Multi-Organ-on-a-Chip Systems: A New Paradigm for Immunotoxicity Assessment in Drug Development
This article explores the transformative role of multi-organ-on-a-chip (MOC) systems in advancing immunotoxicity studies.
Multi-Organ-on-a-Chip Systems: A New Paradigm for Immunotoxicity Assessment in Drug Development
Abstract
This article explores the transformative role of multi-organ-on-a-chip (MOC) systems in advancing immunotoxicity studies. Tailored for researchers and drug development professionals, it provides a comprehensive overview of how these microphysiological systems replicate human organ interactions and immune responses to overcome the limitations of traditional 2D cultures and animal models. Covering foundational principles, methodological applications, troubleshooting, and validation strategies, the content synthesizes the latest technological breakthroughs and their practical implementation for predicting systemic immune-related adverse effects, aligning with modern regulatory shifts toward human-relevant testing methodologies.
The Foundation of MOC Systems for Immune Response Modeling
Defining Multi-Organ-on-a-Chip and Its Relevance to Immunotoxicity
Multi-organ-on-a-chip (multi-OoC) platforms are advanced microfluidic cell culture systems that integrate engineered or natural miniature tissues from multiple organs to mimic systemic physiological responses [1] [2]. These systems represent a significant evolution from single organ models by connecting separated organ chambers via microfluidic flow channels that emulate blood circulation, thereby enabling the study of complex inter-organ communication and its role in physiological and pathological processes [3] [4]. By supporting cross-organ communication, multi-OoC devices allow researchers to model multiorgan processes and systemic diseases, providing insights that would be lost using single-OoC models [1].
The relevance of multi-OoC technology to immunotoxicity assessment is particularly profound. Immunotoxicity—the adverse effects on the immune system resulting from exposure to chemical substances, drugs, or medical devices—has been challenging to evaluate using traditional models due to the systemic nature of immune responses [5] [6]. Multi-OoC platforms address this limitation by enabling the study of how substances breach biological barriers in one organ and trigger immune activation in distant organs, thereby providing a powerful tool for investigating systemic immunotoxicity [5].
Key Advantages for Immunotoxicity Assessment
Technical Capabilities
Multi-OoC platforms offer several distinct advantages over traditional models for immunotoxicity studies:
Recapitulation of Physiological Crosstalk: These systems simulate mutual and multiplex physiological communication between distant organs that may not be physically connected, known as multiorgan crosstalk [3]. This crosstalk is mediated by various factors including cells, soluble mediators (growth factors, cytokines), and cellular vesicles that regulate metabolic, inflammatory, and tissue repair processes in the body [3].
Integration of Immune Components: Advanced multi-OoC models incorporate key elements of the immune system, including Langerhans cells (skin), macrophages, and other immune cells, allowing for the study of complex immunotoxicological responses [5]. This capability is essential for investigating how exposure to sensitizing chemicals at one body site can lead to allergic responses such as contact dermatitis in distant organs [5].
Human-Relevance and Personalized Medicine Potential: By using human-derived cells, including patient-specific induced pluripotent stem cells (iPSCs), these platforms can model human-specific immune responses and interindividual variations in immunotoxicity [3] [7].
Long-Term Testing Capability: Recent advancements enable long-term cultivation (up to 4 weeks in some systems) of multiple tissues under dynamic flow conditions, allowing researchers to study chronic cellular reactions and delayed immune responses to pharmaceutical compounds and environmental toxicants [8] [4].
Comparison with Traditional Models
Table 1: Comparison of Model Systems for Immunotoxicity Assessment
| Feature | In vitro 2D Cell Culture | In vitro 3D Spheroid | In vivo Animal Models | Multi-OoC Platforms |
|---|---|---|---|---|
| Human Relevance | Low | Medium | Variable (species differences) | High |
| Complex 3D Microenvironment | No | Yes | Yes | Yes |
| Systemic Immune Response Capability | No | No | Yes | Yes |
| Flow/Perfusion | No | Limited | Yes | Yes |
| Multi-organ Interactions | No | No | Yes | Yes |
| Long-term Study Capability | <7 days | <7 days | >4 weeks | ~4 weeks |
| New Drug Modality Compatibility | Low | Medium | Low | Medium/High |
| Throughput | High | Medium | Low | Medium |
| Time to Result | Fast | Fast | Slow | Fast |
| High-content Data | Limited | Limited | Yes | Yes |
Experimental Platform: Investigating Systemic Immunotoxicity
Case Study: Nickel-Induced Systemic Immunotoxicity
A representative example of multi-OoC application in immunotoxicity assessment comes from a study investigating how oral exposure to metals can cause systemic toxicity leading to Langerhans cell activation in skin [5]. This research exemplifies the unique capabilities of multi-OoC platforms for studying systemic immunotoxicity mechanisms.
Experimental Design and Workflow
The study utilized a HUMIMIC Chip3plus platform (TissUse) to connect reconstructed human gingiva (RHG) and reconstructed human skin containing MUTZ-3-derived Langerhans cells (RHS-LC) through dynamic microfluidic flow [5]. The experimental workflow is illustrated below:
Diagram 1: Experimental workflow for nickel immunotoxicity study
Key Findings and Significance
This study demonstrated that nickel sulfate applied topically to reconstructed human gingiva resulted in increased activation of Langerhans cells in the distant skin model, observed through elevated mRNA levels of CD1a, CD207, HLA-DR, and CD86 in the dermal compartment [5]. Critically, this immune activation occurred without major histological changes in either tissue or significant cytokine release into the microfluidics compartment, highlighting the sensitivity of multi-OoC platforms in detecting subtle immunotoxic effects that might be missed in conventional models [5].
This approach provides a framework for studying systemic immunotoxicity where a chemical breaching one biological barrier (oral mucosa) triggers an immune response in a distant organ (skin), replicating clinical observations of systemic allergic responses to dental materials [5].
Technical Specifications of Representative Multi-OoC Platforms
Table 2: Technical Specifications of Commercial Multi-OoC Platforms
| Platform | Manufacturer | Key Features | Immunotoxicity Applications | Supported Organ Models |
|---|---|---|---|---|
| HUMIMIC | TissUse | On-chip microfluidic channels connecting organ compartments; supports long-term dynamic co-culture | Gut-liver, liver-brain, liver-kidney crosstalk; systemic toxicity | Gut, liver, skin, brain, kidney |
| PhysioMimix Core | CN Bio | PDMS-free multi-chip plates; adjustable recirculating flow; up to 4-week culture | ADME toxicity; immune cell recruitment | Liver, intestine, pancreas, tumor |
| Omni | Axion BioSystems | Real-time electrophysiological monitoring; high-content imaging | Neural-immune interactions; chemotaxis studies | Brain, cardiac, neural spheroids |
| OrganoPlate | MIMETAS | Phaseguides for membrane-free co-cultures; pump-free perfusion | Barrier integrity; immune cell migration | Gut, blood-brain barrier, kidney |
| Emulate OOC | Emulate | Flexible membranes with mechanical stimulation (breathing, peristalsis) | Innate immune responses to pathogens | Lung, intestine, liver, brain |
Detailed Experimental Protocol
Protocol for Systemic Immunotoxicity Assessment
This protocol outlines the methodology for assessing systemic immunotoxicity using a multi-OoC platform, adapted from the nickel exposure study [5] with additional technical details for broader application.
Platform Preparation and Tissue Integration
- Microfluidic Chip Setup: Assemble the HUMIMIC Chip3plus according to manufacturer specifications, ensuring all microfluidic connections are secure and leak-free [5].
- Tissue Model Integration:
- Place reconstructed human gingiva (RHG) in the designated chamber
- Place reconstructed human skin with Langerhans cells (RHS-LC) in the adjacent chamber
- Verify tissue orientation to ensure proper epithelial alignment
- Initiate microfluidic perfusion at physiological flow rates (typical range: 0.1-10 μL/min)
- Stabilization Phase: Culture tissues under dynamic flow conditions for 24 hours to achieve stable culture parameters before experimental manipulation [5].
System Monitoring and Viability Assessment
- Metabolic Monitoring:
- Measure glucose consumption and lactate production every 12 hours
- Monitor lactate dehydrogenase (LDH) release as a cytotoxicity indicator
- Use on-chip sensors or collect effluent for analysis
- Barrier Function Assessment:
- For epithelial barriers, measure transepithelial electrical resistance (TEER) where applicable
- Assess barrier integrity using fluorescent tracers (e.g., FITC-dextran)
- Optimal Culture Parameters:
- Maintain glucose uptake between 0.5-1.0 mg/mL per 24 hours
- Ensure lactate production remains stable without significant increases
- Confirm LDH release <15% of total content indicating acceptable viability [5]
Compound Exposure and Endpoint Analysis
- Test Compound Application:
- Prepare test compounds in appropriate vehicles at physiologically relevant concentrations
- Apply topically to the RHG chamber for localized exposure
- Maintain circulation for 24 hours to allow systemic distribution
- Post-Exposure Incubation: Continue dynamic culture for additional 24 hours to observe delayed responses
- Endpoint Assessments:
- Histological Analysis: Fix and section tissues for H&E staining and morphological assessment
- Immune Cell Activation: Isolve RNA from dermal compartment for qPCR analysis of activation markers (CD1a, CD207, HLA-DR, CD86)
- Cytokine Profiling: Analyze effluent for cytokine release using multiplex immunoassays
- Cell Migration: Quantify Langerhans cell migration from epidermis to dermis [5]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Multi-OoC Immunotoxicity Studies
| Reagent/Material | Function | Example Specifications |
|---|---|---|
| HUMIMIC Chip3plus | Microfluidic platform for multi-tissue integration | Polysulfate or PDMS construction; 3+ tissue chambers; recirculating flow [5] |
| Reconstructed Human Gingiva (RHG) | Oral mucosa model for exposure site | Primary human keratinocytes/fibroblasts; air-liquid interface; 3D architecture [5] |
| Reconstructed Human Skin with Langerhans Cells (RHS-LC) | Target tissue for immune activation assessment | MUTZ-3-derived Langerhans cells; stratified epithelium; fibroblast-populated hydrogel [5] |
| MUTZ-3 Cell Line | Source of human Langerhans cells | CD34+ progenitor cell line; GM-CSF/TGF-β differentiation capability [5] |
| Cell Culture Media | Tissue maintenance and differentiation | Serum-free formulations; organ-specific growth factors; antibiotics [5] |
| Nickel Sulfate | Model immunotoxicant | >99% purity; prepared in aqueous solution; sterile filtered [5] |
| qPCR Reagents | Immune activation marker quantification | Primers for CD1a, CD207, HLA-DR, CD86; reverse transcription kit; SYBR Green master mix [5] |
| Lactate Dehydrogenase (LDH) Assay Kit | Cytotoxicity assessment | Colorimetric detection; compatible with microfluidic effluent [5] |
| Glucose/Lactate Assay Kits | Metabolic monitoring | Enzymatic assays; adapted for small volume samples [5] |
| Cytokine Multiplex Assay | Inflammatory response profiling | Human cytokine panels; high-sensitivity detection [5] |
| Ergothioneine-d3 | Ergothioneine-d3, MF:C9H15N3O2S, MW:232.32 g/mol | Chemical Reagent |
| KRAS inhibitor-6 | KRAS inhibitor-6, MF:C27H30ClF2N5O3, MW:546.0 g/mol | Chemical Reagent |
Technological Implementation and Integration
Integration with Analytical Systems
The full potential of multi-OoC platforms for immunotoxicity assessment is realized through integration with advanced analytical systems:
- Real-time Biosensing: Incorporation of oxygen, pH, and metabolic sensors enables continuous monitoring of tissue viability and function during long-term experiments [4].
- Multi-omic Analysis: Advanced platforms support transcriptomic, proteomic, and metabolomic analyses of both tissues and circulating factors, providing comprehensive mechanistic insights [1] [8].
- Microelectrode Arrays (MEAs): Integration with MEAs allows functional assessment of electrically active tissues (e.g., brain, heart) and their responses to immunotoxicants [4].
- High-Content Imaging: Compatibility with live-cell imaging and automated microscopy enables spatial and temporal analysis of immune cell behavior and tissue responses [9].
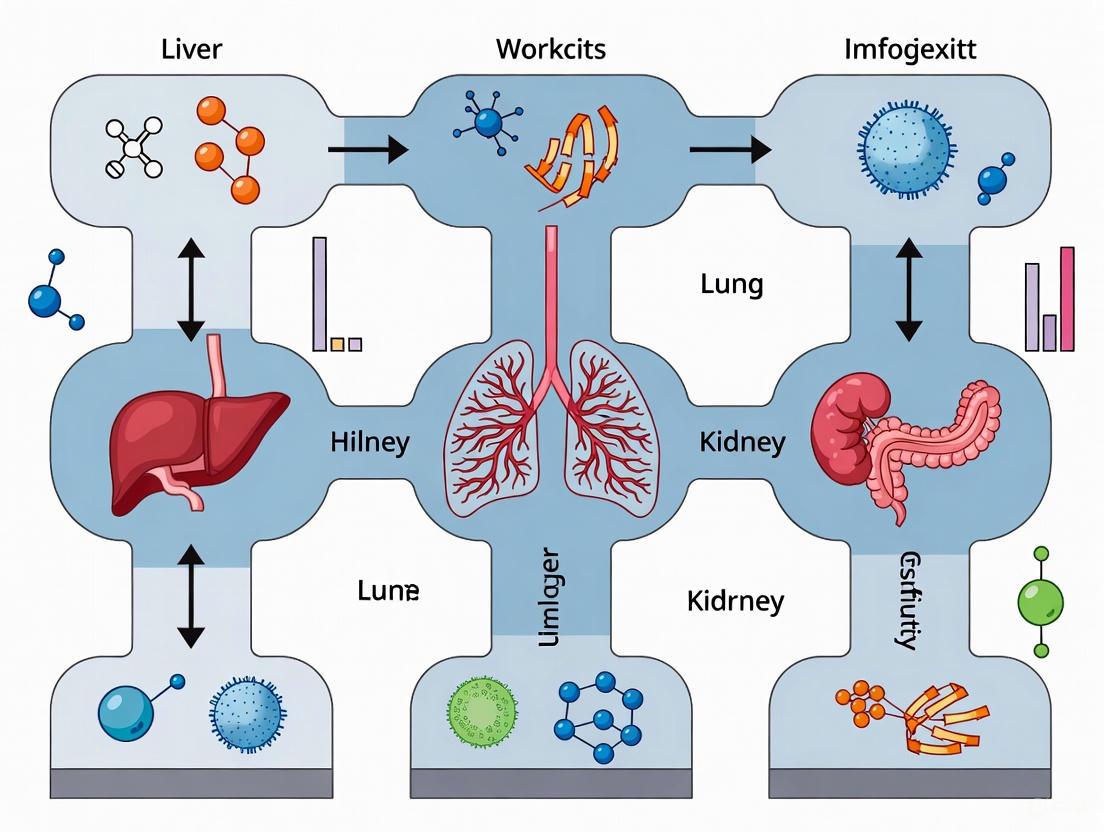
Inter-organ Communication in Immunotoxicity
The following diagram illustrates the key biological processes involved in systemic immunotoxicity that can be modeled using multi-OoC platforms:
Diagram 2: Key processes in systemic immunotoxicity
Multi-organ-on-a-chip technology represents a transformative approach for immunotoxicity assessment, addressing critical limitations of traditional models by enabling the study of systemic immune responses in a human-relevant context. The ability to model inter-organ communication and complex immune crosstalk provides unprecedented opportunities for understanding mechanisms of systemic immunotoxicity, screening potential immunotoxicants, and developing safer pharmaceuticals and consumer products.
As the field advances, key developments will focus on enhancing platform sophistication through integration of more complex immune components (lymph nodes, bone marrow), improving biosensing capabilities for real-time monitoring, and establishing standardized protocols for regulatory acceptance [1] [6] [4]. The ongoing transition toward personalized multi-OoC models using patient-derived cells will further advance our ability to predict individual-specific immunotoxic responses and support the development of precision medicine approaches.
With recent regulatory changes such as the FDA's phased plan to prioritize non-animal testing methods, multi-OoC platforms are poised to play an increasingly important role in safety assessment and drug development, potentially reducing reliance on animal models while improving the human predictivity of preclinical immunotoxicity evaluation [7].
Key Advantages Over Traditional 2D Cultures and Animal Models
Organ-on-a-Chip (OoC) technology represents a transformative approach in biomedical research, enabling the emulation of human organ structures and functions on microfluidic platforms [10]. For researchers focused on immunotoxicity studies within multi-organ systems, OoC technology provides a sophisticated and physiologically relevant in vitro model that bridges the critical gap between traditional 2D cell cultures and animal models. By replicating the dynamic, three-dimensional microenvironments of human tissues, these systems offer unprecedented insights into complex immunological interactions and systemic responses, thereby enhancing the predictive accuracy for human outcomes in drug development and toxicological assessment [11].
Key Advantages of Organ-on-Chip Technology
The transition from conventional models to OoC platforms is driven by several distinct advantages that address fundamental limitations of existing approaches. The table below summarizes the core benefits for immunotoxicity research.
Table 1: Key Advantages of Organ-on-Chip Models for Immunotoxicity Studies
| Feature | Traditional 2D Cultures | Animal Models | Organ-on-Chip Platforms |
|---|---|---|---|
| Physiological Microenvironment | Static, flat cell growth; lacks tissue-specific architecture and mechanical cues [11]. | Species-specific physiology; may not accurately mimic human tissue barriers and immune responses [12] [13]. | Recreates 3D tissue architecture, dynamic fluid flow, and mechanical forces (e.g., breathing motions, peristalsis) [14] [11]. |
| Systemic Immunotoxicity Analysis | Limited to single cell types; cannot model inter-organ communication [5]. | Can observe systemic effects but with significant species-specific immunological differences [15]. | Enables interconnection of multiple organ models (e.g., gut-liver-skin) to study systemic immune activation and distant organ effects [10] [5]. |
| Predictive Value for Human Response | Poorly predictive of human in vivo organ-level responses and toxicity [11]. | Inefficient at predicting human responses; high failure rate in translating drug safety and efficacy [12] [15]. | Incorporates human cells; demonstrates higher relevance for predicting human drug responses and toxicity profiles [12] [14]. |
| Integration of Immune Components | Difficult to co-culture and maintain functional immune cells with organ-specific cells. | Possesses a full, but genetically distinct, immune system. | Capable of incorporating immune cells (e.g., Langerhans cells, PBMCs) into tissue models to study innate and adaptive immune responses [5] [16]. |
| Ethical & Regulatory Considerations | Ethically uncomplicated but biologically simplistic. | Raises significant ethical concerns; subject to strict regulations and high public scrutiny [15]. | Reduces reliance on animal testing; aligns with 3R principles (Replacement, Reduction, Refinement) and modern regulatory shifts (e.g., FDA Modernization Act 2.0) [15] [13]. |
Beyond the comparative advantages, the quantitative challenges of current models further highlight the need for OoC technology. The U.S. Government Accountability Office (GAO) has identified specific hurdles that limit wider adoption of OOCs, which also underscore the limitations of existing paradigms [12].
Table 2: Quantitative Challenges in Model Development and Implications
| Challenge | Quantitative/Severity Data | Impact on Research |
|---|---|---|
| Cell Sourcing | Only 10-20% of purchased human cells are of high enough quality for OOC studies [12]. | Limits reproducibility and scalability of both advanced OoC and simpler 3D models. |
| Lack of Validation | Lack of sufficient benchmarks and validation studies against human clinical data [12]. | Hinders end-user (e.g., drug companies) ability to trust and adopt new models over conventional methods. |
| Data Sharing | Limited data sharing between competing companies and institutions [12]. | Slows collective learning and validation of the technology across the scientific community. |
Application Note: Investigating Systemic Immunotoxicity in a Multi-Organ Setting
Background and Objective
A critical challenge in immunotoxicology is understanding how a topical exposure in one part of the body can trigger an immune response in a distant organ. A 2022 study detailed a methodology to investigate this phenomenon, specifically how oral exposure to metals like nickel can lead to Langerhans cell activation in the skin, a event in allergic contact dermatitis [5]. This application note outlines the protocol for establishing a multi-organ-on-chip system to model this systemic immunotoxicity.
Experimental Workflow
The following diagram illustrates the key stages of the multi-organ immunotoxicity experiment.
Detailed Protocol
Objective: To assess systemic immunotoxicity by measuring Langerhans cell (LC) activation in a skin model following topical nickel application to a connected gingiva model within a multi-organ-chip [5].
Materials and Equipment
Table 3: Research Reagent Solutions and Essential Materials
| Item | Function/Description |
|---|---|
| HUMIMIC Chip3plus | A microfluidic bioreactor platform enabling dynamic flow and connection of multiple tissue models in a closed circulatory system [5]. |
| Reconstructed Human Gingiva (RHG) | 3D model of human oral mucosa, consisting of a differentiated epithelium on a fibroblast-populated collagen hydrogel [5]. |
| Reconstructed Human Skin with Langerhans Cells (RHS-LC) | 3D skin model incorporating MUTZ-3-derived Langerhans cells into the epidermis, allowing for the study of LC maturation and migration [5]. |
| Nickel Sulfate (NiSOâ‚„) | A known skin sensitizer used as the model toxicant applied topically to the gingiva to simulate exposure from dental materials [5]. |
| Microfluidic Perfusion System | Provides dynamic, continuous flow of culture medium, mimicking blood circulation and enabling inter-organ communication [5] [11]. |
| Cell Culture Medium | Sustains the connected tissues under dynamic flow conditions; metabolites like glucose and lactate can be monitored for system health [5]. |
Methodology
Step 1: Chip Assembly and Tissue Integration 1.1. Incorporate the pre-formed Reconstructed Human Gingiva (RHG) and Reconstructed Human Skin with Langerhans Cells (RHS-LC) into the designated compartments of the HUMIMIC Chip3plus [5]. 1.2. Connect the tissue compartments via the microfluidic channels to establish a shared circulation.
Step 2: System Stabilization 2.1. Initiate dynamic flow of culture medium through the microfluidic circuit. 2.2. Culture the connected system for 24 hours under stable flow conditions to achieve equilibrium. Monitor system health by assessing glucose uptake, lactate production, and lactate dehydrogenase (LDH) release in the effluent medium [5].
Step 3: Toxicant Exposure 3.1. After the stabilization period, apply a solution of nickel sulfate topically to the surface of the RHG (Reconstructed Human Gingiva) model. 3.2. Maintain the exposure for 24 hours under continuous dynamic flow.
Step 4: Post-Exposure Incubation 4.1. Remove the nickel source and continue perfusing the multi-organ system with fresh culture medium for an additional 24 hours. This allows for the dissemination of soluble factors and the manifestation of the immune response in the distant skin model [5].
Step 5: Endpoint Analysis Harvest the RHS-LC model and perform the following analyses: 5.1. Histology: Process tissues for histological staining (e.g., H&E) to assess major structural changes in both RHG and RHS-LC [5]. 5.2. Langerhans Cell Activation: * Migration Analysis: Identify and quantify LCs that have migrated from the epidermis into the dermal hydrogel (a key indicator of activation) [5]. * Gene Expression: Isulate RNA from the dermal compartment and analyze the mRNA expression levels of LC activation markers (e.g., CD1a, CD207, HLA-DR, and CD86) using quantitative PCR (qPCR) [5]. 5.3. Cytokine Profiling: Collect effluent medium and analyze for the presence of inflammatory cytokines using multiplex immunoassays (e.g., Luminex or ELISA). In the referenced study, no major cytokine release was detected, highlighting the specificity of the readout to LC activation [5].
Key Technical Considerations
- Quality Control: The stability of the dynamic culture is paramount. Consistently monitor metabolic parameters (glucose/lactate) throughout the experiment to ensure tissue viability and system integrity [5].
- Controls: Always include control chips that are treated with vehicle-only (e.g., PBS) instead of nickel sulfate to establish baseline levels of LC activation and gene expression.
- Reprodubility: Perform independent replicate experiments (e.g., n=3) with intra-experiment replicates to account for technical and biological donor variations [5].
Organ-on-Chip technology provides a paradigm shift for immunotoxicity research, moving beyond the static, single-type environment of 2D cultures and overcoming the species-specific limitations of animal models. The ability to interconnect organ models within a dynamic circulatory system, as demonstrated in the investigation of nickel-induced systemic immunotoxicity, allows scientists to dissect complex immunological cascades across multiple tissues. By offering a more human-relevant, controllable, and ethically advanced platform, OoC technology is poised to significantly improve the predictive power of preclinical safety assessments, thereby de-risking drug development and enhancing our understanding of human immunobiology.
Application Notes
This document details the application of a multi-organ-on-chip (MuOOC) platform for investigating systemic immunotoxicity triggered by topical exposure to chemical sensitizers. The platform is designed to model the remote activation of skin-based immune cells following exposure of a distant oral mucosal barrier, providing a novel in vitro method for studying complex adverse outcome pathways (AOPs) that cannot be recapitulated using single-organ models [5].
The specific case study involves connecting Reconstructed Human Gingiva (RHG) and Reconstructed Human Skin with integrated MUTZ-3-derived Langerhans cells (RHS-LC) within a microfluidic circulation. The primary readout is the activation of Langerhans cells in the skin compartment following topical application of nickel sulfate to the gingiva, mimicking systemic immune activation that can lead to conditions like allergic contact dermatitis [5].
Key Quantitative Parameters from the Model System
Table 1: Key quantitative parameters and culture conditions for the multi-organ-on-chip immunotoxicity study.
| Parameter | Detail / Value | Context / Significance |
|---|---|---|
| Organ Models | Reconstructed Human Gingiva (RHG), Reconstructed Human Skin with Langerhans Cells (RHS-LC) | Replicates human oral and skin barriers with integrated immune components [5]. |
| Chip System | HUMIMIC Chip3plus (TissUse GmbH) | Enables stable dynamic flow within a closed circuit with physiologically relevant shear stress [5]. |
| Total Culture Period | 72 hours | Standard duration for a complete experimental run [5]. |
| Dynamic Flow Stabilization | 24 hours | Initial period to achieve stable dynamic culture conditions before toxicant exposure [5]. |
| Toxicant Exposure Period | 24 hours | Duration of topical nickel sulfate application to the RHG [5]. |
| Post-Exposure Incubation | 24 hours | Time after exposure before analysis of Langerhans cell activation [5]. |
| Replication Strategy | Three independent experiments, each with an intra-experiment replicate | Assesses both donor and technical variations [5]. |
| Key Functional LC Markers | CD1a, CD207, HLA-DR, CD86 | mRNA levels measured in the dermal hydrogel to quantify LC activation and maturation [5]. |
Table 2: Key metabolic and cytotoxicity markers monitored in the microfluidic circuit.
| Marker | Measurement Purpose | Findings in Nickel Exposure |
|---|---|---|
| Glucose Uptake | Indicator of metabolic activity and tissue viability under dynamic flow [5]. | Stable levels indicated healthy culture conditions. |
| Lactate Production | Metabolic waste product; indicator of cellular stress and viability [5]. | Stable levels indicated healthy culture conditions. |
| Lactate Dehydrogenase (LDH) Release | Cytotoxicity marker; released upon cell damage [5]. | No major release, suggesting no significant cytotoxicity from nickel exposure. |
| Inflammatory Cytokine Release | Measures general immune activation and inflammatory response in the circuit [5]. | No major changes detected in the microfluidics compartment. |
Experimental Protocols
Protocol 1: Establishing the Multi-Organ-on-Chip Co-Culture
Objective: To integrate RHG and RHS-LC into the HUMIMIC Chip3plus and establish a stable, dynamic co-culture for 24 hours prior to toxicant exposure [5].
Materials:
- HUMIMIC Chip3plus system (TissUse GmbH)
- Prepared RHG tissue equivalents
- Prepared RHS-LC tissue equivalents
- Appropriate organ-specific maintenance medium
Procedure:
- Chip Priming: Flush all microfluidic channels of the HUMIMIC Chip3plus with culture medium to remove air bubbles and condition the system.
- Organoid Integration: Carefully transfer one RHG and one RHS-LC construct into their respective organ compartments on the chip.
- Initiate Dynamic Flow: Connect the chip to the perfusion system and initiate circulation at a physiologically low flow rate to minimize initial shear stress.
- Stabilization Culture: Maintain the connected system under dynamic flow conditions for 24 hours at 37°C and 5% CO₂.
- Viability Assessment: After the stabilization period, collect effluent from the microfluidic circuit and assess levels of glucose, lactate, and LDH to confirm stable metabolic activity and absence of significant cytotoxicity [5].
Protocol 2: Topical Toxicant Exposure and Assessment of Systemic Immunotoxicity
Objective: To apply a chemical sensitizer (nickel sulfate) to the RHG and quantify the subsequent activation of Langerhans cells in the distant RHS-LC construct [5].
Materials:
- Prepared nickel sulfate solution in an appropriate vehicle (e.g., water or PBS)
- RNA extraction kit
- qRT-PCR reagents and equipment
- Primers for CD1a, CD207, HLA-DR, and CD86
Procedure:
- Toxicant Application: After the 24-hour stabilization period, topically apply a defined volume and concentration of nickel sulfate solution directly onto the surface of the RHG tissue. Include vehicle-only controls in a parallel chip.
- Exposure Incubation: Continue the dynamic co-culture for an additional 24 hours post-application.
- Post-Exposure Incubation: Replace the circulating medium with fresh medium (without toxicant) and continue the dynamic culture for a further 24 hours.
- Tissue Harvest and Analysis:
- Dismantle the circuit and carefully separate the RHS-LC construct from the chip.
- Dissect the dermal compartment (hydrogel) from the epidermal compartment of the RHS-LC.
- Isolate total RNA from the dermal hydrogel.
- Perform qRT-PCR analysis to quantify the mRNA expression levels of the Langerhans cell activation markers CD1a, CD207, HLA-DR, and CD86 [5].
- Additional Endpoints: (Optional) Culture supernatants from the microfluidic circuit can be analyzed via multiplex immunoassays for cytokine release, and tissues can be processed for histology to assess structural integrity.
System Workflow and Signaling Visualization
Experimental Workflow for Immunotoxicity Assessment
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential materials and reagents for replicating the multi-organ-on-chip immunotoxicity assay.
| Item | Function / Application in the Protocol |
|---|---|
| HUMIMIC Chip3plus (TissUse GmbH) | The core microfluidic bioreactor platform that provides a closed-circuit system with dynamic flow for connecting multiple organ models [5]. |
| Reconstructed Human Gingiva (RHG) | 3D tissue construct mimicking the oral mucosal barrier. Serves as the site for topical toxicant application in this model [5]. |
| Reconstructed Human Skin with MUTZ-LC (RHS-LC) | 3D skin equivalent with integrated, functional Langerhans cells. Acts as the distant target organ for monitoring systemic immunotoxicity [5]. |
| MUTZ-3 Cell Line | A human myeloid cell line that can be differentiated into Langerhans Cells (MUTZ-LC) for integration into 3D tissue models to introduce immune competence [5]. |
| Nickel Sulfate | A known metal sensitizer used as a model toxicant to trigger a systemic immune response from the oral mucosa to the skin [5]. |
| qRT-PCR Assays for CD1a, CD207, HLA-DR, CD86 | Key molecular tools for quantifying the activation (maturation) of Langerhans cells in the dermal compartment of the RHS-LC model [5]. |
| Metabolic Assay Kits (Glucose/Lactate/LDH) | Commercial colorimetric or fluorometric kits are essential for monitoring the metabolic state and viability of tissues in the microfluidic circuit during the stabilization and experimental phases [5]. |
| Trpc5-IN-2 | TRPC5-IN-2|Potent TRPC5 Channel Inhibitor|RUO |
| GLS1 Inhibitor-4 | GLS1 Inhibitor-4, MF:C29H27F3N10O2S2, MW:668.7 g/mol |
Mimicking Physiological Organ Crosstalk and Systemic Immunity
The study of immunotoxicity in drug development presents a significant challenge, as the immune system's effects are often systemic and involve complex crosstalk between multiple organs. Traditional in vitro models fail to recapitulate these dynamic interactions, leading to high failure rates in preclinical research. Multi-organ-on-a-chip (multi-OoC) platforms have emerged as a transformative technology that can mimic human physiological systems by supporting cross-organ communication through vascular perfusion, enabling the study of systemic immunity and immunotoxicity with unprecedented human relevance [1]. These microphysiological systems (MPS) provide a ground-breaking approach to evaluate the toxicity and therapeutic efficacy of compounds, including nanoparticles and biologics, by maintaining tissue-specific functions and enabling immune cell trafficking between connected organ compartments [17] [18]. This application note details protocols and methodologies for leveraging multi-OoC technology to advance immunotoxicity studies, with a focus on reproducing physiological organ crosstalk and systemic immune responses.
Multi-OoC Platform Configurations for Immunotoxicity Testing
Multi-OoC platforms are designed to simulate human physiological systems by connecting individual organ models within a circulating fluidic system. This configuration allows for the study of compound distribution, metabolism, and immune cell trafficking across different tissue barriers. Two primary architectural approaches have been developed: integrated body-on-a-chip devices and modular interconnected organ-specific modules [1].
Integrated Systems feature multiple organ chambers fabricated within a single microfluidic device, typically using soft lithography with materials like poly(dimethylsiloxane) (PDMS). These systems benefit from controlled fluidic paths and reduced dead volumes but offer less flexibility for post-assay analysis.
Modular Systems consist of separate organ-specific modules that can be connected via tubing in various configurations to mimic different physiological scenarios. This approach, exemplified by platforms like the AVA Emulation System, offers greater flexibility for independent analysis of individual tissues and scalable experimental designs [18].
Advanced multi-OoC platforms now incorporate key elements of the immune, nervous, and vascular systems to better emulate human complexity in vivo [1]. The integration of patient-specific immune cells and tissue models further enables the development of personalized immunotoxicity profiles, potentially revolutionizing safety assessment in drug development.
Table 1: Comparison of Multi-OoC Platform Configurations for Immunotoxicity Studies
| Platform Type | Key Features | Advantages | Limitations | Example Applications |
|---|---|---|---|---|
| Integrated Body-on-Chip | Single device with multiple organ chambers; Fabricated via soft lithography [9] | Controlled fluidic paths; Minimal dead volume; Reduced bubble formation | Limited post-assay flexibility; Fixed organ combinations | High-throughput screening; ADME studies [1] |
| Modular Interconnected | Separate organ modules connected via tubing; Self-contained incubator systems [18] | Flexible configurations; Independent tissue analysis; Scalable design | Potential for bubble accumulation; More complex fluidic control | Personalized immunotoxicity; Complex disease modeling [18] |
| Vascularized Systems | Endothelialized channels connecting organ compartments; Recirculating perfusion [1] | Physiological barrier function; Immune cell trafficking; Realistic compound distribution | Increased complexity of culture; Specialized media requirements | Immune cell recruitment studies; Nanoparticle transport [17] |
Quantitative Benefits of Multi-OoC Platforms in Preclinical Research
The implementation of multi-OoC technology in immunotoxicity assessment offers significant quantitative advantages over traditional models. These systems can dramatically reduce drug development timelines and costs while providing more human-relevant data. Recent advancements in high-throughput systems, such as the AVA Emulation System, have further enhanced these benefits by enabling parallel processing of up to 96 independent Organ-Chip samples in a single run [18].
The data generation capacity of modern multi-OoC platforms is particularly noteworthy for building robust datasets for machine learning applications. A typical 7-day experiment can generate >30,000 time-stamped data points from daily imaging and effluent assays, with post-takedown omics pushing the total into the millions [18]. This rich, multi-modal data provides a foundation for advanced computational modeling of immunotoxicity.
Table 2: Quantitative Benefits of Multi-OoC Platforms in Immunotoxicity Studies
| Parameter | Traditional Models | Multi-OoC Platforms | Improvement Factor | Impact on Immunotoxicity Studies |
|---|---|---|---|---|
| Development Timeline | 2-5 years for preclinical | 6-18 months with OoC [17] | 60-70% reduction | Faster identification of immune-related toxicities |
| Compound Screening Cost | High (animal models) | Up to 50% reduction in consumables [18] | Significant cost savings | More extensive immunotoxicity screening within budget |
| Data Points per Experiment | Limited by endpoint assays | >30,000 in 7-day experiment [18] | Orders of magnitude increase | Comprehensive immune response profiling |
| Cell Requirement per Sample | Conventional culture volumes | Up to 50% fewer cells [18] | 2-fold improvement | Studies with limited primary human cells |
| Throughput | Low with complex co-cultures | 96 independent chips in single run [18] | High-throughput capability | Multiple immune cell conditions in parallel |
Protocol: Establishing a Multi-OoC Platform for Systemic Immunotoxicity Assessment
Materials and Equipment
Research Reagent Solutions
Table 3: Essential Research Reagents for Multi-OoC Immunotoxicity Studies
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Chip-R1 Rigid Chips [18] | Low-drug-absorbing plastic consumables | Minimally adsorbing plastics; Shorter vascular channel for physiological shear stress |
| Chip-S1 Stretchable Chips [18] | Models requiring mechanical stimulation | Intestine-chip with peristalsis-like motions; Lung-chip with breathing motions |
| Chip A1 Accessible Chips [18] | Enhanced sampling capability | Easy access for tissue manipulation and analysis |
| Hydrogel Scaffolds [18] | 3D extracellular matrix support | RGD-modified hyaluronic acid hydrogel for enhanced cell resilience |
| Primary Human Cells | Patient-specific modeling | Hepatocytes, renal tubular cells, endothelial cells from human donors |
| iPSC-Derived Cells [9] | Disease modeling & personalized medicine | iPSC-derived endothelial cells and tissue-specific cells |
| Specialized Media | Tissue-specific support | Differentiation and maintenance media for multiple organ types |
Equipment
- AVA Emulation System or comparable multi-OoC platform [18]
- Zoë-CM2 Culture Module for continuous perfusion [18]
- Automated imaging system integrated with incubation
- Microfluidic perfusion controllers
- Laminar flow hood for sterile operations
- Incubator maintaining 37°C, 5% CO₂, and controlled humidity
Protocol Steps
Platform Assembly and Sterilization
- Chip Preparation: Select appropriate chip type based on experimental needs. For immunotoxicity studies with small molecules, use Chip-R1 rigid chips to minimize compound absorption [18]. For barrier function studies, use Chip-S1 stretchable chips.
- Sterilization: Sterilize chips and fluidic connections using appropriate methods (UV irradiation, autoclaving, or ethanol flushing) under sterile conditions.
- Matrix Coating: Coat chip chambers with appropriate extracellular matrix proteins (e.g., collagen IV, fibronectin) diluted in PBS at 100-200 µg/mL concentration. Incubate for 2 hours at 37°C or overnight at 4°C.
- Platform Priming: Assemble the multi-OoC system and prime with culture media, ensuring no bubble formation in microfluidic channels. Use degassed media and controlled flow rates (10-100 µL/hour depending on organ requirements) during priming.
Cell Seeding and Tissue Maturation
- Sequential Seeding: Seed endothelial cells in vascular channels first (1-2×10ⶠcells/mL), followed by tissue-specific cells in parenchymal channels after 4-24 hours.
- Establishment of Flow: Initiate perfusion 12-24 hours post-seeding, beginning with low flow rates (50 µL/hour) and gradually increasing to physiological levels (100-400 µL/hour) over 3-5 days.
- Tissue Maturation: Maintain tissues under flow conditions for 7-14 days to allow functional maturation, with media changes every 24-48 hours depending on metabolic activity.
- Quality Control Assessment: Verify tissue integrity and function through daily microscopy, transepithelial/transendothelial electrical resistance (TEER) measurements where applicable, and effluent analysis for tissue-specific biomarkers.
Immunotoxicity Testing
- Compound Administration: Introduce test compounds through the vascular channel at clinically relevant concentrations. Include appropriate controls (vehicle alone).
- Immune Challenge: Introduce immune cells (PBMCs or specific immune cell populations) at physiological ratios (1:10 to 1:100 immune cells to parenchymal cells) through the vascular channel to assess recruitment and activation.
- Real-time Monitoring: Collect data through integrated sensors, daily imaging, and effluent sampling for cytokine analysis, metabolic markers, and tissue-specific biomarkers.
- Endpoint Analysis: At experiment conclusion, harvest tissues for histology, omics analysis (transcriptomics, proteomics), or other specialized assays to elucidate mechanisms of immunotoxicity.
Case Study: Lymph Node-Chip for Preclinical Immunotoxicity Prediction
Background and Rationale
Immunotoxicity remains a major challenge in drug development, particularly for novel modalities like biologics and immunomodulatory therapies. Pfizer has developed a Lymph Node-Chip capable of predicting antigen-specific immune responses, representing a significant advancement for preclinical immunotoxicity testing [18]. This model recapitulates key aspects of human immune responses, including antigen presentation, T-cell activation, and cytokine signaling, within a multi-OoC framework that enables systemic analysis.
Experimental Workflow
The following diagram illustrates the experimental workflow for establishing and utilizing the Lymph Node-Chip for immunotoxicity assessment:
Key Methodological Details
- Chip Configuration: Use a specialized chip design with dedicated compartments for antigen-presenting cells (dendritic cells) and T-cells, separated by microfluidic barriers that allow soluble factor exchange while controlling cell migration.
- Cell Sources: Utilize primary human dendritic cells derived from CD34+ hematopoietic progenitors and autologous CD4+ and CD8+ T-cells from the same donor to maintain immune compatibility.
- Antigen Challenge: Introduce test compounds together with model antigens (e.g., ovalbumin, tetanus toxoid) or specific antigens relevant to the therapeutic area.
- Response Assessment: Monitor T-cell activation through:
- Effluent analysis for cytokine release (IL-2, IFN-γ, IL-6, TNF-α) at 6, 24, 48, and 72 hours
- Imaging of immune cell migration and cluster formation
- Expression of activation markers (CD69, CD25) via endpoint immunostaining
- Systemic Connection: For comprehensive immunotoxicity assessment, connect the Lymph Node-Chip to other organ models (liver, gut) to evaluate systemic effects of localized immune activation.
Data Interpretation and Analysis
The Lymph Node-Chip generates multi-parametric data that requires integrated analysis. Key parameters for immunotoxicity assessment include:
- Immunostimulation: Significant increase in T-cell activation markers and pro-inflammatory cytokines compared to controls may indicate undesirable immunostimulation.
- Immunosuppression: Failure to mount an appropriate immune response to challenge antigens may indicate immunosuppressive effects.
- Cytokine Release Syndrome (CRS) Risk: Specific cytokine profiles (particularly high IL-6 and IFN-γ) may predict potential for CRS, a serious adverse effect of many immunotherapies.
Advanced Protocol: Multi-OoC Platform for Nanomedicine Immunotoxicity
Background
Nanoparticles (NPs) have unique properties that make them promising for various biomedical applications, but their immunotoxicity profile is complex and often involves multiple organ systems [17]. Traditional in vitro and in vivo models struggle to predict NP-induced immunotoxicity due to species-specific differences in immune responses and the lack of integrated organ crosstalk. Multi-OoC platforms provide a human-relevant alternative for comprehensive NP immunotoxicity assessment.
Specialized Methodology for NP Testing
Platform Configuration
Establish a multi-OoC platform connecting liver, spleen, and lung models to assess NP immunotoxicity, as these organs represent primary sites of NP accumulation and immune processing.
- Liver-Chip: Incorporate hepatocytes and Kupffer cells (liver-resident macrophages) to model NP metabolism and initial immune recognition.
- Spleen-Chip: Include dendritic cells and B-cells to model antigen presentation and humoral immune responses to NPs.
- Lung-Chip: Feature airway epithelium and alveolar macrophages to assess pulmonary immune responses, particularly relevant for inhaled NPs.
NP Administration and Tracking
- Dosing Strategy: Introduce NPs through the vascular channel at concentrations reflecting expected human exposure (typically 0.1-100 µg/mL depending on application).
- Real-time Monitoring: Utilize label-free imaging techniques (phase contrast, hyperspectral imaging) to track NP distribution and accumulation in different organ compartments.
- Biodistribution Assessment: Quantify NP accumulation in different tissues through endpoint analysis using ICP-MS for metallic NPs or fluorescence measurement for labeled NPs.
Immunotoxicity Endpoints
- Innate Immune Activation: Monitor cytokine secretion (IL-1β, TNF-α, IL-6) and complement activation in effluent samples.
- Adaptive Immune Responses: Assess T-cell and B-cell activation in the spleen compartment through flow cytometry of harvested cells.
- Barrier Integrity: Measure TEER and permeability markers in epithelial barriers to assess NP-induced tissue damage.
- Oxidative Stress: Evaluate reactive oxygen species production in different tissue compartments using fluorescent probes.
The following diagram illustrates the inter-organ signaling pathways involved in NP-induced immunotoxicity within a multi-OoC system:
Data Analysis and Integration Framework
Multi-modal Data Integration
Modern multi-OoC platforms generate diverse data types that require sophisticated integration approaches. Establish a structured framework for data analysis that incorporates:
- High-content Imaging Data: Automated analysis of tissue morphology, immune cell infiltration, and cell viability using machine learning-based image segmentation.
- Effluent Biomarker Profiles: Time-course analysis of cytokines, metabolic markers, and tissue-specific enzymes using multiplex assays (Luminex, MSD) with appropriate normalization to tissue mass or DNA content.
- Functional Metrics: Integrate TEER measurements, metabolic activity (e.g., albumin production for liver models), and barrier integrity assessments.
- Endpoint Omics Data: Incorporate transcriptomic, proteomic, and metabolomic data from harvested tissues to elucidate mechanisms of immunotoxicity.
Cross-Species Correlation Analysis
For validation purposes, compare multi-OoC immunotoxicity data with historical in vivo results to establish correlation metrics. Focus on:
- Cytokine Storm Prediction: Develop predictive models for cytokine release syndrome based on early cytokine secretion patterns in multi-OoC platforms.
- Immune Cell Activation Thresholds: Establish quantitative relationships between compound concentration and immune cell activation across species.
- Organ-Specific Sensitivity: Compare relative sensitivity of different organ models to known immunotoxicants with established clinical profiles.
Table 4: Multi-OoC Data Correlation with Clinical Immunotoxicity Findings
| Immunotoxicity Endpoint | Multi-OoC Readout | Clinical Correlation | Predictive Value |
|---|---|---|---|
| Cytokine Release Syndrome | Early IL-6 & IFN-γ surge in Lymph Node-Chip | CRS severity in patients | High correlation established for biologics [18] |
| Drug-Induced Autoimmunity | Loss of B-cell tolerance in Spleen-Chip | Autoantibody production | Potential for early detection; under validation |
| Hypersensitivity Reactions | Mast cell activation & histamine release | Clinical hypersensitivity incidence | Improved prediction over standard assays |
| Organ-Specific Inflammation | Tissue-specific cytokine patterns & immune infiltration | Target organ toxicity in clinical trials | Tissue-specific prediction enabling mitigation strategies |
Troubleshooting and Technical Considerations
Common Challenges and Solutions
- Bubble Formation: Degas all media and solutions at least 24 hours before use. Implement bubble traps in the fluidic path and establish priming protocols with gradual flow rate increases.
- Contamination Control: Implement strict sterile techniques during setup and regular antibiotic/antimycotic testing in media. Use integrated sensors for early detection of microbial contamination.
- Cell Viability Issues: Optimize seeding densities for each cell type and validate tissue-specific media formulations. Monitor nutrient and waste levels through frequent effluent analysis.
- Inconsistent Tissue Formation: Standardize cell source and passage number. Implement quality control checkpoints during tissue maturation using functional readouts rather than just temporal benchmarks.
Technical Optimization Guidelines
- Flow Rate Calibration: Determine optimal flow rates for each tissue type based on glucose consumption rates and tissue-specific shear stress requirements. Typical ranges are 50-100 µL/hour for barrier tissues and 100-400 µL/hour for vascularized tissues.
- Media Compatibility: Develop shared media formulations that support all connected tissues without compromising specific functions. Consider sequential media exposure strategies for tissues with incompatible requirements.
- Sampling Frequency Optimization: Balance data density with media volume constraints. For typical 100-200 µL recirculating volumes, limit sampling to 10-20% of total volume per day to maintain system stability.
- Endpoint Analysis Planning: Pre-plan harvest protocols for different analytical techniques (histology, omics, etc.) to ensure appropriate sample preservation and minimize experimental variability.
Implementing MOC Assays for Immunotoxicity Testing: Protocols and Case Studies
Multi-organ-on-chip (MOC) systems have emerged as transformative tools for investigating systemic toxicity and immunotoxicity, addressing critical limitations of traditional two-dimensional cell cultures and animal models. These microphysiological systems simulate human organ-level physiology by fluidically coupling microscale tissue models, enabling the recapitulation of complex organ-organ interactions and systemic drug responses. Within the context of immunotoxicity, MOCs provide a unique platform to study how drug candidates and environmental toxins trigger immune-mediated toxic responses across different organ systems, including bone marrow, liver, and skin. The integration of these three organ models is particularly valuable, as it captures the interplay between immune cell production (bone marrow), xenobiotic metabolism (liver), and external exposure (skin) – a triad crucial for comprehensive safety assessment in drug development.
Established MOC Platforms and Their Applications
Commercially Available MOC Systems
Table 1: Commercial Multi-Organ-on-Chip Platforms for Toxicity Testing
| Platform Name | Key Features | Supported Organ Models | Relevant Applications |
|---|---|---|---|
| TissUse HUMIMIC | Microfluidic channels connecting organ compartments; supports long-term co-culture; option for automation [3] | Gut, liver, skin, kidney, brain, lymph node [3] | ADMET profiling, systemic toxicity, inter-organ crosstalk studies |
| Emulate Organ-Chip | Incorporates flexible membranes and mechanical stimulation (e.g., breathing, peristalsis) [3] | Lung, gut, liver, kidney, blood vessels | Barrier function studies, absorption, toxicity with biomechanical cues |
| CN Bio PhysioMimix | Liver-centric platform for long-term co-culture under flow [3] | Liver with other organ models (e.g., gut, kidney) | ADME studies, metabolism-dependent toxicity |
| MIMETAS OrganoPlate | Uses Phaseguides for membrane-free co-cultures; pump-free, automated perfusion [3] | Various tissue models, including skin and liver | High-throughput screening, barrier models, toxicity |
| InSphero Akura | Integrates 3D organoids under gravity-driven perfusion [3] | Liver, pancreas, tumor models with immune components | Scalable toxicity testing, immune-tumor interactions |
Key Technological Advancements in MOCs
Recent technological innovations have significantly enhanced the physiological relevance and application potential of MOC systems for toxicology studies. These include:
- Physiological Vascular Networks: Advanced MOC designs now incorporate vascular networks that replicate in vivo blood distribution among organs, enabling more realistic systemic exposure and toxicokinetic profiles [19].
- Functional Excretion Systems: Integration of excretory systems with micro-stirrers enhances the elimination of waste and toxic metabolites, maintaining long-term tissue viability and mimicking renal clearance [19].
- Integrated Immune Components: Incorporation of immune system elements, including lymph nodes and circulating immune cells, allows for modeling immunosuppressive effects, cytokine storms, and other immune-related toxicities [20] [21].
- Sensor Integration: Incorporation of biosensors for real-time monitoring of oxygen, pH, and tissue barrier integrity provides continuous data on tissue health and toxic responses [22].
- 3D Bioprinting: Utilization of 3D bioprinting enables precise fabrication of complex tissue architectures, including vascularized models, for more physiologically accurate toxicity assays [22].
Experimental Protocols for Systemic Toxicity Assessment
Protocol 1: Establishing a Tri-Culture MOC for Systemic Toxicity Screening
This protocol outlines the methodology for co-culturing bone marrow, liver, and skin models within an interconnected MOC platform to assess compound-induced systemic toxicity.
Principle: Fluidically coupling tissue models of bone marrow (immune cell production), liver (metabolism), and skin (primary exposure) enables the recapitulation of systemic toxicological pathways, including metabolic activation, immune-mediated responses, and multi-organ damage.
Materials:
- MOC Device: TissUse HUMIMIC Starter Chip or equivalent 2- or 3-organ platform [3]
- Cell Sources:
- Liver: Primary human hepatocytes (PHHs) or HepaRG cells for metabolically functional tissue [23]
- Bone Marrow: Primary human hematopoietic stem/progenitor cells (HSPCs) or immortalized cell lines (e.g., THP-1) [20]
- Skin: Commercially available full-thickness skin models (e.g., EpiDerm, MatTek) or primary keratinocytes/fibroblasts [3]
- Culture Media: A common circulation medium compatible with all three tissues, often a customized serum-free formulation to avoid undefined variables [19] [3]
- Characterization Reagents: ELISA kits for cytokines (e.g., IL-6, TNF-α) and organ-specific biomarkers (e.g., Albumin for liver, LDH for general cytotoxicity)
Procedure:
- Tissue Model Preparation:
- Liver Spheroids: Generate 3D liver spheroids using PHHs in ultra-low attachment plates or on-chip. Differentiate HepaRG cells if used, following established protocols [23].
- Bone Marrow Culture: Seed HSPCs or bone marrow-derived cells into an appropriate 3D scaffold (e.g., collagen gel) within the designated organ chamber to support hematopoiesis and immune cell function.
- Skin Model: If using reconstructed human skin models, acclimate them according to the manufacturer's instructions before transferring to the MOC skin chamber.
MOC Assembly and Initiation:
- Load each tissue model into its respective chamber on the sterilized MOC device.
- Connect the organ chambers via the microfluidic network according to the manufacturer's instructions. A physiologically relevant configuration might sequence Skin → Liver → Bone Marrow to model topical exposure, hepatic metabolism, and systemic effects on hematopoiesis.
- Fill the system with the common circulation medium and initiate perfusion at a low flow rate (e.g., 1-10 µL/min) to allow tissue acclimation without excessive shear stress.
Maintenance and Dosing:
- Maintain the tri-culture under continuous perfusion at 37°C and 5% CO₂. Replace the common medium reservoir periodically (e.g., every 24-48 hours) [19].
- After a stabilization period (typically 3-7 days), administer the test compound. For skin-focused exposure, apply topically to the skin model. For systemic exposure, introduce the compound directly into the circulating medium.
- Maintain the MOC under treatment for a predetermined period (e.g., 7-14 days) to observe both acute and sub-chronic effects.
Endpoint Analysis:
- Viability and Cytotoxicity: Measure LDH release and ATP content in the medium and/or tissue lysates for each organ compartment.
- Functional Biomarkers:
- Liver: Quantify albumin and urea production in the medium. Assess CYP450 activity (e.g., using midazolam as a substrate) [23].
- Bone Marrow: Analyze immune cell population dynamics (e.g., CD4+/CD8+ T cells, monocytes) in the circulating medium and within the tissue compartment using flow cytometry.
- Skin: Measure Transepithelial Electrical Resistance (TEER) and assess tissue morphology via H&E staining.
- Systemic Inflammatory Response: Quantify a panel of pro-inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α) in the circulating medium via multiplex ELISA.
- Histological Analysis: At the experiment terminus, fix and section tissues from each chamber for H&E and immunohistochemical staining to assess structural integrity and specific protein expression.
Protocol 2: Assessing Drug-Induced Liver-Bone Axis Toxicity
This protocol details the use of a simplified liver-bone marrow MOC to investigate toxicity along the liver-bone axis, relevant for drugs known to cause metabolic bone disease or suppress bone marrow function.
Principle: Co-culturing liver and bone marrow tissues allows for the study of how drug metabolites produced by the liver can directly impact bone marrow function and viability, modeling conditions like drug-induced osteoporosis or myelosuppression.
Materials:
- MOC Device: A two-organ MOC platform (e.g., CN Bio PhysioMimix or a custom PDMS chip) [3]
- Liver Model: Differentiated HepaRG spheroids [24] [23]
- Bone Marrow Model: THP-1 cells or primary human bone marrow-derived mesenchymal stem cells (hBM-MSCs) seeded in a 3D scaffold [24]
- Test Compound: Diclofenac (3-6 µM) or other drugs with known bone toxicity [24]
- Analysis Kits: ALT/AST assay kits, TRAP staining kit for osteoclast activity, Alizarin Red S for mineralization (if using hBM-MSCs)
Procedure:
- Establish Co-culture:
- Load liver spheroids and the 3D bone marrow construct into their respective chambers in the MOC.
- Connect the chambers and initiate perfusion with a suitable common medium (e.g., a 50:50 mix of liver- and bone-specific media may be optimized for co-culture [24]).
Compound Exposure:
- After stabilization, expose the system to the test compound (e.g., Diclofenac at 3-6 µM) via the circulating medium for up to 21 days to model chronic exposure [24].
Endpoint Analysis:
- Liver Toxicity: Monitor the culture medium for elevated levels of liver enzymes ALT and AST [23].
- Bone Marrow/Osteotoxicity:
- Osteoclast Activity: Quantify TRAP-positive multinucleated cells in the bone compartment. Co-culture with liver has been shown to significantly upregulate osteoclast activity following diclofenac exposure [24].
- Cytokine Analysis: Measure RANKL, OPG, and oxidative stress markers (e.g., ROS) in the medium, as these are implicated in drug-induced bone loss.
- Gene Expression: Analyze expression of osteogenic (e.g., Runx2) and osteoclastic (e.g., NFATc1) genes in the bone tissue via qPCR.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for MOC-based Toxicity Assays
| Reagent / Material | Function / Application | Examples / Specifications |
|---|---|---|
| Primary Human Hepatocytes (PHHs) | Gold standard for liver metabolism and toxicity studies; express full complement of drug-metabolizing enzymes and transporters [23] | Sourced from commercial providers (e.g., Discovery Life Sciences); require specialized media for long-term culture [23] |
| HepaRG Cell Line | Bipotent progenitor cell line that differentiates into hepatocyte-like and biliary-like cells; highly metabolic competence [24] [23] | Requires differentiation with DMSO; used for liver spheroid generation in toxicity models [24] |
| 3D Organotypic Skin Models | Reconstructed human epidermis or full-thickness skin models for topical exposure and barrier function assessment [3] | Commercially available (e.g., EpiDerm, MatTek); used for dermatotoxicity and absorption studies |
| THP-1 Cell Line | Human monocytic cell line; used as osteoclast precursors or to model innate immune responses in bone marrow compartments [24] | Can be differentiated into osteoclasts or macrophages using PMA or other inducing agents |
| Customized Common Media | Serum-free formulation designed to support the viability and functionality of multiple co-cultured tissue types simultaneously [19] [24] | Often requires empirical optimization (e.g., 50:50 mix of liver and bone media [24]) to maintain all tissues |
| Parylene C Coating | Biocompatible polymer coating for 3D-printed MOC devices; improves cell compatibility and prevents small molecule absorption [21] | Applied via gas-phase deposition onto 3D-printed chips to create a bioinert barrier [21] |
| Antibacterial agent 78 | Antibacterial agent 78, MF:C16H23N3S2, MW:321.5 g/mol | Chemical Reagent |
| KRAS inhibitor-8 | KRAS inhibitor-8, MF:C26H24ClF4N5O3, MW:565.9 g/mol | Chemical Reagent |
Signaling Pathways and Experimental Workflow
Key Signaling Pathways in Systemic Immunotoxicity
The following diagram illustrates the proposed signaling pathways mediating immunotoxic crosstalk between liver, bone marrow, and skin in a tri-culture MOC system, particularly following drug exposure like diclofenac.
Diagram 1: Proposed Signaling Pathways in Systemic Immunotoxicity. This diagram illustrates how drug exposure can trigger metabolic and inflammatory responses in the liver, which subsequently drive toxicity in the bone marrow and skin, culminating in systemic immunotoxicity. Key mediators include reactive metabolites and pro-inflammatory cytokines.
Workflow for MOC Systemic Toxicity Assay
The following diagram outlines the generalized experimental workflow for conducting a systemic toxicity assessment using a multi-organ-on-chip platform.
Diagram 2: Workflow for MOC Systemic Toxicity Assay. This flowchart outlines the key stages of a standard MOC experiment, from tissue preparation through to data integration, highlighting the multi-parametric analysis required for a comprehensive toxicity assessment.
Nickel is a widespread environmental metal and a common cause of allergic contact dermatitis, affecting a significant portion of the population. The Systemic Nickel Allergy Syndrome (SNAS) describes a condition where ingested or systemically absorbed nickel can provoke or exacerbate cutaneous inflammation at sites distant from the exposure, such as the skin, even in the absence of local oral inflammation [5] [25]. This phenomenon presents a significant challenge for traditional single-tissue in vitro models, which cannot recapitulate the complex inter-organ communication required for systemic immune responses. Multi-organ-on-chip (MOC) technology represents a transformative approach for investigating such systemic immunotoxicity, allowing for the cultured interconnection of different tissue models under physiologically relevant dynamic flow conditions [5].
This application note details a specific MOC methodology developed to investigate how oral exposure to nickel, via a reconstructed human gingiva model, can initiate an immune cascade leading to the activation of Langerhans cells (LCs) in a physically separated reconstructed human skin model. This approach provides a novel framework for mechanistic toxicology studies, enabling the deconstruction of the key events in the Adverse Outcome Pathway (AOP) for sensitization across different organ systems, from chemical bioavailability to immune cell activation [5].
The core finding of this investigation was that topical application of nickel sulfate to the reconstructed human gingiva (RHG) in a dynamic MOC system resulted in the activation of Langerhans cells within the distant reconstructed human skin model (RHS-LC). This systemic effect was demonstrated without direct exposure of the skin model to the allergen [5].
Notably, the exposure did not cause major histological changes in either the gingiva or skin models, nor a significant release of most cytokines into the microfluidic circulation. The primary readout for systemic immunotoxicity was the observed LC activation, characterized by their increased migration from the epidermis to the dermal compartment and an upregulation of activation markers [5].
Table 1: Summary of Key Quantitative Data from the Gingiva-Skin MOC Experiment
| Parameter | Control Conditions | Post-Nickel Exposure | Measurement Technique |
|---|---|---|---|
| Culture Stability | Stable glucose uptake, lactate production, and LDH release | Maintained stable levels | Biochemical analysis of microfluidic medium |
| Tissue Histology | Normal, stratified structure of RHG & RHS | No major histological changes | Histological analysis (H&E staining) |
| LC Migration | Baseline level of LC in dermis | Increased migration to dermal hydrogel | Quantitative PCR on dermal compartment |
| LC Activation Markers | Baseline mRNA expression | Increased mRNA levels of CD1a, CD207, HLA-DR, CD86 | Quantitative PCR on dermal compartment |
These findings align with clinical observations of systemic nickel allergy, where nickel sensitization and dietary nickel are considered a substantial trigger for the provocation and persistence of symptoms in patients with chronic allergic-like dermatitis syndromes [25]. The MOC model successfully captured this systemic effect, providing a platform to study the underlying mechanisms.
Detailed Experimental Protocol
This protocol outlines the procedure for co-culturing reconstructed human gingiva (RHG) and reconstructed human skin with Langerhans cells (RHS-LC) in a HUMIMIC Chip3plus to investigate nickel-induced systemic immunotoxicity.
Materials and Reagents
- HUMIMIC Chip3plus (TissUse GmbH): A microfluidic bioreactor enabling a dynamic flow circuit with 4 independent organ niches.
- Reconstructed Human Gingiva (RHG): Comprises a differentiated gingiva epithelium on a fibroblast-populated collagen hydrogel.
- Reconstructed Human Skin with LC (RHS-LC): Contains integrated MUTZ-3-derived Langerhans cells within the epidermis on a fibroblast-populated hydrogel.
- MUTZ-3 Cell Line: A human myeloid cell line used as a source for deriving Langerhans cells.
- Culture Medium: Standard tissue maintenance medium for dynamic culture.
- Nickel Sulfate (NiSOâ‚„): Test compound, prepared in an appropriate vehicle (e.g., water or PBS).
- RNA Extraction Kit (e.g., Qiagen RNeasy).
- cDNA Synthesis Kit (e.g., Reverse Transcription System).
- Quantitative PCR (qPCR) reagents and primers for CD1a, CD207, HLA-DR, CD86, and housekeeping genes.
Methodologies
MOC Assembly and Dynamic Culture Initiation
- Tissue Integration: Carefully transfer the pre-formed RHG and RHS-LC tissues into their respective niches within the HUMIMIC Chip3plus.
- Circuit Connection: Connect the tissue compartments via the microfluidic channels to establish a common, dynamic flow of culture medium.
- Stabilization Culture: Initiate dynamic medium flow and culture the interconnected system for an initial 24-hour period. This allows the tissues to acclimate and achieve stable culture conditions under flow.
- Viability Assessment: Monitor the stability of the system by assessing glucose uptake, lactate production, and lactate dehydrogenase (LDH) release into the microfluidic medium.
Nickel Exposure and Post-Exposure Culture
- Topical Application: After the 24-hour stabilization, apply a defined volume and concentration of nickel sulfate solution topically to the surface of the RHG tissue. The vehicle alone should be applied to control chips.
- Exposure Period: Maintain the chips under dynamic flow for a 24-hour exposure period.
- Post-Exposure Incubation: Carefully remove the nickel solution from the RHG surface and continue the dynamic co-culture of the connected tissues for an additional 24-hour period to allow for systemic signaling and immune cell activation.
Endpoint Analysis
- Tissue Viability and Histology: Process the RHG and RHS-LC tissues for standard histological analysis (e.g., H&E staining) to assess overall tissue structure and health.
- LC Migration and Activation Analysis:
- Separate the epidermis from the dermal hydrogel of the RHS-LC.
- Isolate total RNA from the dermal hydrogel compartment.
- Perform cDNA synthesis and subsequent qPCR analysis for Langerhans cell markers (CD1a, CD207) and activation markers (HLA-DR, CD86).
- The increase in mRNA of these markers in the dermis quantitatively reflects LC migration and activation.
- Cytokine Profiling: Collect microfluidic medium samples at the end of the experiment and analyze using a multiplex immunoassay (e.g., Luminex) to quantify the release of a panel of inflammatory cytokines.
Workflow Visualization
Underlying Molecular Mechanisms
Nickel exposure is known to exert diverse immunotoxic effects, and the systemic response observed in the MOC model can be understood through its impact on specific immune pathways and cells.
Immunotoxicity of Nickel
Excessive nickel exposure can inhibit the development of immune organs by inducing excessive apoptosis and inhibiting cell proliferation. It affects lymphocyte subpopulations, decreasing T and B lymphocytes, though the precise mechanisms require further elucidation [26]. Nickel's effect on immunoglobulins appears complex, with animal models showing suppressed IgA, IgG, and IgM levels, while some human studies have shown the opposite, indicating species-specific or context-dependent effects [26]. A key aspect of nickel's immunotoxicity is its dual role in cytokine regulation: it can inhibit cytokine production in non-inflammatory responses, but in the context of an inflammatory reaction, it significantly promotes cytokine production [26].
Nickel-Induced Inflammatory Signaling
A central mechanism for nickel-induced inflammation involves the activation of innate immune signaling pathways. Nickel ions can activate the Toll-like Receptor 4 (TLR4) pathway. This activation triggers two major downstream signaling cascades: the NF-κB pathway and the Mitogen-Activated Protein Kinase (MAPK) pathway (including JNK, ERK, and p38) [26]. These pathways are master regulators of inflammatory gene expression, leading to the increased production and release of pro-inflammatory cytokines such as IL-1β, IL-6, and TNF-α. This inflammatory milieu is critical for the maturation and activation of antigen-presenting cells like Langerhans cells.
Langerhans Cell Activation
In the skin model, Langerhans cells (LCs) reside in the epidermis as immune sentinels. Upon receiving inflammatory signals (either directly from nickel that has systemically circulated or indirectly via cytokine signaling from the gingiva), these LCs undergo maturation and activation. This process is characterized by:
- Upregulation of surface markers such as HLA-DR (Major Histocompatibility Complex class II) and co-stimulatory molecules like CD86, which are essential for efficient antigen presentation to T-cells [5].
- Migration from the epidermis into the dermal compartment, a crucial step for initiating an adaptive immune response [5]. The increased mRNA levels of CD1a, CD207, HLA-DR, and CD86 in the dermal compartment of the RHS-LC, as quantified by qPCR, are direct molecular correlates of this activation process [5].
Signaling Pathway Diagram
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Gingiva-Skin MOC Experiments
| Reagent / Material | Function in the Experiment | Specific Examples / Notes |
|---|---|---|
| HUMIMIC Chip3plus | Microfluidic bioreactor platform providing a dynamic flow circuit for interconnecting multiple tissue models. | Enables perfusion under physiologically relevant shear stress and tissue-to-fluid ratios [5]. |
| Reconstructed Human Gingiva (RHG) | Represents the oral mucosa barrier; site of topical nickel application to mimic oral exposure. | Comprises a differentiated epithelium on a fibroblast-populated collagen hydrogel [5]. |
| RHS with MUTZ-3 LC (RHS-LC) | Distant target organ model containing immune sentinels (Langerhans Cells) to monitor systemic effects. | MUTZ-3 derived LCs closely resemble their in vivo counterparts in function and phenotype [5]. |
| MUTZ-3 Cell Line | Source for generating human Langerhans cells (LCs) for integration into skin models. | Provides a reproducible and reliable source of functional LCs [5]. |
| Nickel Sulfate (NiSOâ‚„) | Model skin sensitizer and immunotoxicant used to induce systemic immune activation. | A soluble nickel compound; effects can be compared to other forms like NiO particulates [27]. |
| qPCR Assays | Quantitative measurement of LC activation and migration markers (CD1a, CD207, HLA-DR, CD86). | Key molecular endpoint for quantifying immunotoxicity in the dermal compartment [5]. |
| Cytokine Profiling Kits | Multiplexed measurement of cytokine release into the microfluidic medium as a systemic inflammation readout. | Can detect IL-1α, IL-8, and other analytes to assess inflammatory status [5] [27]. |
| KRAS inhibitor-13 | KRAS Inhibitor-13|High-Purity Research Compound | KRAS Inhibitor-13 is a small molecule targeting oncogenic KRAS mutations. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| Sos1-IN-5 | Sos1-IN-5, MF:C26H31F3N4O5, MW:536.5 g/mol | Chemical Reagent |
The rapid development of organ-on-chip (OoC) technology has transformed the landscape of preclinical research, offering in vitro models that recapitulate key aspects of human physiology with remarkable fidelity [9]. These microphysiological systems (MPS) support miniature tissue models under dynamic flow conditions, enabling the study of organ-level responses in a controlled environment [1]. However, a significant limitation of many existing OoC models has been the inadequate incorporation of immune system components, which are crucial for understanding human physiology and pathology [28]. The immune system plays a fundamental role in nearly all disease processes, from cancer and metabolic disorders to infections and autoimmune conditions [28]. Without proper immune integration, these models provide an incomplete picture of human responses to drugs, toxins, and other stimuli.
Recent advances have begun to address this critical gap through the development of immunocompetent OoC models that incorporate various immune cell types, including tissue-resident macrophages and Langerhans cells (LCs) [29] [30]. These models are particularly valuable for systemic immunotoxicity studies, where communication between different organs and immune components is essential for accurate risk assessment [29]. This application note provides detailed protocols and methodologies for integrating key immune players—with special emphasis on Langerhans cells and macrophages—into multi-organ-on-chip platforms to advance immunotoxicity research and drug development.
Key Immune Players in Cutaneous and Systemic Immunity
Langerhans Cells: Sentinel Immune Cells of the Epidermis
Biological Function and Characteristics: Langerhans cells (LCs) are a unique population of tissue-resident macrophages that form a network across the epidermis and possess dendritic cell functionality [31] [32]. Originally classified as dendritic cells due to their ability to migrate to skin-draining lymph nodes, recent lineage tracing and ontogeny studies have demonstrated that LCs originate from embryonic macrophage precursors and represent a specialized subset of tissue-resident macrophages with acquired DC-like properties [32]. Their strategic location at the skin barrier interface positions them as crucial immune sentinels and a first line of immunological defense [31].
LCs constantly extend and retract dendrites between keratinocytes in a behavior termed "dendritic surveillance extension and retraction cycling habitude" [31]. This dynamic surveillance occurs without compromising barrier integrity, as LCs form tight junctions with neighboring keratinocytes that are maintained even during dendrite extension [31]. This allows continuous sampling of the extra-tight junction environment for potential threats while preserving the skin's protective function.
Functional Plasticity and Immunoregulatory Roles: LCs demonstrate remarkable functional plasticity, capable of either immunogenic or tolerogenic responses depending on microenvironmental cues [32]. At steady state, LCs contribute significantly to immune tolerance through multiple mechanisms:
- Phagocytosis of apoptotic keratinocytes: LC-mediated clearance of apoptotic cells suppresses inflammatory responses, a process enhanced by TGF-β1-induced expression of the TAM receptor tyrosine kinase Axl, which recognizes Gas6-expressing apoptotic keratinocytes [31] [32].
- Treg activation and expansion: Resting LCs selectively induce the activation and proliferation of skin-resident regulatory T cells (Tregs), maintaining immune homeostasis in normal skin [32].
- Continuous migration to lymph nodes: Non-activated LCs constitutively migrate to draining lymph nodes to present self-antigen and establish immune tolerance during homeostatic conditions [32].
During inflammatory conditions or pathogen challenge, LCs undergo functional adaptation, shifting toward immunogenic antigen presentation that activates effector T cells while limiting Treg activation [32]. This plasticity makes LCs particularly important for understanding immunotoxicological responses in skin and systemic contexts.
Macrophages and Other Innate Immune Cells
Tissue-Resident Macrophages: Beyond LCs, various tissue-specific macrophage populations play crucial roles in organ homeostasis and immune surveillance. These cells perform phagocytic clearance of cellular debris, produce regulatory cytokines, and help maintain tissue integrity [30]. In barrier tissues like skin, lung, and intestine, resident macrophages are among the first immune cells to encounter environmental challenges.
Monocytes, Neutrophils, and Dendritic Cells: The innate immune system additionally comprises circulating monocytes, neutrophils, and dendritic cells, which can be recruited to sites of inflammation or infection [33]. Neutrophils serve as rapid first responders, employing mechanisms including phagocytosis, reactive oxygen species production, and neutrophil extracellular trap (NET) formation to contain threats [30]. Monocytes can differentiate into macrophage or dendritic cell populations in tissues, while dendritic cells specialize in antigen presentation and T cell activation [33].
Table 1: Key Immune Cell Types for Integration into Multi-Organ-on-Chip Systems
| Immune Cell Type | Origin/Lineage | Primary Functions | Relevance to OoC Models |
|---|---|---|---|
| Langerhans Cells (LCs) | Tissue-resident macrophages (embryonic origin) with DC functionality | Immune surveillance, antigen presentation, immunoregulation, maintenance of skin homeostasis | Key for skin models, immunotoxicity testing, tolerance/sensitization studies |
| Dermal Macrophages | Tissue-resident macrophages (embryonic and monocyte-derived) | Phagocytosis, tissue remodeling, cytokine production, immune regulation | Important for skin inflammation and systemic immune responses |
| Monocytes | Bone marrow-derived (circulating) | Differentiation into macrophages/DCs, phagocytosis, cytokine production | Model innate immune recruitment and inflammatory responses |
| Neutrophils | Bone marrow-derived (circulating) | Phagocytosis, NETosis, reactive oxygen species production, cytokine signaling | Essential for acute inflammation and infection models |
| Dendritic Cells (DCs) | Bone marrow-derived | Antigen presentation, T cell activation, immune regulation | Bridge innate and adaptive immunity in multi-OoC systems |
Protocol: Establishing a Multi-Organ-on-Chip Platform for Systemic Immunotoxicity Assessment
Experimental Design and Workflow
This protocol describes the establishment of a multi-organ-on-chip platform incorporating reconstructed human gingiva (RHG) and reconstructed human skin with Langerhans cells (RHS-LC) to investigate systemic immunotoxicity following topical exposure to metals, adapted from Koning et al. [29]. The approach demonstrates how immune activation in a distant organ can be triggered by topical exposure at a different site, replicating clinical observations of systemic allergic contact dermatitis.
Materials and Reagents
Table 2: Essential Research Reagent Solutions for Immunocompetent Multi-Organ-on-Chip Models
| Reagent/Material | Specifications | Function/Application |
|---|---|---|
| HUMIMIC Chip3plus (TissUse GmbH) | Multi-organ microfluidic platform with closed-circuit circulation | Provides dynamic flow and inter-organ communication capabilities |
| Reconstructed Human Gingiva (RHG) | Organotypic model with differentiated epithelium on fibroblast-populated collagen hydrogel | Represents oral mucosa for topical exposure site |
| Reconstructed Human Skin with Langerhans Cells (RHS-LC) | Organotypic model with MUTZ-3-derived LCs in epidermis on fibroblast-populated hydrogel | Target tissue for assessing systemic immunotoxicity |
| MUTZ-3-derived Langerhans Cells (MUTZ-LC) | LC model differentiated from MUTZ-3 cell line | Provides consistent, functional LC population for immunotoxicity assessment |
| Nickel Sulfate | 1-10 mM concentration in appropriate vehicle | Model sensitizing chemical for topical exposure |
| Cell Culture Medium | Serum-free defined medium with essential supplements | Supports viability and function of both tissue models during dynamic flow |
| Collagen Hydrogel | Type I collagen matrix (1.5-3 mg/mL) with embedded fibroblasts | Provides physiological dermal equivalent for tissue models |
| qPCR Reagents | Primers for CD1a, CD207, HLA-DR, CD86, and housekeeping genes | Quantifies LC activation markers |
Detailed Methodology
Step 1: Microfluidic System Assembly and Tissue Loading
- Prepare the HUMIMIC Chip3plus according to manufacturer specifications, ensuring all microfluidic connections are secure and sterile.
- Load reconstructed human gingiva (RHG) into the designated compartment, ensuring proper contact with the microfluidic channel.
- Load reconstructed human skin with Langerhans cells (RHS-LC) into the adjacent compartment, maintaining the same orientation (epithelium facing upward).
- Establish dynamic flow at a physiologically relevant shear stress (typically 0.1-1.0 dyne/cm²) using a serum-free defined culture medium.
- Initiate the closed-circuit circulation between the two tissue compartments to enable systemic communication.
Step 2: System Stabilization and Baseline Assessment
- Maintain the system under dynamic flow conditions for 24 hours to achieve stable culture conditions.
- Monitor metabolic parameters including:
- Glucose consumption (target: 5-20% depletion from baseline)
- Lactate production (target: maintained ratio to glucose consumption)
- Lactate dehydrogenase (LDH) release (target: <15% increase, indicating acceptable viability)
- Verify tissue viability through visual inspection and preliminary molecular analysis if required.
Step 3: Topical Exposure and Experimental Timeline
- After the 24-hour stabilization period, topically apply 20-50 μL of nickel sulfate solution (1-10 mM in appropriate vehicle) to the RHG epithelium.
- For control conditions, apply vehicle only to parallel systems.
- Maintain the exposure for 24 hours under continuous dynamic flow conditions.
- After 24 hours of exposure, remove the nickel sulfate solution and gently rinse the RHG surface with fresh medium.
- Continue dynamic culture for an additional 24 hours with fresh medium circulating through the system.
- Harvest tissues and collect media after the total 72-hour culture period for endpoint analysis.
Step 4: Endpoint Analysis of Immune Activation
- Assess LC migration and activation in RHS-LC through:
- mRNA extraction and qPCR analysis for LC markers (CD1a, CD207, HLA-DR, CD86)
- Histological examination of LC distribution within the epidermis and dermis
- Immunofluorescence staining for LC-specific proteins
- Evaluate tissue integrity through histological analysis (H&E staining) of both RHG and RHS-LC.
- Measure cytokine release into the microfluidic compartment using multiplex ELISA or similar approaches.
- Document any morphological changes in both tissue models compared to controls.
Data Analysis and Interpretation
Quantitative Assessment of Langerhans Cell Activation
In the referenced study [29], nickel exposure resulted in significant LC activation as evidenced by increased mRNA levels of key immune markers, without major histological changes or substantial cytokine release into the microfluidics compartment. This pattern suggests that LC activation may represent an early, sensitive indicator of systemic immunotoxicity that precedes overt tissue damage or generalized inflammation.
Table 3: Expected Langerhans Cell Activation Markers in Systemic Immunotoxicity
| Activation Marker | Function in Immune Response | Expected Change with Nickel Exposure | Detection Method |
|---|---|---|---|
| CD1a | Lipid antigen presentation to T cells | Increased expression | qPCR, Immunofluorescence |
| CD207 (Langerin) | LC-specific C-type lectin, pathogen recognition | Increased expression | qPCR, Immunofluorescence |
| HLA-DR | MHC Class II antigen presentation | Increased expression | qPCR, Flow Cytometry |
| CD86 | Co-stimulatory molecule for T cell activation | Increased expression | qPCR, Flow Cytometry |
| Migration to Dermis | Indication of maturation and initiation of immune response | Increased LC numbers in dermal compartment | Histology, Immunofluorescence |
Troubleshooting and Technical Considerations
Common Challenges and Solutions:
Poor tissue viability during dynamic culture:
- Optimize flow rates to ensure adequate nutrient delivery without excessive shear stress
- Monitor metabolic parameters regularly to establish system stability before experimental interventions
Variable LC activation responses:
- Standardize LC differentiation protocols if using MUTZ-3 derived LCs
- Include appropriate positive controls (e.g., known sensitizers) to validate system responsiveness
Inconsistent inter-organ communication:
- Verify integrity of microfluidic connections and absence of air bubbles in the system
- Ensure proper tissue sizing to maintain physiologically relevant tissue-to-media ratios
High background inflammation:
- Use serum-free media to minimize non-specific immune activation
- Include multiple vehicle controls to account for background responses
Application in Systemic Immunotoxicity Assessment
The protocol described above represents a significant advancement over traditional single-organ models for immunotoxicity assessment [29]. By connecting multiple tissue models through dynamic flow, this approach enables researchers to:
- Investigate systemic effects of locally applied compounds, mimicking real-world exposure scenarios
- Identify organ-specific immune responses that may not be apparent in isolated tissue models
- Evaluate cross-organ communication in immune activation, particularly relevant for sensitization reactions that manifest at sites distant from the exposure
- Reduce reliance on animal models while providing human-relevant data for safety assessment
This multi-organ approach is particularly valuable for studying conditions such as systemic contact dermatitis, where materials like dental metals (e.g., nickel) can cause skin inflammation without obvious local mucosal responses [29]. The integration of functional immune components, specifically Langerhans cells, provides critical insight into the mechanisms underlying these systemic reactions.
The integration of immune competence—particularly Langerhans cells and macrophages—into multi-organ-on-chip systems represents a transformative approach for immunotoxicity research and drug development. The protocol outlined here provides a framework for establishing such models, with specific application to systemic immunotoxicity assessment following topical exposure.
Future developments in this field will likely focus on increasing model complexity through incorporation of additional immune components, including adaptive immune cells (T and B cells) and lymphoid tissue constructs [28] [30]. Additionally, technological advances in real-time monitoring and multi-omic analysis will further enhance the information yield from these systems [1]. As these models continue to evolve, they will play an increasingly important role in bridging the gap between traditional in vitro assays and clinical responses, ultimately improving the prediction of human immunotoxicity and efficacy for new compounds and materials.
Multi-organ-on-a-chip (MOC) systems represent a transformative approach in immunotoxicity studies, enabling the simulation of complex physiological interactions between different organs linked by vascular perfusion. These microphysiological systems allow researchers to investigate how a stimulus or toxicant applied to one organ can lead to a systemic immune response in a distant organ, a process known as inter-organ crosstalk [3] [5]. For drug development professionals, establishing robust, quantitative readouts from these systems is paramount for predicting clinical immunotoxicity and efficacy during preclinical development.
This application note details four key analytical readouts—cytokine analysis, cell migration, metabolic markers, and gene expression—within the context of MOC platforms. We provide standardized protocols and data interpretation frameworks to enhance the reliability and translational value of immunotoxicity assessments, supporting the growing regulatory acceptance of these human-relevant models [34].
Key Readouts for Immunotoxicity Assessment in MOC Systems
The complexity of MOC systems necessitates a multi-parametric analytical approach. The following key readouts provide complementary information for a comprehensive assessment of immune responses.
Table 1: Key Readouts and Their Significance in MOC Immunotoxicity Studies
| Readout Category | Specific Metrics | Biological Significance | Application in Immunotoxicity |
|---|---|---|---|
| Cytokine Analysis | IL-6, IL-1β, TNF-α, IL-18, IFNs | Indicates immune cell activation, pro-/anti-inflammatory status, and chemotactic signaling [5]. | Identifies systemic inflammation and potential cytokine release syndrome. |
| Cell Migration | Immune cell trafficking (e.g., Langerhans cells, T cells) from one organ compartment to another; Transendothelial migration [5] [21]. | Measures functional immune cell recruitment and homing. | Assesses sensitization potential and antigen-specific immune responses. |
| Metabolic Markers | Glucose uptake, Lactate production, Lactate Dehydrogenase (LDH) release [5]. | Reports on overall tissue viability and metabolic activity. | Distinguishes between cytotoxic and immunomodulatory effects. |
| Gene Expression | mRNA levels of immune activation markers (e.g., CD1a, CD207, HLA-DR, CD86) [5]. | Reveals early-stage immune cell maturation and activation pathways. | Provides mechanistic insights into immunogenic or tolerogenic outcomes. |
Quantitative Data from a Representative MOC Study
The data in the table below, inspired by a published study investigating nickel-induced systemic immunotoxicity, exemplifies how these readouts can be quantified in a connected MOC platform [5].
Table 2: Exemplar Quantitative Data from a Gingiva-Skin MOC Immunotoxicity Study
| Experimental Group | CD86 Gene Expression (Fold Change) | HLA-DR Gene Expression (Fold Change) | LDH Release (Relative Units) | Langerhans Cell Migration |
|---|---|---|---|---|
| Control (Untreated) | 1.0 ± 0.2 | 1.0 ± 0.3 | 1.0 ± 0.1 | Baseline |
| Nickel-Treated | 2.5 ± 0.4 | 3.1 ± 0.5 | 1.2 ± 0.2 | Significantly Increased |
Detailed Experimental Protocols
This section outlines a generalized workflow for a multi-organ immunotoxicity study, adaptable to specific organ combinations and research questions.
Protocol: Systemic Immunotoxicity in a Gingiva-Skin MOC
Background: This protocol models systemic immunotoxicity where a topical exposure in the oral cavity (e.g., to leached metals from dental materials) triggers an immune response in distant skin [5]. The platform uses the HUMIMIC Chip3plus with reconstructed human gingiva (RHG) and reconstructed human skin with integrated Langerhans cells (RHS-LC) connected by dynamic microfluidic flow.
Materials:
- MOC Platform: HUMIMIC Chip3plus or equivalent dual-organ system [5].
- Biological Models: Reconstructed Human Gingiva (RHG) and Reconstructed Human Skin with integrated MUTZ-3-derived Langerhans Cells (RHS-LC) [5].
- Test Article: e.g., Nickel sulfate solution.
- Culture Media: Standard tissue maintenance medium, circulating through the microfluidic circuit.
- Analysis Kits: LDH assay kit, Glucose/Lactate assay kit, RNA extraction kit, qRT-PCR reagents, ELISA kits for cytokines (e.g., IL-18).
Procedure:
- Chip Priming and Tissue Loading: Load the RHG and RHS-LC models into their respective compartments on the HUMIMIC Chip3plus. Establish dynamic flow of culture medium to connect the two organ models in a closed circulatory system [5].
- System Stabilization: Maintain the connected system under dynamic flow conditions for 24 hours to achieve stable culture parameters. Monitor glucose uptake and lactate production to confirm tissue viability [5].
- Compound Exposure: After stabilization, topically apply the test article (e.g., Nickel Sulfate) directly to the RHG model for 24 hours. The circulatory flow allows systemic distribution of potential metabolites or signaling factors [5].
- Post-Exposure Incubation: Remove the test article and continue dynamic co-culture for an additional 24 hours to allow for the development of a systemic immune response in the skin compartment [5].
- Sample Collection and Analysis:
- Media Sampling: Collect circulating medium at the end of the experiment for analysis of metabolic markers (glucose, lactate, LDH) and cytokines (e.g., via ELISA) [5].
- Tissue Harvest: Harvest the RHS-LC model. Separate the epidermis and dermis-equivalent hydrogel for analysis.
- Cell Migration Analysis: Isolate cells from the dermal hydrogel and analyze by flow cytometry or qPCR to quantify the migration of Langerhans cells out of the epidermis [5].
- Gene Expression Analysis: Extract total RNA from the dermal compartment and perform qRT-PCR for immune activation markers (CD1a, CD207, HLA-DR, CD86) [5].
Protocol: Cytokine Profiling in MOC Effluent Media
Purpose: To quantify soluble immune mediators in the recirculating culture medium as a measure of local and systemic immune activation.
Procedure:
- Collect medium samples from the MOC's microfluidic circuit at defined time points (pre-exposure, post-exposure, and endpoint).
- Centrifuge samples to remove cellular debris.
- Analyze clarified supernatant using a multiplex bead-based immunoassay (Luminex) or ELISA kits specific for human cytokines (e.g., IL-6, IL-8, IL-1β, TNF-α, IFN-γ). Normalize cytokine levels to total protein content or tissue volume.
- Data from a nickel exposure study showed that while major inflammatory cytokines in the effluent may not show significant changes, key local immune activation is detectable via gene expression in the target tissue [5].
Protocol: Gene Expression Analysis of Immune Activation
Purpose: To detect early and specific molecular markers of immune cell maturation and activation within a target tissue in the MOC.
Procedure:
- RNA Extraction: Homogenize harvested tissue (e.g., the dermal hydrogel of the RHS model) and extract total RNA using a commercial kit.
- cDNA Synthesis: Reverse transcribe 500 ng - 1 µg of total RNA into cDNA.
- Quantitative PCR (qPCR): Perform qPCR using primers for immune cell markers.
- Data Analysis: Calculate fold-change in gene expression using the 2^(-ΔΔCt) method relative to the control MOC group.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for MOC Immunotoxicity Studies
| Item | Function/Description | Example Use Case |
|---|---|---|
| HUMIMIC Chip3plus (TissUse) | A commercial multi-organ-chip platform enabling the dynamic connection of up to 4 organ models in a closed circulatory system [3] [5]. | Studying systemic toxicity and immunotoxicity across gut-liver-skin-kidney axes [3] [5]. |
| MUTZ-3 Derived Langerhans Cells (MUTZ-LC) | A human cell line-derived model of epidermal Langerhans cells, used to incorporate functional immune cells into reconstructed skin models [5]. | Modeling antigen presentation and LC migration in response to skin sensitizers in a MOC [5]. |
| Reconstructed Human Tissues (RhE, RHG, RHS) | 3D, organotypic tissue models with stratified epithelium, often produced from primary human cells [5]. | Providing physiological barriers (skin, gingiva) for topical application in MOC studies. |
| Lactate Dehydrogenase (LDH) Assay Kit | A colorimetric kit to measure LDH enzyme released upon cell damage, quantifying general cytotoxicity [5]. | Monitoring tissue health and viability in MOC compartments during experiments. |
| Multiplex Cytokine Array (Luminex/ELISA) | Immunoassays for simultaneous quantification of multiple cytokines/chemokines from small volume samples [35]. | Profiling comprehensive immune signatures in the circulating medium of a MOC. |
Data Interpretation and Integration
The power of MOC systems lies in the integration of multi-parametric data. A positive immunotoxicity signal is confirmed by a cohesive story across readouts. For instance, in the nickel exposure model, the lack of elevated LDH or inflammatory cytokines in the media suggests an absence of overt cytotoxicity or a massive inflammatory cascade. However, the significant upregulation of CD86 and HLA-DR gene expression, coupled with observed Langerhans cell migration, provides a clear molecular and functional signature of a specific, sensitization-driven immune activation [5].
This integrated approach, correlating metabolic stability with specific immune activation, provides a robust and human-relevant model for identifying compounds with immunotoxic potential, thereby de-risking drug development pipelines.
Overcoming Technical Hurdles: Ensuring Robust and Reproducible MOC Data
Addressing the Long-Term Culture and Viability Challenge
Maintaining the viability and functionality of interconnected organ models during long-term culture is a pivotal challenge in multi-organ-on-chip (MOC) systems research, especially for immunotoxicity studies that require extended periods to observe systemic effects. Achieving stable multi-organ cultures is critical for modeling complex physiological processes such as the absorption, distribution, metabolism, excretion, and toxicity (ADMET) of compounds, which are fundamental to accurate preclinical safety assessment [36] [3]. Success hinges on replicating physiologically relevant organ-to-organ signaling and overcoming technical hurdles related to cell sourcing, medium composition, and environmental control.
This application note provides a detailed framework for establishing robust, long-term MOC cultures, using a specific immunotoxicity case study to illustrate key principles, protocols, and quantitative viability metrics.
Core Challenges in Long-Term MOC Culture
Sustaining MOCs for extended periods (typically >72 hours to several weeks) presents several interconnected challenges:
- Metabolic Imbalance: Different organ types possess varying metabolic rates and nutrient requirements. In a shared medium circulation system, rapidly metabolizing tissues can deplete essential nutrients and accumulate waste products, starving more sensitive organ models [3].
- Cumulative Toxicity of Materials: Some microfluidic chip materials, such as PDMS, can absorb critical compounds like drugs or hormones from the circulating medium, reducing their bioavailability and skewing experimental results [18].
- Loss of Organ-specific Functionality: Without precise physiological cues—such as organ-specific mechanical stimulation (e.g., cyclic stretch for lungs, shear stress for endothelium), and proper 3D polarization—tissues can dedifferentiate and lose their functional phenotype over time [36] [3].
Case Study: Systemic Immunotoxicity from Oral Exposure
A landmark study demonstrates a successful approach to a 72-hour MOC culture to investigate how nickel sulfate applied to reconstructed human gingiva (RHG) triggers Langerhans cell activation in distant reconstructed human skin (RHS) [5].
Key Quantitative Viability Metrics
Table 1: Key Viability and Metabolic Metrics from a 72-Hour MOC Culture [5]
| Parameter | Measurement Method | Results Indicating Stable Culture | Time Point |
|---|---|---|---|
| Glucose Uptake | Assay of medium compartment | Consistent consumption rate | Monitored over 72h |
| Lactate Production | Assay of medium compartment | Stable production rate | Monitored over 72h |
| Lactate Dehydrogenase (LDH) Release | Assay of medium compartment | Low/stable levels, indicating minimal cell death | Monitored over 72h |
| Tissue Histology | H&E staining | Preservation of stratified epithelial structure in both RHG and RHS | 72h |
| Immune Cell Function | mRNA analysis of dermal hydrogel (qPCR) | Increased activation markers (CD1a, CD207, HLA-DR, CD86) in RHS-LC post-exposure | 72h |
Experimental Workflow
The following diagram illustrates the integrated experimental workflow for the 72-hour immunotoxicity study, from platform setup to endpoint analysis.
Detailed Protocols for Long-Term MOC Culture
Protocol: Establishing a Stable Multi-Organ Culture
This protocol is adapted from the cited immunotoxicity study and commercial platform best practices [5] [3].
Objective: To co-culture reconstructed human gingiva (RHG) and reconstructed human skin with Langerhans cells (RHS-LC) in a dynamic flow system for 72 hours, maintaining tissue viability and functionality for immunotoxicity assessment.
Materials:
- MOC Platform: HUMIMIC Chip3plus or equivalent system with a closed-circuit microfluidic network [5].
- Biological Models: Pre-formed, matured RHG and RHS-LC tissue constructs.
- Cell Culture Medium: Serum-free, defined medium suitable for multi-organ culture (e.g., MCTT CMⓇ or other specialized formulations) [3].
- Peristaltic or Pneumatic Pump: Integrated into the MOC platform to provide continuous, low-shear flow.
- Humidified Incubator: Maintained at 37°C, 5% CO₂.
Procedure:
- Chip Priming: Flush all microfluidic channels of the sterile chip with culture medium to remove air bubbles and condition the system.
- Tissue Loading: Aseptically place the pre-formed RHG and RHS-LC constructs into their respective organ compartments on the chip.
- System Assembly: Connect the organ compartments via microfluidic channels according to the platform's instructions. Ensure a leak-proof seal.
- Initiate Dynamic Flow: Start the pump system to initiate circulation of culture medium between the organ compartments. A flow rate generating physiologically relevant shear stress (e.g., 0.5 - 4 dyn/cm²) is recommended.
- Stabilization Culture: Culture the connected system under dynamic flow for 24 hours to achieve stable, homeostatic conditions before applying any test substances. Monitor medium reservoirs for evaporation.
- Viability Monitoring (During Culture):
- Daily: Collect small aliquots (e.g., 100 µL) of circulating medium from the reservoir or a designated sampling port.
- Assay: Use colorimetric or fluorometric assays to quantify glucose consumption, lactate production, and LDH release as indicators of metabolic activity and cytotoxicity.
- Benchmarking: Compare values against established baselines for the specific tissue models used.
Protocol: Assessing Tissue Viability and Immune Response
Objective: To evaluate the structural integrity and functional immune activation in tissues after the 72-hour culture and toxicant exposure.
Materials:
- Tissue Fixative: e.g., 4% Paraformaldehyde (PFA) in PBS.
- RNA Extraction Kit: e.g., RNeasy Mini Kit (Qiagen).
- cDNA Synthesis Kit.
- qPCR Master Mix and primers for immune markers (CD1a, CD207, HLA-DR, CD86).
- Cytokine ELISA Kits: e.g., for IL-6, IL-8, etc.
Procedure:
- Terminate Culture: After 72 hours, stop the flow and carefully disassemble the chip.
- Tissue Processing:
- For Histology: Gently retrieve RHG and RHS-LC constructs and fix in 4% PFA for 24 hours. Process for standard paraffin embedding, sectioning, and Hematoxylin & Eosin (H&E) staining to assess tissue architecture.
- For Gene Expression: Separately dissect the epidermal and dermal (hydrogel) components of the RHS-LC model. Homogenize tissues and extract total RNA. Synthesize cDNA and perform quantitative PCR (qPCR) for Langerhans cell activation markers.
- For Cytokine Analysis: Analyze the stored medium samples using ELISA to quantify the release of pro-inflammatory cytokines.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for Long-Term MOC Immunotoxicity Studies
| Reagent / Material | Function in the Protocol | Specific Example / Note |
|---|---|---|
| HUMIMIC Chip3plus | Microfluidic platform providing a closed-circuit, dynamic flow environment for connecting organ models. | Enables systemic circulation and organ crosstalk [5]. |
| Serum-Free Defined Medium | Provides nutrients for multiple cell types without the variability and immunomodulatory effects of serum. | Critical for avoiding unintended immune cell activation and ensuring reproducibility [3]. |
| Reconstructed Human Gingiva (RHG) | A 3D model of the oral mucosa, serving as the site of topical exposure in the immunotoxicity workflow. | Contains stratified epithelium on a fibroblast-populated collagen hydrogel [5]. |
| Reconstructed Human Skin with Langerhans Cells (RHS-LC) | A 3D skin model containing integrated immune cells (MUTZ-3-derived LCs) as a reporter for systemic immunotoxicity. | Allows monitoring of LC activation and migration [5]. |
| LDH / Glucose / Lactate Assay Kits | Reagents for colorimetric/fluorometric quantification of metabolic markers in the circulating medium. | Used for non-destructive, real-time monitoring of multi-organ viability during culture [5]. |
| Low-Absorption Chip Materials (e.g., Chip-R1) | Rigid, non-PDMS plastic consumables for the MOC platform. | Minimizes nonspecific absorption of test compounds (e.g., drugs, cytokines), ensuring accurate dosing [18]. |
Long-term culture of multi-organ-on-chip systems for immunotoxicity studies is achievable through careful attention to platform design, continuous metabolic monitoring, and the use of highly functional 3D tissue models. The protocols and data presented here provide a validated roadmap for maintaining viability and capturing complex systemic immune responses, thereby enhancing the predictive power of preclinical safety assessments. As the field progresses, integrating automated monitoring and data analysis will be key to further improving the robustness and scalability of these advanced models.
Strategies for Standardization and Improving Reproducibility
The integration of multi-organ-on-chip (multi-OoC) systems into immunotoxicity studies represents a paradigm shift in preclinical research, offering a more physiologically relevant alternative to traditional animal models and static 2D cell cultures [37]. These sophisticated microfluidic devices emulate human organ-level functionality, enabling the investigation of complex inter-organ interactions following chemical or drug exposure [9]. However, the full potential of this technology is hampered by significant challenges in standardization and reproducibility, which are critical for regulatory acceptance and industrial adoption [38] [39].
Standardization in multi-OoC systems encompasses the establishment of uniform protocols, materials, and performance metrics to ensure consistent and comparable results across different laboratories and platforms [38]. For immunotoxicity studies specifically, this involves controlling numerous variables including cell sources, microfluidic parameters, culture media, and endpoint analyses to reliably assess how substances affect immune function [40]. The complexity of multi-OoC systems, which often aim to recapitulate human physiological interactions between different tissue types under dynamic flow conditions, further amplifies these challenges [5] [37].
This application note provides a comprehensive framework of strategies to address standardization and reproducibility challenges in multi-OoC platforms for immunotoxicity assessment. By implementing these structured approaches, researchers can enhance the reliability and regulatory acceptance of their immunotoxicity data, accelerating the integration of these advanced systems into drug development pipelines.
Key Standardization Challenges in Multi-OoC Immunotoxicity Studies
Technical and Biological Variability
The development and operation of multi-OoC systems involve numerous technical and biological parameters that introduce variability if not properly controlled. Table 1 summarizes the primary standardization challenges specific to immunotoxicity applications.
Table 1: Key Standardization Challenges in Multi-OoC Immunotoxicity Studies
| Challenge Category | Specific Challenges | Impact on Immunotoxicity Assessment |
|---|---|---|
| Device Materials & Fabrication | Absence of standardized materials; prevalent use of PDMS with small molecule absorption issues [38] | Alters drug/chemical bioavailability and pharmacokinetics; potentially masks immunotoxic effects |
| Microfluidic Parameters | Lack of agreed performance indicators for flow rates, shear stress, and tissue-to-media ratios [38] | Affects immune cell trafficking, cytokine distribution, and organ-organ communication |
| Cell Sources | Diversity in primary cells, iPSCs, and cell lines without standardized differentiation protocols [38] | Creates inconsistent immune cell phenotypes and functionalities across studies |
| Culture Media | No universal blood-mimetic medium capable of supporting diverse tissue types simultaneously [37] | Compromises tissue viability and function; particularly affects sensitive immune cells |
| Functional Endpoints | Organ-specific and application-specific endpoints without standardized assays or readouts [38] | Hinders comparison of immunotoxicity data across different platforms and studies |
| Data Integration | Complex data from multiple organs and immune parameters without standardized analysis pipelines [39] | Obscures system-level understanding of immunotoxic responses |
Analytical and Reporting Challenges
Beyond technical variability, the field lacks standardized analytical frameworks and reporting standards for multi-OoC immunotoxicity studies. The integration of advanced technologies such as biosensors, multimodal imaging, and artificial intelligence generates high-content data that requires standardized processing and interpretation [39]. Additionally, inconsistent reporting of experimental parameters, such as flow conditions, cell seeding densities, and differentiation protocols, impedes experimental replication and cross-platform validation [38].
Strategic Framework for Standardization
Device Characterization and Qualification
Establishing comprehensive device characterization protocols is fundamental to standardization. The technical performance of each OoC device should be rigorously quantified before biological experiments, with particular attention to parameters critical for immune function.
Table 2: Essential Technical Parameters for Device Qualification
| Parameter | Standardization Approach | Recommended Methods |
|---|---|---|
| Flow Rate Stability | Continuous monitoring with predefined acceptable variance (±5% of set point) | Integrated flow sensors; quantitative particle image velocimetry |
| Shear Stress | Computational modeling with experimental validation | CFD simulation combined with bead tracking or surface sensor measurements |
| Oxygen Concentration | Real-time monitoring in each organ chamber | Fluorescent-based sensors; optical fiber probes |
| Temperature Stability | Maintenance at 37°C ± 0.5°C | Integrated temperature sensors with feedback control to heating elements |
| pH Stability | Maintenance at 7.4 ± 0.2 in recirculating systems | pH sensors; periodic sampling and analysis |
| Molecule Absorption | Quantification for common materials (e.g., PDMS) | Measurement of reference compound recovery using LC-MS/MS |
Biological Standardization
Biological standardization ensures consistent cellular composition and function across experiments, which is particularly crucial for immunotoxicity assessment where immune cell responses must be reproducible.
Cell Source Standardization: Implement strict protocols for cell sourcing, differentiation, and characterization. For immune components, this includes defining specific markers for dendritic cells, lymphocytes, and macrophages derived from primary tissues or iPSCs [5] [16]. Regular functional validation through challenge with reference immunomodulators should be performed.
Culture Media Harmonization: Develop optimized universal media formulations that support all integrated tissue types while maintaining immune competence. Systematic testing of basal media supplements should identify compositions that maintain tissue functionality without suppressing immune responses [37].
Functional Benchmarking: Establish standardized challenge tests using reference compounds with known immunotoxic profiles (e.g., immunosuppressants, sensitizers) to qualify each new multi-OoC platform or batch of cells [40]. System responsiveness should be demonstrated through appropriate endpoint measurements.
The following workflow diagram illustrates the comprehensive standardization strategy for multi-OoC immunotoxicity studies:
Experimental Protocols for Reproducible Immunotoxicity Assessment
Protocol: Systemic Immunotoxicity Assessment Using Connected Barrier Models
This protocol adapts the methodology described by CeÌline et al. for investigating how oral exposure to metals causes systemic toxicity leading to Langerhans cell activation in skin [5]. The approach connects reconstructed human gingiva (RHG) with reconstructed human skin containing Langerhans cells (RHS-LC) in a multi-OoC platform.
Materials and Equipment
Table 3: Research Reagent Solutions for Multi-OoC Immunotoxicity Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Multi-OoC Platform | HUMIMIC Chip3plus (TissUse) or equivalent [5] | Provides microfluidic environment for organ interconnection |
| Reconstructed Tissues | Reconstructed human gingiva (RHG), Reconstructed human skin with Langerhans cells (RHS-LC) [5] | Represents barrier organs with immune components |
| Immune Cells | MUTZ-3-derived Langerhans cells (MUTZ-LC) [5] | Provides standardized source of antigen-presenting cells |
| Culture Media | Tissue-specific differentiation media; universal circulation medium [5] [37] | Supports tissue viability and function during interconnection |
| Test Compounds | Nickel sulfate; other metal salts; reference immunotoxicants [5] [40] | Positive controls for immunotoxicity assessment |
| Viability Assays | Glucose consumption, lactate production, LDH release kits [5] | Monitors tissue viability during dynamic culture |
| Molecular Biology | RNA isolation kits, cDNA synthesis kits, qPCR reagents [5] | Measures immune activation markers |
| Immunoassays | ELISA kits for cytokines (IL-1β, IL-6, IL-8, TNF-α) [5] | Quantifies inflammatory mediator release |
Procedure
Day 0: Platform Assembly and Tissue Integration
- Sterilize the multi-OoC device (e.g., HUMIMIC Chip3plus) using appropriate methods (UV irradiation, ethanol flushing).
- Integrate pre-differentiated reconstructed human gingiva (RHG) into the first tissue chamber.
- Integrate reconstructed human skin containing MUTZ-3-derived Langerhans cells (RHS-LC) into the second tissue chamber.
- Connect chambers with microfluidic channels and establish basal medium flow at 25 µL/h.
- Place the assembled platform in a humidified incubator at 37°C, 5% CO₂.
Day 1: System Equilibrium and Baseline Measurements
- Continue dynamic culture with tissue-specific medium for 24 hours to achieve stable culture conditions.
- After 24 hours, collect effluent medium samples for baseline measurements.
- Measure glucose uptake, lactate production, and lactate dehydrogenase (LDH) release as viability indicators.
- Assess baseline cytokine levels (IL-1β, IL-6, IL-8, TNF-α) in effluent medium via ELISA.
- Document system stability before compound exposure.
Day 2: Compound Exposure
- Prepare fresh solution of nickel sulfate (or other test compound) in appropriate vehicle.
- Apply compound topically to the reconstructed human gingiva (RHG) tissue at concentrations based on preliminary range-finding studies.
- Maintain flow rate at 25 µL/h for 24-hour exposure period.
- For controls, apply vehicle only to RHG tissues in parallel systems.
Day 3: Post-Exposure Analysis
- After 24-hour exposure, switch to compound-free medium.
- Continue dynamic culture for additional 24 hours to assess delayed responses.
- Collect medium samples at defined intervals for subsequent cytokine analysis.
Day 4: Endpoint Analysis
- Terminate experiment after total 72-hour culture period (24h stabilization + 24h exposure + 24h post-exposure).
- Carefully harvest tissues from both chambers for analysis.
- Process tissues for:
- Histological evaluation (H&E staining)
- Immunohistochemistry for immune cell markers (CD1a, CD207, HLA-DR)
- RNA extraction and qPCR analysis of activation markers (CD1a, CD207, HLA-DR, CD86)
- Migration assays to quantify Langerhans cell movement from epidermis to dermis
Data Analysis and Interpretation
- Calculate glucose consumption and lactate production rates as indicators of metabolic activity.
- Normalize LDH release to total tissue protein content to quantify cytotoxicity.
- Express cytokine levels as fold-change compared to vehicle-treated controls.
- Analyze immune cell activation through:
- Migration index (ratio of Langerhans cells in dermis versus epidermis)
- Activation marker expression (qPCR data normalized to housekeeping genes)
- Compare results to established positive controls (known immunotoxicants) and negative controls (vehicle alone).
Protocol: Standardized Quality Control for Multi-OoC Systems
Regular quality control assessments are essential to ensure system reproducibility. This protocol outlines key quality control measures that should be implemented routinely.
Materials and Equipment
- Reference compounds with known immunotoxic profiles (e.g., lipopolysaccharide (LPS) for innate immune activation, nickel sulfate for sensitization)
- Barrier integrity assay reagents (e.g., FITC-dextran, TEER measurement equipment)
- Viability/cytotoxicity assay kits
- Cytokine ELISA kits for key inflammatory markers
- Microfluidic flow sensors and bubble detectors
Procedure
Barrier Function Assessment (Weekly)
- For barrier tissues (skin, gingiva, intestinal models), measure transepithelial electrical resistance (TEER) using microelectrodes.
- Perform permeability assays using fluorescent tracers (e.g., FITC-dextran, 4 kDa).
- Document baseline values and establish acceptance criteria for each tissue type.
Flow Rate Verification (Before Each Experiment)
- Calibrate and verify flow rates using integrated sensors or external flow measurement tools.
- Confirm absence of bubbles in microfluidic circuits that could disrupt flow dynamics.
- Document flow rate stability over a 24-hour period.
System Sterility Checks (Weekly)
- Collect effluent medium samples for microbial culture.
- Monitor for pH shifts or turbidity that may indicate contamination.
- Visually inspect for fungal growth under microscope.
Reference Compound Responses (Monthly)
- Challenge systems with reference immunotoxicants at established concentrations.
- Quantify expected immune activation endpoints (cytokine release, immune cell activation).
- Compare response magnitudes to historical data for system performance tracking.
Data Analysis and Interpretation
- Establish quality control charts for key parameters (barrier function, flow rates, reference compound responses).
- Define acceptance ranges for each parameter based on cumulative historical data.
- Implement corrective action procedures when parameters fall outside acceptance ranges.
Implementation Considerations
Integration with Existing Frameworks
Standardization efforts for multi-OoC immunotoxicity assessment should align with existing regulatory frameworks and testing guidelines. The tiered testing approach traditionally used for immunotoxicity evaluation can be adapted for OoC applications [40]. Initial screening (Tier 1) should include hematological parameters and histopathology, while more detailed evaluation (Tier 2) can incorporate immune function assessments such as lymphocyte proliferation and cytokine production measured in multi-OoC platforms.
Data Standardization and Reporting
Consistent data reporting is equally important as experimental standardization. Minimum information standards should be developed specific to multi-OoC immunotoxicity studies, including:
- Detailed device specifications (materials, dimensions, surface treatments)
- Cell source information (donor characteristics, passage number, differentiation protocols)
- Microfluidic parameters (flow rates, shear stresses, volume ratios)
- Environmental conditions (temperature, gas concentrations, humidity)
- Experimental timeline (stabilization, exposure, and analysis periods)
- Positive and negative control responses
- Analytical methods and normalization procedures
Technology Integration for Enhanced Reproducibility
Emerging technologies offer promising approaches to address reproducibility challenges in multi-OoC systems. Table 4 highlights key technologies and their applications for standardization.
Table 4: Enabling Technologies for Enhanced Reproducibility in Multi-OoC Systems
| Technology | Application in Standardization | Benefits for Immunotoxicity Studies |
|---|---|---|
| Bioprinting [39] | Precise, reproducible spatial organization of multiple cell types | Consistent tissue architecture; standardized immune cell positioning |
| Integrated Sensors [39] | Real-time monitoring of physiochemical parameters (Oâ‚‚, pH, metabolites) | Continuous quality control; immediate detection of system deviations |
| Multimodal Imaging [39] | Standardized image acquisition and analysis of immune cell trafficking | Quantitative assessment of immune cell migration and localization |
| AI/ML Algorithms [39] | Automated analysis of complex datasets from multiple organs | Objective, standardized data interpretation; identification of subtle immunotoxic effects |
| Modular Design [37] | Interchangeable organ modules with standardized interfaces | Flexible yet reproducible system configuration for different study designs |
Standardization and reproducibility in multi-organ-on-chip systems for immunotoxicity assessment require a systematic, multi-faceted approach addressing technical, biological, and analytical parameters. By implementing the strategies outlined in this application note—comprehensive device characterization, biological standardization, rigorous quality control protocols, and consistent reporting frameworks—researchers can significantly enhance the reliability and regulatory acceptance of multi-OoC platforms.
The future of reproducible multi-OoC technology will likely involve closer collaboration between academic researchers, industry partners, and regulatory bodies to establish consensus standards. Organizations such as the European Organ-on-Chip Society (EUROoCS) and the U.K. Organ-on-a-Chip Technologies Network are already facilitating this dialogue [37]. As these efforts mature, standardized multi-OoC platforms will become increasingly valuable tools for screening immunotoxicity during drug development and chemical safety assessment, potentially reducing reliance on animal testing while providing more human-relevant data.
The predictive power of preclinical drug safety testing, particularly for immunotoxicity, is often hampered by the limited biological complexity of traditional models. Multi-organ-on-a-chip (multi-OoC) systems are emerging as a transformative technology that can bridge this gap by recapitulating systemic human physiology in vitro [1]. A significant frontier in this field is the precise incorporation of immune cells, stromal components, and the microbiome—key players in drug responses and toxicity pathways. These elements are critical for modeling the immune system's role as a systemic communicator between organs and for understanding how host-microbiome interactions can influence drug metabolism and safety [41] [42] [43]. This application note provides detailed protocols and strategies for integrating these complex biological components into multi-OoC platforms to advance the accuracy of immunotoxicity studies.
Experimental Protocols for Incorporating Biological Complexity
Protocol for Establishing an Immune-Competent Multi-Organ Chip
This protocol outlines the development of a multi-OoC system featuring a vascular channel shared between organ-specific compartments, enabling the study of immune cell trafficking and systemic immunotoxicity.
Materials and Reagents:
- Microfluidic device (e.g., PDMS-based chip with multiple chambers or a modular system [44] [18])
- Primary human endothelial cells (e.g., HUVEC)
- Organ-specific primary cells or stem cell-derived lineages (e.g., hepatocytes, renal tubular cells)
- Immune cells (e.g., peripheral blood mononuclear cells (PBMCs) or isolated monocytes)
- Endothelial cell growth medium (e.g., EGM-2)
- Organ-specific media
- Cell culture medium (e.g., RPMI-1640)
- Fetal Bovine Serum (FBS)
- Phosphate Buffered Saline (PBS)
- Fluorescent cell tracker dyes (e.g., CFSE)
- Adhesion molecules (e.g., recombinant ICAM-1, VCAM-1)
Procedure:
- Device Preparation: Sterilize the microfluidic device using UV light for 30 minutes per side. Coat the vascular channel with a fibronectin solution (10 µg/mL in PBS) for at least 2 hours at 37°C to promote endothelial cell adhesion.
- Endothelial Barrier Seeding: Introduce a suspension of human endothelial cells (5-10 x 10^6 cells/mL) into the vascular channel. Allow cells to adhere for 15-20 minutes before connecting the chip to a perfusion system. Culture under continuous flow (shear stress of 1-4 dyn/cm²) for 3-5 days to form a confluent, mature endothelial barrier [1] [9].
- Organ Compartment Seeding: In separate, fluidically connected organ chambers, seed organ-specific cells. For instance, seed primary human hepatocytes in a collagen-Matrigel mix in the "liver" chamber and primary renal proximal tubular epithelial cells in the "kidney" chamber. Use organ-specific media and allow the tissues to differentiate for 5-7 days [1].
- Immune Cell Introduction: Isolate PBMCs from whole blood using density gradient centrifugation. Resuspend PBMCs (1-2 x 10^6 cells/mL) in endothelial cell growth medium supplemented with 2% FBS. Gently introduce the immune cell suspension into the vascular channel via perfusion.
- Immunotoxicity Testing: After 24 hours of immune cell incorporation, introduce the test compound into the vascular circulation medium at the desired concentration. Perfuse the system for 24-72 hours.
- Real-Time Analysis:
- Immune Cell Adhesion & Extravasation: Monitor the behavior of fluorescently labeled immune cells in real-time using on-chip or confocal microscopy. Quantify adhesion to the endothelium and migration into organ compartments [42].
- Endpoint Analysis: Collect effluent from the vascular and organ compartments for cytokine analysis (e.g., IL-6, TNF-α, IFN-γ) via ELISA. Fix the tissues for immunostaining of cell-specific markers (e.g., CD45 for immune cells, ZO-1 for endothelial barriers) [18].
Protocol for Integrating a Functional Microbiome in a Gut-on-a-Chip System
This protocol details the co-culture of a complex human gut microbiome with an immune-competent intestinal epithelium to study microbiome-drug-immune interactions.
Materials and Reagents:
- Gut-on-a-Chip device (e.g., Emulate's Intestine-Chip or a custom two-channel PDMS chip [18] [43])
- Human primary intestinal epithelial cells or induced pluripotent stem cell (iPSC)-derived intestinal organoids
- Primary human intestinal microvascular endothelial cells
- Commensal and pathogenic bacterial strains (e.g., Faecalibacterium prausnitzii, Escherichia coli)
- Reduced growth factor Matrigel
- Intestinal epithelial cell medium
- Anaerobic bacterial culture medium
- Antibiotic-Anatimycin solution
Procedure:
- Differentiation of the Intestinal Epithelium: On one side of a porous membrane, seed human intestinal epithelial cells. If using organoids, dissociate them into single cells and seed at high density. Culture under continuous flow and cyclic mechanical deformation (10% strain, 0.15 Hz) to promote polarization and the formation of intestinal villi and a mucus layer [43].
- Establishment of the Endothelial Layer: Seed human intestinal endothelial cells on the opposite side of the membrane to create a vascular channel. Culture under flow to form a confluent layer.
- Microbiome Preparation: Grow bacterial strains anaerobically to mid-log phase. Centrifuge, wash, and resuspend in anaerobic culture medium at a high density (e.g., 10^8 CFU/mL). Combine different strains to create a defined microbial community.
- Introduction of the Microbiome: Introduce the bacterial suspension into the epithelial lumen channel. To establish stable co-culture, temporarily switch the perfusion of the epithelial channel to a very low flow rate or use a stop-flow strategy for 4-6 hours to allow for bacterial adhesion and colonization [43].
- Immune Cell Recruitment: Introduce human immune cells (e.g., monocyte-derived macrophages or dendritic cells) into the vascular channel. The presence of the microbiome and its metabolites will stimulate the endothelium to express adhesion molecules, recruiting immune cells [42].
- Perturbation and Analysis:
- Barrier Function: Measure transepithelial electrical resistance (TEER) regularly to monitor barrier integrity.
- Host-Microbiome-Immune Crosstalk: Collect effluent from both channels for metabolomic analysis (e.g., SCFA quantification) and cytokine profiling.
- Spatial Analysis: Fix the chip at endpoint and perform fluorescence in situ hybridization (FISH) combined with immunostaining to visualize the spatial distribution of bacteria relative to the epithelium and immune cells.
Research Reagent Solutions and Materials
Table 1: Essential Research Reagents for Complex OoC Models
| Reagent/Material | Function in the Model | Example Product/Catalog Number |
|---|---|---|
| Primary Human Endothelial Cells | Forms the vascular barrier; regulates immune cell trafficking and recruitment. | HUVEC, TeloHAEC |
| Primary Organ-Specific Cells | Recapitulates the functional unit of a target organ (e.g., liver, kidney) for metabolism and toxicity studies. | Primary Human Hepatocytes, Renal Proximal Tubular Epithelial Cells |
| Peripheral Blood Mononuclear Cells (PBMCs) | Source of multiple immune cell types (T cells, B cells, monocytes) for modeling systemic immune responses. | Isolated from whole blood or commercially available |
| Stem Cell-Derived Intestinal Organoids | Provides a patient-specific, physiologically relevant intestinal epithelium containing multiple cell types (enterocytes, goblet, Paneth cells). | iPSC-derived intestinal organoids |
| Defined Microbial Communities | Represents the human gut microbiome for studying host-microbe-immune interactions and drug metabolism. | Synthetic Microbial Communities (e.g., SIHUMI) |
| Matrigel / Hydrogels | Provides a 3D extracellular matrix (ECM) scaffold to support complex tissue morphogenesis and cell-ECM interactions. | Corning Matrigel, Fibrin I, Collagen I |
| Polydimethylsiloxane (PDMS) | The most common elastomer for fabricating OoC devices; optically clear, gas-permeable, and biocompatible. | SYLGARD 184 Silicone Elastomer Kit |
| Chip-R1 Rigid Chip | A non-PDMS consumable with low drug-absorbing properties, ideal for ADME and toxicology studies. | Emulate Bio Chip-R1 [18] |
Multi-Organ Integration and Systemic Immunotoxicity Assessment
Integrating individual immune-competent organ models into a multi-OoC platform is crucial for detecting systemic immunotoxicity. The configuration of these platforms can vary from integrated body-on-a-chip devices to interconnected modular setups [1].
Table 2: Strategies for Coupling Organ Models in Multi-OoC Platforms
| Coupling Configuration | Description | Advantages | Considerations for Immunotoxicity |
|---|---|---|---|
| Shared Common Media Reservoir | Effluent from all organ compartments mixes in a single reservoir before being recirculated. | Simple design, easy to implement. | Does not model organ-specific vascular barriers; immune cells have non-physiological access to all tissues. |
| Direct Fluidic Interconnection | Organ compartments are connected in a physiologically relevant sequence (e.g., gut-liver-kidney) via microchannels. | Models first-pass metabolism; allows for sequential processing of compounds. | Requires careful balancing of flow rates and organ sizes; may lack endothelial barriers between organs. |
| Vascularized Interlinks | Organ-specific compartments are connected via a common, continuous endothelialized vascular channel [1]. | Most physiologically relevant; models immune cell extravasation; maintains tissue-specific endothelial barriers. | Technically complex; requires a universal endothelial cell type or co-culture strategies. |
The following diagram illustrates the workflow for designing and conducting an immunotoxicity study using a multi-OoC platform with vascularized interlinks.
Immunotoxicity Study Workflow in Multi-OoC
Key metrics for systemic immunotoxicity assessment in such a system include:
- Cytokine Storm Signature: System-wide measurement of pro-inflammatory cytokines (e.g., IL-6, IL-1β, TNF-α) in the recirculating medium.
- Immune Cell Activation: Flow cytometry analysis of immune cells recovered from the vascular effluent for activation markers (e.g., CD69, CD25).
- Organ-Specific Damage: Measurement of tissue-specific damage biomarkers (e.g., ALT for liver, KIM-1 for kidney) in the medium and via tissue staining.
- Barrier Integrity Loss: Real-time measurement of TEER in barrier tissues (gut, vascular, blood-brain barrier) and quantification of fluorescent dextran leakage.
Data Presentation and Analysis
Quantitative data generated from these complex models require robust analysis. The table below summarizes key data types and analytical methods.
Table 3: Quantitative Data Analysis in Immune-Competent OoC Models
| Data Type | Measurement Technique | Key Parameters | Interpretation in Immunotoxicity |
|---|---|---|---|
| Immune Cell Dynamics | Live-cell imaging / Time-lapse microscopy | Velocity, migration track, transendothelial migration rate | Compound-induced inhibition or enhancement of immune cell function. |
| Cytokine Secretion | Multiplex ELISA / Luminex | Concentration (pg/mL) of IL-6, IL-8, TNF-α, IFN-γ, IL-10 | Pro-inflammatory vs. anti-inflammatory response; identification of a cytokine release syndrome (CRS) signature. |
| Barrier Function | Transepithelial/Transendothelial Electrical Resistance (TEER) | Resistance (Ω·cm²) over time | Compound-induced barrier disruption, a key event in inflammation and toxicity. |
| Metabolomic Profile | Mass Spectrometry (LC-MS/GC-MS) | Concentration of SCFAs, bile acids, neurotransmitters, drugs/metabolites | Impact of compound on host and microbial metabolism; identification of toxic metabolites. |
| Cell Viability | Calcein-AM/EthD-1 staining / LDH assay | Percentage of live/dead cells | Direct cytotoxic effect of the compound on specific cell types (organ-specific toxicity). |
| Gene Expression | RNA Sequencing / qRT-PCR | Fold-change in gene expression of immune and toxicity markers | Pathways analysis to elucidate mechanisms of immunotoxicity. |
Leveraging AI and Biosensors for Real-Time Monitoring and Data Analysis
The integration of artificial intelligence (AI) with biosensor-equipped multi-organ-on-a-chip (multi-OoC) systems is establishing a new paradigm for immunotoxicity studies in preclinical drug development. These advanced microphysiological systems (MPS) mimic human physiological responses more accurately than traditional 2D cultures or animal models, which often fail to predict human-specific immunotoxic outcomes due to species differences [45] [46]. The core of this technological synergy lies in the continuous, real-time monitoring of cellular and microenvironmental parameters by embedded biosensors, generating complex, high-volume datasets. AI and machine learning algorithms are crucial for interpreting this data, identifying subtle patterns indicative of immunotoxicity that might escape conventional analysis. This Application Note provides detailed protocols for implementing these integrated systems, specifically focusing on their application for immunotoxicity assessment within the context of multi-organ-on-a-chip research.
Technical Specifications of Integrated Biosensors for OoC
Embedding biosensors within OoC platforms enables direct, non-invasive, and real-time monitoring of cellular and microenvironmental parameters. This is critical for assessing immunotoxicity, as it allows researchers to capture dynamic cellular responses to compounds without disruptive end-point assays [45] [46]. The selection of an appropriate biosensor depends on the specific parameter being measured and the design of the OoC.
Table 1: Biosensor Types and Their Applications in OoC Immunotoxicity Studies
| Biosensor Type | Measured Parameters | Working Principle | Advantages for Immunotoxicity | Integrated Example |
|---|---|---|---|---|
| Electrochemical | Metabolites (Glucose, Lactate), Cytokines, pH | Measures electrical current/ potential change from biochemical reactions [46]. | High sensitivity, miniaturization, wide dynamic range [46]. | Monitoring metabolic shift in liver spheroids indicating compound toxicity [46]. |
| Electrical (Impedance) | Barrier Integrity, Cell Viability | Measures electrical impedance across cell layers; disruption indicates compromised barriers [45]. | Label-free, continuous monitoring of tissue health. | Real-time assessment of gut or blood-brain barrier integrity during immune cell recruitment [45]. |
| Optical | Oxygen, Specific Biomarkers | Fluorescence or luminescence quenching by target molecules (e.g., oxygen) [46]. | Non-invasive, spatial mapping of analytes. | Phosphorescence-based O2 sensors to monitor metabolic zonation and mitochondrial dysfunction in Liver-Chips [46]. |
Beyond the sensor type, the material of the OoC device itself is a critical consideration. As outlined in Table 2, common materials like PDMS, while popular, have limitations such as drug absorption, which can skew toxicity readouts. Recent innovations like the Chip-R1, a rigid, non-PDMS chip, address this by minimizing drug absorption, thereby improving the precision of toxicology and ADME studies [18].
Table 2: Common OoC Fabrication Materials and Their Properties
| Material | Advantages | Limitations / Impact on Assays |
|---|---|---|
| PDMS | Optically transparent, gas permeable, biocompatible, elastic [44]. | Hydrophobicity; strong adsorption of small molecule drugs, potentially altering effective drug concentrations in immunotoxicity assays [44]. |
| PMMA/Plastics | Biocompatible, optically transparent, low drug absorption [44]. | Low gas permeability; not elastic [44]. |
| Hydrogels | High biocompatibility; mimic extracellular matrix (ECM); tuneable properties [44]. | Inadequate mechanical properties for some architectures; potential degradation by-products can alter local pH [44]. |
| Chip-R1 (Rigid Chip) | Minimally drug-absorbing plastic [18]. | Modified vascular channel design enables physiologically relevant shear stress for immune cell studies [18]. |
Experimental Protocol: Real-Time Immunotoxicity Assessment in a Multi-OoC Platform
This protocol details the setup and execution of an immunotoxicity study using a multi-OoC platform (e.g., a Lymph Node-Chip connected to a Liver-Chip) integrated with electrochemical and impedance biosensors, with data output fed into an AI analysis pipeline.
Safety and Pre-Experiment Preparations
- Personal Protective Equipment (PPE): Lab coat, gloves, and safety glasses.
- Biohazard Procedures: All procedures involving human cells must be conducted in a Class II biosafety cabinet using standard sterile techniques. Contaminated waste must be autoclaved before disposal.
- Software Setup: Ensure data acquisition software for the biosensor platform and AI/ML analysis environment (e.g., Python with TensorFlow/PyTorch, or R) are installed and configured.
Materials and Reagent Solutions
Table 3: Research Reagent Solutions for OoC Immunotoxicity Assays
| Item Name | Function / Description | Application Context in Protocol |
|---|---|---|
| Chip-R1 Consumable | Rigid OoC fabricated from minimally drug-absorbing plastic [18]. | Serves as the physical platform for the Lymph Node-Chip and Liver-Chip in the multi-OoC system. |
| AVA Emulation System | A 3-in-1 platform for high-throughput OoC experiments, combining microfluidic control for 96 chips with automated imaging [18]. | Provides the instrumentation for perfusion control, automated imaging, and environmental control (incubation) for the multi-OoC system. |
| Lato Font | The specific font used for all chart and figure text to ensure a uniform look [47]. | Used for generating all data visualization outputs (e.g., from R or Python) to maintain professional and consistent labeling. |
| PDMS | Polydimethylsiloxane; a common, gas-permeable, and transparent elastomer for OoC fabrication [44]. | May be used for specific chip components requiring elasticity, though its drug absorption liability should be considered. |
| GelMA Hydrogel | Gelatin methacryloyl; a semi-synthetic hydrogel mimicking ECM characteristics [44]. | Used as a 3D cell culture matrix within the Lymph Node-Chip to support immune cell interactions and tissue architecture. |
Step-by-Step Procedure
Part A: OoC Platform Priming and Cell Seeding (Day 1)
- Chip Sterilization: Place the sterile multi-OoC device (e.g., Chip-R1) under the biosafety cabinet. If required, UV-sterilize the fluidic channels for 20 minutes.
- Matrix Coating: For the Liver-Chip chamber, introduce an appropriate extracellular matrix (e.g., Collagen I) into the top channel and incubate for 1 hour at 37°C. For the Lymph Node-Chip, load GelMA hydrogel precursor mixed with dendritic cells into the central chamber and crosslink under UV light per the manufacturer's instructions.
- Priming: Flush all microfluidic channels with pre-warmed (37°C) cell culture medium at a low flow rate (e.g., 5 µL/hour) for 2 hours to remove air bubbles and condition the surface.
- Cell Seeding:
- Liver-Chip: Introduce primary human hepatocytes or HepaRG cells into the top (parenchymal) channel and primary liver sinusoidal endothelial cells into the bottom (vascular) channel. Allow cells to adhere for 6 hours under static conditions.
- Lymph Node-Chip: Seed primary human T cells into the hydrogel matrix containing dendritic cells.
- Initiate Perfusion: After cell adhesion, connect the chip to the perfusion system (e.g., the AVA Emulation System) and initiate a low flow rate (e.g., 10 µL/hour) of culture medium. Gradually increase to the maintenance flow rate (e.g., 30-50 µL/hour) over 12 hours.
Part B: Biosensor Calibration and Baseline Data Acquisition (Day 2-4)
- Sensor Calibration: Follow manufacturer protocols to calibrate integrated biosensors. For optical oxygen sensors, use media equilibrated with 0%, 5%, and 21% O2. For glucose/lactate sensors, use standards of known concentration.
- Baseline Monitoring: Allow the multi-OoC system to stabilize and form mature tissue structures for 48-72 hours. During this time, continuously record baseline data from all biosensors (impedance, O2, metabolites). Automated imaging within the AVA system should also capture baseline morphology.
Part C: Compound Dosing and Real-Time Immunotoxicity Monitoring (Day 5)
- Administer Compound: Introduce the test compound (e.g., a new biologic drug candidate) into the perfusate flowing into the Lymph Node-Chip vascular channel. Include a vehicle control in a parallel run.
- Continuous Data Acquisition: Activate high-frequency data logging from all integrated biosensors (impedance, electrochemical, optical). The AI-ready AVA system can generate >30,000 time-stamped data points in a typical experiment [18]. Monitor for:
- A drop in impedance in the Lymph Node-Chip, indicating immune cell activation or death.
- A surge in cytokine levels (via electrochemical sensors).
- Changes in oxygen consumption and lactate production in the Liver-Chip, suggesting off-target metabolic toxicity.
Part D: AI-Enabled Data Analysis and Interpretation (Post-Experiment)
- Data Preprocessing: Use scripts to normalize the high-volume, multi-modal data (sensor readings, image features) and align time stamps.
- Model Inference: Feed the preprocessed data stream into a pre-trained machine learning model (e.g., a recurrent neural network) to classify the immune response.
- Output and Visualization: The model will output a probability score for immunotoxicity and highlight the key features (e.g., "85% probability of cytokine release syndrome, driven by early IL-6 spike and T-cell impedance drop"). Generate visualizations per the style guide in [47].
Diagram 1: Immunotoxicity assay workflow.
AI Data Processing and Analysis Workflow
The raw data from the OoC biosensors is a continuous, high-dimensional stream. The workflow below, illustrated in Diagram 2, transforms this raw data into an actionable immunotoxicity prediction.
- Data Acquisition & Fusion: The system ingests time-series data from electrochemical (metabolites, cytokines), electrical (impedance), and optical (O2) sensors, along with time-stamped microscopic images from the automated system.
- Preprocessing & Feature Engineering: Raw signals are cleaned (noise filtering, baseline correction) and synchronized. Key features are extracted, such as the rate of impedance change, area-under-the-curve for cytokine spikes, and metabolic flux ratios from the Liver-Chip.
- AI Model Analysis: The processed features are input into a machine learning model. For temporal data, a Recurrent Neural Network (RNN) or Long Short-Term Memory (LSTM) network is ideal for identifying patterns over time. The model is trained on historical data from compounds with known immunotoxicity profiles.
- Prediction & Visualization: The model outputs a quantitative immunotoxicity risk score and classifies the type of response (e.g., cytokine release, immunosuppression). Results are visualized in dashboards for researcher interpretation, adhering to data visualization best practices for clarity [48] [47].
Diagram 2: AI data processing pipeline.
Benchmarking MOC Performance: Validation, Regulatory Acceptance, and Future Outlook
The FDA Modernization Act 2.0, signed into law in December 2022, marks a foundational shift in U.S. preclinical drug development regulation by removing the long-standing mandatory requirement for animal testing and explicitly allowing the use of human-biology-based New Approach Methodologies (NAMs) [49]. This legislative change enables drug sponsors to use sophisticated tools like multi-organ-on-chip (MOC) systems for regulatory submissions. Concurrently, the FDA's ISTAND Pilot Program (Innovative Science and Technology Approaches for New Drugs) provides a critical pathway for qualifying these novel drug development tools (DDTs) for specific regulatory uses [50] [51]. For researchers focused on immunotoxicity studies, understanding the intersection of these two initiatives is essential for designing clinically predictive, human-relevant studies that meet evolving regulatory standards.
Regulatory Framework Analysis
FDA Modernization Act 2.0: From Animal Mandate to Human Biology
The Act amended the 1938 Federal Food, Drug, and Cosmetic Act, replacing the phrase "preclinical tests (including tests on animals)" with the broader term "nonclinical tests" [49]. This legally recognizes microphysiological systems (MPS), including organ-on-chip models, as valid for Investigational New Drug (IND) applications [52]. The primary impact for immunotoxicity researchers is the freedom to design studies using human immune-relevant models without automatic recourse to animal studies, particularly for therapeutics like monoclonal antibodies where species-specific differences often render animal data misleading [53] [54].
ISTAND Program: A Pathway for Qualification
ISTAND, now a permanent DDT qualification program, specifically evaluates novel tools that don't fit existing biomarker or clinical outcome assessment pathways [51]. Its relevance to MOC systems was demonstrated in September 2024, when it accepted the first organ-on-a-chip technology—a human Liver-Chip for predicting drug-induced liver injury (DILI)—into its qualification process [55]. For an immunotoxicity-focused MOC system, successful qualification through ISTAND would provide regulatory certainty that the tool can be relied upon for a specific context of use (COU) in drug development [50].
Recent FDA Implementation Actions
In April 2025, the FDA released a comprehensive roadmap outlining its plan to phase out animal testing, starting with monoclonal antibodies and other biologics [53] [56]. The agency is encouraging the use of AI-based computational models, organoid toxicity testing, and MPS to replace traditional animal studies [53] [54]. This creates an immediate opportunity for immunotoxicity researchers to submit MOC data alongside or in place of animal data, particularly for drugs targeting human-specific immune pathways.
Application Notes: De-Risking Immunotoxicity Studies with MOC Systems
Strategic Advantages for Immunotoxicity Assessment
Multi-organ-on-chip systems offer distinct advantages for immunotoxicity assessment by preserving human-specific immune responses that are often lost in animal models. The case of TGN1412, a monoclonal antibody that caused catastrophic cytokine release syndrome in humans despite passing animal tests in non-human primates, underscores the critical need for human-relevant models [54]. By integrating functional human immune components with other organ systems, MOC platforms can detect systemic immune-mediated toxicities, including:
- Cytokine Release Syndrome (CRS)
- Immune Cell Recruitment and Tissue Infiltration
- Off-Target Immunomodulation
- Autoantibody Generation
Regulatory Context of Use Considerations
When designing MOC studies for regulatory submission, precisely defining the context of use is essential. The qualified COU for the Emulate Liver-Chip accepted into ISTAND is "to assess the risk of DILI in adults to create relevant data for a drug's IND submission" and specifically for evaluating "a drug's relative DILI risk compared to the risk of a drug from the same class" [55]. For immunotoxicity studies, potential COUs could include:
- "Screening for CRS potential of immunomodulatory biologics prior to first-in-human trials"
- "Ranking lead candidates by immunotoxic potential within a therapeutic class"
- "Mechanistic investigation of immune-mediated adverse drug reactions"
Table 1: Quantitative Performance Benchmarks for Human-Relevant Immunotoxicity Models
| Model Type | Predicted Endpoint | Sensitivity | Specificity | Validation Status |
|---|---|---|---|---|
| Liver-Chip | Drug-Induced Liver Injury | 87% | 100% | ISTAND LOI Accepted [52] |
| Human Cytokine Release Assay (CRA) | Cytokine Storm | Not Specified | Not Specified | Standard Post-TGN1412 [54] |
| In Silico Model (CATMoS) | Acute Toxicity | 85% | Not Specified | Retrospective Validation [54] |
Integrated Testing Strategies
Regulatory acceptance will likely follow a "weight of evidence" approach combining multiple NAMs [49]. A comprehensive immunotoxicity assessment strategy could integrate:
- MOC Systems for complex immune-organ interactions
- In Silico Prediction of immunogenicity from amino acid sequences
- Ex Vivo Human Tissue Slices for localized toxicity
- High-Throughput Screening with iPSC-derived immune cells
This combinatorial approach addresses the limitation that no single NAM can currently replicate the full complexity of a human immune system [49].
Experimental Protocols for MOC Immunotoxicity Studies
Protocol: Cytokine Release Syndrome (CRS) Assessment
Purpose: To predict the potential for a therapeutic to cause CRS using a multi-organ platform incorporating immune components.
Materials:
- MOC device with endothelialized vasculature and parenchymal chambers
- Perfusion system with controlled flow rates (typical range: 0.1-1.0 mL/min)
- Cryopreserved human PBMCs from at least 3 donors
- Test article and positive control (e.g., TGN1412 analog)
- Cytokine detection array (IL-6, IL-1β, TNF-α, IFN-γ)
Methodology:
- System Priming: Condition MOC with cell culture medium for 24 hours to establish baseline
- Immune Cell Introduction: Perfuse 1×10ⶠPBMCs/mL through vascular channel at physiologically relevant shear stress (0.5-4.0 dyn/cm²)
- Dosing: Introduce test article at clinical candidate concentrations (typically 0.1-100 µg/mL) via vascular perfusion
- Monitoring: Sample effluent at 0, 6, 24, 48, and 72 hours for cytokine analysis
- Endpoint Analysis:
- Viability: Measure LDH release and metabolic activity (MTT assay)
- Activation: Quantify CD69+ expression on T cells via flow cytometry
- Cytokine Storm Signature: Multiplex analysis of ≥10 proinflammatory cytokines
- Data Normalization: Express results as fold-change over vehicle control and compare to clinical CRS benchmarks
Validation Criteria: System should detect ≥5-fold increase in IL-6 and IL-2 with TGN1412 positive control at clinically relevant concentrations [54].
Protocol: Immune-Mediated Hepatotoxicity Assessment
Purpose: To evaluate drug-induced liver injury with an immune component using a liver-immune MOC model.
Materials:
- Liver-Chip with primary human hepatocytes, Kupffer cells, and endothelial cells
- iPSC-derived immune cells (myeloid and lymphoid lineages)
- Benchmark compounds: Hepatotoxicants with known immune involvement (e.g., trovafloxacin, diclofenac)
- ALT/AST detection kit for effluent analysis
- Immunofluorescence staining for tight junctions (ZO-1) and immune markers
Methodology:
- Model Establishment: Culture liver model for 7-10 days to establish albumin production, urea synthesis, and cytochrome P450 activity
- Immune Integration: Introduce iPSC-derived macrophages (Kupffer cell analogs) and peripheral blood-derived lymphocytes at physiologically relevant ratios
- Compound Exposure: Perfuse test article through vascular channel for 72 hours at multiple concentrations (including clinical Cmax)
- Real-time Monitoring:
- Barrier Function: Transendothelial electrical resistance (TEER) measurements
- Metabolic Function: Albumin and urea production quantification
- Injury Markers: ALT, AST release into effluent
- Post-Experiment Analysis:
- Immunofluorescence: for immune cell infiltration (CD45+ cells in parenchymal space)
- Cytokine Profiling: MCP-1, IL-8, IL-10 as indicators of immune activation
- Histological Assessment: of bile canaliculi disruption and steatosis
Validation: System should correctly classify ≥87% of known hepatotoxicants, matching performance of qualified Liver-Chip models [52].
Diagram 1: Immunotoxicity assessment workflow for MOC systems
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for MOC Immunotoxicity Studies
| Reagent/Material | Function | Example Application |
|---|---|---|
| Human iPSC-Derived Immune Cells | Provides renewable source of human macrophages, T cells, and dendritic cells | Modeling human-specific immune responses in MOC systems [54] [57] |
| opti-ox Cell Programming Technology | Enables precise, consistent differentiation of iPSCs into target immune cell types | Generating standardized immune cells for reproducible MOC studies [57] |
| Cytokine Multiplex Assays | Simultaneous quantification of multiple inflammatory mediators | CRS biomarker profiling in MOC effluent [54] |
| Microphysiological System (MPS) | 3D, flow-based culture platform that mimics organ physiology | Emulate Liver-Chip with integrated Kupffer cells [55] [52] |
| Endothelialized Microfluidic Chips | Creates physiological barrier with immune cell interaction capability | Modeling immune cell extravasation in response to immunotoxicants |
Regulatory Submission Strategy
ISTAND Qualification Pathway
For researchers developing MOC platforms for immunotoxicity assessment, the ISTAND qualification pathway offers a structured approach to regulatory acceptance:
- Letter of Intent (LOI) Submission: Detailed proposal of the MOC platform and its proposed COU for immunotoxicity assessment
- Qualification Plan Development: Collaborative phase with FDA to design validation studies that will generate sufficient evidence for qualification
- Full Qualification Package Submission: Comprehensive data package demonstrating analytical validation and biological relevance for the specified COU
The qualification process emphasizes fit-for-purpose validation, meaning the extent of validation should match the stringency of the proposed COU [50] [55].
Evidence Generation for Regulatory Acceptance
Building a compelling data package for MOC immunotoxicity models requires:
Analytical Validation:
- Precision: Intra- and inter-laboratory reproducibility
- Accuracy: Concordance with known clinical outcomes
- Robustness: Performance across donor variants and operational parameters
Biological Validation:
- Mechanistic Relevance: Demonstration that the model captures key aspects of human immunobiology
- Predictive Capacity: Performance against clinical immunotoxicity data (retrospective analysis)
- Benchmarking: Comparison against existing models and animal data
Technical Documentation:
- Standard Operating Procedures: Detailed protocols for model assembly, maintenance, and endpoint analysis
- Quality Control Metrics: Acceptance criteria for each model batch
- Data Standards: FAIR (Findable, Accessible, Interoperable, Reusable) data principles
The convergence of FDA Modernization Act 2.0 and the ISTAND Program creates an unprecedented opportunity to advance human-relevant immunotoxicity testing using MOC systems. Researchers can now design studies with regulatory acceptance in mind, focusing on qualified contexts of use and robust validation strategies. As the FDA implements its roadmap to reduce animal testing, MOC platforms that successfully demonstrate predictive value for human immunotoxicity outcomes will become increasingly vital tools in the drug development pipeline. The protocols and application notes provided here offer a foundation for designing immunotoxicity studies that meet both scientific and regulatory requirements in this new era of human-focused risk assessment.
The preclinical assessment of immunotoxicity and immunotherapy efficacy remains a significant challenge in drug development. This application note provides a detailed comparative analysis of three pivotal approaches: Mouse Oral Cancer (MOC) syngeneic models, traditional in vivo studies, and emerging in silico projection methods. With increasing recognition of the limitations of conventional models in recapitulating human immune responses, understanding the complementary strengths and weaknesses of these systems is crucial for researchers designing immunotoxicity studies within multi-organ-on-chip (multi-OoC) platforms. We present standardized protocols and analytical frameworks to enable robust cross-platform validation of immunotoxicological findings, thereby enhancing the predictive power of preclinical research.
Comparative Data Analysis of Experimental Platforms
The table below summarizes the key characteristics and performance metrics of MOC models, in vivo data, and in silico projections, highlighting their respective applications and limitations in immunotoxicity research.
Table 1: Comprehensive Comparison of MOC Models, In Vivo Data, and In Silico Projections
| Feature | MOC Syngeneic Models | Traditional In Vivo Models | In Silico Projections |
|---|---|---|---|
| Key Application | Study tumor-immune interactions in immunocompetent hosts [58] | Whole-system biology and pharmacokinetics/pharmacodynamics (PK/PD) [59] | Rapid MoA assessment and target identification [60] [61] |
| Immune Context | Syngeneic; fully murine immune system [58] | Varies (syngeneic, humanized, or immunodeficient) [59] | Not applicable; computational prediction |
| Quantitative Data | Tumor growth kinetics, flow cytometry of Tumor-Infiltrating Lymphocytes (TILs: CD8+, FOXP3+CD4+), MHC class I expression [58] | Tumor volume, survival analysis, immune cell counts via FACS, cytokine levels [59] | Prediction accuracy (e.g., Balanced Accuracy ≥80%), affinity scores (IC50/EC50) [60] [61] |
| Key Strengths | Parallels key infiltrating immune cells found in human cancer; platform for dissecting tumor-host interactions [58] | Incorporates full physiological complexity; gold standard for efficacy/toxicity [59] | High-throughput, cost-effective; enables drug repositioning [60] [62] |
| Major Limitations | Does not fully recapitulate human immune system complexity [59] | Marked interspecies differences; suboptimal recapitulation of human cancer features [59] | Performance depends on quality and quantity of training data [61] |
Table 2: Analysis of Infiltrating Immune Cells in MOC1 vs. MOC2 Models
| Immune Parameter | MOC1 Model (Indolent Phenotype) | MOC2 Model (Aggressive/Metastatic Phenotype) |
|---|---|---|
| CD8+ T-Cell Infiltration | Increased [58] | Not Featured |
| Regulatory T-Cell (Treg) Infiltration | Not Featured | Increased FOXP3+CD4+ [58] |
| MHC Class I Expression | High constitutive and inducible expression [58] | Low constitutive and inducible expression [58] |
| Response to Treg Depletion | Not Featured | Delayed primary tumor growth [58] |
Experimental Protocols
Protocol 1: MOC Syngeneic Model for Tumor-Immune Profiling
This protocol details the use of the C57BL/6 MOC model to analyze tumor-infiltrating lymphocytes (TILs) and their functional impact.
Key Materials:
Procedure:
- Cell Preparation: Culture MOC cells in IMDM/F12 medium supplemented with 5% FCS, EGF, hydrocortisone, and insulin. Harvest cells and wash twice in D-PBS [58].
- Tumor Transplantation: Resuspend MOC cells (e.g., 1x10^5 to 1x10^6) and inject subcutaneously into the right flank of mice [58].
- Tumor Monitoring: Monitor tumor growth biweekly, recording tumor size as the average of the two largest diameters [58].
- Immune Cell Harvest: Upon reaching endpoint (e.g., 8mm diameter), harvest tumors, draining lymph nodes, and spleens.
- Immune Phenotyping by Flow Cytometry:
- Block cells with rat anti-mouse CD16/CD32 for 15 minutes.
- Stain with surface marker antibodies (e.g., anti-CD45, -CD4, -CD8) for 30 minutes at 4°C.
- For intracellular staining (e.g., FOXP3), use a dedicated intracellular staining kit according to the manufacturer's protocol [58].
- Perform flow cytometry using a FACSCalibur and analyze data with FloJo software [58].
- Functional Validation (e.g., Treg Depletion): To validate the functional role of identified immune cells, perform antibody-mediated depletion (e.g., anti-Treg antibodies) and analyze subsequent effects on tumor growth [58].
Protocol 2: Multi-Organ-on-Chip for Systemic Immunotoxicity
This protocol describes a method to investigate systemic immunotoxicity using a multi-organ-on-chip (multi-OoC) platform, where a stimulus applied to one tissue (gingiva) elicits an immune response in a distant, connected tissue (skin).
Key Materials:
- HUMIMIC Chip3plus: A microfluidics bioreactor enabling dynamic flow in a closed circuit (TissUse GmbH) [5] [29].
- Reconstructed Human Tissues: Reconstructed Human Gingiva (RHG) and Reconstructed Human Skin with integrated MUTZ-3-derived Langerhans cells (RHS-LC) [5] [29].
- Test Agent: e.g., Nickel sulfate [5] [29].
Procedure:
- Chip Setup and Stabilization: Incorporate RHG and RHS-LC into the HUMIMIC Chip3plus. Initiate dynamic flow culture and stabilize the system for 24 hours. Monitor stability via glucose uptake, lactate production, and LDH release into the microfluidics compartment [5] [29].
- Topical Exposure: Apply the test compound (e.g., Nickel sulfate) topically to the RHG tissue for 24 hours [5] [29].
- Incubation and Response Analysis: After exposure, maintain the chip under dynamic flow for an additional 24 hours to allow for systemic communication.
- Endpoint Assessment: Analyze LC activation in the distant RHS-LC tissue as a key endpoint. This can include:
- Migration Analysis: Assess LC migration from the epidermis to the dermal compartment (hydrogel) [5] [29].
- Maturation Markers: Quantify mRNA levels of activation markers (e.g., CD1a, CD207, HLA-DR, CD86) in the dermal compartment using PCR [5] [29].
- Cytokine Release: Measure cytokine levels in the microfluidics compartment [5] [29].
Protocol 3: In Silico Target and Mechanism of Action Prediction
This protocol utilizes computational methods to predict the protein targets and Mechanism of Action (MoA) of small molecules, which is valuable for understanding immunotoxicity and repositioning drugs.
Key Materials:
Procedure:
- Data Preparation and Standardization:
- Collect bioactivity data (e.g., Ki, Kd, IC50, EC50 ≤ 10 µM) for human target proteins from relevant databases.
- Prepare chemical structures (remove salts, convert to canonical SMILES) using toolkits like OpenBabel [60].
- Network Construction: Build a global drug-target interaction (DTI) network using the prepared data [60].
- Model Training and Prediction:
- Validation:
- Data Preparation and Standardization:
Visualizing Workflows and Signaling Pathways
Multi-OoC Systemic Immunotoxicity Workflow
The following diagram illustrates the experimental workflow for assessing systemic immunotoxicity using a multi-organ-on-chip system.
Integrated Preclinical Immunotoxicity Assessment
This diagram outlines a strategic framework for integrating MOC, in silico, and multi-OoC models to form a more robust and predictive immunotoxicity assessment pipeline.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Immunotoxicity Studies
| Reagent / Platform | Function / Application | Example Use Case |
|---|---|---|
| C57BL/6 MOC Cell Lines | Syngeneic model for studying tumor-immune interactions in immunocompetent mice. | Comparing immune infiltration in indolent (MOC1) vs. aggressive (MOC2) tumors [58]. |
| HUMIMIC Chip3plus | Microfluidic bioreactor for connecting multiple human tissues under dynamic flow. | Modeling systemic toxicity from oral mucosa to skin [5] [29]. |
| Reconstructed Human Tissues (RHG, RHS-LC) | Organotypic models with integrated immune cells for human-relevant toxicology. | Assessing Langerhans cell activation after exposure to a sensitizer [5] [29]. |
| bSDTNBI Algorithm | Network-based inference method for predicting drug targets and Mechanism of Action (MoA). | In silico drug repositioning and MoA assessment for novel compounds [60]. |
| Flow Cytometry Antibodies (Anti-CD45, CD4, CD8, FOXP3) | Profiling and quantifying specific immune cell populations in heterogeneous samples. | Characterizing Tumor-Infiltrating Lymphocytes (TILs) in MOC models [58]. |
The development of new medicines suffers from high attrition rates, with eight out of nine drug candidates entering clinical testing failing, mostly due to poor safety and efficacy in humans [36]. This high failure rate is largely attributed to the low predictive value of animal models used in preclinical phases, as drug disposition can differ markedly between experimental animals and humans [36]. More than 90% of drugs that appear safe and effective in animals ultimately fail in human trials [63]. This inefficiency not only costs billions of dollars but also delays life-saving treatments and raises serious ethical concerns about the reliance on animal testing.
In response to these challenges, multi-organ-on-chip (MOC) technologies have emerged as a transformative approach that captures human physiology in vitro. These microfluidic devices incorporate human cells to mimic organ-level functionality, providing a more human-relevant platform for assessing drug safety, efficacy, and immunotoxicity [12]. The recent passage of the FDA Modernization Act 2.0 in 2022, which removed the mandatory requirement for animal testing in new drug approvals, has further accelerated the adoption of these human-based systems [64] [65]. This application note examines the economic and ethical imperatives for implementing MOC systems in immunotoxicity studies, providing detailed protocols for their application in preclinical research.
Economic Advantages of Multi-Organ-on-Chip Systems
Market Growth and Industry Adoption
The economic case for MOC technologies is reflected in their rapid market growth and increasing integration into pharmaceutical R&D pipelines. As shown in Table 1, the organs-on-chips market is experiencing remarkable expansion, projected to grow at a compound annual growth rate (CAGR) of 30.0% from 2025 to 2032 [66].
Table 1: Organs-on-Chips Market Overview and Projections
| Market Aspect | 2024 Status | 2032 Projection | CAGR (2025-2032) |
|---|---|---|---|
| Global Market Size | USD 154.1 million [66] | USD 1,322.0 million [66] | 30.0% [66] |
| Liver-on-a-Chip Segment Share | 36.7% [66] | - | - |
| Drug Discovery & Development Application Share | 52.9% [66] | - | - |
| Pharmaceutical & Biotechnology End-user Share | 55.5% [66] | - | - |
This growth is driven by the increasing demand for predictive preclinical models that can provide human-relevant data superior to traditional animal models or 2D cell cultures [66]. For instance, Emulate's Liver-Chip S1 has demonstrated up to 87% sensitivity and 100% specificity in predicting drug-induced liver injury, a significant improvement over animal models [66]. This enhanced predictability allows for earlier identification of ineffective and unsafe compounds, potentially saving substantial resources in the drug development process.
Comparative Cost Analysis and Value Proposition
While the initial development and implementation costs of MOC systems can be high, their long-term value proposition in reducing preclinical expenses is compelling. The technology enables researchers to streamline the research process by replicating the physiology of real organs, thus improving the predictability of toxicity and drug efficacy analyses [66]. Specific economic benefits include:
Reduced Clinical Failure Rates: By providing more human-relevant data early in development, MOCs help identify potential failures before they reach clinical trials, where costs escalate dramatically [63] [66].
Faster Timelines: MOC systems can provide data more quickly than lengthy animal studies, potentially accelerating the drug development pipeline [63].
Selective Animal Testing: In the near term, MOCs enable more selective use of animal studies, focusing them only on filling gaps that models cannot yet cover, thereby reducing animal use and associated costs [63].
The adoption timeline for these technologies is progressing rapidly. Industry experts project that within 1-3 years, companies will meaningfully adopt AI and computational models in preclinical stages, with animal testing becoming more selective. Within 3-5 years, AI-driven and biosimulation platforms are expected to become the default for many preclinical safety and efficacy evaluations, with full replacement realistic for most companies in the 5-10 year timeframe [63].
Technical Protocols for Immunotoxicity Assessment
System Configuration and Experimental Design
Implementing MOC systems for immunotoxicity studies requires careful configuration to ensure physiological relevance. The following protocol outlines the key steps for establishing a multi-organ system capable of assessing immunotoxic responses:
Table 2: Essential Research Reagent Solutions for MOC Immunotoxicity Studies
| Reagent Category | Specific Examples | Function | Technical Notes |
|---|---|---|---|
| Primary Cells | iPSC-derived hepatocytes, macrophages, endothelial cells [66] | Recreate functional human tissue units | Use defined cell ratios; 3D architecture critical |
| Scaffold Materials | Synthetic polymers, collagen matrices [12] | Provide 3D extracellular matrix environment | Ensure permeability and mechanical properties |
| Culture Media | Serum-free specialized media [36] | Support cell viability and function | Eliminate batch variability; enable sampling |
| Analytical Assays | ELISA, LC-MS, functional genomics [36] | Quantify biomarkers, metabolites, gene expression | Enable sampling from all compartments |
| Microfluidic Components | PDMS chips, perfusion systems [12] | Mimic blood flow, mechanical forces | Use materials that don't absorb compounds |
Protocol 1: Establishing a Multi-Organ Immunotoxicity Platform
System Selection and Configuration:
- Select organ models relevant to the test compound's exposure route and metabolic pathway (typically liver-intestine-kidney for oral administration) [36]
- Utilize a commercial multi-organ system (e.g., CN Bio's PhysioMimix Core) or custom-designed platform [66]
- Ensure the system allows for sampling from all major compartments and uses materials that do not absorb or adsorb the compound of interest [36]
Cell Sourcing and Preparation:
- Source human cells that endogenously express main transporters and metabolizing enzymes [36]
- Utilize induced pluripotent stem cells (iPSCs) when possible to enable patient-specific models [66]
- Prepare organ models in 3D configuration with proper polarization [36]
- Pre-validate individual organ models before connecting in multi-organ system
System Integration and Maintenance:
- Connect individual organ models in a physiologically relevant manner [36]
- Establish a tight cellular barrier between compartments [36]
- Maintain system under controlled flow conditions with appropriate mechanical stimuli
- Culture cells in absence of fetal calf serum and Matrigel to reduce variability [36]
Immunotoxicity Assessment Workflow
The following Dot language diagram illustrates the complete experimental workflow for immunotoxicity assessment using multi-organ-on-chip systems:
Protocol 2: Immunotoxicity Evaluation in MOC Systems
Pre-Study Validation:
- Define the Context of Use (COU) for the immunotoxicity assessment
- Select benchmark compounds with known immunotoxic profiles (both positive and negative controls)
- Validate system performance using benchmark compounds prior to testing novel compounds
- Establish acceptance criteria for system performance based on benchmark responses
Compound Exposure and Sampling:
- Introduce test compounds at clinically relevant concentrations
- Utilize both single-dose and repeated-dose regimens as appropriate
- Collect media samples from all compartments at predetermined timepoints
- Monitor barrier integrity in real-time using transepithelial electrical resistance (TEER) where applicable
Endpoint Analysis:
- Assess cell viability using multiple metrics (MTT, ATP content)
- Quantify cytokine/chemokine release profiles using multiplex ELISA
- Evaluate immune cell activation and phenotype changes via flow cytometry
- Monitor tissue-specific functional markers (e.g., albumin for liver, creatinine clearance for kidney)
- Analyze metabolomic and transcriptomic profiles for mechanistic insights
Data Integration and Interpretation:
Ethical Framework and Implementation Strategy
Ethical Dimensions and Regulatory Compliance
The ethical case for adopting MOC technologies extends beyond the obvious animal welfare benefits to encompass broader concerns about human relevance and social responsibility. Key ethical considerations include:
Implementation of 3Rs Principle: MOC technologies directly support the Replacement, Reduction, and Refinement of animal use in research, transitioning these principles from ethical aspirations to enforceable policy [64].
Human Relevance: By using human-derived cells and tissues, MOCs potentially provide more clinically predictive data than animal models, addressing ethical concerns about using animals for human benefit when superior alternatives exist [12].
Regulatory Alignment: Recent regulatory changes, including the FDA Modernization Act 2.0 and initiatives by the NIH and FDA to reduce or phase out animal testing, create both an ethical imperative and practical pathway for adoption [63] [64].
The following Dot language diagram illustrates the key ethical and implementation considerations for adopting MOC technologies:
Implementation Roadmap and Future Directions
Successful implementation of MOC technologies for immunotoxicity assessment requires a strategic approach that addresses both technical and systemic challenges. Key implementation considerations include:
Gradual Integration Strategy:
- Begin with a hybrid approach that combines MOC data with reduced animal studies
- Focus initial applications on specific contexts of use where MOCs show strong predictive value
- Scale toward complete replacement as concordance with human responses improves [64]
Validation and Standardization:
- Conduct rigorous validation studies against clinical outcomes
- Develop standardized protocols through organizations like ISO and OECD
- Establish performance criteria with appropriate controls and acceptance ranges [64]
Addressing Current Limitations:
Regulatory Engagement:
- Engage early with regulators through FDA scientific advice meetings or EMA qualification procedures
- Participate in pilot programs such as the FDA's ISTAND program, which has accepted organ-chip technologies for evaluation [66]
- Contribute to the development of regulatory frameworks for non-animal methods
The future of MOC technologies is closely tied to advancements in complementary fields, particularly artificial intelligence. The integration of AI with multi-organ systems is emerging as a key trend, where AI algorithms enable predictive modeling of human pharmacokinetics and disease progression by analyzing large datasets from chip experiments [66]. Furthermore, the expansion into personalized medicine applications represents a significant opportunity, as MOCs can incorporate patient-specific cells to create individualized disease models and treatment response profiles [66].
Multi-organ-on-chip technologies represent a transformative approach to preclinical immunotoxicity assessment that offers compelling economic and ethical advantages over traditional animal models. By providing more human-relevant data, these systems can reduce clinical failure rates and associated costs while addressing growing ethical concerns about animal testing. The detailed protocols provided in this application note offer researchers a practical framework for implementing MOC systems in immunotoxicity studies, with specific guidance on system configuration, experimental design, and endpoint analysis.
While challenges remain in standardization, validation, and regulatory acceptance, the rapid market growth and increasing integration of MOCs into pharmaceutical R&D pipelines demonstrate their growing value and potential. As the technology continues to evolve through integration with AI and advances in personalized medicine, MOCs are poised to fundamentally reshape the preclinical landscape, creating a more efficient, predictive, and ethical paradigm for drug development.
Organ-on-a-Chip (OoC) technology, a class of microphysiological systems (MPS), has emerged as a transformative platform for biomedical research, particularly in the critical area of immunotoxicity assessment. By simulating human organ-level physiology within microfluidic devices, OoCs provide a groundbreaking alternative to traditional preclinical models, offering enhanced human physiological relevance [17] [67]. The field is experiencing rapid acceleration, driven by significant regulatory shifts, including the FDA Modernization Act 2.0, which now formally permits the use of human-based model data in place of some animal testing requirements [34]. This document details the current landscape, technical requirements, and experimental protocols for deploying multi-organ-on-chip (multi-OoC) systems in immunotoxicity studies, providing researchers and drug development professionals with actionable guidance for implementation.
Industry Trends Driving Adoption
The adoption of OoC technology is propelled by a convergence of scientific, regulatory, and commercial factors. These trends are reshaping the preclinical research paradigm.
- Regulatory Endorsement and Policy Shifts: Recent years have marked a turning point, with regulatory agencies providing a clearer pathway for using MPS data in submissions. The FDA's Innovative Science and Technology Approaches for New Drugs (ISTAND) Pilot Program and the GAO's 2025 report calling for "fit-for-purpose validation" have created a supportive environment for integrating OoC data into regulatory decision-making [34]. This gives pharmaceutical and biotech companies the confidence to embed these tools in their development workflows.
- Technological Diversification and Specialization: The OoC landscape now features a spectrum of platforms tailored to different research needs. This ranges from high-complexity systems (e.g., Emulate's AVA platform, CN Bio's PhysioMimix) that model multi-organ interactions with high fidelity, to simplified, accessible platforms (e.g., AIM Biotech's idenTx and organiX) designed for higher throughput and ease of use [8] [18] [34]. This diversification allows researchers to select a platform based on the specific balance required between physiological complexity and experimental throughput.
- Focus on Immunocompetent Models: There is a growing emphasis on incorporating functional immune components into OoCs. While innate immunity (e.g., macrophages, neutrophils) has been more commonly integrated, the field is advancing towards including adaptive immunity (T and B cells) to more fully recapitulate human immune responses [67]. This is crucial for investigating immunotherapy, autoimmune disorders, and inflammatory diseases. For instance, Pfizer has developed a Lymph Node-Chip capable of predicting antigen-specific immune responses, representing a major leap for preclinical immunotoxicity testing [18].
- Integration into Drug Development Pipelines: OoCs are moving from academic proof-of-concept to tangible tools in the pharmaceutical industry. They are being used for target discovery, lead optimization, safety toxicology, and ADME (Absorption, Distribution, Metabolism, and Excretion) studies [8]. Their ability to provide human-relevant data helps de-risk drug development, potentially reducing the high attrition rates in clinical trials linked to the poor predictivity of animal models [68].
Table 1: Commercial OoC Platforms and Their Applications in Immunotoxicity Research
| Platform (Company) | Key Features | Immunotoxicity/Toxicology Applications |
|---|---|---|
| PhysioMimix (CN Bio) | PDMS-free plates; single- & multi-organ configurations; adjustable flow; validated liver, kidney models [8]. | Cross-species DILI prediction; kidney toxicity for oligonucleotides; multi-organ ADME and toxicity [8] [18]. |
| AVA Emulation System (Emulate) | High-throughput (96 chips); automated imaging; Chip-R1 for low drug absorption [18]. | Antibody-drug conjugate (ADC) safety in Lung-Chip; immunogenicity in Lymph Node-Chip [18]. |
| HUMIMIC Chip2 (TissUse) | Supports up to 4 interconnected organ models in a single microfluidic circuit [67]. | Study of inter-organ crosstalk, systemic toxicity, and immune cell trafficking between tissues. |
| OrganoPlate (MIMETAS) | 3-lane microfluidic 384-well plate format; no pumps; gravity-driven flow [67]. | 3D perfused co-cultures; vascular barrier integrity; immune cell extravasation assays. |
| idenTx & organiX (AIM Biotech) | 3-channel design; no proprietary hardware; supports vascularization and immune cell migration [34]. | Modeling neovascularization, vascular barrier integrity, and immune cell-mediated tumor killing [34]. |
Critical Gaps and Roadblocks
Despite the promising trends, several significant challenges must be addressed to achieve widespread dissemination and deployment of OoC technology for immunotoxicity studies.
- Biomaterial Limitations: Many OoC devices rely on polydimethylsiloxane (PDMS), a material known to absorb small molecule drugs, potentially skewing pharmacokinetic and toxicity data [68]. Furthermore, many standard hydrogels (e.g., collagen, Matrigel) fail to provide the complex, defined extracellular matrix (ECM) composition needed for optimal immune cell function. Matrigel, derived from murine sarcomas, is an ill-defined "black box" that introduces confounding variables [69]. The development of well-defined, engineered biomaterial systems is crucial.
- Immune System Integration Complexity: Faithfully replicating human immunity on a chip is exceptionally challenging. A major hurdle is the HLA-mismatch problem; when adaptive immune cells from one donor are introduced to organ-specific cells from another, it can trigger graft-versus-host-like reactions, masking the intended experimental immune response [67]. Solutions involve using cells from a single donor or HLA-matched sources, which complicates cell sourcing. Furthermore, maintaining the viability and function of a diverse range of immune cell types (both innate and adaptive) alongside organ-specific tissues in a single system remains technically demanding.
- Standardization and Validation Hurdles: For OoCs to be trusted for regulatory decision-making, they must be standardized and validated. There is a lack of universal standards for cell sources, ECM materials, and endpoint analyses [34] [68]. The field is moving towards "fit-for-purpose" validation, where a model is validated for a specific biological context or question (e.g., vascular barrier integrity or immune cell recruitment) rather than attempting to recreate an entire organ [34]. This requires establishing clear, quantitative benchmarks for structure and function.
- Scalability and Throughput: While simpler platforms are achieving higher throughput, complex multi-OoC systems designed to study systemic immunotoxicity remain relatively low-throughput and require specialized expertise to operate [68]. Bridging the gap between physiological complexity and the throughput needed for effective drug screening is an ongoing area of development.
Table 2: Key Gaps in Multi-OoC for Immunotoxicity Studies and Potential Mitigations
| Challenge Area | Specific Gap | Potential Mitigations & Future Directions |
|---|---|---|
| Biological Fidelity | Incomplete recapitulation of adaptive immune responses [67]. | Use of iPSCs to generate HLA-matched tissue and immune cells from the same donor; development of improved biomaterials to support immune cell niches. |
| System Complexity | Technical difficulty in operating and assaying multi-OoC systems [68]. | Development of user-friendly, integrated platforms with automated fluid handling and in-line sensors; creation of standardized operating protocols. |
| Data & Validation | Lack of standardized endpoints and validation frameworks for immune function [34]. | Industry-wide collaboration to define quantitative benchmarks for immunocompetence (e.g., cytokine release, immune cell activation, cell killing). |
| Translation & Adoption | Reluctance to replace established animal models for regulatory studies. | Generating robust, peer-reviewed data comparing OoC predictions to clinical outcomes; continued dialogue with regulatory agencies (FDA, NIH). |
Experimental Protocols for Immunotoxicity Assessment
This section provides a detailed methodology for establishing a co-culture of a liver spheroid and endothelialized channel to assess potential immunotoxicity, such as from a nanoparticle (NP) formulation. The protocol is based on common approaches found in the literature and can be adapted for various OoC platforms that support 3D culture and perfusion [70] [8] [69].
Protocol: Liver Spheroid Model for NP-Induced Immunotoxicity
Objective: To evaluate the potential of a nanoparticle formulation to induce an inflammatory response in a perfused 3D liver model incorporating Kupffer cells.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Material | Function/Explanation |
|---|---|
| Primary Human Hepatocytes (PHHs) | The gold standard for liver functionality (drug metabolism, albumin production) [69]. |
| Liver Extracellular Matrix (ECM) Hydrogel | A defined hydrogel (e.g., HA-based) providing a biomimetic 3D scaffold that supports long-term PHH function [69]. |
| Primary Human Kupffer Cells | Liver-resident macrophages; key innate immune cells for detecting NP-induced damage and initiating inflammation [67]. |
| Primary Human Liver Endothelial Cells | Forms the vascular lining in the chip, crucial for studying immune cell adhesion and extravasation. |
| Cell Culture Media | Advanced hepatocyte maintenance media, supplemented with growth factors and hormones to preserve metabolic function. |
| Pro-inflammatory Cytokine Panel | ELISA or multiplex immunoassay kits to quantify secreted biomarkers (e.g., TNF-α, IL-6, IL-1β) [67]. |
Methodology:
- Spheroid Formation:
- Prepare a co-culture suspension of cryopreserved Primary Human Hepatocytes (PHHs) and Primary Human Kupffer cells at a ratio of 10:1 in liver-specific maintenance media.
- Seed the cell suspension into a low-attachment U-bottom 96-well plate to promote self-aggregation.
- Centrifuge the plate at low speed (e.g., 300 x g for 5 minutes) to encourage cell contact.
- Incubate for 48-72 hours to allow for compact, uniform spheroid formation.
Device Loading and Perfusion:
- Select an appropriate OoC device (e.g., CN Bio's Liver-12 plate or AIM Biotech's organiX platform).
- In the tissue chamber of the device, mix pre-formed liver spheroids with a liver-specific ECM hydrogel (e.g., containing decellularized liver ECM) [69].
- In the adjacent vascular channel, seed a monolayer of Primary Human Liver Endothelial Cells and allow them to form a confluent barrier under static conditions for 24-48 hours.
- After endothelialization, initiate perfusion of culture media through the vascular channel at a low, physiologically relevant flow rate (e.g., 1-5 µL/min). The system should be maintained with constant perfusion for at least 7-14 days to allow for tissue maturation and stabilization of albumin/urea production.
Dosing and Sample Collection:
- After the stabilization period, introduce the nanoparticle formulation into the perfusion media at the desired concentration(s). A negative control (media only) and a positive control (e.g., 1 µM Lipopolysaccharide) should be included.
- Circulate the dosing media for 24-72 hours.
- Collect effluent from the vascular outlet at defined time points (e.g., 0, 6, 24, 48 hours) for subsequent analysis.
- Following the experiment, disassemble the device to extract the spheroids for downstream analysis.
Endpoint Analysis:
- Immunotoxicity Biomarkers: Quantify the levels of pro-inflammatory cytokines (TNF-α, IL-6, IL-1β) in the collected effluent using ELISA or a multiplex Luminex assay [67].
- Liver Functionality: Measure albumin and urea secretion in the effluent as indicators of maintained liver-specific function.
- Viability and Histology: Perform live/dead staining (e.g., Calcein-AM/Propidium Iodide) on the extracted spheroids. For spatial analysis, fix and section the spheroids for H&E staining and immunohistochemistry (e.g., for CD68 to identify Kupffer cells).
- Transcriptomics: Isolate RNA from the spheroids for RNA-seq to analyze global gene expression changes in response to NP exposure, focusing on inflammatory pathways.
The path to widespread adoption of Organ-on-a-Chip technology for immunotoxicity studies is well underway, energized by clear regulatory support, technological innovation, and a pressing industry need for more human-predictive models. The emergence of standardized, commercially available platforms and a focus on developing immunocompetent models are particularly significant advancements. However, critical gaps in biomaterials, full immune system integration, and standardized validation remain active frontiers of research. By addressing these challenges through continued collaboration between engineers, biologists, and regulatory scientists, OoC technology is poised to become a cornerstone of preclinical research, ultimately leading to safer and more effective therapeutics.
Conclusion
Multi-organ-on-chip technology represents a paradigm shift in immunotoxicity testing, offering a human-relevant, physiologically accurate platform that successfully models complex systemic immune responses. By enabling the co-culture of multiple tissue types under dynamic flow, MOCs provide unprecedented insight into organ crosstalk and adverse outcome pathways, as demonstrated in validated models for bone marrow toxicity, skin sensitization, and neurotoxicity. The convergence of this technology with advances in stem cell biology, AI-driven analytics, and sophisticated biosensing is rapidly addressing initial challenges of reproducibility and long-term culture. With growing regulatory acceptance and its proven ability to refine drug safety assessment, MOC technology is poised to become a cornerstone of modern, predictive preclinical research, ultimately accelerating the development of safer therapeutics and advancing the goals of personalized and precision medicine.
References
- 1. Multiorgan-on-a-Chip: A Systemic Approach To Model and ... [https://www.sciencedirect.com/science/article/pii/S0167779920303097]
- 2. Organ-on-a-chip [https://en.wikipedia.org/wiki/Organ-on-a-chip]
- 3. Exploring Multiâ€Organ Crosstalk via the TissUse HUMIMIC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503007/]
- 4. Multi-Organs-on-Chips: Towards Long-Term Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6412790/]
- 5. A Multi-Organ-on-Chip Approach to Investigate How Oral ... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2021.824825/full]
- 6. Lymph Nodes-On-Chip: Promising Immune Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8415712/]
- 7. Organ-on-a-Chip: A Roadmap for Translational Research in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610883/]
- 8. PhysioMimix® Core Microphysiological System MPS [https://cn-bio.com/physiomimix-core/]
- 9. A guide to the organ-on-a-chip [https://www.nature.com/articles/s43586-022-00118-6]
- 10. Organ-on-chip technology: Opportunities and challenges [https://www.sciencedirect.com/science/article/pii/S2665906924000023]
- 11. Exploring Organ-on-a-Chip Technology: A comprehensive ... [https://elveflow.com/microfluidic-reviews/exploring-organ-on-a-chip-technology-a-comprehensive-review/]
- 12. Human Organ-On-A-Chip: Technologies Offer Benefits ... [https://www.gao.gov/products/gao-25-107335]
- 13. Organs-on-a-chip for global equity [https://www.frontiersin.org/journals/lab-on-a-chip-technologies/articles/10.3389/frlct.2025.1669220/full]
- 14. Using Organ-on-a-Chip Technology to Unlock Patient ... [https://emulatebio.com/using-organ-on-a-chip-technology-to-unlock-patient-derived-precision-medicine/]
- 15. Replacing Animal Testing with Stem Cell-Organoids [https://pmc.ncbi.nlm.nih.gov/articles/PMC11319430/]
- 16. Lymph Nodes-On-Chip: Promising Immune Platforms for ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.711307/full]
- 17. Organ-on-chip platforms for nanoparticle toxicity and ... [https://www.sciencedirect.com/science/article/pii/S2590006425006234]
- 18. Expanding the Frontiers of Human Biology with Organ-on-a ... [https://emulatebio.com/expanding-the-frontiers-of-human-biology-with-organ-on-a-chip-technology-highlights-from-the-2025-mps-world-summit/]
- 19. An eighteen-organ microphysiological system coupling a ... [https://www.nature.com/articles/s41378-025-00933-3]
- 20. Advances in engineering immune–tumor microenvironments ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560574/]
- 21. A 3D-printed multi-compartment organ-on-chip platform with a ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc00489b]
- 22. Multi-Organs-on-Chips: Towards Long-Term Biomedical ... [https://www.mdpi.com/1420-3049/24/4/675]
- 23. Bioengineering of novel organotypic 3D human liver tissue ... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1574387/full]
- 24. Establishment of a human 3D in vitro liver-bone model as ... [https://link.springer.com/article/10.1007/s00204-024-03899-9]
- 25. Systemic effects of ingested nickel on the immune ... [https://www.semanticscholar.org/paper/Systemic-effects-of-ingested-nickel-on-the-immune-Boscolo-Andreassi/8987c56721b596cf85e4f2bdb48cf2b2c6b99a7e]
- 26. Immunotoxicity of nickel: Pathological and toxicological ... [https://pubmed.ncbi.nlm.nih.gov/32684520/]
- 27. Differential impacts of nickel toxicity: NiO and NiSO 4 on ... [https://pubmed.ncbi.nlm.nih.gov/40680445/]
- 28. In vitro immunity: an overview of immunocompetent organ-on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11148285/]
- 29. A Multi-Organ-on-Chip Approach to Investigate How Oral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8915798/]
- 30. Modelling the innate immune system in microphysiological ... [https://pubs.rsc.org/en/content/articlehtml/2024/lc/d3lc00812f]
- 31. Redefining the Role of Langerhans Cells As Immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5770803/]
- 32. The Roles of Skin Langerhans Cells in Immune Tolerance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9503294/]
- 33. Integration of immune cells in organs-on-chips: a tutorial - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10267470/]
- 34. Organ-on-Chip in 2025: In the Spotlight After the NIH, FDA, ... [https://www.hmbioconsulting.com/post/organ-on-chip-in-2025-in-the-spotlight-after-the-nih-fda-and-gao-push]
- 35. An overview of immunotoxicity in drug discovery and ... [https://www.sciencedirect.com/science/article/pii/S0378427424020563]
- 36. The potential of multi-organ-on-chip models for ... [https://www.sciencedirect.com/science/article/pii/S2468202021000188]
- 37. Organ-on-chip technology: Opportunities and challenges [https://pmc.ncbi.nlm.nih.gov/articles/PMC11446384/]
- 38. Standardisation needs for organ on chip devices [https://pubs.rsc.org/en/content/articlehtml/2021/lc/d1lc00241d]
- 39. Guiding organs-on-chips towards applications: a balancing ... [https://www.frontiersin.org/journals/lab-on-a-chip-technologies/articles/10.3389/frlct.2024.1376964/full]
- 40. Integrated approaches for immunotoxicity risk assessment [https://link.springer.com/article/10.1007/s44339-024-00010-w]
- 41. Organoids as models of immune-organ interaction [https://www.sciencedirect.com/science/article/pii/S2211124725009854]
- 42. Science in 3D: How organoids and organs-on-chips can ... [https://www.jax.org/news-and-insights/2025/september/science-in-3d-how-organoids-and-organs-on-chips-can-help-scientists-study-host-immune-microbiome-interactions]
- 43. Leveraging Organâ€onâ€Chip Models to Investigate Host ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12004439/]
- 44. Advancements in Microfluidic Organ-on-a-chip for Oral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12329541/]
- 45. Organ-on-a-chip platforms integrated with biosensors for ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993624000517]
- 46. Integrating Biosensors in Organs-on-Chip Devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC7558092/]
- 47. Urban Institute Data Visualization style guide - GitHub Pages [http://urbaninstitute.github.io/graphics-styleguide/]
- 48. Figures and Charts - UNC Writing Center [https://writingcenter.unc.edu/tips-and-tools/figures-and-charts/]
- 49. The FDA Modernisation Act 2.0: Navigating the Regulatory ... [https://www.linkedin.com/pulse/fda-modernisation-act-20-navigating-regulatory-shift-away-uday-shetty-t5qwf]
- 50. ISTAND Program [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/innovative-science-and-technology-approaches-new-drugs-istand-program]
- 51. FDA Advances Drug Development Innovation by ... [https://www.fda.gov/news-events/fda-voices/fda-advances-drug-development-innovation-establishing-istand-permanent-qualification-program]
- 52. A Recent Timeline of U.S. Actions to Reduce and Replace ... [https://emulatebio.com/alternatives-to-animal-testing-in-drug-development/]
- 53. FDA Announces Plan to Phase Out Animal Testing ... [https://www.fda.gov/news-events/press-announcements/fda-announces-plan-phase-out-animal-testing-requirement-monoclonal-antibodies-and-other-drugs]
- 54. Transforming Preclinical Safety Testing: The FDA's ... [https://www.marinbio.com/transforming-preclinical-safety-testing-the-fdas-roadmap-to-replacing-animal-studies-with-human-relevant-models-and-technologies/]
- 55. FDA's ISTAND Pilot Program accepts a submission of first ... [https://www.fda.gov/drugs/drug-safety-and-availability/fdas-istand-pilot-program-accepts-submission-first-organ-chip-technology-designed-predict-human-drug]
- 56. FDA Announces Plan to Phase Out Animal Testing ... [https://www.hklaw.com/en/insights/publications/2025/04/fda-announces-plan-to-phase-out-animal-testing-requirement]
- 57. FDA's decision to phase out animal testing | A new era for ... [https://www.bit.bio/blog/fda-announces-plan-to-phase-out-animal-testing]
- 58. Comparative Analysis of Tumor Infiltrating Lymphocytes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6346425/]
- 59. Preclinical ex vivo and in vivo models to study immunotherapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574409/]
- 60. In silico prediction of chemical mechanism of action via an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5738663/]
- 61. In silico target prediction for elucidating the mode of action ... [https://www.sciencedirect.com/science/article/abs/pii/S109332631630331X]
- 62. Computational/in silico methods in drug target and lead ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7673338/]
- 63. How Technology is Moving the Industry Away from Animal ... [https://www.pharmexec.com/view/technology-moving-industry-away-animal-testing-jo-varshney]
- 64. From 3Rs to 3D-Bioprinting & Organs-on-Chip: The Future ... [https://medium.com/health-science/from-3rs-to-3d-bioprinting-organs-on-chip-the-future-pathways-replacing-animal-testing-350f0e146c33]
- 65. New Drug Approvals: “Human Organ-on-a-Chip†GAO ... [https://www.foley.com/p/102lrjr/new-drug-approvals-human-organ-on-a-chip-gao-report-supports-innovation-and-re/]
- 66. Organs On Chips Market Size, Share | Industry Report [2032] [https://www.fortunebusinessinsights.com/organs-on-chips-market-114512]
- 67. In vitro immunity: an overview of immunocompetent organ- ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1373186/full]
- 68. Roadblocks confronting widespread dissemination and ... [https://www.nature.com/articles/s41467-024-48864-3]
- 69. Grand challenges in organoid and organ-on-a-chip ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10919399/]
- 70. State-of-the-Art Organ-on-Chip Models and Designs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383757/]