Langerhans Cells in 3D Skin Models: Function, Culture, and Applications in Immunology Research
This article provides a comprehensive guide for researchers and pharmaceutical developers on the critical role and study of Langerhans cells (LCs) within in vitro skin models.
Langerhans Cells in 3D Skin Models: Function, Culture, and Applications in Immunology Research
Abstract
This article provides a comprehensive guide for researchers and pharmaceutical developers on the critical role and study of Langerhans cells (LCs) within in vitro skin models. It begins by exploring the fundamental immunobiology of LCs as skin-resident antigen-presenting cells and their necessity in constructing physiologically relevant skin equivalents. The core methodological section details current protocols for generating, integrating, and maturing LCs in 2D co-cultures, 3D reconstructed human epidermis (RHE), and full-thickness skin models. We address common challenges in LC viability, phenotype drift, and functional assays, offering troubleshooting and optimization strategies. Finally, the article evaluates how these LC-containing models perform against traditional methods and animal models for applications in immunotoxicity, sensitization testing (like OECD TG 442E), and inflammatory disease research, highlighting their validation status and translational potential.
Understanding Langerhans Cells: The Skin's Sentinel Immune Population
This technical guide defines the core characteristics of Langerhans cells (LCs), the resident dendritic cells (DCs) of the epidermis. Within the broader thesis on LC function in in vitro skin models for immunotoxicity and drug development, a precise understanding of LC origin, defining markers, and lifespan is critical. These properties directly influence the predictive validity of reconstructed human epidermis (RHE) and full-thickness skin models, where the presence, maturity, and longevity of LCs determine immunological responses to topical compounds, allergens, and sensitizers.
Origin: Embryonic and Postnatal Development
LCs originate from two distinct waves of development, a paradigm essential for designing in vitro models that accurately reflect human skin biology.
| Developmental Origin | Timeframe | Progenitor Cell | Key Regulating Cytokine/Factor | Persistence in Adult Skin |
|---|---|---|---|---|
| Primordial/Embryonic | Fetal development | Yolk-sac derived erythro-myeloid progenitors (EMPs) | TGF-β1 (absolute requirement) | Self-renewing, long-lived pool. Maintains epidermal residence independently of bone marrow. |
| Postnatal/Monocyte-Derived | Post-birth, under inflammatory conditions | Circulating monocytes (from bone marrow HSCs) | IL-34, GM-CSF, TGF-β1 | Replenishes LC pool upon severe depletion. Contributes to in vitro LC generation from CD14+ monocytes. |
Thesis Context: For in vitro skin models, the source of LCs dictates functionality. Models using monocytes (CD14+) recapitulate the inflammatory, inducible pathway, while models incorporating embryonic stem cell or induced pluripotent stem cell (iPSC)-derived LCs aim to mimic the self-renewing, resident population.
Experimental Protocol: Fate-Mapping LC Origin
- Objective: To distinguish embryonic-derived LCs from monocyte-derived LCs in a murine model or in vitro system.
- Method:
- Lineage Tracing: Use Cx3cr1-CreER;R26R-tdTomato mice. Pulse tamoxifen at embryonic day (E) 7.5-8.5 to label yolk-sac derived EMPs. Analyze newborn and adult skin for tdTomato+ LCs (EpCAM+, CD11c+, MHC II+).
- Parabiosis or Bone Marrow Transplant: Surgically join a wild-type and a congenic (CD45.1/45.2) mouse (parabiosis) or lethally irradiate a mouse and transplant congenic bone marrow. Monitor LC chimerism over time via flow cytometry. Embryonic LCs remain host-derived; inflammatory turnover leads to donor-derived LCs.
- In Vitro Modeling: Differentiate human CD14+ monocytes with GM-CSF, IL-4, and TGF-β1 for 5-7 days to generate LC-like cells. Compare their transcriptome (RNA-seq) and function (antigen uptake/presentation) to LCs isolated directly from human skin.
Defining Surface and Intracellular Markers
LC identification requires a combination of markers, critical for their isolation and characterization in in vitro models.
| Marker | Alternative Name | Expression | Primary Function | Role in LC Identification |
|---|---|---|---|---|
| CD1a | R4, T6 | High, surface | Presentation of lipid antigens to T cells (e.g., microbial lipids, self-glycolipids). | Primary defining marker. Distinguishes LCs from dermal DCs and macrophages in human skin. |
| Langerin | CD207 | High, intracellular & surface | C-type lectin receptor; induces Birbeck granule formation; antigen capture. | Specific marker. Intracellular staining identifies Birbeck granules; surface staining identifies mature, stimulatory LCs. |
| MHC Class II | HLA-DR, DP, DQ (human) | Constitutively high, surface | Presentation of peptide antigens to CD4+ T cells. | Maturation/Activation Marker. Expression increases and stabilizes upon activation/migration. |
| EpCAM | CD326, Ber-EP4 | High, surface | Epithelial cell adhesion molecule; maintains LC in epidermis. | Residence Marker. Used for high-purity LC isolation from epidermal cell suspensions. |
| E-Cadherin | CD324 | High (resident state), surface | Adhesion to keratinocytes via homophilic binding. | Residence Marker. Downregulated upon activation to permit migration. |
Thesis Context: In in vitro skin models, the expression profile (e.g., CD1a+/Langerin+/MHC IIlow for resident vs. MHC IIhigh for activated) is a key quality control metric. It determines the model's readiness for immunomodulation assays.
Experimental Protocol: Multicolor Flow Cytometry for LC Phenotyping in RHE
- Objective: To quantify and phenotype LCs in a 3D reconstructed human epidermis model.
- Method:
- Tissue Dissociation: Incubate RHE in Dispase II (2.4 U/mL, 37°C, 1-2 hrs) to separate epidermis. Then dissociate epidermal sheet into single-cell suspension using Trypsin/EDTA or a gentle dissociation enzyme cocktail.
- Antibody Staining: Stain cells with viability dye (e.g., Zombie NIR), then extracellular antibodies: anti-CD45 (hematopoietic lineage), anti-CD3/CD19 (exclude lymphocytes), anti-CD1a-PE, anti-CD207/Langerin-APC, anti-HLA-DR-BV711, anti-EpCAM-FITC. For intracellular Langerin, permeabilize with saponin-based buffer prior to staining.
- Acquisition & Analysis: Acquire on a flow cytometer. Gate: Single, live, CD45+, Lineage-, EpCAM+ → Analyze CD1a and Langerin co-expression. Mean Fluorescence Intensity (MFI) of HLA-DR indicates activation state.
Lifespan and Turnover Dynamics
LC longevity is a key parameter affecting the durability of immune responses in in vitro models.
| State/Condition | Estimated Lifespan/Turnover Rate | Regulating Factors | Experimental Evidence |
|---|---|---|---|
| Steady-State (Resident) | ~50-60 days (murine); Estimated months in humans. | Local TGF-β1, IL-34, and E-Cadherin-mediated keratinocyte interactions maintain survival and immobility. | Fate-mapping shows minimal monocyte contribution in undisturbed skin. BrdU label-retaining studies show slow turnover. |
| Inflammatory/Activated | Days to weeks post-migration. | LC migration to lymph nodes is triggered by TNF-α, IL-1β, and downregulation of E-Cadherin. | UV-induced depletion leads to repopulation from peripheral monocytes within 14-21 days. |
| In Vitro (Monocyte-Derived) | Culture-dependent; typically 5-7 day differentiation, viable for 1-2 weeks. | Requires GM-CSF, IL-4, and TGF-β1. Removal of TGF-β1 leads to loss of LC phenotype. | Cells begin expressing CD1a and Langerin by day 5. Phenotype is stable for several days in cytokine-maintained culture. |
Experimental Protocol: Measuring LC Turnover In Vivo
- Objective: To determine the half-life and replacement kinetics of LCs.
- Method (Murine Model):
- Pulse-Chase with EdU/BrdU: Administer EdU (5-ethynyl-2’-deoxyuridine) in drinking water for 2 weeks to label dividing progenitor cells and newly generated LCs.
- Chase Period: Switch to normal water. Sacrifice cohorts of mice at 0, 2, 4, 8, and 12 weeks post-EdU.
- Analysis: Prepare epidermal sheets, stain for LC markers (Langerin) and EdU (click-chemistry). Quantify the percentage of Langerin+ cells that are EdU+ over time. A slow decline indicates a long-lived, self-renewing population. A rapid decline followed by an EdU- phase suggests replacement from an unlabeled source (monocytes).
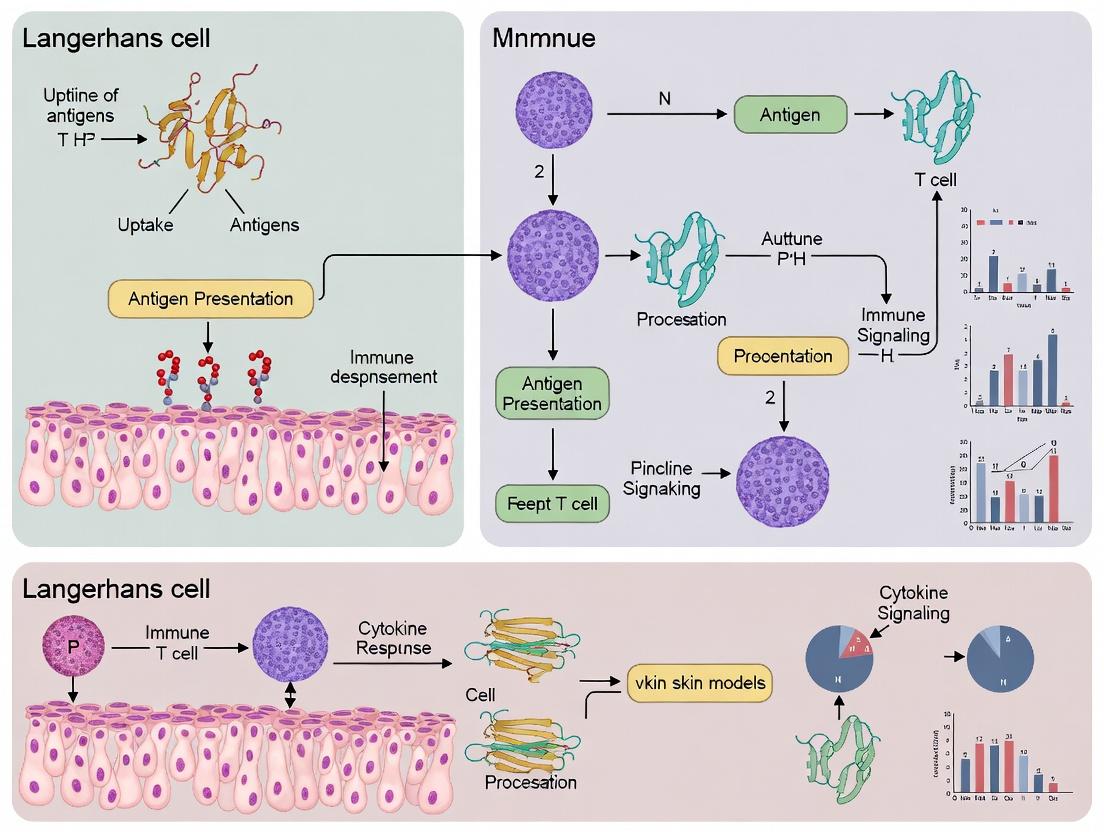
Visualization: LC Development and Activation Pathways
Title: Langerhans Cell Lifecycle and Key Regulatory Signals
The Scientist's Toolkit: Key Reagents for LC Research
| Reagent/Material | Function in LC Research | Example Product/Catalog # |
|---|---|---|
| Recombinant Human TGF-β1 | Essential cytokine for inducing and maintaining the LC phenotype from progenitors or monocytes in vitro. | PeproTech, 100-21 |
| Recombinant Human GM-CSF & IL-4 | Standard cytokine cocktail for generating dendritic cells/LCs from CD14+ monocytes. | Miltenyi Biotec, GM-CSF: 130-093-868, IL-4: 130-093-922 |
| Anti-human CD1a Antibody (clone HI149) | Primary surface marker for identification and isolation of human LCs via flow cytometry or IHC. | BioLegend, 300102 |
| Anti-human Langerin/CD207 Antibody (clone 929F3) | Specific intracellular/surface marker for Birbeck granules and LC identification. | Dendritics, DDX0362 |
| Dispase II (Neutral Protease) | Enzymatic separation of epidermis from dermis or 3D RHE models for LC isolation. | Sigma-Aldrich, D4693 |
| EpCAM MicroBeads (human) | Magnetic-activated cell sorting (MACS) for high-purity isolation of LCs from epidermal cell suspensions. | Miltenyi Biotec, 130-061-101 |
| MHC Class II Tetramers | Functional assay to measure antigen-specific CD4+ T cell activation by LCs. | NIH Tetramer Core Facility or custom synthesis |
| Reconstructed Human Epidermis (RHE) | In vitro 3D model containing keratinocytes and Langerhans cells (LC-RHE) for sensitization testing. | MatTek, EpiDermFT with LCs (EFT-400) |
This whitepaper provides a technical examination of the key immunological functions of Langerhans cells (LCs)—antigen uptake, processing, migration, and T-cell priming—within the context of in vitro skin models. As engineered human skin equivalents become pivotal for research and drug development, understanding and accurately modeling LC biology in vitro is critical. This guide details quantitative benchmarks, experimental protocols, and essential tools for researchers aiming to replicate and study these functions.
Langerhans cells, the resident dendritic cells of the epidermis, are the sentinels of cutaneous immunity. In in vitro skin models, such as reconstructed human epidermis (RHE) or full-thickness skin models incorporating LCs (e.g., LC-RHE), their functional competence validates the model's immunological relevance. This paper deconstructs each key function, providing a framework for their assessment in a research setting.
Antigen Uptake
LCs continuously sample their environment via multiple mechanisms.
Mechanisms and Quantitative Assessment
Primary Uptake Pathways:
- Receptor-Mediated Endocytosis: Utilizes C-type lectin receptors (e.g., langerin/CD207, DEC-205/CD205) and Fc receptors.
- Phagocytosis: For larger particles (>0.5 µm) like bacteria or latex beads.
- Macropinocytosis: Constitutive, fluid-phase uptake of solutes and pathogens.
Table 1: Quantitative Parameters for Antigen Uptake in LCs In Vitro
| Parameter | Typical Assay | Readout | Benchmark (Human LCs, in vitro) |
|---|---|---|---|
| FITC-Dextran Uptake (Macropinocytosis) | Incubation with FITC-dextran (40-70 kDa), 37°C vs. 4°C control. | Flow cytometry (MFI) or confocal microscopy. | >10-fold increase in MFI at 37°C vs. 4°C control within 60 min. |
| Latex Bead Phagocytosis | Incubation with fluorescent, carboxylated latex beads (0.5-1.0 µm). | Flow cytometry (% bead+ cells) or imaging (beads/cell). | 60-80% of LCs phagocytose >3 beads after 2-4 hours. |
| Langerin-mediated Uptake | Incubation with langerin-specific ligand (e.g., anti-langerin Ab). | Internalization assay via Ab staining (surface vs. total). | >50% ligand internalization within 30-60 min. |
Experimental Protocol: FITC-Dextran Uptake Assay
Purpose: To measure constitutive macropinocytic activity. Materials: LC-containing skin model, FITC-dextran (70 kDa, 1 mg/mL in assay medium), ice-cold PBS + 2% FBS (staining buffer), 4% PFA. Procedure:
- Preparation: Rinse models twice with pre-warmed, serum-free culture medium.
- Uptake: Add FITC-dextran solution to models. Incubate at 37°C, 5% CO2 for 45 minutes. Include a control plate kept at 4°C to inhibit active uptake.
- Termination: Wash models 3x vigorously with ice-cold PBS to stop uptake and remove surface-bound dextran.
- LC Isolation & Analysis: For RHE models, enzymatically digest (dispase/ trypsin-EDTA) to isolate LCs. Quench with cold buffer.
- Flow Cytometry: Stain cells for CD45, CD1a, and/or langerin. Gate on live, CD45+ CD1a+ LCs. Analyze FITC signal (MFI) and compare 37°C vs. 4°C control.
Antigen Processing
Internalized antigens are degraded into peptides within the endosomal-lysosomal system and loaded onto MHC molecules.
Pathways and Key Enzymes
- MHC Class II Pathway: Antigens are proteolytically cleaved in late endosomes/lysosomes (involving cathepsins S, L, D). The invariant chain (Ii) is degraded, leaving CLIP, which is exchanged for antigenic peptide via HLA-DM, resulting in surface pMHC-II.
- MHC Class I Cross-Presentation (LC specialty): Extracellular antigens are channeled into a specialized cytosolic or vacuolar pathway for proteasomal degradation, followed by TAP-dependent loading onto MHC-I in the ER or endosomes.
Table 2: Markers of Antigen Processing in LCs
| Process | Key Marker/Method | Detection | Interpretation |
|---|---|---|---|
| Lysosomal Activity | Lysotracker Red Dye | Flow Cytometry / Confocal | High MFI indicates mature lysosomal compartment. |
| MHC-II Maturation | Staining for HLA-DR vs. HLA-DM | Flow Cytometry (co-localization) | Increased HLA-DM co-localization signifies active loading compartments. |
| Proteolytic Activity | DQ-OVA (self-quenched fluorescent substrate) | Flow Cytometry (Green MFI) | Increased fluorescence indicates proteolytic cleavage of antigen. |
Experimental Protocol: DQ-Ovalbumin Processing Assay
Purpose: To visualize and quantify proteolytic degradation of antigen. Materials: LC-containing skin model, DQ Ovalbumin (10 µg/mL in medium), control native OVA, ice-cold PBS. Procedure:
- Uptake: Pulse models with DQ-OVA or control OVA for 60 min at 37°C.
- Chase: Replace with fresh, antigen-free medium and incubate for 0, 30, 90, 180 min (chase periods).
- Termination: Wash models with ice-cold PBS at each time point.
- Analysis: Isolate LCs enzymatically. Analyze by flow cytometry (FITC channel). DQ-OVA fluorescence increases proportionally with proteolytic degradation. Plot MFI over chase time to generate a processing kinetics curve.
Diagram 1: MHC Class II Antigen Processing Pathway in LCs
Migration
Upon activation, LCs downregulate E-cadherin, upregulate CCR7, and migrate via the dermis to draining lymph nodes.
Modeling MigrationIn Vitro
Key Chemokines: CCL19 and CCL21 (ligands for CCR7) are the primary drivers. Assay Types: Transwell migration assays using skin model-derived LCs or integrated model systems.
Table 3: LC Migration Assay Parameters and Benchmarks
| Assay Type | Chemokine (Concentration) | Readout | Typical Efficacy (Activated LCs) |
|---|---|---|---|
| Transwell (Isolated LCs) | CCL19/CCL21 (100-300 ng/mL) in lower chamber. | % Migrated Cells (Flow Count) | 15-30% migration over 18-24 hours. |
| 3D Model to Medium | CCL19/CCL21 in surrounding medium. | LC Count in Medium (ELISA for CD1a) | 2-5% of total LCs emigrate over 48-72h. |
| Integrity Marker | E-cadherin Expression (Pre/Post) | Flow Cytometry (MFI) | >50% downregulation after 24h activation. |
Experimental Protocol: Transwell Migration Assay for Isolated LCs
Purpose: To quantify CCR7-mediated chemotaxis. Materials: 24-well transwell plates (5.0 µm pore), recombinant human CCL19/CCL21, migration medium (RPMI + 0.5% HSA), Calcein-AM. Procedure:
- LC Isolation: Isolate LCs from activated (e.g., TNF-α + IL-1β treated for 24h) and control skin models.
- Labeling: Resuspend LCs at 1x10^6/mL, label with Calcein-AM (1 µM, 30 min, 37°C).
- Setup: Add 600 µL of migration medium ± chemokine (250 ng/mL) to lower chamber. Place 100 µL of cell suspension in upper chamber.
- Migration: Incubate for 3 hours at 37°C.
- Quantification: Collect cells from lower chamber. Count fluorescent cells using a plate reader or flow cytometry with counting beads. Calculate % migration = (number migrated / number input) * 100.
Diagram 2: Key Steps in LC Migration Activation
T-Cell Priming
The culmination of LC function is the presentation of antigenic peptides to naïve T cells, initiating adaptive immunity.
The Immunological Synapse
LCs provide three key signals:
- Signal 1: Peptide-MHC (pMHC) engagement with the T-cell receptor (TCR).
- Signal 2: Co-stimulation (e.g., CD80/CD86 binding to CD28).
- Signal 3: Cytokine polarization (e.g., IL-12 for Th1, IL-23 for Th17).
Experimental Protocol: Allogeneic Mixed Leukocyte Reaction (MLR)
Purpose: To measure the ability of LCs to prime naïve T cell proliferation and differentiation. Materials: Isolated LCs (from skin model, CD1a+ sorted), allogeneic naïve CD4+ T cells (from peripheral blood, CD45RA+ sorted), U-bottom 96-well plates, CFSE, anti-CD3/28 beads (positive control), cytokine ELISA/CBA kits. Procedure:
- LC Preparation: Treat LCs with or without antigen (e.g., 10 µg/mL TT peptide) for 4-6 hours. Irradiate (30 Gy) or treat with mitomycin C to prevent LC proliferation.
- T-cell Labeling: Label purified naïve T cells with CFSE (2.5 µM, 10 min).
- Co-culture: Plate LCs in titrated numbers (e.g., 1x10^3 to 1x10^4) with a constant number of T cells (1x10^5) in 200 µL medium. Include T-cell only and positive control wells.
- Incubation: Culture for 5-7 days.
- Analysis:
- Proliferation: Analyze CFSE dilution by flow cytometry on day 5.
- Phenotype: On day 6, re-stimulate cells with PMA/ionomycin for 4-6h, add protein transport inhibitor, and stain intracellularly for IFN-γ (Th1), IL-4 (Th2), IL-17A (Th17).
- Cytokines: Collect supernatant on day 3 (early) and day 5 (late) for ELISA (e.g., IL-2, IFN-γ, IL-17).
Table 4: Key Reagent Solutions for LC-T Cell Priming Assays
| Reagent | Supplier Examples | Function in Assay |
|---|---|---|
| Recombinant Human GM-CSF & IL-4 | PeproTech, R&D Systems | Differentiation and maintenance of monocyte-derived LCs (MoLCs) for control experiments. |
| Recombinant Human FLT3-Ligand | Miltenyi Biotec, BioLegend | Generation of CD34+-derived LCs, more closely resembling primary LCs. |
| Anti-Human Langerin (CD207) Antibody | Beckman Coulter, Dendritics | Identification and sorting of primary LCs. |
| HLA-DR/DP/DQ Antibodies | BioLegend, BD Biosciences | Blocking antibodies to confirm MHC-II-restricted presentation. |
| CFSE Cell Division Tracker | Thermo Fisher Scientific | Fluorescent dye to track T-cell proliferation cycles. |
| LIVE/DEAD Fixable Viability Dyes | Thermo Fisher Scientific | Exclusion of dead cells in flow cytometry for clean analysis. |
| Mouse Anti-Human CD1a MicroBeads | Miltenyi Biotec | Magnetic isolation of LCs from digested skin models. |
Diagram 3: Three-Signal Model of LC-Mediated T-Cell Priming
Faithfully replicating the key functions of LCs—antigen uptake, processing, migration, and T-cell priming—in in vitro skin models is a stringent but achievable goal. The quantitative benchmarks and detailed protocols provided here serve as a foundational toolkit for researchers. Mastering these assays allows for the development of more physiologically relevant skin models, enhancing their predictive value in immunotoxicity testing, vaccine development, and inflammatory skin disease research. Future directions include integrating more complex cytokine milieus, neural components, and microbiota to further refine these functional readouts.
The study of cutaneous immunology relies on accurate in vitro models. This whitepaper, framed within a broader thesis on Langerhans cell (LC) function, argues that traditional static monolayer keratinocyte cultures fail to replicate the dynamic immunological microenvironment of human skin. We detail the technical limitations, present current comparative data, and provide advanced protocols to bridge this gap, emphasizing the necessity of incorporating flow, immune components, and 3D architecture for meaningful research in dermatology and immunotoxicology.
Langerhans cells (LCs), the resident antigen-presenting cells of the epidermis, function within a complex, stratified tissue. Their maturation, migration, and immunoregulatory capabilities are dictated by a triad of signals: keratinocyte-derived cytokines, biomechanical forces, and positional cues within the epidermal layers. Static, two-dimensional (2D) cultures of primary keratinocytes or immortalized lines (e.g., HaCaT) lack these critical elements, creating an "immunological gap" between in vitro observations and in vivo physiology. This gap fundamentally limits research into allergic contact dermatitis, psoriasis, cutaneous drug delivery, and LC-mediated tolerance.
Quantitative Limitations of Static Cultures
The table below summarizes key immunological parameters deficient in static keratinocyte cultures compared to in vivo epidermis and advanced in vitro models.
Table 1: Immunological Parameter Comparison Across Models
| Parameter | In Vivo Human Epidermis | Static 2D Keratinocyte Culture | Advanced 3D Epidermal Model (with LCs) |
|---|---|---|---|
| Stratification & Barrier | Fully stratified, functional cornified layer | Monolayer, no effective barrier | Multi-layered, developing cornified envelope |
| LC Network Integrity | Dense, dendritic network, ~700 LCs/mm² | Absent or randomly added, no network | Incorporated, can form network |
| Cytokine Gradient | Physiological basolateral-to-apical gradients | Homogeneous distribution | Can be established in air-liquid interface (ALI) models |
| Mechanical Stress | Constant basal layer tension, shear stress | None | Present at basal layer in some dynamic systems |
| LC Migration | Efficient upon activation (e.g., TNF-α) | Aberrant, no directed migration | Can be reconstituted (e.g., towards medium) |
| Key Signaling (e.g., TGF-β) | High TGF-β1 maintains LC homeostasis | Variable, often low | Can be supplemented to maintain LC phenotype |
| Predictive Value (Sensitization) | N/A | Low (~60% accuracy) | High (>90% accuracy in validated tests) |
Core Experimental Protocols
Protocol 3.1: Generation of a Full-Thickness Skin Equivalent with Integrated LCs
This protocol creates a 3D model incorporating fibroblasts, keratinocytes, and CD34+ progenitor-derived LCs.
Materials:
- Collagen Type I from rat tail (or commercial dermal equivalent kit)
- Normal Human Dermal Fibroblasts (NHDFs)
- Normal Human Epidermal Keratinocytes (NHEKs)
- CD34+ Hematopoietic Progenitor Cells (from cord blood or bone marrow)
- Differentiation Cytokines: Recombinant human GM-CSF, IL-4, TGF-β1, BMP-7
- Transwell inserts (porous membrane, 0.4 μm pore size, 24-well format)
- Stratification Medium: Keratinocyte serum-free medium (KSFM) supplemented with Ca²⁺ (1.2 mM), ascorbic acid (50 μg/mL), and other factors to promote cornification.
Method:
- Dermal Equivalent: Mix NHDFs (2 x 10⁵ cells/mL) with neutralized collagen type I (2 mg/mL). Plate 500 μL per insert in a 24-well plate. Incubate (37°C, 5% CO₂) for 48h for contraction and matrix maturation.
- LC Differentiation: Differentiate CD34+ progenitors in medium containing GM-CSF (100 ng/mL), IL-4 (50 ng/mL), and TGF-β1 (10 ng/mL) for 5-7 days to generate LC precursors (CD1a⁺, langerin⁺).
- Seeding: Resuspend LC precursors with NHEKs (2:1 keratinocyte:LC ratio, total 5 x 10⁵ cells/insert) in KSFM. Seed the cell mixture onto the contracted dermal equivalent.
- Air-Liquid Interface (ALI): After 48h of submerged culture, raise the inserts to establish an ALI by removing the apical medium. Feed basally with stratification medium, changing every 2-3 days.
- Maturation: Culture at ALI for 10-14 days to allow full epidermal stratification and LC integration. Confirm by histology (H&E) and immunohistochemistry (CD1a, langerin).
Protocol 3.2: Assessing LC Migration in a Dynamic Flow System
This protocol measures LC emigration from an epidermal model under controlled flow, mimicking lymphatics.
Materials:
- 3D Epidermal Model (from Protocol 3.1).
- Flow Chamber System (commercial or custom).
- Chemoattractant Medium: Containing CCL19/MIP-3β (100 ng/mL) and/or TNF-α (10 ng/mL).
- Live-Cell Imaging Setup with environmental control.
Method:
- Stimulation: Treat the 3D model apically with a sensitizer (e.g., 1% DNFB in acetone:olive oil) or TNF-α (10 ng/mL) for 24h.
- Setup: Place the model in the flow chamber. Establish a unidirectional, low-shear flow (0.02 dyne/cm²) of warmed chemoattractant medium across the basal side.
- Image Acquisition: Use time-lapse microscopy to image the basal chamber every 15 minutes for 24-48h.
- Quantification: Track emigrated CD1a⁺ (fluorescently labeled) cells. Calculate metrics: total emigrated cells, migration velocity, and directional persistence.
Visualizing Key Concepts and Pathways
Title: Immunological Gap Between Static and Dynamic Skin Models
Title: Key Signaling Pathways Governing LC Homeostasis and Migration
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents for Advanced Cutaneous Immunology Models
| Item | Function & Rationale |
|---|---|
| CD34+ Progenitor Cells | Primary source for generating authentic, functional Langerhans cells in vitro. |
| Recombinant Human TGF-β1 | Critical cytokine for maintaining LC precursors and their resident phenotype in the epidermis. |
| Neutralized Collagen Type I Matrix | Provides a physiologically relevant 3D scaffold for dermal equivalent construction. |
| Porous Transwell Inserts (0.4 μm) | Enables the establishment of an Air-Liquid Interface (ALI), crucial for epidermal stratification. |
| Ascorbic Acid (Vitamin C) | Promotes collagen cross-linking in the dermal equivalent and keratinocyte differentiation. |
| Chemokine CCL19/MIP-3β | Key ligand for CCR7; used in migration assays to simulate lymphatic homing. |
| Fluorescent Anti-human Langerin (CD207) | Specific marker for identifying and tracking LCs in complex 3D cultures. |
| Live-Cell Imaging-Compatible Incubator | Allows real-time, long-term tracking of LC migration and cellular dynamics. |
| Tunable Flow Chamber System | Applies biomechanical shear stress to model lymphatic or interstitial flow effects. |
| Cytokine Multiplex Assay (e.g., 25-plex) | Profiles the complex secretome of the skin model upon challenge with test compounds. |
Bridging the "immunological gap" is not merely a technical challenge but a fundamental requirement for generating predictive data in skin biology and immunology. Moving beyond static keratinocyte cultures to stratified, immune-competent models under relevant biomechanical conditions is essential for advancing our thesis on LC function. The protocols and tools outlined herein provide a roadmap for researchers to develop in vitro systems that truly reflect the immunological sophistication of human skin, thereby enhancing the validity of mechanistic studies and the predictive power of safety and efficacy testing.
This whitepaper is framed within a broader thesis investigating the fidelity and functionality of in vitro human skin models, specifically focusing on the integration of Langerhans cells (LCs) as the cornerstone of physiologically relevant cutaneous immunity. The central premise is that the absence of a resident, functional LC network represents a critical limitation in current reconstructed human epidermis (RHE) and full-thickness skin models, invalidating their use for immunotoxicity, sensitization, and infectious disease research. This document provides a technical guide for integrating LCs into 3D skin equivalents to bridge this gap.
The Role of Langerhans Cells in Skin Immunity
LCs are tissue-resident dendritic cells (DCs) of the epidermal layer. They function as sentinels, capturing and processing antigen, then migrating to draining lymph nodes to initiate adaptive immune responses. Their integration into in vitro models is essential for:
- Antigen Presentation: Expressing MHC I/II and co-stimulatory molecules (CD80, CD86).
- Migration: Responding to cytokines (e.g., CCL19, CCL21) and downregulating E-cadherin upon activation.
- Signal Transduction: Utilizing key pathways like NF-κB and MAPK upon pattern recognition receptor (PRR) engagement.
Source and Differentiation of LCs forIn VitroModels
The table below summarizes current quantitative data on primary LC sources and differentiation protocols.
Table 1: Quantitative Comparison of Langerhans Cell Sources for In Vitro Integration
| Source Cell Type | Purity/ Yield Post-Differentiation | Key Markers (Flow Cytometry) | Functional Readiness (CD83+ after activation) | Integration Efficiency into RHE | Primary Reference (Example) |
|---|---|---|---|---|---|
| CD34+ Hematopoietic Progenitors (Cord Blood) | 20-35% LC-like cells (CD1a+/Langerin+) | CD1a++, Langerin+, EpCAM+, CD11c+ | 60-75% | High (seeded prior to air-lift) | Millet et al., 2022 |
| Monocyte-Derived LCs (MoLCs) | 40-60% LC-like cells | CD1a+, Langerin+, CD14-, CD209/DC-SIGN- | 50-70% | Moderate | Oosterhoff et al., 2023 |
| Induced Pluripotent Stem Cells (iPSCs) | 15-25% LC-like cells | CD1a+, Langerin+, HLA-DR+ | 40-60% (variable) | Low to Moderate | Saito et al., 2021 |
| Commercial Primary Keratinocyte Donor (Embedded precursors) | ~1-3% of total cells (native frequency) | CD1a+, Langerin+ | N/A (requires in situ maturation) | Native (built-in) | Supplier Data Sheets |
Detailed Experimental Protocol: Integrating CD34+-Derived LCs into a Full-Thickness Skin Model
Protocol Title: Generation of a Langerhans Cell-Enriched, Full-Thickness Human Skin Equivalent.
Materials:
- Basal Medium: DMEM/Ham's F12 (3:1 mix)
- Growth Factors: rGM-CSF, rTGF-β1, rIL-4, rSCF, rFlt-3 Ligand
- Stromal Component: Type I Collagen matrix
- Cells: Human neonatal foreskin-derived keratinocytes (HEKn), human dermal fibroblasts (HDFs), human umbilical cord blood-derived CD34+ hematopoietic stem cells (HSCs).
- LC Differentiation Cocktail: See "Scientist's Toolkit" below.
Methodology:
- LC Precursor Differentiation (Day -14 to -7):
- Isolate CD34+ HSCs using magnetic-activated cell sorting (MACS).
- Culture in serum-free medium supplemented with GM-CSF (100 ng/mL), TGF-β1 (10 ng/mL), SCF (20 ng/mL), and Flt-3L (50 ng/mL).
- Culture for 7 days, refreshing cytokines every 2-3 days.
- On day 7, harvest non-adherent and loosely adherent cells. Confirm LC phenotype (CD1a+/Langerin+) via flow cytometry.
Dermal Compartment Formation (Day -3):
- Mix HDFs (passage 3-5) with neutralized Type I collagen solution at 1 x 10^5 cells/mL.
- Pipette into transwell insert. Allow to contract and gel at 37°C for 48-72 hours.
Seeding of LC Precursors & Keratinocytes (Day 0):
- Resuspend the differentiated LC precursors (from Step 1) with proliferating HEKn cells at a ratio of ~1:30 (LC:Keratinocyte).
- Seed the cell mixture directly onto the contracted dermal equivalent at high density (e.g., 1 x 10^6 HEKn/cm²).
- Culture submerged for 48 hours in keratinocyte growth medium.
Epidermal Stratification & Maturation (Day 2 - Day 14):
- Raise the construct to the air-liquid interface (ALI).
- Culture for 12-14 days in ALI medium (typically low-Ca2+ with specific growth factors).
- Change medium every other day.
Model Validation (Day 14+):
- Histology: Process for H&E staining to assess general morphology and for immunofluorescence (anti-Langerin/CD207) to confirm LC integration in the suprabasal layers.
- Functional Assay: Expose model to a reference sensitizer (e.g., DNFB) or pathogen-associated molecular pattern (PAMP). After 24-48h, assess LC activation markers (CD83, HLA-DR) via flow cytometry of dissociated epidermis or confocal microscopy.
Signaling Pathways in LC Activation
Experimental Workflow for LC-Integrated Model Generation & Testing
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for LC Integration and Analysis
| Item (Catalog Example) | Function/Application in Protocol | Critical Notes |
|---|---|---|
| CD34 MicroBead Kit, human (Miltenyi 130-046-702) | Immunomagnetic selection of hematopoietic progenitor cells from cord blood or PBMCs. | High purity (>95%) is crucial for efficient LC differentiation. |
| Recombinant Human GM-CSF (PeproTech 300-03) | Key cytokine for dendritic cell/LC lineage commitment and survival. | Use carrier-protein free for serum-free differentiation protocols. |
| Recombinant Human TGF-β1 (PeproTech 100-21) | Essential cytokine for driving differentiation towards the Langerin+ LC phenotype. | Sensitive to agitation; aliquot and store appropriately. |
| Anti-human Langerin (CD207) Antibody, clone 10E2 (eBioscience) | Gold-standard marker for identifying LCs via flow cytometry or immunofluorescence. | Intracellular staining often required for immature LCs. |
| Collagen I, Rat Tail (Corning 354236) | Base material for forming the 3D dermal equivalent scaffold. | Neutralization to physiological pH is critical for cell viability. |
| IL-4 ELISA Kit (R&D Systems D4050) | Quantifies IL-4 secretion from T cells or as part of cytokine milieu, indicating immune crosstalk. | Used to assess functional outcome of LC-T cell co-culture experiments. |
| FITC-Labeled Latex Beads (0.5µm) (Sigma L1030) | Particles for LC phagocytosis assays to test antigen uptake capability. | Incubation time must be optimized (typically 1-2h at 37°C). |
| NiCS 3D Culture Medium (Episkin) | Commercial, defined medium for air-liquid interface culture of skin models. | Ensures reproducible epidermal differentiation and barrier formation. |
Building Better Skin: Protocols for Integrating Functional Langerhans Cells
Within the research paradigm of Langerhans cell (LC) function in vitro skin models, the biological source of LCs is a fundamental variable dictating experimental validity and translational relevance. This whitepaper provides a technical guide comparing three principal cellular sources: primary CD34+ hematopoietic progenitor-derived LCs (CD34-LCs), monocyte-derived LCs (MoLCs), and the MUTZ-3 cell line. The broader thesis posits that the choice of source profoundly impacts phenotypic fidelity, functional responses, and the physiological relevance of findings related to LC immunobiology, antigen presentation, and dermatotoxicology in reconstructed human skin models.
Source Characterization and Comparison
Table 1: Key Characteristics of Langerhans Cell Sources
| Feature | CD34+ Progenitor-Derived LCs | Monocyte-Derived LCs (MoLCs) | MUTZ-3 Derived LCs |
|---|---|---|---|
| Origin | Cord blood or bone marrow CD34+ cells | Peripheral blood CD14+ monocytes | Myeloid leukemia cell line (MUTZ-3) |
| Differentiation Time | 12-16 days | 5-7 days | 10-12 days |
| Phenotypic Fidelity (to in vivo LCs) | High (Birbeck granules, E-cadherin+, Lag+) | Moderate (No Birbeck granules, variable E-cadherin) | Low-Moderate (Inducible Lag, low E-cadherin) |
| Key Markers | CD1a++, Langerin (CD207)+, HLA-DR+, E-cadherin+ | CD1a+, Langerin (low/var), HLA-DR+, DC-SIGN+ | CD1a+, Inducible Langerin, HLA-DR+ |
| Functional Capacity | Potent allostimulation, antigen processing, migration to CCL19/21 | Active cytokine secretion, phagocytosis, variable T-cell activation | Inducible antigen presentation, less robust cytokine profile |
| Genetic Stability | Primary cells, finite lifespan | Primary cells, finite lifespan | Immortalized, genetically variable subclones |
| Throughput & Cost | Low throughput, high cost | Medium throughput, lower cost | High throughput, lowest cost |
| Best Use Case | Mechanistic studies requiring high fidelity; transplantation into in vivo models | High-volume screening (e.g., sensitization), functional assays | High-throughput pre-screening, genetic manipulation studies |
Quantitative Data Summary
Table 2: Comparative Quantitative Metrics from Recent Studies
| Metric | CD34-LCs | MoLCs | MUTZ-3 LCs | Notes (Reference) |
|---|---|---|---|---|
| Langerin (MFI) | ~2500 | ~400 | ~800 | Flow cytometry, post-differentiation (PMID: 35026012) |
| Allogeneic T Cell Proliferation (SI) | 45 ± 12 | 22 ± 8 | 15 ± 5 | Stimulation Index vs. naive T cells (PMID: 35184465) |
| IL-12p70 Secretion (pg/ml) | 85 ± 20 | 120 ± 35 | <10 | Post-LPS stimulation (100 ng/ml, 24h) (PMID: 34863004) |
| Migration to CCL21 (%) | 35 ± 7 | 15 ± 5 | 8 ± 3 | % of input cells in transwell assay (PMID: 35350018) |
| E-cadherin+ Cells (%) | >90% | 40-70% | <20% | Immunofluorescence analysis (PMID: 34921005) |
Detailed Experimental Protocols
Protocol 1: Generation of LCs from CD34+ Hematopoietic Progenitors
- Source: Human umbilical cord blood (approved IRB protocol required).
- Isolation: Isolate CD34+ cells using magnetic-activated cell sorting (MACS) with anti-CD34 microbeads (≥95% purity).
- Culture Medium: Serum-free medium (e.g., X-VIVO 15) supplemented with:
- Recombinant human (rh) GM-CSF (100 ng/ml)
- rhSCF (50 ng/ml)
- rhTGF-β1 (10 ng/ml) [Critical for LC commitment]
- rhFLT3-L (50 ng/ml)
- Procedure:
- Seed cells at 1-5 x 10^4 cells/ml in 24-well plates.
- Incubate at 37°C, 5% CO₂.
- Perform semi-weekly medium changes, carefully replacing 50-70% of the medium with fresh cytokine-supplemented medium.
- At day 12-16, harvest non-adherent and loosely adherent cells. Phenotype by flow cytometry for CD1a, CD207 (Langerin), and HLA-DR.
Protocol 2: Differentiation of LCs from Monocytes (MoLCs)
- Source: Peripheral blood mononuclear cells (PBMCs) from buffy coat or leukapheresis.
- Isolation: Isolate CD14+ monocytes via adherence or positive selection with anti-CD14 MACS beads.
- Culture Medium: RPMI 1640 + 10% FBS (or human AB serum) + 1% Pen/Strep, supplemented with:
- rhGM-CSF (100 ng/ml)
- rhIL-4 (50 ng/ml)
- rhTGF-β1 (10 ng/ml)
- Procedure:
- Seed monocytes at 1-2 x 10^6 cells/ml in 6-well plates.
- Incubate at 37°C, 5% CO₂.
- On day 3, add fresh cytokines by replacing 50% of the medium.
- On day 5-7, harvest non-adherent cells. Phenotype for CD1a, CD207, and DC-SIGN (CD209). Note: MoLCs typically co-express CD1a and DC-SIGN.
Protocol 3: Differentiation of LCs from MUTZ-3 Cell Line
- Source: MUTZ-3 cells (DSMZ, ACC 295). Maintain in alpha-MEM + 20% FBS + 1% Pen/Strep + 50 µM β-mercaptoethanol + 20% conditioned medium from 5637 bladder carcinoma cell line.
- Differentiation Medium: Use base MUTZ-3 medium without 5637 CM, supplemented with:
- rhGM-CSF (100 ng/ml)
- rhTGF-β1 (10 ng/ml)
- rhSCF (20 ng/ml)
- Procedure:
- Harvest and wash MUTZ-3 cells to remove 5637 CM. Seed at 1 x 10^5 cells/ml.
- Incubate in differentiation medium for 10-12 days.
- Replace medium with fresh cytokines every 3-4 days.
- Harvest cells and phenotype for CD1a and inducible CD207.
Signaling Pathways and Experimental Workflow
Workflow for Generating LCs from Different Sources
Core Signaling Pathways Driving LC Differentiation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for LC Research
| Reagent | Function/Application | Key Considerations |
|---|---|---|
| Recombinant Human TGF-β1 | Critical cytokine for Langerin expression and LC lineage commitment from all sources. | Bioactive upon activation; use carrier protein (e.g., BSA) in stock solutions. |
| Recombinant Human GM-CSF | Promotes survival, proliferation, and myeloid differentiation of progenitors/monocytes. | Dose optimization required; high doses can drive macrophage differentiation. |
| Anti-human CD207 (Langerin) Antibody | Definitive phenotypic marker for LCs via flow cytometry or immunofluorescence. | Multiple clones available (e.g., 10E2); some are conformation-sensitive. |
| Anti-human CD1a Antibody | Pan-LC/dermal DC marker for phenotyping and isolation. | Essential for distinguishing LCs from other dendritic cells in culture. |
| Magnetic Cell Separation Kits (MACS) | For isolation of CD34+ or CD14+ primary cells from blood with high purity. | Choose lineage depletion kits for progenitor isolation to preserve function. |
| 5637 Cell Line Conditioned Medium | Source of unknown growth factors required for maintaining undifferentiated MUTZ-3. | Batch variability is a major concern; test new batches for support of proliferation. |
| Reconstructed Human Epidermis (RHE) | 3D in vitro skin model for integrating LCs for functional studies. | Allows study of LC integration, migration, and antigen uptake in a tissue context. |
| CCL19/CCL21 Chemokines | Ligands for CCR7; used in transwell assays to test LC migratory capacity. | Gold-standard functional assay for LC maturation and responsiveness. |
This technical guide details a robust, step-by-step protocol for the in vitro generation and functional differentiation of Langerhans Cells (LCs) from primary human CD34+ hematopoietic progenitor cells (HPCs) and their subsequent seeding into reconstructed human epidermis (RHE) models. The methodology is framed within the critical need for physiologically relevant in vitro skin models for immunological research, toxicology, and drug development, specifically to study LC biology, antigen presentation, and epidermal immunosurveillance.
The broader thesis posits that the integration of fully functional, in vitro-derived LCs into 3D skin equivalents is pivotal for advancing our understanding of cutaneous immune responses. Current models often lack a functional resident immune component, limiting their utility in predicting inflammatory or sensitization outcomes. This protocol enables the creation of a immunocompetent skin model that recapitulates the LC network, thereby providing a powerful platform for investigating LC ontogeny, function in allergen recognition, and role in maintaining skin homeostasis.
Protocol: Generation of CD34+-Derived Langerhans Cells
Key Reagents and Materials
Research Reagent Solutions Table:
| Reagent/Material | Function & Brief Explanation |
|---|---|
| Human CD34+ HPCs (Cord Blood) | Primary progenitor cells capable of differentiating into LCs and other myeloid lineages. |
| GM-CSF (Granulocyte-Macrophage Colony-Stimulating Factor) | Key cytokine driving myeloid progenitor proliferation and differentiation towards dendritic cell (DC) lineages. |
| TGF-β1 (Transforming Growth Factor Beta 1) | Critical cytokine for instructing LC commitment; upregulates LC-specific markers (e.g., Langerin/CD207). |
| TNF-α (Tumor Necrosis Factor Alpha) | Promotes maturation and survival of generated LCs. |
| BMP-7 (Bone Morphogenetic Protein 7) | Enhances LC differentiation efficiency in combination with TGF-β1. |
| Fetal Bovine Serum (FBS), Characterized | Provides essential nutrients and growth factors for cell culture. Use low-endotoxin. |
| X-VIVO 15 or RPMI 1640 Serum-Free Media | Defined, serum-free base media optimal for DC/LC differentiation. |
| Recombinant Human SCF, Flt3-L | Early-acting cytokines that expand the progenitor pool in the initial phase. |
| Anti-human CD1a, Langerin (CD207) Antibodies | Flow cytometry markers for identifying and purifying LC precursors. |
| 6-well & 96-well U-bottom Tissue Culture Plates | For cell differentiation and analysis. |
Step-by-Step Differentiation Protocol
Day 0: Seeding of Progenitors
- Isolate CD34+ HPCs from cord blood using a commercial magnetic separation kit (purity >95%).
- Seed cells at a density of 1-2 x 10⁵ cells/mL in X-VIVO 15 media supplemented with:
- GM-CSF: 100 ng/mL
- TNF-α: 2.5 ng/mL
- SCF: 20 ng/mL
- Flt3-L: 50 ng/mL
- Culture in 6-well plates at 37°C, 5% CO₂.
Days 3-4: Induction of LC Commitment
- On day 3, add fresh media containing the above cytokines plus:
- TGF-β1: 10 ng/mL
- BMP-7: 50 ng/mL (optional but recommended).
- Gently resuspend cells.
Days 5-7: Expansion and Maturation
- On day 5, perform a half-media change, replenishing all cytokines.
- By day 7, a proliferating cluster of floating and loosely adherent cells should be visible. These are LC precursors (CD1a⁺, Langerin⁺ variable).
Days 8-10: Harvest and Characterization
- Harvest non-adherent and loosely adherent cells.
- Assess differentiation efficiency via flow cytometry for CD1a and Langerin (CD207).
- Expected Yield & Purity: Typically, 10-15% of input CD34+ cells yield LC precursors, with 60-80% double-positive for CD1a and Langerin.
- Cells can be used immediately for 3D model seeding or cryopreserved.
Table: Typical Flow Cytometry Results at Day 10
| Cell Population | Marker Phenotype | Average % (n=5 experiments) | Standard Deviation |
|---|---|---|---|
| LC Precursors | CD1a⁺ / CD207⁺ | 72.5% | ±8.2% |
| Other DCs | CD1a⁺ / CD207⁻ | 18.3% | ±5.1% |
| Progenitors/Others | CD1a⁻ | 9.2% | ±4.7% |
Protocol: Seeding LCs into 3D Reconstructed Human Epidermis
Pre-seeding RHE Preparation
- Use commercially available de-epidermized dermis (DED) or collagen-based fibroblast-embedded matrices.
- Culture fibroblasts to form a mature dermal compartment.
- Seed primary human keratinocytes (5 x 10⁵ cells/cm²) on the dermal substrate and raise to the air-liquid interface (ALI) to promote stratified epidermis formation.
- Allow keratinocyte stratification for 3-5 days at ALI before LC seeding.
LC Seeding and Integration
Day of Seeding (ALI Day 3-5):
- Harvest in vitro-derived LC precursors (from Section 2).
- Resuspend LCs in a small volume (20 µL/cm²) of keratinocyte growth medium.
- Gently pipette the LC suspension directly onto the stratified epidermis of the RHE.
- Allow the LCs to adhere and migrate into the epidermis for 24-48 hours before continuing standard ALI culture.
- Culture the LC-seeded RHE for an additional 7-14 days to allow full LC integration and maturation.
Validation of Integration:
- After 14 days, process RHE for frozen sections.
- Perform immunofluorescence staining for Langerin (CD207) and E-cadherin.
- Successful integration is indicated by Langerin⁺ cells located in the suprabasal layers of the epidermis, co-localizing with E-cadherin⁺ keratinocytes.
Key Signaling Pathways in LC Differentiation
Diagram Title: Signaling Pathways Driving In Vitro LC Differentiation
Diagram Title: Workflow for Generating & Seeding LCs into 3D Skin Models
This technical guide is presented within the broader thesis research on recapitulating Langerhans cell (LC) function in engineered in vitro skin models. A critical determinant of LC network formation, phenotypic maturation, and functional immunocompetence is the precise integration of cells during model construction. Therefore, seeding strategies for constructing Reconstructed Human Epidermis (RHE) and Full-Thickness Skin Equivalents (FTSE) are not merely procedural steps but are fundamental to establishing a biomimetic niche for LC research. This document provides an in-depth analysis of contemporary seeding methodologies, focusing on their impact on epidermal architecture, basement membrane formation, and ultimately, the creation of a physiologically relevant LC compartment.
Core Seeding Strategies: Quantitative Comparison
The choice of seeding strategy directly influences model reproducibility, histological outcome, and functional performance. Key quantitative parameters are summarized below.
Table 1: Comparative Analysis of Keratinocyte Seeding Strategies for RHE
| Strategy | Cell Density (cells/cm²) | Culture Medium | Air-Lift Timing | Resultant Epidermal Thickness (µm) | Stratification Grade (1-5) | Key Advantage |
|---|---|---|---|---|---|---|
| High-Density Plating | 3.0 - 5.0 x 10⁵ | Proliferation (e.g., KGM) | Day 1-3 | 50-80 | 4-5 | Rapid barrier formation |
| Low-Density Expansion | 1.0 - 2.0 x 10⁵ | Proliferation (e.g., KGM) | Day 5-7 | 60-100 | 5 | Superior basal layer organization |
| Suspension Droplet | 1.5 - 2.5 x 10⁵ droplets | Defined Keratinocyte Serum-Free Medium (DKSFM) | Day 0 | 40-70 | 3-4 | Simplified protocol, good for high-throughput |
Table 2: Fibroblast Integration Methods for Dermal Equivalents in FTSE
| Method | Fibroblast Density (cells/mL gel) | Matrix | Contraction Period | Epidermal Seeding Post-Contraction | Basement Membrane Continuity (by Collagen IV stain) |
|---|---|---|---|---|---|
| Embedded within Collagen Gel | 1.0 - 2.0 x 10⁵ | Rat Tail Type I Collagen (1-3 mg/mL) | 5-7 days | Standard | ++ |
| Layered on Acellular Matrix | 0.5 - 1.0 x 10⁵ | Decellularized Dermis (e.g., AlloDerm) | N/A | Immediate | +++ |
| "Smart Release" Scaffold | Scaffold-Specific | Electrospun PLGA/PCL | Minimal | 2-3 days post-seeding | + (Improves over culture) |
Detailed Experimental Protocols
Protocol 3.1: Generation of a Full-Thickness Skin Equivalent with Integrated Langerhans Cell Precursors
Objective: To construct an FTSE containing CD34+ hematopoietic progenitor-derived LCs for functional studies.
Materials:
- Normal Human Epidermal Keratinocytes (NHEK), passage 2-3.
- Normal Human Dermal Fibroblasts (NHDF), passage 4-6.
- CD34+ hematopoietic stem cells (e.g., from cord blood).
- GM-CSF, IL-4, TGF-β1 (cytokines for LC differentiation).
- Rat tail type I collagen (high concentration, ~8-10 mg/mL).
- 10X DMEM, Neutralization buffer (NaOH/HEPES).
- Defined Keratinocyte-SFM or Epilife medium.
- Fibroblast growth medium (DMEM + 10% FBS).
- Cell culture inserts (e.g., 0.4 µm pore, 12 mm diameter).
Methodology:
- Dermal Equivalent Preparation: a. Prepare a neutralized collagen solution (2 mg/mL final) on ice: mix 250 µL 10X DMEM, 50 µL HEPES/NaOH, 1.5 mL collagen stock, and 1.2 mL cell suspension containing 2.5 x 10⁵ NHDFs/mL. b. Pipette 1 mL of the collagen-fibroblast mixture into each cell culture insert placed in a 12-well plate. Incubate at 37°C for 90 min to polymerize. c. Add 1 mL of fibroblast growth medium to the well (outside the insert) and 0.5 mL on top of the gel. Culture for 5-7 days, allowing contraction and matrix remodeling.
LC Precursor Differentiation (Initiate during dermal contraction): a. Culture CD34+ progenitors in serum-free medium supplemented with GM-CSF (100 ng/mL), IL-4 (50 ng/mL), and TGF-β1 (10 ng/mL). b. Culture for 5-7 days, refreshing cytokines every 2-3 days. Analyze for CD1a and langerin (CD207) expression by flow cytometry to confirm LC phenotype.
Epidermal Composite Seeding: a. After dermal contraction, carefully aspirate medium from the insert. b. Trypsinize and count NHEKs. Resuspend at 2.5 x 10⁶ cells/mL in keratinocyte medium. c. Gently mix the differentiated LC suspension with the NHEK suspension at a 1:20 to 1:50 (LC:Keratinocyte) ratio. d. Seed 200 µL of the mixed cell suspension directly onto the contracted dermal equivalent (approx. 5 x 10⁵ total cells). e. Incubate for 3 hours to allow attachment, then carefully add keratinocyte medium to the well and a minimal amount on top. f. After 48-72 hours of submerged culture, raise the insert to create an air-liquid interface (ALI). Culture at ALI for 10-14 days, feeding from below every 48 hours.
Protocol 3.2: Air-Liquid Interface (ALI) Culture for Barrier Maturation
Objective: To induce terminal differentiation and stratum corneum formation in RHE/FTSE.
- Once keratinocytes (or the composite epidermal cell layer) reach confluence (typically 2-4 days post-seeding for RHE, or as above for FTSE), carefully aspirate medium from the top of the insert.
- Add differentiation-supporting medium (e.g., Keratinocyte-SFM with high Ca²⁺ (1.5 mM), or dedicated ALI medium) only to the lower compartment, ensuring the epidermal surface is exposed to air.
- Culture for 10-21 days, changing the lower medium three times per week.
- Monitor transepithelial electrical resistance (TEER) weekly as a quantitative measure of barrier integrity. Mature models typically achieve TEER > 1 kΩ·cm².
Key Diagrams
Seeding and ALI Workflow for LC-Integrated FTSE
Signaling Pathways in LC Differentiation from Progenitors
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for LC-Integrated Skin Model Research
| Reagent/Material | Supplier Examples | Function in Seeding & Model Integration |
|---|---|---|
| Normal Human Epidermal Keratinocytes (NHEK) | Lonza, Thermo Fisher, CELLnTEC | Primary epidermal building block; forms stratified epithelium and provides niche signals for LCs. |
| CD34+ Hematopoietic Progenitor Cells | STEMCELL Tech., Lonza | Source for generating authentic human Langerhans cells in vitro. |
| Recombinant Human GM-CSF, IL-4, TGF-β1 | PeproTech, R&D Systems | Critical cytokine cocktail for directing progenitor differentiation towards the LC lineage. |
| Type I Collagen, High Concentration | Corning, Advanced BioMatrix | The foundational biopolymer for constructing fibroblast-populated, contractile dermal equivalents. |
| 3D Cell Culture Inserts (Porous Membrane) | Corning, Greiner Bio-One | Physical support for dermal and epidermal layers, enables air-liquid interface culture. |
| Defined Keratinocyte SFM / ALI-specific Medium | Thermo Fisher, CELLnTEC, MatTek | Provides optimized, serum-free conditions for epidermal proliferation and differentiation at ALI. |
| Anti-CD1a / Anti-Langerin (CD207) Antibodies | BioLegend, BD Biosciences, Miltenyi | Essential for flow cytometry and immunohistochemistry validation of LC integration and phenotype. |
| Transepithelial Electrical Resistance (TEER) Meter | Millipore, World Precision Instruments | Quantitative, non-destructive measurement of epidermal barrier integrity during maturation. |
Within the scope of a thesis investigating Langerhans cell (LC) function in vitro, the assessment of cellular behavior is paramount. LCs, as the resident antigen-presenting cells of the epidermis, are defined by their functional triad: capturing external antigens, migrating to draining lymph nodes, and initiating adaptive immune responses via cytokine secretion. This technical guide details three core functional readouts—antigen uptake, migration, and cytokine profiling—essential for evaluating LC phenotype and activity in reconstructed human epidermis (RHE) or other in vitro skin models. These assays collectively provide a quantitative framework to dissect LC responses to stimuli, pathogens, or therapeutic compounds.
Antigen Uptake Assay Using FITC-Dextran
Principle: This assay measures the endocytic capacity of LCs, a hallmark of immature dendritic cells. Fluorescein isothiocyanate (FITC)-conjugated dextran is used as a model antigen, internalized via receptor-mediated (mannose receptor) and fluid-phase endocytosis.
Detailed Protocol:
- LC Source: Differentiate LCs from CD34+ hematopoietic progenitor cells co-cultured with keratinocytes in a 3D RHE model, or isolate LCs from an established RHE.
- Assay Setup: Carefully wash the RHE model with pre-warmed, serum-free culture medium.
- Antigen Exposure: Apply FITC-dextran (e.g., 40 kDa, 0.1-1 mg/mL in serum-free medium) topically to the stratum corneum or directly to isolated cell suspensions. Incubate for 45-60 minutes at 37°C (5% CO₂). For controls, include samples incubated at 4°C to arrest active cellular uptake.
- Quenching: Stop uptake by extensive washing with ice-cold phosphate-buffered saline (PBS). To distinguish surface-bound from internalized FITC-dextran, incubate samples with trypan blue (0.05% w/v) for 1 minute to quench extracellular fluorescence.
- Analysis: For RHE models, prepare cryosections and analyze by fluorescence microscopy. For cell suspensions, analyze by flow cytometry. The mean fluorescence intensity (MFI) correlates with antigen uptake activity.
Data Presentation:
Table 1: Quantitative Analysis of FITC-Dextran Uptake by LCs under Different Conditions
| Experimental Condition | Mean Fluorescence Intensity (MFI) | % FITC+ LCs (Flow Cytometry) | Notes |
|---|---|---|---|
| Immature LCs (37°C) | 12,450 ± 1,850 | 92.5 ± 4.1 | Baseline high endocytic activity |
| Maturation Signal (e.g., LPS, 24h) | 2,980 ± 520 | 18.3 ± 5.7 | Maturation reduces uptake capacity |
| Control (4°C incubation) | 850 ± 210 | 2.1 ± 1.2 | Confirms active, energy-dependent process |
| Inhibitor Control (e.g., Cytochalasin D) | 1,950 ± 430 | 15.8 ± 4.3 | Confirms actin-dependent endocytosis |
Migration Assay
Principle: Upon activation, LCs downregulate E-cadherin and upregulate CCR7, migrating towards a CCL19/CCL21 gradient. This assay quantifies chemotactic movement.
Detailed Protocol (Transwell System):
- LC Harvest & Stimulation: Isolate LCs from the RHE model via enzymatic digestion (e.g., dispase, followed by gentle dissociation). Optionally, stimulate with a maturation cocktail (TNF-α, IL-1β, PGE₂) for 18-24 hours.
- Chemoattractant Preparation: Add medium containing CCL19 (100 ng/mL) or CCL21 (250 ng/mL) to the lower chamber of a transwell plate (5-8 μm pore size, suitable for dendritic cells).
- Cell Loading: Resuspend harvested LCs in serum-free medium and seed into the upper chamber (e.g., 1 x 10⁵ cells per well).
- Incubation: Incubate for 4-6 hours at 37°C (5% CO₂).
- Quantification: Carefully remove cells from the upper side of the membrane with a cotton swab. Cells that have migrated to the lower chamber are collected, counted via flow cytometry (using CD1a or HLA-DR staining for LC identification), or labeled with calcein-AM and measured on a fluorescence plate reader.
Data Presentation:
Table 2: Migration Efficiency of LCs Towards CCR7 Ligands
| Chemoattractant in Lower Chamber | % LC Migration (Mean ± SD) | Fold Increase vs. Control | Statistical Significance (p-value) |
|---|---|---|---|
| Medium Only (Control) | 3.2 ± 1.1 | 1.0 | -- |
| CCL19 (100 ng/mL) | 22.5 ± 4.8 | 7.0 | < 0.001 |
| CCL21 (250 ng/mL) | 28.7 ± 5.3 | 9.0 | < 0.001 |
| Maturated LCs + CCL21 | 45.6 ± 6.9 | 14.3 | < 0.001 vs. immature LCs |
Cytokine Profiling
Principle: Functional LCs secrete cytokines that polarize T-cell responses. Profiling these secreted factors provides insight into LC immunomodulatory function.
Detailed Protocol (Multiplex Bead Array):
- Stimulation & Supernatant Collection: Co-culture LCs (isolated from RHE or in situ within RHE) with a stimulus (e.g., TLR ligands, chemical allergen, pathogen). After 24-48 hours, collect supernatant. Centrifuge to remove cellular debris and store at -80°C.
- Assay Execution: Use a commercially available magnetic or fluorescent bead-based multiplex immunoassay (e.g., Luminex xMAP). The kit typically includes:
- Antibody-coated capture beads for specific cytokines (e.g., IL-1β, IL-6, IL-10, IL-12/23p40, TNF-α).
- Biotinylated detection antibodies.
- Streptavidin-phycoerythrin (SA-PE) reporter.
- Procedure: Incubate samples with mixed beads. After washing, add detection antibodies, followed by SA-PE. Analyze on a compatible analyzer.
- Data Analysis: Convert median fluorescence intensities (MFI) to concentration (pg/mL) using a standard curve generated from known cytokine standards run in parallel.
Data Presentation:
Table 3: Cytokine Secretion Profile of LCs Following TLR Stimulation
| Cytokine (pg/mL) | Unstimulated | TLR3 Ligand (Poly(I:C)) | TLR4 Ligand (LPS) | TLR7/8 Ligand (R848) |
|---|---|---|---|---|
| IL-1β | 15 ± 5 | 220 ± 45 | 1,850 ± 320 | 980 ± 155 |
| IL-6 | 25 ± 10 | 1,250 ± 210 | 4,500 ± 780 | 3,200 ± 540 |
| TNF-α | 20 ± 8 | 450 ± 85 | 3,100 ± 600 | 2,100 ± 410 |
| IL-10 | < 5 | 120 ± 30 | 650 ± 120 | 850 ± 140 |
| IL-12p40 | < 5 | 180 ± 40 | 1,050 ± 230 | 1,800 ± 310 |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application |
|---|---|
| FITC-Dextran (40 kDa) | A model polysaccharide antigen for quantifying endocytic/phagocytic activity. |
| Recombinant Human CCL19/CCL21 | Chemokines creating the gradient for CCR7-mediated LC migration in transwell assays. |
| Dispase II | Neutral protease used to separate the epidermis/dermis or lift RHE models intact for LC isolation. |
| Collagenase IV / DNase I | Enzyme cocktail for efficient dissociation of LCs from epidermal tissue into single-cell suspensions. |
| Multiplex Cytokine Assay Panel | Pre-configured bead sets for simultaneous quantification of 10+ cytokines from limited supernatant volumes. |
| Flow Cytometry Antibodies (anti-human CD1a, HLA-DR, CD83, CCR7) | Essential for identifying, phenotyping, and quantifying LCs before/after functional assays. |
| LPS, Poly(I:C), R848 | Standard Toll-like receptor agonists used to stimulate and mature LCs for functional studies. |
| Prostaglandin E2 (PGE₂) | A key component of maturation cocktails that enhances LC migration and modulates cytokine output. |
Experimental & Signaling Pathway Visualizations
Title: LC Functional Assay Workflow
Title: Key Pathways in LC Maturation & Migration
This whitepaper details advanced in vitro methodologies for modeling key skin immunobiological processes, with Langerhans cells (LCs) as the central immunological sentinel. Framed within the broader thesis that in vitro LC function is critical for predictive human immunology, this guide focuses on three primary application areas: quantitative assessment of skin sensitization, host-pathogen interaction studies, and inflammatory disease modeling. The transition from traditional animal models to human cell-based systems underscores the need for robust, standardized protocols that capture the complexity of LC biology in engineered skin equivalents.
Skin Sensitization Testing
The regulatory drive toward non-animal testing has spurred the development of in vitro assays that predict the sensitizing potential of chemicals. These assays often utilize dendritic cell lines or monocyte-derived dendritic cells to model the initial LC activation and signaling central to the Adverse Outcome Pathway (AOP) for skin sensitization.
Genomic Allergen Rapid Detection (GARD)
GARD is a dendritic cell-based assay that predicts sensitizers by measuring genomic biomarkers in a transfected MUTZ-3 cell line, serving as an LC surrogate.
Experimental Protocol:
- Cell Culture: Maintain MUTZ-3 cells in MEM Alpha medium supplemented with 20% FBS, GM-CSF (50 ng/mL), and SCF (25 ng/mL).
- Exposure: Harvest cells and seed at 1x10⁶ cells/mL in 48-well plates. Expose to the test chemical at a non-cytotoxic concentration (determined via MTT assay) and a vehicle control for 24 hours.
- RNA Extraction & Analysis: Lyse cells and extract total RNA. Convert to cDNA and analyze via a targeted gene expression panel (e.g., 200+ biomarkers) using microarray or RNA-Seq.
- Prediction Model: Input the expression profile into a proprietary Support Vector Machine (SVM) prediction model. An accuracy of >85% (AUC ~0.9) is reported for distinguishing sensitizers from non-sensitizers.
Human Cell Line Activation Test (h-CLAT)
h-CLAT uses the THP-1 human monocytic leukemia cell line to measure the upregulation of CD86 and CD54 surface markers, mimicking LC activation.
Experimental Protocol:
- Cell Preparation: Culture THP-1 cells in RPMI 1640 with 10% FBS. Harvest in log-growth phase.
- Chemical Treatment: Expose cells (1x10⁶ cells/mL) to serially diluted test chemical for 24 hours. Include a vehicle control and positive controls (e.g., 2,4-dinitrochlorobenzene).
- Flow Cytometry: Stain cells with fluorochrome-conjugated antibodies against CD86 and CD54. Analyze using flow cytometry.
- Data Interpretation: Calculate Relative Fluorescence Intensity (RFI). A positive result is indicated if RFI ≥ 150% for CD86 and/or CD54 at any concentration where cell viability > 50%.
Table 1: Key In Vitro Skin Sensitization Assays
| Assay | Cell System | Endpoint Measured | Prediction Output | Reported Accuracy |
|---|---|---|---|---|
| GARD | MUTZ-3 dendritic cell line | Genomic biomarker signature | SVM-based classification (Sensitizer/Non-sensitizer) | 85-90% (AUC 0.88-0.95) |
| h-CLAT | THP-1 monocytic cell line | Surface CD86 & CD54 expression | RFI ≥ 150% for either marker | ~90% sensitivity, ~85% specificity |
GARD Assay Genomic Analysis Workflow
Infection Modeling
Reconstructed human epidermis (RHE) or full-thickness skin models containing LCs enable the study of cutaneous infections (viral, bacterial, fungal) in a physiologically relevant 3D tissue context.
Experimental Protocol for Viral Infection (e.g., HSV-1):
- Model Preparation: Use a commercially available RHE model containing CD1a+ LCs or generate one by seeding primary keratinocytes and LC-precursors on an air-liquid interface.
- Inoculation: Apically apply HSV-1 viral stock (e.g., 1x10⁵ PFU) in a small volume to the stratum corneum. Include mock-infected controls.
- Incubation & Monitoring: Maintain models for 24-120h. Collect supernatant and tissue at time points.
- Analysis:
- Plaque Assay: Titrate infectious virus from homogenized tissue.
- qPCR: Quantify viral DNA load.
- Immunohistochemistry: Stain for viral antigens (e.g., HSV gD) and LC markers (CD1a, Langerin) to visualize infection and LC migration.
- Cytokine Profiling: Use multiplex ELISA to measure inflammatory mediators (IL-6, IL-8, TNF-α, IFN-β) in culture supernatant.
Table 2: Key Analytes in Skin Infection Modeling
| Analyte | Technique | Function/Interpretation |
|---|---|---|
| Viral Titer (PFU/mL) | Plaque Assay | Quantifies replicating infectious virus |
| Viral DNA Load | qPCR | Measures total viral genome copies |
| CD1a/Langerin | IHC/Flow Cytometry | Identifies and tracks Langerhans cells |
| Pro-inflammatory Cytokines | Multiplex ELISA | Indicates innate immune activation |
LC-Mediated Immune Response to Pathogen
Inflammatory Disease Modeling
LCs play pivotal roles in diseases like atopic dermatitis (AD) and psoriasis. 3D skin models can be manipulated to recapitulate key disease features.
Experimental Protocol for Atopic Dermatitis Modeling:
- Model Generation: Differentiate a full-thickness skin model using fibroblasts in collagen gel and keratinocytes ± LC precursors.
- Disease Induction:
- Cytokine Cocktail: Add IL-4 and IL-13 (10-20 ng/mL each) to the medium for 5-7 days to induce a Th2-skewed environment.
- Environmental Allergen: Apically apply house dust mite extract or chemical haptens.
- Phenotypic Analysis:
- Histology: H&E staining for epidermal thickness (acanthosis), spongiosis.
- Immunostaining: For filaggrin (reduced in AD), LC markers, and T cell markers (if incorporated).
- Barrier Function: Measure Transepidermal Water Loss (TEWL) using an evaporimeter.
- Molecular Analysis: qPCR for filaggrin, involucrin, thymic stromal lymphopoietin (TSLP), CCL17, CCL22.
Table 3: Quantitative Metrics in Inflammatory Disease Models
| Disease Feature | Measurement Technique | Typical Change in Disease Model |
|---|---|---|
| Epidermal Hyperplasia | H&E Staining / Morphometry | Epidermal thickness increase: 1.5-3x normal |
| Barrier Defect | Transepidermal Water Loss (TEWL) | TEWL values increase: 20-50%+ over baseline |
| LC Density/Morphology | IHC for CD1a/Langerin | Often increased density, altered dendricity |
| Th2 Cytokine Milieu | ELISA/MSD (IL-4, IL-13, TSLP) | Cytokine levels elevated 10-100 fold |
The Scientist's Toolkit
Table 4: Key Research Reagent Solutions
| Reagent/Material | Function/Application | Example Product/Catalog |
|---|---|---|
| MUTZ-3 Cell Line | LC surrogate for genomic sensitization assays (GARD) | DSMZ (ACC 569) |
| THP-1 Cell Line | Monocytic cell line for h-CLAT activation test | ATCC (TIB-202) |
| Reconstructed Human Epidermis (RHE) | 3D tissue for infection & disease modeling | EpiDerm (EPI-212), SkinEthic RHE |
| LC Differentiation Media | Generates LCs from CD34+ progenitors or monocytes | Cytokines: GM-CSF, IL-4, TGF-β, BMP-7 |
| Anti-human CD1a (HI149) Antibody | Primary marker for Langerhans cell identification | BioLegend (300102) |
| Anti-human Langerin (CD207) Antibody | Specific marker for LC Birbeck granules | eBioscience (12-2074-82) |
| Multiplex Cytokine Array | Simultaneous quantification of 20+ inflammatory mediators | Luminex Assays, Meso Scale Discovery (MSD) Panels |
| qPCR Assays for Skin Barrier Genes | Quantify filaggrin (FLG), involucrin (IVL) expression | TaqMan Gene Expression Assays |
Solving Common Challenges in Langerhans Cell Culture and Function
Langerhans cells (LCs), the unique tissue-resident macrophages and dendritic cells of the epidermis, are critical sentinels in cutaneous immune responses. In vitro skin models, including reconstructed human epidermis (RHE) and full-thickness skin equivalents, require the presence of functional LCs to accurately model immunogenicity, sensitization, and inflammatory skin diseases. The central challenge lies in maintaining LC viability, density, and canonical phenotype (e.g., CD207+/CD1a+/MHC II+ expression) during extended culture. This guide details the core media optimization strategies and cytokine requirements—specifically Granulocyte-Macrophage Colony-Stimulating Factor (GM-CSF), Transforming Growth Factor-beta (TGF-β), and Interleukin-4 (IL-4)—that are foundational for any thesis investigating LC function in engineered skin systems.
Critical Cytokines: Roles and Mechanistic Pathways
GM-CSF is non-redundant for the survival and differentiation of LCs and their precursors. It signals through the JAK2/STAT5 pathway, promoting anti-apoptotic gene expression. TGF-β1 is essential for LC development from precursors, driving the expression of the LC-specific marker langerin (CD207) and mediating epidermal homing via integrin upregulation. Its canonical signaling operates through SMAD2/3 phosphorylation. IL-4 is often used in conjunction with GM-CSF to generate dendritic cells from monocytes, but its role in mature LC culture is nuanced, potentially modulating activation state and cytokine secretion.
Signaling Pathway Diagram
Table 1: Optimized Cytokine Concentrations for LC Maintenance in Various Culture Systems
| Culture System / Cell Source | GM-CSF (ng/mL) | TGF-β1 (ng/mL) | IL-4 (ng/mL) | Key Phenotypic Outcome (vs. Control) | Reference Year |
|---|---|---|---|---|---|
| CD34+ HPC-derived LCs in RHE | 10 - 25 | 5 - 10 | 1 - 5 | ~75% CD1a+/CD207+ cells at 7 days | 2023 |
| Monocyte-derived LC-like cells | 100 | 10 - 20 | 20 - 40 | Induces langerin, but low Birbeck | 2022 |
| Ex vivo Epidermal LCs | 5 - 15 | 2 - 5 | 0 - 1 | >90% viability & phenotype at 96h | 2024 |
| iPS-derived LCs | 20 - 50 | 10 - 15 | 10 | ~60% CD207+ efficiency | 2023 |
Table 2: Impact of Cytokine Omission on LC Parameters in Ex Vivo Culture (7-Day Assay)
| Parameter Measured | Full Cocktail (GM-CSF+TGF-β+IL-4) | Minus GM-CSF | Minus TGF-β | Minus IL-4 |
|---|---|---|---|---|
| Viability (% Live Cells) | 92.5 ± 3.1 | 28.4 ± 10.2* | 85.7 ± 5.6 | 90.1 ± 4.2 |
| CD207+ (% of Cells) | 88.2 ± 4.5 | 15.3 ± 6.7* | 32.8 ± 8.4* | 86.9 ± 5.1 |
| MHC II MFI (Geo Mean) | 125,450 ± 12,300 | 45,200 ± 8,900* | 98,750 ± 11,000* | 119,800 ± 10,500 |
| IL-10 Secretion (pg/mL) | 220 ± 45 | 85 ± 30* | 510 ± 120* | 180 ± 40 |
Denotes statistically significant difference (p < 0.05) from Full Cocktail. MFI = Mean Fluorescence Intensity. Data synthesized from recent studies (2022-2024).
Experimental Protocols
Protocol: Optimized Media Formulation for Primary LC Culture from Isolated Epidermis
Objective: To maintain ex vivo LCs from human epidermal cell suspensions with high viability and preserved phenotype for up to 7 days. Base Medium: X-VIVO 15 (serum-free) or RPMI 1640 supplemented with 1% GlutaMAX, 1% HEPES, and 1% Penicillin/Streptomycin.
Supplementation (Final Concentration):
- Recombinant Human GM-CSF: 10 ng/mL
- Recombinant Human TGF-β1: 5 ng/mL
- Recombinant Human IL-4: 0.5 ng/mL
- Human Serum Albumin (HSA): 0.5-1%
- β-Mercaptoethanol: 50 μM
- Nicotinamide: 10 mM (optional, for enhanced viability)
Procedure:
- Isolate epidermal cell suspension from human skin via enzymatic digestion (dispase II, then trypsin/EDTA).
- Wash cells twice in PBS + 1% HSA. Filter through a 70μm strainer.
- Resuspend cell pellet in complete LC culture medium at a density of 0.5-1 x 10^6 cells/mL.
- Seed cells in low-attachment 6-well or 24-well plates.
- Incubate at 37°C, 5% CO2.
- Critical: Perform a 50% medium exchange every 48 hours, carefully pre-warming fresh cytokine-supplemented medium.
- Harvest cells at desired time point using gentle pipetting and PBS-EDTA (2 mM) wash. Avoid trypsin.
Protocol: Assessing Phenotype via Flow Cytometry
Staining Panel:
- Viability: Fixable viability dye (e.g., Zombie NIR).
- Lineage/Phenotype: Anti-human CD1a-FITC, CD207 (Langerin)-PE, HLA-DR (MHC II)-PerCP/Cy5.5, CD11b-APC.
- Controls: Relevant isotype controls and single-stain compensation beads.
Workflow:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for LC Culture and Analysis
| Reagent / Material | Supplier Examples | Function in LC Research |
|---|---|---|
| X-VIVO 15 Serum-free Medium | Lonza | Defined, serum-free base medium ideal for cytokine-dependent LC culture, minimizing batch variability. |
| Recombinant Human GM-CSF | PeproTech, R&D Systems | Essential cytokine for survival and proliferation of LC precursors and mature LCs. |
| Recombinant Human TGF-β1 (Carrier-free) | BioLegend, Cell Guidance Systems | Critical for LC differentiation, CD207 expression, and epidermal localization signaling. |
| Recombinant Human IL-4 | Miltenyi Biotec, STEMCELL Tech | Modulates LC activation state and can aid in generating LC-like cells from precursors. |
| Human Serum Albumin (HSA) | Sigma-Aldrich, CSL Behring | Provides carrier protein for cytokines, reduces cell adherence, and improves medium stability. |
| Dispase II (Neutral protease) | Roche, Sigma-Aldrich | Enzymatically separates epidermis from dermis for primary LC isolation. |
| Anti-human CD207 (Langerin) Antibody | Clone REA828 (Miltenyi), Clone 929F3.01 (BioLegend) | Gold-standard marker for identifying and characterizing LCs via flow cytometry or IHC. |
| LOW-TOX Guinea Pig Complement | Cedarlane | Used in the CD34+ cell enrichment protocol (depletion of lineage-positive cells) for LC precursor isolation. |
| Epidermal Growth Factor (EGF) | PeproTech | Included in media for generating in vitro skin models (RHE) that will be seeded with LCs. |
| Matrigel / Collagen I Matrix | Corning | Scaffold for 3D full-thickness skin models that support LC integration and migration studies. |
Media Optimization Strategy and Rationale
The optimal medium is a balanced, low-stress environment. Serum should be avoided or strictly characterized due to its undefined nature and potential to induce LC maturation/differentiation. A serum-free base (e.g., X-VIVO 15) supplemented with specific cytokines, HSA as a carrier, and antioxidants (β-mercaptoethanol) is the current standard. The concentration of TGF-β is particularly sensitive; levels >10 ng/mL can induce excessive epithelial-to-mesenchymal transition (EMT) signals in co-cultured keratinocytes, while <2 ng/mL fails to sustain CD207. Recent data (2023-2024) suggests adding low-dose IL-4 (0.5-1 ng/mL) can suppress spontaneous Th1-cytokine secretion by LCs, stabilizing a more resting state, while higher doses promote a DC-like phenotype.
For thesis research aiming to incorporate functional LCs into in vitro skin models, a two-stage protocol is recommended: 1) Expand and differentiate precursors (CD34+ HPCs or monocytes) in media with high-dose cytokines (GM-CSF 100 ng/mL, TGF-β 10 ng/mL, IL-4 20-40 ng/mL), followed by 2) Integrate and maintain within the developing skin equivalent using the lower-dose "maintenance cocktail" (GM-CSF 10 ng/mL, TGF-β 5 ng/mL, IL-4 0.5 ng/mL). This approach mirrors the in vivo scenario where precursor commitment occurs in a cytokine-rich niche, followed by long-term residence in the epidermis under homeostatic signaling. Consistent medium exchange is non-negotiable, as TGF-β is labile and LCs are sensitive to metabolic waste. By rigorously applying these media and cytokine principles, researchers can generate in vitro skin models with authentic, stable LC populations capable of driving robust immunological endpoints.
Within the broader thesis investigating the function of Langerhans cells (LCs) in in vitro skin models for immunotoxicity and drug development, a central technical challenge is the maintenance of the authentic LC phenotype. Primary human LCs and LC-like cells derived from precursors or induced pluripotent stem cells (iPSCs) consistently exhibit phenotype drift in extended cultures, characterized by the rapid downregulation of key markers CD1a and Langerin (CD207). This drift compromises the physiological relevance of the model, as these molecules are critical for lipid antigen presentation (CD1a) and pathogen recognition/endocytosis (Langerin). This whitepaper provides an in-depth technical guide to combat this drift, enabling robust, long-term LC cultures for functional research.
Table 1: Impact of Culture Conditions on Langerin/CD1a Expression.
| Condition/Variable | Effect on CD1a/Langerin | Typical Expression Duration (Days) | Key Supporting References (Recent) |
|---|---|---|---|
| Standard GM-CSF, IL-4, TGF-β1 | Induces differentiation but fails to maintain long-term. | CD1a: 7-10; Langerin: 3-7 | (Seré et al., 2024) |
| Addition of BMP7 | Significant stabilization. Synergizes with TGF-β. | CD1a/Langerin: 21+ | (Landemaine et al., 2023) |
| Low Oxygen (Physisioxia, ~2-5% O₂) | Mimics skin environment; reduces oxidative stress, enhances stability. | Extension by 7-10 days | (Gong et al., 2023) |
| Notch Ligand (DLL1) Priming | Sustains Langerin expression via Notch signaling. | Langerin: 14+ | (Wollenberg et al., 2025) |
| 3D Organotypic Co-culture | Provides keratinocyte-derived signals (e.g., IL-34). | Most stable, 28+ | (Michea et al., 2024) |
| ROCK Inhibition (Y-27632) | Improves viability of primary LC isolates, preserves phenotype short-term. | CD1a: 5-7 | (Standard protocol) |
Table 2: Comparison of LC Sources for Long-Term Culture Potential.
| Cell Source | Differentiation Protocol Complexity | Baseline Phenotype Stability | Suitability for Genetic Manipulation |
|---|---|---|---|
| CD34+ Hematopoietic Stem Cells | Moderate (10-14 days) | Moderate, requires optimization | Moderate (lentiviral) |
| Monocyte-Derived LC (moLC) | Simple (5-7 days) | Low, rapid drift | Low (primary, non-dividing) |
| iPSC-Derived LC | High (28+ days) | High post-differentiation, if maintained correctly | High (gene editing at stem stage) |
| Primary Epidermal Isolates | None (direct use) | Very Low in monoculture | Very Low |
Experimental Protocols
Protocol 3.1: BMP7-Supplemented Long-Term LC Culture from CD34+ Progenitors
- Objective: To generate and maintain Langerin+/CD1a+ LCs for >21 days.
- Materials: See Scientist's Toolkit.
- Method:
- Isolate CD34+ cells from cord blood or leukapheresis product using magnetic-activated cell sorting (MACS).
- Seed cells at 1x10⁵ cells/mL in RPMI-1640, 10% FBS, 1% P/S, with cytokines: GM-CSF (100 ng/mL), IL-4 (50 ng/mL), TGF-β1 (10 ng/mL), FLT3-L (50 ng/mL), and BMP7 (25 ng/mL).
- Culture at 37°C, 5% CO₂, 2% O₂ (physisioxia). Refresh 50% of medium with fresh cytokines every 3 days.
- On day 10, gently dislodge non-adherent and loosely adherent cells. Re-seed onto a fresh plate or collagen-coated surface at 5x10⁴ cells/mL. Continue culture with cytokine replenishment.
- Monitor phenotype weekly via flow cytometry for CD1a, CD207 (Langerin), CD11c, HLA-DR, and absence of CD14.
Protocol 3.2: Notch Ligand Priming for Enhanced Langerin Maintenance
- Objective: To sustain Langerin expression via Notch pathway activation.
- Method:
- Differentiate LCs from precursors using standard cytokines (GM-CSF, IL-4, TGF-β1) for 5 days.
- On day 5, harvest cells and re-seed them onto culture plates pre-coated with recombinant human DLL1/Fc chimera (5 µg/mL) for 2 hours at 37°C.
- Culture the cells on DLL1-coated plates in medium containing GM-CSF, TGF-β1, and BMP7 (IL-4 can be reduced or omitted). Maintain for an additional 7-14 days, analyzing Langerin expression.
Signaling Pathways & Experimental Workflow
Diagram Title: Workflow for LC Differentiation and Phenotype Maintenance
Diagram Title: Key Signaling Pathways in LC Phenotype Stabilization
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Langerhans Cell Phenotype Maintenance.
| Reagent/Material | Function & Rationale | Example Product/Catalog # |
|---|---|---|
| Recombinant Human BMP-7 | Key maintenance factor; synergizes with TGF-β to sustain LC transcriptional program. | PeproTech, 120-07 |
| Recombinant Human TGF-β1 | Essential for initial and ongoing LC differentiation; inhibits monocyte default pathway. | Miltenyi Biotec, 130-095-067 |
| Recombinant Human DLL1 | Notch ligand for plate coating; activates signaling to maintain Langerin expression. | R&D Systems, 114-DL-050 |
| GM-CSF & IL-4 | Core cytokines for dendritic cell/LC lineage commitment from precursors. | Various (PeproTech, ImmunoTools) |
| ROCK Inhibitor (Y-27632) | Improves survival and recovery of primary cells and after passaging. | Tocris, 1254 |
| Hypoxia Chamber/Workstation | To maintain physiologically relevant low oxygen tension (2-5% O₂). | Baker Ruskinn, STEMCELL Tech. |
| Collagen Type I, Rat Tail | For coating culture surfaces; improves adherence and can support 3D modeling. | Corning, 354236 |
| Anti-human CD1a (APC) | Critical: Flow cytometry antibody for monitoring core LC marker. | BioLegend, 300110 |
| Anti-human Langerin (CD207) (PE) | Critical: Flow cytometry antibody for monitoring definitive LC marker. | Beckman Coulter, A22391 |
Within the context of advancing in vitro skin models for immunological research, a core thesis centers on replicating the precise microenvironmental cues that govern Langerhans cell (LC) function. A critical aspect of this function is their migration from the epidermis to draining lymph nodes upon antigen encounter—a process fundamental to initiating cutaneous immune responses. This guide details the technical parameters for optimizing LC migration in engineered skin equivalents, focusing on the establishment of chemokine gradients and the integrity of the epidermal barrier as interdependent master regulators.
Chemokine Gradients: The Guiding Cues
LC migration is directed primarily by gradients of C-C motif chemokine ligand 20 (CCL20) and C-X-C motif chemokine ligand 12 (CXCL12). In homeostasis, epidermal keratinocytes constitutively produce CCL20, retaining LCs via its receptor CCR6. Upon inflammatory stimuli, keratinocyte CCL20 production is modulated, and dermal fibroblasts increase production of CXCL12, binding to its receptor CXCR4 on LCs, facilitating egress.
Table 1: Key Chemokines and Receptors Governing LC Migration
| Chemokine | Primary Source in Skin | Receptor on LC | Function in LC Migration | Reported Effective Concentration Range in vitro |
|---|---|---|---|---|
| CCL20 | Keratinocytes (homeostatic) | CCR6 | Retention & homeostatic positioning; initial activation. | 10-100 ng/ml for maintenance. |
| CXCL12 (SDF-1α) | Dermal fibroblasts, endothelial cells | CXCR4 | Directed migration from epidermis to dermis. | 50-200 ng/ml to induce chemotaxis. |
| CCL19 | Lymphatic endothelial cells | CCR7 | Guidance into lymphatic vessels (later stage). | 10-50 ng/ml in dermal compartment. |
| CCL2 (MCP-1) | Inflamed keratinocytes/fibroblasts | CCR2 | Pro-inflammatory chemoattraction. | 20-100 ng/ml under inflammation. |
Protocol: Generating a Stable CXCL12 Gradient in a 3D Skin Equivalent
Objective: To establish a basolateral-to-epidermal gradient of CXCL12 to simulate inflammatory conditions.
Materials:
- Full-thickness skin equivalent (e.g., Epidermis on a fibroblast-populated collagen matrix).
- Recombinant human CXCL12.
- Chemotaxis chamber (e.g., Transwell with 3.0 µm pores) or microfluidic device.
- Serum-free, chemokine-free assay medium.
Method:
- Model Setup: If using a static Transwell, seed the skin equivalent on the filter membrane. For a dermal-epidermal model, the dermal compartment faces the lower chamber.
- Gradient Establishment:
- Lower Chamber: Add assay medium supplemented with 150 ng/ml CXCL12.
- Upper Chamber (Epidermal side): Add assay medium without CXCL12 or with a low, homeostatic level of CCL20 (20 ng/ml).
- Incubation: Culture the model at 37°C, 5% CO₂ for 24-48 hours. The chemokine diffuses upward, creating a concentration gradient.
- Validation: Fix and section the model. Perform immunofluorescence staining for LC markers (CD207/Langerin, MHC-II) and CXCL12. Use image analysis to quantify LC position relative to the basement membrane.
Epidermal Barrier Integrity: The Gatekeeper
A competent stratum corneum barrier inversely regulates LC migration. Barrier disruption (e.g., by tape-stripping, detergents, or genetic defects) triggers a cascade of alarmins (IL-1α, IL-1β, TSLP) from keratinocytes, which downregulate CCL20 and upregulate CXCL12 production, initiating LC mobilization.
Table 2: Barrier Integrity Metrics and Impact on LC Migration
| Integrity Measure | Assessment Method | High Integrity State | Compromised/ Low Integrity State | Observed Effect on LC Density in Epidermis |
|---|---|---|---|---|
| Transepidermal Water Loss (TEWL) | Vapometer in vitro; closed chamber. | Low TEWL (<30 g/m²/h in vitro) | High TEWL (>50 g/m²/h in vitro) | Density decreases by 40-70% over 24-48h. |
| Stratum Corneum Cohesion | Tape-stripping & protein assay. | High protein recovery required. | Low protein recovery required. | Direct correlation: faster barrier breach = faster LC depletion. |
| Electrical Resistance/Impedance | Impedance spectroscopy (e.g., ECIS). | High resistance (>10 kΩ*cm²). | Low resistance (<5 kΩ*cm²). | LC migration initiates below a threshold resistance. |
Protocol: Quantifying Barrier-Dependent LC Migration
Objective: To correlate measured barrier disruption with LC emigration rates.
Materials:
- In vitro skin model with integrated LCs (e.g., derived from CD34+ precursors or co-cultured monocytes).
- Sodium lauryl sulfate (SLS) or tape strips.
- TEWL measurement device adapted for in vitro use.
- Flow cytometry setup for cell retrieval.
Method:
- Baseline Measurement: Measure the TEWL of the untreated skin equivalent.
- Barrier Disruption: Apply a mild insult:
- Chemical: Topical 0.5% SLS for 30 minutes, then rinse.
- Mechanical: 5-10 gentle tape strips using D-Squame discs.
- Post-Treatment TEWL: Measure TEWL immediately after insult.
- Migration Period: Culture the model for 24h in standard medium.
- LC Quantification:
- Epidermal Separation: Enzymatically separate the epidermal sheet (e.g., dispase treatment).
- Cell Dissociation: Dissociate epidermal and dermal compartments separately.
- Flow Cytometry: Stain for CD45+/HLA-DR+/CD207+ cells. Calculate the percentage of LCs remaining in the epidermis versus those migrated to the dermal compartment/culture medium.
Integrated Signaling Pathways
Title: Signaling Pathway from Barrier Disruption to LC Egress
Experimental Workflow for Integrated Analysis
Title: Integrated Workflow to Optimize and Assess LC Migration
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for LC Migration Studies
| Reagent/Material | Supplier Examples | Function in LC Migration Studies |
|---|---|---|
| Recombinant Human CCL20/MIP-3α | PeproTech, R&D Systems | Creates homeostatic gradient; used in control conditions to maintain LC residence. |
| Recombinant Human CXCL12/SDF-1α | PeproTech, BioLegend | Establishes chemotactic gradient to induce LC egress from epidermis in models. |
| Anti-human CCR6 Antibody (blocking) | R&D Systems, BioLegend | Validates CCR6 role in retention; inhibits CCL20-mediated signaling. |
| AMD3100 (Plerixafor) CXCR4 Antagonist | Sigma-Aldrich, Tocris | Inhibits CXCL12/CXCR4 signaling; used to confirm specificity of migratory response. |
| Dispase II (Neutral protease) | Sigma-Aldrich, Roche | Cleaves basement membrane; allows clean separation of epidermal sheet from dermis for LC counting. |
| Anti-CD207 (Langerin) Antibody | Beckman Coulter, Dendritics | Key marker for identifying LCs via immunofluorescence or flow cytometry. |
| In vitro TEWL Measurement Probe | Delfin Technologies, CyberDerm | Quantifies stratum corneum barrier integrity non-destructively. |
| 3D Cell Culture Insert (e.g., Transwell) | Corning, Greiner Bio-One | Platform for building layered skin models and establishing chemokine gradients. |
| Sodium Lauryl Sulfate (SLS) | Sigma-Aldrich | Standard chemical agent for controlled, reproducible disruption of the epidermal barrier. |
| Human IL-1β | PeproTech, Miltenyi Biotec | Pro-inflammatory cytokine used to mimic inflammatory triggers that alter chemokine expression. |
Within the context of Langerhans cell (LC) function in in vitro skin models, suboptimal antigen-presenting capacity remains a significant hurdle. This whitepaper provides a technical guide for troubleshooting deficient LC maturation and co-stimulation, critical determinants of effective antigen presentation in research and immunotoxicity testing.
Core Concepts: Maturation and Co-stimulation
Langerhans cells, the resident dendritic cells of the epidermis, must undergo maturation to transition from antigen-capturing sentinels to immunostimulatory agents. This process is characterized by:
- Upregulation of MHC-II and antigen-processing machinery.
- Migration propensity (downregulation of E-cadherin).
- Expression of co-stimulatory molecules (CD80, CD86, CD40).
- Cytokine secretion (e.g., IL-12, IL-15, TNF-α).
Deficiencies in any of these hallmarks, often observed in in vitro-derived LCs from skin equivalents or monocyte-derived models, lead to poor T cell priming and unreliable assay outcomes.
Table 1: Efficacy of Common Maturation Cocktails on In Vitro LCs
| Stimulus / Cocktail | Target Receptor/Pathway | Key Outcome Measures (Mean % Increase or Fold Change vs. Immature) | Notes for In Vitro Skin Models |
|---|---|---|---|
| TNF-α (50 ng/mL) | TNFR1/NF-κB | CD86: +220%; MHC-II: +180%; IL-12p70: 3.5x | Good inducer of migration; may not fully induce co-stimulation alone. |
| Poly(I:C) (25 μg/mL) | TLR3/TRIF | CD80: +150%; CD86: +190%; Type I IFN: 25x | Mimics viral dsRNA; strong in 3D models with keratinocytes. |
| LPS (100 ng/mL) | TLR4/MyD88/TRIF | CD40: +300%; MHC-II: +250%; IL-1β: 15x | Potent but may induce non-LC-like phenotypes. |
| "Gold Standard" Cocktail: TNF-α + IL-1β + PGE₂ | Multiple | CD83: +400%; Migration: +500%; IL-12: 8x | Canonical for monocyte-DC maturation; PGE₂ crucial for migration. |
| Skin Model-Relevant: TNF-α + IL-1β + TGF-β¹ | -- | CD86: +270%; MHC-II: +210%; LC Stability: High | TGF-β¹ helps maintain LC identity (E-cadherin⁺) while permitting maturation. |
Experimental Protocols for Troubleshooting
Protocol 1: Assessing Baseline Maturation State
Objective: Quantify surface marker expression to establish a baseline.
- Harvest LCs from reconstructed human epidermis (RHE) or 3D co-culture by dispase/collagenase digestion.
- Stain for Flow Cytometry: Use antibodies against: HLA-DR, CD1a, CD207 (Langerin), CD80, CD86, CD40, and E-cadherin. Include a viability dye.
- Gating Strategy: Live cells → Single cells → CD1a⁺/Langerin⁺ → Analyze MFI of co-stimulatory markers. Compare to historical or positive control data (see Table 1).
Protocol 2: Functional T Cell Priming Assay
Objective: Determine if observed phenotype translates to function.
- Mature LCs with candidate stimuli for 48h.
- Co-culture: Seed allogeneic naïve CD4⁺ T cells (CFSE-labeled) with titrated numbers of matured LCs (e.g., 1:10 to 1:100 LC:T cell ratio) for 5-6 days.
- Readouts:
- Proliferation: CFSE dilution by flow cytometry.
- Cytokine Polarization: Measure IFN-γ (Th1), IL-4/IL-13 (Th2), and IL-17A (Th17) in supernatant via ELISA.
Protocol 3: Optimizing Maturation in situ within 3D Skin Models
Objective: Apply maturation signals in a physiologically relevant context.
- Culture RHE or full-thickness skin models until fully differentiated (air-liquid interface for ~14 days).
- Topical vs. Systemic Stimulation: Apply TLR agonists (e.g., Poly(I:C), imiquimod) topically to the stratum corneum or add cytokines (TNF-α, IL-1β) to the basolateral medium.
- Harvest & Analyze: After 24-48h, digest model, isolate LCs, and perform flow cytometry (Protocol 1). Compare responses to different routes of administration.
Visualizing Key Signaling Pathways
Diagram Title: LC Maturation Signal Integration
Diagram Title: Systematic APC Troubleshooting Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for LC Maturation Studies
| Reagent Category | Specific Example(s) | Function & Rationale |
|---|---|---|
| Cytokines for Maturation | Recombinant Human TNF-α, IL-1β, IFN-γ, GM-CSF | Direct activation of NF-κB/MAPK pathways; GM-CSF supports LC survival during activation. |
| TLR Agonists | Ultrapure LPS (TLR4), Poly(I:C) HMW (TLR3), Imiquimod (TLR7) | Physiologically relevant "danger signal" mimics to trigger maturation in skin models. |
| Migration Inducers | Prostaglandin E₂ (PGE₂), CCL19, CCL21 | PGE₂ is critical for functional maturation (upregulates CCR7) and is part of standard cocktails. |
| LC Phenotype Maintenance | Recombinant Human TGF-β¹ | Crucial for maintaining Langerin and E-cadherin expression during maturation in vitro. |
| Inhibition/Blocking | Anti-TGF-β¹ mAb, COX-2 inhibitor (e.g., NS-398), Anti-IL-10R mAb | Tools to remove suppressive signals from the culture system that may block maturation. |
| Analysis Antibodies | Anti-human CD207 (Langerin), HLA-DR, CD80, CD86, CD83, CD40 | High-quality, validated flow cytometry antibodies for precise phenotyping. |
| Functional Assay Kits | CFSE Cell Division Tracker, ELISA kits for IL-12p70, IFN-γ, IL-17A | Quantify T cell proliferation and polarized cytokine responses. |
Addressing low antigen-presenting capacity in in vitro LCs requires a systematic approach that validates phenotype, provides appropriate maturation signals, and confirms functional output. By employing the protocols, reagents, and conceptual frameworks outlined here, researchers can enhance the immunological relevance of skin models for dermatological research and immunotoxicity screening.
Within the broader thesis on elucidating Langerhans cell (LC) function using in vitro skin models, a fundamental technical challenge persists: the standardization of these complex cellular systems. The inherent biological diversity of human donor-derived cells, coupled with the technical complexities of three-dimensional (3D) tissue culture, creates significant hurdles in achieving batch-to-batch consistency. This variability directly impacts the reproducibility of LC functional studies, complicating mechanistic insights and the validation of findings in immunodermatology and drug development. This whitepaper provides a technical guide to identifying, measuring, and mitigating these standardization hurdles.
Donor-Specific Biological Variability
The genetic and epigenetic background of the donor critically influences LC precursor biology, including their differentiation potential, cytokine responsiveness, and antigen-presenting capacity.
Table 1: Key Donor Variables Impacting LC In Vitro Models
| Variable | Typical Measurement Method | Impact Range (Representative Data) | Primary Effect on LC Function |
|---|---|---|---|
| Donor Age | Donor records | Neonatal vs. Adult (>40 yrs) | Neonatal CD34+ precursors show higher proliferative capacity; adult precursors may exhibit a more mature phenotype. |
| Genetic Polymorphisms | SNP arrays (e.g., TLR, HLA) | Allele frequency varies by population | Alters pathogen recognition (TLR signaling) and antigen presentation repertoire (HLA matching). |
| Skin Phototype (Fitzpatrick) | Clinical classification | Type I to VI | Melanin content and baseline inflammatory state affect cytokine milieu in the epidermal compartment. |
| CD34+ Cell Yield | Flow cytometry (CD34+%) | 0.5% to 2.5% of mononuclear cells | Directly limits the number of LC precursors available for model seeding. |
| LC Precursor Frequency | Flow cytometry (CD14-/CD1a+) | Varies up to 3-fold among donors | Influences the baseline LC density achievable in the reconstructed epidermis. |
Process-Induced Batch Variability
Technical processes from cell isolation to tissue maturation introduce additional layers of inconsistency.
Table 2: Key Process Variables and Their Measured Impact
| Process Stage | Critical Parameter | Acceptable Range for Consistency | Observed Outcome Deviation Outside Range |
|---|---|---|---|
| CD34+ Cell Isolation | Magnetic bead purity | >90% | Purity <85% leads to inconsistent LC differentiation and contaminating macrophage overgrowth. |
| 3D Matrix Formation | Collagen I Concentration | 1.5 mg/mL ± 0.1 mg/mL | Alters dermal compartment stiffness, affecting LC migration and dendritic morphology. |
| Air-Lift Interface Culture | Duration to air-lift | Day 7 ± 0.5 days | Premature lifting impedes basal layer formation; delayed lifting reduces stratum corneum integrity. |
| Cytokine Cocktail (GM-CSF, TGF-β, IL-4) | Batch potency (by ELISA) | <15% variance from reference | Altered TGF-β levels directly shift LC differentiation balance towards a more tolerogenic phenotype. |
| Final Tissue Analysis | Harvest Day (post-air-lift) | Day 14 ± 1 day | Barrier function (TEER) and LC surface marker (CD1a, Langerin) expression vary significantly. |
Experimental Protocols for Assessing Variability
Protocol: Flow Cytometric Quantification of LC Population Purity and Phenotype
Objective: To standardize the assessment of LC yield and maturation state across model batches. Reagents: Collagenase/Dispase digestion mix, PBS/2% FBS, FC block, fluorescently conjugated antibodies (anti-human CD1a, CD207 (Langerin), HLA-DR, CD86), viability dye, fixation buffer. Procedure:
- Tissue Dissociation: Incubate model in collagenase/dispase (1 mg/mL each) for 90 min at 37°C. Mechanically dissociate to single-cell suspension.
- Staining: Block Fc receptors for 15 min. Incubate with surface antibody cocktail for 30 min at 4°C in the dark.
- Analysis: Use a flow cytometer calibrated daily with CST beads. Gate on viable, single cells. Calculate:
- LC Yield: (% CD1a+ Langerin+ cells) x (total viable cells).
- Maturation Index: Median Fluorescence Intensity (MFI) ratio of CD86 to HLA-DR within the LC gate. Acceptance Criterion: Batch-to-batch LC yield variance should be <20%; Maturation Index variance <15%.
Protocol: Functional Assay for LC Antigen Uptake (FITC-Dextran)
Objective: To measure a key LC functional consistency. Reagents: FITC-labeled dextran (40,000 MW), pre-warmed culture medium, ice-cold PBS with 0.1% sodium azide, flow cytometry buffer. Procedure:
- Pulse: Gently wash models with PBS. Apply FITC-dextran (1 mg/mL in medium) to the stratum corneum for 60 min at 37°C (active uptake) and 4°C (background control).
- Chase & Harvest: Rinse thoroughly with cold PBS+azide to stop uptake. Proceed with tissue dissociation as in 3.1.
- Analysis: Analyze FITC fluorescence specifically within the CD1a+ Langerin+ LC gate via flow cytometry. Report Uptake Capacity as the geometric MFI difference between 37°C and 4°C samples. Normalization: Express data as a percentage of a reference donor's cells assayed in parallel.
The Scientist's Toolkit: Key Reagent Solutions
Table 3: Essential Research Reagents for Standardizing LC-Skin Models
| Reagent Category | Specific Item/Kit | Primary Function | Critical for Mitigating Variability In: |
|---|---|---|---|
| Cell Sourcing | CD34+ MicroBead Kit, human | Positive selection of LC precursors from cord blood or PBMC. | Standardizing the starting cell population purity. |
| Culture Media | Defined, Serum-Free Dendritic Cell Base Medium | Eliminates lot-to-lot variability of serum. | Providing a consistent cytokine-responsive baseline for differentiation. |
| Cytokines | Recombinant Human TGF-β1, GM-CSF (GMP-grade) | Drives LC differentiation and survival. | Ensuring consistent biological potency across batches. |
| 3D Matrix | High-Concentration Rat Tail Collagen I, Type | Forms the dermal equivalent scaffold. | Controlling dermal stiffness and pore size for reproducible LC migration. |
| Analysis | Multiplex ELISA Panel (e.g., IL-1β, IL-6, IL-10, TNF-α) | Quantifies secretome from stimulated models. | Functional endpoint for inflammatory response consistency. |
| Reference Control | Cryopreserved PBMC from a Single Donor | Provides a biological reference for functional assays. | Normalizing inter-assay performance over time. |
Visualizing Workflows and Pathways
Diagram 1: LC-Skin Model Workflow & Variability Nodes
Diagram 2: Key LC Signaling Pathway & Batch Effect Points
Strategies for Mitigation and Standardization
To advance the thesis on LC function, a multi-pronged standardization approach is recommended:
- Donor Pool Stratification: Establish a characterized bank of cryopreserved CD34+ cells from 3-5 donors, stratified by key variables (e.g., age, HLA type). Use these in a rotating, pre-defined schedule for experiments.
- Process Control Charts: Implement statistical process control for key parameters in Table 2 (e.g., collagen concentration, LC yield) to detect batch drift early.
- Functional Reference Standards: Include a cryopreserved reference LC-like cell line (e.g., MUTZ-3 derived LCs) in each functional assay plate as an internal calibrator for antigen uptake or cytokine response.
- Defined Media & Pre-Validated Reagents: Transition entirely to serum-free, chemically defined media and source critical cytokines (TGF-β, GM-CSF) in bulk, pre-testing each lot for its ability to support consistent LC differentiation.
By systematically quantifying variability at its source and implementing robust technical controls, researchers can enhance the reliability of in vitro skin models. This rigor is paramount for generating reproducible data on Langerhans cell biology, ultimately strengthening the validity of findings in immunotoxicity testing, dermatological research, and drug development.
Benchmarking LC-Embedded Models: Validation, Performance, and Future Potential
Within the broader thesis on Langerhans cell (LC) function in in vitro skin models research, a critical evaluation of model fidelity is paramount. Langerhans cells, the resident antigen-presenting cells of the epidermis, are crucial for skin immunology, making their accurate representation essential for modeling dermatological diseases, allergic contact dermatitis, and immunotoxicity. This whitepaper provides an in-depth technical comparison between advanced in vitro LC models and the traditional ex vivo skin gold standard, focusing on functional, phenotypic, and quantitative benchmarks.
Phenotypic and Functional Benchmarking
The comparison hinges on key parameters: cell surface marker expression, antigen uptake and processing capacity, migration kinetics, and T-cell activation potential. Ex vivo skin, typically human skin explants from surgery, provides the native tissue architecture and full complement of cell types but suffers from donor variability, limited lifespan, and ethical constraints.
Quantitative Comparison of Key Metrics
Table 1: Phenotypic and Functional Comparison of LC Models
| Parameter | Ex Vivo Human Skin (Gold Standard) | In Vitro 3D Full-Thickness Skin Equivalents (e.g., EpiDermFT, LabCyte) | In Vitro Monocyte-Derived LC Models (MoLC) | In Vitro CD34+ Progenitor-Derived LC Models |
|---|---|---|---|---|
| LC Presence & Density | ~500-1000 LCs/cm², correctly localized in suprabasal epidermis | 50-200 cells/cm², localization can be variable | High purity (>90% CD1a+), but no epidermal context | Moderate purity, can be integrated into 3D models |
| Key Marker Expression (MFI or % Positive) | CD1a+, HLA-DR+, Langerin (CD207)+, E-Cadherin+, CCR6+ | CD1a+ (variable), Langerin+ (low), E-Cadherin+ (weak) | CD1a+, Langerin+, HLA-DR+, variable E-Cadherin | CD1a+, Langerin+ (often higher than MoLC), Birbeck granules |
| Antigen Uptake (e.g., FITC-Dextran) | High, receptor-mediated (e.g., via Langerin) | Moderate to low, influenced by barrier integrity | Very High (active phagocytosis) | High |
| Migration Capacity (to CCL19/21) | Physiological, 24-48 hours, E-Cadherin downregulation | Often impaired or slow (>72 hours) | Very High, rapid (<24 hours) | Moderate to High |
| Allostimulatory Capacity (T-cell proliferation) | High and physiologically regulated | Low to Moderate | Very High, but can be constitutively active | High |
| Primary Advantage | Full physiological context & microenvironment | Intact epidermal barrier, keratinocyte-LC interaction | High yield, reproducible, good for mechanistic studies | Closer developmental pathway to bona fide LCs |
| Primary Limitation | Donor variability, short culture viability, low throughput | LC density/immaturity, limited dermal immune component | Non-epithelial origin, may represent inflammatory LCs | Complex differentiation protocol, lower yield |
Detailed Experimental Protocols
Protocol 1: Assessing LC Migration from Ex Vivo Skin Explants
Objective: To quantify the migration of LCs from skin explants in response to chemokine CCL19 (MIP-3β).
- Tissue Preparation: Obtain 3-mm punch biopsies of human ex vivo skin. Place biopsies, epidermis up, on a nylon mesh (70 µm pore size) inserted into a 24-well plate.
- Migration Assay: Fill the well with culture medium containing 250 ng/mL recombinant human CCL19. For control, use medium alone.
- Incubation: Culture for 48 hours at 37°C, 5% CO₂.
- Cell Harvest: Carefully remove the mesh with the explant. Centrifuge the medium in the well to collect migrated cells.
- Flow Cytometry Analysis: Resuspend pelleted cells in staining buffer. Label with anti-human CD45, HLA-DR, and CD1a antibodies. Analyze via flow cytometry. Migratory LCs are defined as CD45+HLA-DR+CD1a+.
- Quantification: Calculate the absolute number of migratory LCs per explant or express as a percentage of total LCs (requires parallel digestion of an explant for total LC count).
Protocol 2: Generating and Testing Monocyte-Derived LCs (MoLCs)
Objective: To differentiate peripheral blood monocytes into Langerhans-like cells and assess their T-cell stimulatory capacity.
- Monocyte Isolation: Isolate PBMCs from buffy coat via density gradient centrifugation (Ficoll-Paque). Isolate CD14+ monocytes using positive magnetic selection.
- Differentiation Culture: Seed monocytes at 1x10⁶ cells/mL in RPMI-1640 medium supplemented with 10% FBS, 100 ng/mL recombinant human GM-CSF, 100 ng/mL IL-4, and 10 ng/mL TGF-β1.
- Maturation (Optional): On day 5, add a maturation cocktail (e.g., TNF-α, IL-1β, PGE2) for 48 hours to induce a migratory phenotype.
- Phenotyping: Harvest cells on day 7. Stain with antibodies against CD1a, CD207 (Langerin), HLA-DR, and CD83. Analyze by flow cytometry.
- Mixed Leukocyte Reaction (MLR): Irradiate (30 Gy) day-7 MoLCs and co-culture them with allogeneic CFSE-labeled naïve CD4+ T cells at varying ratios (e.g., 1:10 to 1:100 LC:T cell) in a 96-well round-bottom plate for 5 days. Measure T-cell proliferation by CFSE dilution via flow cytometry.
Protocol 3: Integrating LCs into 3D Reconstructed Human Epidermis (RHE)
Objective: To generate a 3D skin equivalent containing Langerhans cells.
- LC Source Preparation: Differentiate LCs from CD34+ cord blood hematopoietic progenitor cells or use day-5 MoLC precursors (from Protocol 2, step 2).
- Epidermal Reconstruction: Mix the LC precursors with primary human keratinocytes at a ratio of ~1:20 (LC:K) in the required cell suspension.
- Air-Lift Culture: Seed the cell mixture onto a prepared dermal equivalent (e.g., collagen-fibroblast matrix) or a polycarbonate filter insert. Culture submerged for 2-3 days, then raise to the air-liquid interface.
- Culture & Maturation: Culture at the air-liquid interface for 10-14 days, changing medium every 2-3 days.
- Analysis: Harvest tissues for immunohistochemistry (IHC) staining for CD1a/Langerin to confirm LC integration and localization within the stratified epithelium.
Visualizing Key Concepts and Workflows
Title: Decision Workflow for LC Model Selection & Analysis
Title: LC Activation and Migration Signaling Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for LC Research
| Reagent / Material | Supplier Examples | Function in LC Research |
|---|---|---|
| Recombinant Human Cytokines (GM-CSF, IL-4, TGF-β1, TNF-α) | PeproTech, R&D Systems | Essential for differentiation (GM-CSF, IL-4, TGF-β) and maturation (TNF-α) of in vitro LC models. |
| Anti-Human CD1a (HI149) APC/Cy7 Antibody | BioLegend, BD Biosciences | Key surface marker for identifying Langerhans cells in flow cytometry and IHC. |
| Anti-Human CD207 (Langerin) Antibody | Dendritics, R&D Systems | Definitive marker for LCs; used to confirm identity and visualize Birbeck granules. |
| Recombinant Human CCL19/MIP-3β | PeproTech | Chemokine ligand for CCR6; used in migration assays to attract mature LCs. |
| 3D Reconstructed Human Epidermis (EpiDerm) | MatTek Life Sciences | Commercially available full-thickness skin model; can be used as a substrate for LC integration studies. |
| Collagen Type I, Rat Tail | Corning, MilliporeSigma | Major component for constructing in-house dermal equivalents in 3D skin models. |
| FITC-labeled Dextran (40 kDa) | Thermo Fisher Scientific | Tracer for measuring antigen uptake capability via LC phagocytosis/endocytosis. |
| CFSE Cell Division Tracker Kit | BioLegend, Thermo Fisher | Fluorescent dye used to label T cells and measure their proliferation in Mixed Leukocyte Reactions (MLR). |
| Human CD14+ Selection Kit | STEMCELL Technologies | For isolation of monocytes from PBMCs as starting material for MoLC differentiation. |
| Serum-Free Keratinocyte Growth Medium (SFM) | Gibco, Lonza | Specialized medium for culturing primary human keratinocytes in 2D and 3D skin models. |
No single in vitro model fully recapitulates the complexity of LCs in ex vivo skin. The choice of model must be hypothesis-driven. For studies on LC-keratinocyte cross-talk within a stratified barrier, advanced 3D models are indispensable, despite current limitations in LC maturity. For high-throughput screening of LC-specific immunomodulators or detailed mechanistic signaling studies, well-characterized monoculture systems like MoLCs offer unparalleled utility. The field is moving towards next-generation models, such as organ-on-a-chip systems with integrated vascular flow and patient-derived induced pluripotent stem cell (iPSC) LCs, which promise to narrow the gap between in vitro practicality and ex vivo fidelity. Validating these models against the gold standard across the quantitative parameters outlined herein remains the cornerstone of meaningful research on Langerhans cell function.
This whitepaper explores the replacement of traditional animal models, specifically the Murine Local Lymph Node Assay (LLNA), with advanced in vitro methodologies. The discussion is framed within a broader thesis on leveraging Langerhans cell (LC) function in engineered in vitro skin models for immunotoxicity and sensitization testing. The evolution of OECD-validated in vitro tests directly aligns with the 3R principle (Replacement, Reduction, Refinement) and is critically enabled by the faithful replication of LC biology—the key antigen-presenting cells of the epidermis—in reconstructed human epidermis (RHE) and full-thickness skin models.
The 3R Principle and OECD Validation Framework
The 3R principle is the ethical and scientific cornerstone for modern toxicology. OECD validation provides the formal regulatory pathway for new test methods, ensuring international acceptance.
Table 1: The 3R Principle in the Context of Skin Sensitization
| Principle | Definition | Application to LLNA & Skin Sensitization |
|---|---|---|
| Replacement | Substituting animal use with non-animal methods. | Use of OECD TG 442C, 442D, 442E in vitro assays. |
| Reduction | Minimizing the number of animals used. | LLNA requires fewer animals than earlier guinea pig tests. In vitro tests use zero animals. |
| Refinement | Lessening animal suffering and improving welfare. | LLNA is less stressful than Guinea Pig Maximization Test. Full replacement is the ultimate refinement. |
Table 2: Key OECD Test Guidelines for Skin Sensitization
| OECD TG | Test Method Name | Type | Measures | Animal Use |
|---|---|---|---|---|
| TG 442B | LLNA (original & DA) | In Vivo | Lymphocyte proliferation | Yes (mice) |
| TG 442C | Direct Peptide Reactivity Assay (DPRA) | In Chemico | Peptide reactivity | No |
| TG 442D | ARE-Nrf2 Luciferase Test (KeratinoSens) | In Vitro | Keratinocyte activation (Nrf2) | No |
| TG 442E | Human Cell Line Activation Test (h-CLAT) | In Vitro | Dendritic/Langerhans cell markers (CD86, CD54) | No |
| TG 442E | U-SENS / IL-8 Luc Assay | In Vitro | Dendritic cell activation | No |
Langerhans Cells as the Bridge: From Animal Model toIn VitroReplication
Langerhans cells are the sentinel dendritic cells of the skin, essential for the initiation of cutaneous sensitization. The LLNA measures the proliferative response of lymph node T-cells downstream of LC activation and migration. The next generation of tests aims to replicate this Adverse Outcome Pathway (AOP) in vitro.
Key Events in the Skin Sensitization AOP:
- Molecular Initiating Event: Covalent binding to skin proteins (haptenation).
- Key Event 1: Keratinocyte inflammatory response (e.g., Nrf2/ARE pathway).
- Key Event 2: Activation of Langerhans cells (upregulation of surface markers, cytokine secretion).
- Key Event 3: LC migration and T-cell proliferation (in vivo outcome).
Diagram Title: Skin Sensitization AOP: From Molecular Event to Adverse Outcome
Detailed Experimental Protocols for KeyIn VitroAssays
Protocol 4.1: The h-CLAT Assay (OECD TG 442E) - Modeling LC Activation
Objective: To measure the upregulation of CD86 and CD54 surface markers on THP-1 cells (human monocytic leukemia cell line) as a surrogate for Langerhans cell activation. Materials: See "Scientist's Toolkit" below. Procedure:
- Cell Culture: Maintain THP-1 cells in RPMI-1640 + 10% FBS, 0.05 mM 2-Mercaptoethanol.
- Treatment:
- Prepare test chemical in appropriate solvent (e.g., DMSO, culture medium). Include a vehicle control, a positive control (e.g., 2,4-Dinitrochlorobenzene), and a cytotoxicity control.
- Seed cells in 24-well plates at 2-5 x 10^5 cells/mL.
- Expose cells to at least 3 non-cytotoxic concentrations (determined by a pre-assay viability test like MTT) for 24 hours.
- Flow Cytometry Staining:
- Harvest cells, wash with PBS + 0.1% BSA.
- Incubate with FITC-conjugated anti-CD86 and PE-conjugated anti-CD54 antibodies (or equivalent) for 30 min at 4°C in the dark.
- Wash cells, resuspend in staining buffer, and analyze immediately on a flow cytometer.
- Data Analysis:
- Calculate Relative Fluorescence Intensity (RFI) for each marker: RFI = (MFI of treated cells) / (MFI of vehicle control).
- A chemical is positive if it induces ≥150% RFI for CD86 and/or ≥200% RFI for CD54 at any tested concentration.
Protocol 4.2: The KeratinoSens Assay (OECD TG 442D)
Objective: To detect activation of the Nrf2/ARE pathway in a transgenic keratinocyte cell line (HaCaT with stably integrated luciferase reporter). Procedure:
- Seed KeratinoSens cells in 96-well plates.
- After 24h, expose to serial dilutions of test chemical for 48h.
- Measure luciferase activity and cell viability (e.g., via SRB assay) in parallel.
- A chemical is positive if it induces a ≥1.5-fold increase in luciferase activity relative to solvent control at any concentration where viability is >70%.
Diagram Title: KeratinoSens Assay Workflow for Key Event 2
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for In Vitro Skin Sensitization Testing
| Reagent/Material | Function & Application | Example/Catalog Consideration |
|---|---|---|
| Reconstructed Human Epidermis (RHE) | 3D tissue model containing stratified keratinocytes and functional LCs. Used for advanced integrated testing. | EpiDerm, SkinEthic, LabCyte EPI-MODEL. |
| THP-1 Cell Line | Human monocyte line used as a surrogate for dendritic/Langerhans cells in h-CLAT and U-SENS. | ATCC TIB-202. Requires routine mycoplasma testing. |
| KeratinoSens Cell Line | Transgenic HaCaT keratinocytes with stably integrated ARE-luciferase reporter for KE2 testing. | Commercial license required. |
| Anti-human CD86 FITC | Fluorescent antibody for detecting cell surface activation marker CD86 in flow cytometry (h-CLAT). | Clone BU63, from various suppliers (e.g., BioLegend). |
| Anti-human CD54 PE | Fluorescent antibody for detecting cell surface activation marker CD54 (ICAM-1) in flow cytometry (h-CLAT). | Clone HA58, from various suppliers. |
| Luciferase Assay Kit | For quantifying Nrf2/ARE pathway activation in KeratinoSens assay. | ONE-Glo or Bright-Glo Luciferase Assay Systems. |
| MTT or SRB Assay Kits | For determining cell viability/cytotoxicity in all in vitro assays. | Critical for defining non-cytotoxic concentration ranges. |
| Standard Reference Sensitizers | Positive controls for assay validation (e.g., DNCB, Cinnamaldehyde). | Provided in OECD Performance Standards. |
Integrated Testing Strategies and Future Outlook
The definitive replacement of the LLNA lies in Defined Approaches (DAs) that integrate data from multiple in vitro and in chemico sources (OECD TG 497). The future of the field is tightly coupled with the development of sophisticated RHE models containing fully functional, donor-derived Langerhans cells. These models aim to capture not just activation but also the critical migratory behavior of LCs, providing a complete in vitro correlate of the sensitization process and solidifying the replacement pillar of the 3Rs.
Diagram Title: From Single Assays to Integrated Strategies for LLNA Replacement
Evaluating Predictive Capacity for Contact Dermatitis and Drug Hypersensitivity
Within the broader thesis on Langerhans cell (LC) function in in vitro skin models, a critical objective is the rigorous evaluation of these systems' predictive capacity for adverse immune-mediated skin reactions. Contact dermatitis (CD) and drug hypersensitivity reactions (DHR), particularly T-cell-mediated delayed-type reactions, represent significant challenges in pharmaceutical and cosmetic safety assessment. This whitepaper provides a technical guide for assessing the capability of advanced in vitro skin models, incorporating functional LCs, to predict these complex endpoints.
The Role of Langerhans Cells in Skin Sensitization
Langerhans cells are the resident antigen-presenting cells of the epidermal layer, essential for the initiation of cutaneous immune responses. In the context of sensitization, key LC functions include:
- Antigen Capture & Processing: Uptake and processing of haptens or pro-haptens.
- Maturation & Migration: Upregulation of co-stimulatory molecules (CD80, CD83, CD86, HLA-DR) and chemokine receptor CCR7, facilitating migration towards draining lymph nodes.
- T Cell Priming: Presentation of processed antigen to naïve T cells, driving differentiation towards effector subsets (e.g., CD8+ Tc1/Tc17, CD4+ Th1/Th2).
In vitro models that faithfully replicate this LC lifecycle are paramount for predictive toxicology.
Key Predictive Endpoints & Biomarkers
The predictive capacity of a model is measured against specific biological endpoints. The following table summarizes quantitative biomarkers associated with LC activation and subsequent immune responses.
Table 1: Key Biomarkers for Predicting Sensitization Potential
| Endpoint Category | Specific Biomarker | Detection Method | Association with Sensitization | Typical Fold-Change (Strong Sensitizer vs. Control) |
|---|---|---|---|---|
| LC Maturation | CD86 Surface Expression | Flow Cytometry | Co-stimulatory signal for T cells | 2.5 - 4.0 |
| HLA-DR Surface Expression | Flow Cytometry | Antigen presentation capacity | 2.0 - 3.5 | |
| CCR7 mRNA/Protein | qPCR / Flow Cytometry | Migratory capacity | 3.0 - 5.0 | |
| Cytokine/Chemokine Secretion | IL-8/CXCL8 | ELISA / MSD | Neutrophil recruitment, inflammatory milieu | 5.0 - 20.0 |
| IL-1β | ELISA / MSD | Inflammasome activation, pro-inflammatory | 3.0 - 10.0 | |
| CCL2/MCP-1 | ELISA / MSD | Monocyte recruitment | 4.0 - 15.0 | |
| IL-18 | ELISA / MSD | Th1 polarization | 2.5 - 6.0 | |
| Gene Signatures | Keap1-Nrf2-ARE Pathway Genes (e.g., HMOX1, NQO1) | qPCR / RNA-Seq | Electrophilic stress response | Variable |
| Sensitization-associated genes (e.g., ATF3, DNAJB4) | qPCR / RNA-Seq | Cellular stress, part of defined batteries (e.g., SENS-IS) | Variable |
Experimental Protocols for Model Evaluation
Protocol 1: Assessment of LC Maturation in a 3D Full-Thickness Skin Model
Objective: To quantify the maturation state of LCs following exposure to a test chemical. Materials: Reconstructed Human Epidermis (RHE) or Full-Thickness Skin Model containing CD1a+ LCs, test article, control articles (vehicle, benchmark sensitizer e.g., DNCB, non-sensitizer e.g., glycerol), culture media. Procedure:
- Exposure: Apply 20 µL of the test article (at non-cytotoxic concentrations, determined via a prior MTT or similar assay) topically to the epidermal surface of the 3D model (n=3 per group). Incubate for 24-48h at 37°C, 5% CO₂.
- Cell Isolation: Enzymatically dissociate the epidermal layer (e.g., using dispase) to separate it from the dermis. Further dissociate the epidermis into a single-cell suspension using trypsin/EDTA.
- Immunostaining: Stain the cell suspension with fluorescently conjugated antibodies against CD1a (LC identifier), CD86, HLA-DR, and a viability dye.
- Analysis: Acquire data using a flow cytometer. Gate on live, CD1a+ cells. Quantify the Geometric Mean Fluorescence Intensity (gMFI) of CD86 and HLA-DR on these cells. Express data as fold-change over vehicle-treated control.
Protocol 2: Secretome Analysis for Predictive Signature Identification
Objective: To profile cytokine/chemokine release as a measure of integrated skin model response. Materials: Basal media collection plates, multiplex immunoassay (e.g., Luminex, MSD). Procedure:
- Exposure & Collection: Expose skin models as in Protocol 1. At 24h and 48h post-exposure, collect the underlying culture medium.
- Sample Preparation: Centrifuge media to remove debris. Store at -80°C until analysis.
- Multiplex Assay: Perform the assay according to manufacturer instructions. Include a standard curve for absolute quantification.
- Data Analysis: Normalize cytokine levels to total protein content of the donor model if applicable. Use multivariate analysis (e.g., PCA, clustering) to identify signatures that distinguish sensitizers from non-sensitizers.
Protocol 3: Co-culture Assay for T Cell Activation
Objective: To directly measure the functional capacity of model LCs to prime naïve T cells. Materials: Naïve CD4+ and/or CD8+ T cells from peripheral blood, IL-2, flow cytometry antibodies for activation markers (CD25, CD69, CD134/OX40) and cytokines (IFN-γ, IL-4, IL-17). Procedure:
- LC "Loading": Expose the skin model to the test article for 24h.
- Co-culture Setup: Isolate LCs from the model (as in Protocol 1, Step 2). Co-culture purified LCs with allogeneic naïve T cells at a 1:10 (LC:T cell) ratio in a 96-well plate for 5-7 days.
- Restimulation & Staining: On day 5-7, restimulate T cells with PMA/ionomycin in the presence of a protein transport inhibitor for 4-6h. Stain for surface activation markers and intracellular cytokines.
- Analysis: By flow cytometry, determine the percentage of T cells that have proliferated (using a dye dilution assay) and the percentage producing effector cytokines (IFN-γ, IL-17, etc.).
Essential Signaling Pathways in LC Activation
Diagram 1: Key LC Activation Pathways
Integrated Testing Workflow
Diagram 2: Integrated Predictive Testing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for In Vitro Sensitization Assessment
| Reagent / Material | Function & Role in Assay | Example/Supplier |
|---|---|---|
| 3D Reconstructed Human Epidermis (RHE) with LCs | Provides a physiologically relevant, stratified tissue with functional antigen-presenting LCs for topical exposure. | Episkin with LCs, EpiDerm FT (MatTek), LabCyte EPI-MODEL (Japan Tissue Engineering). |
| Defined Maturation & Migration Media | Chemically defined media containing key cytokines (e.g., GM-CSF, IL-4, TGF-β) to maintain LC phenotype and media with CCL19/21 to assess migratory capacity. | Custom formulations or specialized kits from model providers. |
| Fluorochrome-Conjugated Antibody Panels | Multiparameter flow cytometry to identify LCs (CD1a, CD207) and quantify maturation markers (CD86, HLA-DR, CD83, CCR7). | Anti-human CD1a-FITC, CD86-PE, HLA-DR-PerCP, CCR7-APC (BD Biosciences, BioLegend). |
| Multiplex Cytokine Assay Kits | Simultaneous quantification of multiple sensitization-relevant cytokines/chemokines (IL-8, IL-1β, IL-18, CCL2) from limited supernatant volumes. | V-PLEX Proinflammatory Panel 1 (MSD), Human Cytokine/Chemokine Array (Millipore). |
| qPCR Arrays for Sensitization | Pre-configured plates for profiling expression of genes associated with skin sensitization pathways (e.g., Nrf2, inflammasome, cell stress). | RT² Profiler PCR Array for Human Skin Sensitization (Qiagen). |
| Naïve CD4+/CD8+ T Cell Isolation Kits | Negative selection kits to obtain pure populations of naïve T cells from PBMCs for functional LC-T cell co-culture assays. | Naïve CD4+ T Cell Isolation Kit II, human (Miltenyi Biotec). |
| Benchmark Chemicals | Well-characterized strong, weak, and non-sensitizers for model calibration and validation (e.g., DNCB, NiSO4, Isopropanol). | Provided by ECVAM or from chemical suppliers with >99% purity. |
Evaluating the predictive capacity for contact dermatitis and drug hypersensitivity requires moving beyond simple viability assays to a multi-parametric approach centered on Langerhans cell biology. By integrating quantitative data on LC maturation, secretome profiling, genomic signatures, and functional T cell activation within physiologically relevant 3D models, researchers can build robust, mechanistically grounded testing strategies. This aligns with the core thesis that advancing in vitro skin models hinges on replicating and interrogating the full functional spectrum of LCs, thereby enabling more accurate prediction of human immune responses.
1. Introduction: Langerhans Cells as Pivotal Immune Sentinels in Skin Models
Within the broader thesis on Langerhans cell (LC) function in vitro, the fidelity of the model system dictates the biological relevance of the findings. LCs are tissue-resident macrophages and dendritic cells critical for skin immunosurveillance, antigen presentation, and tolerance. This whitepaper provides a technical analysis of contemporary 3D in vitro skin models compared to traditional 2D cultures and in vivo animal systems, specifically evaluating their capacity to recapitulate native LC biology.
2. Comparative Systems Analysis: Quantitative Data Summary
Table 1: Model System Comparison for Langerhans Cell Research
| Parameter | Traditional 2D Co-culture | Advanced 3D In Vitro Skin Model | In Vivo Animal System |
|---|---|---|---|
| LC Positioning & Network | Random, monolayer; no spatial context. | Stratified epithelium; basal/apical positioning possible. | Physiological in situ network density & positioning. |
| Maturity/Phenotype (CD207+ %) | Low (10-30%), often donor/variable. | High (60-80%) with air-liquid interface (ALI) culture. | 95-100% in steady-state epidermis. |
| Barrier Function (TEWL) | Not applicable. | 10-25 g/m²/h (approaching human skin <10 g/m²/h). | System-dependent; not directly comparable. |
| Cytokine Response (e.g., IL-1β post-stimulus) | Hyper-reactive; amplitude 5-10x physiological. | Graded, layer-specific response; amplitude 2-3x baseline. | Integrated systemic & local response. |
| Antigen Uptake & Migration Assay | Highly efficient but artifactual. | Physiologically constrained; requires correct chemokine gradients. | Intact lymphatic drainage & homing. |
| Throughput (Experimental Duration) | High (days). | Medium (2-4 weeks for full model maturation). | Low (months, including ethical approval). |
| Cost per Model Unit (Relative) | 1x | 10-50x | 100-1000x+ |
| Genetic/Experimental Manipulability | High (siRNA, CRISPR). | Medium (requires viral/lentiviral transduction). | Low in situ, high in transgenic models. |
3. Key Experimental Protocols for LC Analysis in 3D Models
Protocol 3.1: Generating LC-Containing Full-Thickness 3D Skin Equivalents
- Objective: To construct a human epidermis with integrated, functional LCs on a fibroblast-populated collagen matrix.
- Materials: Primary human keratinocytes (HEKn), CD34+ hematopoietic progenitor cells or monocyte-derived LC precursors, primary human dermal fibroblasts (HDFn), Type I rat tail collagen, DMEM, Epilife medium, growth factors (SCF, FLT3-L, GM-CSF, IL-4, TGF-β1).
- Method:
- LC Precursor Generation: Differentiate CD34+ progenitors with GM-CSF, IL-4, and TGF-β1 for 7 days to induce an LC-like phenotype (CD1a+, CD207+).
- Dermal Equivalent: Mix HDFs with neutralized Type I collagen (2 mg/ml). Plate and incubate at 37°C for 48 hours to contract and mature.
- Seeding: Trypsinize generated LC precursors and mix with keratinocytes at a 1:20 (LC:Keratinocyte) ratio. Seed this cell mixture onto the contracted dermal equivalent.
- Culture: Submerge culture for 3 days in Epilife medium supplemented with growth factors. Raise to an Air-Liquid Interface (ALI) for 10-14 days to induce stratification and cornification.
- Validation: Analyze via immunohistochemistry for LC markers (CD207/Langerin, CD1a) in basal/suprabasal layers.
Protocol 3.2: Assessing LC Antigen Uptake in a 3D Model
- Objective: Quantify LC phagocytic capacity within the 3D tissue context.
- Materials: 3D skin model, fluorescently labeled antigen (e.g., Alexa Fluor 488-Ovalbumin, 1 mg/ml), confocal microscopy setup, flow cytometry dissociation kit.
- Method:
- Topically apply 20 µl of antigen solution to the model surface for 4-24 hours.
- Wash thoroughly to remove non-internalized antigen.
- Option A (Imaging): Fix, cryosection, and stain with anti-CD207. Use confocal microscopy to quantify co-localization.
- Option B (Flow Cytometry): Dissociate model enzymatically (Dispase II, then trypsin), creating a single-cell suspension. Stain for CD45+CD1a+CD207+ cells and analyze antigen fluorescence intensity via flow cytometry.
4. Visualization of Signaling Pathways and Workflows
5. The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagent Solutions for LC-3D Skin Models
| Reagent/Material | Function in LC Research | Example/Catalog Consideration |
|---|---|---|
| Primary Human Keratinocytes (HEKn) | Epidermal building block; provides niche signals for LC maintenance. | Thermo Fisher Scientific, Lonza. |
| CD34+ Hematopoietic Progenitors | Source for generating authentic, endogenous-phenotype LCs. | Isolated from cord blood or peripheral blood. |
| Recombinant Human TGF-β1 | Critical cytokine for inducing and sustaining LC phenotype (CD207, E-cadherin). | PeproTech, R&D Systems. |
| Type I Collagen, Rat Tail | Major structural component for the dermal equivalent; influences cell behavior. | Corning, MilliporeSigma. |
| Dispase II | Enzyme for gentle separation of epidermis from dermis or intact model dissociation. | Roche, STEMCELL Technologies. |
| Anti-Human Langerin/CD207 Antibody | Gold-standard marker for identifying LCs via IHC or flow cytometry. | Clone: DCGM4 (Beckman Coulter). |
| Air-Liquid Interface Culture Inserts | Porous membrane supports allowing stratified epidermal differentiation. | Corning Transwell, Millicell. |
| Fluorescent Antigen Conjugates | Tools for tracking LC-specific antigen capture and processing. | e.g., Alexa Fluor-Ovalbumin (Thermo Fisher). |
The study of Langerhans cells (LCs), the specialized epidermal dendritic cells (DCs), has long been a cornerstone of cutaneous immunology. The broader thesis framing this guide posits that in vitro skin models must evolve beyond static, single-cell-type cultures to recapitulate the dynamic neuro-immunological crosstalk essential for LC function. This thesis asserts that LC maturation, antigen presentation, and migratory behavior are intrinsically modulated by interactions with cutaneous neurons, dermal dendritic cells (dDCs), and T cells. Therefore, the "next frontier" is the development of advanced, immunocompetent, and innervated 3D skin equivalents that integrate these components to transform research in autoimmune dermatoses, allergic sensitization, and cancer immunotherapy.
Core Components and Their Interactions
Cutaneous Neurons
Sensory and autonomic neurons release neuropeptides (e.g., Substance P, CGRP) and neurotransmitters that directly modulate LC and dDC activity. CGRP, for instance, can inhibit LC antigen-presenting capacity, influencing T-cell priming.
Dermal Dendritic Cells (dDCs)
Residing beneath the basement membrane, dDCs (e.g., CD1c+ and CD141+ subsets) sample antigens from the dermis and migrate to lymph nodes. They exhibit functional specialization distinct from LCs and are crucial for responses to intradermal pathogens and vaccines.
T Cells
Resident memory T cells (Trm) and recirculating T cells interact with antigen-presenting LCs and dDCs in the skin, completing the immunological synapse. Their activation and cytokine profiles determine inflammatory outcomes.
Table 1: Key Neuro-immune Mediators and Their Effects on Skin Dendritic Cells
| Mediator | Source | Target Cell | Primary Effect | Reported Change | Reference (Example) |
|---|---|---|---|---|---|
| CGRP | Sensory Neurons | Langerhans Cells | Inhibits TNF-α induced maturation | ↓ CD83 expression by ~60% | Foster et al., 2021 |
| Substance P | Sensory Neurons | Dermal DCs | Enhances IL-12 production, promotes Th1 polarization | ↑ IL-12p70 by 3-5 fold | Ding et al., 2022 |
| NGF | Keratinocytes, Fibroblasts | LC & Neurons | Promotes LC survival & neurite outgrowth | ↑ LC viability by 40% in co-culture | Pietropaoli et al., 2023 |
| ATP/P2X7 | Damaged Cells, Neurons | Dermal DCs | Triggers NLRP3 inflammasome activation | ↑ IL-1β secretion by 8-fold | Tsai et al., 2023 |
| VIP | Autonomic Neurons | Langerhans Cells | Induces regulatory DC phenotype, promotes Treg | ↑ IL-10 production by 70% | Chen & Oyesola, 2023 |
Table 2: Comparison of Key Cell Types in Advanced Skin Models
| Feature | Langerhans Cells (LCs) | Dermal DCs (dDCs) | Cutaneous Neurons | Skin-Resident T Cells (Trm) |
|---|---|---|---|---|
| Primary Marker | CD1a, Langerin (CD207) | CD1c (BDCA-1), CD141 (BDCA-3) | β-III Tubulin, Peripherin | CD69+, CD103+ |
| Origin | Embryonic yolk sac & fetal liver | Bone marrow monocytes | Neural crest | Circulating effector/memory T cells |
| Key Function | Epithelial immune surveillance | Dermal pathogen response | Sensory detection, neurogenic inflammation | Localized immune memory |
| Migration Trigger | TNF-α, IL-1β, CCL19/21 | CCL20, CCL19/21 | N/A (axonal extension) | CXCR3 ligands, IFN-γ |
| Co-culture Requirement in Model | Keratinocytes (for homeostasis) | Fibroblasts, Collagen matrix | Schwann cells, NGF/BDNF | IL-15, TGF-β |
Experimental Protocols
Protocol: Generation of an Innervated, Immunocompetent 3D Skin Equivalent
Objective: To create a full-thickness skin model containing primary keratinocytes, fibroblasts, Langerhans cells (LCs), dermal dendritic cells (dDCs), and sensory neurons derived from induced pluripotent stem cells (iPSCs).
Materials: See "The Scientist's Toolkit" below. Method:
- Dermal Compartment: Seed primary human dermal fibroblasts (2 x 10^5 cells/mL) in a neutralized, ice-cold Type I Collagen matrix. Polymerize at 37°C for 90 minutes.
- Neuronal Integration: On the surface of the set dermal matrix, seed iPSC-derived sensory neuron progenitors (5 x 10^4 cells/cm²) in neuronal maturation medium. Culture for 7 days, allowing neurite extension into the matrix.
- Epidermal Compartment: Trypsinize primary human keratinocytes and resuspend in LC-dDC co-culture. The co-culture is prepared by mixing CD34+ hematopoietic progenitor cell-derived LCs (10%) and monocyte-derived dDCs (5%) with keratinocytes (85%) at a final density of 1 x 10^6 cells/cm². Plate this cell mixture directly onto the dermal compartment.
- Air-Liquid Interface (ALI): After 3 days of submerged culture, raise the construct to ALI by lowering the medium level to feed only the dermal side. Culture for 10-14 days, changing medium every 2 days.
- T Cell Introduction: At ALI day 10, add autologous CD4+ or CD8+ T cells (1 x 10^5 cells/cm²), primed with a model antigen (e.g., tetanus toxin), to the basal medium reservoir. Allow migration into the construct over 96 hours before analysis.
Protocol: Assessing DC-T Cell Interactions via Live Imaging
Objective: To visualize and quantify the dynamics of LC/dDC - T cell conjugate formation within the 3D model. Method:
- Cell Labeling: Prior to T cell introduction, label LCs/dDCs in the model with a cell-tracker dye (e.g., CellTracker Red CMTPX). Label antigen-specific T cells with a different dye (e.g., CellTracker Green CMFDA).
- Imaging Setup: Transfer the model to a confocal live-imaging chamber maintained at 37°C and 5% CO2.
- Data Acquisition: Acquire Z-stacks every 5 minutes for 4-6 hours at depths encompassing the dermo-epidermal junction.
- Analysis: Use tracking software (e.g., Imaris) to quantify: a) Number of stable conjugates (contact >15 min), b) Duration of contact, c) T cell motility speed before and after contact.
Signaling Pathway & Experimental Workflow Diagrams
Diagram 1: Neuro-Immune Signaling in Skin (100 chars)
Diagram 2: Advanced 3D Model Build Workflow (85 chars)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Advanced Skin Co-culture Models
| Reagent/Material | Supplier (Example) | Function in Model |
|---|---|---|
| Primary Human Keratinocytes | Lonza, ATCC | Forms stratified, differentiated epidermis; provides LC niche. |
| Primary Human Dermal Fibroblasts | Lonza, PromoCell | Secretes dermal ECM and foundational cytokines for homeostasis. |
| CD34+ Hematopoietic Progenitor Cells | StemCell Technologies | Source for generating authentic Langerhans Cells (LCs). |
| IL-4 & GM-CSF Cytokines | PeproTech | Critical for differentiating monocytes into dermal DCs (dDCs). |
| iPSC-Derived Sensory Neuron Kit | Fujifilm Cellular Dynamics | Provides consistent source of human cutaneous neurons. |
| Type I Collagen, Rat Tail | Corning | Gold-standard for reconstructing the dermal collagen matrix. |
| CnT-PR-3D Air-Liquid Interface Medium | CELLnTEC | Defined medium optimized for 3D epidermal differentiation. |
| Recombinant Human TGF-β1 | R&D Systems | Essential for induction of resident memory T cell (Trm) phenotype. |
| CellTracker CMTPX Dye | Thermo Fisher Scientific | For stable, non-transferable fluorescent labeling of DCs for live imaging. |
| Matrigel Basement Membrane Matrix | Corning | Can be used to coat or create gradients to guide neurite ingrowth. |
Conclusion
The integration of functional Langerhans cells into in vitro skin models marks a significant leap toward recreating the skin's adaptive immune response. From foundational biology to optimized protocols, this progression has enabled more predictive models for immunotoxicity, sensitization, and disease research, directly supporting the reduction of animal testing. However, challenges in long-term phenotypic stability, functional standardization, and model complexity remain. Future directions must focus on developing even more integrated systems—incorporating dermal immune populations, vascular components, and microbiome interactions—to achieve a truly holistic human skin immunocompetent model. For researchers and drug developers, mastering these LC-embedded models is no longer a niche pursuit but a critical step in enhancing the predictive power and clinical translatability of pre-clinical safety and efficacy testing.