In Silico Mechanistic Modeling of the Immune Response to Burn Injuries: From Cellular Dynamics to Clinical Translation
This article provides a comprehensive overview of in silico mechanistic modeling approaches for deciphering the complex immune response following burn injuries.
In Silico Mechanistic Modeling of the Immune Response to Burn Injuries: From Cellular Dynamics to Clinical Translation
Abstract
This article provides a comprehensive overview of in silico mechanistic modeling approaches for deciphering the complex immune response following burn injuries. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of post-burn immunology, details cutting-edge computational methodologies like Agent-Based Models and neural networks, and addresses key challenges in model optimization and validation. By synthesizing recent scientific advances, this resource highlights how these computational tools can identify critical therapeutic targets, predict patient-specific outcomes, and ultimately guide the development of novel treatment strategies to improve burn care.
Decoding the Complexity of Post-Burn Immunology: The Foundation for In Silico Models
Severe burn injury triggers a complex and prolonged inflammatory cascade, characterized by a dynamic and often dysregulated immune response that evolves from acute to chronic phases [1]. This response is not a linear sequence but a unstable equilibrium between pro-inflammatory and anti-inflammatory forces, whose balance determines clinical outcomes such as sepsis, multiple organ dysfunction, and mortality [2]. The initial Systemic Inflammatory Response Syndrome (SIRS) is characterized by a massive release of pro-inflammatory mediators, which is subsequently counterbalanced by a Compensatory Anti-Inflammatory Response Syndrome (CARS) [1]. Advances in medical care have allowed patients to survive the initial acute phase, leading to the recognition of a persistent third phase known as Persistent Inflammation, Immunosuppression, and Catabolism Syndrome (PICS), which can last for months to years post-injury [1]. Understanding the temporal dynamics of this biphasic response is crucial for developing targeted immunomodulatory therapies and improving patient outcomes.
Characterizing the Phases: From Acute SIRS to Chronic PICS
Acute Inflammatory Phase (0-72 hours post-injury)
The acute phase initiates within hours of injury and is mediated by the innate immune system. Damage-associated molecular patterns (DAMPs) released from necrotic tissue, such as High Mobility Group Box 1 (HMGB1) and mitochondrial DNA, are recognized by Pattern Recognition Receptors (PRRs) on immune cells including macrophages and neutrophils [1] [3]. This recognition triggers the release of a storm of pro-inflammatory cytokines including interleukin (IL)-6, IL-8, IL-1β, tumor necrosis factor-α (TNF-α), and monocyte chemoattractant protein-1 (MCP-1) [2] [3]. These cytokines recruit additional immune cells to the site of injury and initiate the acute phase response, characterized by the liver production of C-reactive protein (CRP) and other acute phase proteins [2] [3]. The acute phase is a necessary response for tissue protection and initial repair; however, its excessive and persistent magnitude contributes to early complications such as distributive shock and organ failure [1] [4].
Chronic Inflammatory Phase (≥14 days post-injury)
Following the initial hyperinflammatory state, a prolonged phase of immune dysfunction ensues, now better defined as PICS [1]. This phase is marked by concurrent persistent inflammation, broad immunosuppression, and significant catabolism. A critical feature is a shift in adaptive immunity, characterized by suppressed T-helper 1 (Th1) responses, a shift towards Th2-type responses, T cell exhaustion, and increased activity of regulatory T cells (Tregs) [1]. Macrophages polarize toward an M2 phenotype, and the release of anti-inflammatory cytokines like IL-10 creates an environment susceptible to hospital-acquired infections [1] [4]. Recent research highlights the role of extracellular vesicles (EVs) in sustaining this chronic phase; EVs isolated late after burn injury carry an immunosuppressive protein cargo that reprograms macrophages toward an anti-inflammatory state, thereby perpetuating immune paralysis [4].
Table 1: Key Mediators in Post-Burn Inflammatory Phases
| Mediator Type | Specific Molecule | Acute Phase (0-72h) | Chronic Phase (≥14 days) | Primary Source |
|---|---|---|---|---|
| Pro-inflammatory Cytokines | IL-6 | Sharp increase, peaks 1-4 days [2] [3] | Can remain elevated for years [3] | Macrophages, neutrophils |
| IL-8 | Rapid increase in first 4 days [2] | Persists for several weeks [2] | Epithelial cells, macrophages | |
| TNF-α | Surge within 2.5 days [3] | Local persistence for weeks [3] | Macrophages, neutrophils | |
| IL-1β | Increases from day 1, peaks day 3 [2] [3] | — | Macrophages | |
| Anti-inflammatory Cytokines | IL-10 | Increases from day 1, peaks early [2] [3] | Gradual decrease over weeks [2] | M2 macrophages, T cells |
| Chemokines | MCP-1 | Early increase [2] | Correlates with mortality [2] | Endothelial cells, macrophages |
| Damage Signals | HMGB1 | Released from damaged tissue [1] | — | Necrotic cells |
| Acute Phase Proteins | C-reactive Protein (CRP) | Sharp increase, persists for months [2] | — | Liver |
Quantitative Biomarker Dynamics and Correlations with Outcomes
The systematic measurement of inflammatory mediators provides critical prognostic information and guides potential therapeutic interventions. Elevated levels of specific cytokines have been consistently correlated with adverse clinical outcomes. For instance, early increases in MCP-1, IL-6, IL-8, and IL-10 are significantly correlated with 28-day mortality [2]. Furthermore, a meta-analysis has confirmed that an elevated admission Neutrophil-to-Lymphocyte Ratio (NLR) is an independent predictor of mortality in burn patients [2].
The dynamic nature of these biomarkers is evident in their temporal patterns. IL-6 increases sharply within the first 1-4 days post-burn and can remain elevated for months or even years, with levels correlating with the percentage of total body surface area (TBSA) burned [3]. Non-survivors often present with significantly higher plasma IL-6 levels on the day of injury compared to survivors [3]. Similarly, IL-8 serum levels can be dramatically elevated—up to 2000-fold compared to healthy controls [3]. Anti-inflammatory mediators like IL-10 peak on the first day post-burn and gradually decrease, with the highest concentrations correlating with both TBSA and the development of sepsis [3].
Table 2: Biomarker Associations with Clinical Outcomes in Burn Patients
| Biomarker | Correlation with Injury Severity | Association with Mortality | Association with Sepsis/Infection | Other Clinical Outcomes |
|---|---|---|---|---|
| IL-6 | Correlates with %TBSA and depth [3] | Higher in non-survivors [3] | — | Stimulates acute phase proteins, angiogenesis [3] |
| IL-8 | — | — | — | Neutrophil recruitment, tissue remodeling [3] |
| IL-10 | Correlates with %TBSA [3] | Levels >60 pg/ml distinguish survivors/non-survivors [5] | Higher in septic vs. non-septic patients [3] | — |
| MCP-1 | Correlates with burn severity [3] | Higher in non-survivors on day 1 [2] [3] | — | Recruits monocytes to injury site [3] |
| NLR | — | Independent predictor of mortality [2] | — | Systemic inflammation index [2] |
| HMGB1 | Positive correlation with injury size (murine model) [3] | — | — | DAMP signaling via TLR4 [1] |
Experimental Protocols for Immune Monitoring
Protocol 1: Longitudinal Cytokine Profiling in Human Plasma
Objective: To quantitatively measure the dynamic changes in pro- and anti-inflammatory cytokine levels in burn patient plasma over time, from the acute phase through the chronic phase.
Materials and Reagents:
- Sodium Heparin Tubes: For blood collection and plasma separation.
- Multiplex Bead-Based Immunoassay Kit: Validated for human cytokines (e.g., IL-6, IL-8, IL-10, TNF-α, MCP-1, IL-1β).
- Luminex Platform or ELISA Plate Reader: For signal detection and quantification.
- Recombinant Cytokine Standards: For generating standard curves.
Methodology:
- Sample Collection: Collect venous blood from severe burn patients (e.g., >20% TBSA) at predetermined time points: admission (<6h), 24h, 72h, 7 days, 14 days, and 30 days post-injury. Process samples within 1 hour by centrifugation at 2,000 x g for 15 minutes to isolate plasma. Store aliquots at -80°C.
- Assay Procedure:
- Thaw plasma samples on ice and clarify by high-speed centrifugation (10,000 x g for 10 minutes) to remove particulates.
- Follow the manufacturer's protocol for the multiplex immunoassay. Briefly, add standards and samples to the bead plate in duplicate.
- Incubate, wash, then add biotinylated detection antibodies.
- After another incubation and wash, add streptavidin-PE, then read on the Luminex analyzer.
- Data Analysis: Use software to calculate cytokine concentrations from standard curves. Perform statistical analysis (e.g., ANOVA with post-hoc tests) to compare levels across time points and correlate with clinical outcomes (e.g., sepsis, mortality) using logistic regression models.
Protocol 2: Isolation and Proteomic Analysis of Immunomodulatory Extracellular Vesicles (EVs)
Objective: To isolate EVs from patient plasma at different post-burn phases and characterize their protein cargo to understand their role in immune reprogramming.
Materials and Reagents:
- Differential Centrifugation Equipment: Ultracentrifuge and fixed-angle rotors.
- Phosphate-Buffered Saline (PBS), Filtered (0.22 µm): For EV washing and resuspension.
- Nanoparticle Tracking Analysis (NTA) Instrument: e.g., ZetaView QUATT, for EV quantification and sizing.
- Mass Spectrometry-Grade Reagents: For proteomic sample preparation (e.g., trypsin, RIPA buffer, protease inhibitors).
Methodology:
- EV Isolation from Plasma:
- Centrifuge plasma at 2,000 x g for 20 minutes to remove cells.
- Transfer supernatant and centrifuge at 10,000 x g for 30 minutes to remove cell debris.
- Ultracentrifuge the resulting supernatant at 21,000 x g for 1 hour at 4°C to pellet EVs.
- Wash the pellet in filtered PBS and repeat the ultracentrifugation step.
- Resuspend the final EV pellet in 100-200 µL of saline and filter through a 0.22 µm syringe filter. Store at -80°C [4].
- EV Characterization: Dilute an aliquot of EVs in filtered PBS and analyze using NTA to determine particle concentration (particles/mL) and mode size (nm).
- Proteomic Analysis:
- Lyse EVs in RIPA buffer with protease inhibitors.
- Digest proteins using trypsin and desalt the resulting peptides.
- Analyze peptides by liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS).
- Identify proteins and perform pathway analysis using bioinformatics tools (e.g., Gene Ontology, KEGG) to identify enriched biological processes in early vs. late EVs.
In Silico Modeling of Post-Burn Inflammation
Computational models have emerged as powerful tools to decipher the complexity of the post-burn immune response, offering a platform for hypothesis testing and in silico experimentation.
Agent-Based Modeling (ABM) of Acute Inflammation
Objective: To develop a spatio-temporal model simulating cellular interactions and cytokine dynamics in the first 0-4 days post-burn.
Model Framework: The Glazier-Graner-Hogeweg (GGH) model, a type of ABM, can be implemented using CompuCell3D software [6] [7]. The simulation domain is separated into blood and tissue compartments.
Model Components:
- Agents (Cells): Model key immune cells as independent agents, including mast cells, neutrophils, and macrophages. Each agent is motile and exhibits chemotaxis based on concentration gradients of solutes [6].
- Solutes (Signaling Molecules): Define pro-inflammatory cytokines (e.g., IL-6, TNF-α), anti-inflammatory cytokines (e.g., IL-10), and inflammation-triggering factors (e.g., DAMPs). Solutes diffuse throughout the domain based on their concentration profiles [6].
- Rules and Interactions: Program behavioral rules for agents. For example, neutrophils are recruited to the tissue compartment by gradients of IL-8; activated macrophages secrete pro-inflammatory cytokines; endothelial cells express adhesion molecules.
Simulation and Output: The model tracks changes in cell counts and cytokine levels over time and space. A key finding from such models is the identification of the initial endothelial cell count as a pivotal parameter determining the intensity and progression of acute inflammation [6] [8].
Physics-Informed Neural Networks (PINNs) for Cytokine Prediction
Objective: To create a surrogate model that approximates and forecasts cytokine concentration dynamics from ABM simulations with lower computational cost.
Workflow:
- Data Generation: Run multiple simulations of the baseline ABM to generate extensive spatio-temporal data on cytokine concentrations.
- Data Preprocessing: Clean the data and transform it into a suitable format for neural network training, such as a time-series dataset with spatial grids.
- Model Training: Implement and train a Spatio-Temporal Attention Long Short-Term Memory (STA-LSTM) neural network. This architecture is designed to capture both temporal dependencies and spatial relationships in the cytokine data. The model is evaluated using metrics like Mean Squared Error and R-squared [7].
- Prediction: Use the trained STA-LSTM model to predict cytokine concentrations over time and space under different initial conditions, providing a rapid forecasting tool.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Post-Burn Immunity
| Reagent / Material | Function / Application | Specific Example / Target |
|---|---|---|
| Multiplex Cytokine Panels | Simultaneous quantification of multiple cytokines in serum/plasma. | IL-6, IL-8, IL-10, TNF-α, MCP-1, IL-1β [2] [3] |
| Anti-HMGB1 Antibodies | Detection and inhibition of DAMP signaling. | Neutralizing HMGB1 to study its role via TLR4 [1] [3] |
| Luminex/xMAP Technology | High-throughput, multiplexed immunoassay platform. | Profiling cytokine kinetics from minimal sample volume [3] |
| EV Isolation Kits | Purification of exosomes and microvesicles from biofluids. | Differential centrifugation for plasma EV isolation [4] |
| NTA Instrumentation | Characterization of EV size and concentration. | ZetaView QUATT system [4] |
| CompuCell3D Software | Platform for GGH/ABM model implementation. | Simulating immune cell migration and interaction [6] [7] |
| Primary Cell Cultures | In vitro validation of immune cell functions. | Human THP-1 macrophages for EV stimulation assays [4] |
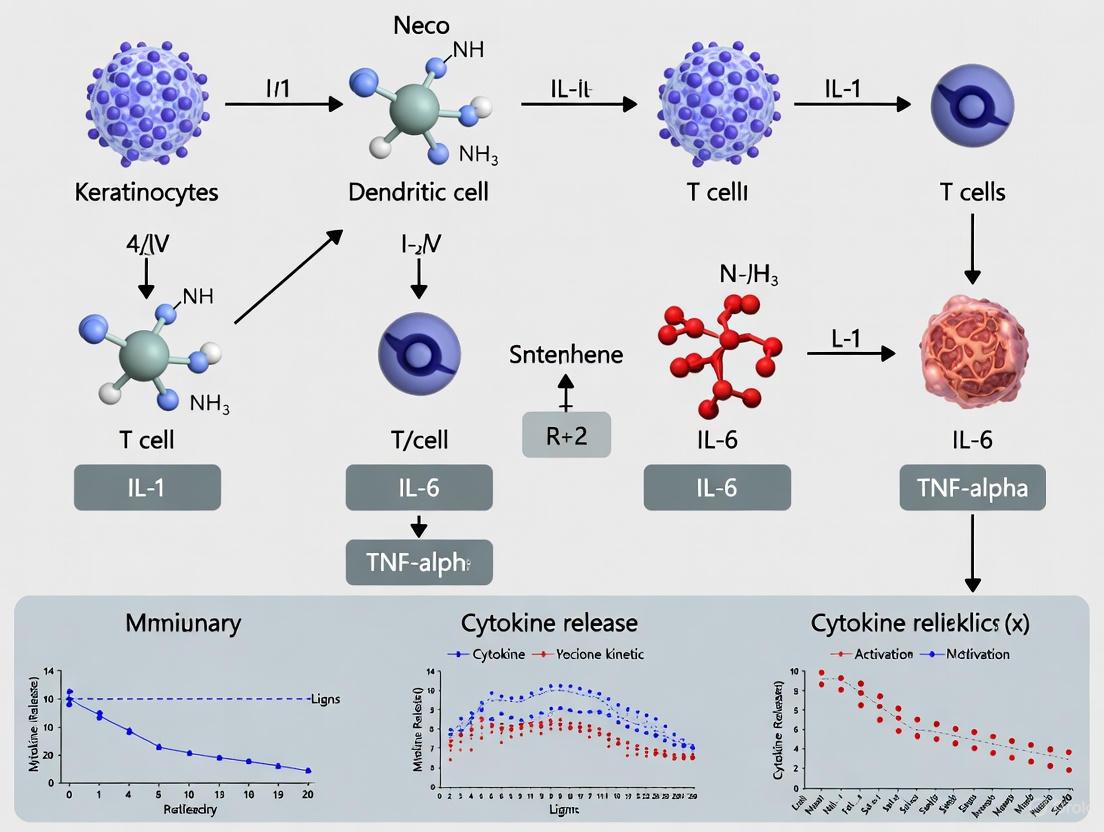
Signaling Pathways and Conceptual Workflows
The following diagrams, generated using Graphviz DOT language, illustrate key signaling pathways and experimental workflows central to post-burn immune research.
The immune response to burn injury is a carefully orchestrated process involving complex interactions between various cellular players. Among these, neutrophils, macrophages, and endothelial cells emerge as critical regulators that coordinate the transition from inflammation to tissue repair. Understanding the precise roles and interactions of these cells provides valuable insights for developing targeted therapeutic strategies and building accurate in silico models of burn pathophysiology.
This application note synthesizes current research findings to detail the specific functions, activation mechanisms, and temporal dynamics of these key cellular players during burn immune responses. We further provide detailed experimental protocols for investigating their roles and visualize critical signaling pathways to support mechanistic modeling efforts.
Quantitative Profiles of Key Cellular Players
The following tables summarize quantitative data and temporal dynamics for neutrophils, macrophages, and endothelial cells in burn injury responses, providing essential parameters for computational modeling.
Table 1: Temporal Dynamics and Key Functions of Cellular Players in Burn Injury
| Cell Type | Key Functions in Burn Response | Peak Activation Time | Phenotypic Markers |
|---|---|---|---|
| Neutrophils | First responders; phagocytosis; release of TNF-α, IL-1β, IL-6; matrix production; bacterial clearance [2] [9] | Immediate surge, persistent for weeks [9] | CD15⁺; MPO⁺ [9] |
| Macrophages | Phagocytosis; debris clearance; phenotype transition (M1→M2); release of cytokines & growth factors; tissue repair [6] [10] | M1: Days 1-3; M2: Days 3+ [6] [10] | M1: CD68⁺, CD86⁺; M2: CD206⁺ [10] [11] |
| Endothelial Cells | Initiate inflammatory response; express adhesion molecules & chemokines; recruit immune cells; angiogenesis [6] | Early responder (0-4 days post-burn) [6] | N/A |
Table 2: Secretory Profile and Associated Experimental Models
| Cell Type | Key Secretory Products | Primary Experimental Models | Computational Modeling Considerations |
|---|---|---|---|
| Neutrophils | TNF-α, IL-1β, IL-6, IL-8, collagen, matrix proteins [2] [12] | Human burn eschar analysis [9], murine models [12] | Prolonged presence vs. normal healing; matrix production function |
| Macrophages | M1: IL-1β, TNF-α, iNOS; M2: IL-4, IL-13, EGF, bFGF, VEGF [10] | THP-1 cell line, RAW 264.7 cells, murine burn models [10] [11] [13] | Response to mechanical stretch; non-monotonic input-output relationships |
| Endothelial Cells | Adhesion molecules, chemokines (e.g., IL-8) [6] | In silico modeling (GGH method) [6] | Pivotal parameter for model intensity; initial cell count is crucial |
Detailed Cellular Mechanisms and Functions
Neutrophils: First Responders and Barrier Strengtheners
Neutrophils are the first immune cells recruited to the burn site, showing an immediate and strong increase that persists for weeks, unlike the transient response observed in normal wound healing [9]. Their classical functions include phagocytosing microbes and necrotic cells, and releasing pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 to attract monocytes and macrophages [2].
Recent research has revealed a previously unexpected function of neutrophils: producing collagen and other matrix proteins that strengthen the skin barrier [12]. This specialized population of skin-resident neutrophils helps maintain skin resistance and integrity under normal conditions and is activated in response to injury to generate protective structures around wounds that prevent bacterial entry [12]. Their activity follows a day-night pattern, adjusting extracellular matrix production according to the body's circadian cycle, resulting in higher skin resistance at night [12].
Macrophages: Dynamic Regulators of Inflammation and Repair
Macrophages play pivotal roles throughout all stages of burn wound healing, demonstrating remarkable plasticity [10]. Following injury, pro-inflammatory M1 macrophages are recruited to the wound site to release cytokines (IL-1β, TNF-α) and facilitate clearance of bacteria and deceased cells [10]. As tissue repair commences, the macrophage population undergoes a critical transition toward an anti-inflammatory M2 phenotype, which releases anti-inflammatory cytokines (IL-4, IL-13) and growth factors (EGF, bFGF, VEGF) that support tissue regeneration [10].
Macrophages exhibit a non-monotonic response to mechanical stretch across different amplitudes (7%-21%), with 15% stretch promoting optimal M2 polarization, enhanced release of anti-inflammatory factors, and activation of YAP/TAZ mechanotransduction pathways [10]. This mechanical responsiveness highlights how physical cues in the wound environment can shape immune function.
Therapeutic strategies can target macrophage polarization. For instance, Isosteviol has been shown to upregulate MMP-9 in macrophages, leading to M2 polarization and reduced levels of pro-inflammatory cytokines IL-2 and TNF-α [13]. Similarly, Lyophilized Horizontal Platelet Rich Fibrin (Ly-H-PRF) reduces LPS-induced macrophage M1 polarization while promoting M2 polarization [11].
Endothelial Cells: Orchestrators of Immune Cell Recruitment
Endothelial cells are among the first responders at the site of burn damage and play a crucial role in initiating and balancing the inflammatory response [6]. Among their primary functions, they initiate the inflammatory response during the acute phase by expressing adhesion molecules and chemokines, thereby facilitating the recruitment of immune cells such as neutrophils and monocytes to the wound area [6].
In silico modeling approaches have highlighted the pivotal role of the initial endothelial cell count as a key parameter determining the intensity and progression of acute inflammation during the critical 0-4 days post-burn period [6] [8]. These models separate the simulation domain into blood and tissue compartments, with endothelial cells mediating the critical interactions between these compartments.
Experimental Protocols for Cellular Analysis
Protocol 1: Immune Cell Isolation from Burn Wound Tissue (Eschar)
This protocol adapts the methodology used by Mulder et al. (2022) for isolating viable immune cells from human burn wound tissue for flow cytometric analysis [9].
Reagents and Materials:
- RPMI 1640 medium with 1% penicillin/streptomycin
- Collagenase I (80 mg/mL in PBS)
- FCM buffer (PBS with 1% BSA, 0.05% sodium azide, and 1 mM EDTA)
- Erythrocyte lysis buffer (1.5 mM NH₄Cl, 0.1 mM NaHCO₃, 0.01 mM EDTA)
- C-tubes (Miltenyi Biotec)
- Cell strainers (500 µm and 40 µm)
- gentleMACS Dissociator (Miltenyi Biotec) or similar tissue dissociator
Procedure:
- Sample Collection: Collect burn wound tissue (eschar) during surgical debridement and store in RPMI 1640 with antibiotics at 4°C overnight.
- Tissue Processing: Take approximately 600 mg of tissue from viable areas (white or red with bleeding spots). Cut into small pieces and distribute into 2 C-tubes, each containing 5 mL of RPMI 1640 with antibiotics.
- Mechanical Dissociation: Place C-tubes on gentleMACS dissociator and run program "B" for initial dissociation.
- Enzymatic Digestion: Add 150 µL of collagenase I solution (80 mg/mL) to each tube. Incubate in a shaking water bath at 37°C for 1 hour.
- Secondary Dissociation: Return tubes to dissociator and run program "B" again.
- Cell Strainer Filtration: Pass the cell suspension sequentially through 500 µm and 40 µm cell strainers.
- Erythrocyte Lysis: Centrifuge at 450 × g for 10 minutes, discard supernatant. Resuspend pellet in erythrocyte lysis buffer for 10 minutes at room temperature.
- Cell Washing: Add 20 mL FCM buffer and centrifuge at 450 × g for 10 minutes.
- Cell Counting: Resuspend in 5 mL FACS buffer and count cells using a flow cytometer or hemocytometer.
Applications: This protocol enables subsequent flow cytometric analysis of immune cell populations, including neutrophil maturity assessment, macrophage polarization status, and lymphocyte subtyping.
Protocol 2: Macrophage Stretch Assay for Mechanobiological Studies
This protocol describes the application of static mechanical stretch to macrophages in vitro to study how mechanical cues in the wound environment influence their phenotype, based on the methods of Wang et al. (2025) [10].
Reagents and Materials:
- THP-1 human monocytic cell line or primary human monocytes
- PMA (phorbol 12-myristate 13-acetate) for THP-1 differentiation
- Flexible-bottom 6-well culture plates (precoated with type I collagen)
- Custom cell-stretching device (vacuum pump, pressure reservoir, negative pressure controller)
- Macrophage polarization markers: anti-CD68, CD86, CD206 antibodies
Procedure:
- Macrophage Differentiation: Seed THP-1 cells at 2×10⁵ cells/well in flexible-bottom plates. Differentiate into macrophages using 100 ng/mL PMA for 48 hours.
- Cell Stretching: Culture differentiated macrophages for 12 hours to allow attachment. Apply static mechanical stretch at desired amplitudes (7%, 15%, 21%) for 24 hours using the stretching device.
- Conditioned Medium Collection: Collect conditioned medium (MS-CM) from stretched macrophages and control (unstretched) macrophages. Centrifuge at 500 × g for 10 minutes, then at 2000 × g for 5 minutes to remove cells and debris.
- Flow Cytometric Analysis: Analyze macrophage polarization using fluorescence-conjugated antibodies against CD68 (pan-macrophage), CD86 (M1 marker), and CD206 (M2 marker).
- Functional Assays: Apply MS-CM to keratinocytes, fibroblasts, or endotheliocytes to assess paracrine effects on migration, proliferation, and tube formation.
Applications: This assay enables investigation of how mechanical forces in the wound environment influence macrophage polarization and subsequent paracrine signaling to other skin cells involved in tissue repair.
Signaling Pathways and Experimental Workflows
Macrophage Polarization Signaling Pathway
The following diagram illustrates key signaling pathways involved in macrophage polarization in response to burn injury and mechanical stimuli, integrating findings from multiple studies [10] [13]:
Experimental Workflow for Burn Immune Response Studies
This workflow diagrams the integrated experimental approach for studying cellular immune responses to burn injury, from sample processing to computational modeling:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Studying Burn Immune Responses
| Reagent/Category | Specific Examples | Research Application | Key References |
|---|---|---|---|
| Cell Culture Models | THP-1 human monocytic cell line, RAW 264.7 murine macrophages, primary HUVECs | In vitro mechanistic studies of immune cell function | [10] [11] |
| Macrophage Polarization Reagents | PMA (for THP-1 differentiation), LPS (M1 polarization), IL-4/IL-13 (M2 polarization) | Directing macrophage phenotype for functional assays | [10] [11] |
| Flow Cytometry Antibodies | Anti-human: CD14, CD16, CD45, CD3, CD15, CD68, CD86, CD206 | Immune cell phenotyping and polarization assessment | [9] [10] |
| Mechanical Stretch Equipment | Flexible-bottom culture plates, vacuum pump systems, pressure controllers | Studying mechanobiology of immune cells in wound environment | [10] |
| Cytokine Analysis Kits | Multiplex cytokine arrays (IL-1β, TNF-α, IL-6, IL-8, IL-10, VEGF etc.) | Secretome profiling of immune cells and tissue explants | [9] [3] |
| Computational Modeling Tools | Glazier-Graner-Hogeweg (GGH) method, Agent-based modeling (ABM) platforms | In silico simulation of immune dynamics | [6] [8] |
The coordinated functions of neutrophils, macrophages, and endothelial cells create a complex network that drives the immune response to burn injury. For in silico modeling, each cell type presents specific parameters critical for accurate simulation: the prolonged presence and matrix-producing functions of neutrophils; the phenotypic plasticity and mechanoresponsiveness of macrophages; and the orchestrating role of endothelial cells in initial immune cell recruitment.
The experimental protocols and signaling pathways detailed in this application note provide a framework for generating quantitative data to parameterize computational models. Future modeling efforts should particularly focus on the non-linear relationships between mechanical stimuli and macrophage polarization, the circadian regulation of neutrophil function, and the feedback loops between endothelial cell activation and immune cell infiltration. Such integrated experimental-computational approaches will accelerate the development of targeted interventions to modulate burn immune responses for improved patient outcomes.
Severe burn injuries trigger a complex and dynamic immune response that originates locally but rapidly progresses to a systemic inflammatory state, often culminating in single or multiple organ dysfunction syndrome (MODS). This application note synthesizes current clinical and computational research to outline the pathophysiological mechanisms and key biomarkers linking local burn trauma to remote organ failure. We provide structured experimental protocols and in silico modeling approaches to aid researchers in investigating these critical pathways and developing targeted therapeutic interventions.
Severe burn trauma initiates a profound systemic stress response characterized by a massive, and often prolonged, release of inflammatory mediators. Unlike other forms of trauma, this inflammatory state can persist for months post-injury, creating a unique clinical challenge [14]. The initial local destruction of tissue releases damage-associated molecular patterns (DAMPs), which activate both local and systemic immune cells, triggering a cytokine storm. This response is not a linear sequence but a dynamic and unstable equilibrium between pro- and anti-inflammatory forces, where the persistence of dysregulation, rather than the initial cytokine magnitude, often determines patient outcomes [15]. The failure to re-establish homeostasis leads to a catabolic, hypermetabolic state that can destroy host tissue and propagate organ injury far from the original burn site [14].
The transition from local injury to systemic complication is a critical focus for both clinical management and pharmaceutical development. Understanding the precise mechanisms and timing of organ failure is essential for risk stratification and the design of effective anti-inflammatory and pro-resolving therapies.
Key Pathophysiological Pathways and Clinical Evidence
The Mediators of Systemic Inflammation
The systemic inflammatory response is driven by a complex network of soluble mediators and cellular actors. Pro-inflammatory cytokines such as IL-6, IL-8, TNF-α, and IL-1β are released early and in abundance, while anti-inflammatory mediators like IL-10 attempt to counterbalance this response [15] [6]. The failure of these compensatory anti-inflammatory mechanisms is a key factor in the progression to organ dysfunction [15]. Furthermore, acute-phase proteins and complement fragments contribute to the widespread endothelial damage and microvascular hyperpermeability that underlies distributive shock and organ hypoperfusion [15] [16].
Table 1: Key Inflammatory Mediators in Post-Burn Systemic Complications
| Mediator Type | Key Examples | Primary Source | Role in Systemic Complications & Organ Dysfunction |
|---|---|---|---|
| Pro-inflammatory Cytokines | IL-6, IL-8, TNF-α, IL-1β | Immune cells (e.g., macrophages, neutrophils) | Drive hypermetabolism, fever, acute phase response; induce endothelial dysfunction and direct tissue injury [15] [6]. |
| Anti-inflammatory Cytokines | IL-10 | Immune cells (e.g., M2 macrophages) | Counteracts pro-inflammatory response; failure is associated with poor outcomes and persistent inflammation [15]. |
| Acute Phase Proteins | C-Reactive Protein (CRP) | Liver | Marker of systemic inflammation; contributes to opsonization and complement activation [15]. |
| Damage-Associated Molecular Patterns (DAMPs) | HMGB1, Heat Shock Proteins | Damaged/necrotic cells | Trigger initial immune activation via pattern recognition receptors (e.g., TLRs), perpetuating the cytokine storm [6]. |
Temporal Patterns of Organ Failure
Clinical studies have revealed that organ failure post-burn follows a distinct and predictable temporal pattern, which has critical implications for monitoring and intervention strategies.
Table 2: Temporal Patterns of Organ Failure Following Major Burn Injury
| Organ System | Incidence & Onset | Key Clinical Associations |
|---|---|---|
| Cardiac | Highest incidence throughout acute hospital stay [17]. | Associated with cardiomyocyte apoptosis, dilative cardiomyopathy, and toxic agents [17]. |
| Respiratory | Highest incidence in the early phase; decreases starting ~5 days post-burn [17]. | Strongly linked to inhalation injury and ventilator-associated pneumonia (VAP) [15] [17]. |
| Hepatic | Incidence increases with the length of hospital stay; high mortality in the late phase [17]. | Linked to the hypermetabolic response, vast catabolism, and drug-induced toxicity [17]. |
| Renal | Lower incidence but associated with very high mortality, especially in the first 3 weeks [17]. | Results from initial trauma, myoglobinuria, and inappropriate fluid resuscitation [17]. |
| Hematologic | Very common (up to 68.6%) in major burns, often occurring early (<5 days) [16]. | A frequent component of early multiple organ dysfunction syndrome (MODS) [16]. |
The failure of three or more organs is associated with a very high mortality rate, underscoring the critical need for early prediction and prevention [17].
Predictive Clinical Factors for Organ Dysfunction
Identifying patients at highest risk for MODS enables targeted, intensive care. Large-scale clinical studies have consistently identified several key risk factors.
Table 3: Clinical Predictors of Multiple Organ Dysfunction Syndrome (MODS) after Severe Burns
| Predictor | Association with MODS | Clinical Evidence |
|---|---|---|
| Total Body Surface Area (TBSA) | Strong, independent predictor. A TBSA ≥55% significantly increases risk [16]. | Odds Ratio (OR): 3.83; 95% CI: 1.29–11.37 for early MODS [16]. |
| Inhalation Injury | Strong, independent predictor, particularly for early-onset MODS (within 3 days) [18]. | Significantly increases incidence of MOF (57% vs. 29% without) [17]. |
| Hypoalbuminemia | Independent predictor. Serum albumin <2.1 g/dL upon admission is a significant risk factor [16]. | OR: 3.43; 95% CI: 1.01–11.57 for early MODS [16]. |
| Advanced Age | Independent predictor of MODS in adult populations [18]. | Associated with increased mortality and morbidity [14]. |
| Elevated Lactate & Denver Score | Predictive of late-onset MODS (after 3 days) [18]. | Indicates tissue hypoperfusion and established organ stress [18]. |
In Silico Modeling of the Post-Burn Immune Response
Computational models provide a powerful platform for investigating the complex, non-linear dynamics of the immune response to burns without the ethical and practical constraints of purely clinical or animal studies.
Agent-Based Modeling (ABM) of Acute Inflammation
The Glazier-Graner-Hogeweg (GGH) method, a type of Agent-Based Model, simulates the behavior and interactions of individual cells (agents) within a defined spatial environment [6] [8]. In a typical model setup, the domain is separated into blood and tissue compartments. Key cellular agents include mast cells, neutrophils, and macrophages, while solutes comprise pro- and anti-inflammatory cytokines and DAMPs [6]. These agents interact based on rules derived from experimental data, such as secreting cytokines and exhibiting chemotaxis along concentration gradients.
Simulations from day 0 to 4 post-burn have identified the initial endothelial cell count as a pivotal parameter determining the intensity and progression of acute inflammation [6] [8]. Endothelial cells are among the first responders, initiating the inflammatory response by expressing adhesion molecules and chemokines that recruit immune cells to the site of injury and systemically [6].
Diagram 1: From Local Burn to Systemic Organ Dysfunction. This pathway illustrates the key steps through which a local burn injury propagates to cause remote organ failure, highlighting the central role of endothelial activation.
Neural Networks as Surrogate Models
While ABMs are highly detailed, they are computationally intensive. To address this, surrogate neural network (NN) models are being developed to approximate ABM simulations, enabling faster predictions of cytokine dynamics over time and space [7]. Architectures like STA-LSTM (Spatio-Temporal Attention Long Short-Term Memory) have demonstrated superior performance in capturing the temporal and spatial dependencies of cytokine concentrations, outperforming other models in statistical metrics such as Mean Squared Error and R-squared [7]. Physics-Informed Neural Networks (PINNs) also show promise by incorporating physical laws governing cytokine diffusion and cell interaction, improving the biological plausibility of predictions [7].
Experimental Protocols and Research Tools
Protocol: Electrical Impedance Spectroscopy for Assessing Red Blood Cell Damage
This protocol quantifies the degree of systemic burn injury by measuring the electrical impedance of blood, which changes with the proportion of damaged (heated) red blood cells (HRBCs) [19].
1. Sample Preparation:
- Collect whole blood (e.g., swine model) within 12 hours of draw, using trisodium citrate (3.28%) as an anticoagulant (1:9 ratio).
- To mimic varying degrees of burn injury, centrifuge separate aliquots at 2000× g for 30 min to isolate plasma, RBCs, and heated RBCs (HRBCs).
- Create HRBCs by incubating whole blood in a thermostatic water bath at 55°C for 1 hour before centrifugation.
- Mix plasma with RBCs and HRBCs in different proportions (e.g., HCT from 20% to 80%; HHCT from 0% to 40%) to create experimental samples simulating different injury severities.
2. Impedance Measurement:
- Use an impedance analyzer (e.g., Hioki IM7581) with a fixture and a custom cuvette with copper electrodes (e.g., 10mm x 20mm, 2mm gap).
- Load the sample into the cuvette and measure electrical impedance across a frequency sweep from 100 kHz to 300 MHz with an applied current of 10 mA.
- Perform all measurements under controlled room temperature (e.g., 25°C).
3. Data Analysis:
- Plot Nyquist plots (imaginary vs. real impedance) for each sample.
- Extract the characteristic frequency (f~c~) and the corresponding imaginary part of the impedance (Z~Imt~) at the peak of the plot.
- Correlate Z~Imt~ with the HHCT. A linear relationship is expected: Z~Imt~ = -2.56 HHCT - 2.01 (R² = 0.96) [19].
- Alternatively, fit the data to a seven-parameter equivalent circuit model and extract the plasma resistance (R~p~), which also correlates linearly with HHCT [19].
Protocol: Cytokine Profiling for Predicting Organ Failure
Monitoring the dynamic changes in cytokine levels is crucial for understanding the systemic inflammatory state.
1. Sample Collection:
- Collect blood from burn patients at standardized time points: admission, pre-operatively, and then serially post-operatively (e.g., every 5 days for 4 weeks) [17].
- Draw blood into serum-separator tubes and centrifuge for 10 minutes at 1320 rpm.
- Aliquot the serum and store at -70°C until assayed.
2. Multiplex Immunoassay:
- Use a multiplex bead-based array system (e.g., Bio-Plex Human Cytokine 17-Plex panel on a Bio-Plex Suspension Array System).
- Following the manufacturer's protocol, incubate serum samples with antibody-conjugated magnetic beads.
- After washing, detect bound cytokines using a biotinylated detection antibody and a streptavidin-phycoerythrin conjugate.
- Measure fluorescence and calculate cytokine concentrations from standard curves.
3. Data Interpretation:
- Analyze the trajectory of key cytokines (e.g., IL-6, IL-8, TNF-α, IL-10) rather than single time-point measurements.
- Correlate persistent elevations or specific ratios of pro- to anti-inflammatory cytokines with the development of sepsis, ventilator-associated pneumonia (VAP), or organ dysfunction [15].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Investigating Post-Burn Systemic Complications
| Reagent / Material | Function and Application in Burn Research |
|---|---|
| Multiplex Cytokine Panels (e.g., Bio-Plex Human Cytokine Panels) | Simultaneous quantification of a broad spectrum of pro- and anti-inflammatory cytokines (e.g., IL-6, IL-8, TNF-α, IL-10) from serum/plasma to profile the systemic inflammatory state [17]. |
| Electrical Impedance Analyzer | Quantitative assessment of red blood cell damage (a marker of systemic injury) by measuring the impedance characteristics of blood samples; used to calculate the proportion of heated red blood cells (HHCT) [19]. |
| Cell Culture Models (Endothelial Cells) | In vitro investigation of the pivotal role of endothelial cells in initiating inflammation, expressing adhesion molecules, recruiting immune cells, and regulating vascular permeability [6]. |
| DENVER2 Score Criteria | Validated clinical tool for prospective, daily monitoring of organ-specific function (cardiac, respiratory, hepatic, renal) in burn patients to define and track single or multiple organ failure [17]. |
| CompuCell3D Software | A flexible modeling environment for developing Glazier-Graner-Hogeweg (GGH) method-based agent-based models (ABM) to simulate spatial-temporal dynamics of the immune response to burns [6] [7]. |
Diagram 2: In Silico Research Workflow. This diagram outlines the iterative cycle of using computational models to generate and leverage biological data for predicting patient outcomes.
The link between local burn injury and remote organ dysfunction is mediated by a persistent, dysregulated systemic inflammatory response. Clinical risk factors such as large TBSA, inhalation injury, and early hypoalbuminemia provide actionable criteria for identifying high-risk patients. The integration of clinical monitoring with advanced research techniques—from electrical impedance spectroscopy to cytokine profiling—and sophisticated in silico models offers a powerful, multi-faceted approach to deconstruct this complexity. By applying these detailed protocols and computational frameworks, researchers and drug developers can gain deeper mechanistic insights and accelerate the development of therapies aimed at modulating the immune response to improve survival and long-term outcomes for burn patients.
Burn injuries trigger a complex and prolonged immune response that remains challenging to fully understand and treat through experimental methods alone. The massive, persistent inflammation can negatively affect wound healing and lead to multiple organ dysfunction [6]. The intricate spatial and temporal interactions between various immune cells, cytokines, and tissue components create a highly dynamic system that is difficult to analyze with traditional approaches. Computational modeling has emerged as a powerful tool to bridge this knowledge gap, providing a framework to simulate, analyze, and predict the behavior of the post-burn immune system in ways that laboratory experiments cannot [6] [7]. These in silico approaches enable researchers to uncover underlying mechanisms, test hypotheses in a controlled environment, and identify key intervention points for therapeutic development, ultimately accelerating progress in burn care.
Current Computational Approaches in Burn Research
Agent-Based Modeling (ABM) of Immune Dynamics
Agent-based modeling, particularly the Glazier-Graner-Hogeweg (GGH) method, also known as the Cellular Potts Model (CPM), has proven valuable for capturing the complexities of post-burn inflammation [6]. This approach simulates individual cells as independent agents that interact within defined biological compartments:
- Spatial Organization: Models typically separate the simulation domain into blood and tissue compartments, each containing solutes and cell agents [6]
- Cellular Agents: Include mast cells, neutrophils, and macrophages that are motile and exhibit chemotaxis based on concentration gradients of solutes [6]
- Molecular Components: Comprise pro-inflammatory cytokines, anti-inflammatory cytokines, and inflammation-triggering factors that diffuse throughout the domain [6]
Through simulations spanning days 0-4 post-burn, ABM has successfully identified the initial endothelial cell count as a pivotal parameter determining inflammation intensity and progression [6] [8]. This finding highlights how computational approaches can reveal key biological insights that might be overlooked in conventional studies.
Neural Network Surrogates for Enhanced Prediction
While ABMs provide detailed mechanistic insights, they are computationally intensive. Recent research has explored neural networks as surrogate models to approximate and forecast ABM simulation results:
- STA-LSTM (Spatio-Temporal Attention Long Short-Term Memory) generally performs best across statistical metrics for predicting cytokine concentrations [7]
- C-LSTM (Convolutional LSTM) significantly outperforms other networks in capturing spatial dependencies of cytokine concentrations [7]
- Physics-Informed Neural Networks (PINN) produce a standard deviation that better reflects the expected variability in individual predictions [7]
These surrogate models enable rapid exploration of intervention strategies and parameter spaces that would be prohibitively time-consuming with full ABM simulations.
Quantitative Burn Assessment Through Electrical Impedance Spectroscopy
Electrical Impedance Spectroscopy (EIS) provides a quantitative approach for burn injury detection by measuring the electrical impedance characteristics of blood with different volume proportions of red blood cells (RBCs) and heated red blood cells (HRBCs) [19]. The method employs a seven-parameter equivalent circuit to quantify the relationship between electrical properties and burn severity:
Table 1: Electrical Impedance Parameters for Burn Injury Assessment
| Parameter | Relationship with HHCT | Correlation Coefficient (R²) | Application in Burn Assessment |
|---|---|---|---|
| Imaginary part of impedance (ZImt) | ZImt = -2.56HHCT - 2.01 | 0.96 | Primary parameter for injury degree detection |
| Plasma resistance (Rp) | Rp = -7.2HHCT + 3.91 | 0.96 | Verification parameter for injury severity |
| Characteristic frequency (fc) | Varies with HHCT | N/A | Identifies peak point Zt in Nyquist plots |
This approach demonstrates feasibility for rapid, quantitative burn injury detection through parameters ZImt and Rp, potentially enabling more efficient clinical treatment planning [19].
Precision Imaging and Predictive Modeling
Advanced imaging techniques combined with predictive modeling have revolutionized burn assessment accuracy:
- Adaptive Complex Independent Components Analysis (ACICA) and Reference Region (TBSA) methods enable precise estimation of burn depth and Total Body Surface Area with 96.7% accuracy using RNN models [20]
- Dynamic Contrast Enhancement (DCE) with GLCM-based texture analysis provides detailed tissue characterization, facilitating differentiation between various burn types [20]
- Deep neural network classification covers categories including healthy skin, superficial burn, superficial dermal burn, deep dermal burn, and full-thickness burn [20]
These technologies provide nuanced insights into burn severity, improving diagnostic accuracy and treatment planning beyond subjective clinical evaluations.
Application Notes & Experimental Protocols
Protocol 1: Agent-Based Modeling of Acute Inflammation (Days 0-4 Post-Burn)
Objective: To simulate the spatial-temporal dynamics of immune cell interactions and cytokine signaling during the acute inflammatory phase following burn injury.
Workflow:
Key Parameters to Monitor:
- Initial endothelial cell count (critical determinant of inflammation intensity) [6]
- Chemotaxis threshold and chemoattractant levels [6]
- Neutrophil activation and macrophage polarization states [6]
- Pro- to anti-inflammatory cytokine ratios
Validation: Compare simulation outputs with experimental data from animal burn models, including cell counts and cytokine levels across the 4-day timeframe [6].
Protocol 2: Neural Network Surrogate Model Development
Objective: To create efficient neural network surrogates for predicting cytokine concentration dynamics in burn wounds.
Workflow:
Architecture Specifications:
- STA-LSTM: Implement spatial and temporal attention mechanisms for optimal statistical performance [7]
- C-LSTM: Use convolutional layers to capture spatial dependencies of cytokine distributions [7]
- PINN: Incorporate physical constraints to ensure biologically plausible predictions [7]
Evaluation Metrics: Mean Squared Error (MSE), R-squared, Mean Absolute Percentage Error (MAPE) [7].
Protocol 3: Electrical Impedance Spectroscopy for Burn Severity Quantification
Objective: To quantitatively assess burn injury severity through electrical impedance characteristics of blood components.
Table 2: Experimental Setup for EIS Burn Assessment
| Component | Specification | Purpose |
|---|---|---|
| Impedance Analyzer | IM7581 (Hioki E.E. Corporation) | Measure electrical impedance parameters |
| Fixture | 16092A (Agilent Technologies) | Secure cuvette during measurement |
| Cuvette | 12 mm × 12 mm × 45 mm with copper electrodes | Hold blood sample for testing |
| Electrodes | 10 mm × 20 mm with 2 mm distance | Enable electrical current application |
| Blood Sample Preparation | Swine blood with 3.28% trisodium citrate (1:9 ratio) | Prevent coagulation while maintaining physiological properties |
| Heating Protocol | 55°C for 1 hour in thermostatic water bath | Mimic burn injury effects on blood components |
| Centrifugation | 2000× g for 30 minutes at room temperature | Separate HRBCs, RBCs, and plasma |
Procedure:
- Prepare blood samples with varying proportions of HRBCs and RBCs (HCT + HHCT = 40%) [19]
- Measure impedance across frequency spectrum (100 kHz to 300 MHz) with applied current of 10 mA [19]
- Analyze Nyquist plots to identify characteristic frequency (fc) and peak point Zt (ZRet, ZImt) [19]
- Calculate HHCT using established linear relationships: ZImt = -2.56HHCT - 2.01 [19]
- Correlate HHCT with burn injury severity for clinical assessment
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Computational Burn Immunology
| Reagent/Material | Function/Application | Specifications |
|---|---|---|
| CompuCell3D | Software platform for GGH/ABM simulations | Enables modeling of cell behaviors, solute diffusion, and chemotaxis in burn wounds [6] |
| Neural Network Frameworks | Implementation of surrogate models (TensorFlow, PyTorch) | Facilitates development of STA-LSTM, C-LSTM, and PINN architectures [7] |
| Impedance Analyzer | Measurement of electrical characteristics in blood | IM7581 system with frequency range 100 kHz-300 MHz for EIS burn assessment [19] |
| Dynamic Contrast Enhancement | Burn depth analysis via medical imaging | ACICA and RR methods for precise burn classification in transformed RGB to LUV images [20] |
| Animal Burn Model Data | Validation of computational predictions | Longitudinal cytokine levels and immune cell counts from rodent studies [6] |
| Seven-Parameter Equivalent Circuit | Quantitative analysis of EIS data | Electrical model correlating impedance parameters with HHCT for burn severity assessment [19] |
Signaling Pathways in Post-Burn Immune Response
The computational approaches outlined herein provide powerful methodologies for unraveling the complexity of post-burn immune responses. By integrating agent-based modeling, neural network surrogates, electrical impedance spectroscopy, and precision imaging, researchers can overcome traditional limitations in burn research. These protocols and application notes offer practical frameworks for implementing these cutting-edge computational techniques, accelerating the development of improved therapeutic interventions for burn patients. The continued refinement of these in silico methods promises to further bridge the knowledge gap between experimental observations and clinical applications in burn care.
A Technical Deep Dive into In Silico Modeling Frameworks for Burn Immunology
Within the context of in silico mechanistic modeling of the immune response to burn injuries, Agent-Based Modeling (ABM) provides a powerful computational framework for simulating complex biological systems. ABM breaks down a system into its constituent entities, treating each as an independent agent that makes decisions based on its local environment [21]. This paradigm is exceptionally well-suited for immunology because it enables the assignment of known cellular characteristics to each cell-agent, allowing researchers to simulate how mesoscopic entities' actions and interactions lead to macro-level events—a phenomenon known as emergent behavior [21].
The Glazier-Graner-Hogeweg (GGH) method, also known as the Cellular Potts Model (CPM), is a specific, versatile ABM formulation that allows for the representation of non-uniform cell shapes as agents in multi-cell systems [6]. Unlike simpler ABM approaches, the GGH framework can capture the spatial heterogeneity and complex cell-cell interactions characteristic of biological tissues. This capability is crucial for modeling the immune response to burn injuries, which involves a massive and prolonged acute inflammation involving intricate interactions between various cellular and molecular components [6]. The GGH method has recently been successfully deployed to investigate the dynamics of inflammation after burn injuries, identifying key factors such as the initial endothelial cell count that influence the acute inflammatory response [6] [8].
Key Quantitative Parameters for Simulating Post-Burn Immune Response
The development of a biologically relevant GGH model requires the careful definition of numerous parameters based on experimental data. The following tables summarize core cell behaviors and cytokine interactions identified as critical for simulating the first 0-4 days post-burn, a key period for acute inflammatory response [6] [22].
Table 1: Key Cellular Agents and Their Behaviors in Post-Burn Immune Response
| Cell Agent | Key Behaviors & Functions in Post-Burn Context | Temporal Dynamics (0-96h Post-Burn) |
|---|---|---|
| Endothelial Cells | Initiate inflammatory response; express adhesion molecules and chemokines; facilitate recruitment of immune cells; crucial for angiogenesis [6]. | Pivotal role in intensity and progression of acute inflammation (0-4 days) [6] [8]. |
| Neutrophils | Among first immune responders; remove necrotic tissue; release pro-inflammatory factors [22]. | Activated neutrophils (AN) increase (↑) then decline (); Resting neutrophils (RN) show a decrease (↓) by 48h [6]. |
| Macrophages | Differentiate into pro-inflammatory (M1) or "pro-healing" (M2) phenotypes; clear debris; regulate fibroblast behavior [6] [22]. | M1 macrophages increase (↑) around 48h then decline (); M2 macrophages show growth () from 72h [6]. |
| Fibroblasts | Migrate to wound site; key players in tissue regeneration and matrix deposition [6]. | Presence increases (↑) from 72h post-burn [6]. |
| Satellite Stem Cells (SSCs) | Activate, proliferate, and differentiate to repair damaged muscle fibers; behavior regulated by macrophages [22]. | Critical in the regeneration phase following initial inflammation [22]. |
Table 2: Critical Diffusing Factors and Their Roles in a Post-Burn GGH Model
| Diffusing Factor | Primary Function & Cellular Source | Impact on Burn Wound Healing Dynamics |
|---|---|---|
| Pro-inflammatory Cytokines (IL-8, IL-6, TNF-α, IL-1β) | Released by immune cells (e.g., neutrophils, M1 macrophages) post-burn; trigger and amplify immune response [6] [23]. | Drive acute inflammation; elevated levels associated with massive, prolonged inflammation post-burn [6]. |
| Anti-inflammatory Cytokines (IL-10) | Secreted by M2 macrophages and other cells; modulates inflammatory response [6] [22]. | Essential for transitioning from pro-inflammatory to pro-healing phase; prevents excessive tissue damage. |
| MCP-1 (Monocyte Chemoattractant Protein-1) | Chemokine recruiting monocytes/macrophages [22]. | Key for monocyte recruitment from blood to burn site; influences macrophage population dynamics. |
| TGF-β (Transforming Growth Factor Beta) | Secreted by macrophages, fibroblasts; regulates cell proliferation and differentiation [22]. | Plays a complex role in regeneration and fibrosis; potential target for therapeutic intervention. |
| HGF (Hepatocyte Growth Factor) | Involved in SSC activation and regeneration [22]. | Promotes muscle recovery; dynamics crucial for successful regeneration post-injury. |
Experimental Protocol: Implementing a GGH Model for Acute Burn Inflammation
This protocol outlines the steps to develop a GGH model simulating the immune response during the first 0-4 days post-burn, based on established methodologies [6] [22].
Pre-Simulation Setup and Model Configuration
- Software Selection: Implement the model using the CompuCell3D (CC3D) environment, a specialized, Python-based platform for CPM/GGH simulations (version 4.3.1 or higher) [22].
- Spatial Domain Definition: Create a 2D simulation lattice representing a cross-section of tissue and an adjacent blood compartment. A common size is 256x256 pixels, balancing computational cost and resolution [24].
- Agent Initialization: Populate the domain with agents based on pre-burn homeostasis. Stochastically induce injury by converting a defined region of healthy tissue to necrotic tissue to simulate the burn [22].
- Parameter Definition: Set the key parameters governing cell behaviors and interactions. The values below are illustrative and require calibration to specific experimental conditions.
Table 3: Core GGH Energy Hamiltonian Parameters (Illustrative)
| Parameter | Description | Example Value/Range |
|---|---|---|
J_cell,medium |
Contact energy between cell and medium. | 8.2 [24] |
J_cell,cell |
Contact energy between two cells. | 6 [24] |
λ_volume |
Constraint strength for maintaining target cell volume. | 5 [24] |
λ_surface |
Constraint strength for maintaining target cell surface. | 1 [24] |
λ_chemotaxis |
Strength of chemotactic response to a diffusing factor. | 2000 [24] |
Simulation Execution and Data Collection
- Monte Carlo Step (MCS) Loop: Run the simulation for a predefined number of MCS, where each step represents a unit of simulated time. The core algorithm involves:
- Pixel Copy Attempt: Randomly select a lattice pixel and a neighboring target pixel.
- Energy Change Calculation (
ΔH): Compute the change in the system's effective energy if the pixel copy were to occur. The Hamiltonian (H) includes terms for adhesion, volume constraint, surface constraint, and chemotaxis [24]:H = ∑[Adhesion Energy] + λ_volume(V_cell - V_target)² + λ_surface(S_cell - S_target)² + ∑[-λ_chemotaxis * (C_dest - C_source)] - Boltzmann Acceptance Function: Accept or reject the pixel copy based on the probability:
Pr = exp(-max(0, ΔH / B)), whereBrepresents the membrane fluctuation amplitude [24].
- Solute Diffusion: Simultaneously, at each MCS, update the concentration of every diffusing factor (cytokines, chemokines) across the lattice by solving a partial differential equation that includes diffusion, decay, and secretion terms:
∂c/∂t = D∇²c - kc + secretion[24]. - Data Logging: At regular intervals, record system-level data (e.g., cell counts, cytokine concentrations) and agent-level data (e.g., cell positions, state changes) for post-processing.
Model Calibration and Validation
- Calibration: Use parameter density estimation to refine parameters not available from literature by fitting model outputs to temporal biological datasets (e.g., cell counts from animal studies) [22]. The dataset from Mulder et al. (2022), which includes cytokine levels and immune cell counts from rodent burn models, is a key resource for this step [6].
- Validation: Qualitatively and quantitatively compare simulation outputs (e.g., dynamics of neutrophil infiltration, macrophage polarization, endothelial cell changes) against independent experimental data not used for calibration [6] [22]. For burn models, a critical validation is confirming that the simulated initial endothelial cell count directly correlates with the intensity and duration of the acute inflammatory response [6] [8].
Signaling and Workflow Visualization
Diagram 1: Core Signaling in Post-Burn Immune Response.
Diagram 2: GGH Model Development Workflow.
Table 4: Key Research Reagent Solutions for GGH Model Development
| Tool / Resource | Type | Primary Function in GGH Modeling |
|---|---|---|
| CompuCell3D (CC3D) | Software Platform | Primary simulation environment for developing, executing, and visualizing GGH/CPM models; handles core algorithms [22]. |
| Cell Studio | Software Platform / Framework | A hybrid platform for creating visualized, interactive 3D immune simulations; can use game engine technology [21]. |
| Parameter Density Estimation | Computational Method | An iterative protocol to calibrate unknown model parameters by fitting to temporal biological data [22]. |
| Animal Model Data (e.g., rodent burn studies) | Experimental Dataset | Provides critical, quantitative time-series data on cell counts and cytokine levels for model calibration and validation [6]. |
| Unity3D Game Engine | Software Platform | Can be used as a client for real-time 3D visualization and interaction with running simulations in a framework like Cell Studio [21]. |
| U-Net Convolutional Neural Network | Deep Learning Model | Can serve as a surrogate model to drastically accelerate simulation evaluation, e.g., predicting 100 MCS ahead [24]. |
In the field of in silico mechanistic modeling of the immune response to burn injuries, researchers face a significant computational challenge. High-fidelity models that simulate complex biological systems at a detailed level are often prohibitively slow for tasks requiring rapid iteration, such as parameter exploration, uncertainty quantification, or potential treatment screening. Surrogate modeling has emerged as a powerful solution, where data-driven models—particularly neural networks (NNs)—are trained to approximate the input-output behavior of complex mechanistic models with dramatically reduced computational cost [25] [26].
This paradigm is especially valuable in burn immunology, where the post-burn immune response involves intricate spatiotemporal interactions between numerous cell types, cytokines, and signaling molecules that evolve over time [6] [27]. Neural network surrogates enable researchers to accelerate simulations from hours to seconds while maintaining acceptable accuracy, thus enhancing both the speed and scalability of predictive modeling in burn research [26] [28].
Surrogate Model Applications in Burn Immunology and Related Fields
Table 1: Quantitative Performance of Neural Network Surrogates Across Domains
| Application Domain | Base Model | Surrogate Model | Speed Increase | Accuracy vs. Base Model | Reference |
|---|---|---|---|---|---|
| 3D Wind Farm Wake Prediction | SOWFA (CFD) | Physics-Inspired NN + Autoencoder | Hours → Seconds | RMSE < 0.2 m/s (<2-5% error) | [26] |
| 3D Geotechnical Consolidation | Finite Element Method | Physics-Informed Neural Networks | N/A → <1 second | >98% accuracy | [28] |
| Dragonfly Network Simulation | PDES (CODES) | GNN + LLM (Smart) | 0.515 seconds inference | Outperformed statistical/ML baselines | [25] |
In burn immunology research, agent-based models (ABM) such as the Glazier-Graner-Hogeweg (GGH) method have been employed to simulate the dynamics of inflammation after burn injuries, capturing complexities including changes in cell counts and cytokine levels [6]. These models simulate individual cellular agents (e.g., mast cells, neutrophils, macrophages) and molecular solutes (e.g., pro-inflammatory and anti-inflammatory cytokines) across tissue and blood compartments, with cells exhibiting behaviors such as chemotaxis in response to concentration gradients [6] [8].
While these mechanistic models provide valuable insights, they can be computationally intensive for exploring the vast parameter space of biological conditions. Surrogate modeling approaches similar to those successfully applied in other fields (Table 1) could significantly accelerate burn immunology simulations, enabling rapid prediction of inflammation progression based on initial conditions such as endothelial cell count, a key parameter identified in recent research [6].
Protocol: Implementing NN Surrogates for Immune Response Prediction
Data Generation and Preparation Protocol
Table 2: Training Data Requirements for Effective Surrogate Models
| Data Type | Source | Key Parameters | Preprocessing Steps | Volume Requirements |
|---|---|---|---|---|
| Spatiotemporal cell density data | GGH model simulations [6] | Cell counts (neutrophils, macrophages), cytokine concentrations | Spatial normalization, time-series alignment | 100+ simulation runs |
| Router performance data | PDES simulations [25] | Port-level features, application characteristics | Temporal alignment, graph structuring | Two dedicated datasets for training/validation |
| 3D Flow field data | SOWFA CFD simulations [26] | Velocity fields, turbulence parameters | Wind box decomposition, spatial encoding | Multiple farm layouts and conditions |
| Transcriptomic profiles | RNA-seq of burn-affected liver tissue [29] | Gene expression values, pathway activation | Log transformation, batch effect correction | Young/aged mice, multiple time points |
Procedure:
- Execute Base Model Simulations: Run multiple iterations of the high-fidelity GGH model [6] with varied initial conditions (endothelial cell count, chemotaxis thresholds, cytokine concentrations) to generate training data.
- Extract Spatial-Temporal Features: Capture cell density distributions and cytokine concentration profiles across both blood and tissue compartments at regular time intervals (e.g., hourly from day 0-4 post-burn).
- Implement Wind Box Decomposition (for spatial systems): For large or complex spatial domains, apply decomposition strategies that divide the simulation domain into smaller "wind boxes" or subregions, enabling modular training and enhanced scalability [26].
- Normalize and Partition Data: Apply min-max scaling or z-score normalization to numerical features, then split data into training (70%), validation (15%), and test (15%) sets, ensuring temporal consistency in time-series data.
Neural Network Architecture Selection and Training
Materials:
- Python 3.8+ with TensorFlow 2.8+ or PyTorch 1.10+
- High-performance computing node with NVIDIA GPU (16GB+ VRAM)
- Custom data loaders for spatiotemporal biological data
Procedure:
- Architecture Selection:
- For spatial graph data (e.g., cell interactions across compartments): Implement Graph Neural Networks (GNNs) with message passing to capture neighborhood dependencies [25].
- For temporal sequences (e.g., cytokine level evolution): Integrate Long Short-Term Memory (LSTM) networks or transformer-based temporal encoders [25].
- For incorporating physical constraints: Employ Physics-Informed Neural Networks (PINNs) that embed biological conservation laws directly into the loss function [28].
Model Implementation:
- Define encoder-decoder architecture with 3-5 hidden layers
- Incorporate skip connections to facilitate gradient flow
- Apply spatial pooling operations for multi-scale feature extraction
Training Configuration:
- Initialize weights using Glorot uniform initialization
- Set initial learning rate of 0.001 with exponential decay
- Use combined loss function: Mean Squared Error + Physical consistency term
- Implement early stopping with patience of 100 epochs
- Train for maximum 2000 epochs with batch size of 32-128
Diagram 1: Neural Network Surrogate Architecture for Burn Immune Response Prediction
Model Validation and Deployment Protocol
Procedure:
- Quantitative Validation:
- Compare surrogate predictions against held-out GGH simulation results using multiple metrics: Mean Absolute Error (MAE), Root Mean Square Error (RMSE), and R² correlation coefficient.
- Establish accuracy thresholds: RMSE of cell counts <5% of dynamic range, R² >0.9 for cytokine trajectories.
Physical Consistency Checking:
- Verify that predictions obey biological conservation laws (e.g., mass balance of cells, energy constraints).
- Validate temporal monotonicity where biologically appropriate (e.g., non-decreasing scar tissue formation).
Uncertainty Quantification:
- Implement Monte Carlo dropout during inference to estimate prediction uncertainty.
- Flag predictions with high uncertainty for potential refinement through full simulation.
Deployment Optimization:
- Convert trained model to TensorFlow Lite or ONNX format for efficient inference.
- Implement caching mechanism for frequently queried initial conditions.
- Develop API interface for integration with existing research workflows.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Resources for Surrogate Modeling in Burn Immunology
| Resource Category | Specific Tools/Solutions | Function/Purpose | Implementation Example |
|---|---|---|---|
| Simulation Platforms | GGH Model [6], CODES [25], SOWFA [26] | Generate high-fidelity training data through mechanistic simulation | Simulate post-burn immune cell dynamics across compartments |
| NN Frameworks | TensorFlow, PyTorch, JAX | Implement and train surrogate model architectures | Build GNN-LSTM hybrids for spatiotemporal prediction |
| Specialized Architectures | Graph Neural Networks [25], Physics-Informed NNs [28] | Capture spatial relationships and embed physical constraints | Enforce biological conservation laws in prediction tasks |
| Training Data Sources | Animal study data [6], Transcriptomics [29], Clinical immune parameters [27] | Provide experimental validation and system-specific parameters | Parameterize initial conditions from murine burn studies |
| Deployment Tools | TensorFlow Serving, ONNX Runtime, FastAPI | Enable production deployment and integration | Create web API for research team access to surrogate |
Application Notes for Burn Immunology Research
The implementation of NN surrogates for predicting post-burn immune responses requires special considerations specific to the biological domain:
Key Biological Parameters for Surrogate Modeling
- Initial endothelial cell count: Identified as a pivotal parameter influencing inflammation intensity and progression during acute inflammation (0-4 days post-burn) [6].
- Chemotaxis thresholds: Critical for accurate spatial prediction of immune cell migration toward inflammation sites.
- Cytokine dynamics: Pro-inflammatory (IL-6, IL-8, TNF-α) and anti-inflammatory (IL-10) mediators that exhibit characteristic temporal patterns post-burn [27].
- Cell-type specific responses: Neutrophils, monocytes, macrophages (M1/M2 phenotypes), and fibroblasts each play distinct roles with different temporal dynamics [6].
Domain-Specific Adaptation Requirements
- Multi-scale modeling: Surrogates must bridge cellular-level events with tissue-level and systemic responses.
- Time-scale separation: Acute inflammatory processes (hours-days) versus healing and remodeling (weeks-months) require different modeling approaches.
- Aging considerations: Surrogate models may need age-specific parameters, as transcriptomic analyses reveal significantly different hepatic responses to burns in aged versus young mice [29].
Validation Against Experimental Data
Surrogate predictions should be validated against both in silico data and experimental observations:
- Immune cell infiltration patterns from histology
- Cytokine level measurements from blood/tissue samples
- Transcriptomic profiles from affected tissues [29]
- Clinical outcomes from burn patient studies [27]
Neural network surrogate models represent a powerful methodology for accelerating in silico research into the immune response following burn injuries. By implementing the protocols outlined in this document, researchers can develop accurate, efficient predictive tools that maintain the biological fidelity of complex mechanistic models while achieving speedups of several orders of magnitude. This approach enables previously infeasible large-scale parameter studies, uncertainty quantification, and potential real-time predictive capabilities that can advance our understanding of post-burn immunology and contribute to improved therapeutic strategies.
The immune response to burn injuries is a complex, multi-system process that involves intricate interactions between inflammatory mediators, immune cells, and metabolic pathways. Understanding these dynamics is crucial for improving patient outcomes, particularly because burns extend beyond the skin, inflicting damage on distant organs such as the liver and exacerbating poor outcomes in burn victims [29]. The mortality rate after burns in the elderly population is significantly higher than in any other age group, highlighting the need for precise mechanistic understanding [29].
Integrating transcriptomics and metabolomics provides a powerful framework for elucidating the underlying mechanisms of burn-induced pathology. While transcriptomics determines the functional response to burn injury and helps predict its master regulators, metabolomics provides a downstream, phenotype-proximal description of the biological processes [29]. This multi-omics approach enables researchers to move beyond correlative observations to build predictive in silico models that can simulate the dynamics of the immune response and identify potential therapeutic interventions.
This Application Note provides a detailed protocol for integrating transcriptomic and metabolomic data to construct mechanistic models of the immune response to burn injuries, with a specific focus on hepatic dysfunction. We summarize key quantitative findings, outline experimental and computational methodologies, and visualize critical signaling pathways to facilitate research in this area.
Key Omics Findings in Burn Injury and Related Inflammatory Conditions
Multi-omics studies have revealed consistent patterns of pathway dysregulation in burn injuries and other inflammatory conditions like sepsis. The table below summarizes key differentially expressed genes and metabolites identified in preclinical models.
Table 1: Key Omics Alterations in Inflammatory Injury Models
| Study Model | Differentially Expressed Genes | Altered Metabolites | Affected Pathways |
|---|---|---|---|
| Burn-Induced Liver Damage (Aged Mice) [29] | • Up: Derl3, Hyou1, Hspa5, Lcn2, S100a8/9• Down: Cyp2c29, Cyp2c38, Cyp2c54, Gsta3, Gsta4 |
Valine, Methionine, Tyrosine, Phenylalanine, Leucine [29] | • Protein processing in ER• IL-17 signaling• Chemical carcinogenesis• Steroid hormone biosynthesis• Xenobiotics metabolism by CYP450 |
| Agmatine-Treated Septic Liver Injury (Rats) [30] | 17 differentially expressed genes (e.g., involved in arginine/proline and arachidonic acid metabolism) | 26 significant metabolites | • Arginine and proline metabolism• Arachidonic acid metabolism• Linoleic acid metabolism• NF-κB and AMPK-PPARα signaling |
| Hypertension-Induced Hippocampal Injury (Rats) [31] | 103 differentially expressed genes | 56 significant metabolites (e.g., various amino acids) | Amino acid metabolism and related pathways |
These consistent findings across models provide a foundational dataset for building and validating in silico models of inflammatory organ damage.
Experimental Protocol for Generating Multi-Omics Data from Burn Models
This section details a standardized protocol for obtaining transcriptomic and metabolomic data from a murine burn model, as derived from published studies [29].
Animal Model and Burn Injury Induction
- Animal Subjects: Young and aged mice (e.g., 8-12 weeks for young; over 18 months for aged).
- Anesthesia: Anesthetize animals using intraperitoneal injection of pentobarbital sodium (45 mg/kg) [30].
- Burn Procedure: Perform a standardized scald burn injury (e.g., ~30% total body surface area) on the shaved dorsal surface. Administer analgesic and fluid resuscitation post-procedure.
- Control Groups: Include sham-treated groups (anesthetized and shaved, but not burned).
- Sample Collection: At designated endpoint (e.g., 24 hours post-burn), euthanize animals and rapidly collect liver tissue. Snap-freeze tissue in liquid nitrogen and store at -80°C until analysis.
Transcriptomic Profiling via RNA-Seq
- RNA Extraction: Homogenize ~30 mg of liver tissue. Extract total RNA using a commercial kit (e.g., Trizol reagent). Determine RNA purity and concentration using NanoDrop and Qubit RNA HS Assay Kit. Assess RNA integrity (RIN > 8.0) using an Agilent Bioanalyzer or TapeStation system [30] [31].
- Library Preparation & Sequencing: Use Illumina-based protocols for library preparation (e.g., Illumina TruSeq Stranded mRNA). Perform paired-end sequencing (e.g., 2x150 bp) on an Illumina platform (e.g., Novaseq 6000) [31].
- Bioinformatic Analysis:
- Quality Control: Use FastQC to assess raw read quality.
- Alignment: Align reads to the reference genome (e.g., mm10 for mouse) using STAR aligner.
- Quantification: Generate count data for genes using featureCounts.
- Differential Expression: Identify differentially expressed genes (DEGs) using DESeq2 with thresholds of \|log2(Fold Change)\| > 1 and adjusted p-value (FDR) < 0.05 [29] [31].
- Pathway Analysis: Perform Gene Ontology (GO) and KEGG pathway enrichment analysis on DEGs using ClusterProfiler [30].
Metabolomic Profiling via LC-MS/MS
- Metabolite Extraction:
- Weigh ~30 mg of frozen liver tissue.
- Add 500 μL of pre-cooled extraction solvent (e.g., Methanol:Acetonitrile:Water = 2:2:1) [31].
- Homogenize tissue using a bead beater (35 Hz, 4 min) and sonicate in an ice-water bath for 5 min. Repeat 3 times.
- Incubate at -40°C for 1 hour to precipitate proteins.
- Centrifuge at 12,000-15,000 rpm for 15 min at 4°C.
- Collect the supernatant for LC-MS/MS analysis.
- LC-MS/MS Analysis:
- Chromatography: Use a UHPLC system with a reverse-phase or HILIC column (e.g., UPLC BEH Amide column, 2.1 mm × 100 mm, 1.7 μm). Maintain auto-sampler at 4°C and use an injection volume of 2-5 μL. Employ a gradient elution with mobile phases A (e.g., water with ammonium acetate/ammonia hydroxide) and B (e.g., acetonitrile) [31].
- Mass Spectrometry: Couple to a high-resolution mass spectrometer (e.g., Q Exactive HFX). Operate in both positive and negative electrospray ionization (ESI) modes. Set spray voltage to ±3.0-3.6 kV, capillary temperature to ~350°C, and perform full MS and MS/MS data acquisition [31].
- Metabolomic Data Processing:
- Use software (e.g., XCMS, MS-DIAL) for peak picking, alignment, and integration.
- Annotate metabolites by matching accurate mass and MS/MS spectra against public databases (e.g., HMDB, MassBank).
- Perform statistical analysis in SIMCA (V16.0.2). Use Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA) to model group separation. Identify significant metabolites with Variable Importance in Projection (VIP) > 1.0 and p-value < 0.05 (Student's t-test) [31].
Protocol for Integrated Data Analysis and In Silico Model Building
The integration of transcriptomic and metabolomic data is crucial for generating a systems-level understanding.
Data Integration and Correlation Analysis
- Pathway Integration: Map DEGs and significantly altered metabolites onto KEGG pathways to identify concordantly disturbed pathways (e.g., Arginine and Proline Metabolism, Arachidonic Acid Metabolism) [30].
- Correlation Analysis: Perform Spearman correlation analysis between the expression levels of key DEGs and the abundance of related metabolites. Strong correlations (e.g., \|r\| > 0.8, p < 0.05) can suggest potential regulatory relationships [31].
- Visualization: Use multi-omics visualization tools like the Pathway Tools Cellular Overview, which can paint up to four omics datasets (e.g., transcriptomics as reaction arrow color, metabolomics as metabolite node color) onto organism-specific metabolic charts [32].
Building an Agent-Based Model of the Post-Burn Immune Response
Agent-based modeling (ABM) is a powerful computational technique for simulating complex systems like the immune response. The following protocol is based on the Glazier-Graner-Hogeweg (GGH) method [6] [8].
- Step 1: Define the Simulation Domain and Compartments
- Create a 2D or 3D lattice representing the burn wound microenvironment.
- Separate the domain into blood and tissue compartments [6].
- Step 2: Populate with Agents
- Cell Agents: Define the following motile agents with specific properties and behavioral rules:
- Endothelial Cells: Key parameter for inflammation intensity; express adhesion molecules [6].
- Neutrophils: Exhibit chemotaxis toward pro-inflammatory cytokine gradients (e.g., IL-8); phagocytose debris [6].
- Macrophages (M1/M2): Differentiate into pro-inflammatory (M1) or pro-healing (M2) phenotypes; secrete various cytokines [6].
- Mast Cells: Release early inflammatory mediators [6].
- Solute Agents (Diffusible Molecules):
- Pro-inflammatory cytokines: IL-8, IL-6, TNF-α, IL-1β.
- Anti-inflammatory cytokines: IL-10.
- Inflammation triggering factors: DAMPs/PAMPs [6].
- Cell Agents: Define the following motile agents with specific properties and behavioral rules:
- Step 3: Define Agent Behaviors and Rules
- Chemotaxis: Cells move along concentration gradients of chemoattractants (e.g., neutrophils toward IL-8) based on a defined chemotaxis threshold [6].
- Secretion: Cells secrete solutes (e.g., macrophages secrete TNF-α) based on their state and local environment [6].
- Diffusion: Solutes diffuse through the domain based on their concentration profiles [6].
- State Transitions: e.g., Neutrophils become activated or necrotic; Macrophages polarize to M1/M2.
- Step 4: Parameterize the Model with Omics Data
- Initialize agent counts and solute concentrations using quantitative data from transcriptomics/metabolomics and literature (e.g., initial endothelial cell count is a pivotal parameter) [6].
- Use time-course omics data to constrain and validate the model's dynamics.
- Step 5: Run Simulations and Analyze Results
- Simulate the system from day 0 to 4 post-burn.
- Analyze output metrics: spatial-temporal patterns of cell infiltration, cytokine levels, and identify key factors driving the inflammatory response [6].
Diagram 1: In Silico ABM Workflow for simulating post-burn immune response using multi-omics data.
Visualization of Key Signaling Pathways
Integrating omics data often reveals critical signaling pathways. The following diagram illustrates a key pathway - the interplay between inflammatory signaling and metabolic dysregulation in the liver, commonly identified in burn and sepsis models [29] [30].
Diagram 2: Signaling in Burn/Sepsis-Induced Liver Injury showing inflammatory and metabolic dysregulation.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Kits for Multi-Omics Burn Injury Research
| Item Name | Function/Application | Example Usage in Protocol |
|---|---|---|
| Trizol Reagent | Total RNA isolation from tissue/cells. | Extraction of high-quality RNA from snap-frozen liver tissue for RNA-seq [30] [31]. |
| Qubit RNA HS Assay Kit | Accurate fluorometric quantification of RNA concentration. | Quantifying RNA after extraction prior to library prep [29]. |
| Agilent Bioanalyzer/TapeStation | Assessment of RNA Integrity Number (RIN). | Quality control of RNA samples; ensures only high-integrity RNA (RIN > 8.0) is sequenced [29]. |
| Illumina TruSeq Stranded mRNA Kit | Preparation of sequencing libraries from purified mRNA. | Construction of cDNA libraries for transcriptome sequencing on Illumina platforms [31]. |
| DESeq2 R Package | Statistical analysis of differential gene expression from RNA-seq count data. | Identifying genes with significant expression changes ( |log2FC|>1, FDR<0.05) between burn and sham groups [29] [31]. |
| Methanol:Acetonitrile:Water (2:2:1) | Efficient extraction of a wide range of polar and non-polar metabolites. | Metabolite extraction from liver tissue homogenates for LC-MS/MS analysis [31]. |
| UPLC BEH Amide Column | Hydrophilic interaction liquid chromatography (HILIC) for polar metabolite separation. | Chromatographic separation of metabolites in complex biological samples prior to MS detection [31]. |
| SIMCA Software | Multivariate data analysis (e.g., OPLS-DA) for metabolomics. | Statistical modeling to identify metabolites (VIP >1.0) that discriminate between experimental groups [31]. |
| Pathway Tools Software | Multi-omics data visualization on metabolic charts. | Painting transcriptomics and metabolomics data onto organism-specific metabolic network diagrams for integrated analysis [32]. |
The field of immunology faces a significant translational gap, often termed the "valley of death," between animal studies and human clinical trials [33]. Despite mice being the most widely used and cost-effective model for studying human diseases, substantial differences exist due to evolutionary distance, lifespan variations, environmental factors, and the artificiality of many disease models [34]. These differences form formidable barriers to translational research that ultimately hinder the success of clinical trials. In burn injury research specifically, this challenge is particularly acute, as the immune response involves complex interactions between various cellular and molecular components that differ significantly between species [6] [35].
The translational gap is quantifiable and stark. Systematic analysis reveals that when directly translating mouse gene expression results to human equivalents, at best only one out of three genes is shared, with a mean of just one out of twenty genes showing consistent expression patterns [34]. This discrepancy underscores the urgent need for sophisticated methodologies that can systematically incorporate the wealth of knowledge on species differences in the interpretation of animal model data. New Approach Methods (NAMs), including in silico modeling and advanced machine learning techniques, are emerging as powerful tools to bridge this gap, offering more ethical, accurate, and human-relevant alternatives to traditional animal-based research [33].
Computational Approaches for Cross-Species Translation
The Found In Translation (FIT) Model
The Found In Translation (FIT) model represents a groundbreaking data-driven statistical methodology that leverages public domain gene expression data to predict human disease-associated genes from mouse experimental results [34]. This approach addresses the fundamental limitation of direct cross-species extrapolation by incorporating prior knowledge on mouse-human biological differences when prioritizing genes, rather than relying solely on mouse data and ortholog information.
Key Components of the FIT Model:
- Training Compendium: FIT utilizes manually annotated microarray and RNA-seq gene expression datasets from GEO, consisting of 170 paired human and mouse model datasets spanning 28 different diseases [34].
- Algorithmic Foundation: The model employs a regularized linear model (LASSO) that predicts human effect-size per gene by combining measured mouse gene expression with knowledge of mouse-human similarities and differences [34].
- Prediction Mechanism: Through a bootstrapping approach with 100 iterations, FIT generates confidence intervals and predicts expected human effect-size values, outputting a new effect-size value for each gene that can be used in downstream analyses [34].
Table 1: Performance Comparison of Direct Mouse-to-Human Translation vs. FIT Model
| Metric | Direct Translation | FIT Model | Improvement |
|---|---|---|---|
| Max True Positive Fraction | 34% (at best) | 20-50% increase in overlap | Significant signal gain |
| Mean True Positive Fraction | 5% (1 in 20 genes) | Substantially higher | Major reduction in false leads |
| Applicability Prediction | Not applicable | 80% accuracy in predicting when FIT will provide benefit | Enables robust use |
| Experimental Cost | High (requires additional validation) | Zero experimental cost | Direct resource savings |
In Silico Modeling of Burn Immune Responses
For burn injury research specifically, computational modeling approaches offer unprecedented opportunities to understand the dynamics of the post-burn immune response. Agent-based modeling techniques, particularly the Glazier-Graner-Hogeweg (GGH) model, enable simulation of inflammatory agents and the dynamics of entities involved in burn wound inflammation [6].
Model Architecture and Components:
- Spatial Organization: The simulation domain is separated into blood and tissue compartments, each containing solutes and cell agents [6].
- Cellular Components: Includes mast cells, neutrophils, and macrophages modeled as independent agents that are motile and exhibit chemotaxis based on concentration gradients [6].
- Molecular Factors: Solutes comprise pro-inflammatory cytokines, anti-inflammatory cytokines, and inflammation-triggering factors that diffuse throughout the domain based on concentration profiles [6].
This modeling approach has successfully identified key factors influencing acute inflammatory response, particularly highlighting the pivotal role of the initial endothelial cell count as a determinant of inflammation intensity and progression during 0-4 days post-burn [6] [8].
Experimental Protocols for Human-Relevant Data Generation
Protocol: Ex Vivo Human Skin Burn Model
Objective: To establish a reproducible, clinically relevant human skin model for studying thermal injury and early wound healing processes while accounting for inter-individual variability [35].
Materials and Reagents:
- Human skin samples from elective reconstructive surgeries
- Customized burn device with pulley system
- Culture media: DMEM/F12 with 10% FBS, 1% Antibiotic-Antimycotic
- Histology equipment and reagents (H&E staining)
- Viability assay kits (e.g., MTT, AlamarBlue)
Methodology:
- Tissue Preparation: Process human skin samples within one hour after surgery. Remove excess subcutaneous fat to create an even skin surface [35].
- Burn Induction: Use a customized burn device set at 100°C. Apply contact times of 5, 15, or 30 seconds to generate graded burn injury depths simulating superficial, partial, or deep partial thickness injuries [35].
- Culture Conditions: Maintain burned skin samples at air-liquid interface using cell culture inserts with appropriate media, changing every 2-3 days [35].
- Assessment:
- Evaluate cellular viability immediately post-burn and at regular intervals
- Process tissues for histology at days 0, 1, 3, 7, and 14
- Analyze re-epithelialization and tissue remodeling
Validation: This model successfully demonstrates time-dependent burn depth progression and captures significant inter-individual variability in healing responses, mirroring clinical observations [35].
Protocol: Machine Learning Prediction of ICU Delirium in Burn Patients
Objective: To develop a machine learning model for predicting delirium in burn patients during ICU stay using patient data from the first 24 hours of admission [36].
Materials and Reagents:
- Electronic medical records system
- Data extraction and preprocessing tools
- Machine learning platform (Python/R with appropriate libraries)
- ICDSC (Intensive Care Delirium Screening Checklist) forms
Methodology:
- Data Collection: Extract 70 explanatory variables including physiological, biochemical, and clinical data from burn patients upon ICU admission [36].
- Delirium Assessment: Assess delirium every 8 hours after ICU admission using ICDSC, with a score ≥4 indicating delirium [36].
- Model Development: Implement 10 different machine learning algorithms including logistic regression, support vector machine, random forest, and neural networks [36].
- Model Validation: Use stratified k-fold cross-validation, allocating 80% of data for training and 20% for internal validation [36].
- Feature Importance Analysis: Apply SHAP (Shapley Additive Explanations) to identify top predictors of ICU delirium [36].
Key Outcomes: The model identified 24-hour urine output, oxygen saturation, burn area, total bilirubin level, and intubation upon ICU admission as major risk factors for delirium onset [36].
Table 2: Performance Metrics of Machine Learning Models for ICU Delirium Prediction
| Model | Mean AUC | Standard Deviation | Key Strengths |
|---|---|---|---|
| Logistic Regression | 0.906 | 0.073 | High accuracy, interpretability |
| Support Vector Machine | 0.897 | 0.056 | Effective in high-dimensional spaces |
| K-Nearest Neighbor | 0.894 | 0.060 | Simple, no assumptions about data |
| Neural Network | 0.857 | 0.058 | Captures complex nonlinear relationships |
| Random Forest | 0.850 | 0.074 | Handles missing data, feature importance |
| Naïve Bayes | 0.827 | 0.095 | Computational efficiency |
| Adaptive Boosting | 0.832 | 0.094 | Ensemble method, reduces bias |
| Gradient Boosting | 0.821 | 0.074 | Sequential error correction |
Integrated Workflow: From Mouse Data to Human Predictions
Figure 1: Integrated translational research workflow that systematically bridges mouse experimental data to human clinical predictions through computational and experimental validation.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for Translational Burn Immunology
| Reagent/Solution | Function | Application Context |
|---|---|---|
| Ex Vivo Human Skin Culture System | Maintains physiological skin biology and barrier function | Bridge between in vitro models and clinical practice [35] |
| Customized Burn Device with Pulley System | Ensures reproducible contact burn application | Standardized thermal injury models [35] |
| FIT (Found In Translation) Software | Predicts human disease genes from mouse data | Cross-species computational translation [34] |
| Agent-Based Modeling Platform (GGH) | Simulates immune cell interactions and spatial dynamics | In silico modeling of burn inflammation [6] |
| Multi-Organ-on-Chip Systems | Replicates systemic immunological processes with multiple tissue types | Studying immunotoxicity and inter-tissue communication [33] |
| 24-Color Flow Cytometry Panel | Comprehensive immunophenotyping of human peripheral blood cells | High-throughput screening of immune responses [33] |
| ICDSC (Intensive Care Delirium Screening Checklist) | Standardized assessment of delirium in ICU patients | Clinical validation of predictive models [36] |
| SHAP (Shapley Additive Explanations) | Interprets feature importance in machine learning models | Identifying key predictive factors in clinical data [36] |
Data Visualization and Interpretation Strategies
Effective data presentation is crucial for translating complex research findings into actionable insights. The choice between tables and charts should be guided by the specific communication goal:
Use Tables when presenting precise values, detailed comparisons, or data-heavy reports where exact figures are essential for analysis [37] [38]. In translational research, tables are particularly valuable for displaying gene lists with effect sizes, clinical parameters with exact values, and statistical summaries of model performance.
Use Charts when illustrating trends, patterns, relationships, or providing quick insights from complex datasets [39] [37]. For immunology research, charts effectively show time-course data of cytokine levels, cellular infiltration patterns, and model performance comparisons.
For the quantitative data generated through the protocols described in this article, structured tables provide the necessary precision for scientific validation, while well-designed charts can effectively communicate the overarching trends and relationships discovered through computational and experimental approaches.
The integration of computational models, machine learning, and human-relevant experimental systems represents a paradigm shift in translational immunology research. The approaches outlined in this application note—from the FIT model for cross-species gene expression translation to agent-based modeling of burn inflammation and machine learning for clinical prediction—provide a comprehensive framework for overcoming the traditional barriers between mouse studies and human clinical applications.
By adopting these integrated methodologies, researchers can significantly enhance the predictive value of preclinical data, identify more reliable biomarkers, and ultimately accelerate the development of effective therapeutics for burn injuries and other immune-related conditions. The future of translational research lies in the intelligent combination of computational power and human-relevant experimental data, moving beyond simple extrapolation to create truly predictive models of human biology.
Overcoming Computational Hurdles: Strategies for Robust and Efficient Model Performance
In silico mechanistic modeling, particularly Agent-Based Modeling (ABM), has become an indispensable tool for studying the complex, non-linear dynamics of the immune response to burn injuries. These models simulate interactions between individual cellular agents (e.g., neutrophils, macrophages) and molecular species (e.g., cytokines), providing unparalleled insight into emergent system behavior [6]. However, as models grow in sophistication to more accurately represent biological reality, they encounter a significant barrier: extreme computational cost. High-fidelity simulations can require hours or days to run, rendering comprehensive parameter exploration, sensitivity analysis, and uncertainty quantification—essential for robust scientific inference and clinical translation—prohibitively expensive [40]. This application note outlines the strategic adoption of surrogate models, computationally efficient substitutes for complex ABMs, as a core solution to this challenge, with a specific focus on applications within burn immunology.
Surrogate Model Performance for Burn Immune Response Prediction
A critical evaluation of surrogate models involves assessing their accuracy and computational efficiency in approximating ABM outputs. Recent research has benchmarked various neural network architectures for predicting spatial-temporal cytokine concentrations in a burn wound ABM.
Table 1: Performance Benchmark of Neural Network Surrogates for Cytokine Prediction
| Model Architecture | Key Strengths | Statistical Performance | Computational Scalability |
|---|---|---|---|
| STA-LSTM | Excels at capturing spatio-temporal dependencies [7]. | Best overall performance across multiple statistical metrics (e.g., Mean Squared Error, R-squared) [7]. | Good |
| C-LSTM | Superior at capturing spatial dependencies of cytokine concentrations [7]. | High performance in spatial correlation tasks [7]. | Poor at higher grid dimensions [7]. |
| CT-LSTM | Designed for complex temporal dynamics. | Not Specified | Poor at higher grid dimensions [7]. |
| Physics-Informed Neural Networks (PINNs) | Incorporates physical laws into the learning process [7]. | Produces a standard deviation that better reflects expected individual prediction variability [7]. | Good |
Protocol: Implementing an LSTM-Based Surrogate for an Immune ABM
This protocol details the steps to create and validate a Long Short-Term Memory (LSTM) network as a surrogate for a burn immune response ABM, based on methodologies from recent literature [7] [6].
Reagents and Computational Tools
Table 2: Research Reagent Solutions for Surrogate Modeling
| Item Name | Function/Application | Specifications |
|---|---|---|
| CompuCell3D | A development environment for ABMs. Used to generate high-fidelity simulation data for training [7]. | Multi-platform software; C++, Python, or Java. |
| Python Data Stack | Core programming environment for data processing, model building, and analysis [7]. | Libraries: TensorFlow/PyTorch (NNs), Scikit-learn (data prep), Pandas/NumPy (data handling). |
| High-Performance Computing (HPC) Cluster | Provides the computational power for large-scale ABM simulations and training of complex surrogate models [40]. | CPU/GPU nodes, large memory capacity, parallel processing. |
| Zenodo Repository | A data repository used for sharing the code and ABM data required to reproduce surrogate modeling experiments [7]. | FAIR (Findable, Accessible, Interoperable, Reusable) principles. |
Procedure
Step 1: ABM Data Generation and Curation
- Simulation Setup: Configure the baseline burn injury ABM in CompuCell3D [7]. The model should include key agents: mast cells, neutrophils, macrophages, and endothelial cells, as well as solutes like pro- and anti-inflammatory cytokines [6].
- Parameter Sampling: Systematically vary key input parameters (e.g., initial endothelial cell count, chemotaxis thresholds) across a defined physiological range using a space-filling design (e.g., Latin Hypercube Sampling) to ensure broad coverage of the parameter space [40].
- Output Recording: For each simulation run, record the time-series and spatial-grid data of key output variables (e.g., cytokine concentrations, cell counts) at a specified temporal resolution.
Step 2: Data Preprocessing and Engineering
- Data Cleaning: Handle any missing or anomalous data points originating from simulation artifacts.
- Structuring for Training: Transform the raw spatio-temporal ABM output into a format suitable for LSTM training. This typically involves creating samples where a sequence of past time steps is used to predict the next time step(s).
- Train-Test Split: Perform a time-series-aware split of the data (e.g., 80-20) to prevent data leakage and ensure the model is evaluated on a temporally distinct dataset [7].
Step 3: Surrogate Model Architecture and Training
- Model Design: Implement an LSTM architecture. A recommended starting point is the STA-LSTM variant, which has demonstrated top performance [7]. Tune hyperparameters (number of LSTM layers, neurons per layer, learning rate) via cross-validation.
- Loss Function: Define the loss function, typically Mean Squared Error (MSE), to minimize the difference between the ABM's output and the surrogate's prediction.
- Model Training: Train the LSTM model on the prepared training dataset. Utilize GPU acceleration to expedite the process. Implement early stopping to prevent overfitting.
Step 4: Model Validation and Deployment
- Quantitative Validation: Evaluate the trained model on the held-out test dataset using metrics beyond MSE, such as R-squared and Mean Absolute Percentage Error, to assess predictive accuracy and robustness [7].
- Sensitivity Analysis: Use the validated surrogate model to perform a rapid, computationally cheap global sensitivity analysis (e.g., using Sobol' indices) on the original ABM. This identifies which input parameters most significantly influence the model outputs, providing crucial biological insights [40].
Conceptual Framework for Scalable Immune Digital Twins
The ultimate application of these models is in creating "Immune Digital Twins" (IDTs)—personalized computational models that evolve with a patient's state. Surrogate modeling is a key enabling technology for making IDTs computationally feasible [41]. The following diagram illustrates the modular architecture and data flow of a scalable IDT system that leverages surrogate models.
Advanced Strategies and Future Outlook
Beyond standalone surrogate models, the field is moving toward hybrid and multi-scale approaches. Physics-Informed Neural Networks (PINNs) show promise by embedding known physical laws (e.g., diffusion equations for cytokines) directly into the loss function of the neural network, improving generalizability when data is sparse [7]. Furthermore, the concept of modularity is critical for scalability. Complex IDTs can be constructed by linking simpler, validated modules—each with its own surrogate—representing different biological scales or organ systems (e.g., a skin burn module connected to a liver metabolism module) [41]. This aligns with findings from transcriptomic studies which show distinct organ-specific responses to burn injury, underscoring the need for such modularity [29].
Finally, the integration of AI with mechanistic modeling is pushing the boundaries of what is possible. AI can be used to generate synthetic data to augment training sets, while mechanistic models provide a scaffold for interpretability, creating a powerful synergy for scalable, insightful, and clinically relevant in silico research in burn immunology [41].
Application Notes & Protocols for In Silico Modeling of Immune Response to Burn Injuries
In silico mechanistic modeling of the post-burn immune response provides a powerful framework for understanding complex inflammatory dynamics and identifying key therapeutic targets [6]. However, the development of robust models is frequently hampered by data scarcity, a consequence of the ethical and practical challenges in obtaining comprehensive longitudinal data from burn patients or animal models, and data quality issues, including significant gaps and noise in available datasets [6] [42]. This document outlines standardized protocols and analytical techniques to overcome these hurdles, ensuring model reliability and predictive power.
Quantitative Characterization of Post-Burn Immune Dynamics
A critical first step is a systematic analysis of available data to define the system's quantitative behavior. The following table summarizes typical cell count dynamics in the acute phase (0-96 hours) post-burn, synthesized from animal model data [6]. This provides a crucial benchmark for model calibration.
Table 1: Qualitative Dynamics of Key Cell Populations Post-Burn [6]
| Cell Type | 0h | ~24h | ~48h | ~72h | ~96h |
|---|---|---|---|---|---|
| Resting Neutrophils (RN) | – | ↓ | – | ||
| Activated Neutrophils (AN) | – | ↑ | ↓ | – | |
| Monocytes (M) | – | – | ↑ | – | |
| Macrophages type I (M1) | – | – | – | ↑ | |
| Macrophages type II (M2) | – | – | – | – | |
| Fibroblasts (F) | – | – | – | – | ↑ |
| Myofibroblasts (My) | – | – | – | – |
Symbols: - No data; Growth; ↑ Increase; Decline; ↓ Decrease
Analysis of in silico models has identified several parameters with significant influence on simulation outcomes. The relative impact of these parameters is summarized below.
Table 2: Key Model Parameters Influencing Acute Inflammatory Intensity (Days 0-4) [6]
| Parameter | Theoretical Impact on Inflammation | Justification |
|---|---|---|
| Initial Endothelial Cell Count | High | Endothelial cells are first responders, initiating inflammation via adhesion molecules and chemokines [6]. |
| Level of Chemoattractants | Medium | Directly controls chemotaxis and recruitment of immune cells like neutrophils and macrophages [6]. |
| Chemotaxis Threshold | Medium | Determines the sensitivity of immune cells to chemoattractant gradients, affecting cell migration efficiency [6]. |
Protocol 1: Generative Adversarial Networks for Synthetic Data Generation
3.1. Objective To generate high-fidelity synthetic run-to-failure data that mimics the complex relationships in observed, but scarce, post-burn immunology data, thereby expanding the effective training dataset for mechanistic models [42].
3.2. Background and Rationale Machine learning, particularly deep learning, requires large datasets to learn failure patterns effectively. Data scarcity is a fundamental challenge in predictive domains like burn immunology, where failure instances (e.g., severe dysregulation) are rare [42]. Generative Adversarial Networks (GANs) address this by learning the underlying data distribution and generating novel, plausible data points.
3.3. Experimental Workflow
3.4. Research Reagent Solutions
Table 3: Essential Components for a GAN-based Data Generation Pipeline
| Component / Tool | Function / Explanation | Example / Alternative |
|---|---|---|
| Run-to-Failure Datasets | The scarce, real-world data on immune parameters (cell counts, cytokines) used to train the GAN. | Data from animal models or human cohorts [6] [42]. |
| GAN Framework | Software library providing the building blocks for constructing and training GAN models. | TensorFlow, PyTorch. |
| Generator (G) Network | A neural network (e.g., multi-layer perceptron) that maps random noise to synthetic data points. | Custom architecture designed for tabular time-series data. |
| Discriminator (D) Network | A neural network that acts as a binary classifier to distinguish real from synthetic data. | Custom architecture that mirrors the Generator's complexity. |
| Normalization Scaler | Preprocessing tool to maintain data consistency by scaling features to a specific range (e.g., 0-1). | Min-Max Scaler [42]. |
3.5. Step-by-Step Methodology
- Data Preprocessing: Clean the original dataset. Handle missing values (e.g., via imputation) and normalize numerical features using min-max scaling to a [0, 1] range [42].
- Model Architecture Definition:
- Generator (G): Design a neural network that takes a vector of random noise as input and outputs a synthetic data sample with the same structure as the real data.
- Discriminator (D): Design a neural network that takes a data sample (real or synthetic) and outputs a single probability (real or fake).
- Adversarial Training:
- Train D to correctly classify real data as "real" and data from G as "fake."
- Simultaneously, train G to fool D by generating data that D classifies as "real."
- Iterate until an equilibrium is reached where D cannot distinguish real from synthetic data [42].
- Synthetic Data Generation & Validation: Use the trained Generator to produce the required volume of synthetic data. Validate by ensuring statistical properties (e.g., means, variances, correlations) are consistent with the original dataset.
Protocol 2: Addressing Data Imbalance via Failure Horizons
4.1. Objective To rectify severe class imbalance in run-to-failure data, where "failure" or "pre-failure" states are drastically outnumbered by "healthy" states, by strategically relabeling data to create a more balanced dataset for model training [42].
4.2. Background and Rationale In burn immunology data, a component (e.g., a tissue microenvironment) is typically in a healthy state, with only the final time point(s) representing a failure state. This leads to a dataset where failure cases may constitute a tiny fraction (e.g., <0.01%), causing models to be biased toward the majority class and miss critical failure predictors [42].
4.3. Experimental Workflow
4.4. Step-by-Step Methodology
- Define Horizon Window ('n'): Determine the number of time points preceding a failure event that exhibit pre-failure signatures. This is a critical parameter based on domain knowledge [42].
- Data Relabeling: For each run-to-failure sequence:
- Identify the time of failure
t. - Relabel the last
nobservations (e.g.,t,t-1, ...,t-n+1) as belonging to the "Failure" class. - Label all preceding observations as "Healthy."
- Identify the time of failure
- Dataset Reformation: Combine the relabeled data from all runs to form a new, balanced dataset suitable for training classification models to predict impending failure.
Protocol 3: Neural Network Surrogates for Enhanced Prediction
5.1. Objective To develop accurate and computationally efficient surrogate models using specialized neural networks that can approximate complex, computationally intensive agent-based models (ABMs) of the immune response, facilitating rapid prediction and scenario testing [7].
5.2. Background and Rationale While ABMs are excellent for capturing the spatio-temporal complexity of the immune response to burns, they are computationally demanding, limiting their use for rapid exploration and forecasting [6] [7]. Neural network surrogates can learn the input-output relationships of the ABM and provide predictions orders of magnitude faster.
5.3. Research Reagent Solutions
Table 4: Key Tools for Neural Network Surrogate Modeling
| Component / Tool | Function / Explanation | Application Context |
|---|---|---|
| Agent-Based Model (ABM) | The high-fidelity, computationally expensive model to be approximated. | Glazier-Graner-Hogeweg (GGH) model of post-burn inflammation [6] [7]. |
| Spatio-Temporal Attention LSTM (STA-LSTM) | A neural network architecture that excels at capturing both temporal patterns and spatial dependencies in data. | Found to outperform other networks in predicting cytokine concentrations over time and space [7]. |
| Physics-Informed Neural Network (PINN) | A network that incorporates physical laws or domain knowledge as constraints during training, improving generalizability with less data. | Can produce predictions with variability that better reflects expected biological noise [7]. |
| CompuCell3D | A simulation environment for ABMs, used here to generate high-volume training data for the surrogate model. | Used to simulate innate immune response and cytokine data [7]. |
5.4. Step-by-Step Methodology
- ABM Simulation & Data Generation: Run the high-fidelity ABM (e.g., in CompuCell3D) under a wide range of initial conditions and parameters to generate a comprehensive dataset of inputs (e.g., initial cell counts) and outputs (e.g., cytokine concentrations over time and space) [7].
- Data Preprocessing: Clean the ABM output data and transform it into a suitable format for neural network training (e.g., sequences for LSTM models).
- Surrogate Model Selection and Training:
- Select an appropriate architecture (e.g., STA-LSTM for spatio-temporal data, PINN for incorporating biological constraints) [7].
- Train the network to map ABM inputs to its outputs, using standard loss functions like Mean Squared Error.
- Validation and Deployment: Rigorously validate the surrogate model against held-out ABM simulation data. Once validated, the surrogate can be deployed for rapid prediction and analysis, freeing researchers from the computational burden of the full ABM.
The development of high-fidelity in silico models of the post-burn immune response represents a transformative approach to understanding the complex, multi-scale physiological processes that determine patient outcomes. These mechanistic models simulate intricate interactions between cellular agents and molecular mediators across tissue compartments, providing a powerful platform for hypothesis testing and therapeutic discovery [6]. However, the predictive utility of these computational frameworks is entirely dependent on the rigorous application of parameter sensitivity analysis and model calibration techniques, which together ensure that simulations maintain biological fidelity while remaining mathematically robust.
Burn injuries trigger a massive and prolonged inflammatory response that persists for months after the initial trauma, characterized by dynamic changes in immune cell populations and cytokine signaling patterns [6] [8]. The complexity of these physiological responses, involving spatially distributed interactions between neutrophils, macrophages, endothelial cells, and inflammatory mediators, creates substantial challenges for traditional experimental approaches. Mechanistic computational modeling has emerged as an essential tool for deciphering these dynamics, particularly through agent-based modeling frameworks like the Glazier-Graner-Hogeweg (GGH) method, which can capture cellular behaviors and solute diffusion across tissue compartments [6]. The fidelity of these models hinges on precisely parameterized interactions, making sensitivity analysis and calibration indispensable components of model development.
Foundational Principles of Model Calibration
Model calibration in burn immunology requires integration of heterogeneous data types spanning multiple biological scales. The foundational dataset provided by Mulder et al. exemplifies this approach, encompassing cytokine levels and immune cell counts from 14 different cell types across 247 animal studies [6]. These longitudinal measurements capture temporal dynamics essential for calibrating time-dependent processes in silico. However, such datasets frequently exhibit significant gaps, necessitating careful statistical imputation and validation to ensure data quality before parameter estimation [6].
Experimental models provide crucial data for different aspects of burn pathophysiology. Local burn wounds are typically inflicted under controlled conditions with precise temperature and duration parameters, ranging from 54 to 330°C for 4 seconds to 5 minutes depending on the model system [43]. For systemic response studies, burn injuries affecting 15-40% of total body surface area (TBSA) are required to induce meaningful pathophysiological responses, with even 6% TBSA sufficient to trigger systemic reactions in murine models [43]. These standardized injury parameters establish essential baseline conditions for model initialization.
Table 1: Experimental Burn Models for Data Generation
| Model Type | Burn Method | Typical Parameters | Primary Applications |
|---|---|---|---|
| Cutaneous Burn | Thermal contact | 54-330°C for 4s-5min | Local wound progression, topical therapeutics [43] |
| Scald Burn | Hot liquid/steam | Varied temperature exposure | Systemic response, antimicrobial therapies [43] |
| Inhalation Burn | Smoke/inhalants | Species-specific exposure | Pulmonary immunosuppression, multiple organ dysfunction [43] |
| Corneal Burn | Chemical application | NaOH solution (1N, 15-60s) | Corneal fibrosis, neovascularization, limbal stem cell deficiency [43] |
Parameter Estimation Techniques
Parameter estimation employs both manual and automated approaches to determine values that minimize discrepancy between model outputs and experimental data. In developing their inflammatory response model, Dobreva et al. fixed 23 parameter values directly from literature and estimated the remaining parameters through a combination of manual adjustment and automated optimization algorithms [5]. This hybrid approach leverages established biological knowledge while refining parameters that are poorly constrained by existing data.
Advanced calibration workflows incorporate profile likelihood analysis (PLA) to assess parameter identifiability—determining whether available data sufficiently constrain estimated parameters [5]. This analysis confirmed that six key parameters governing mRNA half-lives and cytokine scaling factors were uniquely identifiable using their calibration dataset [5]. For models targeting age-specific responses, such as the differential liver damage in young versus aged burn victims, transcriptomic and metabolomic data provide additional constraints for parameter estimation [29].
Methodological Approaches to Sensitivity Analysis
Global Sensitivity Analysis Framework
Sensitivity analysis systematically quantifies how uncertainty in model outputs can be apportioned to different sources of uncertainty in model inputs. Local sensitivity approaches vary one parameter at a time around a nominal value, while global methods explore the entire parameter space simultaneously. The inflammatory response model developed by Dobreva et al. employed global sensitivity analysis to identify parameters with greatest influence on model outputs, selecting six key parameters for re-estimation based on their high sensitivity indices [5].
In complex immune response models, sensitivity analysis reveals which cellular and molecular parameters most strongly influence system dynamics. The GGH-based burn model identified three factors as particularly influential: the initial endothelial cell count, chemotaxis threshold, and chemoattractant levels [6] [8]. This finding highlights the pivotal role of vascular components in modulating acute inflammatory responses 0-4 days post-burn, providing mechanistic insights while prioritizing parameters for precise estimation.
Integration with Multi-Omics Data
Contemporary sensitivity analysis increasingly incorporates multi-omics data to validate identified sensitive parameters against experimental evidence. Research on burn-induced liver damage demonstrated age-dependent sensitivity patterns, with cytochrome P450 genes (particularly Cyp2c family members) showing pronounced sensitivity to burn injury in aged animals [29]. Transcriptomic validation through qPCR at multiple time points confirmed the dynamical behavior of these sensitive system components, with downregulation becoming more severe as time progressed post-burn [29].
Table 2: Key Sensitive Parameters in Burn Immune Response Models
| Parameter Category | Specific Parameters | Biological Impact | Validation Approach |
|---|---|---|---|
| Cellular Parameters | Initial endothelial cell count | Intensity and progression of acute inflammation [6] [8] | Histological analysis, cell counting [6] |
| Molecular Parameters | Chemoattractant levels | Immune cell recruitment dynamics [6] | Cytokine measurements, inhibition studies [6] |
| Behavioral Parameters | Chemotaxis threshold | Spatial distribution of immune cells [6] | Migration assays, computational analysis [6] |
| Metabolic Parameters | Cytochrome P450 expression | Hepatic metabolism, drug processing [29] | RNA sequencing, metabolomics [29] |
Experimental Protocols for Model Validation
Protocol 1: In Vivo Burn Model and Tissue Analysis
Purpose: Generate quantitative data on immune cell dynamics and cytokine profiles for model calibration and validation.
Materials:
- Animal subjects (rat/mouse models)
- Thermal burn device with temperature control
- Anesthetic agents (xylazine/ketamine mixture)
- Tissue collection supplies (fixatives, homogenizers)
- Multiplex cytokine assay kits
- Flow cytometry equipment with cell surface markers
Procedure:
- Anesthetize animals using intraperitoneal injection of xylazine (5 mg/kg) and ketamine (50 mg/kg) [44].
- Remove dorsal hair using clippers followed by depilatory cream to ensure uniform exposure [44].
- Administer standardized burn injury using calibrated thermal device; typical parameters for partial-thickness burns: 75°C for 10 seconds on shaved dorsal skin [43].
- Collect tissue and blood samples at predetermined time points (0, 6, 12, 24, 48, 72, 96 hours post-burn) [6] [29].
- Process tissue samples for histopathological analysis (H&E staining) and homogenize for cytokine measurement.
- Analyze immune cell populations using flow cytometry with specific markers for neutrophils, monocytes, macrophages [6].
- Quantify cytokine concentrations (IL-6, IL-8, TNF-α, IL-1β, IL-10) using multiplex immunoassays [6] [5].
- Validate transcriptomic findings using qPCR for identified sensitive parameters (e.g., Cyp2c genes) across multiple time points [29].
Protocol 2: In Silico Parameter Sensitivity Analysis
Purpose: Identify parameters with greatest influence on model outputs to guide refinement and experimental design.
Materials:
- Calibrated mathematical model of immune response
- High-performance computing resources
- Parameter sampling algorithms (Latin Hypercube Sampling)
- Sensitivity analysis toolbox (SALib, MATLAB)
- Visualization software
Procedure:
- Define parameter ranges based on literature values and experimental uncertainty [5].
- Generate parameter samples using Latin Hypercube Sampling to efficiently explore parameter space.
- Run model simulations for each parameter set, recording key outputs (cell counts, cytokine levels, tissue damage) [5].
- Calculate sensitivity indices using variance-based methods (Sobol indices) or regression-based approaches (Partial Rank Correlation Coefficient) [5].
- Identify most sensitive parameters contributing >80% of output variance.
- Validate sensitivity results through targeted in silico interventions (parameter modulation) [6].
- Cross-reference sensitive parameters with multi-omics data to confirm biological relevance [29].
- Refine measurement protocols for high-sensitivity parameters to reduce uncertainty.
Computational Implementation and Workflow
Figure 1: Model Calibration and Sensitivity Analysis Workflow
Table 3: Research Reagent Solutions for Burn Immune Modeling
| Reagent/Resource | Specifications | Research Application |
|---|---|---|
| Multiplex Cytokine Assays | Panel including IL-6, IL-8, TNF-α, IL-1β, IL-10 | Quantification of inflammatory mediators in tissue homogenates and plasma [6] [5] |
| Flow Cytometry Antibodies | Cell surface markers for neutrophils (CD11b+), monocytes (CD14+), macrophages (F4/80+) | Immune cell population analysis in blood and tissue samples [6] |
| RNA Sequencing Kits | High-throughput transcriptomic profiling | Identification of differentially expressed genes in burn-affected tissues [29] |
| LC-MS/MS Systems | Liquid chromatography with tandem mass spectrometry | Metabolite profiling and identification of bioactive compounds [44] |
| GGH Modeling Framework | Glazier-Graner-Hogeweg method implementation | Agent-based simulation of cellular interactions in burn wounds [6] |
| Digital Twin Platform | BioUML with SBML/SBGN support | Modular mathematical modeling of immune response [45] |
Case Studies in Burn Injury Modeling
Case Study 1: Acute Inflammatory Response Model
A GGH-based model of post-burn immune response successfully identified the initial endothelial cell count as a critical determinant of inflammation intensity during the first 4 days post-injury [6] [8]. Through systematic parameter variation and comparison with temporal cell count data, the model revealed that endothelial cells act as first responders, initiating inflammatory responses through adhesion molecule expression and chemokine production [6]. This finding was validated through histological analysis showing endothelial activation and subsequent immune cell recruitment dynamics.
Case Study 2: Age-Specific Liver Response to Burns
Integration of transcriptomics and metabolomics data from young versus aged mice revealed differential sensitivity to burn-induced liver damage [29]. Cytochrome P450 genes, particularly Cyp2c family members, showed pronounced downregulation in aged animals post-burn, validated through qPCR at multiple time points [29]. This age-dependent sensitivity pattern informed a computational model of hepatic dysfunction that successfully predicted metabolic alterations and identified potential therapeutic targets through in silico drug screening.
Parameter sensitivity analysis and model calibration represent indispensable components in the development of biologically faithful computational models of post-burn immune responses. The rigorous application of these methodologies transforms abstract mathematical constructs into predictive tools capable of capturing the essential dynamics of burn pathophysiology. As the field advances, several emerging trends promise to enhance these approaches further.
Future developments will likely include increased integration of multi-omics data streams, with transcriptomic, metabolomic, and proteomic profiles providing additional constraints for parameter estimation [29] [44]. Additionally, the adoption of digital twin frameworks—virtual representations of individual patients—will require novel calibration approaches that can efficiently personalize model parameters using limited patient-specific data [45]. These advances, coupled with increasingly sophisticated sensitivity analysis techniques, will accelerate the development of predictive models that can guide therapeutic interventions and improve outcomes for burn patients.
Physics-Informed Neural Networks (PINNs) represent a transformative paradigm at the intersection of machine learning and mechanistic modeling, enabling the integration of known physical or biological laws directly into the learning process of neural networks. Unlike traditional, purely data-driven models, PINNs incorporate governing equations—typically expressed as Ordinary or Partial Differential Equations (ODEs/PDEs)—as soft constraints in the loss function during training [46] [47] [48]. This hybrid approach ensures that the model's predictions are not only consistent with observed data but also adhere to established scientific principles, thereby enhancing their generalizability, interpretability, and reliability, especially in data-sparse regimes [47].
Within the specific context of in silico mechanistic modeling of the immune response to burn injuries, this integration is critically important. The post-burn inflammatory response is a complex, spatio-temporal process involving intricate interactions between various immune cells (e.g., neutrophils, macrophages) and molecular components (e.g., cytokines) [6]. Agent-Based Models (ABMs) have been valuable for studying these interactions but are often computationally prohibitive for large-scale or long-term simulations [7]. PINNs offer a powerful alternative as surrogate models that can approximate and forecast the dynamics of these computationally intensive mechanistic models, such as those simulating cytokine concentrations over time and space [7]. By embedding the known biological rules of the immune response into the neural network, PINNs facilitate accurate, efficient, and physiologically consistent predictions, accelerating research into wound healing and therapeutic strategies.
Application Note: Forecasting Cytokine Dynamics in Burn Wounds
Background and Rationale
Following a burn injury, a massive and prolonged inflammatory response is triggered, characterized by dynamic changes in the concentrations of key cytokines across the wound domain [6]. Accurately predicting these spatio-temporal cytokine profiles is essential for understanding the progression of healing and potential systemic complications. While agent-based models (ABMs) built in platforms like CompuCell3D can simulate the innate immune response and generate detailed cytokine data, they are computationally demanding, limiting their utility for rapid forecasting and parameter exploration [7].
PINN Implementation and Comparative Performance
A study directly addressed this challenge by developing neural network surrogates, including PINNs, to approximate ABM outputs for cytokine concentrations [7]. The performance of various architectures was quantitatively evaluated, yielding the following results:
Table 1: Performance of different neural network architectures in predicting cytokine concentrations.
| Model Architecture | Key Strengths | Key Limitations |
|---|---|---|
| STA-LSTM | Best overall performance across statistical metrics (e.g., Mean Squared Error, R-squared) [7]. | Specific limitations not detailed in the provided results [7]. |
| C-LSTM | Excelled at capturing spatial dependencies of cytokine concentrations [7]. | Exhibited poor computational scalability at higher grid dimensions [7]. |
| PINN | Produced a standard deviation that better reflected the expected variability in individual predictions [7]. | Performance is highly sensitive to network architecture and hyperparameter tuning [46]. |
| CT-LSTM | Information not specified in search results. | Exhibited poor computational scalability at higher grid dimensions [7]. |
This application demonstrates that PINNs and other advanced neural networks can effectively serve as data-driven surrogates for complex mechanistic models of the immune response, offering a balance between statistical accuracy and physical plausibility.
Protocol: Implementing a PINN for an ODE-Based Immune Response Model
This protocol details the steps for developing a PINN to solve a system of ODEs representing a simplified immune response to a burn injury, such as the dynamics of pro- and anti-inflammatory cytokines.
Prerequisites and Data Preparation
- Programming Environment: A Python environment with TensorFlow or PyTorch is required. The
ODE-PINNPython package can serve as a useful reference and starting point [46]. - Governing Equations: Define the system of ODEs representing the biological system. For instance, this could involve equations for the rates of change of pro-inflammatory (e.g., IL-6, TNF-α) and anti-inflammatory (e.g., IL-10) cytokine concentrations [6].
- Observation Data: Collect or generate time-series data for the cytokine concentrations. This data can come from experimental measurements (e.g., animal studies [6]) or high-fidelity simulations (e.g., ABM outputs [7]).
- Initial and Boundary Conditions: Precisely define the initial state of the system and any relevant boundary conditions.
Model Definition and Architecture Selection
- Network Inputs and Outputs: The input node is typically time. The output layer should have multiple nodes, each predicting the concentration of a different cytokine or the solution to a different state variable in the ODE system.
- Network Architecture: A feedforward neural network is commonly used as a backbone. Based on the application note, an LSTM-based architecture (like STA-LSTM) may be preferable for capturing temporal dependencies, though it may increase complexity [7].
- Physics-Informed Loss Function: The core of a PINN is its loss function, which is a weighted sum of two components:
- Data Loss (( \mathcal{L}{data} ): The mean squared error (MSE) between the network's predictions and the observed training data.
- Physics Loss (( \mathcal{L}{physics} ): The MSE of the residual of the ODE system. This is calculated by applying automatic differentiation to the network's outputs with respect to its inputs (time) and evaluating how well the derivatives satisfy the predefined ODEs.
Workflow Diagram
The following diagram illustrates the logical workflow and architecture of a PINN for this application.
Training, Validation, and Deployment
- Hyperparameter Tuning: Systematically adjust key hyperparameters, including the learning rate, the number of layers and neurons, and the weighting parameter (( \lambda )) that balances the data and physics loss components. Performance is highly sensitive to these choices [46].
- Model Training: Use a gradient-based optimizer (e.g., Adam) to minimize the total loss function. Employ techniques like learning rate scheduling to improve convergence.
- Model Validation and Testing: Validate the trained model on a held-out test set. Evaluate its performance using metrics such as Mean Absolute Percentage Error and R-squared [7].
- Solution and Analysis: Deploy the trained PINN to predict cytokine dynamics under new initial conditions or over longer time horizons, providing insights into the system's behavior.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential computational tools and data for implementing PINNs in burn immune response modeling.
| Tool/Resource | Type | Primary Function in Research |
|---|---|---|
| CompuCell3D | Software Platform | A development environment for building and executing high-fidelity Agent-Based Models (ABMs) of the immune response, which can generate training data for PINN surrogates [7]. |
| ODE-PINN Package | Software Tool | A dedicated Python package provided by researchers to facilitate the reproduction of results and implementation of PINNs for ODE-based systems [46]. |
| Long Short-Term Memory (LSTM) | Algorithm | A type of neural network architecture highly effective for capturing temporal dependencies in time-series data, such as cytokine concentration trajectories [7]. |
| Experimental Cytokine & Cell Count Data | Dataset | Longitudinal data on immune cell counts and cytokine levels from (pre)clinical studies, used for model training and validation [6]. |
| TensorFlow / PyTorch | Software Library | Core open-source machine learning frameworks that provide the necessary infrastructure, including automatic differentiation, for building and training custom PINNs [46] [47]. |
The application of PINNs to in silico modeling of the immune response to burn injuries is still nascent but holds immense promise. Future research directions should focus on developing more sophisticated multi-scale PINN architectures that can seamlessly integrate intracellular signaling pathways with tissue-level and organism-level responses [6] [48]. Furthermore, addressing the challenge of computational scalability for high-dimensional problems will be crucial for modeling larger and more biologically realistic domains [7] [49]. Another key area is the development of robust hyperparameter optimization strategies and loss-balancing techniques to improve training stability and predictive accuracy [46] [47].
In conclusion, PINNs represent a powerful and versatile framework for enhancing the scope and scalability of mechanistic models in immunology. By seamlessly integrating established biological rules with data-driven learning, they provide a compelling approach for forecasting the complex dynamics of burn wound healing, ultimately contributing to the development of improved diagnostic tools and therapeutic interventions.
Benchmarking Model Efficacy: Validation Frameworks and Comparative Analysis of Methodologies
The transition from animal studies to human clinical outcomes represents a critical pathway in biomedical research, particularly in complex pathophysiological conditions such as burn injuries. This application note provides a structured framework for the qualitative and quantitative validation of experimental data across species barriers, with specific emphasis on in silico mechanistic modeling of the immune response to burn trauma. We present standardized protocols for data collection, computational model development, and multi-scale validation strategies that integrate transcriptomic, metabolomic, and immunological profiling to bridge the translational gap. The methodologies outlined herein support the refinement of animal-to-human extrapolation and enhance the predictive power of computational models in burn immunology, ultimately facilitating more efficient drug development and personalized therapeutic strategies.
Burn injuries trigger a complex and prolonged immune response characterized by massive inflammation that can persist for months after the initial trauma [6]. The pathophysiological complexity of burns extends beyond the visible skin damage to systemic effects involving multiple organs, including the liver, and profound alterations in immune and metabolic pathways [29] [3]. Despite significant advances in burn care, mortality and morbidity rates remain high, undersc the critical need for more predictive research models that can accurately simulate human responses [3] [43].
Experimental burn models, particularly those utilizing animals, have been indispensable tools for studying the mechanisms of tissue damage, inflammation, and wound healing [43]. However, significant interspecies differences often limit the translation of findings from animal models to human clinical applications [43]. The emergence of sophisticated in silico modeling approaches presents a promising frontier for integrating multi-scale data from animal and human studies, creating predictive frameworks that can accelerate therapeutic development and improve patient outcomes [6] [29].
This application note details standardized methodologies for generating high-quality qualitative and quantitative data from animal models and executing robust validation processes to ensure clinical relevance, with specific application to immune response modeling in burn injuries.
Quantitative Data Generation from Animal Models
Experimental Burn Model Establishment
Objective: To create reproducible and clinically relevant burn injuries in animal models for quantitative data collection on immune and inflammatory responses.
Materials:
- Adult rodents (e.g., mice or rats, 8-12 weeks old) or other appropriate species
- Anesthesia equipment and reagents (e.g., ketamine/xylazine)
- Controlled-temperature heating device or hot water scald apparatus
- Template for standardized burn area (e.g., 2x3 cm)
- Analgesics for post-procedural care
- Tissue collection supplies (e.g., scissors, forceps, cryovials)
Protocol:
- Anesthetize animals using approved protocols (e.g., ketamine 80-100 mg/kg and xylazine 5-10 mg/kg via intraperitoneal injection).
- Shave the dorsal fur and clean the skin with antiseptic solution.
- Apply a predefined template to delimit the burn area.
- For contact burns: Apply a heated metal rod (54-100°C) for 4-30 seconds, depending on desired burn depth [43].
- For scald burns: Immerse the templated area in heated water (65-95°C) for 10-30 seconds [43].
- Administer postoperative analgesia (e.g., buprenorphine 0.05-0.1 mg/kg) and fluid resuscitation (lactated Ringer's solution, 2 mL/%TBSA/kg).
- Monitor animals regularly until fully recovered from anesthesia.
- At predetermined time points (e.g., 6h, 12h, 24h, 72h post-burn), euthanize animals and collect tissues (blood, skin, liver) for analysis.
Validation Parameters:
- Histological confirmation of burn depth
- Measurement of inflammatory markers in serum (e.g., IL-6, TNF-α)
- Assessment of wound healing progression
Data Collection for Computational Modeling
Objective: To generate comprehensive quantitative datasets on immune cell dynamics and cytokine profiles for parameterizing in silico models.
Protocol:
- Blood Collection and Analysis:
- Collect blood via cardiac puncture at euthanasia time points.
- Perform complete blood count (CBC) with differential to quantify neutrophils, lymphocytes, monocytes, and platelets [50].
- Calculate inflammatory indices: NLR (Neutrophil/Lymphocyte Ratio), PIV (Pan-Immune Inflammation Value) = (Neutrophils × Platelets × Monocytes)/Lymphocytes [50].
- Separate plasma for cytokine analysis via ELISA or multiplex assays.
Tissue Processing and Transcriptomics:
- Homogenize tissue samples (skin, liver) in appropriate lysis buffers.
- Extract total RNA using commercial kits.
- Perform RNA sequencing or qPCR analysis of key immune genes:
Metabolomic Profiling:
- Prepare tissue extracts for mass spectrometry analysis.
- Perform targeted metabolomics for amino acids (valine, methionine, tyrosine, phenylalanine, leucine) and lipid mediators [29].
- Integrate metabolomic data with transcriptomic findings to identify pathway interactions.
Table 1: Key Quantitative Parameters from Animal Burn Models
| Parameter Category | Specific Measures | Time Points | Expected Changes |
|---|---|---|---|
| Immune Cell Counts | Neutrophils, Lymphocytes, Monocytes, Platelets | 0h, 24h, 48h, 72h, 96h | Early neutrophilia, followed by lymphopenia [50] |
| Inflammatory Cytokines | IL-6, IL-8, TNF-α, IL-1β, IL-10, MCP-1 | 6h, 12h, 24h, 72h | Peak IL-6 at 24-72h; correlates with burn severity [3] |
| Liver Enzymes | ALT, AST, Cytochrome P450 isoforms | 24h, 72h | Transaminase elevation; CYP450 downregulation [29] |
| Metabolites | Amino acids, Lipid mediators | 24h | Decreased valine, methionine, tyrosine [29] |
| Histological Damage | Epidermal necrosis, Inflammatory infiltrate | 24h, 72h | Progressive tissue damage up to 3 days post-burn [43] |
In Silico Model Development and Integration
Agent-Based Modeling of Immune Response
Objective: To develop a computational framework that simulates the spatial and temporal dynamics of the post-burn immune response.
Computational Approach:
- Model Architecture:
- Utilize the Glazier-Graner-Hogeweg (GGH) method, also known as the Cellular Potts Model, to represent individual cells as autonomous agents [6].
- Define a simulation domain with separate blood and tissue compartments [6].
- Incorporate solute components (pro-inflammatory cytokines, anti-inflammatory cytokines, inflammation-triggering factors) that diffuse based on concentration gradients [6].
Cell Agent Definitions:
- Program motile cell agents (mast cells, neutrophils, macrophages) that exhibit chemotaxis based on solute concentration gradients [6].
- Define behavioral rules for each cell type, including secretion of specific solutes, response to signals, and lifespan [6].
- Parameterize initial cell counts based on experimental animal data [6].
Model Parameterization:
- Use quantitative data from animal studies (Section 2) to set initial conditions and parameter values.
- Calibrate diffusion coefficients for cytokines based on measured concentration profiles.
- Adjust chemotaxis sensitivity thresholds to match observed cell migration patterns.
Simulation Execution:
The diagram below illustrates the structure of this multi-scale validation approach:
Diagram 1: Multi-scale validation framework integrating animal data, clinical biomarkers, and in silico modeling for therapeutic predictions.
Qualitative Validation through Pathway Analysis
Objective: To ensure the biological plausibility of computational models through qualitative assessment of simulated pathway activations against experimental findings.
Protocol:
- Pathway Mapping:
- Identify key signaling pathways activated in burn response from transcriptomic data (e.g., PPAR signaling, IL-17 signaling, cytochrome P450 metabolism) [29].
- Map temporal activation patterns observed in animal models.
Model Output Assessment:
- Analyze in silico model outputs for emergent pathway activations.
- Compare simulated cytokine cascades and cellular behaviors to qualitative patterns described in experimental literature.
Expert Validation:
- Engage domain experts to assess the biological plausibility of model behaviors.
- Conduct structured comparisons against established knowledge of burn immunology.
Table 2: Key Signaling Pathways in Burn Immune Response for Qualitative Validation
| Pathway | Key Components | Biological Role in Burn Response | Validation Approach |
|---|---|---|---|
| IL-17 Signaling | Cebpb, S100a9, Nfkbia, S100a8, Cxcl1 [29] | Neutrophil recruitment, inflammation amplification | Compare activation timing in model vs. animal data |
| PPAR Signaling | Pck1, Angptl4, Plin5, Cyp4a32, Cyp4a14 [29] | Metabolic regulation, inflammation resolution | Assess pathway activity correlation |
| Cytochrome P450 Metabolism | Cyp2c29, Cyp2c38, Cyp2c40, Cyp2c54 [29] | Drug metabolism, inflammatory mediator production | Validate downregulation pattern post-burn |
| Endothelial Cell Activation | Adhesion molecules, Chemokines [6] | Immune cell recruitment to wound site | Verify initial response timing in model |
Bridging to Clinical Outcomes
Clinical Biomarker Validation
Objective: To validate computational model predictions against clinically relevant biomarkers and outcomes in human burn patients.
Protocol:
- Patient Recruitment and Data Collection:
- Recruit burn patients with ≥20% TBSA burns admitted within 24 hours of injury [50].
- Collect blood samples at admission and at predefined intervals (daily for first week, then weekly).
- Record clinical outcomes: mortality, organ dysfunction, infection episodes, length of stay.
Biomarker Analysis:
Data Correlation:
- Compare biomarker levels between survivors and non-survivors.
- Establish correlation between biomarker trajectories and clinical outcomes.
- Validate computational model predictions against observed clinical courses.
Table 3: Clinically Validated Biomarkers for Burn Severity and Outcomes
| Biomarker | Sample Type | Predictive Value | Clinical Application |
|---|---|---|---|
| Pan-Immune Inflammation Value (PIV) | Blood | Cut-off 1185: 69.6% sensitivity, 66.2% specificity for mortality [50] | Early mortality risk stratification |
| IL-6 | Serum/Plasma | Significantly higher in non-survivors; correlates with TBSA and depth [3] | Prognostication, monitoring response to therapy |
| IL-8 | Serum/Plasma | 2000-fold increase in severe burns; correlates with injury size [3] | Assessment of systemic inflammation |
| MCP-1 | Serum/Plasma | Higher in non-survivors on day 1 post-burn [3] | Early prediction of poor outcomes |
| Liver Transaminases (ALT, AST) | Serum | Peak during first week; higher mortality with elevated levels [29] | Detection of remote organ damage |
Quantitative Clinical Validation of Computational Models
Objective: To statistically validate in silico model predictions against quantitative clinical data.
Protocol:
- Model Predictions:
- Use calibrated in silico models to simulate immune response trajectories for virtual patient cohorts.
- Generate predictions for clinical biomarkers (PIV, cytokine levels) at multiple time points.
Statistical Comparison:
- Calculate correlation coefficients between simulated and measured biomarker values.
- Assess predictive accuracy for clinical outcomes (mortality, sepsis) using receiver operating characteristic (ROC) analysis.
- Compare model performance against established clinical scoring systems (ABSI, rBaux, BOBI) [50].
Model Refinement:
- Iteratively adjust model parameters to improve agreement with clinical data.
- Validate refined models on independent patient cohorts.
The diagram below illustrates the inflammatory signaling pathways identified as critical in burn response:
Diagram 2: Key inflammatory signaling pathways in burn response, showing the progression from initial injury to systemic complications.
Table 4: Key Research Reagent Solutions for Burn Immune Response Studies
| Research Tool | Specific Examples | Application/Function | Experimental Notes |
|---|---|---|---|
| Animal Burn Models | Contact burn (54-100°C), Scald burn (65-95°C), Inhalation injury models [43] | Creating reproducible burn injuries with controlled depth and area | Temperature and exposure time critical for burn depth consistency |
| Computational Modeling Platforms | Glazier-Graner-Hogeweg (GGH) method, Cellular Potts Model [6] | Simulating spatial-temporal dynamics of immune cells and cytokines | Requires parameterization with experimental data |
| Transcriptomic Profiling | RNA sequencing, qPCR arrays for immune genes [29] | Measuring gene expression changes in response to burns | Validate with functional assays (e.g., cytochrome P450 activity) |
| Metabolomic Analysis | Targeted mass spectrometry for amino acids, lipids [29] | Characterizing metabolic alterations post-burn | Integrate with transcriptomic data for pathway analysis |
| Immunoassays | ELISA, Multiplex arrays for cytokines (IL-6, IL-8, TNF-α, IL-1β) [3] | Quantifying inflammatory mediators in serum/tissue | Establish temporal profiles across acute phase |
| Inflammatory Indices | PIV, NLR, MLR, SII calculations from CBC [50] | Predicting clinical outcomes and mortality | Standardize sampling time for comparative analysis |
The structured integration of quantitative animal data, clinical biomarkers, and in silico modeling presented in this application note provides a robust framework for advancing burn immunology research. The validation methodologies outlined enable researchers to bridge the translational gap between experimental findings and clinical applications, enhancing the predictive power of computational models. By adopting these standardized protocols and validation strategies, researchers can accelerate the development of targeted therapeutic interventions for burn patients, ultimately improving survival and long-term outcomes. The iterative process of model refinement through continuous incorporation of clinical data will further enhance the biological fidelity and utility of these computational approaches in both basic research and drug development.
Within the context of in silico mechanistic modeling of the immune response to burn injuries, selecting an appropriate computational approach is paramount for generating reliable, interpretable, and actionable insights. Agent-based models (ABMs) can simulate complex emergent behaviors but are often hampered by significant computational costs. Neural network architectures, including Convolutional Neural Networks (CNNs), Long Short-Term Memory (LSTM) networks, and Physics-Informed Neural Networks (PINNs), offer powerful alternatives or complementary surrogates. This application note provides a structured, comparative analysis of these four algorithms—ABM, CNN, LSTM, and PINN—summarizing their quantitative performance in predicting cytokine concentrations and detailing standardized protocols for their implementation in burn immune response research.
The following tables consolidate key performance metrics from benchmark studies that evaluated these algorithms in modeling biological systems, particularly in predicting cytokine concentrations following burn injuries and other time-series forecasting tasks.
Table 1: Overall Model Performance on Cytokine Concentration Prediction [7] [51]
| Model Type | Key Strength | Key Limitation | Mean Squared Error (MSE) | R-squared (R²) | Mean Absolute Percentage Error (MAPE) |
|---|---|---|---|---|---|
| Agent-Based Model (ABM) | High mechanistic detail; captures emergent spatial dynamics | Extremely computationally demanding; slow for large-scale simulations | Used as baseline data generator | Used as baseline data generator | Used as baseline data generator |
| CNN | Excels at extracting spatial features from data | Limited inherent capability for modeling long-term temporal dependencies | Higher than STA-LSTM/PINN | Lower than STA-LSTM/PINN | Higher than STA-LSTM/PINN |
| LSTM | Excellent at capturing temporal dependencies and sequences | May struggle with complex spatial dynamics without architectural additions | Higher than STA-LSTM | Lower than STA-LSTM | Higher than STA-LSTM |
| STA-LSTM | Captures both spatial and temporal dependencies effectively | Complex architecture; requires more data for training | Lowest among tested NN models | Highest among tested NN models | Lowest among tested NN models |
| PINN | Incorporates physical laws; better generalization with less data | Performance sensitive to network architecture and hyperparameters | Low (but generally higher than STA-LSTM) | High | Low |
Table 2: Performance in Related Time-Series Forecasting Tasks
| Application Area | Model | Performance Metric | Result | Citation |
|---|---|---|---|---|
| Battery State-of-Health | LSTM-PINN | Mean Absolute Error (MAE) | 0.594% - 0.746% | [52] |
| Root Mean Square Error (RMSE) | 0.791% - 0.897% | |||
| Infectious Disease (COVID-19) | PINN | Weighted Interval Score (WIS) | Outperformed basic NN and naive baseline | [53] |
| Burn Wound Segmentation | Mask R-CNN (CNN) | Dice Coefficient (DC) | 0.9496 | [54] |
Detailed Experimental Protocols
Protocol 1: Agent-Based Model (ABM) for Simulating Innate Immune Response
Objective: To generate a high-fidelity baseline dataset of cytokine concentration dynamics in a simulated burn wound environment.
Simulation Setup:
- Platform: Utilize CompuCell3D for simulating the innate immune response [7] [51].
- Simulated Processes: Model key cellular activities including neutrophil and macrophage recruitment, phagocytosis, and cytokine secretion.
- Output Data: Record spatiotemporal concentrations of multiple cytokines (e.g., IL-1β, TNF-α, IL-8) across the simulated tissue grid over time.
Data Generation:
- Execute multiple ABM runs under varying initial conditions (e.g., differing burn severities, pathogen loads) to create a comprehensive dataset.
- The output of these simulations serves as the ground-truth dataset for training and validating the neural network surrogate models.
Protocol 2: Neural Network Surrogate Model Training and Evaluation
Objective: To develop and benchmark CNN, LSTM, STA-LSTM, and PINN models that can accurately approximate the ABM's cytokine predictions.
Data Preprocessing:
- Cleaning & Transformation: Clean the ABM-generated data and transform it into formats suitable for different neural networks [7]. For spatial models (CNN), structure data as 2D/3D grids. For temporal models (LSTM), structure as sequential time steps.
- Train-Test Split: Perform a time-series-aware split of the data to prevent data leakage (e.g., 80% for training, 20% for testing).
Model Implementation:
- CNN Architecture: Design a network with convolutional layers (kernels of 3x3) to extract spatial features, followed by fully connected layers for regression [7].
- LSTM Architecture: Implement a network with one or more LSTM layers (e.g., 32, 64, or 128 neurons) to capture temporal dynamics, using ReLU or linear activation functions in output layers [55] [7]. A dropout rate of 0.3 is recommended to prevent overfitting.
- STA-LSTM Architecture (Spatio-Temporal Attention LSTM): Combine convolutional layers for spatial feature extraction with LSTM layers equipped with an attention mechanism. The attention mechanism allows the model to focus on the most relevant time steps and spatial locations for making predictions [7].
- PINN Architecture: Construct a fully connected neural network. The key differentiator is the loss function, which is a composite of:
Total Loss = Data Loss + Physics LossThe Data Loss (e.g., Mean Squared Error) quantifies the difference between the model's prediction and the ABM training data. The Physics Loss is the residual of known or hypothesized biological governing equations (e.g., differential equations for cytokine diffusion and decay), ensuring the model's predictions are physically plausible [7] [46] [52].
Model Training & Evaluation:
- Training: Train each model on the preprocessed dataset. For PINNs, this involves minimizing the composite loss function. Use the Adam optimizer for initial fast convergence, potentially switching to SGD for fine-tuning (SWATS strategy) [56].
- Evaluation: Benchmark all models against the held-out test set using metrics such as Mean Squared Error (MSE), R-squared (R²), and Mean Absolute Percentage Error (MAPE) [7].
Workflow Visualization
The following diagram illustrates the integrated experimental workflow, from baseline simulation to surrogate model benchmarking.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational and Biological Resources
| Item Name | Type | Function/Description | Example/Reference |
|---|---|---|---|
| CompuCell3D | Software Platform | Enables the development and execution of agent-based models for simulating multicellular systems, including tissue-level immune responses. | [7] [51] |
| TensorFlow/PyTorch | Programming Framework | Open-source libraries for building and training deep learning models (CNN, LSTM, PINN). Provide flexibility for custom architecture design. | [55] [52] |
| NASA/CALCE Battery Datasets | Benchmark Data | Publicly available time-series degradation data, useful for validating temporal model architectures like LSTM and PINN on physiological degradation analogs. | [52] |
| Google Community Mobility Reports | Epidemiological Covariate Data | Real-world data on human behavior that can be integrated as time-dependent covariates in models (e.g., for tuning parameters like transmission rate in epidemiological PINNs). | [53] |
| Cytokine Panel Assays | Wet-Lab Reagent | Used to experimentally measure cytokine protein concentrations (e.g., via ELISA or multiplex immunoassays) for initial model validation in real-world biological systems. | Not specified in results |
| Laser Doppler Imaging (LDI) | Diagnostic Tool | Provides objective measurement of tissue perfusion, correlating with burn wound healing potential and usable as an input feature or validation metric for predictive models. | [54] |
The pathophysiological response to burn injury is characterized by a complex and prolonged immune reaction, the dynamics of which are critical to patient outcomes [57] [6]. A pivotal early responder in this cascade is the endothelial cell, which recent in silico mechanistic modeling has highlighted as a key parameter determining the intensity and progression of acute inflammation during the critical 0-4 days post-burn [6] [8]. This application note delineates the protocols for quantifying endothelial-related cellular biomarkers and integrating this data with computational models to derive clinically actionable insights for burn patient stratification and therapeutic development.
Quantitative Data on Key Cellular Biomarkers in Burn Injury
Systemic mobilization and local recruitment of specific cell populations are hallmarks of the burn response. The following tables summarize quantitative changes in key cellular biomarkers as identified from clinical and preclinical studies.
Table 1: Dynamics of Circulating Angiogenic Cells (CACs)/Endothelial Progenitor Cells (EPCs) Post-Burn Injury
| Study / Context | CAC/EPC Characterization | Temporal Dynamics Post-Burn | Correlation with Burn Severity |
|---|---|---|---|
| Major Burn (>15% TBSA) [57] | CD133+/KDR+/CD15- | Transient mobilization peaking at 12 hours, returning to baseline by 24-48 hours. | Preceded by a systemic rise in VEGF at 6-12 hours. |
| Human Burn Patients [57] | CD45dim/-/CD133+/CD144+/KDR+ | Significant rise peaking at 24 hours, returning to baseline after 72 hours. | Positive correlation between CAC level and percent TBSA burned. |
| Human Burn Patients (Extensive vs. Smaller Burns) [57] | CD34+/KDR+/acLDL+/lectin+ | Significantly lower CAC count on admission in extensive burns (>25% TBSA); levels rose in all patients, reaching significance by day 5 in extensive burns. | Lower initial counts associated with more extensive injury. |
| Animal Model (30% TBSA) [57] | CD34+/KDR+/acLDL+ | Significant drop during insult, rapid increase to half baseline at 2 hours, stable for 48 hours. | Standardized injury model showing defined mobilization pattern. |
Table 2: Dynamics of Key Inflammatory Cells in the First 96 Hours Post-Burn (Preclinical Data) [6]
| Cell Type | 0h | 24h | 48h | 72h | 96h |
|---|---|---|---|---|---|
| Activated Neutrophils (AN) | – | ↑ | ↓ | – | – |
| Monocytes (M) | – | – | ↑ | – | |
| Macrophages type I (M1) | – | – | – | ↑ | |
| Macrophages type II (M2) | – | – | – | – | |
| Fibroblasts (F) | – | – | – | – | ↑ |
| Myofibroblasts (My) | – | – | – | – |
Symbols: ↑/↓ = Increase/Decrease; / = Growth/Decline; -- = No significant change or data not available.
Experimental Protocols
Protocol for Flow Cytometric Analysis of Circulating Angiogenic Cells (CACs) from Human Peripheral Blood
Principle: This protocol details the isolation of peripheral blood mononuclear cells (PBMCs) and their subsequent characterization via multiparameter flow cytometry to identify and quantify CAC populations in burn patient blood samples [57].
Materials:
- Sodium Heparin or EDTA blood collection tubes
- Ficoll-Paque PLUS density gradient medium
- Phosphate-Buffered Saline (PBS), sterile
- Flow Cytometry Staining Buffer (PBS with 1-2% FBS)
- Fluorescently conjugated monoclonal antibodies: anti-human CD34, CD45, KDR (VEGFR2), CD133
- Appropriate Isotype controls
- Fixation buffer (e.g., 1-4% Paraformaldehyde)
- 40 μm cell strainer
- Flow cytometer with 488nm, 633nm, and 405nm lasers recommended
Procedure:
- Blood Collection and PBMC Isolation: Draw venous blood from burn patients at specified time points (e.g., admission, 12h, 24h, 72h) into heparin or EDTA tubes. Dilute blood 1:1 with PBS. Carefully layer the diluted blood over Ficoll-Paque in a centrifuge tube. Centrifuge at 400-500 x g for 30-35 minutes at 20°C with the brake off. Harvest the opaque PBMC layer at the interface and wash twice with PBS.
- Cell Staining: Resuspend the PBMC pellet in flow cytometry staining buffer. Aliquot approximately 1x106 cells per staining tube. Add predetermined optimal concentrations of fluorescent antibodies (e.g., CD34-FITC, CD45-PerCP, CD133-APC, KDR-PE) to the cell pellets. Include single-stained controls and isotype controls for compensation and gating. Vortex gently and incubate for 30 minutes in the dark at 4°C.
- Wash and Fix: Add 2 mL of staining buffer to each tube, centrifuge at 300 x g for 5 minutes, and decant the supernatant. Repeat the wash step. Resuspend the final cell pellet in 200-300 μL of fixation buffer.
- Data Acquisition and Analysis: Pass cells through a cell strainer into flow cytometry tubes. Acquire data on a flow cytometer, collecting a minimum of 100,000 events per sample. Analyze data using flow cytometry software. Identify CACs using sequential gating: first, lymphocytes/monocytes based on FSC/SSC; second, CD45dim or CD45- population; third, double-positive cells for CD34 and KDR, with or without CD133 [57]. Report results as a percentage of parent population or absolute count after standardization.
Protocol for In Silico Modeling of Post-Burn Immune Response Using an Agent-Based Model (GGH/CPM)
Principle: This protocol describes the setup and execution of a Glazier-Graner-Hogeweg (GGH) or Cellular Potts Model (CPM) to simulate the spatial-temporal dynamics of the acute immune response, with a focus on the role of initial endothelial cell count [6].
Materials:
- Computer workstation with multicore processor and ≥16GB RAM
- Modeling software: CompuCell3D, Morpheus, or equivalent CPM simulation platform
- (Pre)clinical dataset for parameterization and validation (e.g., cell counts, cytokine levels over time) [6]
Procedure:
- Model Domain and Compartmentalization: Define a 2D or 3D simulation lattice representing a cross-section of skin tissue and an adjacent blood vessel compartment. Set boundary conditions (e.g., periodic, constant).
- Agent and Solute Definition:
- Define Cell Agents: Create cell types with specific attributes: Endothelial Cells, Mast Cells, Neutrophils (Resting, Activated), Macrophages (M1, M2). Assign properties: volume, surface area, motility, chemotaxis sensitivity, and secretion profiles.
- Define Soluble Factors (Diffusible): Create fields for pro-inflammatory cytokines (IL-6, IL-8, TNF-α), anti-inflammatory cytokines (IL-10), and inflammation-triggering factors (DAMPs/PAMPs). Set diffusion constants and decay rates.
- Rule Implementation (Hamiltonian/Energy Functions):
- Cell Adhesion: Set adhesion energies to ensure proper tissue architecture (e.g., high adhesion between like-cells, lower adhesion to ECM).
- Chemotaxis: Implement rules where immune cells (Neutrophils, Macrophages) perform biased random walks up concentration gradients of specific chemoattractants (e.g., IL-8, MCP-1).
- Secretion and Signaling: Program cells to secrete solutes based on their state and local environment (e.g., DAMPs from necrotic zones trigger endothelial cells to express adhesion molecules and cytokines).
- Proliferation/Differentiation/Death: Define rules for cell state transitions (e.g., Monocyte -> M1/M2 Macrophage, Endothelial Cell proliferation) based on local solute concentrations and cell-cell contact.
- Parameterization and Initialization: Initialize the simulation by populating the tissue compartment with a defined number of Endothelial Cells and other resident cells. The initial endothelial cell count should be treated as a key input variable. Introduce a "burn zone" with necrotic cells releasing DAMPs. Parameterize the model using the provided (pre)clinical data [6].
- Simulation Execution and Analysis: Run the simulation from day 0 to day 4 post-burn. Track outputs over time: counts of each cell type, spatial distribution of cells, and concentration maps of cytokines. Systematically vary the initial endothelial cell count to analyze its impact on the intensity and duration of the acute inflammatory response [6].
Visualizing Pathways and Workflows
Diagram 1: Integrated pathway from burn injury to in silico modeling, showing key cellular and molecular events.
Diagram 2: Logic flow of the in silico model, illustrating how the initial endothelial cell count drives specific outputs and insights.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for Burn Immune Response Studies
| Item | Function/Application in Research | Example/Specification |
|---|---|---|
| Anti-human CD34 Antibody | Fluorescent labeling of hematopoietic progenitor cells and endothelial precursors for flow cytometry. | Clone: 581 (QIAGEN), Conjugate: FITC, PE. |
| Anti-human KDR (VEGFR2) Antibody | Identification of endothelial lineage cells expressing VEGF receptor 2. | Clone: 7D2-6 (Miltenyi Biotec), Conjugate: PE, APC. |
| Anti-human CD133 Antibody | Labeling of primitive stem/progenitor cells, including a subset of EPCs. | Clone: AC133 (Miltenyi Biotec), Conjugate: APC. |
| Recombinant Human SDF-1α | In vitro chemotaxis assays to study EPC migration and mobilization mechanisms. | Carrier-free, >97% purity. |
| Ficoll-Paque PLUS | Density gradient medium for the isolation of PBMCs from human peripheral blood. | Sterile, ready-to-use solution. |
| CompuCell3D Modeling Software | Open-source simulation environment for constructing and executing GGH/CPM agent-based models. | Version 3.7.5 or higher. |
| Murine Burn Injury Model | Preclinical in vivo system for studying the time-course of immune and EPC responses. | C57BL/6 mice, 30% TBSA full-thickness scald burn [6]. |
Severe burn injuries trigger a complex and prolonged systemic immune response, which is increasingly recognized to be significantly influenced by the gut microbiome. The gastrointestinal tract, the body's largest microbial reservoir, undergoes profound dysbiosis following burn trauma, characterized by a disruption in the composition and function of the gut microbial community [58] [59]. This dysbiosis is not merely a consequence of injury but is an active contributor to post-burn pathophysiology, including systemic inflammation, sepsis, and multiple organ failure [58]. The interplay between gut microbiota and the host's immune system creates a critical axis that can determine clinical outcomes. Traditional methods struggle to capture the complexity of these interactions, but machine learning (ML) approaches are revolutionizing the field by integrating multi-omics data to identify reliable biomarkers and uncover novel mechanistic insights [60] [61]. This protocol details a computational workflow for applying ML to discover gut microbiome-derived biomarkers that correlate with specific burn phenotypes, thereby facilitating the development of personalized diagnostic and therapeutic strategies.
Background
Post-Burn Immune Response and Gut Dysbiosis
A severe burn injury initiates a massive, systemic inflammatory cascade. This response is characterized by the release of pro-inflammatory cytokines such as IL-6, IL-1β, TNF-α, and IL-8, which can lead to systemic inflammatory response syndrome (SIRS) and compromise organ function [6] [59]. Concurrently, the body may enter a state of immunosuppression, increasing susceptibility to infections [62].
The gut is particularly vulnerable in this context. Burn shock and fluid shifts can cause mesenteric ischemia, damaging the intestinal mucosal barrier [58] [59]. This damage, coupled with changes in intestinal motility and mucus secretion, disrupts the homeostatic balance of the gut microbiome, leading to dysbiosis. Key alterations observed post-burn include:
- A reduction in microbial diversity [59].
- A decrease in beneficial genera like Bifidobacterium and Faecalibacterium [58] [59].
- An expansion of potentially pathogenic bacteria from the Proteobacteria phylum [58] [59].
This dysbiosis compromises intestinal barrier integrity, facilitating the translocation of live bacteria and endotoxins (e.g., LPS) into the systemic circulation. This process, often termed "bacterial translocation," is a key event that fuels the persistent inflammatory fire and can precipitate sepsis [58] [59].
The Rationale for Machine Learning
The relationship between gut microbiota, host immunity, and burn progression is not linear but involves high-dimensional, non-linear interactions. ML algorithms are uniquely suited to decode this complexity by:
- Integrating multi-omics data (metagenomics, metabolomics, transcriptomics) with clinical and demographic information [60] [63].
- Identifying complex, non-linear patterns within large-scale datasets that are undetectable by traditional statistical methods [60] [61].
- Discovering biomarkers that can diagnose, prognosticate, or predict responses to interventions, paving the way for precision medicine in burn care [64] [63].
The following diagram illustrates the integrated computational and experimental workflow for identifying gut microbiome-based biomarkers in burn phenotypes.
Materials and Reagents
Research Reagent Solutions
Table 1: Essential research reagents and computational tools for gut microbiome biomarker discovery in burn research.
| Item Name | Function/Application | Specifications/Examples |
|---|---|---|
| Stool DNA Extraction Kit | Isolation of high-quality microbial genomic DNA from fecal samples. | Kits with mechanical lysis for Gram-positive bacteria (e.g., QIAamp PowerFecal Pro DNA Kit). |
| 16S rRNA Gene Primers | Amplification of hypervariable regions for taxonomic profiling. | Primers targeting V3-V4 regions (e.g., 341F/806R). |
| Shotgun Metagenomic Library Prep Kit | Preparation of libraries for whole-genome sequencing of microbial communities. | Enables functional gene analysis (e.g., Illumina Nextera XT DNA Library Prep Kit). |
| RNA Stabilization Reagent | Preservation of RNA integrity in host tissue (e.g., intestinal mucosa). | Prevents degradation for transcriptomic analysis (e.g., RNAlater). |
| Cytokine Multiplex Assay | Quantification of systemic and local inflammatory mediators. | Luminex or ELISA-based panels for IL-6, TNF-α, IL-1β, IL-10. |
| IntelliGenes Pipeline | A specialized ML software for multi-genomic biomarker discovery. | Generates I-Gene scores to rank biomarker importance [64]. |
| SHAP (SHapley Additive exPlanations) | Explainable AI tool for interpreting ML model output. | Quantifies the contribution of each feature (e.g., microbe) to a prediction [64] [61]. |
| Agent-Based Modeling (ABM) Framework | In silico simulation of the post-burn immune response. | Platforms like NetLogo or CompuCell3D for simulating immune cell and cytokine interactions [6] [8]. |
Step-by-Step Protocol
Phase I: Cohort Definition and Multi-Omics Data Acquisition
Objective: To collect a comprehensive dataset from a well-characterized cohort of burn patients.
Cohort Stratification:
- Recruit severe burn patients (e.g., >20% TBSA in adults) and matched controls.
- Collect detailed metadata: age, sex, %TBSA, burn mechanism, comorbidities, medications (especially antibiotics and opioids), and nutritional support [58] [59].
- Stratify patients by outcome phenotypes (e.g., uncomplicated healing, sepsis, multiple organ dysfunction) for supervised ML.
Biospecimen Collection and Omics Profiling:
- Fecal Samples: Collect serial samples (e.g., at admission, 24h, 72h, 1 week) in sterile containers and immediately freeze at -80°C.
- Perform DNA extraction and conduct either:
- 16S rRNA sequencing for cost-effective taxonomic profiling.
- Shotgun metagenomics for high-resolution taxonomic and functional analysis (e.g., identification of microbial genes and pathways) [61].
- Perform DNA extraction and conduct either:
- Blood Samples:
- Fecal Samples: Collect serial samples (e.g., at admission, 24h, 72h, 1 week) in sterile containers and immediately freeze at -80°C.
Phase II: Data Preprocessing and Feature Engineering
Objective: To transform raw data into a structured, analysis-ready format.
Microbiome Data:
- Process raw sequencing reads using QIIME 2 (for 16S) or KneadData/MetaPhlAn (for shotgun data) for quality control, denoising, and taxonomic assignment.
- Generate feature tables of microbial abundances (OTUs or species-level counts).
- Calculate ecological metrics (e.g., Shannon Diversity, Bray-Curtis Dissimilarity) to quantify dysbiosis [61].
Data Integration and Labeling:
- Create a unified data matrix where rows are patients/timepoints and columns are features (microbial taxa, cytokine levels, clinical variables).
- Label each sample according to the burn phenotype of interest (e.g., "Sepsis" vs. "No-Sepsis").
Phase III: Machine Learning for Biomarker Discovery
Objective: To identify a minimal set of gut microbial features predictive of burn phenotypes.
Feature Selection:
- Apply conventional statistical tests (e.g., ANOVA, Kruskal-Wallis) and ML-based methods (e.g., Recursive Feature Elimination) to reduce dimensionality and select the most relevant microbial and host features [64].
Model Training and Validation:
- Implement a suite of ML classifiers. The following performance metrics should be tracked for each model.
Table 2: Key performance metrics for evaluating trained ML models.
Model Primary Application Key Hyperparameters Reported Advantages Random Forest (RF) Robust classification with high-dimensional data. nestimators, maxdepth Handles non-linear data; resists overfitting [64] [63]. Support Vector Machine (SVM) Effective for small sample sizes with high-dimensionality. Kernel (e.g., RBF), C Powerful for distinguishing subtle patterns [64] [63]. XGBoost High-accuracy prediction and winning complex competitions. learningrate, maxdepth High predictive performance on structured data [64]. - Split data into training (e.g., 70%) and hold-out test (e.g., 30%) sets. Use k-fold cross-validation (e.g., k=5) on the training set to tune hyperparameters and avoid overfitting.
- Evaluate final model performance on the untouched test set using metrics: Accuracy, Precision, Recall, and Area Under the ROC Curve (AUC-ROC).
- Implement a suite of ML classifiers. The following performance metrics should be tracked for each model.
Table 2: Key performance metrics for evaluating trained ML models.
Biomarker Interpretation with Explainable AI:
- Apply SHAP analysis to the best-performing model (e.g., Random Forest or XGBoost) [64] [61].
- Calculate I-Gene Scores (as implemented in the IntelliGenes pipeline) to rank the importance of individual microbial features [64].
- Determine if a specific biomarker's association is linked to its overexpression or underexpression in a particular phenotype.
Phase IV: In Silico Mechanistic Modeling and Validation
Objective: To contextualize ML-derived biomarkers within the dynamics of the post-burn immune response.
Agent-Based Model (ABM) Setup:
- Develop an ABM using a framework like the Glazier-Graner-Hogeweg (GGH) model to simulate the tissue environment post-burn [6] [8].
- Define agents: Endothelial cells, neutrophils, macrophages (M1/M2).
- Define solutes/diffusible factors: Pro-inflammatory cytokines (IL-6, IL-8, TNF-α), anti-inflammatory cytokines (IL-10), and bacterial endotoxins (LPS) [6].
Model Integration and Simulation:
- Incorporate the ML-derived biomarkers into the ABM logic. For example, if a specific microbe (e.g., Enterobacteriaceae) is identified as a key biomarker, model its product (e.g., LPS) as a solute that increases endothelial dysfunction and chemotaxis.
- Run simulations to test hypotheses, such as how an increase in a "pathogenic" biomarker influences the dynamics of neutrophil infiltration or the duration of the acute inflammatory phase (days 0-4 post-burn) [6].
- Validate the ABM by ensuring it can recapitulate known clinical dynamics, such as the pivotal role of the initial endothelial cell count in driving inflammation [6] [8].
The signaling pathways connecting gut-derived signals to the systemic immune response, as simulated in the ABM, can be visualized as follows:
Anticipated Results and Analysis
Successful execution of this protocol will yield a ranked list of gut microbial biomarkers (e.g., specific taxa, functional genes, or metabolites) strongly associated with defined burn phenotypes. The ML model is expected to achieve a high AUC-ROC (>0.8) in classifying patients based on their microbiome profile. The SHAP analysis will provide both global and local interpretability, indicating which features were most important overall and for individual patient predictions.
The ABM simulations will offer a mechanistic narrative, showing how these microbial biomarkers potentially influence the trajectory of the immune response. For instance, the model might demonstrate that an early bloom of Enterobacteriaceae predicts sustained high levels of IL-6 in the simulation, leading to a "sepsis" phenotype. This integrated in silico approach generates testable hypotheses for subsequent wet-lab validation, such as in vitro assays with specific bacterial strains or in vivo studies in gnotobiotic mouse models of burn injury.
This application note presents a robust, ML-driven framework for discovering gut microbiome-based biomarkers in severe burn injuries. By integrating multi-omics data with explainable AI and in silico mechanistic modeling, researchers can move beyond correlation towards a causal understanding of how the gut microbiome shapes post-burn immunity. The biomarker signatures identified through this pipeline hold significant promise for enabling early risk stratification, guiding targeted microbial therapies (e.g., probiotics, FMT), and ultimately improving personalized care and outcomes for burn patients.
Conclusion
In silico mechanistic modeling has emerged as a transformative tool for unraveling the complexities of the post-burn immune response. By integrating foundational immunology with advanced computational methodologies, these models have successfully identified pivotal regulators, such as the initial endothelial cell count, and provided novel insights into systemic complications affecting the liver and gut. Future directions must focus on developing multi-scale, multi-organ models that can seamlessly integrate diverse data types, from genomics to clinical vitals. The ultimate challenge and opportunity lie in translating these powerful in silico predictions into targeted clinical interventions, paving the way for personalized medicine in burn care and significantly improving patient outcomes.
References
- 1. Systemic immune response of burns from the acute to chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11184575/]
- 2. Variation of Pro- and Anti-Inflammatory Factors in Severe Burns [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562903/]
- 3. Decoding burn trauma: biomarkers for early diagnosis of burn ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-024-00707-5]
- 4. Temporal changes in the protein cargo of extracellular ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1596598/full]
- 5. Mathematical model of the inflammatory response to acute ... [https://www.nature.com/articles/s41540-024-00473-y]
- 6. An in silico modeling approach to understanding the dynamics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10859697/]
- 7. Neural networks enhancing burn wound healing predictions [https://www.sciencedirect.com/science/article/pii/S1877750325000705]
- 8. An in silico modeling approach to understanding the ... [https://pubmed.ncbi.nlm.nih.gov/38348032/]
- 9. Burn-injured skin is marked by a prolonged local acute ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.1034420/full]
- 10. Non-monotonic response of macrophages to mechanical ... [https://cmbl.biomedcentral.com/articles/10.1186/s11658-025-00764-0]
- 11. Lyophilized horizontal platelet rich fibrin promotes the ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1666265/full]
- 12. Researchers discover neutrophils that strengthen skin barrier [https://www.news-medical.net/news/20250319/Researchers-discover-neutrophils-that-strengthen-skin-barrier.aspx]
- 13. Isosteviol reduces the acute inflammatory response after ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576922000935]
- 14. Burn injury - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC7224101/]
- 15. Variation of Pro- and Anti-Inflammatory Factors in Severe ... [https://pubmed.ncbi.nlm.nih.gov/41155423/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1R3QZIpFgeaXQJt8K9w8_oRDFOUkgIho18PKxDpWTR1UFZLoNX&fc=None&ff=20251030161421&v=2.18.0.post22+67771e2]
- 16. Predictors of Early Onset Multiple Organ Dysfunction in ... [https://www.nature.com/articles/s41598-018-29158-3]
- 17. OCCURRENCE OF MULTI-ORGAN DYSFUNCTION IN ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3731402/]
- 18. Associations between clinical characteristics and the ... [https://www.sciencedirect.com/science/article/abs/pii/S0305417918303279]
- 19. Quantitative Evaluation of Burn Injuries Based on Electrical ... [https://www.mdpi.com/1424-8220/21/4/1496]
- 20. Precision diagnosis of burn injuries using imaging and ... [https://www.nature.com/articles/s41598-025-92096-4]
- 21. Cell studio: A platform for interactive, 3D graphical simulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6481718/]
- 22. Agent-based model demonstrates the impact of nonlinear, ... [https://elifesciences.org/reviewed-preprints/91924v2]
- 23. PLOS Computational Biology [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1008451]
- 24. 使用U-Net神经网络架构作为代理模型对基于Cellular-Potts ... [https://blog.csdn.net/u013524655/article/details/147691658]
- 25. A Surrogate Model for Predicting Application Runtime in ... [https://arxiv.org/html/2511.11111v1]
- 26. A Scalable Data-Driven Surrogate Model for 3D Dynamic ... [https://www.mdpi.com/1996-1073/18/13/3356]
- 27. The Complexity of the Post-Burn Immune Response [https://www.mdpi.com/2073-4409/12/3/345]
- 28. Physics-Informed Neural Networks for Fast 3D ... [https://link.springer.com/article/10.1007/s13369-025-10602-2]
- 29. Transcriptomics, metabolomics, and in-silico drug ... [https://www.nature.com/articles/s42003-023-04964-2]
- 30. Transcriptomics combined with metabolomics analysis of the ... [https://atm.amegroups.org/article/view/95666/html]
- 31. Integrating transcriptomics and metabolomics to analyze ... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2023.1146525/full]
- 32. Visual analysis of multi-omics data [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2024.1395981/full]
- 33. Editorial: New approach methods in immunology [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1488534/full]
- 34. A machine learning model for improving mouse to human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12396630/]
- 35. Modeling early thermal injury using an ex vivo human skin ... [https://www.sciencedirect.com/science/article/abs/pii/S0305417920305118]
- 36. Machine Learning–Based Prediction of Delirium and Risk ... [https://formative.jmir.org/2025/1/e65190]
- 37. Charts vs. Tables: When to Use One Over the Other? [https://wpdatatables.com/charts-vs-tables/]
- 38. Table vs. Chart: Precision or Visual Impact – What's Right ... [https://ppcexpo.com/blog/table-vs-chart]
- 39. 7 Best Comparison Charts for Effective Data Visualization [https://ninjatables.com/types-of-comparison-charts/?srsltid=AfmBOop47M9e2GK806HglxXPUKLDuhBPx8wBV6dLeH1ocxJYWtzljNjz]
- 40. Advances in Surrogate Modeling for Biological Agent-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12047901/]
- 41. Immune digital twins for complex human pathologies [https://www.nature.com/articles/s41540-024-00450-5]
- 42. Strategies for overcoming data scarcity, imbalance, and ... [https://www.nature.com/articles/s41598-024-59958-9]
- 43. Recent Advances in Experimental Burn Models [https://www.mdpi.com/2079-7737/10/6/526]
- 44. Wound Healing, Metabolite Profiling, and In Silico Studies ... [https://www.mdpi.com/1467-3045/46/10/694]
- 45. A Modular Mathematical Model of the Immune Response ... [https://www.mdpi.com/1999-4915/17/5/589]
- 46. Using Physics-Informed Neural Networks for Modeling ... [https://www.mdpi.com/2227-7390/13/10/1664]
- 47. Physics-informed neural networks for physiological signal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308510/]
- 48. Understanding Physics-Informed Neural Networks [https://www.mdpi.com/2673-2688/5/3/74]
- 49. A physics-informed neural network for modeling fracture ... [https://arxiv.org/abs/2507.07272]
- 50. Pan-Immune Inflammation Value as a Novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471703/]
- 51. Neural networks enhancing burn wound healing predictions [https://pure.amsterdamumc.nl/en/publications/from-simulations-to-surrogates-neural-networks-enhancing-burn-wou/]
- 52. Integrated Framework of LSTM and Physical-Informed Neural Network for Lithium-Ion Battery Degradation Modeling and Prediction [https://www.mdpi.com/2673-2688/6/7/149]
- 53. Physics-informed deep learning for infectious disease ... [https://arxiv.org/html/2501.09298v1]
- 54. Deep Learning–Assisted Burn Wound Diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8686480/]
- 55. Guide to Long ( Short ) Term in... | Medium Memory LSTM models [https://abdullahsaka.medium.com/long-short-term-memory-lstm-model-in-stock-prediction-d0e1c93717b3]
- 56. CNN-LSTM optimized with SWATS for accurate state-of-charge estimation in lithium-ion batteries considering internal resistance | Scientific Reports [https://www.nature.com/articles/s41598-025-15597-2]
- 57. Endothelial progenitor cells and burn injury [https://pmc.ncbi.nlm.nih.gov/articles/PMC4964096/]
- 58. The role and therapeutic potential of gut microbiome in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9714625/]
- 59. GUT MICROBIAL CHANGES AND THEIR CONTRIBUTION TO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8292439/]
- 60. Advanced computational tools, artificial intelligence and ... [https://pubmed.ncbi.nlm.nih.gov/40303946/]
- 61. Smart Microbiomes: How AI Is Revolutionizing ... [https://www.mdpi.com/2306-5354/12/9/944]
- 62. Burns [https://www.sciencedirect.com/science/article/abs/pii/S0305417924002237]
- 63. Machine Learning in Biomarker Discovery for Precision ... [https://esmed.org/machine-learning-in-biomarker-discovery-for-precision-medicine/]
- 64. IntelliGenes: a novel machine learning pipeline for biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10739559/]