twice with stain buffer.
Intracellular Staining (45 minutes)
- Incubate with antibodies against intracellular targets for 20 minutes at room temperature in the dark.
- Wash twice with stain buffer.
- Resuspend fixed cells in 1% PFA for acquisition or acquire unfixed samples immediately.
Data Analysis Framework for High-Dimensional Immunophenotyping
The analysis of high-dimensional flow cytometry data from large cohorts requires a structured computational approach to extract meaningful biological insights from complex datasets. The following diagram illustrates the key stages in this process:
Critical Analysis Considerations for Cohort Data
When analyzing immunophenotyping data from large cohorts, several specific considerations ensure robust and interpretable results:
- Batch Effect Correction: Implement rigorous normalization across experimental batches to minimize technical variation [15]. This is particularly crucial when processing thousands of samples over extended periods.
- Automated Population Identification: Utilize computational approaches like FlowSOM clustering for objective, reproducible cell population identification [15]. This reduces investigator bias, especially when analyzing dozens of immune subsets.
- Multivariate Analysis: Apply hierarchical cluster analysis (HCA) and other multivariate methods to identify complex immune signatures associated with clinical phenotypes [16].
- Covariate Adjustment: Account for technical (sample processing time, instrument settings) and biological (age, sex, BMI) covariates that influence immune measurements [15] [9].
- Longitudinal Modeling: For cohorts with repeated sampling, employ mixed-effects models to account within-individual correlation over time.
This comprehensive approach to data analysis has enabled discoveries such as age-associated immune dynamics, including decreasing T and B cell subsets with age, and identification of unique immune signatures associated with genetic polymorphisms [15].
Application in Clinical Research: Case Example in Cardiovascular Disease
The integration of high-throughput immunophenotyping in cohort studies has generated significant insights into disease mechanisms, as demonstrated by this cardiovascular research example:
Study Objective: To identify shifts in the circulating T-cell compartment following reperfusion in patients with acute myocardial infarction [16].
Cohort Design:
- 55 men with angiographically confirmed coronary heart disease
- 31 patients with acute ST-elevation myocardial infarction (STEMI)
- 24 stable patients with healed STEMI
- 18 healthy male controls
Immunophenotyping Approach:
- 13-parameter flow cytometry panel targeting T-cell differentiation and senescence markers
- Analysis of cryopreserved PBMCs using standardized protocols
- Hierarchical cluster analysis to identify distinct T-cell signatures
Key Findings:
- Identification of specific T-cell immunophenotypes associated with acute myocardial infarction
- Revealed changes in T-cell compartments following reperfusion therapy
- Demonstrated application of high-throughput immunophenotyping in multicenter clinical trial setting
This case study illustrates how cohort designs integrated with advanced immunophenotyping can reveal novel immunological aspects of disease pathogenesis and progression, potentially identifying new therapeutic targets or biomarkers for risk stratification.
Large cohort studies provide an indispensable framework for advancing our understanding of immune system function in health and disease. When integrated with standardized, high-throughput flow cytometry protocols, these studies enable deep immunophenotyping at population scale, revealing complex relationships between immune variation and clinical outcomes. The rigorous methodological approaches outlined in this application note—from sample processing and instrument standardization to computational analysis—provide a roadmap for generating reproducible, high-quality immunophenotyping data in large populations. As cohort studies continue to evolve with advancing technologies and analytical methods, they will remain essential for discovering novel immunological insights with potential to transform disease prevention, diagnosis, and treatment.
Major Immune Cell Populations Identifiable in Human Blood
Immunophenotyping via high-throughput flow cytometry is an indispensable technique for quantifying and characterizing the diverse immune cell populations within human blood. This application note provides a detailed protocol for a multi-parametric flow cytometry panel designed for the deep immunophenotyping of human whole blood, enabling the simultaneous identification of major lineages and functional subsets. Standardized methodologies are critical for generating reproducible data in research and drug development [17].
Major Immune Cell Populations and Phenotypic Markers
The following table summarizes the key surface and intracellular markers used to identify major immune cell populations and their functional subsets in human blood.
Table 1: Key Markers for Identifying Major Immune Cell Populations
| Cell Population | Key Identifying Markers | Subset Markers | Primary Function |
|---|---|---|---|
| T Lymphocytes | CD3, TCRαβ | CD4, CD8, CD45RA, CCR7, CD25, CD127, CD28, CD57 | Cell-mediated immunity, T-helper and cytotoxic responses [18] [19] |
| B Lymphocytes | CD19, CD20 | CD24, CD27, CD38, IgD, IgM, IgG | Antibody production, antigen presentation [20] [19] |
| Natural Killer (NK) Cells | CD56, CD16, CD2 | CD159a (NKG2A), CD159c (NKG2C), CD337 (NKp30) | Cytolysis of virally infected and cancerous cells [20] [19] |
| Monocytes | CD14, CD16, HLA-DR | CD11c, CD64, CCR5, CD38 | Phagocytosis, antigen presentation, cytokine secretion [20] [19] |
| Dendritic Cells (DCs) | HLA-DR, CD11c, CD141, CD123 | CD1c, CD38, CXCR3 | Antigen capture and presentation, T cell priming [19] |
| Granulocytes | High SSC, CD16, CD11b | CD15, CD66b, CD24, CD59 | Innate immune defense, phagocytosis, inflammation [18] [20] |
| Regulatory T Cells (Tregs) | CD4, CD25, CD127lo/– | FoxP3 (intracellular), CD39, HLA-DR | Suppression of immune responses, maintenance of tolerance [20] [19] |
Experimental Workflow for Whole Blood Immunophenotyping
The diagram below illustrates the comprehensive workflow for sample processing, staining, and data acquisition.
Detailed Protocol: 13-Parameter Immunophenotyping of Lysed Whole Blood
This protocol, adapted from a validated application note, outlines a stain/lyse procedure for immunophenotyping human whole blood using a 4-laser flow cytometer capable of detecting 13 colors [20].
Materials and Reagents
Table 2: Research Reagent Solutions
| Item | Function/Purpose | Example |
|---|---|---|
| Antibody Panels | Identification of specific cell surface/intracellular antigens. | Pre-titrated, fluorochrome-conjugated antibodies (e.g., CD3, CD4, CD8, CD19, CD45) [20]. |
| Viability Dye | Discrimination and exclusion of dead cells from analysis. | Propidium Iodide (PI), 7-AAD, or amine-reactive dyes [20] [21]. |
| Lysing Buffer | Hypotonic lysis of red blood cells to enrich for leukocytes. | 1X ACK (Ammonium-Chloride-Potassium) Lysing Buffer [20]. |
| Compensation Beads | Capture antibodies to create single-color controls for accurate spectral overlap compensation. | AbC Total Antibody Compensation Bead Kit or similar [22] [20]. |
| Wash/Stain Buffer | Diluent and wash solution for antibody staining steps. | Phosphate-Buffered Saline (PBS) with 1% BSA and 2mM sodium azide [20]. |
| Fixation Solution | Preserves cellular integrity and stabilizes antibody binding for delayed acquisition. | 1.5% Paraformaldehyde (PFA) [23]. |
Step-by-Step Procedure
- Sample Collection and Preparation: Collect human whole blood into sodium heparin or EDTA vacutainers. For fixation and long-term storage considerations, specialized kits like TokuKit can preserve cell counts and population frequencies for up to 72 hours, mitigating the significant cell loss observed in fresh samples [23].
- Red Blood Cell Lysis:
- Dilute whole blood 1:10 in 1X ACK Lysing Buffer.
- Incubate for 30 minutes at room temperature on a rotator.
- Centrifuge at 300 × g for 5 minutes and carefully decant the supernatant.
- Wash the cell pellet with PBS containing 1% BSA.
- Perform a white blood cell count using an automated cell counter [20].
- Antibody Staining:
- Resuspend approximately 1 × 10^6 cells in 50 μL of staining buffer.
- Add pre-titrated volumes of fluorochrome-conjugated antibodies directly to the cell suspension. The total staining volume should be adjusted to 100 μL with buffer.
- Mix the tubes gently and incubate for 15 minutes at room temperature, protected from light.
- Centrifuge at 300 × g for 5 minutes, remove the supernatant, and resuspend the cells in 1 mL of PBS or sheath fluid for acquisition [20].
- Compensation Controls:
- Use compensation beads per manufacturer's instructions. Add one drop of capture beads to separate tubes.
- Add the same pre-titrated amount of each antibody conjugate used in the panel to its respective bead tube.
- Incubate for 15 minutes at room temperature, protected from light.
- Wash beads, resuspend in buffer, and analyze on the flow cytometer to generate single-color controls [20].
- Data Acquisition:
- Create a workspace on the flow cytometer software with the necessary scatter plots and fluorescence channels.
- Set photomultiplier tube (PMT) voltages and compensation values using the bead controls.
- Acquire data from the stained sample, collecting a sufficient number of events (e.g., 50,000-100,000 leukocyte events) for robust statistical analysis of rare subsets [20].
Data Analysis and Gating Strategy
A hierarchical gating strategy is essential for accurate population identification and to exclude artifacts. The following diagram outlines the sequential gating logic.
Step-by-Step Gating Explanation:
- Exclude Debris: Gate on the main population of events in a FSC-A vs. SSC-A plot to exclude subcellular debris and platelets (Gate P1) [21].
- Exclude Doublets: Plot FSC-A vs. FSC-W (Width) and gate on the population with a linear relationship to exclude cell doublets and aggregates, ensuring analysis is performed on single cells (Gate P2) [21].
- Exclude Dead Cells: Using a viability dye (e.g., PI or 7-AAD), gate on the negative population to exclude dead cells, which cause nonspecific antibody binding and autofluorescence (Gate P3) [20] [21].
- Identify Leukocytes: Create a CD45 vs. SSC-A plot. All nucleated hematopoietic cells express CD45 at varying densities. Gate on CD45-positive cells to exclude any remaining non-leukocyte events (Gate P4) [21].
- Identify Major Lineages: From the CD45+ gate, revert to FSC-A vs. SSC-A to visually identify and gate populations based on size and granularity:
- Lymphocytes: Low FSC and low SSC.
- Monocytes: Intermediate FSC and medium SSC.
- Granulocytes: High FSC and high SSC [20].
- Immunophenotyping within Lymphocyte Gate: From the lymphocyte gate, use fluorescence plots to identify specific subsets:
- T Cells: Plot CD3 vs. SSC or other markers. Gate on CD3+ cells [20].
- Helper T Cells: From CD3+ gate, plot CD4 vs. CD8. Gate on CD3+CD4+ cells.
- Cytotoxic T Cells: From the same plot, gate on CD3+CD8+ cells [20].
- B Cells: Plot CD19 vs. SSC. Gate on CD19+ cells [20].
- NK Cells: Plot CD3 vs. CD56. Gate on CD3-CD56+ cells [20].
This application note provides a standardized framework for the comprehensive immunophenotyping of human whole blood. Adherence to detailed protocols for sample preparation, instrument setup, compensation, and a rigorous hierarchical gating strategy is paramount for generating high-quality, reproducible data. This enables reliable identification of major immune cell populations and their functional subsets, supporting advanced research and drug development in immunology.
Flow cytometry stands as one of the most stable and productive marriages in recent scientific history, fundamentally transforming immunological research and clinical diagnostics [24]. The technology's evolution from simple cell counting to sophisticated multiparametric analysis has enabled unprecedented dissection of the immune system at single-cell resolution. Within modern research, high-throughput flow cytometry immunophenotyping of human blood has emerged as a cornerstone technology for investigating complex physiological and pathological processes, from the gradual alterations of immune aging to the dynamic responses in cancer immunotherapy [15]. The ability to rapidly analyze multiple physical and chemical characteristics of thousands of cells per second provides a powerful tool for comprehending system-wide immune changes [1]. Recent technological advancements, including full-spectrum flow cytometry and mass cytometry, have further expanded our analytical capabilities, allowing simultaneous measurement of up to 40 cellular parameters from a single sample [25] [2]. This application note details standardized protocols and analytical frameworks for employing high-throughput flow cytometry in two critical research domains: deciphering age-related immune alterations and advancing cancer immunotherapy development.
High-Throughput Flow Cytometry in Immune Aging Research
Experimental Protocol for Large-Scale Immune Aging Studies
Sample Processing Pipeline:
- Sample Collection: Collect peripheral blood mononuclear cells (PBMCs) from participants using standardized venipuncture procedures into anticoagulant tubes. Process samples within 4-8 hours of collection to maintain cell viability [15].
- PBMC Isolation: Isolate PBMCs using density gradient centrifugation (Ficoll-Paque PLUS) at 400-500 × g for 30-35 minutes at room temperature with minimal brake. Wash cells twice in PBS and count using automated cell counters [15].
- Cryopreservation: Resuspend PBMCs in freeze medium (90% FBS, 10% DMSO) at 5-10×10^6 cells/vial. Use controlled-rate freezing containers overnight at -80°C before transfer to liquid nitrogen for long-term storage [15].
High-Throughput Staining Protocol:
- Thawing and Recovery: Rapidly thaw cryopreserved PBMCs in a 37°C water bath. Transfer dropwise to pre-warmed complete medium. Centrifuge at 300 × g for 5 minutes. Resuspend in culture medium with DNase I (0.1 mg/mL) and incubate for 1-2 hours at 37°C to recover [15].
- Viability Staining: Use live/dead fixable viability dyes (e.g., Zombie UV) at 1:1000 dilution in PBS for 15 minutes at room temperature. Wash with FACS buffer (PBS + 2% FBS) [15].
- Surface Staining: Incubate cells with preconjugated antibody cocktails for 30 minutes at 4°C in the dark. Use optimized antibody concentrations determined through prior titration [15].
- Intracellular Staining (Optional): For transcription factors or cytokines, fix and permeabilize cells using commercial fixation/permeabilization buffers according to manufacturer protocols [15].
- Data Acquisition: Acquire data on calibrated spectral flow cytometers with daily QC using calibration beads. Collect a minimum of 2×10^6 events per sample to ensure adequate representation of rare populations [15].
Table 1: Key Immune Subsets for Aging Studies
| Immune Compartment | Specific Subsets | Phenotypic Markers | Age-Associated Changes |
|---|---|---|---|
| T Cells | Naïve CD4+ T cells | CD3+, CD4+, CD45RA+, CCR7+ | Decreased with age [15] |
| T Cells | Naïve CD8+ T cells | CD3+, CD8+, CD45RA+, CCR7+ | Decreased with age [15] |
| T Cells | Effector Memory CD4+ T cells | CD3+, CD4+, CD45RO+, CCR7- | Increased with age [15] |
| T Cells | Terminal Differentiated CD8+ T cells | CD3+, CD8+, CD45RA+, CD57+ | Increased with age [15] |
| B Cells | Naïve B cells | CD19+, CD27-, IgD+ | Decreased with age [15] |
| B Cells | Memory B cells | CD19+, CD27+ | Variable changes with age [15] |
| Monocytes | Classical monocytes | CD14++, CD16- | Increased inflammatory profile [15] |
Data Analysis Workflow for Aging Studies
Automated Analysis Pipeline:
- Data Pre-processing: Implement bead-based normalization and batch effect correction algorithms. Apply doublet exclusion gates based on FSC-H vs FSC-A parameters [15].
- Unsupervised Analysis: Utilize FlowSOM clustering for population identification without researcher bias. Run t-distributed Stochastic Neighbor Embedding (t-SNE) or Uniform Manifold Approximation and Projection (UMAP) for visualization [15].
- Population Tracking: Identify and quantify 30+ immune subsets simultaneously using automated gating strategies validated against manual analysis [15].
- Immune Age Modeling: Integrate flow cytometry data with clinical parameters to develop predictive models of immunological aging [2].
Flow Cytometry Applications in Cancer Immunotherapy
Diagnostic and Monitoring Applications
Flow cytometry has become indispensable in cancer immunotherapy, from initial diagnosis to treatment monitoring [26]. In hematological malignancies, immunophenotyping enables precise classification of leukemias and lymphomas by identifying aberrant expression profiles not visible to morphological examination alone [1]. The technology's true power emerges in its ability to track minimal residual disease (MRD) with sensitivity sufficient to predict relapse in patients with acute lymphoblastic leukemia, as demonstrated by studies showing day 22 MRD assessment is predictive of relapse [2]. Beyond diagnostics, flow cytometry facilitates critical evaluation of engineered cellular therapies, including detection of chimeric antigen receptors (CARs) on various engineered effector cells and assessment of their specificity in engaging targets [26].
Table 2: Flow Cytometry Applications in Cancer Immunotherapy
| Application Domain | Specific Use Cases | Key Parameters | Clinical Utility |
|---|---|---|---|
| Diagnosis & Classification | Leukemia/Lymphoma immunophenotyping | CD markers, light chain restriction, aberrant markers | Disease classification according to WHO guidelines [1] |
| Treatment Monitoring | Minimal Residual Disease (MRD) | Leukemia-associated immunophenotypes (LAIPs) | Predict relapse, guide treatment intensity [2] |
| Cellular Therapy | CAR-T cell monitoring | CAR expression, activation markers, memory subsets | Assess persistence and functionality [26] |
| Immune Checkpoint Inhibition | T-cell exhaustion profile | PD-1, CTLA-4, LAG-3, TIM-3 | Predict response to checkpoint inhibitors [25] |
| Tumor Microenvironment | Immune contexture analysis | Myeloid-derived suppressor cells, Tregs, macrophage polarization | Understand mechanisms of resistance [25] |
Protocol for Immunotherapy Monitoring
Comprehensive Immunophenotyping Panel for Immunotherapy:
- Sample Requirements: Bone marrow aspirates (for MRD), peripheral blood (for circulating biomarkers), or tumor biopsies (for microenvironment analysis) [26] [1].
- Antibody Panel Design: Incorporate 20-30 parameters covering lineage markers (CD3, CD19, CD56), activation markers (CD25, CD69, HLA-DR), exhaustion markers (PD-1, CTLA-4, LAG-3, TIM-3), memory subsets (CD45RA, CCR7, CD27), and functional markers (CD107a, cytokines) [25].
- Staining Procedure: Follow similar protocol as in Section 2.1 with extended antibody panel. Include Fc receptor blocking step to minimize non-specific binding [26].
- CAR-T Cell Detection: Use target-specific tetramers or labeled ligands to confirm CAR specificity and functionality [26].
- Functional Assessment: Stimulate cells with PMA/ionomycin or specific antigens in the presence of brefeldin A/monensin for 4-6 hours to evaluate cytokine production (IFN-γ, TNF-α, IL-2) [26].
Advanced Analytical Approaches:
- High-Dimensional Analysis: Apply CITRUS or ACCENSE algorithms to identify correlative cell populations associated with treatment response [25].
- Longitudinal Monitoring: Establish baseline immunophenotypes pre-treatment and track dynamic changes throughout therapy [26].
- Biomarker Identification: Correlate specific immune signatures with clinical outcomes to identify predictive biomarkers [25].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for High-Throughput Immunophenotyping
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Viability Dyes | Zombie dyes, Fixable Viability Dye eFluor | Distinguish live/dead cells | Critical for accurate population quantification [15] |
| Antibody Panels | CD markers, cytokine antibodies, signaling molecules | Cell population identification and characterization | Require extensive titration and validation [1] |
| Intracellular Staining Kits | FoxP3/Transcription Factor Staining Buffer Set | Permeabilization for intracellular targets | Essential for transcription factors, cytokines [26] |
| Standardization Beads | Rainbow beads, calibration beads | Instrument standardization and QC | Enable cross-experiment comparison [15] |
| Cell Preparation Reagents | Ficoll-Paque, RBC lysis buffers, DNase I | Sample processing and preparation | Affect cell recovery and viability [15] |
| CyTOF Reagents | Metal-tagged antibodies, cell intercalators | Mass cytometry analysis | Enables 40+ parameter analysis [2] |
Technological Advances and Standardization
The field of flow cytometry continues to evolve with recent technological advances significantly enhancing our research capabilities. Full Spectrum Flow Cytometry (FSFC) represents a particularly impactful innovation, capturing the complete emission spectrum of fluorescent molecules using arrays of highly sensitive light detectors and enabling characterization of 40+ parameters in a single sample [25]. This technology provides improved sensitivity, especially for dim and rare cell populations in complex multicolor samples. Similarly, mass cytometry (CyTOF) combines traditional flow cytometry with mass spectroscopy, allowing highly multiplexed measurements of up to 40 cellular parameters without compensation challenges [2].
Standardization remains crucial for generating reproducible, reliable data, particularly in multi-center studies and clinical trials. Implementation of standardized panels and protocols ensures consistency and accuracy in disease monitoring across different laboratories [1]. Recent efforts have focused on reducing variability through rigorous instrument standardization, staining protocols, quality controls, and automated data analysis [15]. The integration of artificial intelligence with multi-parameter flow cytometry shows particular promise for improving diagnostic efficiency, with one innovative model demonstrating 91.8% sensitivity and 92.5% specificity for diagnosing myelodysplastic syndromes [2]. These technological and methodological advances collectively enhance the precision and throughput of immunophenotyping studies, solidifying flow cytometry's role as an indispensable tool in both basic research and clinical translation.
In the realm of high-throughput flow cytometry for immunophenotyping human blood, large-scale studies are pivotal for advancing biomarker discovery and therapeutic development. However, their success is often hampered by technical challenges that introduce variability, potentially compromising data quality, reproducibility, and the validity of translational findings [27] [28]. This application note details the primary sources of variability and provides standardized protocols to mitigate them, ensuring robust and reliable data in large cohort analyses.
Major Technical Challenges and Mitigation Strategies
The transition of flow cytometry from a low-throughput research tool to a high-throughput platform for large studies exposes several inherent challenges. The table below summarizes the key sources of variability and recommended mitigation approaches.
Table 1: Key Sources of Variability and Strategic Mitigations in Large Studies
| Challenge Category | Specific Source of Variability | Impact on Data | Recommended Mitigation Strategy |
|---|---|---|---|
| Sample Preparation | Variation in tissue dissociation methods [27]; Use of erythrolytic solutions & density gradients [29]; Anticoagulant choice & sample aging [30] [28] | Altered cell viability, loss of rare populations, changes in surface marker expression [27] [29] | Adopt standardized, minimal manipulation protocols (e.g., "no-wash, no-lyse") [29]; Define strict sample acceptance & processing time windows [28] |
| Instrument Operation | Daily performance fluctuation; Inter-instrument variability between sites; Differences in laser power & detector sensitivity [27] | Inconsistent fluorescence measurements, preventing cross-site & longitudinal data comparison | Implement daily quality control with calibration beads; Standardize instrument settings across sites; Use cross-laboratory Standard Operating Procedures (SOPs) [27] [28] |
| Panel Design & Reagents | Spectral overlap & improper compensation [31]; Lot-to-lot variability of antibodies [27] | False-positive signals, inaccurate population quantification, inability to resolve dim markers | Careful fluorophore selection to minimize spillover; Use of bright fluorophores for low-abundance targets [31]; Validate panels with reference standards [27] |
| Data Analysis | Subjective or non-standardized gating strategies; Complex high-dimensional data interpretation [27] | Inconsistent population definitions, introduction of analyst bias, failure to detect rare events | Utilize automated analysis pipelines & clustering algorithms; Establish pre-defined, validated gating strategies; Leverage AI/machine learning tools [27] |
Quantitative Impact of Variability
Understanding the scale of these challenges is crucial for risk assessment. The following table compiles quantitative data related to market growth, technical capabilities, and variability thresholds.
Table 2: Quantitative Data in Flow Cytometry Applications
| Parameter | Quantitative Value | Context / Significance |
|---|---|---|
| Market Growth (CAGR) | 7.53% (2025-2035) | Reflects expanding use in drug discovery and clinical trials in Europe [32]. |
| High-Throughput Speed | Tens of thousands of cells per second | Enables screening of tens of thousands of compounds per day [27]. |
| Multiparameter Analysis | >40 fluorophores simultaneously [28] | Allows for deep, comprehensive immune profiling at a single-cell level. |
| Viability Cutoff | Sample aging and staining stability studies required | Determines the cutoff for sample testing and acquisition to ensure data quality [28]. |
| Compensation Control | Positive population should be at least 10% of total sample | A guideline for setting accurate fluorescence compensation [31]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
A successful large study relies on consistent and high-quality materials. The following table lists essential reagents and their functions in the workflow.
Table 3: Key Research Reagent Solutions for Blood Immunophenotyping
| Item | Function / Application | Example Product Types |
|---|---|---|
| Blood Collection Tubes | Prevents coagulation for viable cell analysis; choice of anticoagulant (e.g., Heparin, EDTA) can be critical. [30] | Heparin, K2EDTA, or K3EDTA tubes [30] |
| Flow Cytometry Staining Buffer | Provides an optimized medium for antibody staining and washing steps while preserving cell integrity. | Phosphate-buffered saline (PBS)-based buffers [30] |
| Fluorophore-conjugated Antibodies | Specific detection of surface, intracellular, and intranuclear antigens. Validation for flow cytometry is key. | Invitrogen Flow Cytometry Antibodies [30] |
| Viability Dye | Distinguishes live from dead cells, preventing false-positive staining from compromised cells. | SYTOX Dead Cell Stain (non-fixable, impermeant nucleic acid dye) [30] |
| RBC Lysis Buffer | Removes red blood cells from whole blood samples to facilitate analysis of leukocytes. | 1X or 10X RBC Lysis Buffer (multi-species) [30] |
| Fixation/Permeabilization Buffers | Enables intracellular (e.g., cytokines, transcription factors) and intranuclear staining by making membranes permeable. | 1-Step Fix/Lyse Solution, 10X Permeabilization Buffer [30] |
| Compensation Beads | Highly uniform particles used to set fluorescence compensation controls for each fluorophore independently of biological samples. | Antibody capture beads [31] |
Experimental Protocol: Standardized Whole Blood Immunophenotyping with Minimal Sample Manipulation
This detailed protocol is designed for the immunophenotyping of human whole blood, prioritizing minimal sample perturbation to reduce variability associated with preparation [29]. It is optimized for high-throughput workflows.
Sample Acquisition and Initial Handling
- Blood Collection: Collect venous blood into tubes containing an anticoagulant such as K2EDTA, K3EDTA, or heparin [30].
- Aliquoting: Aliquot 100 µL of unlysed whole blood into a 12 x 75 mm round-bottom polystyrene tube for each staining condition. This small volume is suitable for high-throughput screens [30].
- Controls: Prepare separate aliquots for unstained cells and single-color compensation controls for every fluorophore used in the panel [30] [31].
Cell Surface Staining (No-Wash, No-Lyse Method)
- Antibody Cocktail Preparation: Prepare the antibody master mix in flow cytometry staining buffer. Critical: Titrate all antibodies beforehand. For low-abundance antigens or rare cell populations, use the brightest fluorophores (e.g., PE, APC) [31].
- Staining: Add the antibody cocktail directly to the 100 µL whole blood aliquot.
- Incubation: Incubate for 30 minutes at 2–8°C (on ice, protected from light). Do not wash. [29]
- Optional Viability Staining: If using a non-fixable viability dye like SYTOX, add 0.5 µL per 500 µL of sample, incubate for 20 minutes at room temperature in the dark, and proceed without washing [30].
Optional Erythrocyte Lysis and Fixation
- If lysing RBCs is necessary for the analytical workflow, add 2 mL of a room-temperature 1-Step Fix/Lyse Solution per 100 µL of blood at this stage [30].
- Invert gently and incubate for 15-60 minutes at room temperature, protected from light. Samples can then be stored at 2–8°C for up to 48 hours before acquisition [30].
Data Acquisition on Flow Cytometer
- Instrument Setup: Prior to sample acquisition, run compensation controls and use calibration beads to ensure consistent instrument performance [27].
- Acquisition: Analyze samples on a flow cytometer. Filter samples through a 0.45 µM cell strainer if debris is present [30].
- High-Throughput Tip: For large studies, utilize cytometers with autoloaders capable of acquiring samples from 96-, 384-, or 1536-well plates [27].
Figure 1: Simplified workflow for minimal manipulation immunophenotyping.
Data Analysis and Gating Strategy for Standardization
Standardizing data analysis is as critical as standardizing wet-lab procedures.
- Automated Gating and AI Assistance: For large studies, employ automated clustering algorithms and machine learning tools to minimize subjective bias and increase analysis throughput and reproducibility [27].
- Pre-defined Gating Strategy: Establish and validate a gating strategy before the study begins. An example for identifying T regulatory (Treg) cells is: CD4+ → CD25+ → CD127- → Foxp3+ [28].
- Optimal Visualization for Gating:
- Dot Plots: Use for accurate gating, especially for resolving tightly clustered populations [33].
- Contour or Density Plots: Ideal for visualizing the overall structure and density of cell populations [33].
- Cumulative Distribution Function (CDF) Plots: Powerful for overlaying and comparing fluorescence intensity distributions between samples, such as from drug-treated vs. control groups [33].
Figure 2: Key sources of variability impacting data harmonization in multi-center studies.
Implementing High-Throughput Pipelines: From Sample Processing to Data Acquisition
High-throughput flow cytometry is a cornerstone of modern immunology and drug development, enabling the detailed characterization of immune cells from hundreds to thousands of human blood samples. The reliability of these studies hinges on stringent sample processing protocols that minimize technical variability. This application note details optimized methodologies for thawing, staining, and quality control specifically designed for high-throughput immunophenotyping studies, providing a robust pipeline essential for large cohort human blood research [15].
Critical Pre-Analytical Considerations
Sample Type Selection
The choice between whole blood (WB) and peripheral blood mononuclear cells (PBMCs) significantly impacts the immunophenotypic profile. While PBMCs are a common source for immunometabolic profiling, recent evidence suggests that WB can serve as a viable alternative, offering a more physiologically relevant representation for certain markers and simplifying logistics for multicenter studies [34]. However, Table 1 highlights key comparative considerations.
Table 1: Comparison of Whole Blood and PBMC Samples for High-Throughput Immunophenotyping
| Parameter | Whole Blood (WB) | Peripheral Blood Mononuclear Cells (PBMCs) |
|---|---|---|
| Physiological Relevance | Higher; fewer ex vivo processing steps [34] | Lower; isolation process can alter cell state |
| Granulocyte Inclusion | Yes, includes all blood immune cells [34] | No, loses granulocytes during density gradient separation [34] |
| Processing Complexity | Less technically challenging; suitable for resource-limited settings [34] | Requires specialized equipment and skilled personnel [34] |
| Required Blood Volume | Small volumes (e.g., 200 µL) sufficient [34] | Larger blood volumes typically needed [34] |
| Marker Concordance | High global similarity to PBMCs, but differences in specific markers like GLUT1 in certain subsets exist [34] | Gold standard, but may not reflect full in vivo state for all markers |
Cryopreservation Methods
The choice of cryopreservation method profoundly affects cell viability and marker integrity. A systematic comparison of five cryopreservation methods revealed that methods using dimethyl sulfoxide (DMSO)-based solutions (e.g., CryoStor) generally produced immunophenotyping data most similar to fresh samples. In contrast, methods relying on fixative solutions often prevented the reliable detection of critical markers such as CD27, CXCR3, and CCR6 [35]. Long-term stabilization of WB for up to 48 months is achievable with reagents like TransFix, which maintains lymphocyte subset proportions with no significant differences from fresh samples [36].
Experimental Protocols
Protocol: Thawing Cryopreserved PBMCs
This protocol is adapted from the HANC member network IMPAACT PBMC Thawing SOP, a gold-standard guideline for clinical trial research [37].
- Step 1. Rapid Thawing: Thaw cryovials in a 37°C water bath for approximately 2 minutes, until only a small ice crystal remains. Ensure the vial cap is above the water line to prevent contamination.
- Step 2. Dilution and Washing: Transfer the cell suspension to a 15 mL tube prefilled with 5-10 mL of pre-warmed (37°C) thawing media (e.g., RPMI-1640 supplemented with 20-50% Fetal Bovine Serum). Gently mix by pipetting. Centrifuge at 400*g for 5-10 minutes at room temperature. Note: The protein in the serum is critical for protecting cell membranes during this vulnerable step.
- Step 3. Red Blood Cell Lysis (if needed): For WB samples or PBMC preparations contaminated with RBCs, resuspend the cell pellet in 3 mL of Ammonium-Chloride-Potassium (ACK) lysis buffer. Incubate for 2 minutes at room temperature. Quench the reaction with 10 mL of wash buffer (e.g., PBS with 0.5-1% BSA) [34].
- Step 4. Final Wash and Resuspension: Centrifuge the cells again at 400*g for 5-10 minutes. Carefully decant the supernatant and resuspend the cell pellet in an appropriate staining buffer or culture medium. Keep samples at 4°C throughout the subsequent procedures to maintain viability [38] [34].
Protocol: High-Throughput In-Plate Staining for Spectral Flow Cytometry
This protocol is optimized for 96-well plates and clinical trial samples, enabling the processing of 192 samples per experiment [15] [39].
- Step 1. Plate Preparation and Viability Staining: Distribute up to 10^7 cells per well of a 96-well conical-bottom plate. Pellet cells by centrifugation (300-400*g for 5 minutes) and decant the supernatant. Resuspend cells in 100 µL of PBS containing a live/dead fixable viability dye (e.g., Zombie NIR, diluted 1:1,250), 1:20 True-Stain Monocyte Blocker, and 1:50 Fc block. Incubate for 15 minutes at room temperature in the dark [34] [39].
- Step 2. Surface Staining: Without a washing step, add directly titrated antibody cocktails diluted in FACS buffer (PBS with 2mM EDTA and 0.5% BSA). The final volume per well is typically 100 µL. Incubate for 30 minutes at 4°C in the dark. Note: Antibody titration and the use of counting beads are mandatory for assay accuracy and reproducibility [39].
- Step 3. Washing and Fixation: Add 180 µL of FACS buffer to each well and centrifuge at 300-400*g for 5 minutes. Decant the supernatant by inverting the plate. Repeat this wash step. After the final wash, resuspend cells in 100-200 µL of FACS buffer, possibly containing 1-4% paraformaldehyde (PFA) for fixation. Filter the cell suspension through a 70 µm strainer before acquisition to remove clumps [38] [39].
- Step 4. Data Acquisition: Acquire data on a spectral flow cytometer (e.g., Sony ID7000). For ultra-high-throughput, platforms like HyperCyt can be integrated, automating sample aspiration from plates and achieving analysis rates of up to 40 samples per minute [39] [40].
Diagram 1: High-throughput immunophenotyping workflow.
Quality Control and Troubleshooting
Implementing Quality Control Checkpoints
Robust quality control (QC) is non-negotiable for high-throughput studies. Key checkpoints include:
- Instrument Standardization: Daily calibration using standardized beads ensures consistent performance across experiments [15].
- Viability and Purity: Cell viability should be >85% post-thaw for reliable results. Use a live/dead stain for accurate assessment [38].
- Clump and Debris Prevention: Add DNase I to buffers and include EDTA to prevent calcium-dependent aggregation. Gentle handling, avoiding vigorous vortexing, and using round-bottom tubes facilitate complete resuspension [38].
Troubleshooting Common Issues
Table 2 outlines common staining problems and their solutions.
Table 2: Troubleshooting Guide for Flow Cytometry Staining
| Problem | Likely Cause | Solution |
|---|---|---|
| High Background Staining | Insufficient washing; antibody concentration too high [38] | Increase wash steps; titrate antibodies to determine optimal concentration [38] |
| Low Positive Signal | Antibody concentration too low; inadequate permeabilization for intracellular targets [38] | Optimize antibody concentration; extend permeabilization step [38] |
| Compensation Issues | Inadequate single-color controls [38] | Use compensation beads if there are few positive cells in the sample [38] [39] |
| Low Cell Viability | Harsh processing; extended storage at room temperature [38] | Gentle handling; keep samples at 4°C throughout procedure [38] |
| Cell Clumping | DNA release from dead cells; Ca²⁺/Mg²⁺ in buffers [38] | Add DNase I; use metal-free buffers like HBSS without Ca²⁺/Mg²⁺ [38] |
Data Analysis and Integration
For high-dimensional data, automated analysis pipelines are essential. Integrating tools like FlowSOM for unsupervised clustering facilitates rapid and reproducible cell population discovery [15]. Furthermore, advanced computational frameworks like Interact-omics can be applied a posteriori to existing cytometry data to map physical cell-cell interactions, extracting additional layers of biological insight from high-throughput datasets [41].
The Scientist's Toolkit
Table 3: Essential Reagents and Materials for High-Throughput Flow Cytometry
| Item | Function/Purpose | Example Products/Formats |
|---|---|---|
| Cryopreservation Medium | Preserves cell viability and antigen integrity during frozen storage | CryoStor CS10, 10% DMSO in FBS [34] [35] |
| Cell Stabilization Reagent | Enables long-term ambient or frozen storage of whole blood | TransFix [36] |
| Viability Dye | Distinguishes live from dead cells, critical for data accuracy | Zombie NIR Fixable Viability Kit, Live/Dead Fixable Blue [34] [39] |
| Fc Receptor Block | Reduces non-specific antibody binding | Human TruStain FcX, True-Stain Monocyte Blocker [34] [39] |
| Brilliant Stain Buffer | Prevents fluorochrome interaction and degradation, essential for polychromatic panels | BD Horizon Brilliant Stain Buffer Plus [39] |
| Counting Beads | Enables absolute cell counting, improving data quantification | CountBright Plus Beads [39] |
| Compensation Beads | Generate consistent single-color controls for spectral unmixing | UltraComp eBeads Plus, ArC Amine Reactive Beads [39] |
In high-throughput flow cytometry immunophenotyping of human blood, the design of multicolor panels is a critical step that directly impacts data quality and experimental conclusions. Fluorescence spillover, the phenomenon where a fluorochrome's signal is detected in channels beyond its primary emission peak, is an inherent challenge in multiparametric flow cytometry [42] [43]. Effective management of this spillover through careful fluorochrome selection and experimental design is essential for maintaining resolution and sensitivity, particularly when detecting low-abundance antigens in complex populations like human peripheral blood mononuclear cells (PBMCs) [3].
Spillover arises from three primary sources: the broad emission spectra of fluorochromes leading to spectral overlap between adjacent detectors; the partial dissociation of tandem dyes which releases emission from the donor fluorophore; and cross-laser excitation where a fluorochrome is excited by multiple laser lines [43] [44]. While compensation mathematically corrects for spillover, it cannot fully restore the loss of sensitivity caused by spillover spreading—the increased variance in detection channels affected by bright fluorochromes [42] [3]. For high-throughput immunophenotyping studies where reproducibility across plates and batches is paramount, implementing rigorous spillover management strategies during panel design is non-negotiable.
Principles of Fluorochrome Selection
Strategic Antigen-Fluorophore Pairing
The cornerstone of effective panel design is the strategic pairing of antigens with appropriate fluorophores based on their expression patterns and biological context [3] [44].
Bright fluorophores for low-abundance antigens: Allocate your brightest fluorophores (e.g., PE, APC, Brilliant Violet 421) to markers expressed at low levels on target cells [45] [3]. For human blood immunophenotyping, this might include cytokines, transcription factors, or low-density surface receptors.
Dim fluorophores for highly expressed antigens: Assign dimmer fluorophores (e.g., FITC, PerCP-Cy5.5) to abundantly expressed markers such as CD45, CD3, CD4, or CD19 in human blood samples [3]. This practice minimizes spillover spreading into other channels.
Spectral characteristics for co-expressed markers: When measuring co-expressed markers (e.g., CD4 and CD8 on different T-cell subsets), use fluorophores with minimal spectral overlap to maintain clear population resolution [3]. Conversely, markers expressed on mutually exclusive cell populations can share more similar emission spectra [44].
Fluorochrome Performance Characteristics
Different fluorochrome classes exhibit distinct performance characteristics that must be considered during selection. The table below summarizes key properties of common fluorochromes used in human blood immunophenotyping:
Table 1: Performance Characteristics of Common Fluorochromes in Human Blood Immunophenotyping
| Fluorochrome | Relative Brightness | Excitation Laser(s) | Emission Peak (nm) | Spillover Profile | Best Use Cases |
|---|---|---|---|---|---|
| Brilliant Violet 421 | Very bright | Violet | 421 | Moderate | Low-abundance antigens |
| FITC | Dim | Blue | 525 | Low | Highly expressed antigens |
| PE | Very bright | Blue | 575 | High | Critical low-expression markers |
| PE-Cy7 | Bright | Blue | 785 | Very high (multiple lasers) | With careful spillover management |
| APC | Bright | Red | 660 | Moderate | Medium to high expression markers |
| APC-Cy7 | Bright | Red | 785 | High (multiple lasers) | With careful spillover management |
| PerCP-Cy5.5 | Moderate | Blue | 690 | High (into PE, BV711) [3] | Medium expression markers |
When selecting fluorochromes, prioritize those with minimal cross-laser excitation, as they produce cleaner signals with lower impact on other fluorochromes in the panel [42]. For example, in a comparative evaluation of blue laser-excited fluorochromes with emission around 700 nm, BD Horizon RealBlue 705 (RB705) and NovaFluor Blue 690 (NFB690) demonstrated the least emission into other channels, making them superior choices for complex panels [42].
Experimental Protocols for Spillover Management
Protocol 1: Antibody Titration for Optimal Signal-to-Noise
Purpose: To determine the antibody concentration that provides optimal separation between positive and negative populations while minimizing spillover spreading [3].
Materials:
- Antibody of interest, conjugated to selected fluorophore
- Fresh human PBMCs or relevant cell line
- Flow cytometry staining buffer (PBS + 1-2% FBS + 0.09% sodium azide)
- 96-well U-bottom plates
- Flow cytometer with appropriate lasers and filters
Procedure:
- Prepare a single-cell suspension of human PBMCs at 5-10 × 10^6 cells/mL in flow cytometry buffer.
- Perform serial 2-fold dilutions of the antibody, starting from the manufacturer's recommended concentration.
- Aliquot 100 µL of cell suspension (0.5-1 × 10^6 cells) into each well of a 96-well plate.
- Add 100 µL of each antibody dilution to separate wells, including an unstained control.
- Incubate for 30 minutes in the dark at 4°C.
- Wash cells twice with 200 µL flow cytometry buffer.
- Resuspend cells in 200 µL flow cytometry buffer and acquire immediately on flow cytometer.
- Calculate the Stain Index (SI) for each dilution: SI = (Meanpositive - Meannegative) / (2 × SD_negative) [3].
- Plot SI versus antibody concentration and select the "separating concentration" at the point where the SI begins to plateau.
Table 2: Example Antibody Titration Data for CD8-APC in Human PBMCs
| Antibody Dilution | Mean Positive | Mean Negative | SD Negative | Stain Index | Recommended Use |
|---|---|---|---|---|---|
| 1:10 | 45,280 | 890 | 210 | 105.7 | Saturating |
| 1:20 | 38,150 | 820 | 195 | 95.8 | Saturating |
| 1:40 | 25,430 | 780 | 188 | 65.6 | Separating |
| 1:80 | 12,560 | 745 | 182 | 32.5 | Suboptimal |
| 1:160 | 5,230 | 720 | 175 | 12.9 | Too dilute |
Protocol 2: Validation of Compensation Controls
Purpose: To prepare and validate single-stained compensation controls that accurately measure spectral spillover for proper compensation [43].
Materials:
- UltraComp compensation beads or ArC amine-reactive compensation beads
- Identical antibody conjugates used in the panel
- Viability dye (if used in panel)
- Cell staining buffer
- Unstained cells matching experimental samples
Procedure:
- Substrate Selection: For most surface markers, use antibody capture compensation beads. For viability dyes and intracellular markers, use amine-reactive compensation beads or heat-killed cells [43].
- Staining: Follow manufacturer's instructions for staining compensation beads with each antibody conjugate. For cellular controls, use bright, specific populations (e.g., CD4+ T-cells for anti-CD4 antibodies).
- Quality Control: Verify that the positive signal for each control is at least as bright as the fully stained experimental samples [43].
- Negative Control Preparation: Include unstained beads and unstained cells as separate negative controls if using both substrates [43].
- Acquisition: Acquire compensation controls before experimental samples using the same instrument settings.
- Validation: Check for contamination by ensuring each single-stained control shows spillover only into expected channels.
Diagram 1: Compensation Control Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for High-Throughput Flow Cytometry
| Reagent/Category | Specific Examples | Function/Purpose | Application Notes |
|---|---|---|---|
| Compensation Beads | UltraComp eBeads, ArC Beads | Provide consistent, bright signals for spillover calculation | Antibody-capture beads for surface markers; amine-reactive for viability dyes [43] |
| Viability Dyes | LIVE/DEAD Fixable Stains, ViaComp Beads | Distinguish live/dead cells to exclude apoptotic cells | Dead cells nonspecifically bind antibodies; exclusion critical for accuracy [3] |
| FMO Controls | Custom mixtures minus one antibody | Establish accurate gating boundaries | Essential for setting gates in multicolor panels [3] |
| Reference Fluorophores | RB705, NFB690, BB700 | Low-spillover fluorophores for panel benchmarking | Fluorochromes with minimal cross-laser excitation improve panel resolution [42] |
| High-Throughput Platform | HTFC Screening System | Automated sample acquisition | Enables processing of 384-well plates in ~12 minutes [46] |
Panel Validation and Troubleshooting
Spillover Spread Matrix Analysis
Purpose: To visualize and quantify the impact of spillover spreading across all detector channels in a multicolor panel [3].
Procedure:
- Prepare single-stained controls for each fluorophore in the panel using the validated compensation control protocol.
- Acquire data for each control using the same voltage settings as the full panel.
- Analyze data using flow cytometry analysis software (e.g., FlowJo, FCS Express) to generate a spillover spread matrix.
- Identify problematic fluorophores that contribute excessive spreading error into multiple channels.
- Iteratively replace high-spread fluorophores with alternatives that have cleaner emission profiles.
Table 4: Example Spillover Spread Matrix (Percent Spread Values)
| Fluorophore | FITC | PE | PerCP-Cy5.5 | PE-Cy7 | APC | APC-Cy7 | BV421 |
|---|---|---|---|---|---|---|---|
| FITC | - | 0.5 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 |
| PE | 1.2 | - | 2.5 | 8.5 | 0.8 | 0.3 | 0.2 |
| PerCP-Cy5.5 | 0.3 | 15.2 | - | 1.2 | 5.7 | 0.5 | 0.2 |
| PE-Cy7 | 0.2 | 2.8 | 1.5 | - | 1.3 | 12.5 | 0.1 |
| APC | 0.1 | 0.5 | 3.2 | 0.8 | - | 8.5 | 0.1 |
| APC-Cy7 | 0.1 | 0.3 | 0.8 | 3.2 | 5.5 | - | 0.1 |
| BV421 | 0.1 | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | - |
Troubleshooting Common Issues
Diagram 2: Troubleshooting Flow Cytometry Issues
When troubleshooting panel performance in high-throughput immunophenotyping, several systematic approaches can identify and resolve common issues:
- Poor resolution between positive and negative populations: Re-titrate antibodies and verify detector voltages using the voltage walk method to ensure optimal signal separation [3].
- Compensation artifacts or diagonal spreading: Prepare fresh single-stained controls and check for contamination during staining [43].
- Unexpected population shifts in fully stained samples: Run FMO controls to establish correct gating boundaries and identify spillover effects [3].
- Inconsistent results across high-throughput screens: Standardize reagent lots and ensure identical staining protocols across all plates to minimize technical variability.
Effective design of multicolor flow cytometry panels for high-throughput immunophenotyping requires a systematic approach to fluorochrome selection and spillover management. By implementing the protocols and principles outlined in this application note—including strategic antigen-fluorophore pairing, rigorous antibody titration, validation of compensation controls, and thorough panel validation—researchers can maximize panel resolution and data quality. The integration of these practices with appropriate experimental controls and troubleshooting methodologies ensures reliable, reproducible results in drug development and clinical research applications involving human blood immunophenotyping.
Automated Staining and Acquisition Systems for 96/384-Well Plates
The integration of high-throughput flow cytometry into immunophenotyping studies has become crucial for advancing human immunology research and drug development. This approach enables the comprehensive analysis of complex immune systems in large cohorts, facilitating discoveries in immune aging, cancer biology, and therapeutic development. The evolution of automated staining and acquisition systems for 96 and 384-well plates addresses critical limitations of manual methods, including technical variability, substantial time requirements, and inconsistencies in data quality that can compromise research outcomes in large-scale studies [15]. Recent advancements have focused on creating fully automated, zero-waste systems that maintain data quality comparable to conventional methods while dramatically increasing throughput and reproducibility [47]. This application note details the current technologies, protocols, and analytical frameworks that support robust, high-throughput immunophenotyping of human blood samples.
Automated Staining Systems and Technologies
Advanced Staining Platforms
The Staining Triad represents a significant innovation in flow cytometry sample preparation, achieving full automation of the staining process from sample and reagent input to final output without manual intervention. This system demonstrates comparable biomarker profiles to conventional manual staining while addressing sustainability concerns through zero-waste operation. Key to its design is the elimination of pipette tips, the primary source of plastic waste in flow cytometry workflows. The system exemplifies the transition from 3R (Reduce, Reuse, Recycle) to 4R (Remove/Replace) sustainability strategies in laboratory practice. Its modular and adaptable design allows flexibility in throughput and assay-specific requirements, extending its applicability to various plate-based ligand binding assays [47].
For robotic liquid handling, systems like the Hamilton Microlab VANTAGE Liquid Handling System provide superior consistency and precision compared to manual pipetting. These systems incorporate automated randomization capabilities essential for high-throughput experimental designs. While requiring significant upfront financial and personnel investment, robotic systems overcome the limitations of manual methods, which are constrained by throughput limitations, operator dependency, and experience-based variability [48].
High-Throughput Staining Protocols
In-plate staining protocols for spectral flow cytometry have been optimized specifically for high-throughput analysis of peripheral blood mononuclear cell (PBMC) samples from clinical research correlative studies. These protocols enable reliable immunophenotyping through rigorous antibody titration, validation, and standardized procedures. The incorporation of counting beads throughout the staining process allows for accurate, reproducible measurements of cell populations, enhancing interpretation of cell numbers in clinical contexts [39].
Table 1: Comparison of Automated Staining Systems
| System/Platform | Throughput Capacity | Key Features | Sustainability Attributes | Applications |
|---|---|---|---|---|
| Staining Triad [47] | Adaptable to 96/384-well formats | Full automation; Zero pipette tip use; Modular design | Zero-waste; Eliminates primary plastic waste source | Flow cytometry staining; Plate-based ligand binding assays |
| Robotic Liquid Handling [48] | 96/384-well formats | Consistent liquid transfers; Automated randomization; High precision | Reduces reagent consumption through precision | Organoid screening; High-content screening; 3D cell culture assays |
| High-Throughput Pipeline [15] | 192 samples/experiment | 28-color flow cytometry; Quality control checkpoints; Minimal batch effects | Reduces experimental variation and repeat work | Large immunophenotyping studies; Genetic association studies |
Automated Acquisition Systems
Spectral Flow Cytometry Acquisition
The Sony ID7000 spectral cell analyzer enables high-throughput spectral flow cytometry acquisition for 96-well plates, supporting high-parameter immunophenotyping panels. This technology is particularly valuable for comprehensive immune monitoring in clinical trial contexts, allowing simultaneous detection of numerous cell surface and intracellular markers with minimal spreading error [39]. Spectral cytometry reduces autofluorescence and improves resolution in complex panels, making it ideal for detailed immunophenotyping of human blood leukocytes.
High-Content Imaging Systems
While primarily used for imaging applications, systems like the ImageXpress Pico Automated Cell Imaging System offer complementary capabilities for plate-based screening with 96/384-well compatibility. Featuring automated brightfield, fluorescence, and Digital Confocal imaging, these systems provide preconfigured protocols for various cell-based assays including apoptosis, mitochondrial evaluation, and 3D cell models. The environmental control options (humidity, CO2, and O2) support multi-day, time lapse, and live cell assays [49].
Experimental Protocols for High-Throughput Immunophenotyping
Protocol: In-Plate Staining for Spectral Flow Cytometry of PBMCs
This protocol is optimized for high-throughput immunophenotyping of human PBMCs from clinical samples using 96-well plates [39].
Pre-Staining Preparation
- Antibody Titration: Titrate all antibodies and viability dyes using negative and positive control cells to determine optimal staining concentrations. Use compensation beads for multicolor panels.
- Panel Design: Follow established panel design rules: pair bright fluorochromes with markers of low antigen density; assign dim fluorochromes to markers with high co-expression potential to minimize spreading error.
- Validation Strategy: Devise and implement an assay validation strategy following guidelines from the International Clinical Cytometry Society and Clinical and Laboratory Standards Institute (CLSI) H62.
Staining Procedure
- Plate Preparation: Aliquot 1-2×10^6 PBMCs per well in a 96-well V-bottom plate. Centrifuge at 400-500×g for 5 minutes and decant supernatant.
- Viability Staining: Resuspend cell pellets in 100μL of diluted viability dye (e.g., Zombie NIR at 1:1,250 dilution) in PBS. Incubate for 15 minutes at room temperature protected from light.
- FC Receptor Blocking: Add human TruStain FcX without washing. Incubate for 10 minutes at 4°C.
- Surface Marker Staining: Add pre-titrated antibody cocktail directly to the viability stain. Mix gently and incubate for 30 minutes at 4°C protected from light.
- Washing: Add 200μL of flow cytometry staining buffer (e.g., PBS with 2% BSA). Centrifuge at 400-500×g for 5 minutes. Decant supernatant. Repeat twice.
- Fixation: Resuspend cells in 200μL of 1-2% paraformaldehyde in PBS. Transfer to acquisition tubes or acquire directly from plate.
- Acquisition: Add counting beads to samples for absolute cell counting. Acquire data on spectral cytometer (e.g., Sony ID7000) using validated instrument settings.
Quality Control Measures
- Instrument Standardization: Implement daily quality control using calibration particles to ensure consistent instrument performance.
- Batch Controls: Include control samples in each processing batch to monitor technical variation.
- Data Tracking: Record processing order and timing to account for potential batch effects during analysis.
Protocol: Automated High-Throughput Immunophenotyping Pipeline
This protocol outlines a robust pipeline for processing 192 samples per experiment with minimal technical variation [15].
Sample Processing Workflow
- Standardized Instrument Setup: Perform daily instrument calibration using standardized particles. Verify laser delays and photomultiplier tube voltages.
- Automated Staining: Utilize liquid handling robots for consistent reagent dispensing across all samples in 96-well plates.
- Quality Control Checkpoints:
- Pre-staining cell count and viability assessment
- Standardized incubation times across all samples
- Validation of washing efficiency through recovery calculations
- Data Acquisition: Use standardized acquisition settings with periodic quality control checks during long runs.
Data Analysis Framework
- Automated Pre-processing: Implement computational pipelines for data cleaning and normalization.
- Unsupervised Analysis: Apply FlowSOM clustering for population identification without operator bias.
- Batch Effect Correction: Use statistical methods to identify and correct for technical variation between processing batches.
- Validation: Compare results with manual gating strategies to ensure analytical accuracy.
Table 2: Essential Research Reagent Solutions for High-Throughput Flow Cytometry
| Reagent Category | Specific Examples | Function in Workflow | Application Notes |
|---|---|---|---|
| Viability Stains [39] | Zombie NIR fixable viability kit | Distinguishes live/dead cells; Critical for data quality | Titrate for optimal concentration; Use with amine-reactive compensation beads |
| FC Receptor Blockers [39] | Human TruStain FcX | Reduces nonspecific antibody binding | Add before surface staining without washing |
| Compensation Beads [39] | UltraComp eBeads Plus; ArC amine reactive compensation bead kit | Instrument compensation; Standardization | Use for both instrument setup and experimental compensation |
| Brilliant Stain Buffers [39] | Brilliant stain buffer plus | Prevents tandem dye degradation | Essential for polymer dye-based panels (Brilliant Violet) |
| Absolute Counting Beads [39] | CountBright Plus absolute counting beads | Quantifies absolute cell counts | Add before acquisition for accurate cell concentration measurement |
| Fixation Reagents [39] | Paraformaldehyde (PFA) | Preserves cellular integrity and staining | Use at 1-2% concentration; Avoid prolonged fixation |
Data Analysis and Presentation Standards
Gating Strategies for High-Throughput Data
Effective gating strategies are essential for accurate interpretation of high-throughput flow cytometry data. Interest-based gating focuses on specific cell populations or characteristics within heterogeneous samples. Sequential gating should include:
- Doublet Discrimination: Use forward scatter height versus area to exclude cell aggregates.
- Live/Dead Gating: Utilize viability dye staining to exclude dead cells.
- Lineage Gating: Identify major populations (e.g., T cells, B cells, monocytes) using lineage markers.
- Subset Analysis: Apply additional markers to identify specific subpopulations of interest [5].
When calculating population percentages, ensure proper back-calculation through gating hierarchies. For example, if 30.1% of total cells are neutrophils and 14.5% of neutrophils express IL-17a, then 4.36% (30.1 × 0.145) of the total sample are IL-17a-expressing neutrophils [5].
Data Visualization and Presentation
For publication-quality presentation of flow cytometric data:
- Graphical Standards: Use histogram overlays for marker expression comparisons, dot plots for population identification, and contour plots for visualizing density distributions.
- Statistical Annotation: Provide numerical statistics alongside graphical representations rather than relying on visual estimation of differences.
- Gating Examples: Include representative gating strategies to demonstrate the analytical approach [50].
Workflow Visualization
High-Throughput Immunophenotyping Workflow
The implementation of automated staining and acquisition systems for 96/384-well plates has transformed the landscape of high-throughput immunophenotyping in human blood research. These integrated systems provide the robustness, reproducibility, and scalability required for large cohort studies, clinical trials, and drug development applications. By adopting standardized protocols, rigorous quality control measures, and automated analytical pipelines, researchers can generate high-quality data with minimal technical variation. The continued evolution of these technologies, particularly the integration of zero-waste systems and enhanced computational analysis, will further advance our understanding of human immunology in health and disease.
Standardized Protocols for Instrument Setup and Performance Tracking
In high-throughput flow cytometry immunophenotyping of human blood, the comparison of data across different instruments, centers, and extended time periods represents a significant challenge. Variations in instrument performance, reagent lots, and operator techniques can introduce substantial variability that compromises data integrity and cross-study comparisons. Recent multicenter studies demonstrate that implementing a rigorous standardization procedure enables comparison of leukocyte population frequencies, absolute numbers, and mean fluorescence intensities (MFIs) even when data are generated from different instruments and manufacturers over extended periods [51]. For comprehensive immunophenotyping studies involving thousands of participants over several years, establishing robust protocols for instrument setup and performance tracking is not merely beneficial—it is essential for generating scientifically valid and reproducible data.
Core Standardization Workflow
A successfully implemented standardization workflow for a multicenter flow cytometry study encompasses both initial instrument harmonization and continuous performance monitoring. The following diagram illustrates this comprehensive approach:
Figure 1: Comprehensive workflow for flow cytometry standardization in multicenter studies, integrating initial calibration with ongoing quality control and data processing steps [51].
Instrument Setup and Calibration Procedures
Detector Optimization and Voltage Setting
Proper instrument setup begins with detector optimization to ensure the highest data quality. The voltage walk method represents a best practice for determining the optimal voltage setting for each flow cytometer detector. This procedure involves running dimly fluorescent beads at a series of increasing voltage settings and plotting the spread of the signal (coefficient of variation, CV) against the voltages. The minimum voltage requirement (MVR) is identified as the lowest voltage on the %rCV curve before the increase in the robust standard deviation (rSD). This ensures clear resolution of dim fluorescent signals from background instrument noise without pushing brightest signals beyond the detector's linear range [3].
Initial Instrument Harmonization
For multicenter studies, a standardized operating procedure (SOP) for instrument harmonization is critical. This process utilizes calibration beads (such as VersaComp Capture beads) to establish instrument settings that generate similar MFIs when acquiring identical samples across different instruments. In the PRECISESADS study, this approach enabled harmonization across eleven different instruments (Navios, Gallios, Canto II, Fortessa, Verse, Aria) from multiple manufacturers. The objective was to achieve inter-instrument coefficients of variation (CVs) of less than 5% during the initial calibration phase [51].
Antibody Titration and Panel Design
Antibody titration is essential for minimizing nonspecific binding and optimizing signal detection in multiparameter flow cytometry. A standard approach involves starting with the manufacturer's recommended concentration and performing serial 2-fold dilutions, then calculating the stain index (SI) for each dilution. The stain index is determined as (Mean positive cells - Mean negative cells) / (2 × SD negative cells). Researchers can then select either a separating concentration (providing optimal separation between labeled and unlabeled cells) or a saturating concentration (for low-abundance antigens), with the understanding that saturating concentrations may increase spillover spreading [3].
Table 1: Antibody Titration Results Example
| Antibody Dilution | Stain Index | Population Resolution | Spillover Spreading | Recommended Use |
|---|---|---|---|---|
| 1:50 (Manufacturer) | 18.5 | Excellent | Moderate | General use |
| 1:100 | 22.1 | Optimal | Low | Separation concentration |
| 1:200 | 19.3 | Good | Low | Conservation use |
| 1:500 | 12.7 | Moderate | Low | Bright antigens only |
| 1:1000 | 8.2 | Poor | Minimal | Not recommended |
Fluorophore Selection and Spillover Management
Careful fluorophore selection is crucial when designing multiparameter panels. The guiding principles include using bright fluorophores with antibodies for low-abundance targets, dim fluorophores with antibodies for highly expressed antigens, and minimizing spectral overlap between fluorophores. Tools such as spillover spread matrices help visualize the spreading error into all detectors for each fluorophore, enabling researchers to identify problematic combinations. For example, tandem fluorophores such as PE-Cy7 may exhibit significant spreading error that impacts resolution of dimly expressed antigens in other channels [3].
Performance Tracking and Quality Control
Daily Quality Control Procedures
Implementing daily quality control using 8-peak beads provides continuous monitoring of instrument stability. This procedure tracks the MFI of each bead population across all channels to detect deviations from the initial calibration targets. In the PRECISESADS study, researchers developed an R script to normalize results over the 4-year study period for each center based on these daily QC measurements. The script applies normalization using linear regression with determined alpha and beta parameters, using the MFI of the 8-peak beads obtained during the initial calibration procedure as reference [51].
Intra-Center Normalization Algorithm
The intra-center normalization process involves several computational steps: (1) loading necessary R packages (flowCore, flowStats, flowViz, ggcyt); (2) revising channel name position and standard names when necessary; (3) extracting the MFI from 8-peak beads files with identification of instrument-specific files and debris; (4) defining alpha and beta transformation parameters for normalization; (5) applying normalization function using linear regression; and (6) verifying the effect across all channels. Validation experiments demonstrated that this approach could correct deliberately introduced PMT variations of 10-15%, reducing coefficients of variation to less than 2.5% for bead samples and less than 5% for stained blood samples [51].
Essential Controls and Validation Procedures
Critical Experimental Controls
Implementing appropriate controls is fundamental for generating high-quality flow cytometry data. The essential controls include:
- Fluorescence Minus One (FMO) Controls: Contain all markers except the one of interest, essential for setting gates when multiple fluorophores are used together and when markers are expressed on a continuum [3].
- Viability Controls: Fluorescent probes that identify dead cells, which must be excluded from analysis because they nonspecifically bind antibodies and other probes [3].
- Compensation Controls: Single-stained samples used to calculate compensation matrices that correct for spectral overlap between fluorophores [3] [52].
Automated Gating Validation
For large-scale studies, automated gating approaches provide consistency and reproducibility superior to manual analysis. Supervised machine learning methods can be trained using manually gated datasets to create automated pipelines (automatons) that replicate manual analysis. Validation studies comparing automated gating with traditional manual analysis on 300 patients across multiple centers showed very good correlation for frequencies, absolute values, and MFIs [51]. The Human ImmunoPhenotyping Consortium (HIPC) similarly demonstrated that automated gating could match the performance of central manual analysis for standardized panels, exhibiting little to no bias and comparable variability [53].
Reagent and Lot Management
Lyophilized Reagent Systems
The use of lyophilized reagent cocktails in 96-well plates provides significant advantages for standardization by protecting against pipetting errors, providing improved reagent stability, and simplifying assay setup [53]. The HIPC consortium developed pre-configured, lyophilized eight-color panels specifically designed to standardize immunophenotyping across multiple sites [53].
Batch Effect Correction
Even with standardized reagents, lot-to-lot variation requires careful management. In a four-year study, three different lots of DuraClone antibody panels were used, necessitating the development of a Python script to correct data between batches for each instrument. This script also accounted for variations observed after the seven calibration procedures repeated during the study period [51].
Table 2: Research Reagent Solutions for Standardized Flow Cytometry
| Reagent Type | Specific Examples | Function | Standardization Benefit |
|---|---|---|---|
| Calibration Beads | VersaComp Capture Beads, 8-Peak Beads | Instrument harmonization and daily QC | Enables cross-instrument comparison and longitudinal tracking |
| Lyophilized Antibody Panels | BD Lyoplate, DuraClone | Pre-configured multicolor panels | Reduces pipetting errors and lot-to-lot variability |
| Viability Dyes | Fixable viability stains | Dead cell exclusion | Prevents nonspecific antibody binding |
| Compensation Beads | Single-stained compensation beads | Spillover correction | Ensures proper spectral compensation |
| Control Cells | CytoTrol frozen control cells | Process control | Monitors entire staining and acquisition process |
Performance Metrics and Validation Outcomes
Implementation of these standardized protocols yields quantifiable improvements in data quality. In the PRECISESADS study, analysis of the same control blood stained with DuraClone panel 1 after 4 years showed frequency variation coefficients between centers ranging from 2.3% for neutrophils to 17.7% for monocytes, and MFI variation coefficients ranging from 10.9% for CD3 to 30.9% for CD15 [51]. The HIPC consortium reported that centralized manual gating and automated gating both reduced cross-site variability compared to site-specific analysis, with automated methods matching the performance of central manual analysis for all tested panels [53].
Standardized protocols for instrument setup and performance tracking form the foundation of robust, reproducible high-throughput flow cytometry immunophenotyping. The integration of initial instrument harmonization, daily quality control, computational normalization, automated analysis, and careful reagent management creates a comprehensive system that minimizes technical variability while maximizing biological insight. As flow cytometry continues to evolve with increasing parameter numbers and application complexity, these standardization approaches will remain essential for generating reliable data that can be compared across studies, centers, and timeframes—ultimately accelerating discoveries in immunology and drug development.
High-dimensional flow cytometry is the gold standard for studying the human immune system in large cohorts, enabling deep immunophenotyping of diverse cell populations [15]. However, large sample sizes introduce significant non-biological data variation due to technical and experimental inaccuracies from batch variability, which critically impacts data precision and reproducibility [15] [1]. This application note details a robust pipeline for high-content, high-throughput immunophenotyping that successfully measured 3,357 samples across 19 experiments, revealing age- and genetics-dependent changes in blood leukocytes [15]. The methodology focuses on maximizing throughput while maintaining data precision through stringent standardization, quality controls, and automated analysis, providing a versatile framework for large-scale immune discovery in clinical and research settings.
Experimental Workflow and Design
The implemented workflow was systematically designed to address key challenges in high-throughput flow cytometry, including batch effects, technical variation, and analytical consistency. The pipeline integrates standardized sample preparation, high-dimensional staining, rigorous quality control, and automated computational analysis to ensure reproducible results across large sample batches.
Core Experimental Objectives and Design
This study established a high-throughput pipeline capable of processing 192 samples per experiment with high reproducibility for large-scale immunophenotyping studies [15]. The experimental design incorporated stringent quality controls at multiple checkpoints to minimize technical and experimental variation while enabling the measurement of age-associated immune dynamics in 2,300 individuals and identification of unique immune signatures related to genetic variations [15].
Table: Key Experimental Parameters and Outcomes
| Parameter | Specification | Application/Result |
|---|---|---|
| Total Samples Processed | 3,357 samples | Human blood leukocytes from 2,300 individuals |
| Experimental Runs | 19 experiments | Distributed sample processing |
| Throughput per Experiment | 192 samples/experiment | Optimized for large cohorts |
| Flow Cytometry Panel | 28-color spectral panel | Comprehensive immunophenotyping of T cells, B cells, NK cells |
| Key Findings | Age-associated decrease in T and B cell subsets; Immune signatures linked to CD45 splicing SNP | Revealed genetics-dependent immune changes |
Detailed Methodologies
Sample Preparation and Processing
Blood samples were collected into Acid Citrate Dextrose (ACD)-coated tubes and mixed by inversion before processing at room temperature [54]. Peripheral blood mononuclear cells (PBMCs) were isolated using Ficoll-Paque density gradient centrifugation with Leucosep tubes [54]. Specifically, 30 mL of blood was added to pre-filled Leucosep tubes and centrifuged for 15 minutes at 800×g at 21°C with no brake applied [54]. The buffy coat containing PBMCs was carefully transferred to a clean 50 mL tube using a sterile transfer pipette [54]. Cells were washed with phosphate buffered saline (PBS) and centrifuged for 5 minutes at 400×g at 21°C with brake applied [54]. Cell counting was performed via trypan blue exclusion using an automated cell counter, after which cells were resuspended in freezing media (90% heat-inactivated fetal calf serum and 10% dimethyl sulfoxide) at 5 × 10^6 cells/mL [54]. Cells were aliquoted into cryovials and frozen using a controlled-rate freezing apparatus before transfer to -80°C storage [54].
For thawing, wash medium (RPMI with 10% v/v HI-FCS) was pre-warmed to 37°C [54]. Cryovials were thawed until cool but not completely warm, and cells were transferred to a 15 mL tube where wash medium was added dropwise to a total volume of 10 mL [54]. Tubes were centrifuged for 5 minutes at 400×g at 21°C with brakes on, supernatant was decanted, and the cell pellet was resuspended in 1 mL of warm FACS wash (1X PBS with 2.5% v/v FCS and 0.1% sodium azide) [54].
Antibody Titration and Panel Validation
Comprehensive antibody titration was performed to determine optimal staining concentrations [54]. For each antibody, 2.5 × 10^5 cells were plated in a 96-well U-bottom plate [54]. Antibodies were diluted in FACS wash in a separate plate, creating a 1:12.5 dilution followed by serial 2-fold dilutions until reaching 1:200 [54]. Cells were centrifuged, supernatant was removed, and 25 µL of each antibody dilution was mixed with cells for 30 minutes on ice [54]. Ghost Dye v450 (diluted 1:4000 in PBS determined by prior titration) was added as a viability marker and incubated for 20 minutes at room temperature [54]. Cells were fixed using either the eBioscience Foxp3/Transcription Factor Staining Buffer Set or 1% paraformaldehyde in PBS for 20 minutes at room temperature [54].
High-Throughput Staining Protocol
For full-panel staining, 2 × 10^6 cells were plated into wells of a 96-well U-bottom plate [54]. Wells were topped up to 120 μL with FACS wash and centrifuged for 5 minutes at 400×g at 21°C [54]. The optimized 28-color panel included markers for T cell (CD3, CD4, CD8), B cell (CD19, CD20), and NK cell (CD16, CD56) identification, along with markers for activation (HLA-DR, CD38), proliferation (Ki-67), regulatory function (FOXP3), and exhaustion (PD-1) [15] [55]. Antibody cocktail was added to cell pellets and incubated for 30 minutes on ice, protected from light [54]. Cells were washed twice with FACS wash, then fixed with 1% paraformaldehyde [54]. For intracellular staining, cells were permeabilized using the eBioscience Foxp3/Transcription Factor Staining Buffer Set according to manufacturer instructions [54].
Instrumentation and Data Acquisition
Samples were acquired using spectral flow cytometers capable of detecting 28 parameters [15] [55]. The platform employed multiple lasers (V-B-R configuration) and sensitive detectors to capture the full fluorescence emission spectrum [56]. Daily quality control was performed using calibration beads to ensure consistent instrument performance [4]. PMT voltages were optimized using the "peak 2" method, where dim particles were run over a voltage series and the coefficient of variation (CV) was plotted against voltage to identify the inflection point where increasing voltage no longer decreases CV [4]. This ensured optimal signal detection with minimal electronic noise contribution. Instrument performance was tracked using Levey-Jennings plots with target values established during experimental optimization, enabling troubleshooting before sample collection when values fell outside ±2 standard deviations [4].
Data Analysis Pipeline
The data analysis approach combined automated preprocessing with advanced computational methods to handle the high-dimensional dataset while minimizing analytical bias. The pipeline transformed raw spectral data into biologically meaningful population statistics through sequential gating and clustering steps.
Data Preprocessing and Quality Control
Raw flow cytometry data files underwent automated preprocessing to mitigate technical variations [15]. Automated compensation was performed using single-color controls that met three critical criteria: (1) controls were at least as bright as experimental samples, (2) backgrounds of positive and negative samples were identical, and (3) controls exactly matched experimental fluorochromes and were acquired at the same voltages [4]. Fluorescence Minus One (FMO) controls were essential for determining positive populations, especially for rare events or dimly expressed markers [4]. Data display optimization included using contour plots for better population visualization and bi-exponential scaling to correctly display data values below zero and visualize compensation accuracy [57].
Gating Strategy and Population Identification
The initial gating strategy utilized forward scatter (FSC) versus side scatter (SSC) plots to identify viable lymphocytes and exclude debris [6]. Single cells were selected using FSC-A versus FSC-H parameters [6]. Live cells were identified using viability dyes such as Ghost Dye v450 [54]. Subsequent gating steps employed bivariate scatter plots to differentiate major lymphocyte populations: CD3+ for T cells, CD19+/CD20+ for B cells, and CD16+/CD56+ for NK cells [6]. Subpopulation analysis used multiparameter gating to identify T cell subsets (CD4+ helper, CD8+ cytotoxic, Tregs), B cell subsets (naive, memory), and functional subsets based on activation and exhaustion markers [15] [55].
High-Dimensional Data Analysis
Unsupervised clustering using FlowSOM algorithm enabled automated discovery of cell populations without prior gating biases [15]. This approach facilitated identification of novel rare cellular subsets and comprehensive mapping of immune phenotypes across the large cohort [15] [55]. Data were visualized through dimensionality reduction techniques and heatmaps to illustrate population frequencies and marker expression patterns [15]. Quantitative analysis included calculation of subset frequencies, absolute counts, and mean fluorescence intensities (MFI) for marker expression levels [1]. Statistical analysis revealed age-associated dynamics and genetic associations through linear modeling and hypothesis testing [15].
Essential Research Reagents and Materials
The successful implementation of this high-throughput pipeline relied on carefully selected and validated reagents that ensured consistency across the large study.
Table: Key Research Reagent Solutions
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Viability Stains | Ghost Dye v450 | Distinguishes live/dead cells; critical for data quality |
| Surface Stain Antibodies | CD45, CD3, CD4, CD8, CD19, CD20, CD16, CD56 | Identifies major lymphocyte populations and subsets |
| Intracellular/Functional Antibodies | FOXP3 (Tregs), Ki-67 (proliferation), HLA-DR/CD38 (activation) | Reveals functional and differentiation states |
| Fixation/Permeabilization Reagents | eBioscience Foxp3/Transcription Factor Staining Buffer Set, 1% PFA | Preserves cells and enables intracellular staining |
| Cell Processing Reagents | Ficoll-Paque, ACD tubes, RPMI, HI-FCS, DMSO | Supports sample collection, PBMC isolation, and cryopreservation |
| Quality Control Materials | Calibration beads, single-color controls, FMO controls | Ensures instrument performance and staining specificity |
Key Findings and Applications
The robust pipeline enabled significant biological discoveries and demonstrated practical applications for large-scale immunophenotyping studies.
Table: Key Findings from the Large-Scale Immunophenotyping Study
| Finding Category | Specific Results | Biological/Clinical Significance |
|---|---|---|
| Age-Associated Changes | Decreasing T and B cell subsets with advancing age | Documents immune aging patterns in large population |
| Genetic Associations | Unique immune signatures with CD45 isoform splicing SNP (PTPRC) | Links genetic variation to specific immune phenotypes |
| Technical Performance | Minimal non-biological variation across 19 experiments | Validates pipeline robustness for large studies |
| Clinical Applications | Identification of exhausted T cells, Th17 cells, memory γδ T cells | Reveals disease-relevant immune subsets in autoimmunity |
Technical Validation and Performance Metrics
The pipeline demonstrated exceptional technical performance, achieving minimal non-biological variation across all 3,357 samples processed in 19 independent experiments [15]. Quality control metrics showed high reproducibility, with standardized instrument calibration and staining protocols effectively mitigating batch effects [15]. The implementation of automated data preprocessing and unsupervised analysis facilitated rapid discovery while maintaining analytical consistency [15]. The 28-color panel provided comprehensive immunophenotyping capacity in a single-tube format, reducing sample consumption and processing time compared to conventional multi-tube approaches [55] [56].
Biological Insights and Clinical Relevance
Analysis of 2,300 individuals revealed significant age-dependent dynamics in immune cell composition, particularly declining T and B cell subsets with advancing age [15]. Integration of genetic analysis identified distinct immune signatures associated with a single nucleotide polymorphism that disrupts CD45 isoform splicing, demonstrating the pipeline's utility for mapping genotype-immunophenotype relationships [15]. In clinical applications, similar high-dimensional panels have identified disease-relevant immune alterations including exhausted T cells, Th17 cells, and rare memory γδ T cells in autoimmune conditions such as systemic lupus erythematosus and rheumatoid arthritis [55]. The platform has also been successfully deployed in clinical trials for blood cancers, enabling deep immune profiling for biomarker discovery and therapy monitoring [55].
Optimizing Assay Performance: Quality Control and Troubleshooting Strategies
Minimizing Batch Effects and Technical Variation
Batch effects and technical variation present significant challenges in high-throughput flow cytometry immunophenotyping of human blood, potentially compromising data quality and leading to erroneous biological conclusions. These non-biological variations arise from multiple sources including reagent lot differences, instrument performance fluctuations, operator technique variability, and sample processing inconsistencies [58]. In longitudinal studies spanning weeks, months, or years—common in clinical trials and large cohort immunophenotyping studies—these effects can confound biological signals and reduce statistical power [59] [58]. As flow cytometry panels increase in complexity to measure dozens of parameters simultaneously, implementing robust strategies to minimize technical variation becomes essential for generating reproducible, clinically meaningful data [15] [31].
Technical variation in flow cytometry manifests primarily through shifts in signal intensity and population frequencies that are unrelated to biological variables of interest. Common sources include:
- Reagent variability: Lot-to-lot differences in antibody-fluorochrome conjugates, particularly tandem dyes with unstable donor-acceptor ratios, can cause significant signal variation [58].
- Instrument performance: Laser power fluctuations, detector sensitivity changes, and instrument maintenance events such as laser replacement can alter signal detection [58].
- Operator technique: Differences in sample processing between technicians, including pipetting consistency, incubation timing, and washing efficiency, introduce methodological variation [58].
- Sample handling: Variations in sample storage conditions, anticoagulant use, and processing timelines affect cell integrity and marker expression [58].
- Acquisition parameters: Changes in instrument settings between runs or failure to allow sufficient instrument warm-up time can generate systematic biases [58].
Table 1: Common Sources of Batch Effects and Their Impact on Data Quality
| Source Category | Specific Examples | Primary Impact |
|---|---|---|
| Reagent Issues | Antibody lot variation, Tandem dye degradation, Buffer composition differences | Signal intensity shifts, Spillover spreading |
| Instrument Factors | Laser replacement, Detector sensitivity drift, Daily performance fluctuation | Marker expression levels, Population resolution |
| Sample Processing | Technician technique, Incubation time variability, Cell count normalization | Population frequencies, Background staining |
| Study Design | All samples from one group run together, Storage time differences | Confounded batch and biological effects |
Experimental Design Strategies for Batch Effect Minimization
Sample Randomization and Processing Controls
Effective batch effect control begins with strategic experimental design. Samples from different experimental groups should be randomly distributed across processing batches and acquisition sessions rather than processing all samples from one group together [58]. This approach ensures that technical variability is distributed evenly across biological conditions, preventing confounding of batch effects with experimental groups.
Implementation of technical controls is critical for monitoring and correcting batch effects. Including "bridge," "anchor," or "validation" samples in each batch provides a biologically constant reference for quantifying inter-batch variation [59] [58]. For human blood immunophenotyping studies, this typically involves aliquoting and cryopreserving peripheral blood mononuclear cells (PBMCs) from a single donor or pool of donors, then including one aliquot in each processing batch throughout the study duration.
Fluorescent Cell Barcoding
For high-throughput applications, fluorescent cell barcoding represents the most effective strategy for eliminating intra-batch variability. This technique involves labeling individual samples with unique combinations of fluorescent dyes before pooling, enabling simultaneous processing and acquisition of multiple samples under identical conditions [58]. The barcoding approach significantly reduces technical variability arising from staining inconsistencies and instrument performance fluctuations during acquisition.
Sample Size and Cell Number Normalization
Accurate antibody titration and cell count normalization are essential for consistent staining efficiency. Understaining or overstaining due to incorrect antibody-to-cell ratios can dramatically affect population resolution and marker expression measurements [58]. Implementing rigorous cell counting procedures and validating antibody concentrations for each specific cell type and staining condition ensures optimal signal-to-noise ratio across batches.
Quality Control and Monitoring Procedures
Instrument Quality Assurance
Regular instrument quality control using standardized particles or stable reference cells is fundamental for maintaining detection consistency across acquisition sessions. Modern cytometers, including spectral systems like the Cytek Aurora and Northern Lights platforms, incorporate built-in QC programs that monitor laser power, detector efficiency, and fluidic stability [58]. Establishing and tracking quality control metrics over time enables early detection of instrument performance drift that could introduce batch effects.
Table 2: Essential Quality Control Measures for Minimizing Technical Variation
| QC Category | Specific Procedure | Frequency | Acceptance Criteria |
|---|---|---|---|
| Instrument QC | Laser power validation, Detector voltage calibration, Fluidics pressure check | Daily | <2% CV in target channel for reference beads |
| Staining QC | Antibody titration verification, Cell count normalization, Viability assessment | Each experiment | >95% cell viability, Optimal signal-to-noise |
| Reference Samples | Anchor sample acquisition, Biological control processing | Each batch | <15% CV in population frequencies |
| Data Quality | Spectral unmixing verification, Doublet discrimination, Background assessment | Each sample | <5% doublets, <10% autofluorescence variation |
Anchor Sample Performance Tracking
Implementing Levy-Jennings charts for tracking anchor sample performance provides a powerful visual tool for monitoring batch effects over time [58]. Plotting key population frequencies or median fluorescence intensity values from anchor samples run in each batch enables rapid identification of systematic shifts exceeding expected technical variation. Statistical process control limits can be established to flag batches requiring investigation or exclusion.
Computational Approaches for Batch Effect Correction
Reference-Based Normalization
When anchor samples are included in each batch, reference-based normalization algorithms can effectively remove technical variation. These methods directly estimate batch effects by comparing anchor samples across batches and applying derived adjustment parameters to all samples within each batch [59]. Location and scale adjustment methods harmonize batches based on signal variance, mean, median, or user-defined percentiles, effectively aligning population distributions across batches.
The CytoNorm algorithm implements a normalization framework specifically designed for cytometry data, utilizing technical replicates or anchor samples to estimate and correct batch effects [60]. Recent implementations such as CytoNormPy provide Python-based tools with significantly improved computational efficiency, enabling rapid processing of large-scale cytometry datasets [60].
Unsupervised Batch Correction Methods
For studies where including anchor samples is not feasible, unsupervised computational methods can identify and correct batch effects. Algorithms such as Harmony and iMUBAC employ sophisticated statistical frameworks to disentangle technical artifacts from biological signals without requiring explicit controls [58]. These methods typically leverage characteristic patterns of batch effects across multiple samples to estimate correction parameters.
Implementation Protocols
Standardized Staining Protocol for Human Blood Immunophenotyping
The following protocol outlines a standardized approach for high-dimensional immunophenotyping of human whole blood, optimized to minimize technical variation:
Reagents and Materials
- Anticoagulated human whole blood (sodium heparin or EDTA)
- Pre-titrated antibody panels validated for specific cytometer configuration
- Phosphate-buffered saline (PBS)
- Fc receptor blocking solution
- Viability dye (cisplatin or fixable viability dyes)
- Red blood cell lysis buffer
- Fixation buffer (1-4% paraformaldehyde)
- Cryopreserved anchor sample PBMCs
Staining Procedure
- Sample Preparation: Aliquot 100-200μl whole blood into staining tubes. Include anchor sample in each processing batch.
- Viability Staining: Resuspend cells in cisplatin (50μM) or fixable viability dye and incubate for 5 minutes at room temperature.
- Fc Blocking: Add Fc receptor blocking antibody and incubate for 10 minutes at room temperature.
- Surface Staining: Add pre-mixed antibody cocktail and incubate for 30 minutes at room temperature protected from light.
- RBC Lysis: Add 2-3ml of lyzing solution, incubate for 10 minutes, then centrifuge at 500×g for 5 minutes.
- Wash and Fix: Resuspend cells in PBS, centrifuge, decant supernatant, and resuspend in fixation buffer.
- Acquisition: Store samples at 4°C protected from light and acquire within 24 hours on standardized cytometer.
Anchor Sample Implementation Protocol
Anchor Sample Preparation
- Obtain leukopak or large volume blood donation from single healthy donor.
- Isolate PBMCs using density gradient centrifugation.
- Aliquot PBMCs at optimal concentration (5-10×10^6 cells/vial) in cryopreservation medium.
- Freeze aliquots using controlled-rate freezing apparatus.
- Store in vapor phase liquid nitrogen until use.
Batch Quality Control
- For each processing batch, thaw one anchor sample aliquot alongside experimental samples.
- Process anchor sample using identical staining protocol as experimental samples.
- Acquire anchor sample using standardized instrument settings.
- Calculate key population frequencies and median fluorescence intensity values.
- Compare to established reference ranges using Levy-Jennings charts.
- Proceed with experimental sample acquisition only if anchor sample parameters fall within acceptable limits.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Batch Effect Minimization
| Reagent/Material | Function | Implementation Considerations |
|---|---|---|
| Cryopreserved PBMCs | Anchor sample biological material | Single donor leukopak aliquoted for entire study duration |
| Lytic Reagents | Red blood cell removal | Consistent lot usage throughout study |
| Viability Dyes | Discrimination of live/dead cells | Critical for accurate population frequency quantification |
| Fc Blocking Reagents | Reduce nonspecific antibody binding | Minimizes background staining variation |
| Standardized Antibody Panels | Cell population identification | Master mixes prepared in bulk and aliquoted for each batch |
| Compensation Beads | Fluorescence compensation controls | Required for multicolor panel optimization |
| QC Beads | Instrument performance tracking | Daily monitoring of laser and detector stability |
| Cell Barcoding Dyes | Sample multiplexing | Enables staining of multiple samples in single tube |
Minimizing batch effects and technical variation in high-throughput flow cytometry immunophenotyping requires integrated approach spanning experimental design, standardized operating procedures, robust quality control systems, and computational correction methods. Implementation of strategic controls including anchor samples, fluorescent barcoding, and instrument standardization enables generation of high-quality, reproducible data suitable for clinical and translational research applications. As cytometry technologies continue to evolve toward higher parameter configurations, maintaining vigilance against technical variation remains essential for extracting biologically meaningful insights from human blood immunophenotyping studies.
The reliability of high-throughput flow cytometry data in immunophenotyping studies is fundamentally dependent on a rigorous, multi-layered quality control (QC) framework. Technical and experimental variations introduced through reagents, instruments, and operator techniques can significantly compromise data integrity, particularly in large-cohort studies [15]. The implementation of standardized QC checkpoints from initial reagent selection through final data acquisition is therefore paramount. This is especially critical for high-throughput pipelines analyzing hundreds of samples per experiment, where minor, unaddressed variations can propagate into substantial batch effects, obscuring genuine biological signals [17] [15]. This application note details a comprehensive QC protocol, framed within the context of high-throughput immunophenotyping of human blood, to ensure the precision, accuracy, and reproducibility required for robust scientific discovery and drug development.
Essential Quality Control Checkpoints
Reagent Quality Control and Validation
The foundation of any reliable flow cytometry experiment is the use of highly validated reagents. Consistent reagent performance is critical for generating comparable data across long-term or large-scale studies.
- Antibody Titration and Validation: A core QC practice is the titration of all fluorescently conjugated antibodies to determine the optimal staining concentration that provides the best signal-to-noise ratio [17]. This involves staining cells with a series of antibody dilutions to identify the concentration that achieves maximal specific staining with minimal background. Furthermore, each antibody lot should be validated against the previous lot to ensure consistent performance, especially for multicolor panels.
- Specificity Reagents: The use of specificity reagents, including isotype controls and FMO (Fluorescence Minus One) controls, is essential for distinguishing specific antibody binding from non-specific background fluorescence and for accurately setting positive population gates [61].
- Preparation of Staining Panels: When building multicolor panels, careful consideration must be given to fluorochrome brightness, antigen density, and spectral overlap. Antibodies for low-abundance markers should be conjugated to bright fluorochromes, while those for highly expressed markers can be paired with dimmer fluorochromes. This optimization minimizes spillover and enhances the resolution of distinct cell populations [17].
Table 1: Key Reagent Quality Control Measures
| QC Checkpoint | Objective | Recommended Procedure | Acceptance Criteria |
|---|---|---|---|
| Antibody Titration | Determine optimal staining concentration | Stain cells with serial antibody dilutions; calculate Stain Index [17] | Concentration yielding peak Stain Index |
| Lot-to-Lot Validation | Ensure consistency between reagent batches | Parallel staining of reference samples with old and new lots | < 20% deviation in Median Fluorescence Intensity (MFI) |
| Specificity Controls (FMO) | Define gates and identify spreading error | Stain samples with all antibodies except one [61] | Accurate delineation of negative populations |
| Panel Stability | Assess reagent interaction over time | Stain reference sample at time zero and after panel storage | Consistent population distribution and MFI |
Instrument Performance Qualification and Standardization
A well-characterized and standardized instrument is non-negotiable for generating high-quality, reproducible flow cytometry data. The goal is to minimize instrument-derived variation.
- Daily QC and Performance Tracking: The use of standardized fluorescent beads for daily QC is a cornerstone of instrument monitoring. Key parameters like laser power, fluorescence sensitivity, and optical alignment are tracked over time. This allows for the detection of performance drift, such as a decline in laser power or PMT sensitivity, which could adversely affect experimental results [62] [17].
- Standardization and Calibration: To enable longitudinal study comparison and data pooling, instruments must be standardized. This involves calibrating detectors using beads with known fluorescence intensities to ensure that measurements (e.g., MFI) are consistent across different instruments and over time [63] [15]. Calibration and validation reagents are critical for this process, ensuring accuracy and reproducibility [61].
- Spectral Compensation: In multicolor flow cytometry, accurate compensation is vital to correct for spectral overlap between fluorochromes. This should be performed using single-stain controls for each fluorochrome in the panel, ideally stained on the same cells or beads used in the experiment. For spectral cytometers, regular validation and updating of the spectral library is the equivalent critical step [64].
Table 2: Key Instrument Performance QC Checkpoints
| QC Checkpoint | Measured Parameters | Frequency | Acceptance Criteria |
|---|---|---|---|
| Daily QC with Beads | Laser delay, PMT voltages, background noise | Each day of use | Values within pre-established control limits |
| Fluorescence Sensitivity | Detection threshold for dim signals | Weekly / Monthly | e.g., > 3000 MESF for FITC |
| Standardization (Cross-Instrument) | Median Fluorescence Intensity (MFI) | Before a study series | < 5% CV for key channels across instruments |
| Compensation | Spectral spillover correction | Per experiment | Residual compensation < 2% |
Diagram 1: Overall QC Workflow
Implementation in a High-Throughput Pipeline
For large-scale immunophenotyping studies, the standard QC practices must be integrated into an automated, high-throughput pipeline to maintain efficiency without sacrificing data quality.
- Minimizing Batch Effects: In a high-throughput pipeline processing 192 samples per experiment, stringent standardization of instrument setup, staining protocols, and sample handling is crucial to minimize technical variation [15]. This includes using precision liquid handlers for reagent dispensing and fixed time intervals for staining and acquisition.
- Integrated Quality Controls: The pipeline should incorporate internal QC checkpoints. This involves running a standardized control sample (e.g., frozen peripheral blood mononuclear cells or calibration beads) in every experiment to monitor and correct for inter-experimental variation [15]. Automated data pre-processing scripts can then flag samples that deviate from expected QC metrics.
- Unsupervised Analysis and Validation: Following data acquisition, the use of automated, unsupervised analysis algorithms, such as FlowSOM clustering, facilitates robust and reproducible cell population identification [15]. The resulting data should then be subjected to quality checks that quantify technical and experimental variation to ensure data precision before any biological interpretation [15].
The Scientist's Toolkit: Essential Research Reagents and Materials
A successful high-throughput immunophenotyping study relies on a suite of specialized reagents and materials. The selection below outlines the core components of the workflow.
Table 3: Essential Research Reagent Solutions for High-Throughput Immunophenotyping
| Item | Function / Application | Key Characteristics |
|---|---|---|
| Fluorochrome-conjugated Antibodies | Specific detection of cell surface and intracellular markers [64] | High specificity, validated for flow cytometry, optimal brightness for antigen density |
| Viability Dye | Exclusion of dead cells from analysis [64] [61] | Distinguishes live/dead cells, compatible with fixation, minimal spectral overlap |
| Standardized QC Beads | Daily instrument performance tracking and calibration [62] | Stable fluorescence, lot-to-lot consistency, covers multiple laser lines |
| Compensation Beads | Generation of single-stain controls for spectral compensation [64] | Bind antibodies uniformly, low background fluorescence |
| Lysing/Fixation Solutions | Red blood cell lysis and sample preservation post-staining [17] | Maintains light scatter and antigen integrity, compatible with downstream analysis |
| Laser Alignment Beads | Optimizing instrument fluidics and laser intercept | Distinct size and uniform fluorescence |
Detailed Experimental Protocols
Protocol: Antibody Titration for Optimal Staining
This protocol is adapted from methodologies used in deep immunophenotyping studies [17].
- Prepare Cells: Use a fresh or viably frozen reference sample of human peripheral blood mononuclear cells (PBMCs). Count and aliquot cells into 8 tubes (~1-2 x 10^5 cells/tube).
- Prepare Antibody Dilutions: Reconstitute the antibody according to the manufacturer's instructions. Prepare a series of two-fold dilutions (e.g., 1:50, 1:100, 1:200, 1:400, 1:800) in a suitable buffer. Include a negative control with no antibody.
- Stain Cells: Add each antibody dilution to a cell aliquot. Incubate in the dark for 20-30 minutes at 4°C.
- Wash and Resuspend: Wash cells twice with flow cytometry staining buffer. Resuspend in a fixed volume of buffer containing a viability dye.
- Acquire Data: Acquire data on a flow cytometer that has been performance-tested. Record the Median Fluorescence Intensity (MFI) of the positive and negative populations for each dilution.
- Calculate and Analyze: For each dilution, calculate the Stain Index: (MFIpositive - MFInegative) / (2 * SD_negative). The optimal staining concentration is the one that yields the highest Stain Index, indicating the best separation between positive and negative events.
Protocol: Daily Instrument Quality Control and Standardization
This procedure aligns with recommendations from CLSI guideline H62 and high-throughput methodologies [62] [15].
- Power Up and Sanitize: Power on the cytometer and fluidics system. Run a decontamination or sanitization solution through the fluidic path if the instrument was previously shut down.
- Run QC Beads: Vortex standardized fluorescent beads thoroughly and run the sample. Allow the signal to stabilize.
- Record Key Metrics: Document the following parameters in a QC log (electronic or physical):
- Time and Laser Power: For all lasers.
- Mean Fluorescence Intensity (MFI): For all fluorescence channels.
- Coefficient of Variation (CV): For the main fluorescence peak.
- Background/Noise: Signal in any fluorescence channel when no beads are present.
- Plot and Monitor: Plot the daily MFI and CV values on a Levey-Jennings control chart. Establish warning (mean ± 2SD) and control (mean ± 3SD) limits based on historical data. Any reading outside the control limits indicates the instrument requires maintenance or repair before experimental use.
- Perform Cleaning: After QC, run a cleaning solution or high-purity water through the system to prevent clogging and bacterial growth.
Diagram 2: Daily Instrument QC Process
The integration of comprehensive quality control checkpoints across the entire flow cytometry workflow—from reagent validation to instrument standardization—is a critical determinant of success in high-throughput immunophenotyping. The protocols and frameworks outlined here, derived from current standards and cutting-edge research, provide a robust foundation for generating precise, accurate, and reproducible data. Adherence to such a rigorous QC regimen mitigates technical noise, empowers the detection of subtle biological signals in large human cohorts, and ultimately bolsters the validity of scientific findings in immunology research and drug development.
High-throughput flow cytometry immunophenotyping of human blood represents a powerful tool for drug development and clinical research, enabling detailed characterization of immune cell populations at a single-cell level. However, the reliability of this data is highly dependent on rigorous sample and reagent preparation. Inaccurate results often stem from three common yet critical pitfalls: the presence of dead cells, the occurrence of cell doublets or multiplets, and suboptimal antibody concentrations. This application note provides detailed protocols and solutions to address these challenges, ensuring the generation of high-quality, reproducible data in large-scale immunophenotyping studies.
The Critical Role of Viability Staining
Why Viability Matters
The presence of non-viable cells in a flow cytometry specimen is a serious issue, as these cells can bind antibodies non-specifically or exhibit unusual autofluorescence, potentially leading to the spurious identification of abnormal cell populations [65]. This is particularly critical in quantitative assays, such as those measuring T-cell subsets or CD34+ stem cells, where non-viable cells can cause significant inaccuracy [65]. The need for viability staining is specimen-dependent; while fresh blood specimens typically have excellent viability, it decreases as the specimen ages. Viability is also commonly compromised in tissues, body fluids, and high-grade neoplasms with high turnover rates [65].
Choosing and Using Viability Dyes
Selecting the appropriate viability dye depends on the experimental workflow, particularly whether intracellular staining or cell fixation is required.
- DNA-binding Dyes (Propidium Iodide, 7-AAD): These dyes are impermeant to live cells but freely enter dead cells with compromised membranes and intercalate with DNA [66] [14]. A key limitation is their incompatibility with intracellular staining protocols, as fixation permeabilizes all cells, allowing the dye to enter indiscriminately [66]. When using these dyes, they must remain in the buffer during acquisition and not be washed out [66].
- Fixable Viability Dyes (FVDs): These dyes are amine-reactive and covalently cross-link to cellular proteins, irreversibly labeling dead cells [66]. This allows samples to undergo cryopreservation, fixation, and permeabilization procedures without loss of dead cell staining, making them essential for intracellular staining protocols [66] [14]. For optimal results, it is recommended to stain with FVDs in an azide- and protein-free PBS buffer [66].
Table 1: Comparison of Common Viability Dyes for Flow Cytometry
| Dye Type | Examples | Mechanism | Compatible with Fixation/Permeabilization? | Key Considerations |
|---|---|---|---|---|
| DNA-binding Dyes | Propidium Iodide (PI), 7-AAD, DAPI [66] [14] | Intercalates into DNA of membrane-compromised cells [66] [14] | No [66] | Must not be washed out after staining; analyze samples within 4 hours [66]. |
| Fixable Viability Dyes (FVD) | eFluor 506, eFluor 780, and other dye-conjugated polymers [66] | Covalently bonds to cellular amines in dead cells [66] | Yes [66] | Staining is stable through fixation/permeabilization; requires titration for optimal concentration [66]. |
| Live Cell Enzymatic Dyes | Calcein AM, Calcein Violet AM [66] | Enzymatically converted to a fluorescent compound retained in live cells [66] | No [66] | Labels live cells; not retained in cells with compromised membranes [66]. |
Robust Doublet Discrimination for Authentic Single-Cell Data
The Doublet Problem
In flow cytometry, a "doublet" is an event where two or more cells pass through the detector simultaneously, being measured as a single, aberrant cell [67]. This can lead to incorrect identification of rare cell populations and misinterpretation of data. Traditional methods for identifying doublets often rely on gating on two-dimensional plots using light scatter properties (FSC-H vs FSC-A) or DNA content [67]. However, these methods can be imprecise; for instance, bivariate gating can mistake single cells with high DNA content, such as eosinophils, for doublets [67].
An Advanced Computational Solution
A more robust, automated alternative is the Cleanet method, which identifies doublets based on protein expression patterns rather than light scatter alone [67]. This approach is inspired by methods used in single-cell transcriptomics and involves two key steps:
- Doublet Simulation: Synthetic doublet events are computationally generated from the existing single-cell data.
- Similarity Identification: The algorithm then identifies real events whose protein expression profiles are similar to the simulated doublets [67].
This method is effective for detecting both homotypic (two cells of the same type) and heterotypic (two cells of different types) doublets. Furthermore, Cleanet can classify doublets based on their component cell types, potentially providing extra information about cell-cell interactions that would otherwise be discarded [67].
Optimizing Antibody Titration for Precision and Cost-Effectiveness
The Necessity of Titration
Antibody titration is a critical but often overlooked step in panel design. Using antibody concentrations straight from the manufacturer's datasheet can lead to suboptimal results, as the recommended volume is often excessive to ensure it works under a wide range of conditions. Over-staining increases non-specific binding and background noise, while under-staining reduces the signal from positive cells [68]. Proper titration identifies the concentration that provides the best separation between positive and negative populations, maximizing resolution and minimizing reagent costs.
Titration Protocols and Calculation
The fundamental principle of titration is to test a range of antibody dilutions on a sample containing both positive and negative cell populations. The procedure below outlines a standard serial dilution approach suitable for directly conjugated antibodies.
Serial Dilution Titration Protocol (adapted from [69] [70]):
- Harvest Cells: Prepare a single-cell suspension of your target cells (e.g., PBMCs) in staining buffer at a concentration of 1x10^6 cells per 100 µL. Using the specific cell type of interest (e.g., lung cells instead of spleen) is critical for accurate results [69].
- Block Fc Receptors: Add an Fc blocking reagent (e.g., human IgG or specific FcR blocking buffer) to prevent non-specific antibody binding. Incubate for 10 minutes at room temperature [69].
- Prepare Serial Dilutions: Create a series of antibody dilutions. A common method is to perform serial 2-fold dilutions. For example, prepare an intermediate dilution of the antibody and then serially dilute it across several tubes to achieve concentrations of 1:100, 1:200, 1:400, 1:800, etc. [69] [68].
- Stain Cells: Aliquot cells into staining tubes. Add the different antibody dilutions to each tube, including an unstained control. Incubate in the dark for 20-30 minutes at room temperature [69] [70].
- Wash and Resuspend: Wash cells twice with cold flow cytometry staining buffer, centrifuge, and resuspend in a fixed volume of buffer for acquisition [70].
- Acquire and Analyze: Run the samples on a flow cytometer. For each dilution, record the Mean Fluorescence Intensity (MFI) of both the positive and negative cell populations.
Determining the Optimal Titer
The optimal antibody concentration is not simply the one with the highest MFI on positive cells, but the one that provides the best distinction from the negative population. This is quantified using the Staining Index (SI) [69] [68].
Staining Index (SI) = (MFI of Positive Population - MFI of Negative Population) / (2 x standard deviation of Negative Population) [69]
The dilution that yields the highest Staining Index should be selected for future experiments [69]. This approach ensures optimal signal-to-noise ratio.
Table 2: Antibody Titration Methods for High-Parameter Panels
| Method | Principle | Advantage | Best For |
|---|---|---|---|
| Signal-to-Noise Ratio (SNR) [68] | Ratio of MFI between positive and negative groups. | Simple calculation. | Initial, quick assessment of a single antibody. |
| Staining Index (SI) [69] [68] | (MFI Pos - MFI Neg) / (2 x rSD Neg); selects for peak separation. | Optimizes resolution between positive and negative populations; recommended best practice [69]. | Standard panel optimization for any cell type. |
| Serial Titration [68] | Titrates one antibody at a time after setting lineage markers. | Methodical; reduces complexity. | Panels with complex cell types or many dead cells. |
| Combinatorial Titration [68] | Titrates multiple antibodies simultaneously in a single tube. | Saves significant time and reagent costs. | Establishing high-parameter panels (e.g., >15 colors). |
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Reagents for High-Quality Immunophenotyping
| Reagent / Material | Function | Example Products / Notes |
|---|---|---|
| Fixable Viability Dye (FVD) [66] | Labels dead cells for exclusion; compatible with fixation/permeabilization. | eFluor 506, eFluor 780; must be titrated and stored at ≤ -70°C [66]. |
| Fc Receptor Blocking Reagent [69] [14] | Blocks non-specific antibody binding to Fc receptors on immune cells. | Human IgG, mouse anti-CD16/CD32; essential for reducing background [69] [14]. |
| Flow Cytometry Staining Buffer [66] [14] | Buffer for washing and resuspending cells; typically contains protein (e.g., BSA) to enhance cell health and reduce sticking. | PBS with 0.5-2% BSA or FCS; some protocols require azide-/protein-free buffer for FVD staining [66] [14]. |
| Cell Barcoding Reagents [71] | Allows pooling of multiple samples into one tube, reducing staining variability and acquisition time. | Palladium-based barcoding kits for mass cytometry; can also be applied to flow cytometry. |
| Antibody Stabilizer [71] | Buffer for storing conjugated antibodies to maintain stability and activity over time. | Typically contains protein and sodium azide; used for long-term storage at 4°C [71]. |
Meticulous attention to viability staining, doublet discrimination, and antibody titration is non-negotiable for generating robust and reliable data in high-throughput flow cytometry. By integrating the standardized protocols and quality control measures outlined here—employing fixable viability dyes for complex staining panels, adopting advanced tools like Cleanet for doublet detection, and using the Staining Index to determine optimal antibody concentrations—researchers can significantly enhance the accuracy and reproducibility of their immunophenotyping studies. This rigorous approach is fundamental for advancing drug development and achieving a precise understanding of the human immune response.
In the realm of high-throughput flow cytometry immunophenotyping for human blood research, the strategic pairing of fluorochrome brightness with cellular marker expression levels is a fundamental determinant of experimental success. Multicolor flow cytometry enables the simultaneous analysis of multiple parameters at the single-cell level, but this powerful capability introduces complexity in panel design [72]. As drug development professionals and researchers strive to interrogate increasingly complex immune cell populations from limited clinical samples, optimal fluorochrome-antigen matching becomes critical for maximizing data quality and ensuring reliable detection of rare cell populations. The core principle is straightforward: bright fluorochromes should be paired with low-density antigens, while dim fluorochromes are best suited for highly expressed targets [72] [45] [73]. This application note provides detailed protocols and frameworks to systematically implement this principle within high-throughput immunophenotyping workflows, ensuring sensitive, reproducible results for drug discovery and translational research applications.
Theoretical Framework: Fluorochrome Brightness and Antigen Density
Categorizing Fluorochrome Brightness
Fluorochromes vary significantly in their photon output upon laser excitation, leading to natural classification into brightness categories. This inherent brightness, combined with instrument configuration and detector efficiency, determines the practical signal intensity observed during data acquisition.
Table 1: Relative Brightness of Common Flow Cytometry Fluorochromes
| Brightness Category | Example Fluorochromes | Relative Brightness | Recommended Application |
|---|---|---|---|
| Bright | PE, APC, Brilliant Violet 421 | High | Low-density antigens (Tertiary markers, cytokines, checkpoints) |
| Medium | PE-Cy7, APC-Cy7, PerCP-Cy5.5 | Medium | Moderately expressed antigens |
| Dim | FITC, Alexa Fluor 488, Pacific Blue | Low | High-density antigens (Lineage markers, CD4, CD8) |
Classifying Antigen Expression Levels
Cellular markers exhibit distinct expression patterns across different cell types, which can be systematically categorized to guide fluorochrome assignment [72] [74]:
- Primary Antigens: Expressed at high density and often used to define major cell lineages (e.g., CD3, CD19, CD14). These robust markers can be effectively detected with dimmer fluorochromes [72].
- Secondary Antigens: Often expressed over a continuum or at intermediate levels (e.g., CD27, CD28, activation markers). These require medium-brightness fluorochromes for clear resolution.
- Tertiary Antigens: Critical markers expressed at low density, such as cytokines (IFN-γ, IL-2), transcription factors, or low-abundance surface receptors (e.g., CD127, chemokine receptors) [72] [74]. These demand the brightest available fluorochromes to achieve detectable signal above background autofluorescence.
The following workflow diagram illustrates the logical decision process for optimal fluorochrome assignment:
Experimental Protocols
Protocol: Systematic Panel Design for High-Throughput Immunophenotyping
Objective: To design an optimized multicolor flow cytometry panel for high-throughput immunophenotyping of human peripheral blood mononuclear cells (PBMCs), ensuring sensitive detection of all cellular subsets through strategic fluorochrome-antigen pairing.
Materials:
- Human PBMC samples (fresh or viably frozen)
- Flow cytometry staining buffer (PBS containing 1-2% FBS and 2mM EDTA) [73]
- Antibody cocktails (pre-titrated)
- Viability dye (e.g., amine-reactive viability marker) [74]
- Fixation solution (if intracellular staining required)
- 96-well or 384-well U-bottom plates
- High-throughput flow cytometer (e.g., configured with blue, red, and violet lasers)
Procedure:
Define Experimental Hypothesis and Marker Selection [72]
- Identify the specific biological question and target cell populations.
- Compile a "wish list" of markers required to identify populations of interest, categorizing each as primary, secondary, or tertiary based on expected expression levels.
- Rank markers by biological importance to guide potential compromises during optimization.
Instrument Configuration Assessment [72] [45]
- Document all available lasers (wavelengths) and corresponding optical filters on your flow cytometer.
- Verify laser alignment and detector performance using calibration beads before beginning panel design.
Fluorochrome Assignment Strategy [72] [45] [73]
- Refer to Table 1 for fluorochrome brightness classification.
- Assign brightest fluorochromes (PE, APC) to lowest-expression markers (tertiary antigens).
- Assign medium-brightness fluorochromes (PE-Cy7, APC-Cy7) to moderately expressed markers.
- Assign dimmest fluorochromes (FITC, Alexa Fluor 488) to highest-expression markers.
- Use a spectral viewer to visualize potential spillover and confirm minimal overlap between assigned fluorochromes.
Staining Procedure for Surface Antigens
- Prepare single-cell suspension of human PBMCs, ensuring complete dissociation and viability >95% [73].
- Transfer 1-2 × 10^6 cells per well into 96-well U-bottom plate.
- Add Fc receptor blocking reagent (optional but recommended for human blood samples).
- Add viability dye diluted in PBS, incubate 10-15 minutes at room temperature, protected from light.
- Wash cells with 200μL flow cytometry staining buffer, centrifuge at 400 × g for 5 minutes, aspirate supernatant.
- Resuspend cell pellet in antibody cocktail (typically 50-100μL total volume) containing all surface antibodies.
- Incubate for 30 minutes at 4°C, protected from light.
- Wash twice with 200μL staining buffer, centrifuge, and aspirate supernatant.
Intracellular Staining (if required)
- After surface staining, fix cells using appropriate fixation buffer (e.g., 2-4% paraformaldehyde), incubate 20 minutes at room temperature.
- Permeabilize cells using permeabilization buffer (e.g., saponin-based or methanol-based).
- Centrifuge and aspirate supernatant.
- Add intracellular antibody cocktail in permeabilization buffer.
- Incubate 30-60 minutes at 4°C, protected from light.
- Wash twice with permeabilization buffer, then once with staining buffer.
- Resuspend in 200μL staining buffer for acquisition.
Data Acquisition and Quality Control
- Acquire data on flow cytometer within 24 hours of staining (preferably immediately).
- Include appropriate controls: unstained cells, single-color compensation controls, and fluorescence-minus-one (FMO) controls for each parameter.
- For high-throughput systems, implement sample barcoding and automated acquisition protocols.
Protocol: Titration of Conjugated Antibodies
Objective: To determine the optimal working concentration for each antibody-fluorochrome conjugate in the panel, maximizing signal-to-noise ratio while minimizing nonspecific binding and waste of valuable reagents.
Procedure:
- Prepare a single-cell suspension of human PBMCs.
- Aliquot equal cell numbers (e.g., 0.5-1 × 10^6) into multiple tubes.
- Prepare serial dilutions of each antibody (e.g., 0.125×, 0.25×, 0.5×, 1×, 2× manufacturer's recommended concentration).
- Stain cells with each antibody dilution following the standard staining protocol.
- Acquire data and analyze the median fluorescence intensity (MFI) of positive and negative populations.
- Plot MFI versus antibody concentration for each reagent.
- Select the concentration that provides the best separation between positive and negative populations (typically at the plateau phase of the binding curve).
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for High-Throughput Immunophenotyping
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Viability Markers | Amine-reactive dyes (ViViD, Zombie dyes), DNA intercalators (7-AAD, DAPI) | Distinguish live/dead cells; critical for excluding false-positive events from dead cells [74]. |
| Bright Fluorochromes | PE, APC, Brilliant Violet 421 | Highest photon output; ideal for low-density antigens (cytokines, chemokine receptors) [72] [45]. |
| Tandem Dyes | PE-Cy7, APC-Cy7, Brilliant Violet 785 | Provide additional laser options; note potential instability issues with some tandems - protect from light [45]. |
| Common Dim Fluorochromes | FITC, Alexa Fluor 488, Pacific Blue | Lower photon output; suitable for highly expressed lineage markers (CD3, CD4, CD8) [72] [45]. |
| Fc Receptor Blocking Reagents | Human Fc Block, IgG from same species | Reduce nonspecific antibody binding; essential for human blood samples with abundant Fc receptor-expressing cells. |
| Cell Preparation Reagents | EDTA, DNase, Ca2+/Mg2+-free buffer | Maintain single-cell suspensions; prevent cell aggregation during high-throughput processing [73]. |
Troubleshooting and Optimization
Addressing Common Challenges
Poor Resolution of Dim Markers: Verify bright fluorochrome assignment to low-density antigens. Check instrument sensitivity using calibration beads. Increase antibody concentration (after titration) or cell number. Review fixation/permeabilization impact if staining intracellularly [72] [74].
Excessive Spillover Spread: Re-evaluate fluorochrome combinations using spectral viewer. Consider alternative fluorochromes with less spectral overlap. Verify compensation matrix using single-stained controls. Ensure proper voltage settings on cytometer [72].
High Background/Non-specific Staining: Include Fc receptor blocking step. Titrate all antibodies to determine optimal concentration. Use viability marker to exclude dead cells. Include FMO controls to set appropriate gates [73] [74].
Inconsistent Results Between Experiments: Standardize sample processing protocols. Use consistent antibody lots where possible. Monitor instrument performance daily with quality control beads. Implement systematic panel template documentation.
Validation and Quality Control Measures
- Fluorescence-Minus-One (FMO) Controls: Essential for setting gates in multicolor panels, especially for dim populations and closely spaced markers [73] [74].
- Compensation Controls: Required for each fluorochrome using single-stained samples or compensation beads [73].
- Biological Controls: Include reference samples with known expression patterns to monitor assay performance over time.
- Instrument QC: Regular performance tracking using calibration beads ensures consistent sensitivity and detection across experiments.
Strategic pairing of fluorochrome brightness with antigen expression level represents a cornerstone principle in flow cytometry panel design, particularly for high-throughput immunophenotyping applications in human blood research. By systematically implementing the protocols and frameworks outlined in this application note, researchers and drug development professionals can significantly enhance the quality, reproducibility, and biological relevance of their data. The iterative process of panel optimization—incorporating appropriate controls, rigorous validation, and careful troubleshooting—ensures sensitive detection of all cellular subsets, ultimately supporting robust conclusions in basic research and therapeutic development. As flow cytometry continues to evolve toward higher parameter configurations, these fundamental principles of fluorochrome-antigen pairing will remain essential for maximizing the information content derived from precious clinical samples.
Implementing FMO Controls and Viability Staining for Data Accuracy
In high-throughput flow cytometry immunophenotyping of human blood, data accuracy is paramount for generating biologically and clinically relevant findings. Two fundamental pillars supporting this accuracy are the proper implementation of fluorescence minus one (FMO) controls and viability staining. These controls are not merely optional; they are essential for validating gating strategies and ensuring that observed phenotypes reflect true biology rather than experimental artifacts [75]. In the context of complex multicolor panels, such as the 30-color spectral panel described by Davies et al., rigorous controls become even more critical to minimize data variability arising from non-biological factors and to ensure the panel accurately captures biological variation [54]. This application note provides detailed protocols and frameworks for integrating these controls to fortify the integrity of immunophenotyping data.
The Critical Role of Controls in Immunophenotyping
The Consequences of Poor Viability Assessment
Dead cells are a significant source of inaccuracy in flow cytometry. They exhibit increased autofluorescence and bind antibodies non-specifically, leading to false-positive results and misinterpretation of data [75]. In high-throughput research, where samples may be processed in large batches, excluding dead cells is crucial for achieving a clean analysis of rare populations and for ensuring accurate sorting outcomes.
The Necessity of FMO Controls in Multicolor Panels
In multicolor flow cytometry, spectral overlap (or spillover) between fluorophores is inevitable. While electronic compensation corrects for this overlap, it cannot address the spreading error that broadens the negative population in a given channel. FMO controls are the gold standard for correctly setting gates to distinguish dimly positive from negative populations, as they account for the background fluorescence spread from all other fluorophores in the panel [75]. Using an unstained control or an isotype control for this purpose often leads to over-gating and an inaccurate assessment of population frequencies.
Experimental Protocols
Protocol for Cell Preparation and Viability Staining
Summary: This protocol outlines the procedure for preparing a single-cell suspension from human peripheral blood mononuclear cells (PBMCs) and staining with a viability dye to discriminate live from dead cells.
Reagents:
- FACS wash (1X PBS with 2.5% v/v FCS and 0.1% sodium azide) [54]
- Ghost Dye v450 (or equivalent viability dye such as 7-AAD, propidium iodide) [75] [54]
- Fixative (e.g., 1% paraformaldehyde (PFA) in PBS or commercial fixation buffer) [54]
Procedure:
- Cell Thawing and Washing: Thaw frozen PBMCs rapidly and transfer them to a 15 mL tube. Add pre-warmed wash medium (RPMI with 10% HI-FCS) dropwise to a total volume of 10 mL. Centrifuge for 5 minutes at 400g at 21°C [54].
- Cell Counting: Decant the supernatant, resuspend the cell pellet in 1 mL of FACS wash, and count the cells using an automated cell counter or hemocytometer [54].
- Resuspension: Centrifuge again and resuspend the cell pellet to a concentration of 1 x 10^7 cells/mL in FACS wash [54].
- Viability Staining: Aliquot the required number of cells (e.g., 2.5 x 10^5 for a control) into a U-bottom 96-well plate. Centrifuge the plate for 5 minutes at 400g to pellet cells and flick off the supernatant.
- Note: For cell-impermeant dyes like 7-AAD or propidium iodide, staining is typically performed on unfixed cells just before acquisition. Follow manufacturer instructions.
- Stain with Viability Dye: Resuspend the cell pellet in 100 µL of PBS containing a pre-titrated dilution of viability dye (e.g., Ghost Dye v450 at 1:4000 dilution). Incubate for 20 minutes at room temperature, protected from light [54].
- Washing and Fixation: Add 150 µL of FACS wash to the well and centrifuge. Flick off the supernatant. Resuspend cells in 200 µL of FACS wash or fix with 1% PFA for 20 minutes at RT if not acquiring immediately. Fixed samples should be acquired within a reasonable timeframe to preserve signal [54].
- Acquisition: Resuspend the final cell pellet in an appropriate volume of FACS wash (e.g., 200-300 µL) for analysis on the flow cytometer. Ensure the final cell concentration is between 1-10 million cells per mL [76].
Protocol for FMO Control Preparation
Summary: This protocol describes the creation of an FMO control for a specific channel (e.g., PE) within a multicolor panel.
Reagents:
- Master mix of all fluorophore-conjugated antibodies for the full panel except the one being controlled (e.g., all antibodies minus the PE-conjugated antibody).
- FACS wash.
Procedure:
- Panel Design: During multicolor panel design, identify all markers requiring FMO controls. These are typically markers with dim expression or where the positive and negative populations are difficult to resolve.
- Stain Experimental Sample: Stain the experimental sample with the complete antibody panel, following standard staining procedures (e.g., 30 minutes on ice, followed by washes).
- Stain FMO Control: In a separate tube, stain the same number of cells from the same source with the "minus one" antibody master mix. The volume and staining conditions must be identical to the full panel sample [75].
- Viability Staining and Fixation: Include the same viability dye used in the experimental samples in the FMO control tube. After antibody staining, wash, and fix the cells using the same method as the full stain sample [75] [76].
- Acquisition: Acquire the FMO control sample on the flow cytometer using the same instrument settings as the experimental samples.
Data Presentation and Analysis
Common Viability Dyes and Their Properties
Table 1: Characteristics of common viability dyes for flow cytometry.
| Dye Name | Excitation Laser (nm) | Emission Peak (nm) | Cell Permeability | Compatible with Fixation? | Primary Use |
|---|---|---|---|---|---|
| Propidium Iodide (PI) | 488, 532 | ~617 | Impermeant | No (fixation permeabilizes cells) | DNA content; dead cell discrimination on unfixed cells [75] |
| 7-AAD | 488, 532 | ~647 | Impermeant | No | DNA content; dead cell discrimination on unfixed cells [75] |
| DRAQ7 | 488, 633 | ~697 | Impermeant | No | DNA content; dead cell discrimination on unfixed cells [75] |
| Ghost Dye v450 | 405 | ~450 | Impermeant | Yes (post-stain) | Viability staining, compatible with subsequent fixation [54] |
| Calcein AM | 488 | ~517 | Permeant (converted intracellularly) | Yes (post-stain) | Viability staining; marks live cells via esterase activity [75] |
Gating Strategy Guided by FMO Controls
The following workflow diagram illustrates the sequential gating strategy for immunophenotyping, highlighting the critical points where viability staining and FMO controls are applied to ensure data accuracy.
Implementation in High-Throughput Research
Essential Research Reagent Solutions
Table 2: Key reagents and materials required for implementing FMO controls and viability staining.
| Item | Function/Description | Example/Citation |
|---|---|---|
| Viability Dyes | Distinguish live from dead cells to reduce non-specific binding and autofluorescence. | Ghost Dye v450, 7-AAD, Propidium Iodide, DRAQ7 [75] [54] |
| Fc Receptor Blocking Reagent | Reduces non-specific antibody binding via Fc receptors on phagocytic cells. | Specific blocking reagents used prior to staining [75] |
| Compensation Beads | Used to create single-stained controls for accurate calculation of compensation matrices. | Synthetic beads that bind conjugated antibodies [75] |
| Cell Strainers | Ensure a single-cell suspension, preventing clogs and data artifacts. | 35 µm filter cap FACS tubes [76] |
| Validated Antibody Panels | Antibodies specifically validated for flow cytometry to ensure specificity and lack of cross-reactivity. | Critical for reproducible, robust data [75] |
| FACS Buffer | Buffer for washing and resuspending cells. Typically Ca/Mg-free PBS with protein. | PBS with 0.5% BSA or 1-2% FBS [76] |
Integrating Controls into a Spectral Cytometry Workflow
The rise of high-parameter spectral cytometry, as demonstrated by the 30-color panel developed for immunophenotyping, intensifies the need for rigorous controls. The increased number of fluorophores elevates the potential for data variability from non-biological factors. In this context, viability staining and FMO controls are non-negotiable for producing high-resolution data with minimal error, enabling reliable cross-batch and cross-study comparisons [54]. The following diagram outlines the integrated experimental workflow from sample preparation to data analysis, showing where controls are incorporated.
Ensuring Data Reproducibility: Standardization and Analytical Validation
Standardized Operating Procedures for Cross-Study Comparisons
The expansion of high-throughput flow cytometry (HTFC) has revolutionized immunophenotyping in clinical research and drug discovery, enabling the detailed characterization of complex cellular subsets in human blood [46]. However, the comparability of data across different studies, instruments, and centers remains a significant challenge, potentially compromising the validation of biomarkers and therapeutic targets [51]. Variations in sample preparation, instrument configuration, and data analysis can introduce substantial technical noise, obscuring true biological signals.
The implementation of Standardized Operating Procedures (SOPs) is therefore critical for ensuring data reproducibility and harmonization in multicenter studies. This application note details established, practical protocols for cross-study standardization, framed within the context of a broader thesis on high-throughput flow cytometry immunophenotyping of human blood. The procedures outlined herein are designed to provide researchers, scientists, and drug development professionals with a robust framework for generating reliable, comparable data, thereby enhancing the scientific rigor of immunophenotyping studies.
Key Challenges in Multi-Center Flow Cytometry
Before detailing the protocols, it is essential to understand the primary sources of variability that SOPs must address:
- Instrument-Based Variance: Different flow cytometers, even of the same model from the same manufacturer, can yield divergent results due to variations in laser power, optical alignment, and detector sensitivity [51].
- Sample Preparation Artifacts: The use of erythrolytic solutions, density gradients, and multiple washing steps can significantly alter cell integrity and antigen expression, leading to inconsistent results [77].
- Reagent and Panel Design Flaws: Incompatible fluorophore combinations or suboptimal antibody titrations can cause excessive spectral spillover, compromising data quality and resolution [78] [79].
- Analysis Inconsistencies: Subjective "manual" gating strategies are a major source of variation, especially when data analysis is performed by multiple operators across different centers [51].
Standardized Protocols for Data Harmonization
Standardized Sample Preparation from Whole Blood
Minimizing pre-analytical variables is the first critical step. The following no-wash, no-lyse protocol for human whole blood helps preserve native cell states and functions [77] [30].
Materials & Reagents:
- Anticoagulated Whole Blood: Collected in heparin or K₂EDTA/K₃EDTA tubes [30].
- Monoclonal Antibodies: Fluorophore-conjugated, titrated for optimal signal-to-noise ratio.
- Staining Buffer: e.g., Invitrogen eBioscience Flow Cytometry Staining Buffer.
- Viability Dye: e.g., SYTOX Dead Cell Stain or 7-AAD, to exclude non-viable cells.
- DNA Stain for Nucleated Cells: e.g., Vybrant DyeCycle Violet, to discriminate nucleated cells from erythrocytes in unlysed blood [77].
Procedure:
- Blood Collection and Aliquoting: Collect fresh peripheral blood into anti-coagulant tubes. Within 2 hours of collection, aliquot 100 µL of unlysed whole blood into a 12 x 75 mm tube for each staining condition [30] [79].
- Antibody Staining: Add a pre-mixed antibody cocktail directly to the 100 µL blood aliquot. Incubate for 30 minutes at 2–8°C, protected from light.
- Erythrocyte Exclusion (Optional): Do not perform a lysing step. Instead, add a cell-permeant DNA stain (e.g., Vybrant DyeCycle Violet) to the stained, unlysed sample. This stain will label only nucleated cells (leukocytes), allowing erythrocytes to be gated out during analysis based on the lack of DNA signal [77].
- Sample Acquisition: Dilute the sample sufficiently in buffer to reduce coincidence of red blood cells and acquire directly on the flow cytometer without washing [77].
Instrument Setup and Cross-Center Harmonization
A rigorous and continuous standardization procedure is mandatory for reconciling data from different instruments.
Materials & Reagents:
- Calibration Beads: e.g., BD Cytometer Setup and Tracking (CS&T) Beads or VersaComp Capture Beads [51] [79].
- Standardization Beads: e.g., 8-peak beads (Beckman Coulter) for daily quality control [51].
Procedure:
- Initial Instrument Harmonization: Using identical calibration beads, adjust the photomultiplier tube (PMT) voltages on all cytometers involved in a study to achieve matching target Mean Fluorescence Intensities (MFIs) for all fluorescence channels. This establishes a baseline for inter-instrument comparability [51].
- Daily Quality Control (QC): Prior to sample acquisition, run 8-peak beads to monitor instrument performance. Record the MFIs for each peak to track laser stability and detector sensitivity over time [51].
- Intra-Center Normalization via Computational Scripting: Develop and apply an R script to normalize daily QC data. The script should perform a linear regression that adjusts the day's MFI readings back to the targets established during the initial harmonization, correcting for any minor instrument drift. This ensures longitudinal stability for each instrument throughout the project duration [51].
High-Throughput Acquisition
For screening campaigns, a dedicated High-Throughput Flow Cytometry (HTFC) system can be employed.
System Configuration:
- Platform: The HTFC Screening System (IntelliCyt Corporation), which integrates an autosampler with flow cytometer.
- Core Technology: The HyperCyt autosampler, which rapidly aspirates samples from microplates separated by air bubbles, enabling continuous data acquisition from an entire 384-well plate in approximately 12 minutes [46].
- Data Analysis: Embedded HyperView software is used for the rapid identification of hits from multiplexed assays.
Application: This system is optimal for high-throughput, cell-based applications such as drug efflux transporter screens, functional G-protein-coupled receptor (GPCR) assays, and antibody screening using suspension cells [46].
Automated, Supervised Gating for Unified Analysis
To eliminate operator-based bias in data interpretation, a supervised machine learning approach for automated gating is recommended.
Procedure:
- Create a Training Set: A single, expert operator manually gates a diverse set of FCS files representing the full biological and technical spectrum of the study.
- Algorithm Training: Use these manually gated datasets to train a supervised machine learning algorithm (automaton). The automation pipeline can be built in two steps: the first is instrument-specific to handle variations in forward and side scatter signals, and the second is a universal gating step for identifying final cell populations [51].
- Validation and Application: Validate the algorithm's performance by comparing its output with a traditional manual analysis on a separate set of samples. Once validated, the automaton is applied to all study files to extract population frequencies, absolute counts, and MFIs consistently and without bias [51].
The following workflow diagram synthesizes these protocols into a single, integrated process for cross-study standardization.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of the above protocols relies on the use of specific, high-quality reagents. The table below details key materials and their functions.
Table 1: Essential Research Reagents for Standardized Flow Cytometry
| Item | Specific Example | Function in Protocol |
|---|---|---|
| Calibration Beads | BD CS&T Beads, VersaComp Beads | Standardize PMT voltages across instruments to achieve matched MFIs for harmonization [51] [79]. |
| QC Beads | 8-Peak Beads (Beckman Coulter) | Daily monitoring of laser power and detector sensitivity to track instrument performance over time [51]. |
| Viability Dye | SYTOX Dead Cell Stain, 7-AAD | Impermeant nucleic acid stain that labels dead cells, allowing for their exclusion during analysis to improve data quality [77] [30]. |
| Nucleated Cell Stain | Vybrant DyeCycle Violet | Cell-permeant DNA stain used in no-lyse protocols to identify and gate nucleated leukocytes amidst erythrocytes [77]. |
| Pre-mixed Antibody Panels | DuraClone Tubes (Beckman Coulter) | Dried, pre-titrated antibody panels in single-use tubes that enhance staining reproducibility and minimize pipetting errors [51]. |
| Bright Fluorophores | Super Bright, Brilliant Violet Dyes | Conjugates for detecting low-abundance antigens; require careful pairing with antigen density in panel design [78] [79]. |
Quantitative Outcomes of Standardization
Implementing the described SOPs leads to measurable improvements in data quality and comparability, as demonstrated by the following quantitative metrics from published studies.
Table 2: Measurable Outcomes of Standardization Protocols
| Standardization Metric | Performance Outcome | Context & Validation |
|---|---|---|
| Inter-Instrument CV for MFI | < 5% | Achieved across 11 different flow cytometers in a multicenter study after initial harmonization with calibration beads [51]. |
| Post-Normalization CV for MFI | < 5% | Maintained after applying computational normalization to correct for daily instrument drift observed in QC data [51]. |
| Machine Learning Classification Accuracy | 93.88% - 98.15% | Robust accuracy maintained by a machine learning framework for classifying acute myeloid leukemia across different institutes and panel configurations [80]. |
| High-Throughput Sampling Rate | ~40 wells/minute | Throughput enabled by HyperCyt technology, allowing a 384-well plate to be processed in about 12 minutes [46]. |
The integration of standardized protocols for sample handling, instrument setup, high-throughput acquisition, and automated data analysis creates a robust pipeline for cross-study comparisons in flow cytometry. The meticulous approach outlined in this application note—from using no-wash, no-lyse staining methods to computational normalization and machine learning-based gating—provides a clear pathway to achieving reproducible, reliable, and comparable immunophenotyping data. For researchers engaged in large-scale biomarker discovery, clinical trial monitoring, or drug development, adherence to such SOPs is not merely a best practice but a fundamental requirement for generating scientifically valid and translatable findings.
Flow cytometry immunophenotyping of human blood is a cornerstone of modern immunological research and drug development. The analytical process of gating—identifying and refining cellular populations of interest—is critical for generating accurate, reproducible data. Traditionally performed manually, this process is increasingly being augmented or replaced by automated computational methods. In the context of high-throughput studies involving hundreds or thousands of human blood samples, the choice between manual and automated gating significantly impacts analytical variability, data reproducibility, and ultimately, the reliability of scientific conclusions [81] [15]. This application note examines the sources and extent of variability introduced by each method and provides detailed protocols for implementing automated gating to enhance data precision in large-scale immunophenotyping studies.
Quantitative Comparison of Gating Variability
Table 1 summarizes key performance indicators for manual and automated gating, highlighting the substantial benefits of automation in reducing variability, especially as data complexity increases.
Table 1: Quantitative Comparison of Manual vs. Automated Gating Performance
| Performance Metric | Manual Gating | Automated Gating | Notes & Context |
|---|---|---|---|
| Technical Variability (Inter-operator) | Up to 78% [81] | Significantly lower [81] | Estimated from comparisons of manual gating strategies |
| Coefficient of Variation (CV) | 6% (3-step data) to 57% (8-step data) [82] | Not explicitly quantified, but methods like UNITO deviate from human consensus by no more than any individual [83] | CV increases with data complexity in manual analysis |
| Analysis Time | >15 hours for 130-1000 samples [81] | Reduction from hours to minutes [81] | Time is dependent on the number of experimental units and marker parameters |
| Impact of Data Complexity | High negative impact; variability increases with parameters [82] | Robust; designed for high-dimensional data [15] [83] | Automated methods better handle multi-parameter data |
| Discovery Capability | Limited by pre-defined gating strategy | High; can identify novel, unexpected populations [81] | Requires biological validation |
| Performance Benchmark | Subjective and variable | UNITO matches consensus of multiple human experts [83] | Human consensus used as ground truth |
Experimental Protocols for Gating Methodology
Protocol for Manual Gating and Variability Assessment
This protocol outlines the steps for manual gating and includes a procedure to quantify inter-operator variability, a critical quality control measure.
- Required Materials: Flow cytometry data files (e.g., .fcs), proprietary or open-source analysis software (e.g., FlowJo), multiple trained operators.
- Sample Preparation: Process human peripheral blood mononuclear cells (PBMCs) to a single-cell suspension. Stain cells with a predefined panel of fluorescently conjugated antibodies targeting human leukocyte antigens (e.g., CD45, CD3, CD4, CD8, CD19, CD14) [84]. Include fluorescence-minus-one (FMO) controls for setting boundaries.
- Instrument Setup & Data Acquisition: Calibrate the flow cytometer using standard beads. Acquire data for all samples and controls, ensuring event counts are sufficient for robust statistics (e.g., >100,000 events per sample) [85].
- Sequential Gating Hierarchy:
- Singlet Gate: Plot Forward Scatter Area (FSC-A) vs. Height (FSC-H) to exclude cell doublets and aggregates [84].
- Live Cell Gate: Use a viability dye (e.g., PI) to select live cells and exclude debris and dead cells [85].
- Lymphocyte Gate: On an FSC-A vs. Side Scatter-A (SSC-A) plot, draw a gate around the lymphocyte population based on size and granularity [84].
- Lineage Gates: Apply successive two-parameter density plots (e.g., CD3+ for T-cells, CD19+ for B-cells) to identify target populations [81] [1].
- Variability Assessment: Provide the same dataset to at least 3-4 operators. Each operator applies the gating hierarchy independently. Calculate the Coefficient of Variation (CV) for the final population percentages (e.g., % CD4+ T-cells) across operators. For a more granular uncertainty analysis, track the number and percentage of events excluded/included at each gating step by each operator [82].
Protocol for Automated Gating with flowDensity
flowDensity is an R/Bioconductor package that automates a predefined sequential bivariate gating strategy, emulating a human expert's approach in a data-driven manner [86].
- Required Materials: R programming environment, flowDensity package, openCyto framework, flow cytometry data files (.fcs).
- Software Installation: Install the flowDensity package from Bioconductor using R. Ensure dependencies are installed.
- Data Pre-processing: Load .fcs files into R. Perform quality control checks and compensation for spectral overlap if not applied during acquisition.
- Gating Template Definition: Define the gating hierarchy programmatically. This mirrors the sequential steps of manual gating (e.g., singlet -> live -> lymphocytes -> CD3+ -> CD4+/CD8+).
- Threshold Calculation & Gating: flowDensity automatically calculates thresholds for each marker in each sample by analyzing the density distribution of the data [86]. It identifies peaks and determines the optimal cut-off using slope tracking, percentiles, or the minimum intersection point between peaks.
- Handling Rare Populations: For rare cell populations, the algorithm checks if the slope of the density curve drops below a threshold. If not, it uses a percentile (default: 90th) or the peak value plus a multiplier of the standard deviation [86].
- Utilizing Control Samples: If FMO or other control samples are available, they can be provided to the algorithm to improve the accuracy of gating threshold calculations [86].
- Output & Validation: The output is a set of population percentages. Validate the results by comparing them to manual gating from an expert or by using the consensus of multiple experts as a benchmark [83].
Protocol for Automated Gating with UNITO
UNITO is a recently developed framework that transforms the cell classification task into an image-based segmentation problem, demonstrating human-level performance [83].
- Required Materials: UNITO framework, a set of 30-40 manually gated cytometry samples for training, defined gating hierarchy.
- Training Data Preparation: For each gate in the hierarchy, normalize the protein expression data to a range of [0, 100]. Convert the normalized bivariate data (e.g., CD45 vs. SSC) into a 2D density plot. Use manually drawn gates from experts to create a corresponding binary mask for the population of interest. Apply a convex hull processing step to fill any empty space within the mask [83].
- Model Training: Train a separate deep learning model for each gate in the hierarchy. The model learns to associate the pattern of the density plot (input) with the binary mask (label). This process requires a defined gating hierarchy and is most effective when panel design is stable [83].
- Inference on New Data: For new, unseen samples, preprocess the data similarly to generate normalized density plots. The trained UNITO model then predicts a binary mask for each gate, which is post-processed to assign cell-type labels to each individual cell [83].
- Output: The framework outputs both a cell-type label for every cell and a convex contour on the density map that closely resembles a manual gate, allowing for intuitive post-hoc inspection [83].
The following workflow diagram illustrates the comparative stages of manual and automated gating processes, highlighting key points of variability and standardization.
Diagram Title: Manual vs Automated Gating Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2 lists essential reagents, software, and tools required for implementing robust and reproducible flow cytometry gating, whether manual or automated.
Table 2: Essential Research Reagents and Tools for Flow Cytometry Gating
| Item | Function/Description | Example Use Case |
|---|---|---|
| Fluorochrome-conjugated Antibodies | Specific recognition of cell surface and intracellular antigens. Clone and fluorochrome choice impact binding and resolution. | Immunophenotyping human blood leukocytes (e.g., CD45-APC, CD3-FITC) [85] [1]. |
| Viability Dye (e.g., PI, DAPI) | Distinguishes live cells from dead cells and debris during the initial gating step. | Creating a "live cell gate" to exclude false positives from dead cells [85]. |
| Compensation Beads | Used to calculate compensation matrices for correcting spectral overlap between fluorochromes. | Critical for accurate multi-color flow cytometry panel setup [85]. |
| Flow Cytometry Software (Proprietary) | GUI-based software for manual data acquisition and analysis (e.g., FlowJo, FACSDiva). | Initial data visualization, manual gating strategy development, and comparison with automated results [81] [84]. |
| Automated Gating Software (Open Source) | Command-line or scriptable tools for reproducible analysis (e.g., flowDensity, UNITO, FlowSOM). | High-throughput, reproducible analysis of large immunophenotyping datasets [86] [15] [83]. |
| Synthetic Data Generators (e.g., CluGen) | Generates data with absolute ground truth for validating gating algorithms and operator performance. | Benchmarking automated gating tools and training new analysts to reduce variability [87]. |
| Standardized Antibody Panels | Pre-validated sets of antibodies for specific cell types, as defined by working groups (e.g., WHO, Bethesda). | Ensuring consistency and accuracy in diagnosing and monitoring hematological malignancies [1]. |
The transition from manual to automated gating is a critical step in mitigating analytical variability for high-throughput flow cytometry immunophenotyping. Manual gating, while intuitive, introduces significant technical variation and is not scalable for large cohort studies. Automated methods like flowDensity and UNITO offer a compelling alternative, providing superior speed, reproducibility, and reduced operator-dependent bias. For drug development professionals and researchers, adopting automated gating protocols, complemented by standardized reagent panels and rigorous quality control using tools like synthetic data, is essential for generating the high-precision data required to uncover robust biological insights and advance human immunology research.
Validation Frameworks for Instrument Performance and Linearity
This application note provides a detailed framework for validating instrument performance and linearity in high-throughput flow cytometry for immunophenotyping human blood. It outlines key experimental protocols, performance criteria, and analytical tools essential for generating reliable, reproducible data in drug development and clinical research.
For researchers and scientists engaged in high-throughput flow cytometry immunophenotyping, robust validation of instrument performance and assay linearity is a critical prerequisite for generating reliable and reproducible data. Flow cytometry enables the rapid, multiparametric analysis of single cells within heterogeneous populations, making it indispensable for the diagnosis and classification of hematological malignancies, monitoring of minimal residual disease (MRD), and evaluation of immune responses in clinical trials [1]. However, the technique involves numerous manual steps and variables susceptible to operator bias and human error, necessitating rigorous standardization and validation to ensure data accuracy, reproducibility, and trueness across different laboratories and studies [1] [53]. This document provides a standardized framework and detailed protocols for validating two cornerstone aspects of flow cytometry performance: instrument stability and assay linearity.
Quantitative Performance Standards and Acceptance Criteria
Successful validation requires defining and adhering to quantitative performance standards. The following table summarizes the key parameters, their definitions, and typical acceptance criteria for a validated flow cytometry method, based on regulatory guidance and industry best practices [88].
Table 1: Key Validation Parameters and Acceptance Criteria for Flow Cytometry Assays
| Parameter | Definition | Acceptance Criteria |
|---|---|---|
| Accuracy | Closeness of agreement between the test value and an accepted reference value. | Comparison to a reference material or standardized control. |
| Precision | Closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample. | Intra- and inter-day precision values (e.g., %CV) within 20% at multiple concentration levels [88]. |
| Linearity | The ability of an assay to obtain results directly proportional to the analyte concentration within a given range. | Demonstration of a linear response across the intended range with a high coefficient of determination (R²). |
| Range | The interval between the upper and lower analyte concentrations for which suitable precision, accuracy, and linearity have been demonstrated. | Validated from the Lower Limit of Quantification (LLOQ) to the Upper Limit of Quantification (ULOQ). |
| Limit of Quantitation (LOQ) | The lowest amount of analyte that can be quantitatively determined with suitable precision and accuracy. | Signal-to-noise ratio typically >10; %CV ≤ 20-25% [89]. |
| Limit of Detection (LOD) | The lowest amount of analyte that can be detected, but not necessarily quantified. | Signal-to-noise ratio typically >3. |
| Specificity | The ability to assess the analyte unequivocally in the presence of other components. | No significant interference from matrix components or similar analytes. |
A cross-laboratory study by the Human ImmunoPhenotyping Consortium (HIPC) demonstrated that within-site variability is generally low, but cross-site variability can be significant. This variability was lower for clearly defined cell subsets than for those based on dim markers or rare populations [53]. Implementing the validation framework below is designed to minimize this cross-site variability.
Experimental Protocol 1: Instrument Performance Qualification (PQ)
This protocol ensures the flow cytometer is performing within specified parameters before running analytical samples.
Materials and Reagents
- Quality Control Beads: Commercially available fluorescent beads (e.g., rainbow beads) for daily instrument tracking and performance validation [89].
- Lyophilized Peripheral Blood Mononuclear Cells (PBMCs): Provide a consistent biological control with a certificate of analysis detailing predetermined percentages of major immune cell subsets [53] [89].
- Cell Mimics: Synthetic, polymer-based particles (e.g., TruCytes, HyParComp) that replicate cellular features like size, granularity, and specific protein expression. These offer minimal lot-to-lot variability and a shelf life of up to 18 months, making them ideal for standardization and antibody titration [89].
Step-by-Step Procedure
- Power-up and Sanitization: Power on the instrument and fluidics system. Perform a sanitization or decontamination procedure if required.
- Laser Warm-up: Allow all lasers to stabilize for a minimum of 30 minutes, or as recommended by the manufacturer.
- QC Bead Run: Vortex the QC beads thoroughly and run the sample. Adjust photomultiplier tube (PMT) voltages for each channel to place the bead population in its historical target channel, as defined during instrument calibration.
- Performance Tracking: Record the mean fluorescence intensity (MFI) and coefficient of variation (CV) for each fluorescence channel. Compare these values to established historical means and standard deviations to ensure the instrument is in control.
- Biological Control Verification (Recommended): Run a lyophilized PBMC or cell mimic control stained with a standard antibody panel (e.g., CD45, CD3, CD4, CD8, CD19, CD56). Analyze the data to verify that the percentages of major lymphocyte subsets fall within the expected ranges provided by the manufacturer.
Data Analysis and Interpretation
- Calculate the daily %CV for each fluorescence channel from the QC beads.
- Apply statistical process control (SPC): Plot the daily MFI values on a Levey-Jennings chart. Data points should fall within ±2 standard deviations of the historical mean. Points outside ±3 standard deviations indicate the process is out of control, and the instrument may require service.
- For biological controls, ensure that the coefficient of variation for cell population percentages between runs is within acceptable limits (e.g., <20%).
The workflow for this qualification process is systematic and ensures all critical components are assessed.
Experimental Protocol 2: Determining Assay Linearity and Limit of Quantification
This protocol describes a method to establish the linear range and LOQ for a quantitative flow cytometry assay, using cell mimics to overcome challenges associated with biological sample variability.
Materials and Reagents
- Test Sample: The cell population of interest (e.g., patient T cells) or a suitable surrogate.
- Negative Diluent: A matrix that does not generate a positive signal. This can be "naked" cell mimics (without target proteins) or negative control cells [89].
- HyParComp Beads or Similar: A system consisting of 100% positive and 100% negative beads, designed for compensation and linearity studies [89].
- Staining Antibodies: Validated antibody conjugates for the target epitopes.
Step-by-Step Procedure
Two parallel approaches are recommended for a robust assessment [89]:
Sample-Based Dilution Series:
- Start with a 100% positive sample (e.g., purified T cells).
- Create a series of dilutions (e.g., 80%, 60%, 40%, 20%, 10%, 5%, 3%, 1%, 0.5%, 0%) using the negative diluent. Ensure cell viability is high and consistent.
- Stain all samples with the relevant antibodies and acquire data on the flow cytometer.
Cell Mimic-Based Dilution Series:
- Start with 100% HyParComp positive beads.
- Create an identical series of dilutions using the HyParComp negative ("naked") beads.
- Stain and acquire data as above.
Data Analysis and Interpretation
- For each dilution, calculate the percentage of positive events and the MFI.
- Plot the measured percentage (y-axis) against the expected percentage (x-axis) for both the biological sample and the cell mimic series.
- Perform linear regression analysis to determine the R² value. An R² value >0.98 indicates excellent linearity [89].
- The LOQ is the lowest concentration where the %CV is ≤20-25%. Cell mimics typically show a lower LOQ (e.g., ~1%) due to minimal variability, whereas biological cells may have a higher LOQ (e.g., ~3%) due to heterogeneity [89].
The process for establishing linearity and LOQ involves careful preparation of a dilution series and quantitative analysis.
The quantitative outcomes from a typical linearity and LOQ experiment are summarized below.
Table 2: Example Results from a Linearity and LOQ Experiment [89]
| Sample Type | Linearity (R² Value) | Achieved LOQ | Notes |
|---|---|---|---|
| HyParComp Cell Mimics | 0.999 | ~1.1% | Minimal variability; clean, consistent results. |
| Tumor-Infiltrating Lymphocytes (TILs) | 0.991 | ~3.0% | Higher variability due to non-uniform cell distribution. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents that are critical for implementing robust validation frameworks.
Table 3: Essential Reagents for Flow Cytometry Validation
| Reagent / Solution | Function | Key Benefit |
|---|---|---|
| Lyophilized PBMCs | Biological control for immunophenotyping assays. | Pre-characterized cell populations ensure consistency across runs and labs [53] [89]. |
| Fluorescent QC Beads | Daily instrument performance tracking and standardization. | Allows for monitoring of laser power, fluidics, and detector sensitivity over time [89]. |
| Cell Mimics (e.g., TruCytes) | Synthetic particles for antibody titration and assay development. | Minimize lot-to-lot variability; provide a standardized substrate for titrating new antibody lots [89]. |
| Linearity Beads (e.g., HyParComp) | Determination of assay linearity and LOQ. | Provide a clean 0% and 100% positive reference for constructing a standard curve, overcoming biological sample heterogeneity [89]. |
| Lyophilized Antibody Panels | Pre-configured, multi-color staining panels. | Reduces pipetting errors, improves inter-laboratory reproducibility, and simplifies assay setup [53]. |
Implementing the validation frameworks and protocols outlined in this document is essential for ensuring the generation of high-quality, reliable flow cytometry data in high-throughput immunophenotyping studies. The integration of novel tools like synthetic cell mimics and lyophilized controls directly addresses historical challenges in standardization, linearity assessment, and inter-laboratory reproducibility. By adhering to these rigorous validation practices, researchers and drug development professionals can have greater confidence in their data, ultimately accelerating biomarker discovery and therapeutic development.
Comparative Analysis of Flow Cytometry vs. Mass Cytometry Approaches
In the field of single-cell proteomic analysis, spectral flow cytometry and mass cytometry have emerged as powerful technologies enabling deep immunophenotyping of human blood, which is crucial for both basic research and clinical diagnostics [90] [91]. These platforms overcome the limitations of conventional flow cytometry by allowing the simultaneous assessment of dozens of parameters, thus providing a comprehensive view of immune cell heterogeneity [92]. For researchers working within the context of high-throughput immunophenotyping, selecting the appropriate technology is paramount to the success of their projects. This application note provides a comparative analysis of these two platforms, supported by quantitative data, detailed protocols, and experimental workflows, to guide researchers and drug development professionals in making an informed choice based on their specific clinical and research objectives.
Fundamental Principles
Spectral Flow Cytometry operates on principles similar to conventional flow cytometry but with a fundamental difference in detection. Instead of using optical filters to direct narrow bands of light to individual detectors, spectral cytometers capture the full emission spectrum of every fluorophore across a wide range of wavelengths [90]. This is achieved through the use of a prism or diffraction grating that scatters the emitted light onto an array of highly sensitive detectors (typically 32-64 channels) [90]. The resulting full spectral data is then deconvoluted using mathematical algorithms to identify the individual contribution of each fluorophore in the panel [93]. This approach allows for the resolution of fluorophores with significant spectral overlap, provided their complete spectral signatures are distinct [90].
Mass Cytometry (CyTOF) replaces fluorescence with mass spectrometry as its detection method. Antibodies are conjugated to stable heavy metal isotopes rather than fluorochromes [91] [93]. Cells labelled with these metal-tagged antibodies are nebulized into single-cell droplets, which are then ionized and passed through a time-of-flight (TOF) mass spectrometer [93]. The mass spectrometer quantifies the metal isotopes attached to each cell, effectively measuring marker expression [92]. A key advantage of this approach is the virtual absence of signal overlap between metal isotopes, as the mass resolution of the CyTOF instrument can distinguish between isotopes with minimal mass differences [92].
Comparative Performance Characteristics
The table below summarizes the key technical characteristics and performance metrics of both platforms, which are critical considerations for experimental design in high-throughput immunophenotyping studies.
Table 1: Key Performance Characteristics of Spectral Flow Cytometry and Mass Cytometry
| Characteristic | Spectral Flow Cytometry | Mass Cytometry (CyTOF) |
|---|---|---|
| Detection Principle | Full fluorescence spectrum measurement [90] | Heavy metal isotope detection via mass spectrometry [93] |
| Panel Size | Up to 40+ markers [92] | Up to 40+ markers [92] |
| Acquisition Rate | High (~20,000 events/second) [93] | Low (~300-500 events/second) [93] |
| Sensitivity | High (~40 molecules/cell) [93] | Lower (~400-500 molecules/cell) [93] |
| Cell Input Requirements | Lower, suitable for low-yield samples (e.g., biopsies) [92] | Higher (2-3 fold more than spectral) [92] |
| Throughput | Higher throughput, suitable for larger sample numbers [92] | Slower acquisition limits daily sample throughput [92] |
| Post-stain Stability | Limited (typically <24 hours) [92] | Exceptionally long due to stable metal tags [92] |
| Autofluorescence | Can be measured and subtracted [93] | Not applicable [93] |
| Cell Morphology (FSC/SSC) | Yes | No [93] |
Experimental Protocols for Blood Immunophenotyping
Protocol for Spectral Flow Cytometry
A. Sample Preparation and Staining for Human Peripheral Blood Mononuclear Cells (PBMCs)
This protocol is optimized for minimal sample perturbation, preserving native cell states for accurate immunophenotyping [94].
- Blood Collection and PBMC Isolation: Collect peripheral blood using citrate anticoagulant. Isolate PBMCs within 2 hours of collection using Ficoll-Paque Plus gradient centrifugation [93]. Wash cells and resuspend in phosphate-buffered saline (PBS). Count cells using an automated hematology analyzer.
- Antibody Staining:
- Aliquot Cells: Distribute 5x10^6 PBMCs per staining tube [93].
- Titrate Antibodies: Prior to the experiment, titrate all antibody reagents to determine optimal signal-to-noise ratios [93].
- Stain: Incubate cells with the pre-mixed antibody cocktail for a standardized time at room temperature, protected from light.
- Wash: Remove unbound antibody by washing with PBS buffer.
- Resuspend: Resuspend the stained cell pellet in a suitable buffer for acquisition (e.g., PBS with 0.5% BSA). If not acquired immediately, fix samples gently.
B. Data Acquisition on a Spectral Cytometer
- Instrument Setup: Start the instrument and software (e.g., SpectroFlo for Sony instruments). Perform quality control and calibration using manufacturer-recommended beads.
- Load Sample: Introduce the sample tube or well plate.
- Acquire Data: Set the acquisition rate and target event count. For rare populations, ensure a sufficiently high total event count is collected (e.g., 1-5 million events per sample). Record data in the native file format.
C. Data Analysis
- Spectral Unmixing: Use the instrument's software to apply the spectral unmixing algorithm, which deconvolutes the full emission spectrum into the signal from each individual fluorophore.
- Gating and Population Identification: Export the unmixed FCS files. Proceed with manual gating in flow cytometry analysis software (e.g., FlowJo) or use automated clustering algorithms (e.g., in R or Python) to identify cell populations of interest [53].
Protocol for Mass Cytometry
A. Sample Preparation and Barcoding
- Cell Staining: The initial steps for PBMC isolation are identical to the spectral protocol. Stain cells with the metal-tagged antibody panel.
- Cell Barcoding (Optional but Recommended): To minimize technical variability and reduce antibody consumption, use a live-cell barcoding kit. This involves staining individual samples with unique combinations of metal-tagged barcoding antibodies (e.g., targeting CD45). After staining, samples can be pooled for subsequent processing [93].
- Viability Staining: Stain cells with an intercalator-Ir (Iridium) or Rh (Rhodium) to identify and exclude dead cells during analysis.
- Fixation: Fix cells with a paraformaldehyde solution (e.g., 1.6%) to preserve the sample for acquisition, which may occur at a later time.
B. Data Acquisition on a Mass Cytometer
- Instrument Tuning: Tune the CyTOF instrument according to the manufacturer's specifications to ensure optimal sensitivity and resolution. This typically involves adjusting the ionization source and TOF settings.
- Sample Introduction: Dilute the fixed, stained cell suspension in deionized water containing a normalization standard (e.g., EQ Beads). The system will nebulize the sample into single-cell droplets for introduction into the plasma ion source.
- Acquire Data: Set the acquisition rate to the recommended level (e.g., 300-500 events/second) to minimize cell coincidences (doublets). Acquire data until the desired number of events is collected.
C. Data Analysis
- Preprocessing: If barcoded, use the barcoding software to deconvolute the single data file into individual sample files based on the barcode signatures.
- Normalization: Apply a normalization algorithm to correct for minor instrument sensitivity fluctuations during the run using the bead standard signals.
- Cell Population Identification: As with spectral data, use either manual gating or, more commonly for high-dimensional data, automated clustering approaches (e.g., t-SNE, UMAP, PhenoGraph) to identify and characterize cell populations.
Workflow Diagram
The following diagram illustrates the key procedural differences between the two cytometry workflows, from sample preparation to data analysis.
Performance Assessment in Research Settings
Quantitative Data Comparison
Independent studies have directly compared the performance of these two platforms using identical antibody panels. One such study employed a 33-color panel on samples from healthy donors and found a strong overall concordance.
Table 2: Experimental Results from a Comparative Study Using a 33-Color Panel [91]
| Performance Metric | Spectral Flow Cytometry | Mass Cytometry (CyTOF) | Implication for Research |
|---|---|---|---|
| Correlation of Major Populations | ρ = 0.99 (Pearson’s) [93] | ρ = 0.99 (Pearson’s) [93] | Excellent concordance for abundant cell types. |
| Staining Resolution | ρ = 0.55 (Pearson’s) [93] | ρ = 0.55 (Pearson’s) [93] | Good correlation for marker intensity. |
| Intra-measurement Variability | Lower (Median CV: 42.5%) [93] | Higher (Median CV: 68.0%) [93] | Spectral shows better technical reproducibility. |
| Cell Recovery Rate | Higher (Median: 53.1%) [93] | Lower (Median: 26.8%) [93] | Spectral is superior for limited samples. |
| Acquisition Time per Sample | Faster (Median: 16 min) [93] | Slower (Median: 159 min) [93] | Spectral offers higher throughput. |
Platform Selection Guide
The choice between spectral and mass cytometry is not a matter of one being universally superior, but rather which is best suited for a specific study's requirements.
Table 3: Platform Selection Guide for Specific Research Scenarios
| Research Scenario / Need | Recommended Platform | Rationale |
|---|---|---|
| High-Throughput Screening | Spectral Flow Cytometry | Faster acquisition rates enable processing of hundreds of samples in a feasible timeframe [95]. |
| Very Large Panels (>50 markers) | Mass Cytometry | Minimal channel crosstalk due to detection of distinct heavy metals [92]. |
| Limited Sample (e.g., TILs, biopsies) | Spectral Flow Cytometry | Lower cell input requirements and higher recovery rates preserve rare events [92]. |
| Analysis of Cell Morphology (FSC/SSC) | Spectral Flow Cytometry | Provides forward and side scatter data, which is not available in CyTOF [93]. |
| Requirement for Long-Term Sample Stability | Mass Cytometry | Metal-tagged antibodies are extremely stable, allowing analysis days after staining [92]. |
| Focus on Low-Abundance Proteins | Spectral Flow Cytometry | Higher sensitivity allows for better detection of proteins with low expression [93]. |
The Scientist's Toolkit: Essential Reagent Solutions
Successful execution of high-dimensional immunophenotyping requires careful selection and validation of key reagents. The following table details essential materials and their functions.
Table 4: Key Research Reagent Solutions for High-Dimensional Cytometry
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| Pre-configured Lyophilized Antibody Panels | Standardized, multi-color antibody cocktails in 96-well plates. | Reduces preparation errors, improves inter-laboratory reproducibility, and simplifies assay setup [53]. |
| Cell Barcoding Kit (for CyTOF) | A set of metal-tagged antibodies for live-cell sample multiplexing. | Reduces technical variability, reagent consumption, and acquisition time by pooling samples [93]. |
| Viability Stains | To identify and exclude dead cells during analysis. | Critical for data quality. Use fixable viability dyes (e.g., near-IR) for spectral; intercalator-Ir/Rh for CyTOF [93]. |
| Quality Control Beads | For daily instrument performance tracking and calibration. | Ensures data consistency and allows for performance monitoring over time and across core facilities. |
| Custom Conjugation Services | For conjugating antibodies to desired fluorochromes or heavy metals. | Essential for panel flexibility, especially for mass cytometry where commercial reagents are more limited [92]. |
| Standardized Buffer Systems | For cell staining, washing, and resuspension. | Minimizes non-specific binding and preserves cell integrity, leading to cleaner data and higher cell recovery. |
Spectral flow cytometry and mass cytometry are both powerful and highly complementary technologies for deep immunophenotyping in human blood research. The evidence demonstrates a strong overall concordance in their ability to identify and quantify major immune cell populations [91] [93]. The decision for one platform over the other must be guided by the specific demands of the clinical or research study. Spectral flow cytometry generally offers advantages in throughput, sensitivity, and suitability for precious, low-yield samples. In contrast, mass cytometry excels in panel size potential, long-term sample stability, and minimal signal overlap. By aligning the strengths of each technology with project goals—throughput, panel complexity, sample type, and data analysis strategy—researchers can effectively leverage these advanced tools to unlock the complexities of the immune system and accelerate drug discovery.
Implementing Automated Analysis with FlowAI and FlowSOM Clustering
This application note provides a detailed protocol for implementing an automated analysis pipeline integrating FlowAI for data quality control and FlowSOM for clustering in high-throughput flow cytometry immunophenotyping of human blood. This integrated approach enhances analytical reproducibility and enables robust, unbiased population identification, which is crucial for large-scale immunophenotyping studies in drug development and clinical research. The methodology presented streamlines the transition from raw data to biologically interpretable results while maintaining rigorous quality standards.
High-dimensional flow cytometry has become an indispensable tool for comprehensive immunophenotyping of human blood, enabling simultaneous measurement of dozens of cellular parameters. However, the analytical process remains challenging due to data quality issues and the complexity of population identification. Automated analysis pipelines that combine rigorous quality control with sophisticated clustering algorithms address these challenges effectively.
FlowAI provides an automated method for identifying and removing anomalies in flow cytometry data caused by instrument issues, samples, or acquisition problems [96]. These anomalies—including clogs, bubbles, or flow rate irregularities—can confound downstream analysis if not properly addressed [97].
FlowSOM (Flow Self-Organizing Maps) represents a state-of-the-art clustering and visualization tool that facilitates the analysis of high-dimensional data by arranging clusters via a Self-Organizing Map into a Minimum Spanning Tree [98]. This two-level clustering approach (initial clustering followed by meta-clustering) enables researchers to discern biological similarity between cell populations with high resolution [99].
The integration of these tools creates a robust pipeline for high-throughput immunophenotyping studies, ensuring that data quality issues are addressed prior to the computationally intensive clustering process.
Materials and Methods
Research Reagent Solutions
Table 1: Essential Research Reagents for High-Throughput Immunophenotyping
| Reagent Category | Specific Examples | Function and Application Notes |
|---|---|---|
| Viability Probe | Slingshot ViaComp particles, amine-reactive dyes | Critical for excluding dead cells that cause non-specific binding and autofluorescence with aberrant spectra [100]. |
| Blocking Buffers | Fc receptor blockers, Brilliant Stain Buffer, monocyte blockers | Reduce non-specific antibody binding. Fc blockers are essential for monocytes, B cells, and dendritic cells [100]. |
| Fluorophore-Conjugated Antibodies | Brilliant Violet series, Super Bright polymers, Alexa Fluor dyes | Panel design should match antigen abundance to fluorophore brightness and consider staining index [78]. |
| Reference Control Particles | Unstained controls, single-color controls | Essential for spectral unmixing and establishing baseline fluorescence [78]. |
Instrumentation and Software Requirements
For optimal implementation of this pipeline, the following resources are required:
- Flow Cytometers: Spectral analyzers (e.g., Cytek Aurora, Sony SA3800) or conventional flow cytometers capable of high-parameter data acquisition
- Analysis Software: Platforms supporting FlowAI and FlowSOM implementation, such as OMIQ [96], FCS Express [98], or FlowJo with appropriate plugins [99]
- Computational Environment: R/Bioconductor for custom implementation (flowAI package, FlowSOM package) [97]
Integrated Workflow Protocol
The following diagram illustrates the complete analytical workflow from sample preparation through data interpretation:
Figure 1. Integrated analytical workflow for high-throughput immunophenotyping.
FlowAI Quality Control Implementation Protocol
FlowAI performs three sequential anomaly detection methods to clean FCS data. The algorithm examines all three properties and generates a comprehensive quality report, though users can select which methods to apply for actual event rejection [96].
Figure 2. FlowAI's three-step anomaly detection process.
Flow Rate Analysis (FR)
Purpose: Identifies significant deviations from median flow rate caused by instrument issues such as clogs or bubbles [96].
Protocol:
- Parameter Setting: Set Time Feature to appropriate time channel
- Bin Calculation: Define Seconds Fraction (default = 0.1) to establish time bins for event counting
- Statistical Testing: Apply generalized extreme studentized deviate (ESD) test with Alpha (significance) typically set at 0.05
- Decomposition: Enable "Decompose Flow Rate" for stringent analysis considering trend and cyclical components
Table 2: Key FlowAI Parameters for Flow Rate Analysis
| Parameter | Recommended Setting | Impact of Modification |
|---|---|---|
| Seconds Fraction | 0.1 | Increasing speeds computation, provides smoothing effect |
| Alpha (significance) | 0.05 | Lower values reduce rejections (requires larger deviations) |
| Decompose Flow Rate | Enabled | More stringent, considers global file characteristics |
Signal Acquisition Analysis (FS)
Purpose: Identifies regions of unstable signal acquisition across channels by detecting changepoints in signal over time [96].
Protocol:
- Outlier Removal: Enable "Remove Outliers" to exclude outlier bins before changepoint detection
- Changepoint Detection: Set penalty value (default = 0.5); lower values increase changepoint sensitivity
- Stable Region Identification: Algorithm identifies the most stable contiguous time region across all channels
- Region Selection: The most stable region is kept; remainder is rejected
Dynamic Range Analysis (FM)
Purpose: Identifies negative and positive outlier events across all channels that may represent measurement artifacts [96].
Protocol:
- Channel Selection: Include all relevant fluorescent parameters
- Threshold Application: Algorithm automatically identifies outliers beyond dynamic range limits
- Event Rejection: Negative outliers and margin events in upper limit are flagged for removal
FlowSOM Clustering Implementation Protocol
FlowSOM utilizes a two-level clustering approach to efficiently analyze high-dimensional cytometry data. The method first organizes cells into a Self-Organizing Map (SOM) followed by meta-clustering to group similar clusters [98] [99].
Figure 3. FlowSOM clustering workflow with two-level clustering approach.
Self-Organizing Map (SOM) Construction
Purpose: Creates an organized grid of nodes where similar cells are grouped together, preserving the topological structure of the data [98].
Protocol:
- Data Preparation: Use FlowAI-cleaned data and select relevant markers for clustering
- Grid Size Definition: Typically use a 10×10 grid (100 clusters) for balanced resolution and interpretability
- Training Iterations: Allow sufficient iterations for model convergence (typically 10,000-100,000)
- Node Assignment: Each cell is assigned to the most similar node (cluster) based on marker expression
Meta-Clustering Implementation
Purpose: Groups similar SOM clusters into meta-clusters representing biologically distinct populations [98].
Protocol:
- Similarity Calculation: Compute similarities between all SOM clusters based on marker expression patterns
- Consensus Clustering: Apply hierarchical consensus clustering to group similar SOM clusters
- Cluster Number Determination: Use automatic determination or specify expected population number (typically 10-30 for immunophenotyping)
- Meta-Cluster Assignment: Assign each SOM cluster to a meta-cluster
Application to Human Blood Immunophenotyping
Panel Design Considerations for High-Throughput Studies
Effective panel design is crucial for successful immunophenotyping. These principles are especially important when transferring panels to spectral cytometers capable of analyzing 50-color panels [100]:
- Brightness Matching: Match fluorophore brightness to antigen abundance; bright fluorophores (PE, BV421) for low-abundance markers
- Complexity Index Management: Use tools like IntelliPanel to calculate complexity index and minimize spectral overlap within co-expression groups
- Spillover Consideration: Avoid combinations of fluorophores with heavy spectral overlap for markers expressed on the same cell population
- Validation Controls: Include single-color controls and unstained samples for proper unmixing and autofluorescence extraction [78]
Data Interpretation and Validation
The integrated FlowAI and FlowSOM pipeline produces several key outputs that require biological interpretation:
- FlowAI Quality Report: Provides percentage of events removed for each anomaly type and visualizations of affected regions
- FlowSOM Minimum Spanning Tree: Visual representation of clusters and their relationships
- Meta-Cluster Phenotypes: Characterize each meta-cluster based on marker expression patterns
- Population Abundances: Quantify frequencies of identified populations across samples
Validation should include comparison with manual gating strategies, assessment of population purity, and correlation with biological expectations based on experimental conditions.
Troubleshooting and Optimization
FlowAI Performance Issues
- High Event Rejection: Adjust Alpha significance level upward (less stringent) or disable Decompose Flow Rate
- Computational Speed: Increase Seconds Fraction parameter or apply subsampling to large files
- Inadequate Cleaning: Lower Alpha value (more stringent) or enable Decompose Flow Rate for comprehensive analysis
FlowSOM Clustering Challenges
- Over-clustering: Reduce SOM grid size or meta-cluster number
- Under-clustering: Increase SOM grid size or meta-cluster number
- Unstable Clusters: Increase training iterations or check for batch effects
The integrated FlowAI and FlowSOM pipeline presented here provides a robust, automated solution for high-throughput flow cytometry immunophenotyping of human blood. This approach ensures data quality through systematic anomaly detection while enabling comprehensive population identification through advanced clustering. The methodology enhances reproducibility in large-scale studies and facilitates discovery of novel cell populations in drug development research.
Conclusion
High-throughput flow cytometry immunophenotyping has emerged as a powerful platform for large-scale immune monitoring, enabling the precise characterization of human blood immune cells across thousands of samples. The integration of robust sample processing pipelines, standardized protocols, rigorous quality control, and automated analysis frameworks is crucial for generating reproducible, high-dimensional data with minimal technical variation. As demonstrated in recent large cohort studies, these approaches can reveal subtle immune dynamics associated with aging, genetics, and disease. Future directions will focus on further automation, integration with other omics technologies, and the development of even more sophisticated computational tools. This progression will continue to enhance our understanding of immune system complexity and accelerate biomarker discovery and therapeutic development in immunology and oncology.
References
- 1. An Update on Flow Cytometry Analysis of Hematological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190783/]
- 2. Twenty years' development and application of flow cytometry [https://link.springer.com/article/10.1007/s12519-025-00949-9]
- 3. Best Practices for Multiparametric Flow Cytometry [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-79/best-practices-multiparametric-flow-cytometry.html]
- 4. 5 Best Practices For Accurate Flow Cytometry Results [https://expertcytometry.com/best-practices-for-accurate-flow-cytometry-results/]
- 5. Data analysis in flow cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/data-analysis-in-flow-cytometry]
- 6. How to Interpret Flow Cytometry Data [https://www.fortislife.com/resources/antibody-resources/how-to-interpret-flow-cytometry-data]
- 7. Advanced flow cytometry data analysis ... [https://www.flowjo.com/advanced_analysis.html]
- 8. The benefit of large-scale cohort studies for health research [https://pubmed.ncbi.nlm.nih.gov/26077870/]
- 9. Deep Immunophenotyping of Human Whole Blood by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10260734/]
- 10. What Is A Cohort Study: Cohort Studies In Clinical Trials [https://www.allclinicaltrials.com/blog/what-is-a-cohort-study]
- 11. The Strengths of Historical Cohort Studies [https://www.redalyc.org/journal/1993/199365992002/html/]
- 12. Importance of cohort and target trial emulation in clinical ... [https://www.sciencedirect.com/science/article/pii/S2666379125001545]
- 13. Population-based cohort studies [https://unityinsights.co.uk/news/population-based-cohort-studies/]
- 14. Flow Cytometry Protocol | Abcam [https://www.abcam.com/en-us/technical-resources/protocols/flow-cytometry-for-intracellular-and-extracellular-targets]
- 15. A robust pipeline for high-content, high-throughput ... [https://www.sciencedirect.com/science/article/pii/S2667237523002837]
- 16. High-Throughput 13-Parameter Immunophenotyping Identifies ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0047155]
- 17. Deep Immunophenotyping of Human Whole Blood by ... [https://pubmed.ncbi.nlm.nih.gov/37325713/]
- 18. Flow Cytometry Blood Cell Identification - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK608011/]
- 19. Full immune cell profile | Translational Immunology Core [https://humanimmunology.sites.uiowa.edu/flow-cytometry-panels/full-immune-cell-profile]
- 20. 13-Parameter Immunophenotyping of Human Lysed Whole ... [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/flow-cytometry/flow-cytometry-learning-center/flow-cytometry-resource-library/flow-cytometry-application-notes/multiparameter-immunophenotyping-human-lysed-whole-blood-attune-nxt-flow-cytometer-b-cells-nk-cells-t-cells-myeloid-cells.html]
- 21. Comprehensive Guide to Gating Strategies in Flow Cytometry [https://www.bosterbio.com/blog/post/comprehensive-guide-to-gating-strategies-in-flow-cytometry?srsltid=AfmBOoqo4QP5UdRg8hZwFpmqGQDuKqKBwgnA5upQdzzml2Ii63IGn6lR]
- 22. Setting Compensation Multicolor Flow [https://www.bdbiosciences.com/en-us/resources/protocols/setting-compensation-multicolor-flow]
- 23. 25-Marker Spectral Flow Panel for Immune Profiling ... [https://www.teiko.bio/publication/spectral-whole-blood-cyto-2025]
- 24. Guidelines for the use of flow cytometry and cell sorting in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9165548/]
- 25. Full Spectrum Flow Cytometry as a Powerful Technology ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2020.612801/full]
- 26. Clinical Applications of Flow Cytometry in Cancer ... [https://pubmed.ncbi.nlm.nih.gov/36513926/]
- 27. The future direction and applications of flow cytometry [https://www.ddw-online.com/the-future-direction-and-applications-of-flow-cytometry-34291-202504/]
- 28. The Power of Flow Cytometry in Biomarker-Driven Clinical ... [https://www.precisionformedicine.com/blog/harnessing-flow-cytometry-biomarker-driven-clinical-trials/]
- 29. Flow-cytometry-based protocols for human blood/marrow ... [https://pubmed.ncbi.nlm.nih.gov/34693361/]
- 30. Whole Blood Staining Protocol for Flow Cytometry Analysis [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/immunology-at-work/immunology-protocols/whole-blood-staining-protocol-flow-cytometry.html]
- 31. Designing a multicolor flow cytometry protocol [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/designing-a-multicolor-protocol]
- 32. Europe Flow Cytometry Research Report 2025: Market to [https://www.globenewswire.com/news-release/2025/09/18/3152221/28124/en/Europe-Flow-Cytometry-Research-Report-2025-Market-to-Surpass-2-Billion-by-2035-Expanding-Use-in-Drug-Discovery-Translational-Research-and-Clinical-Trials.html]
- 33. Display Comparison - FlowJo Documentation [https://docs.flowjo.com/flowjo/graphs-and-gating/data-visualization-and-display/gw-compare/]
- 34. Comparison of immunometabolic profiles in whole blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12604536/]
- 35. Comparison of Whole Blood Cryopreservation Methods for ... [https://www.mdpi.com/2073-4409/11/9/1527]
- 36. Flow cytometry reveals constant lymphocyte proportions ... [https://www.sciencedirect.com/science/article/pii/S0022175925000535]
- 37. Technical pitfalls when collecting, cryopreserving, thawing ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1382192/full]
- 38. Flow Cytometry Staining Protocols for High-Quality Data [https://www.technologynetworks.com/cell-science/infographics/flow-cytometry-staining-protocols-for-high-quality-data-404722]
- 39. Protocol for in-plate staining of clinical peripheral blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12139499/]
- 40. High Content Screening: Flow Cytometry Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4476789/]
- 41. Ultra-high-scale cytometry-based cellular interaction ... [https://www.nature.com/articles/s41592-025-02744-w]
- 42. Fluorochrome Spillover Game [https://www.bdbiosciences.com/en-eu/learn/campaigns/flow-cytometry-dyes-performance/flow-cytometry-spillover]
- 43. Compensation in Flow Cytometry [https://fluorofinder.com/compensation-flow-cytometry/]
- 44. Flow Cytometry Color Matching Principles: Lesson 2 [https://www.elabscience.com/resources/flow-cytometry-experiment-guidelines-and-q&a/1860?srsltid=AfmBOoq-mpG7rglpXPTDT-1yplniwmk9GIuOxTtYdIAl7iqT3ijLaTCF]
- 45. How to choose fluorophore combinations for Flow Cytometry [https://www.bio-techne.com/resources/blogs/choose-fluorophore-combinations-for-flow-cytometry]
- 46. Cell-Based Screening Using High-Throughput Flow Cytometry [https://pmc.ncbi.nlm.nih.gov/articles/PMC3045571/]
- 47. Staining Triad: A fully automated and zero-waste flow ... [https://www.sciencedirect.com/science/article/pii/S2472630325001037]
- 48. Development of an automated 3D high content cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12380041/]
- 49. ImageXpress Pico Automated Cell Imaging System [https://www.moleculardevices.com/products/cellular-imaging-systems/high-content-imaging/imagexpress-pico]
- 50. Guidelines for the Presentation of Flow Cytometric Data [https://www.sciencedirect.com/science/article/abs/pii/S0091679X04750104]
- 51. Standardization procedure for flow cytometry data ... [https://www.nature.com/articles/s41598-020-68468-3]
- 52. Publishing flow cytometry data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2822558/]
- 53. Standardizing Flow Cytometry Immunophenotyping ... [https://www.nature.com/articles/srep20686]
- 54. Advanced immunophenotyping of lymphocyte and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1577206/full]
- 55. ICCS 2025 [https://cytometry.org/public-admin/mobile/show_presentation.php?abstractno=154]
- 56. Beyond the Limits: How Is Spectral Flow Cytometry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12248732/]
- 57. Quick Tips on Flow Cytometry Data Analysis [https://www.bdbiosciences.com/en-us/learn/science-thought-leadership/blogs/flow-cytometry-data-analysis-quick-tips]
- 58. How to Identify and Prevent Batch Effects in Longitudinal ... [https://cytekbio.com/blogs/blog/how-to-identify-and-prevent-batch-effects-in-longitudinal-flow-cytometry-research-studies]
- 59. Minimizing Batch Effects in Mass Cytometry Data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6803429/]
- 60. CytoNormPy Enables a Fast and Scalable Removal of ... [https://pubmed.ncbi.nlm.nih.gov/40879360/]
- 61. Flow Cytometry Reagents Market Size, Growth Demand & ... [https://www.consegicbusinessintelligence.com/flow-cytometry-reagents-market]
- 62. H62 | Validation of Assays Performed by Flow Cytometry [https://clsi.org/shop/standards/h62/]
- 63. AI in flow cytometry: Current applications and future ... [https://pubmed.ncbi.nlm.nih.gov/40985220/]
- 64. Flow Cytometry: An Overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5939936/]
- 65. How and in what situations should viability of specimens ... [https://www.cytometry.org/web/q_view.php?id=78&filter=Set-up%20and%20Validation%20of%20Flow%20Cytometry%20Panels]
- 66. BestProtocols: Viability Staining Protocol for Flow Cytometry [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/viability-staining-flow-cytometry.html]
- 67. Cleanet: Robust Doublet Detection in Cytometry Data Based ... [https://pubmed.ncbi.nlm.nih.gov/41065042/]
- 68. Flow Cytometry Antibody Titration Protocol [https://www.fn-test.com/news/product-news/flow-cytometry-antibody-titration-protocol/]
- 69. Titration of Antibody Protocol | Flow Cytometry Core | ECU [https://medicine.ecu.edu/flow-core/titration-of-antibody-protocol/]
- 70. Antibody Titration - Protocols - Flow Cytometry [https://sites.medschool.ucsd.edu/research/moores/shared-resources/flow-cytometry/protocols/Pages/antibody-titration.aspx]
- 71. Functional analysis of human circulating immune cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9010797/]
- 72. Panel Design [https://www.bdbiosciences.com/en-us/resources/panel-design]
- 73. Optimizing Your Immunophenotyping Assay [https://fluorofinder.com/immunophenotyping/]
- 74. Optimizing a Multi-colour Immunophenotyping Assay - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2034273/]
- 75. Recommended controls for flow cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/recommended-controls-for-flow-cytometry]
- 76. Protocols and Guidelines - McGovern Medical School [https://med.uth.edu/imm/flow-cytometry-services/protocols-and-guidelines/]
- 77. Flow-cytometry-based protocols for human blood/marrow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8517606/]
- 78. A Guide to Spectral Flow Cytometry Fluorophore Selection [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/flow-cytometry/flow-cytometry-learning-center/flow-cytometry-resource-library/flow-cytometry-methods/spectral-flow-cytometry-fluorophore-selection.html]
- 79. Standardisation of flow cytometry for whole blood ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0217163]
- 80. A machine learning framework for cross-institute ... [https://www.sciencedirect.com/science/article/pii/S0010482525007450]
- 81. An Introduction to Automated Flow Cytometry Gating Tools ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4515551/]
- 82. 31 Applying uncertainty analysis to assess the variation of ... [https://www.sciencedirect.com/science/article/pii/S1465324920300980]
- 83. Automated cytometric gating with human-level ... [https://www.nature.com/articles/s41467-025-56622-2]
- 84. Flow Cytometry Gating: Everything You Need to Know [https://nanocellect.com/blog/flow-cytometry-gating-everything-you-need-to-know/]
- 85. Separating Stem Cells By Flow Cytometry [https://pmc.ncbi.nlm.nih.gov/articles/PMC3076188/]
- 86. flowDensity: reproducing manual gating of flow cytometry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4325545/]
- 87. REDUCING VARIABILITY IN FLOW CYTOMETRY ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925003251]
- 88. A fully validated flow cytometry method to quantitatively ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708523002522]
- 89. Navigating the opportunities and challenges in analytical ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/3366/navigating-the-opportunities-and-challenges-in-analytical-development-of-flowcytometry-for-tcell-therapy]
- 90. Spectral Flow Cytometry: The Current State and Future of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193525/]
- 91. Comparative assessment of cytometry by time-of-flight and ... [https://www.sciencedirect.com/science/article/pii/S0022175924000267]
- 92. Spectral Flow and Mass Cytometry: Select the Right Platform [https://cellcarta.com/science-hub/spectral-flow-and-mass-cytometry/]
- 93. Performance of spectral flow cytometry and mass ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1191992/full]
- 94. Flow-cytometry-based protocols for human blood/marrow ... [https://www.sciencedirect.com/science/article/pii/S266616672100589X]
- 95. How high-throughput flow cytometry is transforming drug ... [https://www.drugdiscoverynews.com/how-high-throughput-flow-cytometry-is-transforming-drug-discovery-16312]
- 96. Guide to flowAI in OMIQ [https://www.omiq.ai/guides/flowai-cleaning-algorithms]
- 97. flowAI: automatic and interactive anomaly discerning tools ... [https://pubmed.ncbi.nlm.nih.gov/27153628/]
- 98. What is FlowSOM? [https://denovosoftware.com/faq/kb-what-is-flowsom/]
- 99. FlowSOM | FlowJo, LLC [https://www.flowjo.com/exchange/plugin/flowsom]
- 100. Spectral Panel Design [https://fluorofinder.com/spectral-panel-design-2/]