Validating Multi-Organ-on-a-Chip Systems to Recapitulate Human Immunity for Next-Generation Therapeutic Development
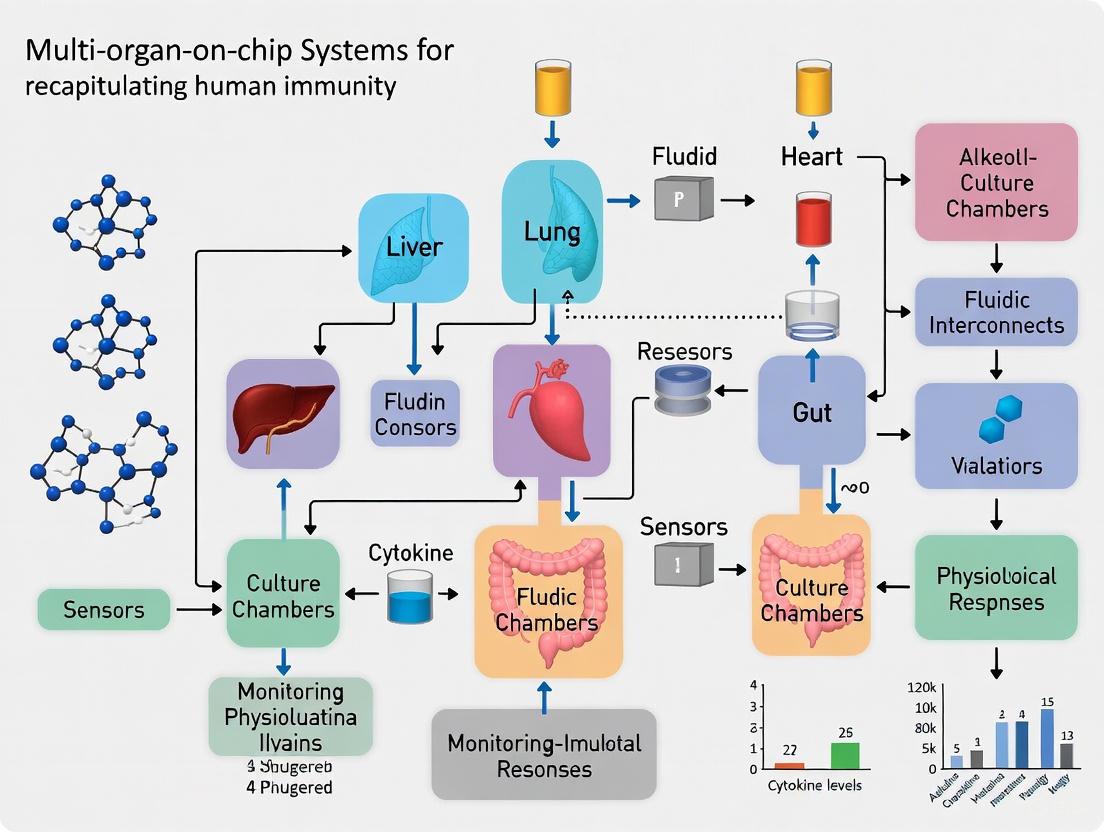
This article explores the groundbreaking role of validated multi-organ-on-a-chip (MOC) systems in revolutionizing preclinical research by accurately modeling human immune responses.
Validating Multi-Organ-on-a-Chip Systems to Recapitulate Human Immunity for Next-Generation Therapeutic Development
Abstract
This article explores the groundbreaking role of validated multi-organ-on-a-chip (MOC) systems in revolutionizing preclinical research by accurately modeling human immune responses. Tailored for researchers, scientists, and drug development professionals, it provides a comprehensive analysis spanning the foundational principles of microphysiological systems (MPS), their methodological applications in immunotherapy and toxicology, strategies for overcoming critical technical challenges, and rigorous validation frameworks. By synthesizing the latest advancements, this resource aims to equip professionals with the knowledge to leverage these human-relevant platforms for enhancing drug efficacy, predicting systemic toxicity, and accelerating the development of personalized immunotherapies, thereby bridging a critical gap between animal studies and clinical trials.
The Foundation of Immunity-on-a-Chip: Principles and System Design
Defining Multi-Organ-on-a-Chip (MOC) and Microphysiological Systems (MPS)
Microphysiological Systems (MPS) are advanced in vitro platforms that mimic the functional units of human organs at a miniature scale. They represent a technological evolution from traditional two-dimensional (2D) cell culture, incorporating three-dimensional (3D) structures, dynamic fluid flow, and biomechanical cues to recreate tissue- and organ-level physiology more accurately [1]. MPS encompass a range of technologies, including organoids and 3D bioprinted tissues [2]. Their primary purpose is to provide a more human-relevant experimental platform for biomedical research, drug development, and toxicology testing, thereby reducing reliance on animal models, which often poorly predict human responses [1] [3].
A Multi-Organ-on-a-Chip (MOC) is a specific type of MPS that interconnects two or more individual organ models via microfluidic channels. This creates a simulated "human-on-a-chip" that enables the study of complex organ-organ interactions, such as organ crosstalk, the pharmacokinetics (PK) and pharmacodynamics (PD) of drugs, and off-target toxicity [4] [2]. By linking organs, MOCs aim to replicate the systemic responses of the human body to therapeutic compounds, offering a powerful tool for predicting efficacy and safety in preclinical trials [5].
Comparative Analysis of MPS Platforms and Applications
The landscape of MPS technologies is diverse, with platforms differing in their design, throughput, and specific applications. The table below summarizes how MPS compare to traditional preclinical models and highlights the specifications of leading commercial platforms.
Table 1: Preclinical Model Comparison and Commercial MPS Platforms
| Feature | In vitro 2D Cell Culture | In vitro 3D Spheroid | In vivo Animal Models | Microphysiological System (MPS) | Emulate AVA System | CN Bio PhysioMimix |
|---|---|---|---|---|---|---|
| Human Relevance | Low | Medium | Low (due to species differences) | Medium / High | High (Human cell-based) | High (Human cell-based) |
| Complex 3D Organs/Tissues | No | Limited (Avascular) | Yes | Yes | Yes | Yes |
| (Blood)/Flow Perfusion | No | No | Yes | Yes | Yes (Microfluidic) | Yes (Tubeless microfluidics) |
| Multi-organ Capability | No | No | Yes (Systemic) | Yes | Via linking chips | Yes (Single- to multi-organ) |
| Longevity | < 7 days | < 7 days | > 4 weeks | ~ 4 weeks | Up to 7-day experiments | Up to 4 weeks |
| New Drug Modality Compatibility | Low | Medium | Low | Medium / High | High (Antibody-drug conjugates, Cell therapies) | High (mAbs, oligonucleotides, AAVs) |
| Throughput | High | High | Low | Variable (Medium to High) | High (96 chips per run) | High (Up to 288 samples) |
| Key Advantages | Simple, cheap, high-throughput | Better cell-cell interaction than 2D | Intact systemic physiology | Human-relevant, mechanistic insights, reduces animal use | High-throughput, automated imaging, AI-ready datasets | Open architecture, PDMS-free, validated protocols |
| Documented Applications | Basic cell functions | Cancer cell research, initial drug screening | Pharmacology, PK/PD, toxicity | ADME, toxicity, disease modeling, personalized medicine [3] | Toxicological and ADME studies [6] | Safety toxicology, ADME, disease modeling [3] |
Beyond commercial platforms, academic and institutional research continues to push the boundaries of complexity. A landmark 2025 study detailed an eighteen-organ MOC that incorporated a physiologically realistic vascular network and an excretory system with a micro-stirrer to mimic kidney function [2]. This system demonstrated the capability to maintain viability for almost two months and successfully modeled two-compartment pharmacokinetics, a task challenging for simpler in vitro models [2]. Furthermore, MPS are proving invaluable in specialized fields like cancer research and immunology. For instance, Pfizer has shared data on a Lymph Node-on-a-Chip capable of predicting antigen-specific immune responses, a significant advance for preclinical immunotoxicity testing [6].
Experimental Validation: Recapitulating Human Biology
Validating MOC models requires demonstrating that they replicate key structural and functional characteristics of human physiology. The following case studies and experimental data highlight this process.
Case Study: Building Blocks of Learning in a Neural MPS
A 2025 study used a brain MPS (neural organoids) to investigate the foundations of learning and memory. The researchers conducted a multi-faceted validation to confirm the model's relevance for neurophysiological studies [7].
Table 2: Key Experimental Findings in a Neural MPS Model
| Biological Process Investigated | Experimental Readout/Metric | Key Finding in Neural MPS | Technique/Method Used |
|---|---|---|---|
| Synapse Formation | Presence of pre- and post-synaptic markers | Detected punctate staining for Synaptophysin (presynaptic) and HOMER1 (postsynaptic) [7] | Immunofluorescence staining |
| Receptor Expression | Gene expression of key neurotransmitter receptors | Expression of glutamatergic (GRIN1, GRIN2A, GRIN2B, GRIA1) and GABAergic (GABRA1) receptors increased over time, plateauing at maturity (weeks 8-12) [7] | RNA-sequencing, qPCR |
| Immediate Early Gene (IEG) Expression | Basal and evoked expression of IEGs (e.g., FOS, NPAS4, NR4A1) | Organoids showed basal IEG expression, which was modulated by chemical stimuli, indicating activation of pathways critical for memory [7] | RNA-sequencing, Immunofluorescence |
| Synaptic Plasticity | Neuronal response to Theta Burst Stimulation (TBS) | Input-specific TBS induced short-term potentiation (STP) and long-term potentiation (LTP), the cellular correlates of learning and memory [7] | High-Density Microelectrode Arrays (HD-MEAs), Pharmacological modulation |
| Network Dynamics | Functional connectivity and criticality analysis | Organoids exhibited highly interconnected neural networks with critical dynamics, which optimize information encoding and processing [7] | Calcium imaging, HD-MEA data analysis |
Experimental Protocol: Investigating Synaptic Plasticity in a Neural MPS
The following workflow, derived from the same study [7], details the key steps for a functional investigation of synaptic plasticity.
Case Study: A Vascularized Multi-Organ MOC for Pharmacokinetics
The aforementioned eighteen-organ MOC was rigorously validated for its ability to mimic systemic drug disposition [2]. A key experiment involved characterizing the "blood" circulation to ensure physiological relevance. The design achieved a "blood" flow distribution across the 18 organ compartments that closely mimicked in vivo patterns in animal models, a critical prerequisite for meaningful pharmacokinetic studies [2]. The system's integrated excretion system, featuring a dialysis membrane and a micro-stirrer, allowed researchers to adjust the elimination rate of small molecules, thereby replicating a fundamental pharmacokinetic process typically absent in vitro models [2].
The Scientist's Toolkit: Essential Research Reagents and Materials
Building and running a successful MOC experiment requires a suite of specialized materials and reagents. The selection is critical for ensuring biological relevance, reproducibility, and accurate data collection.
Table 3: Essential Research Reagent Solutions for MOC Studies
| Item Category | Specific Examples | Function & Importance in MOC Experiments |
|---|---|---|
| Cell Sources | Primary human hepatocytes [1], Primary gut epithelial & goblet cells [4], HepaRG cell line [1], Patient-derived organoids (PDOs) [5], Human induced pluripotent stem cells (hiPSCs) [7] | Forms the biological foundation of the organ model. Primary cells and PDOs offer high physiological relevance, while immortalized lines offer consistency. hiPSCs enable patient-specific models. |
| Chip/MPS Hardware | Emulate Chip-R1 (Rigid, plastic) [6], CN Bio PhysioMimix Multi-chip Plates (PDMS-free, COC) [3] [4], PDMS-based chips [1] | The physical platform that houses the cells and microfluidics. Material choice is critical; PDMS can absorb small drugs, skewing results, while materials like COC (cyclic olefin copolymer) minimize non-specific binding [4]. |
| Scaffolds & Matrices | Extracellular matrix (ECM) components [1], Hydrogels [6], 3D bioprinting bioinks [5] | Provides the 3D structural and biochemical support for cells, mimicking the native tissue microenvironment. Essential for proper cell differentiation, organization, and function. |
| Culture Media | Customized culture medium [2], Cell-type specific media | Supplies nutrients, growth factors, and hormones to sustain cell viability and function. Recirculating media in MOCs enables systemic signaling between organ compartments. |
| Sensors & Assays | Embedded sensors for pH, O₂ [8], Effluent collection for -omics and biomarker analysis [6] [3], High-Density Microelectrode Arrays (HD-MEAs) [7] | Enables real-time monitoring of the microenvironment and post-experiment analysis of drug metabolites, secreted biomarkers, and tissue transcriptomics/proteomics. |
Multi-Organ-on-a-Chip technology, situated within the broader field of Microphysiological Systems, has moved from a promising concept to a powerful, validated tool for biomedical research. By integrating multiple human organ models with physiologically relevant features like vascular flow and excretory functions, MOCs offer a uniquely human-relevant platform for modeling systemic drug pharmacokinetics, organ-organ crosstalk, and complex disease states. As validation studies, such as those demonstrating neural plasticity and multi-organ pharmacokinetics, continue to accumulate, the scientific and regulatory confidence in these systems grows. This progress, supported by a robust toolkit of reagents and commercial platforms, is paving the way for MOCs to reduce the high failure rates in drug development and usher in a new era of precision medicine.
The convergence of microfluidics, three-dimensional (3D) cell culture, and integrated sensing is revolutionizing the development of in vitro models, particularly in the quest to create validated multi-organ-on-chip (multi-OoC) systems that recapitulate human immunity. Traditional drug development suffers from high failure rates, in part because conventional 2D cell cultures and animal models poorly predict human physiological responses [9] [10]. Microphysiological Systems (MPS), or Organ-on-Chip (OoC) technologies, address this gap by combining micro-engineered environments with living human cells to create more physiologically relevant models [9]. The incorporation of a functional immune system is a critical frontier for these models, as immunity underlies the pathophysiology of nearly every human disease, from cancer and infection to autoimmunity [10]. This guide provides a comparative analysis of the core technological components—3D cell culture matrices, microfluidic flow, and sensing modalities—that are essential for building immunocompetent multi-OoC platforms, providing experimental data and protocols to inform their selection and use.
Comparative Analysis of 3D Cell Culture Matrices
The transition from two-dimensional (2D) to three-dimensional (3D) cell culture is fundamental to creating in vivo-like microenvironments in organ-on-chip systems. Cells grown in 3D exhibit significant differences in morphology, differentiation, viability, gene expression, and drug metabolism compared to their 2D counterparts [11]. Selecting an appropriate 3D scaffold is therefore a critical first step in model development.
Types of 3D Cell Culture Scaffolds
The table below compares the four primary methods for incorporating 3D cell culture into microfluidic devices [12] [13].
| Method | Description | Key Advantages | Key Limitations | Common Applications |
|---|---|---|---|---|
| Suspension/Hanging Drop | Cells aggregate into spheroids in suspended media droplets [12] [13]. | Simple setup; homogeneous spheroid formation; high-throughput potential [12] [13]. | Limited to non-adherent or spheroid-forming cells; poor control over ECM composition [12]. | Embryoid bodies, tumor spheroids, mammospheres [13]. |
| Hydrogel Scaffolds | Cells are encapsulated within a hydrated polymer network that mimics the native extracellular matrix (ECM) [12] [14]. | Excellent biomimicry of ECM; tunable mechanical and biochemical properties; high porosity for nutrient diffusion [12] [14]. | Batch-to-batch variability (natural hydrogels); potential lack of mechanical rigidity [13] [14]. | Tissue engineering, drug screening, studying cell migration and invasion [12] [14]. |
| Paper-Based Scaffolds | Cells are seeded onto a porous, fibrous cellulose matrix [12] [13]. | Inexpensive; commercially available; facile stacking to create complex 3D structures [12] [13]. | Fiber size (>1µm) is larger than native ECM (~500nm); poor mimicry of ECM composition [13]. | Low-cost diagnostic assays, fundamental cell proliferation studies [12]. |
| Fiber-Based Scaffolds | Cells grow on synthetic or natural nano- to micro-scale fibers created by techniques like electrospinning [12] [13]. | Combines advantages of hydrogels and paper; highly tunable fiber size, composition, and alignment; excellent stability [12] [13]. | Complex fabrication process; requires specialized knowledge for development [13]. | Co-culture systems, studying endothelial cell morphogenesis and migration [12] [13]. |
Hydrogel Materials: A Deeper Dive
Given their widespread use, the choice of hydrogel material is crucial. The table below lists common hydrogels and their specific functions in microfluidic cell culture [14].
| Hydrogel Name | Origin | Primary Function in Culture | Example Composites (Cells, Drugs) |
|---|---|---|---|
| Collagen | Natural | Barrier, Drug Screening | Primary human kidney cells; cisplatin [14] |
| Polyethylene Glycol (PEG) | Synthetic | Cell Delivery, Encapsulation | Hepatocytes, leukemia cells, stem cells [14] |
| Hyaluronic Acid (HA) | Natural | Drug Screening/Delivery | Prostate cancer cells; camptothecin, docetaxel [14] |
| Alginate | Natural | Encapsulation, Drug Delivery | Hybridoma cells; mouse breast cancer cells; Vitamin B12 [14] |
| PuraMatrix | Synthetic | Drug Screening | Breast cancer, lung cancer, microvascular endothelial cells [14] |
| Fibrin | Natural | Cell Delivery | Not specified in search results [14] |
The Impact of Microfluidic Flow in MPS
Microfluidic flow is a defining feature of OoC systems, enabling dynamic perfusion that can significantly influence cell phenotype and function.
Quantitative Impact of Perfusion vs. Static Culture
A 2023 meta-analysis of 1718 ratios from 95 articles provides robust, quantitative data on how perfusion affects various cell types and biomarkers compared to static culture [15]. The gains from perfusion are not uniform but are highly dependent on the cell type and the specific biomarker measured.
| Cell Type / System | Key Biomarkers/Responses Enhanced by Perfusion | Reported Fold-Change (Flow vs. Static) | Context / Notes |
|---|---|---|---|
| General 2D Cultures | Most biomarkers | Overall very little improvement [15] | Perfusion alone in 2D settings shows minimal benefit. |
| General 3D Cultures | Cellular functions | Slight improvement [15] | High-density cultures benefit more from enhanced mass transfer. |
| CaCo2 (Intestinal) | CYP3A4 activity | >2-fold induction [15] | One of the most consistent biomarker inductions. |
| Hepatocytes (Liver) | PXR mRNA levels | >2-fold induction [15] | Key regulator of xenobiotic metabolism. |
| Blood Vessel Walls | Specific biomarkers | Reacted most strongly [15] | Cell types are naturally shear-sensitive. |
| Tumours, Pancreatic Islet, Liver | Specific biomarkers | Reacted strongly [15] | Highlights importance of flow for metabolic tissues. |
| Reproducibility | Various biomarkers | Low between articles [15] | 52 of 95 articles showed inconsistent responses for a given biomarker. |
Advanced Flow Systems for Immunity
For immunocompetent models, flow enables the study of complex processes like immune cell recruitment and extravasation. Advanced systems go beyond simple perfusion:
- Single-Phase Flow Culture: Uses microchambers and channels for well-defined, continuous perfusion, allowing for co-cultures and integration of sensors for parameters like dissolved oxygen (DO) and pH [16].
- Droplet-Based Culture: Encapsulates single cells or small populations in picoliter to nanoliter water-in-oil droplets, enabling ultra-high-throughput screening (up to 10^7 droplets) and analysis of cellular heterogeneity [16].
Integrated Sensing for Real-Time Monitoring
Integrating sensors directly into MPS is critical for non-invasive, real-time monitoring of both the cellular microenvironment and tissue functionality, moving beyond endpoint analyses.
Sensing Modalities
The following table details key sensing modalities that can be integrated into microfluidic MPS.
| Sensing Modality | Measured Parameter | Biologically Relevance | Example Implementation |
|---|---|---|---|
| Transepithelial/Transendothelial Electrical Resistance (TEER) | Barrier Integrity | Key indicator of tissue health and model maturity, especially in barriers like intestine, lung, and blood-brain barrier (BBB) [17] [10]. | Integrated gold electrodes in an OSTE-based chip measured TEER before and after pulsed electric field treatment [17]. |
| Electrochemical Sensors | Oxygen, pH, Glucose, Lactate | Metabolic activity of tissues; indicators of cell viability and inflammatory responses [17] [10]. | An OSTE-based chip with integrated sensors monitored oxygen and pH shifts in real-time following cell treatment [17]. |
| Optical Sensors | Oxygen, pH | Non-invasive monitoring of the physicochemical microenvironment [17]. | Oxygen "sensor spots" were integrated upstream and downstream of a treatment chamber for localized monitoring [17]. |
Case Study: A Sensor-Integrated MPS
A 2024 study demonstrated a microphysiological system fabricated from Off-Stoichiometry Thiol-Ene (OSTE) polymer, which avoids the small molecule absorption issues of PDMS [17]. This chip featured:
- Integrated Electrodes: Used for both applying Pulsed Electric Fields (PEF) and measuring TEER.
- Optical Sensors: For monitoring oxygen concentration and pH in the microchannel. The system successfully treated C6 glioma cells with PEF and detected subsequent physiological changes: a decrease in oxygen concentration without PEF, an increase with PEF, and a pH shift towards alkalinity post-PEF [17]. This showcases the power of integrated sensing for capturing dynamic cellular responses.
Experimental Protocols for Key Applications
Protocol: Assessing On-Target, Off-Tumor Toxicity of T-Cell Bispecific Antibodies (TCBs)
This protocol, adapted from Kerns et al. (2021), details the use of a human Alveolus Lung-Chip to evaluate the safety profile of cancer immunotherapeutics [18].
Objective: To reproduce and predict target-dependent TCB safety liabilities in a human immunocompetent organ chip platform.
Materials:
- Organ-Chip Platform: Human Alveolus Lung-Chip (e.g., from Emulate) featuring two parallel microchannels separated by a porous, ECM-coated membrane [18].
- Cells: Human primary alveolar epithelial cells and human primary lung microvascular endothelial cells.
- Immune Cells: Peripheral Blood Mononuclear Cells (PBMCs) isolated from human whole blood.
- Test Article: T-cell bispecific antibodies (TCBs) with known target (e.g., FOLR1) and control molecules.
Workflow Diagram: Lung-Chip Toxicity Assay
Procedure:
- Chip Seeding and Maturation: Seed alveolar epithelial cells in the top channel and lung microvascular endothelial cells in the bottom channel. Culture under liquid-liquid conditions for 5 days, then establish an air-liquid interface (ALI) for an additional 5 days to promote tissue maturation [18].
- Target Expression Validation: Use flow cytometry and immunofluorescence to confirm the expression level and pattern of the TCB target antigen (e.g., FOLR1) on the chip's epithelium. Compare to expression in positive control tumor cell lines [18].
- Introduction of Immune Compartment: Add PBMCs to the epithelial channel of the mature chip to create an immunocompetent system [18].
- TCB Exposure: Introduce the TCB into the system via the fluidic flow.
- Endpoint Analysis: Monitor the chips for 1-3 days for signs of toxicity.
- Cytokine Release: Measure levels of pro-inflammatory cytokines (e.g., IL-6, IL-2, IL-8) in the effluent using ELISA.
- Immune Cell Activation and Infiltration: Use real-time imaging to visualize T-cell attachment to the epithelium and morphological changes.
- Epithelial Damage: Quantify barrier integrity by measuring Transepithelial Electrical Resistance (TEER) and assess cell death via staining for viability/cytotoxicity markers [18].
Protocol: Real-Time Monitoring of Barrier Function and Metabolism
This protocol outlines the use of a sensor-integrated MPS for continuous monitoring.
Objective: To non-invasively track barrier integrity and metabolic shifts in a 3D tissue model under flow.
Materials:
- MPS Platform: A microfluidic chip with integrated electrodes for TEER and optical/electrochemical sensors for oxygen and pH (e.g., as described in [17]).
- Cells: Relevant barrier-forming cells (e.g., endothelial cells, intestinal epithelial cells) potentially co-cultured with other tissue-specific cells in a 3D hydrogel.
Procedure:
- Chip Preparation and Cell Seeding: Load the chip with a cell-laden hydrogel (e.g., collagen or Matrigel) in the central chamber. Initiate continuous, low-flow perfusion of culture media.
- Baseline Recording: Once cells adhere and form initial contacts, begin continuous recording of TEER, oxygen concentration (upstream and downstream of the tissue), and media pH. Continue until values stabilize, indicating the formation of a mature barrier and stable metabolic activity.
- Experimental Intervention: Introduce the test compound (e.g., a drug, inflammatory cytokine, or toxin) into the media stream.
- Real-Time Data Acquisition: Continuously monitor the sensor outputs throughout the exposure period and during a recovery phase (if applicable).
- A drop in TEER indicates a loss of barrier integrity.
- Changes in the oxygen gradient across the tissue reflect alterations in metabolic activity.
- A shift in media pH can indicate changes in glycolytic flux or other metabolic pathways [17].
- Correlation with Endpoint Assays: At the end of the experiment, perform endpoint analyses (e.g., immunofluorescence, gene expression) on the tissue and correlate findings with the kinetic sensor data.
Essential Research Reagent Solutions
The table below catalogs key materials and reagents essential for building and operating immunocompetent MPS, as cited in the research.
| Item Name | Function / Application | Key Characteristics |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Material for microfluidic device fabrication [12] [17]. | Gas permeable, optically transparent, easy to mold; but can absorb small molecules [12] [17]. |
| Off-Stoichiometry Thiol-Ene (OSTE) | Alternative polymer for microfluidic device fabrication [17]. | Reduced small molecule absorption, biocompatible, good alternative to PDMS for drug studies [17]. |
| PuraMatrix | Synthetic, peptide-based hydrogel for 3D cell culture [14]. | Defined composition, self-assembling into nanofibrous scaffold, suitable for drug screening co-cultures [14]. |
| PEG-DA (Poly(Ethylene Glycol) Diacrylate) | Synthetic hydrogel for cell encapsulation and delivery [14]. | Tunable mechanical properties, photopolymerizable for precise patterning within microchannels [14]. |
| Peripheral Blood Mononuclear Cells (PBMCs) | Source of human immune cells for immunocompetent models [18] [10]. | Provide T cells, B cells, NK cells, and monocytes; can be isolated from blood of specific donors [18]. |
| Transepithelial/Transendothelial Electrical Resistance (TEER) Electrodes | Integrated sensors for quantifying barrier integrity in real-time [17]. | Typically gold or other inert metals; can be multiplexed with other sensor functions [17]. |
| Oxygen Sensor Spots | Optical sensors for non-invasive monitoring of dissolved oxygen [17]. | Can be glued inside microchannels; read by an external fluorescence detector [17]. |
The strategic integration of microfluidics, physiologically relevant 3D cell cultures, and real-time sensing is paramount for developing validated multi-organ-on-chip systems that can accurately model human immunity. The experimental data and comparisons presented in this guide demonstrate that there is no one-size-fits-all solution. The choice of 3D matrix—whether hydrogel, spheroid, or scaffold—must be tailored to the specific organ and biological question. The application of microfluidic flow shows clear, though variable, benefits in enhancing the physiological relevance of cellular phenotypes, particularly in 3D cultures and for specific biomarkers. Finally, the integration of sensing technologies for parameters like TEER, oxygen, and pH is transitioning MPS from static endpoint analysis tools to dynamic platforms capable of capturing the complex kinetics of immune and tissue responses. As these core components continue to mature and standardize, their combined power will unlock more predictive models for drug development and the study of human disease.
Engineering the Immune-Tumor Microenvironment (TME) on a Chip
The tumor microenvironment (TME) represents a complex ecosystem where cancer cells interact with immune components, stromal cells, and extracellular matrix in a dynamic interplay that critically influences disease progression and therapeutic response [19] [20]. Engineering the immune-TME on a chip has emerged as a transformative approach to overcome the limitations of traditional models, offering unprecedented precision in mimicking human physiology for cancer research and drug development [19]. These microfluidic platforms integrate immune system components with tumor models within architecturally and biochemically defined contexts, enabling systemic analysis of immune-tumor interactions under fluidically dynamic conditions that more accurately reflect in vivo realities [5].
The validation of multi-organ-on-chip systems recapitulating human immunity represents a critical frontier in preclinical research, addressing the significant translational gap between animal models and human clinical outcomes [21]. By preserving key histopathological, genetic, and phenotypic features of parent tumors while incorporating functional immune elements, these chips provide a physiologically relevant platform for investigating immune surveillance, evasion mechanisms, and therapeutic interventions [5] [20]. This guide objectively compares leading immune-TME chip platforms, their performance metrics, and experimental applications to inform researchers and drug development professionals.
Technology Comparison: Platform Capabilities and Specifications
Commercial Immune-TME Platform Comparison
Table 1: Comparative analysis of commercial platforms for immune-TME modeling
| Platform Feature | Emulate Organ-Chip | MIMETAS OrganoPlate | ChipShop Fluidic 480 |
|---|---|---|---|
| Microfluidic Design | Multi-channel with mechanical stretch capabilities | 3-lane 40-chip plate, membrane-free | Cross-flow membrane chip, two independent chambers |
| Throughput Capacity | Medium | High (96 tissues per plate) | Medium |
| Key Analytical Tools | Integrated software for barrier function, immune cell recruitment, CAR-T analysis [22] | PhaseGuide technology for ECM patterning, gravity-driven flow [23] | Permeable membrane for tissue interface formation |
| Imaging Compatibility | Standard microscopy systems | High-content confocal imaging compatible [23] | Standard microscopy systems |
| Primary Applications | Barrier integrity studies, immune cell recruitment, CAR-T cell therapy assessment [22] | Angiogenesis, neurite outgrowth, permeability studies [23] | Gut-on-chip, brain-on-chip, multi-tissue interfaces |
| Flow Control System | Proprietary perfusion systems | Gravity-driven flow (no external pumps) [23] | Compatible with external flow controllers (e.g., Elveflow) [24] |
Performance Metrics in TME Recapitulation
Table 2: Quantitative performance assessment of immune-TME chip models
| Performance Parameter | Traditional 2D Models | 3D Organoids | Immune-TME Chips |
|---|---|---|---|
| Tumor Heterogeneity Preservation | Limited (<20%) [5] | High (>87% in colorectal PDOs) [5] | High (up to 95% by vascular integration) [5] |
| Immune Cell Infiltration Capacity | Non-existent | Limited | High (controlled recruitment assays) [22] |
| Angiogenic Sprouting Measurement | Not possible | Possible but static | Quantitative (sprout number, length, volume) [23] |
| Drug Response Prediction Accuracy | 30-40% | 70-87% [5] | 85-95% (vascularized models) [5] |
| Multicellular Complexity | Low (1-2 cell types) | Medium (3-4 cell types) | High (5+ cell types with spatial control) [19] |
| Physiological Flow Shear Stress | Absent | Absent | Tunable (0.1-20 dyn/cm²) [24] |
Experimental Protocols for Immune-TME Modeling
Protocol 1: Vascularized Tumor-Immune Chip Assembly
This protocol establishes a perfusable vascular network integrated with tumor organoids and immune components for evaluating trafficking and therapeutic responses [5].
Day 1: Microfluidic Device Preparation
- Select appropriate chip architecture (e.g., 3-lane OrganoPlate or parallel channel designs)
- Treat chip surfaces with 0.1% pluronic F-127 for 30 minutes to prevent non-specific adhesion
- Coat channels with collagen-I (6-8 mg/mL) or Matrigel (8-10 mg/mL) and incubate (37°C, 1 hour)
Day 1-3: Endothelial Network Formation
- Introduce HUVECs or patient-derived endothelial cells (2-3×10⁶ cells/mL) in EGM-2 medium
- Allow initial adhesion (2 hours) before initiating perfusion (0.5-1.0 µL/min)
- Culture for 3 days with stepwise flow rate increases (up to 5 µL/min) to mature vessels
Day 4: Tumor Organoid Integration
- Prepare patient-derived tumor organoids (50-100 µm diameter) in defined culture medium
- Introduce 20-30 organoids per chip into the stromal compartment
- Co-culture for 24 hours under continuous perfusion (1 µL/min) to establish tumor-endothelial contacts
Day 5: Immune Component Introduction
- Isolate PBMCs or specific immune subsets from patient blood using Ficoll gradient
- Introduce immune cells (1-2×10⁶ cells/mL) into the vascular channel
- Monitor immediate adhesion and extravasation events via time-lapse microscopy
Day 5-10: Experimental Applications
- For immunotherapy testing: Introduce checkpoint inhibitors (e.g., anti-PD-1, 10 µg/mL) via perfusion
- For immune recruitment studies: Fix and stain at specific timepoints for quantification
- For cytotoxicity assessment: Live-track immune-tumor interactions every 12 hours
Protocol 2: Immune Cell Recruitment and Cytotoxicity Assessment
This methodology quantifies immune cell migration and tumor cell killing within the engineered TME, adapted from Emulate's immune cell recruitment analysis [22].
Immune Cell Labeling and Introduction
- Isolate CD8+ T cells or NK cells from donor blood using magnetic separation
- Label with CellTracker Green CMFDA dye (5 µM, 37°C, 30 minutes)
- Wash twice with PBS and resuspend in complete RPMI at 1×10⁶ cells/mL
- Introduce labeled cells into the immune compartment of the chip
Time-Lapse Imaging and Tracking
- Place chip in environmental chamber (37°C, 5% CO₂) on confocal microscope
- Acquire images at 10-minute intervals for 24-48 hours using 10× objective
- Track individual immune cells using automated cell tracking software (e.g., MetaXpress)
Quantitative Analysis of Recruitment
- Calculate migration velocity (µm/min) from track displacements
- Determine meandering index (net displacement/total path length)
- Quantify contact duration between immune and tumor cells
- Measure apoptosis induction in tumor cells using caspase-3/7 reporters
Endpoint Immunostaining
- Fix cells with 4% PFA (15 minutes, room temperature)
- Permeabilize with 0.1% Triton X-100 (10 minutes)
- Stain for: CD8 (T cells), CD56 (NK cells), CD3 (T cells), Granzyme B (cytotoxicity)
- Image using high-content confocal system (e.g., ImageXpress Micro Confocal)
Data Analysis Parameters
- Immune cell recruitment rate: cells/mm²/hour
- Cytotoxic engagement frequency: contacts/immune cell/hour
- Target elimination efficiency: tumor cells lysed/immune cell/24h
Signaling Pathways in the Engineered Immune-TME
The engineered immune-TME on chip recapitulates critical signaling pathways that govern immune-tumor interactions. These pathways can be modulated and observed in real-time within the microfluidic environment.
Pathway 1: Anti-Tumor Immune Activation Cascade (Green) The anti-tumor immunity cycle initiates with tumor antigen release following cell death or treatment [20]. Antigen-presenting cells (dendritic cells, macrophages) process and present these antigens to T cells, leading to immune activation and proliferation [19]. Activated T cells and NK cells then execute direct cytotoxicity through perforin/granzyme release and Fas/FasL interactions, while simultaneously secreting chemotactic cytokines (CXCL9, CXCL10, CCL5) that recruit additional immune effectors to the TME [20].
Pathway 2: Tumor-Mediated Immunosuppression (Red) Tumors evade immune destruction through multiple mechanisms, including upregulation of immune checkpoint molecules (PD-L1, CTLA-4) that engage inhibitory receptors on T cells [19]. Concurrent secretion of immunosuppressive factors (TGF-β, IL-10, VEGF) and metabolic competition (tryptophan depletion via IDO, adenosine production) further dampens immune function, leading to T cell exhaustion and functional impairment [20]. These pathways can be quantitatively measured in immune-TME chips through real-time monitoring of cytokine fluxes and immune cell functional status.
Experimental Workflow for Immune-TME Validation
The validation of multi-organ-chip systems recapitulating human immunity follows a systematic workflow encompassing design, fabrication, biological integration, and functional assessment.
Phase 1: Platform Establishment Chip design incorporates microfluidic architectures that enable precise spatial organization of tumor, stromal, and immune compartments while permitting controlled perfusion [25]. Biomaterial selection ranges from natural matrices (collagen, Matrigel) to synthetic polymers (PDMS, PMMA) with specific modification to support cellular viability and function [25]. The tumor compartment can be established using patient-derived organoids, spheroids, or dissociated tumor cells that preserve original tumor heterogeneity [5] [20].
Phase 2: Application and Validation System validation requires confirmation of key TME features: immune cell extravasation, antigen-specific recognition, cytokine gradient formation, and pharmacodynamic responses to immunomodulators [19]. Functional testing includes quantifying immune-mediated cytotoxicity, profiling immune cell activation states, and measuring metabolic interactions between cellular components [22] [20]. Advanced systems may incorporate multiple organ equivalents (liver, lymph node) to study systemic immune effects and off-target toxicities [5].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for immune-TME chip experimentation
| Reagent Category | Specific Examples | Function in Immune-TME Modeling |
|---|---|---|
| Extracellular Matrices | Collagen-I (6-8 mg/mL), Matrigel (8-10 mg/mL), Fibrin (5-7 mg/mL) | Provides 3D structural support, biomechanical cues, and biochemical signals for cell organization [20] |
| Endothelial Cells | HUVECs, patient-derived endothelial cells, iPSC-ECs (2-3×10⁶ cells/mL) | Forms perfusable vascular networks enabling immune cell trafficking and nutrient delivery [5] |
| Immune Cell Media | RPMI-1640 + 10% FBS + 1% P/S, TexMACS, ImmunoCult | Maintains immune cell viability and function during perfusion culture [20] |
| Cell Tracking Dyes | CellTracker CMFDA (5 µM), CFSE (5 µM), CellTrace Violet (5 µM) | Enables real-time monitoring of immune cell migration and interactions [23] |
| Immunotherapy Agents | Anti-PD-1 (10 µg/mL), Anti-PD-L1 (10 µg/mL), Anti-CTLA-4 (10 µg/mL) | Tests checkpoint blockade efficacy in controlled TME context [19] |
| Cytokine/Chemokine Arrays | Luminex 45-plex, CBA Flex Sets, ELISA kits | Quantifies secretory profiles and gradient formation in microfluidic channels [19] |
| Microfluidic Controllers | Elveflow OB1, Fluigent MFCS, Syringe pumps | Maintains precise perfusion (0.1-20 µL/min) with physiological shear stress [24] |
| Live-Cell Imaging Dyes | Caspase-3/7 Green, Calcein AM, Propidium Iodide | Monitors real-time cytotoxicity and cell viability under flow conditions [23] |
Engineered immune-TME chips represent a validated approach for recapitulating human immunity in multi-organ systems, bridging critical gaps between conventional models and clinical reality. The technology platforms, experimental protocols, and analytical frameworks presented enable researchers to quantitatively investigate immune-tumor interactions with unprecedented physiological relevance. As these systems continue to evolve through increased cellular complexity, improved biomaterials, and enhanced analytical capabilities, they promise to transform cancer immunotherapy development and personalized treatment optimization.
The successful recapitulation of human physiology in Multi-Organ-on-Chip (MOC) systems hinges on the precise engineering of key physico-chemical microenvironmental parameters. For immunology research, where cellular behavior is profoundly influenced by environmental cues, the control of fluid shear stress, chemical concentration gradients, and mechanical cues becomes paramount [26]. These parameters are not merely technical specifications but fundamental biological determinants that regulate immune cell recruitment, differentiation, activation, and inflammatory responses [27] [28].
Traditional 2D cell culture systems fail to incorporate these dynamic mechanical forces, severely limiting their physiological relevance, especially for studying interactions between immune cells, blood, and tissue barriers [3] [27]. Similarly, animal models exhibit fundamental species-specific differences in immune responses, rendering them poor predictors of human immunology [29]. Immunocompetent MOC platforms address these limitations by providing engineered microenvironments where fluid flow, mechanical forces, and biochemical gradients can be controlled to emulate in vivo-like conditions. This control enables researchers to investigate complex immune processes such as neuroinflammation, immune cell recruitment in inflammatory bowel disease, and bone marrow toxicity with unprecedented human relevance [29] [30]. The integration of these design parameters transforms MOCs from simple cellular assays into sophisticated tools capable of predicting human immune responses for drug development and disease modeling.
Quantitative Comparison of Key Parameters Across Commercial Platforms
The implementation of key design parameters varies significantly across commercial MOC platforms, influencing their applicability for specific immunology research applications. The table below summarizes the capabilities of major platforms regarding fluid shear stress, gradient generation, and mechanical cue integration.
Table: Comparison of Key Design Parameters in Commercial Multi-Organ-on-Chip Platforms
| Platform/System | Fluid Shear Stress Control | Concentration Gradient Generation | Integrated Mechanical Cues | Primary Immunology Applications |
|---|---|---|---|---|
| PhysioMimix Core | Adjustable recirculating flow; rates matched to organ/tissue type [3] | Recirculating flow prevents biomarker dilution; enables clinical translatability [3] | Open architecture for customization; longer-term studies (up to 4 weeks) [3] | Safety toxicology; ADME; disease modeling [3] |
| Emulate Organ-Chips | Microfluidic flow for shear stress application [29] | Not explicitly detailed | Incorporation of organ-relevant mechanical forces (e.g., breathing motions, peristalsis) [29] | Colon immune cell recruitment; neuroinflammation; cytokine-mediated barrier disruption [29] |
| TissUse Humimic | Circulating media crucial for maintaining organ niches (e.g., bone marrow) [30] | Compartmentalization for PK/PD modeling; mass conservation for ADME [30] | 3D ceramic scaffolds for bone marrow niche; fluid flow for tissue interaction [30] | BBB permeability & neurotoxicity; bone marrow toxicity; intestine-liver ADME [30] |
| Custom Microfluidic Systems | Osmotic pumps for slow, controlled flow (<µm/s) [31] [32] | Stable, wide chemical diffusion fields alongside shear stress gradients [31] [32] | Passive generation of combined chemical and mechanical stress gradients [31] [32] | Cancer metastasis; stem cell differentiation; fundamental cell response studies [32] |
Experimental Protocols for Parameter Implementation and Validation
Generating and Measuring Physiological Fluid Shear Stress
Objective: To establish physiologically relevant laminar fluid shear stress in a microfluidic device to mimic venous/arterial conditions and study its effect on immune-endothelial interactions.
Background: In vivo, endothelial cells experience wall shear stress ranging from 2-20 dyne/cm² in arteries and 1-6 dyne/cm² in veins, with critical impacts on immune cell adhesion and vascular inflammation [27]. These forces trigger morphological changes, cytoskeletal reorganization, and altered gene expression in endothelial cells [27].
Table: Physiologically Relevant Shear Stress Ranges for Different Vessel Types
| Vessel Type | Typical Shear Stress Range (dyne/cm²) | Flow Pattern |
|---|---|---|
| Large Arteries (e.g., near branches) | 30 - 100 [27] | Pulsatile, Laminar |
| Small Arteries | 2 - 20 [27] | Laminar |
| Veins | 1 - 6 [27] | Laminar |
| Interstitial Flow | < a few µm/s velocity [31] [32] | Slow, Osmotically-driven |
Protocol for Setting Up Shear Stress:
- Chip Design and Calculation: For a rectangular microfluidic channel, calculate the required flow rate (Q) to achieve the target wall shear stress (τ) using the formula: τ = (6ηQ)/(h²w), where η is fluid viscosity, h is channel height, and w is channel width [27].
- Flow Control System Selection: Utilize a pressure-controlled or syringe pump system that provides precise, smooth flow without pulsations (unless pulsatile flow is desired) to avoid unwanted fluctuations in shear stress [27].
- Cell Seeding and Adaptation: Seed primary human endothelial cells (e.g., HUVECs or iPSC-derived) into the microfluidic channel and allow them to form a confluent monolayer under static conditions for 24-48 hours.
- Application of Flow: Initiate flow at a low rate (e.g., corresponding to 1 dyne/cm²) and gradually ramp up to the target physiological shear stress over 24 hours to allow for cellular adaptation.
- Validation and Measurement:
- Computational Modeling: Use the Navier-Stokes equation to model the velocity profile and resulting shear stress within the chip geometry [27].
- Real-time Sensing: Integrate transepithelial/transendothelial electrical resistance (TEER) electrodes to monitor barrier integrity in real-time under flow [28].
- Cell-based Sensors: Employ genetically encoded fluorescent biosensors that react to shear stress-induced signaling pathway activation (e.g., NF-κB or KLF2) [27].
Establishing Stable Chemical Concentration Gradients
Objective: To create stable, long-term chemical concentration gradients (e.g., of chemokines or nutrients) alongside mechanical shear stress gradients in a single microfluidic device.
Background: Immune cell migration and function are directed by chemokine gradients. Simultaneous exposure to chemical and mechanical cues more accurately represents the in vivo microenvironment that cells experience, such as in interstitial flow or during inflammatory responses [32].
Protocol for Simultaneous Gradient Generation:
- Device Fabrication: Fabricate a PDMS or polysulfone (PSF) plastic microfluidic chip containing a main culture channel and a parallel side channel for chemical introduction, connected via a porous membrane or microchannels [31] [33] [32].
- Osmotic Pump Integration: Implement an osmotic pump to generate very slow (< few µm/s), controlled flow, mimicking interstitial flow. This slow flow allows for wide and stable diffusion of chemicals, establishing a persistent concentration gradient across the cell culture chamber [31] [32].
- Passive Shear Stress Gradient: Design the main cell culture channel with a circular or varying geometry. The changing cross-section along the channel length passively creates a gradient of shear stress, with higher stress in narrower sections and lower stress in wider sections [32].
- Simultaneous Culture and Exposure: Seed cells such as L929 fibroblasts or primary endothelial cells in the main channel. Simultaneously expose the cells to the established shear stress gradient and a gradient of a chemical stimulus (e.g., a nutrient or chemokine like TNF-α) introduced from the side channel [32].
- Readout and Analysis: Assess cell alignment and mobility velocity (primarily affected by the shear stress level) and cell proliferation or differentiation (primarily reflecting the nutrient or chemical concentration level) after 24-72 hours of culture [32].
Integrating Complex Mechanical Cues in Multi-Organ Systems
Objective: To incorporate and monitor organ-specific mechanical cues, such as cyclic stretch and compression, into a multi-organ system to model integrated immune responses.
Background: Mechanical actuation is essential for realistic organ function. For example, breathing motions (cyclic stretch) in lung chips are essential for a physiological inflammatory response, and peristalsis-like motions in intestine chips create a robust barrier to bacterial infection [28].
Diagram: Integration of Mechanical Cues and Sensor Readouts in OoCs. The workflow shows how applied mechanical cues induce cellular responses that lead to measurable functional outcomes, which are quantified by integrated sensors to inform and validate the system.
Protocol for a Stretchable Lung-on-a-Chip with Immune Components:
- Chip Fabrication with Flexible Membrane: Fabricate the chip using a thin, flexible polymer membrane (e.g., PDMS or polyurethane) positioned between two microfluidic channels [33] [28].
- Cell Co-culture: Seed primary human alveolar epithelial cells on one side of the membrane and human lung microvascular endothelial cells on the other side to recreate the alveolar-capillary interface.
- Application of Cyclic Strain: Connect the side chambers of the chip to a vacuum system. Apply cyclic suction (e.g., 0.5 Hz, 10% strain) to the side chambers to rhythmically stretch the central membrane, mimicking physiological breathing motions [28].
- Introduction of Immune Components: Perfuse the endothelial channel with medium containing primary human peripheral blood mononuclear cells (PBMCs) or whole blood from specific donors under physiological shear stress.
- Challenge and Readout: Expose the epithelial channel to inflammatory stimuli such as TNF-α or bacterial lipopolysaccharide (LPS). Monitor the real-time recruitment of immune cells across the endothelial and epithelial layers in response to inflammation under breathing-mimetic conditions [28] [29].
The Scientist's Toolkit: Essential Reagents and Materials
Successfully implementing the aforementioned protocols requires a specific set of reagents, cells, and hardware. The following table details key components for building immunocompetent MOCs.
Table: Essential Research Reagent Solutions for Immunocompetent MOC Research
| Item Category | Specific Examples | Function & Application |
|---|---|---|
| Primary & iPSC-Derived Cells | Primary human endothelial cells (HUVEC), iPSC-derived brain microvascular endothelial-like cells, human bone marrow CD34+ cells, primary hepatocytes, EpiIntestinal cells [30] | Provide human-relevant cellular basis for organ models; enable creation of patient-specific models for precision medicine [34] [30]. |
| 3D Culture Matrices | Hydrogel scaffolds (e.g., collagen, Matrigel), 3D bioprinted composite bio-inks, 3D ceramic (hydroxyapatite) scaffolds [33] [30] | Support the formation of complex 3D tissue architectures that better mimic in vivo organ structure and function compared to 2D cultures. |
| Specialized Media & Supplements | Co-culture media, defined differentiation kits, cytokine supplements (e.g., TNF-α, interleukins) [3] [29] | Support the growth and maintenance of multiple cell types in one system and are used to induce inflammatory or differentiation states. |
| Microfluidic Chips & Consumables | PDMS-free multi-chip plates (PhysioMimix), TissUse Humimic Chips (2-, 4-organ), Emulate Organ-Chips [3] [30] | The physical platform that houses the organ models, providing perfused scaffolds and enabling microfluidic control. |
| Flow Control Systems | PhysioMimix Controller, pressure-controlled pumps, syringe pumps [3] [27] | Precisely manipulate fluid flow to generate physiological shear stress and enable inter-organ communication on-chip. |
| Integrated Sensors | TEER measurement electrodes, electrochemical sensors for metabolites, multi-electrode arrays (MEA) for electrophysiology [28] | Enable real-time, non-destructive monitoring of tissue barrier integrity, metabolic activity, and electrophysiological function. |
The advancement of immunocompetent Multi-Organ-on-Chip systems is intrinsically linked to the sophisticated integration of fluid shear stress, chemical gradients, and mechanical cues. As evidenced by the capabilities of commercial platforms and experimental protocols, these parameters are not isolated features but interdependent elements that collectively dictate the physiological fidelity of the model [26] [28]. The future of this field lies in the continued refinement of these parameters, coupled with the development of non-invasive, real-time biosensors [28] and their integration with PBPK modeling to create powerful predictive tools for drug absorption, distribution, metabolism, and excretion (ADME) and toxicity [33]. Furthermore, the trend toward personalization—using patient-derived primary cells, iPSCs, and biometric data—will enable these platforms to account for individual genetic and physiological variations, ultimately accelerating the development of effective, personalized immunotherapies and more precise safety toxicology assessments [34]. By systematically implementing and validating these key design parameters, researchers can leverage MOC technology to bridge the critical gap between animal models and human clinical outcomes in immunology research.
Incorporating Innate and Adaptive Immune Cells for Systemic Response Modeling
Microphysiological systems (MPS), or organ-on-a-chip (OOC) technologies, represent a transformative approach in biomedical research by recreating human physiology in vitro. These microfluidic devices contain hollow channels lined with living human cells arranged to simulate tissue-level functions [35]. A critical advancement in this field is the incorporation of both innate and adaptive immune cells to create immunocompetent models that more accurately mimic human systemic responses [10]. The rising recognition that the immune system underpins nearly every disease pathology—from cancer and infectious diseases to autoimmune disorders—has driven innovation in this area [10]. This guide objectively compares current technologies and methodologies for modeling human immunity in MPS, providing researchers with experimental data and protocols to advance their work in drug development and disease modeling.
Technology Platforms for Immune System Modeling
Commercial MPS Platforms at a Glance
Several commercial platforms now enable researchers to create immunocompetent MPS models. The table below compares key technologies and their capabilities for immune system integration.
Table 1: Commercial MPS Platforms for Immune System Modeling
| Platform Name | Manufacturer | Key Features for Immune Modeling | Throughput Capabilities | Demonstrated Immune Applications |
|---|---|---|---|---|
| AVA Emulation System | Emulate [6] | 3-in-1 Organ-Chip platform; High-throughput; Automated imaging; Chip-R1 for immune cell recruitment | 96 Organ-Chip "Emulations" in a single run | Lymph Node-Chip for antigen-specific immune responses; Intestine-Chip for IBD studies |
| PhysioMimix Core | CN Bio [3] | PDMS-free plates; Adjustable recirculating flow; Open architecture for model customization | Up to 288 samples per controller unit (6 plates) | Liver and kidney safety assessment; Multi-organ crosstalk studies |
| OrganoPlate | MIMETAS [10] | 3-lane channel design; Gravity-driven flow; 64-chips per plate | 64 chips per plate | Barrier immunity models (intestine, lung, blood-brain barrier) |
| HUMIMIC Chip2 | TissUse [10] | Multi-organ capability; Up to four organ compartments connected by fluidic channels | Two or four organ compartments per chip | Systemic toxicity and ADME studies with immune components |
Technical Specifications of Featured Platforms
For researchers considering specific platforms, detailed technical specifications inform experimental design and infrastructure requirements.
Table 2: Detailed Technical Specifications of Select MPS Platforms
| Parameter | PhysioMimix Core [3] | AVA Emulation System [6] | Emulate Chip-S1/Chip-A1 [6] [10] |
|---|---|---|---|
| Platform Dimensions | Controller: 230mm (W) x 430mm (D) x 415mm (H) | Combined microfluidic control, imaging, and incubation | Varies by chip type (e.g., rigid vs. stretchable chips) |
| Incubator Requirements | Standard cell culture incubator with side/rear port | Self-contained incubator | Requires external incubator |
| Multi-Organ Capability | Yes, seamless progression from single- to multi-organ | Not explicitly stated | Yes, via fluidic linking of multiple single-organ chips |
| Fluidic Flow Control | Adjustable recirculating flow rate | Precision microfluidic control | Applied mechanical forces and fluid flow |
| Throughput | Up to 6 plates (6-288 samples) per controller | 96 independent Organ-Chip samples | Lower throughput, more specialized models |
| Primary Cell Compatibility | Yes, with validated kits | Yes, as demonstrated in published applications | Yes, including patient-derived cells |
| Key Immune Application | ADME and toxicology with immune components | Lymph Node-Chip for immunotoxicity testing | Innate immune responses in Lung-Chip and Intestine-Chip |
Experimental Data from Immunocompetent MPS Models
Quantitative Assessment of Immune Responses
Recent studies have generated robust quantitative data demonstrating the functionality of immune cells within MPS. The following table summarizes key experimental findings from immunocompetent models.
Table 3: Experimental Immune Response Data from Immunocompetent MPS
| MPS Model Type | Immune Components Integrated | Challenge/Stimulus | Key Quantitative Readouts | Reference |
|---|---|---|---|---|
| Small Airway Lung-Chip [36] | Tissue-resident macrophages, DCs, granulocytes, neutrophils, T cells, B cells, NK cells | Severe H1N1 infection (MOI 5) | • Significant cytokine storm (IL-6, IL-8, MCP-1) • Epithelial cell damage • Immune cell activation and migration | Singh et al., 2025 |
| Lymph Node-Chip [6] | Antigen-presenting cells, T cells | Antigen-specific challenge | • Predictive antigen-specific immune responses • T cell activation markers • Cytokine secretion profiles | Pfizer Data, 2025 |
| Intestine-Chip [6] | Peripheral immune cells, tissue-resident immune populations | Inflammatory Bowel Disease (IBD) therapeutics | • Impact on goblet cells and barrier integrity • Cytokine levels • Immune cell recruitment | AbbVie Data, 2025 |
| Bone Marrow-Chip [37] | Hematopoietic stem and progenitor cells (HSPCs) | Trained immunity inducers (BCG, β-glucan) | • Epigenetic reprogramming (H3K4me3, H3K27ac) • Metabolic shifts (aerobi glycolysis) • Enhanced cytokine production | Netea et al., 2025 |
Protocol: Establishing an Immunocompetent Small Airway Lung-Chip
The following detailed methodology is adapted from Singh et al. (2025) for creating a sophisticated immunocompetent small airway lung-on-a-chip model [36].
Device Fabrication and Preparation
- Microfluidic Device: Utilize a two-channel microfluidic device separated by a porous (5.0 µm) polyester track-etched (PETE) membrane to allow immune cell migration.
- Surface Treatment: Treat the device with 0.1% pluronic F-127 for 30 minutes at room temperature to prevent non-specific cell adhesion, followed by PBS rinsing.
- Extracellular Matrix Coating:
- Airway channel: Coat with 30 µg/mL collagen IV at 37°C for 2 hours.
- Vascular channel: Coat with 100 µg/mL fibronectin at 37°C for 2 hours.
Cell Seeding and Culture
Day 0: Endothelial Network Formation
- Prepare a hydrogel solution containing human pulmonary fibroblasts (1.5 × 10^6 cells/mL) and human umbilical vein endothelial cells (HUVECs) (5 × 10^6 cells/mL) in a fibrinogen (6 mg/mL) and collagen I (1.5 mg/mL) mixture.
- Inject the hydrogel-cell mixture into the vascular channel and allow polymerization at 37°C for 30 minutes.
- Flow endothelial cell medium through the vascular channel continuously at 30 µL/hour.
Day 2: Epithelial Layer Seeding
- Seed small airway epithelial cells (SAECs) (2 × 10^6 cells/mL) into the airway channel.
- Culture submerged for 3 days with daily medium changes.
Day 5: Air-Liquid Interface (ALI) Establishment
- Drain apical medium from the airway channel to establish ALI.
- Continue feeding the vascular channel continuously and provide medium to the airway channel basolaterally only.
- Culture for 10-14 days to allow epithelial differentiation and mucociliary clearance development.
Day 14-16: Immune Cell Integration
- Tissue-resident immune cells: Introduce during hydrogel formation or after endothelial network maturation.
- Circulatory immune cells: Introduce through the vascular channel after ALI establishment, using whole blood or isolated PBMCs at physiological ratios.
Infection and Analysis
- Viral Infection: Apply H1N1 influenza virus at MOI 5 in small volume to the apical surface of the airway epithelium for 2 hours, then remove.
- Readouts and Measurements:
- Cytokine profiling: Collect effluents daily for multiplex cytokine analysis (IL-6, IL-8, MCP-1, TNF-α, IFNs).
- Immunofluorescence: Fix devices and stain for cell-specific markers (CD45 for immune cells, CD31 for endothelium, TUBB4A for ciliated cells).
- Transcriptomics: Process cells for single-cell RNA sequencing to identify pathway alterations.
- Permeability assays: Measure FITC-dextran flux across the epithelial-endothelial barrier.
Figure 1: Experimental workflow for establishing an immunocompetent small airway lung-on-a-chip model.
Signaling Pathways in Immunocompetent MPS
Key Immune Signaling Pathways in Influenza Infection Model
Research using immunocompetent lung-on-a-chip models has elucidated critical signaling pathways that regulate immune responses to viral infection. The following diagram illustrates the key pathways identified in severe influenza infection models [36].
Figure 2: Key immune signaling pathways in a lung-on-a-chip model of severe influenza.
Pathway Inhibition and Therapeutic Implications
Experimental manipulation of these pathways in the immunocompetent lung-chip revealed important therapeutic insights [36]:
- IL-1β inhibition: Completely ameliorated the cytokine storm, suggesting potential for severe influenza treatment.
- TNF-α inhibition: Resulted in a highly increased inflammatory response, indicating its critical regulatory role.
- CXCR4 axis inhibition: Modulated the inflammatory landscape by decreasing pro-inflammatory cytokines while increasing antiviral interferons.
The Scientist's Toolkit: Essential Research Reagents
Successful establishment of immunocompetent MPS requires specific reagents and materials. The following table details essential components for modeling innate and adaptive immunity in microphysiological systems.
Table 4: Essential Research Reagents for Immunocompetent MPS
| Reagent Category | Specific Examples | Function in Immunocompetent MPS | Application Notes |
|---|---|---|---|
| Primary Cells | Small airway epithelial cells (SAECs), HUVECs, pulmonary fibroblasts | Form the foundational tissue structure and microvasculature | Source from reputable providers; maintain donor records for HLA matching [36] |
| Immune Cells | PBMCs, tissue-resident macrophages, neutrophils, T cells, B cells, DCs | Mediate immune responses and recapitulate inflammatory processes | Isate fresh or use cryopreserved vials from same donor; use HLA-matched cells when possible [10] |
| ECM Components | Collagen IV, fibronectin, fibrinogen, Matrigel | Provide structural support and biochemical cues for cell organization | Tailor composition to specific organ microenvironment [36] |
| Cell Culture Media | Endothelial cell medium, epithelial air-liquid interface medium | Support cell viability, differentiation, and function | Use specialized media formulations for different cell types; consider custom blends [36] |
| Cytokines/Chemokines | IL-1β, TNF-α, CXCL12, IFN-γ | Modulate immune cell behavior and signaling pathways | Use for controlled immune activation studies; validate concentrations [36] [37] |
| Analysis Reagents | Multiplex cytokine arrays, immunofluorescence antibodies, scRNA-seq kits | Enable quantitative assessment of immune responses | Plan analysis workflow ahead; ensure antibody compatibility with fixed chip samples [36] |
The integration of innate and adaptive immune cells into MPS represents a significant advancement in modeling human systemic responses. Current technologies from commercial providers like Emulate, CN Bio, and MIMETAS offer diverse platforms suited to different research needs, from high-throughput screening to complex multi-organ studies. Experimental data demonstrates that these immunocompetent models can recapitulate critical aspects of human immune responses, including cytokine storms, immune cell recruitment, and antigen-specific activation.
Future developments will likely focus on improving long-term immune cell viability, establishing standardized protocols for immune cell integration, and addressing the challenge of HLA matching between different cell types from various donors [10]. Additionally, the incorporation of trained immunity concepts—where innate immune cells develop memory-like characteristics through epigenetic and metabolic reprogramming—opens new avenues for modeling chronic inflammation and vaccine responses [37]. As these technologies continue to mature, immunocompetent MPS will play an increasingly vital role in drug development, personalized medicine, and fundamental immunology research.
From Theory to Therapy: Applications in Immunotherapy and Systemic Toxicology
Screening and Optimizing Cancer Immunotherapies (e.g., CAR-T, Checkpoint Inhibitors)
Cancer immunotherapy, particularly Chimeric Antigen Receptor T-cell (CAR-T) therapy and immune checkpoint inhibitors (ICIs), has revolutionized oncology treatment by harnessing the body's immune system to combat cancer. Despite remarkable success in hematological malignancies, the development of novel immunotherapeutic agents faces persistent challenges due to poor translation from preclinical to clinical stages [38]. A significant barrier is the limited predictive value of traditional preclinical models; animal models often fail to recapitulate human immune responses due to species-specific differences, while conventional 2D in vitro cultures lack the physiological complexity of the human tumor microenvironment (TME) [9] [18].
Within this challenging landscape, human organ-on-chip (Organ-Chip) systems have emerged as a transformative technology to bridge this translational gap. These microfluidic devices are lined with living human cells cultured under fluid flow to recapitrate organ-level physiology and pathophysiology with high fidelity [9]. This review objectively compares the performance of Organ-Chip platforms against traditional models in screening and optimizing cancer immunotherapies, focusing on their experimental application, quantitative outcomes, and specific protocols that demonstrate their value in predicting human clinical responses.
Performance Comparison: Organ-Chip vs. Traditional Models
The table below summarizes a direct comparison of key performance metrics between Organ-Chip systems and traditional preclinical models, based on experimental data from published studies.
Table 1: Performance Comparison of Preclinical Models in Cancer Immunotherapy Safety and Efficacy Assessment
| Performance Metric | Traditional 2D Models | Animal Models | Human Organ-Chip Models |
|---|---|---|---|
| Prediction of Clinical Immunotoxicity | Poor (Failed to predict FOLR1 TCB toxicity) [18] | Variable (Failed in TGN1412 trial; predicted FOLR1 TCB lung toxicity in primates) [18] [39] | High (Accurately replicated FOLR1 & CEA TCB toxicity profiles and affinity-dependent effects) [18] [40] |
| Physiological Antigen Expression | Non-physiological, altered levels and patterns [18] | Species-specific differences (e.g., human CEA not cross-reactive) [18] | Physiologically relevant (e.g., CEA expression gradient in intestine chips mimicking human tissue) [18] [40] |
| Immune Cell Recruitment & Function | Limited, lacks vascular perfusion and cell migration [39] | Intact but species-specific [38] | Demonstrated (T-cell infiltration, activation, and target-cell killing quantified on-chip) [18] |
| Throughput & Scalability | High | Low | Medium (Increasing with multi-organ systems and robotic coupling) [9] [38] |
| Key Supporting Experimental Data | Transwell cultures failed to recapitulate primate toxicity data [40] | Severe lung toxicity in primates with FOLR1(Hi) TCB [18] | Quantified epithelial cytotoxicity: ~60% (Colon) vs ~20% (Duodenum) with CEA TCB; Affinity-dependent safety profile confirmed [18] |
Experimental Protocols for Immunotherapy Evaluation on Organ-Chips
This section details the specific methodologies used to generate the comparative data, providing a toolkit for researchers to implement these models.
Protocol: Evaluating On-Target, Off-Tumor Toxicity of T-Cell Bispecific Antibodies (TCBs)
This protocol, adapted from Kerns et al. and Cabon et al., outlines the steps for assessing the safety of TCBs using human immunocompetent Organ-Chips [18] [40].
Chip Fabrication and Seeding:
- Device: Use a two-channel microfluidic device made of Polydimethylsiloxane (PDMS) or other polymers, separated by a porous membrane coated with extracellular matrix (e.g., collagen IV) [18].
- Tissue-Specific Cells: Seed primary human organ-specific cells (e.g., lung alveolar epithelial cells, intestinal duodenum/colon epithelial cells) in the top channel. Culture at an air-liquid interface (ALI) for lung or liquid-liquid interface for intestine to promote maturation [18] [40].
- Vascular Channel: Seed primary human microvascular endothelial cells in the bottom channel to form a vascular tube [18].
Model Maturation:
- Culture the chips for 5-14 days to allow the formation of confluent, differentiated, and functional tissue barriers. Maturity is assessed by measuring transepithelial/transendothelial electrical resistance (TEER) and immunostaining for tight junction proteins [18].
Introduction of Immune Compartment:
- Isulate Peripheral Blood Mononuclear Cells (PBMCs) from healthy human donors.
- Perfuse PBMCs through the vascular channel, allowing them to interact with the endothelium and, under inflammatory cues, migrate into the tissue compartment [18].
Immunotherapy Treatment:
- Introduce the therapeutic agent (e.g., FOLR1-TCB or CEA-TCB) into the vascular channel at clinically relevant concentrations. Include control groups with non-targeting antibodies [18].
Real-Time Monitoring and Endpoint Analysis:
- Cell Killing/Viability: Quantify apoptosis and cell death in the tissue layer in real-time using live-cell imaging of fluorescent dyes (e.g., caspase-3/7 reagents) or by endpoint measurement of lactate dehydrogenase (LDH) release [18].
- Immune Cell Activation: Collect effluent from the vascular channel and analyze by flow cytometry for T-cell activation markers (e.g., CD69, CD25) and cytokine release (e.g., IL-2, IFN-γ, IL-6) via ELISA or multiplex assays [18].
- Morphological and Barrier Function Analysis: Fix and immunostain chips for microscopy to assess tissue integrity, immune cell infiltration, and target antigen expression. Monitor barrier function via TEER throughout the experiment [18].
Protocol: Assessing CAR-T Cell Trafficking and Tumor Cell Killing
While the search results focus on TCBs, the principles can be extended to CAR-T cells, a key area of development in microfluidic models [38].
Tumor Microenvironment (TME) Compartment Setup:
- In one channel of a multi-channel chip, embed cancer cells (as a monolayer, spheroid, or patient-derived organoid) within a 3D hydrogel matrix (e.g., Matrigel, collagen) to mimic the TME [38].
Vascular Compartment Setup:
- Seed endothelial cells in an adjacent channel to form a perfusable vessel. The hydrogel and vascular channels can be separated by a membrane or directly abutted to allow for cell migration [38].
CAR-T Cell Introduction and Trafficking:
- Generate CAR-T cells specific to a tumor antigen (e.g., CD19, BCMA, or solid tumor targets like GD2 or MSLN) [41] [42].
- Perfuse fluorescently labeled CAR-T cells through the vascular channel.
- Quantify CAR-T cell adhesion to the endothelium, extravasation, and migration towards the tumor compartment using time-lapse microscopy [38].
Tumor Killing Efficacy Assessment:
- Co-culture CAR-T cells with the established tumor compartment.
- Measure tumor cell death in real-time using live-cell imaging and fluorescent viability/cell death markers.
- Analyze cytokine profiles in the effluent to assess the potency and potential cytokine release syndrome (CRS)-like activity [38].
Visualization of Experimental Workflow and Signaling
The following diagram illustrates the core experimental workflow and key biological events in a generalized immunocompetent Organ-Chip model for immunotherapy testing.
Figure 1: Workflow for Evaluating Immunotherapies on Organ-Chips. This diagram outlines the key steps, from chip establishment to quantitative endpoint analysis, for assessing both efficacy and on-target, off-tumor toxicity.
The diagram below details the molecular mechanism of action of a T-cell engaging bispecific antibody (TCB) within the Organ-Chip, leading to either intended tumor cell killing or unintended on-target, off-tumor toxicity in healthy tissue.
Figure 2: Mechanism of TCB-Mediated Target Cell Killing. The TCB crosslinks the CD3 complex on T-cells with a Tumor-Associated Antigen (TAA) on a target cell, triggering T-cell activation and cytotoxic killing of the target cell, which can be either a tumor cell (desired) or a healthy cell expressing the TAA (on-target, off-tumor toxicity).
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential materials and reagents used in the featured Organ-Chip experiments, providing a practical resource for protocol implementation.
Table 2: Essential Research Reagents for Organ-Chip Immunotherapy Studies
| Reagent / Material | Function / Application | Specific Examples from Literature |
|---|---|---|
| Primary Human Cells | Recreate organ-specific parenchyma and vasculature with human-specific biology. | Lung alveolar epithelial cells, intestinal epithelial cells, lung microvascular endothelial cells [18]. |
| Hydrogel Matrix | Provide a 3D scaffold to support cell growth and mimic the extracellular matrix (ECM). | Collagen IV, Matrigel [18]. |
| Peripheral Blood Mononuclear Cells (PBMCs) | Source of human immune cells (T-cells, NK cells, monocytes) for immunocompetence. | Isolated from healthy human donor blood [18]. |
| T-Cell Bispecific Antibodies (TCBs) | Engineered immunotherapeutics to test efficacy and safety. | FOLR1-targeting TCB, CEA-targeting TCB, with high- and low-affinity variants [18] [40]. |
| Microfluidic Device | Platform housing the living cellular model and enabling controlled perfusion. | PDMS-based chips with two parallel channels separated by a porous membrane [9] [18]. |
| Cell Viability/Cytotoxicity Assays | Quantify target cell death and overall tissue health. | Live-cell imaging with caspase-3/7 reagents, Lactate Dehydrogenase (LDH) release assays [18]. |
| Cytokine Detection Kits | Measure immune cell activation and potential for cytokine release syndrome (CRS). | ELISA, multiplex bead-based arrays for IL-2, IFN-γ, IL-6, IL-8 [18]. |
The experimental data and protocols detailed herein demonstrate that human immunocompetent Organ-Chip systems offer a quantitatively superior and more physiologically relevant platform for screening and optimizing cancer immunotherapies compared to traditional models. Their proven ability to recapitulate on-target, off-tumor toxicities, predict affinity-dependent safety profiles, and model human-specific immune responses positions this technology as a critical tool for de-risking drug candidates prior to clinical trials [18] [40]. As the field advances, the integration of multiple organ systems into a "human-on-a-chip" represents the next frontier, promising a holistic, systemic view of immunotherapy efficacy and safety that could fundamentally accelerate and improve the drug development process [9] [39].
Modeling ADME and Pharmacokinetics (PK/PD) in Connected Organ Systems
The high failure rate of drug candidates in clinical trials, often due to unforeseen human Absorption, Distribution, Metabolism, and Excretion (ADME) and toxicity profiles, underscores a critical inadequacy in conventional preclinical models [9] [1]. Traditional 2D cell cultures cannot replicate organ-level physiology, while animal models frequently suffer from species-specific differences that limit their predictive power for human responses [30] [1]. Microphysiological Systems (MPS), often called Multi-Organ-on-a-Chip (MOC), have emerged as a transformative technology designed to bridge this gap. These microfluidic devices culture living, functional human tissues in fluidically connected chambers, recapitulating the dynamic organ-organ crosstalk essential for accurate modeling of systemic drug disposition and pharmacological effects [43] [44] [45]. By replicating a human pharmacokinetic-pharmacodynamic (PK-PD) model in vitro, MOCs offer a powerful platform for predicting a drug's journey through the body and its ultimate effect on its target [33] [45].
Comparative Analysis of Multi-Organ-on-Chip Platforms for ADME/PK
Various MOC platforms have been developed and validated to study specific ADME and PK/PD pathways. The table below summarizes key assays, their configurations, and their primary applications in drug development.
Table 1: Comparison of Validated Multi-Organ-on-Chip Assays for ADME/PK Modeling
| Organ Model | Key Organs Included | Primary ADME/PK Application | Notable Features & Validated Compounds | Supporting In Vivo Studies |
|---|---|---|---|---|
| Intestine-Liver-Kidney-Neuro MOC [30] | Small intestine, Liver, Kidney, Neural Spheroids | Comprehensive ADME profiling, PBPK modeling, first-pass metabolism, organ toxicity. | Models excretion (kidney), metabolism (liver), distribution, and absorption (intestine). Validated with Haloperidol, Carbamazepine. | In vivo PBPK profiling, in vivo ADME [30] |
| Gut/Liver-on-a-Chip [30] [4] | Small intestine, Liver | Oral bioavailability, first-pass metabolism, organ-organ crosstalk. | Compares oral vs. IV dosing; open system for sampling drug/metabolite kinetics. | In vivo PK/PD profiling, in vivo ADME [30] |
| BBB-Liver MPS [30] | Blood-Brain Barrier (BBB), Liver | BBB permeability, neurotoxicity, metabolite neurotoxicity. | Uses iPSC-derived brain endothelial cells & neural spheroids; incorporates fluidic shear stress. Validated with Atenolol, Propranolol. | In vivo PK/PD profiling, efficacy in neurodegenerative models [30] |
| Lung/Liver-on-a-Chip [4] | Lung (Bronchial/Alveolar), Liver | PK of inhaled drugs, systemic effects of pulmonary exposure, inflammatory response. | Models air-liquid interface; co-cultures epithelial and endothelial layers. | Determines uptake and metabolism of inhaled/IV drugs [4] |
| Bone Marrow MPS [30] | Bone Marrow (hematopoietic niche) | Hematological toxicity, dose-range finding. | Uses human CD34+ cells & mesenchymal stromal cells in a 3D scaffold; tracks lineage cell output. | In vivo toxicology testing, in vivo dose response [30] |
Key Advantages Over Traditional Models
The predictive power of MOCs stems from their ability to more accurately mimic human physiology:
- Enhanced Metabolic Competence: Liver-on-chip models maintain higher and more sustained expression of Cytochrome P450 (CYP) enzymes compared to static cultures. For instance, the Liver Acinus Dynamic (LADY) chip showed remarkably increased CYP2E1 expression, which is crucial for accurate drug metabolism data [1].
- Physiological Barriers and Transport: MOCs support the correct polarization of cells and the expression of native arrays of drug transporters. For example, human kidney epithelial cells in a microfluidic device demonstrated higher P-glycoprotein (P-gp) expression and activity than in conventional cultures [1].
- Systemic Toxicity and Off-Target Effects: MOCs enable the detection of secondary organ toxicity. The inclusion of a liver model can reveal how metabolites produced by hepatic metabolism might affect other tissues, such as the brain in the BBB-Liver model [30].
Experimental Protocols for Key Multi-Organ Assays
Protocol: ADME Profiling Using a Gut-Liver-Kidney-Neuro MOC
This protocol outlines the steps for assessing the comprehensive ADME profile of a drug candidate using a four-organ system [30].
- Objective: To quantify the absorption, metabolism, distribution, and excretion of a test compound and its metabolites across multiple human organ barriers.
- Cell Sources:
- Intestine: Primary small intestine barrier cells on a Transwell insert.
- Liver: Primary liver spheroids (e.g., mu-tissue spheroids).
- Kidney: iPSC-derived glomerular cells and proximal tubule lines.
- Neuro: iPSC-derived glial spheroids.
- Methodology:
- System Assembly: Seed each cell type into its respective chamber of the MOC platform (e.g., TissUse's Humimic Chip). Connect chambers via microfluidic channels to allow shared circulation of medium.
- Tissue Maturation: Perfuse the system with culture medium for several days to allow tissues to mature and establish stable, organ-specific functions.
- Dosing: Introduce the test compound into the intestinal chamber (for oral absorption simulation) or directly into the common medium reservoir (for systemic exposure simulation).
- Sampling and Kinetic Analysis:
- Collect serial samples from the common medium circuit over a defined period (e.g., 0, 1, 2, 4, 8, 24, 48 hours).
- Analyze samples using LC-MS/MS to quantify the parent compound and its metabolites.
- Generate concentration-time profiles for the parent drug and major metabolites.
- Endpoint Analysis:
- Measure tissue viability and integrity (e.g., TEER for barrier tissues).
- Analyze gene expression (qPCR) of key transporters and metabolizing enzymes.
- Perform immunohistochemistry on tissue constructs to assess morphology and toxicity.
- Data Output: Compound and metabolite kinetic profiles, extraction of PK parameters (e.g., AUC, C~max~, T~max~, half-life), and assessment of primary and secondary organ toxicity.
Protocol: Assessing Blood-Brain Barrier Permeability with a BBB-Liver MOC
This protocol is designed to evaluate a compound's ability to cross the BBB and the potential role of liver metabolism in modifying this process [30].
- Objective: To determine the brain/circulation ratio of a compound and investigate the neurotoxicity of its liver-generated metabolites.
- Cell Sources:
- BBB: Brain microvascular endothelial-like cells derived from induced pluripotent stem cells (iPSCs).
- Brain: Neural spheroids.
- Liver: Primary hepatocytes or hepatocyte-like cells.
- Methodology:
- Chip Preparation: The BBB is formed on a porous membrane separating a "vascular" channel from a "brain parenchymal" channel where neural spheroids are located. The liver chamber is connected downstream.
- Integrity Validation: Measure Transendothelial Electrical Resistance (TEER) regularly to confirm the formation of a tight BBB.
- Compound Perfusion: Perfuse the test compound through the "vascular" channel.
- Sampling: Collect effluent from the "brain parenchymal" channel and the common circulation over time.
- Analysis:
- Quantify the compound concentration in both brain and circulation compartments to calculate the brain/circulation ratio.
- Identify metabolites formed by the liver compartment.
- Assess neural spheroid viability and function (e.g., electrophysiology, biomarker release) to evaluate neurotoxicity.
- Validation: The assay is validated using control compounds like atenolol (low permeability) and propranolol (high permeability), confirming its ability to replicate known in vivo BBB properties [30].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of MOC technology relies on a suite of specialized materials and reagents that ensure physiological relevance and data accuracy.
Table 2: Key Reagents and Materials for MOC Experiments
| Item Category | Specific Examples | Function & Importance | Technical Considerations |
|---|---|---|---|
| Chip Materials | Cyclic Olefin Copolymer (COC), Polysulfone (PSF) [33] [4] | Inert materials that minimize non-specific binding of small molecules, crucial for accurate PK predictions. | Preferred over PDMS for drug testing due to PDMS's adsorption of hydrophobic molecules [33] [4]. |
| Cell Sources | Primary human hepatocytes [1], iPSC-derived cells (BBB, neural, renal) [30], Organoids [9] | Provide human-specific and physiologically relevant responses. iPSCs enable patient-specific modeling. | Primary cells can have high variability; HepaRG cells are a promising alternative with high metabolic activity [1]. |
| Scaffolds & ECM | 3D Hydrogels, Ceramic Scaffolds (e.g., hydroxyapatite for bone marrow) [30] | Provide a 3D architecture that supports complex cell-cell interactions and tissue-specific differentiation. | Bioprinting with composite bio-inks can be used to create endothelialized tissues [33]. |
| Analysis Kits & Assays | TEER Measurement Kits [30], LC-MS/MS | TEER quantifies barrier tissue integrity. LC-MS/MS is the gold standard for quantifying drugs and metabolites in kinetic studies. | Integrated biosensors for real-time monitoring of O~2~, pH, and metabolites are an emerging advancement [45]. |
| Culture Media | Specialized perfusion media | Dynamic flow in microfluidic channels supplies nutrients and removes waste, maintaining long-term tissue viability. | Medium composition must be optimized to support multiple different cell types simultaneously [45]. |
Visualizing MOC Workflows and Physiological Principles
The predictive power of MOCs is rooted in their ability to replicate human physiology. The diagram below illustrates the core physiological processes and technological workflow integrated into these systems.
Diagram 1: Recapitulating Systemic ADME in a Multi-Organ-Chip. The MOC technology (bottom) mirrors the key stages of the human ADME process (top) by connecting individual organ models via a microfluidic circulatory system.
The integration of MOC data with computational models creates a powerful feedback loop for prediction. The following diagram outlines this workflow for a specific application.
Diagram 2: AI-PBPK and MOC Workflow for PK/PD Prediction. This workflow combines in silico predictions (AI-PBPK modeling) with experimental data from MOCs to refine and validate models for predicting human in vivo outcomes [46].
Multi-Organ-on-Chip technology represents a paradigm shift in preclinical ADME and PK/PD modeling. By providing a human-relevant, system-level platform that recapitulates critical organ-organ interactions, MOCs significantly enhance the predictive accuracy of drug disposition, metabolic fate, and toxicity. The ongoing integration of these systems with PBPK modeling and artificial intelligence promises to further strengthen their utility, potentially reducing the pharmaceutical industry's reliance on animal models and accelerating the development of safer, more effective therapeutics [33] [46]. As standardization and validation efforts continue, MOCs are poised to become an indispensable tool in the drug developer's toolkit, bridging the long-standing gap between traditional in vitro assays and clinical outcomes in humans.
Systemic immunotoxicity testing represents a critical challenge in drug development and chemical safety assessment. Traditional methods, particularly animal models, face significant limitations in predicting human responses due to species-specific differences in immune function and drug metabolism [47]. This case study examines nickel-induced skin sensitization as a paradigm for evaluating how multi-organ-on-chip (MOC) systems can recapitulate complex human immune responses. Nickel allergy affects approximately 20% of the general population in European countries and serves as an ideal model for understanding Type IV (delayed-type) hypersensitivity reactions [48] [49].
The transition toward human-relevant testing platforms is accelerating due to scientific, regulatory, and ethical considerations. With the FDA announcing plans to phase out animal testing requirements for monoclonal antibodies and Congress passing the FDA Modernization Act 3.0 in 2024, the regulatory landscape is increasingly supportive of alternative methods [47]. This analysis compares traditional, emerging, and next-generation approaches for investigating nickel sensitization, with particular emphasis on their application in validating MOC systems that incorporate human immunity.
Nickel Sensitization: Pathophysiological Framework
Immunological Mechanisms of Nickel Allergy
Nickel (Ni) functions as a hapten, a low molecular weight chemical (under 500 Da) that becomes immunogenic after binding to self-proteins [48]. The most common oxidation state for nickel is +2 (Ni2+), which preferably binds to proteins through the imidazole nitrogen of histidine and the thiol groups of cysteine residues [50]. This binding represents the molecular initiating event (MIE) in the Adverse Outcome Pathway (AOP) for skin sensitization [51] [48].
The subsequent immune response involves both innate and adaptive components. Ni2+ ions can directly bind to specific T-cell receptors, particularly engaging the TRAV9-2 gene segment or a histidine residue in the CDR3 region [50]. This unique mechanism enables nickel to bypass conventional MHC-restricted antigen presentation, triggering the proliferation of allergen-specific T lymphocytes [50] [49]. The sensitization phase culminates in the generation of memory T cells, which upon re-exposure to nickel, initiate the elicitation phase characterized by inflammatory skin reactions including erythema, eczema, and itching [48].
Adverse Outcome Pathway for Skin Sensitization
The OECD-defined Adverse Outcome Pathway for skin sensitization provides a structured framework for understanding the sequence of events from chemical exposure to clinical manifestation [51] [48]. The AOP organizes the process into four key events (KE):
- KE1 (Molecular Initiating Event): Covalent binding of electrophilic substances (haptens) to nucleophilic centers in skin proteins.
- KE2 (Keratinocyte Response): Keratinocyte activation and release of inflammatory mediators, including IL-18 and IL-1α.
- KE3 (Dendritic Cell Activation): Dendritic cells capture and process hapten-protein complexes, then mature and migrate to lymph nodes.
- KE4 (T-cell Proliferation): Antigen presentation to naïve T-cells, leading to proliferation and differentiation of hapten-specific T cells.
The following diagram illustrates this pathway and the alternative testing methods that address each key event:
Comparative Analysis of Testing Platforms
Traditional Animal Models
Animal tests have historically formed the cornerstone of regulatory safety assessment for skin sensitization potential. The following table summarizes the primary in vivo methods:
Table 1: Traditional Animal Models for Skin Sensitization Assessment
| Test Method | Species | Key Endpoint | OECD Guideline | Advantages | Limitations |
|---|---|---|---|---|---|
| Guinea Pig Maximization Test (GPMT) | Guinea pig | Challenge-induced erythema | OECD 406 | Established historical data | Subjective scoring, high animal use |
| Buehler Test | Guinea pig | Epidermal reactivity | OECD 406 | Non-adjuvanted method | Lower sensitivity |
| Local Lymph Node Assay (LLNA) | Mouse | Lymphocyte proliferation | OECD 429 | Quantitative, reduced suffering | Radioactive labeling required |
| LLNA: DA | Mouse | Lymphocyte ATP levels | OECD 442A | Non-radioactive | Moderate predictivity for metals |
| LLNA: BrdU-ELISA/FCM | Mouse | Lymphocyte proliferation | OECD 442B | Non-radioactive | Limited potency estimation |
While animal models provide whole-organism responses, significant limitations impact their predictive value for human immunotoxicity. Species differences in immune repertoire, cytokine expression, and pathogen recognition pathways frequently lead to misleading results [47] [52]. Analysis of clinical trial data shows that up to half of failures occur because drugs do not demonstrate efficacy in humans, with approximately 30% failing due to unmanageable toxicity not predicted by animal studies [47]. For nickel specifically, the LLNA has demonstrated approximately 89% repeatability in mice, but inter-species agreement between mouse and guinea pig models is only 77% [51].
Emerging Non-Animal Alternative Methods
The ban on animal testing for cosmetics in the European Union (EU Cosmetics Regulation 1223/2009) has accelerated development of alternative methods aligned with the Adverse Outcome Pathway [48]. These approaches include in chemico, in vitro, and in silico methods:
Table 2: Alternative Non-Animal Methods for Skin Sensitization Assessment
| Method Category | Examples | Key Event Addressed | Measurement Endpoint | Regulatory Status |
|---|---|---|---|---|
| In chemico | DPRA, ADRA, kDPRA | KE1 (Protein binding) | Peptide depletion kinetics | OECD Guideline 442C |
| In vitro (Keratinocyte) | LuSens, SENS-IS | KE2 (Keratinocyte activation) | Gene expression (ARE/Nrf2 pathway) | OECD Guideline 442D |
| In vitro (Dendritic cell) | h-CLAT, U-SENS | KE3 (Dendritic cell activation) | Surface marker expression (CD86, CD54) | OECD Guideline 442E |
| Reconstructed Human Epidermis | EpiSensA | KE1 & KE2 combined | Multiple endpoints | OECD Guideline 442D |
| In silico | QSAR, Read-across | KE1 (Predicted reactivity) | Structural alert identification | Regulatory support |
These individual methods face technical limitations including issues with highly lipophilic substances and lack of reliable potency estimation [48]. No single alternative method currently serves as a stand-alone replacement for the reference murine LLNA, leading to the development of integrated testing strategies that combine data from multiple sources [51] [48].
Multi-Organ-on-Chip Platforms
Multi-organ-on-chip (MOC) technology represents a transformative approach that integrates multiple microphysiological systems on a single platform to simulate systemic drug absorption, distribution, metabolism, and excretion [53]. These microfluidic devices create dynamic, human-relevant environments that recapitulate tissue-tissue interfaces and vascular perfusion more accurately than static in vitro models [53] [6].
For immune-specific applications, immune-system-on-chip (ISOC) technology has been developed to model the complex interactions between innate and adaptive immunity [19]. These platforms can incorporate circulating immune cells, enabling simulation of immune surveillance processes that are crucial for predicting immunosuppressive effects or cytokine storms [19]. Recent advancements include:
- Lymph Node-on-Chip: Pfizer has developed a platform capable of predicting antigen-specific immune responses, representing a significant advancement for preclinical immunotoxicity testing [6].
- Integrated Skin-Liver Models: Systems combining human liver and skin cocultures have been used to investigate dose-dependent toxicity of compounds like troglitazone over extended periods (6 days post-incubation) [53].
- Four-Organ MOC: Platforms integrating sequentially connected intestine, liver, skin, and kidney components demonstrate stable homeostasis and enable investigation of systemic toxicity for drug candidates [53].
The following experimental workflow illustrates how MOC systems can be applied to investigate nickel sensitization:
Recent technological innovations are enhancing MOC capabilities for immunotoxicity testing. The AVA Emulation System introduced in 2025 enables high-throughput Organ-Chip experiments with 96 independent samples in a single run, significantly expanding experimental power while reducing operating costs [6]. Similarly, the Chip-R1 Rigid Chip addresses drug absorption issues associated with traditional PDMS materials through minimally drug-absorbing plastics, particularly valuable for ADME and toxicology applications [6].
Experimental Protocols for MOC Validation
Protocol 1: MOC-Based Skin Sensitization Assessment
This protocol outlines the procedure for evaluating nickel sensitization using a multi-organ-chip system incorporating skin and immune components:
MOC Configuration: Utilize a multi-organ-chip platform with interconnected microchambers containing:
- 3D reconstructed human epidermis (e.g., EpiDerm, EpiSkin)
- Human fibroblast-embedded collagen matrix representing the dermis
- Microfluidic channel with dendritic cells and T-cells in circulation medium
Exposure Regimen:
- Prepare nickel sulfate solutions in relevant vehicles at concentrations ranging from 0.1-10 mM
- Apply 20 μL topically to the epidermal component or introduce systemically via microfluidic circulation
- Maintain flow rate of 50-100 μL/hour to simulate physiological conditions
- Include positive control (e.g., DNCB) and negative control (PBS) in parallel chips
Endpoint Analysis:
- KE1 Assessment: Analyze haptenization via LC-MS/MS detection of nickel-histidine complexes in epidermal lysates
- KE2 Assessment: Measure IL-18 and IL-1α release in effluent media using ELISA
- KE3 Assessment: Track dendritic cell migration and CD86/CD54 expression via immunofluorescence
- KE4 Assessment: Quantify T-cell proliferation using CFSE dilution assay and TCR sequencing
Data Interpretation:
- Compare response thresholds to historical LLNA data
- Establish benchmark doses for potency classification
- Evaluate cross-predictivity with existing in chemico and in vitro methods
Protocol 2: Integrated Testing Strategy for Validation
A comprehensive validation approach combining MOC with traditional alternative methods:
Tier 1 Screening:
- Perform DPRA assay to confirm nickel reactivity with cysteine and lysine peptides
- Conduct h-CLAT assay to assess dendritic cell activation potential
Tier 2 MOC Investigation:
- Employ skin-lymph node MOC to model systemic immune response
- Monitor real-time lymphocyte recruitment using embedded sensors
- Analyze tissue sections for Langerhans cell migration and T-cell priming
Omics Integration:
- Conduct transcriptomic analysis of epidermal and immune cells
- Perform proteomic profiling of secreted inflammatory mediators
- Integrate data using adverse outcome pathway framework
Cross-Species Correlation:
- Compare MOC results with existing human patch test data
- Evaluate concordance with historical animal study results
- Establish quantitative in vitro to in vivo extrapolation (QIVIVE) models
Research Reagent Solutions
The following table details essential materials and reagents for conducting MOC-based immunotoxicity studies:
Table 3: Essential Research Reagents for MOC Immunotoxicity Studies
| Reagent Category | Specific Examples | Research Application | Supplier Considerations |
|---|---|---|---|
| Primary Cells | Human keratinocytes, Langerhans cells, donor-matched T-cells | Recapitulating human immune response | Source from reputable providers with ethical consent procedures |
| Specialized Media | Defined keratinocyte serum-free media, dendritic cell differentiation kits | Maintaining cell-specific phenotypes | Optimize for microfluidic environment with reduced serum requirements |
| Chip Materials | PDMS, Chip-R1 Rigid Chips (minimally absorbing) | Microfluidic platform fabrication | Select based on drug absorption characteristics and optical properties |
| Detection Antibodies | Anti-CD86, anti-CD54, anti-HLA-DR, cytokine-specific ELISA kits | Quantifying cell activation and inflammatory responses | Validate for use in microfluidic effluent samples |
| Molecular Probes | CFSE cell proliferation dye, calcium flux indicators, viability stains | Real-time monitoring of cellular responses | Confirm compatibility with chip imaging systems |
| Reference Compounds | Nickel sulfate, DNCB, resveratrol, SDS | System qualification and benchmark doses | Source high-purity materials with certificate of analysis |
Discussion and Future Perspectives
The integration of MOC technology into systemic immunotoxicity assessment represents a paradigm shift in safety science. For nickel sensitization, MOC platforms offer the unique capability to model the complex crosstalk between skin and immune cells that is crucial for a complete understanding of sensitization [48]. This addresses a critical gap in current testing strategies, where individual alternative methods capture isolated key events but fail to recapitulate integrated immune responses.
Validation studies demonstrate that MOC systems provide enhanced physiological relevance through preservation of tissue microstructure, application of physiological shear stress, and establishment of tissue-tissue interfaces [53] [6]. The incorporation of patient-derived cells further enables investigation of individual susceptibility factors that influence chemical sensitivity, moving beyond population-level hazard identification to personalized risk assessment [54].
The convergence of MOC with advanced analytical technologies is creating powerful new opportunities in immunotoxicity testing. Artificial intelligence and machine learning algorithms can integrate the complex, multi-modal data generated by MOC platforms (including imaging, cytokine profiling, and transcriptomics) to identify novel biomarkers and build predictive models of immune response [6] [52]. Additionally, 3D bioprinting techniques enable precise spatial control over tissue architecture, allowing creation of more physiologically realistic skin and lymphoid structures [53].
Despite these advancements, challenges remain in fully replicating the systemic complexity of human immunity, particularly the integration of neuroendocrine interactions and the full repertoire of circulating immune cells [19] [52]. Future development efforts should focus on standardizing MOC platforms, improving scalability for high-throughput screening, and establishing rigorous validation frameworks based on human clinical data rather than animal test results.
As regulatory agencies increasingly accept human-relevant data, MOC technology is poised to transform safety assessment paradigms—shifting from traditional animal models to integrated testing strategies that combine in silico predictions, in chemico reactivity assays, and in vitro MOC data to more accurately protect human health against systemic immunotoxicants like nickel.
Target validation is a critical, early step in the drug development pipeline, ensuring that a molecular target is genuinely involved in a disease process and is amenable to therapeutic intervention. For decades, this process has relied heavily on animal models, which often fail to predict human therapeutic responses due to fundamental species-specific differences in physiology and genetics [9]. This translation gap is particularly pronounced in immunology and oncology, where the human immune system's complexity is difficult to replicate in animals [38].
The field is now undergoing a paradigm shift with the adoption of patient-derived cell models (PDCMs). These models, which include both simple 2D cultures and complex 3D systems like organoids and organs-on-chips, leverage cells obtained directly from patients to create more physiologically relevant human in vitro platforms [55] [56]. Using patient-derived cells for target validation incorporates the individual's unique genetic background, disease-specific mutations, and tumor microenvironment (TME) directly into the discovery process. This approach is particularly powerful for personalized medicine, as it allows for the functional testing of potential therapeutic targets on a patient's own cells before a treatment is ever administered [55] [57]. This review will objectively compare the performance of various patient-derived cell models in recapitulating human biology for target validation, with a specific focus on their integration into multi-organ-on-chip systems that incorporate human immunity.
Comparative Analysis of Patient-Derived Cell Platforms
Different patient-derived cell models offer varying advantages and limitations. The table below provides a structured comparison of their key characteristics, performance metrics, and suitability for target validation.
Table 1: Performance Comparison of Patient-Derived Cell Models for Target Validation
| Model Type | Key Characteristics | Throughput & Scalability | Physiological Recapitulation | Primary Applications in Target Validation | Key Limitations |
|---|---|---|---|---|---|
| 2D Primary Cell Cultures [55] [56] | Cells cultured flat on plates; Patient-derived nasal/bronchial/rectal cells. | High; Amenable to high-throughput screening. | Low; Lacks tissue structure, cell-cell/cell-matrix interactions, and physiological gradients. | Initial drug screening; Functional assays (e.g., Western blot, qPCR); Theratyping of rare mutations [55]. | Rapid dedifferentiation; Loss of native tissue polarity and function. |
| Organoids [55] [58] | 3D self-organizing structures from stem/progenitor cells in a matrix (e.g., Matrigel). | Medium; Self-assembly can lead to variability, limiting scalability and reproducibility. | Medium-High; Exhibits histology, some architecture, and cellular diversity of the source tissue. | Disease modeling (e.g., Cystic Fibrosis [55]); Personalized cancer therapy response profiling [56]. | Often lack vascularization and integrated immune cells; Batch-to-batch variability in matrix. |
| Organ-on-a-Chip (OoC) [9] [58] | Microfluidic devices with living cells under dynamic fluid flow and mechanical cues. | Low-Medium; Increasing with new platforms (e.g., 96-chip systems [6]). | High; Recapitulates tissue-tissue interfaces, vascular perfusion, mechanical forces (e.g., shear stress, breathing motions). | Studying complex human pathophysiology; ADME and toxicology studies; Modeling host-microbiome and immune interactions [9] [6]. | High complexity and cost; Requires specialized equipment and expertise; Small molecule absorption in some materials (e.g., PDMS). |
| Multi-organ-chip Systems with Immunity [59] [60] | Fluidically coupled OoCs, often with an integrated immune component (e.g., PBMCs, macrophages). | Low (current systems); A major focus of ongoing development and automation [6] [60]. | Very High; Models systemic inter-organ communication, immune cell trafficking, and whole-body responses to drugs or pathogens. | Most relevant for thesis context: Validating targets in a systemic, immunocompetent context; Predicting on-target/off-tissue toxicity; Studying immune-mediated mechanisms [59] [60]. | Highly complex; Challenging to maintain system stability; Data interpretation requires sophisticated computational modeling. |
The choice of model is dictated by the specific research question. While 2D cultures offer simplicity and throughput for initial screens, and organoids excel at capturing patient-specific histology, OoCs provide superior organ-level functionality. The most advanced systems for studying immunity are the emerging multi-organ platforms, which aim to replicate whole-body physiology [59].
Experimental Protocols for Key Applications
Protocol 1: Theratyping of Rare CFTR Mutations using Patient-Derived Nasal Epithelial Cultures
Objective: To characterize the molecular defect of a rare Cystic Fibrosis (CF) mutation and test its functional response to CFTR modulator therapies (correctors/potentiators) in vitro [55].
Methodology:
- Cell Sourcing: Obtain human nasal epithelial (HNE) cells via a non-invasive brushing procedure of the inferior turbinate.
- Cell Culture and Differentiation: Expand cells using conditional reprogrammed culture (CRC) techniques. Seed cells onto porous membrane supports and culture at an air-liquid interface (ALI) for 20-30 days to form a differentiated, pseudostratified epithelium [55].
- Therapeutic Intervention: Treat the ALI cultures with CFTR modulators (e.g., correctors: VX-445, VX-661; potentiator: VX-770) for a predetermined period (e.g., 24-48 hours).
- Functional Assessment (Ussing Chamber): Mount the epithelial layer in an Ussing chamber to measure transepithelial short-circuit current, a direct electrophysiological readout of CFTR-mediated ion transport. Forskolin (to activate CFTR) and CFTR-specific inhibitors are used to confirm the response is CFTR-dependent [55].
- Alternative Functional Assay (Spheroid Swelling): Culture patient-derived cells in Matrigel to form 3D spheroids. Activate CFTR with modulators and agonists; functional CFTR will transport ions and fluid into the spheroid lumen, causing measurable swelling [55].
Protocol 2: Validating Cancer Immunotherapy Targets in a Tumor-on-a-Chip
Objective: To investigate the mechanisms of immune-cancer interactions and validate the efficacy of T-cell recruiting bispecific antibodies or immune checkpoint inhibitors in a perfused, humanized tumor microenvironment [38].
Methodology:
- Device Fabrication: Use a microfluidic device (e.g., from AIM Biotech or custom-made from PDMS) featuring a central gel channel flanked by two media channels [38].
- TME Reconstitution: Embed patient-derived cancer cells (as a single-cell suspension or pre-formed spheroids) in a hydrogel (e.g., collagen or Matrigel) within the central channel. This constitutes the tumor compartment.
- Immune Cell Introduction: Perfuse autologous or donor-matched human peripheral blood mononuclear cells (PBMCs) containing T cells through one of the side channels, mimicking vascular delivery.
- Therapeutic Intervention: Introduce the therapeutic agent (e.g., an anti-PD-1 immune checkpoint inhibitor or a CD3xTAA bispecific antibody) into the perfusion medium.
- Multi-Parameter Readout:
- Imaging: Use time-lapse microscopy to quantify immune cell infiltration into the tumor compartment and real-time cytotoxicity.
- Effluent Analysis: Collect perfusate to measure secreted cytokines (e.g., IL-2, IFN-γ) via ELISA.
- Endpoint Analysis: Immunofluorescence staining of the chip for cell markers (e.g., CD3, CD8, Granzyme B) and viability assays [38].
Signaling Pathways in Patient-Specific Immune Evasion
The following diagram illustrates key signaling pathways that can be studied and validated using patient-derived cancer cells in immunocompetent models. These pathways are central to how tumors evade the immune system.
Key pathways validated in patient-derived models include the PD-1/PD-L1 axis, where inflammatory signals like IFN-γ and oncogenic pathways drive PD-L1 expression on tumor cells, leading to T-cell inhibition [61]. The TGF-β pathway suppresses effector immune cells while promoting regulatory T cells (Tregs) [61]. Furthermore, tumor metabolism, such as lactate production, creates an acidic TME that directly impairs T-cell and dendritic cell function and promotes immunosuppressive macrophage polarization [61]. These mechanisms are prime targets for immunotherapies, and their function can be directly tested in patient-specific contexts using the models described.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the aforementioned protocols relies on a suite of specialized reagents and tools. The following table details key solutions for establishing these advanced models.
Table 2: Essential Research Reagent Solutions for Patient-Derived Cell Models
| Research Reagent / Solution | Function & Application | Example Use Case |
|---|---|---|
| Matrigel / ECM Hydrogels | Provides a 3D, biologically active scaffold that mimics the native extracellular matrix to support organoid and spheroid formation and growth. | Used for culturing patient-derived rectal organoids for CFTR function assays [55] and embedding tumor cells in tumor-on-a-chip models [38]. |
| Air-Liquid Interface (ALI) Media | Specialized media formulations designed to promote the differentiation of primary airway epithelial cells into a functional, pseudostratified epithelium with cilia and mucus production. | Crucial for creating differentiated human nasal and bronchial epithelial cultures from patient cells for Ussing chamber experiments [55]. |
| Microfluidic Chips (PDMS, PMMA) | The physical device that houses the cell culture. PDMS is gas-permeable and optically clear, while plastics like PMMA reduce small molecule absorption. | PDMS chips are standard for custom organ-on-a-chip models. Newer rigid chips (e.g., Chip-R1) are designed for more predictable drug absorption in ADME studies [6] [38] [58]. |
| Cytokine & Growth Factor Cocktails | Defined mixtures of signaling proteins (e.g., EGF, Noggin, R-spondin) that guide stem cell fate, differentiation, and maintenance in 3D organoid cultures. | Essential for the long-term expansion and maintenance of patient-derived organoids, ensuring they retain key characteristics of the original tissue [58]. |
| PK/PD Modeling Software | Computational tools for Pharmacokinetic/Pharmacodynamic modeling. Used to translate in vitro dose-response data into predictions of human in vivo outcomes. | Used to create "digital twins" from multi-organ-chip data, predicting clinical efficacy and toxicity, as demonstrated in a malaria-on-a-chip model [59]. |
The evidence clearly demonstrates that patient-derived cell models are no longer a niche technology but are central to the future of target validation. The progression from 2D cultures to 3D organoids and, most powerfully, to dynamic organ-on-a-chip and multi-organ systems represents a concerted effort to capture the complexity of human physiology and disease in vitro.
The critical frontier, and the core of the stated thesis on "validation multi-organ-on-chip systems recapitulating human immunity," is the robust and standardized integration of a functional immune system. Government initiatives like the ImmuneChip+ program are actively addressing this challenge by funding the development of MPS with fully integrated immune components to model infectious disease and injury [60]. Furthermore, the convergence of biological data from these systems with computational PK/PD modeling is creating a path toward "digital twins" of human patients, enabling unprecedented prediction of drug responses before clinical trials begin [59].
For researchers and drug development professionals, the implication is that target validation must now be considered in a human-specific and system-wide context. The future of personalized medicine lies not only in sequencing a patient's genome but also in functionally testing potential therapies on their cells within a reconstructed, immunocompetent human microenvironment. This approach promises to de-risk drug development, maximize therapeutic efficacy, and usher in a new era of truly personalized and effective patient care.
Multi-organ-on-a-chip (MOC) systems, also known as microphysiological systems (MPS), represent a groundbreaking innovation in preclinical research, designed to overcome the significant limitations of traditional two-dimensional (2D) in vitro models and animal testing [30]. By replicating key in vivo tissue environments—including blood flow, three-dimensional (3D) architecture, cell-cell interactions, and concentration gradients—these platforms provide a more accurate representation of human biological responses [30] [62]. This is particularly vital for studying complex processes like pharmacokinetics (ADME), organ toxicity, and human immunity, where species-specific differences often limit the predictive value of animal models [30] [47]. This guide objectively compares three advanced MOC assays—BBB-Liver, Bone Marrow, and a comprehensive Intestine-Liver-Kidney-Neuro system—evaluating their performance based on experimental data, design, and their application in validating models of human physiology.
Comparative Analysis of Featured Multi-Organ-on-a-Chip Assays
The following table provides a detailed, data-driven comparison of the three core MOC assays, summarizing their configurations, key applications, and validated readouts.
Table 1: Performance and Application Comparison of Featured Multi-Organ-Chip Assays
| Assay Name | Organ Configuration & Cell Types | Primary Applications & Uses | Key Available Readouts & Experimental Data |
|---|---|---|---|
| BBB-Liver MOC [30] | 2-Organ Chip• Brain: iPSC-derived brain microvascular endothelial-like cells, neural spheroids.• Liver: Primary liver spheroid hepatocytes. | • Study of BBB permeability & neurotoxicity.• Assessment of metabolite neurotoxicity.• Organ toxicity screening. | • TEER measurement for barrier integrity.• Brain/Circulation ratio for permeation.• Metabolite identification (e.g., glucose/lactate).• Validation: Permeation behavior of atenolol and propranolol aligned with known in vivo BBB properties [30]. |
| Bone Marrow MOC [30] | 2-Organ Chip• Bone Marrow: Human mesenchymal stromal cells (hMSC), human bone marrow CD34+ cells on a 3D hydroxyapatite scaffold. | • Bone marrow toxicity.• Dose-range finding studies.• Refining treatment/dose scheduling. | • Flow Cytometry for full lineage cell output tracking.• Cytokine, glucose, or LDH analysis.• Mature lineage-specific cell output, overcoming progenitor-only limits of 2D models [30]. |
| Intestine-Liver-Kidney-Neuro MOC [30] | 4-Organ Chip• Intestine: Primary small intestine barrier.• Liver: Primary liver mu-tissue spheroids.• Kidney: iPSC-derived glomerular cells & proximal tubules.• Neuro: iPSC-derived neuro glial spheroids. | • ADME profiling & PBPK modeling.• First-pass metabolism.• Primary & secondary organ toxicity. | • Compound and metabolite kinetic (ADME) profile.• Validation: Reliably assessed behavior of approved drugs (e.g., Haloperidol, Carbamazepine) [30]. |
Experimental Protocols and Methodologies
To ensure reproducibility and provide a clear framework for researchers, this section outlines the detailed experimental protocols for each featured assay.
BBB-Liver Assay Protocol
This protocol is designed to study blood-brain barrier permeability and metabolite-mediated neurotoxicity.
Step 1: Chip Priming and Seeding
- Utilize a commercial microfluidic chip (e.g., TissUse's Humimic Chip 2 or 4) [30].
- Prime the liver compartment with a collagen-based extracellular matrix (ECM) and seed with primary human liver spheroid hepatocytes (e.g., 3D InSight) [30].
- In the brain compartment, seed a pre-formed neural spheroid and then introduce iPSC-derived brain microvascular endothelial-like cells into the adjacent vascular channel to form the BBB [30].
Step 2: System Integration and Culture
- Connect the compartments via the microfluidic circulatory system.
- Initiate a physiologically relevant fluid flow to introduce shear stress on the endothelial cells, which is critical for BBB integrity [30].
- Culture the system for several days to allow for tissue maturation and stable barrier formation.
Step 3: Compound Exposure and Sampling
- Introduce the test compound into the circulatory medium (vascular inlet) at the desired concentration.
- Circulate the medium for a set period (e.g., 24-72 hours) to simulate systemic exposure.
- Collect effluent samples from the vascular and brain compartments at multiple time points for analysis.
Step 4: Endpoint Analysis
- Barrier Integrity: Perform daily Transendothelial Electrical Resistance (TEER) measurements non-invasively [30].
- Permeability: Quantify the test compound and its metabolites in the brain compartment effluent using LC-MS/MS to calculate the brain/circulation ratio [30].
- Viability and Function: Fix tissues for immunostaining (e.g., for tight junction proteins) or analyze for metabolite levels (glucose/lactate), gene expression (qPCR), or liver-specific function markers [30].
Bone Marrow Toxicity Assay Protocol
This protocol enables the assessment of hematological toxicity by recapitulating the human bone marrow niche.
Step 1: Scaffold Preparation and Stromal Cell Seeding
- Place a 3D ceramic scaffold (hydroxyapatite) into the tissue chamber of the chip to mimic the bone's inorganic matrix [30].
- Seed the scaffold with human Mesenchymal Stromal Cells (hMSCs) and culture them to allow for attachment and ECM deposition, creating a supportive stromal niche.
Step 2: Hematopoietic Stem Cell Introduction
- Isolate human CD34+ hematopoietic stem cells from donor tissue.
- Introduce the CD34+ cells into the MSC-seeded scaffold within the microfluidic chip [30].
Step 3: Perfusion Culture and Differentiation
- Circulate a specialized hematopoiesis medium through the system via integrated microfluidic pumps.
- Maintain the culture for 2-4 weeks, allowing for the differentiation of CD34+ cells into various mature leukocyte lineages within the 3D niche [30].
Step 4: Toxicity Testing and Analysis
- After the maturation period, introduce the test compound (e.g., a chemotherapeutic agent) into the circulatory medium.
- Continue perfusion culture for a defined toxicity period (e.g., 7-14 days).
- Endpoint Analysis: Collect cells from the effluent and within the scaffold for analysis by flow cytometry to track and quantify the output of specific, mature blood cell lineages (e.g., granulocytes, lymphocytes, monocytes) [30]. This allows for direct measurement of compound-induced suppression of lineage-specific differentiation.
Intestine-Liver-Kidney-Neuro ADME Profiling Protocol
This protocol provides a comprehensive system for predicting human drug ADME and multi-organ toxicity.
Step 1: Multi-Tissue Integration
- On a multi-organ chip (e.g., TissUse's 4-organ platform), seed individual compartments with relevant tissues:
Step 2: System Circulation and Baseline Monitoring
- Connect all organ compartments via a common circulatory medium, often referred to as a "blood surrogate" [30] [62].
- Initiate perfusion to allow for organ crosstalk through circulating secreted factors and metabolites.
- Monitor baseline levels of key biomarkers and metabolites in the circulatory medium.
Step 3: Drug Administration and Kinetic Sampling
- Introduce the drug candidate into the system, typically via the intestinal compartment for oral administration studies or directly into the circulation.
- Continuously circulate the medium to simulate systemic distribution.
- Collect serial samples from the common circulatory medium over a prolonged period (e.g., 168 hours) to track the parent compound and the formation and clearance of metabolites [30].
Step 4: Multi-Endpoint Analysis
- ADME Kinetics: Use techniques like LC-MS to generate a full kinetic profile of the drug and its metabolites, enabling the calculation of absorption rates, metabolic half-lives, and clearance values [30].
- Toxicity Assessment: Analyze the tissues post-study for organ-specific toxicities via gene expression (qPCR), immunofluorescence, or functional assays (e.g., albumin production for liver, barrier integrity for intestine) [30].
- Validation: Compare the generated in vitro ADME parameters and toxicity findings to known clinical data for validated drugs like Haloperidol and Carbamazepine [30].
Visualizing System Workflows and Interactions
The following diagrams illustrate the core structures and functional relationships within the featured multi-organ-chip assays.
BBB-Liver Chip Experimental Workflow
Intestine-Liver-Kidney-Neuro ADME Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of MOC assays relies on specialized reagents and platforms. The table below lists key solutions used in the featured experiments and the broader field.
Table 2: Key Research Reagent Solutions for Multi-Organ-Chip Research
| Reagent / Material | Function & Application in MOC Assays | Examples in Featured Assays |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Differentiate into various human cell types (e.g., endothelial, neural, kidney), enabling patient-specific and human-relevant models [30] [63]. | • iPSC-derived brain microvascular endothelial-like cells (BBB-Liver) [30].• iPSC-derived glomerular cells and neuro spheroids (4-organ chip) [30]. |
| Primary Human Cells | Provide a highly physiologically relevant cell source, directly isolated from human tissue, preserving native functionality [62]. | • Primary liver spheroid hepatocytes (BBB-Liver, 4-organ) [30].• Primary small intestine cells (4-organ) [30].• Human bone marrow CD34+ cells (Bone Marrow) [30]. |
| 3D Scaffolds & Hydrogels | Provide a three-dimensional extracellular matrix (ECM) to support complex tissue architecture and cell-ECM interactions [30] [64]. | • Hydroxyapatite ceramic scaffold for bone marrow niche (Bone Marrow) [30].• Collagen I or other ECM hydrogels for general tissue support [65]. |
| Specialized Microfluidic Platforms | The physical chips and controllers that enable precise fluid handling, perfusion, and interconnection of organ compartments [30] [65]. | • TissUse's Humimic Chip 2 and 4 [30].• Emulate's AVA Emulation System & Chip-R1 [6].• MIMETAS OrganoPlate [65]. |
| Defined Co-culture Media | A common nutrient medium formulated to support the viability and function of multiple, distinct cell types simultaneously within a single circulatory system [64]. | Used in all featured assays to sustain intestine, liver, kidney, and neural cells in one circulating stream [30] [64]. |
The BBB-Liver, Bone Marrow, and Intestine-Liver-Kidney-Neuro assays exemplify the significant progress in MOC technology, moving from simple cellular models to integrated systems capable of recapitulating complex human physiology. Quantitative data from these systems, such as the accurate prediction of BBB permeation and drug ADME profiles, demonstrate their superior clinical translatability compared to traditional models [30]. As the field advances, the integration of these platforms with emerging technologies like high-throughput automation [6] [65] and digital twin computational models [59] is poised to further transform preclinical drug development. This convergence will ultimately enhance the predictive power of research, reduce the reliance on animal testing, and accelerate the delivery of safer, more effective therapies to patients.
Overcoming Technical Hurdles: Ensuring System Reliability and Scalability
Addressing Scalability and Standardization for High-Throughput Screening
The integration of microphysiological systems (MPS), particularly multi-organ-on-chip (OOC) platforms, into high-throughput screening (HTS) paradigms represents a transformative frontier in drug discovery and immunology research. This guide objectively compares the performance of emerging OOC technologies against traditional screening methods, focusing on their capacity to recapitulate human immunity. The global HTS market, a cornerstone of modern drug discovery, is projected to grow from USD 26.12 billion in 2025 to USD 53.21 billion by 2032, exhibiting a compound annual growth rate (CAGR) of 10.7% [66]. This growth is increasingly fueled by the adoption of more physiologically relevant, human-based models. However, the path to routine use of MPS in HTS is paved with two interconnected challenges: achieving the scalability necessary for screening vast compound libraries and establishing the standardization required for reproducible, reliable data. This guide dissects these challenges, provides a comparative analysis of current solutions, and outlines detailed experimental protocols for validating these sophisticated systems within a framework of human immunology.
Table 1: Global High-Throughput Screening Market Overview
| Metric | Value (2025-2032) | Source |
|---|---|---|
| 2025 Market Size | USD 26.12 Billion | [66] |
| 2032 Market Size | USD 53.21 Billion | [66] |
| CAGR | 10.7% | [66] |
| Leading Technology Segment (2025) | Cell-Based Assays (33.4% share) | [66] |
| Leading Application (2025) | Drug Discovery (45.6% share) | [66] |
| Fastest Growing Region | Asia Pacific (24.5% share in 2025) | [66] |
The Scalability Challenge: From Macro to Micro-Physiological Screening
Scalability in HTS traditionally refers to the ability to process thousands to millions of chemical compounds rapidly. Translating this to MPS requires miniaturizing complex human biology without sacrificing physiological relevance.
Throughput and Capability Comparison of Screening Platforms
The table below provides a performance comparison of traditional and emerging screening platforms, highlighting the trade-offs between throughput and physiological relevance.
Table 2: Performance Comparison of Screening Platforms for Immunological Research
| Platform | Max Throughput (Compounds/Week) | Key Strengths | Key Limitations in Immunology | Relative Cost per Data Point |
|---|---|---|---|---|
| Traditional 2D Cell Culture | > 100,000 | High throughput, cost-effective, simple data readouts | Low physiological relevance; lacks tissue-level structure and immune crosstalk [67]. | Low |
| Animal Models (e.g., Mice) | 10 - 100 | Whole-organism systemic biology; complex immune responses [47]. | Significant species-specific differences in immune pathways; poor human translation [52] [47]. | Very High |
| Single Organ-on-a-Chip | 1,000 - 10,000 | Human-relevant tissue structure; incorporates mechanical forces (e.g., shear stress) [4]. | Limited to single-organ immune responses; misses systemic effects [4]. | Medium-High |
| Multi-Organ-on-a-Chip | 100 - 1,000 | Models organ-organ crosstalk and systemic immune effects; predicts PK/PD [4]. | Lowest throughput; high complexity and cost; nascent standardization [6] [4]. | High |
Technological Advances Driving MPS Scalability
Recent innovations are specifically aimed at closing the throughput gap between traditional HTS and complex MPS:
- Automated and Integrated Platforms: The 2025 launch of the AVA Emulation System marks a significant leap, integrating microfluidic control, automated imaging, and an incubator for 96 independent Organ-Chip experiments in a single run. This design reduces hands-on lab time by more than 50% and cuts consumable costs four-fold compared to previous-generation systems [6].
- Miniaturization and Consumable Design: The shift from polydimethylsiloxane (PDMS)—a material known for absorbing small molecules and distorting pharmacokinetic data—to inert materials like cyclic olefin copolymer (COC) is critical for reliable screening. The Chip-R1 Rigid Chip and plates with larger sampling volumes (e.g., up to 1 mL per chip) enable more accurate kinetic measurements and are compatible with automated liquid handlers [6] [4].
- AI-Powered Data Analytics: A typical 7-day experiment on a platform like the AVA system can generate over 30,000 data points. Artificial Intelligence (AI) and machine learning are now essential for analyzing these massive datasets to identify patterns of immune response, predict toxicity, and optimize assay design, thereby improving the efficiency and predictive power of HTS campaigns [66] [52].
Standardization: The Key to Reproducible Human Immunology Data
Standardization is the foundation upon which the scientific validity of MPS-based HTS rests. Without it, data cannot be reliably reproduced or compared across laboratories.
Framework for Standardizing Multi-Organ MPS
A robust standardization framework should address the following critical pillars, derived from expert recommendations and industry practices [4]:
- Cell Sourcing and Characterization: Use primary human cells or donor-matched cells wherever possible. For immune-specific models, this includes accurately replicating innate (e.g., NK cells, ILCs) and adaptive (B cells, T cells) populations [67]. The ratio of parenchymal to non-parenchymal cells (e.g., Kupffer cells in liver models) must be consistent and documented.
- Experimental Protocol and Controls: Implement strict positive and negative controls for each assay. For instance, in a Lymph Node-on-a-Chip designed to predict immune response, a known immunogen should be included as a positive control, while a non-immunogenic compound serves as a negative control [6].
- Data Reporting and Analysis: Adopt standardized metrics for data analysis. This includes using the Z-factor for assessing assay quality and robustness in HTS, and clearly reporting key pharmacokinetic (PK) parameters like AUC (Area Under the Curve) and Cmax (Maximum Concentration) in multi-organ studies [4] [68].
Experimental Protocol: Validating a Multi-Organ MPS for Innate Immune Response
This protocol outlines the methodology for validating a Gut-Liver-Lymph Node MPS to screen for compound-induced inflammatory responses, a common cause of drug attrition.
Objective: To assess the ability of a multi-organ MPS to recapitulate a human-like innate immune response to a toll-like receptor (TLR) agonist and an experimental drug candidate. Hypothesis: The MPS will exhibit a dose-dependent inflammatory cytokine release upon exposure to a TLR agonist (positive control), which can be modulated by a anti-inflammatory drug candidate, mimicking a human in vivo response.
Materials and Equipment (The Scientist's Toolkit)
Table 3: Essential Research Reagent Solutions for MPS Immune Validation
| Item | Function | Example |
|---|---|---|
| PhysioMimix Multi-Chip System | Provides the hardware platform for housing and perfusing the multi-organ circuit. | CN Bio PhysioMimix [4] |
| Gut-Liver-Lymph Node Chip Consumable | The microfluidic device containing compartments and channels for co-culturing the three tissue types. | Chip A1 Accessible Chip or equivalent [6] |
| Cryopreserved Primary Human Cells | Source of biologically relevant human tissue. Includes hepatocytes, intestinal epithelial cells, and peripheral blood mononuclear cells (PBMCs). | Commercially available from tissue banks |
| TLR4 Agonist (Lipopolysaccharide, LPS) | Positive control stimulus to trigger a robust, predictable innate immune response. | Ultrapure LPS from E. coli |
| Cell Culture Media & Supplements | Provides nutrients and specific factors to maintain tissue viability and differentiated function over the experiment's duration. | Specific serum-free media formulations |
| Multiplex Cytokine ELISA Kit | To quantitatively measure a panel of key inflammatory cytokines (e.g., IL-1β, IL-6, IL-8, TNF-α) from the circulating effluent. | ProcartaPlex or similar |
| Liquid Handling Robot | For automated, precise dosing of compounds and sampling of effluent to ensure reproducibility and minimize human error. | Beckman Coulter BioMek NGeniuS or Tecan Fluent [66] [69] |
Step-by-Step Methodology
- System Assembly and Priming: Load the Gut-Liver-Lymph Node Chip into the PhysioMimix system under sterile conditions. Prime the entire microfluidic circuit with pre-warmed, oxygenated culture media and allow the system to stabilize for 24 hours.
- Cell Seeding and Tissue Maturation: Seed primary human cells into their respective compartments following the manufacturer's optimized protocol: hepatocytes in the liver chamber, intestinal epithelial cells in the gut chamber, and PBMCs in the lymph node chamber. Perfuse the system for 7-10 days to allow for tissue formation and maturation, as indicated by established biomarkers (e.g., albumin production for liver, transepithelial electrical resistance (TEER) for gut).
- Compound Dosing and Sampling:
- Day 0 (Baseline): Collect effluent samples from the common medium reservoir for baseline cytokine measurement.
- Day 1 (Induction): Introduce the TLR4 agonist (LPS) at a range of concentrations (e.g., 0.1, 1, 10 ng/mL) into the gut chamber lumen to simulate a localized immune trigger. Continue perfusion.
- Day 2 (Intervention): Add the experimental anti-inflammatory drug candidate at its proposed therapeutic concentration to the circulating medium.
- Daily Monitoring: Collect effluent samples daily for 5-7 days for cytokine analysis. Monitor tissue viability daily using automated imaging or released biomarkers like LDH.
- Endpoint Analysis: At the end of the experiment, disassemble the chip and fix the tissues for subsequent histology and immunostaining to assess tissue morphology and immune cell infiltration.
Data Analysis and Validation
- Kinetic Cytokine Profile: Plot the concentration of each cytokine (from the multiplex ELISA) over time for each experimental condition. A validated system will show a clear, dose-dependent spike in pro-inflammatory cytokines post-LPS exposure, which is subsequently dampened by the anti-inflammatory drug.
- Comparative PK/PD Modeling: Calculate the pharmacokinetic parameters of the drug candidate from its concentration in the medium over time. Correlate this with the pharmacodynamic (PD) response (cytokine reduction) to build a PK/PD model.
- Benchmarking Against Clinical Data: The magnitude and timing of the cytokine storm and its suppression should be qualitatively and quantitatively compared to known clinical responses from human studies or historical data to assess the predictive value of the MPS.
Visualizing the Experimental Workflow and Immune Signaling
The following diagrams, generated using DOT language, illustrate the core experimental workflow and the key innate immune signaling pathway under investigation.
MPS Immune Validation Workflow
Innate Immune TLR4 Signaling Pathway
The integration of multi-organ-on-chip systems into high-throughput screening is no longer a speculative future but an active and necessary evolution in drug discovery. While challenges in scalability and standardization remain significant, the technological trajectory is clear. Advances in automated platforms like the AVA Emulation System, coupled with AI-driven data analysis and a concerted push toward standardized materials and protocols, are rapidly closing the gap. The experimental validation framework provided here serves as a template for researchers to rigorously assess these systems, particularly for their ability to model complex human immune responses. The successful adoption of MPS in HTS will ultimately hinge on a collaborative effort across academia, industry, and regulators to validate these models against human data, moving us toward a more predictive, efficient, and human-relevant paradigm for developing new therapeutics.
Maintaining Long-Term Immune Cell Viability and Function
The development of multi-organ-on-chip (multi-OOC) systems that accurately recapitulate human immune responses represents a transformative frontier in preclinical research. However, maintaining long-term immune cell viability and function remains a significant technical hurdle. The high attrition rate in drug development—with approximately 90% of candidates that pass animal studies failing in human trials—is largely attributable to species-specific differences in immune responses and drug metabolism that animal models cannot accurately predict [47]. Immunocompetent OOC platforms aim to bridge this translational gap by incorporating functional human immune cells into microphysiological systems, thereby providing a more human-relevant platform for evaluating drug safety, efficacy, and immunotoxicity.
Achieving physiological immune function in vitro requires recapitulating the dynamic multi-step process of immune cell recruitment and activation. This includes immune cell extravasation—the coordinated cascade of capture, rolling, arrest, crawling, and transmigration across endothelial barriers—followed by chemotactic migration through tissue interstitium toward sites of infection or inflammation [70]. Maintaining these complex functions over extended periods demands careful attention to cellular microenvironments, including appropriate mechanical stimuli, chemokine gradients, cell-cell interactions, and stromal support that collectively enable physiologically relevant immune responses impossible to achieve in conventional static cultures.
Comparative Analysis of Platform Strategies and Performance
Different technological approaches have emerged to address the challenge of maintaining immune competence in multi-OOC systems, each with distinct advantages and limitations. The table below summarizes the key characteristics of these platforms:
Table 1: Comparison of Platform Approaches for Immune Cell Maintenance
| Platform Type | Key Features | Immune Components | Reported Culture Duration | Primary Applications |
|---|---|---|---|---|
| Lymph Node-on-Chip (e.g., Pfizer platform) | Models antigen-specific immune responses; Includes lymphoid tissue organization | T cells, B cells, antigen-presenting cells | 1-2 weeks | Preclinical immunotoxicity testing; Vaccine response modeling |
| Organoid-on-Chip | Stem cell-derived 3D structures; Self-organized tissue architecture | Tissue-resident immune cells (macrophages, ILCs) | Several weeks to months | Disease modeling; Host-microbiome interactions; Personalized medicine |
| Perfused Human Organ Systems | Uses donated human organs; Maintains native tissue architecture | Full native immune populations in physiological distribution | Hours to days | Drug biodistribution; Toxicity assessment; Inflammation modeling |
| Multi-OOC with Circulating Immunity | Interconnected organ compartments with shared vascular circulation | Circulating immune cells (monocytes, neutrophils, lymphocytes) | 2-4 weeks | Systemic drug responses; ADME studies; Immunotoxicity |
The selection of an appropriate platform depends heavily on the specific research objectives. For systemic immune responses and drug pharmacokinetics, multi-OOC systems with circulating immunity provide the most comprehensive approach, allowing immune cells to traffic between organ compartments as they do in the human body [71] [10]. For modeling organ-specific immune functions or barrier immunity, specialized single-organ systems with tissue-resident immune populations may be more appropriate [10].
Experimental Protocols for Key Functional Assays
Protocol: Modeling Immune Cell Extravasation in OOC Platforms
The recruitment of circulating immune cells into tissues is fundamental to inflammatory responses. The following protocol outlines key steps for establishing this process in microfluidic systems:
Endothelial Barrier Formation: Seed human primary endothelial cells (e.g., HUVEC or organ-specific microvascular endothelial cells) into the vascular channel of a microfluidic device. Culture under continuous perfusion (typical shear stress: 0.5-4 dyn/cm²) for 3-7 days until a confluent, tight monolayer forms. Confirm barrier integrity through measurement of transendothelial electrical resistance (TEER > 20 Ω·cm²) or permeability to fluorescent dextran [70].
Inclusion of Extracellular Matrix: Fill the adjacent tissue compartment with a physiological hydrogel (e.g., collagen I, fibrin, or Matrigel at 3-5 mg/mL concentration) containing relevant stromal cells if needed. The hydrogel should incorporate proteoglycans for chemokine binding to establish stable gradients [70].
Immune Cell Introduction and Activation: Introduce fluorescently labeled immune cells (e.g., primary human neutrophils, monocytes, or T cells at 0.5-1×10⁶ cells/mL) into the vascular channel. Activate the endothelium by introducing inflammatory cytokines (e.g., TNF-α at 10-50 ng/mL, IL-1β at 5-20 ng/mL) or through direct pathogen exposure to upregulate adhesion molecules [70].
Real-Time Imaging and Quantification: Monitor immune cell interactions with the endothelium using time-lapse microscopy. Quantify rolling velocity, firm adhesion (cells remaining stationary >30 seconds), and transmigration (movement across the endothelial layer into the matrix). Typical assays run for 2-6 hours post-activation [70].
Protocol: Co-culture of Immune Cells with Organ-Specific Tissues
Maintaining functional immune populations within tissue microenvironments requires careful optimization:
Source Selection and HLA Matching: For adaptive immune components (T and B cells), use HLA-matched cells from the same donor or induced pluripotent stem cell (iPSC) line to prevent graft-versus-host-like responses. This is particularly critical for multi-OOC systems incorporating lymphoid components [10].
Integration Methods: Two primary approaches exist:
- Direct incorporation: Immune cells are added directly to the tissue compartment during initial culture (suitable for tissue-resident macrophages, dendritic cells).
- Vascular introduction: Immune cells are introduced via perfusion through vascular channels, allowing natural extravasation (more physiological for circulating immune populations) [10].
Cytokine Supplementation: Maintain appropriate cytokine mixtures to support immune cell survival and function without inducing exhaustion. Common supplements include IL-2 for T cells (1-10 ng/mL), IL-7 for lymphocyte homeostasis (5-20 ng/mL), and GM-CSF for myeloid cells (5-20 ng/mL) [10].
Functional Validation: Assess immune competence through:
Visualization of Key Immune Processes
The following diagram illustrates the core process of immune cell recruitment in organ-on-chip platforms, integrating the critical cellular and molecular components:
Diagram 1: Immune Cell Recruitment Cascade in OOC Models
This multi-step process highlights the critical biological components that must be maintained in immunocompetent OOC systems, from initial endothelial activation to final tissue migration. Successful recapitulation requires appropriate expression of adhesion molecules, establishment of chemokine gradients, and provision of suitable extracellular matrix for migration.
Essential Research Reagent Solutions
The table below summarizes key reagents and materials critical for maintaining immune cell viability and function in OOC systems:
Table 2: Essential Research Reagents for Immunocompetent OOC Models
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Primary Cells | Human PBMCs, CD4+ T cells, monocytes, neutrophils, HUVEC | Provide physiological immune responses; Patient-specific modeling | Require HLA-matching for adaptive immunity; Limited expansion capacity |
| iPSC-Derived Immune Cells | iPSC-derived macrophages, T cells, dendritic cells | Unlimited supply; Genetic engineering potential; HLA-matched banks | Functional maturity requires validation; Differentiation protocols complex |
| Specialized Media | Immune cell-specific basal media; Cytokine cocktails (IL-2, IL-7, GM-CSF) | Support viability and maintain functional phenotypes | Must be optimized for each immune cell type; Cost considerations |
| Hydrogel Matrices | Collagen I, fibrin, synthetic PEG-based hydrogels | Provide 3D migration environment; Bind chemokines | Composition affects immune cell migration; Batch variability in natural hydrogels |
| Microfluidic Materials | PDMS, cyclic olefin copolymer (COC), polystyrene | Device fabrication; Low compound absorption critical | PDMS absorbs small molecules; COC preferred for drug studies |
| Analysis Reagents | Live-cell tracking dyes, cytokine ELISA/MSD kits, viability stains | Enable functional assessment of immune responses | Multiplexing preferred for limited sample volumes |
Material selection significantly impacts experimental outcomes. For example, polydimethylsiloxane (PDMS), commonly used in academic chip fabrication, can absorb small molecule drugs and hydrophobic cytokines, potentially altering immune responses [4]. Alternative materials like cyclic olefin copolymer (COC) show reduced compound absorption, making them more suitable for drug studies [4]. Similarly, hydrogel composition directly influences immune cell migration, with natural matrices like collagen and fibrin providing inherent bioactive cues that support physiological migration, while synthetic hydrogels offer greater control and reproducibility [70].
Maintaining long-term immune cell viability and function in multi-OOC systems remains challenging but is increasingly achievable through optimized platform designs and culture conditions. The most successful approaches incorporate physiological shear stresses, HLA-matched cellular components, appropriate cytokine milieus, and validated functional assays to ensure immune competence throughout experimental timelines.
Future advancements will likely focus on improved iPSC-derived immune cell generation, standardized validation protocols, and increasing system complexity to better model human immune responses. As these technologies mature, immunocompetent multi-OOC platforms are poised to significantly enhance our understanding of human immunology and transform preclinical drug development by providing more predictive, human-relevant models that bridge the translational gap between animal studies and clinical trials.
Cytochrome P450 (CYP450) enzymes represent a cornerstone of pharmaceutical metabolism, responsible for the biotransformation of approximately 70-80% of all clinically used drugs. These hemeproteins facilitate Phase I metabolism through oxidation reactions, critically determining drug clearance, bioavailability, and potential toxicity. The expression and functional activity of CYP450 isoforms directly influence therapeutic outcomes, yet traditional preclinical models often fail to recapitulate human-specific metabolic profiles. Conventional two-dimensional (2D) hepatocyte cultures notoriously suffer from rapid dedifferentiation, manifesting as precipitous declines in CYP450 activity within 24-48 hours, severely compromising their utility for chronic toxicity studies and drug-drug interaction assessments [71] [62].
The emergence of microphysiological systems (MPS), particularly organ-on-chip (OoC) technologies, offers a transformative approach to overcoming these limitations. By recreating critical aspects of the native liver microenvironment—including three-dimensional (3D) architecture, physiological shear stress, and multi-cellular interactions—these advanced platforms promote enhanced tissue complexity and maintain stable, physiologically relevant CYP450 expression. Furthermore, the integration of these hepatic models into multi-organ systems enables the study of organ-organ interactions and metabolite-mediated toxicity, providing a more comprehensive assessment of a drug's fate and effects within the human body [71] [72] [62]. This guide compares current strategies for enhancing CYP450 function in OoC models, providing researchers with validated experimental protocols and analytical frameworks to advance predictive toxicology and drug development.
Comparative Analysis of Hepatic Organ-on-Chip Models
The replication of human hepatophysiology in vitro requires careful consideration of cellular composition, structural design, and microenvironmental conditioning. The table below summarizes the core configurations of advanced liver models and their relative impact on CYP450 expression and metabolic competence.
Table 1: Comparison of Hepatic Organ-on-Chip Models for CYP450 Expression
| Model Type | Key Cell Types | Architectural Features | CYP450 Enhancement Strategies | Reported Metabolic Strengths |
|---|---|---|---|---|
| Primary Human Hepatocyte Spheroid Chips [72] [62] | Primary human hepatocytes, Kupffer cells | 3D polystyrene scaffolds, collagen coating, perfusable channels | Co-culture with immune cells (Kupffers), physiological shear stress (0.3-0.6 dyne cm⁻²) | Maintained urea & albumin production for 2+ weeks; functional CYP3A4 and CYP2C9 activity |
| iPSC-Derived Hepatocyte Chips [10] [62] | iPSC-derived hepatocytes, stellate cells, endothelial cells | Self-assembled organoids in microfluidic chambers | Patient-specific autologous cells, complex differentiation protocols | Model personalized drug metabolism; potential for genetic disease modeling |
| Lobule-Mimetic Chips [62] | Hepatocytes, liver sinusoidal endothelial cells (LSECs) | Radial geometry mimicking liver lobules, vascularized channels | Zoned oxygen gradients (periportal vs. pericentral), high permeability for metabolite exchange | Recapitulation of zonated metabolism; enhanced transcriptional activity of CYP genes |
| Multi-Cellular Liver Chips [18] [62] | Hepatocytes, Kupffer cells, stellate cells, cholangiocytes | Layered tissue structures, bile canaliculi formation | Comprehensive cell-cell interactions; inclusion of stellate cells for ECM remodeling | Superior long-term (>4 weeks) metabolic stability; accurate prediction of drug-induced liver injury (DILI) |
Experimental Protocols for CYP450 Assessment in OoC Models
Validating the metabolic competence of a liver-on-chip model necessitates a multifaceted experimental approach. The following section details key methodologies for quantifying CYP450 expression and function, drawn from established OoC research.
Protocol 1: Quantitative PCR for CYP450 Isoform Expression
Objective: To measure the baseline transcriptional activity of major CYP450 genes (e.g., CYP3A4, CYP2D6, CYP2C9) in hepatocytes cultured under static (e.g., Transwell) versus dynamic (OoC) conditions [62].
- Cell Lysis and RNA Extraction: At predetermined time points (e.g., days 1, 7, 14, 21), lyse cells directly within the microfluidic chip or on the scaffold using a commercial lysis buffer (e.g., TRIzol Reagent). Recover the lysate and extract total RNA according to the manufacturer's protocol.
- cDNA Synthesis: Synthesize cDNA from 1 µg of purified RNA using a High-Capacity cDNA Reverse Transcription Kit.
- qPCR Amplification: Perform qPCR reactions in triplicate using TaqMan Gene Expression Assays specific for the CYP450 isoforms and housekeeping genes (e.g., GAPDH, β-actin). Use the following cycling conditions: 50°C for 2 min, 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min.
- Data Analysis: Calculate fold-change differences using the 2^(-ΔΔCt) method, normalizing CYP450 expression to housekeeping genes and relative to the static control model at day 1.
Protocol 2: Functional Metabolic Activity via Substrate Conversion
Objective: To quantify the functional activity of specific CYP450 enzymes using probe substrates and measure the formation of their metabolites [72] [62].
- Dosing: Introduce a cocktail of CYP450 isoform-specific probe substrates (e.g., Testosterone for CYP3A4, Bupropion for CYP2B6) into the systemic circulation mimic (vascular channel) of the liver-chip or multi-organ system. A typical final concentration is 5-10 µM in the common media.
- Sampling: Collect effluent media from the chip's outlet at regular intervals (e.g., 0, 1, 2, 4, 8, 24 hours) post-dosing.
- Sample Analysis: Quantify metabolite formation (e.g., 6β-Hydroxytestosterone for CYP3A4, Hydroxybupropion for CYP2B6) using sensitive analytical techniques such as Liquid Chromatography with tandem mass spectrometry (LC-MS/MS).
- Kinetic Calculation: Calculate metabolic clearance values (e.g., intrinsic clearance, CLint) from the substrate depletion or metabolite formation rates over time. Compare these values to known human hepatic clearance data to validate predictive capacity.
Protocol 3: Immunofluorescence Staining for Protein Localization
Objective: To visualize the 3D spatial expression and localization of CYP450 enzymes and confirm the formation of polarized tissue structures [18].
- Fixation and Permeabilization: Gently perfuse the chip with 4% paraformaldehyde for 20 min at room temperature, followed by 0.1% Triton X-100 for 10 min.
- Blocking and Staining: Block non-specific sites with 2% donkey serum for 1 hour. Incubate with primary antibodies (e.g., mouse anti-CYP3A4, rabbit anti-Albumin) overnight at 4°C.
- Visualization: After washing, incubate with fluorophore-conjugated secondary antibodies (e.g., Alexa Fluor 488 anti-mouse IgG, Alexa Fluor 546 anti-rabbit IgG) for 2 hours at room temperature. Use DAPI for nuclear counterstaining.
- Imaging: Image the stained tissues using confocal microscopy to generate Z-stacks, allowing for 3D reconstruction and analysis of protein expression patterns within the tissue architecture.
Visualization of a Multi-Organ Chip for Metabolism Studies
The following diagram illustrates the functional connectivity and key processes in a gut-liver multi-organ-chip, a common configuration for studying first-pass metabolism.
Diagram 1: Gut-Liver-Axis Multi-Organ Chip for ADME Studies.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successfully implementing the aforementioned protocols requires a suite of reliable reagents and materials. The table below catalogs essential solutions for developing and analyzing CYP450-competent liver-on-chip models.
Table 2: Key Research Reagent Solutions for CYP450 OoC Studies
| Reagent / Material | Supplier Examples | Critical Function | Application Notes |
|---|---|---|---|
| Primary Human Hepatocytes | Lonza, Thermo Fisher | Gold standard for human-relevant metabolism; express full complement of CYP450s | Limited lifespan; high donor variability; requires specialized plating media. |
| iPSC-Derived Hepatocytes | Fujifilm Cellular Dynamics, Stemcell Technologies | Patient-specific; enable genetic disease modeling; renewable source | Require rigorous quality control for functional maturity (CYP450 activity). |
| Hepatocyte Plating & Maintenance Media | Thermo Fisher, Lonza | Supports attachment, viability, and phenotypic maintenance of hepatocytes | Formulations often include hydrocortisone, insulin, and ascorbic acid. |
| CYP450 Probe Substrate Cocktails | Corning, BioIVT | Isoform-specific substrates for functional activity assessment (e.g., CYP3A4, 2C9, 2D6) | Allows for simultaneous evaluation of multiple enzyme activities. |
| LC-MS/MS Grade Solvents & Columns | Agilent, Waters, MilliporeSigma | Essential for sensitive and specific quantification of drugs and their metabolites | Requires dedicated instrumentation and expert operational knowledge. |
| CYP450 Isoform-Specific Antibodies | Abcam, Santa Cruz Biotechnology | Enables protein-level validation and spatial localization via immunofluorescence | Confirm specificity with appropriate positive and negative controls. |
| Microfluidic Chips (PDMS/PS) | Emulate, Mimetas, TissUse | Provides the physical scaffold and microfluidic environment for 3D culture | PDMS can absorb small molecules; polystyrene (PS) is non-sorptive. |
The strategic enhancement of tissue complexity in organ-on-chip models directly addresses a critical bottleneck in drug development: the reliable prediction of human drug metabolism and toxicity. By moving beyond simple 2D cultures to incorporate 3D cellular architecture, physiologically relevant mechanical forces, and multi-lineage co-cultures, these advanced MPS significantly improve the expression and sustained functionality of CYP450 enzymes. The experimental frameworks and comparative data provided herein offer researchers a validated roadmap for building and qualifying these sophisticated models. As the field progresses, the integration of patient-specific iPSC-derived cells and the standardized linking of multiple organ models will further solidify the role of OoC technology in creating more effective and safer medicines, ultimately reducing the high attrition rates in clinical trials [71] [35] [62].
This guide objectively compares the performance of cutting-edge experimental platforms that integrate advanced readouts for multi-organ-on-a-chip (multi-OoC) systems, providing supporting data and methodologies to inform their application in human immunology research.
Technology Platforms for Advanced Read-Outs
The table below compares three primary technology platforms that enable omics analysis and real-time monitoring in advanced in vitro systems.
| Technology Platform | Key Performance Metrics | Sample Volume / Throughput | Key Advantages | Primary Applications in OoC |
|---|---|---|---|---|
| Multi-omics Microsampling [73] | - Analyzes thousands of metabolites, lipids, cytokines, and proteins from a 10 µL sample [73]- Protein CV (Stability): Median 0.397 [73]- Lipid CV (Stability): Median 0.335 [73] | 10 µL per microsample; enables high-frequency sampling (minutes-scale) [73] | - Enables high-frequency molecular profiling outside clinics- Fixed-volume collection minimizes variability [73] | - Profiling dynamic responses to interventions (e.g., nutrients, drugs) [73]- Longitudinal monitoring of molecular fluctuations [73] |
| High-Throughput Single-Cell Multi-Omics [74] | - Measures >40 parameters per cell (Mass Cytometry) [74]- Multiplexing: Up to 100 samples in parallel (barcoding) [74] | High-throughput; thousands to millions of individual cells [74] | - No spectral overlap vs. fluorescence flow cytometry- Ideal for limited clinical samples (e.g., biopsies) [74] | - Deep immune phenotyping (e.g., T-cell/myeloid subsets) [74]- Biomarker discovery in clinical trials [74] |
| Automated Organ-on-Chip Systems [6] | - Throughput: 96 independent Organ-Chip samples in a single run [6]- Data Generation: >30,000 time-stamped data points in a typical 7-day experiment [6] | - 4-fold drop in consumable spend vs. previous systems [6]- 50% fewer cells and media per sample [6] | - Automated imaging and microfluidic control- Generates AI-ready, multi-modal datasets [6] | - High-throughput compound screening- Toxicological and ADME studies [6] |
Experimental Protocols for Integrated Read-Outs
Protocol for Multi-Omics Microsampling from Microphysiological Systems
This protocol enables the dense molecular profiling of effluent or cell lysates from OoC systems [73].
- Step 1: Sample Collection
- Collect 10 µL of effluent or cell lysate from the OoC outlet using a volumetric absorptive microsampling (VAMS) device (e.g., Mitra device). This ensures a fixed, precise volume is collected, critical for quantitative analysis [73].
- Step 2: Biphasic Extraction
- Process the microsample using a biphasic extraction with methyl tert-butyl ether (MTBE).
- Organic Phase: Contains hydrophobic metabolites and lipids.
- Aqueous Phase: Contains hydrophilic metabolites.
- Protein Pellet: Recovered after methanol precipitation for proteomics [73].
- Step 3: Multi-Omics Data Acquisition
- Metabolomics and Lipidomics: Analyze organic and aqueous phases using Liquid Chromatography-Mass Spectrometry (LC-MS).
- Proteomics: Digest the protein pellet and analyze using LC-MS/MS.
- Cytokines/Hormones: Perform multiplexed immunoassays (e.g., Luminex platform) on a separate, aqueous-extracted microsample [73].
- Step 4: Data Integration
- Process and annotate individual omics datasets.
- Use data-driven integration strategies (e.g., correlation networks, WGCNA, xMWAS) to identify cross-omics relationships and biomarkers [75].
Protocol for Spatial Multi-Omic Analysis of OoC Tissue Constructs
This protocol details how to retrieve spatially resolved molecular information from tissue constructs cultured within OoC devices [74].
- Step 1: On-Chip Fixation and Preparation
- At the experimental endpoint, perfuse the OoC channels with a fixation buffer (e.g., 4% Paraformaldehyde) to preserve tissue architecture.
- Carefully disassemble the chip to extract the membrane or 3D matrix containing the cultured tissue.
- Step 2: Tissue Sectioning and Staining
- Embed the extracted construct in Optimal Cutting Temperature (O.C.T.) compound and cryosection it into thin slices (5-10 µm).
- Stain tissue sections with metal-tagged antibodies (for Imaging Mass Cytometry) or oligonucleotide-barcoded antibodies (for genomic cytometry like CiteSeq).
- Step 3: Data Acquisition
- For Imaging Mass Cytometry (e.g., Hyperion system): Use a laser to ablate stained tissue spots and a mass spectrometer to detect metal isotopes. This generates a high-dimensional image where each pixel contains quantitative proteomic data [74].
- For Genomic Cytometry: Perform single-cell RNA sequencing on the stained cell suspension, simultaneously capturing transcriptomic and proteomic (surface protein) data from the same cell [74].
- Step 4: Data Analysis
- Use computational tools to segment cells based on protein markers and correlate spatial localization with transcriptomic and proteomic expression to identify cell-cell interactions and niche-specific functions.
Diagram 1: Experimental workflows for OoC multi-omics readouts.
Data Integration and Analysis Pathways
Integrating data from multiple omics layers is crucial for extracting systemic biological insights. The following diagram and table summarize a standard analytical pathway.
Diagram 2: Data analysis pathway for multi-omics integration.
| Integration Method | Description | Typical Use Case |
|---|---|---|
| Correlation Networks (xMWAS) [75] | Performs pairwise association analysis using PLS components and regression coefficients to build integrative network graphs. Communities of highly interconnected nodes are identified. | Uncovering interconnections between different omics layers (e.g., which metabolites correlate with which proteins). |
| Weighted Gene Correlation Network Analysis (WGCNA) [75] | Identifies clusters (modules) of highly correlated genes/proteins/metabolites. Modules can be linked to clinical traits or experimental conditions. | Identifying co-expressed molecular groups associated with a specific OoC perturbation (e.g., inflammatory response). |
| AI/Deep Learning (e.g., AlphaFold 3) [52] | Uses diffusion-based deep learning to model 3D structures of biomolecular complexes (proteins, DNA, RNA, ligands). Predicts molecular interactions. | In silico prediction of drug-target interactions or antibody-antigen binding for vaccines/immunotherapeutics. |
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Experiment | Key Considerations |
|---|---|---|
| Volumetric Absorptive Microsampling (VAMS) Device (e.g., Mitra) [73] | Collects a fixed volume (e.g., 10 µL) of blood or effluent from an OoC system for reproducible quantitative analysis. | Minimizes volume variation compared to traditional dried blood spots (DBS); critical for longitudinal studies [73]. |
| Metal-Tagged Antibodies [74] | Probes for mass cytometry (CyTOF) and imaging mass cytometry (Hyperion). Enable high-parameter protein detection without spectral overlap. | Requires conjugation of pure metal isotopes; availability of pre-conjugated antibodies against targets of interest may be limited [74]. |
| Oligonucleotide-Barcoded Antibodies (e.g., for CiteSeq) [74] | Allow simultaneous quantification of surface proteins and transcriptome in single-cell genomic cytometry workflows. | Enables direct correlation of phenotypic (protein) and functional (gene expression) state at single-cell resolution [74]. |
| Chip-R1 Rigid Chip (Non-PDMS) [6] | An OoC consumable constructed with minimally drug-absorbing plastics. | Reduces nonspecific binding of small molecule drugs, making it superior for ADME and toxicology applications [6]. |
| Chip-S1 Stretchable Chip (PDMS) [6] | An OoC consumable made of Polydimethylsiloxane (PDMS). | Gas-permeable and optically transparent, but can absorb hydrophobic molecules; suitable for models requiring mechanical strain (e.g., lung, gut) [76]. |
Navigating the Costs of In-House Setup vs. Outsourcing to Specialized CROs
The adoption of multi-organ-on-a-chip (OOC) systems represents a paradigm shift in biomedical research, particularly for studies aiming to recapitulate complex human immune responses. For research teams, a critical strategic decision lies in choosing between developing an in-house OOC platform or partnering with a specialized Contract Research Organization (CRO). This guide provides an objective, data-driven comparison of these two paths, focusing on the financial, operational, and scientific considerations specific to validating multi-organ systems that model human immunity.
The Strategic Imperative: OOCs in Immune Research
Traditional preclinical models, including animal studies, have a high failure rate when predicting human immune responses; over 90% of drugs that appear safe in animals fail in human trials, often due to immunological factors such as unmanageable toxicity or lack of efficacy [47]. OOC technology, which uses microfluidic devices lined with living human cells, addresses this translational gap by providing a more accurate, human-relevant platform [35]. The ability to fluidically link multiple organ chips creates a "Body-on-Chips" system that can reveal how drugs or immune triggers impact interconnected organ systems, making it indispensable for modern immunology and drug development projects [35].
Quantitative Comparison: In-House vs. Outsourced OOC Operations
The choice between in-house and outsourced models significantly impacts a project's budget, timeline, and resource allocation. The tables below summarize key quantitative and qualitative differences.
Table 1: Cost and Operational Comparison
| Criteria | In-House Setup | Specialized CRO Partnership |
|---|---|---|
| Initial Setup & Timeline | Can take 30-60 days for onboarding, tool acquisition, and protocol establishment [77]. | Rapid activation, often within 7-14 days, using pre-validated platforms [77]. |
| Annual Operational Cost | High; typically $80,000–$120,000 in salary plus investments in tools and infrastructure [77]. | Flexible monthly packages or project-based pricing; converts fixed costs to variable expenses [77]. |
| Expertise & Experience | Limited to the knowledge of 1-2 hired generalists and their prior context [77]. | Access to a dedicated team with experience from analyzing hundreds of models and projects [77]. |
| Tools & Technology | Requires significant capital investment in microfluidic equipment, imaging systems, and data analysis tools [77]. | Immediate access to already integrated and tested tools, including advanced automated platforms [6]. |
| Hands-on Time | High; requires extensive hands-on lab time for chip culture, maintenance, and data collection [6]. | Significantly reduced; automated systems can cut hands-on lab time by more than half [6]. |
Table 2: Strategic and Scientific Value Comparison
| Aspect | In-House Setup | Specialized CRO Partnership |
|---|---|---|
| Data & Reproducibility | Risk of inconsistency while establishing protocols; challenges in standardizing complex immune-cell interactions. | Higher reliability through proven, standardized workflows; CROs provide robust, reproducible data generation [6]. |
| Scope of Research | Best for focused, proprietary questions with a stable, long-term research scope. | Ideal for accessing diverse model systems (e.g., Lymph Node-Chips, Alveolus Lung-Chips) and patient-specific cells without internal development [6]. |
| Regulatory Compliance | The burden of validating the platform for regulatory submission falls entirely on the internal team. | CROs often have platforms already under regulatory review (e.g., Emulate's Liver-Chip in FDA's ISTAND program), de-risking the path to approval [78]. |
| Access to Innovation | Dependent on internal R&D capacity and budget for upgrading systems. | Direct access to next-generation platforms (e.g., high-throughput AVA Emulation Systems, AI-integrated data analysis) [6] [78]. |
Experimental Protocols and Validation Data
Case Study: Validating a Multi-Organ Immune Response
To illustrate the practical application, consider a study designed to validate a gut-liver-lymph node multi-organ system for evaluating inflammatory responses to a new biologic.
- Objective: To recapitulate a human immune-mediated adverse event (skin rash and liver enzyme elevation) observed in a Phase I clinical trial, which was not predicted by animal studies.
- Experimental System: A fluidically linked co-culture system comprising a Lymph Node-Chip (e.g., from Emulate), a Gut-Chip, and a Liver-Chip [6].
- Key Endpoints: Measurement of pro-inflammatory cytokine release (e.g., IFN-γ, IL-6), T-cell activation in the Lymph Node-Chip, barrier integrity of the Gut-Chip, and markers of drug-induced liver injury (e.g., ALT release) in the Liver-Chip.
Detailed Workflow Methodology
The following diagram outlines the core experimental workflow for this multi-organ study.
Diagram 1: Multi-Organ Immune Response Workflow
- System Priming: The individual Organ-Chips (gut, liver, lymph node) are seeded with relevant primary or iPSC-derived cells. The Lymph Node-Chip is populated with donor-matched peripheral blood mononuclear cells (PBMCs). The system is perfused with a serum-free, common medium for 4-7 days to achieve tissue maturity and stability [6] [35].
- Immune Challenge: The test biologic is introduced into the Gut-Chip lumen or directly into the circulating perfusion medium. A positive control (e.g., lipopolysaccharide) and a negative control (vehicle) are run in parallel systems.
- Multi-Organ Culture: The chips are fluidically linked and maintained in an automated instrument (e.g., Emulate's Zoë-CM2 or AVA Emulation System) that controls perfusion flow and provides real-time, automated imaging for up to 14 days [6].
- Endpoint Analysis:
- Effluent Collection: Daily collection of perfusate for multiplex cytokine analysis via Luminex to track systemic immune activation.
- Metabolic Assay: Analysis of albumin and urea production in Liver-Chip effluent.
- Tissue Analysis: At the experiment terminus, chips are fixed and prepared for immunofluorescence staining (e.g., for CD3+ T-cells, ZO-1 tight junction protein, CYP450 enzymes) or RNA sequencing.
- Data Integration & AI Analysis: Multi-modal data (imaging, cytokine levels, metabolic markers, transcriptomics) are aggregated. AI/ML algorithms are employed to identify complex, non-linear signatures predictive of the human clinical adverse event [78].
Supporting Data and Outcomes
A CRO leveraging a standardized platform can generate robust datasets. For instance, a typical 7-day experiment on a high-throughput system can generate >30,000 time-stamped data points from daily imaging and effluent assays, with post-analysis omics pushing the total into the millions [6]. In a specific example, an Emulate Lymph Node-Chip developed in partnership with Pfizer demonstrated the capability to predict antigen-specific immune responses, a major leap for preclinical immunotoxicity testing [6]. Furthermore, Liver-Chip models have demonstrated up to 87% sensitivity and 100% specificity in predicting drug-induced liver injury in humans, a key metric for validation [78].
The Scientist's Toolkit: Essential Research Reagent Solutions
Success in OOC research, whether in-house or via a CRO, depends on access to high-quality biological and technical materials. The following table details key reagents and their critical functions in multi-organ immunity studies.
Table 3: Key Research Reagent Solutions for Multi-Organ OOC Studies
| Reagent / Material | Function & Importance in Immune Research |
|---|---|
| Primary Human Cells & iPSCs | The foundation of physiological relevance. Using donor-matched primary cells (hepatocytes, enterocytes, immune cells) or iPSC-derived lineages is critical for modeling patient-specific immune responses and genetic diversity [47]. |
| Specialized Extracellular Matrix (ECM) | Hydrogels (e.g., Collagen I, Matrigel) provide the 3D scaffold for cell growth and organization. The specific ECM composition influences immune cell migration and activation, which is crucial for modeling conditions like inflammation [6]. |
| Serum-Free, Chemically Defined Media | Supports the co-culture of multiple cell types without introducing unknown variables from fetal bovine serum. Essential for studying specific immune signaling pathways and cytokine production [6]. |
| Chip-Array Consumables | Microfluidic devices (e.g., Emulate's Chip S1, Chip-R1) are the physical platform. The Chip-R1 is constructed with minimally drug-absorbing plastics, making it well-suited for accurate immunotoxicity and ADME studies [6]. |
| Cytokine & Chemokine Panels | Multiplex immunoassays (e.g., Luminex) are used to quantitatively profile the secretome from the perfusate, providing a dynamic readout of immune and inflammatory status across the multi-organ system. |
| Cell-Specific Antibodies for IF | Validated antibody panels for immunofluorescence (IF) are used for endpoint analysis to identify and localize specific immune cell populations (e.g., T-cells, macrophages) within the tissue context on the chip. |
Visualizing a Key Immune Signaling Pathway
A common finding in multi-organ immune studies is the role of the gut-liver-axis in systemic inflammation. The following diagram illustrates a key signaling pathway that could be modeled in an OOC system, where a gut toxin triggers a systemic immune response.
Diagram 2: Gut-Liver-Lymph Node Immune Signaling Pathway
The decision to build in-house OOC capacity or to partner with a specialized CRO is not one-size-fits-all and hinges on a project's specific goals, constraints, and strategic vision.
- Choose an In-House Setup if your institution has a long-term, dedicated commitment to OOC technology development, possesses the necessary capital and expertise for sustained investment, and requires full control over proprietary models for core research programs.
- Partner with a Specialized CRO when the priorities are speed, cost-efficiency, and de-risking validation. This path is superior for accelerating specific projects, accessing validated and regulatory-endorsed platforms, leveraging deep expertise in complex immunology models, and incorporating the latest technological innovations like AI-driven data analysis without direct capital investment [6] [78] [77].
For the vast majority of research and drug development professionals aiming to validate multi-organ-on-chip systems for human immunity research reliably and efficiently, the data indicates that a strategic partnership with a specialized CRO offers a more robust, economically viable, and scientifically advanced pathway.
Benchmarking Success: Validation Frameworks and Comparative Analysis with Traditional Models
Correlating MOC Data with Clinical Outcomes for Predictive Validation
In the evolving field of multi-organ-on-chip (Multi-OoC) systems research, demonstrating predictive validity against human clinical outcomes is the cornerstone of translational relevance. This process involves correlating in vitro MOC data with in vivo patient outcomes to establish a reliable benchmark for system performance. Current approaches in clinical prediction often address complications individually, limiting integrated risk assessment, a challenge that mirrors the difficulties in validating interconnected multi-organ systems in vitro [79]. The emergence of multitask learning algorithms presents a promising solution to these challenges by leveraging relationships among related tasks, potentially leading to more robust and generalizable models [79]. This approach is particularly advantageous in the medical domain where different outcomes often share common risk factors and physiological pathways, much like the shared physiological pathways recapitulated in multi-OoC systems. This guide objectively compares the performance of a novel, scalable tree-based multitask learning model against traditional single-outcome models, providing a framework for validating the predictive power of complex biological systems.
Model Performance: Comparative Analysis of Predictive Accuracy
Performance Metrics and Experimental Outcomes
The tree-based Multitask Gradient Boosting Machine (MT-GBM) was developed to simultaneously predict three major postoperative complications—acute kidney injury (AKI), postoperative respiratory failure (PRF), and in-hospital mortality—using only 16 preoperative features generally available in Electronic Health Records [79]. Its performance was rigorously evaluated against single-outcome models through external validation across multiple clinical centers.
Table 1: Performance Comparison (AUROC) Across Derivation and Validation Cohorts
| Outcome | Derivation Cohort | Validation Cohort A | Validation Cohort B |
|---|---|---|---|
| Acute Kidney Injury (AKI) | 0.805 | 0.789 | 0.863 |
| Postoperative Respiratory Failure (PRF) | 0.886 | 0.925 | 0.911 |
| In-Hospital Mortality | 0.907 | 0.913 | 0.849 |
All reported AUROCs were statistically significant (p < 0.001), except for AKI in the derivation cohort and PRF in Cohort B [79]. The model demonstrated remarkable generalizability across different healthcare settings, maintaining strong performance in Validation Cohort A (13,285 cases from a secondary-level general hospital) and Validation Cohort B (2,813 cases from a tertiary-level academic referral hospital), despite significant differences in patient characteristics and surgical case mix [79].
Comparative Advantage Over Single-Outcome Models
The MT-GBM model demonstrated several key advantages over traditional single-outcome approaches:
- Integrated Risk Assessment: By capturing interdependencies among different complications, the model provides a comprehensive risk profile, enabling clinicians to prepare for various scenarios and optimize resource allocation [79].
- Computational Efficiency: The model utilizes a minimal set of 16 preoperative variables, enhancing feasibility for widespread clinical adoption across diverse healthcare settings [79].
- Interpretability: Unlike many deep learning approaches, the tree-based architecture allows researchers to elucidate the contribution of each input variable to predictions among different outcomes [79].
Table 2: Feature Analysis Across Predicted Complications
| Preoperative Feature | AKI Contribution | PRF Contribution | Mortality Contribution |
|---|---|---|---|
| ASA Class ≥3 | High | High | High |
| Emergency Surgery | Medium | High | High |
| Age | Medium | Medium | High |
| Serum Creatinine | High | Low | Medium |
| Albumin | Medium | High | High |
| Blood Urea Nitrogen | High | Medium | Medium |
Experimental Protocols: Methodologies for Predictive Validation
Cohort Selection and Data Collection
The experimental protocol for validating the MT-GBM model provides a template for designing validation studies for multi-OoC systems:
Data Source and Eligibility Criteria:
- A total of 72,686 non-cardiac surgery cases met eligibility criteria for inclusion in the derivation cohort [79].
- After applying exclusion criteria, 66,152 cases were used for final analysis [79].
- External validation cohorts were assembled from independent medical centers with different patient demographics and surgical profiles [79].
- The model was designed using a minimal set of 16 preoperative variables readily available in EHR systems, including demographics, ASA physical status, surgery type, and basic laboratory values [79].
Validation Strategy:
- Temporal validation: Data collected from different time periods (January 2018 to August 2023 for Validation Cohort A) [79].
- Geographic validation: Data sourced from different hospital systems with varying patient populations [79].
- Care level validation: Inclusion of both secondary-level general hospitals and tertiary-level academic referral centers [79].
Model Architecture and Training Protocol
Multitask Learning Framework: The MT-GBM algorithm leverages shared representations across related prediction tasks. Unlike single-outcome models that treat each complication in isolation, the multitask approach identifies common risk pathways and feature interactions that manifest across different complications [79].
Implementation Details:
- Architecture: Tree-based gradient boosting machine optimized for multiple related tasks [79].
- Training data: 66,152 cases with complete preoperative profiles and documented postoperative outcomes [79].
- Validation approach: Internal validation followed by external validation on completely independent datasets [79].
- Interpretability features: Implementation of feature importance analysis to elucidate variable contributions across different outcomes [79].
Key Research Reagent Solutions for Validation Studies
Table 3: Essential Research Materials for Predictive Validation Studies
| Reagent/Resource | Function/Purpose | Specification Notes |
|---|---|---|
| Electronic Health Record System | Source of clinical features and outcome data | Minimum 16 preoperative variables; structured data format |
| Multitask Gradient Boosting Machine | Core algorithm for simultaneous outcome prediction | Tree-based architecture; supports shared task representations |
| Data Anonymization Tool | Patient privacy protection during model development | HIPAA-compliant de-identification methods |
| Statistical Analysis Platform | Performance metric calculation and significance testing | AUROC analysis; p-value calculation; confidence intervals |
| External Validation Cohorts | Independent performance assessment | Multi-center datasets with varying patient demographics |
| Feature Importance Analyzer | Model interpretability and biological pathway insight | Quantifies variable contribution across different outcomes |
Signaling Pathways and Biological Mechanisms in Multi-Outcome Prediction
The predictive validation of clinical outcomes relies on understanding shared biological pathways that manifest across multiple complications. The MT-GBM model implicitly captures these relationships through its multitask learning framework.
Implications for Multi-Organ-on-Chip Validation Research
The methodologies and findings from clinical predictive modeling provide valuable insights for validating multi-organ-on-chip systems:
Recapitulating Clinical Correlation in Vitro: Just as the MT-GBM model identifies shared risk factors across complications, multi-OoC systems must replicate interconnected physiological responses. The model's ability to capture relationships between preoperative albumin levels and multiple outcomes (medium for AKI, high for PRF and mortality) suggests that nutritional status biomarkers should be incorporated into multi-OoC systems to better predict clinical relevance [79].
Validation Protocol Design: The successful external validation strategy employed for the clinical prediction model—using geographically and temporally distinct cohorts—provides a template for validating multi-OoC systems. Multi-OoC researchers should implement similar rigorous validation across different cell sources, operator techniques, and laboratory environments to establish generalizability [80].
Interpretability and Biological Plausibility: The emphasis on model interpretability in the MT-GBM approach aligns with the need for mechanistic understanding in multi-OoC systems. Rather than treating these systems as black boxes, researchers should implement similar feature importance analyses to understand which engineered parameters most significantly influence phenotypic outcomes [79].
The integration of multitask learning approaches with multi-OoC systems represents a promising frontier for predictive validation in drug development and personalized medicine. As these technologies converge, they offer the potential to create more robust, clinically relevant models that can accurately forecast human responses to therapeutics and disease interventions [80].
Demonstrating Superior Clinical Predictivity Compared to 2D Cultures and Animal Models
The failure of conventional preclinical models to accurately predict human clinical responses remains a significant bottleneck in drug development, costing the industry time and resources while delaying patient access to new therapies. For decades, research has relied heavily on two-dimensional (2D) cell cultures and animal models, yet these systems often poorly mirror human physiology, disease mechanisms, and treatment responses [9]. This is particularly problematic for studying complex human-specific immune responses, which are critical in areas ranging from infectious disease and vaccine development to cancer immunotherapy and autoimmune disorders. The genomic responses in mouse models, for instance, have been shown to poorly mimic human inflammatory diseases [9].
The emergence of microphysiological systems (MPS), particularly organ-on-a-chip (OoC) and multi-organ-on-a-chip (MOOC) technologies, represents a paradigm shift in preclinical modeling. By engineering miniature, functional units of human tissues and organs within dynamically controlled microenvironments, these systems bridge the critical gap between traditional in vitro models and human in vivo physiology [81] [9]. When these systems specifically incorporate immune components—creating immunocompetent organ-chips—they provide a powerful platform for recapitulating the complex interplay between human tissues and the immune system, offering a path toward unprecedented clinical predictivity [26] [82]. This guide objectively compares the performance of these advanced systems against 2D cultures and animal models, presenting experimental data that validates their superior ability to predict human clinical outcomes.
Comparative Analysis of Model Systems
The following tables provide a structured comparison of 2D cell cultures, animal models, and immunocompetent multi-organ-on-chip systems across key parameters relevant to drug development and disease modeling.
Table 1: Overall Model Characteristics and Capabilities
| Feature | 2D Cell Culture | Animal Models | Immunocompetent Multi-Organ-on-Chip |
|---|---|---|---|
| Physiological Relevance | Low; lacks 3D architecture, tissue-specific forces, and complex cell-cell interactions [81] | Moderate; has whole-body physiology but exhibits species-specific differences [83] [9] | High; recapitulates human 3D tissue structure, mechanical forces, and vascular perfusion [81] [84] [9] |
| Immune System Integration | Minimal; typically limited to single or few immune cell types in isolation [26] | Intact but non-human; immune responses differ from humans [83] | Engineered but human; can incorporate innate/adaptive immune cells and lymphoid tissues [83] [19] [26] |
| Predictivity for Human Response | Poor; fails to predict clinical efficacy and toxicity due to oversimplification [9] | Variable; poor translation of therapeutic responses for inflammation, cancer, and neurodegenerative diseases is common [9] | High; demonstrated accurate recapitulation of human clinical responses to drugs, toxins, and pathogens [83] [9] |
| Throughput & Cost | High throughput, low cost [6] | Low throughput, very high cost [19] | Medium-to-high throughput improving with automation (e.g., 96-chip platforms [6]), moderate cost |
| Human Genetic & Patient Specificity | Possible with patient-derived cells but in non-physiological context [83] | Not possible; requires genetic engineering to mimic human diseases | High; readily incorporates patient-derived stem cells, organoids, and tissue [81] [83] |
Table 2: Experimental Data from Comparative Studies
| Study Focus | 2D Culture Data | Animal Model Data | Organ-on-Chip Data | Clinical Correlation |
|---|---|---|---|---|
| Immune Response to Vaccination/Infection | Static snapshots; no tissue-level organization [81] | Differing immune cell recruitment and cytokine profiles compared to humans [9] | Real-time observation of immune cell migration and organization into specific "zones"; antigen-specific responses [85] [83] | Recapitulated human lymphoid tissue organization and antigen accumulation patterns [85] |
| Drug-Induced Toxicity | Often misses organ-level toxicity due to lack of metabolic function and tissue-tissue crosstalk | Can miss human-specific toxicities (e.g., liver toxicity from a compound safe in animals [9]) | Integrated gut-liver chips predicted species-specific drug toxicity (e.g., acetaminophen) via metabolic coupling [9] | Accurately mirrored human patient toxic responses not seen in animal testing [9] |
| Tumor-Immune Microenvironment | Cannot model immune cell infiltration into 3D tumors or suppressive stromal interactions | Human tumor xenografts require immunocompromised hosts, failing to model human immune-tumor interactions [19] | Modeled T-cell infiltration into tumors and efficacy of T-cell bispecific antibodies; revealed suppressed immune organization in cancer survivors [83] [9] | Reflected the weakened immune response and clinical susceptibility to infection in lymphoma patients [83] |
| Inflammatory Bowel Disease (IBD) | Cannot model complex host-microbiome-immune interactions under flow | Limited in isolating specific human host-microbiome interactions | Real-time observation of microbiome-immune crosstalk, barrier dysfunction, and response to therapies in Gut-Chip [81] [6] | Patient-specific models uncovered triggers of IBD and evaluated therapies [81] |
Key Experimental Protocols in Immunocompetent Organ-on-Chip Research
Protocol 1: Establishing a Gut-on-a-Chip with Integrated Immune and Microbial Components
This protocol is used to model complex human intestinal physiology, host-microbiome interactions, and inflammatory conditions like IBD [81].
- Step 1: Device Fabrication. Utilize a clear plastic microfluidic device roughly the size of a USB stick, containing hollow microchannels. The device can be fabricated via 3D printing using biocompatible resins (e.g., PEGDA) and coated with Parylene C for enhanced biocompatibility [85].
- Step 2: Cell Seeding and Differentiation. Seed human intestinal epithelial cells derived from patient biopsies or stem cells into the central channel of the device, often within an extracellular matrix (ECM) like Matrigel. Apply continuous perfusion of growth factors to promote the formation of 3D intestinal villi structures and a polarized epithelium that secretes mucus [81].
- Step 3: Introduction of Microbiome and Immune Cells. Introduce bacterial communities into the intestinal lumen channel, allowing them to colonize the mucus layer. In a separate, parallel vascular channel, perfuse human immune cells (e.g., peripheral blood mononuclear cells or specific immune cell subtypes) under continuous fluid flow [81].
- Step 4: Perturbation and Real-Time Analysis. Induce inflammation using chemical stimuli or pathogenic bacteria. Use time-lapse microscopy and effluent collection to monitor in real-time key parameters including immune cell migration towards the gut lumen, cytokine production, changes in barrier integrity (e.g., Trans-Epithelial Electrical Resistance), and microbial dynamics [81] [9].
Protocol 2: Modeling Human Vaccination Response in a Lymph Node-on-a-Chip
This protocol models the critical early events following vaccination, where antigen is transported from an injection site to a draining lymph node (LN) to initiate an immune response [85].
- Step 1: Fabrication of a Tubing-Free Multi-Compartment Chip. Employ a 3D-printed multi-compartment device designed with open-top wells for tissue culture, connected by microchannels to form a recirculating fluidic loop. A companion tubing-free magnetic impeller pump integrated into the device drives fluid flow, mimicking lymph circulation [85].
- Step 2: Integration of Lymph Node Tissue. Place a living slice of murine or human lymph node tissue into a 3D-printed mesh support, which is then inserted into one of the culture wells. This mesh suspends the tissue, allowing fluid to flow perpendicularly through it, simulating the physiological flow of lymph through a native LN [85].
- Step 3: Antigen "Vaccination" and Circulation. Inject a model vaccine (antigen with or without adjuvant) into an upstream compartment representing an injection site. The recirculating flow, driven by the impeller pump, carries the antigen to the LN tissue compartment.
- Step 4: Analysis of Immune Activation. After 24-48 hours, analyze the LN tissue and effluent. Techniques include immunofluorescence staining to locate antigen-accumulating cells and assess changes in LN architecture, flow cytometry to quantify activation markers on immune cells (e.g., CD69+ on T cells), and RNA sequencing to evaluate early gene expression changes indicative of an inflammatory response [85].
Protocol 3: Evaluating Patient-Specific Anti-Cancer Immunity in an Immune Organoid
This protocol uses synthetic hydrogels to create a human tonsil and lymph node organoid for evaluating the robustness of an individual's immune response, particularly in cancer patients [83].
- Step 1: Fabrication of Synthetic Hydrogel Microenvironment. Create a gel-like, porous 3D scaffold using synthetic hydrogels (e.g., poly(ethylene glycol)-based) functionalized with cell-adhesion peptides and immune signaling molecules (e.g., cytokines) to mimic the native lymphoid tissue microenvironment.
- Step 2: Isolation and Seeding of Immune Cells. Isolate primary human B cells and other immune cells from the blood or tonsil tissue of a healthy donor or a cancer patient. Seed these cells into the synthetic hydrogel matrix.
- Step 3: On-Chip Culture and Stimulation. Load the immune organoid into a perfused organ-on-chip system to ensure nutrient delivery and waste removal. Challenge the system with model antigens or patient-derived tumor antigens to stimulate an immune response.
- Step 4: Functional Readouts. Monitor the formation of organized germinal center-like "zones" where B cells mature and produce antibodies. Quantify antigen-specific antibody production via ELISA and track the differentiation and class-switching of B cells using flow cytometry. Compare the organizational integrity and antibody output of organoids from cancer survivors versus healthy donors [83].
Visualizing the Enhanced Predictivity of Organ-on-Chip Systems
The following diagram illustrates the core logical pathway through which immunocompetent multi-organ-on-chip systems achieve superior clinical predictivity by integrating critical physiological components missing in traditional models.
The Scientist's Toolkit: Key Research Reagent Solutions
Successfully developing and utilizing immunocompetent organ-on-chip models requires a suite of specialized reagents and materials. The table below details essential components for building these advanced systems.
Table 3: Essential Research Reagents for Immunocompetent Organ-on-Chip Models
| Reagent/Material | Function | Specific Examples & Notes |
|---|---|---|
| Microfluidic Chips | Provides the physical scaffold and microarchitecture for tissue culture and fluid flow. | Chip-S1/S2 (Emulate): Stretchable chips for lung and intestine models [6].Chip-R1 (Emulate): Rigid, low-drug-absorbing plastic for ADME/toxicology [6].Custom 3D-Printed Chips: User-designed platforms, e.g., for lymph node studies [85]. |
| Stem & Primary Cells | Source for generating patient-specific human tissues and immune cells. | Induced Pluripotent Stem Cells (iPSCs): Differentiate into any organ-specific cell type [82].Patient-Derived Organoids: From biopsies, used for personalized gut or tumor models [81] [86].Primary Immune Cells: Isolated from blood (e.g., PBMCs, T cells, B cells) or lymphoid tissues [83] [26]. |
| Advanced Biomaterials | Creates the 3D extracellular matrix (ECM) that supports cell growth and organization. | Synthetic Hydrogels (e.g., PEG-based): Defined, tunable composition; used for immune organoids [83].Matrigel: Basement membrane extract; common but has batch-to-batch variability [86].Fibrin/Collagen Gels: Natural ECM proteins used in many tissue models. |
| Specialized Media & Factors | Supports cell survival, differentiation, and maintains tissue-specific functions. | Cell-Type Specific Differentiation Media: Contains growth factors to guide stem cell fate [86].Cytokines & Chemokines: Critical for immune cell recruitment, activation, and organization (e.g., in lymph node models) [85] [19]. |
| Analysis Kits & Assays | Enables real-time, non-invasive monitoring of tissue health and function. | Transepithelial/Transendothelial Electrical Resistance (TEER) Equipment: For real-time barrier integrity measurement [9].Effluent Analysis Kits: For quantifying secreted cytokines, metabolites, and biomarkers from the chip's outflow [6].Live-Cell Fluorescent Dyes & Antibodies: For time-lapse imaging of cell behavior and endpoint analysis. |
The collective evidence from recent studies demonstrates a clear and compelling trend: immunocompetent multi-organ-on-chip systems consistently outperform traditional 2D cultures and animal models in their ability to predict human clinical responses. By faithfully recapitulating critical aspects of human physiology—including 3D tissue architecture, dynamic fluid flow, and most importantly, the integrated function of the human immune system—these microphysiological systems provide a more human-relevant and predictive platform for disease modeling, drug safety and efficacy testing, and personalized medicine. As the technology continues to advance through standardization, automation, and increased complexity, its adoption is poised to bridge the long-standing translational gap, accelerating the development of safer and more effective therapeutics.
The FDA Modernization Act 2.0, signed into law in December 2022, represents a fundamental shift in drug development regulatory policy [87]. This legislation removes the long-standing mandate, originating from the 1938 Food, Drug, and Cosmetic Act, that required animal testing for all drugs before human clinical trials [87] [88]. Instead, the Act explicitly authorizes the use of New Approach Methodologies (NAMs)—including microphysiological systems (MPS) such as organ-on-chip technology, cell-based assays, sophisticated computer models, and bioprinted tissues—to demonstrate drug safety and effectiveness [89] [87]. This regulatory transformation responds to a critical problem in pharmaceutical development: the persistent high failure rate of clinical trials, with approximately 90% of drugs failing during human trials due largely to lack of efficacy or safety concerns that animal models failed to predict [89] [87] [90].
This guide examines how multi-organ-on-chip systems, particularly those recapitulating human immunity, are positioned within this new framework. We provide objective performance comparisons and detailed experimental methodologies to assist researchers and drug development professionals in validating these systems for regulatory submissions and improved drug safety assessment.
The Scientific and Economic Rationale for Human-Relevant Models
Limitations of Traditional Animal Models
Traditional animal models, primarily rodents, have been the cornerstone of preclinical research for decades. However, significant species differences in pharmacogenomics, including variations in drug absorption, distribution, metabolism, and excretion (ADME), often compromise their predictive value for human responses [89]. Enzymes such as cytochrome P450 that are involved in drug metabolism vary in number and function between species, leading to differences in how drugs are broken down and cleared from the body [89]. The TGN1412 case exemplifies this disconnect: this monoclonal antibody caused a life-threatening cytokine release syndrome in human volunteers despite appearing safe in preclinical monkey studies [90].
Additionally, the limited genetic diversity of inbred animal strains fails to represent human population variability [89]. As few as 1 in 25 people are optimal responders to common medications, highlighting the translational gap between homogeneous animal models and genetically diverse human populations [89].
Economic Impact of Predictive Failure
The economic burden of relying on poorly predictive animal models is substantial. A typical monoclonal antibody program consumes approximately 144 non-human primates at a cost of up to $7 million in animal expenses alone, within a development cycle carrying a $650-750 million price tag [90]. The broader economic impact stems from late-stage clinical failures, costing an estimated $28 billion annually due to poor preclinical predictability [89]. Animal-based data have been particularly poor predictors of drug success for multiple common diseases including cancer, Alzheimer's, and inflammatory diseases [90].
Multi-Organ-on-Chip Systems: Technical Capabilities and Validation
Multi-organ-on-chip systems are bioengineered microfluidic devices that culture living human cells in functional tissue units that recapitulate organ-level functions and interactions. These systems typically incorporate primary human cells or induced pluripotent stem cell (iPSC)-derived tissues, microfluidic channels simulating vascular perfusion, and integrated sensors for functional monitoring [89] [87]. The table below compares leading commercial platforms and their documented capabilities:
Table 1: Comparison of Major Multi-Organ-on-Chip Platforms
| Platform/System | Key Technology Features | Validated Applications | Human Relevance Metrics | Throughput Capability |
|---|---|---|---|---|
| Emulate Liver-Chip [90] [88] | Microfluidic culture with primary human hepatocytes, Kupffer cells, and endothelial cells | Drug-induced liver injury (DILI) prediction; Metabolism studies | 87% sensitivity, 100% specificity for DILI prediction; Correctly identified 87% of hepatotoxic drugs that caused liver injury in patients [90] | Medium; Compatible with automated workflows |
| CN Bio PhysioMimix [87] | Suite of hardware, consumables, and assay protocols for single- and multi-organ studies | Liver models for NASH; Toxicity testing; ADME applications | Recreation of 3D organs with fluid perfusion; Enables organ crosstalk studies [87] | Medium-High; Designed for adoption into preclinical workflows |
| Qureator vTIME [91] | Vascularized tumor immune microenvironment model with AI integration; 3D tumor organoids with human vascular structures | Oncology efficacy testing; Immune checkpoint inhibitor evaluation | FDA IND approval based solely on human vascularized organoid efficacy data without animal proof-of-concept testing [91] | Enhanced predictability with AI integration |
| 4Dcell SmartHeart [90] | hiPSC-derived cardiomyocytes and cardiac fibroblasts in 3:1 physiological ratio | Cardiac safety assessment; Arrhythmia risk prediction | Ejection fractions reaching 30%; Contraction strains of 25% after 7 days in culture [90] | High; 96 tissues per plate in automated formats |
Validation Standards and Regulatory Acceptance
For multi-organ-on-chip systems to gain regulatory acceptance, they must demonstrate rigorous validation against known human outcomes. The FDA roadmap outlines specific validation requirements, including retrospective analyses comparing NAM predictions to known human outcomes, prospective validation trials, and standardization efforts ensuring reproducibility across laboratories [90]. A significant milestone was achieved when the Emulate Liver-Chip was accepted into the FDA's Innovative Science and Technology Approaches for New Drugs (ISTAND) pilot program after demonstrating superior performance in predicting drug-induced liver injury compared to traditional models [90] [88].
The first FDA IND approval utilizing solely human organoid efficacy data (without animal proof-of-concept testing) occurred in October 2025 for a combination therapy of BAL0891 with immune checkpoint inhibitors, based on data from Qureator's vascularized tumor immune microenvironment model [91]. This landmark decision validates the regulatory acceptance of human-based systems for efficacy determination.
Experimental Protocols for Multi-Organ-on-Chip Validation
Protocol 1: Immune-Competent Multi-Organ Toxicity Assessment
This protocol evaluates compound safety in a system recapitulating human immune responses across multiple organs, specifically designed to detect human-specific immunotoxicity missed in animal models.
Table 2: Research Reagent Solutions for Immune-Competent Multi-Organ Chips
| Reagent/Material | Specifications | Function in Experimental System |
|---|---|---|
| Primary Human iPSCs | Sourced from diverse donors; Minimum 2,000 lines recommended [89] | Provides genetically diverse cellular material for generating patient-specific tissue models |
| Lymphocyte Expansion Media | Contains IL-2, IL-7, IL-15 cytokines | Supports proliferation and maintenance of functional immune cells in the system |
| Organ-on-Chip Devices | PDMS-based microfluidic devices with isoporous membranes [89] | Creates physiological tissue-tissue interfaces and enables organ crosstalk |
| Cytokine Release Assay Kits | Multiplexed cytokine panels (IL-6, IL-1β, TNF-α, IFN-γ) | Quantifies immune activation and detects cytokine release syndrome risks |
| Metabolite Measurement Kits | LC-MS/MS compatible sample preparation | Monitors organ-specific metabolic functions and compound clearance |
| Cell Tracking Dyes | Membrane-labeling fluorophores (PKH26, CFSE) | Traces immune cell migration between organ compartments in real-time |
Methodology:
- System Assembly: Seed human iPSC-derived hepatocytes in liver chamber, primary human umbilical vein endothelial cells in vascular channel, and donor-matched immune cells in a dedicated lymphoid tissue compartment [89] [90].
- Perfusion Establishment: Connect organ compartments through microfluidic circulatory system at physiologically relevant flow rates (100-500 μL/min depending on scale).
- Baseline Monitoring: Measure baseline cytokine profiles, metabolic markers (albumin, urea), and barrier integrity (TEER) over 48-72 hours to ensure system stability.
- Compound Dosing: Introduce test compounds at clinically relevant concentrations through the vascular channel; include positive controls (e.g., TGN1412 analog for cytokine release) and vehicle controls.
- Endpoint Assessment: At 24h, 72h, and 7 days, collect effluent for cytokine quantification, image tissue viability via live/dead staining, and perform functional assays (e.g., hepatocyte albumin secretion, endothelial barrier integrity).
- Data Integration: Compare results to historical clinical data using computational models to predict human immunotoxicity risk.
Protocol 2: Vascularized Tumor-Immune Microenvironment (vTIME) for Efficacy Testing
This protocol, adapted from the first FDA-approved organoid-based efficacy study [91], evaluates oncotherapeutic efficacy using vascularized human tumor models with intact immune components.
Methodology:
- Patient-Derived Tissue Sourcing: Obtain tumor tissues from consented patients through surgical resection or biopsy; isolate and expand tumor organoids in defined matrices.
- Vascularization: Generate endothelial networks using primary human endothelial cells and fibroblasts in fibrin or collagen matrices; perfuse with microfluidics for 7-10 days to form mature vessels.
- Immune Component Integration: Introduce autologous peripheral blood mononuclear cells (PBMCs) or tumor-infiltrating lymphocytes (TILs) into the system.
- Treatment Application: Administer test compounds (monotherapies or combinations) through the vascular channel at physiologically achievable concentrations.
- Response Monitoring: Track tumor cell viability via ATP-based assays, immune cell-mediated killing through live imaging, and tumor penetration using fluorescently-labeled compounds.
- Validation Against Clinical Response: Compare preclinical results to clinical outcomes when available; for novel compounds, use benchmark comparisons to established standard-of-care agents.
Quantitative Performance Comparison of Alternative Methods
The transition to human-relevant systems requires clear understanding of their performance metrics compared to traditional approaches. The table below summarizes quantitative comparisons across key parameters:
Table 3: Performance Comparison of Preclinical Testing Modalities
| Parameter | In Vitro 2D Cell Culture | In Vitro 3D Spheroid | In Vivo Animal Models | Organ-on-a-Chip |
|---|---|---|---|---|
| Human Relevance | Low | Medium | Low (species differences) [89] [90] | Medium-High [87] [90] |
| Complex 3D Organs and Tissues | No | Limited complexity | Yes | Yes [87] |
| (Blood)/Flow Perfusion | No | No | Yes | Yes [87] |
| Innate & Adaptive Immune System | Limited | Limited | Yes (but species-specific) | Emerging capability [91] |
| Longevity | < 7 days | < 7 days | > 4 weeks | ~ 4 weeks [87] |
| Acute & Chronic Dosing | Acute only | Acute only | Both possible | Both possible [87] |
| New Modalities Assessment | LOW | MEDIUM | LOW | MEDIUM-HIGH [87] |
| Throughput | High | Medium-High | Low | Medium [87] |
| Time to Result | FAST | FAST | SLOW | FAST [87] |
| High Content Data | Medium | Medium-High | Low (imaging limitations) | High [87] [90] |
| Predictive Accuracy for Human Response | 40-50% | 50-60% | 60-70% [89] | 80-90% (validated systems) [90] [91] |
Implementation Roadmap and Future Directions
The FDA has outlined a clear implementation pathway for adopting NAMs in drug development. The agency will "encourage sponsors to submit NAM data in parallel with animal data to build a repository of experience" and will "offer regulatory relief (e.g., fewer animal study replicates) to those who do so" [90]. The document indicates the FDA will "identify a few pilot cases where, based on strong rationale, an animal study is waived in favor of a NAM" [90]. The ultimate vision is a comprehensive transformation where "no conventional animal testing will be required for mAb safety, and eventually all drugs/therapeutics" with a "comprehensive integrated NAM toolbox (human cell models + computational models)" becoming "the new standard" [90].
Future developments will focus on increasing system complexity through improved multi-organ integration, enhancing immune capabilities to better model human immunology, and advancing standardization to ensure reproducibility across laboratories and applications. The successful regulatory acceptance of organ-on-chip data for both safety and efficacy assessment signals that these human-relevant systems are poised to become central tools in preclinical drug development [88] [91].
The accurate prediction of organ-specific toxicity remains a significant challenge in drug development. Conventional models, including 2D cell cultures and animal studies, often fail to recapitulate human physiological responses, contributing to high drug attrition rates during clinical trials. This case study objectively compares two advanced approaches for validating organ-specific toxicity and metabolic profiles: multi-organ metabolomics in animal models and human organoids-on-chips (OrgOCs) technology. Framed within the broader thesis of validating multi-organ-on-chip systems that recapitulate human immunity, we analyze the capacity of these platforms to provide human-relevant, mechanistic insights into toxicological pathways, thereby supporting more reliable preclinical safety assessment.
Comparative Analysis of Experimental Platforms
To evaluate the efficacy of current models, we compare a traditional animal-based metabolomics approach with an emerging human-cell-based organ-on-chip technology. The following table summarizes their key characteristics.
Table 1: Platform Comparison for Organ-Specific Toxicity Assessment
| Feature | Multi-Organ Animal Metabolomics | Human Organoids-on-Chips (OrgOCs) |
|---|---|---|
| Fundamental Approach | In vivo assessment of metabolic disruptions in organs of laboratory animals [92] [93] | In vitro microphysiological system integrating 3D organoids with microfluidic chips [80] |
| Human Physiological Relevance | Limited by species divergence [80] | High; utilizes human stem cells and recapitulates tissue-specific properties [80] |
| Key Strengths | Provides systemic, whole-organism data; well-established protocols [92] | Recapitulates human-relevant ecological niches, mechanical cues, and tissue interactions [80] |
| Key Limitations | Inter-strain metabolic variability [93]; ethical concerns; poor clinical translatability | Technological complexity; requires multidisciplinary expertise [80] |
| Data Output | Quantitative metabolite profiles and pathway analysis from tissue samples [92] [93] | Real-time analysis of organ function, barrier integrity, and cytokine release [80] |
| Suitability for Immune Studies | Limited ability to model human immune responses | High potential for integrating human immune components [80] |
Platform 1: Multi-Organ Metabolomics in Animal Models
Detailed Experimental Protocol
The following workflow and protocol detail the methodology used in a recent study investigating the organ-specific toxicity of SN-38, the active metabolite of the anticancer drug irinotecan [92].
1. Animal Dosing and Sample Collection:
- Subjects: Male Kunming mice (6-week-old) were divided into two groups: an SN-38 treatment group (20 mg/kg/day, intraperitoneal) and a vehicle control group (5% DMSO in saline) for one week [92].
- Ethical Approval: The study was approved by the Ethics Committee of the Affiliated Hospital of Jining Medical University (Approval No.: JNMC-2022-DW-041) [92].
- Sample Collection: Two weeks post-dosing, mice were euthanized. Blood samples were collected for serum separation, and major organs (lungs, heart, stomach, spleen, liver, intestine, kidneys) were snap-frozen in liquid nitrogen within 30 seconds to quench metabolism [92].
2. Tissue Sample Preparation for GC-MS:
- Homogenization: 50 mg of each tissue was homogenized in methanol containing an internal standard (heptanoic acid) [92].
- Derivatization: The supernatant was incubated with O-methylhydroxylamine hydrochloride in pyridine (70°C for 90 min), followed by a second incubation with N,O-bis(trimethylsilyl)trifluoroacetamide with 1% trimethylchlorosilane (70°C for 60 min) to volatilize metabolites for GC-MS analysis [92].
- Quality Control: Quality control (QC) samples were prepared from a pool of all samples and injected every 10 runs to monitor instrumental stability [92].
3. GC-MS Metabolomic Analysis:
- Instrumentation: Analysis was performed using a 7890B gas chromatography system coupled with a 7000C mass spectrometer and an HP-5MS capillary column [92].
- Chromatography: Helium was used as the carrier gas. Samples were injected at a 50:1 split ratio [92].
4. Data Processing and Multivariate Analysis:
- Raw data from GC-MS underwent peak alignment, normalization, and compound identification using metabolite libraries.
- Principal Component Analysis (PCA) was applied to visualize natural clustering and outliers in the metabolic profiles of different organs and strains [93].
5. Pathway Enrichment Analysis:
- Significantly altered metabolites were mapped to biochemical pathways using the KEGG database. Enrichment analysis identified pathways most significantly disrupted by SN-38 exposure [92].
6. Histopathological Validation:
- Organs were fixed in 4% paraformaldehyde, embedded in paraffin, sectioned (4 μm thickness), and stained with Hematoxylin and Eosin (H&E). A slide scanner and analysis software were used to assess morphological changes [92].
Key Experimental Findings and Data
The application of this protocol generated quantitative, organ-specific data on SN-38-induced metabolic disruptions.
Table 2: SN-38-Induced Metabolic Disruptions Across Mouse Organs [92]
| Organ | Number of Differential Metabolites | Significantly Altered Pathways |
|---|---|---|
| Lungs | 24 | Purine metabolism, Amino acid metabolism, Glyceric acid metabolism |
| Heart | 15 | Purine metabolism, Pyrimidine metabolism, Antioxidant defenses |
| Stomach | 12 | Amino acid metabolism, Cellular homeostasis |
| Blood | 21 | Energy metabolism, Amino acid metabolism |
| Spleen | 35 | Purine and Pyrimidine metabolism, Amino acid metabolism |
| Intestine | 26 | Amino acid metabolism, Glyceric acid metabolism |
| Liver | 18 | Purine metabolism, Energy metabolism |
| Kidneys | 28 | Pyrimidine metabolism, Amino acid metabolism, Antioxidant defenses |
Furthermore, a foundational study highlighted significant inter-strain variability in baseline metabolomes, a critical consideration for experimental design [93]. The table below summarizes these differences.
Table 3: Inter-Strain Variability in Mouse Organ Metabolomes [93]
| Mouse Strain | Genetic Background | Key Metabolic Differences in Organs |
|---|---|---|
| C57BL/6 | Inbred | Considered a general baseline; distinct brain and liver metabolome [93] |
| BALB/c | Inbred | Metabolome of kidney and muscle greatly differs from C57BL/6 and CD1; larger cluster variance in PCA [93] |
| CD1 | Outbred | Mostly overlapping metabolome with C57BL/6 in kidney and muscle; greater heterogeneity [93] |
Platform 2: Human Organoids-on-Chips (OrgOCs)
OrgOCs represent the synergism of human organoids (HOs) derived from stem cells, which recapitulate multicellular tissue-specific properties, and microfluidic organs-on-chips (OOCs), which mimic the extrinsic physicochemical microenvironment of human organs [80].
Key Advantages for Toxicity Assessment
The OrgOC platform offers several distinct advantages for validating organ-specific toxicity and metabolic profiles:
- Recapitulation of Human Ecological Niches: OOCs can independently control dynamic fluids, mechanical cues (e.g., cyclic stretch for breathing lungs), 3D topography, and oxygen gradients. This allows for the mimicry of physiological shear stress and tissue-level interactions that are crucial for maintaining normal organ function and response to toxins [80].
- Systemic Interaction Modeling: Multi-organ-chips can interconnect various organ models via a microfluidic circulatory system. This is essential for studying the systemic distribution of drugs and their metabolites, capturing the complex inter-organ communication that underlies many toxicological responses [43].
- Enhanced Physiological Relevance: Compared to static cultures, perfusion in chips can induce more in vivo-like cellular responses. A meta-analysis found that while gains are biomarker-specific, perfusion improved the function of certain cell types, with CYP3A4 activity in CaCo2 cells and PXR mRNA levels in hepatocytes being induced more than two-fold under flow [15].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and technologies used in the featured experiments, providing a resource for researchers seeking to implement these approaches.
Table 4: Essential Research Reagents and Materials
| Item / Technology | Function / Application | Specific Examples / Notes |
|---|---|---|
| Solid Phase Microextraction (SPME) | Non-exhaustive, in vivo or in situ sampling of unbound metabolites from tissues; combines sampling, quenching, and extraction [93] | Used for direct insertion into mouse organs (brain, liver, etc.); enables detection of short-lived metabolites [93] |
| Gas Chromatography-Mass Spectrometry (GC-MS) | High-separation efficiency analysis of volatile metabolites; ideal for untargeted metabolomics [92] | HP-5MS capillary column; requires metabolite derivatization [92] |
| Liquid Chromatography-Mass Spectrometry (LC-MS/MS) | Targeted, high-sensitivity quantification of specific metabolite-nucleobase adducts [94] | Used to elucidate organ-specific genotoxic chemistry pathways [94] |
| Electrochemiluminescent (ECL) Array | High-throughput, cell-free screening of DNA damage induced by organ-specific metabolites [94] | 64-nanowell chip with DNA/enzyme films; correlates well with cell-based DNA damage assays [94] |
| Human Organ Microsomes & Cytosols | Enzyme sources for metabolic activation in cell-free systems; provide organ-specific metabolic profiles [94] | Used in ECL arrays and LC-MS/MS adduct formation to model liver, lung, kidney, and intestine metabolism [94] |
| Microfluidic Chip Fabrication | Creation of devices that house organ models and control fluid flow [80] | Techniques include photolithography, etching, and 3D bioprinting [80] |
This case study demonstrates that both multi-organ animal metabolomics and human OrgOCs provide powerful, complementary data for validating organ-specific toxicity. The animal model offers a whole-system perspective and generates robust quantitative metabolomic datasets, revealing that toxins like SN-38 disrupt distinct pathways—such as purine and amino acid metabolism—in different organs [92]. However, its clinical translatability is limited by species differences and inter-strain variability [93]. In contrast, the OrgOC platform excels in providing human-relevant, mechanistic insights by recreating tissue-specific properties and physiological cues, showing promise for more accurately predicting human immune and toxicological responses [80]. For the validation of multi-organ-on-chip systems in human immunity research, the quantitative pathway data from animal studies can serve as a valuable benchmark, while the human OrgOCs offer a more physiologically relevant platform for forward-translational research, ultimately strengthening the preclinical assessment pipeline.
Establishing Reproducibility and Inter-Experimental Robustness
The pursuit of human-relevant preclinical models has propelled the development of microphysiological systems (MPS), with multi-organ-on-chip (multi-OoC) platforms representing the cutting edge for investigating systemic human biology [9]. These microfluidic devices, which culture living human tissues under physiological fluid flow, can recapitulate organ-level functions and inter-organ crosstalk with remarkable fidelity [9] [95]. For the critical domain of human immunology research—encompassing immunotherapies, inflammatory diseases, and host-pathogen interactions—the ability to model the recruitment and activation of immune cells within a multi-organ context is paramount [10]. However, the complexity of these systems introduces significant challenges in ensuring that results are both reproducible within a single laboratory and robust across different experimental settings and research sites [96]. This guide objectively compares the performance of various OoC platforms and approaches, focusing on their demonstrated reproducibility and robustness in modeling human immunity, and provides the experimental data and methodologies supporting these assessments.
Comparative Analysis of Platform Performance
Data on the reproducibility and robustness of various OoC platforms are gathered from controlled inter-laboratory studies and published characterizations. The following tables summarize quantitative performance data and key robustness indicators for different systems.
Table 1: Quantitative Assessment of OoC Reproducibility in Inter-Laboratory Studies
| Organ Model / Platform | Key Metrics Measured | Result (Laboratory 1) | Result (Laboratory 2) | Variability | Source |
|---|---|---|---|---|---|
| Liver Acinus MPS (LAMPS) [96] | Basal Albumin Output (μg/day) | ~15 | ~14 | Low | [96] |
| Basal Urea Output (μg/day) | ~40 | ~38 | Low | [96] | |
| Terfenadine Metabolism (Clearance) | Maintained over 9 days | Maintained over 9 days | Low | [96] | |
| Response to Tolcapone (88 μM) | Consistent toxicity profile | Consistent toxicity profile | Low | [96] | |
| Multi-OoC (Gingiva-Skin) [97] | Glucose Uptake (across 3 experiments) | Stable consumption observed | Stable consumption observed | Low inter-experiment | [97] |
| Lactate Production (across 3 experiments) | Stable production observed | Stable production observed | Low inter-experiment | [97] | |
| LDH Release (across 3 experiments) | Stable low levels | Stable low levels | Low inter-experiment | [97] |
Table 2: Key Indicators of Experimental Robustness Across Platforms
| Platform / Study | Cell Sourcing Strategy | Culture Duration | Functional Endpoints Demonstrated | Immune Competence | Source |
|---|---|---|---|---|---|
| Liver Acinus MPS (LAMPS) | Primary Human Hepatocytes & iPSC-derived Hepatocytes | Up to 10 days | Albumin/Urea secretion, drug metabolism, toxicology | Incorporates Kupffer (macrophage) cell line | [96] |
| Immune-Tumor OoC (MIVO) | Primary human NK cells & neuroblastoma cell line | Sufficient for NK infiltration & killing | NK cell migration, extravasation, tumor cell apoptosis | Yes (Innate: NK cells) | [98] |
| Multi-OoC (HUMIMIC Chip3plus) | Reconstructed human gingiva & skin tissues | 72 hours | LC activation (CD1a, CD207, HLA-DR, CD86 mRNA) | Yes (Innate: MUTZ-3 derived Langerhans cells) | [97] |
| Alveolus Lung-Chip (Emulate) | Primary human airway cells & endothelial cells | Up to 2 weeks | Barrier function, cytokine release, pathogen response | Can incorporate primary immune cells (e.g., neutrophils) | [6] [10] |
| PhysioMimix Core (CN Bio) | Primary cells & iPSC-derived cells | Up to 4 weeks | CYP450 activity, albumin (liver), TEER (barrier), multi-organ PK/PD | Capable of integrating immune cells | [3] |
Detailed Experimental Protocols for Key Studies
To facilitate the replication of robust multi-OoC studies, particularly those incorporating immune responses, this section outlines the detailed experimental protocols from two foundational studies cited in the comparison tables.
Protocol 1: Reproducibility Assessment of a Liver Acinus Model (LAMPS)
This protocol is adapted from the inter-laboratory study that demonstrated high reproducibility for liver chip function and toxicology [96].
- 1. Cell Sourcing and Preparation:
- Hepatocytes: Use primary human hepatocytes (e.g., from ThermoFisher) or human induced pluripotent stem cell (iPSC)-derived hepatocytes (e.g., from FujiFilm-CDI). Thaw cells according to supplier instructions.
- Supporting Cells:
- Endothelial: Culture EA.hy926 cells in DMEM supplemented with 10% FBS.
- Kupffer (Macrophage): Differentiate THP-1 cells into adherent macrophages using 200 ng/mL PMA for 48 hours prior to seeding.
- Stellate: Culture LX-2 cells in DMEM with 2% FBS.
- 2. Device Seeding and Culture:
- Chip: Use a microfluidic platform (e.g., Nortis Bio SCC-001).
- Coating: Coat device chambers with a solution of 50 μg/mL fibronectin and 200 μg/mL collagen I in PBS for 1 hour at room temperature.
- Hepatocyte Seeding: Inject hepatocytes at a density of 2.75×10^6 cells/mL in appropriate hepatocyte plating media (HPM).
- Supporting Cell Seeding: After hepatocyte attachment, introduce the supporting cell types (endothelial, Kupffer, stellate) to their respective compartments to form the liver acinus structure.
- Maintenance: Culture chips under continuous, low-rate flow using a defined maintenance medium. Maintain in an incubator (37°C, 5% CO₂) for the duration of the experiment (up to 10 days).
- 3. Functional and Reproducibility Assessment:
- Basal Function: Daily collect effluent from the microfluidic circuit and quantify albumin and urea production using standard biochemical assays (e.g., ELISA). Monitor lactate dehydrogenase (LDH) release as a marker of cytotoxicity.
- Drug Metabolism: On specified days, introduce a model compound like Terfenadine (10 μM) into the system and measure its metabolic clearance from the medium.
- Toxicology Testing: Expose the system to known hepatotoxins (e.g., Tolcapone at 88 μM, Troglitazone at 150 μM) and a negative control (e.g., Caffeine at 600 μM). Monitor the same functional endpoints (albumin, urea, LDH) and specific markers of toxicity over time (e.g., 9-10 days).
Protocol 2: Investigating Systemic Immunotoxicity in a Multi-Organ Setting
This protocol is based on the study that connected reconstructed human gingiva (RHG) and skin (RHS) to model nickel-induced systemic immune activation [97].
- 1. Tissue Model and Immune Cell Preparation:
- Reconstructed Human Gingiva (RHG): Generate 3D gingiva models using primary human gingiva keratinocytes and fibroblasts cultured on a fibroblast-populated collagen hydrogel at the air-liquid interface.
- Reconstructed Human Skin with Langerhans Cells (RHS-LC): Generate 3D skin models analogously, integrating MUTZ-3-derived Langerhans cells (MUTZ-LC) into the epidermis prior to maturation.
- 2. Multi-Organ-on-Chip Assembly:
- Chip: Use a multi-organ bioreactor like the HUMIMIC Chip3plus (TissUse).
- Integration: Place the pre-formed RHG and RHS-LC tissues into separate compartments of the chip.
- Dynamic Culture: Connect the tissue compartments via microfluidic channels to establish a dynamic, recirculating flow of culture medium. Culture the system for 24 hours to achieve stable conditions before compound exposure.
- 3. Compound Exposure and Immune Readout:
- Dosing: Topically apply the test compound (e.g., Nickel Sulfate) to the RHG tissue for 24 hours.
- Post-Incubation: After exposure, replace the medium and continue dynamic culture for an additional 24 hours.
- System Stability Monitoring: Throughout the 72-hour experiment, monitor glucose uptake, lactate production, and LDH release in the circulating medium to ensure system health.
- Endpoint Analysis:
- Langerhans Cell Activation: Harvest the RHS-LC model. Separate the epidermis and dermis (hydrogel). Isolate migrated LC from the hydrogel and analyze the mRNA expression levels of activation/maturation markers (CD1a, CD207, HLA-DR, CD86) using qRT-PCR.
- Histology: Fix and section both RHG and RHS-LC tissues for histological analysis (e.g., H&E staining) to assess structural integrity.
- Cytokine Profiling: Analyze the circulating medium for inflammatory cytokines using a multiplex assay (e.g., Luminex).
Visualization of Experimental Workflows
The following diagrams illustrate the core experimental workflows and system architectures discussed in this guide, providing a logical map for experimental design.
Workflow for Assessing Multi-OoC Reproducibility
Architecture of an Immunocompetent Multi-Organ System
The Scientist's Toolkit: Essential Research Reagents and Materials
Success in establishing reproducible multi-OoC experiments relies on a standardized set of materials and reagents. The following table details key components for building and analyzing immunocompetent OoC models, as derived from the cited protocols.
Table 3: Key Reagents and Materials for Immunocompetent OoC Research
| Item Category | Specific Examples | Function / Application | Source / Reference |
|---|---|---|---|
| Microfluidic Platforms | Nortis Bio SCC-001; TissUse HUMIMIC Chip2/Chip3plus; Emulate Zoë-CM2/AVA; CN Bio PhysioMimix Core | Provides the physical scaffold and microfluidic control for 3D tissue culture and organ interconnection. | [96] [97] [6] |
| Cell Sources (Parenchymal) | Primary human hepatocytes (ThermoFisher); iPSC-derived hepatocytes (FujiFilm CDI); Primary keratinocytes/fibroblasts (from surgical waste) | Forms the core functional tissue of the organ model. Primary cells offer high fidelity, iPSCs offer reproducibility and patient specificity. | [96] [97] |
| Cell Sources (Immune) | THP-1 cell line (differentiated with PMA); MUTZ-3 derived Langerhans Cells (MUTZ-LC); Primary Natural Killer (NK) cells; Peripheral Blood Mononuclear Cells (PBMC) | Introduces immune competence to the model for studying inflammation, immunotherapy, and host-pathogen interactions. | [96] [97] [98] |
| Extracellular Matrix (ECM) | Collagen I; Fibronectin; Fibrin; Alginate-based hydrogels; Commercial basement membrane extracts (e.g., Matrigel) | Provides a 3D scaffold that supports cell growth, differentiation, and mimics the native tissue microenvironment. | [96] [98] [95] |
| Functional Assay Kits | Albumin ELISA Kit; Urea Assay Kit; Lactate Dehydrogenase (LDH) Cytotoxicity Assay Kit; Multiplex Cytokine Panel (e.g., Luminex) | Quantifies organ-specific function and assesses cellular health and inflammatory responses in effluent media. | [96] [97] |
| Analysis Reagents | RNA extraction kits; cDNA synthesis & qPCR kits; Antibodies for flow cytometry (e.g., CD16, CD1a, HLA-DR); Viability dyes (e.g., for live/dead staining) | Enables deep molecular and cellular profiling of tissues post-experiment (transcriptomics, phenotyping, viability). | [98] [97] [96] |
The data and protocols presented herein demonstrate that establishing reproducibility and robustness in multi-organ-on-chip systems is an achievable, though non-trivial, endeavor. Key factors for success include the use of standardized, well-characterized components (cells, matrices), platform stability under defined culture conditions, and the implementation of quantitative functional benchmarks. While innate immunity has been more readily incorporated, the integration of adaptive immune responses remains a frontier, complicated by challenges such as HLA-matching of cells [10]. As the field progresses with clearer standardization and the adoption of advanced engineering solutions—such as the AVA Emulation System for higher throughput [6] and PDMS-free chips like the Chip-R1 to reduce small molecule absorption [6]—the vision of immunocompetent multi-OoCs as reproducible, robust, and human-predictive tools for drug development and personalized medicine moves closer to realization.
Conclusion
The validation of multi-organ-on-a-chip systems that faithfully recapitulate human immunity marks a paradigm shift in preclinical research. By integrating foundational engineering principles with advanced biological models, these platforms offer an unprecedented ability to study systemic diseases, predict drug efficacy and toxicity, and personalize immunotherapy approaches in a human-relevant context. While challenges in scalability and long-term culture persist, the continuous evolution of this technology, supported by regulatory endorsement and robust validation studies, positions it as an indispensable tool for the future. The successful adoption of MOC systems promises to de-risk drug development pipelines, reduce reliance on animal models, and ultimately accelerate the delivery of safer, more effective therapies to patients, heralding a new era in biomedicine.
References
- 1. Microphysiological Systems as an Emerging In Vitro ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955625094966]
- 2. An eighteen-organ microphysiological system coupling a ... [https://www.nature.com/articles/s41378-025-00933-3]
- 3. PhysioMimix® Core Microphysiological System MPS [https://cn-bio.com/physiomimix-core/]
- 4. Organ on a chip Models | Single & Multi Organ Chip [https://cn-bio.com/organ-models/]
- 5. Application and development of Organ-on-a-Chip ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1643230/full]
- 6. Expanding the Frontiers of Human Biology with Organ-on-a ... [https://emulatebio.com/expanding-the-frontiers-of-human-biology-with-organ-on-a-chip-technology-highlights-from-the-2025-mps-world-summit/]
- 7. Human neural organoid microphysiological systems show ... [https://www.nature.com/articles/s42003-025-08632-5]
- 8. How Microphysiological System Works — In One Simple ... [https://www.linkedin.com/pulse/how-microphysiological-system-works-one-simple-gvmyc]
- 9. Human organs-on-chips for disease modelling, drug ... [https://www.nature.com/articles/s41576-022-00466-9]
- 10. In vitro immunity: an overview of immunocompetent organ- ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1373186/full]
- 11. Microfluidics‐based 3D cell culture models: Utility in novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5689508/]
- 12. Review of 3D cell culture with analysis in microfluidic systems [https://pubs.rsc.org/en/content/articlehtml/2019/ay/c9ay01328h]
- 13. Four Methods of 3D Cell Culture in Microfluidic Devices [https://eden-microfluidics.com/news-events/four-methods-for-3d-cell-culture-in-microfluidic-devices/]
- 14. Recent Advances of Biologically Inspired 3D Microfluidic ... [https://www.heraldopenaccess.us/openaccess/recent-advances-of-biologically-inspired-3d-microfluidic-hydrogel-cell-culture-systems]
- 15. A quantitative meta-analysis comparing cell models in ... [https://www.nature.com/articles/s41598-023-35043-5]
- 16. Recent advances of integrated microfluidic suspension cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9996741/]
- 17. Microphysiological system with integrated sensors to study ... [https://www.nature.com/articles/s41598-024-69693-w]
- 18. Human immunocompetent Organ-on-Chip platforms allow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8373379/]
- 19. Advances in engineering immune–tumor microenvironments ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560574/]
- 20. Tumor organoid-immune co-culture models: exploring a ... [https://www.nature.com/articles/s41420-025-02407-x]
- 21. Innovative organ-on-a-chip platforms for exploring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12269115/]
- 22. Emulate Organ-Chip Software [https://emulatebio.com/products/software/]
- 23. Enabling 3D High-Content Imaging on Organ-on-a-Chip ... [https://www.moleculardevices.com/lab-notes/cellular-imaging-systems/enabling-3d-high-content-imaging-and-analysis-on-organ-on-a-chip-platform]
- 24. Organ-on-a-chip pack [https://elveflow.com/microfluidics-application-packs/organ-on-a-chip-pack/]
- 25. Organ-on-a-Chip Models—New Possibilities in Experimental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11674024/]
- 26. an overview of immunocompetent organ-on-chip models [https://pubmed.ncbi.nlm.nih.gov/38835750/]
- 27. Shear stress in microfluidic devices [https://blog.darwin-microfluidics.com/shear-stress-in-microfluidic-devices/]
- 28. Integrating mechanical sensor readouts into organ-on-a- ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.1060895/full]
- 29. Organ-Chips for Immunology Research & Drug Development [https://emulatebio.com/inflammation-application/]
- 30. Top 4 Multi-Organ-on-a-Chip TissUse Assays and Why ... [https://www.innoserlaboratories.com/blog/tissuse-top-4-multi-organ-on-a-chip-assays-and-why-you-should-include-them-in-your-preclinical-research-in-2025/]
- 31. Simultaneous generation of chemical concentration and ... [https://pubs.rsc.org/en/content/articlelanding/2009/lc/b822006a]
- 32. Simultaneous generation of chemical concentration and ... [https://pubmed.ncbi.nlm.nih.gov/19606296/]
- 33. PBPK Modeling on Organs-on-Chips: An Overview of Recent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9046607/]
- 34. Personalised organs-on-chips: functional testing for precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6336148/]
- 35. Human Organs-on-Chips - Wyss Institute [https://wyss.harvard.edu/technology/human-organs-on-chips/]
- 36. An immune-competent lung-on-a-chip for modelling the ... [https://www.nature.com/articles/s41551-025-01491-9]
- 37. Trained immunity: induction of an inflammatory memory in ... [https://www.nature.com/articles/s41422-025-01171-y]
- 38. Organ-on-a-chip models for development of cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10700206/]
- 39. Human immunity in vitro — Solving immunogenicity and ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X13002974]
- 40. Evaluating Cancer Immunotherapy Safety with Organ-Chips [https://emulatebio.com/cancer-immunotherapy-pharmacology-organ-on-chips/]
- 41. current landscape and future prospects of CAR-T cell ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1652329/full]
- 42. CAR-T cell therapy: current limitations and potential ... [https://www.nature.com/articles/s41408-021-00459-7]
- 43. Multiorgan-on-a-Chip: A Systemic Approach To Model and ... [https://www.sciencedirect.com/science/article/pii/S0167779920303097]
- 44. Studying metabolism with multi-organ chips - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8889168/]
- 45. Multi-Organs-on-Chips: Towards Long-Term Biomedical ... [https://www.mdpi.com/1420-3049/24/4/675]
- 46. Prediction of pharmacokinetic/pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1578117/full]
- 47. Beyond animal testing: How human data trials are ... [https://pharmaphorum.com/rd/beyond-animal-testing-how-human-data-trials-are-reshaping-drug-development]
- 48. In Vitro Skin Models for Skin Sensitisation: Challenges and ... [https://www.mdpi.com/2079-9284/12/4/173]
- 49. Sensitization to nickel: etiology, epidemiology, immune ... [https://pubmed.ncbi.nlm.nih.gov/17243350/]
- 50. Immunological Mechanisms of Metal Allergies and the ... [https://www.mdpi.com/1660-4601/18/20/10867]
- 51. Alternative Methods for Skin-Sensitization Assessment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9783525/]
- 52. Artificial intelligence-, organoid-, and organ-on-chip-powered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615408/]
- 53. Multi-Organs-on-Chips for Testing Small-Molecule Drugs [https://pmc.ncbi.nlm.nih.gov/articles/PMC8540732/]
- 54. Organoids and organs-on-chips: Recent advances ... [https://www.sciencedirect.com/science/article/abs/pii/S2666634025000947]
- 55. Patient-Derived Cell Models for Personalized Medicine Approaches in Cystic Fibrosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9992303/]
- 56. Primary Patient-Derived Cancer Cells and Their Potential for Personalized Cancer Patient Care - PubMed [https://pubmed.ncbi.nlm.nih.gov/29241554/]
- 57. Preclinical target validation using patient-derived cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/25722227/]
- 58. Organoids VS Organ-on-a-chip: A Comparative Review ... [https://elveflow.com/microfluidic-reviews/organoids-vs-organ-on-a-chip/]
- 59. Hesperos Demonstrates First Digital Twin of Human ... [https://hesperosinc.com/digital-twin-malaria-on-a-chip-publication/]
- 60. DRIVe | ImmuneChip+ | Advancing multi-organ tissue chips [https://drive.hhs.gov/immunechip.html]
- 61. Immune evasion in cancer: mechanisms and cutting-edge ... [https://www.nature.com/articles/s41392-025-02280-1]
- 62. Advances of dual-organ and multi-organ systems for gut, lung ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc01011f]
- 63. Developments and Applications of Liver-on-a-Chip ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189686/]
- 64. A Comprehensive Review of Organ-on-a-Chip Technology ... [https://www.mdpi.com/2079-6374/14/5/225]
- 65. State-of-the-art in high throughput organ-on-chip for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12149869/]
- 66. High Throughput Screening Market Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/high-throughput-screening-market]
- 67. Advances in engineering immune–tumor microenvironments ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02479-4]
- 68. High Throughput Screening (HTS) Market Size 2025-2029 [https://www.technavio.com/report/high-throughput-screening-market-industry-analysis]
- 69. Top High-throughput Screening Technology Companies & ... [https://www.linkedin.com/pulse/top-high-throughput-screening-technology-companies-fxoqf/]
- 70. Integration of immune cells in organs-on-chips: a tutorial - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10267470/]
- 71. The potential of multi-organ-on-chip models for ... [https://www.sciencedirect.com/science/article/pii/S2468202021000188]
- 72. A Portable and Reconfigurable Multi-Organ Platform for Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5177565/]
- 73. Multi-omics microsampling for the profiling of lifestyle-associated changes in health | Nature Biomedical Engineering [https://www.nature.com/articles/s41551-022-00999-8]
- 74. Frontiers | High Throughput Multi-Omics Approaches for Clinical Trial Evaluation and Drug Discovery [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.590742/full]
- 75. Algorithms and tools for data-driven omics integration to achieve multilayer biological insights: a narrative review | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06446-x]
- 76. Lab on chip for medical and clinical applications [https://pubs.rsc.org/en/content/articlehtml/2025/sd/d5sd00096c]
- 77. CRO Agency Comparison: In-House vs. Expert Partners [https://www.arcticleaf.com/blog/learning-center/cro-agency-comparison-inhouse-vs-expert-partners/]
- 78. Organs On Chips Market Size, Share | Industry Report [2032] [https://www.fortunebusinessinsights.com/organs-on-chips-market-114512]
- 79. Multicenter validation of a scalable, interpretable, multitask ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485121/]
- 80. Human organoids-on-chips for biomedical research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10758054/]
- 81. Science in 3D: How organoids and organs-on-chips can ... [https://www.jax.org/news-and-insights/2025/september/science-in-3d-how-organoids-and-organs-on-chips-can-help-scientists-study-host-immune-microbiome-interactions]
- 82. Developing immunocompetent human organ-on-a-chip ... - NWO [https://www.nwo.nl/en/projects/nwa129219019]
- 83. Lab-Grown Human Immune System Model Uncovers ... [https://news.gatech.edu/news/2024/11/12/lab-grown-human-immune-system-model-uncovers-weakened-response-cancer-patients]
- 84. Organoids-on-a-chip: microfluidic technology enables ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1515340/full]
- 85. A 3D-printed multi-compartment organ-on-chip platform with a ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc00489b]
- 86. Advances in organoid-on-a-chip for recapitulation ... [https://www.sciencedirect.com/science/article/abs/pii/S1369702125000355]
- 87. The FDA Modernization Act 2.0 - What does it mean? [https://cn-bio.com/us-fda-modernization-act-2-what-does-it-mean/]
- 88. A Recent Timeline of U.S. Actions to Reduce and Replace ... [https://emulatebio.com/alternatives-to-animal-testing-in-drug-development/]
- 89. FDA Modernization Act 2.0: transitioning beyond animal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10617761/]
- 90. FDA NAMs Roadmap: Economic and Scientific Impact ... [https://www.4dcell.com/post/fdanamsroadmap]
- 91. First FDA IND Milestone Achieved Using Human ... [https://www.fiercebiotech.com/sponsored/first-fda-ind-milestone-achieved-using-human-vascularized-organoid-efficacy-data]
- 92. Comprehensive metabolomics study identifies SN-38 ... [https://www.nature.com/articles/s41598-025-01753-1]
- 93. Comparison of Metabolomic Profiles of Organs in Mice of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7345432/]
- 94. Elucidating organ-specific metabolic toxicity chemistry from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4364445/]
- 95. State-of-the-Art Organ-on-Chip Models and Designs for ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383757/]
- 96. Analysis of Reproducibility and Robustness of a Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7785655/]
- 97. A Multi-Organ-on-Chip Approach to Investigate How Oral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8915798/]
- 98. A multi-organ-on-chip to recapitulate the infiltration and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.945149/full]