Microfluidic Platforms for Modeling Vascular Inflammation: A Comprehensive Guide to TEER Measurements and Applications
This article provides researchers, scientists, and drug development professionals with a comprehensive overview of microfluidic platforms for modeling vascular inflammation, with a focus on Transendothelial Electrical Resistance (TEER) as a...
Microfluidic Platforms for Modeling Vascular Inflammation: A Comprehensive Guide to TEER Measurements and Applications
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive overview of microfluidic platforms for modeling vascular inflammation, with a focus on Transendothelial Electrical Resistance (TEER) as a key quantitative metric. It covers the foundational biology of vascular inflammation and the principle of TEER, explores the design and fabrication of vascularized microfluidic chips, details methodological protocols for establishing and applying these models in drug screening and disease studies, and addresses critical troubleshooting and validation strategies. By synthesizing current methodologies and applications, this guide aims to serve as a vital resource for advancing the use of these sophisticated in vitro models in preclinical research.
Vascular Inflammation and TEER: Understanding the Biological Basis and Measurement Principle
The Critical Role of the Vasculature in Inflammatory Processes
The vasculature system is not merely a passive network of tubes for blood transport; it is a dynamic, active interface that plays a critical role in the body's inflammatory processes [1]. Vascular endothelial cells provide a selective barrier between the bloodstream and surrounding tissues, regulating the movement of fluids, solutes, and immune cells [2]. During inflammation, this barrier function is deliberately modulated—initially to enable immune cell recruitment for host defense, but when dysregulated, leading to chronic inflammatory diseases and pathological tissue damage [1] [2].
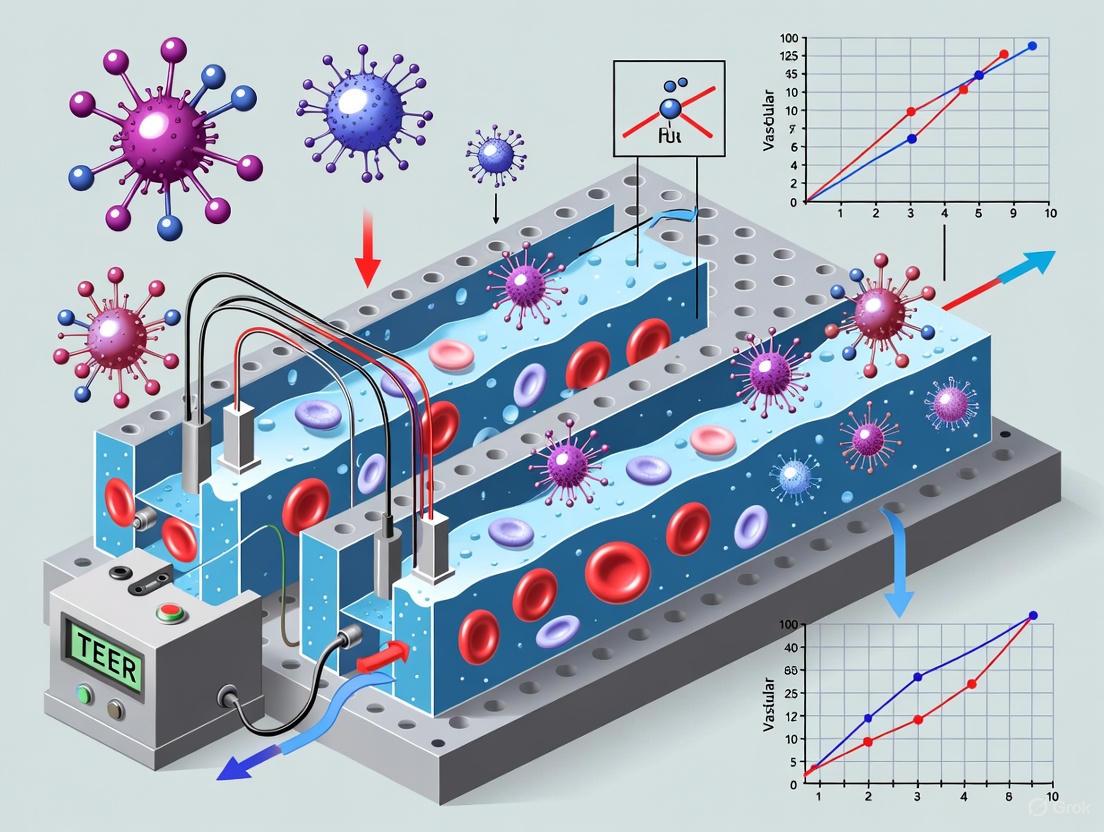
Understanding vascular inflammation requires models that accurately recapitulate the complexity of endothelial barrier function and its disruption. Recent advances in microfluidic organ-on-a-chip technology have enabled the development of sophisticated in vitro models that mimic the physiological conditions of vascular inflammation, allowing for real-time, quantitative assessment of barrier integrity through methods such as Transendothelial Electrical Resistance (TEER) measurements [1] [3]. These models are particularly valuable for drug discovery, providing scalable platforms for screening potential therapeutics targeting vascular inflammatory components [1] [4].
Pathophysiological Mechanisms of Vascular Inflammation
Endothelial Activation and Barrier Dysfunction
In inflammatory states, endothelial cells undergo activation characterized by increased expression of adhesion molecules and changes in cell-cell junctions [1] [5]. Key pro-inflammatory cytokines such as Tumor Necrosis Factor-alpha (TNF-α) and Interferon-gamma (IFN-γ) destabilize vascular endothelial (VE)-cadherin, the main component of endothelial adherens junctions, leading to increased vascular permeability [1]. Simultaneously, endothelial activation promotes increased expression of intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1), facilitating immune cell attachment and transmigration [1] [5].
The integrity of the endothelial barrier is maintained through complex interactions between tight junctions, adherens junctions, and the cytoskeleton. During inflammation, pro-inflammatory mediators trigger intracellular signaling pathways that lead to the phosphorylation of junctional proteins, their internalization, and subsequent breakdown of barrier function [1]. This process is characterized by a shift from a restrictive to a permeable endothelial phenotype, allowing for increased paracellular flux [2].
Signaling Pathways in Vascular Inflammation
The inflammatory response in vasculature involves multiple overlapping signaling pathways. The vascular endothelial growth factor (VEGF) signaling pathway plays a central role, with VEGF-A binding to VEGFR-2 promoting angiogenesis and vascular permeability [2]. Simultaneously, the Angiopoietin-Tie2 system regulates vascular stability, with Ang-2 acting as an antagonist to Tie2 signaling and promoting vascular destabilization during inflammation [2]. In lymphatic vessels, VEGF-C and VEGF-D binding to VEGFR-3 drive lymphangiogenesis, which participates in the resolution of inflammation [2].
Additional inflammatory mediators include chemokines of the CCL and CXCL families, which attract immune cells to sites of inflammation [5]. Activated vascular cells also secrete cytokines including IL-6, IL-8, and MCP-1, further amplifying the inflammatory response [5]. Pattern recognition receptors such as Toll-like receptors (TLRs) and the receptor for advanced glycation endproducts (RAGE) enhance the inflammatory response within the vasculature when activated [5].
Figure 1: Signaling Pathways in Vascular Inflammation. This diagram illustrates the key molecular events in endothelial activation and barrier dysfunction during inflammation, highlighting the roles of pro-inflammatory cytokines, junctional disruption, adhesion molecule expression, and growth factor signaling.
Quantitative Assessment of Vascular Barrier Function
Transendothelial Electrical Resistance (TEER) Principles
Transepithelial/Transendothelial Electrical Resistance (TEER) is a widely accepted quantitative technique to measure the integrity of tight junction dynamics in cell culture models of endothelial and epithelial monolayers [3]. TEER reflects the ionic conductance of the paracellular pathway in the endothelial monolayer, providing a sensitive, non-invasive method to monitor live cells during various stages of growth, differentiation, and inflammatory challenge [3]. The technique can be performed in real-time without cell damage and is based on measuring ohmic resistance or impedance across a wide spectrum of frequencies [3].
The fundamental principle of TEER measurement applies Ohm's law to cellular monolayers. In practice, an alternating current (AC) voltage signal is applied across the endothelial layer, and the resulting current is measured to calculate resistance [3]. TEER values are typically reported in Ω·cm² and are calculated by subtracting the blank resistance of the membrane support and medium from the total resistance, then multiplying by the effective surface area of the membrane [3]. This normalization allows for comparison across different experimental setups and platforms.
TEER Measurement in Microfluidic Platforms
Traditional TEER measurements have been performed using culture inserts with semipermeable membranes, but recent advances have adapted this technique for microfluidic organ-on-a-chip platforms [1] [3]. The OrganoPlate 3-lane 64 platform enables the formation of 64 perfused human umbilical vein endothelial cell (HUVEC) tubules in a standard 384-well plate format, compatible with automated TEER measurement devices [1] [4]. This system allows for continuous TEER monitoring inside an incubator for long-term permeability studies under flow conditions, more closely mimicking the physiological environment than static cultures [1].
Microfluidic TEER platforms offer significant advantages for vascular inflammation studies, including the ability to sensitively detect low barrier resistance characteristic of endothelial models, perform parallel measurements across multiple replicates, and combine TEER with other readouts such as high-content imaging and immunofluorescence [1] [4]. The platform's design incorporates extracellular matrix (ECM) gels in microfluidic channels using capillary barriers (phaseguides), creating independently accessible microfluidic channels on either side of an ECM scaffold where endothelial tubules form [1].
Table 1: Factors Affecting TEER Measurements in Vascular Models
| Factor Category | Specific Factors | Impact on TEER | Optimization Strategies |
|---|---|---|---|
| Biological Factors | Cell type and origin [6] | HUVECs typically show lower baseline resistance than epithelial cells | Select appropriate cell type for physiological context |
| Cell confluency and culture duration [6] | Incomplete monolayers significantly reduce TEER | Ensure full confluency before measurements | |
| Passage number and cell health [3] | Higher passages may exhibit barrier dysfunction | Use consistent, low-passage cells | |
| Environmental Factors | Temperature fluctuations [6] | TEER sensitive to temperature changes | Maintain 37°C during measurements |
| Medium composition and serum [3] [6] | Serum components can affect junction formation | Standardize medium formulation | |
| Contamination (mycoplasma, bacteria) [6] | Dramatically reduces barrier function | Routine contamination checks | |
| Technical Factors | Electrode design and placement [3] [6] | Affects current density distribution | Use appropriate electrodes; standardize placement |
| Measurement frequency [3] | Prevents electrode polarization | Standardize AC frequency (e.g., 12.5 Hz) | |
| Membrane properties and coatings [6] | Affects cell attachment and junction formation | Consistent membrane selection |
Application Notes: Modeling Vascular Inflammation in Microfluidic Platforms
Experimental Workflow for Vascular Inflammation Studies
The following protocol outlines the methodology for establishing and analyzing vascular inflammation models in microfluidic platforms, with integrated TEER measurements as a primary readout of barrier function [1].
Figure 2: Experimental Workflow for Vascular Inflammation-on-a-Chip. This workflow outlines the key steps in establishing, perturbing, and analyzing vascular inflammation models in microfluidic platforms with integrated TEER measurements.
Detailed Protocol: Vascular Inflammation Model with TEER Measurement
Materials and Reagents
- Microfluidic platform: OrganoPlate 3-lane 64 (Mimetas B.V.) [1]
- Cells: HUVECs (Lonza, C2519AS) at passage number 5 or lower [1]
- Culture medium: EGM-2 medium (Lonza, CC-3162) [1]
- Extracellular matrix: Rat tail collagen I (4 mg/mL) [1]
- Inflammatory cytokines: TNF-α and IFN-γ [1]
- Immune cells: Peripheral blood mononuclear cells (PBMCs) isolated from buffy coat [1]
- TEER measurement device: OrganoPlate-compatible TEER instrument [1] [4]
- Immunofluorescence reagents: Antibodies against ICAM-1 and VE-cadherin [1]
Procedure
Day 1: Platform Preparation and ECM Seeding
- Thaw and culture HUVECs in EGM-2 medium according to manufacturer's instructions [1].
- Prepare OrganoReady Blood Vessel HUVEC 3-lane 64 plates according to manufacturer's instructions [1].
- Seed rat tail collagen I (4 mg/mL) into the middle lane of the microfluidic channels using capillary action via phaseguides [1].
- Allow ECM to polymerize under appropriate conditions (37°C, 30-60 minutes).
Day 2: Endothelial Tubule Formation
- Seed HUVECs (passage 3-5) at appropriate density into the perfusion channel adjacent to the ECM gel [1].
- Place the OrganoPlate on an OrganoFlow rocker set at 14 degrees with 8-minute intervals to establish perfusion flow through the forming endothelial tubules [1].
- Culture for 2-3 days to allow formation of confluent endothelial tubules with established barrier function.
Day 4: Baseline Assessment and Inflammation Induction
- Measure baseline TEER values using the OrganoPlate-compatible TEER device [1] [4].
- Record values for all 64 tubules to establish baseline barrier integrity.
- Exclude any tubules with significantly low baseline TEER from further analysis.
- Induce inflammatory response by adding inflammatory stimuli to the perfusion medium:
Days 4-6: Continuous Monitoring and Endpoint Analysis
- Continuously monitor TEER values at regular intervals (e.g., every 4-6 hours) for up to 48 hours using the integrated TEER measurement system [1].
- Record changes in barrier function evidenced by decreasing TEER values.
- At experimental endpoint (typically 24-48 hours post-stimulation), perform additional analyses:
Data Analysis and Interpretation
TEER data should be normalized to baseline values and expressed as percentage change from baseline or as absolute TEER values (Ω·cm²) [3]. Statistical analysis should include appropriate replicates (n ≥ 3 per condition) and account for multiple comparisons when testing various inflammatory stimuli or drug treatments.
In parallel, quantitative analysis of immunofluorescence images should assess:
- ICAM-1 expression levels (intensity and distribution)
- VE-cadherin organization and junctional continuity
- Immune cell adhesion and transmigration rates
Table 2: Quantitative Responses in Vascular Inflammation Models
| Experimental Condition | TEER Response | ICAM-1 Expression | VE-Cadherin Organization | Immune Cell Migration |
|---|---|---|---|---|
| Baseline (No inflammation) | Stable high TEER (>50 Ω·cm²) [3] | Low baseline expression | Continuous junctional staining | Minimal adhesion |
| TNF-α (10 ng/mL) | ~40-60% decrease in 24h [1] | Moderate increase | Discontinuous, internalized | Increased adhesion |
| IFN-γ (50 ng/mL) | ~20-40% decrease in 24h [1] | Moderate increase | Mild disruption | Moderate adhesion |
| TNF-α + IFN-γ | ~60-80% decrease in 24h [1] | Strong increase | Severe disruption | Extensive adhesion/transmigration |
| PBMC Co-culture | ~50-70% decrease in 24h [1] | Strong increase | Severe disruption | Extensive transmigration |
Research Reagent Solutions
Table 3: Essential Research Reagents for Vascular Inflammation Studies
| Reagent Category | Specific Examples | Function in Vascular Research | Application Notes |
|---|---|---|---|
| Endothelial Cells | HUVECs (Lonza C2519AS) [1] | Primary model for human vascular endothelium | Use passages 3-5 for optimal barrier function |
| Culture Media | EGM-2 Medium (Lonza CC-3162) [1] | Supports endothelial growth and function | Contains growth factors for endothelial maintenance |
| Pro-inflammatory Cytokines | TNF-α, IFN-γ [1] | Induce endothelial activation and barrier disruption | Typical working concentrations: 10-100 ng/mL |
| Extracellular Matrix | Rat tail collagen I (4 mg/mL) [1] | Provides physiological substrate for tubule formation | Polymerization conditions critical for channel stability |
| Adhesion Molecule Antibodies | Anti-ICAM-1, Anti-VE-cadherin [1] | Detect endothelial activation and junction disruption | Essential for immunofluorescence endpoint analysis |
| Immune Cells | Peripheral Blood Mononuclear Cells (PBMCs) [1] | Model leukocyte-endothelial interactions | Isolate from buffy coat; can pre-stimulate with CD3/CD28 |
| Viability Dyes | CellTracker Orange CMRA [1] | Label immune cells for tracking | Use working concentration of 2.5 μM |
| Flow Markers | Fluorescent dextrans [1] | Alternative permeability assessment | Complementary to TEER measurements |
Troubleshooting and Technical Considerations
Common Challenges in Vascular Inflammation Models
Low Baseline TEER Values
- Ensure HUVECs are at appropriate passage (3-5) and have reached full confluency [6].
- Verify proper ECM polymerization and endothelial tubule formation through microscopy.
- Check for microbial contamination that may compromise barrier function [6].
Inconsistent TEER Measurements
- Standardize electrode placement and measurement conditions across experiments [3] [6].
- Maintain consistent temperature during measurements, as TEER is temperature-sensitive [6].
- Ensure proper perfusion flow rates and avoid bubble formation in microfluidic channels [1].
Variable Inflammatory Responses
- Quality control cytokine stocks to ensure consistent biological activity.
- Standardize PBMC isolation procedures to minimize donor-to-donor variability.
- Include appropriate positive and negative controls in each experiment.
Advanced Applications and Model Extensions
The basic vascular inflammation model can be extended to study more complex physiological scenarios:
- Co-culture models: Incorporate pericytes or smooth muscle cells to study vascular maturation and stability [2].
- Disease-specific models: Use endothelial cells from patients with specific inflammatory conditions.
- Drug screening applications: Test anti-inflammatory compounds or barrier-stabilizing drugs [1] [4].
- Multi-organ platforms: Connect vascular inflammation chips with other organ models to study systemic effects.
These advanced applications leverage the core principles and protocols outlined above while incorporating additional cellular complexity or experimental endpoints to address specific research questions in vascular inflammation.
Endothelial Dysfunction and Barrier Integrity in Inflammation
The vascular endothelium, a single layer of cells lining the blood vessels, serves as a critical selective barrier between the circulation and surrounding tissues. Endothelial dysfunction is a pivotal event in the initiation and progression of inflammatory diseases, characterized by compromised barrier integrity, enhanced leukocyte adhesion, and aberrant signaling [7] [8]. Inflammatory conditions disrupt the delicate balance of endothelial cell function, leading to increased permeability and the pathological transmigration of immune cells. Understanding these mechanisms is essential for developing novel therapeutic strategies for cardiovascular diseases, inflammatory bowel disease, and other conditions where vascular inflammation plays a central role [7] [8].
The emergence of advanced microfluidic platform models has revolutionized the study of vascular inflammation by providing more physiologically relevant human in vitro systems. These platforms, particularly those enabling real-time, high-throughput measurement of Trans-Endothelial Electrical Resistance (TEER), allow for the precise quantification of endothelial barrier function under controlled inflammatory stimuli [1] [9]. This application note details the integration of these platforms and associated protocols to model endothelial dysfunction, providing researchers with a robust framework for investigating the molecular pathways underlying vascular barrier disruption.
Key Quantitative Findings in Vascular Inflammation Models
Research utilizing microfluidic models has yielded critical quantitative data on endothelial barrier responses. The following tables summarize key findings regarding the impact of inflammatory cytokines on barrier integrity and the expression of associated adhesion molecules.
Table 1: Impact of Inflammatory Cytokines on Endothelial Barrier Integrity (TEER) in Microfluidic Models
| Cytokine Stimulus | Concentration Range | Exposure Time | Effect on TEER | Reported Significance | Source Model |
|---|---|---|---|---|---|
| TNFα | 10–100 ng/mL | 24–48 hours | Significant Decrease | Dose-dependent reduction in barrier function [10] | 3D HUVEC tubules in OrganoPlate [1] |
| IFN-γ | 10–100 ng/mL | 24–48 hours | Significant Decrease | Dose-dependent reduction; synergistic effect with TNFα [1] | 3D HUVEC tubules in OrganoPlate [1] |
| TNFα + IFN-γ | 10–100 ng/mL each | 24–48 hours | Largest Decrease | Synergistic, dose-dependent effect on barrier disruption [1] | 3D HUVEC tubules in OrganoPlate [1] |
Table 2: Inflammatory Marker Expression in 3D Microvessel Models Following TNFα Stimulation
| Parameter Measured | Baseline Expression | Post-TNFα Stimulation | Effect of NFκB Inhibition (BAY 11-7082) | Reference |
|---|---|---|---|---|
| Monocyte Adhesion | Low | Marked Induction | Significantly abrogated | [10] |
| VCAM-1 Expression | Low | Marked Induction | Significantly abrogated | [10] |
| IL-6 Production | Low | Marked Induction | Significantly abrogated | [10] |
| VE-Cadherin Localization | Intact junctions | Disruption | Partial restoration of junction integrity | [10] |
Experimental Protocols for Modeling Inflammation and Assessing Barrier Function
Protocol A: Establishing and Perturbing a 3D Vascular Barrier Model
This protocol outlines the steps for culturing endothelial cells in a microfluidic device and inducing inflammation using cytokines or immune cells [1].
Key Research Reagent Solutions:
- OrganoPlate 3-lane 64: A microfluidic platform with 64 independent perfusion circuits in a standard 384-well plate format, enabling high-throughput 3D cell culture [1].
- Human Umbilical Vein Endothelial Cells (HUVECs): A standard model for studying vascular endothelium. Can be substituted with organ-specific cells like Human Brain Microvascular Endothelial Cells (HBMECs) [1] [11].
- EGM-2MV Medium: A specialized growth medium optimized for microvascular endothelial cells, containing supplements like VEGF, FGF, and EGF [11].
- Rat Tail Collagen-I (4 mg/mL): A common extracellular matrix (ECM) hydrogel used to provide a physiological 3D scaffold for endothelial tubule formation [1].
- Recombinant Human TNFα and IFN-γ: Pro-inflammatory cytokines used to experimentally induce endothelial activation and barrier dysfunction [1] [10].
- Peripheral Blood Mononuclear Cells (PBMCs): A mixed population of human immune cells (lymphocytes, monocytes) used to study leukocyte-endothelium interactions [1].
Procedure:
- Device Preparation: Use a ready-to-use OrganoReady Blood Vessel HUVEC plate or seed the middle channel of an OrganoPlate 3-lane 64 with rat tail collagen-I (4 mg/mL) and allow it to polymerize [1].
- Cell Seeding: Seed HUVECs (passage 4-6) into the appropriate perfusion channel to form a confluent endothelial tubule against the collagen matrix. HUVECs are cultured in EGM-2 medium [1].
- Maintenance of Perfusion: Place the plate on an OrganoFlow rocker set at a 14-degree tilt with 8-minute intervals to establish perfusion flow through the endothelial tubule. Change the medium daily [1].
- Inflammatory Stimulation:
- Cytokine Treatment: After 2-3 days of culture, introduce TNFα (10-100 ng/mL) and/or IFN-γ (10-100 ng/mL) into the perfusion medium. The treatment typically lasts 24-48 hours [1] [10].
- Immune Cell Adhesion/Migration: Isolate PBMCs from human blood. For T-cell studies, stimulate PBMCs with CD3/CD28 activator beads for 48 hours. Label PBMCs with a fluorescent cell tracker (e.g., CellTracker Orange CMRA, 2.5 µM) and perfuse them through the endothelial tubule at a concentration of 400,000 cells/mL [1].
- Barrier Integrity Monitoring: Continuously monitor barrier function throughout the experiment using the integrated TEER measurement system [1].
Protocol B: Real-Time TEER Measurement for Barrier Integrity
This protocol describes the specific methodology for performing continuous TEER measurements in the OrganoPlate platform to quantify barrier function [1] [9].
Procedure:
- TEER Instrument Setup: Use the OrganoTEER measurement apparatus designed for the OrganoPlate 3-lane 64. The device should be placed inside a humidified incubator at 37°C and 5% CO2 for long-term studies [1].
- Baseline Measurement: Record TEER values from all 64 tubules after the endothelial cell layer has reached confluence (typically after 2-3 days of culture) but before applying any inflammatory stimuli. This serves as the internal control (100% integrity) [1].
- Continuous Monitoring: The OrganoTEER system allows for parallel and continuous measurements of all 64 tubules under perfused conditions. Data acquisition software records TEER values at set intervals over the course of the experiment (e.g., 24-72 hours) [1] [9].
- Data Analysis: A decrease in TEER value correlates directly with a reduction in endothelial barrier integrity. Normalize data as a percentage of the baseline measurement. The high sensitivity of the system allows for the detection of even low barrier resistance values characteristic of endothelial models [1].
Protocol C: Multiplexed Endpoint Analyses
Following functional assessments, the same microvessels can be fixed and stained for phenotypic and molecular analysis [1] [11].
Procedure:
- Fixation: Gently perfuse the tubules with a 4% paraformaldehyde solution for 15-20 minutes at room temperature.
- Permeabilization and Blocking: Perfuse with a buffer containing a permeabilizing agent (e.g., 0.1% Triton X-100) and a blocking protein (e.g., 1-5% Bovine Serum Albumin) for 1 hour.
- Immunofluorescence Staining:
- Primary Antibodies: Perfuse antibodies against target proteins. Key targets include:
- VE-Cadherin: To visualize adherens junctions and assess their continuity and morphology [1] [10].
- ICAM-1/VCAM-1: To quantify endothelial activation in response to inflammatory stimuli [1] [10].
- F-actin: Stained with phalloidin to observe cytoskeletal rearrangements, such as stress fiber formation, which occur during barrier disruption [10].
- Secondary Antibodies: After washing, perfuse fluorophore-conjugated secondary antibodies.
- Primary Antibodies: Perfuse antibodies against target proteins. Key targets include:
- Imaging and Analysis: Image the stained tubules using high-content confocal or fluorescence microscopy. Analyze images for changes in junctional morphology, protein expression levels, and co-localization [1].
Signaling Pathways in Endothelial Dysfunction
A key pathway mediating inflammatory responses in the endothelium is the NFκB pathway, activated by cytokines like TNFα.
Diagram 1: TNFα-NFκB Signaling in Endothelial Dysfunction. This pathway shows how TNFα binding triggers NFκB activation, leading to the expression of pro-inflammatory mediators and disruption of endothelial barrier integrity, a process that can be inhibited by BAY 11-7082 [10].
In addition to NFκB signaling, metabolic reprogramming of endothelial cells towards aerobic glycolysis (the Warburg effect) and the induction of oxidative stress are critical mechanisms that disrupt barrier integrity by impairing junctional stability and nitric oxide bioavailability [7] [8].
Integrated Experimental Workflow
A comprehensive study of endothelial dysfunction involves a multi-step process, from model establishment to data analysis.
Diagram 2: Integrated Workflow for Vascular Inflammation Studies. This flowchart outlines the sequential steps for modeling and analyzing endothelial dysfunction in a microfluidic platform, combining functional TEER measurements with molecular endpoint analyses [1] [11] [10].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Vascular Inflammation-on-a-Chip Models
| Item Category | Specific Product/Model | Critical Function in the Protocol |
|---|---|---|
| Microfluidic Platform | OrganoPlate 3-lane 64 | Provides a scalable, high-throughput platform with 64 independent, perfusable microfluidic circuits for 3D cell culture [1]. |
| Endothelial Cells | Primary HUVECs (Lonza, C2519AS) | Standard human endothelial cells for forming the vascular tubule. HBMECs are used for brain-specific models [1] [11]. |
| Cell Culture Medium | EGM-2 BulletKit (Lonza, CC-3162) / EGM-2MV | Optimized medium with growth factors (VEGF, FGF) for the maintenance and proliferation of microvascular endothelial cells [1] [11]. |
| Extracellular Matrix | Rat Tail Collagen-I (4 mg/mL) | Forms the 3D hydrogel scaffold that supports the structure of the endothelial tubule and provides a physiological microenvironment [1]. |
| Inflammatory Cytokines | Recombinant Human TNFα & IFN-γ | Key stimuli to experimentally induce endothelial activation, disrupt junctions, and create an pro-inflammatory state [1] [10]. |
| NFκB Pathway Inhibitor | BAY 11-7082 | A pharmacological inhibitor used to validate the specific role of the NFκB signaling pathway in the inflammatory response [10]. |
| Immunostaining Antibodies | Anti-VE-Cadherin, Anti-ICAM-1, Phalloidin (F-actin) | Essential reagents for endpoint immunofluorescence analysis of junctional integrity, endothelial activation, and cytoskeletal remodeling [1] [10]. |
| TEER Measurement Device | OrganoTEER for OrganoPlate 3-lane 64 | Enables sensitive, real-time, and label-free quantification of endothelial barrier integrity across all 64 chips in the platform [1] [9]. |
| Psma-alb-56 | Psma-alb-56, MF:C66H95N11O18, MW:1330.5 g/mol | Chemical Reagent |
| m-PEG12-Hydrazide | m-PEG12-Hydrazide, MF:C26H54N2O13, MW:602.7 g/mol | Chemical Reagent |
The Principle and Significance of TEER
Transepithelial/Transendothelial Electrical Resistance (TEER) is a quantitative, non-invasive technique used to measure the integrity and function of cellular barriers formed by epithelial and endothelial cell monolayers in vitro [12] [3]. These barriers are critical for controlling the movement of ions, nutrients, and other molecules throughout the body, and their dysfunction is implicated in numerous disease states [13].
The measurement is based on a fundamental electrophysiological principle: the tight junctions between adjacent cells form a paracellular pathway that restricts the passive flow of ions. When these junctions are intact, they create a high-resistance electrical barrier. TEER directly measures this electrical resistance, providing a functional readout of barrier health [12] [14].
- High TEER values indicate well-formed tight junctions and a intact, low-permeability cellular barrier [12].
- Low TEER values suggest compromised barrier function, where ions and molecules can pass more freely through "leaky" junctions, often modeling pathological conditions or cytotoxic effects [12] [15].
TEER's primary advantage lies in its ability to provide real-time, quantitative data without damaging the cells, allowing researchers to monitor the same culture throughout an experiment—from barrier formation and maturation to the application of experimental treatments [12] [13].
Core Measurement Methodologies
Ohm's Law-Based Measurement
The most common method for determining TEER uses Ohm's law (V=IR). In this setup, two electrodes are placed on either side of a cellular monolayer grown on a semi-permeable filter insert [3] [14]. A small, alternating current (AC) is applied across the cell layer, and the resulting voltage drop is measured. The resistance (R) is calculated from the current (I) and voltage (V) [12] [13].
The final TEER value is normalized to the surface area of the membrane to allow for comparisons across different experimental setups, using the formula:
TEER (Ω·cm²) = (RTOTAL - RBLANK) × Membrane Area (cm²) [3]
Where:
- RTOTAL is the resistance measured across the cell monolayer and the supporting membrane.
- RBLANK is the resistance of the supporting membrane and culture medium alone (without cells). Subtracting this background resistance yields the cell-specific resistance [3] [14].
Commercial systems like the EVOM series (World Precision Instruments) typically use a low-frequency AC square wave (e.g., 12.5 Hz) to avoid electrode polarization and cell damage that can be caused by direct current [3].
Electrochemical Impedance Spectroscopy (EIS)
A more advanced technique, Electrochemical Impedance Spectroscopy (EIS), measures the complex impedance of a cell layer across a wide spectrum of frequencies [16] [14]. Unlike single-frequency measurements, EIS can distinguish between the resistive and capacitive properties of the tissue.
- Advantages: EIS does not require a separate background subtraction step, as it can mathematically isolate the solution resistance (Rsol) from the tissue's properties. It also provides additional parameters like transepithelial capacitance (TEC), which can offer insights into cell membrane surface area and other biological properties [16].
- Data Fitting: The impedance data is fit to an equivalent electrical circuit model (e.g., a resistor-capacitor (RC) circuit), which more accurately represents the biological system and yields more robust TEER values [16]. Single-frequency measurements can underestimate true TEER because they do not account for capacitive reactance [16].
Experimental Workflow
The following diagram illustrates the generalized workflow for planning and executing a TEER experiment, from initial setup to data interpretation.
TEER in Vascular Inflammation and Microfluidic Platforms
The application of TEER is particularly powerful in the context of vascular inflammation research using advanced microfluidic "organ-on-a-chip" models. These devices aim to recapitulate the physiological and pathological conditions of human barriers more accurately than traditional static cultures [3] [14].
In vascular models, the endothelium forms a critical barrier between the blood and surrounding tissues. During inflammation, pro-inflammatory cytokines (e.g., TNF-α, IL-1β) disrupt endothelial tight junctions, leading to increased vascular permeability. TEER provides a sensitive, quantitative means to monitor this barrier breakdown in real-time and to evaluate the efficacy of potential therapeutic compounds [13].
However, integrating TEER into microfluidic devices presents unique challenges and considerations:
- Electrode Integration: Miniaturized electrodes must be precisely placed in the microfluidic channels on either side of the cell layer [14].
- Current Distribution: The geometry of microfluidic channels can lead to non-uniform current distribution, potentially causing overestimation of TEER. This can be mitigated by designing electrodes with a large surface area relative to the cell culture area [3] [14].
- Four-Point Probe Method: A four-point probe method, which uses separate pairs of electrodes for current application and voltage sensing, is often preferred in microsystems. This configuration eliminates the contribution of contact and lead resistances, leading to more accurate measurements [14].
- On-Chip Subtraction: Some sophisticated designs incorporate multiple electrodes to perform resistance subtraction directly on the device, removing the variability associated with using separate "blank" chips [14].
Applications in Drug Discovery and Toxicity Testing
TEER measurement is an indispensable tool in pharmaceutical research, applied across multiple stages of drug development.
- Barrier Integrity QC: TEER confirms that in vitro barrier models (e.g., blood-brain barrier, intestinal epithelium) have matured and formed functional tight junctions before they are used in drug transport studies [3] [13].
- Permeability Screening: It serves as a primary screen for a compound's ability to cross biological barriers. A drug that causes a drop in TEER may be disrupting the barrier, while a compound that increases TEER could have a protective or barrier-strengthening effect [13] [15].
- Toxicity Assessment: A decrease in TEER following drug exposure is a clear indicator of cytotoxicity or barrier compromise, providing a rapid and sensitive method for safety screening [13].
- Disease Modeling: TEER is used to create in vitro models of diseases characterized by impaired barrier function, such as inflammatory bowel disease, asthma, and multiple sclerosis, enabling the study of disease mechanisms and the testing of new treatments [13].
Representative TEER Values for Various Barrier Tissues
The table below lists typical TEER values for different cell types as reported in scientific literature, providing a reference for researchers assessing their in vitro models.
| Cell Type / Tissue Model | Representative TEER Value (Ω·cm²) | Significance and Context |
|---|---|---|
| Blood-Brain Barrier (BBB) Endothelium (in vitro) | 500 - 600+ [17] [16] | High resistance is critical for protecting the brain; models aim to achieve high values to be physiologically relevant. |
| Retinal Pigment Epithelium (RPE) | ~500 - 600 [17] | Considered mature and functionally intact at this range. |
| Intestinal Epithelium (e.g., Caco-2) | Varies widely | Model-dependent; used for predicting oral drug absorption. |
| Bronchiolar Epithelium (16HBE) | 955 - 1034 [16] | Represents a tight barrier in the pulmonary system. |
| Generic "Healthy" Barrier | High | Indicates well-formed tight junctions and intact monolayer [12]. |
| Generic "Compromised" Barrier | Low | Suggests leaky junctions due to toxicity, disease, or inflammation [12]. |
Detailed Experimental Protocol: Measuring TEER with a Voltohmmeter
This protocol details the standard method for measuring TEER in Transwell-style cultures using a manual voltohmmeter and "chopstick" electrodes.
Materials and Reagents
Table: Essential Materials for TEER Measurement
| Item | Function | Notes |
|---|---|---|
| TEER Voltohmmeter (e.g., EVOM2) | Instrument that applies AC and measures voltage/current. | Uses a low-frequency AC signal (e.g., 12.5 Hz) to prevent cell damage and electrode polarization [3]. |
| Ag/AgCl "Chopstick" Electrodes (e.g., STX2) | Paired electrodes for current application and voltage sensing. | Silver/Silver Chloride electrodes are standard for stable potential [3] [14]. Handle carefully to avoid distortion. |
| Cell Culture Inserts | Permeable support for growing cell monolayers. | Various sizes (e.g., 6, 12, 24-well format). Material (e.g., polycarbonate, polyester) may vary. |
| Cell Culture Medium | Maintains cell viability during measurement. | Should be equilibrated to experimental temperature and CO2 levels. |
Step-by-Step Procedure
System Calibration and Blank Measurement:
- Calibrate the TEER meter according to the manufacturer's instructions.
- Measure the resistance of a cell-free insert containing culture medium only. This is your RBLANK value. Record this value for every experiment and for each batch of inserts used [3].
Sample Preparation:
- Carefully transfer the cell culture inserts from the incubator to a sterile environment.
- Allow the medium and cells to acclimate to ambient temperature for approximately 15 minutes to minimize the impact of temperature fluctuations on the reading [13].
- Aspirate the old medium and replace it with a fresh, pre-warmed medium of the same composition in both the apical and basolateral compartments.
Resistance Measurement:
- Sterilize the electrodes with 70% ethanol and rinse thoroughly with sterile water or PBS. Caution: Avoid letting ethanol contact the electrode pellets.
- Place the longer (apical) electrode into the insert and the shorter (basolateral) electrode into the outer well. Ensure the electrodes do not touch the membrane to avoid damaging the monolayer or scratching the electrodes [3].
- Record the resistance value displayed on the meter. This is your RTOTAL value.
Data Calculation:
- Calculate the cell-specific resistance: RCELLS = RTOTAL - RBLANK
- Calculate the final TEER value: TEER (Ω·cm²) = RCELLS (Ω) × Membrane Area (cm²) [3].
Post-Measurement Handling:
- Return the culture inserts to the incubator if the experiment is to continue. TEER can be measured repeatedly over time to track barrier development or the temporal effects of a treatment [12].
Critical Factors for Success and Data Interpretation
- Consistency is Key: Maintain consistent environmental conditions (temperature, pH, CO2) and electrode placement between measurements to ensure reproducibility [13].
- Electrode Handling: Disturbing the electrode position during measurement is a major source of error. Use a stable stand if available [3].
- Understanding Limitations: TEER measures ionic conductance primarily through the paracellular pathway. It does not provide direct information on the structure or protein composition of tight junctions. For mechanistic insights, TEER should be complemented with other assays, such as tracer flux studies or immunostaining for tight junction proteins [13].
Advanced Technique: Impedance Spectroscopy Protocol
For researchers requiring more detailed electrical characterization of their barrier models, the following protocol outlines the use of Electrochemical Impedance Spectroscopy (EIS).
Procedure and Data Analysis
- Apparatus Setup: Use an instrument capable of galvanostatic sinusoidal signal processing (e.g., 4 μA amplitude) and frequency sweeps (e.g., 2 Hz to 50 kHz) [16].
- Measurement: Perform an impedance sweep on the cell monolayer grown on a transwell insert placed in a compatible electrophysiology chamber.
- Data Fitting: Fit the resulting complex impedance data to an appropriate electrical circuit model (e.g., the RCRC model from Figure 1D in the search results) using specialized software (e.g., MATLAB) [16]. This fit will output parameters including:
- TER (TEER): A more accurate calculation of transepithelial resistance.
- TEC: Transepithelial capacitance, which can report on cell membrane properties.
- Membrane Ratio (α): A ratio of electrical time constants for the tissue [16].
- Error Quantification: A good fit to the model should have a low mean absolute error (e.g., < 10 Ω) [16].
The relationship between the biological structure and the electrical model used in EIS is illustrated below.
TEER remains the gold standard technique for the functional assessment of in vitro barrier models due to its quantitative, non-invasive, and real-time nature. Its application is vital for validating the integrity of microfluidic vascular models before they are used in inflammation studies, drug permeability screening, or toxicity testing. By following standardized protocols and understanding the critical factors that influence the measurement, researchers can reliably use TEER to generate robust, reproducible data that advances our understanding of barrier function in health and disease.
Transepithelial/transendothelial electrical resistance (TEER) is a gold-standard, quantitative technique used to measure the integrity and permeability of cellular monolayers in vitro [3]. This non-invasive method is paramount for assessing the functionality of biological barriers—such as the blood-brain barrier, intestinal epithelium, and vascular endothelium—by reporting on the tightness of the tight junctions between adjacent cells [18] [19]. In the specific context of microfluidic platform modeling of vascular inflammation, TEER provides a real-time, sensitive readout of endothelial barrier integrity, which is crucial for studying disease mechanisms and screening potential therapeutics [20] [9].
The core electrical principle of TEER is founded on measuring the resistance to the flow of ions across a cellular monolayer. Tight junctions form a seal that controls the paracellular pathway, the route between cells. When these junctions are intact and functional, they restrict the passive flow of ions, resulting in a high electrical resistance. Conversely, compromised barrier function, a hallmark of vascular inflammation, leads to increased ion permeability and a measurable drop in electrical resistance [3] [19]. TEER, therefore, serves as a direct proxy for the dynamic state of tight junctions and the overall health of the cellular barrier.
Electrical Principles and Paracellular Pathway Dynamics
Fundamental Theory of TEER Measurement
The measurement of TEER is a direct application of Ohm's law (V = IR), where the electrical resistance (R) is calculated from a known applied alternating current (AC) and the resulting voltage drop across the cell layer [3]. The use of AC voltage is critical to avoid damaging the cells and electrodes, which can occur with direct current (DC) [3]. The total measured resistance ((R{TOTAL})) across a porous membrane and the cell monolayer is a composite value. To isolate the component specific to the cell layer ((R{TISSUE})), the resistance of a blank membrane ((R_{BLANK})) is measured and subtracted [3]:
[R{TISSUE}(Ω)=R{TOTAL}−R_{BLANK}]
This cell-specific resistance is inversely proportional to the effective membrane area. To enable comparisons across different experimental setups, the TEER value is normalized to the surface area and reported in the standardized units of Ω·cm² [3]:
[TEER{REPORTED} = R{TISSUE}(Ω) \times M_{AREA}(cm^2)]
TEER as a Measure of Paracellular Permeability
The paracellular pathway is the primary route for ion flow measured by TEER. This pathway is gated by tight junctions, multiprotein complexes that form a selective seal between endothelial or epithelial cells [21]. The transmembrane proteins claudins and occludin are the primary architects of these junctional strands, creating a barrier that dictates the selective permeability of ions and small molecules [21]. The integrity of this protein network is dynamically regulated and can be disrupted by inflammatory mediators.
- High TEER Values: Indicate well-formed, functional tight junctions that effectively restrict ion movement through the paracellular space, reflecting a tight, selective barrier [18] [19].
- Low TEER Values: Signal a leaky or compromised barrier, often due to the disassembly or internalization of tight junction proteins, leading to increased paracellular permeability [20] [18].
It is important to distinguish that TEER specifically reflects the ionic conductance of the paracellular pathway. This is different from the permeability to non-electrolyte tracer molecules (e.g., dextrans), which indicates paracellular water flow and effective pore size [3]. This makes TEER an exceptionally sensitive tool for detecting subtle, real-time changes in barrier function that may not be immediately apparent with tracer-based methods.
TEER in Vascular Inflammation Modeling
Tight Junction Dynamics in Endothelial Dysfunction
In vascular inflammation, pro-inflammatory cytokines such as Tumor Necrosis Factor-alpha (TNFα) and Interferon-gamma (IFN-γ) directly target endothelial tight junctions, leading to barrier disruption [20]. These cytokines trigger intracellular signaling pathways that result in the phosphorylation and internalization of key junctional proteins, most notably VE-Cadherin, which is the main component of endothelial adherens junctions and is essential for barrier regulation [20]. The destabilization of VE-Cadherin and associated tight junction proteins like Zonula Occludens-1 (ZO-1) increases paracellular permeability, an effect that is robustly quantified by a decrease in TEER.
Concurrently, endothelial activation occurs, characterized by the increased surface expression of adhesion proteins like ICAM-1 [20]. This facilitates the adhesion and transendothelial migration of immune cells, such as peripheral blood mononuclear cells (PBMCs), which can further exacerbate barrier disruption. The relationship between immune cell migration and vascular leakage is complex and not fully understood, highlighting the need for sophisticated in vitro models that can concurrently monitor TEER and immune cell behavior [20].
Quantifying Inflammatory Disruption with TEER
Advanced organ-on-a-chip platforms, such as the OrganoPlate, have been developed to model vascular inflammation and integrate continuous, high-throughput TEER measurements [20] [9]. These models demonstrate the precise utility of TEER in capturing barrier dynamics. The following table summarizes typical TEER responses to inflammatory stimuli in such a system:
Table 1: TEER Response to Inflammatory Stimuli in a Vascular Inflammation-on-a-Chip Model [20] [9]
| Inflammatory Stimulus | Observed Effect on TEER | Correlated Biological Events |
|---|---|---|
| TNFα & IFN-γ (Cytokines) | Significant, dose-dependent decrease in TEER values over 24-48 hours. | Destabilization of VE-Cadherin, increased ICAM-1 expression, changes in endothelial cell morphology. |
| Activated PBMCs | Decrease in TEER values. | Immune cell adhesion to endothelium via ICAM-1, followed by transendothelial migration. |
| Control (No Stimulus) | Stable, high TEER values. | Intact VE-Cadherin localization, low ICAM-1 expression, confluent endothelial monolayer. |
This data confirms that TEER is a highly sensitive and reliable metric for quantifying the impact of both biochemical (cytokines) and cellular (immune cells) inflammatory triggers on endothelial barrier function.
Experimental Protocols & Methodologies
Protocol: Measuring TEER in a Microfluidic Vascular Model
This protocol details the steps for culturing endothelial tubules in an OrganoPlate 3-lane 64 and performing real-time TEER measurements to assess barrier integrity under inflammatory conditions [20].
Research Reagent Solutions Table 2: Essential Materials for Vascular Inflammation TEER Assay [20]
| Item | Function/Description | Example |
|---|---|---|
| OrganoPlate 3-lane 64 | A microfluidic 384-well plate format with 64 independent chips, each with three channels, enabling high-throughput perfusion culture. | Mimetas |
| Human Umbilical Vein Endothelial Cells (HUVECs) | Primary endothelial cells used to form the vascular tubules. | Lonza, C2519AS |
| EGM-2 Medium | Specialized growth medium for HUVEC culture and maintenance. | Lonza, CC-3162 |
| Extracellular Matrix (ECM) Gel | A hydrogel scaffold (e.g., collagen) injected into the middle channel against which endothelial tubules form. | Corning Matrigel |
| Inflammatory Cytokines | Used to induce endothelial activation and barrier disruption. | Recombinant Human TNFα & IFN-γ |
| Peripheral Blood Mononuclear Cells (PBMCs) | Human immune cells used to model immune-endothelial interactions. | Isolated from buffy coat |
| OrganoTEER Instrument | Automated device for performing parallel TEER measurements across all 64 chips in the OrganoPlate. | Mimetas |
Procedure:
- Plate Preparation and ECM Seeding: Place the OrganoPlate on a cooled (4°C) surface. Using an automated liquid handler or pipette, inject an ECM gel into the middle lane of each microfluidic chip. Incubate the plate at 37°C for at least 30 minutes to allow the gel to polymerize.
- Endothelial Tubule Formation: Seed a suspension of HUVECs (e.g., 5x10^6 cells/mL) into the two perfusion channels adjacent to the gel lane. Place the plate on a perfusion rocker in a 37°C, 5% CO₂ incubator. The rocking motion creates alternating flow, promoting cell attachment and the formation of a confluent endothelial tubule against the ECM gel.
- Barrier Maturation & Baseline TEER: Culture the cells for 2-3 days until a confluent monolayer is formed. Place the OrganoPlate into the OrganoTEER measurement system inside the incubator to initiate continuous, real-time TEER monitoring. Record stable, high baseline TEER values to confirm barrier integrity before experimentation.
- Inflammatory Stimulation: Introduce inflammatory stimuli into the perfusion medium flowing through the lumen of the endothelial tubules.
- For cytokine treatment: Add TNFα and/or IFN-γ at desired concentrations (e.g., 10-100 ng/mL each) to the culture medium.
- For immune cell migration: Label PBMCs with a fluorescent cell tracker (e.g., CellTracker Orange). Resuspend the labeled PBMCs in medium and introduce them into the endothelial tubules.
- Real-Time TEER Monitoring: Continue perfusion culture and record TEER values at regular intervals (e.g., every hour) using the OrganoTEER instrument. A successful inflammatory response is indicated by a significant and sustained decrease in TEER values over 24-48 hours.
- Endpoint Analysis: Following TEER measurements, the model can be fixed and stained for immunofluorescence analysis. Key targets include:
- VE-Cadherin: Visualize junctional integrity and morphology.
- ICAM-1: Confirm endothelial activation.
- Actin Cytoskeleton: Assess cell shape changes.
Protocol: Data Analysis and TEER Normalization
TEER Calculation:
- The instrument typically measures the total impedance ((R_{TOTAL})).
- A baseline resistance value from a cell-free chip ((R{BLANK})) must be predetermined and subtracted to calculate the tissue-specific resistance: (R{TISSUE} = R{TOTAL} - R{BLANK}).
- The TEER value in Ω·cm² is then calculated by multiplying (R_{TISSUE}) by the effective surface area of the endothelial tubule in the microfluidic channel [20] [3].
Interpretation:
- Normalize TEER data from treatment groups to the average of control groups at each time point to account for plate-wide drift and facilitate comparison across experiments.
- Correlate the kinetic TEER data with endpoint immunofluorescence findings. A drop in TEER should correlate with disrupted VE-Cadherin staining, increased ICAM-1 signal, and altered cell morphology.
Visualization of Signaling Pathways and Workflows
Signaling Pathway in Vascular Inflammation
The following diagram illustrates the key signaling pathways involved in inflammatory disruption of endothelial tight junctions, leading to a decrease in TEER.
Diagram 1: Inflammatory disruption of endothelial barrier.
Experimental Workflow for TEER Assay
This workflow outlines the key steps in performing a vascular inflammation assay with integrated TEER measurement.
Diagram 2: TEER assay workflow.
Why Microfluidics? Advantages Over Traditional 2D and Animal Models
Microfluidic technology has emerged as a transformative tool for modeling vascular inflammation, offering significant advantages over conventional 2D cell culture and animal models. These platforms enable the replication of physiological microenvironments with precise control over biochemical and mechanical cues, providing researchers with more human-relevant data for drug development [22]. By mimicking the 3D architecture and hemodynamic forces of human vasculature, microfluidic systems bridge the critical gap between oversimplified traditional in vitro models and species-divergent in vivo studies [23].
The integration of real-time monitoring capabilities such as Trans-Endothelial Electrical Resistance (TEER) measurements further enhances the value of these platforms for assessing vascular barrier function during inflammatory processes [20] [24]. This combination of physiological relevance and advanced readout technologies makes microfluidics particularly valuable for studying complex processes like immune cell migration and endothelial dysfunction in vascular inflammation research.
Quantitative Advantages of Microfluidic Platforms
Table 1: Performance Comparison of Vascular Inflammation Models
| Parameter | Traditional 2D Models | Animal Models | Microfluidic Systems |
|---|---|---|---|
| Analysis Time | Days [25] | Weeks to months [23] | <90 minutes to days [25] [26] |
| Sample Volume | mL range | Not applicable | Microliter range [25] |
| Throughput | Low to moderate | Low | High (40-96 parallel chips) [26] [27] [20] |
| TEER Measurement Sensitivity | Limited by electrode design | Not directly measurable | High (detects early toxicity) [27] |
| Shear Stress Control | Limited or absent | Physiological but not controllable | Precise control (0.01-0.70 dyn/cm²) [27] |
| Species Relevance | Human cells but simplified | Species differences | Human cells in physiological context [22] |
Table 2: Key Functional Advantages of Microfluidic Vascular Models
| Feature | Advantage | Research Impact |
|---|---|---|
| Unidirectional Flow | Mimics physiological blood flow [26] | Promotes endothelial cell alignment; enables study of flow-dependent inflammation |
| Integrated TEER | Real-time, non-invasive barrier monitoring [20] [24] | Detects subtle changes in vascular permeability before cell death occurs [27] |
| Co-culture Capability | Endothelial, smooth muscle, and immune cells [26] [27] | Recapitulates cellular crosstalk in vascular inflammation |
| Inflammatory Response Modeling | Cytokine exposure and immune cell migration [20] | Enables study of TNFα/IFN-γ induced barrier dysfunction and leukocyte transmigration |
| High-Content Imaging | Optical clarity and accessibility [20] | Facilitates morphological analysis and immunofluorescence alongside functional TEER data |
Experimental Protocols
Protocol: Establishing a Vascular Inflammation Model in the OrganoPlate Platform
Purpose: To create a microfluidic model of vascular inflammation for TEER-based assessment of endothelial barrier function.
Materials:
- OrganoPlate 2-lane-48 UF or 3-lane-64 (Mimetas) [26] [20]
- Human Umbilical Vein Endothelial Cells (HUVECs) or Human Coronary Artery Endothelial Cells (HCAECs) [26] [20]
- EGM-2 culture medium [20]
- Fibrin or Collagen I gel matrix
- Inflammatory cytokines: TNFα and IL-1β or IFN-γ [26] [20]
- Peripheral Blood Mononuclear Cells (PBMCs) - optional [20]
- OrganoTEER measurement system [20]
Procedure:
Day 1: Device Preparation and Cell Seeding
- ECM Gel Loading:
- Prepare fibrinogen solution (10 mg/mL) in EGM-2 medium.
- Mix with thrombin solution (2 U/mL) at 9:1 ratio.
- Pipette 2 μL of gel mixture into the gel inlet of each microfluidic chip.
- Incubate plate horizontally for 30 minutes at 37°C for polymerization.
Endothelial Cell Seeding:
- Harvest HUVECs or HCAECs at 80-90% confluence.
- Prepare cell suspension at 8,000 cells/μL in EGM-2 medium.
- Add 2 μL of cell suspension to the perfusion inlet adjacent to the gel channel.
- Rotate plate 90° to allow cells to settle against the gel phaseguide.
- Incubate for 4 hours at 37°C to allow cell attachment.
Medium Perfusion:
- Add 50 μL of EGM-2 medium to the inlet and outlet wells.
- Place OrganoPlate on rocking platform (rocking interval: 8 minutes, 7° inclination).
- Continue culture for 3-5 days with daily medium changes until confluent endothelial tubules form.
Day 4-5: Inflammatory Stimulation and TEER Monitoring
- Baseline TEER Measurement:
Inflammatory Challenge:
Optional Immune Cell Recruitment:
- Isolate PBMCs from human blood using Ficoll gradient [20].
- Label PBMCs with CellTracker Orange CMRA (2.5 μM) for 30 minutes.
- Add 2 μL of PBMC suspension (5,000 cells/μL) to the perfusion inlet.
- Monitor immune cell adhesion and extravasation via time-lapse microscopy.
Day 5-7: Endpoint Analysis
- Immunofluorescence Staining:
- Fix cells with 4% PFA for 20 minutes.
- Permeabilize with 0.1% Triton X-100 for 10 minutes.
- Stain for junctional proteins (VE-Cadherin, ZO-1) and adhesion molecules (ICAM-1).
- Image using confocal microscopy to correlate TEER changes with junctional integrity.
- Data Analysis:
- Normalize TEER values to baseline measurements.
- Calculate rate of TEER decline and minimum TEER value.
- Correlate TEER kinetics with immune cell migration and protein expression.
Protocol: Real-Time TEER Monitoring of Vascular Barrier Function
Purpose: To continuously monitor vascular barrier integrity during inflammatory challenge using integrated electrodes.
Materials:
- Custom PDMS microfluidic chip with integrated Ag/AgCl electrodes [24]
- Lock-in amplifier (Zurich Instruments HF2LI) [24]
- Current amplifier (HF2TA) [24]
- HUVECs or primary human brain microvascular endothelial cells (hBMECs) [28]
- Endothelial cell culture medium
- AC signal source (0.8 V, 10 kHz) [24]
Procedure:
Chip Preparation and Electrode Integration:
- Use oxygen plasma to bond PDMS channels to glass slide.
- Insert Ag/AgCl electrodes into designated side channels.
- Sterilize chip with 70% ethanol and UV exposure.
- Coat membrane with fibronectin (50 μg/mL) for 1 hour at 37°C.
Cell Culture and Barrier Formation:
- Seed endothelial cells at high density (15,000 cells/μL) into apical channel.
- Allow cells to adhere for 4 hours without flow.
- Initiate low flow (0.01 dyn/cm²) for 24 hours, then increase to physiological shear stress (0.70 dyn/cm²).
- Culture for 3-5 days until stable barrier forms, confirmed by preliminary TEER measurements.
TEER Measurement Protocol:
- Connect electrodes to lock-in amplifier and current amplifier.
- Set oscillator frequency to 10 kHz with sampling rate of 1 kHz [24].
- Apply AC signal of 0.8 V between one pair of electrodes.
- Measure impedance values between all electrode combinations.
- Calculate TEER using formula: TEER (Ω·cm²) = (Rsample - Rblank) × A, where A is membrane area.
- Perform measurements every 30 minutes during inflammatory challenge.
Inflammatory Stimulation:
- Once baseline TEER stabilizes (typically 2-5 Ω·cm² for endothelial barriers), introduce inflammatory stimuli.
- Add TNFα (10 ng/mL) and IL-1β (5 ng/mL) to the basal channel.
- Continue TEER monitoring for 24-72 hours.
- Include control chips without inflammatory stimuli for normalization.
Data Interpretation:
- Early dysfunction: >20% decrease in TEER within 4 hours indicates junctional disassembly.
- Severe disruption: >50% decrease in TEER correlates with significant barrier failure.
- Recovery phase: Increasing TEER after removal of stimuli indicates barrier repair.
Signaling Pathways in Vascular Inflammation
Figure 1: Signaling Pathways in Microfluidic Vascular Inflammation Models. This diagram illustrates the key molecular events in cytokine-induced endothelial barrier dysfunction that can be monitored in real-time using TEER measurements in microfluidic platforms.
Experimental Workflow for Vascular Inflammation Studies
Figure 2: Integrated Workflow for Vascular Inflammation and TEER Studies. This workflow demonstrates the sequential steps for establishing, challenging, and analyzing vascular inflammation in microfluidic platforms with integrated TEER measurements.
Research Reagent Solutions
Table 3: Essential Research Reagents for Microfluidic Vascular Inflammation Studies
| Reagent/Cell Type | Function/Application | Example Source/Product |
|---|---|---|
| HUVECs | Primary endothelial cells for vascular tubule formation | Lonza (C2519AS) [20] |
| HCAECs | Coronary artery-specific endothelial cells | Promocell (C-12221) [26] |
| OrganoPlate Platform | Microfluidic device for vessel culture | Mimetas (2-lane-48 UF, 3-lane-64) [26] [20] |
| OrganoTEER System | Automated TEER measurement | Mimetas [20] |
| TNFα & IL-1β | Pro-inflammatory cytokines for barrier challenge | Recombinant human proteins [26] [20] |
| Fibrinogen/Thrombin | ECM hydrogel for 3D support | Sigma-Aldrich [20] |
| Anti-VE-Cadherin | Immunofluorescence of junctions | Various suppliers [20] |
| Anti-ICAM-1 | Marker for endothelial activation | Various suppliers [20] |
| CellTracker Dyes | Immune cell labeling for migration studies | Invitrogen (C34551) [20] |
| PREDICT96 Platform | High-throughput microfluidic system | Nortis [27] |
Building and Using Vascular Inflammation-on-a-Chip Models: From Design to Drug Screening
The development of physiologically relevant in vitro models of the vasculature is a critical endeavor in biomedical research, particularly for the study of vascular inflammation and the assessment of drug efficacy and toxicity. Microfluidic technology has emerged as a powerful tool for creating advanced vascular models, often referred to as vasculature-on-a-chip, that overcome the limitations of conventional two-dimensional (2D) cell cultures and animal studies [22] [29]. These limitations include an inability to replicate the three-dimensional (3D) cellular microenvironment, cell-cell interactions, and dynamic flow conditions present in vivo [22]. Among the various fabrication strategies for engineering microvascular networks in microfluidic devices, two primary approaches have gained prominence: microvessel patterning and vasculogenesis/angiogenesis-based self-assembly [22] [30]. Microvessel patterning involves the direct engraving of vascular-like microchannels into cell-laden hydrogel scaffolds using microfabrication techniques, followed by endothelial cell (EC) seeding [22]. In contrast, the self-assembly approach leverages the innate ability of ECs to form 3D vascular networks spontaneously within hydrogels through vasculogenic and angiogenic processes [22] [30]. This Application Note provides a detailed comparison of these two fabrication strategies, with a specific focus on their application in modeling vascular inflammation and quantifying endothelial barrier integrity via Trans-Endothelial Electrical Resistance (TEER) measurements. We include standardized protocols to facilitate the adoption of these techniques, along with a comparative analysis of their respective strengths and limitations for vascular inflammation research.
Fabrication Strategies: A Comparative Analysis
The choice between patterning and self-assembly strategies is fundamental, as it dictates the model's architecture, physiological relevance, and applicability to specific research questions, such as those involving vascular inflammation.
Table 1: Comparison of Microvessel Patterning and Self-Assembly Fabrication Strategies
| Feature | Microvessel Patterning | Self-Assembly (Vasculogenesis/Angiogenesis) |
|---|---|---|
| Fundamental Principle | Direct engraving of microchannels into hydrogels using microfabrication; subsequent EC seeding [22] [30] | Spontaneous formation of vascular networks by ECs encapsulated in hydrogels [22] [30] |
| Key Characteristics | Pre-defined geometry; high reproducibility; direct control over vessel size and architecture [22] | Complex, biologically relevant networks; lumen formation; branching morphogenesis [30] [31] |
| Vessel Architecture | Single, straight vessels or simple networks; often rectangular cross-section [31] | Interconnected, capillary-like networks with circular cross-sections [30] |
| Throughput | Moderate; suitable for medium-scale studies | High; scalable for drug screening (e.g., 64-96 chips per plate) [1] [32] |
| Barrier Function Assessment | Compatible with permeability assays; TEER measurement can be challenging due to 3D gel configuration | Highly compatible with real-time TEER monitoring in perfused tubules (e.g., in OrganoPlate platform) [1] [9] |
| Primary Applications | Fundamental studies of shear stress, leukocyte adhesion, molecule transport [22] | Disease modeling (e.g., vascular inflammation), drug screening, organ-specific phenotyping [1] [30] |
Protocols for Fabrication and Analysis
Protocol 1: Microvessel Patterning via Sacrificial Micromolding
This protocol details the creation of a single, perfusable microvessel within a 3D collagen gel using a needle-based sacrificial molding technique [22] [31].
Materials
- Polydimethylsiloxane (PDMS) or other device substrate
- Type I Collagen solution (e.g., rat tail collagen, 4 mg/mL)
- Sterile stainless-steel needle or wire (diameter 120-150 µm)
- Human Umbilical Vein Endothelial Cells (HUVECs) or other relevant ECs
- Endothelial Cell Growth Medium (e.g., EGM-2)
Procedure
- Device Fabrication: Fabricate a microfluidic device featuring a central gel chamber and two adjacent medium channels using standard soft lithography and PDMS bonding techniques [29].
- Needle Insertion and Gel Loading: Position a sterile steel needle across the central gel chamber, ensuring it spans the entire chamber and is suspended. Then, pipette the neutralized Type I collagen solution into the gel chamber around the needle. Incubate the device at 37°C for 30-45 minutes to allow for complete collagen polymerization.
- Needle Removal: Gently and carefully withdraw the needle from the polymerized collagen gel. This will leave behind a hollow, cylindrical microchannel within the gel.
- Endothelial Cell Seeding: Introduce a high-density suspension of HUVECs (e.g., 10-20 million cells/mL) into the newly formed microchannel. Allow the cells to adhere to the internal surface of the channel for 20-30 minutes.
- Perfusion and Culture: Connect the device to a perfusion system or place it on a rocker platform to establish continuous flow of EGM-2 medium through the endothelialized channel. Culture the vessel for 3-5 days to allow the formation of a confluent and mature endothelial monolayer.
Protocol 2: Self-Assembled Microvascular Network via Vasculogenesis
This protocol describes the formation of a self-assembled, capillary-like network by co-culturing ECs with supporting stromal cells in a fibrin hydrogel within a microfluidic device [30].
Materials
- OrganoPlate (e.g., 3-lane 64 or 96) or similar microfluidic platform
- Fibrinogen solution
- Thrombin solution
- Human Umbilical Vein Endothelial Cells (HUVECs)
- Normal Human Lung Fibroblasts (NHLFs) or other supporting stromal cells
- Endothelial Cell Growth Medium supplemented with angiogenic factors (e.g., 50 ng/mL VEGF)
Procedure
- Cell Preparation: Mix HUVECs with NHLFs at a defined ratio (e.g., 4:1) in a fibrinogen solution.
- Gel Loading: Combine the cell-fibrinogen mixture with thrombin and immediately pipette it into the central gel channel of the OrganoPlate. The device's phaseguides will confine the gel. Allow the fibrin gel to polymerize for 15-20 minutes at 37°C.
- Perfusion Culture: Add culture medium to the two adjacent perfusion channels. Place the OrganoPlate on a rocker platform to establish autonomous, bidirectional perfusion flow through the channels. This mimics interstitial flow and provides nutrients.
- Network Formation: Culture the device for 5-7 days, changing the medium every 2-3 days. Over this period, the ECs will spontaneously form an interconnected, perfusable 3D microvascular network within the fibrin gel.
Protocol 3: Assessing Vascular Inflammation and Barrier Integrity via TEER
This protocol is optimized for measuring TEER in self-assembled endothelial tubules within the OrganoPlate platform to quantify inflammatory activation and barrier dysfunction [1] [9].
Materials
- OrganoPlate 3-lane 64 with pre-formed self-assembled HUVEC tubules
- OrganoTEER measurement system or equivalent
- Inflammatory Cytokines: Tumor Necrosis Factor-alpha (TNFα) and Interferon-gamma (IFN-γ)
- Human Peripheral Blood Mononuclear Cells (PBMCs), isolated and optionally stimulated
- Fixation and Permeabilization Buffer
- Primary Antibodies: anti-VE-Cadherin, anti-ICAM-1
- Fluorescently-labeled Secondary Antibodies
Procedure
- Baseline TEER Measurement: Using the OrganoTEER system, perform an initial TEER measurement for all 64 chips on the plate to establish a baseline barrier integrity value.
- Inflammatory Challenge: Introduce an inflammatory stimulus into the perfusion medium. This can be:
- Option A (Cytokines): Add TNFα and IFN-γ at desired concentrations (e.g., 10-100 ng/mL each).
- Option B (Immune Cells): Introduce fluorescently labeled PBMCs (e.g., 400,000 cells/mL) into the perfusion channel containing the endothelial tubule.
- Continuous TEER Monitoring: Place the plate back on the rocker and inside the incubator. Use the OrganoTEER system to automatically and continuously monitor TEER values across all chips for the duration of the experiment (e.g., 24-72 hours). A decrease in TEER indicates increased permeability and barrier disruption.
- Endpoint Immunofluorescence Analysis: At the conclusion of the TEER measurements, fix the endothelial tubules, permeabilize them, and perform immunofluorescence staining for VE-Cadherin (to visualize adherens junctions) and ICAM-1 (to visualize endothelial activation). Image using confocal microscopy.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the protocols above requires a set of core reagents and specialized equipment.
Table 2: Key Research Reagent Solutions for Vascular-on-Chip Models
| Item | Function/Description | Example Use Case |
|---|---|---|
| OrganoPlate | Microfluidic platform with 40, 64, or 96 chips in a standard microtiter plate format; enables high-throughput, perfused 3D cell culture [1] [9]. | Foundation for self-assembled network formation and continuous TEER measurement. |
| OrganoTEER | Automated instrument for continuous, non-invasive Trans-Endothelial Electrical Resistance measurement in the OrganoPlate [1] [9]. | Gold-standard quantification of endothelial barrier integrity in response to inflammatory stimuli. |
| Type I Collagen | Natural hydrogel derived from rat tail; provides a biocompatible 3D scaffold for cell growth and morphogenesis. | The primary matrix for the sacrificial molding protocol (Protocol 1). |
| Fibrin Gel | Natural hydrogel formed from fibrinogen and thrombin; highly conducive to endothelial cell sprouting and network formation. | The preferred matrix for the self-assembly vasculogenesis protocol (Protocol 2) [30]. |
| HUVECs | Primary Human Umbilical Vein Endothelial Cells; a standard and widely used model for studying vascular endothelium. | The core cellular component for forming the endothelial lumen in both patterning and self-assembly strategies. |
| TNFα & IFN-γ | Pro-inflammatory cytokines that synergistically activate endothelial cells, disrupting junctions and upregulating adhesion molecules [1]. | Used to induce a controlled and reproducible state of vascular inflammation in the model. |
| Anti-VE-Cadherin Antibody | Target for immunofluorescence staining to visualize and quantify the integrity of endothelial adherens junctions. | Endpoint analysis to correlate TEER drop with structural disassembly of the barrier. |
| Anti-ICAM-1 Antibody | Target for immunofluorescence staining to visualize and quantify endothelial activation in response to inflammation [1]. | Endpoint analysis to confirm the pro-inflammatory phenotype of the endothelium. |
| DSPE-PEG46-Folate | DSPE-PEG46-Folate|Folate-Targeted PEG Lipid | DSPE-PEG46-Folate is a high-affinity ligand for targeted drug delivery to folate receptor-rich cancer cells. For Research Use Only. Not for human use. |
| FAK inhibitor 6 | FAK inhibitor 6, MF:C25H24FN5O2S, MW:477.6 g/mol | Chemical Reagent |
Within the context of vascular inflammation research using microfluidic platforms, the ability to quantify endothelial barrier integrity is paramount. The Transendothelial Electrical Resistance (TEER) assay is a gold-standard, non-invasive, and quantitative method for real-time assessment of this barrier function. This application note details a integrated protocol for establishing a functional Human Umbilical Vein Endothelial Cell (HUVEC) tubule network on a basement membrane matrix within a microfluidic device, followed by its validation through TEER measurement. This methodology is essential for researchers and drug development professionals modeling diseases like atherosclerosis or thrombosis, where barrier dysfunction is a critical pathological event [33] [34] [35].
Experimental Workflow and Signaling Pathways
The following diagrams outline the core experimental workflow and the key signaling pathways modulating endothelial barrier function, providing a conceptual map for the protocol.
Diagram 1: A sequential workflow for establishing HUVEC tubules and measuring TEER.
Diagram 2: Key signaling pathways regulating endothelial barrier integrity and TEER.
Materials and Reagent Solutions
Table 1: Essential research reagents and materials for the HUVEC tubule formation and TEER assay.
| Item | Function / Description | Example & Notes |
|---|---|---|
| Endothelial Cells | Primary cell source for tubule formation. | Primary HUVEC or HUVEC-CS immortalized line [36]. Use low-passage cells (P2-P8) [37]. |
| Basement Membrane Extract (BME) | 3D substrate that supports tube formation. | Geltrex or Matrigel [37] [38]. Use a reduced-growth factor formulation; concentration is critical (>10 mg/mL) [38]. |
| Endothelial Cell Medium | Base culture medium. | Medium 200PRF, supplemented appropriately [37] [34]. |
| Low Serum Growth Supplement (LSGS) | Provides essential pro-angiogenic factors. | Contains FBS, bFGF, EGF, hydrocortisone, and heparin [37] [34]. |
| cAMP-Elevating Agents | Pharmacological enhancers of barrier function. | 8-CPT-cAMP (250 µM) and Ro-20-1724 (17.5 µM) as positive control [34]. |
| Pro-Inflammatory Cytokines | Inducers of barrier dysfunction for disease modeling. | TNF-α and IL-1β (e.g., 2 ng/mL) to simulate vascular inflammation [33]. |
| Cell Viability Stain | For fluorescent visualization of tubular networks. | Calcein AM (2 µg/mL final concentration) [37] [38]. |
| Microfluidic Chip | Platform with microchannels and integrated electrodes. | PDMS-based chips with or without embedded electrodes for TEER [33]. |
| TEER Measurement System | Instrument for real-time, label-free impedance monitoring. | Electric Cell-substrate Impedance Sensing (ECIS) or similar systems [34]. |
Quantitative Data and Parameters
Table 2: Key quantitative parameters for HUVEC tube formation and TEER response to stimuli.
| Parameter | Typical Value / Range | Context and Notes |
|---|---|---|
| Cell Seeding Density | 35,000 - 45,000 cells/cm² [37] | Must be optimized for specific microfluidic device geometry. |
| BME Coating Volume | 50 - 100 µL/cm² [37] | Thicker gels (100 µL/cm²) for smaller wells to prevent drying. |
| Time to Initial Tube Formation | 1 - 2 hours [38] | Endothelial cells begin to align and form cords. |
| Peak Tube Formation | 4 - 6 hours (HUVEC) [37] | Well-defined, lumen-containing tubules are visible. |
| Tube Network Apoptosis | ~18 - 24 hours [37] [38] | Networks begin to deteriorate after this period. |
| Baseline TEER (Confluent HUVEC) | 600 - 1200 Ω [34] | Measured using ECIS system; baseline for healthy monolayer. |
| IC₅₀ of RAP in 3D Pathological Model | 55.36 µM [33] | Highlights altered drug efficacy in a 3D perfused AS model vs. 2D (32.69 µM). |
Step-by-Step Protocol
A. HUVEC Culture and Pre-Assay Preparation (Days 1-5)
- Cell Culture: Maintain HUVECs in a T-75 flask with supplemented Medium 200PRF (containing LSGS). Change the medium 24 hours after seeding and every other day thereafter until cells reach approximately 80% confluency (typically 5-6 days) [37].
- Serum Starvation: One day prior to the assay, aspirate the growth medium and replace it with reduced-serum medium (e.g., Medium 200PRF with 0.2% FBS) to synchronize the cell cycle and reduce background proliferative signals [38].
B. Microfluidic Chip Preparation and Cell Seeding (Day 6)
- Matrix Coating: Pre-cool a microfluidic chip (and pipette tips) on ice. Thaw the BME on ice or in a refrigerator to keep it liquid. Pipette the appropriate volume of chilled BME into the main channel of the microfluidic device, ensuring complete and even coverage. Incubate the chip at 37°C for 30 minutes to allow the matrix to solidify [37] [38].
- Cell Harvest and Staining (Optional): Harvest HUVECs using trypsin-EDTA, neutralize with a trypsin neutralizer, and centrifuge to form a pellet. Resuspend the cell pellet in non-supplemented medium. For fluorescent visualization, incubate cells with Calcein AM (2 µg/mL) for 30 minutes at 37°C protected from light prior to harvesting or after tube formation [37].
- Cell Seeding: Resuspend the harvested HUVECs at a high concentration (e.g., 7.5 x 10ⶠcells/mL) in complete medium, optionally mixed with pro-angiogenic, barrier-enhancing (e.g., cAMP agonists), or pro-inflammatory stimuli. Gently introduce the cell suspension into the BME-coated channel of the microfluidic chip. Allow the cells to attach by incubating the chip statically at 37°C and 5% CO₂ for 1 hour.
- Perfusion Culture: Connect the chip to a perfusion system and initiate a low flow rate (e.g., 20 µL/h) to provide continuous nutrient supply and physiological shear stress, which enhances biological performance and tube formation [33].
C. Tube Formation, TEER Measurement, and Analysis (Day 6-7)
- Monitoring Tube Formation: Monitor the formation of capillary-like structures using an inverted phase-contrast or fluorescence microscope. Initial tube alignment should be visible within 1-2 hours, with a peak network typically forming between 4-6 hours for HUVECs [37] [38].
- TEER Measurement:
- If using a chip with integrated electrodes, initiate real-time TEER measurements once a confluent monolayer or tubule network is established. Record the impedance frequently.
- For chips without integrated electrodes, cells may need to be trypsinized after tube imaging and re-seeded into a dedicated electrode-containing well (e.g., an ECIS array) pre-coated with a physiological matrix like gelatin or fibronectin for TEER measurement [34].
- To assess barrier function, compare the normalized TEER values of treated samples (e.g., with cAMP-elevating agents) against controls. A successful barrier-enhancing treatment should show a significant increase in TEER compared to the baseline [34].
- Endpoint Quantification and Imaging:
- Tube Network: Quantify the tube network from microscope images using software like ImageJ with the Angiogenesis Analyzer plugin. Key parameters include the number of branch points (nodes), total tube length, and the number of meshes (loops) [38].
- Immunostaining: Fix the tubules with 4% paraformaldehyde for 15 minutes for subsequent immunocytochemistry. Stain for junctional proteins like VE-cadherin (adherens junctions) and ZO-1 (tight junctions) to visually confirm the maturation and strengthening of cell-cell contacts, which correlates with higher TEER readings [34].
Troubleshooting and Technical Notes
- No Tube Formation in Positive Control: Ensure cells are healthy and at a low passage number (P2-P8). Optimize the cell seeding density, as both overly high and low densities can prevent proper network formation. Verify the quality and concentration of the BME [37].
- Low or Highly Variable TEER Readings: Confirm that a confluent monolayer/tubule network has formed before measurement. Check for contamination with mycoplasma, which can degrade barrier function. Ensure consistent and firm contact of electrodes with the measurement medium or substrate [34].
- Integration with Pathological Modeling: To model vascular inflammation, perfuse the established HUVEC tubules with pro-inflammatory cytokines (e.g., TNF-α, IL-1β) or oxidized low-density lipoprotein (ox-LDL) [33]. Monitor the subsequent drop in TEER as a quantitative indicator of barrier disruption, and test therapeutic candidates for their ability to prevent or rescue this decline.
Within vascular biology and drug development research, robust in vitro models of inflammation are crucial. This application note provides detailed protocols for inducing and quantifying inflammatory responses in microfluidic vascular platforms, specifically tailored for research on Transendothelial Electrical Resistance (TEER) within a thesis context. We focus on the application of key effector cytokines—Tumor Necrosis Factor-alpha (TNF-α) and Interferon-gamma (IFN-γ)—and Peripheral Blood Mononuclear Cells (PBMCs) to model vascular inflammation, assess barrier integrity, and investigate underlying mechanobiological phenomena [39] [40].
The tables below summarize standard concentrations and key quantitative data for inducing inflammation with cytokines and PBMCs, providing a reference for experimental design.
Table 1: Standard Cytokine Concentrations for Inflammatory Induction
| Cytokine | Typical Working Concentration | Key Functions in Vascular Inflammation | Primary Source |
|---|---|---|---|
| TNF-α | 10-100 ng/mL [39] | Promotes endothelial activation, adhesion molecule (ICAM-1, VCAM-1) expression, and pro-inflammatory cytokine secretion. | Activated macrophages, T cells [39] |
| IFN-γ | 10-100 ng/mL [39] | Synergizes with TNF-α, enhances antigen presentation, and drives Th1-type immune responses. | Activated T cells (Th1), NK cells [39] |
Table 2: Key Quantitative Data from Cytokine and PBMC Assays
| Parameter | Measured Value / Observation | Experimental Context | Significance |
|---|---|---|---|
| PBMC Proliferation (with PHA) | Varies significantly between donor lots [41] | One-way MLR assay; 0.5-1.0 µg/mL PHA [41] | Highlights need for PBMC lot quality control. |
| IFN-γ & TNF-α in PBMC Supernatant | High levels correlate with robust MSC immunosuppressive potency assays [41] | PHA-stimulated PBMCs (0.2-1.0 µg/mL) [41] | Serves as a quality marker for effective PBMC responses. |
| Duration of IFN-γ Neutralization | Required prolonged intervention (>6 days) to attenuate kidney injury [39] | Established anti-MPO glomerulonephritis model in mice [39] | Suggests sustained cytokine presence is critical in chronic models. |
Experimental Protocols
Protocol 1: Cytokine-Induced Vascular Inflammation and TEER Measurement
This protocol describes the direct activation of endothelial cells using recombinant cytokines to model vascular inflammation and monitor barrier dysfunction via TEER.
Materials:
- Microfluidic organ-on-chip device with a vascular channel.
- Human Umbilical Vein Endothelial Cells (HUVECs) or other relevant endothelial cells.
- Endothelial Cell Growth Medium.
- Serum-free or low-serum medium for cytokine stimulation.
- Recombinant Human TNF-α and IFN-γ.
- TEER measurement system compatible with the microfluidic device.
Procedure:
- Cell Seeding and Barrier Formation: Seed HUVECs into the vascular channel of the microfluidic device at a high density (e.g., 1-5 x 10^6 cells/mL). Allow the cells to form a confluent monolayer under continuous, physiologically relevant flow (e.g., 0.5 - 5 dyn/cm² shear stress) for 2-4 days [22] [40].
- Baseline TEER Measurement: Measure the TEER value of the endothelial monolayer before cytokine application. This serves as the baseline (100%) barrier integrity.
- Cytokine Stimulation: Prepare a cytokine cocktail in serum-free medium containing both TNF-α (10-50 ng/mL) and IFN-γ (10-50 ng/mL) [39]. Replace the medium in the vascular channel with the cytokine-containing medium.
- Incubation and Monitoring: Maintain the device under static conditions or continuous flow. Monitor TEER at regular intervals (e.g., 4h, 8h, 24h, 48h) post-stimulation. A significant drop in TEER indicates barrier disruption and successful induction of inflammation [40].
- Endpoint Analysis: Following TEER measurements, the device can be fixed for immunostaining (e.g., for VE-Cadherin, F-actin) or the effluent collected for analysis of secreted cytokines (e.g., IL-6, IL-8) via ELISA.
Protocol 2: PBMC-Mediated Vascular Inflammation and Transendothelial Migration (TEM)
This protocol leverages the activation of PBMCs to induce a more complex, cellular model of inflammation, culminating in immune cell transmigration.
Materials:
- Microfluidic device with a confluent endothelial monolayer.
- Freshly isolated or cryopreserved human PBMCs.
- RPMI 1640 medium supplemented with 10% FBS.
- Mitogen: Phytohemagglutinin (PHA-P).
- DNase I solution.
Procedure:
- PBMC Preparation: Thaw cryopreserved PBMCs rapidly and wash in warm RPMI 1640 medium containing 20 U/mL DNase I. Centrifuge and resuspend in complete medium. Allow cells to recover for 1 hour at 37°C [41].
- Endothelial Pre-stimulation (Optional but recommended): To enhance TEM, pre-treat the endothelial monolayer in the microfluidic device with TNF-α (10 ng/mL) for 4-6 hours prior to adding PBMCs. This upregulates adhesion molecules [40].
- PBMC Activation and Introduction: Activate PBMCs (5 x 10^5 cells/mL) with PHA at 0.5 - 1.0 µg/mL [41]. Immediately introduce the activated PBMC suspension into the vascular channel of the microfluidic device.
- Co-culture and TEM Induction: Co-culture the PBMCs with the endothelium for 24-48 hours. The presence of activated PBMCs and their secreted cytokines (including IFN-γ and TNF-α) will activate the endothelium and promote TEM [41] [42].
- Quantification of TEM:
- Real-time Imaging: Use live-cell imaging to track the migration of fluorescently labeled PBMCs across the endothelium.
- Endpoint Quantification: After co-culture, collect cells from the parenchymal channel and count the number of transmigrated PBMCs using flow cytometry.
- TEER Correlation: Measure TEER throughout the co-culture period to correlate the extent of immune cell adhesion and transmigration with the loss of endothelial barrier function [40].
Signaling Pathways and Experimental Workflow
The following diagrams, created using the specified color palette, illustrate the core signaling pathways and experimental workflows.
Cytokine Signaling in Endothelial Cells
Vascular Inflammation Assay Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Vascular Inflammation Assays
| Item | Function / Application | Example / Note |
|---|---|---|
| Recombinant TNF-α & IFN-γ | Direct induction of endothelial inflammation and barrier dysfunction. | Use high-purity, carrier-free proteins. Aliquot and store at -80°C [39]. |
| PBMCs | Provide a complex, physiologically relevant immune challenge. | Quality varies by donor lot; pre-screen for consistent inflammatory response (high IFN-γ/TNF-α production) [41]. |
| PHA (Phytohemagglutinin) | Mitogen used to activate T-cells within PBMC populations. | Optimal concentration for activation is typically 0.5-1.0 µg/mL [41]. |
| Microfluidic Platform | Provides a dynamic, shear-stress-enabled environment for realistic vascular models. | Devices should allow for TEER measurement and real-time imaging [22] [40]. |
| TEER Measurement System | Quantitative, non-invasive monitoring of endothelial barrier integrity. | Key metric for assessing inflammatory insult and therapeutic intervention [40]. |
| Anti-inflammatory mAbs | Tool for validating specific cytokine pathways (e.g., anti-TNF-α, anti-IFN-γ). | Used as positive controls to confirm mechanism [39]. |
| Collagen I / IV, Fibronectin | ECM coatings for the vascular channel to support endothelial cell adhesion and function. | Mimics the native basement membrane [22]. |
| ACP-5862-d4 | ACP-5862-d4, MF:C26H23N7O3, MW:485.5 g/mol | Chemical Reagent |
| Inosine-2,8-d2 | Inosine-2,8-d2, MF:C10H12N4O5, MW:270.24 g/mol | Chemical Reagent |
Transepithelial/transendothelial electrical resistance (TEER) is a widely accepted quantitative technique to measure the integrity of tight junction dynamics in cell culture models of endothelial and epithelial monolayers [3]. In the context of drug development, TEER values are strong indicators of the integrity of cellular barriers before they are evaluated for transport of drugs or chemicals [3]. The capability to perform TEER measurements in real-time without cell damage makes it particularly valuable for preclinical screening, enabling researchers to monitor barrier integrity throughout the course of an experiment and identify subtle, dynamic responses to compounds [3] [27]. This application note details the implementation of TEER within microfluidic platforms, specifically framing its utility for screening drug efficacy and toxicity in models of vascular inflammation and kidney function.
TEER Principles and Significance in Screening
TEER is a direct measure of the ionic conductance of the paracellular pathway in an epithelial or endothelial monolayer [3]. It reflects the integrity of tight junctions—the specialized cell-cell adhesions that regulate paracellular transport. A higher TEER value indicates a tighter, more selective barrier, while a decrease in TEER signifies increased paracellular permeability and a potential loss of barrier integrity [3] [27].
In toxicity and efficacy screening, this is critical because many drug-induced injuries and inflammatory conditions manifest through the disruption of these cellular barriers. TEER serves as a sensitive, non-invasive, and label-free metric to quantify this disruption. Unlike endpoint assays that require cell lysis or fluorescent labels, TEER allows for the repeated assessment of the same tissue replicate over time, enabling the tracking of the onset, progression, and potential recovery from toxic or therapeutic insults [27]. This can reveal early indicators of toxicity before cell death occurs, providing a more nuanced understanding of a compound's mechanism of action [27].
Table 1: Advantages of TEER for Drug Screening Applications
| Feature | Benefit in Drug Screening |
|---|---|
| Non-invasive & Label-free | Permits real-time, longitudinal monitoring of the same tissue; avoids interference from dyes or labels. |
| Quantitative & Sensitive | Provides a numerical value (Ω·cm²) for high-resolution tracking of subtle barrier changes. |
| Early Indicator of Toxicity | Can detect barrier disruption prior to the onset of cell death, offering an earlier readout. |
| Functional Readout | Directly measures a key physiological property—barrier function—rather than a surrogate marker. |
| Compatibility with Microfluidics | Enables integration into high-throughput, physiologically relevant organ-on-a-chip platforms. |
TEER in Action: Key Application Data
Recent studies demonstrate the practical application of TEER in high-throughput screening environments. The following tables summarize key quantitative findings from seminal research in nephrotoxicity and vascular inflammation.
Table 2: TEER as a Metric for Nephrotoxicity Screening in a High-Throughput Microfluidic Platform (PREDICT96) [27]
| Experimental Condition | Baseline TEER (Ω·cm²) | Response to Cisplatin (40 µM) | Correlation with Other Assays |
|---|---|---|---|
| PT (hRPTEC) / Microvascular (hMVEC) Co-culture | 5 - 10 Ω·cm² | Dose-dependent decrease in TEER. | Well-correlated with LDH cytotoxicity and loss of tight junction coverage. |
| PT (hRPTEC) Mono-culture | 5 - 10 Ω·cm² | No dose-dependent TEER change observed. | Higher baseline LDH release; less differentiated phenotype. |
| Key Finding | Co-culture model is essential for TEER to function as a reliable metric of toxicity. | TEER decrease was detectable prior to increases in cell death, highlighting its early-indicator capability. |
Table 3: TEER for Monitoring Vascular Inflammation in a Scalable Organ-on-a-Chip Platform (OrganoPlate) [20]
| Treatment Condition | Effect on TEER (HUVEC Tubules) | Additional Phenotypic Observations |
|---|---|---|
| Inflammatory Cytokines (TNF-α & IFN-γ) | Significant decrease in TEER values. | Increased ICAM expression; changes in endothelial morphology; destabilization of VE-Cadherin. |
| Human Peripheral Blood Mononuclear Cells (PBMCs) | Decrease in TEER values. | Increased immune cell adhesion and migration. |
| Key Finding | Platform allows parallel TEER measurements in 64 perfused tubules, demonstrating suitability for high-throughput screening of anti-inflammatory compounds. |
Another study utilizing a tissue-engineered venule-like model demonstrated that perfusion with aged human serum (average donor age 65) resulted in increased paracellular permeability and transcriptomic signatures of aging compared to young serum (average donor age 25), further underscoring TEER's role in modeling age-related vascular dysfunction and compound sensitivity [43].
Detailed Experimental Protocols
Protocol 1: Assessing Drug-Induced Nephrotoxicity in a Microfluidic Co-culture Model
This protocol is adapted from a study using the PREDICT96 platform to evaluate cisplatin-induced toxicity in a human primary kidney proximal tubule (PT) model [27].
4.1.1 Research Reagent Solutions
Table 4: Essential Materials for Nephrotoxicity Screening
| Item | Function / Description | Example |
|---|---|---|
| Primary Cells | Forms the functional kidney barrier. | Human Renal Proximal Tubule Epithelial Cells (hRPTEC). |
| Support Cells | Co-culture to improve physiological relevance and model differentiation. | Human Microvascular Endothelial Cells (hMVEC). |
| Microfluidic Platform | High-throughput culture and measurement. | PREDICT96 system (96 independent microfluidic tissues). |
| TEER Measurement System | Integrated, rapid TEER measurement capability. | PREDICT96 TEER system. |
| Culture Medium | Cell-specific growth medium. | EGM-2 for hMVEC; PT-specific medium for hRPTEC. |
| Toxicant | Model nephrotoxic compound. | Cisplatin. |
| Validation Assays | Endpoint assays to correlate with TEER data. | Lactate Dehydrogenase (LDH) Cytotoxicity Assay; Immunofluorescence for ZO-1. |
4.1.2 Methodological Workflow
4.1.3 Procedure
- Cell Seeding: Seed human primary renal proximal tubule epithelial cells (hRPTEC) onto the porous membrane of the microfluidic device (apical side). Culture for 24-48 hours to allow initial attachment.
- Co-culture Establishment: Seed human primary microvascular endothelial cells (hMVEC) on the opposite side of the membrane (basolateral side) to establish a co-culture model.
- Barrier Maturation: Apply continuous physiological fluid shear stress (e.g., 0.70 dyn/cm²) to both channels. Culture for 5-10 days, with periodic medium changes, until a stable barrier is formed, as indicated by a consistent baseline TEER reading.
- Baseline Measurement: Measure the baseline TEER value for each tissue replicate using the integrated TEER system. The model is ready for dosing when TEER values are stable, typically between 5-10 Ω·cm² for this primary cell model [27].
- Compound Exposure: Administer the test compound (e.g., Cisplatin at various doses) to the apical channel. Include vehicle controls.
- Longitudinal TEER Monitoring: Measure TEER at regular intervals (e.g., 4h, 24h, 48h, 72h) post-exposure. A dose-dependent decrease in TEER indicates loss of barrier integrity and potential nephrotoxicity.
- Endpoint Analysis: Correlate TEER data with endpoint assays. For cytotoxicity, measure LDH release in the effluent. For junctional integrity, fix the tissues and perform immunofluorescence staining for tight junction proteins like ZO-1.
Protocol 2: Screening for Vascular Inflammatory Compounds
This protocol is based on a scalable platform for modeling vascular inflammation in the OrganoPlate, combining TEER with immune cell migration assays [20].
4.2.1 Research Reagent Solutions
Table 5: Essential Materials for Vascular Inflammation Screening
| Item | Function / Description | Example |
|---|---|---|
| Endothelial Cells | Forms the vascular tubule barrier. | Human Umbilical Vein Endothelial Cells (HUVECs). |
| Immune Cells | To model immune cell interaction and migration. | Human Peripheral Blood Mononuclear Cells (PBMCs). |
| Microfluidic Platform | Membrane-free, ECM-supported 3D culture. | OrganoPlate 3-lane 64. |
| Automated TEER Reader | For high-throughput TEER measurements. | OrganoTEER measurement system. |
| Extracellular Matrix (ECM) | Physiological scaffold for tubule formation. | Fibrin or Collagen I gel. |
| Inflammatory Cytokines | To induce endothelial activation and barrier disruption. | TNF-α and IFN-γ. |
| Cell Tracking Dye | To visualize and quantify immune cell migration. | CellTracker Orange CMRA. |
4.2.2 Methodological Workflow
4.2.3 Procedure
- Tubule Formation:
- Load an extracellular matrix (ECM) gel, such as fibrin or collagen, into the middle channel of the OrganoPlate 3-lane 64.
- Seed HUVECs into one of the two perfusion channels, where they will form a monolayer against the ECM gel, creating a 3D endothelial tubule.
- Culture the plate under continuous perfusion for 3-5 days to form a confluent, functional endothelial barrier.
- Baseline TEER: Use the OrganoTEER system to measure the baseline electrical resistance across the endothelial tubules.
- Inflammatory Challenge:
- To induce inflammation, perfuse the endothelial tubules with culture medium containing inflammatory cytokines (e.g., 10 ng/mL TNF-α and 10 ng/mL IFN-γ) for 24-48 hours.
- Alternatively, or in addition, introduce fluorescently labeled human PBMCs into the lumen of the endothelial tubule.
- Real-Time Monitoring:
- Continuously monitor TEER values throughout the inflammatory challenge. A significant drop in TEER indicates cytokine-induced barrier disruption [20].
- If using PBMCs, use time-lapse imaging to quantify immune cell adhesion and trans-endothelial migration.
- Multiplexed Analysis: Following the experiment, fix and stain the tubules for markers of endothelial activation (e.g., ICAM-1) and junctional integrity (e.g., VE-Cadherin). Correlate the immunofluorescence data with the kinetic TEER profiles.
Critical Factors for Reliable TEER Screening
Successful implementation of TEER for screening requires careful control of experimental conditions:
- Cell Source: Primary cells or stem cell-derived lineages often provide more physiologically relevant barrier properties than immortalized cell lines. Co-culture with supportive cells (e.g., pericytes, fibroblasts) is critical for achieving mature, stable barriers in many models [43] [27].
- Fluid Flow: The application of physiological levels of fluid shear stress is a key driver of endothelial and epithelial differentiation and function, and must be incorporated to generate predictive models [27].
- Measurement Consistency: Electrode placement and geometry can significantly impact TEER readings. Use integrated electrode systems where possible to ensure uniformity and reproducibility across a screening platform [3].
- Data Reporting: Always report TEER values normalized to the surface area of the barrier (Ω·cm²) to enable cross-study comparisons. Subtract the resistance of a cell-free blank insert or device to calculate the tissue-specific resistance [3].
Integrating TEER measurement into microfluidic organ-on-a-chip platforms transforms it from a simple integrity check into a powerful, dynamic tool for drug discovery. Its ability to provide non-invasive, real-time, and functional data on barrier health makes it ideal for identifying subtle toxicities and efficacious compounds early in the development pipeline. The protocols and data outlined herein provide a framework for deploying TEER in robust, high-throughput screening campaigns for nephrotoxicity and vascular inflammation, ultimately contributing to the development of safer and more effective therapeutics.
Optimizing Reliability and Accuracy in Microfluidic TEER Measurements
Within microfluidic platform modeling of vascular inflammation, the accurate assessment of tissue barrier integrity is paramount. Transepithelial/transendothelial electrical resistance (TEER) has emerged as a gold-standard, non-invasive technique to quantify the integrity of cellular monolayers in real-time [3]. For researchers and drug development professionals, selecting the appropriate measurement system is a critical step in experimental design. This application note provides a detailed comparison between the widely used EVOM2 volt-ohmmeter and the more comprehensive approach of impedance spectroscopy, framing their application within the context of vascular inflammation research on microfluidic platforms. We present structured quantitative data, detailed experimental protocols, and essential toolkits to guide this decision-making process.
Technical Comparison: EVOM2 vs. Impedance Spectroscopy
The choice between an EVOM2 system and an impedance spectroscopy-based approach hinges on the specific requirements of the experimental workflow, including throughput, data richness, and compatibility with dynamic culture systems.
Table 1: System Comparison for Vascular Inflammation Research
| Feature | EVOM2 (Volt-Ohmmeter) | Impedance Spectroscopy |
|---|---|---|
| Core Measurement | Ohmic resistance at a single, low frequency (e.g., 12.5 Hz) [3] | Complex impedance (magnitude and phase) across a frequency spectrum [44] |
| Primary Output | TEER value (Ω·cm²) | Nyquist plots, Bode plots, equivalent circuit parameters (e.g., TEER, membrane capacitance) [44] |
| Information Depth | Primarily reflects paracellular ionic conductance (tight junction integrity) [3] | Distinguishes paracellular (TEER) and transcellular (cell membrane capacitance) pathways [45] |
| Throughput | EVOM2 Auto: ~96 wells in <3.5 minutes [46] | Varies by system; typically slower than single-frequency readers |
| Key Advantage | Speed, simplicity, and established workflows for standard Transwells [46] | Richer data for mechanistic studies, detects subtle barrier changes [47] [44] |
| Best Suited For | High-throughput integrity screening in standard static or dynamic cultures [46] | Advanced R&D, investigating barrier formation kinetics, and complex co-culture models [47] |
Table 2: Microfluidic Integration and Data Output
| Aspect | EVOM2 | Impedance Spectroscopy |
|---|---|---|
| Integration with Microfluidics | Often uses external ("chopstick") electrodes or custom-integrated wires [17] [45] | Often features electrodes embedded within the microfluidic device itself [47] |
| Spatial Resolution | Low; provides an average resistance for the entire membrane area [3] | Can be very high with HD-MEA chips, enabling impedance mapping of tissue heterogeneity [47] |
| Real-Time Monitoring | Possible with custom add-ons or auto-sampling systems [48] | Inherent capability; standard for many commercial systems [44] |
Experimental Protocols
Protocol 1: TEER Measurement in a Microfluidic Bioreactor Using an EVOM2 System
This protocol adapts the standard EVOM2 for use in a dual-flow milli-fluidic bioreactor model of vascular inflammation, based on established methods in the literature [45].
Research Reagent Solutions & Materials
- Cellular Model: Human Umbilical Vein Endothelial Cells (HUVECs) or a relevant endothelial cell line.
- Microfluidic Bioreactor: A dual-flow bioreactor with a semi-permeable membrane and ports for electrode access [45].
- Measurement System: EVOM2 volt-ohmmeter (WPI) [46].
- Electrodes: Ag/AgCl electrodes, either external "chopstick" style or custom-integrated into the bioreactor housing [45].
- Cell Culture Medium: Appropriate endothelial cell growth medium (e.g., EGM-2).
Procedure
- System Sterilization and Seeding: Sterilize the bioreactor and associated fluidic lines. Seed endothelial cells at a defined density (e.g., 50,000 cells/cm²) onto the semi-permeable membrane within the bioreactor. Allow cells to adhere under static conditions for 4-8 hours.
- Initiate Flow and Culture: Connect the bioreactor to a perfusion system and initiate flow at a low, physiologically relevant shear stress (e.g., 1-5 dyn/cm²). Continue culture until a confluent monolayer is expected (typically 3-7 days).
- Blank Measurement: Before seeding cells, perfuse the bioreactor with culture medium alone. Insert the electrodes into their designated ports, ensuring they are immersed in medium on opposite sides of the membrane. Record the resistance value (Rblank). This represents the background resistance of the system.
- Sample Measurement: At each measurement time point, pause the flow to minimize electrical noise. Carefully insert the electrodes into the same predefined positions. Record the total resistance value (Rtotal).
- TEER Calculation: Calculate the cell layer-specific TEER using the formula, accounting for the membrane area (A) of the bioreactor:
- TEER (Ω·cm²) = (Rtotal - Rblank) × A (cm²) [3].
- Data Logging: For real-time monitoring, connect the EVOM2's analog output to a custom data logger [48] or use an automated system like the EVOM Auto to record measurements at defined intervals.
The workflow for this protocol is summarized in the following diagram:
Protocol 2: High-Resolution Impedance Mapping of an Inflammatory Response
This protocol utilizes a High-Density Microelectrode Array (HD-MEA) chip to monitor endothelial barrier function with high spatiotemporal resolution before and after an inflammatory stimulus [47].
Research Reagent Solutions & Materials
- Cellular Model: HUVECs or other relevant endothelial cells.
- HD-MEA Chip: A CMOS-integrated microelectrode array, e.g., featuring 16,384 electrodes [47].
- Impedance Analyzer: A system capable of performing electrochemical impedance spectroscopy (EIS) or single-frequency monitoring, integrated with the HD-MEA.
- Inflammatory Agent: Tumor Necrosis Factor-alpha (TNF-α).
- Coating Solution: Collagen Type I, diluted in 0.02N Acetic Acid to 0.1 mg/mL [47].
Procedure
- Chip Preparation: Sterilize the HD-MEA chip and attach a culture insert to define the growth area. Coat the chip surface with the collagen solution for at least 1 hour at 37°C.
- Cell Seeding and Culture: Seed endothelial cells onto the coated HD-MEA chip at a confluent density. Culture the cells under standard conditions, allowing them to form a tight monolayer.
- Baseline Impedance Measurement: Once confluent (as verified by a stable impedance signal), acquire baseline impedance maps. A single frequency (e.g., 1 kHz) is often sufficient for monitoring barrier integrity [47]. The system will generate a 2D map of |Z|1kHz across thousands of electrodes, providing a baseline picture of barrier homogeneity.
- Application of Inflammatory Stimulus: Introduce an inflammatory stimulus (e.g., 10 ng/mL TNF-α) into the culture medium.
- Continuous Impedance Monitoring: Continue to acquire impedance maps at regular intervals (e.g., every 20 minutes) for 24-48 hours post-stimulation.
- Data Analysis: Analyze the |Z|1kHz maps over time. The overall decrease in impedance indicates global barrier disruption. Furthermore, leverage the high spatial resolution to identify heterogeneous responses within the monolayer, such as areas with varying susceptibility to disruption [47].
The workflow for this advanced protocol is as follows:
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for TEER Studies
| Item | Function & Application |
|---|---|
| EVOM2 with EVOM Auto System | Automated TEER measurement system for high-throughput screening in 96-well plates, minimizing handling errors and contamination [46]. |
| High-Density Microelectrode Array (HD-MEA) Chip | A CMOS-integrated chip with thousands of microelectrodes for impedance mapping of epithelial/endothelial tissues with subcellular spatial resolution [47]. |
| Dual-Flow Milli-fluidic Bioreactor | A cell culture system that allows independent perfusion of apical and basal channels, subjecting cells to physiological shear stress while enabling integrated TEER measurements [45]. |
| Ag/AgCl Electrodes | The standard electrode type for TEER, used in EVOM2 "chopstick" electrodes or for custom integration into bioreactors due to their stable and non-polarizable properties [3] [45]. |
| Collagen Type I Coating | A common extracellular matrix protein used to coat microfluidic channels and solid substrates (like HD-MEA chips) to promote endothelial cell adhesion and spreading [47]. |
| Csf1R-IN-6 | Csf1R-IN-6, MF:C20H18N8O3, MW:418.4 g/mol |
| 3CPLro-IN-1 | 3CPLro-IN-1, MF:C29H25NO3, MW:435.5 g/mol |
In the field of microfluidic platform modeling of vascular inflammation, the accurate assessment of barrier integrity is paramount. Transepithelial/transendothelial electrical resistance (TEER) serves as a gold-standard, quantitative technique for measuring the integrity of tight junction dynamics in endothelial and epithelial monolayers [3]. The reliability of TEER data, however, is highly dependent on the method used for electrical measurement. The integration of either two-point or four-point probe methods represents a critical methodological choice, with significant implications for minimizing measurement error and enhancing data accuracy. This application note details the principles, advantages, and limitations of both probe configurations. It provides structured experimental protocols tailored for researchers developing robust models for drug development and vascular inflammation studies, where sensitive and accurate barrier function assessment is essential.
Theoretical Foundations and Comparative Analysis
Fundamental Principles of Probe Configurations
The core difference between the two methods lies in the separation of current injection and voltage measurement functions.
Two-Point Probe Method: This configuration uses two electrodes to perform both current injection and voltage measurement simultaneously [49]. The measured resistance (Rmeasured) is the sum of the true sample resistance (Rsample) and the contact resistances (Rc1, Rc2) at the electrode-sample interfaces, such that Rmeasured = Rsample + Rc1 + Rc2 [50]. This introduces significant error, especially when the sample resistance is low.
Four-Point Probe Method: This system employs four distinct electrodes: the two outer electrodes act as current (or driving) electrodes for current injection, while the two inner electrodes function as voltage (or sensing) electrodes to determine the resulting potential [51]. A key advantage is that the voltage electrodes do not carry significant current, which effectively eliminates the influence of electrode polarization and contact impedance from the measurement [51] [49]. This allows for the determination of the absolute resistance value of the sample itself.
Quantitative Comparison and Error Analysis
The following table summarizes the key performance differences between the two methods, particularly in the context of biological and materials testing.
Table 1: Comparative Analysis of Two-Point and Four-Point Probe Methods
| Aspect | Two-Point Probe | Four-Point Probe |
|---|---|---|
| Measured Value | Total system resistance (sample + contact resistances) [50] | Absolute sample resistance [50] |
| Contact Resistance | Included in measurement, causing significant error [49] | Effectively eliminated from measurement [51] [49] |
| Typical Resistivity Trend | Higher measured values (Single probe > Two-point > Four-point) [50] | Lower, more accurate absolute values [50] |
| Ideal Use Case | Measuring high-resistance samples; assessing total through-thickness resistance [49] | Measuring low-resistance samples; determining intrinsic material resistivity [49] |
| Data Stability | Challenging for low-resistance samples due to contact noise [49] | High accuracy for low-resistance samples; requires high instrument precision [49] |
| Practical Application | Suitable for testing all types of battery electrodes and supercapacitors [49] | Can fail to distinguish coating influence on low-resistance foil-based electrodes [49] |
The choice of method is heavily influenced by the sample's electrical properties. For high-resistance samples, the contact resistance may be negligible compared to the sample resistance, making the two-point method acceptable. However, for low-resistance samples, such as many biological tissues or conductive foils, the contact resistance can constitute the majority of the measured signal, leading to substantial overestimation of the true sample resistance [50] [49]. The four-point probe method is superior in these scenarios as it directly measures the sample's resistance without the confounding effect of contact impedance [51].
Experimental Protocols for TEER Measurement
TEER Measurement Using Two-Point Probe ("Chopstick" Electrodes)
This protocol outlines the use of manual two-point probes, such as the widely used STX2 or STX4 electrodes, often coupled with an Epithelial Voltohmmeter (EVOM) [3] [52].
Materials:
- EVOM meter or equivalent (e.g., EVOM Auto for high-throughput) [52]
- STX2 or STX4 "chopstick" electrodes [52]
- Cell culture grown on a semipermeable membrane insert
- Sterile measurement solution (e.g., culture medium)
Procedure:
- Equipment Setup: Turn on the EVOM meter and allow it to warm up. Ensure the electrodes are clean and sterilized according to manufacturer guidelines to prevent biofilm formation or corrosion [52].
- Background Measurement: Aspirate the culture medium from the insert and surrounding well. Add a fresh, pre-warmed measurement solution to both the apical (inside insert) and basolateral (outside well) compartments. Position the electrodes: the longer electrode in the basolateral compartment and the shorter in the apical compartment, without touching the membrane. Measure and record the blank resistance (RBLANK) of the membrane and medium alone [3].
- Sample Measurement: Seed and culture cells on the membrane insert until a fully confluent monolayer is formed. On the measurement day, repeat Step 2 with the cell-seeded insert and record the total resistance (RTOTAL).
- Data Calculation: Calculate the cell-specific resistance (RTISSUE) and the final TEER value.
- RTISSUE (Ω) = RTOTAL - RBLANK
- TEER (Ω·cm²) = RTISSUE (Ω) × Membrane Area (cm²) [3]
- Considerations: Electrode placement is critical; inconsistent positioning between measurements introduces high variability. The system may overestimate TEER in large-diameter inserts due to non-uniform current density [3]. For higher throughput and reduced user variability, an automated system like the EVOM Auto is recommended [52].
TEER Measurement Using a Four-Electrode System
This protocol is modeled on integrated four-electrode systems, such as the ECIS TEER96 platform, which are designed for continuous, automated measurement within a cell culture incubator [53].
Materials:
- ECIS TEER96 station or equivalent four-electrode instrument [53]
- Specialized multi-well plates with integrated four-electrode arrays
- Cell suspension
Procedure:
- Instrument Initialization: Place the specialized measurement plate into the TEER96 station, which is housed inside a standard 37°C, 5% CO₂ incubator to maintain physiological conditions [53].
- Background Measurement: Add measurement medium or cell-free culture medium to the wells. The instrument automatically measures and stores the baseline background resistance for each well.
- Cell Seeding and Continuous Measurement: Seed cells directly onto the electrode-integrated plate to form a monolayer. The instrument can be programmed to take continuous, real-time TEER measurements at set intervals (e.g., every 10 minutes) without user intervention [53].
- Data Analysis: The instrument's software automatically subtracts the background resistance and calculates the TEER value in Ω·cm². The continuous data stream allows for the analysis of kinetic profiles, such as the formation of a monolayer over days or the rapid disruption of barrier integrity upon compound addition [53].
- Considerations: This method eliminates operator-dependent variability and provides high-resolution, temporal data. It is particularly useful for capturing transient changes in barrier function and for high-throughput screening applications [53].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for TEER and Vascular Inflammation Studies
| Item | Function/Application |
|---|---|
| EVOM Meter & STX/STX-HTS Electrodes [52] | A manual system for reliable two-point TEER measurement in standard well plate formats (e.g., 24-well). |
| EVOM Auto [52] | Automated two-point TEER system for high-throughput screening, eliminating user placement variability in 24- and 96-well formats. |
| ECIS TEER96 [53] | An automated platform for continuous, four-electrode TEER measurement of 96 samples simultaneously in a standard incubator. |
| OrganoPlate & OrganoTEER [20] [4] | A microfluidic organ-on-a-chip platform for 3D vessel culture, with a compatible TEER measurement apparatus for real-time, perfused barrier assessment. |
| Inflammatory Cytokines (TNF-α, INF-γ) [20] | Used to stimulate endothelial cells and induce a controlled inflammatory response, mimicking vascular inflammation in vitro. |
| Human Umbilical Vein Endothelial Cells (HUVECs) [20] [4] | A primary cell line commonly used to establish in vitro models of the vascular endothelium. |
| FITC-labeled Dextrans [32] | A fluorescent tracer for parallel validation of barrier integrity via macromolecular permeability assays. |
Method Selection and Workflow Integration
The decision-making process for integrating a probe method into a vascular inflammation study is critical. The following diagram outlines the logical workflow for method selection based on experimental goals and constraints.
The integration of two-point versus four-point probe methods presents a fundamental trade-off between practical convenience and measurement accuracy. The two-point probe, while versatile and cost-effective, is susceptible to error from contact resistance, making it less suitable for low-resistance endothelial barriers. The four-point probe excels in accuracy by eliminating this error and is ideal for sensitive, continuous monitoring and high-throughput applications. In the context of microfluidic modeling of vascular inflammation, where detecting subtle changes in barrier function is crucial, the four-point probe method offers a clear advantage. By aligning the measurement technology with the experimental requirements as outlined in this document, researchers can minimize error and generate more reliable, reproducible data for drug development research.
Within the field of microfluidic platform modeling of vascular inflammation, the measurement of Transendothelial Electrical Resistance (TEER) is a critical, non-invasive technique for quantifying endothelial barrier integrity [54] [55]. The reliability of this data is paramount, as TEER serves as a key indicator in studies of inflammatory conditions [1] [56], drug permeability [57] [54], and toxicology [58]. Achieving consistent and reproducible TEER measurements is not trivial, as they are susceptible to influence by a range of biological and technical factors. This application note details the roles of three fundamental variables—temperature, culture medium, and cell passage number—and provides validated protocols to control these factors in the context of vascular inflammation research.
The following table synthesizes the specific effects of and requirements for temperature, medium, and passage number to ensure experimental consistency.
Table 1: Key Factors Influencing TEER Measurements
| Factor | Quantitative/Qualitative Effect on TEER | Recommended Specification for Vascular Models |
|---|---|---|
| Temperature | TEER is highly sensitive to fluctuations; readings taken outside incubator conditions can rapidly decline [59]. | Maintain a stable 37°C during both culture and measurement. For measurements outside an incubator, use a warming plate or acclimate plates to room temperature for comparisons [59]. |
| Culture Medium | Variations in serum concentration, supplements, and pH can modulate tight junction formation and affect TEER values [59]. The type and temperature of the electrolyte solution impact measured resistance [58]. | Use a consistent, pre-warmed medium formulation (e.g., EGM-2 for HUVECs [1] [60]). Report the full composition, including serum and supplement batches [58]. |
| Cell Passage Number | The passage number of cells is a known factor that can influence TEER levels [54] [61]. Using high-passage cells can lead to inconsistent barrier properties. | Use cells within a validated, low-passage range (e.g., HUVECs at passage 5-10 [60]). Strictly document the passage number used in all experiments [58]. |
Detailed Experimental Protocols
Protocol for Controlling Temperature During TEER Measurement
Principle: TEER is a temperature-sensitive measurement, and ionic conductance of the medium and cell membrane properties change with temperature. Uncontrolled temperature is a significant source of experimental variability [59].
Materials:
- TEER measurement system (e.g., EVOM2 with electrodes or an integrated platform like the OrganoPlate [1] [60])
- Cell culture platform (e.g., microfluidic chip, Transwell insert)
- Humidified CO₂ incubator at 37°C
- Pre-warmed culture medium
- Temperature-controlled warming plate (optional)
Procedure:
- Pre-equilibration: Prior to measurement, ensure all reagents are stable. Pre-warm the culture medium to 37°C in a water bath.
- In-Incubator Measurement (Preferred):
- If using a system designed for continuous monitoring inside an incubator (e.g., [1]), perform TEER measurements without moving the cell culture.
- This provides the most stable environment, minimizing thermal stress to the cells.
- Ex-Situ Measurement (With Precautions):
- If measurements must be performed outside the incubator, work efficiently to minimize time outside a controlled environment.
- Option A (Warming Plate): Place the cell culture platform on a warming plate set to 37°C during the measurement procedure [59].
- Option B (Room Temperature Acclimation): For comparative studies where absolute TEER is less critical than relative changes, acclimate all samples and reagents to a consistent room temperature before measuring [59]. Record the room temperature.
- Measurement: Perform the TEER measurement according to the manufacturer's instructions, ensuring the electrodes are sterile and properly positioned.
- Return to Incubator: Immediately after measurement, return the cell culture to the 37°C, 5% CO₂ incubator.
Protocol for Standardizing Medium and Reagents
Principle: The composition and physical properties of the culture medium and electrolyte solutions directly impact cell health and the conductivity of the solution, thereby influencing TEER readings [59] [58].
Materials:
- Standardized cell culture medium (e.g., EGM-2 for HUVECs) [1]
- Serum and supplement batches with documented lot numbers
- Phosphate-Buffered Saline (PBS) or other standardized electrolyte solution
Procedure:
- Medium Preparation:
- Use a single, validated lot of culture medium, serum, and all supplements for an entire study or series of experiments.
- Prepare medium aseptically and store it according to the manufacturer's recommendations. Avoid repeated freezing and thawing of supplements.
- Pre-Measurement Handling:
- For TEER measurement, the medium in the cell culture system itself often serves as the electrolyte.
- If the medium is changed immediately before a measurement, use pre-warmed (37°C) medium to avoid thermal shock.
- Document the exact medium formulation used in all experimental reports [58].
- Blank Resistance Measurement:
- Before seeding cells, measure the resistance of the culture system (e.g., membrane + medium) to establish a blank resistance value (
R_blank). - Perform this blank measurement with the same medium and at the same temperature used for subsequent biological measurements.
- The true TEER is calculated as:
TEER = (R_total - R_blank) × Membrane Area[55].
- Before seeding cells, measure the resistance of the culture system (e.g., membrane + medium) to establish a blank resistance value (
Protocol for Managing Cell Passage Number
Principle: As cells undergo repeated passaging, their genetic and phenotypic characteristics can drift, leading to reduced capacity to form robust, consistent barrier layers [54] [61].
Materials:
- Cryopreserved stock of low-passage cells (e.g., HUVECs, Lonza)
- Standard cell culture reagents for passaging (e.g., trypsin-EDTA, trypsin neutralizer)
- Culture flasks/plates
Procedure:
- Cell Sourcing and Bank Preparation:
- Obtain cells from a reputable source and create a large, master bank of low-passage cryopreserved vials (e.g., HUVECs frozen at passage 5 [1]).
- Use a working cell bank derived from the master bank to ensure a consistent supply of low-passage cells.
- Defining a Valid Passage Range:
- Prior to experimentation, validate the barrier-forming capability of your specific cell line across a range of passages.
- Establish a maximum passage number for use in experiments. For example, multiple protocols use HUVECs within passages 5-10 [60].
- Documentation and Tracking:
- Meticulously record the passage number for every experiment.
- In publications and internal reports, explicitly state the passage number range of the cells used, as this is a critical detail for reproducibility [58].
Signaling Pathways and Experimental Workflow
The following diagram illustrates the logical relationship between the three key factors, the cellular responses they influence, and the ultimate TEER outcome.
Logical Workflow of Key TEER Factors
The Scientist's Toolkit: Essential Research Reagents & Materials
This table provides a curated list of essential materials used in the featured vascular inflammation-on-a-chip studies for reliable TEER measurement.
Table 2: Research Reagent Solutions for Vascular TEER Models
| Item | Function/Application | Example Products / Cell Lines |
|---|---|---|
| Endothelial Cells | Forms the vascular barrier in the model. | HUVECs (Lonza) [1]; hCMEC/D3 (for BBB models) [60] |
| Cell Culture Medium | Provides nutrients and specific signaling cues to maintain cell health and phenotype. | EGM-2 Medium (Lonza) [1] [60] |
| Microfluidic Platform | Provides a perfusable, physiologically relevant 3D microenvironment for tubule formation and shear stress application. | OrganoPlate (Mimetas) [1] [9] |
| TEER Measurement Instrument | Device for applying current and measuring voltage to calculate resistance. | EVOM2 (WPI) [59] [60]; Custom integrated systems [1] [56] |
| Inflammatory Stimuli | Used to experimentally induce endothelial dysfunction and model vascular inflammation. | TNF-α, INF-γ [1]; Peripheral Blood Mononuclear Cells (PBMCs) [1] |
| Junctional Staining Markers | Endpoint validation of barrier integrity via immunofluorescence. | Antibodies against VE-Cadherin, ICAM, ZO-1 [1] [60] |
In conclusion, rigorous control of temperature, culture medium, and cell passage number is non-negotiable for generating robust and reproducible TEER data in vascular inflammation models. By adhering to the detailed protocols and recommendations outlined in this application note, researchers can minimize technical variability, thereby ensuring that observed changes in endothelial barrier integrity accurately reflect the biological effects of their experimental conditions.
Transendothelial/epithelial electrical resistance (TEER) is a gold-standard, non-invasive technique for quantifying the integrity and barrier function of cellular layers in vitro [20]. However, a significant technical challenge in the field is that in vitro models of endothelial barriers typically show much lower TEER values than other epithelial models [20]. This inherent difference in signal strength necessitates specialized approaches for measurement setup, instrumentation sensitivity, and data interpretation when working with vascular models. This Application Note details the specific considerations and protocols required for obtaining reliable TEER measurements from endothelial barriers, with a focus on microfluidic platforms modeling vascular inflammation.
Quantitative Differences: Endothelial vs. Epithelial Barrier Resistance
The core challenge in endothelial TEER measurement stems from the fundamental physiological differences between endothelial and epithelial tissues. Endothelial barriers in vivo are more permeable than many epithelial barriers (e.g., intestinal, pulmonary), and this characteristic is reflected in their lower electrical resistance [24]. The table below summarizes the typical TEER value ranges for various barrier types.
Table 1: Typical TEER Value Ranges for Different Barrier Types In Vitro
| Barrier Type | Typical TEER Range | Context and Measurement Platform |
|---|---|---|
| Endothelial Barriers | ~5-10 Ω·cm² | Human Primary Renal Proximal Tubule Epithelial Cells (hRPTEC) in co-culture within the PREDICT96 microfluidic system [27]. |
| Endothelial Barriers | "Much lower" than epithelial | General observation for in vitro endothelial models compared to epithelial models [20]. |
| Kidney Proximal Tubule (in vivo-like, leaky) | ~5-10 Ω·cm² | Primary cell-based model in a high-throughput microfluidic system [27]. |
| Blood-Brain Barrier (BBB) on a chip | 30-fold increase over static model | A dynamic 3D BBB model demonstrating effective barrier formation [62]. |
These quantitative differences highlight a critical consideration: instruments used for TEER measurements of endothelial barriers require a significant increase in sensitivity compared to those used for high-resistance epithelial models [20].
Experimental Protocol: TEER Measurement in a Vascular Inflammation Model
This protocol details the methodology for culturing endothelial tubules and performing continuous, high-sensitivity TEER measurements to study vascular inflammation, based on the platform described by M. D. B. et al. [20].
Materials and Reagents
Table 2: Research Reagent Solutions for Endothelial TEER Studies
| Item | Function / Application | Example & Specifications |
|---|---|---|
| Microfluidic Platform | Provides a scalable, automation-compatible platform for perfused 3D cell culture. | OrganoPlate 3-lane 64 (Mimetas B.V.); 64 chips in a 384-well plate format [20]. |
| TEER Measurement Apparatus | Enables long-term, sensitive TEER measurements for low-resistance endothelial barriers. | OrganoTEER system, commercially available and compatible with OrganoPlate models [20]. |
| Endothelial Cells | Forms the vascular tubule barrier. | Human Umbilical Vein Endothelial Cells (HUVECs), e.g., from Lonza (C2519AS) [20]. |
| Endothelial Cell Medium | Supports growth and maintenance of endothelial cells. | EGM-2 medium (Lonza, CC-3162) [20]. |
| Inflammatory Cytokines | Induces endothelial activation and barrier dysfunction. | Tumor Necrosis Factor-alpha (TNF-α) and Interferon-gamma (IFN-γ) [20]. |
| Immune Cells | Used to study transendothelial migration and its impact on barrier function. | Human Peripheral Blood Mononuclear Cells (PBMCs) [20]. |
| Extracellular Matrix (ECM) | Provides a 3D scaffold for cell culture and tubule formation. | Fibril-based collagen or other hydrogel (e.g., Corning Matrigel) [20]. |
| Cell Tracking Dye | Labels immune cells for visualization during migration assays. | CellTracker Orange CMRA (Invitrogen, C34551) [20]. |
Step-by-Step Workflow
The following diagram illustrates the key experimental steps for setting up and conducting TEER measurements in a microfluidic model of vascular inflammation.
Step 1: Device Preparation Ensure the microfluidic plate (e.g., OrganoPlate) is sterile. Prior to cell seeding, coat the vascular channels with an appropriate adhesion factor, such as Matrigel, by pipetting the solution into the channels and incubating [20] [63].
Step 2: Extracellular Matrix (ECM) Loading Load a fibril-based ECM hydrogel (e.g., collagen) into the designated gel channel of the microfluidic device. The ECM will act as a scaffold and the abluminal surface for the endothelial tubule [20].
Step 3: Endothelial Cell Seeding and Tubule Formation
- Detach and resuspend endothelial cells (e.g., HUVECs) at a high density (e.g., 2.5 million cells/ml) in complete medium [63].
- Introduce the cell suspension into the perfusion channel of the device. Tilting the plate allows the suspension to fill the channel.
- Incubate the plate statically to allow cells to adhere to the ECM-glass phase and form a confluent monolayer, typically overnight [20].
- Apply continuous flow using a rocker system or pump to mature the tubule and condition it under physiological shear stress.
Step 4: Baseline TEER Measurement Once a stable, confluent endothelial barrier is formed (typically after 2-5 days of culture), measure the baseline TEER value using a sensitive TEER instrument (e.g., OrganoTEER). This value serves as the internal control for each tubule (Day 0) [20] [27].
Step 5: Experimental Intervention Induce vascular inflammation by introducing inflammatory stimuli into the medium perfusing the endothelial tubule. This can include:
- Cytokine Challenge: Add pro-inflammatory cytokines such as TNF-α (e.g., 10-100 ng/mL) and IFN-γ (e.g., 10-100 ng/mL) [20].
- Immune Cell Recruitment: Add fluorescently labeled PBMCs to the perfusion medium to study their adhesion and migration under inflammatory conditions [20].
Step 6: Continuous TEER Monitoring Place the microfluidic plate in the TEER measurement apparatus inside the incubator for long-term, continuous monitoring. Measure TEER at regular intervals (e.g., every few hours or daily) over the course of the experiment (e.g., 24-72 hours post-intervention) [20].
Step 7: Endpoint Analysis Correlate TEER data with other readouts:
- Immunofluorescence: Fix and stain for proteins like VE-Cadherin and ICAM-1 to visualize junctional integrity and endothelial activation [20].
- Imaging: Use phase-contrast or confocal microscopy to assess cell morphology and immune cell migration [20] [24].
Data Interpretation and Troubleshooting
- Understanding Low Values: Recognize that a "low" TEER value (e.g., 5-10 Ω·cm²) can represent a confluent and functional, but physiologically permeable, endothelial barrier, as seen in kidney proximal tubule models [27].
- Signal Sensitivity: Ensure the measurement system is calibrated for low-resistance tissues. Even small, sub-confluent gaps (0.4%) can cause an ~80% drop in measured TEER, which a sensitive system must detect [64].
- Geometry Matters: Be aware that TEER values obtained in microfluidic systems are not directly comparable to those from Transwell systems due to profound differences in device geometry, which affects the current path and field [64].
- Early Indicator: In toxicity or inflammation studies, a decrease in TEER can be an early indicator of barrier disruption, detectable before a significant increase in cell death markers like LDH [27].
Successful TEER measurement for endothelial barriers in vascular inflammation models hinges on acknowledging and addressing their inherently low signal. This requires a combination of a high-sensitivity measurement platform, a physiologically relevant microfluidic culture system, and careful data interpretation that considers the biological context of a dynamic, permeable endothelium. The protocols outlined herein provide a robust framework for researchers to reliably quantify and interrogate endothelial barrier function in health and disease.
Transepithelial/transendothelial electrical resistance (TEER) is a quantitative, non-invasive technique used to assess the integrity of cellular barriers in vitro, a critical parameter in microfluidic models of vascular inflammation [54] [14]. The electrical resistance across a cellular monolayer serves as a strong indicator of tight junction dynamics, which are central to barrier function [54]. In the context of vascular inflammation, pro-inflammatory cytokines such as TNFα and INF-γ are known to disrupt endothelial junctions, leading to increased vascular permeability, a hallmark of chronic inflammation [1]. Accurate TEER measurement is therefore paramount, as it allows researchers to quantify this disruption and screen potential therapeutic compounds in real-time. However, obtaining accurate and comparable TEER values requires two essential data integrity procedures: subtracting the background electrical resistance of the system itself and normalizing the measured resistance to the effective surface area of the barrier [14]. This application note provides detailed protocols and guidelines for performing these critical calculations to ensure robust and reliable data in vascular inflammation research.
Theoretical Foundations
The Electrical Circuit Model of an Endothelial Barrier
In a TEER measurement system, the electrical current passing through a cellular barrier can take two primary pathways: the paracellular route (between cells, regulated by tight junctions) and the transcellular route (through the cells) [14]. The simplified equivalent circuit model consists of these two resistance pathways in parallel. Due to the high resistance of cell membranes, the applied alternating current (AC) predominantly flows through the paracellular route, making the measured total resistance a close approximation of the paracellular resistance, which is directly influenced by tight junction integrity [14]. The total resistance (Rtotal) is thus governed by the resistance through the transcellular pathway (Rtc) and the paracellular pathway (Rpc), as defined by the formula: 1/Rtotal = 1/Rtc + 1/Rpc [14].
The Imperative for Blank Subtraction and Area Normalization
The raw resistance value (Rtotal) obtained from a TEER measurement is not solely attributable to the cellular barrier. It is a sum of resistances from multiple components, including the culture medium, the porous membrane on which the cells grow, and the electrode-medium interfaces [14]. To isolate the resistance specific to the cell layer (Rcells), the system resistance must be measured without cells present; this is the "blank" resistance (Rblank). The fundamental calculation for obtaining the cellular resistance is: Rcells = Rtotal - Rblank [14].
Furthermore, the measured Rcells is inversely proportional to the surface area of the monolayer. A larger area provides more parallel paths for current to flow, resulting in a lower overall resistance [14]. To compare TEER values across different experimental setups, platforms, or laboratories, the resistance must be normalized to the effective membrane surface area using the formula: TEER (Ω·cm²) = Rcells (Ω) × Membrane Area (cm²) [14]. Reporting TEER in the standardized unit of Ω·cm² is a critical convention that enables meaningful comparison of data.
Core Calculations and Data Presentation
Table 1: Core Formulas for Calculating Area-Normalized TEER.
| Calculation Step | Formula | Variables and Units | Application Note |
|---|---|---|---|
| 1. Blank Subtraction | Rcells = Rtotal - Rblank | Rcells: Cell layer resistance (Ω)Rtotal: Measured resistance with cells (Ω)Rblank: Measured resistance without cells (Ω) | An Rblank measurement must be performed for each unique device, medium, and condition. |
| 2. Area Normalization | TEER = Rcells × A | TEER: Area-normalized resistance (Ω·cm²)Rcells: Cell layer resistance (Ω)A: Membrane/growth surface area (cm²) | The growth area (A) is a fixed design parameter of the microfluidic device or Transwell insert. |
Workflow for Accurate TEER Data Acquisition
The following workflow diagrams the essential steps for obtaining a single, validated TEER measurement, from experimental setup through to final calculation.
Exemplar TEER Data in Vascular Inflammation Models
To contextualize expected values, the table below presents illustrative TEER data from vascular-related studies, demonstrating the application of these calculations.
Table 2: Exemplar TEER Values from Barrier Integrity Studies.
| Cell Type/Model | Platform | Typical Baseline TEER (Ω·cm²) | Post-Inflammatory Challenge (e.g., TNFα) | Key Reference |
|---|---|---|---|---|
| HUVEC Tubules | OrganoPlate (3-lane 64) | Not explicitly quantified | Significant decrease observed | [1] |
| Kidney Proximal Tubule (Co-culture) | PREDICT96 | 5 - 10 Ω·cm² | N/A (Model used for nephrotoxicity) | [27] |
| hMVEC (Microvascular, Co-culture) | PREDICT96 | 5 - 10 Ω·cm² | N/A (Model used for nephrotoxicity) | [27] |
Detailed Experimental Protocols
Protocol 1: Measuring Blank Resistance (Rblank)
Purpose: To determine the baseline electrical resistance of the experimental system without a cellular monolayer, which will be subtracted from future measurements to isolate the contribution of the cells.
Materials:
- Microfluidic device (e.g., PREDICT96, OrganoPlate) or Transwell insert
- Culture medium identical to that used for cell culture
- TEER measurement system (e.g., EVOM2, Millicell ERS, or integrated electrodes with impedance spectrometer)
Procedure:
- System Assembly: Assemble the microfluidic device or prepare the Transwell insert exactly as it would be for cell culture, ensuring all channels are properly connected and free of air bubbles.
- Introduce Medium: Fill the apical and basolateral compartments (or top and bottom channels) with the appropriate culture medium. Ensure that the fluid levels are correct and that the membrane is fully submerged.
- Equilibration: Place the entire system in the incubator (37°C, 5% CO₂) for at least 15-30 minutes to allow the medium to equilibrate in terms of temperature, pH, and gas concentration. Temperature is a critical factor affecting resistance.
- Measurement:
- Connect the electrodes to the TEER meter, ensuring they are sterile if they will contact the medium for subsequent cell culture.
- Carefully place the electrodes into their respective compartments, ensuring they are fully immersed but not touching the membrane.
- Record the stable resistance value. This is Rblank.
- Replication: Repeat this measurement for at least n=3 independent device/insert setups to establish a reliable average Rblank value. This protocol should be repeated for every new batch of medium or device type.
Protocol 2: Calculating Area-Normalized TEER for a Confluent Monolayer
Purpose: To accurately calculate the area-normalized TEER value of a confluent endothelial monolayer, reflecting its barrier integrity.
Materials:
- Confluent endothelial cell monolayer (e.g., HUVEC) grown in the system.
- TEER measurement system.
- Pre-determined Rblank value and membrane surface area (A).
Procedure:
- Preparation: Follow Steps 1-3 from Protocol 1 using the cell-cultured device. Handle the system aseptically to maintain sterility for long-term studies.
- Measure Rtotal:
- With the electrodes correctly positioned, take the resistance measurement.
- For increased accuracy, take multiple readings over a short period and use the average value. This is Rtotal.
- Calculate Rcells:
- Subtract the average Rblank from the measured Rtotal.
- Data Integrity Check: If the result is zero or negative, the measurement is invalid. Investigate potential causes such as non-confluent monolayers, damaged electrodes, or incorrect Rblank values.
- Area Normalization:
- Multiply Rcells by the growth surface area (A) of the membrane.
- Example: If Rcells is 50 Ω and the membrane area is 0.33 cm², then TEER = 50 Ω × 0.33 cm² = 16.5 Ω·cm².
- Documentation: Report the final value as TEER in Ω·cm². Always include the Rblank value and membrane area in the methodology section of any report or publication to ensure reproducibility.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for TEER Measurements.
| Item | Specification/Example | Critical Function in TEER Assay |
|---|---|---|
| Microfluidic Platform | PREDICT96, OrganoPlate 3-lane 64 | Provides a high-throughput, perfusable environment with integrated electrodes or compatibility with TEER measurement, enabling physiologically relevant shear stress [1] [27]. |
| TEER Measurement Instrument | EVOM2 (WPI), Millicell ERS (Millipore), CellZscope | Applies a low-amplitude AC signal and measures voltage/current to calculate resistance. Systems like CellZscope use impedance spectroscopy for more robust data [54] [14]. |
| Electrodes | Ag/AgCl "Chopstick" Electrodes, Integrated Silver Electrodes | Serve as the interface for applying current and measuring voltage. Ag/AgCl provides a stable, non-polarizable interface, minimizing measurement drift [14]. |
| Cell Culture Medium | EGM-2 for HUVECs, OrganoMedium HUVEC-BM | Provides nutrients and essential factors for cell growth and maintenance of barrier function. Consistency is key to avoid TEER fluctuations [1] [54]. |
| Inflammatory Stimuli | Recombinant Human TNFα, INF-γ | Used to experimentally induce endothelial activation and disrupt tight junctions, modeling vascular inflammation and enabling the study of barrier breakdown [1]. |
Advanced Considerations for Microfluidic Systems
Implementing TEER in microfluidic Body-on-a-Chip devices presents unique challenges. The geometry of microfluidic channels can lead to a non-uniform current distribution, potentially causing an overestimation of the cellular resistance if not properly accounted for during system design [14]. To mitigate this, devices can be engineered with multiple electrodes. A four-point probe method, which separates current-passing and voltage-sensing electrodes, eliminates the contribution of contact and lead resistances, providing a more accurate measurement [14]. Furthermore, an advanced technique involves integrating two pairs of electrodes on the same side of the membrane. By measuring and subtracting the resistance between electrodes on the same side, the system can automatically correct for the background resistance of the medium, a method known as "on-device subtraction" [14]. For the highest data integrity, electrochemical impedance spectroscopy (EIS) is recommended over single-frequency measurements. EIS measures impedance across a spectrum of frequencies, allowing for the fitting of a more detailed electrical circuit model. This separates the resistive component of the cell layer from the capacitive components of the cell membranes, yielding a more accurate and biologically informative TEER value [16].
Validating Chip Performance and Comparing TEER with Complementary Assays
Within vascular inflammation research, assessing the integrity of the endothelial barrier is paramount. Transendothelial Electrical Resistance (TEER) serves as a functional, real-time measure of barrier integrity, where decreasing TEER values indicate increased permeability. These functional changes are biologically rooted in the molecular reorganization of endothelial junctions and the upregulation of adhesion molecules. Specifically, the expression of VE-Cadherin, a key protein in adherens junctions, and ICAM-1, an inducible adhesion molecule, are critical biological endpoints that correlate strongly with TEER measurements. This application note details protocols and data for modeling vascular inflammation in a high-throughput microfluidic platform, establishing a direct correlation between TEER and the expression of ICAM and VE-Cadherin.
Data Correlation: TEER, ICAM, and VE-Cadherin
The following tables summarize key quantitative and qualitative findings from vascular inflammation models, demonstrating the consistent inverse relationship between barrier function (TEER) and the expression of ICAM-1 and VE-Cadherin.
Table 1: Quantitative and Qualitative Correlations in Inflammatory Models
| Induction Method | Effect on TEER | Effect on ICAM-1 | Effect on VE-Cadherin | Key Findings |
|---|---|---|---|---|
| TNFα & IFN-γ (Cytokines) [1] [20] | ↓ Decrease (dose- and time-dependent) | ↑ Increase (expression) | ↓ Destabilization; Fragmented membrane distribution | - Barrier disruption quantified by continuous TEER. [1]- Correlated with increased immune cell adhesion/migration. [1] |
| PBMC Addition [1] [20] | ↓ Decrease | ↑ Increase (expression) | ↓ Changes in morphology & staining | - Combines functional permeability (TEER) with immune cell interaction. [1] |
| ICAM-1 Overexpression [65] | ↓ Decrease (independent of junction changes at mod. levels) | N/A | Unchanged at moderate levels | - ICAM-1 expression alone can reduce TEER. [65]- Higher levels alter cytoskeleton and junctions. [65] |
| EZH2 Knockdown [66] | ↑ Increased barrier stability | Not Reported | ↑ Increased expression | - H3K27me3 silences VE-cadherin (CDH5). [66]- Reducing this silencing improves barrier. [66] |
| Cortactin (Cttn) Knock-Out [67] | ↓ Impaired basal barrier function | Not Reported | ↓ Fragmented membrane distribution | - Cttn is part of the VE-cadherin complex. [67]- Its absence slows barrier recovery. [67] |
Table 2: Key Signaling Mediators in Endothelial Barrier Dysfunction
| Signaling Molecule / Pathway | Effect on Barrier | Proposed Mechanism |
|---|---|---|
| TGF-β [68] | Disrupts Barrier | Induces Endothelial-to-Mesenchymal Transition (EndMT), leading to loss of endothelial markers (VE-Cadherin) and gain of mesenchymal markers. [68] |
| Rho-ROCK [68] [65] | Disrupts Barrier | Mediates cytoskeletal stress fiber formation and increased F/G-actin ratios, downstream of TGF-β and high ICAM-1 expression. [68] [65] |
| cAMP-Rap1/Rac1 [67] | Stabilizes Barrier | Promotes cortical actin formation and stable adherens junctions; requires Cortactin for efficient activation. [67] |
| NF-κB [65] | Disrupts Barrier | Key transcription factor for ICAM-1 induction; inhibition blocks TNF-induced ICAM-1 expression and TEER reduction. [65] |
The relationships between these key components in vascular inflammation can be visualized in the following pathway diagram.
Figure 1: Signaling Pathways in Endothelial Barrier Regulation. Pro-inflammatory stimuli trigger pathways that disrupt junctions and reduce TEER, while the cAMP pathway promotes barrier stability.
Experimental Protocols
Protocol 1: Vascular Inflammation-on-a-Chip with Real-Time TEER
This protocol outlines the process for modeling vascular inflammation and simultaneously measuring barrier integrity in a high-throughput microfluidic platform [1] [20].
Workflow Overview:
Figure 2: Experimental Workflow for Vascular Inflammation-on-a-Chip. The process involves preparing the microfluidic chip, establishing endothelial tubules under perfusion, applying inflammatory stimuli, and performing continuous and endpoint measurements.
Materials:
- Microfluidic Platform: OrganoPlate 3-lane 64 (Mimetas B.V., MI-OR-BV-02) [1] [9].
- Cells: Human Umbilical Vein Endothelial Cells (HUVECs), e.g., Lonza, C2519AS [1] [20].
- Culture Medium: EGM-2 medium (Lonza, CC-3162) [1] [20].
- Inflammatory Agents:
- TEER Measurement System: OrganoTEER device, compatible with the OrganoPlate 3-lane 64 [1] [9].
Step-by-Step Procedure:
- Chip Preparation: Use ready-to-use OrganoReady Blood Vessel HUVEC 3-lane 64 plates. On the day of receipt, change the medium to OrganoMedium HUVEC-BM [1].
- Perfusion Establishment: Place the plate on an OrganoFlow rocker set at a 14-degree angle with 8-minute intervals to establish perfusion flow through the endothelial tubules [1].
- Baseline TEER: Before applying any inflammatory triggers, measure the baseline TEER for all 64 chips using the OrganoTEER device placed inside the incubator [1].
- Inflammatory Challenge:
- Cytokine Model: Add Titration curves of TNFα and IFN-γ to the perfusion medium. A typical concentration range is 1-100 ng/mL for each [1].
- Immune Cell Model: Isolate and label PBMCs with a fluorescent dye (e.g., CellTracker Orange CMRA). Add PBMCs (e.g., at a concentration of 400,000 cells/mL) to the endothelial tubules [1] [20].
- Continuous TEER Monitoring: Keep the plate on the rocker and in the incubator, performing automatic, continuous TEER measurements for the duration of the experiment (e.g., 48 hours) [1].
- Endpoint Immunofluorescence: Following TEER measurements, fix the cells and perform immunofluorescence staining for ICAM and VE-cadherin.
- Fix with 4% paraformaldehyde for 15-20 minutes.
- Permeabilize and block with a solution containing 0.1% Triton X-100 and 1-5% BSA.
- Incubate with primary antibodies: mouse anti-VE-cadherin and rabbit anti-ICAM-1.
- Incubate with fluorescently labeled secondary antibodies (e.g., Alexa Fluor 488 and 647).
- Image using a high-content or confocal microscope compatible with the OrganoPlate [1] [20].
Protocol 2: ICAM-1 and VE-Cadherin Analysis via Immunofluorescence and Image Analysis
This protocol details the specific steps for analyzing junctional integrity and adhesion molecule expression.
Materials:
- Primary Antibodies: Anti-VE-cadherin, Anti-ICAM-1, Anti-β-catenin, Anti-ZO-1 [1] [67].
- Secondary Antibodies: Fluorescently conjugated antibodies (e.g., Alexa Fluor series).
- Mounting Medium: with DAPI for nuclear counterstaining.
- Imaging: High-content imaging system or confocal microscope.
Procedure:
- After the experimental time course, fix the cells in the OrganoPlate as described in Protocol 1, Step 6.
- Carry out the immunofluorescence staining protocol.
- Acquire high-resolution z-stack images of the endothelial tubules for each condition.
- Image Analysis:
- VE-Cadherin Junction Analysis: Quantify the continuity of VE-cadherin staining at cell-cell junctions. Calculate a "junctional fragmentation index" by measuring the ratio of discontinuous (fragmented) junctions to the total junction length in the image [67]. A higher index indicates greater barrier disruption.
- ICAM-1 Expression Analysis: Measure the mean fluorescence intensity of ICAM-1 staining per cell or per unit area. Normalize this value to the control condition to determine fold-increase in expression [1].
- Co-localization Analysis: If using multiple markers, perform co-localization analysis (e.g., for VE-cadherin and β-catenin) to assess complex integrity [67].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for Vascular Inflammation Models
| Item | Function / Application | Example Product / Source |
|---|---|---|
| OrganoPlate 3-lane 64 | High-throughput microfluidic platform for 3D perfused vessel culture. | Mimetas B.V. (MI-OR-BV-02) [1] |
| OrganoTEER | Automated instrument for continuous, parallel TEER measurements in OrganoPlates. | Mimetas B.V./Sciospec GmbH [1] [20] |
| HUVECs | Primary human endothelial cells for constructing the vascular model. | Lonza (C2519AS) [1] [20] |
| Recombinant TNFα & IFN-γ | Pro-inflammatory cytokines to induce endothelial activation and barrier disruption. | Various commercial suppliers (e.g., PeproTech, R&D Systems) |
| Anti-VE-cadherin Antibody | Immunofluorescence staining of adherens junctions; marker for barrier integrity. | Various commercial suppliers [1] [67] |
| Anti-ICAM-1 Antibody | Immunofluorescence staining of induced adhesion molecule; marker for activation. | Various commercial suppliers [1] [65] |
| CellTracker Dyes | Fluorescent labeling of PBMCs for tracking immune cell adhesion and migration. | e.g., CellTracker Orange CMRA (Invitrogen) [1] [20] |
| Rocking Platform | Generates perfusion flow in the OrganoPlate microchannels. | OrganoFlow (Mimetas B.V.) [1] |
1 Introduction In vascular inflammation research, accurately assessing endothelial barrier integrity is paramount. Two principal techniques employed for this purpose are Transepithelial/Transendothelial Electrical Resistance (TEER) and fluorescent dextran permeability assays. TEER measures the ionic conductance across the paracellular pathway, serving as a sensitive, real-time indicator of tight junction dynamics [3]. In contrast, fluorescent dextran assays quantify the physical passage of molecules, typically fluorescein isothiocyanate (FITC)-labeled dextrans, across the cellular monolayer, providing a direct measure of macromolecular permeability [69] [70]. Within microfluidic platforms modeling vascular inflammation, integrating these complementary methods offers a robust framework for evaluating barrier function, enabling researchers to dissect the effects of inflammatory mediators and potential therapeutics with high resolution and physiological relevance [20] [71]. This application note details the protocols, comparative analysis, and practical integration of these techniques in a vascular inflammation-on-a-chip context.
2 Principle and Comparison of Assays TEER and fluorescent dextran permeability assays measure distinct but complementary aspects of cellular barrier function.
2.1 TEER Measurement Principle TEER is a quantitative technique that measures the electrical resistance across a cellular monolayer, reflecting the integrity of tight junctions. The resistance is inversely proportional to the ionic permeability of the paracellular pathway [3] [72]. In practice, an alternating current (AC) voltage is applied via electrodes placed on the apical and basolateral sides of the monolayer. The resulting current is measured, and the resistance is calculated using Ohm's law (R = V/I). The cell-specific resistance (RTISSUE) is obtained by subtracting the blank resistance of the membrane support (RBLANK) from the total measured resistance (RTOTAL). This value is then multiplied by the effective surface area of the membrane (MAREA) to report TEER in the standardized unit of Ω·cm² [3]:
TEERREPORTED = (RTOTAL - RBLANK) × MAREA
2.2 Fluorescent Dextran Assay Principle The fluorescent dextran permeability assay directly tracks the flux of a macromolecular tracer across the cellular barrier. FITC-dextran is a commonly used, membrane-impermeant polysaccharide conjugate that is biologically inert and available in a range of molecular weights (e.g., 4 kDa, 40 kDa, 70 kDa) [69] [70] [73]. The tracer is added to the donor compartment (e.g., the apical side for vascular models), and its appearance in the acceptor compartment (e.g., the basolateral side) is quantified over time using a fluorometer. The permeability coefficient (Papp) is calculated from the flux rate, providing a direct measure of paracellular solute leakage [70].
2.3 Comparative Strengths and Limitations The following table summarizes the core characteristics of each method for easy comparison.
Table 1: Key comparisons between TEER and fluorescent dextran permeability assays
| Feature | TEER Assay | Fluorescent Dextran Assay |
|---|---|---|
| Parameter Measured | Ionic permeability via electrical resistance [3] | Macromolecular permeability via tracer flux [70] |
| Key Output | Resistance (Ω·cm²) | Permeability Coefficient (Papp, cm/s) [70] |
| Temporal Resolution | Real-time, continuous monitoring [72] | Endpoint or time-point measurements [70] |
| Invasiveness | Non-invasive, permits repeated measures on same sample [3] [72] | Invasive, often requires sample collection/destruction [3] |
| Throughput | High, especially with automated systems [20] | Moderate, can be multiplexed but typically lower throughput |
| Information Provided | Integrity of tight junctions and cell membranes [74] | Functional pore size and solute passage [3] |
| Key Limitations | Does not directly quantify macromolecule transport [72] | Does not provide real-time kinetics on barrier tightness [3] |
3 Integrated Experimental Workflow for Vascular Inflammation Models The following diagram outlines a synergistic workflow for implementing both assays in a microfluidic vascular inflammation study, such as in the OrganoPlate platform [20].
4 Detailed Protocols 4.1 Protocol for Real-Time TEER Measurement in a Microfluidic Platform This protocol is adapted for systems like the OrganoPlate, compatible with an automated TEER measurement device (OrganoTEER) [20] [4].
Key Materials:
- OrganoPlate 3-lane 64 (or similar microfluidic platform)
- Human Umbilical Vein Endothelial Cells (HUVECs)
- OrganoTEER or equivalent automated TEER measurement station
- Cell culture incubator (37°C, 5% CO₂)
- EGM-2 culture medium
Procedure:
- Chip Seeding and Culture: Seed HUVECs into the appropriate channel of the OrganoPlate according to the manufacturer's instructions. Culture the cells under perfusion if applicable until a confluent monolayer is formed, typically requiring 3-5 days [20].
- System Calibration: Prior to measurements, calibrate the TEER instrument according to the manufacturer's guidelines. Acquire a baseline resistance measurement from a cell-free chip (RBLANK) to account for the system's background resistance [3].
- TEER Measurement:
- Place the OrganoPlate into the pre-warmed (37°C) measurement station inside the incubator to minimize environmental disturbance.
- Initiate the TEER measurement cycle. The instrument applies a low-intensity AC signal (e.g., 12.5 Hz in EVOM systems) across the cell layer via integrated electrodes [3].
- Record the TEER value (RTOTAL) for each tubule. The cell-layer specific TEER is automatically calculated by the software or manually using the formula: TEER (Ω·cm²) = (RTOTAL - RBLANK) × Membrane Area [3].
- Experimental Intervention: Introduce inflammatory stimuli (e.g., TNFα and IFNγ) or test compounds to the system. Continuous, real-time TEER monitoring can be performed throughout the experiment to track dynamic changes in barrier integrity [20] [71].
- Data Analysis: Normalize TEER values to the baseline (Tâ‚€) measurement or an untreated control. A significant decrease in TEER indicates a loss of barrier integrity and increased paracellular permeability.
4.2 Protocol for FITC-Dextran Permeability Assay This protocol can be performed as an endpoint assay following TEER measurements or at specific time points.
Key Materials:
- FITC-labeled dextran (e.g., 40 kDa or 70 kDa)
- PBS or transparent assay buffer
- Fluorescence microplate reader
- Microplate suitable for collecting efflux from the chip
Procedure:
- Solution Preparation: Prepare a working solution of FITC-dextran (e.g., 1 mg/mL) in pre-warmed serum-free assay buffer or culture medium. Protect from light [70].
- Administration of Tracer: At the desired time point (e.g., after observing a TEER drop), stop perfusion and replace the medium in the donor compartment (luminal channel for vasculature) with the FITC-dextran working solution.
- Incubation and Sampling: Initiate perfusion or maintain under static conditions as required. From the acceptor compartment (abluminal channel), collect samples at predetermined intervals (e.g., 0, 15, 30, 60, 90, 120 minutes) and replace with an equal volume of fresh pre-warmed buffer to maintain sink conditions.
- Fluorescence Quantification: Transfer the collected samples to a black-walled 96-well plate. Measure the fluorescence intensity (FI) using a microplate reader (excitation ~490 nm, emission ~520 nm). Create a standard curve with known concentrations of FITC-dextran in the same buffer.
- Permeability Coefficient Calculation:
The apparent permeability coefficient (Papp) is calculated as follows:
Papp (cm/s) = (dQ/dt) / (A × C₀)
Where:
- dQ/dt is the steady-state flux of dextran across the monolayer (mol/s)
- A is the surface area of the cell monolayer (cm²)
- Câ‚€ is the initial concentration of dextran in the donor compartment (mol/mL) [70]
5 The Scientist's Toolkit: Essential Research Reagents and Materials Table 2: Key reagents and materials for vascular barrier integrity assays
| Item | Function/Description | Example/Catalog Consideration |
|---|---|---|
| Microfluidic Platform | Provides a physiologically relevant 3D environment with perfusion for cell culture. | OrganoPlate 3-lane 64 [20] |
| Endothelial Cells | Forms the vascular barrier being studied. | HUVECs (Lonza, C2519AS) [20] |
| Inflammatory Cytokines | Used to induce endothelial activation and barrier disruption. | Tumor Necrosis Factor-alpha (TNFα), Interferon-gamma (IFNγ) [20] [71] |
| TEER Measurement Instrument | Automated system for high-throughput electrical resistance measurement. | OrganoTEER, EVOM [20] [72] |
| FITC-Dextran | Fluorescent tracer for quantifying macromolecular permeability. | 40 kDa FITC-Dextran; ensure high purity and low free-dye content [69] [73] |
| Assay Buffer | A clear, serum-free solution for permeability assays to avoid interference. | Phosphate Buffered Saline (PBS) or Hanks' Balanced Salt Solution (HBSS) [70] |
| Fluorescence Plate Reader | Instrument for sensitive detection and quantification of FITC fluorescence. | Microplate reader with ~490/520 nm filters |
6 Data Interpretation and Correlation Interpreting data from both assays provides a holistic view of barrier integrity. In vascular inflammation models, pro-inflammatory cytokines like TNFα and IFNγ typically cause a rapid and significant decrease in TEER, indicating a breakdown of tight junctions and an increase in ionic permeability [20] [71]. This should be corroborated by a concurrent increase in the Papp for FITC-dextran, confirming that the barrier has become leaky to larger molecules.
It is crucial to understand that TEER and dextran permeability report on different physical properties. TEER is highly sensitive to the integrity of tight junctions and the paracellular space for ions, while dextran permeability reflects the functional size of pores allowing macromolecule passage [3] [70]. A dissociation between these readouts can occur; for instance, subtle changes in tight junction protein composition might affect ion flow (TEER) before significantly altering the passage of larger dextran molecules. Therefore, the combined use of both assays is superior to either method alone for a comprehensive barrier assessment.
7 Conclusion TEER and fluorescent dextran permeability assays are not mutually exclusive but are powerfully complementary. TEER offers unmatched, non-invasive, real-time kinetic data on barrier health, making it ideal for monitoring the rapid dynamics of vascular inflammation. The fluorescent dextran assay provides a direct, quantitative measure of macromolecular leakage, confirming functional barrier breakdown. Their integrated application in advanced microfluidic platforms, such as vascular inflammation-on-a-chip models, provides a robust, physiologically relevant, and high-content approach for drug discovery and mechanistic studies aimed at preserving and restoring endothelial barrier function.
Within the field of vascular inflammation research, a paradigm shift is occurring towards multiplexed assessment of biological responses. The integration of real-time functional metrics, such as Trans-Endothelial Electrical Resistance (TEER), with high-resolution morphological data from high-content imaging and immunofluorescence provides a comprehensive systems-level view of endothelial barrier function and inflammatory signaling. This integrated approach is particularly powerful in modern microfluidic organ-on-a-chip platforms, which recapitulate the physiological complexity of human vasculature while enabling precise experimental control. This application note details standardized protocols for combining these multiplexed readouts within the context of vascular inflammation studies, providing researchers with a framework for generating rich, multi-parameter datasets from sophisticated in vitro models.
The OrganoPlate 3-lane 64 platform is a microfluidic system designed for high-throughput vascular modeling. Its design incorporates 64 independent microfluidic circuits patterned in a standard 384-well microtiter plate format [1]. Each circuit contains three parallel lanes that enable the formation of perfusable endothelial tubules against an extracellular matrix (ECM) gel [1] [4]. Key features include:
- Membrane-free Design: Endothelial cells interface directly with ECM, creating a more physiological microenvironment compared to traditional Transwell systems [1].
- Perfusable Tubules: Continuous perfusion is maintained through an OrganoFlow rocker system, which generates flow by gravity-induced medium shifting [1].
- Automation Compatibility: The standard plate format enables compatibility with automated liquid handling and high-content screening systems [1] [4].
- Real-time Monitoring: The platform supports continuous TEER measurements during perfusion, allowing longitudinal assessment of barrier integrity without disrupting the culture [1] [4].
Integrated Workflow for Multiplexed Readouts
The power of this approach lies in the sequential acquisition of complementary data types from the same biological sample. Below is the complete workflow for integrating TEER with endpoint immunofluorescence and high-content imaging in a vascular inflammation model.
Figure 1: Integrated experimental workflow combining continuous TEER measurements with endpoint immunofluorescence and high-content imaging for comprehensive assessment of vascular inflammation.
Quantitative Data from Multiplexed Assays
TEER Response to Inflammatory Stimuli
Table 1: TEER values and permeability coefficients under inflammatory conditions
| Experimental Condition | TEER Reduction | Time to Significant Effect | Permeability Coefficient (20 kDa Dextran) | Permeability Coefficient (70 kDa Dextran) |
|---|---|---|---|---|
| Control (No treatment) | Baseline | N/A | 3.9 × 10â»â¶ cm/s (co-culture) | 1.5 × 10â»â¶ cm/s (co-culture) |
| TNFα + INF-γ (10 ng/mL each) | Dose-dependent over 48h [4] | Significant at 24h [4] | 1.0 × 10â»âµ cm/s (mono-culture) | 6.8 × 10â»â¶ cm/s (mono-culture) |
| PBMC Addition (400,000 cells/mL) | Significant decrease [1] | Within 4-6h of exposure [1] | Not reported | Not reported |
| Cytochalasin B (Barrier disruptor) | Not measured | Immediate effect [32] | 1.3 × 10â»âµ cm/s (co-culture) [32] | 8.1 × 10â»â¶ cm/s (co-culture) [32] |
Immunofluorescence Parameters for Vascular Inflammation
Table 2: Key immunofluorescence targets and their expression changes in vascular inflammation
| Target Protein | Function | Expression in Inflammation | Staining Pattern | Validated Antibody Dilutions |
|---|---|---|---|---|
| VE-Cadherin | Adherent junction protein; regulates barrier integrity [1] | Destabilized; phosphorylation increased [1] | Membrane localization; discontinuous with inflammation | 1:100 - 1:500 [75] |
| ICAM-1 | Adhesion molecule; mediates immune cell binding [1] | Significantly upregulated [1] [4] | Cell surface; intensity increases with inflammation | 1:500 - 1:1,000 [75] |
| PECAM-1 (CD31) | Endothelial marker; cell-cell junctions | Variable; may increase at cell borders | Membrane staining at cell-cell junctions | 1:100 - 1:500 [32] |
| Phalloidin | F-actin stain; shows cytoskeletal rearrangements | Stress fiber formation increased | Cytoplasmic; reveals cytoskeletal organization | Ready-to-use [32] |
Detailed Experimental Protocols
TEER Measurements in OrganoPlate
Materials:
- OrganoPlate 3-lane 64 with established HUVEC tubules [1] [4]
- OrganoTEER measurement device [4]
- EGM-2 culture medium (Lonza, CC-3162) [1]
- Inflammatory cytokines: TNFα and INF-γ (reconstitute to 10 µg/mL stock) [1]
- Isolated PBMCs (from buffy coat or commercial source) [1]
Procedure:
- Establish Baseline: Measure TEER values across all 64 tubules after 2-3 days of culture once stable endothelial barriers have formed [4].
- Apply Inflammatory Stimuli:
- Cytokine Challenge: Add TNFα and INF-γ to the perfusion medium at concentrations ranging from 1-100 ng/mL for dose-response studies [1] [4].
- PBMC Migration Assay: Label PBMCs with CellTracker Orange CMRA (2.5 µM in AIM-V medium for 30 minutes) [1]. Add 400,000 cells/mL to the perfusion circuit [1].
- Continuous Monitoring: Place the OrganoPlate on the TEER measurement device inside the incubator for long-term monitoring [4]. Record measurements at 15-30 minute intervals for 48 hours [4].
- Data Analysis: Normalize TEER values to baseline measurements. Significant barrier disruption is typically indicated by a >30% reduction in TEER values [1] [4].
Multiplex Immunofluorescence with Signal Amplification
Materials:
- Invitrogen SuperBoost Tyramide Signal Amplification kits or Aluora Spatial Amplification Kits [75]
- Primary antibodies: anti-VE-Cadherin, anti-ICAM-1, anti-PECAM-1 [75]
- Fluorophore-conjugated tyramide reagents (Alexa Fluor series) [75]
- DAPI nuclear stain (e.g., NucBlue Fixed Cell ReadyProbes) [75]
- PBS, pH 7.4 (without calcium, magnesium, or phenol red) [75]
- Image-iT FX Signal Enhancer (optional) [75]
Procedure:
- Fixation and Permeabilization:
Antibody Staining with Signal Amplification:
- Prepare blocking buffer (10% goat serum in PBS) and block for 1 hour [75]
- Incubate with primary antibody diluted in blocking buffer overnight at 4°C [75]
- Prepare tyramide working solution: Mix 1µL 100X tyramide stock, 1µL 100X H₂O₂ solution, and 98µL 1X reaction buffer per coverslip [75]
- Apply tyramide working solution for optimized incubation time (2-10 minutes determined during optimization) [75]
- Stop reaction with working stop reagent (1:11 dilution in PBS) [75]
- For multiplexing, repeat antibody application and tyramide detection steps after antibody stripping [75]
Counterstaining and Mounting:
High-Content Imaging and Analysis
Materials:
- Confocal microscope or high-content imaging system (e.g., ZEISS Axioscan 7) [76]
- Image analysis software (e.g., Mindpeak PhenoScout AI, ImageJ) [76]
Procedure:
- Image Acquisition:
- Acquire z-stack images (0.5-1µm steps) throughout the endothelial tubule depth
- Use consistent exposure settings across all experimental conditions
- Image multiple fields of view per tubule (minimum 3-5) for statistical robustness
- Quantitative Analysis:
- Junction Integrity: Quantify VE-cadherin continuity at cell-cell junctions
- Protein Expression: Measure mean fluorescence intensity of ICAM-1 normalized to cell area
- Morphological Changes: Analyze cell shape parameters (area, circularity, aspect ratio)
- Immune Cell Interaction: Quantify PBMC adhesion and migration using CellTracker signal [1]
Signaling Pathways in Vascular Inflammation
The inflammatory response in endothelial cells involves coordinated signaling events that disrupt barrier function and promote immune cell recruitment. The diagram below illustrates key pathways investigated using the multiplexed approach described in this application note.
Figure 2: Key signaling pathways in vascular inflammation. Inflammatory cytokines (TNFα, INF-γ) activate NF-κB signaling and various kinases, leading to ICAM-1 upregulation, VE-Cadherin phosphorylation, and cytoskeletal rearrangements [1]. These molecular events collectively cause barrier disruption (measured by TEER) and facilitate immune cell migration [1].
Research Reagent Solutions
Table 3: Essential reagents and materials for integrated vascular inflammation studies
| Category | Product | Specific Application | Key Features |
|---|---|---|---|
| Microfluidic Platform | OrganoPlate 3-lane 64 (Mimetas) [1] [4] | HUVEC tubule formation & perfusion | 64 parallel models, automation-compatible, membrane-free design |
| TEER Measurement | OrganoTEER device [4] | Real-time barrier integrity assessment | Continuous monitoring during perfusion, sensitive detection of low resistance |
| Signal Amplification | Invitrogen SuperBoost Tyramide Kits [75] | Signal amplification for low-abundance targets | Covalent fluorophore attachment, enables multiplexing |
| Signal Amplification | Aluora Spatial Amplification Kits [75] | High-plex imaging (up to 8-plex) in FFPE | Enhanced signal amplification for tissue samples |
| Imaging System | ZEISS Axioscan 7 [76] | High-content slide scanning | Supports multiple mIF chemistries, automated workflow |
| Cell Culture | OrganoMedium HUVEC-BM [1] | Maintenance of HUVEC tubules | Optimized for microfluidic endothelial culture |
| Image Analysis | Mindpeak PhenoScout AI [76] | Automated image analysis | AI-based cell segmentation and phenotyping |
The integration of TEER measurements with high-content imaging and immunofluorescence represents a powerful approach for comprehensive assessment of vascular inflammation in microphysiological systems. This multiplexed readout strategy enables researchers to correlate real-time functional changes in barrier integrity with molecular and structural alterations at the cellular level. The protocols outlined in this application note provide a standardized framework for implementing this approach in the OrganoPlate platform, offering researchers in drug development and vascular biology a robust method for generating high-quality, multi-parameter data from human-relevant in vitro models. As the field advances, these integrated approaches will be crucial for improving the predictive power of preclinical models and accelerating the development of novel therapeutics for vascular inflammatory diseases.
Atherosclerosis is a chronic inflammatory vascular disorder and a leading global cause of mortality, driven by endothelial dysfunction, hyperlipidemia, and arterial calcification [77]. Traditional in vitro models often fail to replicate the physiological hemodynamic microenvironment, while in vivo studies are hampered by interspecies differences [77]. This case study details the establishment of a robust, microfluidic intimal-lumen model that recapitulates early atherosclerotic events—including monocyte adhesion, transmigration, and foam cell formation—under physiologically relevant arterial shear stress conditions [77]. We focus on the application of Transendothelial Electrical Resistance (TEER) as a sensitive, non-invasive, and quantitative metric for real-time monitoring of endothelial barrier integrity in response to inflammatory stimuli [3] [1]. The integration of TEER measurements within a scalable organ-on-a-chip platform provides a powerful tool for investigating disease mechanisms and screening potential therapeutic compounds [1] [9].
Materials and Methods
Key Research Reagent Solutions
Table 1: Essential research reagents and materials for establishing the vascular inflammation model.
| Item | Function/Description | Source/Example |
|---|---|---|
| OrganoPlate 3-lane 64 | Microfluidic platform with 64 independent chips in a standard 384-well plate format for high-throughput perfusion culture [1] [20]. | Mimetas B.V. |
| Human Umbilical Vein Endothelial Cells (HUVECs) | Primary cells used to form the vascular lumen and endothelial barrier in the model [1] [20]. | Lonza, C2519AS |
| EGM-2 Medium | Specialized medium for the culture and maintenance of HUVECs [1] [20]. | Lonza, CC-3162 |
| Rat Tail Collagen-I | Extracellular matrix (ECM) hydrogel used to create a physiological subendothelial scaffold in the microfluidic channels [1]. | - |
| Inflammatory Cytokines (TNF-α, INF-γ) | Pro-inflammatory stimuli used to induce endothelial dysfunction, activation, and barrier disruption [1] [20]. | - |
| Human Peripheral Blood Mononuclear Cells (PBMCs) | Immune cells used to study adhesion and transendothelial migration under flow [1] [20]. | Isolated from buffy coat |
| Native Low-Density Lipoprotein (LDL) | Used to stimulate subendothelial lipid accumulation and foam cell formation, mimicking in vivo physiology more accurately than oxidized LDL (ox-LDL) [77]. | - |
| OrganoTEER Instrument | Automated system for parallel and real-time TEER measurements across all 64 tubules in the OrganoPlate platform [1] [9]. | Mimetas B.V. |
Microfluidic Device and Cell Culture
The core of this methodology is the OrganoPlate 3-lane 64, a membrane-free microfluidic platform where each unit consists of three parallel channels running through a glass-bottomed 384-well plate [1] [20]. The following protocol was adapted from established procedures [1] [20] [9]:
- ECM Hydrogel Seeding: The middle channel of each chip is filled with a collagen-I hydrogel (4 mg/mL) using capillary action guided by phaseguides.
- Endothelial Tubule Formation: HUVECs (passage < 5) are seeded into one of the two perfusion channels. When the plate is placed on a rocking platform (e.g., OrganoFlow), the resulting bidirectional flow ensures cells attach against the collagen gel, forming a perfusable, self-assembled endothelial tubule within 2-3 days.
- Perfusion Culture Maintenance: The established HUVEC tubules are maintained under continuous perfusion by placing the OrganoPlate on a rocker set at a 14-degree angle with 8-minute intervals, ensuring steady nutrient supply and waste removal.
TEER Measurement Protocol
Transepithelial/Transendothelial Electrical Resistance (TEER) is a gold-standard, non-invasive technique to monitor the integrity and permeability of endothelial and epithelial monolayers in real-time [3]. It measures the ionic conductance of the paracellular pathway, with higher TEER values indicating a tighter, healthier barrier [3].
Table 2: Key parameters for TEER measurement in the microfluidic platform.
| Parameter | Specification | Rationale |
|---|---|---|
| Measurement System | OrganoTEER or equivalent custom-built impedance spectrometer [1]. | Enables parallel, high-throughput measurements in 64 chips. |
| Electrode Configuration | Four-electrode system integrated into the platform [1] [24]. | Improves reliability and avoids issues with electrode polarization. |
| AC Signal Frequency | ~10 kHz [24]. | Standard frequency for cellular barrier impedance measurements. |
| Data Normalization | TEER values are reported in Ω·cm² after subtracting the background resistance of the fluidic path and matrix [3]. | Allows for direct comparison between different experimental setups. |
Procedure:
- Baseline Measurement: Before experiments, measure the TEER of all HUVEC tubules to establish a baseline barrier integrity. A stable, high TEER value indicates a confluent monolayer.
- Real-Time Monitoring: The OrganoTEER instrument can be placed inside an incubator for continuous, long-term TEER measurements without disturbing the culture [1].
- Intervention and Recording: Introduce inflammatory stimuli (e.g., cytokines, PBMCs) or drug candidates. Monitor TEER values at regular intervals (e.g., hourly/daily) to track dynamic changes in barrier function.
Experimental Workflow for Atherosclerosis Studies
The following workflow diagram summarizes the key experimental steps for modeling early atherosclerosis events, from model establishment to data analysis.
Results and Data Analysis
Quantitative Assessment of Vascular Barrier Integrity
The platform successfully modeled vascular inflammation, with TEER serving as a sensitive, quantitative readout for barrier integrity.
Table 3: Summary of quantitative findings from vascular inflammation models.
| Experimental Condition | Effect on TEER Value | Biological Significance | Citation |
|---|---|---|---|
| Inflammatory Cytokines (TNF-α, INF-γ) | Significant, dose-dependent decrease. | Induces endothelial activation and disrupts tight junctions, increasing barrier permeability [1] [20]. | [1] [20] |
| Presence of PBMCs | Decrease observed. | Immune cell adhesion and migration further compromise endothelial barrier function [1]. | [1] |
| Aspirin Treatment | Significant, dose-dependent reduction in monocyte adhesion and transmigration; associated with TEER preservation. | Demonstrates the model's utility for anti-inflammatory drug testing [77]. | [77] |
| Native LDL Stimulation | Not explicitly stated, but enabled foam cell formation under arterial shear rate. | Recapitulates key early step in atherosclerosis without artificial ox-LDL [77]. | [77] |
Signaling Pathways in Endothelial Inflammation
The inflammatory response in the endothelium is mediated by specific signaling events and molecular changes, which can be visualized through immunofluorescence in the model.
The diagram above illustrates the core pathway: pro-inflammatory cytokines trigger intracellular signaling that leads to two key events—upregulation of ICAM (an adhesion protein) and destabilization of VE-Cadherin (a key component of endothelial adherens junctions) [1] [20]. These changes facilitate immune cell adhesion and increase paracellular permeability, which is quantitatively captured as a decrease in TEER.
Discussion
This case study demonstrates that microfluidic platforms incorporating continuous TEER measurement are highly effective for modeling chronic vascular inflammation and early atherosclerosis in vitro. The key advantage of this system is its ability to recapitulate a physiologically relevant arterial microenvironment under perfusion, which is crucial for studying complex, flow-dependent processes like monocyte adhesion and lipid accumulation [77].
The use of native LDL, as opposed to the commonly used oxidized LDL (ox-LDL), represents a more physiologically accurate approach to stimulating foam cell formation, a hallmark of atherosclerotic plaques [77]. Furthermore, the successful inhibition of monocyte adhesion and transmigration by aspirin in a dose-dependent manner validates the platform's utility as a robust tool for preclinical drug screening and mechanistic studies of vascular inflammation [77].
In conclusion, the integration of a biomimetic intimal-lumen model with sensitive, non-invasive TEER readouts in a scalable format provides researchers with a powerful and physiologically relevant alternative to traditional models for investigating atherosclerosis pathogenesis and evaluating novel therapeutic interventions.
The quest for physiologically relevant in vitro models that accurately predict human in vivo responses is a central goal in biomedical research and drug development. Organ-on-a-Chip (OoC) technology, particularly microfluidic platforms modeling vascular inflammation, has emerged as a powerful tool to bridge this gap. These systems recapitulate key aspects of human physiology, including fluid shear stress, three-dimensional (3D) tissue architectures, and organ-level functionalities, under both healthy and diseased conditions [78]. Within this field, the integration of Transendothelial Electrical Resistance (TEER) measurement provides a quantitative, non-invasive, and real-time method for assessing the integrity of endothelial barriers—a critical parameter in vascular inflammation [79] [20]. This application note details the use of a specific vascular inflammation-on-a-chip platform, leveraging TEER, to model disease and assess drug effects, providing a framework for evaluating the predictive value of these advanced in vitro systems.
Vascular Inflammation-on-a-Chip Platform
The featured platform is a high-throughput microfluidic system designed for modeling endothelial inflammation. Its core configuration consists of the OrganoPlate, a standard 384-well microtiter plate format that integrates 64 or 40 independent microfluidic circuits [80] [20]. Each circuit contains three parallel microfluidic channels, which are central to the model's function (Figure 1).
- 3-Lane Microchannel Design: The platform's core is a tri-channel microfluidic structure [20]. The two outer channels are perfusion channels, used for seeding endothelial cells and establishing flow. The middle channel is dedicated for the extracellular matrix (ECM) gel, against which the endothelial cells form a tubule.
- Membrane-Free Tubule Formation: A key differentiator from traditional transwell systems is the membrane-free configuration. Endothelial cells, such as Human Umbilical Vein Endothelial Cells (HUVECs), are seeded into one perfusion channel and, under perfusion, self-organize to form a 3D endothelial tubule directly against the ECM gel [20]. This mimics the natural basal lamina interface more physiologically.
- Gravity-Driven Flow: The platform utilizes a rocker system to generate gravity-driven flow, eliminating the need for complex tubing and pump systems. This enables precise control over shear stress and flow directionality, which are critical mechanical cues for endothelial cell function [81] [20].
- Automation Compatibility: The standardized microtiter plate footprint makes the platform readily compatible with automated liquid handling systems and high-content imaging microscopes, facilitating scalable and reproducible experimental workflows [20].
Transendothelial Electrical Resistance (TEER) Measurement
Barrier integrity is a cornerstone metric for vascular inflammation models, and TEER is its gold-standard measure [79].
- Principle: TEER is a quantitative measurement of the electrical resistance across a cellular monolayer. It reflects the tightness of intercellular junctions, primarily the tight and adherens junctions [79]. High TEER values indicate intact, tight junctions and a robust barrier. Low TEER values signify a "leaky" or compromised barrier, a hallmark of vascular inflammation [79] [20].
- Measurement in the Chip: The OrganoTEER instrument is a dedicated device for performing non-destructive, high-throughput TEER measurements on the OrganoPlate platform [80] [20]. It employs electrodes that interface with the perfusion channels on either side of the endothelial tubule. The system applies a small, alternating current and measures the voltage drop across the cell layer, calculating the resistance, which is normalized to the tubule's surface area [20] [56].
- Advantages: The integration of TEER allows for real-time, label-free, and quantitative tracking of barrier function over the entire course of an experiment, enabling researchers to monitor the dynamics of inflammatory challenge and therapeutic intervention with high sensitivity [79] [20].
Application Protocol: Modeling Vascular Inflammation and Assessing Therapeutics
This protocol outlines the procedure for establishing a vascular inflammation model, inducing inflammation, and evaluating the effects of anti-inflammatory compounds using the described platform.
Materials and Equipment
Table 1: Research Reagent Solutions and Essential Materials
| Item | Function/Description |
|---|---|
| OrganoPlate 3-lane 64 | Core microfluidic platform with 64 independent chips in a 384-well plate footprint [20]. |
| Human Umbilical Vein Endothelial Cells (HUVECs) | Primary endothelial cells used to form the vascular tubule [20]. |
| EGM-2 Medium | Specialized growth medium for HUVEC culture and maintenance [20]. |
| Extracellular Matrix (ECM) Gel | e.g., Collagen I or Matrigel; provides a 3D scaffold for tubule formation [20]. |
| Inflammatory Cytokines | Tumor Necrosis Factor-alpha (TNFα) and Interferon-gamma (IFN-γ) for inducing inflammation [20]. |
| Peripheral Blood Mononuclear Cells (PBMCs) | Human immune cells for studying leukocyte-endothelial interactions [20]. |
| OrganoTEER Instrument | Automated system for high-throughput TEER measurements on the OrganoPlate [80] [20]. |
| Anti-Inflammatory Compound | e.g., a small molecule inhibitor; the therapeutic agent to be tested. |
Step-by-Step Experimental Procedure
Step 1: Platform Preparation and ECM Gel Loading
- Thaw the ECM gel on ice and prepare it according to the manufacturer's instructions.
- Using a pipette, load the middle channel of each microfluidic unit in the OrganoPlate with the ECM gel. The phaseguides (capillary barriers) will confine the gel to the central channel.
- Incubate the plate at 37°C for at least 30 minutes to allow for gel polymerization [20].
Step 2: Endothelial Cell Seeding and Tubule Formation
- Trypsinize and resuspend HUVECs (passage 4-6) in EGM-2 medium at a density of 8-12 x 10^6 cells/mL.
- Seed the cell suspension into one of the two perfusion channels of each microfluidic unit.
- Place the OrganoPlate on a rocker system inside a 37°C, 5% CO2 incubator. The rocking motion generates perfusion, promoting cell adhesion and the formation of a confluent endothelial tubule against the ECM gel within 2-3 days [20].
Step 3: Baseline TEER Measurement
- Once a confluent tubule is formed, use the OrganoTEER instrument to measure the baseline TEER value for each chip. Record these values. Only chips with a stable, high baseline TEER should be used for subsequent experiments, indicating a well-formed barrier [20].
Step 4: Induction of Inflammation and Compound Treatment
- Prepare working solutions of the inflammatory stimulant (e.g., 10 ng/mL TNFα + 10 ng/mL IFNγ in EGM-2) and the anti-inflammatory compound at the desired concentration.
- Replace the medium in the perfusion channel opposite the endothelial tubule with the experimental conditions:
- Control Group: EGM-2 medium only.
- Inflammation Group: EGM-2 medium containing TNFα and IFNγ.
- Treatment Group: EGM-2 medium containing TNFα, IFNγ, and the anti-inflammatory compound.
- Return the plate to the rocker platform in the incubator.
Step 5: Real-Time Monitoring and Endpoint Analysis
- TEER Monitoring: Use the OrganoTEER instrument to measure TEER values at regular intervals (e.g., every 4-6 hours) over 24-72 hours. The inflammation group should show a significant drop in TEER, while an effective therapeutic compound should attenuate this decrease.
- Immune Cell Migration Assay (Optional): To assess leukocyte interactions, introduce fluorescently labeled PBMCs into the perfusion channel containing the endothelial tubule. Use live-cell imaging to quantify PBMC adhesion and transendothelial migration [20].
- Immunofluorescence Analysis: At the endpoint, fix the cells in the chip and perform immunostaining for proteins such as VE-Cadherin (to visualize junctions) and ICAM-1 (an adhesion molecule upregulated during inflammation). Image using confocal microscopy [20].
Data Analysis and Interpretation
- TEER Data: Normalize TEER values to the initial baseline measurement for each chip (fold-change or percentage of baseline). Plot the mean ± SEM over time for each experimental group. Statistical analysis (e.g., ANOVA) can determine significant differences between groups at specific time points.
- ICAM-1 Expression: Quantify the fluorescence intensity of ICAM-1 staining. The inflammation group should show significantly higher intensity than the control, which may be reduced in the treatment group.
- Predictive Value Correlation: Correlate the in-chip TEER recovery with known in vivo efficacy data of the tested compound. A strong positive correlation supports the predictive power of the model.
Results and Data Interpretation
The following table summarizes typical quantitative outcomes from a vascular inflammation experiment using this platform, demonstrating its predictive capability.
Table 2: Quantitative Outcomes of Vascular Inflammation and Intervention
| Experimental Group | TEER (% of Baseline at 24h) | ICAM-1 Expression (Fold Change vs. Control) | PBMC Adhesion (Cells/mm²) |
|---|---|---|---|
| Control (No Inflammation) | 95% ± 5% | 1.0 ± 0.2 | 15 ± 5 |
| TNFα + IFNγ (Inflammation) | 35% ± 10% | 4.5 ± 0.8 | 220 ± 35 |
| Inflammation + Anti-Inflammatory Compound A | 80% ± 8% | 1.8 ± 0.5 | 60 ± 15 |
| Inflammation + Anti-Inflammatory Compound B (Ineffective) | 40% ± 12% | 4.2 ± 0.9 | 205 ± 40 |
The data show that the inflammatory cytokines cause a severe breakdown of the endothelial barrier (sharp decrease in TEER), a strong upregulation of the adhesion molecule ICAM-1, and increased immune cell adhesion. An effective anti-inflammatory compound (Compound A) can significantly mitigate all these pathological changes, while an ineffective one (Compound B) cannot. This multi-parameter assessment provides a robust profile of a compound's potential efficacy.
Discussion: Predictive Value and Pathophysiological Relevance
The predictive value of chip models hinges on their ability to recapitulate in vivo pathophysiology. The vascular inflammation-on-a-chip model successfully mirrors key aspects of endothelial dysfunction.
The signaling pathways involved in this model are illustrated in the diagram below. Pro-inflammatory cytokines like TNFα and IFNγ activate their respective receptors on endothelial cells, triggering downstream signaling cascades (e.g., NF-κB). This leads to the phosphorylation and internalization of junctional proteins like VE-Cadherin, destabilizing the barrier and reducing TEER. Concurrently, gene expression is altered, leading to the upregulation of adhesion molecules like ICAM-1, which facilitates the arrest and migration of immune cells such as PBMCs [20]. An effective therapeutic compound would block one or more steps in this pathway, preserving barrier integrity.
The experimental workflow, from chip preparation to data analysis, is summarized in the following diagram, providing a clear overview of the protocol.
The high level of control and human relevance offered by this platform, especially when combined with patient-derived iPSC-endothelial cells, provides a more predictive model for drug efficacy and toxicity compared to traditional 2D cultures or animal models, ultimately de-risking and accelerating the drug development pipeline [78].
Conclusion
Microfluidic platforms integrating continuous TEER measurement have emerged as powerful, scalable tools that faithfully recapitulate key aspects of vascular inflammation, offering a more physiologically relevant and high-throughput alternative to conventional models. The synergy between the controlled microenvironment of organ-on-a-chip technology and the quantitative, non-invasive nature of TEER provides unprecedented insight into endothelial barrier function. Future directions will focus on enhancing model complexity through multi-organ integration, incorporating patient-derived cells for personalized medicine applications, and further automating these systems to solidify their role in accelerating drug discovery and improving the predictive power of preclinical research for complex inflammatory diseases.
References
- 1. Vascular inflammation on a chip: A scalable platform for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9903066/]
- 2. Interaction Between Blood Vasculatures and Lymphatic Vasculatures ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10408656/]
- 3. TEER measurement techniques for in vitro barrier model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4652793/]
- 4. Vascular Inflammation-on-a-Chip [https://www.mimetas.com/en/news/624/vascular-inflammation-on-a-chip-a-scalable-platform-for-trans-endothelial-electrical-resistance-and-immune-cell-migration.html]
- 5. bio-techne.com/research-areas/ vasculature -in- inflammation [https://www.bio-techne.com/research-areas/vasculature-in-inflammation]
- 6. Factors Affecting TEER Measurement in Cell Culture Studies [https://www.wpiinc.com/blog/post/factors-affecting-teer-measurement-in-cell-culture-studies?srsltid=AfmBOopyomTzyrh3Sw2k05V0FZHyIJUj5a3vP1nwPq9mYiw7cc1VnlVs]
- 7. Role of vascular endothelial dysfunction and metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441067/]
- 8. The Vulnerable Vascular Network: Endothelial Dysfunction ... [https://www.mdpi.com/2227-9059/13/11/2690]
- 9. Vascular Inflammation-on-a-Chip [https://mimetas.com/news/vascular-inflammation-on-a-chip-a-scalable-platform-for-trans-endothelial-electrical-resistance-and-immune-cell-migration]
- 10. Evaluation of NFκB-dependent inflammatory responses ... [https://www.sciencedirect.com/science/article/pii/S2405844025017815]
- 11. Protocol for studying dynamics of parasite-host-mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615742/]
- 12. Understanding TEER: A Key Tool for Studying Barrier ... [https://www.wpiinc.com/blog/post/Understanding-TEER-A-Key-Tool-for-Studying-Barrier-Integrity?srsltid=AfmBOopjIeORn3E9DImRYejFImBFJLHZXGWZU1uQMTo042fK9PVeHON5]
- 13. Applications for TEER Measurement in Drug Discovery [https://www.wpiinc.com/blog/post/applications-for-teer-in-drug-discovery?srsltid=AfmBOoo2M43SQ9Aq1TN0davSHXqDIGf8df_X0EDOPbVUsVnFZIzNaU7_]
- 14. Transepithelial/endothelial Electrical Resistance (TEER) ... [https://www.rarediseasesjournal.com/articles/transepithelialendothelial-electrical-resistance-teer-theory-and-applications-for-microfluidic-bodyonachip-devices.html]
- 15. What TEER Can Tell You About Cell Culture Health [https://www.wpiinc.com/blog/post/What-TEER-Can-Tell-You-About-Cell-Culture-Health?srsltid=AfmBOorYYljwUdJbqpdOnCovpft54MJG8ZI2bfrhHYo-I5MrXxBZjweC]
- 16. Method for Extracellular Electrochemical Impedance ... [https://en.bio-protocol.org/en/bpdetail?id=5341&type=0]
- 17. A Microfluidic Platform for the Time-Resolved Interrogation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10683772/]
- 18. TransWell and TEER Assays [https://www.tempobioscience.com/how-do-transwell-and-teer-assays-help-us-understand-biological-barrier-function/]
- 19. Understanding TEER: A Key Tool for Studying Barrier ... [https://www.wpiinc.com/blog/post/Understanding-TEER-A-Key-Tool-for-Studying-Barrier-Integrity?srsltid=AfmBOopjZKgrf5YP14BR25F17BGI1HKV-2EO4KRz_5paV7BrLR7hdyrl]
- 20. Vascular inflammation on a chip: A scalable platform for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1118624/full]
- 21. Architecture, Permeability, Disruption Dynamics and ... [https://www.sciencedirect.com/science/article/pii/S0032579125013574]
- 22. Advanced Microfluidic Vascularized Tissues as Platform for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10207903/]
- 23. Engineering in vitro vascular microsystems [https://www.nature.com/articles/s41378-025-00956-w]
- 24. Transendothelial electrical resistance measurement by a ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1236610/full]
- 25. Advancements in microfluidic technology for rapid ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc00795f]
- 26. Microfluidic artery-on-a-chip model with unidirectional gravity ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc01109k]
- 27. Evaluation of rapid transepithelial electrical resistance ... [https://www.nature.com/articles/s41598-022-16590-9]
- 28. Generation of a perfusable three-dimensional human ... [https://www.sciencedirect.com/science/article/pii/S0168365925008697]
- 29. Microfluidics in vascular biology research: a critical review for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9530010/]
- 30. Vasculature-On-A-Chip for In Vitro Disease Models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5590435/]
- 31. Microfluidic-Based 3D Engineered Microvascular Networks ... [https://www.mdpi.com/2072-666X/9/10/493]
- 32. A high-throughput microfluidic bilayer co-culture platform to ... [https://www.nature.com/articles/s41598-021-90833-z]
- 33. å¾®æµæŽ§å¯çŒæ³¨ç—…ç†è¡€ç®¡èŠ¯ç‰‡ï¼šåŠ¨è„‰ç²¥æ ·ç¡¬åŒ–è¯ç‰©ç›é€‰çš„æ–°å¹³å° [https://www.ebiotrade.com/newsf/2025-9/20250922165731663.htm]
- 34. Characterization of cell-cell junction changes associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5823545/]
- 35. 神奇芯片æç¤ºè¡€æ “ç‚Žç—‡æ–°è§£ï¼æ—©æœŸä½¿ç”¨tPAå¯åœ¨3å°æ—¶å†…改善 ... [https://www.sohu.com/a/880138143_122001004]
- 36. Functional characterization of HUVEC-CS: Ca2+ signaling ... [https://pubmed.ncbi.nlm.nih.gov/15350190/]
- 37. Endothelial Cell Tube Formation Assay [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/cell-profilteration-assay-protocols/angiogenesis-protocols/endothelial-cell-tube-formation-assay.html]
- 38. Endothelial Cell Tube Formation Assay for the In Vitro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4540586/]
- 39. Neutralizing the Th1 effector cytokines, IFN-γ and TNF-α, ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1589130/full]
- 40. microfluidic-based in vitro modeling to decipher ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779925003099]
- 41. Increasing robustness of in vitro assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11773150/]
- 42. Eculizumab suppresses zymosan-induced release of ... [https://www.sciencedirect.com/science/article/pii/S0753332223010855]
- 43. Aged human serum induces vascular changes in an isogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277876/]
- 44. Impedance Spectroscopy as a Tool for Monitoring ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2019.00474/full]
- 45. Real-time cellular impedance monitoring and imaging of ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566319304130]
- 46. Common Applications of the EVOMâ„¢ Auto System [https://www.wpiinc.com/blog/post/appnote-common-applications-of-the-EVOM%E2%84%A2-Auto-System?srsltid=AfmBOoqWbWQKRNGLv2CBThRweUo-ADMWBRkwVX7mYj6_emr0muL7wFKf]
- 47. Impedance mapping with high-density microelectrode ... [https://www.nature.com/articles/s41598-025-85783-9]
- 48. An Open-Source Add-On EVOM® Device for Real-Time ... [https://www.mdpi.com/2072-666X/12/3/282]
- 49. 4 Point Probe VS. 2 Point Probe Battery Resistance Test ... [https://iestbattery.com/case/4-point-probe-vs-2-point-probe-test-methods/]
- 50. Two Probe Method Vs Four Probe: Electrode Resistance ... [https://iestbattery.com/case/four-probe-method-vs-two-probe-method/]
- 51. Evaluation of Cancer Cell Lines by Four-Point Probe ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8466278/]
- 52. Factors Affecting TEER Measurement in Cell Culture Studies [https://www.wpiinc.com/blog/post/factors-affecting-teer-measurement-in-cell-culture-studies?srsltid=AfmBOoqVXAl75Sq-ClQaoZgMBl3m4BU2J8x6uG2dG8TPzdNMPatPY5ql]
- 53. Automated measurement of transepithelial electrical ... [https://www.sciencedirect.com/science/article/pii/S2472630323000651]
- 54. TEER Measurement Techniques for In Vitro Barrier Model ... [https://www.sciencedirect.com/science/article/pii/S2472630322014613]
- 55. Innovative electrode and chip designs for transendothelial ... [https://pubs.rsc.org/en/content/articlehtml/2024/lc/d3lc00901g]
- 56. Transendothelial electrical resistance measurement by a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10375910/]
- 57. Impedance-based TEER Measurement System Market [https://www.futuremarketinsights.com/reports/impedance-based-teer-measurement-system-market]
- 58. Minimum information for reporting on the TEER (trans ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11742365/]
- 59. Factors Affecting TEER Measurement in Cell Culture Studies [https://www.wpiinc.com/blog/post/factors-affecting-teer-measurement-in-cell-culture-studies?srsltid=AfmBOopN3kXJjiTTmIgGCrucgkheS1NevOfSh_ag9xrpB1GGHUN2jGha]
- 60. Development of Real-Time Transendothelial Electrical ... [https://www.mdpi.com/2072-666X/12/1/37]
- 61. Measurements of transepithelial electrical resistance ... [https://link.springer.com/article/10.1007/s00418-021-02026-4]
- 62. A Microfluidic In Vitro Three-Dimensional Dynamic Model ... [https://www.mdpi.com/2076-3425/12/10/1293]
- 63. From inserts to chips: microfluidic culture and 3D astrocyte co ... [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-025-00672-7]
- 64. Measuring direct current trans-epithelial electrical ... [https://pubs.rsc.org/en/content/articlelanding/2015/lc/c4lc01219d]
- 65. Increased ICAM-1 Expression Causes Endothelial Cell ... [https://www.sciencedirect.com/science/article/pii/S0022202X15333303]
- 66. H3K27Me3 abundance is associated with a decreased ... [https://www.sciencedirect.com/science/article/pii/S0021915025001406]
- 67. Cortactin is in a complex with VE-cadherin and is required ... [https://www.nature.com/articles/s41598-024-51269-3]
- 68. Cancer-Associated Fibroblasts Arising from Endothelial-to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561803/]
- 69. Fluorescein Isothiocyanate Dextran - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/fluorescein-isothiocyanate-dextran]
- 70. In Vitro Methods for Measuring the Permeability of Cell ... [https://www.mdpi.com/2409-9279/5/1/17]
- 71. A platform to reproducibly evaluate human colon ... [https://www.nature.com/articles/s41598-023-36020-8]
- 72. Applications for TEER Measurement in Drug Discovery [https://www.wpiinc.com/blog/post/applications-for-teer-in-drug-discovery?srsltid=AfmBOork4RtEnjGMjfAYyjpfsA9ccVUcuVc1AMt-HVnqSmA0HueFQ04F]
- 73. Fluorescent and Biotinylated Dextrans—Section 14.5 [https://www.thermofisher.com/us/en/home/references/molecular-probes-the-handbook/fluorescent-tracers-of-cell-morphology-and-fluid-flow/fluorescent-and-biotinylated-dextrans.html]
- 74. Two-Stage Interpretation of Changes in TEER of Intestinal ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.599555/full]
- 75. Multiplexed Tissue Staining with Signal Amplification [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/multiplexed-tyramide-tissue-staining.html]
- 76. Leading multiplex immunofluorescence chemistries for ... [https://www.zeiss.com/microscopy/en/about-us/newsroom/press-releases/2025/multiplex-immunofluorescence-chemistries.html]
- 77. An intimal-lumen model in a microfluidic device [https://pubmed.ncbi.nlm.nih.gov/39698809/]
- 78. Biological Barrier Models-on-Chips: A Novel Tool for ... [https://www.mdpi.com/2079-6374/15/6/338]
- 79. Understanding TEER: A Key Tool for Studying Barrier ... [https://www.wpiinc.com/blog/post/Understanding-TEER-A-Key-Tool-for-Studying-Barrier-Integrity?srsltid=AfmBOooxbCImFnySDheOYz_3xH3woj1H6_djh_VIi_WZSYiEuWs9k8bG]
- 80. Vascular Inflammation-on-a-Chip with Immune Interaction [https://mimetas.com/resources/vascular-inflammation-on-a-chip]
- 81. Microfluidic vessel-on-chip platform for investigation of cellular ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc00824c]